TRIHEXYPHENIDYL HYDROCHLORIDE syrup
Trihexyphenidyl Hydrochloride by
Drug Labeling and Warnings
Trihexyphenidyl Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by Versapharm Incorporated, Akorn Operating Company LLC, Mikart, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
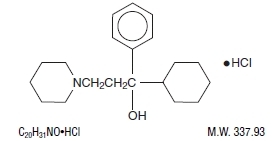
DESCRIPTION
Trihexyphenidyl Hydrochloride Oral Solution USP is a synthetic antispasmodic drug. It is designated chemically as α-Cyclohexyl-α-phenyl-1-piperidinepropanol hydrochloride and its structural formula is as follows:
Trihexyphenidyl hydrochloride occurs as a white or creamy-white, almost odorless, crystalline powder. It is very slightly soluble in ether and benzene, slightly soluble in water and soluble in methanol.
Each 5 mL (teaspoonful) for oral administration contains 2 mg trihexyphenidyl hydrochloride and alcohol 5% in a clear, colorless, lime-mint flavored preparation. In addition, it contains the following inactive ingredients: citric acid, flavoring, methylparaben, propylparaben, purified water and sorbitol solution.
-
CLINICAL PHARMACOLOGY
Trihexyphenidyl exerts a direct inhibitory effect upon the parasympathetic nervous system. It also has a relaxing effect on smooth musculature; exerted both directly upon the muscle tissue itself and indirectly through an inhibitory effect upon the parasympathetic nervous system. Its therapeutic properties are similar to those of atropine although undesirable side effects are ordinarily less frequent and severe than with the latter.
-
INDICATIONS AND USAGE
Trihexyphenidyl is indicated as an adjunct in the treatment of all forms of parkinsonism (postencephalitic, arteriosclerotic, and idiopathic). It is often useful as adjuvant therapy when treating these forms of parkinsonism with levodopa. Additionally, it is indicated for the control of extrapyramidal disorders caused by central nervous system drugs such as the dibenzoxazepines, phenothiazines, thioxanthenes, and butyrophenones.
- CONTRAINDICATIONS
-
WARNINGS
Patients to be treated with trihexyphenidyl should have a gonioscope evaluation prior to initiation of therapy and close monitoring of intraocular pressures. The use of anticholinergic drugs may precipitate angle closure with an increase in intraocular pressure. If blurring of vision occurs during therapy, the possibility of narrow angle glaucoma should be considered. Blindness has been reported due to aggravation of narrow angle glaucoma. (See CONTRAINDICATIONS and ADVERSE REACTIONS).
Trihexyphenidyl should be administered with caution in hot weather, especially when given concomitantly with other atropine-like drugs to the chronically ill, alcoholics, those who have central nervous system disease, or those who do manual labor in a hot environment. Anhidrosis may occur more readily when some disturbance of sweating already exists. If there is evidence of anhidrosis, the possibility of hyperthermia should be considered. Dosage should be decreased so that the ability to maintain body heat equilibrium via perspiration is not impaired. Severe anhidrosis and fatal hyperthermia have occurred with the use of anticholinergics under the conditions described above.
Neuroleptic Malignant Syndrome
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) has been reported in association with dose reduction or discontinuation of trihexyphenidyl. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis and cardiac dysrhythmias).
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever, and primary central nervous system (CNS) pathology.
-
PRECAUTIONS
General
Patients with cardiac, liver, or kidney disorders, or with hypertension, should be closely monitored.
Since trihexyphenidyl has atropine-like properties, patients on long-term treatment should be carefully monitored for untoward reactions.
Since trihexyphenidyl has parasympatholytic activity, it should be used with caution in patients with glaucoma, obstructive disease of the gastrointestinal or genitourinary tracts, and in elderly males with possible prostatic hypertrophy. Incipient glaucoma may be precipitated by parasympatholytic drugs such as trihexyphenidyl.
Tardive dyskinesia may appear in some patients on long-term therapy with antipsychotic drugs or may occur after therapy with these drugs has been discontinued. Antiparkinsonism agents do not alleviate the symptoms of tardive dyskinesia, and in some instances may aggravate them.
However, parkinsonism and tardive dyskinesia often coexist in patients receiving chronic neuroleptic treatment, and anticholinergic therapy with trihexyphenidyl may relieve some of these parkinsonism symptoms. Trihexyphenidyl is not recommended for use in patients with tardive dyskinesia unless they have concomitant Parkinson’s disease.
Patients with arteriosclerosis or with a history of idiosyncrasy to other drugs may exhibit reactions of mental confusion, agitation, disturbed behavior, or nausea and vomiting. Such patients should be allowed to develop a tolerance through the initial administration of a small dose and gradual increase in dose until an effective level is reached. If a severe reaction should occur, administration of the drug should be discontinued for a few days and then resumed at a lower dosage. Psychiatric disturbances can result from indiscriminate use (leading to overdosage) to sustain continued euphoria. (See DRUG ABUSE AND DEPENDENCE).
Abrupt withdrawal of treatment for parkinsonism may result in acute exacerbation of parkinsonism symptoms; therefore, abrupt withdrawal should be avoided (See DOSAGE AND ADMINISTRATION).
Information for Patients
Trihexyphenidyl may impair mental and/or physical abilities required for performance of hazardous tasks, such as operating machinery or driving a motor vehicle. Patients should be cautioned about operating machinery, including automobiles, until they are reasonably certain that trihexyphenidyl therapy does not adversely affect their ability to engage in such activities.
Because of increased sedative effects, patients should be cautioned to avoid the use of alcohol or other CNS depressants while taking trihexyphenidyl.
Since this medication may increase the susceptibility to heat stroke (gastrointestinal (GI) problems, fever, heat intolerance), use with caution during hot weather. (See WARNINGS).
Patients should be advised to report the occurrence of GI problems, fever, or heat intolerance promptly since paralytic ileus, hyperthermia, or heat stroke may occur.
If GI upset occurs, trihexyphenidyl may be taken with food.
Patients should have close monitoring of intraocular pressure. (See WARNINGS).
Drug Interactions
Cannabinoids, barbiturates, opiates, and alcohol may have additive effects with trihexyphenidyl, and thus, an abuse potential exists.
Concurrent use of alcohol or other CNS depressants with trihexyphenidyl may cause increased sedative effects.
Monoamine oxidase inhibitors and tricyclic antidepressants possessing significant anticholinergic activity may intensify the anticholinergic effects of antidyskinetic agents because of the secondary anticholinergic activities of these medications.
Prophylactic administration of anticholinergic agents, such as trihexyphenidyl, as a prevention of drug-induced parkinsonism during neuroleptic therapy is not recommended. There may be an increased risk for the development of tardive dyskinesia during concomitant administration of anticholinergics and neuroleptics (See PRECAUTIONS, General).
The usual dose of either trihexyphenidyl or levodopa may need to be reduced during concomitant therapy, since concomitant administration may increase drug-induced involuntary movements (See DOSAGE AND ADMINISTRATION).
Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity studies or adequate genotoxicity or fertility studies have been conducted for trihexyphenidyl.
Pregnancy
Pregnancy Category C
Animal reproduction studies to evaluate teratogenic and embryotoxic potential have not been conducted with trihexyphenidyl. It is also not known whether trihexyphenidyl can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Trihexyphenidyl should be given to a pregnant woman only if clearly needed.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when trihexyphenidyl is administered to a nursing woman.
As with other anticholinergics, trihexyphenidyl may cause suppression of lactation. Therefore, trihexyphenidyl should only be used if the expected benefit to the mother outweighs the potential risk to the infant.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established. (See also ADVERSE REACTIONS).
Geriatric Use
Sensitivity to the actions of parasympatholytic drugs may increase with age, particularly over the age of 60; therefore, elderly patients generally should be started on low doses of trihexyphenidyl and observed closely.
Trihexyphenidyl has been shown to cause some cognitive dysfunctions in the elderly, including confusion and memory impairment. (See ADVERSE REACTIONS and DOSAGE AND ADMINISTRATION).
-
ADVERSE REACTIONS
Minor side effects, such as dryness of the mouth, blurred vision, dizziness, mild nausea or nervousness, will be experienced by 30 to 50 percent of all patients. These sensations, however, are much less troublesome with trihexyphenidyl than with belladonna alkaloids and are usually less disturbing than unalleviated parkinsonism. Such reactions tend to become less pronounced, and even to disappear, as treatment continues. Even before these reactions have remitted spontaneously, they may often be controlled by careful adjustment of dosage form, amount of drug, or interval between doses.
Isolated instances of suppurative parotitis secondary to excessive dryness of the mouth, skin rashes, dilatation of the colon, paralytic ileus, and certain psychiatric manifestations such as delusions, hallucinations, and paranoia, all of which may occur with any of the atropine-like drugs, have been reported rarely with trihexyphenidyl.
Potential side effects associated with the use of any atropine-like drugs, including trihexyphenidyl, include cognitive dysfunctions, including confusion and memory impairment; constipation, drowsiness, urinary hesitancy or retention, tachycardia, dilation of the pupil, increased intraocular pressure, choreiform movements, weakness, vomiting, and headache. Exacerbation of parkinsonism with abrupt treatment withdrawal has been reported. Neuroleptic malignant syndrome with abrupt treatment withdrawal has been reported (See WARNINGS, Neuroleptic Malignant Syndrome).
The occurrence of angle-closure glaucoma in patients receiving trihexyphenidyl has been reported (blindness has been reported in some cases). Paradoxical sinus bradycardia, dry skin, and cycloplegia have been reported.
In addition to adverse events seen in adults, the following adverse events have been reported in the literature in pediatric patients: hyperkinesia, psychosis, forgetfulness, weight loss, restlessness, chorea, and sleep alterations.
- DRUG ABUSE AND DEPENDENCE
-
OVERDOSAGE
The mean oral LD50 of trihexyphenidyl has been reported to be 365 mg/kg (range, 325 to 410 mg/kg) in mice and 1660 mg/kg (1420 to 1940 mg/kg) in rats. At a dose of 40 mg/kg, dogs have exhibited emesis, restlessness followed by drowsiness, equilibrium disturbances, and mydriasis.
In humans, doses up to 300 mg (5 mg/kg) have been ingested without fatalities or sequelae. However, rare cases of death associated with trihexyphenidyl overdosages taken in conjunction with other CNS-depressant agents have been reported or in patients with a compromised respiratory condition. Trihexyphenidyl blood concentrations associated with the fatalities ranged from 0.03 to 0.80 mg/l.
Signs and Symptoms
Overdosage with trihexyphenidyl produces typical central symptoms of atropine intoxication (the central anticholinergic syndrome). Correct diagnosis depends upon recognition of the peripheral signs of parasympathetic blockade, including dilated and sluggish pupils; warm, dry skin; facial flushing; decreased secretions of the mouth, pharynx, nose, and bronchi; foul-smelling breath; elevated temperature; tachycardia, cardiac arrhythmias; decreased bowel sounds; and urinary retention. Neuropsychiatric signs such as delirium, disorientation, anxiety, hallucinations, illusions, confusion, incoherence, agitation, hyperactivity, ataxia, lip smacking and tasting movements, loss of memory, paranoia, combativeness, and seizures may be present. The condition can progress to stupor, coma, paralysis, cardiac and respiratory arrest, and death.
Treatment
Treatment of acute overdose involves symptomatic and supportive therapy. Gastric lavage or other methods to limit absorption should be instituted. A small dose of diazepam or a short-acting barbiturate may be administered if CNS excitation is observed. Phenothiazines are contraindicated because the toxicity may be intensified due to their antimuscarinic action, causing coma. Respiratory support, artificial respiration or vasopressor agents may be necessary. Hyperpyrexia must be reversed, fluid volume replaced and acid-balance maintained. Urinary catheterization may be necessary. It is not known if trihexyphenidyl is dialyzable.
-
DOSAGE AND ADMINISTRATION
Dosage should be individualized. The initial dose should be low and then increased gradually, especially in patients over 60 years of age.Whether trihexyphenidyl may best be given before or after meals should be determined by the way the patient reacts. Postencephalitic patients, who are usually more prone to excessive salivation, may prefer to take it after meals and may, in addition, require small amounts of atropine which, under such circumstances, is sometimes an effective adjuvant. If trihexyphenidyl tends to dry the mouth excessively, it may be better to take it before meals, unless it causes nausea. If taken after meals, the thirst sometimes induced can be allayed by mint candies, chewing gum or water.
Abrupt withdrawal of treatment for parkinsonism may result in acute exacerbation of parkinsonism symptoms; therefore, abrupt withdrawal should be avoided.
Abrupt withdrawal of treatment may result in neuroleptic malignant syndrome (NMS) (See WARNINGS).
Idiopathic Parkinsonism
As initial therapy for parkinsonism, 1 mg of trihexyphenidyl hydrochloride may be administered the first day. The dose may then be increased by 2 mg increments at intervals of three to five days, until a total of 6 to 10 mg is given daily. The total daily dose will depend upon what is found to be the optimal level. Many patients derive maximum benefit from this daily total of 6 to 10 mg, but some patients, chiefly those in the postencephalitic group, may require a total daily dose of 12 to 15 mg.
Drug-Induced Parkinsonism
The size and frequency of the trihexyphenidyl dose needed to control extrapyramidal reactions to commonly employed tranquilizers, notably the phenothiazines, thioxanthenes, and butyrophenones, must be determined empirically. The total daily dosage usually ranges between 5 and 15 mg although, in some cases, these reactions have been satisfactorily controlled with as little as 1 mg daily. It may be advisable to commence therapy with a single 1 mg dose. If the extrapyramidal manifestations are not controlled in a few hours, the subsequent doses may be progressively increased until satisfactory control is achieved. Satisfactory control may sometimes be more rapidly achieved by temporarily reducing the dosage of the tranquilizer when instituting trihexyphenidyl therapy and then adjusting the dosage of both drugs until the desired ataractic effect is retained without onset of extrapyramidal reactions.
It is sometimes possible to maintain the patient on a reduced trihexyphenidyl dosage after the reactions have remained under control for several days. Instances have been reported in which these reactions have remained in remission for long periods after trihexyphenidyl therapy was discontinued.
Concomitant Use with Levodopa
When trihexyphenidyl is used concomitantly with levodopa, the usual dose of each may need to be reduced. Careful adjustment is necessary, depending on side effects and degree of symptom control. A trihexyphenidyl dosage of 3 to 6 mg daily, in divided doses, is usually adequate.
Concomitant Use with Other Parasympathetic Inhibitors
Trihexyphenidyl may be substituted, in whole or in part, for other parasympathetic inhibitors. The usual technique is partial substitution initially, with progressive reduction in the other medication as the dose of trihexyphenidyl is increased.
The total daily intake of trihexyphenidyl hydrochloride oral solution USP is tolerated best if divided into 3 doses and taken at mealtimes. High doses (>10 mg daily) may be divided into 4 parts, with 3 doses administered at mealtimes and the fourth at bedtime.
-
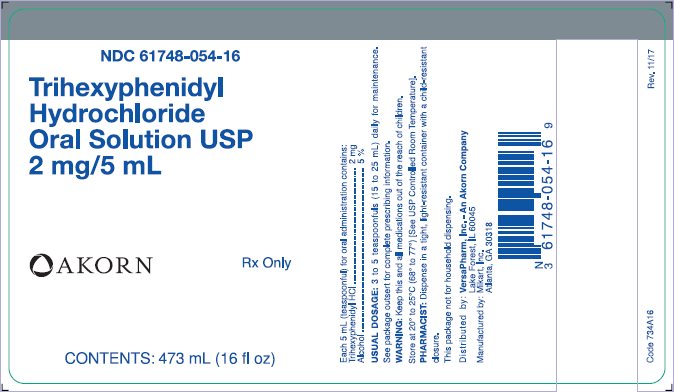
HOW SUPPLIED
Trihexyphenidyl Hydrochloride Oral Solution, containing trihexyphenidyl hydrochloride 2 mg per 5 mL, is a clear, colorless lime-peppermint flavored liquid supplied in 473 mL (16 fl. oz) bottles, NDC: 61748-054-16.
Dispense in a tight, light-resistant container with a child-resistant closure.
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
DO NOT FREEZE.
Rx Only
Manufactured by:
MIKART, INC.
Atlanta, GA 30318Marketed by:
VersaPharm, Inc. – An Akorn Company
Lake Forest, IL 60045
Code 734A00
Rev 03/17
-
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
NDC: 61748-054-16
Trihexyphenidyl
Hydrochloride
Oral Solution USP
2 mg/5 mL
Akorn
Rx only
CONTENTS: 473 mL (16 fl oz)
-
INGREDIENTS AND APPEARANCE
TRIHEXYPHENIDYL HYDROCHLORIDE
trihexyphenidyl hydrochloride syrupProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 61748-054 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TRIHEXYPHENIDYL HYDROCHLORIDE (UNII: AO61G82577) (TRIHEXYPHENIDYL - UNII:6RC5V8B7PO) TRIHEXYPHENIDYL HYDROCHLORIDE 2 mg in 5 mL Inactive Ingredients Ingredient Name Strength ALCOHOL (UNII: 3K9958V90M) ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) METHYLPARABEN (UNII: A2I8C7HI9T) PROPYLPARABEN (UNII: Z8IX2SC1OH) WATER (UNII: 059QF0KO0R) SORBITOL (UNII: 506T60A25R) PEPPERMINT (UNII: V95R5KMY2B) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 61748-054-16 473 mL in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 03/01/2001 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA040251 03/01/2001 Labeler - VersaPharm, Inc. - An Akorn Company (956741896) Establishment Name Address ID/FEI Business Operations Mikart, Inc. 030034847 MANUFACTURE(61748-054) , PACK(61748-054) , ANALYSIS(61748-054)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.