FLUVASTATIN SODIUM tablet, film coated, extended release
Fluvastatin Sodium by
Drug Labeling and Warnings
Fluvastatin Sodium by is a Prescription medication manufactured, distributed, or labeled by Lannett Company, Inc., Beijing Sciecure Pharmaceutical Co., Ltd.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use FLUVASTATIN SODIUM EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for FLUVASTATIN SODIUM EXTENDED-RELEASE TABLETS.
FLUVASTATIN SODIUM extended-release tablets, for oral use
Initial U.S. Approval: 1993RECENT MAJOR CHANGES
Contraindications, Pregnancy and Lactation (4) Removed 11/2023
INDICATIONS AND USAGE
Fluvastatin sodium extended-release tablets are indicated ( 1):
- To reduce the risk of undergoing coronary revascularization procedures and slow the progression of coronary atherosclerosis in adults with clinically evident coronary heart disease.
- As an adjunct to diet to reduce low-density lipoprotein cholesterol (LDL-C) in adults with primary hyperlipidemia.
- As an adjunct to diet to reduce LDL-C in adults and pediatric patients 10 years of age and older with heterozygous familial hypercholesterolemia (HeFH) who require 80 mg
DOSAGE AND ADMINISTRATION
- Fluvastatin sodium extended-release tablets can be taken with or without food and may be taken at any time of the day. (2.1)
- Do not break, crush or chew fluvastatin sodium extended-release tablets prior to administration. (2.1)
- Adults: The recommended starting dose is 80 mg (administered as one 80 mg fluvastatin sodium extended-release tablet once daily). (2.2) Children: The recommended dose is 80 mg once daily in pediatric patients 10 years of age and older who require 80 mg of fluvastatin. Fluvastatin sodium extended-release tablets are not recommended for dosage initiation in pediatric patients because the recommended starting dosage cannot be achieved with the available strength of 80 mg. (2.3)
DOSAGE FORMS AND STRENGTHS
Extended-release tablets: 80 mg of fluvastatin ( 3)
CONTRAINDICATIONS
- Acute liver failure or decompensated cirrhosis (4)
- Hypersensitivity to fluvastatin or any excipient in fluvastatin sodium extended-release tablets (4)
WARNINGS AND PRECAUTIONS
- Myopathy and Rhabdomyolysis: Risk factors include age 65 years or greater, uncontrolled hypothyroidism, renal impairment, and concomitant use with certain other drugs. Discontinue fluvastatin if markedly elevated creatine kinase (CK) levels occur, or myopathy is diagnosed or suspected. Temporarily discontinue fluvastatin in patients experiencing an acute or serious condition at high risk of developing renal failure secondary to rhabdomyolysis. Inform patients of the risk of myopathy and rhabdomyolysis when starting or increasing fluvastatin dosage. Instruct patients to promptly report unexplained muscle pain, tenderness, or weakness, particularly if accompanied by malaise or fever. (5.1)
- Immune-Mediated Necrotizing Myopathy (IMNM): Rare reports of IMNM, an autoimmune myopathy, have been reported with statin use. Discontinue fluvastatin if IMNM is suspected. (5.2)
- Hepatic Dysfunction: Increases in serum transaminases have occurred, some persistent. Rare reports of fatal and non-fatal hepatic failure have occurred. Consider testing liver enzyme before initiating therapy and as clinically indicated thereafter. If serious hepatic injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs, promptly discontinue fluvastatin sodium extended-release tablets (5.3)
ADVERSE REACTIONS
Most frequent adverse reactions occurring in ≥ 2.5% of subjects treated with fluvastatin sodium extended-release tablets and more than placebo are: influenza-like symptoms, sinusitis, dyspepsia, urinary tract infection, bronchitis, and nausea. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Lannett Company, Inc. at 1-844-834-0530 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Gemfibrozil: Avoid use with fluvastatin. (7.1)
- Cyclosporine and Fluconazole: Avoid use with fluvastatin. (7.1)
- Fibrates, Lipid-modifying doses (≥ 1 g/day) of Niacin, and Colchicine: Consider if the benefit of concomitant use with fluvastatin outweighs the increased risk of myopathy and rhabdomyolysis. If concomitant use is decided, monitor patients for signs and symptoms of myopathy, particularly during initiation of therapy and during upward dose titration. (7.1)
- Warfarin: Obtain an International Normalized Ratio (INR) before starting and frequently enough after initiation or discontinuation to ensure that no significant alteration in INR occurs. Once the INR is stable, monitor INR at regular intervals. (7.2)
- Glyburide: Monitor blood glucose levels when fluvastatin is initiated. (7.2)
- Phenytoin: Monitor plasma phenytoin levels when fluvastatin treatment is initiated. (7.2)
USE IN SPECIFIC POPULATIONS
- Pregnancy: May cause fetal harm (8.1)
- Lactation: Breastfeeding not recommended during treatment with fluvastatin (8.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 2/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
RECENT MAJOR CHANGES
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage Information
2.2 Recommended Dosage in Adult Patients
2.3 Recommended Dosage in Pediatric Patients Aged 10 Years of Age and Older with HeFH
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myopathy and Rhabdomyolysis
5.2 Immune-Mediated Necrotizing Myopathy
5.3 Hepatic Dysfunction
5.4 Increases in HbA1c and Fasting Serum Glucose Levels
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Drug Interactions That Increase the Risk of Myopathy and Rhabdomyolysis with Fluvastatin
7.2 Fluvastatin Effects on Other Drugs
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Fluvastatin sodium extended-release tablets are indicated:
- To reduce the risk of undergoing coronary revascularization procedures and slow the progression of coronary atherosclerosis in adults with clinically evident coronary heart disease.
- As an adjunct to diet to reduce low-density lipoprotein cholesterol (LDL-C) in adults with primary hyperlipidemia.
- As an adjunct to diet to reduce LDL-C in adults and pediatric patients 10 years of age and older with heterozygous familial hypercholesterolemia (HeFH) who require 80 mg of fluvastatin daily.
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage Information
- Take fluvastatin sodium extended-release tablets orally once daily as a single dose, with or without food.
- Do not break, crush, or chew fluvastatin sodium extended-release tablets.
- Fluvastatin sodium extended-release tablet is only available as an 80 mg tablet. Fluvastatin sodium extended-release tablets cannot be titrated [see Dosage and Administration (2.2, 2.3)].
- For patients that require a high-intensity statin or are unable to achieve their LDL-C goal receiving fluvastatin sodium extended-release tablets 80 mg daily, prescribe alternative LDL-C-lowering treatment.
- Assess LDL-C when clinically appropriate, as early as 4 weeks after initiating fluvastatin sodium extended-release tablets.
2.2 Recommended Dosage in Adult Patients
The recommended dosage for fluvastatin sodium extended-release tablets is 80 mg once daily.
2.3 Recommended Dosage in Pediatric Patients Aged 10 Years of Age and Older with HeFH
Fluvastatin sodium extended-release tablets are not recommended for dosage initiation in pediatric patients because the recommended starting dosage cannot be achieved with the available strength of 80 mg. Recommend use of another fluvastatin product to initiate dosing in pediatric patients.
The recommended dosage of fluvastatin sodium extended-release tablets is 80 mg once daily in pediatric patients 10 years of age and older who require 80 mg of fluvastatin. - 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Fluvastatin sodium extended-release tablets are contraindicated in patients with:
- Acute liver failure or decompensated cirrhosis [see Warnings and Precautions (5.3)].
- Hypersensitivity to fluvastatin or any of the excipients in fluvastatin sodium extended-release tablets. Hypersensitivity reactions, including anaphylaxis, angioedema, and Stevens-Johnson syndrome have been reported [see Adverse Reactions (6.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Myopathy and Rhabdomyolysis
Fluvastatin may cause myopathy (muscle pain, tenderness, or weakness associated with elevated creatine kinase [CK]) and rhabdomyolysis. Acute kidney injury secondary to myoglobinuria and rare fatalities have occurred as a result of rhabdomyolysis with statins, including fluvastatin.
Myopathy, defined as muscle aching or muscle weakness in conjunction with increases in CK, values to greater than 10 times the upper limit of normal (ULN) was < 0.1% in fluvastatin clinical trials [see Adverse Reactions (6.1)].
Risk Factors for Myopathy
Risk factors for myopathy include age 65 years or greater, uncontrolled hypothyroidism, renal impairment, and concomitant use with certain other drugs (including other lipid-lowering therapies) [see Drug Interactions (7.1)].
Steps to Prevent or Reduce the Risk of Myopathy and Rhabdomyolysis
Avoid concomitant use of fluvastatin with gemfibrozil, cyclosporin, and fluconazole. When used concomitantly with fluvastatin, lipid modifying doses (≥ 1 g/day) of niacin, fibrates, and colchicine may also increase the risk of myopathy and rhabdomyolysis [see Drug Interactions (7.1)].
Discontinue fluvastatin if markedly elevated CK levels occur or if myopathy is either diagnosed or suspected. Muscle symptoms and CK increases may resolve if fluvastatin is discontinued. Temporarily discontinue fluvastatin in patients experiencing an acute or serious condition at high risk of developing renal failure secondary to rhabdomyolysis, e.g., sepsis, shock, severe hypovolemia, major surgery, trauma, severe metabolic, endocrine, or electrolyte disorders, or uncontrolled epilepsy.
Inform patients of the risk of myopathy and rhabdomyolysis when starting fluvastatin. Instruct patients to promptly report any unexplained muscle pain, tenderness, or weakness, particularly if accompanied by malaise or fever.
5.2 Immune-Mediated Necrotizing Myopathy
There have been rare reports of immune-mediated necrotizing myopathy (IMNM), an autoimmune myopathy, associated with statin use, including reports of recurrence when the same or a different statin was administered. IMNM is characterized by proximal muscle weakness and elevated serum CK, which persist despite discontinuation of statin treatment; positive anti-HMG CoA reductase antibody, muscle biopsy showing necrotizing myopathy, and improvement with immunosuppressive agents. Additional neuromuscular and serologic testing may be necessary. Treatment with immunosuppressive agents may be required. Discontinue fluvastatin if IMNM is suspected.
5.3 Hepatic Dysfunction
Increases in serum transaminases have been reported with use of fluvastatin [see Adverse Reactions (6.1)].In most cases, these changes appeared soon after initiation, were transient, were not accompanied by symptoms, and resolved or improved on continued therapy or after a brief interruption in therapy. Persistent increases to more than three times the ULN in serum transaminases have occurred in approximately 1.1% of patients receiving fluvastatin in clinical trials. Marked persistent increases of hepatic transaminases have also occurred with fluvastatin. There have been rare post-marketing reports of fatal and non-fatal hepatic failure in patients taking statins, including fluvastatin.
Patients who consume substantial quantities of alcohol and/or have a history of liver disease may be at increased risk for hepatic injury.
Consider liver enzyme testing before fluvastatin initiation and thereafter, when clinically indicated. Fluvastatin sodium extended-release tablets are contraindicated in patients with acute liver failure or decompensated cirrhosis [see Contraindications (4)].If serious hepatic injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs, promptly discontinue fluvastatin sodium extended-release tablets.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in other sections of the label:
- Myopathy and Rhabdomyolysis [see Warnings and Precautions (5.1)]
- Immune-Mediated Necrotizing Myopathy [see Warnings and Precautions (5.2)]
- Hepatic Dysfunction [see Warnings and Precautions (5.3)]
- Increases in HbA1c and Fasting Serum Glucose Levels [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In the fluvastatin capsule, clinical trials there were 2,326 patients treated with fluvastatin (age range, 18 to 75 years, 44% women, 94% White, 4% Black or African American, 2% other ethnicities) with a median treatment duration of 24 weeks. The most common adverse reactions that led to treatment discontinuation and occurred at an incidence greater than placebo were: transaminase increased (0.8%), upper abdominal pain (0.3%), dyspepsia (0.3%), fatigue (0.2%), and diarrhea (0.2%).
In the fluvastatin sodium extended-release tablets clinical trials there were 912 patients treated with fluvastatin sodium extended-release tablets (age range, 21 to 87 years, 52% women, 91% White, 4% Black of African American, 5% other ethnicities) with a median treatment duration of 24 weeks. The most common adverse reactions that led to treatment discontinuation were abdominal pain (0.7%), diarrhea (0.5%), nausea (0.4%), dyspepsia (0.4%) and chest pain (0.3%).
Adverse reactions occurring in the fluvastatin capsules and fluvastatin sodium extended-release tablets controlled trials with a frequency 2% included the following:
Table 1. Adverse Reactions Reported in 2% in Patients Treated with Fluvastatin Capsules/Fluvastatin Sodium Extended-Release Tablets and at an Incidence Greater Than Placebo in Placebo-Controlled Trials Pooled Dosages Adverse reaction Placebo a
N = 960
(%)Fluvastatin capsulesa
N = 2,326
(%)Fluvastatin sodium extended-release tablets b
N = 912
(%)Influenza-like symptoms 5.7 5.1 7.1 Headache 7.8 8.9 4.7 Myalgia 4.5 5.0 3.8 Abdominal pain 3.8 4.9 3.7 Dyspepsia 3.2 7.9 3.5 Sinusitis 1.9 2.6 3.5 Diarrhea 4.2 4.9 3.3 Arthropathy NA NA 3.2 Urinary tract infection 1.1 1.6 2.7 Nausea 2.0 3.2 2.5 Bronchitis 1.0 1.8 2.6 Fatigue 2.3 2.7 1.6 Flatulence 2.5 2.6 1.4 Arthritis 2.0 2.1 1.3 Allergy 2.2 2.3 1.0 Insomnia 1.4 2.7 0.8 aControlled trials with fluvastatin capsules (20 mg and 40 mg daily and 40 mg twice daily) compared to placebo.
bControlled trials with fluvastatin sodium extended-release 80 mg Tablets as compared to fluvastatin capsules.In the Fluvastatin Capsule Intervention Prevention Study (LIPS), the effect of fluvastatin capsules 40 mg, administered twice daily on the risk of recurrent cardiac events was assessed in 1,677 patients with coronary heart disease who had undergone a percutaneous coronary intervention. This was a multicenter, randomized, double-blind, placebo-controlled trial, patients were treated with dietary/lifestyle counseling and either fluvastatin capsules 40 mg (n = 844) or placebo (n = 833) given twice daily for a median of 3.9 years [see Clinical Studies (14.3)].
Table 2. Adverse Reactions Reported in ≥ 2% in Patients Treated with Fluvastatin Capsules/Fluvastatin Sodium Extended-Release Tablets and at an Incidence Greater Than Placebo in the LIPS Trial Adverse reaction Placebo
N = 818
(%)Fluvastatin Capsules
40 mg twice daily
N = 822
(%)Abdominal pain upper 4.5 6.3 Hypertension 4.2 5.8 Fatigue 3.8 4.7 Dyspepsia 4.0 4.5 Edema peripheral 2.9 4.4 Pain in extremity 2.7 4.1 Dizziness 3.5 3.9 Constipation 2.1 3.3 Nasopharyngitis 2.1 2.8 Dyspnea exertional 2.4 2.8 Gastric disorder 2.1 2.7 Nausea 2.3 2.7 Atrial fibrillation 2.0 2.4 Syncope 2.2 2.4 Bronchitis 2.0 2.3 Intermittent claudication 2.1 2.3 Myalgia 1.6 2.2 Arthralgia 1.8 2.1 Elevations in Liver Enzyme Tests
Approximately 1.1% of patients treated with fluvastatin capsules in clinical trials developed dose-related, persistent elevations of serum transaminase levels to more than 3 times the ULN. Fourteen of these patients (0.6%) were discontinued from therapy. In all clinical trials, a total of 33/2,969 patients (1.1%) had persistent transaminase elevations with an average fluvastatin exposure of approximately 71.2 weeks; 19 of these patients (0.6%) were discontinued. The majority of patients with these abnormal biochemical findings were asymptomatic.
In a pooled analysis of all placebo-controlled studies in which fluvastatin capsules were used, persistent transaminase elevations (> 3 times the ULN on two consecutive weekly measurements) occurred in 0.2%, 1.5%, and 2.7% of patients treated with daily doses of 20, 40, and 80 mg (titrated to 40 mg twice daily) fluvastatin capsules, respectively. Ninety-one percent of the cases of persistent ALT/AST increased abnormalities (20 of 22 patients) occurred within 12 weeks of therapy and in all patients with persistent liver function test abnormalities there was an abnormal liver function test present at baseline or by Week 8.
In the pooled analysis of 24-week controlled trials, persistent transaminase elevation occurred in 1.9%, 1.8%, and 4.9% of patients treated with fluvastatin sodium extended-release tablets 80 mg, fluvastatin capsules 40 mg and fluvastatin capsules 40 mg twice daily, respectively. In 13 of 16 patients treated with fluvastatin sodium extended-release tablets the abnormality occurred within 12 weeks of initiation of treatment with fluvastatin sodium extended-release tablets 80 mg.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of fluvastatin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Musculoskeletal:Muscle cramps, myopathy, rhabdomyolysis, arthralgias, muscle spasms, muscle weakness, myositis. There have been rare reports of IMNM associated with statin use [see Warnings and Precautions (5.2)].
Neurological:Dysfunction of certain cranial nerves (including alteration of taste, impairment of extra-ocular movement, facial paresis), tremor, vertigo, paresthesia, hypoesthesia, dysesthesia, peripheral neuropathy, peripheral nerve palsy. There have been rare postmarketing reports of cognitive impairment (e.g., memory loss, forgetfulness, amnesia, memory impairment, confusion) associated with the use of all statins. The reports are generally nonserious, and reversible upon statin discontinuation, with variable times to symptom onset (1 day to years) and symptom resolution (median of 3 weeks). There have been rare reports of new-onset or exacerbation of myasthenia gravis, including ocular myasthenia, and reports of recurrence when the same or a different statin was administered.
Psychiatric:Anxiety, depression, psychic disturbances
Respiratory:Interstitial lung disease
Hypersensitivity reactions:An apparent hypersensitivity syndrome has been reported rarely which has included one or more of the following features: anaphylaxis, angioedema, lupus erythematosus-like syndrome, polymyalgia rheumatica, vasculitis, purpura, thrombocytopenia, leukopenia, hemolytic anemia, positive ANA, ESR (erythrocyte sedimentation rate) increase, eosinophilia, arthritis, arthralgia, urticaria, asthenia, photosensitivity reaction, fever, chills, flushing, malaise, dyspnea, toxic epidermal necrolysis, erythema multiforme, including Stevens-Johnson syndrome.
Gastrointestinal:Pancreatitis, hepatitis, including chronic active hepatitis, cholestatic jaundice, fatty change in liver, cirrhosis, fulminant hepatic necrosis, hepatoma, anorexia, vomiting, fatal and non-fatal hepatic failure.
Skin:Rash, dermatitis, including bullous dermatitis, eczema, alopecia, pruritus, lichen planus, a variety of skin changes (e.g., nodules, discoloration, dryness of skin/mucous membranes, changes to hair/nails).
Reproductive:Gynecomastia, loss of libido, erectile dysfunction.
Eye:Progression of cataracts (lens opacities), ophthalmoplegia.
Laboratory abnormalities:elevated transaminases, alkaline phosphatase, gamma-glutamyl transpeptidase and bilirubin; thyroid function abnormalities.
-
7 DRUG INTERACTIONS
7.1 Drug Interactions That Increase the Risk of Myopathy and Rhabdomyolysis with Fluvastatin
Table 3 includes a list of drugs that increase the risk of myopathy and rhabdomyolysis when used concomitantly with fluvastatin and instructions for preventing or managing them [see Warnings and Precautions (5.1), Clinical Pharmacology (12.3)].
Table 3. Drug Interactions That Increase the Risk of Myopathy and Rhabdomyolysis with Fluvastatin Gemfibrozil Clinical impact There is an increased risk of myopathy/rhabdomyolysis when fluvastatin is administered with gemfibrozil Intervention Avoid concomitant use of gemfibrozil with fluvastatin. Cyclosporine Clinical impact Cyclosporine coadministration increases fluvastatin exposure. The risk of myopathy and rhabdomyolysis may be increased with concomitant use of cyclosporine with fluvastatin. Intervention Avoid concomitant use of cyclosporine with fluvastatin. Fluconazole Clinical impact Fluconazole coadministration increases fluvastatin exposure. The risk of myopathy and rhabdomyolysis may be increased with concomitant use of fluconazole with fluvastatin. Intervention Avoid concomitant use of fluconazole with fluvastatin Niacin Clinical impact Risk of myopathy and rhabdomyolysis may be enhanced with concomitant use with lipid-modifying doses (≥ 1 g/day) of niacin with fluvastatin. Intervention Consider if the benefit of using lipid-modifying doses (≥ 1 g/day) of niacin concomitantly with fluvastatin outweighs the increased risk of myopathy and rhabdomyolysis. If concomitant use is decided, monitor patients for signs and symptoms of myopathy, particularly during initiation of therapy and during upward dose titration. Fibrates Clinical impact Fibrates may cause myopathy when given alone. The risk of myopathy and rhabdomyolysis may be increased with concomitant use of fibrates with fluvastatin. Intervention Consider if the benefit of using fibrates concomitantly with fluvastatin outweighs the increased risk of myopathy and rhabdomyolysis. If concomitant use is decided, monitor patients for signs and symptoms of myopathy, particularly during initiation of therapy and during upward dose titration. Colchicine Clinical impact Cases of myopathy and rhabdomyolysis have been reported with concomitant use of colchicine with fluvastatin. Intervention Consider if the benefit of using colchicine concomitantly with fluvastatin outweighs the increased risk of myopathy and rhabdomyolysis. If concomitant use is decided, monitor patients for signs and symptoms of myopathy, particularly during initiation of therapy and during upward dose titration. 7.2 Fluvastatin Effects on Other Drugs
Table 4 presents fluvastatins effect on other drugs and instructions for preventing or managing them.
Table 4. Fluvastatin Effects on Other Drugs Warfarin Clinical impact There are postmarketing reports of clinically evident bleeding and/or increased INR in patients taking concomitant statins and warfarin. Intervention In patients taking warfarin, obtain an INR before starting fluvastatin and frequently enough after initiation or discontinuation to ensure that no significant alteration in INR occurs. Once the INR is stable, monitor INR at regularly recommended intervals. Glyburide Clinical impact Concomitant administration of fluvastatin and glyburide increased glyburide exposures [see Clinical Pharmacology (12.3)]. Intervention Monitor blood glucose levels when fluvastatin is initiated. Phenytoin Clinical impact Concomitant administration of fluvastatin and phenytoin increased phenytoin exposures [see Clinical Pharmacology (12.3)]. Intervention Monitor plasma phenytoin levels when fluvastatin is initiated. -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Discontinue fluvastatin when pregnancy is recognized. Alternatively, consider the ongoing therapeutic needs of the individual patient. Fluvastatin decreases synthesis of cholesterol and possibly other biologically active substances derived from cholesterol; therefore, fluvastatin may cause fetal harm when administered to pregnant patients based on the mechanism of action [see Clinical Pharmacology (12.1)]. In addition, treatment of hyperlipidemia is not generally necessary during pregnancy. Atherosclerosis is a chronic process and the discontinuation of lipid-lowering drugs during pregnancy should have little impact on the outcome of long-term therapy of primary hyperlipidemia for most patients.
Available data from case series and prospective and retrospective observational cohort studies over decades of use with statins in pregnant women have not identified a drug-associated risk of major congenital malformations. Published data from prospective and retrospective observational cohort studies with fluvastatin use in pregnant women are insufficient to determine if there is a drug-associated risk of miscarriage (see Data).
In animal reproduction studies, no adverse developmental effects were observed in pregnant rats or rabbits orally administered fluvastatin during the period of organogenesis at doses that resulted in 2 and 5 times, respectively, the human exposure at the maximum recommended human dosage of 40 mg/day, based on body surface area (mg/m 2) (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data
A Medicaid cohort linkage study of 1,152 statin-exposed pregnant women compared to 886,996 controls did not find a significant teratogenic effect from maternal use of statins in the first trimester of pregnancy, after adjusting for potential confounders, including maternal age, diabetes mellitus, hypertension, obesity, and alcohol and tobacco use using propensity score-based methods. The relative risk of congenital malformations between the group with statin use and the group with no statin use in the first trimester was 1.07 (95% CI: 0.85 to 1.37) after controlling for confounders, particularly preexisting diabetes mellitus. There were also no statistically significant increases in any of the organ-specific malformations assessed after accounting for confounders. In the majority of pregnancies, statin treatment was initiated prior to pregnancy and was discontinued at some point in the first trimester when pregnancy was identified. Study limitations include reliance on physician coding to define the presence of a malformation, lack of control for certain confounders such as body mass index, use of prescription dispensing as verification for the use of a statin, and lack of information on non-live births.
Animal Data
Fluvastatin sodium given to rats during organogenesis at doses of 12 mg/kg/day and in rabbits at doses of 10 mg/kg/day produced delays in skeletal development. These doses resulted in 2 times (rat at 12 mg/kg) or 5 times (rabbit at 10 mg/kg) the 40 mg human exposure based on mg/m 2surface area. Malaligned thoracic vertebrae were seen in rats at 36 mg/kg, a dose that produced significant maternal toxicity. A study in which female rats were given fluvastatin during the third trimester at 12 and 24 mg/kg/day resulted in maternal mortality at or near term and postpartum. In addition, fetal and neonatal lethality were apparent. No effects on the dam or fetus occurred at 2 mg/kg/day. A second study at levels of 2, 6, 12 and 24 mg/kg/day confirmed the findings in the first study with neonatal mortality beginning at 6 mg/kg. Rats were given fluvastatin from Gestation Day 15 to Lactation Day 21 at doses of 12 or 24 mg/kg/day with or without the presence of concurrent supplementation with mevalonic acid, a product of HMG-CoA reductase which is essential for cholesterol biosynthesis. The concurrent administration of mevalonic acid completely prevented the maternal and neonatal mortality but did not prevent low body weights in pups at 24 mg/kg on Days 0 and 7 postpartum.
8.2 Lactation
Risk Summary
There is no information about the presence of fluvastatin in human milk, the effects of the drug on the breastfed infant or the effects of the drug on milk production. However, it has been shown that another drug in this class passes into human milk. Studies in rats have shown that fluvastatin and/or its metabolites are present in the milk of lactating rats. When a drug is present in animal milk, it is likely that the drug will be present in human milk (see Data).Statins, including fluvastatin, decrease cholesterol synthesis and possibly the synthesis of other biologically active substances derived from cholesterol and may cause harm to the breastfed infant.
Because of the potential for serious adverse reactions in a breastfed infant, based on the mechanism of action, advise patients that breastfeeding is not recommended during treatment with fluvastatin [see Use in Specific Populations (8.1), Clinical Pharmacology (12.1)].
Data
Following a single oral administration of 1 mg/kg of radioactive fluvastatin to lactating rats, the concentration of total radioactivity was determined. Fluvastatin and/or its metabolites were measured in the breast milk at a 2:1 ratio (milk:plasma).
8.4 Pediatric Use
The safety and effectiveness of fluvastatin as an adjunct to diet to reduce LDL-C have been established in pediatric patients 10 years of age and older with HeFH. Use of fluvastatin for this indication is based on open-label, uncontrolled clinical trials in 114 pediatric patients 9 years of age and older with HeFH. In these limited uncontrolled studies, there was no significant effect on growth or sexual maturation in the males or females, or on menstrual cycle length in females.
The safety and effectiveness of fluvastatin have not been established in pediatric patients younger than 10 years of age with HeFH or in pediatric patients with other types of hyperlipidemia (other than HeFH).
8.5 Geriatric Use
Fluvastatin exposures were not significantly different between the nonelderly and elderly populations (age ≥ 65 years) [see Clinical Pharmacology (12.3)].
Advanced age (≥ 65 years) is a risk factor for fluvastatin-associated myopathy and rhabdomyolysis. Dose selection for an elderly patient should be cautious, recognizing the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy and the higher risk of myopathy. Monitor geriatric patients receiving fluvastatin for the increased risk of myopathy [see Warnings and Precautions (5.1)].
8.6 Renal Impairment
Renal impairment is a risk factor for myopathy and rhabdomyolysis. Dose adjustments for mild to moderate renal impairment are not necessary. Fluvastatin has not been studied at doses greater than 40 mg in patients with severe renal impairment; therefore, use fluvastatin with caution in patients with severe renal impairment. Monitor all patients with renal impairment for development of myopathy [see Warnings and Precautions (5.1), Clinical Pharmacology (12.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
Fluvastatin sodium inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase.
Fluvastatin sodium is [R*,S*-(E)]-(±)-7-[3-(4-fluorophenyl)-1-(1-methylethyl)-1H-indol-2-yl]- 3,5-dihydroxy-6-heptenoic acid, monosodium salt. The empirical formula of fluvastatin sodium is C24H25FNO4Na, its molecular weight is 433.46 g/mol and its structural formula is:
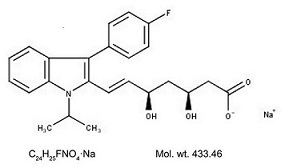
Fluvastatin sodium, USP is a white to pale yellow, brownish-pale yellow, or reddish-pale yellow, hygroscopic powder soluble in alcohol, in methanol, and in water. Fluvastatin sodium extended-release tablets are supplied as extended-release tablets containing fluvastatin sodium, equivalent to 80 mg of fluvastatin, for oral use. Fluvastatin sodium extended-release tablets contain the following inactive ingredients: glycerol dibehenate, pregelatinized starch, hypromellose, potassium bicarbonate, magnesium stearate, polyvinyl alcohol, titanium dioxide, talc, lecithin (soya), yellow iron oxide non-irradiated, shellac glaze (modified) in SD-45, isopropyl alcohol, black iron oxide non-irradiated, N-butyl alcohol, propylene glycol, ammonium hydroxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Fluvastatin is a competitive inhibitor of HMG-CoA reductase, the rate limiting enzyme that converts 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) to mevalonate, a precursor of cholesterol.
12.2 Pharmacodynamics
Inhibition of HMG-CoA reductase by fluvastatin accelerates the expression of LDL-receptors, followed by the uptake of LDL-C from blood to the liver, leading to a decrease in plasma LDL-C and total cholesterol. Sustained inhibition of cholesterol synthesis in the liver also decreases levels of very-low-density lipoproteins. The maximum LDL-C reduction of fluvastatin is usually achieved by 4 weeks and is maintained after that.
12.3 Pharmacokinetics
Absorption
Fluvastatin administered as fluvastatin sodium extended-release 80 mg tablets reaches peak concentration in approximately 3 hours under fasting conditions, after a low-fat meal, or 2.5 hours after a low-fat meal. The mean relative bioavailability of the extended-release tablet is approximately 29% (range, 9% to 66%) compared to that of the fluvastatin immediate-release capsule administered under fasting conditions. Administration of a high-fat meal delayed the absorption (Tmax 6h) and increased the bioavailability of the extended-release tablet by approximately 50%. However, the maximum concentration of fluvastatin sodium extended-release tablets seen after a high-fat meal is less than the peak concentration following a single dose or twice daily dose of the 40 mg fluvastatin capsule.
Distribution
Fluvastatin is 98% bound to plasma proteins. The mean volume of distribution (VDss) is estimated at 0.35 L/kg. At therapeutic concentrations, the protein binding of fluvastatin is not affected by warfarin, salicylic acid and glyburide.
Elimination
Metabolism
Fluvastatin is metabolized in the liver, primarily via hydroxylation of the indole ring at the 5- and 6-positions. N-dealkylation and beta-oxidation of the side-chain also occurs. The hydroxy metabolites have some pharmacologic activity, but do not circulate in the blood. Fluvastatin has two enantiomers. Both enantiomers of fluvastatin are metabolized in a similar manner.
In vitro data indicate that fluvastatin metabolism involves multiple Cytochrome P450 (CYP) isozymes. CYP2C9 isoenzyme is primarily involved in the metabolism of fluvastatin (approximately 75%), while CYP2C8 and CYP3A4 isoenzymes are involved to a much less extent, i.e., approximately 5% and approximately 20%, respectively.
Excretion
Following oral administration, fluvastatin is primarily (about 90%) excreted in the feces as metabolites, with less than 2% present as unchanged drug. Approximately 5% of a radiolabeled oral dose were recovered in urine. The elimination half-life (t 1/2) of fluvastatin is approximately 3 hours.
Specific Populations
Geriatric Patients
Plasma levels of fluvastatin are not significantly different in patients age > 65 years compared to patients age 21 to 49 years.
Gender
In a study evaluating the effect of age and gender on fluvastatin pharmacokinetics, there were no significant differences in fluvastatin exposures between males and females, except between younger females and younger males (both ages 21-49 years), where there was an approximate 30% increase in area under the curve (AUC) in females. Adjusting for body weight decreases the magnitude of the differences seen. For fluvastatin sodium extended-release tablets, the AUC increases 67% and 77% for women compared to men under fasted and high-fat meal fed conditions, respectively.
Pediatric Patients
Pharmacokinetic data in the pediatric population are not available.
Patients with Renal Impairment
In patients with moderate to severe renal impairment (CLCr 10-40 mL/min), AUC and Cmax increased approximately 1.2-fold after administration of a single dose of 40 mg fluvastatin compared to healthy volunteers. In patients with end-stage renal disease on hemodialysis, the AUC increased by approximately 1.5-fold. Fluvastatin sodium extended-release tablets were not evaluated in patients with renal impairment [see Use in Specific Populations (8.6)].However, systemic exposures after administration of fluvastatin sodium extended-release tablets are lower than after the 40 mg immediate release capsule.
Patients with Hepatic Impairment
In patients with hepatic impairment due to liver cirrhosis, fluvastatin AUC and Cmax increased approximately 2.5-fold compared to healthy subjects after administration of a single 40 mg dose [see Use in Specific Populations (8.7)].The enantiomer ratios of the two isomers of fluvastatin in hepatic impairment patients were comparable to those observed in healthy subjects.
Drug Interaction Studies
Data from drug-drug interactions studies involving coadministration of gemfibrozil, niacin, itraconazole, erythromycin, tolbutamide or clopidogrel indicate that the PK disposition of fluvastatin is not significantly altered when fluvastatin is coadministered with any of these drugs.
The below listed drug interaction information is derived from studies using fluvastatin capsules. Similar studies have not been conducted using the fluvastatin sodium extended-release tablets.
Table 5. Effect of Coadministered Drugs on Fluvastatin Systemic Exposure Coadministered drug and dosing regimen Fluvastatin Dose (mg) a Change in AUC b Change in Cmax b Cyclosporine – stable dose (twice daily) c 20 mg once daily for 14 weeks ↑90% ↑30% Fluconazole 400 mg once daily 1,200 mg twice daily 2 to 4 c 40 mg once daily ↑84% ↑44% Cholestyramine 8 g once daily 20 mg once daily administered 4 hrs after a meal plus cholestyramine ↓51% ↓83% Rifampicin 600 mg once daily for 6 days 20 mg once daily ↓53% ↓42% Cimetidine 400 mg twice daily for 5 days, once daily on Day 6 20 mg once daily ↑30% ↑40% Ranitidine 150 mg twice daily for 5 days, once daily on Day 6 20 mg once daily ↑10% ↑50% Omeprazole 40 mg once daily for 6 days 20 mg once daily ↑20% ↑37% Phenytoin 300 mg once daily 40 mg twice daily for 5 days ↑40% ↑27% Propranolol 40 mg twice daily for 3.5 days 40 mg once daily ↓5% No change Digoxin 0.1 to 0.5 mg once daily for 3 weeks 40 mg once daily No change ↑11% Diclofenac 25 mg once daily 40 mg once daily for 8 days ↑50% ↑80% Glyburide 5 mg to 20 mg once daily for 22 days 40 mg twice daily for 14 days ↑51% ↑44% Warfarin 30 mg once daily 40 mg once daily for 8 days ↑30% ↑67% Clopidogrel 300 mg loading dose on Day 10, 75 mg once daily on Days 11 to 19 80 mg extended-release once daily for 19 days ↓2% ↑27% Abbreviation: AUC, area under the curve.
aSingle dose unless otherwise noted.
bMean ratio (with/without coadministered drug and no change = 1-fold) or % change (with/without coadministered drug and no change = 0%); symbols of ↑ and ↓ indicate the exposure increase and decrease, respectively.
cConsidered clinically significant [see Dosage and Administration (2.4), Drug Interactions (7.1)].Data from drug-drug interaction studies involving fluvastatin and coadministration of either gemfibrozil, tolbutamide or losartan indicate that the PK disposition of either gemfibrozil, tolbutamide or losartan is not significantly altered when coadministered with fluvastatin.
Table 6. Effect of Fluvastatin Coadministration on Systemic Exposure of Other Drugs Co-administered drug Fluvastatin dosage regimen Name and dose (mg) a Change in AUC b Change in Cmax b 40 mg once daily for 5 days Phenytoin 300 mg once daily c ↑20% ↑5% 40 mg twice daily for 21 days Glyburide 5 to 20 mg once daily for 22 days c ↑70% ↑50% 40 mg once daily for 8 days Diclofenac 25 mg once daily ↑25% ↑60% 40 mg once daily for 8 days Warfarin 30 mg once daily S-warfarin: ↑7% S-warfarin: ↑10% R-warfarin: no change R-warfarin: ↑6% Abbreviation: AUC, area under the curve.
aSingle dose unless otherwise noted.
bMean ratio (with/without coadministered drug and no change = 1-fold) or % change (with/without coadministered drug and no change = 0%); symbols of ↑ and ↓ indicate the exposure increase and decrease, respectively.
cConsidered clinically significant [see Drug Interactions (7.2)]. -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2-year carcinogenicity study in rats at doses of 6, 9, and 18 to 24 (escalated after 1 year) mg/kg/day, there was an increased incidence of thyroid follicular cell adenomas and carcinomas in males treated with 18 to 24 mg/kg/day. Additionally, a low incidence of forestomach squamous papillomas and one forestomach carcinoma were observed at the 18 to 24 mg/kg/day dose, likely due to prolonged direct contact exposure rather than a systemic effect. This dose represents a plasma AUC exposure approximately 26 to 35 times the mean human plasma drug concentration after a 40 mg oral dose.
A carcinogenicity study conducted in mice at doses of 0.3, 15 and 30 mg/kg/day revealed a statistically significant increase in forestomach squamous cell papillomas in females at 15 mg/kg/day and in males and females at 30 mg/kg/day. These doses represent plasma AUC exposures approximately 2 and 7 times the mean human plasma drug concentration after a 40 mg oral dose.
No evidence of mutagenicity was observed in vitro, with or without rat-liver metabolic activation, in the following studies: microbial mutagen tests using mutant strains of Salmonella typhimurium or Escherichia coli; malignant transformation assay in BALB/3T3 cells; unscheduled DNA synthesis in rat primary hepatocytes; chromosomal aberrations in V79 Chinese Hamster cells; HGPRT V79 Chinese Hamster cells. In addition, there was no evidence of genotoxicity in vivo in either a rat chromosome aberration study or mouse micronucleus test.
In a fertility study in rats with daily doses up to 6 mg/kg/day for females and 20 mg/kg/day for males, fluvastatin sodium had no adverse effects on the fertility or reproductive performance.
Hamsters treated for 3 months at 20 mg/kg/day (approximately three times the 40 mg human daily dose based on body surface area, mg/m 2) showed small seminal vesicles and testes, along with tubular degeneration and aspermatogenesis in the testes and vesiculitis in the seminal vesicles. Rats treated for 2 years at 18 mg/kg/day (approximately four times human exposure based on body surface area) exhibited vesiculitis in the seminal vesicles and edema in the testes.
-
14 CLINICAL STUDIES
Secondary Prevention of Cardiovascular Disease
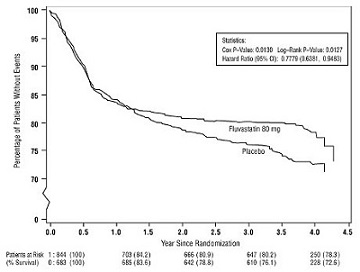
In the Fluvastatin Capsules Intervention Prevention Study (LIPS), the effect of fluvastatin capsules 40 mg administered twice daily on the risk of recurrent cardiac events (time to first occurrence of cardiac death, nonfatal myocardial infarction, or revascularization) was assessed in 1,677 adult patients with CHD who had undergone a percutaneous coronary intervention (PCI) procedure (mean time from PCI to randomization = 3 days). In this multicenter, randomized, double-blind, placebo-controlled trial, patients were treated with dietary/lifestyle counseling and either fluvastatin 40 mg (n = 844) or placebo (n = 833) given twice daily for a median of 3.9 years. The study population was 84% male, 98% White, with 37% > 65 years of age. Mean baseline lipid concentrations were: total cholesterol 201 mg/dL, LDL-C 132 mg/dL, triglycerides 70 mg/dL, and HDL-C 39 mg/dL.
Fluvastatin capsules significantly reduced the risk of recurrent cardiac events (Figure 1) by 22% (p = 0.013, 181 patients in the fluvastatin capsules group versus 222 patients in the placebo group). Revascularization procedures comprised the majority of the initial recurrent cardiac events (143 revascularization procedures in the fluvastatin capsules group and 171 in the placebo group). Consistent trends in risk reduction were observed in patients > 65 years of age.
Figure 1. Primary Endpoint – Recurrent Cardiac Events (Cardiac Death, Nonfatal MI or Revascularization Procedure) (ITT Population)
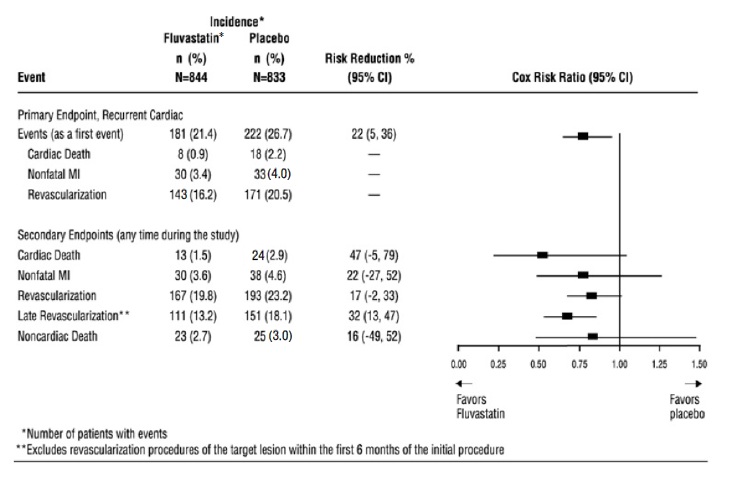
Outcome data for the Fluvastatin Capsules Intervention Prevention Study are shown in Figure 2. After exclusion of revascularization procedures (CABG and repeat PCI) occurring within the first 6 months of the initial procedure involving the originally instrumental site, treatment with fluvastatin capsules was associated with a 32% (p = 0.002) reduction in risk of late revascularization procedures (CABG or PCI occurring at the original site > 6 months after the initial procedure, or at another site).
Figure 2. Fluvastatin Capsules Intervention Prevention Study - Primary and Secondary Endpoints
In the Lipoprotein and Coronary Atherosclerosis Study (LCAS), the effect of fluvastatin capsule therapy on coronary atherosclerosis was assessed by quantitative coronary angiography (QCA) in patients with CAD and mild to moderate hypercholesterolemia (baseline LDL-C range 115 to 190 mg/dL). In this randomized double-blind, placebo-controlled trial, 429 patients were treated with conventional measures (Step 1, AHA Diet) and either fluvastatin 40 mg/day or placebo. In order to provide treatment to patients receiving placebo with LDL-C levels ≥ 160 mg/dL at baseline, adjunctive therapy with cholestyramine was added after Week 12 to all patients in the study with baseline LDL-C values of ≥ 160 mg/dL, which were present in 25% of the study population. Quantitative coronary angiograms were evaluated at baseline and 2.5 years in 340 (79%) angiographic evaluable patients.
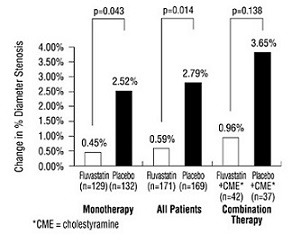
Compared to placebo, fluvastatin capsules significantly slowed the progression of coronary atherosclerosis as measured by within-patient per-lesion change in minimum lumen diameter (MLD), the primary endpoint (Figure 3 below), percent diameter stenosis (Figure 4), and the formation of new lesions (13% of all fluvastatin patients versus 22% of all placebo patients). A significant difference in favor of fluvastatin capsules was found between all fluvastatin and all placebo patients in the distribution among the three categories of definite progression, definite regression, and mixed or no change. Beneficial angiographic results (change in MLD) were independent of patients’ gender and consistent across a range of baseline LDL-C levels.
Figure 3. Change in Minimum Lumen Diameter (mm)
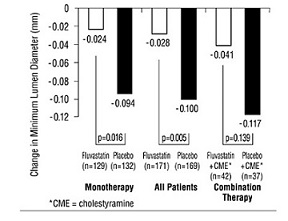
Figure 4. Change in % Diameter Stenosis
Primary Hyperlipidemia in Adults
Fluvastatin sodium extended-release tablets have been studied in five controlled trials of adult patients with primary hyperlipidemia and mixed dyslipidemia. Fluvastatin sodium extended-release tablets were administered to over 900 patients in trials from 4 to 26 weeks in duration. In the three largest of these trials, fluvastatin sodium extended-release tablets given as a single daily dose of 80 mg significantly reduced Total-C, LDL-C, TG, and Apo B (Table 5).
In patients with primary mixed dyslipidemia as defined by baseline plasma TG levels ≥ 200 mg/dL and < 400 mg/dL, treatment with fluvastatin produced significant decreases in Total-C, LDL-C, TG, and Apo B (see Table 7).
Table 7. Median Percent Change in Lipid Levels in Adult Patients with Primary Hyperlipidemia and Mixed Dyslipidemia From Baseline to Week 24 Endpoint All Active Controlled Trials (Fluvastatin sodium extended-release tablets) TotalChol TG LDL Apo B HDL Dose N % ∆ N % ∆ N % ∆ N % ∆ N % ∆ All Patients Fluvastatin sodium extended-release tablets 80 mg a 750 -25 750 -19 748 -35 745 -27 750 +7 Baseline TG ≥ 200 mg/dL Fluvastatin sodium extended-release tablets 80 mg a 239 -25 239 -25 237 -33 235 -27 239 +11 aData for fluvastatin sodium extended-release 80 mg tablet from three 24-week controlled trials. HeFH in Pediatric Patients Aged 10 Years and Older
Fluvastatin capsules were studied in two open-label, uncontrolled, dose-titration trials. The first trial enrolled 29 pre-pubertal males, 9 to 12 years of age, who had an LDL-C level > 90th percentile for age and one parent with primary hypercholesterolemia and either a family history of premature ischemic heart disease or tendon xanthomas. The mean baseline LDL-C was 226 mg/dL (range, 137 to 354 mg/dL). All patients were started on fluvastatin capsules 20 mg daily with dose adjustments every 6 weeks to 40 mg daily then 80 mg daily (40 mg twice daily) to achieve an LDL-C goal between 97 to 124 mg/dL. Endpoint analyses were performed at Year 2. Fluvastatin decreased plasma levels of Total-C and LDL-C by 21% and 27%, respectively. The mean achieved LDL-C was 161 mg/dL (range, 74 to 336 mg/dL).
The second trial enrolled 85 male and female patients, 10 to 16 years of age, who had an LDL-C > 190 mg/dL or LDL-C > 160 mg/dL and one or more risk factors for coronary heart disease, or LDL-C > 160 mg/dL and a proven LDL-receptor defect. The mean baseline LDL-C was 225 mg/dL (range, 148 to 343 mg/dL). All patients were started on fluvastatin capsules 20 mg daily with dose adjustments every 6 weeks to 40 mg daily then 80 mg daily (fluvastatin sodium 80 mg extended-release tablets) to achieve an LDL-C goal of < 130 mg/dL. Endpoint analyses were performed at Week 114. Fluvastatin decreased plasma levels of Total-C and LDL-C by 22% and 28%, respectively. The mean achieved LDL-C was 159 mg/dL (range, 90 to 295 mg/dL).
The majority of patients in both trials (83% in the first trial and 89% in the second trial) were titrated to the maximum daily dose of 80 mg.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
Fluvastatin sodium extended-release tablets supplied as:
Strength How supplied NDC Tablet description 80 mg of fluvastatin bottles of 30 0527-2580-32 Yellow, round, slightly biconvex film-coated tablets, imprinted with “BS08” and “80” on one side, plain on the other side. bottles of 100 0527-2580-37 Store and Dispense
Store at 20ºC to 25ºC (68ºF to 77ºF); excursions permitted to15ºC to 30ºC (59ºF to 86ºF) [see USP Controlled Room Temperature]. Dispense in a tight container. Protect from light.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Myopathy and Rhabdomyolysis
Advise patients that fluvastatin may cause myopathy and rhabdomyolysis. Instruct patients to promptly report any unexplained muscle pain, tenderness, or weakness particularly if accompanied by malaise or fever [see Warnings and Precautions (5.1), Drug Interactions (7.1)].
Hepatic Dysfunction
Inform patients that fluvastatin may cause liver enzyme elevations and possibly liver failure. Advise patients to promptly report fatigue, anorexia, right upper abdominal discomfort, dark urine, or jaundice [see Warnings and Precautions (5.3)].
Increases in HbA1c and Fasting Serum Glucose Levels
Inform patients that increases in HbA1c and fasting serum glucose levels may occur with fluvastatin. Encourage patients to optimize lifestyle measures, including regular exercise, maintaining a healthy body weight, and making healthy food choices [see Warnings and Precautions (5.4)].
Pregnancy
Advise pregnant patients and patients who can become pregnant of the potential risk to a fetus. Advise patients to inform their healthcare provider of a known or suspected pregnancy to discuss if fluvastatin should be discontinued [see Use in Specific Populations (8.1)].
Lactation
Advise patients that breastfeeding is not recommended during treatment with fluvastatin [see Use in Specific Populations (8.2)].
Distributed by:
Lannett Company, Inc.
Philadelphia, PA 19136Manufactured by:
Beijing Sciecure Pharmaceutical Co., Ltd.
Zhongbei Industrial Park, Beishicao Town, Shunyi District, Beijing 101301, ChinaRevised: XX 2024
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
FLUVASTATIN SODIUM EXTENDED-RELEASE TABLETS
(fluvastatin)
extended-release tablets, for oral useYou must read and follow all instructions before using fluvastatin sodium extended-release tablets.
Read this Patient Information before you start taking fluvastatin sodium extended-release tablets and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment. If you have any questions about fluvastatin sodium extended-release tablets, ask your doctor or pharmacist.
What are fluvastatin sodium extended-release tablets?
Fluvastatin sodium extended-release tablets are prescription medicines “that contain the cholesterol lowering medicine, fluvastatin.”
Fluvastatin sodium extended-release tablets are used in adults with heart disease (coronary artery disease) to:
- lower the need for heart and blood vessel procedures to improve flow to the heart, called coronary revascularization.
- slow the buildup of too much cholesterol in the arteries of the heart.
Fluvastatin sodium extended-release tablets are used along with diet to lower the level of:
- low-density lipoprotein cholesterol (LDL-C) or “bad” cholesterol in adults with hyperlipidemia (high levels of fat in the blood)
- LDL-C in adults and children 10 years of age and older with heterozygous familial hypercholesterolemia (HeFH), an inherited condition that causes high levels of LDL, who require 80 mg of fluvastatin daily.
The safety and effectiveness of fluvastatin has not been established in children younger than 10 years of age with heterozygous familial hypercholesterolemia (HeFH) or in children with other types of hyperlipidemia (high levels in fat in the blood) other than HeFH.
Do not take fluvastatin sodium extended-release tablets if you:
- have liver problems (acute liver failure or decompensated cirrhosis)
- are allergic to fluvastatin or any of the ingredients in fluvastatin sodium extended-release tablets. See the end of this Patient Information leaflet for a complete list of ingredients in fluvastatin sodium extended-release tablets.
Before you take fluvastatin sodium extended-release tablets, tell your healthcare provider about all of your medical conditions, including if you:
- have muscle aches or weakness
- drink more than 2 glasses of alcohol daily
- have diabetes
- have a thyroid problem
- have kidney problems
- are pregnant or plan to become pregnant. If you become pregnant while taking fluvastatin sodium extended-release tablets, stop taking fluvastatin sodium extended-release tablets and call your healthcare provider.
- are breastfeeding or plan to breastfeed. It is not known if fluvastatin sodium extended-release tablets pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby if you take fluvastatin sodium extended-release tablets. You should not breastfeed while taking fluvastatin sodium extended-release tablets
Tell your healthcare provider about all the medicines you take,including prescription and over-the-counter medicines, vitamins, and herbal supplements. Talk to your healthcare provider before you start taking any new medicines. Tell your healthcare provider who prescribes fluvastatin sodium extended-release tablets if another healthcare provider increases the dose of another medicine you are taking.
Fluvastatin sodium extended-release tablets may affect the way other medicines work, and other medicines may affect how fluvastatin sodium extended-release tablets work. Especially tell your healthcare provider if you take:
- warfarin (a medicine used to reduce blood clotting)
- glyburide (a medicine used to treat diabetes)
- phenytoin (a medicine used to treat epilepsy)
Taking fluvastatin sodium extended-release tablets with certain medicines can also increase the risk of muscle problems. Especially tell your healthcare provider if you take:
- gemfibrozil (a medicine used to lower triglycerides)
- cyclosporine (a medicine used to suppress the immune system)
- fluconazole (a medicine used to treat fungal infections)
- fibrates or niacin
- colchicine
Ask your healthcare provider or pharmacist for a list of medicines if you are not sure. Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I take fluvastatin sodium extended-release tablets?
- Take fluvastatin sodium extended-release tablets exactly as your healthcare provider tells you to take it.
- Do notchange your dose or stop taking fluvastatin sodium extended-release tablets without talking to your healthcare provider.
- Take fluvastatin sodium extended-release tablets 1 time each day, at any time of the day. Fluvastatin sodium extended-release tablets can be taken with or without food.
- Fluvastatin sodium extended-release tablets must be swallowed whole with a liquid. Do not break, crush or chew fluvastatin sodium extended-release tablets. Tell your healthcare provider if you cannot swallow tablets whole. You may need fluvastatin capsules or a different medicine instead of fluvastatin sodium extended-release tablets.
- While taking fluvastatin sodium extended-release tablets, continue to follow your cholesterol-lowing diet and exercise as your healthcare provider told you to.
- In case of overdose, get medical help or contact a Poison Center expert right away at 1-800-222-1222. Advice is also available online at poisonhelp.org.
What are the possible side effects of fluvastatin sodium extended-release tablets?
Fluvastatin sodium extended-release tablets may cause serious side effects, including:
- Muscle pain, tenderness, and weakness (myopathy).Muscle problems, including muscle breakdown, can be serious in some people and rarely cause kidney damage that can lead to death.
Tell your healthcare provider right away if you have:
- unexplained muscle pain, tenderness, or weakness, especially if you have a fever or feel more tired than usual, while you take fluvastatin sodium extended-release tablets.
- muscle problems that do not go away even after your healthcare provider has advised you to stop taking fluvastatin sodium extended-release tablets. Your healthcare provider may do further tests to diagnose the cause of your muscle problems. Your chances of getting muscle problems are higher if you:
◦ are taking certain other medicines while you take fluvastatin sodium extended-release tablets
◦ are 65 years of age or older
◦ have thyroid problems (hypothyroidism) that are not controlled
◦ have kidney problems- Liver problems.Your healthcare provider should do blood tests to check your liver before you start taking fluvastatin sodium extended-release tablets, and if you have symptoms of liver problems while you take fluvastatin sodium extended-release tablets. Call your healthcare provider right away if you have the following symptoms of liver problems:
◦ feel tired or weak
◦ loss of appetite
◦ right sided upper belly pain
◦ dark amber colored urine
◦ yellowing of your skin or the whites of your eye- Increase in blood sugar (glucose) levels.Fluvastatin sodium extended-release tablets may cause an increase in your blood sugar levels.
The most common side effects of fluvastatin sodium extended-release tablets include:
- flu-like symptoms
- sinus infection
- upset stomach and stomach pain
- urinary tract infections
- bronchitis
- nausea
These side effects are usually mild and may go away. The following additional side effects have been reported with fluvastatin sodium extended-release tablets:
- memory loss and confusion
Talk to your healthcare provider or pharmacist if you have side effects that bother you or does not go away.
These are not all the possible side effects of fluvastatin sodium extended-release tablets. Call your healthcare provider for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.How should I store fluvastatin sodium extended-release tablets?
- Store fluvastatin sodium extended-release tablets at room temperature 68°F to 77°F (20°C to 25°C). Protect from light.
- Keep fluvastatin sodium extended-release tablets out of the reach of children.Be sure that if you throw medicines away, it is out of the reach of children.
General information about safe and effective use of fluvastatin sodium extended-release tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information Leaflet. Do not use fluvastatin sodium extended-release tablets for a condition for which it was not prescribed. Do not give fluvastatin sodium extended-release tablets to other people, even if they have the same medical condition you have; it may harm them.
You can ask your pharmacist or healthcare provider for information about fluvastatin sodium extended-release tablets that is written for health professionals.What are the ingredients in fluvastatin sodium extended-release tablets?
Active Ingredient: fluvastatin
Inactive Ingredients: glycerol dibehenate, pregelatinized starch, hypromellose, potassium bicarbonate, magnesium stearate, polyvinyl alcohol, titanium dioxide, talc, lecithin (soya), yellow iron oxide non-irradiated, shellac glaze (modified) in SD-45, isopropyl alcohol, black iron oxide non-irradiated, N-butyl alcohol, propylene glycol, ammonium hydroxide.Distributed by:
Lannett Company, Inc.
Philadelphia, PA 19136Manufactured by:
Beijing Sciecure Pharmaceutical Co., Ltd.
Zhongbei Industrial Park, Beishicao Town, Shunyi District, Beijing 101301, ChinaThis Patient Information has been approved by the U.S. Food and Drug Administration. Revised: XX/2024
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL – 80 mg
NDC 0527- 2580-32
Fluvastatin Sodium
Extended-Release
Tablets
80 mg*30 Tablets
Rx only
*Each film-coated tablet contains fluvastatin
sodium, USP equivalent to 80 mgof fluvastatin.Usual Dosage:See package insert.
Store at 25°C (77°F); excursions permitted to
15-30°C (59-86°F)
[see USP controlled room temperature].
Protect from light. Dispense in a tight container.
Keep this and all drugs out of the reach of children.Mfd by:
Beijing Sciecure Pharmaceutical Co. Ltd.Distributed by:
Lannett Company, Inc.
Philadelphia, PA 19136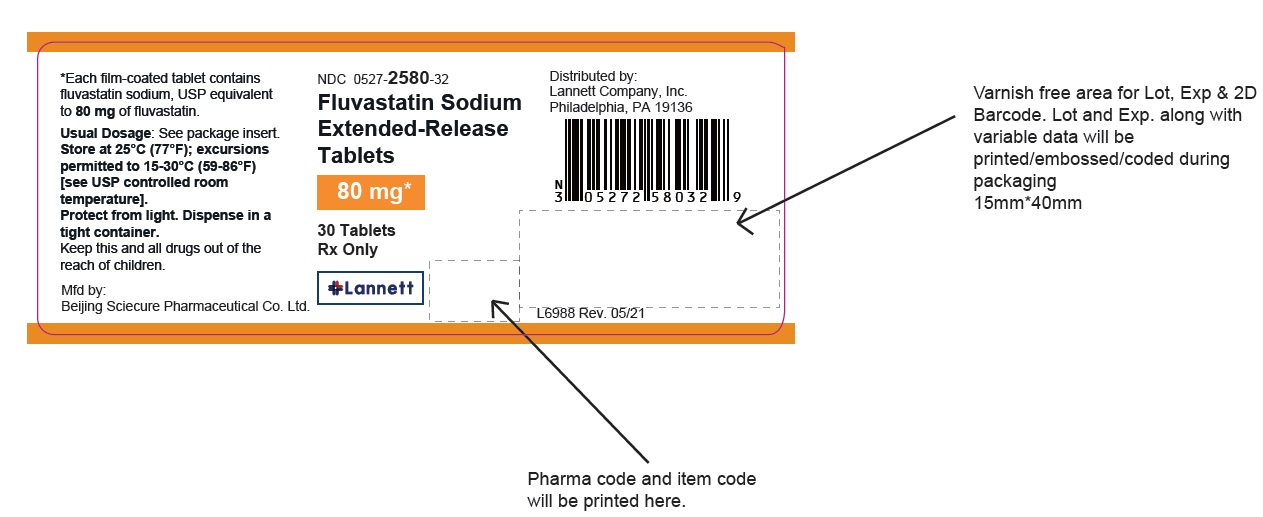
NDC 0527- 2580-37
100 Tablets
Rx only

-
INGREDIENTS AND APPEARANCE
FLUVASTATIN SODIUM
fluvastatin sodium tablet, film coated, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0527-2580 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FLUVASTATIN SODIUM (UNII: PYF7O1FV7F) (FLUVASTATIN - UNII:4L066368AS) FLUVASTATIN 80 mg Inactive Ingredients Ingredient Name Strength GLYCERYL DIBEHENATE (UNII: R8WTH25YS2) STARCH, PREGELATINIZED CORN (UNII: O8232NY3SJ) HYPROMELLOSE 2208 (100 MPA.S) (UNII: B1QE5P712K) HYPROMELLOSE 2910 (15 MPA.S) (UNII: 36SFW2JZ0W) POTASSIUM BICARBONATE (UNII: HM5Z15LEBN) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TALC (UNII: 7SEV7J4R1U) LECITHIN, SOYBEAN (UNII: 1DI56QDM62) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color yellow Score no score Shape ROUND Size 10mm Flavor Imprint Code BS08;80 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0527-2580-32 30 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 05/07/2021 2 NDC: 0527-2580-37 100 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 03/14/2022 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209397 05/07/2021 Labeler - Lannett Company, Inc. (002277481) Registrant - Lannett Company, Inc. (002277481) Establishment Name Address ID/FEI Business Operations Beijing Sciecure Pharmaceutical Co., Ltd. 547707195 manufacture(0527-2580)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.