JARDIANCE ®(empagliflozin tablets), for oral use
Jardiance by
Drug Labeling and Warnings
Jardiance by is a Prescription medication manufactured, distributed, or labeled by Praxis, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
JARDIANCE- empagliflozin tablet, film coated
Praxis, LLC
----------
JARDIANCE ®(empagliflozin tablets), for oral use
10 OVERDOSAGE
In the event of an overdose with JARDIANCE, consider contacting the Poison Help line (1-800-222-1222) or a medical toxicologist for additional overdosage management recommendations. Removal of empagliflozin by hemodialysis has not been studied.
11 DESCRIPTION
JARDIANCE tablets for oral use contain empagliflozin, an inhibitor of the SGLT2.
The chemical name of empagliflozin is D-Glucitol,1,5-anhydro-1-C-[4-chloro-3-[[4-[[(3S)-tetrahydro-3-furanyl]oxy]phenyl]methyl]phenyl]-, (1S).
Its molecular formula is C 23H 27ClO 7and the molecular weight is 450.91. The structural formula is:
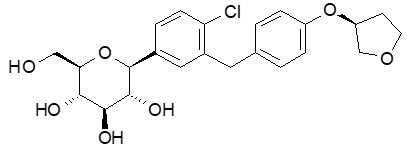
Empagliflozin is a white to yellowish, non-hygroscopic powder. It is very slightly soluble in water, sparingly soluble in methanol, slightly soluble in ethanol and acetonitrile, soluble in 50% acetonitrile/water, and practically insoluble in toluene.
Each film-coated tablet of JARDIANCE contains 10 mg or 25 mg of empagliflozin (free base) and the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hydroxypropyl cellulose, lactose monohydrate, magnesium stearate, and microcrystalline cellulose. In addition, the film coating contains the following inactive ingredients: hypromellose, polyethylene glycol, talc, titanium dioxide, and yellow ferric oxide.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Empagliflozin is an inhibitor of SGLT2, the predominant transporter responsible for reabsorption of glucose from the glomerular filtrate back into the circulation. By inhibiting SGLT2, empagliflozin reduces renal reabsorption of filtered glucose and lowers the renal threshold for glucose, and thereby increases urinary glucose excretion.
Empagliflozin also reduces sodium reabsorption and increases the delivery of sodium to the distal tubule. This may influence several physiological functions including, but not restricted to, increasing tubuloglomerular feedback and reducing intraglomerular pressure, lowering both pre- and afterload of the heart and downregulating sympathetic activity.
12.2 Pharmacodynamics
Urinary Glucose Excretion
In patients with type 2 diabetes mellitus, urinary glucose excretion increased immediately following a dose of empagliflozin and was maintained at the end of a 4-week treatment period averaging at approximately 64 grams per day with 10 mg empagliflozin and 78 grams per day with 25 mg empagliflozin once daily [see Clinical Studies (14)]. Data from single oral doses of empagliflozin in healthy subjects indicate that, on average, the elevation in urinary glucose excretion approaches baseline by about 3 days for the 10 mg and 25 mg doses.
Urinary Volume
In a 5-day study, mean 24-hour urine volume increase from baseline was 341 mL on Day 1 and 135 mL on Day 5 of empagliflozin 25 mg once daily treatment.
Cardiac Electrophysiology
In a randomized, placebo-controlled, active-comparator, crossover study, 30 healthy subjects were administered a single oral dose of empagliflozin 25 mg, empagliflozin 200 mg (8 times the maximum dose), moxifloxacin, and placebo. No increase in QTc was observed with either 25 mg or 200 mg empagliflozin.
12.3 Pharmacokinetics
The pharmacokinetics of empagliflozin has been characterized in healthy volunteers and patients with type 2 diabetes mellitus and no clinically relevant differences were noted between the two populations. The steady-state mean plasma AUC and C maxwere 1,870 nmol∙h/L and 259 nmol/L, respectively, with 10 mg empagliflozin once daily treatment, and 4,740 nmol∙h/L and 687 nmol/L, respectively, with 25 mg empagliflozin once daily treatment. Systemic exposure of empagliflozin increased in a dose-proportional manner in the therapeutic dose range. Empagliflozin does not appear to have time-dependent pharmacokinetic characteristics. Following once-daily dosing, up to 22% accumulation, with respect to plasma AUC, was observed at steady-state.
Absorption
After oral administration, peak plasma concentrations of empagliflozin were reached at 1.5 hours post-dose. Administration of 25 mg empagliflozin after intake of a high-fat and high-calorie meal resulted in slightly lower exposure; AUC decreased by approximately 16% and C maxdecreased by approximately 37%, compared to fasted condition. The observed effect of food on empagliflozin pharmacokinetics was not considered clinically relevant and empagliflozin may be administered with or without food.
Distribution
The apparent steady-state volume of distribution was estimated to be 73.8 L based on a population pharmacokinetic analysis. Following administration of an oral [ 14C]-empagliflozin solution to healthy subjects, the red blood cell partitioning was approximately 36.8% and plasma protein binding was 86.2%.
Elimination
The apparent terminal elimination half-life of empagliflozin was estimated to be 12.4 h and apparent oral clearance was 10.6 L/h based on the population pharmacokinetic analysis.
Metabolism
No major metabolites of empagliflozin were detected in human plasma and the most abundant metabolites were three glucuronide conjugates (2-O-, 3-O-, and 6-O-glucuronide). Systemic exposure of each metabolite was less than 10% of total drug-related material. In vitrostudies suggested that the primary route of metabolism of empagliflozin in humans is glucuronidation by the uridine 5'-diphospho-glucuronosyltransferases UGT2B7, UGT1A3, UGT1A8, and UGT1A9.
Excretion
Following administration of an oral [ 14C]-empagliflozin solution to healthy subjects, approximately 95.6% of the drug-related radioactivity was eliminated in feces (41.2%) or urine (54.4%). The majority of drug-related radioactivity recovered in feces was unchanged parent drug and approximately half of drug-related radioactivity excreted in urine was unchanged parent drug.
Specific Populations
Pediatric Patients
The pharmacokinetics and pharmacodynamics of empagliflozin were investigated in pediatric patients aged 10 to 17 years with type 2 diabetes mellitus. Oral administration of empagliflozin at 10 mg and 25 mg resulted in exposure within the range observed in adult patients.
Effects of Age, Body Mass Index, Gender, and Race
Age, body mass index (BMI), gender and race (Asians versus primarily Whites) do not have a clinically meaningful effect on pharmacokinetics of empagliflozin.
Patients with Hepatic Impairment
In adult patients with mild, moderate, and severe hepatic impairment according to the Child-Pugh classification, AUC of empagliflozin increased by approximately 23%, 47%, and 75%, and C maxincreased by approximately 4%, 23%, and 48%, respectively, compared to subjects with normal hepatic function.
Patients with Renal Impairment
In adult patients with type 2 diabetes mellitus with mild (eGFR: 60 to less than 90 mL/min/1.73 m 2), moderate (eGFR: 30 to less than 60 mL/min/1.73 m 2), and severe (eGFR: less than 30 mL/min/1.73 m 2) renal impairment and patients on dialysis due to kidney failure, AUC of empagliflozin increased by approximately 18%, 20%, 66%, and 48%, respectively, compared to subjects with normal renal function. Peak plasma levels of empagliflozin were similar in patients with moderate renal impairment and patients on dialysis due to kidney failure compared to subjects with normal renal function. Peak plasma levels of empagliflozin were roughly 20% higher in patients with mild and severe renal impairment as compared to patients with normal renal function. Population pharmacokinetic analysis showed that the apparent oral clearance of empagliflozin decreased, with a decrease in eGFR leading to an increase in drug exposure. However, the fraction of empagliflozin that was excreted unchanged in urine, and urinary glucose excretion, declined with decrease in eGFR.
Drug Interaction Studies
In vitroAssessment of Drug Interactions
Empagliflozin does not inhibit, inactivate, or induce CYP450 isoforms. In vitrodata suggest that the primary route of metabolism of empagliflozin in humans is glucuronidation by the uridine 5'-diphospho-glucuronosyltransferases UGT1A3, UGT1A8, UGT1A9, and UGT2B7. Empagliflozin does not inhibit UGT1A1, UGT1A3, UGT1A8, UGT1A9, or UGT2B7. Therefore, no effect of empagliflozin is anticipated on concomitantly administered drugs that are substrates of the major CYP450 isoforms or UGT1A1, UGT1A3, UGT1A8, UGT1A9, or UGT2B7. The effect of UGT induction (e.g., induction by rifampicin or any other UGT enzyme inducer) on empagliflozin exposure has not been evaluated.
Empagliflozin is a substrate for P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP), but it does not inhibit these efflux transporters at therapeutic doses. Based on in vitrostudies, empagliflozin is considered unlikely to cause interactions with drugs that are P-gp substrates. Empagliflozin is a substrate of the human uptake transporters OAT3, OATP1B1, and OATP1B3, but not OAT1 and OCT2. Empagliflozin does not inhibit any of these human uptake transporters at clinically relevant plasma concentrations and, therefore, no effect of empagliflozin is anticipated on concomitantly administered drugs that are substrates of these uptake transporters.
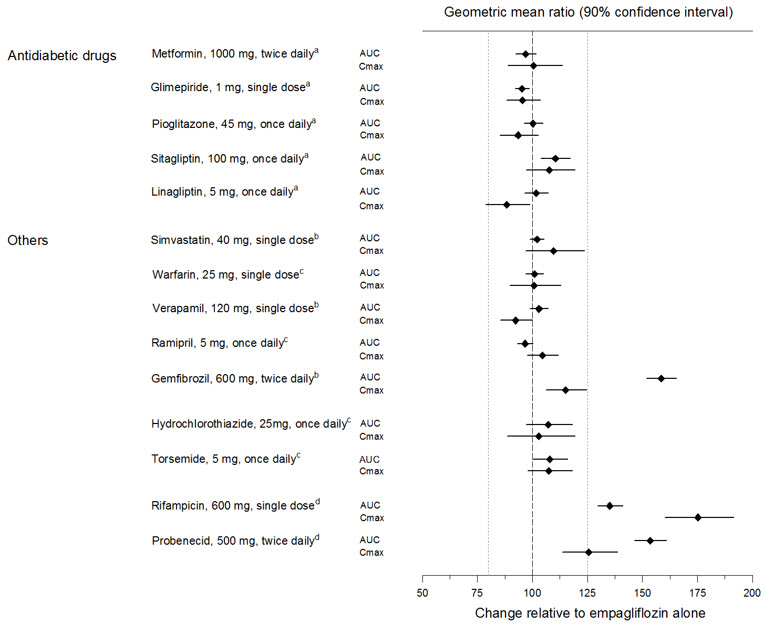
In vivoAssessment of Drug Interactions
Empagliflozin pharmacokinetics were similar with and without coadministration of metformin, glimepiride, pioglitazone, sitagliptin, linagliptin, warfarin, verapamil, ramipril, and simvastatin in healthy volunteers and with or without coadministration of hydrochlorothiazide and torsemide in patients with type 2 diabetes mellitus (see Figure 1). In subjects with normal renal function, coadministration of empagliflozin with probenecid resulted in a 30% decrease in the fraction of empagliflozin excreted in urine without any effect on 24-hour urinary glucose excretion. The relevance of this observation to patients with renal impairment is unknown.
| aempagliflozin, 50 mg, once daily; bempagliflozin, 25 mg, single dose; cempagliflozin, 25 mg, once daily; dempagliflozin, 10 mg, single dose |
 |
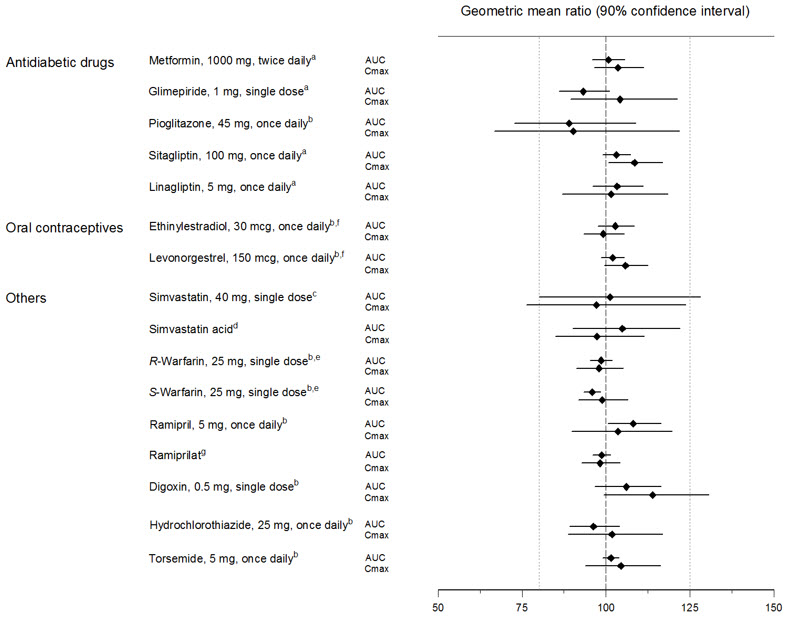
Empagliflozin had no clinically relevant effect on the pharmacokinetics of metformin, glimepiride, pioglitazone, sitagliptin, linagliptin, warfarin, digoxin, ramipril, simvastatin, hydrochlorothiazide, torsemide, and oral contraceptives when coadministered in healthy volunteers (see Figure 2).
| aempagliflozin, 50 mg, once daily; bempagliflozin, 25 mg, once daily; cempagliflozin, 25 mg, single dose; dadministered as simvastatin; eadministered as warfarin racemic mixture; fadministered as Microgynon ®; gadministered as ramipril |
 |
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Carcinogenesis was evaluated in 2-year studies conducted in CD-1 mice and Wistar rats. Empagliflozin did not increase the incidence of tumors in female rats dosed at 100, 300, or 700 mg/kg/day (up to 72 times the exposure from the maximum clinical dose of 25 mg). In male rats, hemangiomas of the mesenteric lymph node were increased significantly at 700 mg/kg/day or approximately 42 times the exposure from a 25 mg clinical dose. Empagliflozin did not increase the incidence of tumors in female mice dosed at 100, 300, or 1,000 mg/kg/day (up to 62 times the exposure from a 25 mg clinical dose). Renal tubule adenomas and carcinomas were observed in male mice at 1,000 mg/kg/day, which is approximately 45 times the exposure of the maximum clinical dose of 25 mg. These tumors may be associated with a metabolic pathway predominantly present in the male mouse kidney.
14 CLINICAL STUDIES
14.1 Glycemic Control Trials in Adults with Type 2 Diabetes Mellitus
JARDIANCE has been studied as monotherapy and in combination with metformin, sulfonylurea, pioglitazone, linagliptin, and insulin. JARDIANCE has also been studied in patients with type 2 diabetes mellitus with mild or moderate renal impairment.
In adult patients with type 2 diabetes mellitus, treatment with JARDIANCE reduced hemoglobin A1c (HbA1c), compared to placebo. The reduction in HbA1c for JARDIANCE compared with placebo was observed across subgroups including sex, race, geographic region, baseline BMI and duration of disease.
Monotherapy
A total of 986 patients with type 2 diabetes mellitus participated in a double-blind, placebo-controlled trial to evaluate the efficacy of JARDIANCE monotherapy.
Treatment-naïve patients with inadequately controlled type 2 diabetes mellitus entered an open-label placebo run-in for 2 weeks. At the end of the run-in period, patients who remained inadequately controlled and had an HbA1c between 7% and 10% were randomized to placebo, JARDIANCE 10 mg, JARDIANCE 25 mg, or a reference comparator.
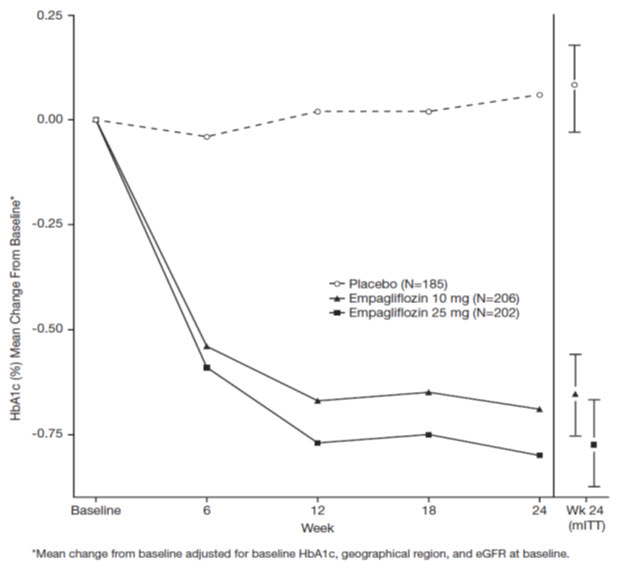
At Week 24, treatment with JARDIANCE 10 mg or 25 mg daily provided statistically significant reductions in HbA1c (p-value <0.0001), fasting plasma glucose (FPG), and body weight compared with placebo (see Table 5and Figure 3).
| JARDIANCE
10 mg N=224 | JARDIANCE
25 mg N=224 | Placebo
N=228 |
|
|---|---|---|---|
| aModified intent-to-treat population. Last observation on trial (LOCF) was used to impute missing data at Week 24. At Week 24, 9.4%, 9.4%, and 30.7% was imputed for patients randomized to JARDIANCE 10 mg, JARDIANCE 25 mg, and placebo, respectively.
bANCOVA derived p-value <0.0001 (HbA1c: ANCOVA model includes baseline HbA1c, treatment, renal function, and region. Body weight and FPG: same model used as for HbA1c but additionally including baseline body weight/baseline FPG, respectively.) cFPG (mg/dL); for JARDIANCE 10 mg, n=223, for JARDIANCE 25 mg, n=223, and for placebo, n=226 |
|||
| HbA1c (%) a | |||
| Baseline (mean) | 7.9 | 7.9 | 7.9 |
| Change from baseline (adjusted mean) | -0.7 | -0.8 | 0.1 |
| Difference from placebo (adjusted mean) (97.5% CI) | -0.7 b(-0.9, -0.6) | -0.9 b(-1.0, -0.7) | -- |
| Patients [n (%)] achieving HbA1c <7% | 72 (35%) | 88 (44%) | 25 (12%) |
| FPG (mg/dL) c | |||
| Baseline (mean) | 153 | 153 | 155 |
| Change from baseline (adjusted mean) | -19 | -25 | 12 |
| Difference from placebo (adjusted mean) (95% CI) | -31 (-37, -26) | -36 (-42, -31) | -- |
| Body Weight | |||
| Baseline (mean) in kg | 78 | 78 | 78 |
| % change from baseline (adjusted mean) | -2.8 | -3.2 | -0.4 |
| Difference from placebo (adjusted mean) (95% CI) | -2.5 b(-3.1, -1.9) | -2.8 b(-3.4, -2.2) | -- |
 |
At Week 24, the systolic blood pressure was statistically significantly reduced compared to placebo by -2.6 mmHg (placebo-adjusted, p-value=0.0231) in patients randomized to 10 mg of JARDIANCE and by -3.4 mmHg (placebo-corrected, p-value=0.0028) in patients randomized to 25 mg of JARDIANCE.
Add-On Combination Therapy with Metformin
A total of 637 patients with type 2 diabetes mellitus participated in a double-blind, placebo-controlled trial to evaluate the efficacy of JARDIANCE in combination with metformin.
Patients with type 2 diabetes mellitus inadequately controlled on at least 1,500 mg of metformin per day entered an open-label 2-week placebo run-in. At the end of the run-in period, patients who remained inadequately controlled and had an HbA1c between 7% and 10% were randomized to placebo, JARDIANCE 10 mg, or JARDIANCE 25 mg.
At Week 24, treatment with JARDIANCE 10 mg or 25 mg daily provided statistically significant reductions in HbA1c (p-value <0.0001), FPG, and body weight compared with placebo (see Table 6).
| JARDIANCE
10 mg N=217 | JARDIANCE
25 mg N=213 | Placebo
N=207 |
|
|---|---|---|---|
| aModified intent-to-treat population. Last observation on trial (LOCF) was used to impute missing data at Week 24. At Week 24, 9.7%, 14.1%, and 24.6% was imputed for patients randomized to JARDIANCE 10 mg, JARDIANCE 25 mg, and placebo, respectively.
bANCOVA p-value <0.0001 (HbA1c: ANCOVA model includes baseline HbA1c, treatment, renal function, and region. Body weight and FPG: same model used as for HbA1c but additionally including baseline body weight/baseline FPG, respectively.) cFPG (mg/dL); for JARDIANCE 10 mg, n=216, for JARDIANCE 25 mg, n=213, and for placebo, n=207 |
|||
| HbA1c (%) a | |||
| Baseline (mean) | 7.9 | 7.9 | 7.9 |
| Change from baseline (adjusted mean) | -0.7 | -0.8 | -0.1 |
| Difference from placebo + metformin (adjusted mean) (95% CI) | -0.6 b(-0.7, -0.4) | -0.6 b(-0.8, -0.5) | -- |
| Patients [n (%)] achieving HbA1c <7% | 75 (38%) | 74 (39%) | 23 (13%) |
| FPG (mg/dL) c | |||
| Baseline (mean) | 155 | 149 | 156 |
| Change from baseline (adjusted mean) | -20 | -22 | 6 |
| Difference from placebo + metformin (adjusted mean) | -26 | -29 | -- |
| Body Weight | |||
| Baseline mean in kg | 82 | 82 | 80 |
| % change from baseline (adjusted mean) | -2.5 | -2.9 | -0.5 |
| Difference from placebo (adjusted mean) (95% CI) | -2.0 b(-2.6, -1.4) | -2.5 b(-3.1, -1.9) | -- |
At Week 24, the systolic blood pressure was statistically significantly reduced compared to placebo by -4.1 mmHg (placebo-corrected, p-value <0.0001) for JARDIANCE 10 mg and -4.8 mmHg (placebo-corrected, p-value <0.0001) for JARDIANCE 25 mg.
Initial Combination Therapy with Metformin
A total of 1,364 patients with type 2 diabetes mellitus participated in a double-blind, randomized, active-controlled trial to evaluate the efficacy of JARDIANCE in combination with metformin as initial therapy compared to the corresponding individual components.
Treatment-naïve patients with inadequately controlled type 2 diabetes mellitus entered an open-label placebo run-in for 2 weeks. At the end of the run-in period, patients who remained inadequately controlled and had an HbA1c between 7% and 10.5% were randomized to one of 8 active-treatment arms: JARDIANCE 10 mg or 25 mg; metformin 1,000 mg, or 2,000 mg; JARDIANCE 10 mg in combination with 1,000 mg or 2,000 mg metformin; or JARDIANCE 25 mg in combination with 1,000 mg or 2,000 mg metformin.
At Week 24, initial therapy of JARDIANCE in combination with metformin provided statistically significant reductions in HbA1c (p-value <0.01) compared to the individual components (see Table 7).
| JARDIANCE
10 mg + Metformin 1,000 mg a N=161 | JARDIANCE
10 mg + Metformin 2,000 mg a N=167 | JARDIANCE
25 mg + Metformin 1,000 mg a N=165 | JARDIANCE
25 mg + Metformin 2,000 mg a N=169 | JARDIANCE
10 mg N=169 | JARDIANCE
25 mg N=163 | Metformin
1,000 mg a N=167 | Metformin
2,000 mg a N=162 |
|
|---|---|---|---|---|---|---|---|---|
| aMetformin total daily dose, administered in two equally divided doses per day.
bp-value ≤0.0062 (modified intent-to-treat population [observed case] MMRM model included treatment, renal function, region, visit, visit by treatment interaction, and baseline HbA1c). cp-value ≤0.0056 (modified intent-to-treat population [observed case] MMRM model included treatment, renal function, region, visit, visit by treatment interaction, and baseline HbA1c). |
||||||||
| HbA1c (%) | ||||||||
| Baseline (mean) | 8.7 | 8.7 | 8.8 | 8.7 | 8.6 | 8.9 | 8.7 | 8.6 |
| Change from baseline (adjusted mean) | -2.0 | -2.1 | -1.9 | -2.1 | -1.4 | -1.4 | -1.2 | -1.8 |
| Comparison vs JARDIANCE (adjusted mean) (95% CI) | -0.6
b
(-0.9, -0.4) | -0.7
b
(-1.0, -0.5) | -0.6
c
(-0.8, -0.3) | -0.7
c
(-1.0, -0.5) | -- | -- | -- | -- |
| Comparison vs metformin (adjusted mean) (95% CI) | -0.8
b
(-1.0, -0.6) | -0.3
b
(-0.6, -0.1) | -0.8
c
(-1.0, -0.5) | -0.3
c
(-0.6, -0.1) | -- | -- | -- | -- |
Add-On Combination Therapy with Metformin and Sulfonylurea
A total of 666 patients with type 2 diabetes mellitus participated in a double-blind, placebo-controlled trial to evaluate the efficacy of JARDIANCE in combination with metformin plus a sulfonylurea.
Patients with inadequately controlled type 2 diabetes mellitus on at least 1,500 mg per day of metformin and on a sulfonylurea, entered a 2-week open-label placebo run-in. At the end of the run-in, patients who remained inadequately controlled and had an HbA1c between 7% and 10% were randomized to placebo, JARDIANCE 10 mg, or JARDIANCE 25 mg.
Treatment with JARDIANCE 10 mg or 25 mg daily provided statistically significant reductions in HbA1c (p-value <0.0001), FPG, and body weight compared with placebo (see Table 8).
| JARDIANCE
10 mg N=225 | JARDIANCE
25 mg N=216 | Placebo
N=225 |
|
|---|---|---|---|
| aModified intent-to-treat population. Last observation on trial (LOCF) was used to impute missing data at Week 24. At Week 24, 17.8%, 16.7%, and 25.3% was imputed for patients randomized to JARDIANCE 10 mg, JARDIANCE 25 mg, and placebo, respectively.
bANCOVA p-value <0.0001 (HbA1c: ANCOVA model includes baseline HbA1c, treatment, renal function, and region. Body weight and FPG: same model used as for HbA1c but additionally including baseline body weight/baseline FPG, respectively.) cFPG (mg/dL); for JARDIANCE 10 mg, n=225, for JARDIANCE 25 mg, n=215, for placebo, n=224 |
|||
| HbA1c (%) a | |||
| Baseline (mean) | 8.1 | 8.1 | 8.2 |
| Change from baseline (adjusted mean) | -0.8 | -0.8 | -0.2 |
| Difference from placebo (adjusted mean) (95% CI) | -0.6 b(-0.8, -0.5) | -0.6 b(-0.7, -0.4) | -- |
| Patients [n (%)] achieving HbA1c <7% | 55 (26%) | 65 (32%) | 20 (9%) |
| FPG (mg/dL) c | |||
| Baseline (mean) | 151 | 156 | 152 |
| Change from baseline (adjusted mean) | -23 | -23 | 6 |
| Difference from placebo (adjusted mean) | -29 | -29 | -- |
| Body Weight | |||
| Baseline mean in kg | 77 | 78 | 76 |
| % change from baseline (adjusted mean) | -2.9 | -3.2 | -0.5 |
| Difference from placebo (adjusted mean) (95% CI) | -2.4 b(-3.0, -1.8) | -2.7 b(-3.3, -2.1) | -- |
In Combination with Linagliptin as Add-On to Metformin Therapy
A total of 686 patients with type 2 diabetes mellitus participated in a double-blind, active-controlled trial to evaluate the efficacy of JARDIANCE 10 mg or 25 mg in combination with linagliptin 5 mg compared to the individual components.
Patients with type 2 diabetes mellitus inadequately controlled on at least 1,500 mg of metformin per day entered a single-blind placebo run-in period for 2 weeks. At the end of the run-in period, patients who remained inadequately controlled and had an HbA1c between 7% and 10.5% were randomized 1:1:1:1:1 to one of 5 active-treatment arms of JARDIANCE 10 mg or 25 mg, linagliptin 5 mg, or linagliptin 5 mg in combination with 10 mg or 25 mg JARDIANCE as a fixed-dose combination tablet.
At Week 24, JARDIANCE 10 mg or 25 mg used in combination with linagliptin 5 mg provided statistically significant improvement in HbA1c (p-value <0.0001) and FPG (p-value <0.001) compared to the individual components in patients who had been inadequately controlled on metformin. Treatment with JARDIANCE/linagliptin 25 mg/5 mg or JARDIANCE/linagliptin 10 mg/5 mg daily also resulted in a statistically significant reduction in body weight compared to linagliptin 5 mg (p-value <0.0001). There was no statistically significant difference in body weight compared to JARDIANCE alone.
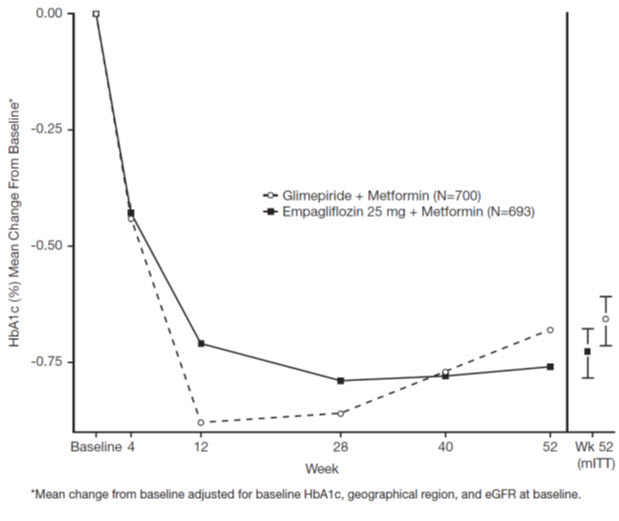
Active-Controlled Trial versus Glimepiride in Combination with Metformin
The efficacy of JARDIANCE was evaluated in a double-blind, glimepiride-controlled, trial in 1,545 patients with type 2 diabetes mellitus with insufficient glycemic control despite metformin therapy.
Patients with inadequate glycemic control and an HbA1c between 7% and 10% after a 2-week run-in period were randomized to glimepiride or JARDIANCE 25 mg.
At Week 52, JARDIANCE 25 mg and glimepiride lowered HbA1c and FPG (see Table 9, Figure 4). The difference in observed effect size between JARDIANCE 25 mg and glimepiride excluded the pre-specified non-inferiority margin of 0.3%. The mean daily dosage of glimepiride was 2.7 mg and the maximal approved dosage in the United States is 8 mg per day.
| JARDIANCE 25 mg
N=765 | Glimepiride
N=780 |
|
|---|---|---|
| aModified intent-to-treat population. Last observation on trial (LOCF) was used to impute data missing at Week 52. At Week 52, data was imputed for 15.3% and 21.9% of patients randomized to JARDIANCE 25 mg and glimepiride, respectively.
bNon-inferior, ANCOVA model p-value <0.0001 (HbA1c: ANCOVA model includes baseline HbA1c, treatment, renal function, and region) cANCOVA p-value <0.0001 (Body weight and FPG: same model used as for HbA1c but additionally including baseline body weight/baseline FPG, respectively.) dFPG (mg/dL); for JARDIANCE 25 mg, n=764, for glimepiride, n=779 |
||
| HbA1c (%) a | ||
| Baseline (mean) | 7.9 | 7.9 |
| Change from baseline (adjusted mean) | -0.7 | -0.7 |
| Difference from glimepiride (adjusted mean) (97.5% CI) | -0.07 b(-0.15, 0.01) | -- |
| FPG (mg/dL) d | ||
| Baseline (mean) | 150 | 150 |
| Change from baseline (adjusted mean) | -19 | -9 |
| Difference from glimepiride (adjusted mean) | -11 | -- |
| Body Weight | ||
| Baseline mean in kg | 82.5 | 83 |
| % change from baseline (adjusted mean) | -3.9 | 2.0 |
| Difference from glimepiride (adjusted mean) (95% CI) | -5.9 c(-6.3, -5.5) | -- |
 |
At Week 52, the adjusted mean change from baseline in systolic blood pressure was -3.6 mmHg, compared to 2.2 mmHg for glimepiride. The differences between treatment groups for systolic blood pressure was statistically significant (p-value <0.0001).
At Week 104, the adjusted mean change from baseline in HbA1c was -0.75% for JARDIANCE 25 mg and -0.66% for glimepiride. The adjusted mean treatment difference was -0.09% with a 97.5% confidence interval of (-0.32%, 0.15%), excluding the pre-specified non-inferiority margin of 0.3%. The mean daily dosage of glimepiride was 2.7 mg and the maximal approved dosage in the United States is 8 mg per day. The Week 104 analysis included data with and without concomitant glycemic rescue medication, as well as off-treatment data. Missing data for patients not providing any information at the visit were imputed based on the observed off-treatment data. In this multiple imputation analysis, 13.9% of the data were imputed for JARDIANCE 25 mg and 12.9% for glimepiride.
At Week 104, JARDIANCE 25 mg daily resulted in a statistically significant difference in change from baseline for body weight compared to glimepiride (-3.1 kg for JARDIANCE 25 mg vs. +1.3 kg for glimepiride; ANCOVA-LOCF, p-value <0.0001).
Add-On Combination Therapy with Pioglitazone with or without Metformin
A total of 498 patients with type 2 diabetes mellitus participated in a double-blind, placebo-controlled trial to evaluate the efficacy of JARDIANCE in combination with pioglitazone, with or without metformin.
Patients with inadequately controlled type 2 diabetes mellitus on metformin at a dose of at least 1,500 mg per day and pioglitazone at a dose of at least 30 mg per day were placed into an open-label placebo run-in for 2 weeks. Patients with inadequate glycemic control and an HbA1c between 7% and 10% after the run-in period were randomized to placebo, JARDIANCE 10 mg, or JARDIANCE 25 mg.
Treatment with JARDIANCE 10 mg or 25 mg daily resulted in statistically significant reductions in HbA1c (p-value <0.0001), FPG, and body weight compared with placebo (see Table 10).
| JARDIANCE
10 mg N=165 | JARDIANCE
25 mg N=168 | Placebo
N=165 |
|
|---|---|---|---|
| aModified intent-to-treat population. Last observation on trial (LOCF) was used to impute missing data at Week 24. At Week 24, 10.9%, 8.3%, and 20.6% was imputed for patients randomized to JARDIANCE 10 mg, JARDIANCE 25 mg, and placebo, respectively.
bANCOVA p-value <0.0001 (HbA1c: ANCOVA model includes baseline HbA1c, treatment, renal function, and background medication. Body weight and FPG: same model used as for HbA1c but additionally including baseline body weight/baseline FPG, respectively.) cFPG (mg/dL); for JARDIANCE 10 mg, n=163 |
|||
| HbA1c (%) a | |||
| Baseline (mean) | 8.1 | 8.1 | 8.2 |
| Change from baseline (adjusted mean) | -0.6 | -0.7 | -0.1 |
| Difference from placebo + pioglitazone (adjusted mean) (95% CI) | -0.5 b(-0.7, -0.3) | -0.6 b(-0.8, -0.4) | -- |
| Patients [n (%)] achieving HbA1c <7% | 36 (24%) | 48 (30%) | 12 (8%) |
| FPG (mg/dL) c | |||
| Baseline (mean) | 152 | 152 | 152 |
| Change from baseline (adjusted mean) | -17 | -22 | 7 |
| Difference from placebo + pioglitazone (adjusted mean) (97.5% CI) | -23 b(-31.8, -15.2) | -28 b(-36.7, -20.2) | -- |
| Body Weight | |||
| Baseline mean in kg | 78 | 79 | 78 |
| % change from baseline (adjusted mean) | -2.0 | -1.8 | 0.6 |
| Difference from placebo (adjusted mean) (95% CI) | -2.6 b(-3.4, -1.8) | -2.4 b(-3.2, -1.6) | -- |
Add-On Combination with Insulin with or without Metformin and/or Sulfonylureas
A total of 494 patients with type 2 diabetes mellitus inadequately controlled on insulin, or insulin in combination with oral drugs participated in a double-blind, placebo-controlled trial to evaluate the efficacy of JARDIANCE as add-on therapy to insulin over 78 weeks.
Patients entered a 2-week placebo run-in period on basal insulin (e.g., insulin glargine, insulin detemir, or NPH insulin) with or without metformin and/or sulfonylurea background therapy. Following the run-in period, patients with inadequate glycemic control were randomized to the addition of JARDIANCE 10 mg, JARDIANCE 25 mg, or placebo. Patients were maintained on a stable dose of insulin prior to enrollment, during the run-in period, and during the first 18 weeks of treatment. For the remaining 60 weeks, insulin could be adjusted. The mean total daily insulin dose at baseline for JARDIANCE 10 mg, 25 mg, and placebo was 45 IU, 48 IU, and 48 IU, respectively.
JARDIANCE used in combination with insulin (with or without metformin and/or sulfonylurea) provided statistically significant reductions in HbA1c and FPG compared to placebo after both 18 and 78 weeks of treatment (see Table 11). JARDIANCE 10 mg or 25 mg daily also resulted in statistically significantly greater percent body weight reduction compared to placebo.
| 18 weeks
(no insulin adjustment) | 78 weeks
(adjustable insulin dose after 18 weeks) |
|||||
|---|---|---|---|---|---|---|
| JARDIANCE
10 mg N=169 | JARDIANCE
25 mg N=155 | Placebo
N=170 | JARDIANCE
10 mg N=169 | JARDIANCE
25 mg N=155 | Placebo
N=170 |
|
| aModified intent-to-treat population. Last observation on trial (LOCF) was used to impute missing data at Week 18 and 78. At Week 18, 21.3%, 30.3%, and 21.8% was imputed for patients randomized to JARDIANCE 10 mg, JARDIANCE 25 mg, and placebo, respectively. At Week 78, 32.5%, 38.1% and 42.4% was imputed for patients randomized to JARDIANCE 10 mg, JARDIANCE 25 mg, and placebo, respectively.
bANCOVA p-value <0.0001 (HbA1c: ANCOVA model includes baseline HbA1c, treatment, and region; FPG: MMRM model includes baseline FPG, baseline HbA1c, treatment, region, visit and visit by treatment interaction. Body weight: MMRM model includes baseline body weight, baseline HbA1c, treatment, region, visit and visit by treatment interaction. cp-value=0.0049 dp-value=0.0052 ep-value=0.0463 |
||||||
| HbA1c (%) a | ||||||
| Baseline (mean) | 8.3 | 8.3 | 8.2 | 8.3 | 8.3 | 8.2 |
| Change from baseline (adjusted mean) | -0.6 | -0.7 | 0 | -0.4 | -0.6 | 0.1 |
| Difference from placebo (adjusted mean) (97.5% CI) | -0.6
b
(-0.8, -0.4) | -0.7
b
(-0.9, -0.5) | -- | -0.5
b
(-0.7, -0.3) | -0.7
b
(-0.9, -0.5) | -- |
| Patients (%) achieving HbA1c <7% | 18.0 | 19.5 | 5.5 | 12.0 | 17.5 | 6.7 |
| FPG (mg/dL) | ||||||
| Baseline (mean) | 138 | 146 | 142 | 138 | 146 | 142 |
| Change from baseline (adjusted mean, SE) | -17.9 (3.2) | -19.1 (3.3) | 10.4 (3.1) | -10.1 (3.2) | -15.2 (3.4) | 2.8 (3.2) |
| Difference from placebo (adjusted mean) (95% CI) | -28.2
b
(-37.0, -19.5) | -29.5
b
(-38.4, -20.6) | -- | -12.9
c
(-21.9, 3.9) | -17.9
b
(-27.0, -8.8) | -- |
| Body Weight | ||||||
| Baseline mean in kg | 92 | 95 | 90 | 92 | 95 | 90 |
| % change from baseline (adjusted mean) | -1.8 | -1.4 | -0.1 | -2.4 | -2.4 | 0.7 |
| Difference from placebo (adjusted mean) (95% CI) | -1.7
d
(-3.0, -0.5) | -1.3
e
(-2.5, -0.0) | -- | -3.0
b
(-4.4, -1.7) | -3.0
b
(-4.4, -1.6) | -- |
Add-on Combination with MDI Insulin with or without Metformin
A total of 563 patients with type 2 diabetes mellitus inadequately controlled on multiple daily injections (MDI) of insulin (total daily dose >60 IU), alone or in combination with metformin, participated in a double-blind, placebo-controlled trial to evaluate the efficacy of JARDIANCE as add-on therapy to MDI insulin over 18 weeks.
Patients entered a 2-week placebo run-in period on MDI insulin with or without metformin background therapy. Following the run-in period, patients with inadequate glycemic control were randomized to the addition of JARDIANCE 10 mg, JARDIANCE 25 mg, or placebo. Patients were maintained on a stable dose of insulin prior to enrollment, during the run-in period, and during the first 18 weeks of treatment. The mean total daily insulin dose at baseline for JARDIANCE 10 mg, JARDIANCE 25 mg, and placebo was 88.6 IU, 90.4 IU, and 89.9 IU, respectively.
JARDIANCE 10 mg or 25 mg daily used in combination with MDI insulin (with or without metformin) provided statistically significant reductions in HbA1c compared to placebo after 18 weeks of treatment (see Table 12).
| JARDIANCE 10 mg
N=186 | JARDIANCE 25 mg
N=189 | Placebo
N=188 |
|
|---|---|---|---|
| aModified intent-to-treat population. Last observation on trial (LOCF) was used to impute missing data at Week 18. At Week 18, 23.7%, 22.8% and 23.4% was imputed for patients randomized to JARDIANCE 10 mg, JARDIANCE 25 mg, and placebo, respectively.
bANCOVA p-value <0.0001 (HbA1c: ANCOVA model includes baseline HbA1c, treatment, renal function, geographical region, and background medication). |
|||
| HbA1c (%) a | |||
| Baseline (mean) | 8.4 | 8.3 | 8.3 |
| Change from baseline (adjusted mean) | -0.9 | -1.0 | -0.5 |
| Difference from placebo (adjusted mean) (95% CI) | -0.4 b(-0.6, -0.3) | -0.5 b(-0.7, -0.4) | -- |
During an extension period with treatment for up to 52 weeks, insulin could be adjusted to achieve defined glucose target levels. The change from baseline in HbA1c was maintained from 18 to 52 weeks with both JARDIANCE 10 mg and 25 mg. After 52 weeks, JARDIANCE 10 mg or 25 mg daily resulted in statistically greater percent body weight reduction compared to placebo (p-value <0.0001). The mean change in body weight from baseline was -1.95 kg for JARDIANCE 10 mg, and -2.04 kg for JARDIANCE 25 mg.
Renal Impairment
A total of 738 patients with type 2 diabetes mellitus and a baseline eGFR less than 90 mL/min/1.73 m 2participated in a randomized, double-blind, placebo-controlled, parallel-group trial to evaluate the efficacy of JARDIANCE in patients with type 2 diabetes mellitus and renal impairment. The trial population comprised of 290 patients with mild renal impairment (eGFR 60 to less than 90 mL/min/1.73 m 2), 374 patients with moderate renal impairment (eGFR 30 to less than 60 mL/min/1.73 m 2), and 74 with severe renal impairment (eGFR less than 30 mL/min/1.73 m 2). A total of 194 patients with moderate renal impairment had a baseline eGFR of 30 to less than 45 mL/min/1.73 m 2and 180 patients had a baseline eGFR of 45 to less than 60 mL/min/1.73 m 2.
At Week 24, JARDIANCE 25 mg provided statistically significant reduction in HbA1c relative to placebo in patients with mild to moderate renal impairment (see Table 13). A statistically significant reduction relative to placebo was also observed with JARDIANCE 25 mg in patients with either mild [-0.7 (95% CI: -0.9, -0.5)] or moderate [-0.4 (95% CI: -0.6, -0.3)] renal impairment and with JARDIANCE 10 mg in patients with mild [-0.5 (95% CI: -0.7, -0.3)] renal impairment.
The glucose lowering efficacy of JARDIANCE 25 mg decreased with decreasing level of renal function in the mild to moderate range. Least square mean HbA1c changes at 24 weeks were -0.6%, -0.5%, and -0.2% for those with a baseline eGFR of 60 to less than 90 mL/min/1.73 m 2, 45 to less than 60 mL/min/1.73 m 2, and 30 to less than 45 mL/min/1.73 m 2, respectively [see Dosage and Administration (2)and Use in Specific Populations (8.6)] . For placebo, least square mean HbA1c changes at 24 weeks were 0.1%, -0.1%, and 0.2% for patients with a baseline eGFR of 60 to less than 90 mL/min/1.73 m 2, 45 to less than 60 mL/min/1.73 m 2, and 30 to less than 45 mL/min/1.73 m 2, respectively.
| Mild and Moderate Impairment b | |
|---|---|
| JARDIANCE 25 mg | |
| ap-value <0.0001 (HbA1c: ANCOVA model includes baseline HbA1c, treatment, renal function, and background medication)
beGFR 30 to less than 90 mL/min/1.73 m 2- Modified intent-to-treat population. Last observation on trial (LOCF) was used to impute missing data at Week 24. At Week 24, 24.6% and 26.2% was imputed for patients randomized to JARDIANCE 25 mg and placebo, respectively. |
|
| HbA1c | |
| Number of patients | n=284 |
| Comparison vs placebo (adjusted mean) (95% CI) | -0.5 a(-0.6, -0.4) |
For patients with severe renal impairment, the analyses of changes in HbA1c and FPG showed no discernible treatment effect of JARDIANCE 25 mg compared to placebo [see Indications and Usage (1), Dosage and Administration (2.1, 2.2)and Use in Specific Populations (8.6)] .
14.2 Glycemic Control Trial in Pediatric Patients Aged 10 to 17 Years with Type 2 Diabetes Mellitus
DINAMO(NCT03429543) was a 26-week, double-blind, randomized, placebo-controlled, parallel group trial, with a double-blind active treatment safety extension period up to 52 weeks to assess the efficacy of JARDIANCE. The trial enrolled pediatric patients aged 10 to 17 years with inadequately controlled type 2 diabetes mellitus (HbA1c 6.5 to 10.5%). Patients treated with metformin (at least 1,000 mg daily or maximally tolerated dose), with or without insulin therapy, and those with a history of intolerance to metformin therapy were enrolled. Patients were randomized to 3 treatment arms (JARDIANCE 10 mg, a dipeptidyl peptidase-4 (DPP-4) inhibitor or placebo), over 26 weeks. Patients in the JARDIANCE 10 mg group who failed to achieve HbA1c <7.0% at Week 12 underwent a second randomization at Week 14 to remain on the 10 mg dose or increase to 25 mg. Patients on placebo were re-randomized at Week 26 to one of the JARDIANCE doses (10 mg or 25 mg) or a DPP-4 inhibitor.
A total of 157 patients were treated with either JARDIANCE (10 mg or 25 mg; N=52), a DPP-4 inhibitor (N=52), or placebo (N=53). Background therapies as adjunct to diet and exercise included metformin (51%), a combination of metformin and insulin (40.1%), insulin (3.2%), or none (5.7%). The mean HbA1c at baseline was 8.0% and the mean duration of type 2 diabetes mellitus was 2.1 years. The mean age was 14.5 years (range: 10-17 years) and 51.6% were aged 15 years and older. Approximately, 50% were White, 6% were Asian, 31% were Black or African American, and 38% were of Hispanic or Latino ethnicity. The mean BMI was 36.0 kg/m 2and mean BMI Z-score was 3.0. Patients with an eGFR less than 60 mL/min/1.73 m 2were not enrolled in the trial. Approximately 25% of the study population had microalbuminuria or macroalbuminuria.
At Week 26, treatment with JARDIANCE was superior in reducing HbA1c from baseline versus placebo (see Table 14).
| JARDIANCE
10 mg and 25 mg | Placebo | |
|---|---|---|
| aModified intent-to-treat set (All randomized and treated patients with baseline measurement).
bMultiple imputations using placebo wash-out approach with 500 iterations for missing data. Imputed for HbA1c (Jardiance N=5 (9.6 %), Placebo N=3 (5.7%)), for FPG (Jardiance N=4 (8.3%), Placebo N=2 (3.8%)). cLeast-Square Mean from Analysis of Covariance (ANCOVA) adjusted for baseline value and baseline age stratum (< 15 years vs 15 to < 18 years). dNot evaluated for statistical significance, not part of sequential testing procedure. ep-value=0.0116 (two-sided) |
||
| HbA1c (%) b | ||
| Number of patients | n=52 | n=53 |
| Baseline (mean) | 8.0 | 8.1 |
| Change from baseline c | -0.2 | 0.7 |
| Difference from placebo c(95% CI) | -0.8 e(-1.5, -0.2) | -- |
| FPG (mg/dL) b,d | ||
| Number of patients | n=48 | n=52 |
| Baseline (mean) | 154 | 159 |
| Change from baseline c | -19 | 17 |
| Difference from placebo c(95% CI) | -36 (-60.7, -10.7) | -- |
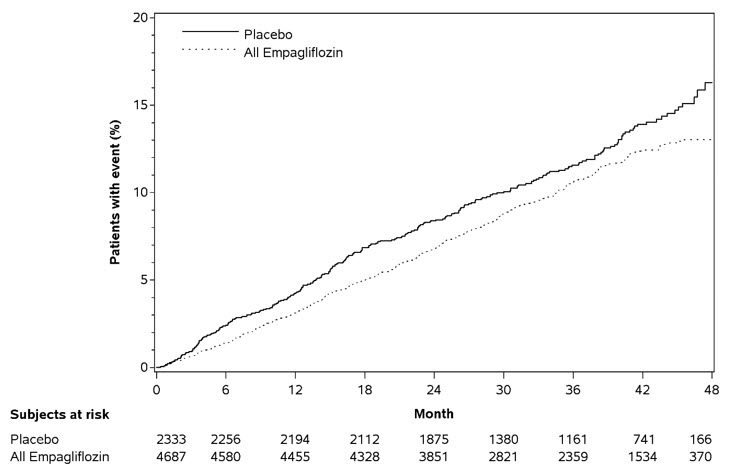
14.3 Cardiovascular Outcomes in Adults with Type 2 Diabetes Mellitus and Atherosclerotic Cardiovascular Disease
The effect of JARDIANCE on cardiovascular (CV) risk in adult patients with type 2 diabetes mellitus and established, stable, atherosclerotic CV disease was evaluated in the EMPA-REG OUTCOME trial, a multicenter, multinational, randomized, double-blind parallel group trial. The trial compared the risk of experiencing a major adverse cardiovascular event (MACE) between JARDIANCE and placebo when these were added to and used concomitantly with standard of care treatments for diabetes mellitus and atherosclerotic CV disease. Concomitant antidiabetic medications were to be kept stable for the first 12 weeks of the trial. Thereafter, antidiabetic and atherosclerotic therapies could be adjusted, at the discretion of investigators, to ensure participants were treated according to the standard care for these diseases.
A total of 7,020 patients were treated (JARDIANCE 10 mg = 2,345; JARDIANCE 25 mg = 2,342; placebo = 2,333) and followed for a median of 3.1 years. Approximately 72% of the trial population was White, 22% was Asian, and 5% was Black. The mean age was 63 years and approximately 72% were male.
All patients in the trial had inadequately controlled type 2 diabetes mellitus at baseline (HbA1c greater than or equal to 7%). The mean HbA1c at baseline was 8.1% and 57% of participants had diabetes mellitus for more than 10 years. Approximately 31%, 22% and 20% reported a past history of neuropathy, retinopathy and nephropathy to investigators, respectively and the mean eGFR was 74 mL/min/1.73 m 2. At baseline, patients were treated with one (~30%) or more (~70%) antidiabetic medications including metformin (74%), insulin (48%), and sulfonylurea (43%).
All patients had established atherosclerotic CV disease at baseline including one (82%) or more (18%) of the following: a documented history of coronary artery disease (76%), stroke (23%) or peripheral artery disease (21%). At baseline, the mean systolic blood pressure was 136 mmHg, the mean diastolic blood pressure was 76 mmHg, the mean LDL was 86 mg/dL, the mean HDL was 44 mg/dL, and the mean urinary albumin to creatinine ratio (UACR) was 175 mg/g. At baseline, approximately 81% of patients were treated with renin angiotensin system inhibitors, 65% with beta-blockers, 43% with diuretics, 77% with statins, and 86% with antiplatelet agents (mostly aspirin).
The primary endpoint in EMPA-REG OUTCOME was the time to first occurrence of a Major Adverse Cardiac Event (MACE). A major adverse cardiac event was defined as occurrence of either a CV death or a non-fatal myocardial infarction (MI) or a non-fatal stroke. The statistical analysis plan had pre-specified that the 10 and 25 mg doses would be combined. A Cox proportional hazards model was used to test for non-inferiority against the pre-specified risk margin of 1.3 for the hazard ratio of MACE and superiority on MACE if non-inferiority was demonstrated. Type-1 error was controlled across multiples tests using a hierarchical testing strategy.
JARDIANCE significantly reduced the risk of first occurrence of primary composite endpoint of CV death, non-fatal myocardial infarction, or non-fatal stroke (HR: 0.86; 95% CI: 0.74, 0.99). The treatment effect was due to a significant reduction in the risk of CV death in subjects randomized to empagliflozin (HR: 0.62; 95% CI: 0.49, 0.77), with no change in the risk of non-fatal myocardial infarction or non-fatal stroke (see Table 15and Figures 5and 6). Results for the 10 mg and 25 mg empagliflozin dosages were consistent with results for the combined dosage groups.
| Placebo
N=2,333 | JARDIANCE
N=4,687 | Hazard ratio vs placebo
(95% CI) |
|
|---|---|---|---|
| aTreated set (patients who had received at least one dose of trial drug)
bp-value for superiority (2-sided) 0.04 cTotal number of events |
|||
| Composite of CV death, non-fatal myocardial infarction, non-fatal stroke (time to first occurrence) b | 282 (12.1%) | 490 (10.5%) | 0.86 (0.74, 0.99) |
| Non-fatal myocardial infarction c | 121 (5.2%) | 213 (4.5%) | 0.87 (0.70, 1.09) |
| Non-fatal stroke c | 60 (2.6%) | 150 (3.2%) | 1.24 (0.92, 1.67) |
| CV death c | 137 (5.9%) | 172 (3.7%) | 0.62 (0.49, 0.77) |
 |
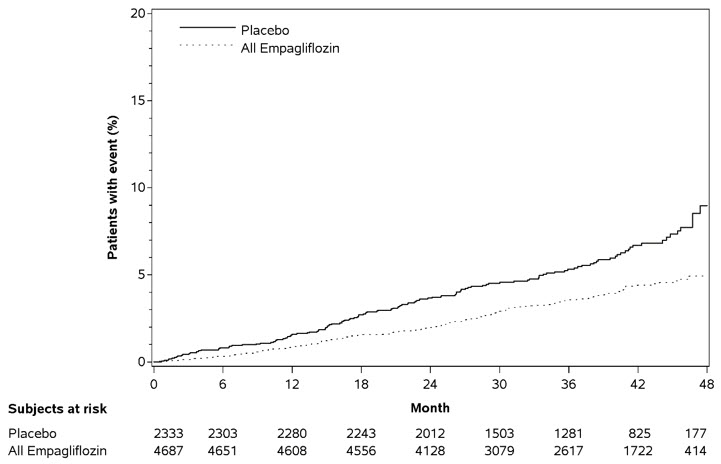 |
The efficacy of JARDIANCE on CV death was generally consistent across major demographic and disease subgroups.
Vital status was obtained for 99.2% of subjects in the trial. A total of 463 deaths were recorded during the EMPA-REG OUTCOME trial. Most of these deaths were categorized as CV deaths. The non-CV deaths were only a small proportion of deaths and were balanced between the treatment groups (2.1% in patients treated with JARDIANCE, and 2.4% of patients treated with placebo).
14.4 Heart Failure Trials in Adults
EMPEROR-Reduced(NCT03057977) was a double-blind trial conducted in adults with chronic heart failure (New York Heart Association [NYHA] functional class II-IV) with left ventricular ejection fraction (LVEF) ≤40% to evaluate the efficacy of JARDIANCE as adjunct to standard of care heart failure therapy.
Of 3,730 patients, 1,863 were randomized to JARDIANCE 10 mg and 1,867 to placebo and were followed for a median of 16 months. The mean age of the trial population was 67 years (range: 25 to 94 years) and 76% were men, 24% were women, and 27% were 75 years of age or older. Approximately 71% of the trial population were White, 18% Asian, and 7% Black or African American. At baseline, 50% of the patients had type 2 diabetes mellitus.
At randomization, 75% of patients were NYHA class II, 24% were class III, and 0.5% were class IV. The mean LVEF was 28%. At baseline, the mean eGFR was 62 mL/min/1.73 m 2and the median urinary albumin to creatinine ratio (UACR) was 22 mg/g. Approximately half of the patients (52%) had eGFR equal to or above 60 mL/min/1.73 m 2, 24% had eGFR 45 to less than 60 mL/min/1.73 m 2, 19% had eGFR 30 to less than 45 mL/min/1.73 m 2, and 5% had eGFR 20 to less than 30 mL/min/1.73 m 2.
At baseline, 88% of patients were treated with angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARB), or angiotensin receptor-neprilysin inhibitors (ARNI), 95% with beta-blockers, 71% with mineralocorticoid receptor antagonists (MRA), and 95% with diuretics.
The primary endpoint was the time to first event of either cardiovascular (CV) death or hospitalization for heart failure (HHF). First and recurrent HHF was assessed as a key secondary endpoint.
JARDIANCE was superior in reducing the risk of the primary composite endpoint of cardiovascular death or hospitalization for heart failure compared with placebo, mostly through a reduction in hospitalization for heart failure. JARDIANCE reduced the risk of first and recurrent HHF (see Table 16and Figures 7and 8).
| Placebo
N=1,867 | JARDIANCE 10 mg
N=1,863 | Hazard ratio vs placebo
(95% CI) | p-value | |
|---|---|---|---|---|
| Number of Patients (%) | ||||
| aTime to first event
bIncludes deaths following hospitalization cJoint frailty model accounting for CV death |
||||
| CV death or HHF a | 462 (24.7%) | 361 (19.4%) | 0.75 (0.65, 0.86) | <0.0001 |
| CV death a,b | 202 (10.8%) | 187 (10.0%) | 0.92 (0.75, 1.12) | |
| HHF a | 342 (18.3%) | 246 (13.2%) | 0.69 (0.59, 0.81) | |
| Number of Events | ||||
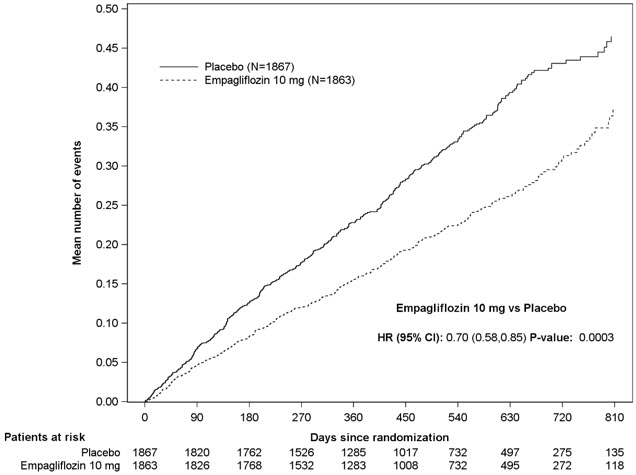
| First and recurrent HHF c | 553 | 388 | 0.70 (0.58, 0.85) | 0.0003 |
Figure 7 Time to First Occurrence of the Primary Composite Endpoint of CV Death or Hospitalization for Heart Failure
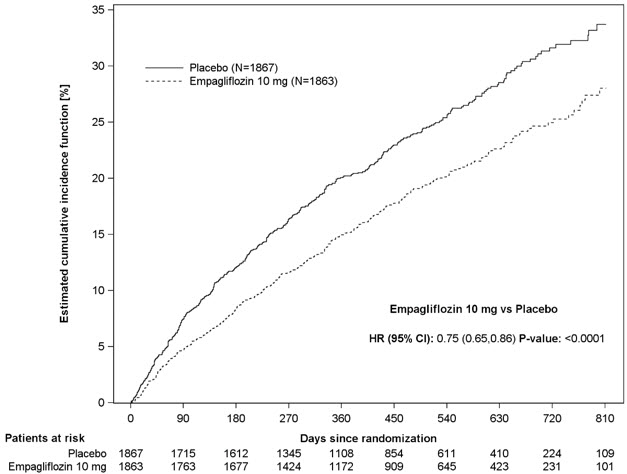
Figure 8 Time to Event of Hospitalization for Heart Failure (First and Recurrent)
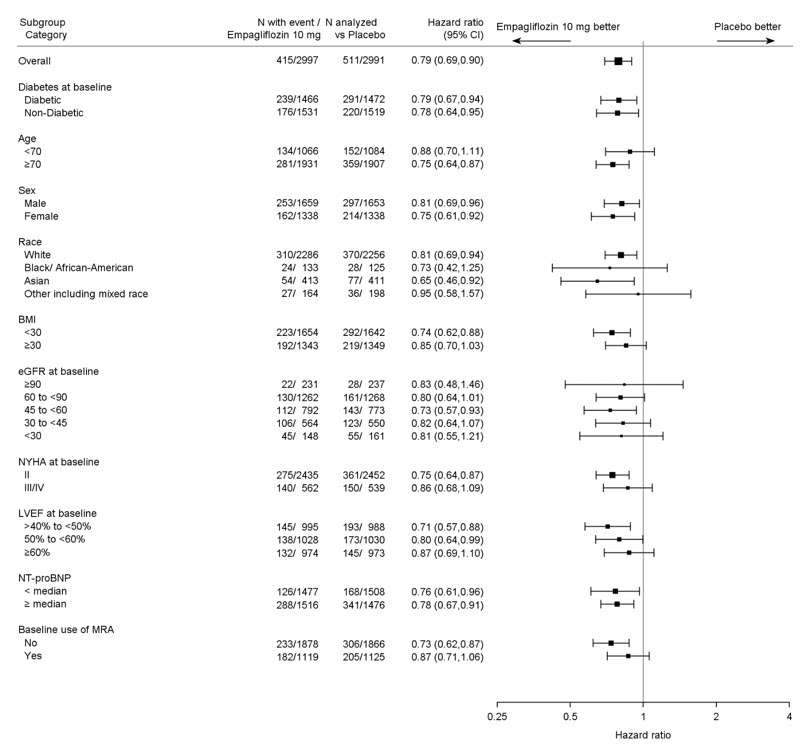
The results of the primary composite were generally consistent across the pre-specified subgroups (see Figure 9).
Figure 9 Treatment Effects for the Primary Composite Endpoint (CV Death and Hospitalization for Heart Failure) Subgroup Analysis (EMPEROR-Reduced)
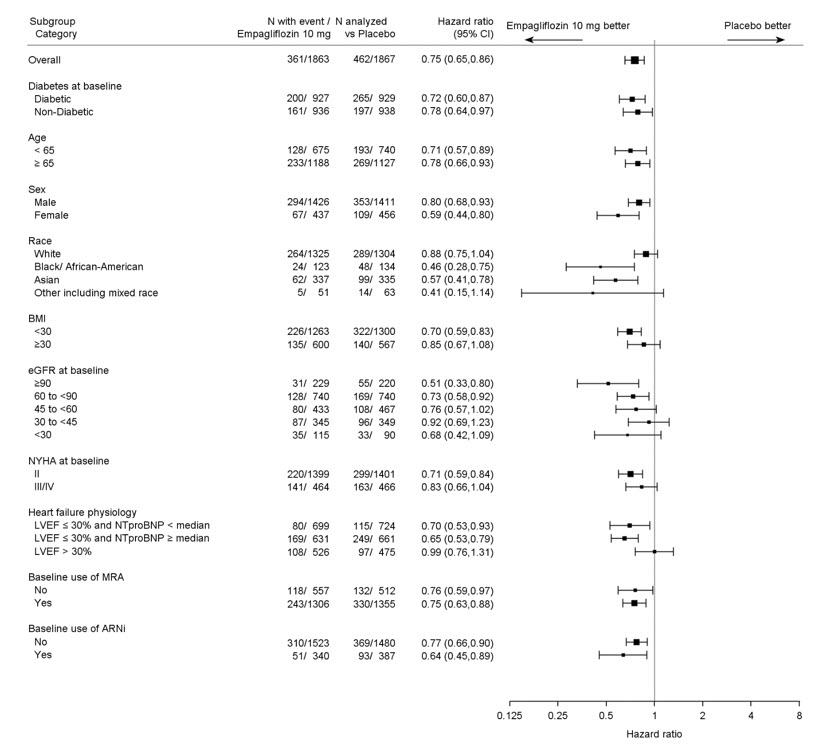
LVEF >30%: Includes both above and below the median NT-proBNP. To be eligible for inclusion, patients with an LVEF >30% were required to meet a higher NT-proBNP threshold than those with LVEF ≤30%, unless they additionally had a history of HHF within the past 12 months.
EMPEROR-Preserved(NCT03057951) was a double-blind trial conducted in adults with chronic heart failure NYHA Class II-IV with LVEF >40% to evaluate the efficacy of JARDIANCE as adjunct to standard of care therapy.
Of 5,988 patients, 2,997 were randomized to JARDIANCE 10 mg and 2,991 to placebo and were followed for a median of 26 months. The mean age of the trial population was 72 years (range: 22 to 100 years) and 55% were men, 45% were women, and 43% were 75 years of age or older. Approximately 76% of the trial population were White, 14% Asian, and 4% Black or African American.
At randomization, 82% of patients were NYHA class II, 18% were class III, and 0.3% were class IV. The EMPEROR-Preserved trial population included patients with a LVEF <50% (33.1%), with a LVEF 50 to <60% (34.4%) and a LVEF ≥60% (32.5%). At baseline, the mean eGFR was 61 mL/min/1.73 m 2and the median urinary albumin to creatinine ratio (UACR) was 21 mg/g. Approximately half of the patients (50%) had eGFR equal to or above 60 mL/min/1.73 m 2, 26% had eGFR 45 to less than 60 mL/min/1.73 m 2, 19% had eGFR 30 to less than 45 mL/min/1.73 m 2, and 5% had eGFR 20 to less than 30 mL/min/1.73 m 2.
At baseline, 81% of patients were treated with ACE inhibitors, ARBs, or ARNI, 86% with beta-blockers, 38% with MRAs, and 86% with diuretics.
The primary endpoint was the time to first event of either CV death or HHF. First and recurrent HHF was assessed as a key secondary endpoint.
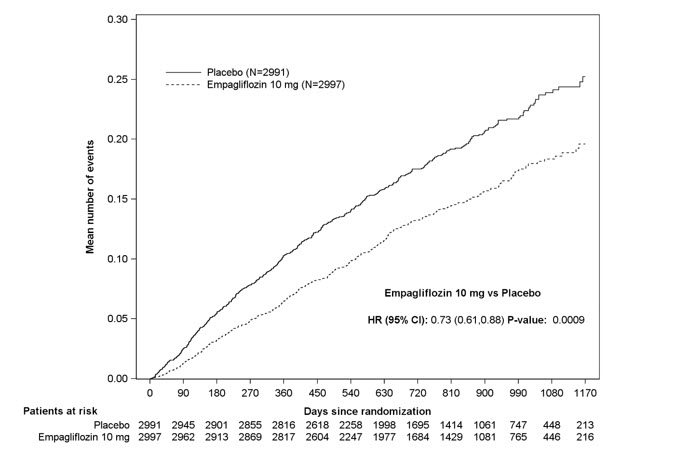
JARDIANCE was superior in reducing the risk of the primary composite endpoint compared with placebo, mostly through a reduction in hospitalization for heart failure. JARDIANCE reduced the risk of first and recurrent HHF (see Table 17and Figures 10and 11).
| Placebo
N=2,991 | JARDIANCE 10 mg
N=2,997 | Hazard ratio vs placebo
(95% CI) | p-value | |
|---|---|---|---|---|
| Number of Patients (%) | ||||
| aTime to first event
bIncludes deaths following hospitalization cJoint frailty model accounting for CV death |
||||
| CV death or HHF a | 511 (17.1%) | 415 (13.8%) | 0.79 (0.69, 0.90) | 0.0003 |
| CV death a,b | 244 (8.2%) | 219 (7.3%) | 0.91 (0.76, 1.09) | |
| HHF a | 352 (11.8%) | 259 (8.6%) | 0.71 (0.60, 0.83) | |
| Number of Events | ||||
| First and recurrent HHF c | 541 | 407 | 0.73 (0.61, 0.88) | 0.0009 |
Figure 10 Time to First Occurrence of the Primary Composite Endpoint of CV Death or Hospitalization for Heart Failure
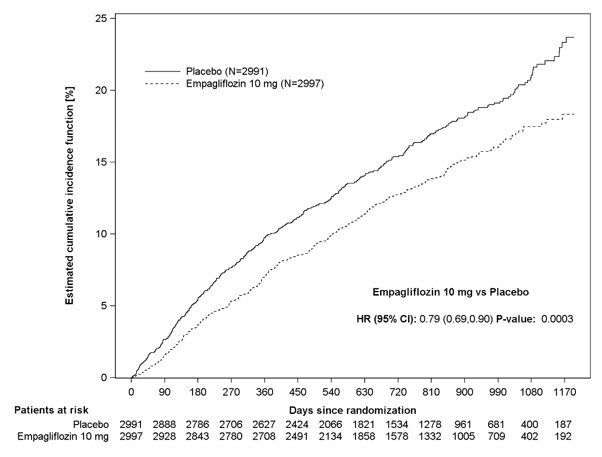
Figure 11 Time to Event of Hospitalization for Heart Failure (First and Recurrent)
The results of the primary composite endpoint were consistent across the pre-specified subgroups (see Figure 12).
Figure 12 Treatment Effects for the Primary Composite Endpoint (CV Death or Hospitalization for Heart Failure) Subgroup Analysis (EMPEROR-Preserved)
14.5 Chronic Kidney Disease Trial in Adults
EMPA-KIDNEY(NCT03594110) was a randomized, double-blind, placebo-controlled trial conducted in adults with chronic kidney disease (eGFR ≥20 to <45 mL/min/1.73 m 2; or eGFR ≥45 to <90 mL/min/1.73 m 2with urine albumin to creatinine ratio [UACR] ≥200 mg/g). The trial excluded patients with polycystic kidney disease or patients requiring intravenous immunosuppressive therapy in the preceding three months or >45 mg of prednisone (or equivalent) at the time of screening. The primary objective of the trial was to assess the effects of empagliflozin as an adjunct to standard of care therapy, including RAS-inhibitor therapy when appropriate, on time to kidney disease progression or cardiovascular death.
A total of 6,609 patients, were equally randomized to JARDIANCE 10 mg or placebo and were followed for a median of 24 months.
The mean age of the study population was 63 years (range: 18 to 94 years) and 67% were male. Approximately 58% of the study population were White, 36% Asian, and 4% Black or African American. Approximately 44% of the patients had type 2 diabetes mellitus.
At baseline, the mean eGFR was 37 mL/min/1.73 m 2, 21% of patients had an eGFR equal to or above 45 mL/min/1.73 m 2, 44% had an eGFR 30 to less than 45 mL/min/1.73 m 2, and 35% had an eGFR less than 30 mL/min/1.73 m 2. The median UACR was 329 mg/g, 20% of patients had a UACR <30 mg/g, 28% had a UACR 30 to ≤300mg/g, and 52% had a UACR >300 mg/g. Approximately 1% of patients had type 1 diabetes at baseline. The most common etiologies of CKD were diabetic nephropathy/diabetic kidney disease (31%), glomerular disease (25%), hypertensive/renovascular disease (22%) and other/unknown (22%).
At baseline, 85% of patients were treated with ACE inhibitor or ARB, 64% with statins, and 34% with antiplatelet agents.
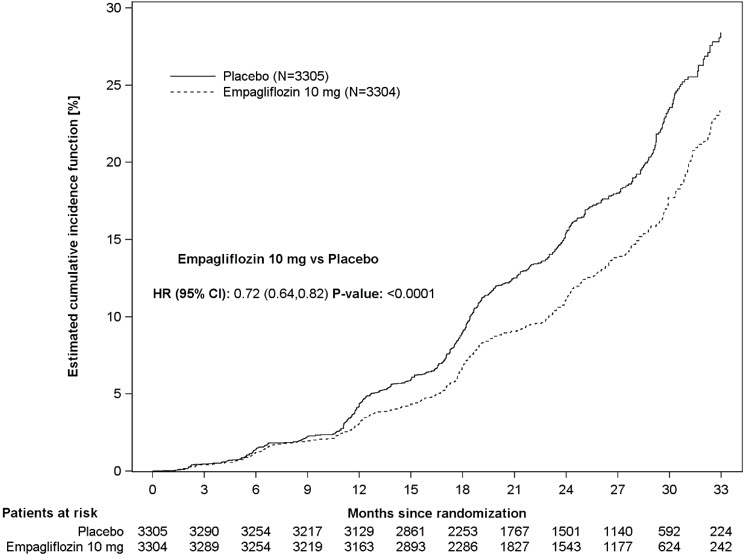
JARDIANCE was superior to placebo in reducing the risk of the primary composite endpoint of sustained ≥40% eGFR decline, sustained eGFR <10 mL/min/1.73 m 2, progression to end-stage kidney disease, or CV or renal death. The treatment effect reflected a reduction in a sustained ≥40% eGFR decline, sustained eGFR <10 mL/min/1.73 m 2, progression to end-stage kidney disease, and CV death. There were few renal deaths during the trial. JARDIANCE also reduced the risk of first and recurrent hospitalization (see Table 18and Figure 13); information collected on the reason for hospitalization was insufficient to further characterize the benefit.
| Placebo
N=3,305 | JARDIANCE 10 mg
N=3,304 | Hazard ratio vs placebo
(95% CI) | p-value | |
|---|---|---|---|---|
| CV=Cardiovascular, eGFR=Estimated glomerular filtration rate, ESKD=End-stage kidney disease | ||||
| aESKD is defined as the initiation of maintenance dialysis or receipt of a kidney transplant. | ||||
| bThere were too few events of renal death to compute a reliable hazard ratio. | ||||
| cInformation collected on the reason for hospitalization was insufficient to further characterize the benefit. | ||||
| Number of Patients (%) | ||||
| Composite of sustained ≥40% eGFR decline, sustained eGFR <10 mL/min/1.73 m 2, ESKD a, or CV or renal death (time to first occurrence) | 558 (16.9) | 432 (13.1) | 0.72 (0.64, 0.82) | <0.0001 |
| Sustained ≥40% eGFR decline | 474 (14.3) | 359 (10.9) | 0.70 (0.61, 0.81) | |
| ESKD aor sustained eGFR <10 mL/min/1.73 m 2 | 221 (6.7) | 157 (4.8) | 0.69 (0.56, 0.84) | |
| Renal death b | 4 (0.1) | 4 (0.1) | ||
| CV death | 69 (2.1) | 59 (1.8) | 0.84 (0.60, 1.19) | |
| Number of Events | ||||
| First and recurrent hospitalization c | 1,895 | 1,611 | 0.86 (0.78, 0.95) | 0.0025 |
Figure 13 Time to First Occurrence of the Primary Composite Endpoint, Sustained ≥40% eGFR Decline, Sustained eGFR <10 mL/min/1.73 m 2, ESKD or Renal Death, or CV Death
The results of the primary composite endpoint were generally consistent across the pre-specified subgroups examined, including eGFR categories, underlying cause of kidney disease, diabetes status, or background use of RAS inhibitors (see Figure 14). The treatment benefit with JARDIANCE on the primary composite endpoint was not evident in patients with very low levels of albuminuria, however there were few events in these patients.
Figure 14 Treatment Effects for the Primary Composite Endpoint (Sustained ≥40% eGFR Decline, Sustained eGFR <10 mL/min/1.73 m 2, ESKD or Renal Death, or CV Death) Subgroup Analysis (EMPA-KIDNEY)
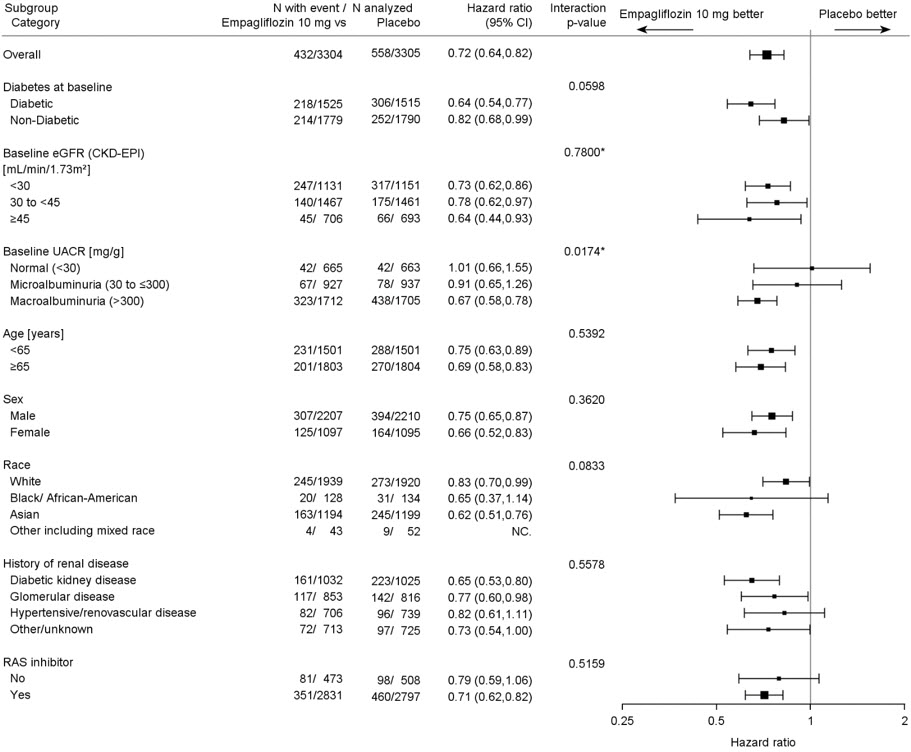
*=Trend test
16 HOW SUPPLIED/STORAGE AND HANDLING
JARDIANCE tablets are available as follows:
10 mg tablets:pale yellow, round, biconvex, and bevel-edged film-coated tablets debossed with "S 10" on one side and the Boehringer Ingelheim company symbol on the other side.
Bottles of 30 (NDC: 0597-0152-30)
Bottles of 90 (NDC: 0597-0152-90)
Cartons containing 3 blister cards of 10 tablets each (3 × 10) (NDC: 0597-0152-37), institutional pack.
25 mg tablets:pale yellow, oval, biconvex film-coated tablets, debossed with "S 25" on one side and the Boehringer Ingelheim company symbol on the other side.
Bottles of 30 (NDC: 0597-0153-30)
Bottles of 90 (NDC: 0597-0153-90)
Cartons containing 3 blister cards of 10 tablets each (3 × 10) (NDC: 0597-0153-37), institutional pack.
Dispense in a well-closed container as defined in the USP.
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Diabetic Ketoacidosis in Patients with Type 1 Diabetes Mellitus and Other Ketoacidosis
In patients with type 1 diabetes mellitus, inform them that using JARDIANCE can increase their risk of life-threatening diabetic ketoacidosis and that fatal ketoacidosis has occurred. For all other patients, inform them that JARDIANCE can cause potentially fatal ketoacidosis and that type 2 diabetes mellitus and pancreatic disorders (e.g., history of pancreatitis or pancreatic surgery) are risk factors.
Educate all patients on precipitating factors (such as insulin dose reduction or missed insulin doses, infection, reduced caloric intake, ketogenic diet, surgery, dehydration, and alcohol abuse) and symptoms of ketoacidosis (including nausea, vomiting, abdominal pain, tiredness, and labored breathing). Inform patients that blood glucose may be normal even in the presence of ketoacidosis.
Advise patients that they may be asked to monitor ketones. If symptoms of ketoacidosis occur, instruct patients to discontinue JARDIANCE and seek medical attention immediately [see Warnings and Precautions (5.1)] .
Volume Depletion
Inform patients that symptomatic hypotension may occur with JARDIANCE and advise them to contact their healthcare provider if they experience such symptoms [see Warnings and Precautions (5.2)] . Inform patients that dehydration may increase the risk for hypotension, and to maintain adequate fluid intake.
Serious Urinary Tract Infections
Inform patients of the potential for urinary tract infections, which may be serious. Provide them with information on the symptoms of urinary tract infections. Advise them to seek medical advice if such symptoms occur [see Warnings and Precautions (5.3)] .
Hypoglycemia
Inform patients that hypoglycemia has been reported when JARDIANCE is used with insulin secretagogues or insulin. Hypoglycemia may occur in pediatric patients regardless of concomitant antidiabetic treatment. Educate patients or caregivers on the signs and symptoms of hypoglycemia [see Warnings and Precautions (5.4)] .
Necrotizing Fasciitis of the Perineum (Fournier's Gangrene)
Inform patients that necrotizing infections of the perineum (Fournier's gangrene) have occurred with JARDIANCE. Counsel patients to promptly seek medical attention if they develop pain or tenderness, redness, or swelling of the genitals or the area from the genitals back to the rectum, along with a fever above 100.4°F or malaise [see Warnings and Precautions (5.5)] .
Genital Mycotic Infections in Females (e.g., Vulvovaginitis)
Inform female patients that vaginal yeast infections may occur and provide them with information on the signs and symptoms of vaginal yeast infections. Advise them of treatment options and when to seek medical advice [see Warnings and Precautions (5.6)] .
Genital Mycotic Infections in Males (e.g., Balanitis or Balanoposthitis)
Inform male patients that yeast infection of the penis (e.g., balanitis or balanoposthitis) may occur, especially in uncircumcised males and patients with chronic and recurrent infections. Provide them with information on the signs and symptoms of balanitis and balanoposthitis (rash or redness of the glans or foreskin of the penis). Advise them of treatment options and when to seek medical advice [see Warnings and Precautions (5.6)] .
Lower Limb Amputation
Counsel patients about the importance of routine preventative foot care. Instruct patients to monitor for new pain or tenderness, sores or ulcers, or infections involving the leg or foot and to seek medical advice immediately if such signs or symptoms develop [see Warnings and Precautions (5.7)] .
Hypersensitivity Reactions
Inform patients that serious hypersensitivity reactions, such as urticaria and angioedema, have been reported with JARDIANCE. Advise patients to report immediately any skin reaction or angioedema, and to discontinue drug until they have consulted prescribing healthcare provider [see Warnings and Precautions (5.8)] .
Laboratory Tests
Inform patients that elevated glucose in urinalysis is expected when taking JARDIANCE [see Drug Interactions (7)] .
Pregnancy
Advise pregnant patients, and patients of reproductive potential, of the potential risk to a fetus with treatment with JARDIANCE [see Use in Specific Populations (8.1)] . Instruct patients to report pregnancies to their healthcare provider as soon as possible.
Lactation
Advise patients that breastfeeding is not recommended during treatment with JARDIANCE [see Use in Specific Populations (8.2)].
Missed Dose
Instruct patients to take JARDIANCE only as prescribed. If a dose is missed, it should be taken as soon as the patient remembers. Advise patients not to double their next dose [see Dosage and Administration (2.3)] .
Distributed by:
Boehringer Ingelheim Pharmaceuticals, Inc.
Ridgefield, CT 06877 USA
Marketed by:
Boehringer Ingelheim Pharmaceuticals, Inc.
Ridgefield, CT 06877 USA
and
Eli Lilly and Company
Indianapolis, IN 46285 USA
Licensed from:
Boehringer Ingelheim International GmbH, Ingelheim, Germany
JARDIANCE is a registered trademark of and used under license from Boehringer Ingelheim International GmbH.
Boehringer Ingelheim Pharmaceuticals, Inc. either owns or uses the EMPA-REG OUTCOME ®, EMPEROR-Reduced ®, EMPEROR-Preserved ®, and EMPA-KIDNEY ®trademarks under license.
The other brands listed are trademarks of their respective owners and are not trademarks of Boehringer Ingelheim Pharmaceuticals, Inc.
Copyright © 2023 Boehringer Ingelheim International GmbH
ALL RIGHTS RESERVED
COL8914OI212023
SPL8934K
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: September 2023 | |||
| MEDICATION GUIDE
JARDIANCE ®(jar DEE ans) (empagliflozin tablets) for oral use |
||||
| What is the most important information I should know about JARDIANCE?
JARDIANCE can cause serious side effects, including:
|
||||
|
| |||
|
||||
|
| |||
| Talk to your healthcare provider about what to do if you get symptoms of a yeast infection of the vagina or penis. Your healthcare provider may suggest you use an over-the-counter antifungal medicine. Talk to your healthcare provider right away if you use an over-the-counter antifungal medication and your symptoms do not go away. | ||||
| What is JARDIANCE?
JARDIANCE is a prescription medicine used to:
JARDIANCE is not for use to lower blood sugar (glucose) in people with type 2 diabetes who have severe kidney problems, because it may not work. JARDIANCE is not for people with polycystic kidney disease, or who are taking or have recently received certain types of immunosuppressive therapy to treat kidney disease. JARDIANCE is not expected to work if you have these conditions. It is not known if JARDIANCE is safe and effective in children under 10 years of age. |
||||
| Who should not take JARDIANCE?
Do not take JARDIANCE if you:
|
||||
| What should I tell my healthcare provider before taking JARDIANCE?
Before taking JARDIANCE, tell your healthcare provider about all of your medical conditions, including if you:
JARDIANCE may affect the way other medicines work, and other medicines may affect how JARDIANCE works. Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine. |
||||
How should I take JARDIANCE?
|
||||
| What are the possible side effects of JARDIANCE?
JARDIANCE may cause serious side effects, including:
|
||||
|
|
|
|
|
|
||||
|
|
|
||
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||
How should I store JARDIANCE?
|
||||
| General information about the safe and effective use of JARDIANCE.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use JARDIANCE for a condition for which it is not prescribed. Do not give JARDIANCE to other people, even if they have the same symptoms you have. It may harm them. You can ask your pharmacist or healthcare provider for information about JARDIANCE that is written for health professionals. |
||||
| What are the ingredients in JARDIANCE?
Active Ingredient:empagliflozin Inactive Ingredients:colloidal silicon dioxide, croscarmellose sodium, hydroxypropyl cellulose, lactose monohydrate, magnesium stearate, and microcrystalline cellulose. In addition, the film coating contains the following inactive ingredients: hypromellose, polyethylene glycol, talc, titanium dioxide, and yellow ferric oxide. Distributed by: Boehringer Ingelheim Pharmaceuticals, Inc.; Ridgefield, CT 06877 USA Marketed by: Boehringer Ingelheim Pharmaceuticals, Inc.; Ridgefield, CT 06877 USA and Eli Lilly and Company, Indianapolis, IN 46285 USA Licensed from: Boehringer Ingelheim International GmbH, Ingelheim, Germany JARDIANCE is a registered trademark of and used under license from Boehringer Ingelheim International GmbH. Boehringer Ingelheim Pharmaceuticals, Inc. either owns or uses the EMPA-REG OUTCOME ®, EMPEROR-Reduced ®, EMPEROR-Preserved ®, and EMPA-KIDNEY ®trademarks under license. The other brands listed are trademarks of their respective owners and are not trademarks of Boehringer Ingelheim Pharmaceuticals, Inc. Copyright © 2023 Boehringer Ingelheim International GmbH ALL RIGHTS RESERVED COL8914OI212023 For more information about JARDIANCE, including current prescribing information and Medication Guide, go to www.jardiance.com, scan the code, or call Boehringer Ingelheim Pharmaceuticals, Inc. at 1-800-542-6257.
|
||||
PRINCIPAL DISPLAY PANEL - 10 mg Tablet Blister Card Carton
NDC: 0597-0152-37
DISPENSE WITH ENCLOSED MEDICATION GUIDE
Jardiance
®
(empagliflozin tablets)
10 mg
This unit dose package is not child-resistant. If dispensed
for outpatient use, a child-resistant container should be
utilized.
Rx only
30 tablets
3 blister cards. Each card contains 10 tablets.
Boehringer
Ingelheim
Lilly
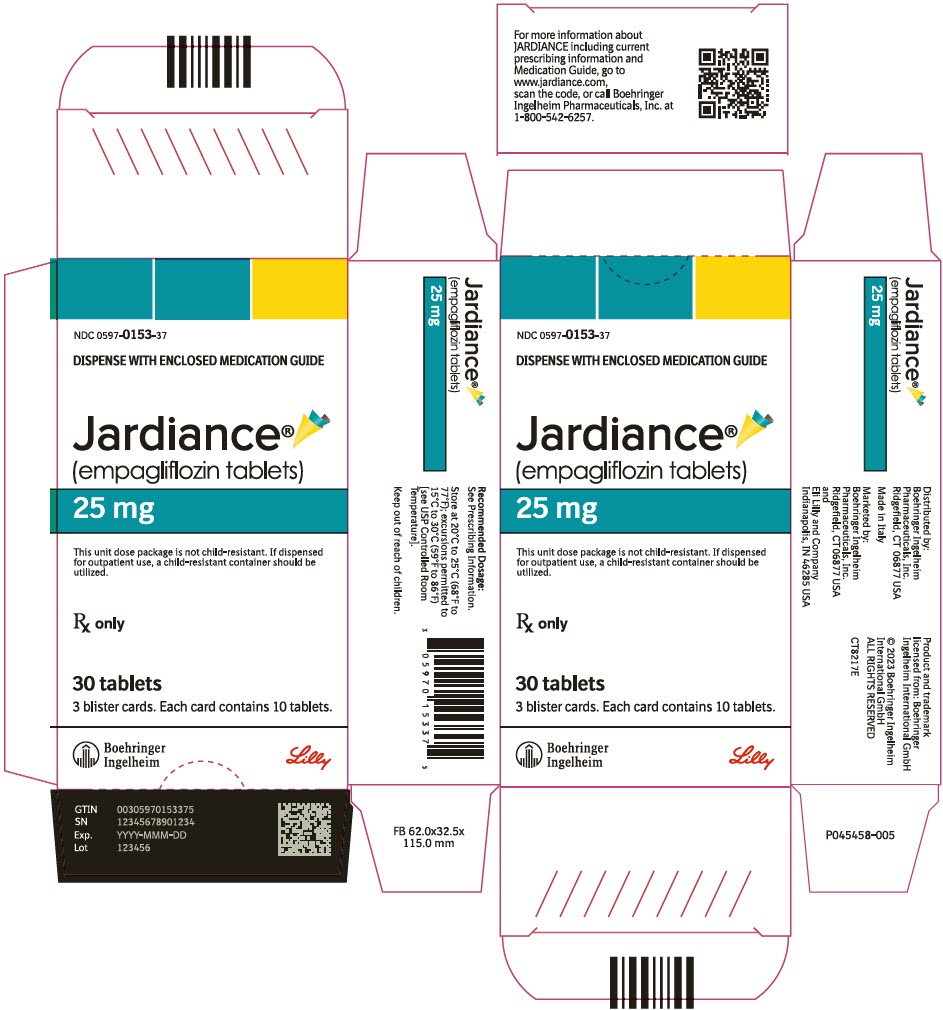
PRINCIPAL DISPLAY PANEL - 25 mg Tablet Blister Card Carton
NDC: 0597-0153-37
DISPENSE WITH ENCLOSED MEDICATION GUIDE
Jardiance
®
(empagliflozin tablets)
25 mg
This unit dose package is not child-resistant. If dispensed
for outpatient use, a child-resistant container should be
utilized.
Rx only
30 tablets
3 blister cards. Each card contains 10 tablets.
Boehringer
Ingelheim
Lilly
| JARDIANCE
empagliflozin tablet, film coated |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| JARDIANCE
empagliflozin tablet, film coated |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Praxis, LLC (016329513) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Praxis, LLC | 016329513 | pack(59368-379, 59368-380) , label(59368-379, 59368-380) , manufacture(59368-379, 59368-380) | |
Trademark Results [Jardiance]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 JARDIANCE 88902811 not registered Live/Pending |
Boehringer Ingelheim International GmbH 2020-05-06 |
 JARDIANCE 79060588 3595152 Live/Registered |
Boehringer Ingelheim International GmbH 2008-09-03 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
