Xepi by Cutanea Life Sciences, Inc. XEPI- ozenoxacin cream
Xepi by
Drug Labeling and Warnings
Xepi by is a Prescription medication manufactured, distributed, or labeled by Cutanea Life Sciences, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use XEPI™ safely and effectively. See full prescribing information for XEPI™.
XEPI™ (ozenoxacin) cream, for topical use
Initial U.S. Approval: 2017INDICATIONS AND USAGE
XEPI is a quinolone antimicrobial indicated for the topical treatment of impetigo due to Staphylococcus aureus or Streptococcus pyogenes in adult and pediatric patients 2 months of age and older (1).
DOSAGE AND ADMINISTRATION
- Apply a thin layer of XEPI topically to the affected area twice daily for 5 days (2).
- Affected area may be up to 100 cm2 in adult and pediatric patients 12 years of age and older or 2% of the total body surface area and not exceeding 100 cm2 in pediatric patients less than 12 years of age (2).
- For topical use only (2).
- Not for oral, ophthalmic, intranasal, or intravaginal use (2).
DOSAGE FORMS AND STRENGTHS
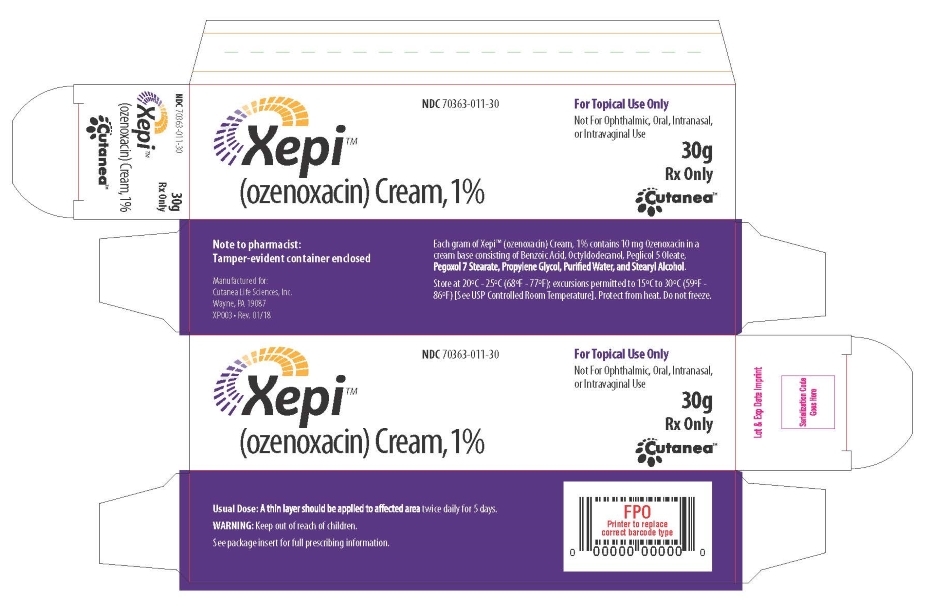
Cream: Each gram contains 10 mg of ozenoxacin (1%) (3).
CONTRAINDICATIONS
None (4)
WARNINGS AND PRECAUTIONS
Potential for Microbial Overgrowth: Prolonged use of XEPI may result in overgrowth of nonsusceptible bacteria and fungi. If such infections occur, discontinue use and institute alternative therapy (5).
ADVERSE REACTIONS
Adverse reactions (rosacea and seborrheic dermatitis) were reported in 1 adult patient treated with XEPI (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Cutanea Life Sciences, Inc. at 1-844-780-8152 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 1/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
XEPI™ is indicated for the topical treatment of impetigo due to Staphylococcus aureus or Streptococcus pyogenes in adult and pediatric patients 2 months of age and older [see Clinical Studies (14)].
-
2 DOSAGE AND ADMINISTRATION
Apply a thin layer of XEPI topically to the affected area twice daily for five days. Affected area may be up to 100 cm2 in adult and pediatric patients 12 years of age and older or 2% of the total body surface area and not exceeding 100 cm2 in pediatric patients less than 12 years of age.
- Wash hands after applying XEPI cream.
- XEPI cream is for topical use only.
- Not for oral, ophthalmic, intranasal, or intravaginal use.
- The treated area may be covered with a sterile bandage or gauze dressing.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety profile of XEPI was assessed in two clinical trials (Trial 1 and Trial 2) in 362 adult and pediatric patients two months of age and older with impetigo. The patients used at least one dose from a 5-day, twice a day regimen of XEPI. Control groups included 361 patients who used placebo and 152 patients who used retapamulin ointment. The median age of the patients enrolled in the clinical trials was 10 years; 3 % of patients were 2 months to less than 2 years of age, 55 % of patients were 2 to less than 12 years of age, 11 % of patients were 12 to less than 18 years of age, and 31 % of patients were 18 years of age or older.
Adverse reactions (rosacea and seborrheic dermatitis) were reported in 1 adult patient treated with XEPI.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on the use of XEPI in pregnant women to inform a drug associated risk. Systemic absorption of XEPI in humans is negligible following topical administration of XEPI (up to twice the concentration of the marketed formulation) [see Clinical Pharmacology (12.3)]. Due to the negligible systemic exposure, it is not expected that maternal use of XEPI will result in fetal exposure to the drug.
Animal reproduction studies were not conducted with XEPI. However, toxicity studies conducted in pregnant rats and rabbits administered the oral form of ozenoxacin showed no significant adverse developmental effects (at >10,000 times the maximum human plasma concentration seen with dermal application of ozenoxacin).
The estimated background risk of major birth defects and miscarriage for the indicated population are unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
8.2 Lactation
Risk Summary
No data are available regarding the presence of ozenoxacin in human milk, and the effects of ozenoxacin on the breastfed infant or on milk production. However, breastfeeding is not expected to result in exposure of the child to ozenoxacin due to the negligible systemic absorption of ozenoxacin in humans following topical administration of XEPI. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for XEPI and any potential adverse effects on the breast-fed child from XEPI or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of XEPI in the treatment of impetigo have been established in pediatric patients 2 months to 17 years of age. Use of XEPI in pediatric patients (2 months to 17 years of age) is supported by evidence from adequate and well-controlled studies of XEPI in which 251 pediatric patients received at least one dose of XEPI. The median age of the patients enrolled in the clinical trials was 10 years; 3 % of patients were 2 months to less than 2 years of age, 55 % of patients were 2 to less than 12 years of age, 11 % of patients were 12 to less than 18 years of age, and 31 % of patients were 18 years of age or older. In these studies, the maximum dose applied was approximately 0.5 g of XEPI applied twice daily for up to 5 days (i.e., up to 10 applications total) [see Clinical Studies (14)].
The safety profile of XEPI in pediatric patients 2 months and older was similar to that of adults [see Adverse Reactions (6.1)].
The safety and effectiveness of XEPI in pediatric patients younger than 2 months of age have not been established [see Clinical Studies (14)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
XEPI contains ozenoxacin, a quinolone antimicrobial. It is intended for topical use only.
The chemical name of ozenoxacin is 1-Cyclopropyl-8-methyl-7-(5-methyl-6-methylamino-pyridin-3-yl)-4-oxo-1,4-dihydro-quinoline-3-carboxylic acid. Ozenoxacin, a white to pale-yellow crystalline solid, has a molecular formula of C21H21N3O3, and a molecular weight of 363.41. The chemical structure is:
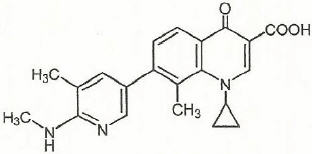
Each gram of cream contains 10 mg of ozenoxacin (1% w/w) and the following inactive ingredients: benzoic acid, octyldodecanol, peglicol 5 oleate, pegoxol 7 stearate, propylene glycol, purified water, stearyl alcohol.
-
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
Exposure-Response Relationship
The exposure response relationship for ozenoxacin following topical application has not been studied, however; a relationship is unlikely because systemic exposure following topical application is negligible [see Clinical Pharmacology (12.3)].
12.3 Pharmacokinetics
Absorption
Four pharmacokinetic studies were conducted in 110 patients utilizing varying strengths of ozenoxacin cream, up to 2% (twice the concentration of the marketed formulation). Three of these studies assessed systemic absorption in healthy subjects and in subjects with impetigo. These studies were conducted with either single or repeated application of up to 1 g ozenoxacin cream to intact or abraded skin (up to 200 cm2 surface area). No systemic absorption was observed in 84 of 86 subjects, and negligible systemic absorption was observed at the level of detection (0.489 ng/mL) in 2 subjects.
12.4 Microbiology
Mechanism of Action
Ozenoxacin is a quinolone antimicrobial drug. The mechanism of action involves the inhibition of bacterial DNA replication enzymes, DNA gyrase A and topoisomerase IV. Ozenoxacin has been shown to be bactericidal against S. aureus and S. pyogenes organisms.
Resistance
The mechanism of quinolone resistance can arise through mutations of one or more of the genes that encode DNA gyrase or topoisomerase IV. Resistant organisms will typically carry a combination of mutations within gyrA and parC subunits.
Overall the frequency of resistant mutants selected by ozenoxacin is ≤10-10.
Interaction with Other Antimicrobials
Ozenoxacin has been tested in combination with 17 other commonly used antimicrobial agents against S. aureus and S.pyogenes. Antagonism interactions with ozenoxacin were observed with ciprofloxacin against S. aureus.
Antimicrobial Activity
Ozenoxacin has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections [see Indications and Usage (1)]:
Gram-positive bacteria
Staphylococcus aureus (including methicillin-resistant isolates)
Streptococcus pyogenes -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals to evaluate carcinogenic potential have not been conducted with ozenoxacin.
Ozenoxacin demonstrated no genotoxicity when evaluated in vitro for gene mutation and/or chromosomal effects in the Ames test, mouse lymphoma cell assay, or when evaluated in vivo in a rat micronucleus test with demonstrated systemic exposure.
Oral doses of ozenoxacin did not affect mating and fertility in male and female rats treated up to 500 mg/kg/day (about 8500 and 16,000 times respectively, the maximum human plasma concentration seen with dermal application of ozenoxacin 1% cream).
-
14 CLINICAL STUDIES
The safety and efficacy of XEPI for the treatment of impetigo was evaluated in two multi-center, randomized, double-blind placebo controlled clinical trials (Trial 1, (NCT01397461) and Trial 2, (NCT02090764)). Seven-hundred twenty-three (723) subjects two months of age and older with an affected body surface area of up to 100 cm2, and not exceeding 2% for subjects aged 2 months to 11 years were randomized to XEPI or placebo. Subjects applied XEPI or placebo twice daily for 5 days. Subjects with underlying skin disease (e.g., preexisting eczematous dermatitis), skin trauma, clinical evidence of secondary infection, or systemic signs and symptoms of infection (such as fever), were excluded from these studies.
Overall clinical success was defined as no need for additional antimicrobial therapy of the baseline affected area(s) and absence/reduction in clinical signs and symptoms assessed at the end of therapy (Day 6-7), as follows: absence of exudates/pus, crusting, tissue warmth, and pain; and erythema/inflammation, tissue edema, and itching assessed as less than mild in Trial 1; and absence of blistering, exudates/pus, crusting, and itching/pain, and mild or improved erythema/inflammation in Trial 2. Table 2 below presents the results for clinical response at the end of therapy.
Table 2 Clinical Response at End of Therapy in Trial 1 and Trial 2 in All Randomized Subjects Trial 1 Trial 2 XEPI Placebo XEPI Placebo (N = 155)
n (%)(N = 156)
n (%)(N = 206)
n (%)(N = 206)
n (%)a The success rates for ozenoxacin were significantly different than placebo in Study 1 and Study 2 (p = 0.002 and p = 0.001). Clinical success 54 (34.8) 30 (19.2) 112 (54.4) 78 (37.9) Clinical failure 98 (63.2) 120 (76.9) 91 (44.2) 121 (58.7) Unable to determine 3 (1.9) 6 (3.8) 3 (1.5) 7 (3.4) The most commonly identified bacteria were S. aureus and S. pyogenes. Table 3 below presents the results for clinical success at end of therapy in subjects with S.aureus or S.pyogenes at baseline.
Table 3 Clinical Success at End of Therapy in Trial 1 and Trial 2 in Subjects with S. aureus or S. pyogenes Trial 1 Trial 2 XEPI Placebo XEPI Placebo Clinical success n/N (%) n/N (%) n/N (%) n/N (%) S. aureus 35/93 (37.6) 16/98 (16.3) 66/115 (57.4) 36/108 (33.3) S. pyogenes 29/73 (39.7) 7/67 (10.4) 15/19 (78.9) 8/20 (40.0) -
16 HOW SUPPLIED/STORAGE AND HANDLING
XEPI cream, 1% is a pale yellow cream supplied in a 30-gram tube. Each gram of cream contains 10 mg of ozenoxacin.
NDC: 70363-011-30 (30-gram tube)
-
17 PATIENT COUNSELING INFORMATION
Advise patients (and/or their caregivers or guardians) using XEPI of the following information and instructions:
- Use XEPI as directed by the healthcare practitioner. As with any topical medication, patients and caregivers should wash their hands after application if the hands are not the area for treatment.
- XEPI is for external use only.Do not swallow XEPI or use it in the eyes, on the mouth or lips, inside the nose, or inside the female genital area.
- The treated area may be covered by a sterile bandage or gauze dressing.
- Use the medication for the entire time recommended by the healthcare practitioner, even though symptoms may have improved.
- Notify the healthcare practitioner if there is no improvement in symptoms within 3 days after starting use of XEPI.
-
SPL UNCLASSIFIED SECTION

Manufactured for :
Cutanea Life Sciences, Inc., Wayne, PA, 19087All product names or other trademarks included herein are trademarks of Dermarc, LLC, a wholly owned subsidiary of Cutanea Life Sciences, Inc., unless otherwise noted. All rights reserved.
Xepi™ is used by Cutanea Life Sciences, Inc. under license from Ferrer Internacional, S.A. and its licensees.© 2019 Dermarc, LLC. All rights reserved.
10000047 - PRINCIPAL DISPLAY PANEL - 30 g Tube Carton
-
INGREDIENTS AND APPEARANCE
XEPI
ozenoxacin creamProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70363-011 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OZENOXACIN (UNII: V0LH498RFO) (OZENOXACIN - UNII:V0LH498RFO) OZENOXACIN 10 mg in 1 g Product Characteristics Color WHITE Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70363-011-30 1 in 1 BOX 10/05/2018 1 30 g in 1 TUBE; Type 0: Not a Combination Product 2 NDC: 70363-011-04 1 in 1 BOX 10/05/2018 2 3 g in 1 TUBE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA208945 10/05/2018 Labeler - Cutanea Life Sciences, Inc. (791866960)
Trademark Results [Xepi]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 XEPI 88767082 not registered Live/Pending |
FERRER INTERNACIONAL S.A. 2020-01-21 |
 XEPI 87820029 not registered Live/Pending |
Medimetriks Pharmaceuticals, Inc. 2018-03-05 |
 XEPI 86566661 not registered Dead/Abandoned |
Medimetriks Pharmaceuticals, Inc. 2015-03-17 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.