BIMATOPROST solution/ drops
bimatoprost by
Drug Labeling and Warnings
bimatoprost by is a Prescription medication manufactured, distributed, or labeled by Alembic Pharmaceuticals Limited, Alembic Pharmaceuticals Limited (F3). Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use BIMATOPROST OPHTHALMIC SOLUTION safely and effectively. See full prescribing information for BIMATOPROST OPHTHALMIC SOLUTION.
BIMATOPROST ophthalmic solution for topical ophthalmic use.
Initial U.S. Approval: 2001INDICATIONS AND USAGE
Bimatoprost ophthalmic solution, for topical ophthalmic use is a prostaglandin analog, indicated to treat hypotrichosis of the eyelashes by increasing their growth including length, thickness and darkness. (1)
DOSAGE AND ADMINISTRATION
Apply nightly directly to the skin of the upper eyelid margin at the base of the eyelashes using the accompanying applicators. Blot any excess solution beyond the eyelid margin. Dispose of the applicator after one use. Repeat for the opposite eyelid margin using a new sterile applicator. (2)
DOSAGE FORMS AND STRENGTHS
Ophthalmic solution containing bimatoprost 0.3 mg/mL. (3)
CONTRAINDICATIONS
Hypersensitivity (4)
WARNINGS AND PRECAUTIONS
Concurrent administration of Bimatoprost ophthalmic solution, for topical ophthalmic use and intraocular pressure (IOP)-lowering prostaglandin analogs in ocular hypertensive patients may decrease the IOP-lowering effect. Patients using these products concomitantly should be closely monitored for changes to their IOP. (5.1)
Pigmentation of the eyelids and iris may occur. Iris pigmentation is likely to be permanent. (5.2,5.3)ADVERSE REACTIONS
Most common adverse reactions (incidence approximately 3% to 4%) are eye pruritus, conjunctival hyperemia, and skin hyperpigmentation. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Alembic Pharmaceutical Inc. at 1-866-210-9797 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatchSee 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 7/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Effects on Intraocular Pressure
5.2 Iris Pigmentation
5.3 Lid Pigmentation
5.4 Hair Growth Outside the Treatment Area
5.5 Intraocular Inflammation
5.6 Macular Edema
5.7 Contamination of bimatoprost ophthalmic solution 0.03% or Applicator
5.8 Use with Contact Lenses
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis and Mutagenesis and Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
Ensure the face is clean, makeup and contact lenses are removed. Once nightly, place one drop of bimatoprost ophthalmic solution, 0.03% on the disposable sterile applicator supplied with the package and apply evenly along the skin of the upper eyelid margin at the base of the eyelashes. The upper lid margin in the area of lash growth should feel lightly moist without runoff. Blot any excess solution runoff outside the upper eyelid margin with a tissue or other absorbent cloth. Dispose of the applicator after one use. Repeat for the opposite eyelid margin using a new sterile applicator.
Do not reuse applicators and do not use any other brush/applicator to apply bimatoprost ophthalmic solution 0.03%.
Do not apply to the lower eyelash line [see Warnings and Precautions (5.3, 5.4 ] and Patient Counseling Information (17)].
Additional applications of bimatoprost ophthalmic solution 0.03% will not increase the growth of eyelashes.
Upon discontinuation of treatment, eyelash growth is expected to return to its pre-treatment level. - 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Effects on Intraocular Pressure
Bimatoprost ophthalmic solution (LUMIGAN®) lowers intraocular pressure (IOP) when instilled directly to the eye in patients with elevated IOP. In clinical trials, in patients with or without elevated IOP, bimatoprost ophthalmic solution 0.03% lowered IOP, however, the magnitude of the reduction was not cause for clinical concern.
In ocular hypertension studies with LUMIGAN®, it has been shown that exposure of the eye to more than one dose of bimatoprost daily may decrease the intraocular pressure lowering effect. In patients using LUMIGAN® or other prostaglandin analogs for the treatment of elevated intraocular pressure, the concomitant use of bimatoprost ophthalmic solution 0.03% may interfere with the desired reduction in IOP. Patients using prostaglandin analogs including LUMIGAN® for IOP reduction should only use bimatoprost ophthalmic solution 0.03% after consulting with their physician and should be monitored for changes to their intraocular pressure.5.2 Iris Pigmentation
Increased iris pigmentation has occurred when bimatoprost solution was administered. Patients should be advised about the potential for increased brown iris pigmentation which is likely to be permanent [see Adverse Reactions (6.2] .
The pigmentation change is due to increased melanin content in the melanocytes rather than to an increase in the number of melanocytes. The long term effects of increased pigmentation are not known. Iris color changes seen with administration of bimatoprost ophthalmic solution may not be noticeable for several months to years. Typically, the brown pigmentation around the pupil spreads concentrically towards the periphery of the iris and the entire iris or parts of the iris become more brownish. Neither nevi nor freckles of the iris appear to be affected by treatment. Treatment with bimatoprost ophthalmic solution 0.03% can be continued in patients who develop noticeably increased iris pigmentation.5.3 Lid Pigmentation
Bimatoprost has been reported to cause pigment changes (darkening) to periorbital pigmented tissues and eyelashes. The pigmentation is expected to increase as long as bimatoprost is administered, but has been reported to be reversible upon discontinuation of bimatoprost in most patients.
5.4 Hair Growth Outside the Treatment Area
There is the potential for hair growth to occur in areas where bimatoprost ophthalmic solution 0.03% comes in repeated contact with the skin surface. It is important to apply bimatoprost ophthalmic solution 0.03% only to the skin of the upper eyelid margin at the base of the eyelashes using the accompanying sterile applicators, and to carefully blot any excess bimatoprost ophthalmic solution 0.03% from the eyelid margin to avoid it running onto the cheek or other skin areas.
5.5 Intraocular Inflammation
Bimatoprost ophthalmic solution 0.03% should be used with caution in patients with active intraocular inflammation (e.g., uveitis) because the inflammation may be exacerbated.
5.6 Macular Edema
Macular edema, including cystoid macular edema, has been reported during treatment with bimatoprost ophthalmic solution (LUMIGAN®) for elevated IOP. Bimatoprost ophthalmic solution 0.03% should be used with caution in aphakic patients, in pseudophakic patients with a torn posterior lens capsule, or in patients with known risk factors for macular edema.
5.7 Contamination of bimatoprost ophthalmic solution 0.03% or Applicator
The Bimatoprost ophthalmic solution 0.03% bottle must be kept intact during use. It is important to use bimatoprost ophthalmic solution 0.03% as instructed, by placing one drop on the single-use- per-eye applicator. The bottle tip should not be allowed to contact any other surface since it could become contaminated. The accompanying sterile applicators should only be used on one eye and then discarded since reuse of applicators increases the potential for contamination and infections. There have been reports of bacterial keratitis associated with the use of multiple-dose containers of topical ophthalmic products [see Patient Counseling Information (17)].
-
6 ADVERSE REACTIONS
The following adverse reactions are described elsewhere in the labeling:
- Effects on Intraocular Pressure [see Warnings and Precautions (5.1)]
- Iris Pigmentation [see Warnings and Precautions (5.2)]
- Lid Pigmentation [see Warnings and Precautions (5.3)]
- Hair Growth Outside the Treatment Area [see Warnings and Precautions (5.4)]
- Intraocular Inflammation [see Warnings and Precautions (5.5)]
- Macular Edema [see Warnings and Precautions (5.6)]
- Hypersensitivity [see Contraindications (4)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The following information is based on clinical trial results from a multicenter, double-masked, randomized, vehicle-controlled, parallel study including 278 adult patients for four months of treatment.The most frequently reported adverse reactions were eye pruritus, conjunctival hyperemia, skin hyperpigmentation, ocular irritation, dry eye symptoms, and periorbital erythema. These reactions occurred in less than 4% of patients. Additional adverse reactions seen in clinical trials experience include foreign body sensation, hair growth abnormal, and iris hyperpigmentation.
Additional adverse reactions reported with bimatoprost ophthalmic solution (LUMIGAN®) for the reduction of intraocular pressure include, ocular dryness, visual disturbance, ocular burning, eye pain, blepharitis, cataract, superficial punctate keratitis, eye discharge, tearing, photophobia, allergic conjunctivitis, asthenopia, conjunctival edema, iritis, infections (primarily colds and upper respiratory tract infections), headaches, and asthenia.6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of bimatoprost ophthalmic solution 0.03%. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The reactions include dry skin of the eyelid and/or periocular area, eye swelling, eyelid edema, hordeolum, hypersensitivity (local allergic reactions), lacrimation increased, madarosis and trichorrhexis (temporary loss of a few lashes to loss of sections of eyelashes, and temporary eyelash breakage, respectively), periorbital and lid changes associated with periorbital fat atrophy and skin tightness resulting in deepening of eyelid sulcus and eyelid ptosis, rash (including macular and erythematous), skin discoloration (periorbital), skin exfoliation of the eyelid and/or periorbital area, trichiasis, and vision blurred.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate and well-controlled studies of bimatoprost ophthalmic solution 0.03% administration in pregnant women. There is no increase in the risk of major birth defects or miscarriages based on bimatoprost postmarketing experience.
In embryofetal development studies, administration of bimatoprost to pregnant mice and rats during organogenesis resulted in abortion and early delivery at oral doses at least 33 times (mice) or 94 times (rats) the human exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily, based on the area under the curve (AUC). These adverse effects were not observed at 2.6 times (mice) and 47 times (rats) the human exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily, based on AUC.
In pre/postnatal development studies, administration of bimatoprost to pregnant rats from organogenesis to the end of lactation resulted in reduced gestation length and fetal body weight, and increased fetal and pup mortality at oral doses at least 41 times the human systemic exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily, based on AUC. No adverse effects were observed in rat offspring at exposures estimated at 14 times the human exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily, based on AUC.
Because animal reproductive studies are not always predictive of human response bimatoprost ophthalmic solution 0.03% should be administered during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Data
Animal Data
In an embryofetal development rat study, abortion was observed in pregnant rats administered bimatoprost orally during organogenesis at 0.6 mg/kg/day (94 times the human systemic exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily , based on AUC). The No Observed Adverse Effect Level (NOAEL) for abortion was 0.3 mg/kg/day (estimated at 47 times the human systemic exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily based on AUC). No abnormalities were observed in rat fetuses at doses up to 0.6 mg/kg/day.
In an embryofetal development mouse study, abortion and early delivery were observed in pregnant mice administered bimatoprost orally during organogenesis at doses greater than or equal to 0.3 mg/kg/day (33 times the human systemic exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily , based on AUC). The NOAEL for abortion and early delivery was 0.1 mg/kg/day (2.6 times the human systemic exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily, based on AUC) . No abnormalities were observed in mouse fetuses at doses up to 0.6 mg/kg/day (72 times the human systemic exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily, based on AUC).
In a pre/postnatal development study, treatment of pregnant rats with bimatoprost orally from gestation day 7 to lactation day 20 resulted in reduced gestation length, increased late resorptions, fetal deaths, and postnatal pup mortality, and reduced pup body weight at doses greater than or equal to 0.3 mg/kg/day. These effects were observed at exposures at least 41 times the human systemic exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily, based on AUC). The NOAEL for postnatal development and mating performance of the offspring was 0.1 mg/kg/day (estimated at 14 times the human systemic exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily, based on AUC).
8.2 Lactation
Risk Summary
It is not known whether topical ocular treatment with bimatoprost ophthalmic solution 0.03% could result in sufficient systemic absorption to produce detectable quantities in human milk. In animal studies, bimatoprost has been shown to be present in breast milk of lactating rats at an intravenous dose (i.e., 1 mg/kg) 324 times the recommended human ophthalmic dose (on a mg/m2 basis), however no animal data is available at clinically relevant doses.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for bimatoprost ophthalmic solution 0.03% and any potential adverse effects on the breastfed child from bimatoprost ophthalmic solution 0.03%.
8.4 Pediatric Use
Use of bimatoprost ophthalmic solution 0.03% was evaluated in a sixteen-week double-masked, randomized, vehicle-controlled study conducted in pediatric patients who were post-chemotherapy or had alopecia areata, and adolescents who had hypotrichosis with no associated medical condition. No new safety issues were observed. The results of the Global Eyelash Assessment (GEA) are provided in Table 1.
Table 1. Number (%) of subjects with at least a 1-grade increase from baseline at month 4 in Global Eyelash Assessment
Age Range
(years)
Bimatoprost ophthalmic solution 0.03%
Vehicle
Difference (95% CI)
Adolescents with hypotrichosis (N=40)
15-17
19/26 (73%)
1/14 (7%)
66% (44%, 88%)
Post Chemotherapy Pediatric Patients (N=16)
5-17
11/13 (85%)
3/3 (100%)
-15% (-35%, 4%)
Alopecia Areata Pediatric Patients (N=15)
5-17
4/9 (44%)
2/6 (33%)
11% (-39%, 61%) -
11 DESCRIPTION
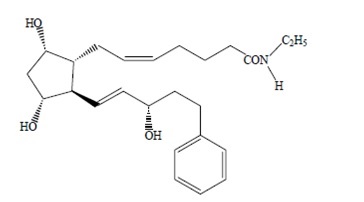
Bimatoprost ophthalmic solution, 0.03% is a synthetic prostaglandin analog. Its chemical name is (Z)-7-[(1R, 2R, 3R, 5S)-3, 5-Dihydroxy-2-[(1E, 3S)-3-hydroxy-5-phenyl-1pentenyl] cyclopentenyl]-5-N-ethylheptenamide, and its molecular weight is 415.58. Its molecular formula is C25H37NO4. Its chemical structure is:
Bimatoprost is a powder, which is soluble in methanol and alcohol. Bimatoprost ophthalmic solution 0.03% is clear, isotonic, colorless, sterile ophthalmic solution with an osmolality of approximately 290 mOsmol/kg.
Bimatoprost Ophthalmic Solution 0.03% contains: Active: bimatoprost 0.3 mg/mL; Preservative: benzalkonium chloride 0.05 mg/mL; Inactives: sodium chloride; sodium phosphate, dibasic; citric acid; and water for injection. Sodium hydroxide and/or hydrochloric acid may be added to adjust pH. The pH during its shelf-life ranges from 6.8 to7.8.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Bimatoprost is a structural prostaglandin analog. Although the precise mechanism of action is unknown, the growth of eyelashes is believed to occur by increasing the percent of hairs in, and the duration of the anagen or growth phase.
12.3 Pharmacokinetics
Absorption
After one drop of bimatoprost ophthalmic solution 0.03% was administered once daily into both eyes (cornea and/or conjunctival sac) of 15 healthy subjects for two weeks, blood concentrations peaked within 10 minutes after dosing and were below the lower limit of detection (0.025 ng/mL) in most subjects within 1.5 hours after dosing. Mean Cmax and AUC0-24hr values were similar on days 7 and 14 at approximately 0.08 ng/mL and 0.09 ng●hr/mL, respectively, indicating that steady state was reached during the first week of ocular dosing. There was no significant systemic drug accumulation over time.
Distribution
Bimatoprost is moderately distributed into body tissues with a steady-state volume of distribution of 0.67 L/kg. In human blood, bimatoprost resides mainly in the plasma. Approximately 12% of bimatoprost remains unbound in human plasma.
Elimination
Metabolism
Bimatoprost is the major circulating species in the blood once it reaches the systemic circulation. Bimatoprost then undergoes oxidation, N-deethylation, and glucuronidation to form a diverse variety of metabolites.Excretion
Following an intravenous dose of radiolabeled bimatoprost (3.12 mcg/kg) to six healthy subjects, the maximum blood concentration of unchanged drug was 12.2 ng/mL and decreased rapidly with an elimination half-life of approximately 45 minutes. The total blood clearance of bimatoprost was 1.5 L/hr/kg. Up to 67% of the administered dose was excreted in the urine while 25% of the dose was recovered in the feces.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis and Mutagenesis and Impairment of Fertility
Carcinogenesis
Bimatoprost was not carcinogenic in either mice or rats when administered by oral gavage for 104 weeks at doses of up to 2 mg/kg/day and 1 mg/kg/day respectively (approximately 192 and 291 times the human systemic exposure following topical administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily based on blood AUC levels).
Mutagenesis
Bimatoprost was not mutagenic or clastogenic in the Ames test, in the mouse lymphoma test, or in the in vivo mouse micronucleus tests.Impairment of Fertility
Bimatoprost did not impair fertility in male or female rats up to doses of 0.6 mg/kg/day(103 times the human systemic exposure following topical ophthalmic administration of bimatoprost 0.03% to the cornea or conjunctival sac bilaterally once daily based on blood AUC levels). -
14 CLINICAL STUDIES
Bimatoprost ophthalmic solution, 0.03% was evaluated for its effect on overall eyelash prominence in a multicenter, double-masked, randomized, vehicle-controlled, parallel study including 278 adult patients for four months of treatment. The primary efficacy endpoint in this study was an increase in overall eyelash prominence as measured by at least a 1-grade increase on the 4-point Global Eyelash Assessment (GEA) scale, from baseline to the end of the treatment period (week 16). Bimatoprost ophthalmic solution, 0.03% was more effective than vehicle as measured by the GEA score, with statistically significant differences seen at 8-week, 12-week, and 16-week (primary endpoint) treatment durations.
Table 2 Number (%) of subjects with at least a 1-grade increase from baseline in Global Eyelash Assessment (Primary Efficacy Endpoint – Week 16)
Week
Bimatoprost ophthalmic solution, 0.03%
N=137
N (%)
Vehicle
N= 141
N (%)
1
7 (5%)
3 (2%)
4
20 (15%)
11 (8%)
8
69 (50%)
21 (15%)
12
95 (69%)
28 (20%)
16
107 (78%)
26 (18%)
20
103 (79%)
27 (21%)
In this study, patients were also evaluated for the effect of bimatoprost ophthalmic solution, 0.03% on the length, thickness and darkness of their eyelashes. Improvements from baseline in eyelash growth as measured by digital image analysis assessing eyelash length, fullness/thickness, and darkness were statistically significantly more pronounced in the bimatoprost group at weeks 8, 12, and 16.
Table 3
Efficacy endpoint at Week 16
(Mean Change from Baseline)
Bimatoprost ophthalmic solution 0.03%
Vehicle
Eyelash growth (length) (mm; % increase)
N=137
1.4; 25%
N=141
0.1; 2%
Fullness/thickness (mm2; % increase)
N=136
0.7; 106%
N=140
0.1; 12%
Eyelash darkness (intensity*; % increase in darkness)
N=135
-20.2; -18%
N=138
-3.6;-3%
* a negative value is representative of eyelash darkening
After the 16-week treatment period, a 4-week post-treatment period followed during which the effects of bimatoprost started to return toward baseline. The effect on eyelash growth is expected to abate following longer term discontinuation.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Bimatoprost ophthalmic solution, 0.03% is supplied sterile in opaque white low-density polyethylene round screw neck bottle and tips with high density polyethylene turquoise opaque screw cap accompanied by sterile, disposable applicators:
5 mL in a 5 mL bottle with 140 applicators NDC: 46708-511-05
3 mL in a 5 mL bottle with 70 applicators NDC: 46708-511-03Storage: Store at 2° to 25°C (36° to 77°F).
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information)
Nightly Application
Inform patients that bimatoprost ophthalmic solution, 0.03% should be applied every night using only the accompanying sterile applicators. They should start by ensuring their face is clean, all makeup is removed, and their contact lenses removed (if applicable). Then, carefully place one drop of bimatoprost ophthalmic solution, 0.03% on the disposable sterile applicator and brush cautiously along the skin of the upper eyelid margin at the base of the eyelashes. If any bimatoprost ophthalmic solution, 0.03% gets into the eye proper, it will not cause harm. The eye should not be rinsed.Additional applications of bimatoprost ophthalmic solution, 0.03% will not increase the growth of eyelashes.
Inform patients not to apply to the lower eyelash line. Any excess solution outside the upper eyelid margin should be blotted with a tissue or other absorbent material.
The onset of effect is gradual but is not significant in the majority of patients until 2 months. Counsel patients that the effect is not permanent and can be expected to gradually return to the original level upon discontinuation of treatment with bimatoprost ophthalmic solution, 0.03%.
Handling the Bottle and Applicator
Instruct patients that the bimatoprost ophthalmic solution, 0.03% bottle must be maintained intact and to avoid allowing the tip of the bottle or applicator to contact surrounding structures, fingers, or any other unintended surface in order to avoid contamination of the bottle or applicator by common bacteria known to cause ocular infections. Instruct patients to only use the applicator supplied with the product once and then discard since reuse could result in using a contaminated applicator. Serious infections may result from using contaminated solutions or applicators.
Potential for Intraocular Pressure Effects
Bimatoprost ophthalmic solution, 0.03% may lower intraocular pressure although not to a level that will cause clinical harm.In patients using LUMIGAN® or other prostaglandin analogs for the treatment of elevated intraocular pressure, the concomitant use of bimatoprost ophthalmic solution, 0.03% may interfere with the desired reduction in IOP. Patients using prostaglandin analogs for IOP reduction should only use bimatoprost ophthalmic solution, 0.03% after consulting with their physician.
Potential for Eyelid Skin Darkening
Inform patients about the possibility of eyelid skin darkening, which may be reversible after discontinuation of bimatoprost ophthalmic solution, 0.03%.Potential for Iris Darkening
Advise patients about the potential for increased brown iris pigmentation which is likely to be permanent. Increased iris pigmentation has occurred when bimatoprost solution was administered.Potential for Unexpected Hair Growth or Eyelash Changes
Inform patients of the possibility of hair growth occurring outside of the target treatment area if bimatoprost ophthalmic solution, 0.03% repeatedly touches the same area of skin outside the treatment area. They should also be informed of the possibility of disparity between eyes in length, thickness, pigmentation, number of eyelashes or vellus hairs, and/or direction of eyelash growth. Eyelash changes are likely reversible upon discontinuation of treatment.When to Seek Physician Advice
Advise patients that if they develop a new ocular condition (e.g., trauma or infection), experience a sudden decrease in visual acuity, have ocular surgery, or develop any ocular reactions, particularly conjunctivitis and eyelid reactions, they should immediately seek their physician’s advice concerning the continued use of bimatoprost ophthalmic solution, 0.03%. Patients on IOP-lowering medications should not use bimatoprost ophthalmic solution, 0.03% without prior consultation with their physician.Contact Lens Use
Advise patients that bimatoprost ophthalmic solution, 0.03% contains benzalkonium chloride, which may be absorbed by and cause discoloration of soft contact lenses. Contact lenses should be removed prior to application of bimatoprost ophthalmic solution, 0.03% and may be reinserted 15 minutes following its administration.
Manufactured by:
Alembic Pharmaceuticals Limited
Karakhadi - 391 450, Gujarat, India.
PATIENT INFORMATION
Bimatoprost Ophthalmic solution, 0.03%.
(bih MAT o prost)Read the Patient Information that comes with bimatoprost ophthalmic solution, 0.03% before you start using it and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your physician about your treatment.
What is hypotrichosis of the eyelashes?
Hypotrichosis is another name for having inadequate or not enough eyelashes.What is bimatoprost ophthalmic solution 0.03%?
Bimatoprost ophthalmic solution 0.03% is a prescription treatment for hypotrichosis used to grow eyelashes, making them longer, thicker and darker.
Who should NOT take bimatoprost ophthalmic solution 0.03%?
Do not use bimatoprost ophthalmic solution 0.03% if you are allergic to one of its ingredients.
Are there any special warnings associated with bimatoprost ophthalmic solution 0.03% use?
Bimatoprost ophthalmic solution 0.03% is intended for use on the skin of the upper eyelid margins at the base of the eyelashes. Refer to Illustration 2 below. DO NOT APPLY to the lower eyelid. If you are using LUMIGAN®, or other products in the same class for elevated intraocular pressure (IOP), or if you have a history of abnormal IOP, you should only use bimatoprost ophthalmic solution 0.03% under the close supervision of your physician.
Bimatoprost ophthalmic solution 0.03% use may cause darkening of the eyelid skin which may be reversible. Bimatoprost ophthalmic solution 0.03% use may also cause increased brown pigmentation of the colored part of the eye which is likely to be permanent.
It is possible for hair growth to occur in other areas of your skin that bimatoprost ophthalmic solution 0.03% frequently touches. Any excess solution outside the upper eyelid margin should be blotted with a tissue or other absorbent material to reduce the chance of this from happening. It is also possible for a difference in eyelash length, thickness, fullness, pigmentation, number of eyelash hairs, and/or direction of eyelash growth to occur between eyes. These differences, should they occur, will usually go away if you stop using bimatoprost ophthalmic solution 0.03%.
Who should I tell that I am using bimatoprost ophthalmic solution 0.03%?
You should tell your physician you are using bimatoprost ophthalmic solution 0.03% especially if you have a history of eye pressure problems.
You should also tell anyone conducting an eye pressure screening that you are using bimatoprost ophthalmic solution 0.03%.
What should I do if I get bimatoprost ophthalmic solution 0.03% in my eye?
Bimatoprost ophthalmic solution 0.03% is an ophthalmic drug product. Bimatoprost ophthalmic solution 0.03% is not expected to cause harm if it gets into the eye proper. Do not attempt to rinse your eye in this situation.
What are the possible side effects of bimatoprost ophthalmic solution 0.03%?
The most common side effects after using bimatoprost ophthalmic solution 0.03% solution are an itching sensation in the eyes and/or eye redness. This was reported in approximately 4% of patients. Bimatoprost ophthalmic solution 0.03% solution may cause other less common side effects which typically occur on the skin close to where bimatoprost ophthalmic solution 0.03% is applied, or in the eyes. These include skin darkening, eye irritation, dryness of the eyes, and redness of the eyelids.If you develop a new ocular condition (e.g., trauma or infection), experience a sudden decrease in visual acuity, have ocular surgery, or develop any ocular reactions, particularly conjunctivitis and eyelid reactions, you should immediately seek your physician’s advice concerning the continued use of bimatoprost ophthalmic solution 0.03% solution.
What happens if I stop using bimatoprost ophthalmic solution 0.03%?
If you stop using bimatoprost ophthalmic solution 0.03%, your eyelashes are expected to return to their previous appearance over several weeks to months.
Any eyelid skin darkening is expected to reverse after several weeks to months.Any darkening of the colored part of the eye known as the iris is NOT expected to reverse and is likely permanent.
How do I use bimatoprost ophthalmic solution 0.03%?
The recommended dosage is one application nightly to the skin of the upper eyelid margin at the base of the eyelashes only.
Once nightly, start by ensuring your face is clean, makeup and contact lenses are removed. Remove an applicator from its tray. Then, holding the sterile applicator horizontally, place one drop of bimatoprost ophthalmic solution 0.03% on the area of the applicator closest to the tip but not on the tip (see Illustration 1). Then immediately draw the applicator carefully across the skin of the upper eyelid margin at the base of the eyelashes (where the eyelashes meet the skin) going from the inner part of your lash line to the outer part (see Illustration 2). Blot any excess solution beyond the eyelid margin. Dispose of the applicator after one use.
Repeat for the opposite upper eyelid margin using a new sterile applicator. This helps minimize any potential for contamination from one eyelid to another.

Illustration 1

Illustration 2
DO NOT APPLY in your eye or to the lower lid. ONLY use the sterile applicators supplied with bimatoprost ophthalmic solution 0.03% to apply the product. If you miss a dose, don't try to "catch up." Just apply bimatoprost ophthalmic solution 0.03% the next evening. Fifty percent of patients treated with bimatoprost ophthalmic solution 0.03% in a clinical study saw significant improvement by 2 months after starting treatment.
If any bimatoprost ophthalmic solution 0.03% gets into the eye proper, it is not expected to cause harm. The eye should not be rinsed.
Don't allow the tip of the bottle or applicator to contact surrounding structures, fingers, or any other unintended surface in order to avoid contamination by common bacteria known to cause infections.
Contact lenses should be removed prior to application of bimatoprost ophthalmic solution 0.03% and may be reinserted 15 minutes following its administration.
Use of bimatoprost ophthalmic solution 0.03% more than once a day will not increase the growth of eyelashes more than use once a day.
Store bimatoprost ophthalmic solution 0.03% at 2° to 25 °C ( 36° to 77 °F).
General Information about bimatoprost ophthalmic solution 0.03%.
Prescription treatments are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use bimatoprost ophthalmic solution 0.03% for a condition for which it was not prescribed. Do not give bimatoprost ophthalmic solution 0.03% to other people. It may not be appropriate for them to use.This leaflet summarizes the most important information about bimatoprost ophthalmic solution 0.03%. If you would like more information, talk with your physician. You can also call Alembic at 1-866-210-9797.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.What are the ingredients in bimatoprost ophthalmic solution 0.03%?
Active ingredient: bimatoprost
Inactive ingredients: benzalkonium chloride; sodium chloride; sodium phosphate, dibasic; citric acid; and water for injection. Sodium hydroxide and/or hydrochloric acid may be added to adjust pH. The pH during its shelf life ranges from 6.8 to 7.8.
Manufactured by:
Alembic Pharmaceuticals Limited
Karakhadi - 391 450, Gujarat, India.LUMIGAN® is registered trademark of Allergan, Inc.
- PATIENT PACKAGE INSERT
-
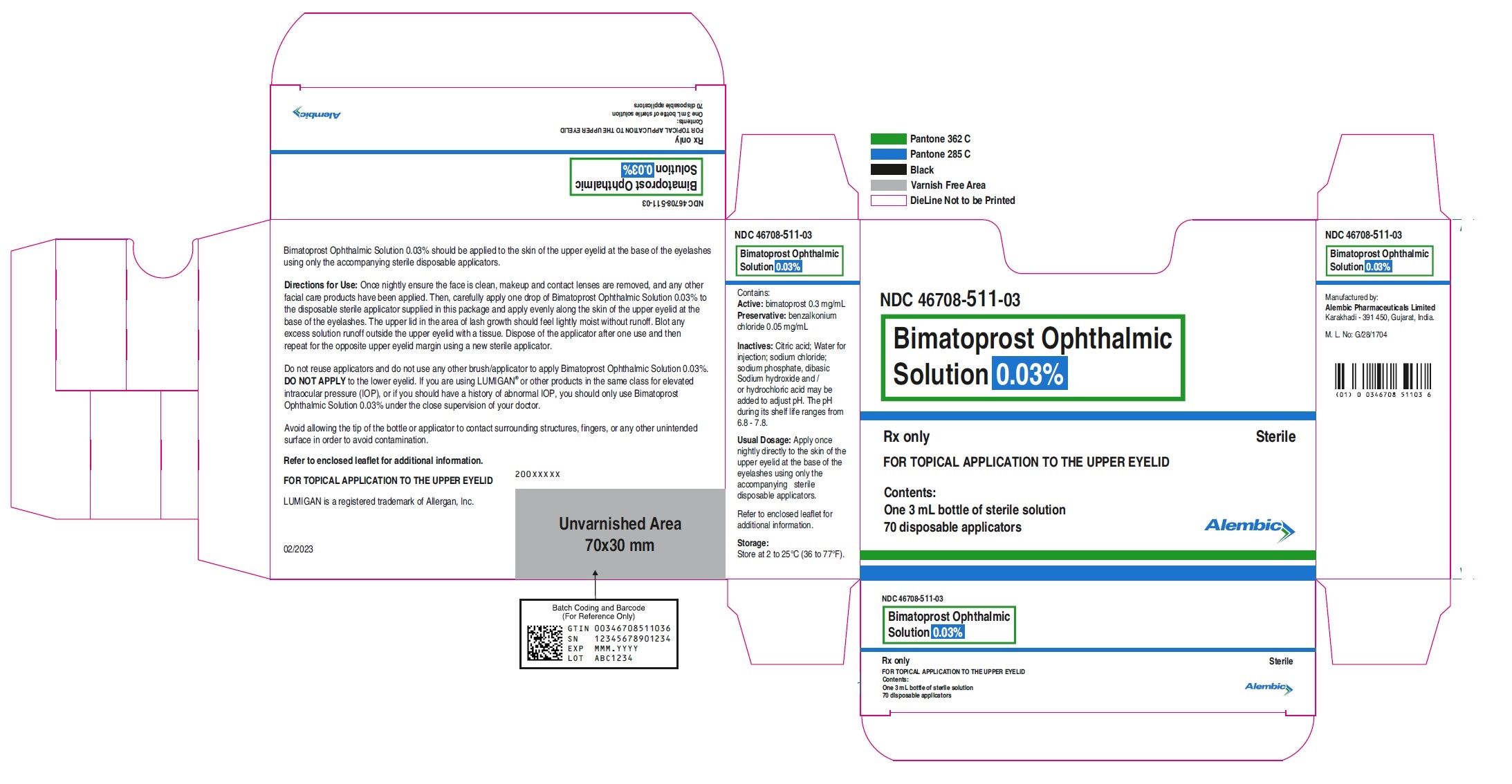
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
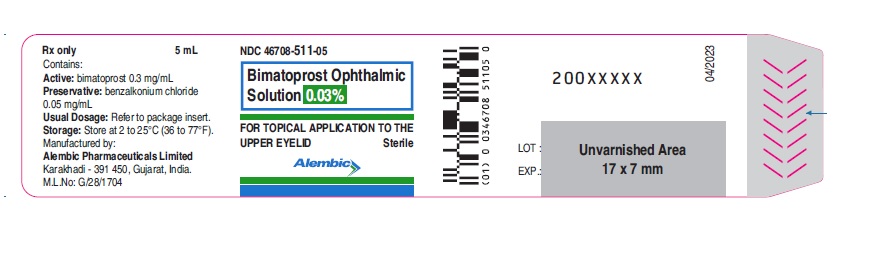
Bimatoprost ophthalmic solution 0.03% Topical - Bottle label - 5 mL - Alembic:
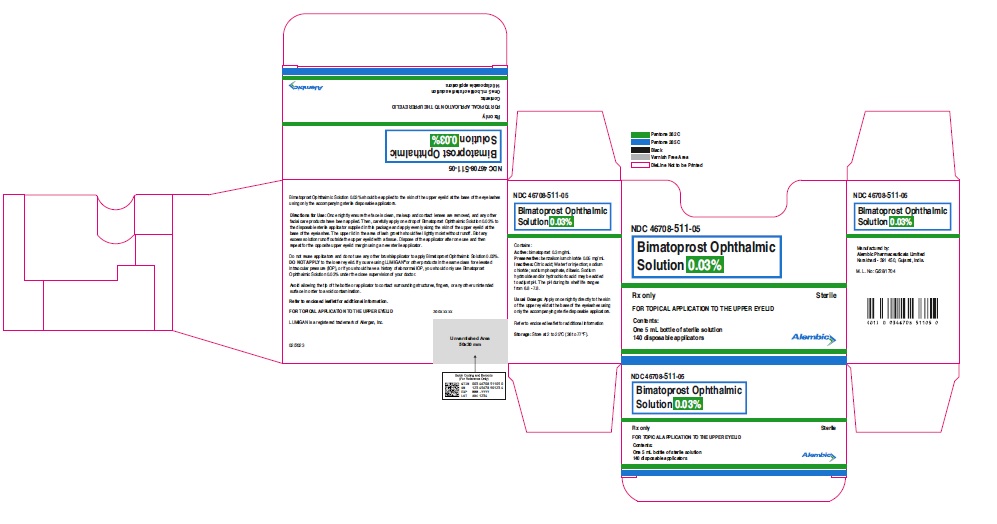
Bimatoprost ophthalmic solution 0.03% Topical - Carton label - 5mL - Alembic:
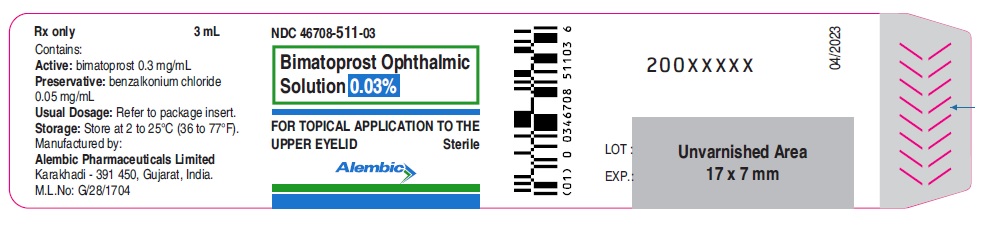
Bimatoprost ophthalmic solution 0.03% Topical - Bottle label - 3 mL - Alembic:
Bimatoprost ophthalmic solution 0.03% Topical - Carton label - 3mL - Alembic:
-
INGREDIENTS AND APPEARANCE
BIMATOPROST
bimatoprost solution/ dropsProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 46708-511 Route of Administration OPHTHALMIC Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BIMATOPROST (UNII: QXS94885MZ) (BIMATOPROST - UNII:QXS94885MZ) BIMATOPROST 0.3 mg in 1 mL Inactive Ingredients Ingredient Name Strength BENZALKONIUM CHLORIDE (UNII: F5UM2KM3W7) SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM PHOSPHATE, DIBASIC, HEPTAHYDRATE (UNII: 70WT22SF4B) CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 46708-511-05 1 in 1 CARTON 07/21/2023 1 5 mL in 1 BOTTLE; Type 0: Not a Combination Product 2 NDC: 46708-511-03 1 in 1 CARTON 07/21/2023 2 3 mL in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA210515 07/21/2023 Labeler - Alembic Pharmaceuticals Limited (650574663) Establishment Name Address ID/FEI Business Operations Alembic Pharmaceuticals Limited (F3) 675480734 MANUFACTURE(46708-511)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.