APOQUEL- oclacitinib maleate tablet, coated
Apoquel by
Drug Labeling and Warnings
Apoquel by is a Animal medication manufactured, distributed, or labeled by Zoetis Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
- Caution
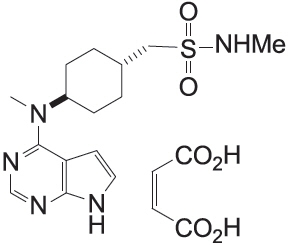
- Description
- Indications
-
Dosage and Administration
The dose of APOQUEL (oclacitinib maleate) tablets is 0.18 to 0.27 mg oclacitinib/lb (0.4 to 0.6 mg oclacitinib/kg) body weight, administered orally, twice daily for up to 14 days, and then administered once daily for maintenance therapy. APOQUEL may be administered with or without food.
Dosing Chart Weight Range
(in lb)Weight Range
(in Kg)Number of Tablets to be Administered Low High Low High 3.6 mg Tablets 5.4 mg Tablets 16 mg Tablets 6.6 9.9 3.0 4.4 0.5 - - 10.0 14.9 4.5 5.9 - 0.5 - 15.0 19.9 6.0 8.9 1 - - 20.0 29.9 9.0 13.4 - 1 - 30.0 44.9 13.5 19.9 - - 0.5 45.0 59.9 20.0 26.9 - 2 - 60.0 89.9 27.0 39.9 - - 1 90.0 129.9 40.0 54.9 - - 1.5 130.0 175.9 55.0 80.0 - - 2 -
Warnings
APOQUEL is not for use in dogs less than 12 months of age (see Animal Safety).
APOQUEL is not for use in dogs with serious infections.
APOQUEL may increase susceptibility to infection, including demodicosis, and exacerbate neoplastic conditions (see Adverse Reactions and Animal Safety).
-
Human Warnings
This product is not for human use. Keep this and all drugs out of reach of children. For use in dogs only. Wash hands immediately after handling the tablets. In case of accidental eye contact, flush immediately with water or saline for at least 15 minutes and then seek medical attention. In case of accidental ingestion, seek medical attention immediately.
-
Precautions
APOQUEL is not for use in breeding dogs, or pregnant or lactating bitches.
The use of APOQUEL has not been evaluated in combination with glucocorticoids, cyclosporine, or other systemic immunosuppressive agents.
Dogs receiving APOQUEL should be monitored for the development of infections, including demodicosis, and neoplasia.
-
Adverse Reactions
Control of Atopic Dermatitis
In a masked field study to assess the effectiveness and safety of oclacitinib for the control of atopic dermatitis in dogs, 152 dogs treated with APOQUEL and 147 dogs treated with placebo (vehicle control) were evaluated for safety. The majority of dogs in the placebo group withdrew from the 112-day study by Day 16. Adverse reactions reported (and percent of dogs affected) during Days 0-16 included diarrhea (4.6% APOQUEL, 3.4% placebo), vomiting (3.9% APOQUEL, 4.1% placebo), anorexia (2.6% APOQUEL, 0% placebo), new cutaneous or subcutaneous lump (2.6% APOQUEL, 2.7% placebo), and lethargy (2.0% APOQUEL, 1.4% placebo). In most cases, diarrhea, vomiting, anorexia, and lethargy spontaneously resolved with continued dosing. Dogs on APOQUEL had decreased leukocytes (neutrophil, eosinophil, and monocyte counts) and serum globulin, and increased cholesterol and lipase compared to the placebo group but group means remained within the normal range. Mean lymphocyte counts were transiently increased at Day 14 in the APOQUEL group.
Dogs that withdrew from the masked field study could enter an unmasked study where all dogs received APOQUEL. Between the masked and unmasked study, 283 dogs received at least one dose of APOQUEL. Of these 283 dogs, two dogs were withdrawn from study due to suspected treatment-related adverse reactions: one dog that had an intense flare-up of dermatitis and severe secondary pyoderma after 19 days of APOQUEL administration, and one dog that developed generalized demodicosis after 28 days of APOQUEL administration. Two other dogs on APOQUEL were withdrawn from study due to suspected or confirmed malignant neoplasia and subsequently euthanized, including one dog that developed signs associated with a heart base mass after 21 days of APOQUEL administration, and one dog that developed a Grade III mast cell tumor after 60 days of APOQUEL administration.
One of the 147 dogs in the placebo group developed a Grade I mast cell tumor and was withdrawn from the masked study. Additional dogs receiving APOQUEL were hospitalized for diagnosis and treatment of pneumonia (one dog), transient bloody vomiting and stool (one dog), and cystitis with urolithiasis (one dog).
In the 283 dogs that received APOQUEL, the following additional clinical signs were reported after beginning APOQUEL (percentage of dogs with at least one report of the clinical sign as a non-pre-existing finding): pyoderma (12.0%), non-specified dermal lumps (12.0%), otitis (9.9%), vomiting (9.2%), diarrhea (6.0%), histiocytoma (3.9%), cystitis (3.5%), anorexia (3.2%), lethargy (2.8%), yeast skin infections (2.5%), pododermatitis (2.5%), lipoma (2.1%), polydipsia (1.4%), lymphadenopathy (1.1%), nausea (1.1%), increased appetite (1.1%), aggression (1.1%), and weight loss (0.7).
Control of Pruritus Associated with Allergic Dermatitis
In a masked field study to assess the effectiveness and safety of oclacitinib for the control of pruritus associated with allergic dermatitis in dogs, 216 dogs treated with APOQUEL and 220 dogs treated with placebo (vehicle control) were evaluated for safety. During the 30-day study, there were no fatalities and no adverse reactions requiring hospital care. Adverse reactions reported (and percent of dogs affected) during Days 0-7 included diarrhea (2.3% APOQUEL, 0.9% placebo), vomiting (2.3% APOQUEL, 1.8% placebo), lethargy (1.8% APOQUEL, 1.4% placebo), anorexia (1.4% APOQUEL, 0% placebo), and polydipsia (1.4% APOQUEL, 0% placebo). In most of these cases, signs spontaneously resolved with continued dosing. Five APOQUEL group dogs were withdrawn from study because of: darkening areas of skin and fur (1 dog); diarrhea (1 dog); fever, lethargy and cystitis (1 dog); an inflamed footpad and vomiting (1 dog); and diarrhea, vomiting, and lethargy (1 dog). Dogs in the APOQUEL group had a slight decrease in mean white blood cell counts (neutrophil, eosinophil, and monocyte counts) that remained within the normal reference range. Mean lymphocyte count for dogs in the APOQUEL group increased at Day 7, but returned to pretreatment levels by study end without a break in APOQUEL administration. Serum cholesterol increased in 25% of APOQUEL group dogs, but mean cholesterol remained within the reference range.
Continuation Field Study
After completing APOQUEL field studies, 239 dogs enrolled in an unmasked (no placebo control), continuation therapy study receiving APOQUEL for an unrestricted period of time. Mean time on this study was 372 days (range 1 to 610 days). Of these 239 dogs, one dog developed demodicosis following 273 days of APOQUEL administration. One dog developed dermal pigmented viral plaques following 266 days of APOQUEL administration. One dog developed a moderately severe bronchopneumonia after 272 days of APOQUEL administration; this infection resolved with antimicrobial treatment and temporary discontinuation of APOQUEL. One dog was euthanized after developing abdominal ascites and pleural effusion of unknown etiology after 450 days of APOQUEL administration. Six dogs were euthanized because of suspected malignant neoplasms: including thoracic metastatic, abdominal metastatic, splenic, frontal sinus, and intracranial neoplasms, and transitional cell carcinoma after 17, 120, 175, 49, 141, and 286 days of APOQUEL administration, respectively. Two dogs each developed a Grade II mast cell tumor after 52 and 91 days of APOQUEL administration, respectively. One dog developed low grade B-cell lymphoma after 392 days of APOQUEL administration. Two dogs each developed an apocrine gland adenocarcinoma (one dermal, one anal sac) after approximately 210 and 320 days of APOQUEL administration, respectively. One dog developed a low grade oral spindle cell sarcoma after 320 days of APOQUEL administration.
To report suspected adverse events, for technical assistance or to obtain a copy of the SDS, contact Zoetis Inc. at 1-888-963-8471 or www.zoetis.com.
For additional information about adverse drug experience reporting for animal drugs, contact FDA at 1-888-FDA-VETS or online at http://www.fda.gov/AnimalVeterinary/SafetyHealth.
-
Clinical Pharmacology
Mechanism of action
Oclacitinib inhibits the function of a variety of pruritogenic cytokines and pro-inflammatory cytokines, as well as cytokines involved in allergy that are dependent on JAK1 or JAK3 enzyme activity. It has little effect on cytokines involved in hematopoiesis that are dependent on JAK2. Oclacitinib is not a corticosteroid or an antihistamine.
Pharmacokinetics
In dogs, oclacitinib maleate is rapidly and well absorbed following oral administration, with mean time to peak plasma concentrations (Tmax) of less than 1 hour. Following oral administration of 0.4-0.6 mg oclacitinib/kg to 24 dogs, the mean (90% confidence limits [CL]) maximum concentration (Cmax) was 324 (281, 372) ng/mL and the mean area under the plasma concentration-time curve from 0 and extrapolated to infinity (AUC0-inf) was 1890 (1690, 2110) ng∙hr/mL. The prandial state of dogs does not significantly affect the rate or extent of absorption. The absolute bioavailability of oclacitinib maleate was 89%.
Oclacitinib has low protein binding with 66.3-69.7% bound in fortified canine plasma at nominal concentrations ranging from 10-1000 ng/mL. The apparent mean (95% CL) volume of distribution at steady-state was 942 (870, 1014) mL/kg body weight.
Oclacitinib is metabolized in the dog to multiple metabolites and one major oxidative metabolite was identified in plasma and urine. Overall the major clearance route is metabolism with minor contributions from renal and biliary elimination. Inhibition of canine cytochrome P450 enzymes by oclacitinib is minimal; the inhibitory concentrations (IC50s) are 50 fold greater than the observed Cmax values at the use dose.
Mean (95% CL) total body oclacitinib clearance from plasma was low – 316 (237, 396) mL/h/kg body weight (5.3 mL/min/kg body weight). Following IV and PO administration, the terminal t1/2 appeared similar with mean values of 3.5 (2.2, 4.7) and 4.1 (3.1, 5.2) hours, respectively.
-
Effectiveness
Control of Atopic Dermatitis
A double-masked, 112-day, controlled study was conducted at 18 U.S. veterinary hospitals. The study enrolled 299 client-owned dogs with atopic dermatitis. Dogs were randomized to treatment with APOQUEL (152 dogs: tablets administered at a dose of 0.4-0.6 mg/kg per dose twice daily for 14 days and then once daily) or placebo (147 dogs: vehicle control, tablets administered on the same schedule). During the study, dogs could not be treated with other drugs that could affect the assessment of effectiveness, such as corticosteroids, anti-histamines, or cyclosporine. Treatment success for pruritus for each dog was defined as at least a 2 cm decrease from baseline on a 10 cm visual analog scale (VAS) in pruritus, assessed by the Owner, on Day 28. Treatment success for skin lesions was defined as a 50% decrease from the baseline Canine Atopic Dermatitis Extent and Severity Index (CADESI) score, assessed by the Veterinarian, on Day 28. The estimated proportion of dogs with Treatment Success in Owner-assessed pruritus VAS score and in Veterinarian-assessed CADESI score was greater and significantly different for the APOQUEL group compared to the placebo group.
Estimated Proportion of Dogs with Treatment Success, Atopic Dermatitis Effectiveness Parameter APOQUEL Placebo P-value Owner-Assessed Pruritus VAS 0.66
(n = 131)0.04
(n = 133)p<0.0001 Veterinarian-Assessed CADESI 0.49
(n = 134)0.04
(n = 134)p<0.0001 Compared to the placebo group, mean Owner-assessed pruritus VAS scores (on Days 1, 2, 7, 14, and 28) and Veterinarian-assessed CADESI scores (on Days 14 and 28) were lower (improved) in dogs in the APOQUEL group. By Day 30, 86% (127/147) of the placebo group dogs and 15% (23/152) of the APOQUEL group dogs withdrew from the masked study because of worsening clinical signs, and had the option to enroll in an unmasked study and receive APOQUEL. For dogs that continued APOQUEL treatment beyond one month, the mean Owner-assessed pruritus VAS scores and Veterinarian-assessed CADESI scores continued to improve through study end at Day 112.
Control of Pruritus Associated with Allergic Dermatitis
A double-masked, 30-day, controlled study was conducted at 26 U.S. veterinary hospitals. The study enrolled 436 client-owned dogs with a history of allergic dermatitis attributed to one or more of the following conditions: atopic dermatitis, flea allergy, food allergy, contact allergy, and other/unspecified allergic dermatitis. Dogs were randomized to treatment with APOQUEL (216 dogs: tablets administered at a dose of 0.4-0.6 mg/kg twice daily) or placebo (220 dogs: vehicle control, tablets administered twice daily). During the study, dogs could not be treated with other drugs that could affect the assessment of pruritus or dermal inflammation such as corticosteroids, anti-histamines, or cyclosporine. Treatment success for each dog was defined as at least a 2 cm decrease from baseline on a 10 cm visual analog scale (VAS) in pruritus, assessed by the Owner, on at least 5 of the 7 evaluation days. The estimated proportion of dogs with Treatment Success was greater and significantly different for the APOQUEL group compared to the placebo group.
Owner-Assessed Pruritus VAS Treatment Success, Allergic Dermatitis Effectiveness Parameter APOQUEL
(n = 203)Placebo
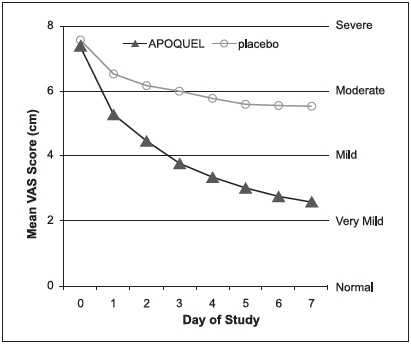
(n = 204)P-value Estimated Proportion of Dogs with Treatment Success 0.67 0.29 p<0.0001 After one week of treatment, 86.4% of APOQUEL group dogs compared with 42.5% of placebo group dogs had achieved a 2 cm reduction on the 10 cm Owner-assessed pruritus VAS. On each of the 7 days, mean Owner-assessed pruritus VAS scores were lower in dogs in the APOQUEL group (See Figure 1). Veterinarians used a 10 cm VAS scale to assess each dog's dermatitis. After one week of treatment, the mean Veterinarian-assessed VAS dermatitis score for the dogs in the APOQUEL group was lower at 2.2 cm (improved from a baseline value of 6.2 cm) compared with the placebo group mean score of 4.9 cm (from a baseline value of 6.2 cm). For dogs that continued APOQUEL treatment beyond one week, the Veterinarian-assessed dermatitis scores continued to improve through study end at Day 30.
Figure 1: Owner Assessed Pruritus VAS Scores by treatment for Days 0-7
-
Animal Safety
Margin of Safety in 12 Month Old Dogs
Oclacitinib maleate was administered to healthy, one-year-old Beagle dogs twice daily for 6 weeks, followed by once daily for 20 weeks, at 0.6 mg/kg (1X maximum exposure dose, 8 dogs), 1.8 mg/kg (3X, 8 dogs), and 3.0 mg/kg (5X, 8 dogs) oclacitinib for 26 weeks. Eight dogs received placebo (empty gelatin capsule) at the same dosage schedule. Clinical observations that were considered likely to be related to oclacitinib maleate included papillomas and a dose-dependent increase in the number and frequency of interdigital furunculosis (cysts) on one or more feet during the study. Additional clinical observations were primarily related to the interdigital furunculosis and included dermatitis (local alopecia, erythema, abrasions, scabbing/crusts, and edema of feet) and lymphadenopathy of peripheral nodes. Microscopic findings considered to be oclacitinib maleate-related included decreased cellularity (lymphoid) in Gut-Associated Lymphoid Tissue (GALT), spleen, thymus, cervical and mesenteric lymph node; and decreased cellularity of sternal and femoral bone marrow. Lymphoid hyperplasia and chronic active inflammation was seen in lymph nodes draining feet affected with interdigital furunculosis. Five oclacitinib maleate-treated dogs had microscopic evidence of mild interstitial pneumonia.
Clinical pathology findings considered to be oclacitinib maleate-related included mild, dose-dependent reduction in hemoglobin, hematocrit, and reticulocyte counts during the twice daily dosing period with decreases in the leukocyte subsets of lymphocytes, eosinophils, and basophils. Total proteins were decreased over time primarily due to the albumin fraction.
Vaccine Response Study
An adequate immune response (serology) to killed rabies (RV), modified live canine distemper virus (CDV), and modified live canine parvovirus (CPV) vaccination was achieved in eight 16-week old vaccine naïve puppies that were administered oclacitinib maleate at 1.8 mg/kg oclacitinib (3X maximum exposure dose) twice daily for 84 days. For modified live canine parainfluenza virus (CPI), < 80% (6 of 8) of the dogs achieved adequate serologic response. Clinical observations that were considered likely to be related to oclacitinib maleate treatment included enlarged lymph nodes, interdigital furunculosis, cysts, and pododermatitis. One oclacitinib maleate-treated dog (26-weeks-old) was euthanized on Day 74 after physical examination revealed the dog to be febrile, lethargic, with pale mucous membranes and frank blood in stool. Necropsy revealed pneumonia of short duration and evidence of chronic lymphadenitis of mesenteric lymph nodes. During the three month recovery phase to this study, one oclacitinib maleate-treated dog (32-weeks old) was euthanized on Day 28 due to clinical signs which included enlarged prescapular lymph nodes, bilateral epiphora, lethargy, mild dyspnea, and fever. The dog showed an elevated white blood cell (WBC) count. Necropsy revealed lesions consistent with sepsis secondary to immunosuppression. Bone marrow hyperplasia was consistent with response to sepsis.
Margin of Safety in 6 Month Old Dogs
A margin of safety study in 6-month-old dogs was discontinued after four months due to the development of bacterial pneumonia and generalized demodex mange infections in dogs in the high dose (3X and 5X) treatment groups, dosed at 1.8 and 3.0 mg/kg oclacitinib twice daily, for the entire study.
- Storage Conditions
- How Supplied:
- SPL UNCLASSIFIED SECTION
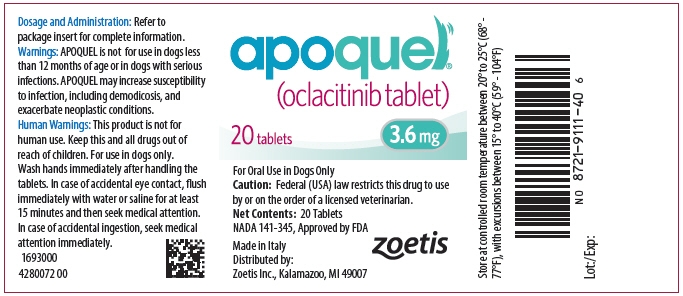
- PRINCIPAL DISPLAY PANEL - 3.6 mg Tablet Bottle Label
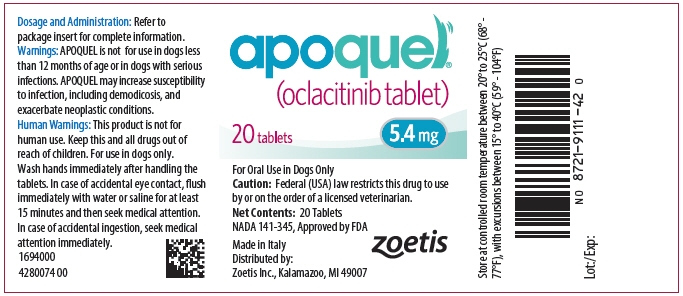
- PRINCIPAL DISPLAY PANEL - 5.4 mg Tablet Bottle Label
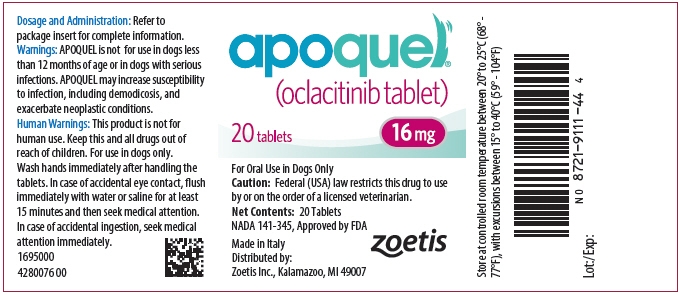
- PRINCIPAL DISPLAY PANEL - 16 mg Tablet Bottle Label
-
INGREDIENTS AND APPEARANCE
APOQUEL
oclacitinib maleate tablet, coatedProduct Information Product Type PRESCRIPTION ANIMAL DRUG Item Code (Source) NDC: 54771-8721 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OCLACITINIB MALEATE (UNII: VON733L42A) (OCLACITINIB - UNII:99GS5XTB51) OCLACITINIB MALEATE 3.6 mg Product Characteristics Color WHITE Score 2 pieces Shape OVAL Size 10mm Flavor Imprint Code AQ;S Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54771-8721-1 20 in 1 BOTTLE 2 NDC: 54771-8721-2 100 in 1 BOTTLE 3 NDC: 54771-8721-3 250 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NADA NADA141345 01/20/2014 APOQUEL
oclacitinib maleate tablet, coatedProduct Information Product Type PRESCRIPTION ANIMAL DRUG Item Code (Source) NDC: 54771-8722 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OCLACITINIB MALEATE (UNII: VON733L42A) (OCLACITINIB - UNII:99GS5XTB51) OCLACITINIB MALEATE 5.4 mg Product Characteristics Color WHITE Score 2 pieces Shape OVAL Size 11mm Flavor Imprint Code AQ;M Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54771-8722-1 20 in 1 BOTTLE 2 NDC: 54771-8722-2 100 in 1 BOTTLE 3 NDC: 54771-8722-3 250 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NADA NADA141345 01/20/2014 APOQUEL
oclacitinib maleate tablet, coatedProduct Information Product Type PRESCRIPTION ANIMAL DRUG Item Code (Source) NDC: 54771-8723 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OCLACITINIB MALEATE (UNII: VON733L42A) (OCLACITINIB - UNII:99GS5XTB51) OCLACITINIB MALEATE 16 mg Product Characteristics Color WHITE Score 2 pieces Shape OVAL Size 16mm Flavor Imprint Code AQ;L Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54771-8723-1 20 in 1 BOTTLE 2 NDC: 54771-8723-2 100 in 1 BOTTLE 3 NDC: 54771-8723-3 250 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NADA NADA141345 01/20/2014 Labeler - Zoetis Inc. (828851555)
Trademark Results [Apoquel]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 APOQUEL 97768338 not registered Live/Pending |
Zoetis Services LLC 2023-01-25 |
 APOQUEL 77820385 3861904 Live/Registered |
ZOETIS SERVICES LLC 2009-09-04 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.