POMALYST- pomalidomide capsule
Pomalyst by
Drug Labeling and Warnings
Pomalyst by is a Prescription medication manufactured, distributed, or labeled by Celgene Corporation. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use POMALYST safely and effectively. See full prescribing information for POMALYST.
POMALYST® (pomalidomide) capsules, for oral use
Initial U.S. Approval: 2013WARNING: EMBRYO-FETAL TOXICITY and VENOUS AND ARTERIAL THROMBOEMBOLISM
See full prescribing information for complete boxed warning
EMBRYO-FETAL TOXICITY
- POMALYST is contraindicated in pregnancy. POMALYST is a thalidomide analogue. Thalidomide is a known human teratogen that causes severe life-threatening birth defects (4, 5.1, 8.1).
-
For females of reproductive potential: Exclude pregnancy before start of treatment. Prevent pregnancy during treatment by the use of 2 reliable methods of contraception (5.1, 8.3).
POMALYST is available only through a restricted program called POMALYST REMS® (5.2).
VENOUS AND ARTERIAL THROMBOEMBOLISM
- Deep venous thrombosis (DVT), pulmonary embolism (PE), myocardial infarction, and stroke occur in patients with multiple myeloma treated with POMALYST. Antithrombotic prophylaxis is recommended (5.3).
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
POMALYST is a thalidomide analogue indicated, in combination with dexamethasone, for patients with multiple myeloma who have received at least two prior therapies including lenalidomide and a proteasome inhibitor and have demonstrated disease progression on or within 60 days of completion of the last therapy (1.1).
DOSAGE AND ADMINISTRATION
Multiple Myeloma: 4 mg per day taken orally on Days 1-21 of repeated 28-day cycles until disease progression (2.1). Refer to section 14.1 for dexamethasone dosing (14.1).
DOSAGE FORMS AND STRENGTHS
Capsules: 1 mg, 2 mg, 3 mg, and 4 mg (3)
WARNINGS AND PRECAUTIONS
- Increased Mortality: Observed in patients with multiple myeloma when pembrolizumab was added to dexamethasone and a thalidomide analogue (5.4).
- Hematologic Toxicity: Neutropenia was the most frequently reported Grade 3/4 adverse event. Monitor patients for hematologic toxicities, especially neutropenia (5.5).
- Hepatotoxicity: Hepatic failure including fatalities; monitor liver function tests monthly (5.6).
- Severe Cutaneous Reactions: Discontinue POMALYST for severe reactions (5.7).
- Tumor Lysis Syndrome (TLS): Monitor patients at risk of TLS (i.e., those with high tumor burden) and take appropriate precautions (5.11).
- Hypersensitivity: Monitor patients for potential hypersensitivity. Discontinue POMALYST for angioedema and anaphylaxis (5.12).
ADVERSE REACTIONS
Most common adverse reactions (≥30%) included fatigue and asthenia, neutropenia, anemia, constipation, nausea, diarrhea, dyspnea, upper-respiratory tract infections, back pain, and pyrexia (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Celgene Corporation at 1-888-423-5436 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
- Lactation: Advise women not to breastfeed (8.2).
- Renal Impairment: Reduce POMALYST dose by at least 25% in patients with severe renal impairment requiring dialysis. Take dose of POMALYST following hemodialysis on hemodialysis days (2.4, 8.6).
- Hepatic Impairment: Reduce POMALYST dose by 25% in patients with mild to moderate hepatic impairment, reduce POMALYST dose by 50% in patients with severe hepatic impairment (2.5, 8.7).
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 10/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: EMBRYO-FETAL TOXICITY and VENOUS AND ARTERIAL THROMBOEMBOLISM
1 INDICATIONS AND USAGE
1.1 Multiple Myeloma
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Dose Adjustment for Toxicities
2.3 Dosage Adjustment for Strong CYP1A2 Inhibitors
2.4 Dosage Adjustment for Patients with Severe Renal Impairment on Hemodialysis
2.5 Dosage Adjustment for Patients with Hepatic Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Pregnancy
4.2 Hypersensitivity
5 WARNINGS AND PRECAUTIONS
5.1 Embryo-Fetal Toxicity
5.2 POMALYST REMS Program
5.3 Venous and Arterial Thromboembolism
5.4 Increased Mortality in Patients with Multiple Myeloma When Pembrolizumab Is Added to a Thalidomide Analogue and Dexamethasone
5.5 Hematologic Toxicity
5.6 Hepatotoxicity
5.7 Severe Cutaneous Reactions
5.8 Dizziness and Confusional State
5.9 Neuropathy
5.10 Risk of Second Primary Malignancies
5.11 Tumor Lysis Syndrome
5.12 Hypersensitivity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Drugs That Affect Pomalidomide Plasma Concentrations
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Smoking Tobacco
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Multiple Myeloma
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage
16.3 Handling and Disposal
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: EMBRYO-FETAL TOXICITY and VENOUS AND ARTERIAL THROMBOEMBOLISM
Embryo-Fetal Toxicity
- POMALYST is contraindicated in pregnancy. POMALYST is a thalidomide analogue. Thalidomide is a known human teratogen that causes severe birth defects or embryo-fetal death. In females of reproductive potential, obtain 2 negative pregnancy tests before starting POMALYST treatment.
- Females of reproductive potential must use 2 forms of contraception or continuously abstain from heterosexual sex during and for 4 weeks after stopping POMALYST treatment [see Contraindications (4), Warnings and Precautions (5.1), and Use in Specific Populations (8.1, 8.3)].
POMALYST is only available through a restricted distribution program called POMALYST REMS [see Warnings and Precautions (5.2)].
Venous and Arterial Thromboembolism
- Deep venous thrombosis (DVT), pulmonary embolism (PE), myocardial infarction, and stroke occur in patients with multiple myeloma treated with POMALYST. Prophylactic antithrombotic measures were employed in clinical trials. Thromboprophylaxis is recommended, and the choice of regimen should be based on assessment of the patient's underlying risk factors [see Warnings and Precautions (5.3)].
-
1 INDICATIONS AND USAGE
1.1 Multiple Myeloma
POMALYST, in combination with dexamethasone, is indicated for patients with multiple myeloma who have received at least two prior therapies including lenalidomide and a proteasome inhibitor and have demonstrated disease progression on or within 60 days of completion of the last therapy.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
Multiple Myeloma
Females of reproductive potential must have negative pregnancy testing and use contraception methods before initiating POMALYST [see Warnings and Precautions (5.1) and Use in Specific Populations (8.3)].
The recommended starting dose of POMALYST is 4 mg once daily orally on Days 1-21 of repeated 28-day cycles until disease progression. POMALYST should be given in combination with dexamethasone [see Clinical Studies (14.1)].
POMALYST may be taken with water. Inform patients not to break, chew, or open the capsules. POMALYST may be taken with or without food.
2.2 Dose Adjustment for Toxicities
Table 1: Dose Modification Instructions for POMALYST for Hematologic Toxicities ANC, absolute neutrophil count Toxicity Dose Modification Neutropenia - ANC <500 per mcL or febrile neutropenia (fever more than or equal to 38.5°C and ANC <1,000 per mcL)
- ANC return to more than or equal to 500 per mcL
- Interrupt POMALYST treatment, follow CBC weekly
- Resume POMALYST treatment at 3 mg daily
- For each subsequent drop <500 per mcL
- Return to more than or equal to 500 per mcL
- Interrupt POMALYST treatment
- Resume POMALYST treatment at 1 mg less than the previous dose
Thrombocytopenia - Platelets <25,000 per mcL
- Interrupt POMALYST treatment, follow CBC weekly
- Platelets return to >50,000 per mcL
- Resume POMALYST treatment at 3 mg daily
- For each subsequent drop <25,000 per mcL
- Return to more than or equal to 50,000 per mcL
- Interrupt POMALYST treatment
- Resume POMALYST treatment at 1 mg less than previous dose
To initiate a new cycle of POMALYST, the neutrophil count must be at least 500 per mcL and the platelet count must be at least 50,000 per mcL. If toxicities occur after dose reductions to 1 mg, then discontinue POMALYST.
Permanently discontinue POMALYST for angioedema, anaphylaxis, Grade 4 rash, skin exfoliation, bullae, or any other severe dermatologic reaction [see Warnings and Precautions (5.7)].
For other Grade 3 or 4 toxicities, hold treatment and restart treatment at 1 mg less than the previous dose when toxicity has resolved to less than or equal to Grade 2 at the physician's discretion.
2.3 Dosage Adjustment for Strong CYP1A2 Inhibitors
Avoid concomitant use of POMALYST with strong inhibitors of CYP1A2. Consider alternative treatments. If a strong CYP1A2 inhibitor must be used, reduce POMALYST dose by 50% [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
2.4 Dosage Adjustment for Patients with Severe Renal Impairment on Hemodialysis
For patients with severe renal impairment requiring dialysis, the recommended starting dose is 3 mg daily (25% dose reduction). Take POMALYST after completion of dialysis procedure on hemodialysis days [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
2.5 Dosage Adjustment for Patients with Hepatic Impairment
For patients with mild or moderate hepatic impairment (Child-Pugh classes A or B), the recommended starting dose is 3 mg daily (25% dose reduction). For patients with severe hepatic impairment (Child-Pugh class C), the recommended dose is 2 mg (50% dose reduction) [see Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].
- ANC <500 per mcL or febrile neutropenia (fever more than or equal to 38.5°C and ANC <1,000 per mcL)
-
3 DOSAGE FORMS AND STRENGTHS
POMALYST is available in the following capsule strengths:
- 1 mg: Dark blue opaque cap and yellow opaque body, imprinted "POML" on the cap in white ink and "1 mg" on the body in black ink
- 2 mg: Dark blue opaque cap and orange opaque body, imprinted "POML" on the cap and "2 mg" on the body in white ink
- 3 mg: Dark blue opaque cap and green opaque body, imprinted "POML" on the cap and "3 mg" on the body in white ink
- 4 mg: Dark blue opaque cap and blue opaque body, imprinted "POML" on the cap and "4 mg" on the body in white ink
-
4 CONTRAINDICATIONS
4.1 Pregnancy
POMALYST is contraindicated in females who are pregnant. POMALYST can cause fetal harm when administered to a pregnant female [see Warnings and Precautions (5.1) and Use in Specific Populations (8.1)]. Pomalidomide is a thalidomide analogue and is teratogenic in both rats and rabbits when administered during the period of organogenesis. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential risk to a fetus.
4.2 Hypersensitivity
POMALYST is contraindicated in patients who have demonstrated severe hypersensitivity (e.g., angioedema, anaphylaxis) to pomalidomide or any of the excipients [see Warnings and Precautions (5.7), Description (11)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Embryo-Fetal Toxicity
POMALYST is a thalidomide analogue and is contraindicated for use during pregnancy. Thalidomide is a known human teratogen that causes severe birth defects or embryo-fetal death [see Use in Specific Populations (8.1)]. POMALYST is only available through the POMALYST REMS program [see Warnings and Precautions (5.2)].
Females of Reproductive Potential
Females of reproductive potential must avoid pregnancy for at least 4 weeks before beginning POMALYST therapy, during therapy, during dose interruptions and for at least 4 weeks after completing therapy.Females must commit either to abstain continuously from heterosexual sexual intercourse or to use 2 methods of reliable birth control, beginning 4 weeks prior to initiating treatment with POMALYST, during therapy, during dose interruptions, and continuing for 4 weeks following discontinuation of POMALYST therapy.
Two negative pregnancy tests must be obtained prior to initiating therapy. The first test should be performed within 10-14 days and the second test within 24 hours prior to prescribing POMALYST therapy and then weekly during the first month, then monthly thereafter in females with regular menstrual cycles, or every 2 weeks in females with irregular menstrual cycles [see Use in Specific Populations (8.3)].
Males
Pomalidomide is present in the semen of patients receiving the drug. Therefore, males must always use a latex or synthetic condom during any sexual contact with females of reproductive potential while taking POMALYST and for up to 4 weeks after discontinuing POMALYST, even if they have undergone a successful vasectomy. Male patients taking POMALYST must not donate sperm [see Use in Specific Populations (8.3)].Blood Donation
Patients must not donate blood during treatment with POMALYST and for 4 weeks following discontinuation of the drug because the blood might be given to a pregnant female patient whose fetus must not be exposed to POMALYST.5.2 POMALYST REMS Program
Because of the embryo-fetal risk [see Warnings and Precautions (5.1)], POMALYST is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS), the "POMALYST REMS" program.
Required components of the POMALYST REMS program include the following:
- Prescribers must be certified with the POMALYST REMS program by enrolling and complying with the REMS requirements.
- Patients must sign a Patient-Physician Agreement Form and comply with the REMS requirements. In particular, female patients of reproductive potential who are not pregnant must comply with the pregnancy testing and contraception requirements [see Use in Specific Populations (8.3)] and males must comply with contraception requirements [see Use in Specific Populations (8.3)].
- Pharmacies must be certified with the POMALYST REMS program, must only dispense to patients who are authorized to receive POMALYST and comply with REMS requirements.
Further information about the POMALYST REMS program is available at www.celgeneriskmanagement.com or by telephone at 1-888-423-5436.
5.3 Venous and Arterial Thromboembolism
Venous thromboembolic events (deep venous thrombosis and pulmonary embolism) and arterial thromboembolic events (myocardial infarction and stroke) have been observed in patients treated with POMALYST. In Trial 2, where anticoagulant therapies were mandated, thromboembolic events occurred in 8.0% of patients treated with POMALYST and low dose-dexamethasone (Low-dose Dex), and 3.3% of patients treated with high-dose dexamethasone. Venous thromboembolic events (VTE) occurred in 4.7% of patients treated with POMALYST and Low-dose Dex, and 1.3% of patients treated with high-dose dexamethasone. Arterial thromboembolic events include terms for arterial thromboembolic events, ischemic cerebrovascular conditions, and ischemic heart disease. Arterial thromboembolic events occurred in 3.0% of patients treated with POMALYST and Low-dose Dex, and 1.3% of patients treated with high-dose dexamethasone.
Patients with known risk factors, including prior thrombosis, may be at greater risk, and actions should be taken to try to minimize all modifiable factors (e.g., hyperlipidemia, hypertension, smoking). Thromboprophylaxis is recommended, and the choice of regimen should be based on assessment of the patient's underlying risk factors.
5.4 Increased Mortality in Patients with Multiple Myeloma When Pembrolizumab Is Added to a Thalidomide Analogue and Dexamethasone
In two randomized clinical trials in patients with multiple myeloma, the addition of pembrolizumab to a thalidomide analogue plus dexamethasone, a use for which no PD-1 or PD-L1 blocking antibody is indicated, resulted in increased mortality. Treatment of patients with multiple myeloma with a PD-1 or PD-L1 blocking antibody in combination with a thalidomide analogue plus dexamethasone is not recommended outside of controlled clinical trials.
5.5 Hematologic Toxicity
In trials 1 and 2 in patients who received POMALYST + Low-dose Dex, neutropenia was the most frequently reported Grade 3/4 adverse reaction, followed by anemia and thrombocytopenia. Neutropenia of any grade was reported in 51% of patients in both trials. The rate of Grade 3/4 neutropenia was 46%. The rate of febrile neutropenia was 8%.
Monitor patients for hematologic toxicities, especially neutropenia. Monitor complete blood counts weekly for the first 8 weeks and monthly thereafter. Patients may require dose interruption and/or modification [see Dosage and Administration (2.2)].
5.6 Hepatotoxicity
Hepatic failure, including fatal cases, has occurred in patients treated with POMALYST. Elevated levels of alanine aminotransferase and bilirubin have also been observed in patients treated with POMALYST. Monitor liver function tests monthly. Stop POMALYST upon elevation of liver enzymes and evaluate. After return to baseline values, treatment at a lower dose may be considered.
5.7 Severe Cutaneous Reactions
Severe cutaneous reactions including Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS) have been reported. DRESS may present with a cutaneous reaction (such as rash or exfoliative dermatitis), eosinophilia, fever, and/or lymphadenopathy with systemic complications such as hepatitis, nephritis, pneumonitis, myocarditis, and/or pericarditis. These reactions can be fatal. Consider POMALYST interruption or discontinuation for Grade 2-3 skin rash. Permanently discontinue POMALYST for Grade 4 rash, exfoliative or bullous rash, or for other severe cutaneous reactions such as SJS, TEN or DRESS [see Dosage and Administration (2.2)].
5.8 Dizziness and Confusional State
In trials 1 and 2 in patients who received POMALYST + Low-dose Dex, 14% of patients experienced dizziness and 7% of patients experienced a confusional state; 1% of patients experienced Grade 3 or 4 dizziness, and 3% of patients experienced Grade 3 or 4 confusional state. Instruct patients to avoid situations where dizziness or confusional state may be a problem and not to take other medications that may cause dizziness or confusional state without adequate medical advice.
5.9 Neuropathy
In trials 1 and 2 in patients who received POMALYST + Low-dose Dex, 18% of patients experienced neuropathy, with approximately 12% of the patients experiencing peripheral neuropathy. Two percent of patients experienced Grade 3 neuropathy in trial 2. There were no cases of Grade 4 neuropathy adverse reactions reported in either trial.
5.10 Risk of Second Primary Malignancies
Cases of acute myelogenous leukemia have been reported in patients receiving POMALYST as an investigational therapy outside of multiple myeloma.
5.11 Tumor Lysis Syndrome
Tumor lysis syndrome (TLS) may occur in patients treated with pomalidomide. Patients at risk for TLS are those with high tumor burden prior to treatment. These patients should be monitored closely and appropriate precautions taken.
5.12 Hypersensitivity
Hypersensitivity, including angioedema, anaphylaxis, and anaphylactic reactions to POMALYST have been reported. Permanently discontinue POMALYST for angioedema or anaphylaxis [see Dosage and Administration (2.2)].
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described in detail in other labeling sections:
- Fetal Risk [see Boxed Warning, Warnings and Precautions (5.1, 5.2)]
- Venous and Arterial Thromboembolism [see Boxed Warning, Warnings and Precautions (5.3)]
- Increased Mortality in Patients with Multiple Myeloma When Pembrolizumab Is Added to a Thalidomide Analogue and Dexamethasone [see Warnings and Precautions (5.4)]
- Hematologic Toxicity [see Warnings and Precautions (5.5)]
- Hepatotoxicity [see Warnings and Precautions (5.6)]
- Severe Cutaneous Reactions [see Warnings and Precautions (5.7)]
- Dizziness and Confusional State [see Warnings and Precautions (5.8)]
- Neuropathy [see Warnings and Precautions (5.9)]
- Risk of Second Primary Malignancies [see Warnings and Precautions (5.10)]
- Tumor Lysis Syndrome [see Warnings and Precautions (5.11)]
- Hypersensitivity [see Warnings and Precautions (5.12)]
6.1 Clinical Trials Experience
Multiple Myeloma
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In Trial 1, data were evaluated from 219 patients (safety population) who received treatment with POMALYST + Low-dose Dex (112 patients) or POMALYST alone (107 patients). Median number of treatment cycles was 5. Sixty-seven percent of patients in the study had a dose interruption of either drug due to adverse reactions. Forty-two percent of patients in the study had a dose reduction of either drug due to adverse reactions. The discontinuation rate due to adverse reactions was 11%.
In Trial 2, data were evaluated from 450 patients (safety population) who received treatment with POMALYST + Low-dose Dex (300 patients) or High-dose Dexamethasone (High-dose Dex) (150 patients). The median number of treatment cycles for the POMALYST + Low-dose Dex arm was 5. In the POMALYST + Low-dose Dex arm, 67% of patients had a dose interruption of POMALYST, the median time to the first dose interruption of POMALYST was 4.1 weeks. Twenty-seven percent of patients had a dose reduction of POMALYST, the median time to the first dose reduction of POMALYST was 4.5 weeks. Eight percent of patients discontinued POMALYST due to adverse reactions.
Tables 2 and 3 summarize the adverse reactions reported in Trials 1 and 2, respectively.
Table 2: Adverse Reactions in Any POMALYST Treatment Arm in Trial 1* * Regardless of attribution of relatedness to POMALYST.
a POMALYST alone arm includes all patients randomized to the POMALYST alone arm who took study drug; 61 of the 107 patients had dexamethasone added during the treatment period.
b Serious adverse reactions were reported in at least 2 patients in any POMALYST treatment arm.
Data cutoff: 01 March 2013All Adverse Reactions ≥10% in
Either ArmGrade 3 or 4 ≥5% in Either Arm Body System
Adverse Reaction
POMALYSTa
(N=107)POMALYST +
Low-dose Dex
(N=112)
POMALYST
(N=107)POMALYST +
Low-dose Dex
(N=112)Number (%) of patients with at least one adverse reaction 107 (100) 112 (100) 98 (91.6) 102 (91.1) Blood and lymphatic system disorders Neutropenia b 57 (53.3) 55 (49.1) 51 (47.7) 46 (41.1) Anemia b 41 (38.3) 47 (42.0) 25 (23.4) 24 (21.4) Thrombocytopenia b 28 (26.2) 26 (23.2) 24 (22.4) 21 (18.8) Leukopenia 14 (13.1) 22 (19.6) 7 (6.5) 11 (9.8) Febrile neutropenia b <10% <10% 6 (5.6) 3 (2.7) Lymphopenia 4 (3.7) 17 (15.2) 2 (1.9) 8 (7.1) General disorders and administration site conditions Fatigue and asthenia b 62 (57.9) 70 (62.5) 13 (12.1) 19 (17.0) Edema peripheral 27 (25.2) 19 (17.0) 0 (0.0) 0 (0.0) Pyrexia b 25 (23.4) 36 (32.1) <5% <5% Chills 11 (10.3) 14 (12.5) 0 (0.0) 0 (0.0) Gastrointestinal disorders Nausea b 39 (36.4) 27 (24.1) <5% <5% Constipation b 38 (35.5) 41 (36.6) <5% <5% Diarrhea 37 (34.6) 40 (35.7) <5% <5% Vomiting b 15 (14.0) 16 (14.3) <5% 0 (0.0) Musculoskeletal and connective tissue disorders Back pain b 37 (34.6) 36 (32.1) 15 (14.0) 11 (9.8) Musculoskeletal chest pain 25 (23.4) 22 (19.6) <5% 0 (0.0) Muscle spasms 23 (21.5) 22 (19.6) <5% <5% Arthralgia 18 (16.8) 17 (15.2) <5% <5% Muscular weakness 15 (14.0) 15 (13.4) 6 (5.6) 4 (3.6) Bone pain 13 (12.1) 8 (7.1) <5% <5% Musculoskeletal pain 13 (12.1) 19 (17.0) <5% <5% Pain in extremity 8 (7.5) 16 (14.3) 0 (0.0) <5% Infections and infestations Upper respiratory tract
infection40 (37.4) 32 (28.6) <5% <5% Pneumonia b 30 (28.0) 38 (33.9) 21 (19.6) 32 (28.6) Urinary tract infection b 11 (10.3) 19 (17.0) 2 (1.9) 10 (8.9) Sepsis b <10% <10% 6 (5.6) 5 (4.5) Metabolism and nutrition disorders Decreased appetite 25 (23.4) 21 (18.8) <5% 0 (0.0) Hypercalcemia b 23 (21.5) 13 (11.6) 11 (10.3) 1 (0.9) Hypokalemia 13 (12.1) 13 (11.6) <5% <5% Hyperglycemia 12 (11.2) 17 (15.2) <5% <5% Hyponatremia 12 (11.2) 14 (12.5) <5% <5% Dehydration b <10% <10% 5 (4.7) 6 (5.4) Hypocalcemia 6 (5.6) 13 (11.6) 0 (0.0) <5% Respiratory, thoracic and mediastinal disorders Dyspnea b 38 (35.5) 50 (44.6) 8 (7.5) 14 (12.5) Cough 18 (16.8) 25 (22.3) 0 (0.0) 0 (0.0) Epistaxis 18 (16.8) 12 (10.7) <5% 0 (0.0) Productive cough 10 (9.3) 14 (12.5) 0 (0.0) 0 (0.0) Oropharyngeal pain 6 (5.6) 12 (10.7) 0 (0.0) 0 (0.0) Nervous system disorders Dizziness 24 (22.4) 20 (17.9) <5% <5% Peripheral neuropathy 23 (21.5) 20 (17.9) 0 (0.0) 0 (0.0) Headache 16 (15.0) 15 (13.4) 0 (0.0) <5% Tremor 11 (10.3) 15 (13.4) 0 (0.0) 0 (0.0) Skin and subcutaneous tissue disorders Rash 22 (20.6) 18 (16.1) 0 (0.0) <5% Pruritus 16 (15.0) 10 (8.9) 0 (0.0) 0 (0.0) Dry skin 10 (9.3) 12 (10.7) 0 (0.0) 0 (0.0) Hyperhidrosis 8 (7.5) 18 (16.1) 0 (0.0) 0 (0.0) Night sweats 5 (4.7) 14 (12.5) 0 (0.0) 0 (0.0) Investigations Blood creatinine increased b 20 (18.7) 11 (9.8) 6 (5.6) 3 (2.7) Weight decreased 16 (15.0) 10 (8.9) 0 (0.0) 0 (0.0) Weight increased 1 (0.9) 12 (10.7) 0 (0.0) 0 (0.0) Psychiatric disorders Anxiety 14 (13.1) 8 (7.1) 0 (0.0) 0 (0.0) Confusional state b 13 (12.1) 15 (13.4) 6 (5.6) 3 (2.7) Insomnia 7 (6.5) 18 (16.1) 0 (0.0) 0 (0.0) Renal and urinary disorders Renal failure b 16 (15.0) 11 (9.8) 9 (8.4) 8 (7.1) Table 3: Adverse Reactions in Trial 2 a Percentage did not meet the criteria to be considered as an adverse reaction for POMALYST for that category of event (i.e., all adverse events or Grade 3 or 4 adverse events).
b Serious adverse reactions were reported in at least 3 patients in the POM + Low-dose Dex arm, AND at least 1% higher than the High-dose-Dex arm percentage.
Data cutoff: 01 March 2013All Adverse Reactions
(≥5% in POMALYST + Low-dose Dex arm, and at least 2% points higher than the High-dose-Dex arm)Grade 3 or 4
(≥1% in POMALYST + Low-dose Dex arm, and at least 1% point higher than the High-dose-Dex arm)Body System
Adverse ReactionPOMALYST +
Low-dose Dex
(N=300)High-dose Dex
(N=150)POMALYST +
Low-dose Dex
(N=300)High-dose Dex
(N=150)Number (%) of patients with at least one adverse reaction 297 (99.0) 149 (99.3) 259 (86.3) 127 (84.7) Blood and lymphatic system disorders Neutropenia b 154 (51.3) 31 (20.7) 145 (48.3) 24 (16.0) Thrombocytopenia 89 (29.7) a 44 (29.3) a 66 (22.0) a 39 (26.0) a Leukopenia 38 (12.7) 8 (5.3) 27 (9.0) 5 (3.3) Febrile neutropenia b 28 (9.3) 0 (0.0) 28 (9.3) 0 (0.0) General disorders and administration site conditions Fatigue and asthenia 140 (46.7) 64 (42.7) 26 (8.7) a 18 (12.0) a Pyrexia b 80 (26.7) 35 (23.3) 9 (3.0) a 7 (4.7) a Edema peripheral 52 (17.3) 17 (11.3) 4 (1.3) a 3 (2.0) a Pain 11 (3.7) a 3 (2.0) a 5 (1.7) 1 (0.7) Infections and infestations Upper respiratory tract infection b 93 (31.0) 19 (12.7) 9 (3.0) 1 (0.7) Pneumonia b 58 (19.3) 20 (13.3) 47 (15.7) 15 (10.0) Neutropenic sepsis b 3 (1.0) a 0 (0.0) a 3 (1.0) 0 (0.0) Gastrointestinal disorders Diarrhea 66 (22.0) 28 (18.7) 3 (1.0) a 2 (1.3) a Constipation 65 (21.7) 22 (14.7) 7 (2.3) 0 (0.0) Nausea 45 (15.0) 17 (11.3) 3 (1.0) a 2 (1.3) a Vomiting 23 (7.7) 6 (4.0) 3 (1.0) 0 (0.0) Musculoskeletal and connective tissue disorders Back pain b 59 (19.7) 24 (16.0) 15 (5.0) 6 (4.0) Bone pain b 54 (18.0) 21 (14.0) 22 (7.3) 7 (4.7) Muscle spasms 46 (15.3) 11 (7.3) 1 (0.3) a 1 (0.7) a Arthralgia 26 (8.7) 7 (4.7) 2 (0.7) a 1 (0.7) a Pain in extremity 20 (6.7) a 9 (6.0) a 6 (2.0) 0 (0.0) Respiratory, thoracic and mediastinal disorders Dyspnea b 76 (25.3) 25 (16.7) 17 (5.7) 7 (4.7) Cough 60 (20.0) 15 (10.0) 2 (0.7) a 1 (0.7) a Chronic obstructive pulmonary
disease b5 (1.7) a 0 (0.0) a 4 (1.3) 0 (0.0) Nervous system disorders Peripheral neuropathy 52 (17.3) 18 (12.0) 5 (1.7) a 2 (1.3) a Dizziness 37 (12.3) 14 (9.3) 4 (1.3) a 2 (1.3) a Headache 23 (7.7) 8 (5.3) 1 (0.3) a 0 (0.0) a Tremor 17 (5.7) 2 (1.3) 2 (0.7) a 0 (0.0) a Depressed level of consciousness 5 (1.7) a 0 (0.0) a 3 (1.0) 0 (0.0) Metabolism and nutrition disorders Decreased appetite 38 (12.7) 12 (8.0) 3 (1.0) a 2 (1.3) a Hypokalemia 28 (9.3) a 12 (8.0) a 12 (4.0) 4 (2.7) Hypocalcemia 12 (4.0) a 9 (6.0) a 5 (1.7) 1 (0.7) Skin and subcutaneous tissue disorders Rash 23 (7.7) 2 (1.3) 3 (1.0) 0 (0.0) Pruritus 22 (7.3) 5 (3.3) 0 (0.0) a 0 (0.0) a Hyperhidrosis 15 (5.0) 1 (0.7) 0 (0.0) a 0 (0.0) a Investigations Neutrophil count decreased 15 (5.0) 1 (0.7) 14 (4.7) 1 (0.7) Platelet count decreased 10 (3.3) a 3 (2.0) a 8 (2.7) 2 (1.3) White blood cell count decreased 8 (2.7) a 1 (0.7) a 8 (2.7) 0 (0.0) Alanine aminotransferase increased 7 (2.3) a 2 (1.3) a 5 (1.7) 0 (0.0) Aspartate aminotransferase
increased4 (1.3) a 2 (1.3) a 3 (1.0) 0 (0.0) Lymphocyte count decreased 3 (1.0) a 1 (0.7) a 3 (1.0) 0 (0.0) Renal and urinary disorders Renal failure 31 (10.3) a 18 (12.0) a 19 (6.3) 8 (5.3) Injury, poisoning and procedural complications Femur fracture b 5 (1.7) a 1 (0.7) a 5 (1.7) 1 (0.7) Reproductive system and breast disorders Pelvic pain 6 (2.0) a 3 (2.0) a 4 (1.3) 0 (0.0) Other Adverse Reactions
Other adverse reactions of POMALYST in patients with multiple myeloma, not described above, and considered important:Cardiac disorders: Myocardial infarction, Atrial fibrillation, Angina pectoris, Cardiac failure congestive
Ear and labyrinth disorders: Vertigo
Gastrointestinal disorders: Abdominal pain
General disorders and administration site conditions: General physical health deterioration, Non-cardiac chest pain, Multi-organ failure
Hepatobiliary disorders: Hyperbilirubinemia
Infections and infestations: Pneumocystis jiroveci pneumonia, Respiratory syncytial virus infection, Neutropenic sepsis, Bacteremia, Pneumonia respiratory syncytial viral, Cellulitis, Urosepsis, Septic shock, Clostridium difficile colitis, Pneumonia streptococcal, Lobar pneumonia, Viral infection, Lung infection
Investigations: Alanine aminotransferase increased, Hemoglobin decreased
Injury, poisoning and procedural complications: Fall, Compression fracture, Spinal compression fracture
Metabolism and nutritional disorders: Hyperkalemia, Failure to thrive
Nervous System disorders: Depressed level of consciousness, Syncope
Psychiatric disorders: Mental status change
Renal and urinary disorders: Urinary retention, Hyponatremia
Reproductive system and breast disorders: Pelvic pain
Respiratory, thoracic, and mediastinal disorders: Interstitial lung disease, Pulmonary embolism, Respiratory failure, Bronchospasm
Vascular disorders: Hypotension6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of POMALYST. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and lymphatic system disorders: Pancytopenia
Endocrine disorders: Hypothyroidism, hyperthyroidism
Gastrointestinal disorders: Gastrointestinal hemorrhage
Hepatobiliary disorders: Hepatic failure (including fatal cases), elevated liver enzymes
Immune system disorders: Allergic reactions (e.g., angioedema, anaphylaxis, urticaria), solid organ transplant rejection
Infections and infestations: Hepatitis B virus reactivation, Herpes zoster
Neoplasms benign, malignant and unspecified (incl cysts and polyps): Tumor lysis syndrome, basal cell carcinoma, and squamous cell carcinoma of the skin
Skin and Subcutaneous Tissue Disorders: Stevens-Johnson Syndrome, toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms (DRESS)
-
7 DRUG INTERACTIONS
7.1 Drugs That Affect Pomalidomide Plasma Concentrations
Pomalidomide is primarily metabolized by CYP1A2 and CYP3A4. Pomalidomide is also a substrate for P-glycoprotein (P-gp).
CYP1A2 inhibitors:
In healthy volunteers, co-administration of fluvoxamine, a strong CYP1A2 inhibitor, increased Cmax and AUC of pomalidomide by 24% and 125% respectively [see Clinical Pharmacology (12.3)]. Increased pomalidomide exposure increases the risk of exposure related toxicities.
Avoid co-administration of strong CYP1A2 inhibitors (e.g. ciprofloxacin and fluvoxamine) [see Dosage and Administration (2.3) and Clinical Pharmacology (12.3)]. If co-administration is unavoidable, reduce the POMALYST dose [see Dosage and Administration (2.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in females exposed to POMALYST during pregnancy as well as female partners of male patients who are exposed to POMALYST. This registry is also used to understand the root cause for the pregnancy. Report any suspected fetal exposure to POMALYST to the FDA via the MedWatch program at 1-800-FDA-1088 and also to Celgene Corporation at 1-888-423-5436.
Risk Summary
Based on the mechanism of action [see Clinical Pharmacology (12.1)] and findings from animal studies, POMALYST can cause embryo-fetal harm when administered to a pregnant female and is contraindicated during pregnancy [see Boxed Warning, Contraindications (4), and Warnings and Precautions (5.1)].
POMALYST is a thalidomide analogue. Thalidomide is a human teratogen, inducing a high frequency of severe and life-threatening birth defects such as amelia (absence of limbs), phocomelia (short limbs), hypoplasticity of the bones, absence of bones, external ear abnormalities (including anotia, micropinna, small or absent external auditory canals), facial palsy, eye abnormalities (anophthalmos, microphthalmos), and congenital heart defects. Alimentary tract, urinary tract, and genital malformations have also been documented, and mortality at or shortly after birth has been reported in about 40% of infants.
Pomalidomide was teratogenic in both rats and rabbits when administered during the period of organogenesis. Pomalidomide crossed the placenta after administration to pregnant rabbits [see Data]. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential risk to a fetus.
If pregnancy does occur during treatment, immediately discontinue the drug. Under these conditions, refer patient to an obstetrician/gynecologist experienced in reproductive toxicity for further evaluation and counseling. Report any suspected fetal exposure to POMALYST to the FDA via the MedWatch program at 1-800-FDA-1088 and also to Celgene Corporation at 1-888-423-5436.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. The estimated background risk in the U.S. general population of major birth defects is 2%-4% and of miscarriage is 15%-20% of clinically recognized pregnancies.
Animal Data
Pomalidomide was teratogenic in both rats and rabbits in the embryo-fetal developmental studies when administered during the period of organogenesis.
In rats, pomalidomide was administered orally to pregnant animals at doses of 25 to 1000 mg/kg/day. Malformations or absence of urinary bladder, absence of thyroid gland, and fusion and misalignment of lumbar and thoracic vertebral elements (vertebral, central, and/or neural arches) were observed at all dose levels. There was no maternal toxicity observed in this study. The lowest dose in rats resulted in an exposure (AUC) approximately 85-fold of the human exposure at the recommended dose of 4 mg/day. Other embryo-fetal toxicities included increased resorptions leading to decreased number of viable fetuses.
In rabbits, pomalidomide was administered orally to pregnant animals at doses of 10 to 250 mg/kg/day. Increased cardiac malformations such as interventricular septal defect were seen at all doses with significant increases at 250 mg/kg/day. Additional malformations observed at 250 mg/kg/day included anomalies in limbs (flexed and/or rotated fore- and/or hindlimbs, unattached or absent digit) and associated skeletal malformations (not ossified metacarpal, misaligned phalanx and metacarpal, absent digit, not ossified phalanx, and short not ossified or bent tibia), moderate dilation of the lateral ventricle in the brain, abnormal placement of the right subclavian artery, absent intermediate lobe in the lungs, low-set kidney, altered liver morphology, incompletely or not ossified pelvis, an increased average for supernumerary thoracic ribs, and a reduced average for ossified tarsals. No maternal toxicity was observed at the low dose (10 mg/kg/day) that resulted in cardiac anomalies in fetuses; this dose resulted in an exposure (AUC) approximately equal to that reported in humans at the recommended dose of 4 mg/day. Additional embryo-fetal toxicity included increased resorption.
Following daily oral administration of pomalidomide from Gestation Day 7 through Gestation Day 20 in pregnant rabbits, fetal plasma pomalidomide concentrations were approximately 50% of the maternal Cmax at all dosages (5 to 250 mg/kg/day), indicating that pomalidomide crossed the placenta.
8.2 Lactation
Risk Summary
There is no information regarding the presence of pomalidomide in human milk, the effects of POMALYST on the breastfed child, or the effects of POMALYST on milk production. Pomalidomide was excreted in the milk of lactating rats [see Data]. Because many drugs are excreted in human milk and because of the potential for adverse reactions in a breastfed child from POMALYST, advise women not to breastfeed during treatment with POMALYST.
Animal Data
Following a single oral administration of pomalidomide to lactating rats approximately 14 days postpartum, pomalidomide was transferred into milk, with milk to plasma ratios of 0.63 to 1.46.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
POMALYST can cause fetal harm when administered during pregnancy [see Use in Specific Populations (8.1)]. Verify the pregnancy status of females of reproductive potential prior to initiating POMALYST therapy and during therapy. Advise females of reproductive potential that they must avoid pregnancy 4 weeks before therapy, while taking POMALYST, during dose interruptions and for at least 4 weeks after completing therapy.
Females of reproductive potential must have 2 negative pregnancy tests before initiating POMALYST. The first test should be performed within 10-14 days, and the second test within 24 hours prior to prescribing POMALYST. Once treatment has started and during dose interruptions, pregnancy testing for females of reproductive potential should occur weekly during the first 4 weeks of use, then pregnancy testing should be repeated every 4 weeks in females with regular menstrual cycles. If menstrual cycles are irregular, the pregnancy testing should occur every 2 weeks. Pregnancy testing and counseling should be performed if a patient misses her period or if there is any abnormality in her menstrual bleeding. POMALYST treatment must be discontinued during this evaluation.
Contraception
Females
Females of reproductive potential must commit either to abstain continuously from heterosexual sexual intercourse or to use 2 methods of reliable birth control simultaneously: one highly effective form of contraception – tubal ligation, IUD, hormonal (birth control pills, injections, hormonal patches, vaginal rings, or implants), or partner's vasectomy, and 1 additional effective contraceptive method – male latex or synthetic condom, diaphragm, or cervical cap. Contraception must begin 4 weeks prior to initiating treatment with POMALYST, during therapy, during dose interruptions, and continuing for 4 weeks following discontinuation of POMALYST therapy. Reliable contraception is indicated even where there has been a history of infertility, unless due to hysterectomy. Females of reproductive potential should be referred to a qualified provider of contraceptive methods, if needed.
Males
Pomalidomide is present in the semen of males who take POMALYST. Therefore, males must always use a latex or synthetic condom during any sexual contact with females of reproductive potential while taking POMALYST and for up to 4 weeks after discontinuing POMALYST, even if they have undergone a successful vasectomy. Male patients taking POMALYST must not donate sperm.
Infertility
Based on findings in animals, female fertility may be compromised by treatment with POMALYST [see Nonclinical Toxicology (13.1)].
8.5 Geriatric Use
No dosage adjustment is required for POMALYST based on age.
Of the total number of patients in clinical studies of POMALYST, 44% were aged older than 65 years, while 10% were aged older than 75 years. No overall differences in effectiveness were observed between these patients and younger patients. In these studies, patients older than 65 years were more likely than patients less than or equal to 65 years of age to experience pneumonia.
8.6 Renal Impairment
In patients with severe renal impairment requiring dialysis, the AUC of pomalidomide increased by 38% and the rate of SAE increased by 64% relative to patients with normal renal function; therefore, starting dose adjustment is recommended. For patients with severe renal impairment requiring dialysis, POMALYST should be administered after the completion of hemodialysis on dialysis days because exposure of pomalidomide could be significantly decreased during dialysis [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Pomalidomide is metabolized primarily by the liver. Following single dose administration, the AUC of pomalidomide increased 51%, 58%, and 72% in subjects with mild (Child-Pugh class A), moderate (Child-Pugh class B), and severe (Child-Pugh class C) hepatic impairment compared to subjects with normal liver function. Dose adjustment is recommended in patients with hepatic impairment [see Dosage and Administration (2.5) and Clinical Pharmacology (12.3)].
8.8 Smoking Tobacco
Cigarette smoking reduces pomalidomide AUC by 32% due to CYP1A2 induction. Advise patients that smoking may reduce the efficacy of pomalidomide [see Clinical Pharmacology (12.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
POMALYST is an immunomodulatory antineoplastic agent. The chemical name is (RS)-4-Amino-2-(2,6-dioxo-piperidin-3-yl)-isoindoline-1,3-dione and it has the following chemical structure:
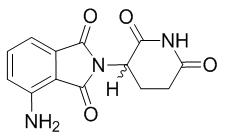
The empirical formula for pomalidomide is C13H11N3O4 and the gram molecular weight is 273.24.
Pomalidomide is a yellow solid powder. It has limited to low solubility into organic solvents and it has low solubility in all pH solutions (about 0.01 mg/mL). Pomalidomide has a chiral carbon atom which exists as a racemic mixture of the R(+) and S(-) enantiomers.
POMALYST is available in 1-mg, 2-mg, 3-mg, and 4-mg capsules for oral administration. Each capsule contains pomalidomide as the active ingredient and the following inactive ingredients: mannitol, pregelatinized starch, and sodium stearyl fumarate. The 1-mg capsule shell contains gelatin, titanium dioxide, FD&C blue 2, yellow iron oxide, white ink, and black ink. The 2-mg capsule shell contains gelatin, titanium dioxide, FD&C blue 2, yellow iron oxide, FD&C red 3, and white ink. The 3-mg capsule shell contains gelatin, titanium dioxide, FD&C blue 2, yellow iron oxide, and white ink. The 4-mg capsule shell contains gelatin, titanium dioxide, FD&C blue 1, FD&C blue 2, and white ink.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Pomalidomide is an analogue of thalidomide with immunomodulatory, antiangiogenic, and antineoplastic properties. Cellular activities of pomalidomide are mediated through its target cereblon, a component of a cullin ring E3 ubiquitin ligase enzyme complex. In vitro, in the presence of drug, substrate proteins (including Aiolos and Ikaros) are targeted for ubiquitination and subsequent degradation leading to direct cytotoxic and immunomodulatory effects. In in vitro cellular assays, pomalidomide inhibited proliferation and induced apoptosis of hematopoietic tumor cells. Additionally, pomalidomide inhibited the proliferation of lenalidomide-resistant multiple myeloma cell lines and synergized with dexamethasone in both lenalidomide-sensitive and lenalidomide-resistant cell lines to induce tumor cell apoptosis. Pomalidomide enhanced T cell- and natural killer (NK) cell-mediated immunity and inhibited production of pro-inflammatory cytokines (e.g., TNF-α and IL-6) by monocytes. Pomalidomide demonstrated anti-angiogenic activity in a mouse tumor model and in the in vitro umbilical cord model.
12.2 Pharmacodynamics
Pomalidomide exposure-response analyses showed that there was no relationship between systemic pomalidomide exposure level and efficacy or safety following pomalidomide dose of 4 mg.
Cardiac Electrophysiology
The QTc prolongation potential of pomalidomide was evaluated in a single center, randomized, double-blind crossover study (N=72) using 4 mg pomalidomide, 20 mg pomalidomide, placebo, and 400 mg moxifloxacin (positive control). No significant QTc prolongation effect of pomalidomide was observed following pomalidomide doses of 4 and 20 mg.
12.3 Pharmacokinetics
In patients with multiple myeloma who received POMALYST 4 mg daily alone or in combination with dexamethasone, pomalidomide steady-state drug exposure was characterized by AUC of 860 ng·h/mL (CV% = 37%) and Cmax of 75 ng/mL (CV% = 32%).
Absorption
Following administration of single oral doses of POMALYST, the maximum plasma concentration (Cmax) for pomalidomide occurs at 2 and 3 hours postdose.
Effect of Food
Co-administration of POMALYST with a high-fat meal (approximately 50% of the total caloric content) and high-calorie meal (approximately 800 to 1000 calories) (the meal contained approximately 150, 250, and 500 to 600 calories from protein, carbohydrates, and fat, respectively) delays the Tmax by 2.5 hours, decreased mean plasma Cmax and AUC in healthy volunteers by about 27% and 8%, respectively.
Distribution
Pomalidomide has a mean apparent volume of distribution (Vd/F) between 62 and 138 L at steady state.
Pomalidomide is distributed in semen of healthy subjects at a concentration of approximately 67% of plasma level at 4 hours postdose (~Tmax) after 4 days of once-daily dosing at 2 mg.
Human plasma protein binding ranges from 12% to 44% and is not concentration dependent. Pomalidomide is a substrate for P-gp.
Elimination
Pomalidomide has a mean total body clearance (CL/F) of 7-10 L/h. Pomalidomide is eliminated with a median plasma half-life of approximately 9.5 hours in healthy subjects and approximately 7.5 hours in patients with multiple myeloma.
Metabolism
Pomalidomide is primarily metabolized in the liver by CYP1A2 and CYP3A4. Minor contributions from CYP2C19 and CYP2D6 were also observed in vitro.
Excretion
Following a single oral administration of [14C]-pomalidomide to healthy subjects, approximately 73% and 15% of the radioactive dose was eliminated in urine and feces, respectively, with approximately 2% and 8% of the radiolabeled dose eliminated unchanged as pomalidomide in urine and feces.
Specific Populations
Age (61 to 85 years old), sex and race had no clinically significant effect on the systemic exposure of pomalidomide. The pharmacokinetics of pomalidomide is unknown in pediatric patients.
Renal Impairment: Pomalidomide pharmacokinetic parameters were not significantly affected in patients with moderate (30 mL/min ≤ CrCL< 60 mL/min) or severe (15 mL/min ≤ CrCL< 30 mL/min) renal impairment relative to patients with normal renal function (CrCL ≥ 60 mL/min). Mean exposure (AUC) to pomalidomide increased by 38% in patients with severe renal impairment requiring dialysis (CrCL< 30 mL/min requiring dialysis) and 40% in patients with end stage renal disease (CrCL< 15 mL/min) on non-dialysis days. In patients with severe renal impairment requiring dialysis, the estimated dialysis clearance is approximately 12 L/h which is higher than pomalidomide total body clearance, indicating hemodialysis will remove pomalidomide from the blood circulation.
Hepatic Impairment: Mean exposure (AUC) increased by 51%, 58% and 72% in subjects with mild, moderate or severe hepatic impairment as defined by Child-Pugh criteria, respectively.
Drug Interaction Studies
Co-administration of POMALYST with the following drugs did not increase pomalidomide exposure to a clinically significant extent: ketoconazole (a strong CYP3A4 and P-gp inhibitor), carbamazepine (a strong CYP3A4 inducer) and dexamethasone (a weak to moderate inducer of CYP3A4). Co-administration of POMALYST with drugs that are CYP1A2 inducers has not been studied.
CYP1A2 Inhibitors: Co-administration of fluvoxamine (a strong CYP1A2 inhibitor) with POMALYST increased mean [90% confidence interval] pomalidomide exposure by 125% [98% to 157%] compared to POMALYST alone in healthy subjects. Co-administration of fluvoxamine in the presence of ketoconazole (a strong CYP3A4 and P-gp inhibitor) with POMALYST increased mean pomalidomide exposure by 146% [126% to 167%] compared to POMALYST administered alone in healthy subjects, indicating the predominant effect of CYP1A2 inhibition in the increase of pomalidomide exposure [see Dosage and Administration (2.3) and Drug Interactions (7.1)].
Strong CYP3A4 and P-gp Inhibitors: Co-administration of ketoconazole (a strong CYP3A4 and P-gp inhibitor) in 16 healthy male subjects increased AUC of pomalidomide by 19% compared to POMALYST administered alone.
Drugs that Induce Pomalidomide Metabolism
Strong CYP1A2 Inducers: Co-administration of POMALYST with drugs that are CYP1A2 inducers has not been studied and may reduce pomalidomide exposure.
Strong CYP3A4 Inducers: Co-administration of carbamazepine to 16 healthy male subjects decreased AUC of pomalidomide by 20% with a 90% confidence interval [13% to 27%] compared to when pomalidomide was administered alone.
Dexamethasone: Co-administration of multiple doses of 4 mg POMALYST with 20 mg to 40 mg dexamethasone (a weak to moderate inducer of CYP3A4) to patients with multiple myeloma had no effect on the pharmacokinetics of pomalidomide compared to when pomalidomide was administered alone.
Smoking: In 14 healthy male subjects who smoked 25 cigarettes per day for a total of 10 days, after single oral dose of 4 mg POMALYST, Cmax of pomalidomide increased 14% while AUC of pomalidomide decreased 32%, compared to that in 13 healthy male volunteers who were non-smokers.
In Vitro Studies
Pomalidomide does not inhibit or induce CYP450 enzymes or transporters in vitro.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies examining the carcinogenic potential of pomalidomide have not been conducted. One of 12 monkeys dosed with 1 mg/kg of pomalidomide (an exposure approximately 15-fold of the exposure in patients at the recommended dose of 4 mg/day) developed acute myeloid leukemia in a 9-month repeat-dose toxicology study.
Pomalidomide was not mutagenic or clastogenic in a battery of tests, including the bacteria reverse mutation assay (Ames test), the in vitro assay using human peripheral blood lymphocytes, and the micronucleus test in orally treated rats administered doses up to 2000 mg/kg/day.
In a fertility and early embryonic development study in rats, drug-treated males were mated with untreated or treated females. Pomalidomide was administered to males and females at doses of 25 to 1000 mg/kg/day. When treated males were mated with treated females, there was an increase in post-implantation loss and a decrease in mean number of viable embryos at all dose levels. There were no other effects on reproductive functions or the number of pregnancies. The lowest dose tested in animals resulted in an exposure (AUC) approximately 100-fold of the exposure in patients at the recommended dose of 4 mg/day. When treated males in this study were mated with untreated females, all uterine parameters were comparable to the controls. Based on these results, the observed effects were attributed to the treatment of females.
-
14 CLINICAL STUDIES
14.1 Multiple Myeloma
Trial 1 was a phase 2, multicenter, randomized open-label study in patients with relapsed multiple myeloma who were refractory to their last myeloma therapy and had received lenalidomide and bortezomib. Patients were considered relapsed if they had achieved at least stable disease for at least 1 cycle of treatment to at least 1 prior regimen and then developed progressive disease. Patients were considered refractory if they experienced disease progression on or within 60 days of their last therapy. A total of 221 patients were randomized to receive POMALYST alone or POMALYST with Low-dose Dex. In Trial 1, the safety and efficacy of POMALYST 4 mg, once daily for 21 of 28 days, until disease progression, were evaluated alone and in combination with Low-dose Dex (40 mg/day given only on Days 1, 8, 15, and 22 of each 28-day cycle for patients aged 75 years or younger, or 20 mg/day given only on Days 1, 8, 15, and 22 of each 28-day cycle for patients aged greater than 75 years). Patients in the POMALYST alone arm were allowed to add Low-dose Dex upon disease progression.
Table 4 summarizes the baseline patient and disease characteristics in Trial 1. The baseline demographics and disease characteristics were balanced and comparable between the study arms.
Table 4: Baseline Demographic and Disease-Related Characteristics – Trial 1 Data cutoff: 01 April 2011 POMALYST
(n=108)POMALYST +
Low-dose Dex
(n=113)Patient Characteristics
Median age, years (range)
61 (37-88)
64 (34-88)
Age distribution, n (%)
<65 years
≥65 years
65 (60.2)
43 (39.8)
60 (53.1)
53 (46.9)Sex, n (%)
Male
Female
57 (52.8)
51 (47.2)
62 (54.9)
51 (45.1)Race/ethnicity, n (%)
White
Black or African American
All other race
86 (79.6)
16 (14.8)
6 (5.6)
92 (81.4)
17 (15)
4 (3.6)ECOG Performance, n (%)
Status 0-1
95 (87.9)
100 (88.5)Disease Characteristics Number of prior therapies
Median (min, max)
5 (2, 12)
5 (2, 13)Prior transplant, n (%) 82 (75.9) 84 (74.3) Refractory to bortezomib and lenalidomide, n (%) 64 (59.3) 69 (61.1) Table 5 summarizes the analysis results of overall response rate (ORR) and duration of response (DOR), based on assessments by the Independent Review Adjudication Committee for the treatment arms in Trial 1. ORR did not differ based on type of prior antimyeloma therapy.
Table 5: Trial 1 Results a Results are prior to the addition of dexamethasone.
b ORR = PR + CR per EBMT criteria.
CI, confidence interval; NE, not established (the median has not yet been reached).
Data cutoff: 01 April 2011POMALYST a
(n=108)POMALYST +
Low-dose Dex
(n=113)Response Overall Response Rate (ORR),b n (%) 8 (7.4) 33 (29.2) 95% CI for ORR (%) (3.3, 14.1) (21.0, 38.5) Complete Response (CR), n (%) 0 (0.0) 1 (0.9) Partial Response (PR), n (%) 8 (7.4) 32 (28.3) Duration of Response (DOR) Median, months NE 7.4 95% CI for DOR (months) NE (5.1, 9.2) Trial 2 was a Phase 3 multi-center, randomized, open-label study, where POMALYST + Low-dose Dex therapy was compared to High-dose Dex in adult patients with relapsed and refractory multiple myeloma, who had received at least two prior treatment regimens, including lenalidomide and bortezomib, and demonstrated disease progression on or within 60 days of the last therapy. Patients with creatinine clearance ≥ 45mL/min qualified for the trial. A total of 455 patients were enrolled in the trial: 302 in the POMALYST + Low-dose Dex arm and 153 in the High-dose Dex arm. Patients in the POMALYST + Low-dose Dex arm were administered 4 mg POMALYST orally on Days 1 to 21 of each 28-day cycle. Dexamethasone (40 mg) was administered once per day on Days 1, 8, 15 and 22 of a 28-day cycle. Patients > 75 years of age started treatment with 20 mg dexamethasone using the same schedule. For the High-dose Dex arm, dexamethasone (40 mg) was administered once per day on Days 1 through 4, 9 through 12, and 17 through 20 of a 28-day cycle. Patients > 75 years of age started treatment with 20 mg dexamethasone using the same schedule. Treatment continued until patients had disease progression.
Baseline patient and disease characteristics were balanced and comparable between the study arms, as summarized in Table 6. Overall, 94% of patients had disease refractory to lenalidomide, 79% had disease refractory to bortezomib and 74% had disease refractory to both lenalidomide and bortezomib.
Table 6: Baseline Demographic and Disease-Related Characteristics – Trial 2 Data cutoff: 01March 2013 POMALYST +
Low-dose Dex
(N=302)High-dose Dex
(N=153)Patient Characteristics Median Age, years (range) 64 (35, 84) 65 (35, 87) Age Distribution n (%)
< 65 years
≥ 65 years
158 (52)
144 (48)
74 (48)
79 (52)Sex n (%)
Male
Female
181 (60)
121 (40)
87 (57)
66 (43)Race/Ethnicity n (%)
White
..Black or African American
..Asian
..Other Race
Not Collected
244 (81)
4 (1)
4 (1)
2 (1)
48 (16)
113 (74)
3 (2)
0 (0)
2 (1)
35 (23)ECOG Performance n (%)
Status 0
Status 1
Status 2
Status 3
Missing
110 (36)
138 (46)
52 (17)
0 (0)
2 (1)
36 (24)
86 (56)
25 (16)
3 (2)
3 (2)Disease Characteristics Number of Prior Therapies
Median, (Min, Max)
5 (2, 14)
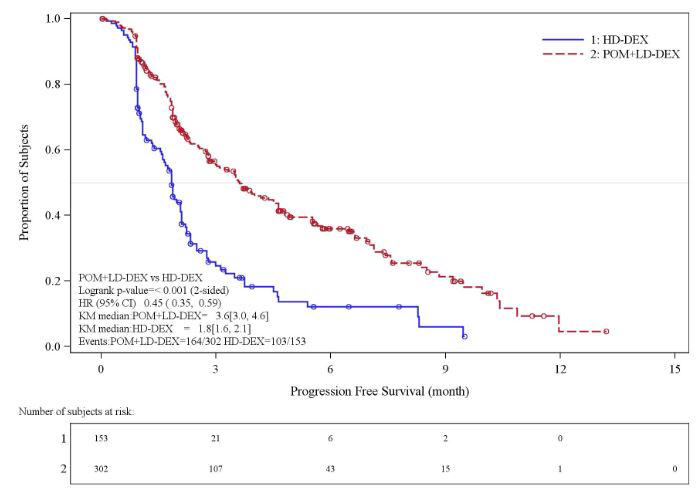
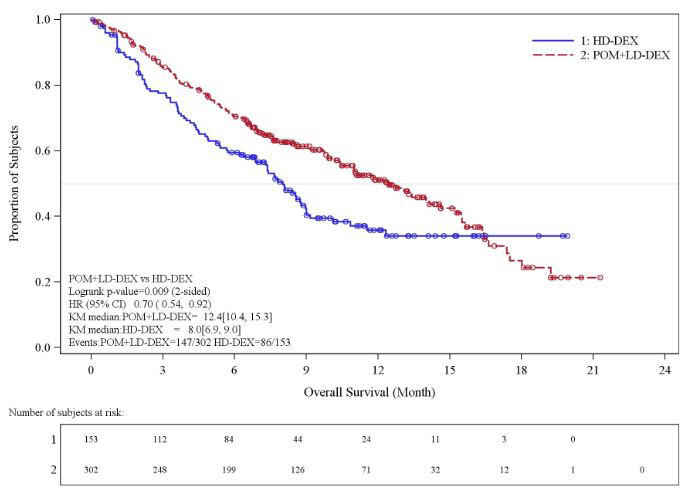
5 (2, 17)Prior stem cell transplant n (%) 214 (71) 105 (69) Refractory to bortezomib and lenalidomide n (%) 225 (75) 113 (74) Table 7 summarizes the progression free survival (PFS) and overall response rate (ORR) based on the assessment by the Independent Review Adjudication Committee (IRAC) review at the final PFS analysis and overall survival (OS) at the OS analysis. PFS was significantly longer with POMALYST + Low-dose Dex than High-dose Dex: HR 0.45 (95% CI: 0.35-0.59 p < 0.001). OS was also significantly longer with POMALYST + Low-dose Dex than High-dose Dex: HR 0.70 (95% CI: 0.54-0.92 p = 0.009). The Kaplan-Meier curves for PFS and OS for the ITT population are provided in Figures 1 and 2, respectively.
Table 7: Trial 2 Results Note: CI=Confidence interval; HD-Dex=High dose dexamethasone; IRAC=Independent Review Adjudication Committee; LD-Dex=Low dose dexamethasone.
a The median is based on Kaplan-Meier estimate.
b Based on Cox proportional hazards model comparing the hazard functions associated with treatment groups, stratified by age (≤75 vs >75), diseases population (refractory to both Lenalidomide and Bortezomib vs not refractory to both drugs), and prior number of antimyeloma therapy (=2 vs >2), stratification factors for the trial.
c The p-value is based on a stratified log-rank test with the same stratification factors as the above Cox model.
d 53% of patients in the High-dose Dex arm subsequently received POMALYST.
e Based on Cox proportional hazards model (unstratified) comparing the hazard functions associated with treatment groups.
f The p-value is based on an unstratified log-rank test.
gAlpha control for PFS and OS.
Data cutoff: 07 Sep 2012 for PFS
Data cutoff: 01 Mar 2013 for OS and ORRPOMALYST +
Low-dose Dex
(N=302)High-dose Dex
(N=153)Progression Free Survival Time Number (%) of events 164 (54.3) 103 (67.3) Mediana (2-sided 95% CI) (months) 3.6 [3.0, 4.6] 1.8 [1.6, 2.1] Hazard Ratio (Pom+LD-Dex:HD-Dex)
2-Sided 95% CIb0.45 [0.35, 0.59] Log-Rank Test 2-sided P-Valuec <0.001 Overall Survival Timed Number (%) of deaths 147 (48.7) 86 (56.2) Mediana (2-sided 95% CI) (months) 12.4 [10.4, 15.3] 8.0[6.9, 9.0] Hazard Ratio (Pom+LD-Dex:HD-Dex)
2-Sided 95% CIe0.70 [0.54, 0.92] Log-Rank Test 2-sided P-Value f, g 0.009 Overall Response Rate, n (%) 71 (23.5) 6 (3.9) Complete Response 1 (0.3) 0 Very Good Partial Response 8 (2.6) 1 (0.7) Partial Response 62 (20.5) 5 (3.3)
Figure 1: Progression Free Survival Based on IRAC Review of Response by IMWG Criteria (Stratified Log Rank Test) (ITT Population)
Data cut-off: 07 Sep 2012
Figure 2: Kaplan-Meier Curve of Overall Survival (ITT Population)
Data cutoff: 01 Mar 2013
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Dark blue opaque cap and yellow opaque body, imprinted "POML" on the cap in white ink and "1 mg" on the body in black ink
1 mg bottles of 21 (NDC: 59572-501-21)
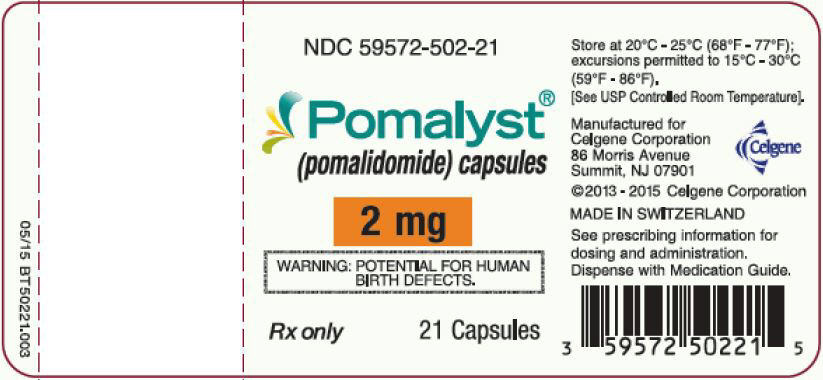
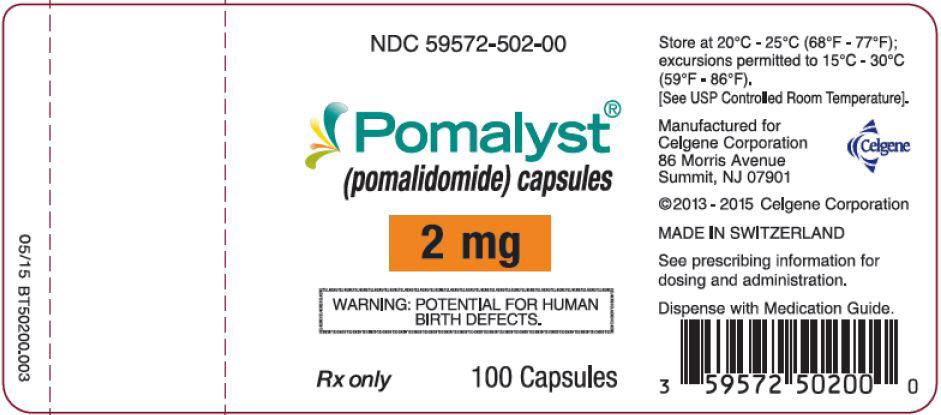
1 mg bottles of 100 (NDC: 59572-501-00)Dark blue opaque cap and orange opaque body, imprinted "POML" on the cap and "2 mg" on the body in white ink
2 mg bottles of 21 (NDC: 59572-502-21)
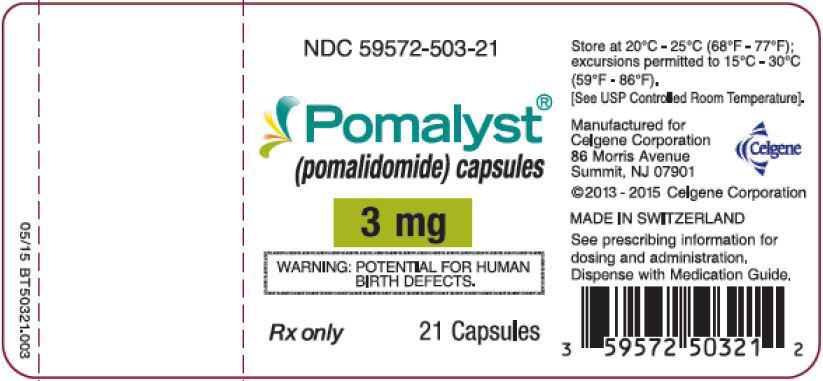
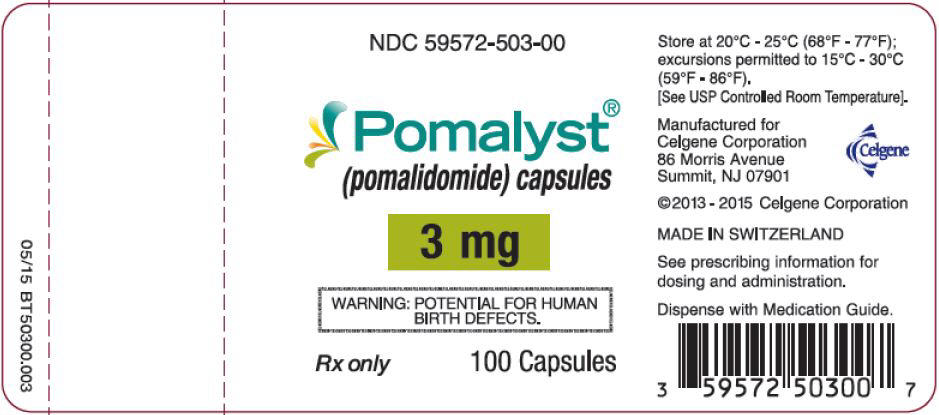
2 mg bottles of 100 (NDC: 59572-502-00)Dark blue opaque cap and green opaque body, imprinted "POML" on the cap and "3 mg" on the body in white ink
3 mg bottles of 21 (NDC: 59572-503-21)
3 mg bottles of 100 (NDC: 59572-503-00)Dark blue opaque cap and blue opaque body, imprinted "POML" on the cap and "4 mg" on the body in white ink
4 mg bottles of 21 (NDC: 59572-504-21)
4 mg bottles of 100 (NDC: 59572-504-00)16.2 Storage
Store at 20°C-25°C (68°F-77°F); excursions permitted to 15°C-30°C (59°F-86°F). [see USP Controlled Room Temperature].
16.3 Handling and Disposal
Care should be exercised in handling of POMALYST. POMALYST capsules should not be opened or crushed. If powder from POMALYST contacts the skin, wash the skin immediately and thoroughly with soap and water. If POMALYST contacts the mucous membranes, flush thoroughly with water.
Follow procedures for proper handling and disposal of anticancer drugs.1
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Embryo-Fetal Toxicity
Advise patients that POMALYST is contraindicated in pregnancy [see Boxed Warning and Contraindications (4)]. POMALYST is a thalidomide analogue and may cause serious birth defects or death to a developing baby [see Warnings and Precautions (5.1) and Use in Specific Populations (8.1)].
- Advise females of reproductive potential that they must avoid pregnancy while taking POMALYST and for at least 4 weeks after completing therapy.
- Initiate POMALYST treatment in females of reproductive potential only following a negative pregnancy test.
- Advise females of reproductive potential of the importance of monthly pregnancy tests and the need to use 2 different forms of contraception, including at least 1 highly effective form, simultaneously during POMALYST therapy, during dose interruptions, and for 4 weeks after she has completely finished taking POMALYST. Highly effective forms of contraception other than tubal ligation include IUD and hormonal (birth control pills, injections, patch, or implants) and a partner's vasectomy. Additional effective contraceptive methods include latex or synthetic condom, diaphragm, and cervical cap.
- Instruct patient to immediately stop taking POMALYST and contact her healthcare provider if she becomes pregnant while taking this drug, if she misses her menstrual period or experiences unusual menstrual bleeding, if she stops taking birth control, or if she thinks FOR ANY REASON that she may be pregnant.
- Advise patient that if her healthcare provider is not available, she should call Celgene Customer Care Center at 1-888-423-5436 [see Warnings and Precautions (5.1) and Use in Specific Populations (8.3)].
- Advise males to always use a latex or synthetic condom during any sexual contact with females of reproductive potential while taking POMALYST and for up to 4 weeks after discontinuing POMALYST, even if they have undergone a successful vasectomy.
- Advise male patients taking POMALYST that they must not donate sperm [see Warnings and Precautions (5.1) and Use in Specific Populations (8.3)].
- All patients must be instructed to not donate blood while taking POMALYST and for 4 weeks following discontinuation of POMALYST [see Warnings and Precautions (5.1)].
POMALYST REMS Program
Because of the risk of embryo-fetal toxicity, POMALYST is only available through a restricted program called POMALYST REMS [see Warnings and Precautions (5.2)].
- Patients must sign a Patient-Physician Agreement Form and comply with the requirements to receive POMALYST. In particular, females of reproductive potential must comply with the pregnancy testing, contraception requirements, and participate in monthly telephone surveys. Males must comply with the contraception requirements [see Use in Specific Populations (8.3)].
- POMALYST is available only from pharmacies that are certified in POMALYST REMS program. Provide patients with the telephone number and website for information on how to obtain the product.
Pregnancy Exposure Registry
Inform females that there is a Pregnancy Exposure Registry that monitors pregnancy outcomes in females exposed to POMALYST during pregnancy and that they can contact the Pregnancy Exposure Registry by calling 1-888-423-5436 [see Use in Specific Populations (8.1)].Venous and Arterial Thromboembolism
Inform patients of the risk of developing DVT, PE, MI, and stroke and to report immediately any signs and symptoms suggestive of these events for evaluation [see Boxed Warning and Warnings and Precautions (5.3)].Hematologic Toxicities
Inform patients on the risks of developing neutropenia, thrombocytopenia, and anemia and the need to report signs and symptoms associated with these events to their healthcare provider for further evaluation [see Warnings and Precautions (5.5)].Hepatotoxicity
Inform patients on the risks of developing hepatotoxicity, including hepatic failure and death, and to report signs and symptoms associated with these events to their healthcare provider for evaluation [see Warnings and Precautions (5.6)].Severe Cutaneous Reactions
Inform patients of the potential risk for severe skin reactions such as SJS, TEN and DRESS and to report any signs and symptoms associated with these reactions to their healthcare provider for evaluation [see Warnings and Precautions (5.7)].Dizziness and Confusional State
Inform patients of the potential risk of dizziness and confusional state with the drug, to avoid situations where dizziness or confusional state may be a problem, and not to take other medications that may cause dizziness or confusional state without adequate medical advice [see Warnings and Precautions (5.8)].Neuropathy
Inform patients of the risk of neuropathy and to report the signs and symptoms associated with these events to their healthcare provider for further evaluation [see Warnings and Precautions (5.9)].Second Primary Malignancies
Inform the patient that the potential risk of developing acute myelogenous leukemia during treatment with POMALYST is unknown [see Warnings and Precautions (5.10)].Tumor Lysis Syndrome
Inform patients of the potential risk of tumor lysis syndrome and to report any signs and symptoms associated with this event to their healthcare provider for evaluation [see Warnings and Precautions (5.11)].Hypersensitivity
Inform patients of the potential for severe hypersensitivity reactions such as angioedema and anaphylaxis to POMALYST. Instruct patients to contact their healthcare provider right away for any signs and symptoms of these reactions. Advise patients to seek emergency medical attention for signs or symptoms of severe hypersensitivity reactions [see Warnings and Precautions (5.12)].Smoking Tobacco
Advise patients that smoking tobacco may reduce the efficacy of POMALYST [see Use in Specific Populations (8.8) and Clinical Pharmacology (12.3)].Dosing Instructions
Inform patients on how to take POMALYST [see Dosage and Administration (2.1)]- POMALYST should be taken once daily at about the same time each day.
- Patients on hemodialysis should take POMALYST following hemodialysis, on hemodialysis days.
- POMALYST may be taken with or without food.
- The capsules should not be opened, broken, or chewed. POMALYST should be swallowed whole with water.
- Instruct patients that if they miss a dose of POMALYST, they may still take it up to 12 hours after the time they would normally take it. If more than 12 hours have elapsed, they should be instructed to skip the dose for that day. The next day, they should take POMALYST at the usual time. Warn patients not to take 2 doses to make up for the one that they missed.
Manufactured for: Celgene Corporation
Summit, NJ 07901
POMALYST®, REVLIMID®, THALOMID®, and POMALYST REMS® are registered trademarks of Celgene Corporation.
Pat. http://www.celgene.com/therapies
© 2005-2019 Celgene Corporation All rights reserved.
POMPI.010/MG.010
-
MEDICATION GUIDE
This Medication Guide has been approved by the U.S. Food and Drug Administration Revised: October 2019 MEDICATION GUIDE
POMALYST® (POM-uh-list)
(pomalidomide)
capsules
What is the most important information I should know about POMALYST?
Before you begin taking POMALYST, you must read and agree to all of the instructions in the POMALYST REMS® program. Before prescribing POMALYST, your healthcare provider will explain the POMALYST REMS program to you and have you sign the Patient-Physician Agreement Form.
POMALYST can cause serious side effects including:
-
Possible birth defects (deformed babies) or death of an unborn baby. Females who are pregnant or who plan to become pregnant must not take POMALYST.
POMALYST is similar to the medicine thalidomide (THALOMID). We know thalidomide can cause severe life-threatening birth defects. POMALYST has not been tested in pregnant females. POMALYST has harmed unborn animals in animal testing.
Females must not get pregnant:- For at least 4 weeks before starting POMALYST
- While taking POMALYST
- During any breaks (interruptions) in your treatment with POMALYST
- For at least 4 weeks after stopping POMALYST
Females who can become pregnant:- Will have pregnancy tests weekly for 4 weeks, then every 4 weeks if your menstrual cycle is regular, or every 2 weeks if your menstrual cycle is irregular.
If you miss your period or have unusual bleeding, you will need to have a pregnancy test and receive counseling. - Must agree to use two acceptable forms of birth control at the same time, for at least 4 weeks before, while taking, during any breaks (interruptions) in your treatment, and for at least 4 weeks after stopping POMALYST.
- Talk with your healthcare provider to find out about options for acceptable forms of birth control that you may use to prevent pregnancy before, during, and after treatment with POMALYST.
If you become pregnant while taking POMALYST, stop taking it right away and call your healthcare provider.
If your healthcare provider is not available, you can call Celgene Customer Care Center at 1-888-423-5436.
Healthcare providers and patients should report all cases of pregnancy to:- FDA MedWatch at 1-800-FDA-1088, and
- Celgene Corporation at 1-888-423-5436
There is a pregnancy exposure registry that monitors the outcomes of females who take POMALYST during pregnancy, or if their male partner takes POMALYST and they are exposed during pregnancy. You can enroll in this registry by calling Celgene Corporation at the phone number listed above.
POMALYST can pass into human semen:- Males, including those who have had a vasectomy, must always use a latex or synthetic condom during any sexual contact with a pregnant female or a female that can become pregnant while taking POMALYST, during any breaks (interruptions) in your treatment with POMALYST, and for 4 weeks after stopping POMALYST.
- Do not have unprotected sexual contact with a female who is or could become pregnant. Tell your healthcare provider if you do have unprotected sexual contact with a female who is or could become pregnant.
- Do not donate sperm while taking POMALYST, during any breaks (interruptions) in your treatment, and for 4 weeks after stopping POMALYST. If a female becomes pregnant with your sperm, the baby may be exposed to POMALYST and may be born with birth defects.
-
Blood clots in your arteries, veins, and lungs, heart attack, and stroke can happen if you take POMALYST.
Most people who take POMALYST will also take a blood thinner medicine to help prevent blood clots.
Before taking POMALYST, tell your healthcare provider:- If you have had a blood clot in the past
- If you have high blood pressure, smoke, or if you have been told you have a high level of fat in your blood (hyperlipidemia)
- About all the medicines you take. Certain other medicines can also increase your risk for blood clots
Call your healthcare provider or get medical help right away if you get any of the following during treatment with POMALYST:- Signs or symptoms of a blood clot in the lung, arm, or leg may include: shortness of breath, chest pain, or arm or leg swelling
- Signs or symptoms of a heart attack may include: chest pain that may spread to the arms, neck, jaw, back, or stomach area (abdomen), feeling sweaty, shortness of breath, feeling sick or vomiting
- Signs or symptoms of stroke may include: sudden numbness or weakness, especially on one side of the body, severe headache or confusion, or problems with vision, speech, or balance.
What is POMALYST?
POMALYST is a prescription medicine, taken along with the medicine dexamethasone, used to treat people with multiple myeloma who:
- have received at least 2 prior medicines to treat multiple myeloma, including a type of medicine known as a proteasome inhibitor and lenalidomide, and
- their disease has become worse during treatment or within 60 days of finishing the last treatment
It is not known if POMALYST is safe and effective in children.
Who should not take POMALYST?
Do not take POMALYST if you:
- are pregnant, plan to become pregnant, or become pregnant during treatment with POMALYST. See "What is the most important information I should know about POMALYST?"
- are allergic to pomalidomide or any of the ingredients in POMALYST. See the end of this Medication Guide for a complete list of ingredients in POMALYST.
What should I tell my healthcare provider before taking POMALYST?
Before you take POMALYST, tell your healthcare provider if you:
- smoke cigarettes. POMALYST may not work as well in people who smoke
- have liver problems
- have kidney problems and are receiving hemodialysis treatment
- have any other medical conditions
- are breastfeeding. You should not breastfeed during treatment with POMALYST. It is not known if POMALYST passes into your breast milk and can harm your baby.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. POMALYST and other medicines may affect each other, causing serious side effects. Talk with your healthcare provider before taking any new medicines.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist.
How should I take POMALYST?
- Take POMALYST exactly as prescribed and follow all the instructions of the POMALYST REMS program.
- Swallow POMALYST capsules whole with water 1 time a day. Do not break, chew, or open your capsules.
- POMALYST may be taken with or without food.
- Take POMALYST at about the same time each day.
- If you are on hemodialysis, take POMALYST after hemodialysis, on hemodialysis days.
- Do not open the POMALYST capsules or handle them any more than needed. If you touch a broken POMALYST capsule or the medicine in the capsule, wash the area of your body right away with soap and water.
- If you miss a dose of POMALYST and it has been less than 12 hours since your regular time, take it as soon as you remember. If it has been more than 12 hours, just skip your missed dose. Do not take 2 doses at the same time.
- If you take too much POMALYST, call your healthcare provider right away.
What should I avoid while taking POMALYST?
- See "What is the most important information I should know about POMALYST?"
- Females: Do not get pregnant and do not breastfeed while taking POMALYST.
- Males: Do not donate sperm.
- Do not share POMALYST with other people. It may cause birth defects and other serious problems.
- Do not donate blood while you take POMALYST, during any breaks (interruptions) in your treatment, and for 4 weeks after stopping POMALYST. If someone who is pregnant gets your donated blood, her baby may be exposed to POMALYST and may be born with birth defects.
- POMALYST can cause dizziness and confusion. Avoid taking other medicines that may cause dizziness and confusion during treatment with POMALYST. Avoid situations that require you to be alert until you know how POMALYST affects you.
What are the possible side effects of POMALYST?
POMALYST can cause serious side effects, including:
- See "What is the most important information I should know about POMALYST?"
- Low white blood cells (neutropenia), low platelets (thrombocytopenia), and low red blood cells (anemia) are common with POMALYST, but can also be serious. You may need a blood transfusion or certain medicines if your blood counts drop too low. Your blood counts should be checked weekly for the first 8 weeks of treatment and monthly after that.
- Severe liver problems, including liver failure and death. Your healthcare provider should do blood tests to check your liver function during your treatment with POMALYST. Tell your healthcare provider right away if you develop any of the following symptoms of liver problems:
- Yellowing of your skin or the white part of your eyes (jaundice)
- Dark or brown (tea-colored) urine
- Pain on the upper right side of your stomach area (abdomen)
- Bleeding or bruising more easily than normal
- Feeling very tired
- Severe allergic reactions and severe skin reactions can happen with POMALYST and may cause death.
Call your healthcare provider if you develop any of the following signs or symptoms during treatment with POMALYST: - a red, itchy, skin rash
- peeling of your skin or blisters
- severe itching
- fever
Get emergency medical help right away if you develop any of the following signs or symptoms during treatment with POMALYST: - swelling of your lips, mouth, tongue, or throat
- trouble breathing or swallowing
- raised red areas on your skin (hives)
- a very fast heartbeat
- you feel dizzy or faint
- Dizziness and confusion. See "What should I avoid while taking POMALYST?"
- Nerve damage. Stop taking POMALYST and call your healthcare provider if you develop symptoms of nerve damage including: numbness, tingling, pain, burning sensation in your hands, legs, or feet.
- Risk of new cancers (malignancies). New cancers, including certain blood cancers (acute myelogenous leukemia or AML) have been seen in people who received POMALYST. Talk with your healthcare provider about your risk of developing new cancers if you take POMALYST.
- Tumor lysis syndrome (TLS). TLS is caused by the fast breakdown of cancer cells. TLS can cause kidney failure and the need for dialysis treatment, abnormal heart rhythm, seizure, and sometimes death. Your healthcare provider may do blood tests to check you for TLS.
The most common side effects of POMALYST include:- tiredness and weakness
- constipation
- nausea
- diarrhea
- shortness of breath
- upper respiratory tract infection
- back pain
- fever
These are not all the possible side effects of POMALYST.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.How should I store POMALYST?
- Store POMALYST at room temperature between 68°F to 77°F (20°C to 25°C).
- Return any unused POMALYST to Celgene or your healthcare provider.
Keep POMALYST and all medicines out of the reach of children.
General information about the safe and effective use of POMALYST.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not take POMALYST for conditions for which it was not prescribed. Do not give POMALYST to other people, even if they have the same symptoms you have. It may harm them and may cause birth defects.
If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about POMALYST that is written for health professionals.
For more information, call 1-888-423-5436 or go to www.CelgeneRiskManagement.com.
What are the ingredients in POMALYST?
Active ingredient: pomalidomide
Inactive ingredients: mannitol, pregelatinized starch, and sodium stearyl fumarate.
The 1-mg capsule shell contains gelatin, titanium dioxide, FD&C blue 2, yellow iron oxide, white ink, and black ink.
The 2-mg capsule shell contains gelatin, titanium dioxide, FD&C blue 2, yellow iron oxide, FD&C red 3, and white ink.
The 3-mg capsule shell contains gelatin, titanium dioxide, FD&C blue 2, yellow iron oxide, and white ink.
The 4-mg capsule shell contains gelatin, titanium dioxide, FD&C blue 1, FD&C blue 2, and white ink.
Manufactured for: Celgene Corporation, Summit, NJ 07901
POMALYST®, REVLIMID®, THALOMID®, and POMALYST REMS® are registered trademarks of Celgene Corporation.
Pat. http://www.celgene.com/therapies © 2005-2019 Celgene Corporation All rights reserved. POMMG.010 10/2019
-
Possible birth defects (deformed babies) or death of an unborn baby. Females who are pregnant or who plan to become pregnant must not take POMALYST.
- Pomalyst® (pomalidomide) Capsules, 1 mg - 21 Count Bottle Label
- Pomalyst® (pomalidomide) Capsules, 1 mg - 100 Count Bottle Label
- Pomalyst® (pomalidomide) Capsules, 2 mg - 21 Count Bottle Label
- Pomalyst® (pomalidomide) Capsules, 2 mg - 100 Count Bottle Label
- Pomalyst® (pomalidomide) Capsules, 3 mg - 21 Count Bottle Label
- Pomalyst® (pomalidomide) Capsules, 3 mg - 100 Count Bottle Label
- Pomalyst® (pomalidomide) Capsules, 4 mg - 21 Count Bottle Label
- Pomalyst® (pomalidomide) Capsules, 4 mg - 100 Count Bottle Label
-
INGREDIENTS AND APPEARANCE
POMALYST
pomalidomide capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59572-501 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength POMALIDOMIDE (UNII: D2UX06XLB5) (POMALIDOMIDE - UNII:D2UX06XLB5) POMALIDOMIDE 1 mg Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) STARCH, CORN (UNII: O8232NY3SJ) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) Product Characteristics Color YELLOW, BLUE Score no score Shape CAPSULE Size 14mm Flavor Imprint Code POML;1;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59572-501-21 21 in 1 BOTTLE; Type 0: Not a Combination Product 02/18/2013 2 NDC: 59572-501-00 100 in 1 BOTTLE; Type 0: Not a Combination Product 02/18/2013 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA204026 02/18/2013 POMALYST
pomalidomide capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59572-502 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength POMALIDOMIDE (UNII: D2UX06XLB5) (POMALIDOMIDE - UNII:D2UX06XLB5) POMALIDOMIDE 2 mg Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) STARCH, CORN (UNII: O8232NY3SJ) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) Product Characteristics Color ORANGE, BLUE Score no score Shape CAPSULE Size 18mm Flavor Imprint Code POML;2;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59572-502-21 21 in 1 BOTTLE; Type 0: Not a Combination Product 02/18/2013 2 NDC: 59572-502-00 100 in 1 BOTTLE; Type 0: Not a Combination Product 02/18/2013 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA204026 02/18/2013 POMALYST
pomalidomide capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59572-503 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength POMALIDOMIDE (UNII: D2UX06XLB5) (POMALIDOMIDE - UNII:D2UX06XLB5) POMALIDOMIDE 3 mg Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) STARCH, CORN (UNII: O8232NY3SJ) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) Product Characteristics Color GREEN, BLUE Score no score Shape CAPSULE Size 18mm Flavor Imprint Code POML;3;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59572-503-21 21 in 1 BOTTLE; Type 0: Not a Combination Product 02/18/2013 2 NDC: 59572-503-00 100 in 1 BOTTLE; Type 0: Not a Combination Product 02/18/2013 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA204026 02/18/2013 POMALYST
pomalidomide capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59572-504 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength POMALIDOMIDE (UNII: D2UX06XLB5) (POMALIDOMIDE - UNII:D2UX06XLB5) POMALIDOMIDE 4 mg Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) STARCH, CORN (UNII: O8232NY3SJ) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) Product Characteristics Color BLUE, BLUE Score no score Shape CAPSULE Size 18mm Flavor Imprint Code POML;4;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59572-504-21 21 in 1 BOTTLE; Type 0: Not a Combination Product 02/18/2013 2 NDC: 59572-504-00 100 in 1 BOTTLE; Type 0: Not a Combination Product 02/18/2013 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA204026 02/18/2013 Labeler - Celgene Corporation (174201137)
Trademark Results [Pomalyst]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 POMALYST 85885565 4388257 Live/Registered |
Celgene Corporation 2013-03-25 |
 POMALYST 85150878 3980998 Live/Registered |
Celgene Corporation 2010-10-12 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.