PHESGO- pertuzumab, trastuzumab, and hyaluronidase-zzxf injection, solution
Phesgo by
Drug Labeling and Warnings
Phesgo by is a Prescription medication manufactured, distributed, or labeled by Genentech, Inc., Roche Diagnostics GmbH, F. Hoffmann-La Roche AG, Genentech, Inc. (Oceanside), Roche Singapore Technical Operations Pte. Ltd. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PHESGO safely and effectively. See full prescribing information for PHESGO.
PHESGO® (pertuzumab, trastuzumab, and hyaluronidase-zzxf) injection, for subcutaneous use
Initial U.S. Approval: 2020WARNING: CARDIOMYOPATHY, EMBRYO-FETAL TOXICITY, and PULMONARY TOXICITY
See full prescribing information for complete boxed warning.
Cardiomyopathy: PHESGO administration can result in subclinical and clinical cardiac failure manifesting as CHF, and decreased LVEF, with greatest risk when administered concurrently with anthracyclines. Evaluate cardiac function prior to and during treatment. Discontinue PHESGO for cardiomyopathy. (2.3, 5.1)
Embryo-fetal Toxicity: Exposure to PHESGO can result in embryo-fetal death and birth defects. Advise patients of these risks and the need for effective contraception. (5.2, 8.1, 8.3)
Pulmonary Toxicity: Discontinue PHESGO for anaphylaxis, angioedema, interstitial pneumonitis, or acute respiratory distress syndrome. (5.3)
INDICATIONS AND USAGE
PHESGO is a combination of pertuzumab and trastuzumab, HER2/neu receptor antagonists, and hyaluronidase, an endoglycosidase, indicated for:
- Use in combination with chemotherapy as:
- neoadjuvant treatment of patients with HER2-positive, locally advanced, inflammatory, or early stage breast cancer (either greater than 2 cm in diameter or node positive) as part of a complete treatment regimen for early breast cancer. (1.1)
- adjuvant treatment of patients with HER2-positive early breast cancer at high risk of recurrence (1.1)
- Use in combination with docetaxel for treatment of patients with HER2-positive metastatic breast cancer (MBC) who have not received prior anti-HER2 therapy or chemotherapy for metastatic disease. (1.2)
DOSAGE AND ADMINISTRATION
- For subcutaneous use in the thigh only. (2.2)
- PHESGO has different dosage and administration instructions than intravenous pertuzumab and trastuzumab products. (2.2)
- Do not administer intravenously. (2.2)
- Perform HER2 testing using FDA-approved tests by laboratories with demonstrated proficiency. (1, 2.1)
- The initial dose of PHESGO is 1,200 mg pertuzumab, 600 mg trastuzumab, and 30,000 units hyaluronidase administered subcutaneously over approximately 8 minutes, followed every 3 weeks by a dose of 600 mg pertuzumab, 600 mg trastuzumab, and 20,000 units hyaluronidase administered subcutaneously over approximately 5 minutes. (2.2)
- Neoadjuvant: administer PHESGO by subcutaneous injection every 3 weeks and chemotherapy by intravenous infusion preoperatively for 3 to 6 cycles. (2.2)
- Adjuvant: administer PHESGO by subcutaneous injection every 3 weeks and chemotherapy by intravenous infusion postoperatively for a total of 1 year (up to 18 cycles). (2.2)
- MBC: administer PHESGO by subcutaneous injection and docetaxel by intravenous infusion every 3 weeks. (2.2)
DOSAGE FORMS AND STRENGTHS
Injection:
- 1,200 mg pertuzumab, 600 mg trastuzumab, and 30,000 units hyaluronidase/15 mL (80 mg, 40 mg, and 2,000 units/mL) of solution in a single-dose vial. (3)
- 600 mg pertuzumab, 600 mg trastuzumab, and 20,000 units hyaluronidase/10 mL (60 mg, 60 mg, and 2,000 units/mL) of solution in a single-dose vial. (3)
CONTRAINDICATIONS
PHESGO is contraindicated in patients with known hypersensitivity to pertuzumab, or trastuzumab, or hyaluronidase, or to any of its excipients. (4)
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
Neoadjuvant and Adjuvant Treatment of Breast Cancer
- The most common adverse reactions (>30%) with PHESGO were alopecia, nausea, diarrhea, anemia, and asthenia. (6.1)
Metastatic Breast Cancer (based on intravenous pertuzumab)
- The most common adverse reactions (> 30%) with pertuzumab in combination with trastuzumab and docetaxel were diarrhea, alopecia, neutropenia, nausea, fatigue, rash, and peripheral neuropathy. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Genentech at 1-888-835-2555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
Females and Males of Reproductive Potential: Verify the pregnancy status of females prior to initiation of PHESGO. (8.3)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 11/2024
- Use in combination with chemotherapy as:
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: CARDIOMYOPATHY, EMBRYO-FETAL TOXICITY, and PULMONARY TOXICITY
1 INDICATIONS AND USAGE
1.1 Early Breast Cancer (EBC)
1.2 Metastatic Breast Cancer (MBC)
2 DOSAGE AND ADMINISTRATION
2.1 Patient Selection
2.2 Important Dosage and Administration Information
2.3 Recommended Doses and Schedules
2.4 Dose Modification
2.5 Preparation for Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiomyopathy
5.2 Embryo-Fetal Toxicity
5.3 Pulmonary Toxicity
5.4 Exacerbation of Chemotherapy-Induced Neutropenia
5.5 Hypersensitivity and Administration-Related Reactions
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.6 Immunogenicity
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Neoadjuvant and Adjuvant Treatment of Breast Cancer
14.2 Metastatic Breast Cancer
14.3 Patient Experience
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: CARDIOMYOPATHY, EMBRYO-FETAL TOXICITY, and PULMONARY TOXICITY
Cardiomyopathy
PHESGO administration can result in subclinical and clinical cardiac failure. The incidence and severity were highest in patients receiving PHESGO with anthracycline-containing chemotherapy regimens. Evaluate cardiac function prior to and during treatment with PHESGO. Discontinue PHESGO treatment in patients receiving adjuvant therapy and withhold PHESGO in patients with metastatic disease for clinically significant decrease in left ventricular function [see Dosage and Administration (2.3) and Warnings and Precautions (5.1)].
Embryo-fetal Toxicity
Exposure to PHESGO can result in embryo-fetal death and birth defects, including oligohydramnios and oligohydramnios sequence manifesting as pulmonary hypoplasia, skeletal abnormalities, and neonatal death. Advise patients of these risks and the need for effective contraception [see Warnings and Precautions (5.2) and Use in Specific Populations (8.1), (8.3)].
Pulmonary Toxicity
PHESGO administration can result in serious and fatal pulmonary toxicity. Discontinue PHESGO for anaphylaxis, angioedema, interstitial pneumonitis, or acute respiratory distress syndrome. Monitor patients until symptoms completely resolve [see Warnings and Precautions (5.3)].
-
1 INDICATIONS AND USAGE
1.1 Early Breast Cancer (EBC)
PHESGO is indicated for use in combination with chemotherapy for
- the neoadjuvant treatment of adult patients with HER2-positive, locally advanced, inflammatory, or early stage breast cancer (either greater than 2 cm in diameter or node positive) as part of a complete treatment regimen for early breast cancer [see Dosage and Administration (2.2) and Clinical Studies (14.2)].
- the adjuvant treatment of adult patients with HER2-positive early breast cancer at high risk of recurrence [see Dosage and Administration (2.2) and Clinical Studies (14.2)].
Select patients for therapy based on an FDA-approved companion diagnostic test [see Dosage and Administration (2.1)].
1.2 Metastatic Breast Cancer (MBC)
PHESGO is indicated for use in combination with docetaxel for the treatment of adult patients with HER2-positive metastatic breast cancer who have not received prior anti-HER2 therapy or chemotherapy for metastatic disease [see Dosage and Administration (2.2) and Clinical Studies (14.1)].
Select patients for therapy based on an FDA-approved companion diagnostic test [see Dosage and Administration (2.1)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Patient Selection
Select patients based on HER2 protein overexpression or HER2 gene amplification in tumor specimens [see Indications and Usage (1) and Clinical Studies (14)]. Assessment of HER2 protein overexpression and HER2 gene amplification should be performed using FDA-approved tests specific for breast cancer by laboratories with demonstrated proficiency. Information on the FDA-approved tests for the detection of HER2 protein overexpression and HER2 gene amplification is available at: http://www.fda.gov/CompanionDiagnostics.
Improper assay performance, including use of suboptimally fixed tissue, failure to utilize specified reagents, deviation from specific assay instructions, and failure to include appropriate controls for assay validation, can lead to unreliable results.
2.2 Important Dosage and Administration Information
PHESGO is for subcutaneous use only in the thigh. Do not administer intravenously.
PHESGO has different dosage and administration instructions than intravenous pertuzumab, intravenous trastuzumab, and subcutaneous trastuzumab when administered alone.
Do not substitute PHESGO for or with pertuzumab, trastuzumab, ado-trastuzumab emtansine, or fam-trastuzumab deruxtecan.
PHESGO must always be administered by a healthcare professional.
In patients receiving an anthracycline-based regimen for early breast cancer, administer PHESGO following completion of the anthracycline.
In patients receiving PHESGO for early breast cancer with docetaxel or paclitaxel, administer docetaxel or paclitaxel after PHESGO.
In patients receiving PHESGO for metastatic breast cancer with docetaxel, administer docetaxel after PHESGO.
Observe patients for a minimum of 30 minutes after initial dose of PHESGO and 15 minutes after each maintenance dose of PHESGO for signs or hypersensitivity symptoms or administration-related reactions. Medications to treat such reactions, as well as emergency equipment, should be available for immediate use [see Warnings and Precautions (5.5)].
2.3 Recommended Doses and Schedules
The recommended dosage and administration schedule for PHESGO are shown in Table 1.
Table 1: Recommended Dosage and Administration Schedule Dose Strength Administration Instructions Initial dose 1,200 mg pertuzumab, 600 mg trastuzumab, and 30,000 units hyaluronidase in 15 mL Administer subcutaneously over approximately 8 minutes (1,200 mg, 600 mg, and 30,000 units/15 mL) Maintenance dose (administer every 3 weeks) 600 mg pertuzumab, 600 mg trastuzumab, and 20,000 units hyaluronidase in 10 mL
(600 mg, 600 mg, and 20,000 units/10 mL)Administer subcutaneously over approximately 5 minutes every 3 weeks No dose adjustments for PHESGO are required for patient body weight or for concomitant chemotherapy regimen.
Patients currently receiving intravenous pertuzumab and trastuzumab can transition to PHESGO. In patients receiving intravenous pertuzumab and trastuzumab with < 6 weeks since their last dose, administer PHESGO as a maintenance dose of 600 mg pertuzumab/600 mg trastuzumab and every 3 weeks for subsequent administrations. In patients receiving intravenous pertuzumab and trastuzumab with ≥ 6 weeks since their last dose, administer PHESGO as an initial dose of 1,200 mg pertuzumab/600 mg trastuzumab, followed by a maintenance dose of 600 mg pertuzumab/600 mg trastuzumab every 3 weeks for subsequent administrations.
Neoadjuvant Treatment of Breast Cancer
Administer PHESGO every 3 weeks for 3 to 6 cycles as part of a treatment regimen for early breast cancer [see Clinical Studies (14.2)].
Refer to the prescribing information for pertuzumab, administered in combination with trastuzumab and chemotherapy, for recommended dose and dosage modifications.
Following surgery, patients should continue to receive PHESGO to complete 1 year of treatment (up to 18 cycles) or until disease recurrence or unmanageable toxicity, whichever occurs first, as a part of a complete regimen for early breast cancer.
Adjuvant Treatment of Breast Cancer
Administer PHESGO every 3 weeks for a total of 1 year (up to 18 cycles) or until disease recurrence or unmanageable toxicity, whichever occurs first, as part of a complete regimen for early breast cancer, including standard anthracycline- and/or taxane-based chemotherapy. Start PHESGO on Day 1 of the first taxane-containing cycle [see Clinical Studies (14.2)].
Metastatic Breast Cancer (MBC)
When administered with PHESGO, the recommended initial dose of docetaxel is 75 mg/m2 administered as an intravenous infusion. The dose may be escalated to 100 mg/m2 administered every 3 weeks if the initial dose is well tolerated. Administer PHESGO until disease progression or unmanageable toxicity, whichever occurs first.
2.4 Dose Modification
Dose Modification for Delayed or Missed Doses
For delayed or missed doses of PHESGO, if the time between two sequential injections is less than 6 weeks, administer the maintenance dose of 600 mg, 600 mg, and 20,000 units/10 mL. Do not wait until the next planned dose.
If the time between two sequential injections is 6 weeks or more, re-administer the initial dose of 1,200 mg, 600 mg, and 30,000 units/15 mL, followed every 3 weeks thereafter by a maintenance dose of 600 mg, 600 mg, and 20,000 units/10 mL.
For chemotherapy dose modifications, see relevant prescribing information.
Cardiomyopathy [see Boxed Warning, Warnings and Precautions (5.1)]
Assess left ventricular ejection fraction (LVEF) prior to initiation of PHESGO and at regular intervals during treatment as indicated in Table 2.
The recommendations on dose modifications in the event of LVEF dysfunction are indicated in Table 2 [see Warnings and Precautions (5.1)].
Table 2: Dose Modifications for Left Ventricular Dysfunction Pre-treatment LVEF: Monitor LVEF every: Withhold PHESGO for at least 3 weeks for an LVEF decrease to: Resume PHESGO after 3 weeks if LVEF has recovered to: - * For patients receiving anthracycline-based chemotherapy, a LVEF of ≥ 50% is required after completion of anthracyclines, before starting PHESGO
Early Breast Cancer ≥ 55%* ~12 weeks (once during neoadjuvant therapy) <50% with a fall of ≥10%-points below pre-treatment value Either ≥50% <10% points below pre-treatment value Metastatic Breast Cancer ≥ 50% ~12 weeks Either Either <40% 40%-45% with a fall of ≥10%-points below pre-treatment value >45% 40%-45% with a fall of <10%-points below pre-treatment value If after a repeat assessment within approximately 3 weeks, the LVEF has not improved, has declined further, and/or the patient is symptomatic, permanently discontinue PHESGO [see Warnings and Precautions (5.1)].
Hypersensitivity and Administration-Related Reactions
Discontinue the injection immediately if the patient experiences a serious hypersensitivity reaction (e.g. anaphylaxis) [see Warnings and Precautions (5.5)].
2.5 Preparation for Administration
To prevent medication errors, it is important to check the vial labels to ensure that the drug being prepared and administered is PHESGO and not intravenous pertuzumab, or intravenous trastuzumab, or subcutaneous trastuzumab.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use vial if particulates or discoloration is present. Do not shake. Discard any unused portion remaining in the vial.
For both the initial and maintenance dose, each corresponding PHESGO vial is ready-to-use for one subcutaneous injection and should not be diluted.
A syringe, a transfer needle, and an injection needle are needed to withdraw PHESGO solution from the vial and inject it subcutaneously. PHESGO may be injected using 25G-27G (3/8"-5/8") hypodermic injection needles.
To avoid needle clogging, attach the hypodermic injection needle to the syringe immediately prior to administration followed by volume adjustment to 15 mL (initial dose) and 10 mL (maintenance dose). If the dose is not to be administered immediately, and the solution of PHESGO has been withdrawn from the vial into the syringe, replace the transfer needle with a syringe closing cap. Label the syringe with the peel-off sticker and store the syringe in the refrigerator [2°C to 8°C (36°F to 46°F)] for up to 24 hours and at room temperature [20°C to 25°C (68°F to 77°F)] for up to 4 hours and avoid unnecessary storage.
PHESGO is compatible with stainless steel, polypropylene, polycarbonate, polyethylene, polyurethane, polyvinyl chloride and fluorinated ethylene polypropylene.
Administration
- Administer PHESGO 1,200 mg, 600 mg, 30,000 units/15 mL subcutaneously over approximately 8 minutes
- Administer PHESGO 600 mg, 600 mg, 20,000 units/10 mL subcutaneously over approximately 5 minutes
The subcutaneous injection site should be alternated between the left and right thigh only. New injections should be given at least 1 inch (2.5 cm) from the previous site on healthy skin and never into areas where the skin is red, bruised, tender, or hard. Do not split the dose between two syringes or between two sites of administration. During the treatment course with PHESGO, other medications for subcutaneous administration should preferably be injected at different sites.
-
3 DOSAGE FORMS AND STRENGTHS
Injection: PHESGO is a clear to opalescent, and colorless to slightly brownish solution provided as:
- 1,200 mg pertuzumab, 600 mg trastuzumab, and 30,000 units hyaluronidase/15 mL (80 mg, 40 mg, and 2,000 units/mL) of solution in a single-dose vial
- 600 mg pertuzumab, 600 mg trastuzumab, and 20,000 units hyaluronidase/10 mL (60 mg, 60 mg, and 2,000 units/mL) of solution in a single-dose vial
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Cardiomyopathy
PHESGO can cause hypertension, arrhythmias, left ventricular cardiac dysfunction, disabling cardiac failure, cardiomyopathy, and cardiac death [see Boxed Warning: Cardiomyopathy]. PHESGO can cause asymptomatic decline in LVEF.
An increased incidence of LVEF decline has been observed in patients treated with intravenous pertuzumab, intravenous trastuzumab, and docetaxel. A 4-6 fold increase in the incidence of symptomatic myocardial dysfunction has been reported among patients receiving trastuzumab, with the highest absolute incidence occurring when trastuzumab was administered with an anthracycline.
Patients who receive anthracycline after stopping PHESGO may also be at increased risk of cardiac dysfunction [see Drug Interactions (7) and Clinical Pharmacology (12.2)].
Cardiac Monitoring
Prior to initiation of PHESGO, conduct a thorough cardiac assessment, including history, physical examination, and determination of LVEF by echocardiogram or MUGA scan.
During treatment with PHESGO, assess LVEF at regular intervals [see Dosage and Administration (2.4)].
If after a repeat assessment within approximately 3 weeks, the LVEF has not improved, has declined further, and/or the patient is symptomatic, permanently discontinue PHESGO.
Following completion of PHESGO, continue to monitor for cardiomyopathy and assess LVEF measurements every 6 months for at least 2 years as a component of adjuvant therapy.
PHESGO
In the FeDeriCa trial, the percentage of patients with at least one cardiac disorder was 22% in the PHESGO arm. The most frequent cardiac adverse reaction in the PHESGO arm was ejection fraction decreased.
The incidence of cardiac failure (NYHA Class III/IV) with a LVEF decline ≥ 10% and a drop to less than 50% was 0.8% in the PHESGO arm. Confirmed asymptomatic or mildly symptomatic (NYHA Class II) declines in LVEF ≥ 10% and a drop to less than 50% was 1.2% in the PHESGO arm [see Adverse Reactions (6.1)].
PHESGO and/or intravenous pertuzumab and trastuzumab have not been studied in patients with a pretreatment LVEF value of < 55% (EBC) or <50% (MBC); a prior history of CHF, conditions that could impair left ventricular function such as uncontrolled hypertension, recent myocardial infarction, serious cardiac arrhythmia requiring treatment or a cumulative prior anthracycline exposure to > 360 mg/m2 of doxorubicin or its equivalent.
5.2 Embryo-Fetal Toxicity
PHESGO can cause fetal harm when administered to a pregnant woman. In post-marketing reports, use of intravenous trastuzumab during pregnancy resulted in cases of oligohydramnios and oligohydramnios sequence manifesting as pulmonary hypoplasia, skeletal abnormalities, and neonatal death. In an animal reproduction study, administration of intravenous pertuzumab to pregnant cynomolgus monkeys during the period of organogenesis resulted in oligohydramnios, delayed fetal kidney development, and embryo-fetal death at exposures 2.5 to 20 times the exposure in humans at the recommended dose, based on Cmax.
Verify the pregnancy status of females of reproductive potential prior to the initiation of PHESGO. Advise pregnant women and females of reproductive potential that exposure to PHESGO during pregnancy or within 7 months prior to conception can result in fetal harm. Advise females of reproductive potential to use effective contraception during treatment and for 7 months following the last dose of PHESGO [see Use in Specific Populations (8.1, 8.3) and Clinical Pharmacology (12.3)].
5.3 Pulmonary Toxicity
PHESGO can cause serious and fatal pulmonary toxicity. These adverse reactions have been reported with intravenous trastuzumab. Pulmonary toxicity includes dyspnea, interstitial pneumonitis, pulmonary infiltrates, pleural effusions, non-cardiogenic pulmonary edema, pulmonary insufficiency and hypoxia, acute respiratory distress syndrome, and pulmonary fibrosis. Patients with symptomatic intrinsic lung disease or with extensive tumor involvement of the lungs, resulting in dyspnea at rest, appear to have more severe toxicity.
5.4 Exacerbation of Chemotherapy-Induced Neutropenia
PHESGO may exacerbate chemotherapy-induced neutropenia. In randomized controlled clinical trials with intravenous trastuzumab, Grade 3-4 neutropenia and febrile neutropenia were higher in patients receiving trastuzumab in combination with myelosuppressive chemotherapy as compared to those who received chemotherapy alone. The incidence of septic death was similar among patients who received trastuzumab and those who did not.
5.5 Hypersensitivity and Administration-Related Reactions
Severe administration-related reactions (ARRs), including hypersensitivity, anaphylaxis, and events with fatal outcomes, have been associated with intravenous pertuzumab and trastuzumab. Patients experiencing dyspnea at rest due to complications of advanced malignancy and comorbidities may be at increased risk of a severe or of a fatal ARR.
In the FeDeriCa trial, the incidence of hypersensitivity was 1.2% in the PHESGO arm. Administration-related reactions occurred in 21% of patients who received PHESGO. In the PHESGO arm, the most common administration-related reactions were injection site reaction (15%) and injection site pain (2%).
Closely monitor patients during and for 30 minutes after the injection of initial dose and during and for 15 minutes following subsequent injections of maintenance dose of PHESGO. If a significant injection-related reaction occurs, slow down or pause the injection and administer appropriate medical therapies. Evaluate and carefully monitor patients until complete resolution of signs and symptoms.
Permanently discontinue with PHESGO in patients who experience anaphylaxis or severe injection-related reactions. Medications to treat such reactions, as well as emergency equipment, should be available for immediate use. For patients experiencing reversible Grade 1 or 2 hypersensitivity reactions, consider pre-medication with an analgesic, antipyretic, or an antihistamine prior to readministration of PHESGO [see Adverse Reactions (6.1)].
PHESGO is contraindicated in patients with known hypersensitivity to pertuzumab, trastuzumab, hyaluronidase or to any of its excipients [see Contraindications (4)].
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the label:
- Cardiomyopathy [see Warnings and Precautions (5.1)]
- Embryo-Fetal Toxicity [see Warnings and Precautions (5.2)]
- Pulmonary Toxicity [see Warnings and Precautions (5.3)]
- Exacerbation of Chemotherapy-Induced Neutropenia [see Warnings and Precautions (5.4)]
- Hypersensitivity and Administration-Related Reactions [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Neoadjuvant and Adjuvant Treatment of Breast Cancer
The safety of PHESGO was evaluated in an open-label, multicenter, randomized trial (FeDeriCa) conducted in 500 patients with HER2 overexpressing early breast cancer [see Clinical Studies (14.2)].
Patients were randomized to receive either PHESGO (1,200 mg pertuzumab, 600 mg trastuzumab, and 30,000 units hyaluronidase/15 mL) followed every 3 weeks by a maintenance dose of 600 mg pertuzumab, 600 mg trastuzumab, and 20,000 units hyaluronidase/10 mL or the recommended dosages for intravenous pertuzumab and intravenous trastuzumab. Patients were randomized to receive 8 cycles of neoadjuvant chemotherapy with concurrent administration of 4 cycles of either PHESGO or intravenous pertuzumab and trastuzumab during cycles 5-8, followed by surgery. Following surgery, patients continued therapy with PHESGO alone or intravenous pertuzumab and trastuzumab (intravenous or subcutaneously administered) as treated prior to surgery, for an additional 14 cycles, to complete 18 cycles. The median duration of treatment for PHESGO was 24 weeks (range: 0-42 weeks).
Serious adverse reactions occurred in 16% of patients who received PHESGO. Serious adverse reactions in > 1% of patients included febrile neutropenia (4%), neutropenic sepsis (1%), and neutrophil count decreased (1%). One fatal adverse reaction occurred in 1/248 (0.4%) of patients, which was due to acute myocardial infarction, and occurred prior to the start of HER2 targeted treatment with PHESGO.
Adverse reactions resulting in permanent discontinuation of any study drug occurred in 8% of patients on the PHESGO arm. Adverse reactions which resulted in permanent discontinuation of PHESGO were ejection fraction decreased (1.2%), cardiac failure (0.8%), and pneumonitis/pulmonary fibrosis (0.8%).
Dosage interruptions due to an adverse reaction occurred in 40% of patients who received PHESGO. Adverse reactions which required dosage interruption in > 1% of patients who received PHESGO included neutropenia (8%), neutrophil count decreased (4%), and diarrhea (7%).
Table 3 summarizes the adverse reactions in FeDeriCa.
Table 3: Adverse Reactions (≥5%) in Patients Who Received PHESGO in FeDeriCa Adverse Reactions PHESGO
(n=248)Intravenous pertuzumab plus intravenous or subcutaneous trastuzumab
(n=252)All Grades
%Grades 3 – 4
%All Grades
%Grades 3 – 4
%Skin and subcutaneous tissue disorders Alopecia 77 0 71 0.4 Dry skin 15 0.4 13 0 Rash 16 0.4 21 0 Nail discoloration 9 0 6 0 Erythema 9 0 5 0 Dermatitis 7 0 6 0 Nail disorder 7 0 7 0.4 Palmar-plantar erythrodysaesthesia syndrome 6 0.8 5 0.4 Gastrointestinal disorders Nausea 60 2 61 1.6 Diarrhea 60 7 57 4.8 Stomatitis 25 0.8 24 0.8 Constipation 22 0 21 0 Vomiting 20 0.8 19 1.2 Dyspepsia 14 0 12 0 Hemorrhoids 9 0 4.0 0 Abdominal pain upper 8 0 6 0 Abdominal pain 9 0.4 6 0 Blood and lymphatic system disorders Anemia 36 1.6 43 4.4 Neutropenia 22 14 27 14 Leukopenia 9 2.4 14 2 Febrile neutropenia 7 7 6 6 General disorders and administration site conditions Asthenia 31 0.4 32 2.4 Fatigue 29 2 24 2 Mucosal inflammation 15 0.8 20 1.2 Injection site reaction 15 0 0.8 0 Pyrexia 13 0 16 0.4 Edema peripheral 8 0 10 0 Malaise 7 0 6 0.4 Influenza-like illness 5 0 3.6 0 Nervous system disorders Dysgeusia 17 0 14 0 Peripheral sensory neuropathy 16 0.8 14 0.4 Headache 17 0 25 0.8 Neuropathy peripheral 12 0.4 15 2 Paresthesia 10 0.8 8 0 Dizziness 13 0 11 0 Investigations Weight decreased 11 0.8 6 0.8 Musculoskeletal and connective tissue disorders Myalgia 25 0.4 19 0.4 Arthralgia 24 0 28 0.4 Back pain 10 0 4.8 0 Bone pain 7 0 5 0 Pain in extremity 6 0 8 0 Muscle spasms 6 0 7 0 Musculoskeletal pain 6 0.4 8 0 Respiratory, thoracic and mediastinal disorder Cough 15 0.4 13 0 Epistaxis 12 0 14 0.4 Dyspnea 10 1.2 5 0 Rhinorrhea 7 0 4.4 0 Infections and infestations Upper respiratory tract infection 11 0 8 0.8 Nasopharyngitis 9 0 10 0 Paronychia 7 0.4 3.6 0 Urinary tract infection 7 0.4 5 0 Injury, poisoning and procedural complications Procedural pain 13 0 10 0 Radiation skin injury 19 0.4 19 0.4 Infusion related reaction 3.6 0 15 0.8 Metabolism and nutrition disorders Decreased appetite 17 0.8 19 0.4 Hypokalemia 7 1.6 8 0 Psychiatric disorders Insomnia 17 0 13 0.4 Eye disorders Lacrimation increased 5 0.4 6 0 Dry eye 5 0.4 3.2 0 Vascular disorders Hot flush 12 0 13 0 Clinically relevant adverse reactions in <5% of patients who received PHESGO include ejection fraction decreased (3.6%) and pruritus (3.2%).
In the FeDeriCa trial, when PHESGO was administered alone, adverse reactions occurred in <10% of patients with the exception of radiation skin injury (20%), arthralgia (19%), diarrhea (17%), injection site reaction (13%), dyspepsia (12%), asthenia (11%), hot flush (11%), and pruritus (10%).
Table 4 summarizes the laboratory abnormalities in FeDeriCa.
Table 4: Select Laboratory Abnormalities (≥5%) that Worsened from Baseline in Patients Who Received PHESGO in FeDeriCa * Laboratory Abnormality PHESGO
(n=248)Intravenous pertuzumab plus intravenous or subcutaneous trastuzumab
(n=252)All Grades
%Grades 3 – 4
%All Grades
%Grades 3 – 4
%- * The denominator used to calculate the rate varied from 163 to 252 based on the number of patients with a baseline value and at least one post-treatment value.
Hematology Hemoglobin (low) 90 2.8 92 4.4 Lymphocytes, Absolute (low) 89 37 88 36 Total Leukocyte Count (low) 82 25 78 25 Neutrophils, Total Absolute (low) 68 30 67 33 Platelet (low) 27 0 28 0.4 Chemistry Creatinine (high) 84 0 87 0.4 Alanine aminotransferase (high) 58 1.6 68 2.4 Aspartate aminotransferase (high) 50 0.8 58 0.8 Potassium (low) 17 5.2 17 2.8 Albumin (low) 16 0 20 0.4 Potassium (high) 13 1.2 9 0 Sodium (low) 13 0.4 10 1.6 Bilirubin (high) 9 0 9 0.4 Glucose (low) 9 0 9 0.4 Sodium (high) 7 0.8 10 0.8 Other Clinical Trials Experience
The safety of the addition of intravenous pertuzumab to trastuzumab in combination with chemotherapy has been established in studies conducted in patients with HER2 overexpressing early breast cancer. The following adverse reactions have been reported following administration of intravenous pertuzumab and trastuzumab: diarrhea, alopecia, nausea, fatigue, neutropenia, vomiting, peripheral neuropathy, constipation, anemia, asthenia, mucosal inflammation, myalgia, and thrombocytopenia. Refer to the Prescribing Information for pertuzumab for more information.
The safety of intravenous pertuzumab, trastuzumab and docetaxel has been established in patients with HER2 overexpressing metastatic breast cancer. The following adverse reactions have been reported following administration of intravenous pertuzumab and trastuzumab: diarrhea, alopecia, neutropenia, nausea, fatigue, rash, and peripheral neuropathy. Refer to the Prescribing Information for pertuzumab for more information.
6.2 Postmarketing Experience
The following adverse reactions have been identified with the use of intravenous pertuzumab and trastuzumab. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Glomerulopathy
- Immune thrombocytopenia
- Tumor lysis syndrome (TLS): Patients with significant tumor burden (e.g. bulky metastases) may be at a higher risk. Patients could present with hyperuricemia, hyperphosphatemia, and acute renal failure which may represent possible TLS. Providers should consider additional monitoring and/or treatment as clinically indicated.
-
7 DRUG INTERACTIONS
Patients who receive anthracycline after stopping PHESGO may be at increased risk of cardiac dysfunction because of PHESGO's long washout period [see Clinical Pharmacology (12.3)]. If possible, avoid anthracycline-based therapy for up to 7 months after stopping PHESGO. If anthracyclines are used, carefully monitor the patient's cardiac function.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Pharmacovigilance Program
There is a pregnancy pharmacovigilance program for PHESGO. If PHESGO is administered during pregnancy, or if a patient becomes pregnant while receiving PHESGO or within 7 months following the last dose of PHESGO, health care providers and patients should immediately report PHESGO exposure to Genentech at 1-888-835-2555.
Risk Summary
PHESGO can cause fetal harm when administered to a pregnant woman. In post-marketing reports, use of intravenous trastuzumab during pregnancy resulted in cases of oligohydramnios and oligohydramnios sequence manifesting as pulmonary hypoplasia, skeletal abnormalities, and neonatal death (see Data). In an animal reproduction study, administration of pertuzumab to pregnant cynomolgus monkeys during the period of organogenesis resulted in oligohydramnios, delayed fetal kidney development, and embryo-fetal deaths at clinically relevant exposures that were 2.5 to 20-fold greater than exposures in humans receiving the recommended dose, based on Cmax (see Data). Apprise the patient of the potential risks to a fetus. There are clinical considerations if PHESGO is used during pregnancy or within 7 months prior to conception (see Clinical Considerations).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Data
Human Data
In post-marketing reports, use of trastuzumab during pregnancy resulted in cases of oligohydramnios and of oligohydramnios sequence, manifesting in the fetus as pulmonary hypoplasia, skeletal abnormalities, and neonatal death. These case reports described oligohydramnios in pregnant women who received trastuzumab either alone or in combination with chemotherapy. In some case reports, amniotic fluid index increased after trastuzumab was stopped. In one case, trastuzumab therapy resumed after amniotic index improved and oligohydramnios recurred.
Animal Data
PHESGO for subcutaneous injection contains pertuzumab, trastuzumab, and hyaluronidase [see Description (11)].
Pertuzumab:
Pregnant cynomolgus monkeys were treated on Gestational Day (GD) 19 with loading doses of 30 to 150 mg/kg pertuzumab, followed by bi-weekly doses of 10 to 100 mg/kg. These dose levels resulted in clinically relevant exposures of 2.5 to 20-fold greater than exposures in humans receiving the recommended dose, based on Cmax. Intravenous administration of pertuzumab from GD19 through GD50 (period of organogenesis) was embryotoxic, with dose-dependent increases in embryo-fetal death between GD25 to GD70. The incidences of embryo-fetal loss were 33, 50, and 85%. At Caesarean section on GD100, oligohydramnios, decreased relative lung and kidney weights, and microscopic evidence of renal hypoplasia consistent with delayed renal development were identified in all pertuzumab dose groups. Pertuzumab exposure was reported in offspring from all treated groups, at levels of 29% to 40% of maternal serum levels at GD100.
Trastuzumab:
In studies where intravenous trastuzumab was administered to pregnant cynomolgus monkeys during the period of organogenesis at doses up to 25 mg/kg given twice weekly (up to 25 times the recommended weekly human dose of 2 mg/kg), trastuzumab crossed the placental barrier during the early (Gestation Days 20 to 50) and late (Gestation Days 120 to 150) phases of gestation. The resulting concentrations of trastuzumab in fetal serum and amniotic fluid were approximately 33% and 25%, respectively, of those present in the maternal serum but were not associated with adverse developmental effects.
Hyaluronidase:
In an embryo-fetal study, mice have been dosed daily by subcutaneous injection during the period of organogenesis with hyaluronidase (recombinant human) at dose levels up to 2,200,000 U/kg, which is >2,400 and 3,600, based on loading and maintenance doses, respectively, times higher than the human dose. The study found no evidence of teratogenicity. Reduced fetal weight and increased numbers of fetal resorptions were observed, with no effects found at a daily dose of 360,000 U/kg, which is >400 and 600, based on loading and maintenance doses, respectively, times higher than the human dose.
In a peri-and post-natal reproduction study, mice have been dosed daily by subcutaneous injection, with hyaluronidase (recombinant human) from implantation through lactation and weaning at dose levels up to 1,100,000 U/kg, which is >1,200 and 1,800, based on loading and maintenance doses, respectively, times higher than the human dose. The study found no adverse effects on sexual maturation, learning and memory or fertility of the offspring.
8.2 Lactation
Risk Summary
There is no information regarding the presence of pertuzumab, trastuzumab or hyaluronidase in human milk, the effects on the breastfed infant, or the effects on milk production. Published data suggest that human IgG is present in human milk but does not enter the neonatal and infant circulation in substantial amounts. Trastuzumab was present in the milk of lactating cynomolgus monkeys but not associated with neonatal toxicity (see Data). Consider the developmental and health benefits of breast feeding along with the mother's clinical need for PHESGO treatment and any potential adverse effects on the breastfed child from PHESGO or from the underlying maternal condition. This consideration should also take into account the elimination half-life of pertuzumab and the trastuzumab wash out period of 7 months [see Clinical Pharmacology (12.3)].
Data
In lactating cynomolgus monkeys, trastuzumab was present in breast milk at about 0.3% of maternal serum concentrations after pre- (beginning Gestation Day 120) and post-partum (through Post-partum Day 28) doses of 25 mg/kg administered twice weekly (25 times the recommended weekly human dose of 2 mg/kg of intravenous trastuzumab). Infant monkeys with detectable serum levels of trastuzumab did not exhibit any adverse effects on growth or development from birth to 1 month of age.
8.3 Females and Males of Reproductive Potential
PHESGO can cause embryo-fetal harm when administered during pregnancy.
Pregnancy Testing
Verify the pregnancy status of females of reproductive potential prior to the initiation of PHESGO.
Contraception
Females
Advise females of reproductive potential to use effective contraception during treatment and for 7 months following the last dose of PHESGO [see Use in Specific Populations (8.1) and Clinical Pharmacology (12.3)].
8.4 Pediatric Use
The safety and effectiveness of PHESGO in pediatric patients have not been established.
8.5 Geriatric Use
Of the total number of patients in the FeDeriCa trial (n=500) treated with PHESGO, 11% were 65 and over, while 1.6% were 75 and over. Clinical studies of PHESGO did not include sufficient numbers of patients age 65 years and older to determine whether they respond differently from younger patients.
In the intravenous trastuzumab trials, the risk of cardiac dysfunction was increased in geriatric patients as compared to younger patients, in both those receiving treatment for adjuvant therapy or metastatic disease. Other differences in safety or effectiveness were not observed between elderly patients and younger patients. In the intravenous pertuzumab in combination with trastuzumab trials, the risk of decreased appetite, anemia, weight decreased, asthenia, dysgeusia, neuropathy peripheral and hypomagnesemia was increased in patients 65 years of age and older compared to patients less than 65 years of age.
-
11 DESCRIPTION
PHESGO is a combination of pertuzumab, trastuzumab, and hyaluronidase.
Pertuzumab is a recombinant humanized monoclonal antibody that targets the extracellular dimerization domain (Subdomain II) of the human epidermal growth factor receptor 2 protein (HER2). Pertuzumab is produced by recombinant DNA technology in a mammalian cell (Chinese Hamster Ovary) culture. Pertuzumab has an approximate molecular weight of 148 kDa.
Trastuzumab is a humanized IgG1 kappa monoclonal antibody that selectively binds with high affinity to the extracellular domain of the human epidermal growth factor receptor 2 protein, HER2. Trastuzumab is produced by recombinant DNA technology in a mammalian cell (Chinese Hamster Ovary) culture. Trastuzumab has a molecular weight of approximately 148 kDa.
Hyaluronidase (recombinant human) is an endoglycosidase used to increase the dispersion and absorption of co-administered drugs when administered subcutaneously. It is a glycosylated single-chain protein produced by mammalian (Chinese Hamster Ovary) cells containing a DNA plasmid encoding for a soluble fragment of human hyaluronidase (PH20). Hyaluronidase (recombinant human) has a molecular weight of approximately 61 kDa.
PHESGO (pertuzumab, trastuzumab, and hyaluronidase-zzxf) injection is a sterile, preservative-free, clear to opalescent, and colorless to slightly brownish solution supplied in single-dose vials for subcutaneous administration.
PHESGO injection is supplied as two different configurations:
- PHESGO is supplied in a 15 mL single-dose vial containing 1,200 mg of pertuzumab, 600 mg of trastuzumab, and 30,000 units of hyaluronidase, and α,α-trehalose (397 mg), L-histidine (6.75 mg), L-histidine hydrochloric monohydrate (53.7 mg), L-methionine (22.4 mg), polysorbate 20 (6 mg), and sucrose (685 mg) with a pH of 5.5.
- PHESGO is supplied in a 10 mL single-dose vial containing 600 mg of pertuzumab, 600 mg of trastuzumab, and 20,000 units of hyaluronidase, and α,α-trehalose (397 mg), L-histidine (4.4 mg), L-histidine hydrochloric monohydrate (36.1 mg), L-methionine (14.9 mg), polysorbate 20 (4 mg), and sucrose (342 mg) with a pH of 5.5.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Pertuzumab targets the extracellular dimerization domain (subdomain II) of HER2 and, thereby, blocks ligand-dependent heterodimerization of HER2 with other HER family members, including EGFR, HER3 and HER4. As a result, pertuzumab inhibits ligand-initiated intracellular signaling through two major signaling pathways, mitogen-activated protein (MAP) kinase and phosphoinositide 3-kinase (PI3K). Inhibition of these signaling pathways can result in cell growth arrest and apoptosis, respectively.
Trastuzumab binds to subdomain IV of the extracellular domain of the HER2 protein to inhibit the ligand-independent, HER2 mediated cell proliferation and PI3K signaling pathway in human tumor cells that overexpress HER2.
Both pertuzumab and trastuzumab-mediated antibody-dependent cell-mediated cytotoxicity (ADCC) have been shown to be preferentially exerted on HER2 overexpressing cancer cells compared with cancer cells that do not overexpress HER2.
While pertuzumab alone inhibited the proliferation of human tumor cells, the combination of pertuzumab and trastuzumab augmented anti-tumor activity in HER2-overexpressing xenograft models.
Hyaluronan is a polysaccharide found in the extracellular matrix of the subcutaneous tissue. It is depolymerized by the naturally occurring enzyme hyaluronidase. Unlike the stable structural components of the interstitial matrix, hyaluronan has a half-life of approximately 0.5 days. Hyaluronidase increases permeability of the subcutaneous tissue by depolymerizing hyaluronan. In the doses administered, hyaluronidase in PHESGO acts transiently and locally.
The effects of hyaluronidase are reversible and permeability of the subcutaneous tissue is restored within 24 to 48 hours.
Hyaluronidase has been shown to increase the absorption rate of a trastuzumab product into the systemic circulation when given in the subcutis of Göttingen Minipigs.
12.2 Pharmacodynamics
The exposure-response relationship and time course of pharmacodynamic response for the safety and effectiveness of pertuzumab and trastuzumab in PHESGO have not been fully characterized.
Cardiac Electrophysiology
The effect of intravenous pertuzumab with an initial dose of 840 mg followed by a maintenance dose of 420 mg every three weeks on QTc interval was evaluated in a subgroup of 20 patients with HER2-positive breast cancer (NCT00567190). No large changes in the mean QT interval (i.e., greater than 20 ms) from placebo based on Fridericia correction method were detected in the trial. A small increase in the mean QTc interval (i.e., less than 10 ms) cannot be excluded because of the limitations of the trial design.
The effects of trastuzumab on electrocardiographic (ECG) endpoints, including QTc interval duration, were evaluated in patients with HER2 positive solid tumors. Trastuzumab had no clinically relevant effect on the QTc interval duration and there was no apparent relationship between serum trastuzumab concentrations and change in QTcF interval duration in patients with HER2 positive solid tumors.
12.3 Pharmacokinetics
The pharmacokinetics (PK) of pertuzumab and trastuzumab were characterized in the FeDeriCa trial following subcutaneous administration of PHESGO (1200 mg pertuzumab/600 mg trastuzumab initial dose followed by 600 mg pertuzumab/600 mg trastuzumab every 3 weeks) and intravenous administration of pertuzumab and trastuzumab (840 mg pertuzumab/8 mg/kg trastuzumab initial dose followed by 420 mg pertuzumab/6 mg/kg trastuzumab every 3 weeks). Trastuzumab is estimated to reach concentrations that are <1 mcg/mL by 7 months in at least 95% patients.
Pertuzumab Cycle 7 Ctrough was 88.7 mcg/mL for PHESGO and 72.4 mcg/mL for intravenous pertuzumab with a geometric mean ratio (GMR) of 1.22 (90% CI: 1.14–1.31). Trastuzumab Cycle 7 Ctrough was 57.5 mcg/mL for PHESGO and 43.2 mcg/mL for intravenous trastuzumab with a GMR of 1.33 (90% CI: 1.24–1.43) [see Clinical Studies (14.2)].
Following subcutaneous administration of PHESGO, the pertuzumab median Cycle 7 Cmax was 34% lower and AUC0-21days was 5% higher than that following intravenous administration of pertuzumab. The median trastuzumab Cycle 7 Cmax was 31% lower and AUC0-21days was 10% higher, than that following intravenous administration of trastuzumab.
Absorption
The mean absolute bioavailability (CV%) was 0.71 (18%) for pertuzumab and 0.77 (13%) for trastuzumab after subcutaneous administration of the approved recommended dosage of PHESGO. The median time to reach Cmax was 3.8 days for both pertuzumab and trastuzumab.
Distribution
The volume of distribution of pertuzumab and trastuzumab at steady state was 2.8 L and 2.9 L, respectively.
Elimination
For pertuzumab, the clearance (CV%) was 0.2 L/day (24%). For trastuzumab, the linear clearance was 0.1 L/day (30%); the non-linear elimination Vmax (CV%) was 12 mg/day (20%) and Km (CV%) was 34 mg/L (39%). The terminal half-life of pertuzumab and trastuzumab was 24 days and 22 days, respectively. Steady state concentration was achieved at Cycle 7 for pertuzumab and at Cycle 11 for trastuzumab.
Specific Populations
No dose adjustments based on body weight or baseline albumin level are needed, as the exposure changes are not considered clinically relevant.
In patients with a body weight <58 kg, mean Cycle 7 AUC0-21 days of trastuzumab was about 33% higher after PHESGO than after intravenous trastuzumab treatment, whereas in the highest BW group (>77 kg) Cycle 7 AUC0-21 days was 24% lower after PHESGO than after intravenous trastuzumab treatment. However, no body weight-based dose adjustments are needed, as the exposure changes are not considered clinically relevant.
No clinically significant differences in the pharmacokinetics of pertuzumab and trastuzumab were observed based on age (25 to 80 years), race (Asian and non-Asian), and renal impairment (creatinine clearance 30 mL/min or greater determined by Cockcroft-Gault). The effects of hepatic impairment on the pharmacokinetics of pertuzumab and trastuzumab are unknown.
12.6 Immunogenicity
The observed incidence of anti-drug antibodies (ADA) is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of ADA in the trial described below, including those of PHESGO or of other pertuzumab or trastuzumab products.
During treatment and post-treatment with subcutaneous administration of PHESGO and concurrent administration with neoadjuvant chemotherapy in the FeDeriCa trial [see Clinical Studies (14.1)], the incidence of anti-pertuzumab and anti-trastuzumab antibodies was 12.9% (31/241) and 2.1% (5/241), respectively. During treatment and post-treatment with intravenous pertuzumab and trastuzumab and concurrent administration with neoadjuvant chemotherapy, the incidence of anti-pertuzumab and anti-trastuzumab antibodies was 10.6 % (26/245) and 0.4% (1/245), respectively. The incidence of neutralizing antibodies (NAb) to pertuzumab and to trastuzumab was 6% (2/31) and 20% (1/5), respectively, in patients treated with PHESGO. The corresponding incidences of NAb were 11.5% (3/26) and 0% (0/1), respectively, in patients treated with intravenous pertuzumab and trastuzumab. Because of limited immunogenicity data, the effect of anti-pertuzumab and anti-trastuzumab antibodies on the pharmacokinetics and effectiveness of PHESGO is unknown. There was no identified clinically significant effect of anti-pertuzumab and anti-trastuzumab antibodies on the safety of PHESGO.
In the FeDeriCa trial, the incidence of anti-rHuPH20 antibodies was 6.3% (15/238) and the incidence of NAb was 0% (0/15) in patients treated with PHESGO. Because of limited immunogenicity data, the clinical impact of anti-rHuPH20 antibodies is unknown.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
PHESGO contains pertuzumab, trastuzumab, and hyaluronidase.
Pertuzumab
Studies have not been performed to evaluate the carcinogenicity or mutagenic potential of pertuzumab. No specific fertility studies in animals have been performed to evaluate the effect of pertuzumab.
No adverse effects on male and female reproductive organs were observed in repeat-dose toxicity studies of up to six months duration in cynomolgus monkeys.
Trastuzumab
Trastuzumab has not been tested for carcinogenicity potential.
No evidence of mutagenic activity was observed when trastuzumab was tested in the standard Ames bacterial and human peripheral blood lymphocyte mutagenicity assays at concentrations of up to 5000 mcg/mL. In an in vivo micronucleus assay, no evidence of chromosomal damage to mouse bone marrow cells was observed following bolus intravenous doses of up to 118 mg/kg of trastuzumab.
A fertility study was conducted in female cynomolgus monkeys at doses up to 25 times the weekly recommended human dose of 2 mg/kg of intravenous trastuzumab and has revealed no evidence of impaired fertility, as measured by menstrual cycle duration and female sex hormone levels.
Hyaluronidase
Hyaluronidases are found in most tissues of the body. Long-term animal studies have not been performed to assess the carcinogenic or mutagenic potential of hyaluronidase. In addition, when subcutaneous hyaluronidase (recombinant human) was administered to cynomolgus monkeys for 39 weeks at dose levels up to 220,000 U/kg, which is >223 and 335, based on loading and maintenance doses, respectively, times higher than the human dose, no evidence of toxicity to the male or female reproductive system was found through periodic monitoring of in-life parameters, e.g., semen analyses, hormone levels, menstrual cycles, and also from gross pathology, histopathology and organ weight data.
-
14 CLINICAL STUDIES
14.1 Neoadjuvant and Adjuvant Treatment of Breast Cancer
The effectiveness of PHESGO for use in combination with chemotherapy has been established for the treatment of patients with HER2-positive early breast cancer. Use of PHESGO for this indication is supported by evidence from adequate and well-controlled studies conducted with intravenous pertuzumab and intravenous trastuzumab administered in combination with chemotherapy in adults with HER2-overexpressing early breast cancer (NCT00545688, NCT00976989, NCT02132949, NCT01358877) and additional pharmacokinetic and safety data that demonstrated comparable pharmacokinetics and safety profiles between PHESGO and intravenous pertuzumab and intravenous trastuzumab in FeDeriCa [see Adverse Reactions (6.1) and Clinical Pharmacology (12.3)].
FeDeriCa
The FeDeriCa trial (NCT03493854) was an open-label, multicenter, randomized trial conducted in 500 patients with operable or locally advanced (including inflammatory) HER2-positive breast cancer with a tumor size >2 cm or node-positive. HER2 overexpression was defined as IHC 3+ in >10% of immunoreactive cells or HER2 gene amplification by ISH (ratio of HER2 gene signals to centromere 17 signals ≥2.0) using an FDA-approved test. Patients were randomized to receive 8 cycles of neoadjuvant chemotherapy with concurrent administration of 4 cycles of either PHESGO or intravenous pertuzumab and trastuzumab during cycles 5-8, followed by surgery. Investigators selected one of two of the following neoadjuvant chemotherapy regimens for individual patients:
- 4 cycles of doxorubicin (60 mg/m2) and cyclophosphamide (600 mg/m2) every 2 weeks followed by paclitaxel (80 mg/m2) weekly for 12 weeks
- 4 cycles of doxorubicin (60 mg/m2) and cyclophosphamide (600 mg/m2) every 3 weeks followed by 4 cycles of docetaxel (75 mg/m2 for the first cycle and then 100 mg/m2 at subsequent cycles at the investigator's discretion) every 3 weeks
Following surgery, patients continued therapy with PHESGO or intravenous pertuzumab and trastuzumab as treated prior to surgery, for an additional 14 cycles, to complete 18 cycles of anti-HER2 therapy. Patients also received adjuvant radiotherapy and endocrine therapy as per investigator's discretion. In adjuvant period, substitution of intravenous trastuzumab for subcutaneous trastuzumab was permitted at investigator discretion. Patients received HER2-targeted therapy every 3 weeks according to Table 5 as follows:
Table 5: Dosing and Administration of PHESGO, Intravenous Pertuzumab, Intravenous Trastuzumab, and Subcutaneous Trastuzumab Medication Administration Dose Initial Maintenance - * In adjuvant period substitution of intravenous trastuzumab for subcutaneous trastuzumab was permitted at investigator discretion
PHESGO Subcutaneously 1200 mg/600 mg 600mg/600 mg Pertuzumab Intravenously 840 mg 420 mg Trastuzumab Intravenously 8 mg/kg 6 mg/kg Trastuzumab-oysk Subcutaneously* 600 mg FeDeriCa was designed to demonstrate non-inferiority of the Cycle 7 (i.e., pre-dose Cycle 8) pertuzumab serum Ctrough from PHESGO pertuzumab to the intravenous pertuzumab (major efficacy outcome measure) [see Clinical Pharmacology 12.3]. Additional outcome measures included Cycle 7 serum trastuzumab Ctrough, efficacy (pathological complete response [pCR], defined as the absence of invasive neoplastic cells in the breast and in the axillary lymph nodes), and safety.
The median age of patients was 51 years (range: 25-81); 99% were female; 66% were White, 21% were Asian, 4% were American Indian or Alaska Native, 1.2% were Black or African American, 15% were Hispanic or Latino. The majority of patients had hormone receptor-positive disease (61%) or node-positive disease (58%).
Table 6: Summary of Pathological Complete Response (pCR) (FeDeriCa) PHESGO
n=248Intravenous pertuzumab + trastuzumab
n=252- * Confidence interval for one sample binomial using Pearson-Clopper method
- † Hauck-Anderson continuity correction has been used in this calculation
pCR: ypT0/is, ypN0 148 (59.7%) 150 (59.5%) Exact 95% CI for pCR Rate* (53.3%, 65.8%) (53.2%, 65.6%) Difference in pCR rate (SC minus IV arm) 0.15% 95% CI for the difference in pCR† rate (-8.7%; 9.0%) 14.2 Metastatic Breast Cancer
The effectiveness of PHESGO for use in combination with docetaxel has been established for the treatment of patients with HER2-positive metastatic breast cancer who have not received prior anti-HER2 therapy or chemotherapy for metastatic disease. Use of PHESGO for this indication is supported by evidence from adequate and well-controlled studies conducted with intravenous pertuzumab and intravenous trastuzumab administered in combination with chemotherapy in adults with HER2-overexpressing metastatic breast cancer (NCT00567190) and additional pharmacokinetic and safety data that demonstrated comparable pharmacokinetics and safety profiles between PHESGO and intravenous pertuzumab and intravenous trastuzumab in FeDeriCa [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14.2)].
14.3 Patient Experience
The PHranceSCa trial (NCT03674112) was a randomized, multi-center, open-label cross-over trial conducted in 160 patients with HER2-positive breast cancer undergoing adjuvant treatment. All patients completed neoadjuvant treatment with pertuzumab, trastuzumab and chemotherapy and had surgery before randomization. Following randomization, 80 patients in arm A received 3 cycles of intravenous pertuzumab and trastuzumab followed by 3 cycles of PHESGO and 80 patients in arm B received 3 cycles of PHESGO followed by 3 cycles of intravenous pertuzumab and trastuzumab. All patients received 18 total cycles of HER2-targeted therapy. After Cycle 6, 136 out of 160 patients (85%) reported preferring subcutaneous administration of PHESGO over intravenous pertuzumab and trastuzumab and the most common reason was that administration required less time in the clinic. After Cycle 6, 22 out of 160 patients (14%) reported preferring intravenous pertuzumab and trastuzumab over PHESGO and the most common reason was feels more comfortable during administration. Two out of 160 patients (1%) had no preference for the route of administration. All 160 patients (100%) completed the preference questionnaire.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
PHESGO (pertuzumab, trastuzumab, and hyaluronidase-zzxf) injection is a sterile, preservative-free, clear to opalescent, and colorless to slightly brownish solution in single-dose vials for subcutaneous administration supplied as each carton containing one single-dose vial:
- 1,200 mg pertuzumab, 600 mg trastuzumab, and 30,000 units hyaluronidase/15 mL (80 mg, 40 mg, and 2,000 units/mL) (NDC: 50242-245-01).
- 600 mg pertuzumab, 600 mg trastuzumab, and 20,000 units hyaluronidase/10 mL (60 mg, 60 mg, 2,000 units/mL) (NDC: 50242-260-01).
-
17 PATIENT COUNSELING INFORMATION
Cardiomyopathy
- Advise patients to contact a health care professional immediately for any of the following: new onset or worsening shortness of breath, cough, swelling of the ankles/legs, swelling of the face, palpitations, weight gain of more than 5 pounds in 24 hours, dizziness or loss of consciousness [see Warnings and Precautions (5.1)].
Embryo-Fetal Toxicity
- Advise pregnant women and females of reproductive potential that exposure to PHESGO during pregnancy or within 7 months prior to conception can result in fetal harm. Advise female patients to contact their healthcare provider with a known or suspected pregnancy [see Use in Specific Populations (8.1)].
- Advise women who are exposed to PHESGO during pregnancy or within 7 months prior to conception that there is a pregnancy pharmacovigilance program that monitors pregnancy outcomes. Encourage these patients to report their pregnancy to Genentech [see Use in Specific Populations (8.1)].
- Advise females of reproductive potential to use effective contraception during treatment and for 7 months following the last dose of PHESGO [see Use in Specific Populations (8.3)].
Hypersensitivity and Administration-Related Reactions
- Advise patients to contact their healthcare provider immediately and to report any symptoms of hypersensitivity and administration-related reactions including dizziness, nausea, chills, fever, vomiting, diarrhea, urticaria, angioedema, breathing problems, or chest pain [see Warnings and Precautions (5.5)].
-
SPL UNCLASSIFIED SECTION
PHESGO® [pertuzumab, trastuzumab, and hyaluronidase-zzxf]
Manufactured by:
Genentech, Inc.
A Member of the Roche Group
1 DNA Way
South San Francisco, CA 94080-4990U.S. License No.: 1048
PHESGO® is a trademark of Genentech, Inc.
©2024 Genentech, Inc.Representative sample of labeling (see the HOW SUPPLIED section for complete listing):
-
PRINCIPAL DISPLAY PANEL - 15 mL Vial Carton
NDC: 50242-245-01
Phesgo®
(pertuzumab, trastuzumab,
and hyaluronidase-zzxf)
Injection1,200 mg, 600 mg, and
30,000 units/15 mL
(80 mg, 40 mg, and 2,000 units/mL)For subcutaneous injection
over 8 minutes
Single-Dose Vial
Discard Unused Portion1 vial
Rx only
Genentech
11021888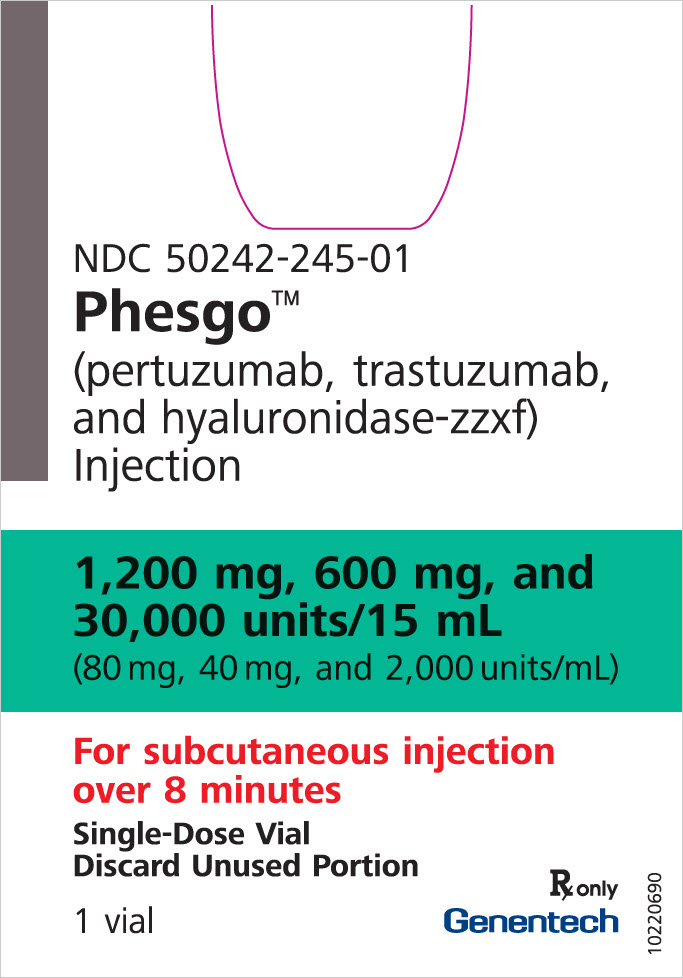
-
PRINCIPAL DISPLAY PANEL - 10 mL Vial Carton
NDC: 50242-260-01
Phesgo®
(pertuzumab, trastuzumab,
and hyaluronidase-zzxf)
Injection600 mg, 600 mg, and
20,000 units/10 mL
(60 mg, 60 mg, and 2,000 units/mL)For subcutaneous injection
over 5 minutes
Single-Dose Vial
Discard Unused Portion1 vial
Rx only
Genentech
11021892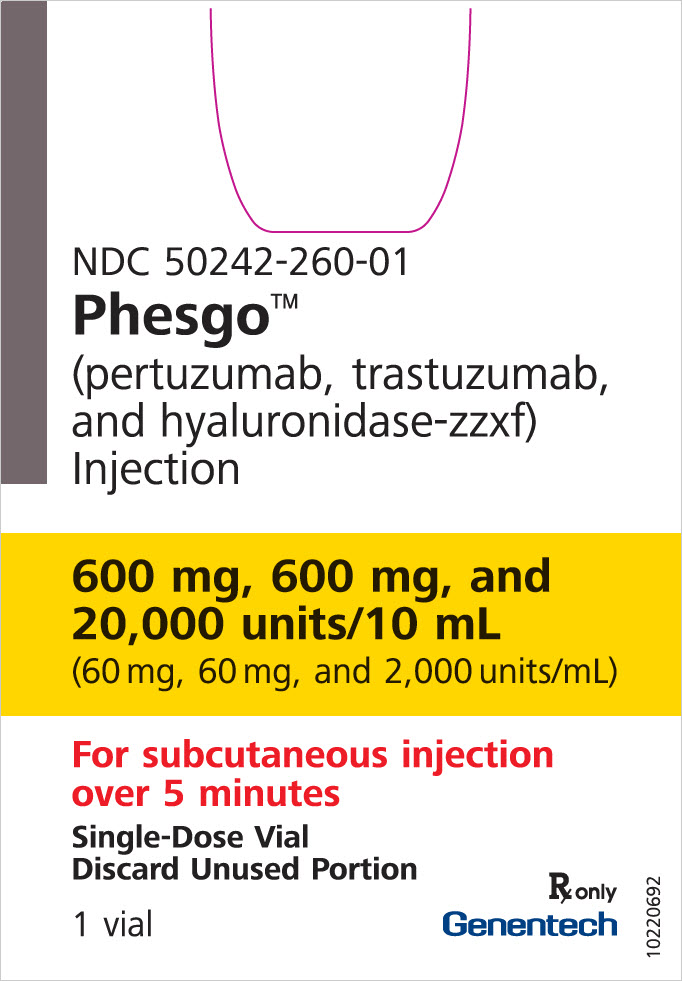
-
INGREDIENTS AND APPEARANCE
PHESGO
pertuzumab, trastuzumab, and hyaluronidase-zzxf injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50242-245 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PERTUZUMAB (UNII: K16AIQ8CTM) (PERTUZUMAB - UNII:K16AIQ8CTM) PERTUZUMAB 1200 mg in 15 mL TRASTUZUMAB (UNII: P188ANX8CK) (TRASTUZUMAB - UNII:P188ANX8CK) TRASTUZUMAB 600 mg in 15 mL HYALURONIDASE (HUMAN RECOMBINANT) (UNII: 743QUY4VD8) (HYALURONIDASE (HUMAN RECOMBINANT) - UNII:743QUY4VD8) HYALURONIDASE (HUMAN RECOMBINANT) 30000 U in 15 mL Inactive Ingredients Ingredient Name Strength HISTIDINE (UNII: 4QD397987E) HISTIDINE HYDROCHLORIDE (UNII: 1D5Q932XM6) TREHALOSE DIHYDRATE (UNII: 7YIN7J07X4) SUCROSE (UNII: C151H8M554) POLYSORBATE 20 (UNII: 7T1F30V5YH) METHIONINE (UNII: AE28F7PNPL) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50242-245-01 1 in 1 CARTON 06/29/2020 1 15 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 2 NDC: 50242-245-86 1 in 1 CARTON 05/03/2021 2 15 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA761170 06/29/2020 PHESGO
pertuzumab, trastuzumab, and hyaluronidase-zzxf injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50242-260 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PERTUZUMAB (UNII: K16AIQ8CTM) (PERTUZUMAB - UNII:K16AIQ8CTM) PERTUZUMAB 600 mg in 10 mL TRASTUZUMAB (UNII: P188ANX8CK) (TRASTUZUMAB - UNII:P188ANX8CK) TRASTUZUMAB 600 mg in 10 mL HYALURONIDASE (HUMAN RECOMBINANT) (UNII: 743QUY4VD8) (HYALURONIDASE (HUMAN RECOMBINANT) - UNII:743QUY4VD8) HYALURONIDASE (HUMAN RECOMBINANT) 20000 U in 10 mL Inactive Ingredients Ingredient Name Strength HISTIDINE (UNII: 4QD397987E) HISTIDINE HYDROCHLORIDE (UNII: 1D5Q932XM6) TREHALOSE DIHYDRATE (UNII: 7YIN7J07X4) SUCROSE (UNII: C151H8M554) POLYSORBATE 20 (UNII: 7T1F30V5YH) METHIONINE (UNII: AE28F7PNPL) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50242-260-01 1 in 1 CARTON 06/29/2020 1 10 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 2 NDC: 50242-260-86 1 in 1 CARTON 05/03/2021 2 10 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA761170 06/29/2020 Labeler - Genentech, Inc. (080129000) Registrant - Genentech, Inc. (080129000) Establishment Name Address ID/FEI Business Operations Roche Diagnostics GmbH 323105205 API MANUFACTURE(50242-245, 50242-260) , ANALYSIS(50242-245, 50242-260) Establishment Name Address ID/FEI Business Operations F. Hoffmann-La Roche AG 485244961 ANALYSIS(50242-245, 50242-260) , MANUFACTURE(50242-245, 50242-260) , PACK(50242-245, 50242-260) , LABEL(50242-245, 50242-260) Establishment Name Address ID/FEI Business Operations Genentech, Inc. (Oceanside) 146373191 API MANUFACTURE(50242-245, 50242-260) , ANALYSIS(50242-245, 50242-260) Establishment Name Address ID/FEI Business Operations Roche Diagnostics GmbH 315028860 ANALYSIS(50242-245, 50242-260) Establishment Name Address ID/FEI Business Operations Roche Singapore Technical Operations Pte. Ltd 937189173 ANALYSIS(50242-245, 50242-260) , API MANUFACTURE(50242-245, 50242-260) Establishment Name Address ID/FEI Business Operations Genentech, Inc. 080129000 ANALYSIS(50242-245, 50242-260)
Trademark Results [Phesgo]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 PHESGO 97934470 not registered Live/Pending |
Genentech, Inc. 2023-05-12 |
 PHESGO 88891147 not registered Live/Pending |
Genentech, Inc. 2020-04-28 |
 PHESGO 88575791 not registered Live/Pending |
Genentech, Inc. 2019-08-12 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.