MERCAPTOPURINE suspension
MERCAPTOPURINE by
Drug Labeling and Warnings
MERCAPTOPURINE by is a Prescription medication manufactured, distributed, or labeled by Hikma Pharmaceuticals USA Inc., West-Ward Columbus Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use MERCAPTOPURINE ORAL SUSPENSION safely and effectively. See full prescribing information for MERCAPTOPURINE ORAL SUSPENSION.
MERCAPTOPURINE oral suspension
Initial U.S. Approval: 1953RECENT MAJOR CHANGES
Warnings and Precautions, Hepatotoxicity (5.2) 7/2024
INDICATIONS AND USAGE
Mercaptopurine is a nucleoside metabolic inhibitor indicated for the treatment of patients with acute lymphoblastic leukemia (ALL) as part of a combination chemotherapy maintenance regimen. (1.1)
DOSAGE AND ADMINISTRATION
- The recommended starting dosage of mercaptopurine oral suspension is 1.5 mg/kg to 2.5 mg/kg (50 mg/m2 to 75 mg/m2) orally once daily as part of a combination chemotherapy maintenance regimen. Adjust dose to maintain desirable absolute neutrophil count and for excessive myelosuppression. (2.1)
- Renal Impairment: Use the lowest recommended starting dose or increase the dosing interval. (2.3, 8.6)
- Hepatic Impairment: Use the lowest recommended starting dose. (2.3, 8.7)
DOSAGE FORMS AND STRENGTHS
Oral suspension: 2,000 mg/100 mL (20 mg/mL) (3)
CONTRAINDICATIONS
- None
WARNINGS AND PRECAUTIONS
- Myelosuppression: Monitor complete blood count (CBC) and adjust the dose of mercaptopurine for excessive myelosuppression. Consider testing in patients with severe myelosuppression or repeated episodes of myelosuppression for thiopurine S-methyltransferase (TPMT) or nucleotide diphosphatase (NUDT15) deficiency. Patients with homozygous-TPMT or homozygous-NUDT15 deficiency may require a dose reduction. (2.2, 5.1)
- Hepatotoxicity: Monitor transaminases, alkaline phosphatase and bilirubin. Withhold mercaptopurine at onset of hepatotoxicity. (5.2)
- Immunosuppression: Response to all vaccines may be diminished and there is a risk of infection with live virus vaccines. Consult immunization guidelines for immunocompromised pediatrics. (5.3)
- Treatment Related Malignancies: Aggressive and fatal cases of hepatosplenic T-cell lymphoma have occurred. (5.4)
- Macrophage Activation Syndrome: Monitor for and treat promptly; discontinue mercaptopurine. (5.5)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise patients of reproductive potential of the potential risk to a fetus and to use effective contraception. (5.6, 8.1, 8.3)
- Phenylketonuria: Patients should be informed that mercaptopurine oral suspension contains phenylalanine, a component of aspartame. Each mL of the 20 mg/mL oral suspension contains 0.015 mg of phenylalanine. (5.7)
ADVERSE REACTIONS
The most common adverse reaction (>20%) is myelosuppression, including anemia, neutropenia, lymphopenia and thrombocytopenia.
Adverse reactions occurring in 5% to 20% of patients include anorexia, nausea, vomiting, diarrhea, malaise and rash. (6.1)To report SUSPECTED ADVERSE REACTIONS, contact Hikma Pharmaceuticals USA Inc. at 1-800-962-8364 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 11/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Acute Lymphoblastic Leukemia
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Dosage Modifications in Patients with TPMT and NUDT15 Deficiency
2.3 Dosage Modifications in Renal and Hepatic Impairment
2.4 Dosage Modification with Concomitant Use of Allopurinol
2.5 Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
5.2 Hepatotoxicity
5.3 Immunosuppression
5.4 Treatment Related Malignancies
5.5 Macrophage Activation Syndrome
5.6 Embryo-Fetal Toxicity
5.7 Risks in Patients with Phenylketonuria
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Allopurinol
7.2 Warfarin
7.3 Myelosuppressive Products
7.4 Aminosalicylates
7.5 Hepatotoxic Products
7.6 Methotrexate
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.5 Pharmacogenomics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
The recommended starting dose of mercaptopurine oral suspension is 1.5 mg/kg to 2.5 mg/kg (50 mg/m2 to 75 mg/m2) orally once daily as part of combination chemotherapy maintenance regimen. Take mercaptopurine oral suspension either consistently with or without food.
After initiating mercaptopurine, monitor complete blood counts (CBC) and adjust the dose to maintain absolute neutrophil count (ANC) at a desirable level and for excessive myelosuppression. Evaluate the bone marrow in patients with prolonged myelosuppression or repeated episodes of myelosuppression to assess leukemia status and marrow cellularity.
Evaluate thiopurine S-methyltransferase (TPMT) and nucleotide diphosphatase (NUDT15) status in patients with severe myelosuppression or repeated episodes of myelosuppression [see Dosage and Administration (2.2)].
If a patient misses a dose, instruct the patient to continue with the next scheduled dose.
2.2 Dosage Modifications in Patients with TPMT and NUDT15 Deficiency
Consider testing for TPMT and NUDT15 deficiency in patients who experience severe myelosuppression or repeated episodes of myelosuppression [see Warnings and Precautions (5.1), Clinical Pharmacology (12.5)].
Homozygous Deficiency in either TPMT or NUDT15
Patients with homozygous deficiency of either enzyme typically require 10% or less of the recommended dosage. Reduce the recommended starting dosage of mercaptopurine in patients who are known to have homozygous TPMT or NUDT15 deficiency.Heterozygous Deficiency in TPMT and/or NUDT15
Reduce the mercaptopurine dosage based on tolerability. Most patients with heterozygous TPMT or NUDT15 deficiency tolerate recommended dosage, but some require dose reduction based on adverse reactions. Patients who are heterozygous for both TPMT and NUDT15 may require more substantial dose reductions.2.3 Dosage Modifications in Renal and Hepatic Impairment
Renal Impairment
Use the lowest recommended starting dosage for mercaptopurine in patients with renal impairment (CLcr less than 50 mL/min). Adjust the dosage to maintain absolute neutrophil count (ANC) at a desirable level and for adverse reactions [see Uses in Specific Populations (8.6)].Hepatic Impairment
Use the lowest recommended starting dosage for mercaptopurine in patients with hepatic impairment. Adjust the dosage to maintain absolute neutrophil count (ANC) at a desirable level and for adverse reactions [see Uses in Specific Populations (8.7)].2.4 Dosage Modification with Concomitant Use of Allopurinol
Reduce the dose of mercaptopurine to one-third to one-quarter of the current dosage when coadministered with allopurinol [see Drug Interactions (7.1)].
2.5 Administration
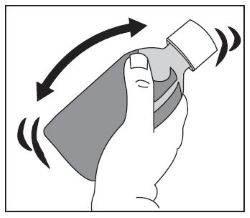
Shake the bottle vigorously for at least 30 seconds to ensure the oral suspension is well mixed. Mercaptopurine oral suspension is a pink to brown viscous oral suspension.
Provide a press-in bottle adapter and two oral dispensing syringes (one 1 mL and one 5 mL).
Train patients or caregivers on proper handling, storage, administration, disposal and clean-up of accidental spillage prior to initiation of mercaptopurine oral suspension and during each visit to the clinic.
Advise patients and caregivers to use mercaptopurine oral suspension within 8 weeks and properly discard remaining mercaptopurine oral suspension after 8 weeks.
Provide instructions regarding which syringe to use and how to administer the specified dose, since mercaptopurine oral suspension is supplied with 1 mL and 5 mL oral dispensing syringes.
Advise patients that the oral dispensing syringe is intended for multiple uses and provide the following instructions:
- Wash the oral dispensing syringe with warm ‘soapy’ water and rinse well;
- Hold the oral dispensing syringe under water and move the plunger up and down several times to make sure the inside of the oral dispensing syringe is clean;
- Ensure the oral dispensing syringe is completely dry before use of the oral dispensing syringe again; and
- Store the oral dispensing syringe in a hygienic place with mercaptopurine oral suspension.
Mercaptopurine is a hazardous drug. Follow special handling and disposal procedures.1
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
The most consistent, dose-related adverse reaction of mercaptopurine is myelosuppression, manifested by anemia, leukopenia, thrombocytopenia, or any combination of these. Monitor CBC and adjust the dosage of mercaptopurine for excessive myelosuppression [see Dosage and Administration (2.1)].
Consider testing for thiopurine S-methyltransferase (TPMT) or nucleotide diphosphatase (NUDT15) deficiency in patients with severe myelosuppression or repeated episodes of myelosuppression. TPMT genotyping or phenotyping (red blood cell TPMT activity) and NUDT15 genotyping can identify patients who have reduced activity of these enzymes. Patients with homozygous TPMT or NUDT15 deficiency may require a dose reduction [see Dosage and Administration (2.2), Clinical Pharmacology (12.5)].
Myelosuppression can be exacerbated by coadministration with allopurinol, aminosalicylates or other products that cause myelosuppression [see Drug Interactions (7.1, 7.3, 7.4)]. Reduce the dosage of mercaptopurine when coadministered with allopurinol [see Dosage and Administration (2.4)].
5.2 Hepatotoxicity
Mercaptopurine is hepatotoxic. There are reports of deaths attributed to hepatic necrosis associated with the administration of mercaptopurine. Hepatic injury can occur with any dosage but seems to occur with greater frequency when the recommended dosage is exceeded. In some patients, jaundice has cleared following withdrawal of mercaptopurine and reappeared with rechallenge.
Usually, clinically detectable jaundice appears early in the course of treatment (1 to 2 months); however, jaundice has been reported as early as 1 week and as late as 8 years after starting mercaptopurine. The hepatotoxicity has been associated in some cases with anorexia, diarrhea, jaundice, ascites, and pruritus. Hepatic encephalopathy has occurred.
Monitor serum transaminase levels, alkaline phosphatase, and bilirubin levels at weekly intervals when first beginning therapy and at monthly intervals thereafter. Monitor liver tests more frequently in patients who are receiving mercaptopurine with other hepatotoxic drugs [see Drug Interactions (7.5)] or with known pre-existing liver disease. Withhold mercaptopurine at onset of hepatotoxicity.
Intrahepatic Cholestasis of Pregnancy
Postmarketing cases of intrahepatic cholestasis of pregnancy (ICP) have been reported in patients with inflammatory bowel disease who received mercaptopurine during pregnancy. Mercaptopurine is not indicated for use in inflammatory bowel disease [see Indications and Usage (1.1)].
Discontinue mercaptopurine if ICP develops in a pregnant woman.
5.3 Immunosuppression
Mercaptopurine is immunosuppressive and may impair the immune response to infectious agents or vaccines. Due to the immunosuppression associated with maintenance chemotherapy for ALL, response to all vaccines may be diminished and there is a risk of infection with live virus vaccines. Consult immunization guidelines for immunocompromised patients.
5.4 Treatment Related Malignancies
Hepatosplenic T-cell lymphoma has been reported in patients treated with mercaptopurine for inflammatory bowel disease (IBD), an unapproved use. Mercaptopurine is mutagenic in animals and humans, carcinogenic in animals, and may increase the risk of secondary malignancies.
Patients receiving immunosuppressive therapy, including mercaptopurine, are at an increased risk of developing lymphoproliferative disorders and other malignancies, notably skin cancers (melanoma and non-melanoma), sarcomas (Kaposi’s and non-Kaposi’s) and uterine cervical cancer in situ. The increased risk appears to be related to the degree and duration of immunosuppression. It has been reported that discontinuation of immunosuppression may provide partial regression of the lymphoproliferative disorder.
A treatment regimen containing multiple immunosuppressants (including thiopurines) should therefore be used with caution as this could lead to lymphoproliferative disorders, some with reported fatalities. A combination of multiple immunosuppressants, given concomitantly increases the risk of Epstein-Barr virus (EBV)-associated lymphoproliferative disorders.
5.5 Macrophage Activation Syndrome
Macrophage activation syndrome (MAS) (hemophagocytic lymphohistiocytosis) is a known, life-threatening disorder that may develop in patients with autoimmune conditions, in particular with inflammatory bowel disease (IBD), and there could potentially be an increased susceptibility for developing the condition with the use of mercaptopurine (an unapproved use). If MAS occurs, or is suspected, discontinue mercaptopurine. Monitor for and promptly treat infections such as EBV and cytomegalovirus (CMV), as these are known triggers for MAS.
5.6 Embryo-Fetal Toxicity
Mercaptopurine can cause fetal harm when administered to a pregnant woman. An increased incidence of miscarriage has been reported in women who received mercaptopurine in the first trimester of pregnancy. Adverse embryo-fetal findings, including miscarriage and stillbirth, have been reported in women who received mercaptopurine after the first trimester of pregnancy. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with mercaptopurine and for 6 months after the last dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with mercaptopurine and for 3 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
5.7 Risks in Patients with Phenylketonuria
Phenylalanine can be harmful to patients with phenylketonuria (PKU). Phenylketonuric patients should be informed that mercaptopurine oral suspension contains phenylalanine, a component of aspartame. Each mL of the mercaptopurine oral suspension, 20 mg/mL contains 0.015 mg of phenylalanine.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Myelosuppression [see Warnings and Precautions (5.1)]
- Hepatotoxicity [see Warnings and Precautions (5.2)]
- Immunosuppression [see Warnings and Precautions (5.3)]
- Treatment Related Malignancies [see Warnings and Precautions (5.4)]
- Macrophage Activation Syndrome [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Based on multicenter cooperative group ALL trials, the most common adverse reaction occurring in > 20% of patients was myelosuppression, including anemia, neutropenia, lymphopenia and thrombocytopenia. Adverse reactions occurring in 5% to 20% of patients included anorexia, nausea, vomiting, diarrhea, malaise, and rash. Adverse reactions occurring in < 5% of patients included urticaria, hyperuricemia, oral lesions, elevated transaminases, hyperbilirubinemia, hyperpigmentation, infections, and pancreatitis. Oral lesions resemble thrush rather than antifolic ulcerations. Delayed or late toxicities include hepatic fibrosis, hyperbilirubinemia, alopecia, pulmonary fibrosis, oligospermia and secondary malignancies [see Warnings and Precautions (5.1, 5.2)].
Drug fever has been reported with mercaptopurine.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of mercaptopurine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These reactions include: photosensitivity, hypoglycemia, portal hypertension, intrahepatic cholestasis of pregnancy (ICP), pellagra, and erythema nodosum.
-
7 DRUG INTERACTIONS
7.1 Allopurinol
Allopurinol can inhibit the first-pass oxidative metabolism of mercaptopurine by xanthine oxidase, which can lead to an increased risk of mercaptopurine adverse reactions [see Warnings and Precautions (5.1), Adverse Reactions (6.1)]. Reduce the dose of mercaptopurine when coadministered with allopurinol [see Dosage and Administration (2.4)].
7.2 Warfarin
The coadministration of mercaptopurine with warfarin may decrease the anticoagulant effectiveness of warfarin. Monitor the international normalized ratio (INR) in patients receiving warfarin and adjust the warfarin dosage as appropriate.
7.3 Myelosuppressive Products
Mercaptopurine can cause myelosuppression. Myelosuppression may be increased when mercaptopurine is coadministered with other drugs that cause myelosuppression. Enhanced myelosuppression has been noted in some patients receiving trimethoprim-sulfamethoxazole. Monitor the CBC and adjust the dose of mercaptopurine for excessive myelosuppression [see Dosage and Administration (2.1), Warnings and Precautions (5.1)].
7.4 Aminosalicylates
Aminosalicylates (e.g., mesalamine, olsalazine or sulfasalazine) may inhibit the TPMT enzyme, which may increase the risk of myelosuppression when coadministered with mercaptopurine. When aminosalicylates and mercaptopurine are coadministered, use the lowest possible doses for each drug and monitor more frequently for myelosuppression [see Warnings and Precautions (5.1)].
7.5 Hepatotoxic Products
Mercaptopurine can cause hepatotoxicity. Hepatotoxicity may be increased when mercaptopurine is coadministered with other products that cause hepatotoxicity. Monitor liver tests more frequently in patients who are receiving mercaptopurine with other hepatotoxic products [see Warnings and Precautions (5.2)].
7.6 Methotrexate
Mercaptopurine dosage may need adjustment when administered concomitantly with high dose methotrexate [see Warnings and Precautions (5.1)]. Mercaptopurine exposure increases with concomitant methotrexate use [see Clinical Pharmacology (12.3)] which may increase the risk of mercaptopurine adverse reactions. The mechanism of this interaction has not been fully characterized [see Clinical Pharmacology (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Mercaptopurine can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. Pregnant women who receive mercaptopurine have an increased incidence of miscarriage and stillbirth (see Data). Advise pregnant women of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population(s) is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data
Women receiving mercaptopurine in the first trimester of pregnancy have an increased incidence of miscarriage; the risk of malformation in offspring surviving first trimester exposure is not known. In a series of 28 women receiving mercaptopurine after the first trimester of pregnancy, 3 mothers died prior to delivery, 1 delivered a stillborn child, and 1 aborted; there were no cases of macroscopically abnormal fetuses.Animal Data
Mercaptopurine was embryo-lethal and teratogenic in several animal species (rat, mouse, rabbit, and hamster) at doses less than the recommended human dose.8.2 Lactation
Risk Summary
There are no data on the presence of mercaptopurine or its metabolites in human milk, the effects on the breastfed child or the effects on milk production. Because of the potential for serious adverse reactions in the breastfed child, advise women not to breastfeed during treatment with mercaptopurine and for 1 week after the last dose.
8.3 Females and Males of Reproductive Potential
Mercaptopurine can cause fetal harm when administered to pregnant women [see Use in Specific Populations (8.1)].
Pregnancy Testing
Verify the pregnancy status in females of reproductive potential prior to initiating mercaptopurine [see Use in Specific Populations (8.1)].
Contraception
Females
Advise females of reproductive potential to use effective contraception during treatment with mercaptopurine and for 6 months after the last dose.Males
Based on genotoxicity findings, advise males with female partners of reproductive potential to use effective contraception during treatment with mercaptopurine and for 3 months after the last dose [see Nonclinical Toxicology (13.1)].Infertility
Females and Males
Based on findings from animal studies, mercaptopurine can impair female and male fertility [see Nonclinical Toxicology (13.1)]. The long-term effects of mercaptopurine on female and male fertility, including the reversibility have not been studied.8.4 Pediatric Use
Safety and effectiveness of mercaptopurine has been established in pediatric patients. Use of mercaptopurine in pediatrics is supported by evidence from the published literature and clinical experience. Symptomatic hypoglycemia has been reported in pediatric patients with ALL receiving mercaptopurine. Reported cases were in pediatrics less than 6 years or with a low body mass index.
8.5 Geriatric Use
Clinical studies of mercaptopurine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or another drug therapy.
8.6 Renal Impairment
Use the lowest recommended starting dosage for mercaptopurine or increase the dosing interval to every 36 to 48 hours in patients with renal impairment (CLcr less than 50 mL/min). Adjust the dose to maintain absolute neutrophil count (ANC) at a desirable level and for adverse reactions [see Dosage and Administration (2.3)].
8.7 Hepatic Impairment
Use the lowest recommended starting dosage for mercaptopurine in patients with hepatic impairment. Adjust the dose to maintain absolute neutrophil count (ANC) at a desirable level and for adverse reactions [see Dosage and Administration (2.3)].
-
10 OVERDOSAGE
Signs and symptoms of mercaptopurine overdosage may be immediate (anorexia, nausea, vomiting, and diarrhea) or delayed (myelosuppression, liver dysfunction, and gastroenteritis). Dialysis cannot be expected to clear mercaptopurine. Hemodialysis is thought to be of marginal use due to the rapid intracellular incorporation of mercaptopurine into active metabolites with long persistence.
Withhold mercaptopurine immediately if severe or life-threatening adverse reactions occur during treatment. If a patient is seen immediately following an accidental overdosage, it may be useful to induce emesis.
-
11 DESCRIPTION
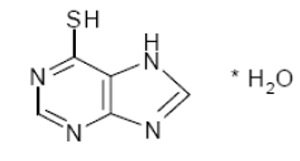
Mercaptopurine is a nucleoside metabolic inhibitor. The chemical name is 6H-purine-6-thione, 1,7-dihydro-, monohydrate. The molecular formula is C5H4N4SH2O and the molecular weight is 170.20. The structural formula is:
Mercaptopurine, USP is a yellow, crystalline powder; odorless. It is practically insoluble in water and in ether; slightly soluble in ethanol (96%). It dissolves in solutions of alkali hydroxides; pKa 7.8, 11.2.
Mercaptopurine oral suspension contains 2,000 mg/100 mL (20 mg/mL) of mercaptopurine, USP. The suspension also contains the following inactive ingredients: aspartame, ethylparaben sodium, hydrochloric acid, methylparaben sodium, potassium sorbate, raspberry juice powder (raspberry juice, rice syrup solids, silicon dioxide), sodium hydroxide, sucrose, water (purified), xanthan gum. Mercaptopurine oral suspension is a pink to brown viscous suspension.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Mercaptopurine is a purine analog that undergoes intracellular transport and activation to form metabolites including thioguanine nucleotides (TGNs). Incorporation of TGNs into DNA or RNA results in cell-cycle arrest and cell death. TGNs and other mercaptopurine metabolites are also inhibitors of de novo purine synthesis and purine nucleotide interconversions. Mercaptopurine was cytotoxic to proliferating cancer cells in vitro and had antitumor activity in mouse tumor models. It is not known which of the biochemical effects of mercaptopurine and its metabolites are directly or predominantly responsible for cell death.
12.2 Pharmacodynamics
Exposure-Response Relationships
Mercaptopurine exposure-response relationships and the time course of pharmacodynamics response are unknown.
12.3 Pharmacokinetics
Following a single oral dose of mercaptopurine 50 mg under fasted conditions to adult healthy subjects, the median (min – max) AUC0-INF was 137 h∙ng/mL (77 – 268 h∙ng/mL) and Cmax was 93 ng/mL (40 – 204 ng/mL).
Absorption
Mercaptopurine is absorbed after oral administration with a median (min – max) Tmax of 0.75 (0.33 – 2.5) hours.
Effect of Food
Food has been shown to decrease the exposure of mercaptopurine.
Distribution
The volume of distribution exceeds total body water with a mean volume of distribution of approximately 0.9 L/kg. There is negligible entry of mercaptopurine into cerebrospinal fluid.
Plasma protein binding averages 19% over the concentration range 10 to 50 mcg/L.
Elimination
The median (min – max) elimination half-life (t1/2) was 1.3 (0.9 – 5.4) hours.
Metabolism
Mercaptopurine is inactivated via two major pathways. One is thiol methylation, which is catalyzed by the polymorphic enzyme thiopurine S-methyltransferase (TPMT), to form the inactive metabolite methyl-mercaptopurine. The second inactivation pathway is oxidation, which is catalyzed by xanthine oxidase. The product of oxidation is the inactive metabolite 6-thiouric acid.
Elimination
After oral administration of mercaptopurine, urine contains intact mercaptopurine, thiouric acid (formed by direct oxidation by xanthine oxidase, probably via 6-mercapto-8-hydroxypurine), and a number of 6-methylated thiopurines. In one subject, a total of 46% of the dose could be accounted for in the urine (as parent drug and metabolites) in the first 24 hours.
Specific Populations
Pediatric Patients
Wide inter individual variations in systemic exposure is observed. Following oral administration of 50 mg/m2 mercaptopurine in 10 children, median plasma concentrations 1 hour post dose was 0.35 (range 0.03 to 1.03) μM and median AUC1–5hours was 56 (range 23 to 65) μM·min. Tmax ranged from 1 to 3 hours.
Drug Interactions Studies
Methotrexate: Mercaptopurine AUC increased by approximately 31% when coadministered with oral methotrexate 20 mg/m2. Mercaptopurine AUC increased by 69% when coadministered with IV methotrexate 2 g/m2, and by 93% when coadministered with IV methotrexate 5 g/m2.
12.5 Pharmacogenomics
Several published studies indicate that patients with reduced TPMT or NUDT15 activity receiving usual doses of mercaptopurine, accumulate excessive cellular concentrations of active 6-TGNs, and are at higher risk for severe myelosuppression [see Warnings and Precautions (5.1)]. In a study of 1028 children with ALL, the approximate tolerated mercaptopurine dosage for patients with TPMT and/or NUDT15 deficiency on mercaptopurine maintenance therapy (as a percentage of the planned dosage) was as follows: heterozygous for either TPMT or NUDT15, 50-90%; heterozygous for both TPMT and NUDT15, 30-50%; homozygous for either TPMT or NUDT15, 5-10%.
Approximately 0.3% (1:300) of patients of European or African ancestry have two loss-of-function alleles of the TPMT gene and have little or no TPMT activity (homozygous deficient or poor metabolizers), and approximately 10% of patients have one loss-of-function TPMT allele leading to intermediate TPMT activity (heterozygous deficient or intermediate metabolizers). The TPMT*2, TPMT*3A, and TPMT*3C alleles account for about 95% of individuals with reduced levels of TPMT activity.
NUDT15 deficiency is detected in <1% of patients of European or African ancestry. Among patients of East Asian ancestry (i.e., Chinese, Japanese, Vietnamese), 2% have two loss-of-function alleles of the NUDT15 gene, and approximately 21% have one loss-of-function allele. The p.R139C variant of NUDT15 (present on the *2 and *3 alleles) is the most commonly observed, but other less common loss-of-function NUDT15 alleles have been observed.
Consider all clinical information when interpreting results from phenotypic testing used to determine the level of thiopurine nucleotides or TPMT activity in erythrocytes, since some coadministered drugs can influence measurement of TPMT activity in blood, and blood from recent transfusions will misrepresent a patient’s actual TPMT activity [see Dosage and Administration (2.2) and Warnings and Precautions (5.1)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Mercaptopurine is carcinogenic in animals.
Mercaptopurine causes chromosomal aberrations in cells derived from animals and humans and induces dominant-lethal mutations in the germ cells of male mice.
Mercaptopurine can impair fertility. In mice, surviving female offspring of mothers who received chronic low doses of mercaptopurine during pregnancy were found sterile, or if they became pregnant, had smaller litters and more dead fetuses as compared to control animals.
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Mercaptopurine Oral Suspension is supplied as 2,000 mg/100 mL (20 mg/mL) pink to brown viscous liquid in amber glass multiple-dose bottles. In addition, a press-in bottle adapter and two oral dispensing syringes (one 1 mL and one 5 mL) are provided.
Each carton NDC: 0054-4582-49 contains 1 bottle of Mercaptopurine Oral Suspension NDC: 0054-4582-49.
- Store Mercaptopurine Oral Suspension at 20º to 25ºC (68º to 77ºF) [see USP Controlled Room Temperature]. Store in a dry place.
Mercaptopurine is a hazardous drug. Follow special handling and disposal procedures.1
-
17 PATIENT COUNSELING INFORMATION
Advise the patients and caregivers to read the FDA-approved patient labelling (Patient Information and Instructions for Use).
Major Adverse Reactions
Advise patients and caregivers that mercaptopurine can cause myelosuppression, hepatotoxicity, and gastrointestinal toxicity. Advise patients to contact their healthcare provider if they experience fever, sore throat, jaundice, nausea, vomiting, signs of local infection, bleeding from any site, or symptoms suggestive of anemia [see Warnings and Precautions (5.1, 5.2, 5.3)].
Proper Preparation and Administration
Advise patients or caregivers on proper handling, storage, preparation, administration, and disposal and clean-up of accidental spillage of the medication prior to initiation and on each visit to the clinic [see Dosage and Administration (2.5)].
Embryo-Fetal Toxicity
- Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.2, 5.6), Use in Specific Populations (8.1)].
- Advise females of reproductive potential to use effective contraception during treatment with mercaptopurine and for 6 months after the last dose [see Use in Specific Populations (8.3)].
- Advise males with female partners of reproductive potential to use effective contraception during treatment with mercaptopurine and for 3 months after the last dose [see Use in Specific Populations (8.3), Nonclinical Toxicology (13.1)].
Lactation
Advise women not to breastfeed during treatment with mercaptopurine and for 1 week after the last dose [see Use in Specific Populations (8.2)].
Infertility
Advise males and females of reproductive potential that mercaptopurine can impair fertility [see Use in Specific Populations (8.3)].
Other Adverse Reactions
Instruct patients to minimize sun exposure due to risk of photosensitivity [see Adverse Reactions (6.2)].
Patients with Phenylketonuria
Inform patients with phenylketonuria that each mL of mercaptopurine oral suspension contains 0.015 mg of phenylalanine [see Warnings and Precautions (5.7)].
Distributed by:
Hikma Pharmaceuticals USA Inc.
Berkeley Heights, NJ 07922
C50001101/04
Revised November 2024
-
PATIENT INFORMATION
PATIENT INFORMATION
Mercaptopurine
(mer kapʺ toe pureʹ een)
Oral SuspensionWhat is Mercaptopurine Oral Suspension?
Mercaptopurine Oral Suspension is a prescription medicine used along with other medicines to treat people with acute lymphoblastic leukemia (ALL).What should I tell my healthcare provider before taking Mercaptopurine Oral Suspension?
Before you take Mercaptopurine Oral Suspension, tell your healthcare provider about all of your medical conditions, including if you:
- have kidney or liver problems.
- have a condition where your body produces too little of the enzyme thiopurine methyltransferase (TPMT) or the enzyme nucleotide diphosphatase (NUDT15).
- have phenylketonuria (PKU). Mercaptopurine contains phenylalanine which is a part of aspartame.
- have recently received or plan to receive a vaccine.
-
are pregnant or plan to become pregnant. Mercaptopurine Oral Suspension can harm your unborn baby.
If you are a female who is able to become pregnant: - o Your healthcare provider will do a pregnancy test before you start treatment with Mercaptopurine Oral Suspension.
- o Use an effective method of birth control (contraception) during treatment with Mercaptopurine Oral Suspension and for 6 months after your last dose. Talk with your healthcare provider about birth control methods you can use during this time.
- o Tell your healthcare provider right away if you become pregnant or think you are pregnant during treatment with Mercaptopurine Oral Suspension.
- If you are a male with a female partner who is able to become pregnant:
- o Use effective birth control (contraception) during treatment with Mercaptopurine Oral Suspension and for 3 months after your last dose.
- o Tell your healthcare provider right away if your female partner becomes pregnant or thinks she is pregnant during your treatment with Mercaptopurine Oral Suspension.
- are breastfeeding or plan to breastfeed. Do not breastfeed during treatment with Mercaptopurine Oral Suspension and for at least 1 week after your last dose.
- Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
How should I take Mercaptopurine Oral Suspension?
- See the detailed “Instructions for Use” that comes with Mercaptopurine Oral Suspension for information about the right way to measure and take a dose of Mercaptopurine Oral Suspension.
- Take Mercaptopurine Oral Suspension exactly as your healthcare provider tells you. Do not stop taking Mercaptopurine Oral Suspension or change your dose without talking to your healthcare provider.
- Take Mercaptopurine Oral Suspension by mouth 1 time each day.
- If Mercaptopurine Oral Suspension comes into contact with skin, eyes, or clothes?
- Remove contaminated clothing.
- Wash skin or eyes immediately with water.
- Contact with skin or eyes can cause hypersensitive reactions resulting in rash, redness, itching and inflammation. If symptoms appear seek medical attention.
- During treatment with Mercaptopurine Oral Suspension, your healthcare provider will do blood tests regularly to check your blood cell counts and liver function. Your healthcare provider may change your dose if you have side effects.
- If you miss a dose of Mercaptopurine Oral Suspension, call your healthcare provider for advice.
- If you take too much Mercaptopurine Oral Suspension, call your healthcare provider or go to the nearest emergency room right away.
What should I avoid while taking Mercaptopurine Oral Suspension?
Mercaptopurine Oral Suspension can make your skin more sensitive to sunlight. Protect yourself from sunlight during treatment with Mercaptopurine Oral Suspension.What are the possible side effects of Mercaptopurine Oral Suspension?
Mercaptopurine Oral Suspension can cause serious side effects, including:
- Decreased blood cell counts are common with Mercaptopurine Oral Suspension but can also be severe. Mercaptopurine Oral Suspension affects your bone marrow and can cause decreased white blood cells, red blood cells, and platelets. Decreased blood cell counts can make you more likely to develop infections, bleeding, or anemia. If you take certain medicines during treatment with Mercaptopurine Oral Suspension, it could make the effects on your bone marrow worse. Tell your healthcare provider if you develop any of the following symptoms during treatment with Mercaptopurine Oral Suspension:
- fever
- sore throat
- cuts or wounds that are red, or swollen, or are draining
- any bleeding
- tiredness or weakness
- shortness of breath
- Liver problems. Increases in liver function test results are common with Mercaptopurine Oral Suspension, but you can also develop severe liver problems with Mercaptopurine Oral Suspension that can lead to death. Your healthcare provider may tell you to stop taking Mercaptopurine Oral Suspension if you develop liver problems. Tell your healthcare provider right away if you develop any of the following symptoms of a liver problem during treatment with Mercaptopurine Oral Suspension:
- decreased appetite
- diarrhea
- nausea or vomiting
- yellowing of your skin or the whites of your eyes
- a build-up of fluid in your stomach-area (ascites)
- Possible increased risk of other cancers. Talk with your healthcare provider about your risk of other cancers if you take Mercaptopurine Oral Suspension.
- Less common side effects of Mercaptopurine Oral Suspension include: loss of appetite, nausea, vomiting, diarrhea, generally do not feel well, and rash.
Low blood sugar (hypoglycemia) can happen, especially in children under six years of age.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of Mercaptopurine Oral Suspension.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store Mercaptopurine Oral Suspension?
- Mercaptopurine Oral Suspension comes in a bottle with a child-resistant cap.
- Store Mercaptopurine Oral Suspension at 20º to 25ºC (68º to 77ºF) [see USP Controlled Room Temperature]. Store in a dry place. Do not store above 25°C.
- Store the oral dispensing syringe in a clean place, with the medicine.
- Mercaptopurine Oral Suspension should be used within 8 weeks after opening the bottle. Dispose of (throw away) any unused medicine after 8 weeks.
- Do not use after the expiry date which is stated on the carton and the bottle after ‘EXP’.
- Keep the bottle tightly closed to prevent spoilage of the medicine and reduce the risk of accidental spillage.
- Keep Mercaptopurine Oral Suspension out of the reach of children, preferably in a locked cupboard. If a child accidentally takes Mercaptopurine Oral Suspension, it could cause death.
How should I dispose of Mercaptopurine Oral Suspension?
- This medicine should not be disposed of in wastewater or household waste. Ask your pharmacist how to dispose of (throw away) Mercaptopurine Oral Suspension that is no longer needed.
General information about the safe and effective use of Mercaptopurine Oral Suspension.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use Mercaptopurine Oral Suspension for a condition for which it was not prescribed. Do not give Mercaptopurine Oral Suspension to other people, even if they have the same symptoms you have. It could harm them. You can ask your healthcare provider or pharmacist for information about Mercaptopurine Oral Suspension that is written for health professionals.What are the ingredients in Mercaptopurine Oral Suspension?
Active ingredient: mercaptopurine, USPInactive ingredients: aspartame, ethylparaben sodium, hydrochloric acid, methylparaben sodium, potassium sorbate, raspberry juice powder (raspberry juice, rice syrup solids, silicon dioxide), sodium hydroxide, sucrose, water (purified), xanthan gum.
This Patient Information has been approved by the U.S. Food and Drug Administration.
Distributed by:
Hikma Pharmaceuticals USA Inc.
Berkeley Heights, NJ 07922
C50001101/04
Revised November 2024 -
INSTRUCTIONS FOR USE
INSTRUCTIONS FOR USE
Mercaptopurine
(mer kapʺ toe pureʹ een)
Oral Suspension
20 mg/mLRead these Instructions for Use before you start taking Mercaptopurine Oral Suspension, and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
Important information about measuring Mercaptopurine Oral Suspension
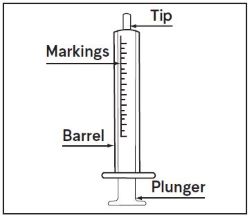
- Always use the oral dispensing syringe provided with your Mercaptopurine Oral Suspension to make sure you measure the right amount.
-
You will be provided:
- 1 bottle of Mercaptopurine Oral Suspension
- 1 bottle adapter
- 2 oral dispensing syringes (one 1 mL and one 5 mL)
If you did not receive an oral dispensing syringe with your Mercaptopurine Oral Suspension, ask your pharmacist to give you one.
You will also need disposable gloves.
Important Information You Need to Know Before Administering Mercaptopurine Oral Suspension:
1.
Wash your hands well with soap and water before and after administering a dose.
2.
Put on disposable gloves before handling Mercaptopurine Oral Suspension.
3.
Shake the bottle vigorously for at least 30 seconds to make sure that the medicine is well mixed (See Figure A).
4.
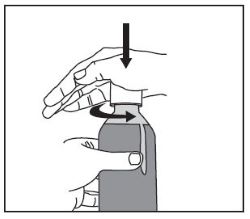
Remove the child-resistant bottle cap (See Figure B).
5.
Push the smaller end of the bottle adapter into the neck of the bottle until it is firmly in place. The bottom edge of the adapter should fully contact the top rim of the bottle (See Figure C). Do not remove the adapter from the bottle after it is inserted.
Preparing a dose of Mercaptopurine Oral Suspension:
6.
Hold the bottle upright. Remove the bottle cap by turning in the direction of the arrow (See Figure B).
7.
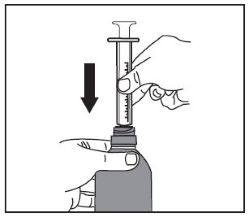
Push the tip of the oral dispensing syringe into the hole in the bottle adapter (See Figure D and Figure E).
8.
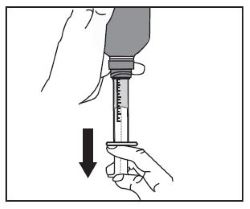
Turn the bottle upside down (See Figure F).
9.
Pull back slowly on the plunger of the oral dispensing syringe to withdraw the prescribed dose of Mercaptopurine Oral Suspension. Pull the plunger back to the mL mark on the syringe that corresponds to the dose prescribed (Figure F). If you are not sure about how much medicine to draw into the oral dispensing syringe, always ask your doctor, pharmacist or nurse for advice.
10.
Leave the oral dispensing syringe in the bottle adapter and turn the bottle right-side up. Place the bottle onto a flat surface. Hold the oral dispensing syringe by the barrel and carefully remove it from the adapter. Do not hold the oral dispensing syringe by the plunger, because the plunger may come out.
11.
Place the tip of the oral dispensing syringe in your mouth and aim the tip toward the inside of your cheek.
12.
Gently squirt the Mercaptopurine Oral Suspension into your mouth by pushing on the plunger until the oral dispensing syringe is empty. Swallow the medicine.
- Do not forcefully push on the plunger.
-
Do not squirt the medicine to the back of your mouth or throat. This may cause you to choke.
13.
Remove the oral dispensing syringe from your mouth.
14.
Swallow the dose of oral suspension then drink some water, making sure no medicine is left in your mouth.
15.
Put the cap back on the bottle with the adapter left in place. Close the cap tightly.
16.
Wash the oral dispensing syringe with warm soapy water and rinse well. Hold the oral dispensing syringe under water and move the plunger up and down several times to make sure the inside of the oral dispensing syringe is clean. Let the oral dispensing syringe dry completely before you use it again for dosing. Do not throw away the oral dispensing syringe after use.
Ingredients in Mercaptopurine Oral SuspensionActive ingredient: mercaptopurine, USP
Inactive ingredients: aspartame, ethylparaben sodium, hydrochloric acid, methylparaben sodium, potassium sorbate, raspberry juice powder (raspberry juice, rice syrup solids, silicon dioxide), sodium hydroxide, sucrose, water (purified), xanthan gum.
Storing Mercaptopurine Oral Suspension
- Store Mercaptopurine Oral Suspension at 20º to 25ºC (68º to 77ºF) [see USP Controlled Room Temperature]. Store in a dry place. Do not store above 25°C.
- Store the oral dispensing syringe in a clean place, with the medicine.
- Mercaptopurine Oral Suspension should be used within 8 weeks after opening the bottle. Dispose of (throw away) any unused medicine after 8 weeks.
- Do not use after the expiry date which is stated on the carton and the bottle after ‘EXP’.
- Keep the bottle tightly closed to prevent spoilage of the medicine and reduce the risk of accidental spillage.
- Keep Mercaptopurine Oral Suspension and all medicines out of the reach of children, preferably in a locked cupboard. If a child accidentally takes Mercaptopurine Oral Suspension, it could cause death. Ask your pharmacist how to dispose of (throw away) Mercaptopurine Oral Suspension that is no longer needed.
Disposing of Mercaptopurine Oral Suspension- Ask your pharmacist how to dispose of Mercaptopurine Oral Suspension that is expired or no longer required. Medicines should not be disposed of via wastewater or household waste.
Clean Up Spillage of Mercaptopurine Oral Suspension
Use appropriate personal protective equipment (disposable gloves and eye protection). Mop up and contain spill material in a compatible container. Wash your hands thoroughly afterwards.Mercaptopurine Oral Suspension Contact with Skin, Eyes, or Clothes
- Remove and launder contaminated clothing.
- Wash skin or eyes immediately with water.
Contact with skin or eyes can cause hypersensitive reactions resulting in rash, redness, itching and inflammation. If symptoms appear, seek medical attention.
This “Instructions for Use” has been approved by the U.S. Food and Drug Administration.
Distributed by:
Hikma Pharmaceuticals USA Inc.
Berkeley Heights, NJ 07922
C50001101/04
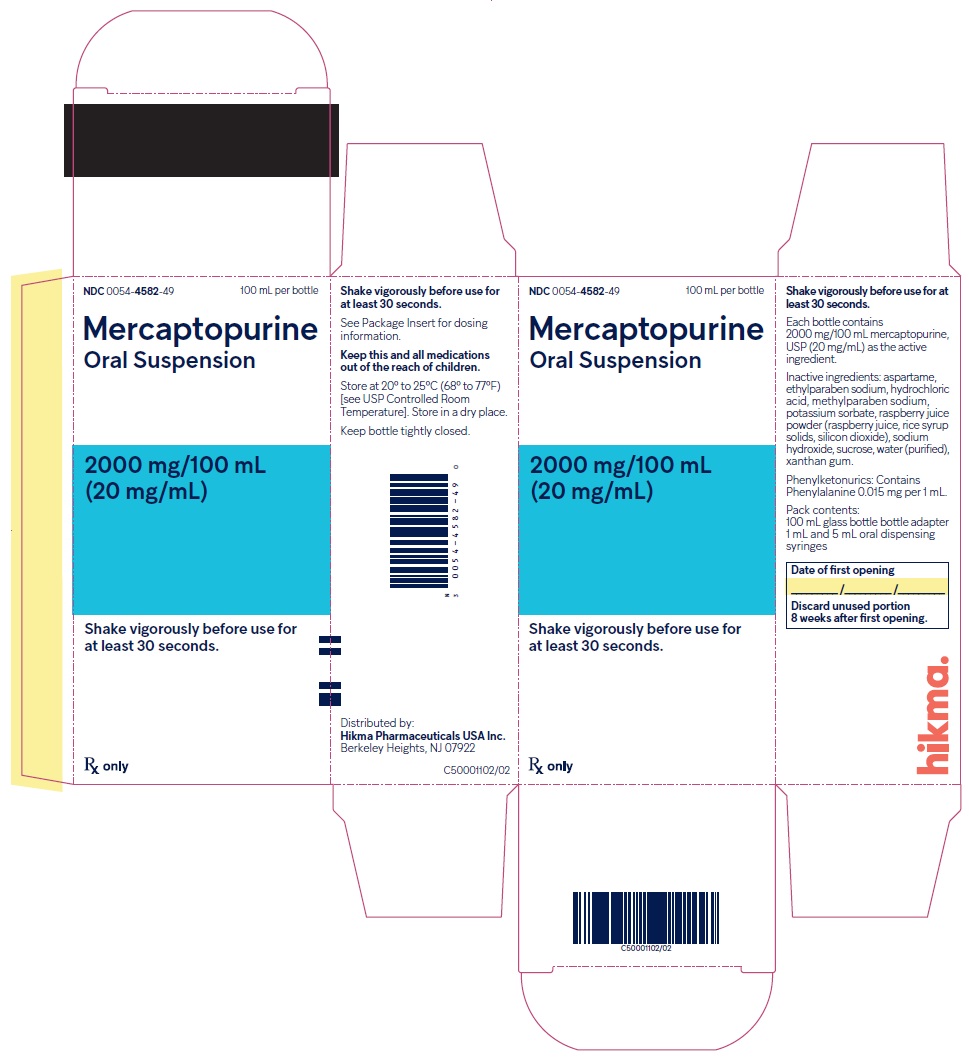
Revised November 2024 - PRINCIPAL DISPLAY PANEL – Bottle Carton
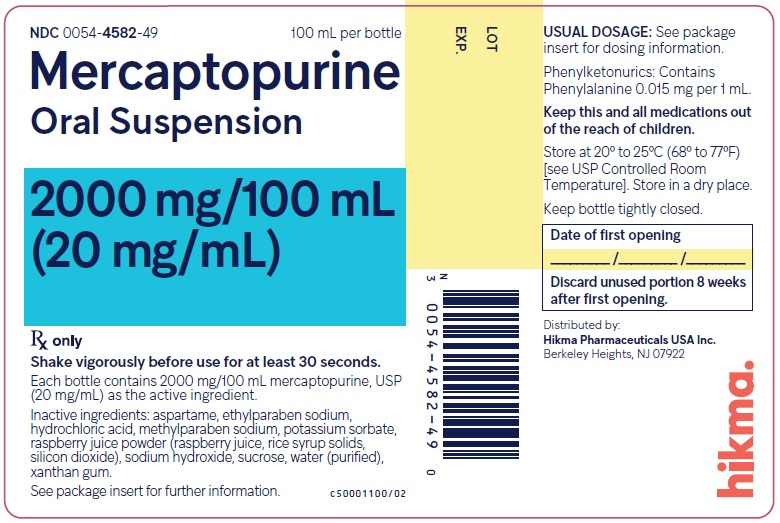
- PRINCIPAL DISPLAY PANEL – Bottle Label
-
INGREDIENTS AND APPEARANCE
MERCAPTOPURINE
mercaptopurine suspensionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0054-4582 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MERCAPTOPURINE (UNII: E7WED276I5) (MERCAPTOPURINE ANHYDROUS - UNII:PKK6MUZ20G) MERCAPTOPURINE 20 mg in 1 mL Inactive Ingredients Ingredient Name Strength ASPARTAME (UNII: Z0H242BBR1) ETHYLPARABEN SODIUM (UNII: Z0D00IVA10) HYDROCHLORIC ACID (UNII: QTT17582CB) METHYLPARABEN SODIUM (UNII: CR6K9C2NHK) POTASSIUM SORBATE (UNII: 1VPU26JZZ4) RASPBERRY JUICE (UNII: 427AYI9PDE) CORN SYRUP (UNII: 9G5L16BK6N) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) SODIUM HYDROXIDE (UNII: 55X04QC32I) SUCROSE (UNII: C151H8M554) WATER (UNII: 059QF0KO0R) XANTHAN GUM (UNII: TTV12P4NEE) Product Characteristics Color PINK (Pink to Brown) Score Shape Size Flavor RASPBERRY Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0054-4582-49 1 in 1 CARTON 02/26/2025 1 100 mL in 1 BOTTLE, GLASS; Type 1: Convenience Kit of Co-Package Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA216418 02/26/2025 Labeler - Hikma Pharmaceuticals USA Inc. (080189610) Establishment Name Address ID/FEI Business Operations West-Ward Columbus Inc. 058839929 MANUFACTURE(0054-4582)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.