DIAZEPAM injection, solution
Diazepam by
Drug Labeling and Warnings
Diazepam by is a Prescription medication manufactured, distributed, or labeled by Dr. Reddy's Laboratories Inc, Dr. Reddy’s Laboratories Limited FTO-9. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
BOXED WARNING
(What is this?)
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; ABUSE, MISUSE, AND ADDICTION; and DEPENDENCE AND WITHDRAWAL REACTIONS
- Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death (see WARNINGS).
- Reserve concomitant prescribing of these drugs in patients for whom alternative treatment options are inadequate.
- Limit dosages and durations to the minimum required.
- Follow patients for signs and symptoms of respiratory depression and sedation (see WARNINGS and PRECAUTIONS).
- The use of benzodiazepines, including diazepam, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes. Before prescribing diazepam and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction (see WARNINGS).
- The continued use of benzodiazepines may lead to clinically significant physical dependence. The risks of dependence and withdrawal increase with longer treatment duration and higher daily dose. Although diazepam is indicated only for intermittent use (see INDICATIONS AND USAGE and DOSAGE AND ADMINISTRATION), if used more frequently than recommended, abrupt discontinuation or rapid dosage reduction of diazepam may precipitate acute withdrawal reactions, which can be life-threatening. For patients using diazepam more frequently than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue diazepam (see WARNINGS).
-
DESCRIPTION
Diazepam is a benzodiazepine derivative. Chemically, diazepam is 7-chloro-1,3-dihydro-1-methyl-5- phenyl-2H-1,4-benzodiazepin-2-one. It is a colorless crystalline compound, insoluble in water, with a molecular weight of 284.74 and with the following molecular structure:
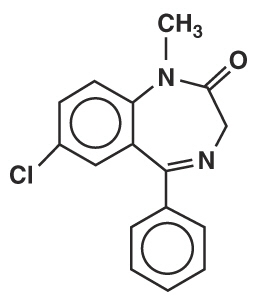 M.W. 284.74
M.W. 284.74
Diazepam Injection, USP is a sterile solution and each mL contains 5 mg diazepam compounded with 40% propylene glycol, 10% alcohol, 5% sodium benzoate and benzoic acid as buffers, and 1.5% benzyl alcohol as preservative. -
CLINICAL PHARMACOLOGY
In animals, diazepam appears to act on parts of the limbic system, the thalamus and hypothalamus, and induces calming effects. Diazepam, unlike chlorpromazine and reserpine, has no demonstrable peripheral autonomic blocking action, nor does it produce extrapyramidal side effects; however, animals treated with diazepam do have a transient ataxia at higher doses. Diazepam was found to have transient cardiovascular depressor effects in dogs. Long-term experiments in rats revealed no disturbances of endocrine function. Injections into animals have produced localized irritation of tissue surrounding injection sites and some thickening of veins after intravenous use.
Population PK analysis in 87 pediatric patients 0.4 to 17.8 years of age with status epilepticus showed that, after initial dosing, the median plasma half-life was 0.5 hours and the median terminal elimination plasma half-life was 18 to 25 hours. -
INDICATIONS AND USAGE
Diazepam is indicated for the management of anxiety disorders or for the short-term relief of the symptoms of anxiety. Anxiety or tension associated with the stress of everyday life usually does not require treatment with an anxiolytic.
In acute alcohol withdrawal, diazepam may be useful in the symptomatic relief of acute agitation, tremor, impending or acute delirium tremens and hallucinosis.
As an adjunct prior to endoscopic procedures if apprehension, anxiety or acute stress reactions are present, and to diminish the patient's recall of the procedures (See WARNINGS).
Diazepam is a useful adjunct for the relief of skeletal muscle spasm due to reflex spasm to local pathology (such as inflammation of the muscles or joints, or secondary to trauma); spasticity caused by upper motor neuron disorders (such as cerebral palsy and paraplegia); athetosis; stiff-man syndrome; and tetanus.
Diazepam injection is a useful adjunct in status epilepticus.
Diazepam is a useful premedication (the intramuscular route is preferred) for relief of anxiety and tension in patients who are to undergo surgical procedures. Intravenously, prior to cardioversion for the relief of anxiety and tension and to diminish the patient's recall of the procedure.
- CONTRAINDICATIONS
-
WARNINGS
Risks from Concomitant Use with Opioids
Concomitant use of benzodiazepines, including diazepam, and opioids may result in profound sedation, respiratory depression, coma, and death. Because of these risks, reserve concomitant prescribing of benzodiazepines and opioids in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe diazepam concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. Advise both patients and caregivers about the risks of respiratory depression and sedation when diazepam is used with opioids (see PRECAUTIONS; Drug Interactions).
Abuse, Misuse, and Addiction
The use of benzodiazepines, including diazepam, exposes users to the risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death (see DRUG ABUSE AND DEPENDENCE: Abuse).
Before prescribing diazepam and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction. Use of diazepam, particularly in patients at elevated risk, necessitates counseling about the risks and proper use of diazepam along with monitoring for signs and symptoms of abuse, misuse, and addiction. Do not exceed the recommended dosing frequency; avoid or minimize concomitant use of CNS depressants and other substances associated with abuse, misuse, and addiction (e.g., opioid analgesics, stimulants); and advise patients on the proper disposal of unused drug. If a substance use disorder is suspected, evaluate the patient and institute (or refer them for) early treatment, as appropriate.
Dependence and Withdrawal Reactions After Use of Diazepam More Frequently Than Recommended
For patients using diazepam more frequently than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue diazepam (a patient-specific plan should be used to taper the dose).
Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages, and those who have had longer durations of use.Acute Withdrawal Reactions
The continued use of benzodiazepines, including diazepam may lead to clinically significant physical dependence. Although diazepam is indicated only for intermittent use (see INDICATIONS AND USAGE and DOSAGE AND ADMINISTRATION), if used more frequently than recommended, abrupt discontinuation or rapid dosage reduction of diazepam, or administration of flumazenil (a benzodiazepine antagonist) may precipitate acute withdrawal reactions, which can be life-threatening (e.g., seizures) (see DRUG ABUSE AND DEPENDENCE, Dependence).
Protracted Withdrawal Syndrome
In some cases, benzodiazepine users have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months (see DRUG ABUSE AND DEPENDENCE: Dependence ).
When used intravenously, the following procedures should be undertaken to reduce the possibility of venous thrombosis, phlebitis, local irritation, swelling, and, rarely, vascular impairment; the solution should be injected slowly, taking at least one minute for each 5 mg (1 mL) given except for treatment of status epilepticus in children (see DOSAGE AND ADMINISTRATION); do not use small veins, such as those on the dorsum of the hand or wrist; extreme care should be taken to avoid intra-arterial administration or extravasation.
Do not mix or dilute diazepam injection with other solutions or drugs in syringe or infusion container. If it is not feasible to administer diazepam directly intravenous, it may be injected slowly through the infusion tubing as close as possible to the vein insertion.
Extreme care must be used in administering diazepam injection, particularly by the intravenous route, to the elderly, to very ill patients, and to those with limited pulmonary reserve because of the possibility that apnea and/or cardiac arrest may occur.Concomitant use of barbiturates, alcohol or other central nervous system depressants increases depression with increased risk of apnea. Resuscitative equipment including that necessary to support respiration should be readily available.
When diazepam is used with a narcotic analgesic, the dosage of the narcotic should be reduced by at least one-third and administered in small increments. In some cases the use of a narcotic may not be necessary.
Diazepam injection should not be administered to patients in shock, coma, or in acute alcoholic intoxication with depression of vital signs. As is true of most CNS-acting drugs, patients receiving diazepam should be cautioned against engaging in hazardous occupations requiring complete mental alertness, such as operating machinery or driving a motor vehicle.
Tonic status epilepticus has been precipitated in patients treated with intravenous diazepam for petit mal status or petit mal variant status.Neonatal Sedation and Withdrawal Syndrome
Use of diazepam injection late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in the neonate (see PRECAUTIONS: Pregnancy). Monitor neonates exposed to diazepam injection during pregnancy or labor for signs of sedation and monitor neonates exposed to diazepam injection during pregnancy for signs of withdrawal; manage these neonates accordingly.
Pediatric Use:
Efficacy and safety of parenteral diazepam has not been established in the neonate (30 days or less of age).
Prolonged central nervous system depression has been observed in neonates, apparently due to inability to biotransform diazepam into inactive metabolites.
In pediatric use for the treatment of status epilepticus, in order to obtain maximal clinical effect with the minimum amount of drug and thus to reduce the risk of hazardous side effects, such as apnea or prolonged periods of somnolence, it is recommended that the drug be given as a slow intravenous push over 1 minute (see DOSAGE AND ADMINISTRATION). The safety and tolerability of the recommended dosage regimen is supported by a randomized, double-blind study that included 162 pediatric patients ages 3 months to 17 years who received intravenous diazepam for the treatment of status epilepticus. In this study, 16% of pediatric patients who received diazepam experienced severe or life-threatening respiratory depression.Benzyl alcohol has been reported to be associated with a fatal gasping syndrome in premature infants.
-
PRECAUTIONS
General
Although seizures may be brought under control promptly, a significant proportion of patients experience a return to seizure activity, presumably due to the short-lived effect of diazepam after intravenous administration. The physician should be prepared to readminister the drug. However, diazepam is not recommended for maintenance, and once seizures are brought under control, consideration should be given to the administration of agents useful in longer term control of seizures.
The usual precautions in treating patients with impaired hepatic function should be observed. Metabolites of diazepam are excreted by the kidney; to avoid their excess accumulation, caution should be exercised in the administration to patients with compromised kidney function.
Since an increase in cough reflex and laryngospasm may occur with peroral endoscopic procedures, the use of a topical anesthetic agent, and the availability of necessary countermeasures are recommended.
Propylene glycol toxicity has been reported in patients treated with diazepam injection at doses significantly greater than recommended. In these cases, diazepam was being used to treat alcohol withdrawal symptoms at doses greater than 900 mg/day. Propylene glycol toxicity is associated with an anion gap metabolic acidosis, serum hyperosmolality, and increased lactate. Propylene glycol toxicity can cause acute tubular necrosis (which can progress to multi-organ failure), mental status changes, hypotension, seizures, and cardiac arrhythmias. Patients at high risk for propylene glycol toxicity include those with renal dysfunction, hepatic dysfunction, impaired alcohol dehydrogenase enzymes, or other comorbidities (such as a history of alcoholism).
Until additional information is available, diazepam injection is not recommended for obstetrical use. Lower doses (usually 2 mg to 5 mg) should be used for elderly and debilitated patients.
Risks from Concomitant Use with Opioids
Advise both patients and caregivers about the risks of potentially fatal respiratory depression and sedation when diazepam is used with opioids and not to use such drugs concomitantly unless supervised by a health care provider. Advise patients not to drive or operate heavy machinery until the effects of concomitant use with the opioid have been determined (see WARNINGS: Risks from Concomitant Use with Opioids and PRECAUTIONS: Drug Interactions).
Abuse, Misuse, and Addiction
Inform patients that the use of diazepam more frequently than recommended, even at recommended dosages, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose and death, especially when used in combination with other medications (e.g., opioid analgesics), alcohol, and/or illicit substances. Inform patients about the signs and symptoms of benzodiazepine abuse, misuse, and addiction; to seek medical help if they develop these signs and/or symptoms; and on the proper disposal of unused drug (see WARNINGS and DRUG ABUSE AND DEPENDENCE).
Withdrawal Reactions
Inform patients that use of diazepam more frequently than recommended may lead to clinically significant physical dependence and that abrupt discontinuation or rapid dosage reduction of diazepam may precipitate acute withdrawal reactions, which can be life-threatening. Inform patients that in some cases, patients taking benzodiazepines have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months (see WARNINGS and DRUG ABUSE AND DEPENDENCE).
Pregnancy
Advise pregnant females that use of diazepam late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in newborns (see WARNINGS: Neonatal Sedation and Withdrawal Syndrome1and PRECAUTIONS: Pregnancy). Instruct patients to inform their healthcare provider if they are pregnant.
Nursing
Advise patients that breastfeeding is not recommended during treatment with diazepam (see PRECAUTIONS: Nursing Mothers).
- 1
Drug Interactions
The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at GABAA sites and opioids interact primarily at mµ receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid-related respiratory depression exists.
Limit dosage and duration of concomitant use of benzodiazepines and opioids, and monitor patients closely for respiratory depression and sedation.
If diazepam is to be combined with other psychotropic agents or anticonvulsant drugs, careful consideration should be given to the pharmacology of the agents to be employed, particularly with known compounds which may potentiate the action of diazepam, such as phenothiazines, narcotics, barbiturates, MAO inhibitors, and other antidepressants. In highly anxious patients with evidence of accompanying depression, particularly those who may have suicidal tendencies, protective measures may be necessary.
Diazepam injection has produced hypotension or muscular weakness in some patients particularly when used with narcotics, barbiturates, or alcohol.
The clearance of diazepam and certain other benzodiazepines can be delayed in association with cimetidine administration. The clinical significance of this is unclear.
Pregnancy
Risk Summary
Neonates born to mothers using benzodiazepines late in pregnancy have been reported to experience symptoms of sedation and/or neonatal withdrawal (see WARNINGS: Neonatal Sedation and Withdrawal Syndrome, and PRECAUTIONS: Clinical Considerations). Available data from published observational studies of pregnant women exposed to benzodiazepines do not report a clear association with benzodiazepines and major birth defects (see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated risk of major birth defects and of miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Benzodiazepines cross the placenta and may produce respiratory depression, hypotonia, and sedation in neonates. Monitor neonates exposed to diazepam injection during pregnancy or labor for signs of sedation, respiratory depression, hypotonia, and feeding problems monitor neonates exposed to diazepam injection during pregnancy for signs of withdrawal. Manage these neonates accordingly (see WARNINGS: Neonatal Sedation and Withdrawal Syndrome).
Data
Human Data
Published data from observational studies on the use of benzodiazepines during pregnancy do not report a clear association with benzodiazepines and major birth defects.
Although early studies reported an increased risk of congenital malformations with diazepam and chlordiazepoxide, there was no consistent pattern noted. In addition, the majority of more recent case-control and cohort studies of benzodiazepine use during pregnancy, which were adjusted for confounding exposures to alcohol, tobacco and other medications, have not confirmed these findings.
Animal Data
Diazepam has been shown to produce increased incidences of fetal malformations in mice and hamsters when given orally at single doses of 100 mg/kg or greater (approximately 20 times the maximum recommended adult dose [0.4 mg/kg/day] or greater on a mg/m2 basis). Cleft palate and exencephaly are the most common and consistently reported malformations produced in these species by administration of high, maternally-toxic doses of diazepam during organogenesis. In published animal studies, administration of benzodiazepines or other drugs that enhance GABAergic inhibition to neonatal rats has been reported to result in widespread apoptotic neurodegeneration in the developing brain at plasma concentrations relevant for seizure control in humans. The window of vulnerability to these changes in rats (postnatal days 0 to 14) includes a period of brain development that takes place during the third trimester of pregnancy in humans.
Nursing Mothers:
Risk Summary
Diazepam is present in breastmilk. There are reports of sedation, poor feeding and poor weight gain in infants exposed to benzodiazepines through breast milk. There are no data on the effects of diazepam on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for diazepam injection and any potential adverse effects on the breastfed infant from diazepam injection or from the underlying maternal condition.
Clinical Considerations
Infants exposed to diazepam injection through breast milk should be monitored for sedation, poor feeding and poor weight gain.
-
ADVERSE REACTIONS
Side effects most commonly reported were drowsiness, fatigue, and ataxia; venous thrombosis and phlebitis at the site of injection. Other adverse reactions less frequently reported include:
CNS: Confusion, depression [including respiratory depressing (seeWARNINGS; Pediatric Use)], dysarthria, headache, hypoactivity, slurred speech, syncope, tremor, vertigo.
G.I.: Constipation, nausea.
G.U.: Incontinence, changes in libido, urinary retention.
Cardiovascular: Bradycardia, cardiovascular collapse, hypotension.
EENT: Blurred vision, diplopia, nystagmus.
Skin: Urticaria, skin rash.Other: Hiccups, changes in salivation, neutropenia, jaundice. Paradoxical reactions such as acute hyperexcited states, anxiety, hallucinations, increased muscle spasticity, insomnia, rage, sleep disturbances and stimulation have been reported; should these occur, use of the drug should be discontinued. Minor changes in EEG patterns, usually low-voltage fast activity, have been observed in patients during and after diazepam therapy and are of no known significance.
In peroral endoscopic procedures, coughing, depressed respiration, dyspnea, hyperventilation, laryngospasm, and pain in throat or chest have been reported.
Because of isolated reports of neutropenia and jaundice, periodic blood counts and liver function tests are advisable during long-term therapy. -
DRUG ABUSE AND DEPENDENCE
Abuse
Diazepam is a benzodiazepine and a CNS depressant with a potential for abuse and addiction. Abuse is the intentional, nontherapeutic use of a drug, even once, for its desirable psychological or physiological effects. Misuse is the intentional use, for therapeutic purposes, of a drug by an individual in a way other than prescribed by a health care provider or for whom it was not prescribed. Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that may include a strong desire to take the drug, difficulties in controlling drug use (e.g., continuing drug use despite harmful consequences, giving a higher priority to drug use than other activities and obligations), and possible tolerance or physical dependence. Even taking benzodiazepines as prescribed may put patients at risk for abuse and misuse of their medication. Abuse and misuse of benzodiazepines may lead to addiction.
Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death. Benzodiazepines are often sought by individuals who abuse drugs and other substances, and by individuals with addictive disorders (see WARNINGS: Abuse, Misuse, and Addiction).
The following adverse reactions have occurred with benzodiazepine abuse and/or misuse: abdominal pain, amnesia, anorexia, anxiety, aggression, ataxia, blurred vision, confusion, depression, disinhibition, disorientation, dizziness, euphoria, impaired concentration and memory, indigestion, irritability, muscle pain, slurred speech, tremors, and vertigo.
The following severe adverse reactions have occurred with benzodiazepine abuse and/or misuse: delirium, paranoia, suicidal ideation and behavior, seizures, coma, breathing difficulty, and death. Death is more often associated with polysubstance use (especially benzodiazepines with other CNS depressants such as opioids and alcohol).
Dependence
Physical Dependence After Use of Diazepam More Frequently than Recommended
Diazepam may produce physical dependence if used more frequently than recommended. Physical dependence is a state that develops as a result of physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug.Although diazepam is indicated only for intermittent use (see INDICATIONS AND USAGE and DOSAGE AND ADMINISTRATION), if used more frequently than recommended, abrupt discontinuation or rapid dosage reduction or administration of flumazenil, a benzodiazepine antagonist, may precipitate acute withdrawal reactions, including seizures, which can be life-threatening. Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages (i.e., higher and/or more frequent doses) and those who have had longer durations of use (seeWARNINGS: Dependence and Withdrawal Reactions ).
For patients using diazepam more frequently than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue diazepam (see WARNINGS: Dependence and Withdrawal Reactions ).
Acute Withdrawal Signs and Symptoms
Acute withdrawal signs and symptoms associated with benzodiazepines have included abnormal involuntary movements, anxiety, blurred vision, depersonalization, depression, derealization, dizziness, fatigue, gastrointestinal adverse reactions (e.g., nausea, vomiting, diarrhea, weight loss, decreased appetite), headache, hyperacusis, hypertension, irritability, insomnia, memory impairment, muscle pain and stiffness, panic attacks, photophobia, restlessness, tachycardia, and tremor. More severe acute withdrawal signs and symptoms, including life-threatening reactions, have included catatonia, convulsions, delirium tremens, depression, hallucinations, mania, psychosis, seizures, and suicidality.
Protracted Withdrawal Syndrome
Protracted withdrawal syndrome associated with benzodiazepines is characterized by anxiety, cognitive impairment, depression, insomnia, formication, motor symptoms (e.g., weakness, tremor, muscle twitches), paresthesia, and tinnitus that persists beyond 4 to 6 weeks after initial benzodiazepine withdrawal. Protracted withdrawal symptoms may last weeks to more than 12 months. As a result, there may be difficulty in differentiating withdrawal symptoms from potential re-emergence or continuation of symptoms for which the benzodiazepine was being used.
Tolerance
Tolerance to diazepam may develop after use more frequently than recommended. Tolerance is a physiological state characterized by a reduced response to a drug after repeated administration (i.e., a higher dose of a drug is required to produce the same effect that was once obtained at a lower dose).
Tolerance to therapeutic effect of benzodiazepines may develop; however, little tolerance develops to the amnestic reactions and other cognitive impairments caused by benzodiazepines.
-
OVERDOSAGE
Overdosage of benzodiazepines is characterized by central nervous system depression ranging from drowsiness to coma. In mild to moderate cases, symptoms can include drowsiness, confusion, dysarthria, lethargy, hypnotic state, diminished reflexes, ataxia, and hypotonia. Rarely, paradoxical or disinhibitory reactions (including agitation, irritability, impulsivity, violent behavior, confusion, restlessness, excitement, and talkativeness) may occur. In severe overdosage cases, patients may develop respiratory depression and coma. Overdosage of benzodiazepines in combination with other CNS depressants (including alcohol and opioids) may be fatal (see Warnings: Abuse, Misuse, and Addiction). Markedly abnormal (lowered or elevated) blood pressure, heart rate, or respiratory rate raise the concern that additional drugs and/or alcohol are involved in the overdosage.
In managing benzodiazepine overdosage, employ general supportive measures, including intravenous fluids and airway maintenance. Flumazenil, a specific benzodiazepine receptor antagonist indicated for the complete or partial reversal of the sedative effects of benzodiazepines in the management of benzodiazepine overdosage, can lead to withdrawal and adverse reactions, including seizures, particularly in the context of mixed overdosage with drugs that increase seizure risk (e.g., tricyclic and tetracyclic antidepressants) and in patients with long- term benzodiazepine use and physical dependency. The risk of withdrawal seizures with flumazenil use may be increased in patients with epilepsy. Flumazenil is contraindicated in patients who have received a benzodiazepine for control of a potentially life-threatening condition (e.g., status epilepticus). If the decision is made to use flumazenil, it should be used as an adjunct to, not as a substitute for, supportive management of benzodiazepine overdosage. See the flumazenil injection Prescribing Information.
Consider contacting a poison center (1-800-222-1222), poisoncontrol.org, or a medical toxicologist for additional overdosage management recommendations.
-
DOSAGE AND ADMINISTRATION
Dosage should be individualized for maximum beneficial effect. The usual recommended dose in older children and adults ranges from 2 mg to 20 mg intramuscular or intravenous, depending on the indication and its severity. In some conditions, e.g., tetanus, larger doses may be required. (See dosage for specific indications.) In acute conditions the injection may be repeated within one hour although an interval of 3 to 4 hours is usually satisfactory. Lower doses (usually 2 mg to 5 mg) and slow increase in dosage should be used for elderly or debilitated patients and when other sedative drugs are administered.(See WARNINGS and ADVERSE REACTIONS).
For dosage in infants above the age of 30 days and children, see the specific indications below. When intravenous use is indicated, facilities for respiratory assistance should be readily available.
Intramuscular: Diazepam injection should be injected deeply into the muscle.
Intravenous Use: For the treatment of status epilepticus in children, the solution should be injected slowly, taking one minute for administration (See WARNINGS, particularly for use in children). For other indications, the solution should be injected slowly taking at least one minute for each 5 mg (1 mL) given. Do not use small veins, such as those on the dorsum of the hand or wrist. Extreme care should be taken to avoid intra-arterial administration or extravasation.Do not mix or dilute diazepam with other solutions or drugs in syringe or infusion container. If it is not feasible to administer diazepam directly intravenous, it may be injected slowly through the infusion tubing as close as possible to the vein insertion.
INDICATION USUAL ADULT DOSAGE
DOSAGE RANGE IN CHILDREN
(Intravenous administration should be made slowly)
Moderate Anxiety Disorders and Symptoms of Anxiety
2 mg to 5 mg, intramuscular or intravenous. Repeat in 3 to 4 hours, if necessary.
Severe Anxiety Disorders and Symptoms of Anxiety
5 mg to 10 mg, intramuscular or intravenous. Repeat in 3 to 4 hours, if necessary.
Acute Alcohol Withdrawal:
As an aid in symptomatic relief of acute agitation, tremor, impending or acute delirium tremens, and hallucinosis.
10 mg, intramuscular or intravenous initially, then 5 mg to 10 mg in 3 to 4 hours, if necessary.
Endoscopic Procedures:
Adjunctively, if apprehension, anxiety or acute stress reaction are present prior to endoscopic procedures. Dosage of narcotics should be reduced by at least a third and in some cases may be omitted. See PRECAUTIONS for peroral procedures.
Titrate intravenous dosage to desired sedative response, such as slurring of speech, with slow administration immediately prior to the procedure. Generally 10 mg or less is adequate, but up to 20 mg intravenous may be given, particularly when concomitant narcotics are omitted. If intravenous cannot be used, 5 mg to10 mg intramuscular approximately 30 minutes prior to the procedure.
Muscle Spasm
Associated with local pathology, cerebral palsy, athetosis, stiff-man syndrome, or tetanus.
5 mg to 10 mg, intramuscular or intravenous initially, then 5 mg to 10 mg in 3 to 4 hours, if necessary. For tetanus, larger doses may be required.
For tetanus in infants over 30 days of age, 1 mg to 2 mg intramuscular or intravenous, slowly, repeated every 3 to 4 hours as necessary. In children 5 years or older, 5 mg to 10 mg repeated every 3 to 4 hours may be required to control tetanus spasms. Respiratory assistance should be available.
Status Epilepticus :
In the convulsing patient, the intravenous route is by far preferred. This injection should be administered slowly. However, if intravenous administration is impossible, the intramuscular route may be used.
5 mg to 10 mg initially (intravenous preferred). This injection may be repeated if necessary at 10 to 15 minute intervals up to a maximum dose of 30 mg. If necessary, therapy with diazepam may be repeated in 2 to 4 hours; however, residual active metabolites may persist, and readministration should be made with this consideration. Extreme caution must be exercised with individuals with chronic lung disease or unstable cardiovascular status.
Children 3 months up to 17 years of age with status epilepticus:
First dose:
0.2 mg/kg (maximum 8 mg) by slow intravenous push (one minute in duration).Second dose (if necessary;
5 minutes after the first dose):
0.1 mg/kg (maximum 4 mg) by slow intravenous push (one minute in duration).EEG monitoring of the seizure may be helpful.
Preoperative Medication
To relieve anxiety and tension. (If atropine, scopolamine or other premedications are desired, they must be administered in separate syringes.)
10 mg, intramuscular (preferred route), before surgery.
Cardioversion
To relieve anxiety and tension and to reduce recall of procedure.
5 mg to 15 mg, intravenous, within 5 to 10 minutes prior to the procedure.
Once the acute symptomatology has been properly controlled with diazepam injection, the patient may be placed on oral therapy with diazepam if further treatment is required.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. -
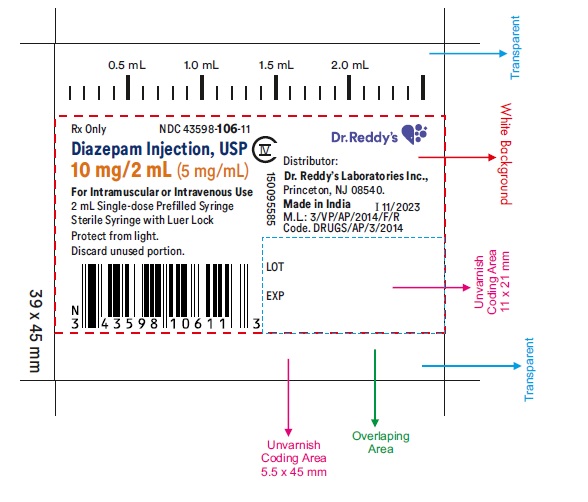
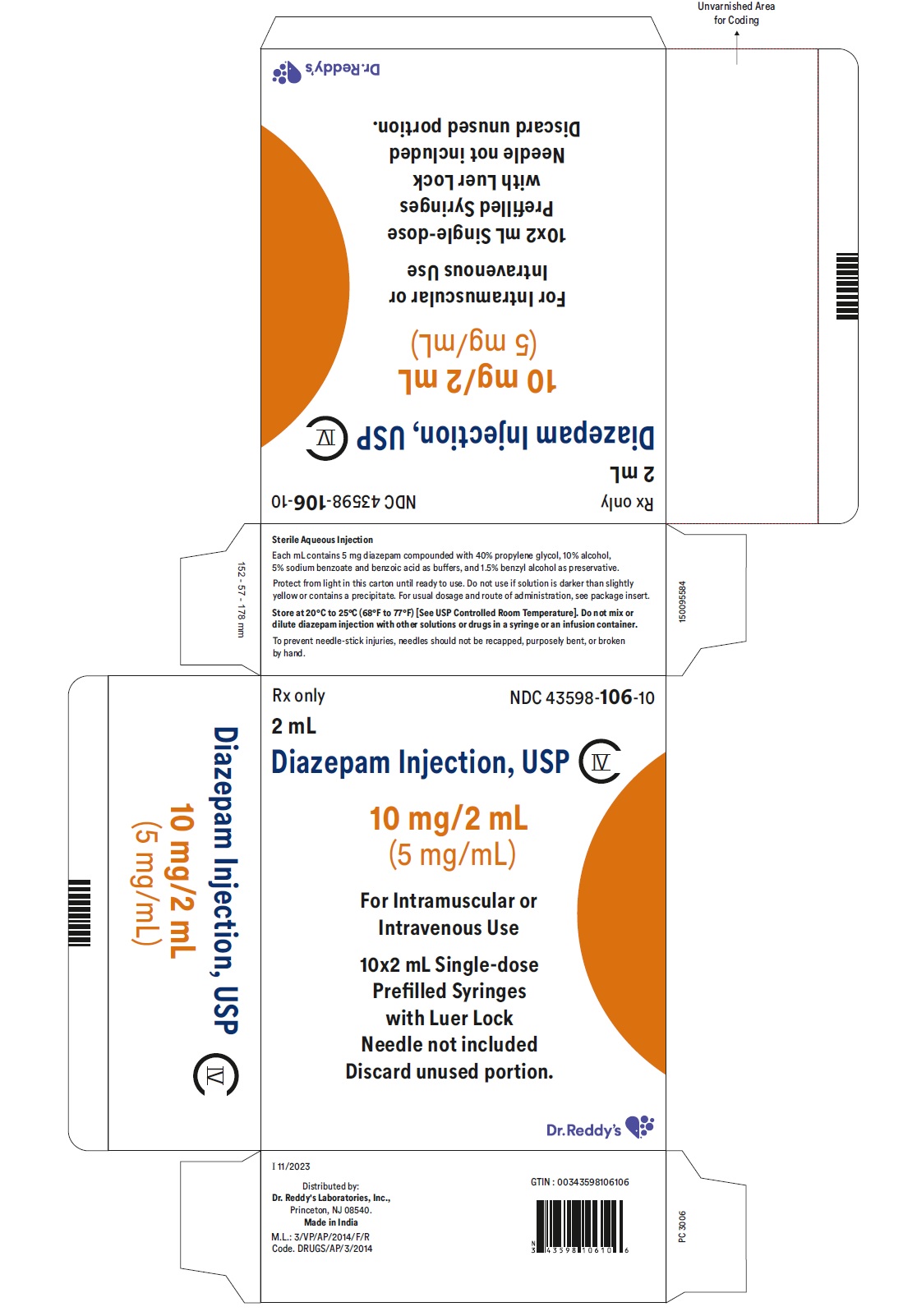
HOW SUPPLIED
Diazepam Injection, USP 10 mg/2 mL is a clear, colorless to slightly yellow solution supplied in 2 mL Prefilled Sterile Single-dose Syringe with Luer Lock.
Unit of Sale
Concentration
Each
NDC: 43598-106-10
Carton of 10
10 mg/2 mL
(5 mg/mL)
NDC: 43598-106-11
Prefilled, Single-dose syringe with Luer Lock
Store at 20°C to 25°C (68°F to 77°F). [See USP Controlled Room Temperature.]
Protect from light.
-
ANIMAL PHARMACOLOGY
Oral LD50 of diazepam is 720 mg/kg in mice and 1,240 mg/kg in rats. Intraperitoneal administration of 400 mg/kg to a monkey resulted in death on the sixth day.
Reproduction Studies:
A series of rat reproduction studies was performed with diazepam in oral doses of 1, 10, 80, and 100 mg/kg given for periods ranging from 60 to 228 days prior to mating. At 100 mg/kg there was a decrease in the number of pregnancies and surviving offspring in these rats. These effects may be attributable to prolonged sedative activity, resulting in lack of interest in mating and lessened maternal nursing and care of the young. Neonatal survival of rats at doses lower than 100 mg/kg was within normal limits. Several neonates, both controls and experimentals, in these rat reproduction studies showed skeletal or other defects. Further studies in rats at doses up to and including 80 mg/kg/day did not reveal significant teratological effects on the offspring. Rabbits were maintained on doses of 1, 2, 5, and 8 mg/kg from day 6 through day 18 of gestation. No adverse effects on reproduction and no teratological changes were noted.
CAUTION: Federal (USA) law prohibits dispensing without prescription.
To report SUSPECTED ADVERSE REACTIONS, contact Dr. Reddy’s Laboratories Inc., at 1-888-375-3784 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Distributed by:Dr. Reddy’s Laboratories Inc.,
Princeton, NJ 08540
Made in India
Issued: 06/2024
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL SECTION
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
DIAZEPAM
diazepam injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 43598-106 Route of Administration INTRAMUSCULAR, INTRAVENOUS DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DIAZEPAM (UNII: Q3JTX2Q7TU) (DIAZEPAM - UNII:Q3JTX2Q7TU) DIAZEPAM 10 mg in 2 mL Inactive Ingredients Ingredient Name Strength PROPYLENE GLYCOL (UNII: 6DC9Q167V3) ALCOHOL (UNII: 3K9958V90M) SODIUM BENZOATE (UNII: OJ245FE5EU) BENZYL ALCOHOL (UNII: LKG8494WBH) BENZOIC ACID (UNII: 8SKN0B0MIM) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 43598-106-10 10 in 1 CARTON 08/07/2024 1 NDC: 43598-106-11 2 mL in 1 SYRINGE, GLASS; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA218422 08/07/2024 Labeler - Dr. Reddy's Laboratories Inc (802315887) Establishment Name Address ID/FEI Business Operations Dr. Reddy’s Laboratories Limited FTO-9 650446243 analysis(43598-106) , manufacture(43598-106)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.