DATROWAY- datopotamab deruxtecan injection, powder, lyophilized, for solution
DATROWAY by
Drug Labeling and Warnings
DATROWAY by is a Prescription medication manufactured, distributed, or labeled by Daiichi Sankyo Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use DATROWAY safely and effectively. See full prescribing information for DATROWAY.
DATROWAY® (datopotamab deruxtecan-dlnk) for injection, for intravenous use
Initial U.S. Approval: 2025INDICATIONS AND USAGE
DATROWAY is a Trop-2-directed antibody and topoisomerase inhibitor conjugate indicated for the treatment of:
- adult patients with locally advanced or metastatic epidermal growth factor receptor (EGFR)-mutated non-small cell lung cancer (NSCLC) who have received prior EGFR-directed therapy and platinum-based chemotherapy. (1.1)
This indication is approved under accelerated approval based on objective response rate and duration of response [see Clinical Studies (14.1)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trial. - adult patients with unresectable or metastatic, hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative (IHC 0, IHC 1+ or IHC 2+/ISH-) breast cancer who have received prior endocrine-based therapy and chemotherapy for unresectable or metastatic disease. (1.2)
DOSAGE AND ADMINISTRATION
- Reconstitute DATROWAY with Sterile Water for Injection. (2.5)
- Dilute with 5% Dextrose Injection. (2.5)
- For intravenous infusion only. Do not administer as an intravenous push or bolus. DO NOT use Sodium Chloride Injection, USP. (2.5)
- Premedicate to reduce the risk of infusion reactions and nausea and vomiting. (2.3)
- The recommended dosage of DATROWAY is 6 mg/kg (up to a maximum of 540 mg for patients ≥90 kg) given as an intravenous infusion once every 3 weeks (21-day cycle) until disease progression or unacceptable toxicity. (2.3, 2.4)
DOSAGE FORMS AND STRENGTHS
For injection: 100 mg lyophilized powder in a single-dose vial. (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
- Interstitial Lung Disease (ILD) and Pneumonitis: DATROWAY can cause severe and fatal cases of ILD/pneumonitis. Monitor for new or worsening signs and symptoms of ILD/pneumonitis. If ILD/pneumonitis is suspected, withhold DATROWAY and initiate corticosteroids. Permanently discontinue DATROWAY in patients with confirmed Grade 2 or higher ILD/pneumonitis. (5.1)
- Ocular Adverse Reactions: DATROWAY can cause ocular adverse reactions including dry eye, keratitis, blepharitis, meibomian gland dysfunction, increased lacrimation, conjunctivitis, and blurred vision. Monitor patients for ocular adverse reactions during treatment with DATROWAY. Advise patients to use preservative-free lubricating eye drops and to avoid using contact lenses during treatment with DATROWAY. Withhold, reduce the dose, or permanently discontinue DATROWAY based on the severity of ocular adverse reactions. Refer patients to an eye care professional for any new or worsening ocular signs and symptoms. (2.3, 2.4, 5.2)
- Stomatitis/Oral Mucositis: DATROWAY can cause stomatitis, including mouth ulcers and oral mucositis. Advise patients to use a steroid-containing mouthwash when starting treatment and to hold ice chips or ice water in mouth during the infusion of DATROWAY. Withhold, reduce the dose, or permanently discontinue DATROWAY based on severity. (2.3, 2.4, 5.3)
- Embryo-Fetal Toxicity: DATROWAY can cause fetal harm. Advise patients of potential risk to a fetus and to use effective contraception. (5.4, 8.1, 8.3)
ADVERSE REACTIONS
The most common adverse reactions (≥20%), including laboratory abnormalities, in patients with:
- EGFR-mutated NSCLC were stomatitis, nausea, alopecia, fatigue, decreased hemoglobin, decreased lymphocytes, constipation, increased calcium, increased AST, decreased white blood cell count, increased lactate dehydrogenase, musculoskeletal pain, decreased appetite, increased ALT, and rash. (6.1)
- HR-positive, HER2-negative breast cancer were stomatitis, nausea, fatigue, decreased leukocytes, decreased calcium, alopecia, decreased lymphocytes, decreased hemoglobin, constipation, decreased neutrophils, dry eye, vomiting, increased ALT, keratitis, increased AST, and increased alkaline phosphatase. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Daiichi Sankyo, Inc. at 1-877-437-7763 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2025
- adult patients with locally advanced or metastatic epidermal growth factor receptor (EGFR)-mutated non-small cell lung cancer (NSCLC) who have received prior EGFR-directed therapy and platinum-based chemotherapy. (1.1)
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Locally Advanced or Metastatic EGFR-Mutated Non-Small Cell Lung Cancer (NSCLC)
1.2 Unresectable or Metastatic, HR-Positive, HER2-Negative Breast Cancer
2 DOSAGE AND ADMINISTRATION
2.1 Patient Selection
2.2 Recommended Dosage
2.3 Premedication, Concomitant Medications, and Required Eye Care
2.4 Dosage Modifications
2.5 Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Interstitial Lung Disease/Pneumonitis
5.2 Ocular Adverse Reactions
5.3 Stomatitis
5.4 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.6 Immunogenicity
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Locally Advanced or Metastatic EGFR-Mutated Non-Small Cell Lung Cancer
14.2 Unresectable or Metastatic, HR-Positive, HER2-Negative Breast Cancer
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Locally Advanced or Metastatic EGFR-Mutated Non-Small Cell Lung Cancer (NSCLC)
DATROWAY is indicated for the treatment of adult patients with locally advanced or metastatic epidermal growth factor receptor (EGFR)-mutated non-small cell lung cancer (NSCLC) who have received prior EGFR-directed therapy and platinum-based chemotherapy.
This indication is approved under accelerated approval based on objective response rate and duration of response [see Clinical Studies (14.1)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trial.
1.2 Unresectable or Metastatic, HR-Positive, HER2-Negative Breast Cancer
DATROWAY is indicated for the treatment of adult patients with unresectable or metastatic, hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative (IHC 0, IHC 1+ or IHC 2+/ISH-) breast cancer who have received prior endocrine-based therapy and chemotherapy for unresectable or metastatic disease.
-
2 DOSAGE AND ADMINISTRATION
2.1 Patient Selection
Select patients with locally advanced or metastatic NSCLC for treatment with DATROWAY based on the presence of epidermal growth factor receptor (EGFR) mutations in tumor or plasma specimens [see Clinical Studies (14.1)]. Testing may be performed at any time from initial diagnosis and does not need to be repeated once EGFR mutation status has been established.
2.2 Recommended Dosage
The recommended dosage of DATROWAY is 6 mg/kg (up to a maximum of 540 mg for patients ≥90 kg) administered as an intravenous infusion once every 3 weeks (21-day cycle) until disease progression or unacceptable toxicity.
If a planned dose is delayed or missed, administer as soon as possible; do not wait until the next planned cycle. Adjust the schedule of administration to maintain a 3-week interval between doses.
2.3 Premedication, Concomitant Medications, and Required Eye Care
Conduct an ophthalmic exam including visual acuity testing, slit lamp examination (with fluorescein staining), intraocular pressure, and fundoscopy at initiation of DATROWAY, annually while on treatment, at end of treatment, and as clinically indicated.
Administer DATROWAY with the premedication and concomitant medications described in Table 1.
Monitor patients for infusion-related reactions in a setting where cardiopulmonary resuscitation medication and equipment are available. Monitor patients for at least 1 hour for the first 2 cycles of DATROWAY infusions. If there are no infusion-related reactions observed, monitor patients for at least 30 minutes for all subsequent cycles of infusions.
Table 1: Premedication and Concomitant Medications Premedication* Examples (or equivalent) Timing of Treatment/Duration - * With or without systemic corticosteroid
Eye drops
[see Warnings and Precautions (5.2)]Preservative-free lubricant eye drops Administer at least four times daily and as needed Mouthwash
[see Warnings and Precautions (5.3)]Steroid-containing mouthwash (dexamethasone oral solution 0.1 mg/mL) Administer four times daily and as needed Antihistamine
[see Adverse Reactions (6.1)]Diphenhydramine (25 to 50 mg) administered intravenously or orally Administer 30-60 minutes prior to each infusion Antipyretic
[see Adverse Reactions (6.1)]Acetaminophen (650 to 1,000 mg) administered intravenously or orally Administer 30-60 minutes prior to each infusion Antiemetics
[see Adverse Reactions (6.1)]5-HT3 serotonin receptor antagonist or appropriate alternatives intravenously or oral Prior to each infusion and thereafter as needed 2.4 Dosage Modifications
Dosage Modifications for Adverse Reactions
The recommended dose reduction levels for adverse reactions are described in Table 2.
Table 2: Recommended Dosage Reductions of DATROWAY for Adverse Reactions Dose Reductions Recommended Dose First 4 mg/kg (up to a maximum of 360 mg for patients ≥90 kg) Second 3 mg/kg (up to a maximum of 270 mg for patients ≥90 kg) Third Permanently discontinue Do not re-escalate the DATROWAY dose after a dose reduction. Permanently discontinue DATROWAY in patients who are unable to tolerate 3 mg/kg intravenously once every 3 weeks.
The recommended dosage modifications and management of adverse reactions for DATROWAY are described in Table 3.
Table 3: Dosage Modifications and Management of Adverse Reactions for DATROWAY Adverse Reaction Severity * Dosage Modifications - * Toxicity grades are in accordance with National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) version 5.0.
Interstitial Lung Disease (ILD)/Pneumonitis
[see Warnings and Precautions (5.1)]Asymptomatic ILD/pneumonitis Grade 1 Withhold DATROWAY until ILD/pneumonitis is completely resolved, then: - if resolved in ≤28 days, maintain current dose.
- if resolved in >28 days, reduce one dose level (see Table 2).
- Consider corticosteroids as soon as ILD/pneumonitis is suspected.
Symptomatic ILD/pneumonitis Grade 2 or greater - Permanently discontinue DATROWAY.
- Administer corticosteroids as soon as ILD/pneumonitis is suspected.
Keratitis
[see Warnings and Precautions (5.2) and Adverse Reactions (6.1)]Nonconfluent superficial keratitis - Monitor.
- Continue DATROWAY at current dose.
Confluent superficial keratitis, a cornea epithelial defect, or 3-line or more loss in best corrected visual acuity - Withhold DATROWAY until improved or resolved
- Restart DATROWAY at the same dose level or consider dose reduction (see Table 2).
Corneal ulcer or stromal opacity or best corrected distance visual acuity 20/200 or worse - Withhold DATROWAY until improved or resolved
- Restart DATROWAY at reduced dose level (see Table 2).
Corneal perforation - Permanently discontinue DATROWAY.
Stomatitis
[see Warnings and Precautions (5.3)]Grade 1 - Optimize prophylactic and supportive medications.
- Continue DATROWAY at current dose.
Grade 2 - Withhold DATROWAY until resolved to ≤Grade 1.
- Restart DATROWAY at the same dose level for first occurrence.
- Recurrence: consider restarting at reduced dose level (see Table 2).
Grade 3 - Withhold DATROWAY until resolved to ≤Grade 1.
- Restart DATROWAY at reduced dose level (see Table 2).
Grade 4 - Permanently discontinue DATROWAY.
Infusion-Related Reactions (IRR)
[see Adverse Reactions (6.1)]Grade 1 - Reduce DATROWAY infusion rate by 50% if IRR is suspected and monitor patient closely.
Grade 2 - Interrupt DATROWAY infusion and administer supportive care medications.
- If the event resolves or improves to Grade 1, restart the infusion at 50% rate.
- Administer all subsequent infusions at the reduced rate.
Grade 3 or 4 - Permanently discontinue DATROWAY.
Other Non-Hematologic Adverse Reactions
[see Adverse Reactions (6.1)]Grade 3 - Withhold dose until resolved to ≤Grade 1 or baseline
- Restart DATROWAY at reduced dose level (see Table 2).
Grade 4 - Permanently discontinue DATROWAY.
2.5 Preparation and Administration
Reconstitute and further dilute DATROWAY prior to intravenous infusion. Use appropriate aseptic technique.
DATROWAY (datopotamab deruxtecan-dlnk) is a hazardous drug. Follow applicable special handling and disposal procedures.1
Reconstitution
- Reconstitute immediately before dilution.
- More than one vial may be needed for a full dose. Calculate the dose (mg), the total volume of reconstituted DATROWAY solution required, and the number of vial(s) of DATROWAY needed [see Dosage and Administration (2.2)].
- Reconstitute each 100 mg vial using a sterile syringe to slowly inject 5 mL of Sterile Water for Injection into each vial to obtain a final concentration of 20 mg/mL.
- Swirl the vial gently until completely dissolved. Do not shake.
- If not used immediately, refrigerate the reconstituted DATROWAY solution in the original vial at 2ºC to 8ºC (36°F to 46°F) for up to 24 hours from the time of reconstitution. Protect the vial from light. Do not freeze.
- The product does not contain a preservative. Discard unused reconstituted DATROWAY after 24 hours refrigerated.
Dilution
- Withdraw the calculated amount from the vial(s) using a sterile syringe. Inspect for particulate matter and discoloration prior to administration. The reconstituted solution should be clear and colorless to light yellow. Do not use if visible particles are observed or if the solution is cloudy or discolored.
- Dilute the calculated volume of reconstituted DATROWAY in an infusion bag containing 100 mL of 5% Dextrose Injection. DO NOT use Sodium Chloride Injection. DATROWAY is compatible with an infusion bag made of polyvinylchloride or polyolefin (polypropylene or copolymer of ethylene and propylene).
- Gently invert the infusion bag to thoroughly mix the solution. Do not shake.
- Cover the infusion bag to protect from light.
- If not used immediately, store at room temperature at up to 25ºC (77°F) for up to 4 hours including preparation or in a refrigerator at 2ºC to 8ºC (36°F to 46°F) for up to 24 hours. Do not freeze.
- Discard any unused portion left in the vial.
Administration
- The maximum time from reconstitution of the vial through the end of administration should not exceed 24 hours. Discard if storage time exceeds these limits.
- If the prepared infusion solution was stored refrigerated at 2ºC to 8ºC (36°F to 46°F), allow the solution to reach room temperature prior to administration, protected from light.
- Inspect for particulate matter and discoloration prior to administration.
- Administer DATROWAY as an intravenous infusion only with an infusion line and tubing set made of polyvinyl chloride, polybutadiene or low-density polyethylene.
- Administer DATROWAY with a 0.2-micron in-line polytetrafluoroethylene, polyethersulfone or nylon 66 filter.
- Do NOT administer as an intravenous push or bolus.
- Cover the infusion bag to protect from light during administration.
- Do not mix DATROWAY with other drugs or administer other drugs through the same intravenous line.
- Instruct the patient to hold ice chips or ice water in the mouth throughout the infusion of DATROWAY.
- First infusion: Administer infusion over 90 minutes. Observe patients during the infusion and for at least 1 hour following the initial dose for signs or symptoms of infusion-related reactions.
- Second Infusion: If first infusion was tolerated, administer second infusion over 30 minutes. Observe patients during the infusion and for at least 1 hour after infusion.
- Subsequent Infusions: Administer infusion over 30 minutes if prior infusions were tolerated. Observe patients during the infusion and for at least 30 min after infusion.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Interstitial Lung Disease/Pneumonitis
DATROWAY can cause severe, life-threatening, or fatal interstitial lung disease (ILD) or pneumonitis.
Locally Advanced or Metastatic NSCLC
In the pooled safety population of 484 patients with NSCLC from TROPION-Lung01, TROPION-Lung05, and TROPION-PanTumor01 [see Adverse Reactions (6.1)], ILD/pneumonitis occurred in 7% of patients treated with DATROWAY, including 0.6% of patients with Grade 3 and 0.4% with Grade 4. There were 8 (1.7%) fatal cases. The median time to onset for ILD was 1.4 months (range: 0.2 months to 9 months). Eleven patients (2.3%) had DATROWAY withheld and 20 patients (4.1%) permanently discontinued DATROWAY due to ILD/pneumonitis. Systemic corticosteroids were required in 79% (26/33) of patients with ILD/pneumonitis. ILD/pneumonitis resolved in 45% of patients.
Unresectable or Metastatic Breast Cancer
In the pooled safety population of 443 patients with breast cancer from TROPION-Breast01 and TROPION-PanTumor01 [see Adverse Reactions (6.1)], ILD/pneumonitis occurred in 3.6% of patients treated with DATROWAY, including 0.7% of patients with Grade 3. There was one fatal case (0.2%). The median time to onset for ILD was 2.8 months (range: 1.1 months to 10.8 months). Four patients (0.9%) had DATROWAY withheld and 7 patients (1.6%) permanently discontinued DATROWAY due to ILD/pneumonitis. Systemic corticosteroids were required in 60% (9/15) of patients with ILD/pneumonitis. ILD/pneumonitis resolved in 40% of patients.
Patients were excluded from clinical studies for a history of ILD/pneumonitis requiring treatment with steroids or for ongoing ILD/pneumonitis.
Monitor patients for new or worsening respiratory symptoms indicative of ILD/pneumonitis (e.g., dyspnea, cough, fever) during treatment with DATROWAY. For asymptomatic (Grade 1) ILD/pneumonitis, consider corticosteroid treatment (e.g., ≥0.5 mg/kg/day prednisolone or equivalent). For symptomatic ILD/pneumonitis (Grade 2 or greater), promptly initiate systemic corticosteroid treatment (e.g., ≥1 mg/kg/day prednisolone or equivalent) and continue for at least 14 days followed by gradual taper for at least 4 weeks.
Withhold DATROWAY in patients with suspected ILD/pneumonitis and permanently discontinue DATROWAY if ≥Grade 2 ILD/pneumonitis is confirmed [see Dosage and Administration (2.4)].
5.2 Ocular Adverse Reactions
DATROWAY can cause ocular adverse reactions including dry eye, keratitis, blepharitis, meibomian gland dysfunction, increased lacrimation, conjunctivitis, and blurred vision.
In the pooled safety population [see Adverse Reactions (6.1)], ocular adverse reactions occurred in 36% of patients treated with DATROWAY. Twenty patients (2.2%) experienced Grade 3 ocular adverse reactions, which included keratitis, dry eye, and blurred vision, and one patient experienced a Grade 4 ocular adverse reaction of conjunctival hemorrhage. The most common (≥5%) ocular adverse reactions were dry eye (17%), keratitis (14%), and increased lacrimation (7%). The median time to onset for ocular adverse reactions was 2.3 months (range: 0.03 months to 23.2 months). Of the patients who experienced ocular adverse reactions, 39% had complete resolution, and 10% had partial improvement (defined as a decrease in severity by one or more grades from the worst grade at last follow up). Ocular adverse reactions led to dosage interruption in 3.6% of patients, dosage reductions in 2.5% of patients, and permanent discontinuation of DATROWAY in 1% of patients.
Patients with clinically significant corneal disease were excluded from clinical studies.
Advise patients to use preservative-free lubricant eye drops several times daily for prophylaxis. Advise patients to avoid use of contact lenses unless directed by an eye care professional.
Refer patients to an eye care professional for an ophthalmic exam including visual acuity testing, slit lamp examination (with fluorescein staining), intraocular pressure, and fundoscopy at treatment initiation, annually while on treatment, at end of treatment, and as clinically indicated.
Promptly refer patients to an eye care professional for any new or worsening ocular adverse reactions. Monitor patients for ocular adverse reactions during treatment with DATROWAY, and if diagnosis is confirmed, withhold, reduce the dose, or permanently discontinue DATROWAY based on severity [see Dosage and Administration (2.4)].
5.3 Stomatitis
DATROWAY can cause stomatitis, including mouth ulcers and oral mucositis.
In the pooled safety population [see Adverse Reactions (6.1)], stomatitis occurred in 63% of patients treated with DATROWAY, including 8% of patients with Grade 3 events and one patient with a Grade 4 reaction. The median time to first onset of stomatitis was 0.5 months (range: 0.03 months to 18.6 months). Stomatitis led to dosage interruption in 6% of patients, dosage reductions in 11% of patients, and permanent discontinuation of DATROWAY in 0.5% of patients.
In patients who received DATROWAY in TROPION-Breast01, 39% used a mouthwash containing corticosteroid for management or prophylaxis of stomatitis/oral mucositis at any time during the treatment.
Advise patients to use a steroid-containing mouthwash for prophylaxis and treatment of stomatitis. Instruct the patient to hold ice chips or ice water in the mouth throughout the infusion of DATROWAY.
Monitor patients for signs and symptoms of stomatitis. If stomatitis occurs, increase the frequency of mouthwash and administer other topical treatments as clinically indicated. Based on the severity of the adverse reaction, withhold, reduce the dose, or permanently discontinue DATROWAY [see Dosage and Administration (2.4)].
5.4 Embryo-Fetal Toxicity
Based on its mechanism of action, DATROWAY can cause embryo-fetal harm when administered to a pregnant woman because the topoisomerase inhibitor component of DATROWAY, DXd [see Description (11)], is genotoxic and affects actively dividing cells [see Use in Specific Populations (8.1), Clinical Pharmacology (12.1), Nonclinical Toxicology (13.1)].
Advise patients of the potential risk to a fetus. Advise female patients of reproductive potential to use effective contraception during treatment with DATROWAY and for 7 months after the last dose. Advise male patients with female partners of reproductive potential to use effective contraception during treatment with DATROWAY and for 4 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Interstitial Lung Disease/Pneumonitis [see Warnings and Precautions (5.1)]
- Ocular Adverse Reactions [see Warnings and Precautions (5.2)]
- Stomatitis [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The pooled safety population described in WARNINGS AND PRECAUTIONS reflects exposure to DATROWAY in 927 patients as a single agent at 6 mg/kg administered as an intravenous infusion once every 3 weeks (21-day cycle) until disease progression or unacceptable toxicity. This included 137 patients with NSCLC in TROPION-Lung05 [see Clinical Studies (14.1)], 297 patients with NSCLC in TROPION-Lung01 [see Clinical Studies (14.1)], 360 patients with HR-positive, HER2-negative breast cancer in TROPION-Breast01 [see Clinical Studies (14.2)], and 50 patients with NSCLC and 83 patients with breast cancer in TROPION-PanTumor01 (NCT03401385). Among 927 patients who received DATROWAY, 45% were exposed for 6 months or longer and 19% were exposed for greater than one year. In this pooled safety population, the most common (≥20%) adverse reactions were stomatitis (63%), nausea (52%), fatigue (45%), alopecia (38%), constipation (28%), decreased appetite (23%), rash (23%), vomiting (22%), and musculoskeletal pain (20%). In this pooled safety population, the most common (≥2%) Grade 3 or 4 laboratory abnormalities were decreased lymphocytes (9%) and decreased hemoglobin (3.5%).
Locally Advanced or Metastatic EGFR-Mutated Non-Small Cell Lung Cancer
TROPION-Lung05, TROPION-Lung01, TROPION-PanTumor01
The safety of DATROWAY was evaluated in 125 patients with EGFR-mutated NSCLC who received DATROWAY 6 mg/kg administered as an intravenous infusion once every 3 weeks (21-day cycle) until disease progression or unacceptable toxicity in TROPION-Lung05 and TROPION-Lung01 [see Clinical Studies (14.1)] as well as TROPION-PanTumor01 (NCT03401385). Among these patients, the median duration of treatment was 6.1 months (range 0.7 months to 41.7 months).
The median age was 63 years (range: 36 to 81), 56% of patients were <65 years, 62% of patients were female; 66% were Asian, 26% were White, 0.8% were Black, 6% were other races; and 2.4% were of Hispanic ethnicity.
Serious adverse reactions occurred in 26% of patients who received DATROWAY. Serious adverse reactions in >1% of patients who received DATROWAY were COVID-19 (4%), stomatitis (2.4%), and pneumonia (1.6%). Fatal adverse reactions occurred in 1.6% of patients who received DATROWAY, due to death not otherwise specified.
Permanent discontinuation of DATROWAY due to an adverse reaction occurred in 8% of patients. Adverse reactions which resulted in permanent discontinuation of DATROWAY in >1% of patients included ILD/pneumonitis (2.4%) and abnormal hepatic function (1.6%).
Dosage interruptions of DATROWAY due to an adverse reaction occurred in 43% of patients. Adverse reactions which required dosage interruption in >1% of patients included COVID-19 (13%), stomatitis (7%), fatigue (6%), pneumonia (4%), anemia (2.4%), amylase increased (2.4%), keratitis (2.4%), ILD/pneumonitis (1.6%), decreased appetite (1.6%), dyspnea (1.6%), rash (1.6%), and infusion-related reaction (1.6%).
Dose reductions of DATROWAY due to an adverse reaction occurred in 26% of patients. Adverse reactions which required dose reduction in >1% of patients included stomatitis (14%), keratitis (1.6%), fatigue (1.6%), decreased weight (1.6%) and COVID-19 (1.6%).
The most common (≥20%) adverse reactions, including laboratory abnormalities, were stomatitis, nausea, alopecia, fatigue, decreased hemoglobin, decreased lymphocytes, constipation, increased calcium, increased AST, decreased white blood cell count, increased lactate dehydrogenase, musculoskeletal pain, decreased appetite, increased ALT, and rash.
Table 4: Adverse Reactions (≥10%) in Patients with Locally Advanced or Metastatic EGFR-Mutated NSCLC Who Received DATROWAY in TROPION-Lung05, TROPION-Lung01, and TROPION-PanTumor01 Adverse Reaction DATROWAY
N=125All Grades
%Grades 3 or 4
%Events were graded using NCI CTCAE v5.0. - * Includes other related terms
- † Includes fatigue, asthenia, and malaise
- ‡ Includes corneal disorder, corneal erosion, keratitis, punctate keratitis, and ulcerative keratitis
Gastrointestinal disorders Stomatitis* 71 9 Nausea 50 0 Constipation 31 0 Vomiting 16 0.8 Diarrhea 12 0 Skin and subcutaneous tissue disorders Alopecia 49 0 Rash* 20 0.8 Pruritus 12 0 General disorders and administration site conditions Fatigue† 42 6 Musculoskeletal and connective tissue disorders Musculoskeletal pain 22 0.8 Metabolism and nutrition disorders Decreased appetite 20 1.6 Infections and Infestations COVID-19* 19 2.4 Respiratory, Thoracic, and Mediastinal Disorders Cough* 18 0 Dyspnea 11 2.4 Eye disorders Dry eye 13 0 Keratitis‡ 12 2.4 Injury, poisoning and procedural complications Infusion-related reaction* 13 0 Nervous system disorders Headache 13 0 Clinically relevant adverse reactions occurring in <10% of patients who received DATROWAY included dry skin, blurred vision, abdominal pain, conjunctivitis, dry mouth, ILD/pneumonitis, skin hyperpigmentation, increased lacrimation, and visual impairment.
Table 5: Select Laboratory Abnormalities (≥20%) that Worsened from Baseline in Patients with Locally Advanced or Metastatic EGFR-Mutated NSCLC Who Received DATROWAY in TROPION-Lung05, TROPION-Lung01, and TROPION-PanTumor01 Laboratory Abnormality* DATROWAY† All Grades
%Grades 3 or 4
%- * Frequencies were based on NCI CTCAE v5.0 grade-derived laboratory abnormalities.
- † The denominator used to calculate the rate varied from 115 to 124 based on the number of patients with a baseline value and at least one post-treatment value.
Hematology Decreased hemoglobin 34 4.8 Decreased lymphocytes 32 11 Decreased white blood cell count 27 1.6 Chemistry Increased calcium 31 0 Increased AST 28 2.4 Increased lactate dehydrogenase 23 0 Increased ALT 20 2.4 Unresectable or Metastatic, HR-Positive, HER2-Negative Breast Cancer
TROPION-Breast01
The safety of DATROWAY was evaluated in 360 patients with unresectable or metastatic HR-positive, HER2-negative (IHC 0, IHC1+ or IHC2+/ISH-) breast cancer who received at least one dose of DATROWAY 6 mg/kg in TROPION-Breast01 [see Clinical Studies (14.2)]. DATROWAY was administered by intravenous infusion once every three weeks. The median duration of treatment was 6.7 months (range: 0.7 months to 16.1 months) for patients who received DATROWAY.
Serious adverse reactions occurred in 15% of patients who received DATROWAY. Serious adverse reactions in >0.5% of patients who received DATROWAY were urinary tract infection (1.9%), COVID-19 infection (1.7%), ILD/pneumonitis (1.1%), acute kidney injury, pulmonary embolism, vomiting, diarrhea, hemiparesis, and anemia (0.6% each). Fatal adverse reactions occurred in 0.3% of patients who received DATROWAY and were due to ILD/pneumonitis.
Permanent discontinuation of DATROWAY due to an adverse reaction occurred in 3.1% of patients. Adverse reactions which resulted in permanent discontinuation of DATROWAY in >0.5% of patients included ILD/pneumonitis (1.7%) and fatigue (0.6%).
Dosage interruptions of DATROWAY due to an adverse reaction occurred in 22% of patients. Adverse reactions which required dosage interruption in >1% of patients included COVID-19 (3.3%), infusion-related reaction (1.4%), ILD/pneumonitis (1.9%), stomatitis (1.9%), fatigue (1.7%), keratitis (1.4%), acute kidney injury (1.1%), and pneumonia (1.1%).
Dose reductions of DATROWAY due to an adverse reaction occurred in 23% of patients. Adverse reactions which required dose reduction in >1% of patients included stomatitis (13%), fatigue (3.1%), nausea (2.5%), and weight decrease (1.9%).
The most common (≥20%) adverse reactions, including laboratory abnormalities, were stomatitis, nausea, fatigue, decreased leukocytes, decreased calcium, alopecia, decreased lymphocytes, decreased hemoglobin, constipation, decreased neutrophils, dry eye, vomiting, increased ALT, keratitis, increased AST, and increased alkaline phosphatase.
Table 6: Adverse Reactions (≥10%) in Patients Who Received DATROWAY in TROPION-Breast01 Adverse Reactions DATROWAY
N=360Chemotherapy
N=351All Grades
%Grades 3 or 4
%All Grades
%Grades 3 or 4
%Events were graded using NCI CTCAE v5.0. - * Includes other related terms.
- † Includes fatigue, asthenia, lethargy, malaise
- ‡ Includes corneal disorder, corneal erosion, corneal infiltrates, corneal lesion, corneal toxicity, injury corneal, keratitis, keratopathy, punctate keratitis, and ulcerative keratitis
Gastrointestinal Disorders Stomatitis * 59 7 17 2.6 Nausea 56 1.4 27 0.6 Constipation 34 0.3 17 0 Vomiting 24 1.1 12 1.1 Diarrhea 11 0.6 19 1.4 Abdominal pain * 11 0.6 15 1.4 General Disorders and Administration Site Conditions Fatigue † 44 4.2 40 3.7 Skin and Subcutaneous Tissue Disorders Alopecia 38 0 22 0 Rash * 19 0 17 2.3 Eye Disorders Dry eye 27 0.8 13 0 Keratitis ‡ 24 1.1 10 0 Metabolism and Nutrition Disorders Decreased appetite 16 1.4 16 0.9 Infections and Infestations COVID-19 * 16 1.4 13 0.9 Respiratory, Thoracic, and Mediastinal Disorders Cough * 15 0 10 0 Clinically relevant adverse reactions occurring in <10% of patients who received DATROWAY included infusion-related reactions (including bronchospasm), ILD/pneumonitis, headache, pruritus, dry skin, dry mouth, conjunctivitis, blepharitis, meibomian gland dysfunction, blurred vision, increased lacrimation, photophobia, visual impairment, skin hyperpigmentation, and madarosis.
Table 7: Select Laboratory Abnormalities (≥20%) in Patients Who Received DATROWAY in TROPION-Breast01 Laboratory Abnormality DATROWAY * Chemotherapy * All Grades
%Grades 3-4
%All Grades
%Grades 3-4
%Frequencies were based on NCI CTCAE v5.0 grade-derived laboratory abnormalities. - * The denominator used to calculate the rate varied from 264 to 359 based on the number of patients with a baseline value and at least one post-treatment value.
Hematology Decreased leukocytes 41 1.1 63 18 Decreased lymphocytes 36 9 42 11 Decreased hemoglobin 35 2.8 51 4.4 Decreased neutrophils 30 1.6 61 35 Chemistry Decreased calcium 39 1.4 43 1.2 Increased AST 23 1.9 28 0.9 Increased ALT 24 1.7 31 0.6 Increased alkaline phosphatase 23 0.6 20 0.6 -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on its mechanism of action, DATROWAY can cause embryo-fetal harm when administered to a pregnant woman because the topoisomerase inhibitor component of DATROWAY, DXd, is genotoxic and affects actively dividing cells [see Clinical Pharmacology (12.1), Nonclinical Toxicology (13.1)]. There are no available data on the use of DATROWAY in pregnant women to inform a drug-associated risk. Advise patients of the potential risks to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
8.2 Lactation
Risk Summary
There are no data regarding the presence of datopotamab deruxtecan-dlnk or its metabolites in human milk, the effects on the breastfed child, or the effects on milk production. Because of the potential for serious adverse reactions in a breastfed child, advise women not to breastfeed during treatment with DATROWAY and for 1 month after the last dose.
8.3 Females and Males of Reproductive Potential
DATROWAY can cause embryo-fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].
Pregnancy Testing
Verify pregnancy status of females of reproductive potential prior to initiation of DATROWAY.
Contraception
Females
Advise females of reproductive potential to use effective contraception during treatment with DATROWAY and for 7 months after the last dose.
Males
Because of the potential for genotoxicity, advise male patients with female partners of reproductive potential to use effective contraception during treatment with DATROWAY and for 4 months after the last dose [see Nonclinical Toxicology (13.1)].
Infertility
Based on findings in animal toxicity studies, DATROWAY may impair male and female reproductive function and fertility. The effects on reproductive organs in animals were irreversible [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
Safety and effectiveness of DATROWAY have not been established in pediatric patients.
8.5 Geriatric Use
Of the 125 patients with EGFR-mutated NSCLC in TROPION-Lung05, TROPION-Lung01, TROPION-PanTumor01 treated with DATROWAY 6 mg/kg, 44% were ≥65 years of age and 10% were ≥75 years of age. No clinically meaningful differences in efficacy and safety were observed between patients ≥65 years of age versus younger patients.
Of the 365 patients in TROPION-Breast01 treated with DATROWAY 6 mg/kg, 25% were ≥65 years of age and 5% were ≥75 years of age. Grade ≥3 and serious adverse reactions were more common in patients ≥65 years (42% and 25%, respectively) compared to patients <65 years (33% and 15%, respectively). In TROPION-Breast01, no other meaningful differences in safety or efficacy were observed between patients ≥65 years of age versus younger patients.
8.6 Renal Impairment
A higher incidence of ILD/pneumonitis has been observed in patients with mild and moderate renal impairment (creatinine clearance [CLcr] 30 to <90 mL/min) [see Warnings and Precautions (5.1)]. Monitor patients with renal impairment for increased adverse reactions, including respiratory reactions. No dosage adjustment is recommended in patients with mild to moderate renal impairment [see Clinical Pharmacology (12.3)]. The effect of severe renal impairment (CLcr <30 mL/min) on the pharmacokinetics of datopotamab deruxtecan-dlnk or DXd is unknown.
8.7 Hepatic Impairment
No dosage adjustment is recommended in patients with mild hepatic impairment (total bilirubin ≤ULN and any AST >ULN or total bilirubin >1 to 1.5 times ULN and any AST). Limited data are available in patients with moderate hepatic impairment (total bilirubin >1.5 to 3 times ULN and any AST). Monitor patients with moderate hepatic impairment for increased adverse reactions [see Dosage and Administration (2.4)]. The recommended dosage of DATROWAY has not been established for patients with severe hepatic impairment (total bilirubin >3 times ULN and any AST) [see Clinical Pharmacology (12.3)].
-
11 DESCRIPTION
Datopotamab deruxtecan-dlnk is a Trop-2-directed antibody and topoisomerase inhibitor conjugate. Datopotamab deruxtecan-dlnk is an antibody-drug conjugate (ADC) composed of three components: 1) a humanized anti-Trop-2 IgG1 monoclonal antibody (mAb), covalently linked to 2) a topoisomerase I inhibitor, via 3) a tetrapeptide-based cleavable linker. Deruxtecan is composed of a protease-cleavable maleimide tetrapeptide linker and the topoisomerase inhibitor, DXd, which is an exatecan derivative.
The antibody is produced in Chinese hamster ovary cells by recombinant DNA technology, and the topoisomerase inhibitor and linker are produced by chemical synthesis. Approximately 4 molecules of deruxtecan are attached to each antibody molecule. Datopotamab deruxtecan-dlnk has the following structure:
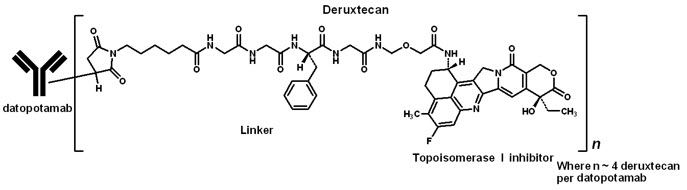
DATROWAY (datopotamab deruxtecan-dlnk) for injection is a sterile, white to yellowish white, preservative-free lyophilized powder in single-dose vials. Each vial delivers 100 mg of datopotamab deruxtecan-dlnk, L-histidine (3.88 mg), L-histidine hydrochloride monohydrate (5.25 mg), polysorbate 80 (1.50 mg), and sucrose (450 mg). Following reconstitution with 5 mL of Sterile Water for Injection, USP, the resulting concentration of datopotamab deruxtecan-dlnk is 20 mg/mL with a pH of 6.0. The resulting solution is administered by intravenous infusion following dilution.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Datopotamab deruxtecan-dlnk, is a Trop-2-directed antibody-drug conjugate. The antibody is a humanized anti-Trop2 IgG1. The small molecule, DXd, is a topoisomerase I inhibitor attached to the antibody by a cleavable linker. Following binding to Trop-2 on cells, including tumor cells, datopotamab deruxtecan-dlnk undergoes internalization and intracellular linker cleavage by lysosomal enzymes. Upon release, the membrane-permeable DXd causes DNA damage and apoptotic cell death. Datopotamab deruxtecan-dlnk had anti-tumor activity in mouse models of lung cancer including EGFR-mutated and breast cancer.
12.2 Pharmacodynamics
Datopotamab deruxtecan-dlnk time course of pharmacodynamic response is unknown.
Exposure-Response Relationships
A relationship between datopotamab deruxtecan-dlnk exposure and efficacy has not been fully characterized in breast cancer or EGFR-mutated NSCLC.
In the pooled population of NSCLC (including EGFR-mutated NSCLC) and breast cancer patients, higher datopotamab deruxtecan-dlnk systemic exposure is associated with a higher incidence rate of serious adverse reactions, dosage interruptions, dose reductions, stomatitis/oral mucositis, ocular adverse reactions, and Grade ≥3 adverse reactions.
12.3 Pharmacokinetics
Datopotamab deruxtecan-dlnk and DXd exposure after the first dose of the approved recommended dosage of cycle 1 are provided in Table 8. Datopotamab deruxtecan-dlnk and released DXd maximum concentration (Cmax) and area under the time-concentration curve (AUC) increases proportionally over a dose range of 4 mg/kg to 10 mg/kg (approximately 0.7 to 1.7 times the approved recommended dosage). No clinically significant datopotamab deruxtecan-dlnk accumulation occurs between cycles 1 and 3.
Table 8: Datopotamab Deruxtecan-dlnk and DXd Mean (CV%) Exposure After the First Dose PK Parameter Datopotamab deruxtecan-dlnk DXd Abbreviations: Cmax =maximum concentration; AUC =area under the time-concentration curve Cmax 154 µg/mL (20%) 2.8 ng/mL (58%) AUC 671 µg*day/mL (31%) 18 ng*day/mL (43%) Distribution
Datopotamab deruxtecan-dlnk mean steady state volume of distribution is 3.5 (23%) L.
DXd plasma protein binding is approximately 98% and the blood-to-plasma concentration ratio is 0.6 in vitro.
Elimination
The datopotamab deruxtecan-dlnk median elimination half-life (t1/2) is 4.8 days (1.0, 8.2) and the released DXd median apparent t1/2 is approximately 5.5 days (3.2, 8.8). The estimated datopotamab deruxtecan-dlnk clearance is 0.6 (31.5%) L/day.
Metabolism
Datopotamab deruxtecan-dlnk undergoes intracellular cleavage by lysosomal enzymes to release DXd.
The humanized Trop-2 IgG1 monoclonal antibody is expected to be degraded into small peptides and amino acids via catabolic pathways in the same manner as endogenous IgG.
In vitro, DXd is primarily metabolized by CYP3A4.
Specific Populations
The mean volume of distribution and clearance of datopotamab deruxtecan-dlnk and DXd increase with increasing body weight (36 kg to 156 kg).
No clinically significant differences in the pharmacokinetics of datopotamab deruxtecan-dlnk or DXd were observed based on age (26 to 86 years), race (Asian, White, or Black), sex, mild hepatic impairment (total bilirubin ≤ULN and any AST >ULN or total bilirubin >1 to 1.5 times ULN and any AST), or mild to moderate renal impairment (CLcr 30 to <90 mL/min).
The pharmacokinetics of datopotamab deruxtecan-dlnk in patients with moderate hepatic impairment (total bilirubin >1.5 to 3 times ULN and any AST) was comparable to patients with normal hepatic function (total bilirubin and AST ≤ULN). The steady state average DXd AUC was 2.4-fold higher in patients with moderate hepatic impairment compared to patients with normal hepatic function. The effect of severe hepatic impairment (total bilirubin >3 times ULN and any AST) or severe renal impairment (CLcr <30 mL/min) on datopotamab deruxtecan-dlnk or DXd pharmacokinetics is unknown.
Drug Interaction Studies
Clinical Studies and Model-Informed Approaches
No clinically significant differences in DXd pharmacokinetics were predicted when used concomitantly with itraconazole (strong CYP3A inhibitor) or ritonavir (dual OATP1B and CYP3A inhibitor).
12.6 Immunogenicity
There is insufficient information from TROPION-Breast01, TROPION-Lung01, and TROPION-Lung05 to characterize the anti-drug antibody response to datopotamab deruxtecan-dlnk and the effects of anti-drug antibodies on pharmacokinetics, pharmacodynamics, safety, or effectiveness of datopotamab deruxtecan-dlnk products.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies have not been conducted with datopotamab deruxtecan-dlnk.
The topoisomerase inhibitor component of datopotamab deruxtecan-dlnk, DXd, was clastogenic in both an in vivo rat bone marrow micronucleus assay and an in vitro Chinese hamster lung chromosome aberration assay and was not mutagenic in an in vitro bacterial reverse mutation assay.
Dedicated fertility studies have not been conducted with datopotamab deruxtecan-dlnk. In a 3-month repeat-dose toxicity study, intravenous administration of datopotamab deruxtecan-dlnk once every 3 weeks in rats resulted in decreased weights in the testes and epididymides, degeneration of the germinal epithelium and atrophy of seminiferous tubules in testes, and cell debris, decreased number of sperm, and single-cell necrosis of the ductal epithelium in epididymides at 200 mg/kg (approximately 29 times the human recommended dose of 6 mg/kg based on AUC). Findings in female rats included increased atretic follicles in the ovary and single cell necrosis of mucosal epithelium in the vagina at 200 mg/kg. These findings, except for the lesions in the testis and epididymis, were not observed after a 2-month recovery period.
-
14 CLINICAL STUDIES
14.1 Locally Advanced or Metastatic EGFR-Mutated Non-Small Cell Lung Cancer
The efficacy of DATROWAY was evaluated in a pooled subgroup of patients with locally advanced or metastatic EGFR-mutated NSCLC who were enrolled across two clinical studies: TROPION-Lung05 and TROPION-Lung01.
TROPION-Lung05 (NCT04484142) was a global, multicenter, single-arm, open-label trial in patients with previously treated NSCLC with an actionable genomic alteration and TROPION-Lung01 (NCT04656652) was a global, multicenter, randomized, active-controlled, open-label trial in patients with previously treated NSCLC with or without an actionable genomic alteration. For both trials, eligible patients with EGFR-mutated NSCLC must have previously received an EGFR-directed therapy and platinum-based chemotherapy. Patients with a history of ILD/pneumonitis requiring treatment with steroids, ongoing ILD/pneumonitis, or clinically significant corneal disease at screening were ineligible. Patients who had brain metastases that were untreated and symptomatic were also ineligible. Patients received DATROWAY 6 mg/kg by intravenous infusion every 3 weeks until unacceptable toxicity or disease progression.
For the pooled efficacy population, the major efficacy outcome measure was overall response rate (ORR) by BICR per RECIST v1.1. An additional efficacy outcome was duration of response (DOR) by BICR.
Efficacy was assessed in 114 patients with EGFR-mutated NSCLC. The median age was 63 years (range 36 to 81); 43% were ≥65 years of age; 63% were female; 70% were Asian and 22% were White; 1.8% were of Hispanic/Latino ethnicity; 68% had ECOG PS of 1 and 32% had ECOG PS of 0; and 33% had brain metastases at baseline. Fifty-three percent (53%) of patients had tumors with exon 19 deletions, 34% had exon 21 L858R mutations, 28% had T790M mutations, 2.6% had exon 20 insertion mutations and 14% had other EGFR mutations. Four percent (4.4%) of patients received one prior line of systemic therapy, 39% received two prior lines of systemic therapy, and 57% received three or more prior lines of systemic therapy in the locally advanced or metastatic setting. All patients received prior EGFR-directed therapy including 84% receiving prior osimertinib; 99% received prior platinum-based chemotherapy and 28% received prior anti-PD-1/ PD-L1 therapy.
Efficacy results are summarized in Table 9.
Table 9: Efficacy Results in TROPION-Lung05 and TROPION-Lung01 by BICR DATROWAY TL05
N=77DATROWAY TL01
N=37DATROWAY Pooled
N=114CI: confidence interval Overall Response Rate (95% CI) 45% (34, 57) 43% (27, 61) 45% (35, 54) Complete Response 5% 2.7% 4.4% Partial Response 40% 41% 40% Duration of Response Median, months (95% CI) 6.9 (4.2, 10.2) 6.5 (4.0, 8.4) 6.5 (4.2, 8.4) ≥6 months 49% 44% 47% ≥12 months 23% 6% 18% In the TROPION-Lung05 trial, a difference was noted between ORR by BICR and ORR assessed by investigator; investigator assessed ORR was 34% (95% CI: 23, 45). In the TROPION-Lung01 trial, ORR assessed by investigator was similar to ORR by BICR.
14.2 Unresectable or Metastatic, HR-Positive, HER2-Negative Breast Cancer
TROPION-Breast01
The efficacy of DATROWAY was evaluated in TROPION-Breast01 (NCT05104866), a multicenter, open-label, randomized trial of 732 patients with unresectable or metastatic HR-positive, HER2-negative (IHC 0, IHC1+ or IHC2+/ISH-) breast cancer. Eligible patients must have progressed on and deemed not suitable for further endocrine therapy. Patients were required to have received 1 or 2 lines of prior chemotherapy in the unresectable or metastatic disease setting. Patients were excluded for a history of ILD/pneumonitis requiring treatment with steroids, ongoing ILD/pneumonitis, clinically active brain metastases, or clinically significant corneal disease at screening. Patients were also excluded for ECOG performance status >1. Randomization was stratified by previous lines of chemotherapy (one or two), prior treatment with a CDK4/6 inhibitor (yes or no), and geographical region.
A total of 732 patients were randomized 1:1 to receive either DATROWAY 6 mg/kg (N=365) by intravenous infusion every 3 weeks or investigator's choice of chemotherapy (N=367) until unacceptable toxicity or disease progression. Single agent chemotherapy was determined by the investigator before randomization from one of the following choices: eribulin (60%), capecitabine (21%), vinorelbine (10%), or gemcitabine (9%).
The major efficacy outcomes were progression-free survival (PFS) as assessed by blinded independent central review (BICR) based on Response Evaluation Criteria in Solid Tumors (RECIST) v.1.1 and overall survival (OS). Additional efficacy outcomes included confirmed objective response rate (ORR) and duration of response (DOR) by BICR.
The median age was 55 years (range 28-86); 22% were ≥65 years; 99% were female; 48% were White, 41% were Asian, 1.5% were Black or African American, and 11% were of Hispanic/Latino ethnicity; 57% had ECOG PS of 0 and 42% had ECOG PS of 1; 97% had visceral disease, 72% had liver metastases, and 8% had stable brain metastases.
Sixty percent (60%) of patients received prior endocrine therapy in the (neo)adjuvant setting, and 89% received prior endocrine therapy in the unresectable or metastatic setting. Eighty-three percent (83%) of patients had prior treatment with a CDK4/6 inhibitor. All patients received prior chemotherapy regimens in the unresectable or metastatic setting (81% received prior taxanes; 64% received prior anthracyclines). Sixty-two percent (62%) of patients had 1 prior chemotherapy regimen and 38% of patients had 2 prior chemotherapy regimens for treatment of unresectable or metastatic disease.
The study demonstrated a statistically significant improvement in PFS in patients randomized to DATROWAY compared to chemotherapy.
Efficacy results are shown in Table 10 and Figure 1.
Table 10: Efficacy Results in TROPION-Breast01 DATROWAY
(n=365)Chemotherapy
(n=367)CI: Confidence interval; NS: not statistically significant - * Assessed by BICR
- † Based on the stratified Cox proportional hazards model
- ‡ Two-sided p-value based on stratified log-rank test.
- § p-value is compared with the allocated alpha of 0.01.
Progression-Free Survival * Number of events (%) 212 (58) 235 (64) Progressive Disease 201 (55) 218 (59) Death 11 (3) 17 (5) Median, months (95% CI) 6.9 (5.7, 7.4) 4.9 (4.2, 5.5) Hazard ratio (95% CI) † 0.63 (0.52, 0.76) p-value ‡, § < 0.0001 Overall Survival Number of events (%) 223 (61) 213 (58) Median, months (95% CI) 18.6 (17.3, 20.1) 18.3 (17.3, 20.5) Hazard ratio (95% CI) † 1.01 (0.83, 1.22) p-value ‡ NS Confirmed Objective Response Rate * n (%) 133 (36) 84 (23) (95% CI) 31, 42 19, 28 Complete Response n (%) 2 (0.5) 0 Partial Response n (%) 131 (36) 84 (23) Duration of Response * Median, months (95% CI) 6.7 (5.6, 9.8) 5.7 (4.9, 6.8) Figure 1: Kaplan-Meier Plot of PFS by BICR in TROPION-Breast-01 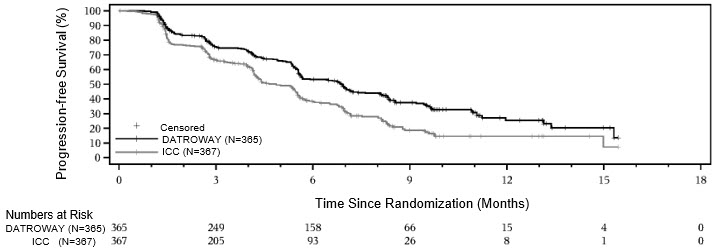
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
DATROWAY (datopotamab deruxtecan-dlnk) for injection is a white to yellowish white lyophilized powder supplied as:
Carton Contents NDC One 100 mg single-dose vial NDC: 65597-801-01 Storage and Handling
Store vials in a refrigerator at 2ºC to 8ºC (36ºF to 46ºF) in the original carton to protect from light until time of reconstitution. Do not freeze. Do not shake the reconstituted or diluted solution [see Dosage and Administration (2.5)].
DATROWAY (datopotamab deruxtecan-dlnk) is a hazardous drug. Follow applicable special handling and disposal procedures.1
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Interstitial Lung Disease/Pneumonitis
- Inform patients of the risks of severe or fatal ILD. Advise patients to contact their healthcare provider immediately for any of the following: cough, shortness of breath, fever, or other new or worsening respiratory symptoms [see Warnings and Precautions (5.1)].
Ocular Adverse Reactions
- Inform patients about the need for eye exams at initiation and during treatment with DATROWAY [see Dosage and Administration (2.3)].
- Advise patients to contact their healthcare provider if they experience any eye symptoms [see Warnings and Precautions (5.2)].
- Advise patients to use preservative-free lubricating eye drops several times daily and to avoid use of contact lenses during treatment with DATROWAY [see Dosage and Administration (2.3, 2.4)].
Stomatitis
- Inform patients of the risk of stomatitis. Advise patients to contact their healthcare provider if they experience any symptoms.
- Inform patients to use a steroid-containing mouthwash for prophylaxis and treatment of stomatitis.
- Instruct patients to hold ice chips or ice water in their mouth throughout the infusion of DATROWAY [see Warnings and Precautions (5.3)].
Embryo-Fetal Toxicity
- Inform female patients of the potential risk to a fetus. Advise female patients to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.4), Use in Specific Populations (8.1)].
- Advise females of reproductive potential to use effective contraception during treatment with DATROWAY and for 7 months after the last dose [see Use in Specific Populations (8.3)].
- Advise male patients with female partners of reproductive potential to use effective contraception during treatment with DATROWAY and for 4 months after the last dose [see Use in Specific Populations (8.3)].
Lactation
- Advise women not to breastfeed during treatment and for 1 month after the last dose of DATROWAY [see Use in Specific Populations (8.2)].
Infertility
- Advise males and females of reproductive potential that DATROWAY may impair fertility [see Use in Specific Populations (8.3)].
-
SPL UNCLASSIFIED SECTION
Manufactured by:
Daiichi Sankyo, Inc., Basking Ridge, NJ 07920U.S. License No. 2128
Marketed by:
Daiichi Sankyo, Inc., Basking Ridge, NJ 07920 and AstraZeneca Pharmaceuticals LP, Wilmington, DE 19850DATROWAY® is a registered trademark of Daiichi Sankyo Company, Ltd.
© 2025 Daiichi Sankyo Co., Ltd.USPI-DAT-C7-0625-r002
-
MEDICATION GUIDE
This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: 06/2025 MEDICATION GUIDE
DATROWAY® (DAT-roe-way)
(datopotamab deruxtecan-dlnk)
for injection, for intravenous useWhat is the most important information I should know about DATROWAY?
DATROWAY can cause serious side effects, including:-
Lung problems that may be severe, life-threatening, or that may lead to death. If you develop lung problems your healthcare provider may treat you with corticosteroid medicines. Tell your healthcare provider right away if you get any of the following signs and symptoms:
- cough
- trouble breathing or shortness of breath
- fever
- other new or worsening breathing symptoms such as chest tightness or wheezing
-
Eye problems. Eye problems are common with DATROWAY and can also be severe. Tell your healthcare provider right away if you develop any new or worsening eye problems during treatment with DATROWAY, including dry eyes, eye pain, eye redness, eye swelling, eye irritation, increased tears, feeling like something is in your eyes, discharge from your eyes, eye crusting, sensitivity to light, blurred vision, or vision changes.
- You should use preservative-free lubricating eye drops at least 4 times a day and as needed.
- Do not wear contact lenses during treatment with DATROWAY unless your eye specialist tells you to.
- Your healthcare provider will send you to an eye specialist to check your eyes when you start your treatment with DATROWAY, every year during treatment, at the end of treatment, and as needed for any new or worsening signs and symptoms of eye problems.
-
Mouth ulcers and sores. Mouth ulcers and sores are common with DATROWAY and can also be severe. Tell your healthcare provider right away if you develop mouth pain, swelling, redness, ulcers, or sores during treatment with DATROWAY.
- Your healthcare provider will prescribe a steroid-containing mouthwash to use 4 times a day and as needed during treatment with DATROWAY.
- You should hold ice chips or ice water in your mouth during your DATROWAY infusions.
-
Harm to your unborn baby. Tell your healthcare provider right away if you become pregnant or think you might be pregnant during treatment with DATROWAY.
- If you are able to become pregnant, your healthcare provider should do a pregnancy test before you start treatment with DATROWAY.
- Females who are able to become pregnant should use effective birth control (contraception) during treatment with DATROWAY and for 7 months after the last dose.
- Males who have female partners that are able to become pregnant should use effective birth control (contraception) during treatment with DATROWAY and for 4 months after the last dose.
What is DATROWAY?
DATROWAY is a prescription medicine used to treat adults who have:- non-small cell lung cancer (NSCLC) that has certain mutations in a gene called epidermal growth factor receptor (EGFR):
- that has spread to areas outside of the lung (locally advanced) or has spread to other parts of the body (metastatic), and
- who have received prior EGFR-directed medicine and platinum-based chemotherapy.
- hormone receptor (HR)-positive and human epidermal growth factor receptor 2 (HER2)-negative breast cancer:
- that cannot be removed by surgery (unresectable) or has spread to other parts of the body (metastatic), and
- who have received prior endocrine-based therapy and chemotherapy treatment for unresectable or metastatic disease.
Before receiving DATROWAY, tell your healthcare provider about all of your medical conditions, including if you: - have lung or breathing problems.
- have eye problems.
- use contact lenses.
- are breastfeeding or plan to breastfeed. It is not known if DATROWAY passes into your breast milk. Do not breastfeed during treatment with DATROWAY and for 1 month after the last dose.
How will I receive DATROWAY? - You will receive DATROWAY into your vein through an intravenous (IV) line by your healthcare provider.
- DATROWAY is usually given 1 time every three weeks (21-day treatment cycle).
- You will receive your first infusion over 90 minutes. If you do not have problems with your first infusion, you may receive your next infusions over 30 minutes.
- You will be monitored for side effects for at least 1 hour after your first 2 infusions. If you do not have problems after your second infusion, you will be monitored for at least 30 minutes after each following infusion.
- Your healthcare provider will decide how many treatments you need.
- Your healthcare provider will give you medicines before your infusion to help prevent nausea, vomiting, and infusion-related reactions.
- Your healthcare provider may slow down or temporarily stop your infusion of DATROWAY if you have an infusion-related reaction, or permanently stop DATROWAY if you have severe infusion reactions.
- If you miss a planned dose of DATROWAY, call your healthcare provider right away to schedule an appointment. Do not wait until the next planned treatment cycle.
What are the possible side effects of DATROWAY?
DATROWAY can cause serious side effects, including: The most common side effects of DATROWAY when used in adults with EGFR-mutated non-small cell lung cancer include:- nausea
- hair loss
- tiredness
- decreased red blood cell counts
- decreased white blood cell counts
- constipation
- increased blood levels of calcium
- increased blood levels of liver enzymes
- increased levels of enzyme called lactate dehydrogenase in the blood
- muscle and joint pain
- rash
- decreased appetite
The most common side effects of DATROWAY when used in adults with HR-positive HER2-negative breast cancer include: - nausea
- tiredness
- decreased white blood cell counts
- decreased blood levels of calcium
- hair loss
- decreased red blood cell counts
- constipation
- dry eye
- vomiting
- increased blood levels of liver enzymes
- an eye problem called keratitis. See "What is the most important information I should know about DATROWAY?"
- increased blood levels of alkaline phosphatase
DATROWAY may cause fertility problems in males and females, which may affect your ability to have children. Talk to your healthcare provider if you have concerns about fertility.
These are not all of the possible side effects of DATROWAY.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.General information about the safe and effective use of DATROWAY.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. You can ask your pharmacist or healthcare provider for information about DATROWAY that is written for health professionals.What are the ingredients in DATROWAY?
Active ingredient: datopotamab deruxtecan-dlnk
Inactive ingredients: L-histidine, L-histidine hydrochloride monohydrate, polysorbate 80, and sucrose
Manufactured by: Daiichi Sankyo, Inc., Basking Ridge, NJ 07920
U.S. License No. 2128
Marketed by: Daiichi Sankyo, Inc., Basking Ridge, NJ 07920 and AstraZeneca Pharmaceuticals LP, Wilmington, DE 19850
DATROWAY® is a registered trademark of Daiichi Sankyo Company, Ltd.
© 2025 Daiichi Sankyo Co., Ltd.
USMG-DAT-C7-0625-r002
For more information, call 1-877-437-7763 or go to https://www.DATROWAY.com. -
Lung problems that may be severe, life-threatening, or that may lead to death. If you develop lung problems your healthcare provider may treat you with corticosteroid medicines. Tell your healthcare provider right away if you get any of the following signs and symptoms:
-
PRINCIPAL DISPLAY PANEL - 100 mg Vial Carton
NDC: 65597-801-01
Rx onlyDATROWAY®
(datopotamab deruxtecan-dlnk)
For Injection100 mg per vial
For Intravenous Infusion Only
Reconstitute and dilute prior to administration.
Single-dose vial. Discard unused portion.
Dispense the enclosed Medication Guide to
each patient.Hazardous Drug
KEEP REFRIGERATED
1 vialDaiichi-Sankyo
AstraZeneca
-
INGREDIENTS AND APPEARANCE
DATROWAY
datopotamab deruxtecan injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65597-801 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DATOPOTAMAB DERUXTECAN (UNII: GD2OWY1DTK) (DATOPOTAMAB DERUXTECAN - UNII:GD2OWY1DTK) DATOPOTAMAB DERUXTECAN 100 mg in 5 mL Inactive Ingredients Ingredient Name Strength HISTIDINE (UNII: 4QD397987E) HISTIDINE HYDROCHLORIDE MONOHYDRATE (UNII: X573657P6P) SUCROSE (UNII: C151H8M554) POLYSORBATE 80 (UNII: 6OZP39ZG8H) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65597-801-01 1 in 1 CARTON 01/17/2025 1 5 mL in 1 VIAL, SINGLE-DOSE; Type 6: Drug/Biologic Combination Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA761394 01/17/2025 Labeler - Daiichi Sankyo Inc. (068605067)
Trademark Results [DATROWAY]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 DATROWAY 79366371 not registered Live/Pending |
DAIICHI SANKYO COMPANY, LIMITED 2023-01-25 |
 DATROWAY 79339642 not registered Live/Pending |
DAIICHI SANKYO COMPANY, LIMITED 2022-03-04 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.