MIRABEGRON tablet, extended release
Mirabegron by
Drug Labeling and Warnings
Mirabegron by is a Prescription medication manufactured, distributed, or labeled by Zydus Pharmaceuticals (USA) Inc., Zydus Lifesciences Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use MIRABEGRON EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for MIRABEGRON EXTENDED-RELEASE TABLETS
MIRABEGRON extended-release tablets, for oral use
Initial U.S. Approval: 2012INDICATIONS AND USAGE
Mirabegron extended-release tablets are a beta-3 adrenergic agonist indicated for the treatment of:
DOSAGE AND ADMINISTRATION
- Mirabegron extended-release tablets and Mirabegron Granules are two different products and they are not substitutable on a milligram-per-milligram basis. Select the recommended product (Mirabegron extended-release tablets and Mirabegron Granules) based on the indication and patient's weight.
OAB in Adults
- The recommended starting dose of mirabegron extended-release tablets is 25 mg orally once daily. (2.2)
- After 4 to 8 weeks, the mirabegron extended-release tablets dose may be increased to 50 mg orally once daily. (2.2)
NDO in Pediatric Patients 3 Years and Older
- Pediatric Patients weighing 35 kg or more: Use mirabegron extended-release tablets:
- The recommended starting dosage of mirabegron extended-release tablets is 25 mg orally once daily. After 4 to 8 weeks, the mirabegron extended-release tablets dose may be increased to 50 mg orally once daily. (2.3)
Adult or Pediatric Patients Patients with Renal or Hepatic Impairment: Refer to the full prescribing information for recommended dosage. (2.4, 2.5)
Administration
- Mirabegron extended-release tablets:
DOSAGE FORMS AND STRENGTHS
Extended-release tablets: 25 mg and 50 mg (3)
CONTRAINDICATIONS
Hypersensitivity to mirabegron or any inactive ingredients. (4)
WARNINGS AND PRECAUTIONS
- Increases in Blood Pressure: Can increase blood pressure in adult or pediatric patients. Periodically monitor blood pressure, especially in hypertensive patients. Mirabegron extended-release tablets are not recommended in patients with severe uncontrolled hypertension. (5.1)
- Urinary Retention in Patients with Bladder Outlet Obstruction and in Patients Taking Muscarinic Antagonist Drugs for Overactive Bladder:Administer with caution in these patients because of risk of urinary retention. (5.2)
- Angioedema:Angioedema of the face, lips, tongue and/or larynx has been reported with mirabegron. (5.3, 6.2)
ADVERSE REACTIONS
- Most commonly reported adverse reactions with mirabegron monotherapy in adult patients with OAB (> 2% and > placebo) were hypertension, nasopharyngitis, urinary tract infection, and headache. (6.1)
- Most commonly reported adverse reactions with mirabegron in pediatric patients with NDO (≥ 3%) were UTI, nasopharyngitis, constipation, and headache. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Zydus Pharmaceuticals (USA) Inc. at 1-877-993-8779 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Drugs Metabolized by CYP2D6: Mirabegron is a CYP2D6 inhibitor and, when used concomitantly with drugs metabolized by CYP2D6, especially narrow therapeutic index drugs, appropriate monitoring and possible dose adjustment of those drugs may be necessary. (5.4, 7.1, 12.3)
- Digoxin: When initiating a combination of mirabegron and digoxin, use the lowest dose of digoxin; monitor serum digoxin concentrations to titrate digoxin dose to desired clinical effect. (7.2, 12.3)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 10/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Adult Overactive Bladder (OAB)
1.2 Pediatric Neurogenic Detrusor Overactivity (NDO)
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage Information
2.2 Recommended Dosage for Adult Patients with OAB
2.3 Recommended Dosage for Pediatric Patients Aged 3 Years and Older with NDO
2.4 Recommended Dosage in Adult Patients with Renal or Hepatic Impairment
2.5 Recommended Dosage in Pediatric Patients with Renal or Hepatic Impairment
2.7 Administration Instructions
2.8 Missed Dose
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Increases in Blood Pressure
5.2 Urinary Retention in Patients with Bladder Outlet Obstruction and in Patients Taking Muscarinic Antagonist Medications for OAB
5.3 Angioedema
5.4 Patients Taking Drugs Metabolized by CYP2D6
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Drugs Metabolized by CYP2D6
7.2 Digoxin
7.3 Warfarin
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Mirabegron Monotherapy for Adult OAB
14.3 Mirabegron for Pediatric Neurogenic Detrusor Overactivity (NDO)
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 Mirabegron extended-release tablets
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage Information
Mirabegron extended-release tablets and Mirabegron Granules are two different products and they are not substitutable on a milligram-per-milligram basis.
2.2 Recommended Dosage for Adult Patients with OAB
The recommended starting dosage of mirabegron extended-release tablets is 25 mg orally once daily. If needed, increase to the maximum dosage of mirabegron extended-release tablets 50 mg orally once daily after 4 to 8 weeks. For administration instructions, see Dosage and Administration (2.7).
2.3 Recommended Dosage for Pediatric Patients Aged 3 Years and Older with NDO
For pediatric patients 3 years of age and older, select the appropriate product (Mirabegron extended-release tablets and Mirabegron Granules) based on the patient's weight.
Pediatric Patients weighing 35 kg or more: Use mirabegron extended-release tablets
The recommended starting dosage of mirabegron extended-release tablets is 25 mg orally once daily. If needed, increase to a maximum dosage of mirabegron extended-release tablets 50 mg orally once daily after 4 to 8 weeks. For administration instructions, see Dosage and Administration (2.7).
2.4 Recommended Dosage in Adult Patients with Renal or Hepatic Impairment
Dosage in Adults with Renal Impairment
The recommended dosage of mirabegron extended-release tablets (administered orally once daily) in adult patients with renal impairment is described in Table 1 [see Use in Specific Populations (8.6)]. For administration instructions, see Dosage and Administration (2.7).
Table 1: Mirabegron Extended-Release Tablets Recommended Dosage in Adult Patients with Renal Impairment (Administered Orally Once Daily)
Estimated GFR1
Starting Dose
Maximum Dose
eGFR 30 to 89 mL/min/1.73 m2
25 mg
50 mg
eGFR 15 to 29 mL/min/1.73 m2
25 mg
25 mg
eGFR < 15 mL/min/1.73 m2 or requiring dialysis
Not Recommended
1. Estimated GFR using the modification of diet in renal disease (MDRD) formula
Dosage in Adults with Hepatic Impairment
The recommended dosage of mirabegron extended-release tablets (administered orally once daily) in adult patients with hepatic impairment is described in Table 2 [see Use in Specific Populations (8.7)]. For administration instructions, see Dosage and Administration (2.7).
Table 2: Mirabegron Recommended Dosage in Adult Patients with Hepatic Impairment (Administered Orally Once Daily)
Hepatic Impairment Classification
Starting Dose
Maximum Dose
Child-Pugh Class A ( Mild hepatic impairment
25 mg
50 mg
Child-Pugh Class B ( Moderate hepatic impairment
25 mg
25 mg
Child-Pugh Class C ( Severe hepatic impairment
Not Recommended
2.5 Recommended Dosage in Pediatric Patients with Renal or Hepatic Impairment
For pediatric patients 3 years of age and older, select the appropriate product (Mirabegron extended-release tablets and Mirabegron Granules) based on the patient's weight.
Pediatric Patients weighing 35 kg or more with renal or hepatic impairment: Use Mirabegron Extended-Release Tablets
Dosage in Pediatric Patients with Renal Impairment
The recommended dosage of mirabegron extended-release tablets in pediatric patients with renal impairment weighing 35 kg or more (administered orally once daily) is described in Table 1 (above). Note that the dosage is the same as for adult patients with renal impairment [see Dosage and Administration (2.4) and Use in Specific Populations (8.6)]. For administration instructions, see Dosage and Administration (2.7).
Dosage in Pediatric Patients with Hepatic Impairment
The recommended dosage of mirabegron extended-release tablets in pediatric patients with hepatic impairment weighing 35 kg or more (administered orally once daily) is described in Table 2 (above). Note that the dosage is the same as for adult patients with hepatic impairment [see Dosage and Administration (2.4) and Use in Specific Populations (8.6)]. For administration instructions, see Dosage and Administration (2.7).
2.7 Administration Instructions
Mirabegron extended-release tablets
Adult patients: Swallow mirabegron extended-release tablets whole with water. Do not chew, divide, or crush. Take with or without food.
Pediatric patients: Swallow mirabegron extended-release tablets whole with water. Do not chew, divide, or crush. Take with food [see Use in Specific Populations (8.4)].
-
3 DOSAGE FORMS AND STRENGTHS
Mirabegron extended-release tablets are supplied in two different strengths as described below:
- 25 mg peach colored, oval shaped, biconvex, film-coated tablets debossed with "1159" on one side and plain on other side
- 50 mg yellow colored, oval shaped, biconvex, film-coated tablets debossed with "1160" on one side and plain on other side.
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Increases in Blood Pressure
Increases in Blood Pressure in Adults
Mirabegron can increase blood pressure. Periodic blood pressure determinations are recommended, especially in hypertensive patients. Mirabegron is not recommended for use in patients with severe uncontrolled hypertension (defined as systolic blood pressure greater than or equal to 180 mm Hg and/or diastolic blood pressure greater than or equal to 110 mm Hg) [see Clinical Pharmacology (12.2)].
In two, randomized, placebo-controlled, healthy adult volunteer studies, mirabegron was associated with dose-related increases in supine blood pressure. In these studies, at the maximum recommended dose of 50 mg, the mean maximum increase in systolic/diastolic blood pressure was approximately 3.5/1.5 mm Hg greater than placebo.
In contrast, in adult OAB patients in clinical trials, mirabegron, taken as monotherapy, the mean increase in systolic and diastolic blood pressure at the maximum recommended mirabegron dose of 50 mg was approximately 0.5 to 1 mm Hg greater than placebo. Worsening of pre-existing hypertension was reported infrequently in patients taking mirabegron.
Increases in Blood Pressure in Pediatric Patients 3 Years and Older
Mirabegron can increase blood pressure in pediatric patients. Blood pressure increases may be larger in children (3 to less than 12 years of age) than in adolescents (12 to less than 18 years of age). Periodic blood pressure determinations are recommended. Mirabegron is not recommended for use in pediatric patients with severe uncontrolled hypertension, defined as a systolic and/or diastolic blood pressure above the 99th percentile plus 5 mm Hg for age, sex, and stature using appropriate reference values [see Adverse Reactions (6.1)].
5.2 Urinary Retention in Patients with Bladder Outlet Obstruction and in Patients Taking Muscarinic Antagonist Medications for OAB
In patients taking mirabegron, urinary retention has been reported to occur in patients with bladder outlet obstruction (BOO) and in patients taking muscarinic antagonist medications for the treatment of OAB. A controlled clinical safety study in patients with BOO did not demonstrate increased urinary retention in patients treated with mirabegron; however, mirabegron should still be administered with caution to patients with clinically significant BOO. For example, monitor these patients for signs and symptoms of urinary retention. Mirabegron should also be administered with caution to patients taking muscarinic antagonist medications for the treatment of OAB [see Clinical Pharmacology (12.2)].
5.3 Angioedema
Angioedema of the face, lips, tongue, and/or larynx has been reported with mirabegron. In some cases, angioedema occurred after the first dose, however, cases have been reported to occur hours after the first dose or after multiple doses. Angioedema, associated with upper airway swelling, may be life-threatening. If involvement of the tongue, hypopharynx, or larynx occurs, promptly discontinue mirabegron and provide appropriate therapy and/or measures necessary to ensure a patent airway [see Adverse Reactions (6.2)].
5.4 Patients Taking Drugs Metabolized by CYP2D6
Since mirabegron is a moderate CYP2D6 inhibitor, the systemic exposure to CYP2D6 substrates is increased when coadministered with mirabegron. Therefore, appropriate monitoring and dose adjustment may be necessary, especially with narrow therapeutic index drugs metabolized by CYP2D6 [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in more detail in other sections of the labeling.
- Hypertension [see Warnings and Precautions (5.1)]
- Urinary Retention [see Warnings and Precautions (5.2)]
- Angioedema [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Mirabegron Monotherapy for Adult OAB
In three, 12-week, double-blind, placebo-controlled, safety and efficacy studies in patients with OAB (Studies 1, 2, and 3), mirabegron was evaluated for safety in 2,736 patients [see Clinical Studies (14.1)]. Study 1 also included an active control. For the combined Studies 1, 2, and 3,432 patients received mirabegron 25 mg, 1,375 received mirabegron 50 mg, and 929 received mirabegron 100 mg once daily. In these studies, the majority of the patients were Caucasian (94%), and female (72%) with a mean age of 59 years (range 18 to 95 years).
Mirabegron was also evaluated for safety in 1,632 patients who received mirabegron 50 mg once daily (n=812 patients) or mirabegron 100 mg (n=820 patients) in a 1-year, randomized, fixed- dose, double-blind, active-controlled, safety study in patients with OAB (Study 4). Of these patients, 731 received mirabegron in a previous 12-week study. In Study 4, 1385 patients received mirabegron continuously for at least 6 months, 1,311 patients received mirabegron for at least 9 months, and 564 patients received mirabegron for at least 1 year.
The most frequent adverse events (0.2%) leading to discontinuation in Studies 1, 2 and 3 for the 25 mg or 50 mg dose were nausea, headache, hypertension, diarrhea, constipation, dizziness, and tachycardia.
Atrial fibrillation (0.2%) and prostate cancer (0.1%) were reported as serious adverse events by more than 1 patient and at a rate greater than placebo.
Table 3 the lists adverse reactions, derived from all adverse events that were reported in Studies 1, 2 and 3 at an incidence greater than placebo and in 1% or more of patients treated with mirabegron 25 mg or 50 mg once daily for up to 12 weeks. The most commonly reported adverse reactions (greater than 2% of mirabegron patients and greater than placebo) were hypertension, nasopharyngitis, urinary tract infection, and headache.
Table 3: Percentages of Patients with Adverse Reactions, Derived from All Adverse Events, Exceeding Placebo Rate and Reported in ≥ 1% of OAB Patients Treated with mirabegron 25 mg or 50 mg Once Daily in Studies 1, 2, and 3
Adverse Reaction
Placebo
(%)
Mirabegron 25 mg
(%)
Mirabegron 50 mg
(%)
Number of Patients
1380
432
1375
Hypertension*
7.6
11.3
7.5
Nasopharyngitis
2.5
3.5
3.9
Urinary Tract Infection
1.8
4.2
2.9
Headache
3.0
2.1
3.2
Constipation
1.4
1.6
1.6
Upper Respiratory Tract Infection
1.7
2.1
1.5
Arthralgia
1.1
1.6
1.3
Diarrhea
1.3
1.2
1.5
Tachycardia
0.6
1.6
1.2
Abdominal Pain
0.7
1.4
0.6
Fatigue
1.0
1.4
1.2
*Includes reports of blood pressure above the normal range, and BP increased from baseline, occurring predominantly in subjects with baseline hypertension.
Other adverse reactions reported by less than 1% of patients treated with mirabegron in Studies 1, 2, or 3 included:
Cardiac disorders: palpitations, blood pressure increased [see Clinical Pharmacology (12.2)]
Eye disorders: glaucoma [see Clinical Pharmacology (12.2)]
Gastrointestinal disorders: dyspepsia, gastritis, abdominal distension
Infections and Infestations: sinusitis, rhinitis
Investigations: GGT increased, AST increased, ALT increased, LDH increased
Renal and urinary disorders: nephrolithiasis, bladder pain
Reproductive system and breast disorders: vulvovaginal pruritus, vaginal infection
Skin and subcutaneous tissue disorders: urticaria, leukocytoclastic vasculitis, rash, pruritus, purpura, lip edema
Table 4 lists the rates of the most commonly reported adverse reactions, derived from all adverse events in patients treated with mirabegron 50 mg for up to 52 weeks in Study 4. The most commonly reported adverse reactions (>3% of mirabegron patients) were hypertension, urinary tract infection, headache, and nasopharyngitis.
Table 4: Percentages of Patients with Adverse Reactions, Derived from All Adverse Events, Reported in >2% of OAB Patients Treated with mirabegron 50 mg Once Daily in Study 4
Adverse Reaction
Mirabegron 50 mg
(%)
Active Control
(%)
Number of Patients
812
812
Hypertension
9.2
9.6
Urinary Tract Infection
5.9
6.4
Headache
4.1
2.5
Nasopharyngitis
3.9
3.1
Back Pain
2.8
1.6
Constipation
2.8
2.7
Dry Mouth
2.8
8.6
Dizziness
2.7
2.6
Sinusitis
2.7
1.5
Influenza
2.6
3.4
Arthralgia
2.1
2.0
Cystitis
2.1
2.3
In Study 4, in patients treated with mirabegron 50 mg once daily, adverse reactions leading to discontinuation reported by more than 2 patients and at a rate greater than active control included: constipation (0.9%), headache (0.6%), dizziness (0.5%), hypertension (0.5%), dry eyes (0.4%), nausea (0.4%), vision blurred (0.4%), and urinary tract infection (0.4%). Serious adverse events reported by at least 2 patients and exceeding active control included cerebrovascular accident (0.4%) and osteoarthritis (0.2%). Serum ALT/AST increased from baseline by greater than 10-fold in 2 patients (0.3%) taking mirabegron 50 mg; and these markers subsequently returned to baseline while both patients continued mirabegron.
In Study 4, serious adverse events of neoplasm were reported by 0.1%, 1.3%, and 0.5% of patients treated with mirabegron 50 mg, mirabegron 100 mg and active control once daily, respectively. Neoplasms reported by 2 patients treated with mirabegron 100 mg included breast cancer, lung neoplasm malignant and prostate cancer. A causal relationship between mirabegron and these reported neoplasms has not been established.
In a separate clinical study in Japan, a single case was reported as Stevens-Johnson syndrome with increased serum ALT, AST, and bilirubin in a patient taking mirabegron 100 mg as well as an herbal medication (Kyufu Gold).
Mirabegron for Pediatric Neurogenic Detrusor Overactivity (NDO)
The safety of mirabegron was evaluated in a 52-week, open-label, baseline-controlled, multicenter, dose titration study (Study 9) [see Clinical Studies (14.3)]. The study included 86 pediatric patients 3 to 17 years of age with neurogenic detrusor overactivity (NDO); 55% were female, 72% were White. Treatment was initiated at the weight-based starting recommended dose and was increased to a dose equivalent of mirabegron 50 mg daily dose in adults by Week 8. Subsequent to the dose titration period, patients continued their optimized dose for the duration of the 52-week study (mean exposure duration 303 days, range 1 to 390 days).
The most commonly reported adverse reactions were UTI, nasopharyngitis, constipation, and headache.
Table 5 lists the adverse reactions that were reported in 2% or more of patients treated with mirabegron in Study 9.
Table 5: Percentages of Patients with Adverse Reactions Reported in ≥ 2% of Patients 3 to 17 Years of Age with Neurogenic Detrusor Overactivity (NDO) Treated with Mirabegron in Study 9 Adverse Reaction
Percentage (%) of Patients Reporting
Adverse Reactions
N=86
N umber of Patients
51 (59.3)
Urinary Tract Infection1
24.4
Nasopharyngitis
5.8
Constipation
4.7
Headache
3.5
Nausea
2.3
Gastroenteritis
2.3
Rhinitis
2.3
Cough
2.3
1. Includes any recorded UTI while patient was on treatment with mirabegron.
Increased Blood Pressure in Pediatric Patients with NDO Treated with mirabegron:
Mean systolic and diastolic blood pressures increased in Study 9 by 4.3 mm Hg and 1.7 mm Hg, respectively, in patients less than 12 years of age on mirabegron at a dose equivalent of mirabegron 50 mg daily dose in adults. The blood pressure increases were larger in patients less than 8 years of age with mean systolic and diastolic blood pressure increases of 5.9 mm Hg and 2.3 mm Hg, respectively. Ten (24%) patients less than 12 years of age who were normotensive at baseline had at least one blood pressure measured at or above the 95th percentile for age, sex, and stature during Study 9. Stage 1 hypertension, defined as repeated blood pressure measurements at or above the 95th percentile for age, sex, and stature, was sustained in six of these 10 patients (60%) at the end of the study.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of mirabegron. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The following events have been reported in association with mirabegron use in worldwide postmarketing experience:
Cardiac disorders: atrial fibrillation
Gastrointestinal disorders: nausea, constipation, diarrhea
Nervous system disorders: dizziness, headache
There have been postmarketing reports of confusion, hallucinations, insomnia and anxiety in patients taking mirabegron. The majority of these patients had pre-existing medical conditions or concomitant medications that may cause confusion, hallucinations, insomnia and anxiety. A causal relationship between mirabegron and these disorders has not been established.
Skin and subcutaneous tissue disorders: angioedema of the face, lips, tongue, and larynx, with or without respiratory symptoms [see Warnings and Precautions (5.3)]; pruritus
Renal and urinary disorders: urinary retention [see Warnings and Precautions (5.2)]
-
7 DRUG INTERACTIONS
Drug interaction studies were conducted in adult patients to investigate the effect of coadministered drugs on the pharmacokinetics of mirabegron and the effect of mirabegron on the pharmacokinetics of coadministered drugs (e.g., ketoconazole, rifampin, solifenacin succinate, tamsulosin, and oral contraceptives) [see Clinical Pharmacology (12.3)]. No dose adjustment is recommended when these drugs are coadministered with mirabegron.
The following are drug interactions for which monitoring is recommended:
7.1 Drugs Metabolized by CYP2D6
Since mirabegron is a moderate CYP2D6 inhibitor, the systemic exposure of drugs metabolized by CYP2D6 enzyme is increased when coadministered with mirabegron. Therefore, appropriate monitoring and dose adjustment may be necessary when mirabegron is coadministered with these drugs, especially with narrow therapeutic index CYP2D6 substrates [see Warnings and Precautions (5.4) and Clinical Pharmacology (12.3)].
7.2 Digoxin
When given in combination, 100 mg mirabegron increased mean digoxin Cmax from 1.01 ng/mL to 1.3 ng/mL (29%) and AUC from 16.7 ng.h/mL to 19.3 ng.h/mL (27%). For patients who are initiating a combination of mirabegron and digoxin, the lowest dose for digoxin should initially be considered. Serum digoxin concentrations should be monitored and used for titration of the digoxin dose to obtain the desired clinical effect [see Clinical Pharmacology (12.3)].
7.3 Warfarin
The mean Cmax of S- and R-warfarin was increased by approximately 4% and AUC by approximately 9% when administered as a single dose of 25 mg after multiple doses of 100 mg mirabegron. Following a single dose administration of 25 mg warfarin, mirabegron had no effect on the warfarin pharmacodynamic endpoints such as International Normalized Ratio (INR) and prothrombin time. However, the effect of mirabegron on multiple doses of warfarin and on warfarin pharmacodynamic end points such as INR and prothrombin time has not been fully investigated [see Clinical Pharmacology (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
There are no studies with the use of mirabegron in pregnant women or adolescents to inform a drug-associated risk of major birth defects, miscarriages, or adverse maternal or fetal outcomes. Mirabegron administration to pregnant animals during organogenesis resulted in reversible skeletal variations (in rats) at 22-fold (via AUC) the maximum recommended human dose (MRHD) of 50 mg/day and decreased fetal body weights (in rabbits) at 14-fold the MRHD. At maternally-toxic exposures in rats (96-fold), decreased fetal weight and increased fetal mortality were observed and, in rabbits (36-fold), cardiac findings (fetal cardiomegaly and fetal dilated aortae) were observed [see Data].
The estimated background risks of major birth defects and miscarriage for the indicated populations are unknown. In the U.S. general population, the estimated background risks of major birth defects or miscarriage in clinically recognized pregnancies are 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
No embryo-fetal lethality or morphological fetal developmental abnormalities were produced in pregnant rats following daily oral administration of mirabegron during the period of organogenesis (Days 7 to 17 of gestation) at 0, 10, 30, 100, or 300 mg/kg, doses which were associated with systemic exposures (AUC) 0, 1, 6, 22, and 96-fold the MRHD. Skeletal variations (wavy ribs, delayed ossification) were observed in fetuses at doses 22-fold the systemic exposure at the MRHD and were reversible during development. Exposures 96-fold the MRHD were maternally-toxic (mortality, decreased body weight gain) and associated with fetal growth reduction.
Pregnant rabbits were treated with daily oral doses of mirabegron at 0, 3, 10, or 30 mg/kg/day during the period of organogenesis (Days 6 to 20 of gestation), which resulted in plasma exposures that were 0, 1, 14, or 36-fold the MRHD based on AUC. At 10 mg/kg/day (14-fold the MRHD) and higher, fetal body weights were reduced. At 30 mg/kg/day, maternal toxicity (increased heart rate, mortality, reduced body weight gain, reduced food consumption) occurred, and fetal deaths, fetal cardiomegaly and fetal dilated aortae were observed at systemic exposure levels (AUC) 36-fold the MRHD.
In a pre-and postnatal developmental study, rats were treated with daily oral doses of mirabegron at 0, 10, 30, or 100 mg/kg/day (0, 1, 6, or 22-fold the MRHD) from day 7 of gestation until day 20 after birth. Decreased maternal body weight was observed along with decreased pup survival in the first few days after birth (92.7% survival) compared to the control group (98.8% survival), at 100 mg/kg/day (22-fold the MRHD). Pup body weight gain was reduced until postnatal day 7 but not further affected throughout the remainder of the lactation period. In utero and lactational exposure did not affect developmental milestones, behavior or fertility of offspring. No effects were observed at 30 mg/kg/day.
8.2 Lactation
There are no data on the presence of mirabegron in human milk, the effects on the breastfed child, or the effects on milk production. Mirabegron-related material was present in rat milk and in the stomach of nursing pups following administrations of a single 10 mg/kg oral dose of 14C-labeled mirabegron to lactating rats. When a drug is present in animal milk, it is likely that the drug will be present in human milk.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for mirabegron and any potential adverse effects on the breastfed child from mirabegron or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness have been established only for the following pediatric indications:
- Mirabegron: Treatment of neurogenic detrusor overactivity (NDO) in pediatric patients 3years of age and older and weighing 35 kg or more.
The safety and effectiveness of mirabegron in pediatric patients aged 3 years and older have been established for the treatment of neurogenic detrusor overactivity (NDO) and the information on this use is discussed throughout the labeling. Use of mirabegron for this indication is supported by evidence from a 52-week, open-label, baseline-controlled, multicenter, dose titration trial in pediatric patients 3 years of age and older with NDO (Study 9) [see Adverse Reactions (6.1), Clinical Studies (14.3)]. Results showed an improvement from baseline in maximum cystometric (bladder) capacity (MCC) with mirabegron use [see Clinical Studies (14.3)]. The most commonly reported adverse reactions in Study 9 (≥3%) were UTI, nasopharyngitis, constipation, and headache. Increased mean systolic and diastolic blood pressures with use of mirabegron occurred in patients less than 12 years of age with larger increases in patients younger than 8 years of age [see Adverse Reactions (6.1)].
Take mirabegron with food to reduce potential exposure-related risks, such as increased heart rate, as predicted by modeling of vital signs data in Study 9 [see Clinical Pharmacology (12.3)].
8.5 Geriatric Use
Of 5,648 patients who received mirabegron monotherapy in the phase 2 and 3 studies for OAB, 2,029 (35.9%) were 65 years of age or older, and 557 (9.9%) were 75 years of age or older. No overall differences in safety or effectiveness were observed between patients younger than 65 years of age and those 65 years of age or older in these studies.
8.6 Renal Impairment
Mirabegron have not been studied in patients with End-Stage Renal Disease (eGFR <15 mL/min/1.73 m2) or patients requiring hemodialysis and, therefore, is not recommended for use in these patient populations. No dose adjustment is necessary in patients with mild or moderate renal impairment (eGFR 30 to 89 mL/min/1.73 m2).
In adult patients with severe renal impairment (eGFR 15 to 29 mL/min/1.73 m2), the daily dose of mirabegron should not exceed 25 mg. In pediatric patients with severe renal impairment, the daily dose of mirabegron should not exceed the recommended starting dose [see Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Mirabegron has not been studied in patients with severe hepatic impairment (Child-Pugh Class C) and, therefore, is not recommended for use in this patient population.
In adult patients with moderate hepatic impairment (Child-Pugh Class B), the daily dose of mirabegron should not exceed 25 mg. In pediatric patients with moderate hepatic impairment (Child-Pugh Class B), the daily dose of mirabegron should not exceed the recommended starting dose [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
Mirabegron has been administered to healthy volunteers at single doses up to 400 mg. At this dose, adverse events reported included palpitations (1 of 6 subjects) and increased pulse rate exceeding 100 beats per minute (bpm) (3 of 6 subjects). Multiple doses of mirabegron up to 300 mg daily for 10 days showed increases in pulse rate and systolic blood pressure when administered to healthy volunteers. Treatment for overdosage should be symptomatic and supportive. In the event of overdosage, pulse rate, blood pressure and ECG monitoring is recommended.
-
11 DESCRIPTION
Mirabegron extended-release tablets for oral use is a beta-3 adrenergic agonist.
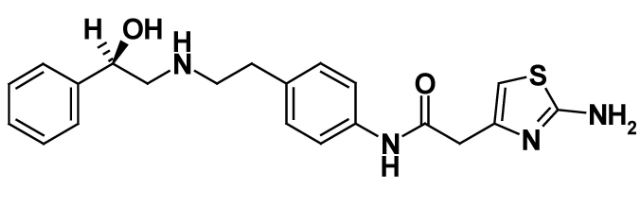
The chemical name is 2-(2-Amonothiazol-4-yl)-N-(4-(2-(2R)-hydroxy-2-phenylethylamino)ethyl)phenyl)acetamide having an empirical formula of C21H24N4O2S and a molecular weight of 396.51. The structural formula of mirabegron is:
Mirabegron is a white powder. It is practically insoluble in water. It is soluble in methanol and dimethyl sulfoxide.
Each mirabegron extended-release tablet for oral use contains either 25 mg or 50 mg of mirabegron and the following inactive ingredients: polyethylene oxide, polyethylene glycol, magnesium stearate, hypromellose, ferrosoferric oxide, yellow iron oxide, and red iron oxide (25 mg tablet only).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Mirabegron is an agonist of the human beta-3 adrenergic receptor (AR) as demonstrated by in vitro laboratory experiments using the cloned human beta-3 AR. Mirabegron relaxes the detrusor smooth muscle during the storage phase of the urinary bladder fill-void cycle by activation of beta-3 AR which increases bladder capacity. Although mirabegron showed very low intrinsic activity for cloned human beta-1 AR and beta-2 AR, results in humans indicate that beta-1 AR stimulation occurred at a mirabegron dose of 200 mg.
12.2 Pharmacodynamics
The effects of mirabegron on maximum urinary flow rate and detrusor pressure at maximum flow rate were assessed in a urodynamic study consisting of 200 male patients with lower urinary tract symptoms (LUTS) and BOO. Administration of mirabegron once daily for 12 weeks did not adversely affect the mean maximum flow rate or mean detrusor pressure at maximum flow rate in this study. Nonetheless, mirabegron should be administered with caution to patients with clinically significant BOO [see Warnings and Precautions (5.2)].
Cardiac Electrophysiology
The effect of multiple doses of mirabegron 50 mg, 100 mg, and 200 mg (four times the maximum recommended dose) once daily on QTc interval was evaluated in a randomized, placebo- and active-controlled (moxifloxacin 400 mg), four-treatment arm, parallel crossover study in 352 healthy subjects. In a study with demonstrated ability to detect small effects, the upper bound of the one-sided 95% confidence interval for the largest placebo-adjusted, baseline-corrected QTc based on individual correction method (QTcI) was below 10 msec. For the 50 mg mirabegron dose group (the maximum approved dosage), the mean difference from placebo on QTcI interval at 4 to 5 hours post-dose was 3.7 msec (upper bound of the 95% CI 5.1 msec).
For the mirabegron 100 mg and 200 mg dose groups (dosages greater than the maximum approved dose and resulting in substantial multiples of the anticipated maximum blood levels at 50 mg), the mean differences from placebo in QTcI interval at 4 to 5 hours post-dose were 6.1 msec (upper bound of the 95% CI 7.6 msec) and 8.1 msec (upper bound of the 95% CI 9.8 msec), respectively. At the mirabegron 200 mg dose, in females, the mean effect was 10.4 msec (upper bound of the 95% CI 13.4 msec).
In this thorough QT study, mirabegron increased heart rate on ECG in a dose-dependent manner. Maximum mean increases from baseline in heart rate for the 50 mg, 100 mg, and 200 mg dose groups compared to placebo were 6.7 bpm, 11 bpm, and 17 bpm, respectively. In the clinical efficacy and safety studies, the change from baseline in mean pulse rate for mirabegron 50 mg was approximately 1 bpm. In this thorough QT study, mirabegron also increased blood pressure in a dose-dependent manner (see Effects on Blood Pressure).
Effects on Blood Pressure
In a study of 352 healthy subjects assessing the effect of multiple daily doses of 50 mg, 100 mg, and 200 mg (four times the maximum recommended dose) of mirabegron for 10 days on the QTc interval, the maximum mean increase in supine systolic blood pressure (SBP)/diastolic blood pressure (DBP) at the maximum recommended dose of 50 mg was approximately 4.0/1.6 mm Hg greater than placebo [see Warnings and Precautions (5.1)]. The 24-hour average increases in SBP compared to placebo were 3.0, 5.5, and 9.7 mm Hg at mirabegron doses of 50 mg, 100 mg, and 200 mg, respectively. Increases in DBP were also dose-dependent, but were smaller than SBP.
In another study in 96 healthy subjects to assess the impact of age on pharmacokinetics of multiple daily doses of 50 mg, 100 mg, 200 mg, and 300 mg (six times the maximum recommended dose) of mirabegron for 10 days, SBP also increased in a dose-dependent manner. The mean maximum increases in SBP were approximately 2.5, 4.5, 5.5, and 6.5 mm Hg for mirabegron exposures associated with doses of 50 mg, 100 mg, 200 mg and 300 mg, respectively.
In three, 12-week, double-blind, placebo-controlled, safety and efficacy studies (Studies 1, 2, and 3) in patients with OAB receiving mirabegron 25 mg, 50 mg, or 100 mg (two times the maximum recommended dose) once daily, mean increases in SBP/DBP compared to placebo of approximately 0.5 - 1 mm Hg were observed. Morning SBP increased by at least 15 mm Hg from baseline in 5.3%, 5.1%, and 6.7% of placebo, mirabegron 25 mg and mirabegron 50 mg patients, respectively. Morning DBP increased by at least 10 mm Hg in 4.6%, 4.1%, and 6.6% of placebo, mirabegron 25 mg, and mirabegron 50 mg patients, respectively. Both SBP and DBP increases were reversible upon discontinuation of treatment.
Effect on Intraocular Pressure (IOP)
Mirabegron 100 mg once daily did not increase IOP in healthy subjects after 56 days of treatment. In a phase 1 study assessing the effect of mirabegron on IOP using Goldmann applanation tonometry in 310 healthy subjects, a dose of mirabegron 100 mg was non-inferior to placebo for the primary endpoint of the treatment difference in mean change from baseline to day 56 in subject-average IOP; the upper bound of the two-sided 95% CI of the treatment difference between mirabegron 100 mg and placebo was 0.3 mm Hg.
12.3 Pharmacokinetics
Mirabegron Monotherapy for Adult OAB
After oral administration of mirabegron in healthy volunteers, mirabegron was absorbed to reach maximum plasma concentrations (Cmax) at approximately 3.5 hours. The absolute bioavailability increased from 29% at a dose of 25 mg to 35% at a dose of 50 mg. Mean Cmax and AUC increased more than dose proportionally. This relationship was more apparent at doses above 50 mg. In the overall population of males and females, a 2-fold increase in dose from 50 mg to 100 mg mirabegron increased Cmax and AUCtau by approximately 2.9- and 2.6-fold, respectively, whereas a 4-fold increase in dose from 50 mg to 200 mg mirabegron increased Cmax and AUCtau by approximately 8.4- and 6.5-fold. Steady-state concentrations were achieved within 7 days of once daily dosing with mirabegron. After once daily administration, plasma exposure of mirabegron at steady-state was approximately double that seen after a single dose.
Mirabegron for Pediatric Neurogenic Detrusor Overactivity (NDO)
The median Tmax of mirabegron following oral administration of a single dose of mirabegron or mirabegron for extended-release oral suspension in pediatric patients under fed state was 4 to 5 hours. Population pharmacokinetic analysis predicted that the median Tmax of mirabegron or mirabegron for extended-release oral suspension at steady-state was 3 to 4 hours.
Effect of Food
Mirabegron Monotherapy for Adult OAB
There were no clinically significant differences in mirabegron pharmacokinetics when administered with or without food in adult patients.
Mirabegron for Pediatric Neurogenic Detrusor Overactivity (NDO)
In the fasted state, steady-state mirabegron AUC increased by 120% relative to the fed state in pediatric patients receiving mirabegron. Fasted Cmax and AUC increased by 170% and 80%, respectively, compared to the fed state following administration of mirabegron in healthy volunteers.
Distribution
Mirabegron Monotherapy for Adult OAB
Mirabegron is extensively distributed in the body. The volume of distribution at steady-state (Vss) is approximately 1,670 L following intravenous administration. Mirabegron is bound (approximately 71%) to human plasma proteins, and shows moderate affinity for albumin and alpha-1 acid glycoprotein. Mirabegron distributes to erythrocytes. Based on an in vitro study, erythrocyte concentrations of 14C-mirabegron were about 2-fold higher than in plasma.
Mirabegron for Pediatric Neurogenic Detrusor Overactivity (NDO)
Mirabegron volume of distribution was relatively large in pediatric patients (the range of mean Vz/F under fed state in pediatric patients across studies: 4,895 to 13,726 L) and increased with increasing body weight.
Elimination
Mirabegron Monotherapy for Adult OAB
The terminal elimination half-life (t1/2) of mirabegron is approximately 50 hours in patients.
Mirabegron for Pediatric Neurogenic Detrusor Overactivity (NDO)
The mean terminal elimination half-life (t1/2) of mirabegron is approximately 26 to 31 hours in pediatric patients.
Metabolism
Mirabegron is metabolized via multiple pathways involving dealkylation, oxidation, (direct) glucuronidation, and amide hydrolysis. Mirabegron is the major circulating component following a single dose of 14C-mirabegron. Two major metabolites were observed in human plasma and are phase 2 glucuronides representing 16% and 11% of total exposure, respectively. These metabolites are not pharmacologically active toward beta-3 adrenergic receptor. Although in vitro studies suggest a role for CYP2D6 and CYP3A4 in the oxidative metabolism of mirabegron, in vivo results indicate that these isozymes play a limited role in the overall elimination. In healthy subjects who were genotypically poor metabolizers of CYP2D6, mean Cmax and AUCtau were approximately 16% and 17% higher than in extensive metabolizers of CYP2D6, respectively. In vitro and ex vivo studies have shown the involvement of butylcholinesterase, uridine diphospho-glucuronosyltransferases (UGT), and possibly alcohol dehydrogenase in the metabolism of mirabegron, in addition to CYP3A4 and CYP2D6.
Excretion
Mirabegron Monotherapy for Adult OAB
Total body clearance (CLtot) from plasma is approximately 57 L/h following intravenous administration. Renal clearance (CLR) is approximately 13 L/h, which corresponds to nearly 25% of CLtot. Renal elimination of mirabegron is primarily through active tubular secretion along with glomerular filtration. The urinary elimination of unchanged mirabegron is dose-dependent and ranges from approximately 6.0% after a daily dose of 25 mg to 12.2% after a daily dose of 100 mg. Following the administration of 160 mg 14C-mirabegron solution to healthy volunteers, approximately 55% of the radioactivity dose was recovered in the urine and 34% in the feces. Approximately 25% of unchanged mirabegron was recovered in urine and 0% in feces.
Mirabegron for Pediatric Neurogenic Detrusor Overactivity (NDO)
Population pharmacokinetic model predicted that mirabegron clearance in pediatric patients increased with body weight.
Specific Populations
Geriatric Patients
The Cmax and AUC of mirabegron following multiple oral doses in elderly volunteers (≥ 65 years) were similar to those in younger volunteers (18 to 45 years) [see Use in Specific Populations (8.5)].
Pediatric Patients
In patients 3 to less than 18 years of age, age was not predicted to affect mirabegron pharmacokinetic parameters after accounting for differences in body weight [see Use in Specific Populations (8.4)].
Gender
Mirabegron Monotherapy for Adult OAB
The Cmax and AUC of mirabegron were approximately 40% to 50% higher in females than in males. When corrected for differences in body weight, the mirabegron systemic exposure was 20% to 30% higher in females compared to males.
Mirabegron for Pediatric Neurogenic Detrusor Overactivity (NDO)
Gender has no meaningful impact on mirabegron pharmacokinetics in the pediatric population from 3 to less than 18 years of age.
Race
The pharmacokinetics of mirabegron were comparable between Caucasians and African-American Blacks. Cross studies comparison showed that the exposure in Japanese subjects were higher than that in North American subjects. However, when the Cmax and AUC were normalized for dose and body weight, the difference was smaller.
Patients with Renal Impairment
Following single-dose administration of 100 mg mirabegron in adult volunteers with mild renal impairment (eGFR 60 to 89 mL/min/1.73 m2 as estimated by MDRD), mean mirabegron Cmax and AUC were increased by 6% and 31% relative to adult volunteers with normal renal function. In adult volunteers with moderate renal impairment (eGFR 30 to 59 mL/min/1.73 m2), Cmax and AUC were increased by 23% and 66%, respectively. In adult volunteers with severe renal impairment (eGFR 15 to 29 mL/min/1.73 m2), mean Cmax and AUC values were 92% and 118% higher compared to healthy subjects with normal renal function. Mirabegron has not been studied in adult patients with End-Stage Renal Disease (ESRD) (eGFR less than 15 mL/min/1.73 m2) or adult patients requiring dialysis.
Patients with Hepatic Impairment
Following single-dose administration of 100 mg mirabegron in adult volunteers with mild hepatic impairment (Child-Pugh Class A), mean mirabegron Cmax and AUC were increased by 9% and 19%, relative to adult volunteers with normal hepatic function. In adult volunteers with moderate hepatic impairment (Child-Pugh Class B), mean Cmax and AUC values were 175% and 65% higher. Mirabegron has not been studied in adult patients with severe hepatic impairment (Child-Pugh Class C).
Drug Interaction Studies
In Vitro Studies
Effect of Other Drugs on Mirabegron
Mirabegron is transported and metabolized through multiple pathways. Mirabegron is a substrate for CYP3A4, CYP2D6, butyrylcholinesterase, UGT, the efflux transporter P-glycoprotein (P-gp), and the influx organic cation transporters (OCT) OCT1, OCT2, and OCT3. Sulfonylurea hypoglycemic agents glibenclamide (a CYP3A4 substrate), gliclazide (a CYP2C9 and CYP3A4 substrate), and tolbutamide (a CYP2C9 substrate) did not affect the in vitro metabolism of mirabegron.
Effect of Mirabegron on Other Drugs
Studies of mirabegron using human liver microsomes and recombinant human CYP enzymes showed that mirabegron is a moderate and time-dependent inhibitor of CYP2D6 and a weak inhibitor of CYP3A. Mirabegron is unlikely to inhibit the metabolism of coadministered drugs metabolized by the following cytochrome P450 enzymes: CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19 and CYP2E1 because mirabegron did not inhibit the activity of these enzymes at clinically relevant concentrations. Mirabegron did not induce CYP1A2 or CYP3A. Mirabegron inhibited P-gp-mediated drug transport at high concentrations. Mirabegron is predicted not to cause clinically relevant inhibition of OCT-mediated drug transport. Mirabegron did not affect the metabolism of glibenclamide or tolbutamide.
In Vivo Studies
Mirabegron Monotherapy for Adult OAB
The effect of coadministered drugs on the pharmacokinetics of mirabegron and the effect of mirabegron on the pharmacokinetics of coadministered drugs was studied after single and multiple doses of mirabegron. Most drug-drug interactions (DDI) were studied using mirabegron 100 mg extended-release tablets. However, interaction studies of mirabegron with metoprolol and with metformin were studied using mirabegron 160 mg immediate-release (IR) tablets.
The effect of ketoconazole, rifampicin, solifenacin succinate, tamsulosin, and metformin on systemic mirabegron exposure is shown in Figure 1.
The effect of mirabegron on metoprolol, desipramine, combined oral contraceptive-COC (ethinyl estradiol-EE, levonorgestrel-LNG), solifenacin succinate, digoxin, warfarin, tamsulosin, and metformin is shown in Figure 2.
In these studies, the largest increase in mirabegron systemic exposure was seen in the ketoconazole DDI study. As a potent CYP3A4 inhibitor, ketoconazole increased mirabegron Cmax by 45% and mirabegron AUC by 80% after multiple dose administration of 400 mg of ketoconazole for 9 days prior to the administration of a single dose of 100 mg mirabegron in 23 male and female healthy subjects.
As a moderate CYP2D6 inhibitor, mirabegron increased the systemic exposure to metoprolol and desipramine:
- Mirabegron increased the Cmaxof metoprolol by 90% and metoprolol AUC by 229% after multiple doses of 160 mg mirabegron IR tablets once daily for 5 days and a single dose of 100 mg metoprolol tablet in 12 healthy male subjects administered before and concomitantly with mirabegron.
- Mirabegron increased the Cmaxof desipramine by 79% and desipramine AUC by 241% after multiple dose administration of 100 mg mirabegron once daily for 18 days and a single dose of 50 mg desipramine before and concomitantly with mirabegron in 28 male and female healthy subjects.
Figures 1 and 2 show the magnitude of these interactions on the pharmacokinetic parameters and the recommendations for dose adjustment, if any:
Figure 1: The Effect of Coadministered Drugs on Exposure of Mirabegron and Dose Recommendation
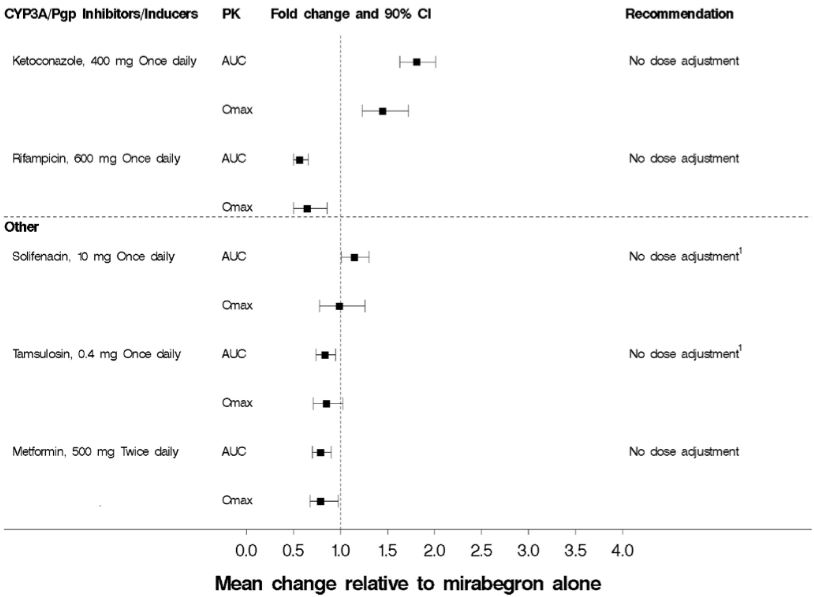
(1) Although no dose adjustment is recommended with solifenacin succinate or tamsulosin based on the lack of pharmacokinetic interaction, mirabegron should be administered with caution to patients taking muscarinic antagonist medications for the treatment of OAB and in patients with clinically significant BOO because of the risk of urinary retention [see Warnings and Precautions (5.2)].
Figure 2: The Effect of Mirabegron on Exposure of Coadministered Medication
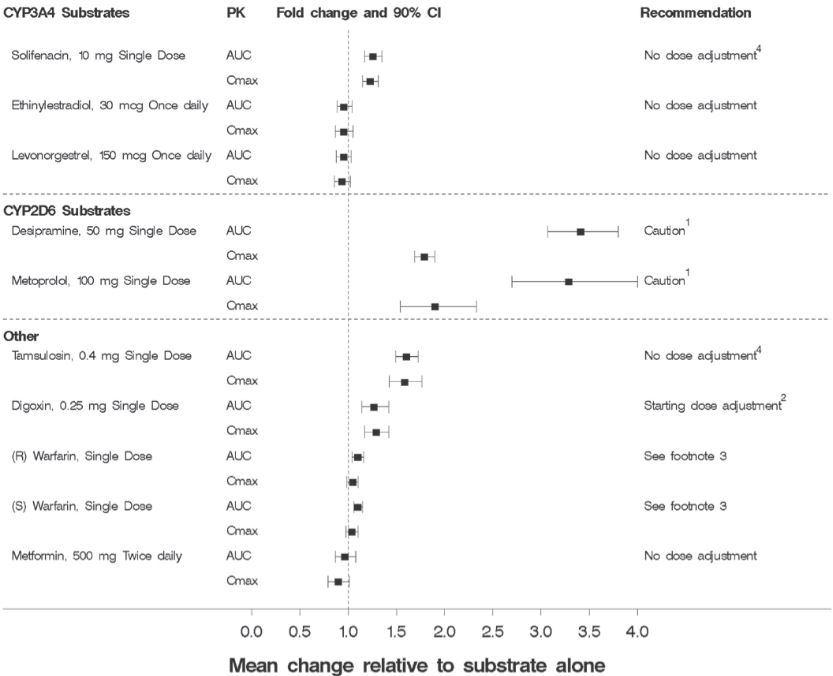
(1) Since mirabegron is a moderate CYP2D6 inhibitor, the systemic exposure to CYP2D6 substrates such as metoprolol and desipramine is increased when coadministered with mirabegron. Therefore, appropriate monitoring and dose adjustment may be necessary, especially with narrow therapeutic index CYP2D6 substrates, such as thioridazine, flecainide, and propafenone [see Warnings and Precautions (5.4) and Drug Interactions (7.1)].
(2) For patients who are initiating a combination of mirabegron and digoxin, the lowest dose for digoxin should initially be prescribed. Serum digoxin concentrations should be monitored and used for titration of the digoxin dose to obtain the desired clinical effect [see Drug Interactions (7.2)].
(3) Warfarin was administered as a single 25 mg dose of the racemate (a mixture of R-warfarin and S-warfarin). Based on this single-dose study, mirabegron had no effect on the warfarin pharmacodynamic endpoints such as INR and prothrombin time. However, the effect of mirabegron on multiple doses of warfarin and on warfarin pharmacodynamic end points such as INR and prothrombin time has not been fully investigated [see Drug Interactions (7.3)].
(4) Although no dose adjustment is recommended with solifenacin succinate or tamsulosin based on the lack of pharmacokinetic interaction, mirabegron should be administered with caution to patients taking muscarinic antagonist medications for the treatment of OAB and in BOO because of the risk of urinary retention [see Warnings and Precautions (5.2)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term carcinogenicity studies were conducted in rats and mice dosed orally with mirabegron for two years. Male rats were dosed at 0, 12.5, 25, or 50 mg/kg/day and female rats and both sexes of mice were dosed at 0, 25, 50, or 100 mg/kg/day. Mirabegron showed no carcinogenic potential at systemic exposures (AUC) 38 to 45-fold higher than the MRHD in rats and 21 to 38-fold higher than the MRHD in mice than the human systemic exposure at the 50 mg dose.
Mutagenesis
Mirabegron was not mutagenic in the Ames bacterial reverse mutation assay, did not induce chromosomal aberrations in human peripheral blood lymphocytes at concentrations that were not cytotoxic, and was not clastogenic in the rat micronucleus assay.
Impairment of Fertility
Fertility studies in rats showed that mirabegron had no effect on either male or female fertility at non-lethal doses up to 100 mg/kg/day. Systemic exposures (AUC) at 100 mg/kg in female rats was estimated to be 22-fold the MRHD in women and 93-fold the MRHD in men.
-
14 CLINICAL STUDIES
14.1 Mirabegron Monotherapy for Adult OAB
Mirabegron was evaluated in three, 12-week, double-blind, randomized, placebo-controlled, parallel group, multicenter clinical trials in patients with overactive bladder with symptoms of urge urinary incontinence, urgency, and urinary frequency (Studies 1, 2, and 3). Entry criteria required that patients had symptoms of overactive bladder for at least 3 months duration, at least 8 micturitions per day, and at least 3 episodes of urgency with or without incontinence over a 3-day period. The majority of patients were Caucasian (94%) and female (72%) with a mean age of 59 years (range 18 to 95 years). The population included both naïve patients who had not received prior muscarinic antagonist pharmacotherapy for overactive bladder (48%) and those who had received prior muscarinic antagonist pharmacotherapy for OAB (52%).
In Study 1 (NCT00689104), patients were randomized to placebo, mirabegron 50 mg, mirabegron 100 mg, or an active control once daily. In Study 2 (NCT00662909), patients were randomized to placebo, mirabegron 50 mg or mirabegron 100 mg once daily. In Study 3 (NCT00912964), patients were randomized to placebo, mirabegron 25 mg or mirabegron 50 mg once daily.
The co-primary efficacy endpoints in all 3 trials were (1) change from baseline to end of treatment (Week 12) in mean number of incontinence episodes per 24 hours and (2) change from baseline to end of treatment (Week 12) in mean number of micturitions per 24 hours, based on a 3-day micturition diary. An important secondary endpoint was the change from baseline to end of treatment (Week 12) in mean volume voided per micturition.
Results for the co-primary endpoints and mean volume voided per micturition from Studies 1, 2, and 3 are shown in Table 6.
Table 6: Mean Baseline and Change from Baseline at Week 12* for Incontinence Episodes, Micturition Frequency, and Volume Voided per Micturition in Patients with Overactive Bladder in Studies 1, 2, and 3
Parameter
Study 1
Study 2
Study 3
Placebo
Mirabegron 50mg
Placebo
Mirabegron 50mg
Placebo
Mirabegron 25mg
Mirabegron 50mg
Number of Incontinence Episodes per 24 Hours †
n
291
293
325
312
262
254
257
Baseline (mean)
2.67
2.83
3.03
2.77
2.43
2.65
2.51
Change from baseline (adjusted mean‡)
-1.17
-1.57
-1.13
-1.47
-0.96
-1.36
-1.38
Difference from placebo (adjusted mean‡)
--
-0.41
--
-0.34
--
-0.40
-0.42
95% Confidence Interval
--
(-0.72, -0.09)
--
(-0.66, -0.03)
--
(-0.74, -0.06)
(-0.76, -0.08)
p-value
--
0.003§
--
0.026§
--
0.005§
0.001§
Number of Micturitions per 24 Hours
n
480
473
433
425
415
410
426
Baseline (mean)
11.71
11.65
11.51
11.80
11.48
11.68
11.66
Change from baseline (adjusted mean‡)
-1.34
-1.93
-1.05
-1.66
-1.18
-1.65
-1.60
Difference from placebo (adjusted mean‡)
--
-0.60
--
-0.61
--
-0.47
-0.42
95% Confidence Interval
--
(-0.90, -0.29)
--
(-0.98, -0.24)
--
(-0.82, -0.13)
(-0.76, -0.08)
p-value
--
<0.001§
--
0.001§
--
0.007§
0.015§
Volume Voided (mL) per Micturition
n
480
472
433
424
415
410
426
Baseline (mean)
156.7
161.1
157.5
156.3
164.0
165.2
159.3
Change from baseline (adjusted mean‡)
12.3
24.2
7.0
18.2
8.3
12.8
20.7
Difference from placebo (adjusted mean‡)
--
11.9
--
11.1
--
4.6
12.4
95% Confidence Interval
--
(6.3, 17.4)
--
(4.4, 17.9)
--
(-1.6, 10.8)
(6.3, 18.6)
p-value
--
< 0.001§
--
0.001§
--
0.15
< 0.001§
* Week 12 is last observation on treatment.
† For incontinence episodes per 24 hours, the analysis population is restricted to patients with at least 1 episode of incontinence at baseline.
‡ Least squares mean adjusted for baseline, gender, and geographical region.
§ Statistically significantly superior compared to placebo at the 0.05 level with multiplicity adjustment.
Mirabegron 25 mg was effective in treating the symptoms of OAB within 8 weeks and mirabegron 50 mg was effective in treating the symptoms of OAB within 4 weeks. Efficacy of both 25 mg and 50 mg doses of mirabegron was maintained through the 12-week treatment period.
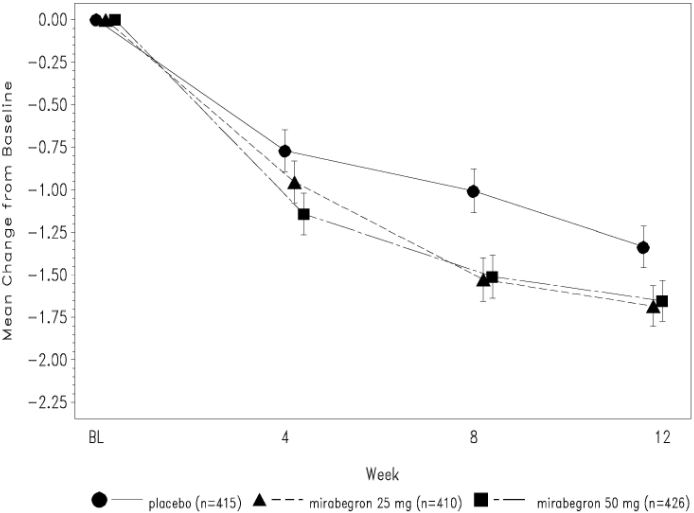
Figures 3 through 8 show the co-primary endpoints, mean change from baseline (BL) over time in number of incontinence episodes per 24 hours, and mean change from baseline over time in number of micturitions per 24 hours, in Studies 1, 2, and 3.
Figure 3: Mean (SE) Change from Baseline in Mean Number of Incontinence Episodes per 24 Hours – Study 1
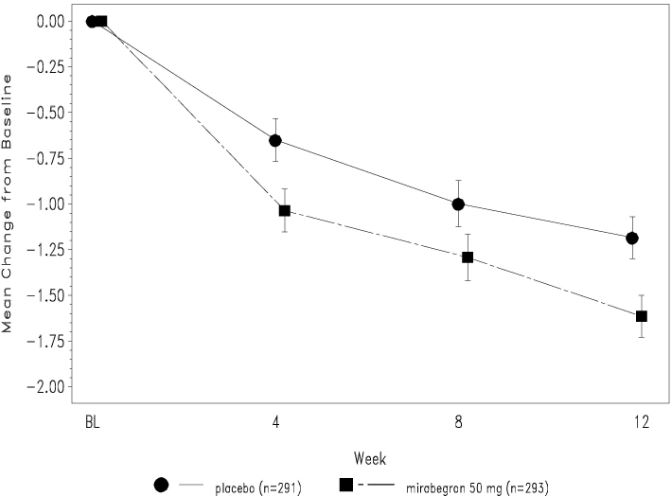
Figure 4: Mean (SE) Change from Baseline in Mean Number of Micturitions per 24 Hours - Study 1
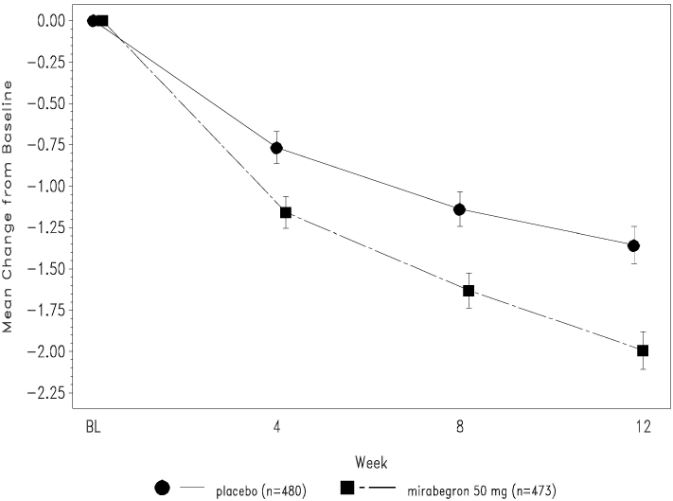
Figure 5: Mean (SE) Change from Baseline in Mean Number of Incontinence Episodes per 24 Hours - Study 2
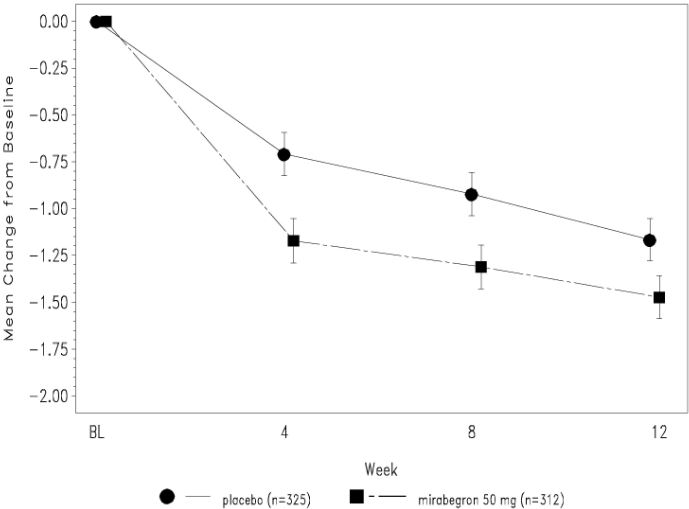
Figure 6: Mean (SE) Change from Baseline in Mean Number of Micturitions per 24 Hours - Study 2
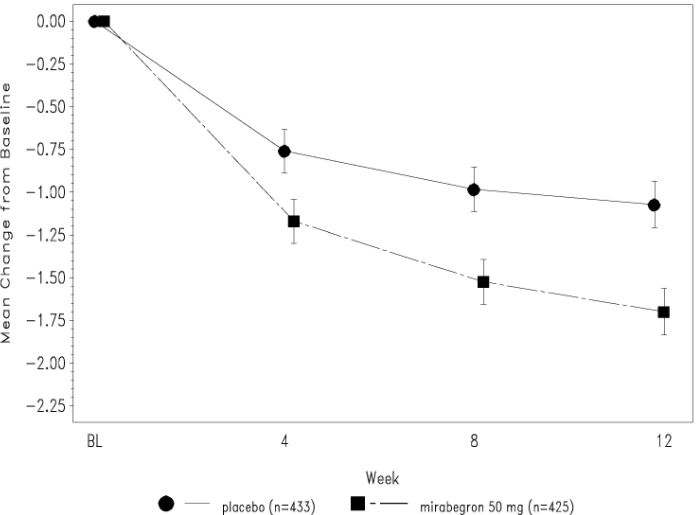
Figure 7: Mean (SE) Change from Baseline in Mean Number of Incontinence Episodes per 24 Hours - Study 3
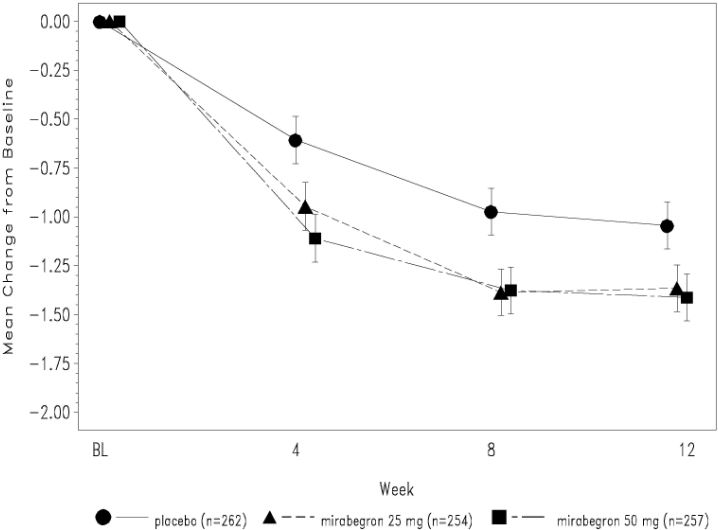
Figure 8: Mean (SE) Change from Baseline in Mean Number of Micturitions per 24 Hours - Study 3
14.3 Mirabegron for Pediatric Neurogenic Detrusor Overactivity (NDO)
efficacy of mirabegron was evaluated in Study 9 (NCT02751931), a 52-week, open-label, baseline-controlled, multicenter, dose titration study in pediatric patients 3 years of age and older for the treatment of neurogenic detrusor overactivity (NDO). Study 9 included patients 3 to 17 years of age. Entry criteria required that patients had a diagnosis of neurogenic detrusor overactivity (NDO) with involuntary detrusor contractions with detrusor pressure increase greater than 15 cm H2O and that patients or their caregivers practiced clean intermittent catheterization (CIC). Mirabegron were administered orally once daily. All patients initially received a weight-based starting dose equivalent to 25 mg daily dose followed by dose titration to a dose equivalent of 50 mg daily dose. The duration of the dose titration period was up to 8 weeks and this period was followed by a dose maintenance period that continued for the duration of the 52-week study.
In Study 9, a total of 86 patients 3 to 17 years of age received mirabegron. Of these, 71 patients completed treatment through week 24 and 70 completed 52 weeks of treatment. A total of 68 patients (43 patients 3 to less than 12 years of age and 25 patients 12 to 17 years of age) had valid urodynamic measurements for evaluation of efficacy. The study population included 39 males (45%) and 47 females (55%). The optimized maintenance dose within this study population included 94% of patients at the maximum dose, and 6% of patients at the starting dose.
The primary efficacy endpoint was change from baseline in the patients' maximum cystometric (bladder) capacity (MCC) after 24 weeks of treatment with mirabegron. As shown in Table 7, improvements in MCC were observed in patients 3 to less than 12 years of age and in patients 12 to 17 years of age. The magnitude of the observed changes from baseline in the primary and secondary efficacy endpoints were comparable between patients 3 to less than 12 years of age and patients 12 to 17 years of age.
Table 7: Change from Baseline in Maximum Cystometric Capacity (MCC) at 24 Weeks in Pediatric Patients with Neurogenic Detrusor Overactivity (NDO) Treated with Mirabegron in Study 9
Parameter
Children
Aged 3 to Less than 12 Years
(N=43)1
Mean (SD)
Adolescents
Aged 12 to 17 Years
(N=25)1
Mean (SD)
Maximum Cystometric Capacity (mL)
Baseline
159 (95)
239 (99)
Week 24
231 (129)
352 (125)
Change from baseline
72 (87)
113 (83)
95% CI
(45, 99)
(79, 147)
1. N is the number of patients who took at least one dose and provided valid values for MCC at Baseline and Week 24.
Secondary efficacy endpoints from Study 9 for mirabegron in pediatric patients with neurogenic detrusor overactivity (NDO) are shown below in Table 8 and Table 9.
Table 8: Changes from Baseline in Other Urodynamic Parameters at Week 24 in Pediatric Patients with Neurogenic Detrusor Overactivity (NDO) Treated with Mirabegron in Study 9
Parameter
Children
Aged 3 to Less than 12 Years
(N=43)1
Mean (SD)
Adolescents
Aged 12 to 17 Years
(N=25)1
Mean (SD)
Bladder Compliance (mL/cm H2O)2
Baseline
16.0 (55.8)
11.1 (10.7)
Change from baseline
14.6 (42.1)
95% CI: -0.3, 29.5
13.6 (15.0)
95% CI: 6.7, 20.4
Number of Overactive Detrusor Contractions (>15 cm H2O)2
Baseline
3.0 (4.0)
2.1 (3.1)
Change from baseline
-1.9 (4.2)
95% CI: -3.3, -0.4
-0.8 (3.9)
95% CI: -2.5, 0.9
Bladder Volume Prior To First Detrusor Contraction (>15 cm H2O)2
Baseline
115 (83)
177 (117)
Change from baseline
93 (88)
95% CI: 64, 122
121 (160)
95% CI: 54, 189
1. N is the number of patients who took at least one dose and provided valid values for MCC at Baseline and Week 24.
2. Number of patients (Children/Adolescents) with data available for both Baseline and Week 24; Bladder Compliance: n=33/21; Number of Overactive Detrusor Contractions: n=36/22; Bladder Volume Prior to First Detrusor Contraction: n=38/24.
Table 9: Changes from Baseline in Maximum Catheterized Urine Volume and Number of Leakage Episodes at Week 24 in Pediatric Patients with Neurogenic Detrusor Overactivity (NDO) Treated with Mirabegron in Study 9 Parameter
Children
Aged 3 to Less than 12 Years
(N=43)1
Mean (SD)
Adolescents
Aged 12 to 17 Years
(N=25)1
Mean (SD)
Maximum Catheterized Urine Volume per Day (mL)2
Baseline
304 (109)
360 (111)
Change from baseline
50 (104)
95% CI: 17, 83
84 (122)
95% CI: 32, 137
Number of Leakage Episodes per Day2
Baseline
2.8 (3.7)
1.8 (1.7)
Change from baseline
-2.0 (3.2)
95% CI: -3.2, -0.7
-1.0 (1.1)
95% CI: -1.5, -0.5
1. N is the number of patients who took at least one dose and provided valid values for MCC at Baseline and Week 24.
2. Number of patients (Children/Adolescents) with data available for both Baseline and Week 24; Maximum Catheterized Urine Volume per Day:
n=41/23; Number of Leakage Episodes per Day: n=26/21.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 Mirabegron extended-release tablets
Mirabegron extended-release tablets, 25mg are peach colored, oval shaped, biconvex, film-coated tablets debossed with "1159" on one side and plain on other side and are supplied as follows:
NDC: 70710-1159-3 in bottles of 30 tablets with child-resistant closure
NDC: 70710-1159-9 in bottles of 90 tablets with child-resistant closure
NDC: 70710-1159-1 in bottles of 100 tablets with child-resistant closure
Mirabegron extended-release tablets, 50mg are yellow colored, oval shaped, biconvex, film-coated tablets debossed with "1160" on one side and plain on other side and are supplied as follows:
NDC: 70710-1160-3 in bottles of 30 tablets with child-resistant closure
NDC: 70710-1160-9 in bottles of 90 tablets with child-resistant closure
NDC: 70710-1160-1 in bottles of 100 tablets with child-resistant closure
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
Advise the patient and/or caregiver to read the FDA-approved patient labeling (Patient Information).
Increases in Blood Pressure
Inform patients and/or their caregivers that mirabegron extended-release tablets may increase blood pressure. Advise patients, especially patients with hypertension, to periodically monitor their blood pressure and report increased measurement to their health care provider [see Warnings and Precautions (5.1)].
Urinary Retention
Inform patients and/or their caregivers that mirabegron may cause urinary retention in adult patients with bladder outlet obstruction and in patients taking muscarinic antagonist medications for the treatment of OAB. Advise patients to contact their physician if they experience these effects while taking mirabegron [see Warnings and Precautions (5.2)].
Angioedema
Inform patients and/or their caregivers that mirabegron may cause angioedema. Advise patients and/or their caregivers to promptly discontinue mirabegron and seek medical attention if angioedema associated with the upper airway swelling occurs as this may be life-threatening [see Warnings and Precautions (5.3)].
Drug Interactions
Advise patients to report their use of any other prescription or nonprescription medications or dietary supplements because co-administration with mirabegron may require a dose adjustment and/or increased monitoring of these drugs [see Drug Interactions (7)].
Administration Instructions
Mirabegron extended-release tablets
Advise adult patients to swallow mirabegron whole with water and not to chew, divide, or crush. Advise adult patients to take mirabegron with or without food.
Advise pediatric patients and/or their caregivers to swallow mirabegron extended-release tablets whole with water and not to chew, divide, or crush. Advise pediatric patients to take mirabegron extended-release tablets with food.
Missed Dose
Instruct patients and/or their caregivers to take any missed doses as soon as they remember, unless more than 12 hours have passed since the missed dose. If more than 12 hours have passed, the missed dose can be skipped and the next dose should be taken at the usual time.
Manufactured by:
Zydus Lifesciences Ltd.,
Matoda, Ahmedabad, India
Distributed by:
Zydus Pharmaceuticals (USA) Inc.
Pennington, NJ 08534
Revised: 10/2024
-
PATIENT INFORMATION
Patient Information
Mirabegron (mir" a beg' ron)
extended-release tablets for oral use
What are mirabegron extended-release tablets? Adults
Mirabegron extended-release tablets is a prescription medicine that can be used to treat adults with the following symptoms due to a condition called overactive bladder (OAB):
○ Urge urinary incontinence: a strong need to urinate with leaking or wetting accidents
○ Urgency: a strong need to urinate right away
○ Frequency: urinating often
Children
Mirabegron extended-release tablet is a prescription medicine used to treat children 3 years of age and older weighing at least 77 pounds (35 kg) , with a condition called neurogenic detrusor overactivity (NDO) .
It is not known if mirabegron extended-release tablets are safe and effective in children under 3 years of age.
Who should not take mirabegron extended-release tablets?
Do not take mirabegron extended-release tablets if you are allergic to mirabegron or any of the ingredients in mirabegron extended-release tablets. See the end of this Patient Information leaflet for a complete list of ingredients in mirabegron extended-release tablets.
Before you take mirabegron extended-release tablets, tell your doctor about all of your medical conditions, including if you :
have liver problems.
have kidney problems.
have very high uncontrolled blood pressure.
have trouble emptying your bladder or you have a weak urine stream.
are pregnant or plan to become pregnant. It is not known if mirabegron extended-release tablets will harm your unborn baby. Talk to your doctor if you are pregnant or plan to become pregnant.
are breastfeeding or plan to breastfeed. It is not known if mirabegron passes into your breast milk. Talk to your doctor about the best way to feed your baby if you take mirabegron extended-release tablets.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Mirabegron extended-release tablets may affect the way other medicines work, and other medicines may affect how mirabegron extended-release tablets work.
Especially tell your doctor if you take:
thioridazine (Mellaril or Mellaril-S)
flecainide (Tambocor)
propafenone (Rythmol)
digoxin (Lanoxin)
How should I take mirabegron extended-release tabl ets ?
Take mirabegron extended-release tablets exactly as your doctor tells you to take it.
You should take 1 mirabegron extended-release tablet 1 time a day
You should take mirabegron extended-release tablet with water and swallow the tablet whole.
Do not chew, break, or crush the tablet.
Adults can take mirabegron extended-release tablet with or without food.
Children should take mirabegron extended-release tablet with food .
If you miss a dose of mirabegron extended-release tablets, take it as soon as possible. If it has been more than 12 hours since taking the last dose of mirabegron extended-release tablets, skip that dose and take the next dose at the usual time.
If you take too much mirabegron extended-release tablets, call your doctor or go to the nearest hospital emergency room right away.
What are the possible side effects of mirabegron extended-release tablets? Mirabegron extended-release tablets may cause serious side effects, including:
increased blood pressure. Mirabegron extended-release tablets may cause your blood pressure to increase or make your blood pressure worse if you have a history of high blood pressure. You and your doctor should check your blood pressure while you are taking mirabegron extended-release tablets. Call your doctor if you have increased blood pressure.
inability to empty your bladder (urinary retention). Mirabegron extended-release tablets may increase your chances of not being able to empty your bladder if you have bladder outlet obstruction or if you are taking other medicines to treat overactive bladder. Tell your doctor right away if you are unable to empty your bladder.
angioedema. Mirabegron extended-release tablets may cause an allergic reaction with swelling of the lips, face, tongue, or throat with or without difficulty breathing. Stop using mirabegron extended-release tablets and go to the nearest hospital emergency room right away.
Adults with Overactive Bladder
The most common side effects of mirabegron extended-release tablets include:
high blood pressure
pain or swelling of the nose or throat (nasopharyngitis)
urinary tract infection
headache
Children with Neurogenic Detrusor Overactivity
The most common side effects of mirabegron extended-release tablets include:
urinary tract infection
pain or swelling of the nose or throat (nasopharyngitis)
constipation
headache
Tell your doctor if you have any side effect that bothers you, does not go away, or if you have swelling of the face, lips, tongue or throat, hives, skin rash or itching while taking mirabegron extended-release tablets.
These are not all the possible side effects of mirabegron extended-release tablets. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
How should I store mirabegron extended-release tablets?
Store mirabegron extended-release tablets between 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature]. Keep the bottle closed.
Throw away (discard) medicine that is out of date or no longer needed.
Keep mirabegron extended-release tablets and all medicines out of the reach of children.
General information about the safe and effective use of mirabegron extended-release tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use mirabegron extended-release tablets for a condition for which it was not prescribed. Do not give mirabegron extended-release tablets to other people, even if they have the same symptoms you have. It may harm them.
This leaflet summarizes the most important information about mirabegron extended-release tablets. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about mirabegron extended-release tablets that is written for health professionals.
For more information, email (MedicalAffairs@zydususa.com) or call (Tel: 1-877-993-8779).
What are the ingredients in mirabegron extended-release tablets?
Active ingredient: mirabegron
Inactive ingredients: polyethylene oxide, polyethylene glycol, magnesium stearate, hypromellose, ferrosoferric oxide, yellow iron oxide, and red iron oxide (25 mg mirabegron extended-release tablet only).
All trademarks or registered trademarks are the property of their respective owners.
Manufactured by:
Zydus Lifesciences Ltd.,
Matoda, Ahmedabad, India
Distributed by:
Zydus Pharmaceuticals (USA) Inc.
Pennington, NJ 08534
This Patient Information has been approved by the U.S. Food and Drug Administration.
Revised: 10/2024
-
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Mirabegron extended-release tablets, 25mg
NDC: 70710-1159-3 in bottles of 30 tablets
30 Tablets
Rx only
Mirabegron extended-release tablets, 50 mg
NDC: 70710-1160-3 in bottles of 30 tablets
30 Tablets
Rx only
-
INGREDIENTS AND APPEARANCE
MIRABEGRON
mirabegron tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70710-1159 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MIRABEGRON (UNII: MVR3JL3B2V) (MIRABEGRON - UNII:MVR3JL3B2V) MIRABEGRON 25 mg Inactive Ingredients Ingredient Name Strength FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERROSOFERRIC OXIDE (UNII: XM0M87F357) HYPROMELLOSE 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYETHYLENE GLYCOL 6000 (UNII: 30IQX730WE) POLYETHYLENE GLYCOL 8000 (UNII: Q662QK8M3B) POLYETHYLENE OXIDE 200000 (UNII: 11628IH70O) POLYETHYLENE OXIDE 2000000 (UNII: 5K3991GVWI) Product Characteristics Color PINK (Peach colored) Score no score Shape OVAL Size 12mm Flavor Imprint Code 1159 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70710-1159-3 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/23/2024 2 NDC: 70710-1159-9 90 in 1 BOTTLE; Type 0: Not a Combination Product 01/23/2024 3 NDC: 70710-1159-1 100 in 1 BOTTLE; Type 0: Not a Combination Product 01/23/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209488 01/23/2024 MIRABEGRON
mirabegron tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70710-1160 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MIRABEGRON (UNII: MVR3JL3B2V) (MIRABEGRON - UNII:MVR3JL3B2V) MIRABEGRON 50 mg Inactive Ingredients Ingredient Name Strength FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERROSOFERRIC OXIDE (UNII: XM0M87F357) HYPROMELLOSE 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYETHYLENE GLYCOL 6000 (UNII: 30IQX730WE) POLYETHYLENE GLYCOL 8000 (UNII: Q662QK8M3B) POLYETHYLENE OXIDE 200000 (UNII: 11628IH70O) POLYETHYLENE OXIDE 2000000 (UNII: 5K3991GVWI) Product Characteristics Color YELLOW Score no score Shape OVAL Size 12mm Flavor Imprint Code 1160 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70710-1160-3 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/23/2024 2 NDC: 70710-1160-9 90 in 1 BOTTLE; Type 0: Not a Combination Product 01/23/2024 3 NDC: 70710-1160-1 100 in 1 BOTTLE; Type 0: Not a Combination Product 01/23/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209488 01/23/2024 Labeler - Zydus Pharmaceuticals (USA) Inc. (156861945) Registrant - Zydus Pharmaceuticals (USA) Inc. (156861945) Establishment Name Address ID/FEI Business Operations Zydus Lifesciences Limited 863362789 ANALYSIS(70710-1159, 70710-1160) , MANUFACTURE(70710-1159, 70710-1160)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.