ACETAMINOPHEN AND CODEINE PHOSPHATE tablet
ACETAMINOPHEN AND CODEINE PHOSPHATE by
Drug Labeling and Warnings
ACETAMINOPHEN AND CODEINE PHOSPHATE by is a Prescription medication manufactured, distributed, or labeled by EPM Packaging Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
Hepatotoxicity
Acetaminophen has been associated with cases of acute liver failure, at times resulting in liver
transplant and death. Most of the cases of liver injury are associated with the use of
acetaminophen at doses that exceed 4000 milligrams per day, and often involve more than one
acetaminophen-containing product.
WARNING: Death Related to Ultra-Rapid Metabolis m of Codeine to Morphine
Respiratory depression and death have occurred in children who received codeine following
tonsillectomy and/or adenoidectomy and had evidence of being ultra-rapid metabolizers of
codeine due to a CYP2D6 polymorphism. -
DESCRIPTION
ACETAMINOPHEN AND CODEINE PHOSPHATE TABLETS, USP CIII
Rx onlyAcetaminophen and codeine are supplied in tablet form for oral administration.
Acetaminophen, USP, 4'-hydroxyacetanilide, a slightly bitter, white, odorless, crystalline powder, is a
non-opiate, non-salicylate analgesic and antipyretic. It has the following structural formula:
C H NO M.W. 151.16
Codeine phosphate, USP, 7,8-didehydro-4,5α-epoxy-3-methoxy-17-methylmorphinan-6α-ol phosphate
(1:1) (salt) hemihydrate, a white crystalline powder, is a narcotic analgesic and antitussive. It has the
following structural formula:
8 9 2
C H NO H PO 1/2H O M.W. 406.37
Each tablet contains:
acetaminophen, USP...........................300 mg
codeine phosphate, USP.......................15 mg
(Warning: May be habit forming)
OR
acetaminophen, USP...........................300 mg
codeine phosphate, USP....................... 30 mg
(Warning: May be habit forming)
OR
acetaminophen, USP...........................300 mg
codeine phosphate, USP....................... 60 mg
(Warning: May be habit forming)
In addition, each tablet contains the following inactive ingredients: corn starch, colloidal silicon
dioxide, croscarmellose sodium, magnesium stearate, and microcrystalline cellulose. The 300 mg/60
mg strength tablets also contain crospovidone, povidone, pregelatinized starch, and stearic acid.
CLINICAL PHARMACOLOGY
This product combines the analgesic effects of a centrally acting analgesic, codeine, with a
peripherally acting analgesic, acetaminophen.
Pharmacokinetics
The behavior of the individual components is described below.
Codeine
Codeine is readily absorbed from the gastrointestinal tract. It is rapidly distributed from the
intravascular spaces to the various body tissues, with preferential uptake by parenchymatous organs
such as the liver, spleen and kidney. Codeine crosses the blood-brain barrier, and is found in fetal tissue
and breast milk. The plasma concentration does not correlate with brain concentration or relief of pain;
however, codeine is not bound to plasma proteins and does not accumulate in body tissues.
The plasma half-life is about 2.9 hours. The elimination of codeine is primarily via the kidneys, and
about 90% of an oral dose is excreted by the kidneys within 24 hours of dosing. The urinary secretion
products consist of free and glucuronide conjugated codeine (about 70%), free and conjugated
norcodeine (about 10%), free and conjugated morphine (about 10%), normorphine (4%), and
hydrocodone (1%). The remainder of the dose is excreted in the feces.
18 21 3 3 4 2
At therapeutic doses, the analgesic effect reaches a peak within 2 hours and persists between 4 and 6
hours.
See OVERDOSAGE for toxicity information.
Acetaminophen
Acetaminophen is rapidly absorbed from the gastrointestinal tract and is distributed throughout most
body tissues. The plasma half-life is 1.25 to 3 hours, but may be increased by liver damage and
following overdosage. Elimination of acetaminophen is principally by liver metabolism (conjugation)
and subsequent renal excretion of metabolites. Approximately 85% of an oral dose appears in the urine
within 24 hours of administration, most as the glucuronide conjugate, with small amounts of other
conjugates and unchanged drug.
See OVERDOSAGE for toxicity information.
INDICATIONS AND USAGE
Acetaminophen and codeine phosphate tablets are indicated for the relief of mild to moderately severe
pain. - CONTRAINDICATIONS
-
WARNINGS
In the presence of head injury or other intracranial lesions, the respiratory depressant effects of codeine
and other narcotics may be markedly enhanced, as well as their capacity for elevating cerebrospinal
fluid pressure. Narcotics also produce other CNS depressant effects, such as drowsiness, that may
further obscure the clinical course of the patients with head injuries.
Codeine or other narcotics may obscure signs on which to judge the diagnosis or clinical course of
patients with acute abdominal conditions.
Codeine is habit-forming and potentially abusable. Consequently, the extended use of this product is not
recommended.
Hepatotoxicity
Acetaminophen has been associated with cases of acute liver failure, at times resulting in liver
transplant and death. Most of the cases of liver injury are associated with the use of acetaminophen at
doses that exceed 4000 milligrams per day, and often involve more than one acetaminophen-containing
product. The excessive intake of acetaminophen may be intentional to cause self-harm or unintentional
as patients attempt to obtain more pain relief or unknowingly take other acetaminophen-containing
products.
The risk of acute liver failure is higher in individuals with underlying liver disease and in individuals
who ingest alcohol while taking acetaminophen.
Instruct patients to look for acetaminophen or APAP on package labels and not to use more than one
product that contains acetaminophen. Instruct patients to seek medical attention immediately upon
ingestion of more than 4000 milligrams of acetaminophen per day, even if they feel well.
Serious Skin Reactions
Rarely, acetaminophen may cause serious skin reactions such as acute generalized exanthematous
pustulosis (AGEP), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN), which can
be fatal. Patients should be informed about the signs of serious skin reactions, and use of the drug
should be discontinued at the first appearance of skin rash or any other sign of hypersensitivity.
Death Related to Ultra-Rapid Metabolis m of Codeine to Morphine
Respiratory depression and death have occurred in children who received codeine in the post-operative
period following tonsillectomy and/or adenoidectomy and had evidence of being ultra-rapid
metabolizers of codeine (i.e., multiple copies of the gene for cytochrome P450 isoenzyme 2D6 or high
morphine concentrations). Deaths have also occurred in nursing infants who were exposed to high
levels of morphine in breast milk because their mothers were ultra-rapid metabolizers of codeine [see
PRECAUTIONS, Nurs ing Mothers ].
Some individuals may be ultra-rapid metabolizers because of a specific CYP2D6 genotype (gene
duplications denoted as *1/*1xN or *1/*2xN). The prevalence of this CYP2D6 phenotype varies widely
and has been estimated at 0.5 to 1% in Chinese and Japanese, 0.5 to 1% in Hispanics, 1 to 10% in
Caucasians, 3% in African Americans, and 16 to 28% in North Africans, Ethiopians, and Arabs. Data are
not available for other ethnic groups. These individuals convert codeine into its active metabolite,
morphine, more rapidly and completely than other people. This rapid conversion results in higher than
expected serum morphine levels. Even at labeled dosage regimens, individuals who are ultra-rapid
metabolizers may have life-threatening or fatal respiratory depression or experience signs of overdose
(such as extreme sleepiness, confusion, or shallow breathing) [see OVERDOSAGE].
Children with obstructive sleep apnea who are treated with codeine for post-tonsillectomy and/or
adenoidectomy pain may be particularly sensitive to the respiratory depressant effects of codeine that
has been rapidly metabolized to morphine. Codeine-containing products are contraindicated for postoperative
pain management in all pediatric patients undergoing tonsillectomy and/or adenoidectomy [seeCONTRAINDICATIONS].
When prescribing codeine-containing products, healthcare providers should choose the lowest
effective dose for the shortest period of time and inform patients and caregivers about these risks and
the signs of morphine overdose [see OVERDOSAGE].
Hypers ens itivity/Anaphylaxis
There have been postmarketing reports of hypersensitivity and anaphylaxis associated with use of
acetaminophen. Clinical signs included swelling of the face, mouth, and throat, respiratory distress,
urticaria, rash, pruritus, and vomiting. There were infrequent reports of life-threatening anaphylaxis
requiring emergency medical attention. Instruct patients to discontinue acetaminophen and codeine
phosphate tablets, USP immediately and seek medical care if they experience these symptoms. Do not
prescribe acetaminophen and codeine phosphate tablets, USP for patients with acetaminophen allergy.
Alcohol Information
Chronic heavy alcohol abusers may be at increased risk of liver toxicity from excessive acetaminophen
use, although reports of this event are rare. Reports almost invariably involve cases of severe chronic
alcoholics and the dosages of acetaminophen most often exceed recommended doses and often involve
substantial overdose. Professionals should alert their patients who regularly consume large amounts of
alcohol not to exceed recommended doses of acetaminophen. -
PRECAUTIONS
In the presence of head injury or other intracranial lesions, the respiratory depressant effects of codeine
and other narcotics may be markedly enhanced, as well as their capacity for elevating cerebrospinal
fluid pressure. Narcotics also produce other CNS depressant effects, such as drowsiness, that may
further obscure the clinical course of the patients with head injuries.
Codeine or other narcotics may obscure signs on which to judge the diagnosis or clinical course of
patients with acute abdominal conditions.
Codeine is habit-forming and potentially abusable. Consequently, the extended use of this product is not
recommended.
Hepatotoxicity
Acetaminophen has been associated with cases of acute liver failure, at times resulting in liver
transplant and death. Most of the cases of liver injury are associated with the use of acetaminophen at
doses that exceed 4000 milligrams per day, and often involve more than one acetaminophen-containing
product. The excessive intake of acetaminophen may be intentional to cause self-harm or unintentional
as patients attempt to obtain more pain relief or unknowingly take other acetaminophen-containing
products.
The risk of acute liver failure is higher in individuals with underlying liver disease and in individuals
who ingest alcohol while taking acetaminophen.
Instruct patients to look for acetaminophen or APAP on package labels and not to use more than one
product that contains acetaminophen. Instruct patients to seek medical attention immediately upon
ingestion of more than 4000 milligrams of acetaminophen per day, even if they feel well.
Serious Skin Reactions
Rarely, acetaminophen may cause serious skin reactions such as acute generalized exanthematous
pustulosis (AGEP), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN), which can
be fatal. Patients should be informed about the signs of serious skin reactions, and use of the drug
should be discontinued at the first appearance of skin rash or any other sign of hypersensitivity.
Death Related to Ultra-Rapid Metabolis m of Codeine to Morphine
Respiratory depression and death have occurred in children who received codeine in the post-operative
period following tonsillectomy and/or adenoidectomy and had evidence of being ultra-rapid
metabolizers of codeine (i.e., multiple copies of the gene for cytochrome P450 isoenzyme 2D6 or high
morphine concentrations). Deaths have also occurred in nursing infants who were exposed to high
levels of morphine in breast milk because their mothers were ultra-rapid metabolizers of codeine [see
PRECAUTIONS, Nurs ing Mothers ].
Some individuals may be ultra-rapid metabolizers because of a specific CYP2D6 genotype (gene
duplications denoted as *1/*1xN or *1/*2xN). The prevalence of this CYP2D6 phenotype varies widely
and has been estimated at 0.5 to 1% in Chinese and Japanese, 0.5 to 1% in Hispanics, 1 to 10% in
Caucasians, 3% in African Americans, and 16 to 28% in North Africans, Ethiopians, and Arabs. Data are
not available for other ethnic groups. These individuals convert codeine into its active metabolite,
morphine, more rapidly and completely than other people. This rapid conversion results in higher than
expected serum morphine levels. Even at labeled dosage regimens, individuals who are ultra-rapid
metabolizers may have life-threatening or fatal respiratory depression or experience signs of overdose
(such as extreme sleepiness, confusion, or shallow breathing) [see OVERDOSAGE].
Children with obstructive sleep apnea who are treated with codeine for post-tonsillectomy and/or
adenoidectomy pain may be particularly sensitive to the respiratory depressant effects of codeine that
has been rapidly metabolized to morphine. Codeine-containing products are contraindicated for postoperative
pain management in all pediatric patients undergoing tonsillectomy and/or adenoidectomy [seeCONTRAINDICATIONS].
When prescribing codeine-containing products, healthcare providers should choose the lowest
effective dose for the shortest period of time and inform patients and caregivers about these risks and
the signs of morphine overdose [see OVERDOSAGE].
Hypers ens itivity/Anaphylaxis
There have been postmarketing reports of hypersensitivity and anaphylaxis associated with use of
acetaminophen. Clinical signs included swelling of the face, mouth, and throat, respiratory distress,
urticaria, rash, pruritus, and vomiting. There were infrequent reports of life-threatening anaphylaxis
requiring emergency medical attention. Instruct patients to discontinue acetaminophen and codeine
phosphate tablets, USP immediately and seek medical care if they experience these symptoms. Do not
prescribe acetaminophen and codeine phosphate tablets, USP for patients with acetaminophen allergy.
Alcohol Information
Chronic heavy alcohol abusers may be at increased risk of liver toxicity from excessive acetaminophen
use, although reports of this event are rare. Reports almost invariably involve cases of severe chronic
alcoholics and the dosages of acetaminophen most often exceed recommended doses and often involve
substantial overdose. Professionals should alert their patients who regularly consume large amounts of
alcohol not to exceed recommended doses of acetaminophen. -
ADVERSE REACTIONS
The most frequently reported adverse reactions are drowsiness, lightheadedness, dizziness, sedation,
shortness of breath, nausea and vomiting. These effects seem to be more prominent in ambulatory than in
non-ambulatory patients, and some of these adverse reactions may be alleviated if the patient lies down.
Other adverse reactions include allergic reactions, euphoria, dysphoria, constipation, abdominal pain,
pruritus, rash, thrombocytopenia, agranulocytosis.
At higher doses codeine has most of the disadvantages of morphine including respiratory depression.
DRUG ABUSE AND DEPENDENCE
Controlled Subs tance
Acetaminophen and codeine phosphate tablets are classified as a Schedule III controlled substance.
Abus e and Dependence
Codeine can produce drug dependence of the morphine type and, therefore, has the potential for being
abused. Psychological dependence, physical dependence, and tolerance may develop upon repeated
administration and it should be prescribed and administered with the same degree of caution appropriate
to the use of other oral narcotic medications. -
OVERDOSAGE
Following an acute overdosage, toxicity may result from codeine or acetaminophen.
Signs and Symptoms
Toxicity from codeine poisoning includes the opioid triad of: pinpoint pupils, depression of respiration,
and loss of consciousness. Convulsions may occur.
In acetaminophen overdosage: dose-dependent, potentially fatal hepatic necrosis is the most serious
adverse effect. Renal tubular necrosis, hypoglycemic coma and coagulation defects may also occur.
Early symptoms following a potentially hepatotoxic overdose may include: nausea, vomiting,
diaphoresis and general malaise. Clinical and laboratory evidence of hepatic toxicity may not be
apparent until 48 to 72 hours post-ingestion.
Treatment
A single or multiple drug overdose with acetaminophen and codeine is a potentially lethal polydrug
overdose, and consultation with a regional poison control center is recommended. Immediate treatment
includes support of cardiorespiratory function and measures to reduce drug absorption.
Oxygen, intravenous fluids, vasopressors, and other supportive measures should be employed as
indicated. Assisted or controlled ventilation should also be considered. For respiratory depression due
to overdosage or unusual sensitivity to codeine, parenteral naloxone is a specific and effective
antagonist.
Gastric decontamination with activated charcoal should be administered just prior to N-acetylcysteine
(NAC) to decrease systemic absorption if acetaminophen ingestion is known or suspected to have
occurred within a few hours of presentation. Serum acetaminophen levels should be obtained
immediately if the patient presents 4 hours or more after ingestion to assess potential risk of
hepatotoxicity; acetaminophen levels drawn less than 4 hours post-ingestion may be misleading. To
obtain the best possible outcome, NAC should be administered as soon as possible where impending or
evolving liver injury is suspected. Intravenous NAC may be administered when circumstances preclude
oral administration.
Vigorous supportive therapy is required in severe intoxication. Procedures to limit the continuing
absorption of the drug must be readily performed since the hepatic injury is dose dependent and occurs
early in the course of intoxication. -
DOSAGE & ADMINISTRATION
Dosage should be adjusted according to severity of pain and response of the patient.
The usual adult dosage is:
Single Doses (range) Maximum 24 Hour Dose
Codeine Phosphate 15 mg to 60 mg 360 mg
Acetaminophen 300 mg to 1000 mg 4000 mg
The usual dose of codeine phosphate in children is 0.5 mg/kg.
Doses may be repeated up to every 4 hours.
The prescriber must determine the number of tablets per dose, and the maximum number of tablets per
24 hours based upon the above dosage guidance. This information should be conveyed in the
prescription.
It should be kept in mind, however, that tolerance to codeine can develop with continued use and that the
incidence of untoward effects is dose related. Adult doses of codeine higher than 60 mg fail to give
commensurate relief of pain but merely prolong analgesia and are associated with an appreciably
increased incidence of undesirable side effects. Equivalently high doses in children would have similar
effects. -
HOW SUPPLIED
HOW SUPPLIED
Acetaminophen and codeine phosphate tablets USP (white, round, unscored):
Acetaminophen and codeine phosphate tablets USP (white, round, unscored):
List No. 0050, acetaminophen 300 mg and codeine phosphate 15 mg, debossed “2” on one side and
“TV”-“50” on the other side of tablet is available in bottles of 100 (NDC: 0093-0050-01) tablets.
List No. 0150, acetaminophen 300 mg and codeine phosphate 30 mg, debossed “3” on one side and
“TV”-“150” on the other side of tablet is available in bottles of 100 (NDC: 0093-0150-01) and 1000
(NDC: 0093-0150-10) tablets.
List No. 0350, acetaminophen 300 mg and codeine phosphate 60 mg, debossed “4” on one side and
“93”-“350” on the other side of tablet is available in bottles of 100 (NDC: 0093-0350-01), 500 (NDC
0093-0350-05), and 1000 (NDC: 0093-0350-10) tablets.
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature]. Protect from moisture.
PROTECT FROM LIGHT
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as
required).
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
Distributed By:
TEVA PHARMACEUTICALS USA, INC.
North Wales, PA 19454
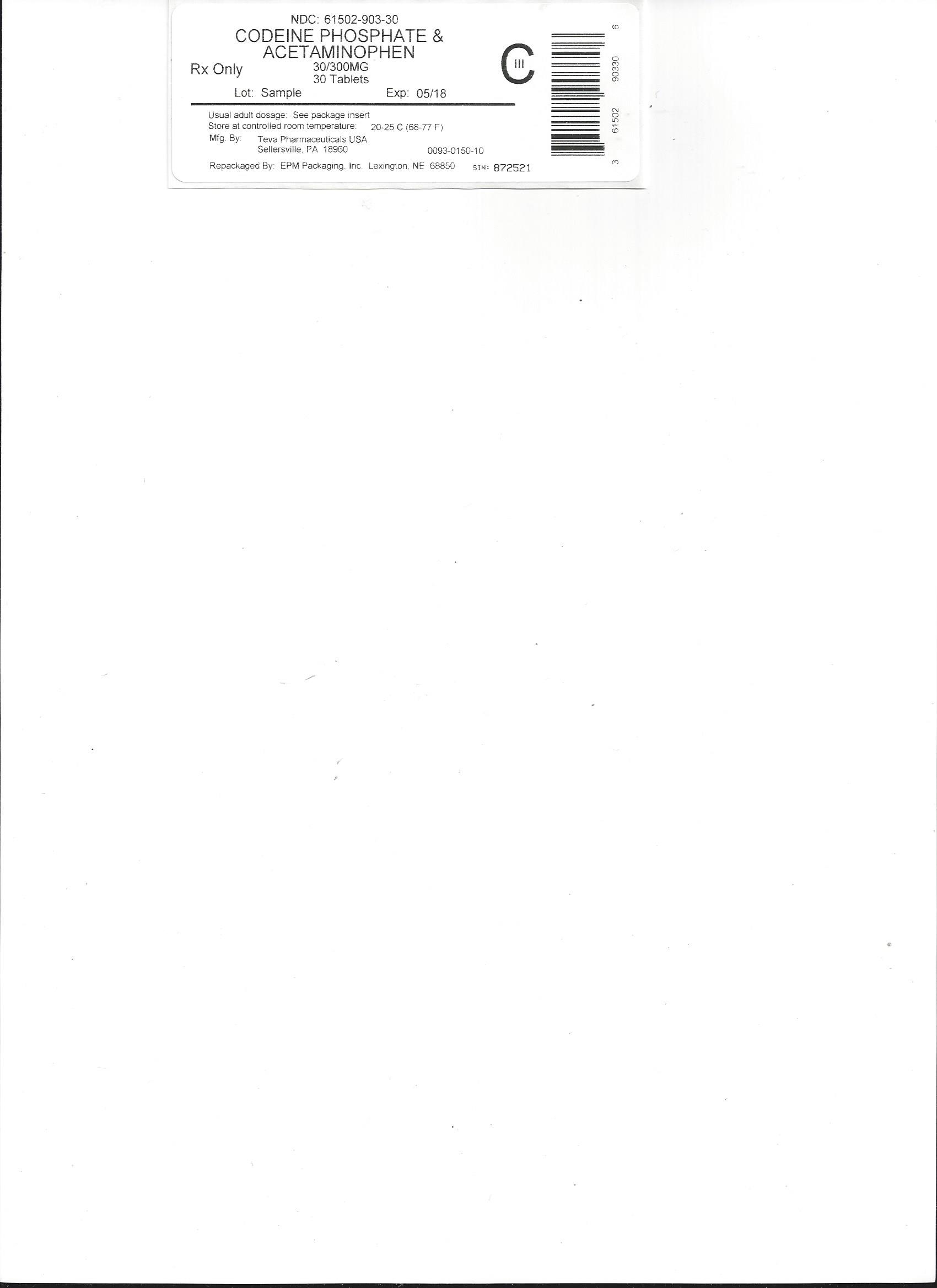
Rev. AI 8/2015 - PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
ACETAMINOPHEN AND CODEINE PHOSPHATE
acetaminophen and codeine phosphate tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 61502-903(NDC:0093-0150) Route of Administration ORAL DEA Schedule CIII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ACETAMINOPHEN (UNII: 362O9ITL9D) (ACETAMINOPHEN - UNII:362O9ITL9D) ACETAMINOPHEN 300 mg CODEINE PHOSPHATE (UNII: GSL05Y1MN6) (CODEINE ANHYDROUS - UNII:UX6OWY2V7J) CODEINE PHOSPHATE 30 mg Product Characteristics Color white Score no score Shape ROUND Size 10mm Flavor Imprint Code 3;TV;150 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 61502-903-97 500 in 1 BOTTLE; Type 0: Not a Combination Product 01/27/2016 2 NDC: 61502-903-96 100 in 1 BOTTLE; Type 0: Not a Combination Product 01/27/2016 3 NDC: 61502-903-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/27/2016 4 NDC: 61502-903-20 20 in 1 BOTTLE; Type 0: Not a Combination Product 01/27/2016 5 NDC: 61502-903-15 15 in 1 BOTTLE; Type 0: Not a Combination Product 01/27/2016 6 NDC: 61502-903-10 10 in 1 BOTTLE; Type 0: Not a Combination Product 01/27/2016 7 NDC: 61502-903-06 6 in 1 BOTTLE; Type 0: Not a Combination Product 01/27/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA088627 01/27/2016 Labeler - EPM Packaging Inc (079124340) Registrant - EPM Packaging Inc (079124340) Establishment Name Address ID/FEI Business Operations EPM Packaging Inc 079124340 repack(61502-903)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.