METRONIDAZOLE- metronidazole tablet
Metronidazole by
Drug Labeling and Warnings
Metronidazole by is a Prescription medication manufactured, distributed, or labeled by STAT Rx USA LLC, PSS World Medical Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
SPL UNCLASSIFIED SECTION
333
334
Rev. A 6/2011
Rx only
To reduce the development of drug-resistant bacteria and maintain the effectiveness of metronidazole and other antibacterial drugs, metronidazole should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
WARNING
Metronidazole has been shown to be carcinogenic in mice and rats (see PRECAUTIONS). Unnecessary use of the drug should be avoided. Its use should be reserved for the conditions described in the INDICATIONS AND USAGE section below.
-
DESCRIPTION
Metronidazole, USP is an oral synthetic antiprotozoal and antibacterial agent, 1-(β-hydroxyethyl)-2-methyl-5-nitroimidazole, which has the following structural formula:
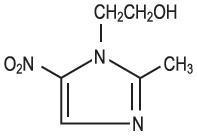
C6H9N3O3 M.W. 171.15
Each tablet for oral administration contains 250 mg or 500 mg of metronidazole, USP. Inactive ingredients include microcrystalline cellulose, crospovidone, colloidal silicon dioxide and hydrogenated vegetable oil.
-
CLINICAL PHARMACOLOGY
Disposition of metronidazole in the body is similar for both oral and intravenous dosage forms, with an average elimination half-life in healthy humans of eight hours.
The major route of elimination of metronidazole and its metabolites is via the urine (60 to 80% of the dose), with fecal excretion accounting for 6 to 15% of the dose. The metabolites that appear in the urine result primarily from side-chain oxidation [1-(β-hydroxyethyl)-2-hydroxymethyl-5-nitroimidazole and 2-methyl-5-nitroimidazole-1-yl-acetic acid] and glucuronide conjugation, with unchanged metronidazole accounting for approximately 20% of the total. Renal clearance of metronidazole is approximately 10 mL/min/1.73 m2.
Metronidazole is the major component appearing in the plasma, with lesser quantities of the 2-hydroxymethyl metabolite also being present. Less than 20% of the circulating metronidazole is bound to plasma proteins. Both the parent compound and the metabolite possess in vitro bactericidal activity against most strains of anaerobic bacteria and in vitro trichomonacidal activity.
Metronidazole appears in cerebrospinal fluid, saliva, and human milk in concentrations similar to those found in plasma. Bactericidal concentrations of metronidazole have also been detected in pus from hepatic abscesses.
Following oral administration, metronidazole is well absorbed, with peak plasma concentrations occurring between one and two hours after administration.
Plasma concentrations of metronidazole are proportional to the administered dose. Oral administration of 250 mg, 500 mg, or 2,000 mg produced peak plasma concentrations of 6 mcg/mL, 12 mcg/mL, and 40 mcg/mL, respectively. Studies reveal no significant bioavailability differences between males and females; however, because of weight differences, the resulting plasma levels in males are generally lower.
Decreased renal function does not alter the single-dose pharmacokinetics of metronidazole. However, plasma clearance of metronidazole is decreased in patients with decreased liver function.
Microbiology
Trichomonas vaginalis, Entamoeba histolytica
Metronidazole possesses direct trichomonacidal and amebacidal activity against T. vaginalis and E. histolytica. The in vitro minimal inhibitory concentration (MIC) for most strains of these organisms is 1 mcg/mL or less.
Anaerobic Bacteria
Metronidazole is active in vitro against most obligate anaerobes but does not appear to possess any clinically relevant activity against facultative anaerobes or obligate aerobes. Against susceptible organisms, metronidazole is generally bactericidal at concentrations equal to or slightly higher than the minimal inhibitory concentrations. Metronidazole has been shown to have in vitro and clinical activity against the following organisms:
Anaerobic gram-negative bacilli, including:
Bacteroides species including the Bacteroides fragilis group (B. fragilis, B. distasonis, B.ovatus, B. thetaiotaomicron, B. vulgatus)
Fusobacterium species
Anaerobic gram-positive bacilli, including:
Clostridium species and susceptible strains of Eubacterium
Anaerobic gram-positive cocci, including:
Peptococcus niger
Peptostreptococcus species
Susceptibility Tests
Bacteriologic studies should be performed to determine the causative organisms and their susceptibility to metronidazole; however, the rapid, routine susceptibility testing of individual isolates of anaerobic bacteria is not always practical, and therapy may be started while awaiting these results.
Quantitative methods give the most precise estimates of susceptibility to antibacterial drugs. A standardized agar dilution method and a broth microdilution method are recommended.1
Control strains are recommended for standardized susceptibility testing. Each time the test is performed, one or more of the following strains should be included: Clostridium perfringens ATCC 13124, Bacteroides fragilis ATCC 25285, and Bacteroides thetaiotaomicron ATCC 29741. The mode metronidazole MICs for those three strains are reported to be 0.25, 0.25, and 0.5 mcg/mL, respectively.
A clinical laboratory is considered under acceptable control if the results of the control strains are within one doubling dilution of the mode MICs reported for metronidazole.
A bacterial isolate may be considered susceptible if the MIC value for metronidazole is not more than 16 mcg/mL. An organism is considered resistant if the MIC is greater than 16 mcg/mL. A report of “resistant” from the laboratory indicates that the infecting organism is not likely to respond to therapy.
-
INDICATIONS AND USAGE
Symptomatic Trichomoniasis
Metronidazole, USP is indicated for the treatment of symptomatic trichomoniasis in females and males when the presence of the trichomonad has been confirmed by appropriate laboratory procedures (wet smears and/or cultures).
Asymptomatic Trichomoniasis
Metronidazole, USP is indicated in the treatment of asymptomatic females when the organism is associated with endocervicitis, cervicitis, or cervical erosion. Since there is evidence that presence of the trichomonad can interfere with accurate assessment of abnormal cytological smears, additional smears should be performed after eradication of the parasite.
Treatment of Asymptomatic Consorts
T. vaginalis infection is a venereal disease. Therefore, asymptomatic sexual partners of treated patients should be treated simultaneously if the organism has been found to be present, in order to prevent reinfection of the partner. The decision as to whether to treat an asymptomatic male partner who has a negative culture or one for whom no culture has been attempted is an individual one. In making this decision, it should be noted that there is evidence that a woman may become reinfected if her consort is not treated. Also, since there can be considerable difficulty in isolating the organism from the asymptomatic male carrier, negative smears and cultures cannot be relied upon in this regard. In any event, the consort should be treated with metronidazole, USP in cases of reinfection.
Amebiasis
Metronidazole, USP is indicated in the treatment of acute intestinal amebiasis (amebic dysentery) and amebic liver abscess. In amebic liver abscess, metronidazole, USP therapy does not obviate the need for aspiration or drainage of pus.
Anaerobic Bacterial Infections
Metronidazole, USP is indicated in the treatment of serious infections caused by susceptible anaerobic bacteria. Indicated surgical procedures should be performed in conjunction with metronidazole, USP therapy. In a mixed aerobic and anaerobic infection, antimicrobials appropriate for the treatment of the aerobic infection should be used in addition to metronidazole, USP.
In the treatment of most serious anaerobic infections, the intravenous form of metronidazole, USP is usually administered initially. This may be followed by oral therapy with metronidazole, USP at the discretion of the physician.
INTRA-ABDOMINAL INFECTIONS, including peritonitis, intra-abdominal abscess, and liver abscess, caused by Bacteroides species including the B. fragilis group (B. fragilis,B. distasonis, B. ovatus, B. thetaiotaomicron, B. vulgatus), Clostridium species, Eubacterium species, Peptococcus niger, and Peptostreptococcus species.
SKIN AND SKIN STRUCTURE INFECTIONS caused by Bacteroides species including the B. fragilis group, Clostridium species, Peptococcus niger, Peptostreptococcus species, and Fusobacterium species.
GYNECOLOGIC INFECTIONS, including endometritis, endomyometritis, tubo-ovarian abscess, and postsurgical vaginal cuff infection, caused by Bacteroides species including the B.fragilis group, Clostridium species, Peptococcus niger, and Peptostreptococcus species.
BACTERIAL SEPTICEMIA caused by Bacteroides species including the B. fragilis group, and Clostridium species.
BONE AND JOINT INFECTIONS, as adjunctive therapy, caused by Bacteroides species including the B. fragilis group.
CENTRAL NERVOUS SYSTEM (CNS) INFECTIONS, including meningitis and brain abscess, caused by Bacteroides species including the B. fragilis group.
LOWER RESPIRATORY TRACT INFECTIONS, including pneumonia, empyema, and lung abscess, caused by Bacteroides species including the B. fragilis group.
ENDOCARDITIS caused by Bacteroides species including the B. fragilis group.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of metronidazole, USP and other antibacterial drugs, metronidazole, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
-
CONTRAINDICATIONS
Metronidazole is contraindicated in patients with a prior history of hypersensitivity to metronidazole or other nitroimidazole derivatives.
In patients with trichomoniasis, metronidazole is contraindicated during the first trimester of pregnancy (see WARNINGS).
-
WARNINGS
Central and Peripheral Nervous System Effects
Convulsive seizures, encephalopathy, aseptic meningitis, optic and peripheral neuropathy, the latter characterized mainly by numbness or paresthesia of an extremity, have been reported in patients treated with metronidazole. The appearance of abnormal neurologic signs demands the prompt discontinuation of metronidazole therapy. Metronidazole should be administered with caution to patients with central nervous system diseases.
-
PRECAUTIONS
General
Patients with severe hepatic disease metabolize metronidazole slowly, with resultant accumulation of metronidazole and its metabolites in the plasma. Accordingly, for such patients, doses below those usually recommended should be administered cautiously.
Known or previously unrecognized candidiasis may present more prominent symptoms during therapy with metronidazole and requires treatment with a candidacidal agent.
Prescribing metronidazole in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Information for Patients
Alcoholic beverages should be avoided while taking metronidazole and for at least one day afterward (see Drug Interactions).
Patients should be counseled that antibacterial drugs including metronidazole should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When metronidazole is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by metronidazole or other antibacterial drugs in the future.
Laboratory Tests
Metronidazole is a nitroimidazole and should be used with caution in patients with evidence of or history of blood dyscrasia. A mild leukopenia has been observed during its administration; however, no persistent hematologic abnormalities attributable to metronidazole have been observed in clinical studies. Total and differential leukocyte counts are recommended before and after therapy for trichomoniasis and amebiasis, especially if a second course of therapy is necessary, and before and after therapy for anaerobic infections.
Drug Interactions
Metronidazole has been reported to potentiate the anticoagulant effect of warfarin and other oral coumarin anticoagulants, resulting in a prolongation of prothrombin time. This possible drug interaction should be considered when metronidazole is prescribed for patients on this type of anticoagulant therapy.
The simultaneous administration of drugs that induce microsomal liver enzymes, such as phenytoin or phenobarbital, may accelerate the elimination of metronidazole, resulting in reduced plasma levels; impaired clearance of phenytoin has also been reported.
The simultaneous administration of drugs that decrease microsomal liver enzyme activity, such as cimetidine, may prolong the half-life and decrease plasma clearance of metronidazole. In patients stabilized on relatively high doses of lithium, short-term metronidazole therapy has been associated with elevation of serum lithium, and in a few cases, signs of lithium toxicity. Serum lithium and serum creatinine levels should be obtained several days after beginning metronidazole to detect any increase that may precede clinical symptoms of lithium intoxication.
Alcoholic beverages should not be consumed during metronidazole therapy and for at least one day afterward because abdominal cramps, nausea, vomiting, headaches, and flushing may occur.
Psychotic reactions have been reported in alcoholic patients who are using metronidazole and disulfiram concurrently. Metronidazole should not be given to patients who have taken disulfiram within the last two weeks.
Drug/Laboratory Test Interactions
Metronidazole may interfere with certain types of determinations of serum chemistry values, such as aspartate aminotransferase (AST, SGOT), alanine aminotransferase (ALT, SGPT), lactate dehydrogenase (LDH), triglycerides, and hexokinase glucose. Values of zero may be observed. All of the assays in which interference has been reported involve enzymatic coupling of the assay to oxidation-reduction of nicotinamide adenine dinucleotide (NAD+
 NADH). Interference is due to the similarity in absorbance peaks of NADH (340 nm) and metronidazole (322 nm) at pH 7.
NADH). Interference is due to the similarity in absorbance peaks of NADH (340 nm) and metronidazole (322 nm) at pH 7.Carcinogenesis, Mutagenesis, Impairment of Fertility
Metronidazole has shown evidence of carcinogenic activity in a number of studies involving chronic, oral administration in mice and rats.
Prominent among the effects in the mouse was the promotion of pulmonary tumorigenesis. This has been observed in all six reported studies in that species, including one study in which the animals were dosed on an intermittent schedule (administration during every fourth week only). At very high dose levels (approx. 500 mg/kg/day which is approximately 33 times the most frequently recommended human dose for a 50 kg adult based on mg/kg body weight) there was a statistically significant increase in the incidence of malignant liver tumors in males. Also, the published results of one of the mouse studies indicate an increase in the incidence of malignant lymphomas as well as pulmonary neoplasms associated with lifetime feeding of the drug. All these effects are statistically significant.
Several long-term, oral-dosing studies in the rat have been completed. There were statistically significant increases in the incidence of various neoplasms, particularly in mammary and hepatic tumors, among female rats administered metronidazole over those noted in the concurrent female control groups.
Two lifetime tumorigenicity studies in hamsters have been performed and reported to be negative.
Although metronidazole has shown mutagenic activity in a number of in vitro assay systems, studies in mammals (in vivo) have failed to demonstrate a potential for genetic damage.
Fertility studies have been performed in mice at doses up to six times the maximum recommended human dose based on mg/m2 and have revealed no evidence of impaired fertility.
Pregnancy
Teratogenic Effects
Pregnancy Category B
Metronidazole crosses the placental barrier and enters the fetal circulation rapidly. Reproduction studies have been performed in rats at doses up to five times the human dose and have revealed no evidence of impaired fertility or harm to the fetus due to metronidazole. No fetotoxicity was observed when metronidazole was administered orally to pregnant mice at 20 mg/kg/day, approximately one and a half times the most frequently recommended human dose (750 mg/day) based on mg/kg body weight; however in a single small study where the drug was administered intraperitoneally, some intrauterine deaths were observed. The relationship of these findings to the drug is unknown. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, and because metronidazole is a carcinogen in rodents, this drug should be used during pregnancy only if clearly needed.
Use of metronidazole for trichomoniasis during pregnancy should be restricted to those in whom alternative treatment has been inadequate. Use of metronidazole for trichomoniasis in pregnancy should be carefully evaluated because metronidazole crosses the placental barrier and its effects on the human fetal organogenesis are not known (see above).
Nursing Mothers
Because of the potential for tumorigenicity, shown for metronidazole in mouse and rat studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. Metronidazole is secreted in human milk in concentrations similar to those found in plasma.
Geriatric Use
Decreased renal function does not alter the single-dose pharmacokinetics of metronidazole. However, plasma clearance of metronidazole is decreased in patients with decreased liver function. Therefore, in elderly patients, monitoring of serum levels may be necessary to adjust the metronidazole dosage accordingly.
-
ADVERSE REACTIONS
The most serious adverse reactions reported in patients treated with metronidazole have been convulsive seizures, encephalopathy, aseptic meningitis, optic and peripheral neuropathy, the latter characterized mainly by numbness or paresthesia of an extremity. Since persistent peripheral neuropathy has been reported in some patients receiving prolonged administration of metronidazole, patients should be specifically warned about these reactions and should be told to stop the drug and report immediately to their physicians if any neurologic symptoms occur.
The most common adverse reactions reported have been referable to the gastrointestinal tract, particularly nausea reported by about 12% of patients, sometimes accompanied by headache, anorexia, and occasionally vomiting; diarrhea; epigastric distress; and abdominal cramping. Constipation has also been reported.
The following reactions have also been reported during treatment with metronidazole:
Mouth: A sharp, unpleasant metallic taste is not unusual. Furry tongue, glossitis, and stomatitis have occurred; these may be associated with a sudden overgrowth of Candida which may occur during therapy.
Hematopoietic: Reversible neutropenia (leukopenia); rarely, reversible thrombocytopenia.
Cardiovascular: Flattening of the T-wave may be seen in electrocardiographic tracings.
Central Nervous System: Encephalopathy, aseptic meningitis, convulsive seizures, optic neuropathy, peripheral neuropathy, dizziness, vertigo, incoordination, ataxia, confusion, dysarthria, irritability, depression, weakness, and insomnia.
Hypersensitivity: Urticaria, erythematous rash, Stevens-Johnson Syndrome, toxic epidermal necrolysis, flushing, nasal congestion, dryness of the mouth (or vagina or vulva), and fever.
Renal: Dysuria, cystitis, polyuria, incontinence, and a sense of pelvic pressure. Instances of darkened urine have been reported by approximately one patient in 100,000. Although the pigment which is probably responsible for this phenomenon has not been positively identified, it is almost certainly a metabolite of metronidazole and seems to have no clinical significance.
Other: Proliferation of Candida in the vagina, dyspareunia, decrease of libido, proctitis, and fleeting joint pains sometimes resembling “serum sickness.” If patients receiving metronidazole drink alcoholic beverages, they may experience abdominal distress, nausea, vomiting, flushing, or headache. A modification of the taste of alcoholic beverages has also been reported. Rare cases of pancreatitis, which generally abated on withdrawal of the drug, have been reported.
Crohn’s disease patients are known to have an increased incidence of gastrointestinal and certain extraintestinal cancers. There have been some reports in the medical literature of breast and colon cancer in Crohn’s disease patients who have been treated with metronidazole at high doses for extended periods of time. A cause and effect relationship has not been established. Crohn’s disease is not an approved indication for metronidazole.
-
OVERDOSAGE
Single oral doses of metronidazole, up to 15 g, have been reported in suicide attempts and accidental overdoses. Symptoms reported include nausea, vomiting, and ataxia.
Oral metronidazole has been studied as a radiation sensitizer in the treatment of malignant tumors. Neurotoxic effects, including seizures and peripheral neuropathy, have been reported after 5 to 7 days of doses of 6 to 10.4 g every other day.
-
DOSAGE AND ADMINISTRATION
In elderly patients, the pharmacokinetics of metronidazole may be altered, and, therefore, monitoring of serum levels may be necessary to adjust the metronidazole dosage accordingly.
Trichomoniasis
In the Female
One-day treatment
Two grams of metronidazole, given either as a single-dose or in two divided doses of one gram each given in the same day.
Seven-day course of treatment
250 mg three times daily for seven consecutive days.
There is some indication from controlled comparative studies that cure rates as determined by vaginal smears, signs and symptoms, may be higher after a seven-day course of treatment than after a one-day treatment regimen.
The dosage regimen should be individualized. Single-dose treatment can assure compliance, especially if administered under supervision, in those patients who cannot be relied on to continue the seven-day regimen. A seven-day course of treatment may minimize reinfection by protecting the patient long enough for the sexual contacts to obtain appropriate treatment. Further, some patients may tolerate one treatment regimen better than the other.
Pregnant patients should not be treated during the first trimester (see CONTRAINDICATIONS). In pregnant patients in whom alternative treatment has been inadequate, the one-day course of therapy should not be used, as it results in higher serum levels which can reach the fetal circulation (see PRECAUTIONS, Pregnancy).
When repeat courses of the drug are required, it is recommended that an interval of four to six weeks elapse between courses and that the presence of the trichomonad be reconfirmed by appropriate laboratory measures. Total and differential leukocyte counts should be made before and after re-treatment.
Amebiasis
Anaerobic Bacterial Infections
In the treatment of most serious anaerobic infections, the intravenous form of metronidazole is usually administered initially.
The usual adult oral dosage is 7.5 mg/kg every six hours (approx. 500 mg for a 70-kg adult). A maximum of 4 g should not be exceeded during a 24-hour period.
The usual duration of therapy is 7 to 10 days; however, infections of the bone and joint, lower respiratory tract, and endocardium may require longer treatment.
Patients with severe hepatic disease metabolize metronidazole slowly, with resultant accumulation of metronidazole and its metabolites in the plasma. Accordingly, for such patients, doses below those usually recommended should be administered cautiously. Close monitoring of plasma metronidazole levels2 and toxicity is recommended.
The dose of metronidazole should not be specifically reduced in anuric patients since accumulated metabolites may be rapidly removed by dialysis.
-
HOW SUPPLIED
Metronidazole tablets USP are available as follows:
250 mg - White, round, convex tablets debossed “PLIVA 333” on one side and unscored on the other side. Available in:
Bottles of 28 - NDC # 16590-385-28
Bottles of 30 - NDC # 16590-385-30
500 mg - White, oblong, convex tablets debossed “PLIVA 334” on one side and unscored on the other side. Available in:
Bottles of 04 - NDC # 16590-152-04
Bottles of 14 - NDC # 16590-152-14
Bottles of 20 - NDC # 16590-152-20
Bottles of 21 - NDC # 16590-152-21
Bottles of 28 - NDC # 16590-152-28
Bottles of 30 - NDC # 16590-152-30
Storage and Stability
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
PROTECT FROM LIGHT
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
______________________________________________________________________________
1. Proposed standard: PSM-11-Proposed Reference Dilution Procedure for Antimicrobic Susceptibility Testing of Anaerobic Bacteria, National Committee for Clinical Laboratory Standards; and Sutter, et al.: Collaborative Evaluation of a Proposed Reference Dilution Method of Susceptibility Testing of Anaerobic Bacteria, Antimicrob. Agents Chemother. 16:495-502 (Oct.) 1979; and Tally, et al.: In Vitro Activity of Thienamycin, Antimicrob. Agents Chemother. 14:436-438 (Sept.) 1978.
2. Ralph, E.D., and Kirby, W.M.M.: Bioassay of Metronidazole With Either Anaerobic or Aerobic Incubation, J. Infect. Dis. 132:587-591 (Nov.) 1975; or Gulaid, et al.: Determination of Metronidazole and Its Major Metabolites in Biological Fluids by High Pressure Liquid Chromatography, Br. J. Clin. Pharmacol. 6:430-432, 1978.
Manufactured In Czech Republic By:
TEVA CZECH INDUSTRIES s.r.o.
Opava-Komarov, Czech Republic
Manufactured For:
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. A 6/2011
Relabeling and Repackaging by:
STAT Rx USA LLC
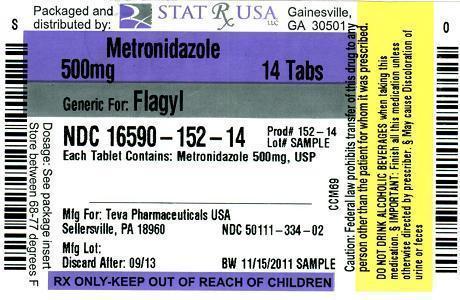
Gainesville, GA 30501 - PACKAGE LABEL - METRONIDAZOLE 250 MG TABLETS
- PACKAGE LABEL - METRONIDAZOLE 500 MG TABLETS
-
INGREDIENTS AND APPEARANCE
METRONIDAZOLE
metronidazole tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 16590-385(NDC:50111-333) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METRONIDAZOLE (UNII: 140QMO216E) (METRONIDAZOLE - UNII:140QMO216E) METRONIDAZOLE 250 mg Inactive Ingredients Ingredient Name Strength CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) CROSPOVIDONE (UNII: 68401960MK) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) HYDROGENATED COTTONSEED OIL (UNII: Z82Y2C65EA) Product Characteristics Color WHITE Score no score Shape ROUND Size 9mm Flavor Imprint Code PLIVA;333 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 16590-385-28 28 in 1 BOTTLE 2 NDC: 16590-385-30 30 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA070027 09/30/1990 METRONIDAZOLE
metronidazole tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 16590-152(NDC:50111-334) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METRONIDAZOLE (UNII: 140QMO216E) (METRONIDAZOLE - UNII:140QMO216E) METRONIDAZOLE 500 mg Inactive Ingredients Ingredient Name Strength CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) CROSPOVIDONE (UNII: 68401960MK) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) HYDROGENATED COTTONSEED OIL (UNII: Z82Y2C65EA) Product Characteristics Color WHITE Score no score Shape OVAL (oblong) Size 16mm Flavor Imprint Code PLIVA;334 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 16590-152-04 04 in 1 BOTTLE 2 NDC: 16590-152-14 14 in 1 BOTTLE 3 NDC: 16590-152-20 20 in 1 BOTTLE 4 NDC: 16590-152-21 21 in 1 BOTTLE 5 NDC: 16590-152-28 28 in 1 BOTTLE 6 NDC: 16590-152-30 30 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA070033 09/30/1990 Labeler - STAT Rx USA LLC (786036330) Registrant - PSS World Medical Inc. (101822682) Establishment Name Address ID/FEI Business Operations STAT Rx USA LLC 786036330 relabel(16590-385, 16590-152) , repack(16590-385, 16590-152)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.