PIASKY- crovalimab injection, solution
Piasky by
Drug Labeling and Warnings
Piasky by is a Prescription medication manufactured, distributed, or labeled by Genentech, Inc., Roche Diagnostics GmbH, F. Hoffmann-La Roche Ltd. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PIASKY safely and effectively. See full prescribing information for PIASKY.
PIASKY (crovalimab-akkz) injection, for intravenous or subcutaneous use
Initial U.S. Approval: 2024WARNING: SERIOUS MENINGOCOCCAL INFECTIONS
See full prescribing information for complete boxed warning.
PIASKY increases the risk of serious and life-threatening infections caused by Neisseria meningitidis.
- Complete or update meningococcal vaccination at least 2 weeks prior to the first dose of PIASKY, unless the risks of delaying PIASKY outweigh the risks of developing a serious infection. Comply with the most current Advisory Committee on Immunization Practices (ACIP) recommendations for meningococcal vaccination in patients receiving a complement inhibitor (5.1).
- Patients receiving PIASKY are at increased risk for invasive disease caused by N. meningitidis, even if they develop antibodies following vaccination. Monitor patients for early signs of meningococcal infections and evaluate immediately if infection is suspected (5.1).
PIASKY is available only through a restricted program called the PIASKY REMS (5.2)
INDICATIONS AND USAGE
PIASKY is a complement C5 inhibitor indicated for the treatment of adult and pediatric patients 13 years and older with paroxysmal nocturnal hemoglobinuria (PNH) and body weight of at least 40 kg (1)
DOSAGE AND ADMINISTRATION
See Full Prescribing Information for instructions on preparation, dosage, and administration. (2.2, 2.3, 2.4, 2.5)
Start with one loading dose administered by intravenous infusion, followed by 4 additional loading doses administered by subcutaneous injection. Then administer a maintenance dose every 4 weeks by subcutaneous injection.
For patients switching from another complement inhibitor, the first loading dose of PIASKY should be administered no sooner than the time of the next scheduled complement inhibitor administration. See Full Prescribing Information for considerations when switching from another C5 inhibitor.
Administer doses based on the patient's actual body weight (2.2)
DOSAGE FORMS AND STRENGTHS
Injection: 340 mg/2 mL (170 mg/mL) in a single-dose vial (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Type III hypersensitivity reactions: Monitor patients switching from another C5 inhibitor to PIASKY or from PIASKY to another C5 inhibitor as they are at risk of Type III hypersensitivity reactions related to the formation of drug-target-drug complexes (5.3)
- Other Infections: PIASKY can increase susceptibility to serious infections especially those caused by encapsulated bacteria. (5.4)
- Infusion- and Injection-Related Reactions: Monitor for these reactions and initiate medical management as needed (5.5)
ADVERSE REACTIONS
The most common adverse drug reactions (incidence ≥10%) were infusion-related reaction, respiratory tract infection, viral infection, and Type III hypersensitivity reactions. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Genentech at 1-888-835-2555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: SERIOUS MENINGOCOCCAL INFECTIONS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Vaccination and Prophylaxis for Meningococcal Infection
2.2 Recommended Dosage Regimen
2.3 Recommended Timing for Switching to PIASKY from Another C5 Inhibitor
2.4 Delayed or Missed Dose
2.5 Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Serious Meningococcal Infection
5.2 PIASKY REMS
5.3 Type III Hypersensitivity Reactions Related to Drug-Target-Drug Complexes
5.4 Other Infections
5.5 Infusion- and Injection-Related Reactions
5.6 Monitoring PNH Manifestations after Discontinuation of PIASKY
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
7. DRUG INTERACTIONS
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.6 Immunogenicity
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14. CLINICAL STUDIES
14.1 Paroxysmal Nocturnal Hemoglobinuria
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SERIOUS MENINGOCOCCAL INFECTIONS
PIASKY, a complement inhibitor, increases the risk of serious infections caused by Neisseria meningitidis [see Warnings and Precautions (5.1)]. Life-threatening and fatal meningococcal infections have occurred in patients treated with complement inhibitors. These infections may become rapidly life-threatening or fatal if not recognized and treated early.
- Complete or update vaccination for meningococcal bacteria (for serogroups A, C, W, Y, and B) at least 2 weeks prior to the first dose of PIASKY, unless the risks of delaying therapy with PIASKY outweigh the risk of developing a serious infection. Comply with the most current Advisory Committee on Immunization Practices (ACIP) recommendations for meningococcal vaccination in patients receiving a complement inhibitor. See Warnings and Precautions (5.1) for additional guidance on the management of the risk of serious infections caused by meningococcal bacteria.
- Patients receiving PIASKY are at increased risk for invasive disease caused by N. meningitidis, even if they develop antibodies following vaccination. Monitor patients for early signs of serious meningococcal infections and evaluate immediately if infection is suspected.
Because of the risk of serious meningococcal infections, PIASKY is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called PIASKY REMS [see Warnings and Precautions (5.2)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Vaccination and Prophylaxis for Meningococcal Infection
Vaccinate patients for meningococcal infection (serogroups A, C, W, Y and B) according to current ACIP recommendations at least 2 weeks prior to initiation of PIASKY [see Warnings and Precautions (5.1)].
If urgent PIASKY therapy is indicated in a patient who is not up to date with meningococcal vaccines according to ACIP recommendations, provide the patient with antibacterial drug prophylaxis and administer these vaccines as soon as possible.
Healthcare providers who prescribe PIASKY must enroll in the PIASKY REMS [see Warnings and Precautions (5.2)].
2.2 Recommended Dosage Regimen
The recommended dosage regimen consists of one loading dose administered by intravenous (IV) infusion (on Day 1), followed by four additional weekly loading doses administered by subcutaneous (SUBQ) injection (on Days 2, 8, 15, and 22). The maintenance dose starts on Day 29 and is then administered every 4 weeks by subcutaneous injection. Administer doses based on the patient's actual body weight, as shown in Table 1.
Table 1 PIASKY Dosage Regimen Based on Body Weight Body Weight ≥ 40 kg to < 100 kg ≥ 100 kg IV = intravenous, SUBQ = subcutaneous - * Q4W=every 4 weeks
Loading Dose
Day 1
Day 2, 8, 15, 22
1,000 mg (IV)
340 mg (SUBQ)
1,500 mg (IV)
340 mg (SUBQ)Maintenance Dose
Day 29 and Q4W* thereafter
680 mg (SUBQ)
1,020 mg (SUBQ)The dosing schedule is allowed to occasionally vary within 2 days of the scheduled administration day (except at Day 1 and Day 2). If this occurs, the subsequent dose should be administered according to the regular schedule.
Modification of the maintenance dose is required if the patient's body weight changes to become consistently greater than or lower than 100 kg during the course of therapy.
2.3 Recommended Timing for Switching to PIASKY from Another C5 Inhibitor
Healthcare providers should consider the benefits of the timing of switching C5 inhibitors vs. the risks of Type III hypersensitivity reactions [see Warnings and Precautions (5.3)]. For patients switching from another C5 inhibitor (e.g., eculizumab or ravulizumab), the first intravenous loading dose of PIASKY should be administered no sooner than the time of the next scheduled complement inhibitor administration. The administration of the additional subcutaneous loading doses and maintenance doses of PIASKY should follow as per the schedule shown in Table 1.
2.4 Delayed or Missed Dose
If an entire planned dose or part of a planned dose of PIASKY is missed, administer the missed dose or remainder of the missed dose as soon as possible before the day of the next scheduled dose. Then administer the next dose on the regularly scheduled dosing day. Do not administer two doses or more than the prescribed dose on the same day to make up for a missed dose.
2.5 Preparation and Administration
Each vial of PIASKY is for one-time use in only one patient.
PIASKY is administered as an intravenous infusion (first dose) and as a subcutaneous injection (subsequent doses). Only healthcare providers should administer PIASKY.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. PIASKY is clear to opalescent, and an almost colorless to brownish-yellow solution. PIASKY should be discarded if the medicine looks cloudy, discolored, or has particles in it.
Preparation of Intravenous Infusion
- Use aseptic technique to prepare PIASKY for intravenous administration. PIASKY must be diluted and administered as an intravenous infusion over 60 minutes ± 10 minutes (1,000 mg) or 90 minutes ± 10 minutes (1,500 mg).
- PIASKY solution must be diluted in 0.9% Sodium Chloride Injection prior to administration. A 0.2 micron in-line filter must be used with the infusion set during administration. A dedicated infusion line must be used during intravenous administration.
- Only dilute PIASKY in 0.9% Sodium Chloride Injection.
Dilution of Intravenous Infusion
- Withdraw the required volume of PIASKY from the vial (see Table 2) using a sterile syringe and dilute into the infusion bag. Use multiple vials to meet the required volume of PIASKY to be added to the infusion bag. Discard any unused portion left in the vial.
Dilution of PIASKY in infusion bags containing 0.9% Sodium Chloride Injection must be in the range of 4-15 mg/mL (final concentration after dilution) (see Table 2).
Intravenous infusion bags of a volume of 100 mL or 250 mL can be used.
Table 2 Dose Example Volume Determination Dose
(mg)Volume of Piasky
(mL)Size of 0.9% Sodium Chloride Injection Bag (mL) Concentration in Bag
(mg/mL)1,000 5.9 250 4 1,500 8.8 250 6 1,000 5.9 100 10 1,500 8.8 100 15 - Gently mix the infusion bag by slowly inverting the bag. Do not shake.
- Inspect the infusion bag for particles and discard if present.
- Flushing of infusion line is required to ensure complete administration of the entire dose.
Storage of Diluted Solution for Infusion
The diluted solution for intravenous infusion should be used immediately because PIASKY does not contain any antimicrobial preservative. If immediate use is not possible, see Table 3 for detailed storage conditions of the prepared solution for infusion, which depends on the type of infusion bags used.
Table 3 Storage Conditions for the Prepared Solution for Infusion Infusion bags Storage conditions polyolefins (PO), polyethylene (PE), polypropylene (PP), polyvinyl chloride (PVC) PO/PE/PP Refrigerate at 2°C to 8°C (36°F to 46°F) for up to 64 hours protected from light, and store at room temperature up to 30°C (86°F) for up to 6 hours including infusion time under ambient light conditions. Protect from direct sunlight. PVC Refrigerate at 2°C to 8°C (36°F to 46°F) for up to 12 hours protected from light, and store at room temperature up to 30°C (86°F) for up to 6 hours including infusion time under ambient light conditions. Protect from direct sunlight. No incompatibilities have been observed between PIASKY and intravenous infusion bags with product-contacting materials made of polyvinyl chloride, or polyolefins such as polyethylene and polypropylene. In addition, no incompatibilities have been observed with infusion sets or infusion aids with product-contacting materials made of polyvinyl chloride, polyethylene, polyurethane, polybutadiene, acrylonitrile butadiene styrene, polycarbonate, or polytetrafluorethylene.
The infusion of PIASKY may be slowed or interrupted if the patient develops an infusion-related reaction. The infusion should be discontinued immediately if the patient experiences a serious hypersensitivity reaction [see Warnings and Precautions (5.5)].
Preparation of the Subcutaneous Injection
For subcutaneous injection, PIASKY must be used undiluted.
- Remove the vial cap and clean the vial rubber stopper.
- Attach the transfer needle on the syringe.
- Withdraw all the medicine from the vial.
- Remove air bubbles if any.
- Remove the transfer needle from the vial.
- Recap the transfer needle using a one-handed scoop technique.
- Detach the transfer needle.
- Attach the injection needle on the syringe.
- Clean the injection site with an alcohol pad and let air dry.
- Inject the medicine subcutaneously.
If the dose requires multiple injections, perform a new injection using a new PIASKY vial.
A syringe, a transfer needle and an injection needle are needed to withdraw PIASKY solution from the vial and inject it subcutaneously.
-
- A 2 mL or 3 mL syringe fulfilling the following criteria are recommended: Transparent polypropylene or polycarbonate syringe with Luer-Lock tip (if not available, a syringe with Luer Slip tip can be used), sterile, single-use, latex-free and non-pyrogenic, and commercially available in the US.
- A transfer needle without a filter fulfilling the following criteria may be used: Stainless steel, sterile, preferably gauge 18 G with single bevel at approximately 45 degrees to reduce risk of needle stick injury (or gauge 21 G standard needle as an alternative), single-use, latex-free and non-pyrogenic, and commercially available in the US.
- An injection needle fulfilling the following criteria may be used: Hypodermic needle, stainless steel, sterile, gauge 25 G, 26 G or 27 G, length 3/8'' to 1/2'', single-use, latex-free and non-pyrogenic, preferably including safety needle shield, and commercially available in the US.
- Each injection is a volume of 2 mL PIASKY, corresponding to 340 mg. A 2 mL-size or 3 mL-size syringe should be used for each injection. A dose of 680 mg is achieved by performing two consecutive subcutaneous injections of 340 mg. A dose of 1020 mg is achieved by performing three consecutive subcutaneous injections of 340 mg.
- Inject PIASKY subcutaneously in the abdomen region and rotate abdominal injection sites with every injection. Consecutive injections must be at least 2 inches apart. No data are available on injection at other sites of the body. Injections should never be given into moles, scars, or areas where the skin is tender, bruised, red, hard, or not intact.
Storage of Solution for Injection
Once transferred from the vial to the syringe, PIASKY should be injected immediately because PIASKY does not contain any antimicrobial-preservative. If immediate use is not possible, the capped syringe can be refrigerated at 2°C to 8°C (36°F to 46°F) for up to 64 hours protected from light and stored at room temperature up to 30°C (86°F) for up to 5 hours under ambient light conditions.
Protect from direct sunlight.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
PIASKY is contraindicated:
- For initiation in patients with an unresolved serious Neisseria meningitidis infection [see Warnings and Precautions (5.1)].
- In patients with a known serious hypersensitivity reaction to crovalimab or any of the excipients [see Warnings and Precautions (5.5)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Serious Meningococcal Infection
PIASKY, a complement inhibitor, increases a patient's susceptibility to serious, life-threatening, or fatal infections caused by meningococcal bacteria (meningococcemia and/or meningitis) in any serogroup, including non-groupable strains. Life-threatening and fatal meningococcal infections have occurred in both vaccinated and unvaccinated patients treated with complement inhibitors. The initiation of PIASKY is contraindicated in patients with a serious unresolved Neisseria meningitidis infection.
Complete or update meningococcal vaccination (for serogroups A, C, W, Y, and B) at least 2 weeks prior to administration of the first dose of PIASKY, according to the current Advisory Committee on Immunization Practices (ACIP) recommendations for patients receiving a complement inhibitor. Revaccinate patients in accordance with ACIP recommendations considering the duration of PIASKY therapy.
Note that ACIP recommends an administration schedule in patients receiving complement inhibitors that differs from the administration schedule in the vaccine prescribing information.
If urgent PIASKY therapy is indicated in a patient who is not up to date with meningococcal vaccines according to ACIP recommendations, provide the patient with antibacterial drug prophylaxis and administer meningococcal vaccines as soon as possible. Various durations and regimens of antibacterial drug prophylaxis have been considered, but the optimal durations and drug regimens for prophylaxis and their efficacy have not been studied in unvaccinated or vaccinated patients receiving complement inhibitors, including PIASKY. The benefits and risks of treatment with PIASKY, as well as the benefits and risks of antibacterial drug prophylaxis in unvaccinated or vaccinated patients, must be considered against the known risks for serious infections caused by N. meningitidis.
Vaccination does not eliminate the risk of meningococcal infections, despite development of antibodies following vaccination.
Closely monitor patients for early signs and symptoms of meningococcal infection and evaluate patients immediately if infection is suspected. Inform patients of these signs and symptoms and instruct patients to seek immediate medical care if these signs and symptoms occur. Promptly treat known infections. Meningococcal infection may become rapidly life-threatening or fatal if not recognized and treated early. Consider interruption of PIASKY in patients who are undergoing treatment for serious meningococcal infection.
PIASKY is available only through a restricted program under a REMS [see Warnings and Precautions (5.2)].
5.2 PIASKY REMS
PIASKY is available only through a restricted program under a REMS called PIASKY REMS, because of the risk of serious meningococcal infections [see Warnings and Precautions (5.1)].
Notable requirements of the PIASKY REMS include the following:
- Prescribers must enroll in the REMS.
- Prescribers must counsel patients about the risk of serious meningococcal infection.
- Prescribers must provide the patients with the REMS educational materials.
- Prescribers must assess patient vaccination status for meningococcal vaccines (against serogroups A, C, W, Y, and B) and vaccinate if needed according to current ACIP recommendations two weeks prior to the first dose of PIASKY.
- Prescribers must provide a prescription for antibacterial drug prophylaxis if treatment must be started urgently, and the patient is not up to date with both meningococcal vaccines according to current ACIP recommendations at least two weeks prior to the first dose of PIASKY.
- Healthcare settings and pharmacies that dispense PIASKY must be certified in the REMS and must verify prescribers are certified.
- Patients must receive counseling from the prescriber about the need to receive meningococcal vaccines per ACIP recommendations, the need to take antibiotics as directed by the prescriber, and the signs and symptoms of meningococcal infection.
- Patients must be instructed to carry the Patient Safety Card with them at all times during and for 11 months following treatment with PIASKY.
Further information is available at www.PIASKYREMS.com or 1-866-4My-Skyy (469-7599).
5.3 Type III Hypersensitivity Reactions Related to Drug-Target-Drug Complexes
Patients who are switching from another C5 inhibitor (e.g., eculizumab or ravulizumab) to PIASKY or from PIASKY to another C5 inhibitor are at risk of serious Type III hypersensitivity reactions related to the formation of drug-target-drug-complexes (DTDCs), because PIASKY and these other C5 inhibitors bind different epitopes of C5 [see Drug Interactions (7)].
In clinical trials, Type III hypersensitivity reactions were reported in 39 of 201 patients (19%) who switched from eculizumab or ravulizumab to PIASKY. Four of these patients (10%) had not fully recovered from symptoms of Type III hypersensitivity reactions at the time of their last follow up visit. In addition, Type III hypersensitivity reactions were reported in 2 of 8 patients (25%) who switched from PIASKY to eculizumab or ravulizumab, including one patient who developed Grade 3 axonal neuropathy [see Adverse Reactions (6)].
Symptoms of Type III hypersensitivity reactions that occurred in more than 2 patients were arthralgia, rash, pyrexia, myalgia, headache, fatigue, petechiae and abdominal pain. Among patients who experienced Type III hypersensitivity reactions, 8 (21%) had events that were considered serious due to hospitalization. Symptoms of serious Type III hypersensitivity reactions included pyrexia and arthralgia. Type III hypersensitivity reactions can also cause renal abnormalities.
Healthcare providers should consider the benefits of the timing of switching C5 inhibitors vs. the risks of Type III hypersensitivity reactions. Patients are expected to no longer be at risk of Type III hypersensitivity reactions if the prior C5 inhibitor has been cleared from the body prior to starting PIASKY or if PIASKY has been cleared from the body prior to starting another C5 inhibitor. Therefore, initiating PIASKY sooner than 5.5 half-lives from the last dose of a C5 inhibitor (e.g., eculizumab or ravulizumab) or initiating a C5 inhibitor (e.g., eculizumab or ravulizumab) sooner than 5.5 half-lives from the last dose of PIASKY increases the risk of Type III hypersensitivity reactions.
Based on time-to-onset of Type III hypersensitivity reactions observed in clinical trials, patients should be monitored for the first 30 days of the new therapy for the occurrence of symptoms of Type III hypersensitivity reactions. For mild or moderate Type III hypersensitivity reactions, administer symptomatic treatment, such as topical corticosteroids, antihistamines, antipyretics, and/or analgesics. For severe reactions, initiate and taper oral or systemic corticosteroid therapy as clinically indicated.
5.4 Other Infections
Due to its mechanism of action, PIASKY may increase susceptibility to infections, especially with encapsulated bacteria, such as infections with Neisseria spp. but also Streptococcus pneumoniae, Haemophilus influenzae, and to a lesser extent, Neisseria gonorrhoeae. Children treated with PIASKY may be at increased risk of developing serious infections due to Streptococcus pneumoniae and Haemophilus influenzae type b (Hib). Vaccinate patients against Streptococcus pneumoniae and Haemophilus influenzae type b (Hib) infections according to ACIP recommendations.
If PIASKY is administered to patients with active systemic infections, monitor closely for signs and symptoms of worsening infection. If the patient's infection worsens, consider whether to discontinue PIASKY.
5.5 Infusion- and Injection-Related Reactions
Administration of PIASKY may cause infusion-related reactions or systemic injection-related reactions, depending on the route of administration [see Adverse Reactions (6)]. These may include hypersensitivity reactions (including anaphylaxis) but also a range of other symptoms such as injection site pain, erythema, headache or myalgia. One patient experienced a serious infusion-related reaction that resolved 4 days after interruption of infusion with PIASKY. Instruct patients/caregivers to seek immediate medical attention if the patient develops symptoms of a serious hypersensitivity reaction and to report this reaction to their healthcare provider.
If a serious hypersensitivity reaction (including anaphylaxis) occurs, discontinue PIASKY treatment immediately, institute appropriate treatment, per standard of care, and monitor until signs and symptoms are resolved. PIASKY is contraindicated in patients with a known serious hypersensitivity reaction to crovalimab or any of the excipients.
5.6 Monitoring PNH Manifestations after Discontinuation of PIASKY
In case of PIASKY discontinuation, patients who do not switch to another treatment for PNH, must be closely monitored for at least 20 weeks for signs and symptoms of serious hemolysis, identified by elevated lactate dehydrogenase (LDH) levels, along with a sudden decrease in hemoglobin, or re-appearance of symptoms such as fatigue, hemoglobinuria, abdominal pain, dyspnea, major adverse vascular events (including thrombosis), dysphagia, erectile dysfunction or renal impairment.
If signs and symptoms of hemolysis occur after discontinuation of PIASKY, consider restarting treatment with PIASKY, if appropriate, or initiating another treatment for PNH.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are discussed in greater detail in other sections of the label:
- Serious Meningococcal Infection [see Warnings and Precautions (5.1)]
- Type III Hypersensitivity Reactions Related to Drug-Target-Drug Complexes [see Warnings and Precautions (5.3)]
- Other Infections [see Warnings and Precautions (5.4)]
- Infusion- and Injection-Related Reactions [see Warnings and Precautions (5.5)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Patients Who are Complement Inhibitor-Naïve
The data described below reflect exposure of 204 patients with PNH who were complement inhibitor-naïve and who were randomized in COMMODORE 2 to receive PIASKY (n = 135) or eculizumab (n = 69) at the recommended dosing regimen for 24 weeks [see Clinical Studies (14)].
Serious adverse reactions occurred in 6% of patients receiving PIASKY in the COMMODORE 2 study, including epistaxis and pneumonia, which occurred in 2 patients each, and infusion related reaction, pyelonephritis, COVID-19, and hypovolemic shock which were reported in 1 patient each.
Table 4 lists adverse reactions that occurred at a rate of 5% or more among patients randomized to PIASKY treatment for 24 weeks in the COMMODORE 2 study. The most common adverse reactions (≥10%) in patients treated with PIASKY were infusion related reaction, respiratory tract infection, and viral infection.
Table 4 Adverse Reactions Reported In 5% or More of Complement-Inhibitor Naïve Patients with PNH Randomized to PIASKY in COMMODORE 2 Adverse reactions PIASKY
(N = 135)
%ECULIZUMAB
(N = 69)
%- * Grouped terms.
Diarrhea includes diarrhea and diarrhea infectious.
Headache includes headache and migraine.
Injection-related reaction includes injection related reaction and injection site reaction.
Respiratory tract infection includes nasopharyngitis, pharyngitis, rhinitis, rhinitis allergic, upper respiratory tract infection and pneumonia.
Viral infection includes viral infection, COVID-19, influenza, herpes virus infection and oral herpes.- † Injection-related reactions are only expected to occur in the PIASKY arm as eculizumab is not given by subcutaneous injection
Infusion-related reaction 16 13 Respiratory tract infection* 13 20 Viral infection* 11 7 Hyperuricemia 8 9 Headache* 8 6 Diarrhea* 7 1 Injection-related reaction† 6 0 Patients Previously Treated with a Complement C5 Inhibitor
The data described below reflect exposure of 86 patients with PNH who received PIASKY (n=44) or eculizumab (n=42) at the recommended dosing regimen for 24 weeks in COMMODORE 1, an open-label, active-controlled, multicenter study conducted in patients switching from eculizumab. The median age was 47 years (range: 21 to 85); 52% were female, and race included White (73%), Asian (19%), unknown (5%), and Black/African-American (3%). The population ethnicities were 17% Hispanic or Latino and 76% not Hispanic or Latino.
Serious adverse reactions in COMMODORE 1 were reported in 3 patients (7%) with PNH receiving PIASKY. Serious adverse reactions included pneumonia, nasopharyngitis, and urinary tract infection, which occurred in 1 patient each.
Table 5 lists adverse reactions that occurred at a rate of 5% or more among patients randomized to PIASKY treatment for 24 weeks in the COMMODORE 1 study. The most common adverse reactions (≥10%) in patients treated with PIASKY were viral infections, respiratory tract infection, Type III hypersensitivity reaction, infusion-related reaction, peripheral edema, and headache.
Table 5 Adverse Reactions Reported In 5% or More of Complement-Inhibitor Treated Patients with PNH Randomized to PIASKY in COMMODORE 1 Adverse reactions PIASKY
(N = 44)
%ECULIZUMAB
(N = 42)
%- * Grouped terms
Fatigue includes fatigue, malaise and asthenia.
Injection-related reaction includes injection related reaction and injection site reaction.
Rash includes rash and skin exfoliation.
Peripheral edema includes edema peripheral and peripheral swelling.
Respiratory tract infection includes respiratory tract infection, nasopharyngitis, pneumonia and upper respiratory tract infection.
Viral infection includes viral infection, influenza, COVID-19, and respiratory syncytial virus infection- † Type III immune complex mediated reaction is only expected to occur in the PIASKY arm as patients in the eculizumab arm did not change C5 inhibitor treatment
- ‡ Infusion-related reactions are not expected to occur in the eculizumab arm as these patients tolerated eculizumab prior to study initiation
- § Injection-related reactions are only expected to occur in the PIASKY arm as eculizumab is not given by subcutaneous injection
Viral infection* 23 21 Respiratory tract infection* 18 5 Type III hypersensitivity reaction† 16 0 Infusion-related reaction‡ 14 0 Peripheral edema* 11 2 Headache 11 2 Injection-related reaction§ 9 0 Fatigue* 9 12 Rash* 9 0 Diarrhea 7 2 Nausea 7 5 Arthralgia 7 0 Type III Hypersensitivity Reactions Related to Drug-Target-Drug Complexes [see Warnings and Precautions (5.3), and Drug Interactions (7)].
Across the COMMODORE 1 and 2 studies, 39 out of 201 (19.4%) patients who switched from eculizumab or ravulizumab to PIASKY experienced a Type III hypersensitivity reaction (reported as Type III immune complex mediated reaction). A total of 6 patients had switched two times and of the 6 patients, 2 patients experienced a second episode of Type III hypersensitivity reaction after discontinuing PIASKY and switching to ravulizumab. One of these patients developed Grade 3 axonal neuropathy and a Type III hypersensitivity reaction could not be excluded and the other developed Grade 2 arthralgia and myalgia. These two events remained unresolved at the last follow up visit of the clinical studies (the duration of the events until last follow-up was 313 days for the event of Grade 3 axonal neuropathy and 142 days for the event of Grade 2 arthralgia and myalgia, respectively). Two additional patients who experienced Grade 3 rash and Grade 3 arthralgia, respectively, had unresolved Type III hypersensitivity reaction at the last follow-up visit.
The median time to onset of Type III hypersensitivity reaction in patients who switched treatment from eculizumab or ravulizumab to PIASKY was 1.6 weeks (range: 0.7 – 4.4 weeks) and the median duration of Type III hypersensitivity reactions was 1.9 weeks (range 0.4 – 34.1 weeks). The majority of events were Grade 1-2. Grade 3 Type III hypersensitivity reaction occurred in 8% of patients who switched from eculizumab or ravulizumab to PIASKY. Out of 42 Type III hypersensitivity reactions, 37 (88%) resolved, including 1 (2.4%) that resolved with PIASKY discontinuation, 2 (4.8%) that resolved with PIASKY interruption and 34 (81%) that resolved without discontinuation, interruption, or dose change in PIASKY therapy.
Axonal Neuropathy
In COMMODORE 1 and 2, Grade 3 distal axonal demyelinating polyneuropathy and Grade 3 axonal neuropathy were reported, each in 1 patient who switched from another C5 inhibitor to PIASKY or from PIASKY to another C5 inhibitor. The Grade 3 distal axonal demyelinating polyneuropathy occurred 11 weeks after a patient switched from eculizumab to PIASKY (with first dose of PIASKY received 12 days after the last dose of eculizumab treatment) and was preceded by a bacterial respiratory tract infection. The Grade 3 axonal neuropathy occurred in a patient who had switched to ravulizumab treatment after 6 weeks of treatment with PIASKY, and previously received ravulizumab treatment prior to switching to treatment with PIASKY [see Warnings and Precautions (5.3)]. Events associated with the axonal neuropathy included COVID-19, sepsis and administration of a fluoroquinolone. In both cases of axonal neuropathy, a Type III hypersensitivity reaction as a cause of, or contributor to, the axonal neuropathy could not be excluded. Both cases of axonal neuropathy remained unresolved at the last follow up visit of the clinical studies.
Pediatric Population with PNH Treated with PIASKY
Twelve pediatric patients with PNH (9 treatment-naïve patients and 3 patients who switched from another C5 inhibitor) were treated with PIASKY in COMMODORE 1 (n=2), COMMODORE 2 (n=7), and in a single-arm trial [(COMMODORE 3 (n=3)]. The safety profile of PIASKY appeared comparable between adult and pediatric patients, but conclusions are limited by the small number of pediatric patients.
-
7. DRUG INTERACTIONS
PIASKY binds different epitopes on C5 compared to eculizumab and ravulizumab, which can lead to the formation of DTDCs when patients switch between PIASKY and either eculizumab or ravulizumab. These DTDCs comprise one or more units of C5 bound to both PIASKY and to eculizumab or ravulizumab. These DTDCs are expected to be cleared within approximately 8 weeks (in the case of eculizumab) or longer (in the case of ravulizumab) and can result in Type III hypersensitivity reactions [see Warnings and Precautions (5.3), Adverse Reactions (6.1) and Clinical Pharmacology (12.3)].
-
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data on PIASKY use in pregnant women are insufficient to evaluate for a drug associated risk of major birth defects, miscarriage, or other adverse maternal or fetal outcomes. Human IgG antibody is known to cross the placenta and its transport increases as pregnancy progresses and peaks during the third trimester; therefore, PIASKY may be transmitted from the mother to the developing fetus. There are risks to the mother and fetus associated with untreated PNH in pregnancy (see Clinical Considerations). In an enhanced pre- and postnatal development study, no adverse developmental outcomes were observed when monkeys were exposed to crovalimab-akkz during the period of organogenesis through parturition at doses that produced maternal exposures 14-times the exposures at the maximum recommended human dose (MRHD), (see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risks of major birth defects and miscarriage in clinically recognized pregnancies are 2-4% and 15-20%, respectively.
Clinical Considerations
Disease-associated maternal and/or fetal/neonatal risk
PNH in pregnancy is associated with adverse maternal outcomes, including worsening cytopenias, thrombosis, infections, bleeding, miscarriages, and increased maternal mortality, and adverse fetal outcomes, including fetal death and premature delivery.
Data
Animal data
In an enhanced pre- and post-natal development study, pregnant cynomolgus monkeys were given an intravenous loading dose of crovalimab-akkz 100 mg/kg on gestation day (GD) 20 followed by weekly subcutaneous injections of up to 100 mg/kg up to parturition. The dams and infants were then observed untreated for 6 months. There were no adverse effects of crovalimab-akkz on pregnancy or on the viability, growth, and development of the infants up to 100 mg/kg at exposures 14-times the human exposure at the MRHD, based on area under the concentration-time curve (AUC).
8.2 Lactation
Risk Summary
There are no data on the presence of crovalimab-akkz in either human or animal milk, the effects on the breastfed child or on milk production. Endogenous IgG and monoclonal antibodies are transferred in human milk. The effects of local gastrointestinal exposure and limited systemic exposure in the breastfed child to crovalimab-akkz is unknown. Because of the potential for serious adverse reactions in a breastfed child, advise patients that breastfeeding is not recommended during treatment with PIASKY and for 9 months after the final dose.
8.4 Pediatric Use
The safety and effectiveness of PIASKY for the treatment of PNH have been established in pediatric patients 13 years and older with a body weight ≥ 40 kg. Use of PIASKY for this indication in pediatric patients is supported by evidence from adequate and well-controlled studies in adults along with additional pharmacokinetic, pharmacodynamic, efficacy and safety data in pediatric patients aged 13 to 17 years [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14.1)].
The safety and effectiveness of PIASKY have not been established in pediatric patients less than 13 years of age and in those with body weight < 40 kg.
8.5 Geriatric Use
Clinical studies of PIASKY did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for elderly patients should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other therapy.
Of the 393 PIASKY-treated patients in COMMODORE 1, 2 and 3, 43 (10.9%) were 65 years of age and older. In patients who were complement inhibitor naïve, serious adverse reactions were reported in 1 patient (8%) who was 65 years or older compared to 6 (4%) patients who were 18 to 64 years of age. In patients who previously received a different C5 inhibitor and switched to PIASKY, serious adverse reactions were reported in 3 (7%) patients who were 65 years or older compared to 12 (4%) patients who were 18 to 64 years of age.
-
11 DESCRIPTION
Crovalimab-akkz, a complement C5 inhibitor, is a humanized monoclonal antibody based on a human IgG1 framework. The recombinant antibody is produced in Chinese hamster ovary CHO cells and consists of two heavy chains (451 amino acid residues each) and two light chains (217 amino acid residues each). The approximate molecular weight is 145 kDa.
PIASKY (crovalimab-akkz) injection is a preservative-free, sterile, clear to opalescent, almost colorless to brownish-yellow, solution supplied in a single-dose vial for intravenous use or subcutaneous use. Intravenous use requires dilution prior to administration.
Each single-dose vial contains a 2 mL solution of crovalimab-akkz (340 mg), arginine hydrochloride (42.2 mg), histidine (9.4 mg), poloxamer 188 (1 mg), and Water for Injection USP. The pH is 5.8. Aspartic acid may be added to adjust the pH.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Crovalimab-akkz is a monoclonal antibody that specifically binds with high affinity to the complement protein C5, inhibiting its cleavage into C5a and C5b, preventing the formation of the membrane attack complex (MAC). Crovalimab-akkz inhibits terminal complement-mediated intravascular hemolysis in patients with PNH.
12.2 Pharmacodynamics
Concentration-dependent inhibition of terminal complement activity following treatment with PIASKY was observed in patients with PNH naïve to complement inhibitor therapy and patients switching from another complement C5 inhibitor therapy. Terminal complement activity (CH50 as measured by Liposome Immunoassay [LIA]) inhibition was achieved by the end of the initial PIASKY infusion and was sustained through the duration of PIASKY treatment. Similarly, mean free C5 concentrations declined to low levels (<0.0001 g/L) in comparison to baseline and remained low throughout the treatment period.
12.3 Pharmacokinetics
Crovalimab-akkz exhibits dose proportional pharmacokinetics over the dose range from 75 to 1500 mg when given as a single intravenous infusion and from 100 to 1020 mg when given as a subcutaneous injection. Following the first intravenous loading dose, crovalimab-akkz concentrations exceeded the target threshold for complete terminal complement inhibition (100 µg/mL). After approximately 12 weeks, with the administration of subsequent subcutaneous doses, crovalimab-akkz attained a steady-state plateau of exposure. Pharmacokinetic exposures in patients with PNH are summarized for the recommended dosage of crovalimab-akkz in Table 6.
Table 6 Mean (%CV) Pharmacokinetic Parameters of Crovalimab-akkz in Subjects with Paroxysmal Nocturnal Hemoglobinuria. Body weight of patients Ctrough,ss (µg/mL) Cmax,ss (µg/mL) AUCτ,ss (µg × day/mL) AUCτ,ss = area under the concentration-time curve for a dosing interval at steady state; Cmax,ss = maximum concentration during a dosing interval at steady state; Ctrough,ss = trough concentration at steady state. ≥ 40 kg to < 100 kg 230 (31.6%) 292 (30.1%) 7478 (30.5%) ≥ 100 kg 205 (31.5%) 265 (30.9%) 6748 (30.7%) Absorption
The mean absorption rate constant is 0.126 day-1 [90% CI: 0.105, 0.176]. Following subcutaneous administration, the bioavailability is 83.0% [90% CI: 69.6, 92.0].
Distribution
The mean central and peripheral volume of distribution is 3.23 L [90% CI: 3.16, 3.29] and 2.32 L [90% CI: 2.02, 2.67], respectively.
Elimination
In PNH treatment-naïve patients, the mean clearance is 0.0791 L/day [90% CI: 0.0678, 0.0872]. The mean estimated terminal half-life is 53.1 days [90% CI: 47.7, 58.6].
Special Populations
After inclusion of body weight, population pharmacokinetic analyses in patients with PNH showed that age (13-85 years of age), gender, and race (Caucasian, Black, and Asian) did not meaningfully influence the pharmacokinetics of PIASKY. No clinically significant differences in the pharmacokinetics of PIASKY were observed based on renal impairment (mild, moderate, and severe) and mild hepatic impairment. PIASKY has not been studied in patients with moderate or severe hepatic impairment.
Pediatric Patients
Data obtained in PNH clinical studies indicates that exposure in pediatric patients weighing ≥ 40 kg was consistent with that of adult patients.
Patients Switching from Another C5 Inhibitor
In patients switching from another C5 inhibitor (e.g., eculizumab or ravulizumab), a transient increase in clearance is observed due to the formation of transient immune complexes, leading to a faster elimination of PIASKY. However, this transiently different clearance does not require dose adjustment in patients switching from another C5 inhibitor.
12.6 Immunogenicity
The observed incidence of anti-drug antibodies is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of anti-drug antibodies in the studies described below with the incidence of anti-drug antibodies in other studies, including other crovalimab-akkz products.
In the active-controlled COMMODORE 2 study, 30% (42/140) of treatment-naïve patients who received PIASKY and 34% (23/67) of patients who switched from treatment with another C5 inhibitor to PIASKY (switch patients) tested positive for anti-crovalimab-akkz-antibodies. The positive antidrug antibodies (ADAs) were detected after a median treatment duration of 48 weeks (range: 0.1 to 108 weeks) in treatment-naïve patients and 24 weeks (range: 0.3 to 76 weeks), in switch patients.
Across COMMODORE 1, COMMODORE 2, and COMMODORE 3, the incidence of treatment-emergent ADAs was 31% (60/191) following a median treatment duration of 52 weeks (range 0.1 to 108 weeks) in treatment-naïve patients and 23% (43/184) following a median treatment duration of 32 weeks (0.3 to 108 weeks) in switch patients.
Among the patients who were randomized to PIASKY, those who developed anti-crovalimab-akkz antibodies had reduced crovalimab-akkz concentrations, geometric mean decrease in the range of 39% to 56%, compared to those who did not develop anti-crovalimab-akkz antibodies through the course of the treatment period in COMMODORE 2. Despite this effect, crovalimab-akkz concentrations remained above 100 µg/mL (the threshold for complete terminal complement inhibition) in more than 80% of ADA-positive patients. Approximately 3% (11/375) of ADA-positive patients had a loss of pharmacological activity (based on CH50 or free C5) coinciding with a loss of exposure and with loss of efficacy, manifesting as a sustained loss of hemolysis control in 1.6% (6/375) of patients with PNH. There was no evidence for a clinical impact of ADA status on the safety profile of PIASKY.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term carcinogenicity studies and genotoxicity studies have not been conducted with crovalimab-akkz. No effects on female or male reproductive organs were observed in cynomolgus monkeys following repeated administration of crovalimab-akkz for up to 6 months with subcutaneous doses up to 100 mg/kg/week which corresponds to 18- and 16- times for males and females, respectively, the MRHD based on AUC.
-
14. CLINICAL STUDIES
14.1 Paroxysmal Nocturnal Hemoglobinuria
The efficacy of PIASKY in patients with PNH was evaluated in COMMODORE 2 (NCT04434092), an active-controlled, open-label, non-inferiority study that randomized 204 patients (body weight ≥ 40 kg) with PNH not previously treated with a complement inhibitor in a 2:1 ratio to receive either PIASKY (n=135) or eculizumab (n=69). The study additionally enrolled 6 pediatric patients (aged >12 years and body weight ≥ 40 kg) to receive PIASKY in a separate non-randomized cohort.
Patients were required to be vaccinated against Neisseria meningitidis, either within 3 years prior to the start of treatment or within 7 days after starting treatment with PIASKY. Patients vaccinated within 2 weeks prior to initiating PIASKY or after the start of study treatment received prophylactic antibiotics until at least 2 weeks after the vaccination.
A single intravenous loading dose of PIASKY was given on Day 1 (1,000 mg for patients weighing ≥40 kg to <100 kg, or 1,500 mg for patients weighing >100 kg), followed by four additional weekly subcutaneous loading doses of 340 mg on Days 2, 8, 15 and 22. Starting at Day 29, maintenance subcutaneous doses were given every 4 weeks (680 mg for patients weighing ≥40 kg to <100 kg, or 1,020 mg for patients weighing ≥100 kg).
The study consisted of a primary treatment period of 24 weeks, after which patients had the option to continue or switch to PIASKY in an extension period.
Eligible patients had LDH level ≥ 2 × upper limit of normal (ULN) and at least one or more PNH-related signs or symptoms in the past 3 months. Randomization was stratified by the most recent LDH value (≥ 2 to ≤ 4 × ULN, or > 4× ULN) and by the transfusion history (0, > 0 to ≤ 6, or > 6 packed red blood cell (pRBC) units administered within 6 months prior to randomization). In the PIASKY and eculizumab arms, the median PNH clone size was 90.9% and 95.1% for monocytes, 91.4% and 93.6% for granulocytes and 25.3% and 44.6% for erythrocytes, respectively.
Demographics and baseline characteristics of the randomized study population were generally balanced between the treatment arms and are presented in Table 7.
Table 7 Demographics and Baseline Characteristics for COMMODORE 2 (Randomized Population) Parameters PIASKY
(N= 135)Eculizumab
(N= 69)pRBCs = packed red blood cells - * Includes medications that were started prior to initiation of study treatment and were either stopped before or were ongoing at time of initiation of study treatment.
Age (years) at PNH diagnosis Mean (SD) 35.8 (15.5) 37.4 (16.4) Median (range) 31.0 (11.5- 74.7) 32.1 (11.2- 76.8) Age (years) at first administration of the study drug Mean (SD) 40.5 (15.2) 41.9 (16.0) Median (range) 36.0 (18-76) 38.0 (17-78) <18 years, n (%) 0 2 (2.9%) 18 – 64 years, n (%) 122 (90.4%) 58 (84.1%) ≥65 years, n (%) 13 (9.6%) 9 (13.0%) Weight 40 to <100 kg, n (%) 131 (97.0%) 66 (95.7%) ≥100 kg, n (%) 4 (3.0%) 3 (4.3%) Sex Male, n (%) 77 (57.0%) 35 (50.7%) Female, n (%) 58 (43.0%) 34 (49.3%) Race Asian 86 (63.7%) 51 (73.9%) White 45 (33.3%) 16 (23.2%) Black or African American 3 (2.2%) 1 (1.4%) Unknown 1 (0.7%) 1 (1.4%) Ethnicity Hispanic or Latino 18 (13.3%) 6 (8.7%) Not Hispanic or Latino 114 (84.4%) 61 (88.4%) Not reported 3 (2.2%) 2 (2.9%) Baseline hemoglobin (g/dL)
Median (range) 8.5 (6.3-13.5) 8.5 (5.8-12.9) LDH levels at baseline (× ULN) Median (range) 7.0 (2.0 – 16.3) 7.7 (2.0 – 20.3) History of pRBC transfusion in the 12 months prior to screening Yes, n (%) 103 (77.4%) 50 (73.5%) Number of pRBC units transfused in the 12 months prior to screening Median (range) 3.8 (0-43.5) 3.0 (0-41.0) History of aplastic anemia Yes, n (%) 53 (39.3%) 26 (37.7%) History of myelodysplastic syndrome Yes, n (%) 6 (4.4%) 6 (8.7%) History of Major Adverse Vascular Event Yes, n (%) 21 (15.6%) 10 (14.5%) Medications at baseline* Anticoagulants, n (%) 35 (25.9%) 17 (24.6%) Systemic corticosteroids, n (%) 46 (34.1%) 25 (36.2%) Immunosuppressive therapy, n (%) 23 (17%) 13 (18.8%) Efficacy was based on hemolysis control, as measured by the mean proportion of patients with LDH ≤ 1.5× ULN from Week 5 to Week 25; and the proportion of patients who achieved transfusion avoidance, defined as patients who were pRBC transfusion-free, from baseline through Week 25. Other efficacy endpoints included the proportion of patients with breakthrough hemolysis and the proportion of patients with stabilized hemoglobin. Breakthrough hemolysis was defined as at least one new or worsening symptom or sign of intravascular hemolysis in the presence of elevated LDH ≥ 2 × ULN after prior reduction of LDH to ≤ 1.5 × ULN on treatment. Hemoglobin stabilization was defined as avoidance of a ≥ 2 g/dL decrease in hemoglobin level from baseline, in the absence of transfusion.
Efficacy results for these endpoints are shown in Table 8.
Table 8 Efficacy Results from COMMODORE 2 (Primary Analysis Population) PIASKY
(N=134) *Eculizumab
(N = 69)CI = confidence interval - * One patient randomized to PIASKY did not have post-baseline LDH and was not included in the primary efficacy analysis
- † Difference calculated as PIASKY minus eculizumab
- ‡ Non-inferiority was demonstrated based on the margin pre-specified in the study protocol
- § Odds ratio calculated as odds for PIASKY divided by odds for eculizumab
Proportion of patients with Transfusion Avoidance, % (95% CI) 65.7 (56.9, 73.5) 68.1 (55.7, 78.5) Difference in proportions†, % (95% CI)‡ -2.8% (-15.7, 11.1) Mean proportion of patients achieving hemolysis control, % (95% CI) 79.3 (72.9, 84.5) 79.0 (69.7, 86.0) Odds Ratio§ (95% CI)‡ 1.02 (0.57, 1.82) Proportion of patients with Breakthrough Hemolysis, % (95% CI) 10.4 (6.0, 17.2) 14.5 (7.5, 25.5) Difference in proportions†, % (95% CI)‡ - 3.9% (-14.8, 5.3) Proportion of patients with stabilized hemoglobin, % (95% CI) 63.4 (54.6, 71.5) 60.9 (48.4, 72.2) Difference in proportions†, % (95% CI)‡ 2.2 (-11.4, 16.3) Pediatric Population with PNH Treated with PIASKY
Efficacy was evaluated in 12 pediatric patients (with body weight ≥ 40 kg) treated with PIASKY in COMMODORE 2 (n=7; 13–17 years old), COMMODORE 1 (n=2, 13 – 16 years old) and in a single arm study in patients who were complement-inhibitor naïve, COMMODORE 3 (NCT04654468; n=3; 15–17 years old).
Nine pediatric patients were treatment-naïve, two patients switched from standard dose eculizumab and one patient switched from ravulizumab. Six pediatric patients were females and six were males. Nine patients were Asian, two were White and for one pediatric patient the race was unknown. The proportion of patients with a history of transfusions in the prior 12 months was 58%, with a median number of 1.3 pRBC units (range: 0-40.5) transfused, and a baseline median LDH of 6.4 × ULN (range 1.1-26.6). Aplastic anemia was reported in 50% of patients. All pediatric patients received the same dosing as adult patients based on body weight [see Dosage and Administration (2.2)]. Hemolysis control (defined as LDH ≤1.5 × ULN) from baseline to Week 25 was achieved in 7 of the 9 patients who were treatment-naïve, and the 3 patients switching from eculizumab or ravulizumab to PIASKY maintained hemolysis control through 24 weeks of PIASKY treatment. Nine (six patients who were treatment-naïve and three patients who switched from eculizumab or ravulizumab) out of the 12 pediatric patients achieved transfusion avoidance and hemoglobin stabilization, and no patients had a breakthrough hemolysis event during the 24-week treatment period.
Overall, the treatment effect of PIASKY in pediatric patients with PNH was consistent with that observed in adults with PNH.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
PIASKY (crovalimab-akkz) injection is a sterile, preservative-free, clear to opalescent, and almost colorless to brownish-yellow solution. Each PIASKY carton contains one 340 mg/2 mL (170 mg/mL) single-dose vial (NDC: 50242-115-01).
16.2 Storage and Handling
- Store refrigerated at 2°C to 8°C (36°F to 46°F) in the outer carton to protect from light. Do not freeze. Do not shake.
- Once removed from the refrigerator, the unopened vial can be kept at room temperature up to 30°C (86°F) in its outer carton for no longer than 7 days.
- Prior to administration, unopened vials of PIASKY may be stored out of the refrigerator at room temperature if needed and then returned to refrigeration. The total combined time out of refrigeration should not exceed 7 days and the temperature should not exceed 30°C (86°F). Discard if stored out of the refrigerator at room temperature for longer than 7 days.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Serious Meningococcal Infection
Advise patients of the risk of serious meningococcal infection. Inform patients of the need to complete or update their meningococcal vaccinations at least 2 weeks prior to receiving the first dose of PIASKY or receive antibacterial drug prophylaxis if PIASKY treatment must be initiated immediately and they have not previously been vaccinated. Inform patients of the requirement to be revaccinated according to current ACIP recommendations for meningococcal infection while on PIASKY therapy.
Inform patients that vaccination may not prevent serious meningococcal infection and to seek immediate medical attention if the following signs or symptoms occur [see Warnings and Precautions (5.1)].
- fever
- fever and a rash
- headache with nausea or vomiting
- fever with a high heart rate
- headache and a fever
- headache with a stiff neck or stiff back
- confusion
- muscle aches, with flu-like symptoms
- eye sensitive to light
Inform patients that they will be given a Patient Safety Card for PIASKY that they should carry with them at all times during and for 11 months following treatment with PIASKY. This card describes symptoms which, if experienced, should prompt the patient to immediately seek medical evaluation.
PIASKY REMS
PIASKY is available only through a restricted program called PIASKY REMS [see Warnings and Precautions (5.2)].
Inform the patient of the following requirements:
- Patients must receive counseling about the risk of serious meningococcal infections.
- Patients must receive written educational materials about this risk.
- Patients must be instructed to carry the Patient Safety Card with them at all times during and for 11 months following treatment with PIASKY.
- Patients must be instructed to complete or update meningococcal vaccines for serogroups A, C, W, Y and B per ACIP recommendations as directed by the prescriber prior to treatment with PIASKY.
- Patients must receive antibiotics as directed by the prescriber if they are not up to date with meningococcal vaccines and have to start PIASKY right away.
Type III Hypersensitivity Reactions
Inform patients of the risk of experiencing a Type III hypersensitivity reaction in the first 30 days after switching from another C5 inhibitor to PIASKY (or if they are planning to switch from PIASKY to another C5 inhibitor) [see Warnings and Precautions (5.3)]. Inform patients about the signs and symptoms of a Type III hypersensitivity reaction, and advise patients to seek immediate medical attention if the following signs or symptoms occur:
- rash
- itching
- joint pain
- numbness and tingling or a feeling of pins and needles, especially of the hands and feet
Other Infections
Counsel patients of the increased risk of infections, particularly those due to encapsulated bacteria, especially Neisseria species [see Warnings and Precautions (5.4)]. Advise patients of the need for vaccination against Streptococcus pneumoniae infections according to current ACIP recommendations. Inform parents or caregivers of children receiving PIASKY that their child should be vaccinated against Streptococcus pneumoniae and Haemophilus influenzae type b (Hib) according to current medical guidelines.
Advise patients to report any new signs and symptoms of infection.
Infusion- and Injection-Related Reactions
Advise patients that administration of PIASKY may result in infusion-related reactions or systemic injection-related reactions depending on the route of administration [see Warnings and Precautions (5.5)]. Advise patients to seek immediate medical attention if symptoms of serious allergic reactions occur.
Discontinuation of PIASKY
Inform patients that they may develop hemolysis due to PNH when PIASKY is discontinued and that they will be closely monitored by their healthcare professional for at least 20 weeks following PIASKY discontinuation [see Warnings and Precautions (5.6)]. Inform patients who discontinue PIASKY to keep the Patient Safety Card with them for 11 months after the last PIASKY dose, because the increased risk of meningococcal infection persists for several months following discontinuation of PIASKY [see Warnings and Precautions (5.1 and 5.2)].
Lactation
Advise patients it is not recommended to breastfeed during treatment with PIASKY and for 9 months after the final dose [see Use in Specific Populations (8.2)].
- SPL UNCLASSIFIED SECTION
-
MEDICATION GUIDE
MEDICATION GUIDE
PIASKY (pea-UH-sky)
(crovalimab-akkz)
injection, for intravenous or subcutaneous useThis Medication Guide has been approved by the U.S. Food and Drug Administration Issued: 06/2024 What is the most important information I should know about PIASKY?
PIASKY is a medicine that affects your immune system. PIASKY may lower the ability of your immune system to fight infections.-
PIASKY increases your chance of getting serious infections caused by Neisseria meningitidis. Meningococcal infections may quickly become life-threatening or cause death if not recognized and treated early.
- You must complete or update your meningococcal vaccines at least 2 weeks before your first dose of PIASKY.
- If you have not completed your meningococcal vaccines and PIASKY must be started right away, you should receive the required vaccines as soon as possible.
- If you have not been vaccinated and PIASKY must be started right away, you should also receive antibiotics to take for as long as your healthcare provider tells you to.
- If you had a meningococcal vaccine in the past, you might need additional vaccines before starting PIASKY. Your healthcare provider will decide if you need additional meningococcal vaccines.
- Meningococcal vaccines do not prevent all meningococcal infections. Call your healthcare provider or get emergency medical care right away if you get any of these signs and symptoms of a serious meningococcal infection:
- fever
- fever and a rash
- fever with a high heart rate
- fever with a headache
- headache with nausea or vomiting
- headache with a stiff neck or stiff back
- confusion
- muscle aches, with flu-like symptoms
- eyes sensitive to light
Your healthcare provider will give you a Patient Safety Card about the risk of serious meningococcal infection.
Carry it with you at all times during treatment and for 11 months after your last dose of PIASKY. Your risk of meningococcal infection may continue for several months after your last dose of PIASKY. It is important to show this card to any healthcare provider who treats you. This will help them diagnose and treat you quickly.
PIASKY is only available through a program called the PIASKY Risk Evaluation and Mitigation Strategy (PIASKY REMS). Before you can receive PIASKY, your healthcare provider must:- enroll in the PIASKY REMS program
- counsel you about the risk of serious meningococcal infection
- give you information about the signs and symptoms of serious meningococcal infection
- make sure that you are vaccinated against serious infections caused by meningococcal bacteria and that you receive antibiotics if you need to start PIASKY right away and you are not up to date on your vaccines
- give you a Patient Safety Card about your risk of meningococcal infection, as discussed above
- Immune system reactions called Type III hypersensitivity reactions are common during treatment with PIASKY and can also be serious. If you are currently being treated with or have been treated with another C5 inhibitor medicine and you switch to PIASKY, PIASKY may cause Type III hypersensitivity reactions. People may also develop Type III hypersensitivity reactions when they switch from PIASKY to another C5 inhibitor medicine. If you have been treated with another C5 inhibitor medicine and you switch to PIASKY, or if you have been treated with PIASKY and you switch to another C5 inhibitor medicine, your healthcare provider should monitor you for 30 days after you switch medicines. Call your healthcare provider or go to the nearest emergency room right away if you develop any signs and symptoms of Type III hypersensitivity reactions, including:
- joint pain
- muscle or bone pain
- rash or skin problems
- itching
- headache
- kidney problems
- numbness and tingling or a feeling of pins and needles, especially of the hands and feet
- fever
- weakness, tiredness, or lack of energy
- stomach trouble or pain
-
PIASKY may also increase the risk of other types of serious infections caused by encapsulated bacteria, including infections caused by Neisseria spp., Streptococcus pneumoniae, and Haemophilus influenzae and Neisseria gonorrhoeae.
- If you receive treatment with PIASKY, you should receive vaccines against Streptococcus pneumoniae.
- If your child receives treatment with PIASKY, your child should receive vaccines against Streptococcus pneumoniae and may receive vaccines against Haemophilus influenzae, depending on their age.
- fever of 100.4°F (38°C) or higher
- cough
- chest pain
- tiredness
- feeling short of breath
- painful rash
- sore throat
- burning pain when passing urine
- feeling weak or generally unwell
For more information about side effects, see "What are the possible side effects of PIASKY?" What is PIASKY?
PIASKY is a prescription medicine used to treat a disease called paroxysmal nocturnal hemoglobinuria (PNH) in adults and children 13 years of age and older who weigh at least 88 pounds (40 kg).
It is not known if PIASKY is safe and effective in children under 13 years of age and in people who weigh less than 88 pounds (40 kg).Who should not receive PIASKY?
Do not receive PIASKY if you:- have a serious meningococcal infection caused by Neisseria meningitidis when you are starting PIASKY treatment.
- are allergic to crovalimab or any of the ingredients in PIASKY. See the end of this Medication Guide for a complete list of ingredients in PIASKY.
Before receiving PIASKY tell your healthcare provider about all of your medical conditions, including if you: - have an infection or fever.
- are pregnant or plan to become pregnant. It is not known if PIASKY will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if PIASKY passes into your breast milk. You should not breastfeed during treatment with PIASKY and for 9 months after your final dose.
Especially tell your healthcare provider if you are currently being treated with or have ever been treated with any other complement C5 inhibitor (C5 inhibitor) medicine. PIASKY is a C5 inhibitor medicine. Ask your healthcare provider if you are not sure if you have been treated with a C5 inhibitor medicine. See "What are the possible side effects of PIASKY?"
Know the medicines you take and the vaccines you receive. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.How should I receive PIASKY? - Your healthcare provider will give you your PIASKY treatment.
- Your first dose will be given through a vein by intravenous (IV) infusion over 60 to 90 minutes on Day 1 by your healthcare provider. This is the first loading dose.
- Another loading dose will be given as an injection under the skin (subcutaneous) on Days 2, 8, 15, and 22.
- Your maintenance doses will begin on Day 29 and then will be given every 4 weeks as a subcutaneous injection.
- Your healthcare provider will prescribe the dose based on your weight. If your weight changes, tell your healthcare provider.
- Talk to your healthcare provider if you miss receiving an entire dose or part of your dose of PIASKY.
- If you are changing treatment from another C5 inhibitor such as eculizumab or ravulizumab to PIASKY, you should receive your first loading dose of PIASKY no sooner than the time you would have received your next scheduled dose of eculizumab or ravulizumab.
-
If you stop taking PIASKY and do not switch to another treatment for your PNH, your healthcare provider will need to monitor you closely for at least 20 weeks after stopping PIASKY. Stopping treatment with PIASKY may cause a breakdown of red blood cells due to PNH.
Symptoms or problems that can happen due to red blood cell breakdown include:
- a lower number of red blood cells (anemia)
- blood in your urine or dark urine
- feeling short of breath
- feeling tired or low energy (fatigue)
- stomach pain
- blood clotting (thrombosis)
- difficulty swallowing
- difficulty getting or keeping an erection (erectile dysfunction)
- kidneys not working properly
What are the possible side effects of PIASKY?
PIASKY may cause serious side effects including:- See "What is the most important information I should know about PIASKY?"
- Infusion- and injection-related reactions. Infusion- or injection-related reactions may happen during or after your PIASKY infusion or injection. Symptoms may include headache, pain at the infusion or injection site or pain in other parts of your body, swelling, bruising or bleeding, red skin, itching and rash. PIASKY can also cause serious allergic reactions. If you have an infusion-related reaction, your healthcare provider may need to infuse PIASKY more slowly, temporarily stop your infusion, or completely stop PIASKY if you develop a serious allergic reaction. Call your healthcare provider right away or go to the nearest emergency room if you develop any signs or symptoms of a serious allergic reaction, including:
- shortness of breath or trouble breathing
- pain or tightness in your chest
- wheezing
- feeling dizzy or lightheaded
- swelling of the throat, lips, tongue, or face
- skin itching, hives, or rash
- fever or chills
The most common side effects of PIASKY include: - infusion-related reactions
- respiratory tract infections including infections of the lungs, cold symptoms, and pain or swelling of the nose or throat
- viral infections
- Type III hypersensitivity reactions
Tell your healthcare provider about any side effect that bothers you or that does not go away.
These are not all of the possible side effects of PIASKY. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.General information about the safe and effective use of PIASKY.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use PIASKY for a condition for which it was not prescribed. You can ask your pharmacist or healthcare provider for information about PIASKY that is written for health professionals.What are the ingredients in PIASKY?
Active ingredient: crovalimab-akkz
Inactive ingredients: arginine hydrochloride, histidine, poloxamer 188, and Water for Injection. Aspartic acid may be added to adjust the pH.
Manufactured by: Genentech, Inc., A Member of the Roche Group, 1 DNA Way, South San Francisco, CA 94080-4990
U.S. License No.: 1048
PIASKY is a registered trademark of Chugai Pharmaceutical Co., Ltd., Tokyo, Japan
©2024 Genentech, Inc. All rights reserved. For more information, go to www.PIASKY.com or call 1-877-436-3683. -
PIASKY increases your chance of getting serious infections caused by Neisseria meningitidis. Meningococcal infections may quickly become life-threatening or cause death if not recognized and treated early.
-
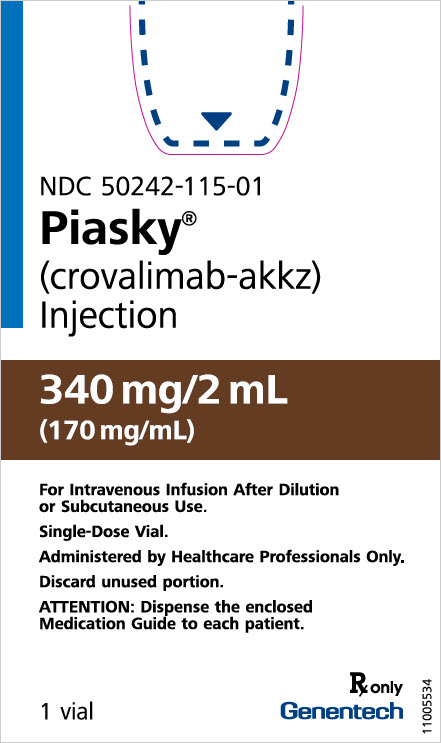
PRINCIPAL DISPLAY PANEL - 340 mg/2 mL Vial Carton
NDC: 50242-115-01
Piasky®
(crovalimab-akkz)
Injection340 mg/2 mL
(170 mg/mL)For Intravenous Infusion After Dilution
or Subcutaneous Use.Single-Dose Vial.
Administered by Healthcare Professionals Only.
Discard unused portion.
ATTENTION: Dispense the enclosed
Medication Guide to each patient.1 vial
Rx only
Genentech
11005534
-
INGREDIENTS AND APPEARANCE
PIASKY
crovalimab injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50242-115 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CROVALIMAB (UNII: H9KH1GP3UU) (CROVALIMAB - UNII:H9KH1GP3UU) CROVALIMAB 340 mg in 2 mL Inactive Ingredients Ingredient Name Strength HISTIDINE (UNII: 4QD397987E) ASPARTIC ACID (UNII: 30KYC7MIAI) ARGININE HYDROCHLORIDE (UNII: F7LTH1E20Y) POLOXAMER 188 (UNII: LQA7B6G8JG) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50242-115-01 1 in 1 CARTON 06/20/2024 1 2 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA761388 06/20/2024 Labeler - Genentech, Inc. (080129000) Registrant - Genentech, Inc. (080129000) Establishment Name Address ID/FEI Business Operations Genentech, Inc. 080129000 ANALYSIS(50242-115) , MANUFACTURE(50242-115) , PACK(50242-115) , LABEL(50242-115) Establishment Name Address ID/FEI Business Operations Roche Diagnostics GmbH 315028860 ANALYSIS(50242-115) , MANUFACTURE(50242-115) , PACK(50242-115) , LABEL(50242-115) Establishment Name Address ID/FEI Business Operations F. Hoffmann-La Roche AG 485244961 PACK(50242-115) , LABEL(50242-115) Establishment Name Address ID/FEI Business Operations Roche Diagnostics GmbH 323105205 API MANUFACTURE(50242-115) , ANALYSIS(50242-115) Establishment Name Address ID/FEI Business Operations Genentech, Inc. 146373191 ANALYSIS(50242-115)
Trademark Results [Piasky]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 PIASKY 98386771 not registered Live/Pending |
CHUGAI SEIYAKU KABUSHIKI KAISHA (ChugaiPharmaceutical Co., Ltd.) 2024-02-01 |
 PIASKY 97616949 not registered Live/Pending |
CHUGAI SEIYAKU KABUSHIKI KAISHA (ChugaiPharmaceutical Co., Ltd.) 2022-10-03 |
 PIASKY 88787187 not registered Live/Pending |
CHUGAI SEIYAKU KABUSHIKI KAISHA (ChugaiPharmaceutical Co., Ltd.) 2020-02-06 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.