MOXIFLOXACIN HYDROCHLORIDE- moxifloxacin hydrochloride tablet, film coated
Moxifloxacin Hydrochloride by
Drug Labeling and Warnings
Moxifloxacin Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by AvPAK. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
Moxifloxacin Hydrochloride Tablets
These highlights do not include all the information needed to use moxifloxacin hydrochloride tablets safely and effectively. See full prescribing information for moxifloxacin hydrochloride tablets.
MOXIFLOXACIN hydrochloride tablet, film-coated for oral use
Initial U.S. Approval: 1999WARNING: TENDON EFFECTS and MYASTHENIA GRAVIS
Fluoroquinolones, including moxifloxacin hydrochloride, are associated with an increased risk of tendinitis and tendon rupture in all ages. This risk is further increased in older patients usually over 60 years of age, in patients taking corticosteroid drugs, and in patients with kidney, heart or lung transplants [see Warnings and Precautions ( 5.1)].
Fluoroquinolones, including moxifloxacin hydrochloride, may exacerbate muscle weakness in persons with myasthenia gravis. Avoid moxifloxacin hydrochloride in patients with known history of myasthenia gravis [see Warnings and Precautions (5.2)].
To reduce the development of drug-resistant bacteria and maintain the effectiveness of moxifloxacin hydrochloride and other antibacterial drugs, moxifloxacin hydrochloride should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. (1)
RECENT MAJOR CHANGES
Warnings and Precautions ( 5.10) 11/14
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
Type of Infection Dose Every 24 hours Duration (days) Acute Bacterial Sinusitis (1.1)
400 mg
10
Acute Bacterial Exacerbation of Chronic Bronchitis (1.2)
400 mg
5
Community Acquired Pneumonia (1.3)
400 mg
7-14
Uncomplicated Skin and Skin Structure Infections (SSSI) (1.4)
400 mg
7
Complicated SSSI (1.5)
400 mg
7-21
Complicated Intra-Abdominal Infections (1.6)
400 mg
5-14
DOSAGE FORMS AND STRENGTHS
- Tablets: 400 mg (3.1)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Increased risk of tendinitis and tendon rupture. This risk is further increased in older patients usually over 60 years of age, in patients taking corticosteroids, and in patients with kidney, heart or lung transplants. Discontinue if pain or inflammation in a tendon occurs. (5.1, 8.5)
- Prolongation of the QT interval and isolated cases of torsade de pointes has been reported. Avoid use in patients with known prolongation, hypokalemia, and with drugs that prolong the QT interval. (5.3, 7.5, 8.5). Use caution in patients with proarrhythmic conditions such as clinically significant bradycardia or acute myocardial ischemia. (5.3)
- Serious and sometimes fatal hypersensitivity reactions, including anaphylactic reactions, may occur after first or subsequent doses. Discontinue drug use at first sign of skin rash, jaundice or any other sign of hypersensitivity. (5.4, 5.5)
- Central nervous system (CNS) events including dizziness, confusion, hallucination, depression, and rarely suicidal thoughts or acts may occur after first dose. Use caution in patients with known or suspected CNS disorders that may predispose to seizures or lower the seizure threshold. (5.6)
- Clostridium difficile-associated diarrhea: Evaluate if diarrhea occurs. (5.7)
- Peripheral neuropathy: Discontinue if symptoms occur. (5.8)
ADVERSE REACTIONS
Most common reactions (≥3%) were nausea, diarrhea, headache, and dizziness. (6.2)
To report SUSPECTED ADVERSE REACTIONS, contact AvKARE, Inc. at 1-855-361-3993 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatchDRUG INTERACTIONS
Interacting Drug
Interaction
Antacids, sucralfate, multivitamins, and other products containing multivalent cations
Moxifloxacin absorption is decreased. Administer moxifloxacin hydrochloride tablet at least 4 hours before or 8 hours after these products. ( 2.2, 7.1, 12.3, 17)
Warfarin
Anticoagulant effect of warfarin may be enhanced. Monitor prothrombin time/INR, watch for bleeding. ( 6.4, 7.2, 12.3)
Class IA and Class III antiarrhythmics:
Proarrhythmic effect may be enhanced. Avoid concomitant use. ( 5.3, 7.5)
Antidiabetic agents
Carefully monitor blood glucose ( 5.10, 7.3)
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 7/2016
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: TENDON EFFECTS and MYASTHENIA GRAVIS
1 INDICATIONS AND USAGE
1.1 Acute Bacterial Sinusitis
1.2 Acute Bacterial Exacerbation of Chronic Bronchitis
1.3 Community Acquired Pneumonia
1.4 Uncomplicated Skin and Skin Structure Infections
1.5 Complicated Skin and Skin Structure Infections
1.6 Complicated Intra-Abdominal Infections
2 DOSAGE AND ADMINISTRATION
2.1 Dosage in Adult Patients
2.2 Drug Interactions with Multivalent Cations
2.3 Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
3.1 Moxifloxacin Hydrochloride Tablets
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Tendinopathy and Tendon Rupture
5.2 Exacerbation of Myasthenia Gravis
5.3 QT Prolongation
5.4 Hypersensitivity Reactions
5.5 Other Serious and Sometimes Fatal Reactions
5.6 Central Nervous System Effects
5.7 Clostridium Difficile-Associated Diarrhea
5.8 Peripheral Neuropathy
5.9 Arthropathic Effects in Animals
5.10 Blood Glucose Disturbances
5.11 Photosensitivity/Phototoxicity
5.12 Development of Drug Resistant Bacteria
6 ADVERSE REACTIONS
6.1 Serious and Otherwise Important Adverse Reactions
6.2 Clinical Trial Experience
6.3 Laboratory Changes
6.4 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Antacids, Sucralfate, Multivitamins and Other Products Containing Multivalent Cations
7.2 Warfarin
7.3 Antidiabetic Agents
7.4 Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
7.5 Drugs that Prolong QT
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
11.1 Moxifloxacin Hydrochloride Tablets
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Acute Bacterial Exacerbation of Chronic Bronchitis
14.2 Community Acquired Pneumonia
14.3 Community Acquired Pneumonia caused by Multi-Drug Resistant Streptococcus pneumoniae (MDRSP)*
14.4 Acute Bacterial Sinusitis
14.5 Uncomplicated Skin and Skin Structure Infections
14.6 Complicated Skin and Skin Structure Infections
14.7 Complicated Intra-Abdominal Infections
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 Moxifloxacin Hydrochloride Tablets
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- MICROBIOLOGY
-
BOXED WARNING
(What is this?)
WARNING: TENDON EFFECTS and MYASTHENIA GRAVIS
Fluoroquinolones, including moxifloxacin hydrochloride, are associated with an increased risk of tendinitis and tendon rupture in all ages. This risk is further increased in older patients usually over 60 years of age, in patients taking corticosteroid drugs, and in patients with kidney, heart or lung transplants [see Warnings and Precautions (5.1)].
Fluoroquinolones, including moxifloxacin hydrochloride, may exacerbate muscle weakness in persons with myasthenia gravis. Avoid moxifloxacin hydrochloride in patients with known history of myasthenia gravis [see Warnings and Precautions (5.2)]. -
1 INDICATIONS AND USAGE
To reduce the development of drug-resistant bacteria and maintain the effectiveness of moxifloxacin hydrochloride tablets and other antibacterial drugs, moxifloxacin hydrochloride tablets should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Moxifloxacin hydrochloride tablets are indicated for the treatment of adults (≥ 18 years of age) with infections caused by susceptible isolates of the designated microorganisms in the conditions listed below [see Dosage and Administration (2) and Use in Specific Populations (8.5)] .
Culture and Susceptibility Testing
Appropriate culture and susceptibility tests should be performed before treatment in order to isolate and identify organisms causing infection and to determine their susceptibility to moxifloxacin [see Clinical Pharmacology (12.4)] . Therapy with moxifloxacin hydrochloride tablets may be initiated before results of these tests are known; once results become available, appropriate therapy should be continued.1.1 Acute Bacterial Sinusitis
Moxifloxacin hydrochloride tablets are indicated for the treatment of Acute Bacterial Sinusitis caused by Streptococcus pneumoniae, Haemophilus influenzae, or Moraxella catarrhalis [see Clinical Studies (14.4)] .
1.2 Acute Bacterial Exacerbation of Chronic Bronchitis
Moxifloxacin hydrochloride tablets are indicated for the treatment of Acute Bacterial Exacerbation of Chronic Bronchitis caused by Streptococcus pneumoniae, Haemophilus influenzae, Haemophilus parainfluenzae, Klebsiella pneumoniae, methicillin-susceptible Staphylococcus aureus, or Moraxella catarrhalis [see Clinical Studies (14.1)] .
1.3 Community Acquired Pneumonia
Moxifloxacin hydrochloride tablets are indicated for the treatment of Community Acquired Pneumonia caused by Streptococcus pneumoniae (including multi-drug resistant isolates*), Haemophilus influenzae, Moraxella catarrhalis, methicillin-susceptible Staphylococcus aureus, Klebsiella pneumoniae, Mycoplasma pneumoniae, or Chlamydophila pneumoniae.
* MDRSP, Multi-drug resistant Streptococcus pneumoniae includes isolates previously known as PRSP (Penicillin-resistant S. pneumoniae), and are isolates resistant to two or more of the following antibiotics: penicillin (minimum inhibitory concentrations [MIC] ≥ 2 mcg/mL), 2 nd generation cephalosporins (for example, cefuroxime), macrolides, tetracyclines, and trimethoprim/sulfamethoxazole [see Clinical Studies (14.2)] .1.4 Uncomplicated Skin and Skin Structure Infections
Moxifloxacin hydrochloride tablets are indicated for the treatment of Uncomplicated Skin and Skin Structure Infections caused by methicillin-susceptible Staphylococcus aureus or Streptococcus pyogenes [see Clinical Studies (14.5)] .
1.5 Complicated Skin and Skin Structure Infections
Moxifloxacin hydrochloride tablets are indicated for the treatment of Complicated Skin and Skin Structure Infections caused by methicillin-susceptible Staphylococcus aureus, Escherichia coli, Klebsiella pneumoniae, or Enterobacter cloacae [see Clinical Studies (14.6)] .
1.6 Complicated Intra-Abdominal Infections
Moxifloxacin hydrochloride tablets are indicated for the treatment of Complicated Intra-Abdominal Infections including polymicrobial infections such as abscess caused by Escherichia coli, Bacteroides fragilis, Streptococcus anginosus, Streptococcus constellatus, Enterococcus faecalis, Proteus mirabilis, Clostridium perfringens, Bacteroides thetaiotaomicron, or Peptostreptococcus species [see Clinical Studies (14.7)] .
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosage in Adult Patients
The dose of moxifloxacin is 400 mg (orally) once every 24 hours. The duration of therapy depends on the type of infection as described in Table 1.
Table 1: Dosage and Duration of Therapy in Adult Patients Type of Infection a Dose Every 24 hours Duration b (days) a) Due to the designated pathogens [see Indications and Usage (1), for IV use, see Use in Specific Populations (8.5)] .
b) Sequential therapy (intravenous to oral) may be instituted at the discretion of the physician.
Acute Bacterial Sinusitis (1.1)
400 mg
10
Acute Bacterial Exacerbation of Chronic Bronchitis (1.2)
400 mg
5
Community Acquired Pneumonia
400 mg
7-14
Uncomplicated Skin and Skin Structure Infections (SSSI ) (1.4)
400 mg
7
Complicated SSSI (1.5)
400 mg
7-21
Complicated Intra-Abdominal Infections (1.6)
400 mg
5-14
Intravenous formulation is indicated when it offers a route of administration advantageous to the patient (for example, patient cannot tolerate an oral dosage form). When switching from intravenous to oral formulation, no dosage adjustment is necessary. Patients whose therapy is started with moxifloxacin hydrochloride IV may be switched to moxifloxacin hydrochloride tablets when clinically indicated at the discretion of the physician.
2.2 Drug Interactions with Multivalent Cations
Oral doses of moxifloxacin should be administered at least 4 hours before or 8 hours after products containing magnesium, aluminum, iron or zinc, including antacids, sucralfate, multivitamins and VIDEX ® (didanosine) chewable/buffered tablets or the pediatric powder for oral solution [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)] .
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Tendinopathy and Tendon Rupture
Fluoroquinolones, including moxifloxacin hydrochloride, are associated with an increased risk of tendinitis and tendon rupture in all ages. This adverse reaction most frequently involves the Achilles tendon, and rupture of the Achilles tendon may require surgical repair. Tendinitis and tendon rupture in the rotator cuff (the shoulder), the hand, the biceps, the thumb, and other tendon sites have also been reported. The risk of developing fluoroquinolone-associated tendinitis and tendon rupture is further increased in older patients usually over 60 years of age, in patients taking corticosteroid drugs, and in patients with kidney, heart or lung transplants. Factors, in addition to age and corticosteroid use, that may independently increase the risk of tendon rupture include strenuous physical activity, renal failure, and previous tendon disorders such as rheumatoid arthritis. Tendinitis and tendon rupture have also occurred in patients taking fluoroquinolones who do not have the above risk factors. Tendon rupture can occur during or after completion of therapy; cases occurring up to several months after completion of therapy have been reported. Moxifloxacin hydrochloride should be discontinued if the patient experiences pain, swelling, inflammation or rupture of a tendon. Patients should be advised to rest at the first sign of tendinitis or tendon rupture, and to contact their healthcare provider regarding changing to a non-quinolone antimicrobial drug. [See Adverse Reactions (6.4) and Patient Counseling Information (17).]
5.2 Exacerbation of Myasthenia Gravis
Fluoroquinolones, including moxifloxacin hydrochloride, have neuromuscular blocking activity and may exacerbate muscle weakness in persons with myasthenia gravis. Postmarketing serious adverse events, including deaths and requirement for ventilatory support, have been associated with fluoroquinolone use in persons with myasthenia gravis. Avoid moxifloxacin hydrochloride in patients with known history of myasthenia gravis [see Patient Counseling Information (17)] .
5.3 QT Prolongation
Moxifloxacin hydrochloride has been shown to prolong the QT interval of the electrocardiogram in some patients. Following oral dosing with 400 mg of moxifloxacin the mean (± SD) change in QTc from the pre-dose value at the time of maximum drug concentration was 6 msec (± 26) (n = 787). Following a course of daily intravenous dosing (400 mg; 1 hour infusion each day) the mean change in QTc from the Day 1 pre-dose value was 10 msec (±22) on Day 1 (n=667) and 7 msec (± 24) on Day 3 (n = 667).
The drug should be avoided in patients with known prolongation of the QT interval, patients with uncorrected hypokalemia and patients receiving Class IA (for example, quinidine, procainamide) or Class III (for example, amiodarone, sotalol) antiarrhythmic agents, due to the lack of clinical experience with the drug in these patient populations.
Pharmacokinetic studies between moxifloxacin hydrochloride and other drugs that prolong the QT interval such as cisapride, erythromycin, antipsychotics, and tricyclic antidepressants have not been performed. An additive effect of moxifloxacin hydrochloride and these drugs cannot be excluded; therefore caution should be exercised when moxifloxacin hydrochloride is given concurrently with these drugs. In premarketing clinical trials, the rate of cardiovascular adverse events was similar in 798 moxifloxacin hydrochloride and 702 comparator treated patients who received concomitant therapy with drugs known to prolong the QTc interval.
Moxifloxacin hydrochloride should be used with caution in patients with ongoing proarrhythmic conditions, such as clinically significant bradycardia, acute myocardial ischemia. The magnitude of QT prolongation may increase with increasing concentrations of the drug or increasing rates of infusion of the intravenous formulation. Therefore the recommended dose or infusion rate should not be exceeded. QT prolongation may lead to an increased risk for ventricular arrhythmias including torsade de pointes. No excess in cardiovascular morbidity or mortality attributable to QTc prolongation occurred with moxifloxacin hydrochloride treatment in over 15,500 patients in controlled clinical studies, including 759 patients who were hypokalemic at the start of treatment, and there was no increase in mortality in over 18,000 moxifloxacin hydrochloride tablet treated patients in a postmarketing observational study in which ECGs were not performed. Elderly patients using IV moxifloxacin hydrochloride may be more susceptible to drug-associated QT prolongation [see Use In Specific Populations (8.5)]. In addition, moxifloxacin hydrochloride should be used with caution in patients with mild, moderate, or severe liver cirrhosis [see Clinical Pharmacology (12.3) and Patient Counseling Information (17)].5.4 Hypersensitivity Reactions
Serious anaphylactic reactions, some following the first dose, have been reported in patients receiving quinolone therapy, including moxifloxacin hydrochloride. Some reactions were accompanied by cardiovascular collapse, loss of consciousness, tingling, pharyngeal or facial edema, dyspnea, urticaria, and itching. Serious anaphylactic reactions require immediate emergency treatment with epinephrine. Moxifloxacin hydrochloride should be discontinued at the first appearance of a skin rash or any other sign of hypersensitivity. Oxygen, intravenous steroids, and airway management, including intubation, may be administered as indicated. [See Adverse Reactions (6) and Patient Counseling Information (17).]
5.5 Other Serious and Sometimes Fatal Reactions
Other serious and sometimes fatal events, some due to hypersensitivity, and some due to uncertain etiology, have been reported rarely in patients receiving therapy with quinolones, including moxifloxacin hydrochloride. These events may be severe and generally occur following the administration of multiple doses. Clinical manifestations may include one or more of the following:
- Fever, rash, or severe dermatologic reactions (for example, toxic epidermal necrolysis, Stevens-Johnson syndrome)
- Vasculitis; arthralgia; myalgia; serum sickness
- Allergic pneumonitis
- Interstitial nephritis; acute renal insufficiency or failure
- Hepatitis; jaundice; acute hepatic necrosis or failure
- Anemia, including hemolytic and aplastic; thrombocytopenia, including thrombotic thrombocytopenic purpura; leukopenia; agranulocytosis; pancytopenia; and/or other hematologic abnormalities
The drug should be discontinued immediately at the first appearance of a skin rash, jaundice, or any other sign of hypersensitivity and supportive measures instituted [see Patient Counseling Information (17) and Adverse Reactions (6.4)] .
5.6 Central Nervous System Effects
Fluoroquinolones, including moxifloxacin hydrochloride, may cause central nervous system (CNS) events, including: nervousness, agitation, insomnia, anxiety, nightmares or paranoia. [See Adverse Reactions (6.2, 6.4).]
Convulsions and increased intracranial pressure (including pseudotumor cerebri) have been reported in patients receiving fluoroquinolones. Fluoroquinolones may also cause central nervous system (CNS) events including: dizziness, confusion, tremors, hallucinations, depression, and, rarely, suicidal thoughts or acts. These reactions may occur following the first dose. If these reactions occur in patients receiving moxifloxacin hydrochloride, the drug should be discontinued and appropriate measures instituted. As with all fluoroquinolones, moxifloxacin hydrochloride should be used with caution in patients with known or suspected CNS disorders (for example, severe cerebral arteriosclerosis, epilepsy) or in the presence of other risk factors that may predispose to seizures or lower the seizure threshold. [See Drug Interactions (7.4) Adverse Reactions (6.2, 6.4) and Patient Counseling Information (17).]
5.7 Clostridium Difficile-Associated Diarrhea
Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including moxifloxacin hydrochloride, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated [see Adverse Reactions (6.2) and Patient Counseling Information (17)] .5.8 Peripheral Neuropathy
Cases of sensory or sensorimotor axonal polyneuropathy affecting small and/or large axons resulting in paresthesias, hypoesthesias, dysesthesias and weakness have been reported in patients receiving fluoroquinolones including moxifloxacin hydrochloride. Symptoms may occur soon after initiation of moxifloxacin hydrochloride and may be irreversible. Moxifloxacin hydrochloride should be discontinued immediately if the patient experiences symptoms of peripheral neuropathy including pain, burning, tingling, numbness, and/or weakness or other alterations of sensation including light touch, pain, temperature, position sense, and vibratory sensation [see Adverse Reactions (6.2, 6.4) and Patient Counseling Information (17)].
5.9 Arthropathic Effects in Animals
The oral administration of moxifloxacin hydrochloride caused lameness in immature dogs. Histopathological examination of the weight-bearing joints of these dogs revealed permanent lesions of the cartilage. Related quinolone-class drugs also produce erosions of cartilage of weight-bearing joints and other signs of arthropathy in immature animals of various species. [see Animal Toxicology and/or Pharmacology (13.2).]
5.10 Blood Glucose Disturbances
As with all fluoroquinolones, disturbances in blood glucose, including hypoglycemia and hyperglycemia have been reported with moxifloxacin hydrochloride. In moxifloxacin hydrochloride-treated patients, dysglycemia occurred predominantly in elderly diabetic patients receiving concomitant treatment with an oral hypoglycemic agent (for example, sulfonylurea) or with insulin. In diabetic patients, careful monitoring of blood glucose is recommended If a hypoglycemic reaction occurs, moxifloxacin hydrochloride should be discontinued and appropriate therapy should be initiated immediately As with all fluoroquinolones, disturbances in blood glucose, including both hypoglycemia and hyperglycemia have been reported with moxifloxacin hydrochloride. In moxifloxacin hydrochloride-treated patients, dysglycemia occurred predominantly in elderly diabetic patients receiving concomitant treatment with an oral hypoglycemic agent (for example, sulfonylurea) or with insulin. In diabetic patients, careful monitoring of blood glucose is recommended [see Adverse Reactions (6.2)]. If a hypoglycemic reaction occurs, moxifloxacin hydrochloride should be discontinued and appropriate therapy should be initiated immediately . [See Adverse Reactions (6.2), and Patient Counseling Information (17).]
5.11 Photosensitivity/Phototoxicity
Moderate to severe photosensitivity/phototoxicity reactions, the latter of which may manifest as exaggerated sunburn reactions (for example, burning, erythema, exudation, vesicles, blistering, edema) involving areas exposed to light (typically the face, “V” area of the neck, extensor surfaces of the forearms, dorsa of the hands), can be associated with the use of quinolone antibiotics after sun or UV light exposure. Therefore, excessive exposure to these sources of light should be avoided. Drug therapy should be discontinued if phototoxicity occurs. [See Adverse Reactions ( 6.4) and Pharmacokinetics (12.3).]
5.12 Development of Drug Resistant Bacteria
Prescribing moxifloxacin hydrochloride in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria [see Patient Counseling Information (17)] .
-
6 ADVERSE REACTIONS
6.1 Serious and Otherwise Important Adverse Reactions
The following serious and otherwise important adverse reactions are discussed in greater detail in the warnings and precautions section of the label:
- Tendinopathy and Tendon Rupture [see Warnings and Precautions (5.1)]
- QT Prolongation [see Warnings and Precautions (5.3)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.4)]
- Other Serious and Sometimes Fatal Reactions [see Warnings and Precautions (5.5)]
- Central Nervous System Effects [see Warnings and Precautions (5.6)]
- Clostridium difficile-Associated Diarrhea [see Warnings and Precautions (5.7)]
- Peripheral Neuropathy that may be irreversible [see Warnings and Precautions (5.8)]
- Blood Glucose Disturbances [see Warnings and Precautions (5.10)]
- Photosensitivity/Phototoxicity [see Warnings and Precautions (5.11)]
- Development of Drug Resistant Bacteria [see Warnings and Precautions (5.12)]
6.2 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data described below reflect exposure to moxifloxacin hydrochloride in 14981 patients in 71 active controlled Phase II to IV clinical trials in different indications [see Indications and Usage (1)] . The population studied had a mean age of 50 years (approximately 73% of the population was <65 years of age), 50% were male, 63% were Caucasian, 12% were Asian and 9% were Black. Patients received moxifloxacin 400 mg once daily PO, IV, or sequentially (IV followed by PO). Treatment duration was usually 6 to 10 days, and the mean number of days on therapy was 9 days.
Discontinuation of moxifloxacin due to adverse events occurred in 5% of patients overall, 4.1% of patients treated with 400 mg PO, 3.9% with 400 mg IV and 8.2% with sequential therapy 400 mg PO/IV. The most common adverse events leading to discontinuation with the 400 mg PO doses were nausea (0.8%), diarrhea (0.5%), dizziness (0.5%), and vomiting (0.4%). The most common adverse event leading to discontinuation with the 400 mg IV dose was rash (0.5%). The most common adverse events leading to discontinuation with the 400 mg IV/PO sequential dose were diarrhea (0.5%), pyrexia (0.4%).
Adverse reactions occurring in ≥1% of moxifloxacin hydrochloride-treated patients and less common adverse reactions, occurring in 0.1 to <1% of moxifloxacin hydrochloride-treated patients, are shown in Table 2 and Table 3, respectively. The most common adverse drug reactions (≥3%) are nausea, diarrhea, headache, and dizziness.
Table 2: Common (≥ 1%) Adverse Reactions Reported in Active-Controlled Clinical Trials with Moxifloxacin Hydrochloride System Organ Class Adverse Reactions a %
(N=14,981)a) MedDRA Version 12.0
Blood and Lymphatic System Disorders
Anemia
1.1
Gastrointestinal Disorders
Nausea
6.9
Diarrhea
6
Vomiting
2.4
Constipation
1.9
Abdominal pain
1.5
Abdominal pain upper
1.1
Dyspepsia
1
General Disorders and Administration Site Conditions
Pyrexia
1.1
Investigations
Alanine aminotransferase increased
1.1
Metabolism and Nutritional Disorders
Hypokalemia
1
Nervous System Disorders
Headache
4.2
Dizziness
3
Psychiatric Disorders
Insomnia
1.9
Table 3: Less Common (0.1 to <1%) Adverse Reactions Reported in Active-Controlled Clinical Trials with Moxifloxacin Hydrochloride (N=14,981) System Organ Class Adverse Reactions a a) MedDRA Version 12.0
Blood and Lymphatic System Disorders
Thrombocythemia
Eosinophilia
Neutropenia
Thrombocytopenia
Leukopenia
Leukocytosis
Cardiac Disorders
Atrial fibrillation
Palpitations
Tachycardia
Cardiac failure congestive
Angina pectoris
Cardiac failure
Cardiac arrest
Bradycardia
Ear and Labyrinth Disorders
Vertigo
Tinnitus
Eye Disorders
Vision blurred
Gastrointestinal Disorders
Dry mouth
Abdominal discomfort
Flatulence
Abdominal distention
Gastritis
Gastroesophageal reflux disease
General Disorders and Administration Site Conditions
Fatigue
Chest pain
Asthenia
Edema peripheral
Pain
Malaise
Infusion site extravasation
Edema
Chills
Chest discomfort
Facial pain
Hepatobiliary Disorders
Hepatic function abnormal
Infections and Infestations
Vulvovaginal candidiasis
Oral candidiasis
Vulvovaginal mycotic infection
Candidiasis
Vaginal infection
Oral fungal infection
Fungal infection
Gastroenteritis
Investigations
Aspartate aminotransferase increased
Gamma-glutamyltransferase increased
Blood alkaline phosphatase increased
Hepatic enzyme increased
Electrocardiogram QT prolonged
Blood lactate dehydrogenase increased
Platelet count increased
Blood amylase increased
Blood glucose increased
Lipase increased
Hemoglobin decreased
Blood creatinine increased
Transaminases increased
White blood cell count increased
Blood urea increased
Liver function test abnormal
Hematocrit decreased
Prothrombin time prolonged
Eosinophil count increased
Activated partial thromboplastin time prolonged
Blood bilirubin increased
Blood triglycerides increased
Blood uric acid increased
Blood pressure increased
Metabolism and Nutrition Disorders
Hyperglycemia
Anorexia
Hypoglycemia
Hyperlipidemia
Decreased appetite
Dehydration
Musculoskeletal and Connective Tissue Disorders
Back pain
Pain in extremity
Arthralgia
Myalgia
Muscle spasms
Musculoskeletal chest pain
Musculoskeletal pain
Nervous System Disorders
Dysgeusia
Somnolence
Tremor
Lethargy
Paresthesia
Tension headache
Hypoesthesia
Syncope
Psychiatric Disorders
Anxiety
Confusional state
Agitation
Depression
Nervousness
Restlessness
Hallucination
Disorientation
Renal and Urinary Disorders
Renal failure
Dysuria
Renal failure acute
Reproductive System and Breast Disorders
Vulvovaginal pruritus
Respiratory, Thoracic, and Mediastinal Disorders
Dyspnea
Asthma
Wheezing
Bronchospasm
Skin and Subcutaneous Tissue Disorders
Rash
Pruritus
Hyperhidrosis
Erythema
Urticaria
Dermatitis allergic
Night sweats
Vascular Disorders
Hypertension
Hypotension
Phlebitis
6.3 Laboratory Changes
Changes in laboratory parameters, without regard to drug relationship, which are not listed above and which occurred in ≥ 2% of patients and at an incidence greater than in controls included: increases in MCH, neutrophils, WBCs, PT ratio, ionized calcium, chloride, albumin, globulin, bilirubin; decreases in hemoglobin, RBCs, neutrophils, eosinophils, basophils, PT ratio, glucose, pO 2, bilirubin, and amylase. It cannot be determined if any of the above laboratory abnormalities were caused by the drug or the underlying condition being treated.
6.4 Postmarketing Experience
Table 4 lists adverse reactions that have been identified during post-approval use of moxifloxacin hydrochloride. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Table 4: Postmarketing Reports of Adverse Drug Reactions System/Organ Class Adverse Reaction Blood and Lymphatic System Disorders
Agranulocytosis
Pancytopenia
[see Warnings and Precautions (5.5)]
Cardiac Disorders
Ventricular tachyarrhythmias (including in very rare cases cardiac arrest and torsade de pointes, and usually in patients with concurrent severe underlying proarrhythmic conditions)
Ear and Labyrinth Disorders
Hearing impairment, including deafness (reversible in majority of cases)
Eye Disorders
Vision loss (especially in the course of CNS reactions, transient in majority of cases)
Hepatobiliary Disorders
Hepatitis (predominantly cholestatic)
Hepatic failure (including fatal cases)
Jaundice
Acute hepatic necrosis
[see Warnings and Precautions (5.5)]
Immune System Disorders
Anaphylactic reaction
Anaphylactic shock
Angioedema (including laryngeal edema)
[see Warnings and Precautions (5.4, 5.5)]
Musculoskeletal and Connective Tissue Disorders
Tendon rupture
[see Warnings and Precautions (5.1)]
Nervous System Disorders
Altered coordination
Abnormal gait
[see Warnings and Precautions (5.8)]
Myasthenia gravis (exacerbation of)
[see Warnings and Precautions (5.2)]
Muscle weakness
Peripheral neuropathy (that may be irreversible), polyneuropathy [see Warnings and Precautions (5.8)]
Psychiatric Disorders
Psychotic reaction (very rarely culminating in self-injurious behavior, such as suicidal ideation/thoughts or suicide attempts [see Warnings and Precautions (5.6)]
Renal and Urinary Disorders
Renal dysfunction
Interstitial nephritis
[see Warnings and Precautions (5.5)]
Respiratory, Thoracic and Mediastinal Disorders
Allergic pneumonitis
[see Warnings and Precautions (5.5)]
Skin and Subcutaneous Tissue Disorders
Photosensitivity/phototoxicity reaction
[see Warnings and Precautions (5.11)]
Stevens-Johnson syndrome
Toxic epidermal necrolysis
[see Warnings and Precautions (5.5)]
To report SUSPECTED ADVERSE REACTIONS contact AvKARE, Inc. at 1-855-361-3993; email drugsafety@avkare.com; or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
-
7 DRUG INTERACTIONS
7.1 Antacids, Sucralfate, Multivitamins and Other Products Containing Multivalent Cations
Quinolones form chelates with alkaline earth and transition metal cations. Oral administration of quinolones with antacids containing aluminum or magnesium, with sucralfate, with metal cations such as iron, or with multivitamins containing iron or zinc, or with formulations containing divalent and trivalent cations such as VIDEX ® (didanosine) chewable/buffered tablets or the pediatric powder for oral solution, may substantially interfere with the absorption of quinolones, resulting in systemic concentrations considerably lower than desired. Therefore, moxifloxacin hydrochloride should be taken at least 4 hours before or 8 hours after these agents. [See Dosage and Administration (2.2), Pharmacokinetics (12.3), and Patient Counseling Information (17).]
7.2 Warfarin
Quinolones, including moxifloxacin hydrochloride, have been reported to enhance the anticoagulant effects of warfarin or its derivatives in the patient population. In addition, infectious disease and its accompanying inflammatory process, age, and general status of the patient are risk factors for increased anticoagulant activity. Therefore the prothrombin time, International Normalized Ratio (INR), or other suitable anticoagulation tests should be closely monitored if a quinolone is administered concomitantly with warfarin or its derivatives. [See Adverse Reactions (6.2, 6.3), Pharmacokinetics (12.3), and Patient Counseling Information (17).]
7.3 Antidiabetic Agents
Disturbances of blood glucose, including hyperglycemia and hypoglycemia, have been reported in patients treated concomitantly with fluoroquinolones and an antidiabetic agent. Therefore, careful monitoring of blood glucose is recommended when these agents are co-administered. If a hypoglycemic reaction occurs, moxifloxacin hydrochloride should be discontinued and appropriate therapy should be initiated immediately. [See Warnings and Precautions (5.10), Adverse Reactions (6.2), and Patient Counseling Information (17).]
7.4 Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Although not observed with moxifloxacin hydrochloride in preclinical and clinical trials, the concomitant administration of a nonsteroidal anti-inflammatory drug with a quinolone may increase the risks of CNS stimulation and convulsions [see Warnings and Precautions ( 5.6), and Patient Counseling Information (17)] .
7.5 Drugs that Prolong QT
There is limited information available on the potential for a pharmacodynamic interaction in humans between moxifloxacin hydrochloride and other drugs that prolong the QTc interval of the electrocardiogram. Sotalol, a Class III antiarrhythmic, has been shown to further increase the QTc interval when combined with high doses of intravenous (IV) moxifloxacin in dogs. Therefore, moxifloxacin hydrochloride should be avoided with Class IA and Class III antiarrhythmics. [See Warnings and Precautions (5.3), Nonclinical Toxicology (13.2), and Patient Counseling Information (17).]
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category C. Because no adequate or well-controlled studies have been conducted in pregnant women, moxifloxacin hydrochloride should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Moxifloxacin was not teratogenic when administered to pregnant rats during organogenesis at oral doses as high as 500 mg/kg/day or 0.24 times the maximum recommended human dose based on systemic exposure (AUC), but decreased fetal body weights and slightly delayed fetal skeletal development (indicative of fetotoxicity) were observed. Intravenous administration of 80 mg/kg/day (approximately 2 times the maximum recommended human dose based on body surface area (mg/m 2) to pregnant rats resulted in maternal toxicity and a marginal effect on fetal and placental weights and the appearance of the placenta. There was no evidence of teratogenicity at intravenous doses as high as 80 mg/kg/day. Intravenous administration of 20 mg/kg/day (approximately equal to the maximum recommended human oral dose based upon systemic exposure) to pregnant rabbits during organogenesis resulted in decreased fetal body weights and delayed fetal skeletal ossification. When rib and vertebral malformations were combined, there was an increased fetal and litter incidence of these effects. Signs of maternal toxicity in rabbits at this dose included mortality, abortions, marked reduction of food consumption, decreased water intake, body weight loss and hypoactivity. There was no evidence of teratogenicity when pregnant cynomolgus monkeys were given oral doses as high as 100 mg/kg/day (2.5 times the maximum recommended human dose based upon systemic exposure). An increased incidence of smaller fetuses was observed at 100 mg/kg/day. In an oral pre- and postnatal development study conducted in rats, effects observed at 500 mg/kg/day included slight increases in duration of pregnancy and prenatal loss, reduced pup birth weight and decreased neonatal survival. Treatment-related maternal mortality occurred during gestation at 500 mg/kg/day in this study.8.3 Nursing Mothers
Moxifloxacin is excreted in the breast milk of rats. Moxifloxacin may also be excreted in human milk. Because of the potential for serious adverse reactions in infants who are nursing from mothers taking moxifloxacin hydrochloride, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients and adolescents less than 18 years of age have not been established. Moxifloxacin hydrochloride causes arthropathy in juvenile animals [see Boxed Warning, Warnings and Precautions (5.9), and Clinical Pharmacology (12.3)] .
8.5 Geriatric Use
Geriatric patients are at increased risk for developing severe tendon disorders including tendon rupture when being treated with a fluoroquinolone such as moxifloxacin hydrochloride. This risk is further increased in patients receiving concomitant corticosteroid therapy. Tendinitis or tendon rupture can involve the Achilles, hand, shoulder, or other tendon sites and can occur during or after completion of therapy; cases occurring up to several months after fluoroquinolone treatment have been reported. Caution should be used when prescribing moxifloxacin hydrochloride to elderly patients especially those on corticosteroids. Patients should be informed of this potential side effect and advised to discontinue moxifloxacin hydrochloride and contact their healthcare provider if any symptoms of tendinitis or tendon rupture occur [see Boxed Warning, Warnings and Precautions (5.1), and Adverse Reactions (6.4)].
In controlled multiple-dose clinical trials, 23% of patients receiving oral moxifloxacin hydrochloride were greater than or equal to 65 years of age and 9% were greater than or equal to 75 years of age. The clinical trial data demonstrate that there is no difference in the safety and efficacy of oral moxifloxacin hydrochloride in patients aged 65 or older compared to younger adults.
In trials of intravenous use, 42% of moxifloxacin hydrochloride patients were greater than or equal to 65 years of age, and 23% were greater than or equal to 75 years of age. The clinical trial data demonstrate that the safety of intravenous moxifloxacin hydrochloride in patients aged 65 or older was similar to that of comparator-treated patients. In general, elderly patients may be more susceptible to drug-associated effects of the QT interval. Therefore, moxifloxacin hydrochloride should be avoided in patients taking drugs that can result in prolongation of the QT interval (for example, class IA or class III antiarrhythmics) or in patients with risk factors for torsade de pointes (for example, known QT prolongation, uncorrected hypokalemia). [See Warnings and Precautions (5.3), Drug Interactions (7.5), and Clinical Pharmacology (12.3).]8.6 Renal Impairment
The pharmacokinetic parameters of moxifloxacin are not significantly altered in mild, moderate, severe, or end-stage renal disease. No dosage adjustment is necessary in patients with renal impairment, including those patients requiring hemodialysis (HD) or continuous ambulatory peritoneal dialysis (CAPD). [See Dosage and Administration (2), and Clinical Pharmacology (12.3).]
8.7 Hepatic Impairment
No dosage adjustment is recommended for mild, moderate, or severe hepatic insufficiency (Child-Pugh Classes A, B, or C). However, due to metabolic disturbances associated with hepatic insufficiency, which may lead to QT prolongation, moxifloxacin hydrochloride should be used with caution in these patients [see Warnings and Precautions (5.3), and Clinical Pharmacology (12.3)] .
-
10 OVERDOSAGE
Single oral overdoses up to 2.8 g were not associated with any serious adverse events. In the event of acute overdose, the stomach should be emptied and adequate hydration maintained. ECG monitoring is recommended due to the possibility of QT interval prolongation. The patient should be carefully observed and given supportive treatment. The administration of activated charcoal as soon as possible after oral overdose may prevent excessive increase of systemic moxifloxacin exposure. About 3% and 9% of the dose of moxifloxacin, as well as about 2% and 4.5% of its glucuronide metabolite are removed by continuous ambulatory peritoneal dialysis and hemodialysis, respectively.
Single oral moxifloxacin doses of 2000, 500, and 1500 mg/kg were lethal to rats, mice, and cynomolgus monkeys, respectively. The minimum lethal intravenous dose in mice and rats was 100 mg/kg. Adverse clinical signs included CNS and gastrointestinal effects such as decreased activity, somnolence, tremor, convulsions, vomiting and diarrhea. -
11 DESCRIPTION
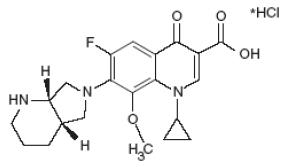
Moxifloxacin hydrochloride is a synthetic broad spectrum antibacterial agent for oral administration. Moxifloxacin, a fluoroquinolone, is available as the monohydrochloride salt of 1-cyclopropyl-7-[(S,S)-2,8-diazabicyclo[4.3.0]non-8-yl]-6-fluoro-8-methoxy-1,4-dihydro-4-oxo-3 quinoline carboxylic acid. It is a slightly yellow to yellow powder or crystals, slightly hygroscopic substance with a molecular weight of 437.9. Its molecular formula is C 21H 24FN 3O 4*HCl and its chemical structure is as follows:
11.1 Moxifloxacin Hydrochloride Tablets
- Moxifloxacin hydrochloride tablets are available as film-coated tablets containing moxifloxacin hydrochloride USP (equivalent to 400 mg moxifloxacin).
- The inactive ingredients are hypromellose, iron oxide red, magnesium stearate, microcrystalline cellulose, polyethylene glycol, povidone, sodium starch glycolate, and titanium dioxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Moxifloxacin hydrochloride is a member of the fluoroquinolone class of antibacterial agents [see Microbiology (12.4)] .
12.3 Pharmacokinetics
Absorption
Moxifloxacin, given as an oral tablet, is well absorbed from the gastrointestinal tract. The absolute bioavailability of moxifloxacin is approximately 90 percent. Co-administration with a high fat meal (that is, 500 calories from fat) does not affect the absorption of moxifloxacin.
Consumption of 1 cup of yogurt with moxifloxacin does not significantly affect the extent or rate of systemic absorption (AUC).Table 5: Mean (± SD) C max and AUC Values Following Single and Multiple Doses of 400 mg Moxifloxacin Given Orally a) Range of means from different studies
C max
(mg/L)
AUC
(mgh/L)
Half-life
(hr)
Single Dose Oral
Healthy (n = 372)
3.1 ± 1
36.1 ± 9.1
11.5 - 15.6 a
Multiple Dose Oral
Healthy young male/female (n = 15)
4.5 ± 0.5
48 ± 2.7
12.7 ± 1.9
Healthy elderly male (n = 8)
3.8 ± 0.3
51.8 ± 6.7
Healthy elderly female (n = 8)
4.6 ± 0.6
54.6 ± 6.7
Healthy young male (n = 8)
3.6 ± 0.5
48.2 ± 9
Healthy young female (n = 9)
4.2 ± 0.5
49.3 ± 9.5
Table 6: Mean (± SD) C max and AUC values following single and multiple doses of 400 mg moxifloxacin given by 1 hour IV infusion a) Range of means from different studies
b) Expected C max (concentration obtained around the time of the end of the infusion)
C max
(mg/L)
AUC
(mgh/L)
Half-life
(hr)
Single Dose IV
Healthy young male/female (n = 56)
3.9 ± 0.9
39.3 ± 8.6
8.2 - 15.4 a
Patients (n = 118)
Male (n = 64)
4.4 ± 3.7
Female ( n = 54)
4.5 ± 2
< 65 years ( n = 58)
4.6 ± 4.2
≥ 65 years (n = 60)
4.3 ± 1.3
Multiple Dose IV
Healthy young male (n = 8)
4.2 ± 0.8
38 ± 4.7
14.8 ± 2.2
Healthy elderly (n=12; 8 male, 4 female)
6.1 ± 1.3
48.2 ± 0.9
10.1 ± 1.6
Patients b (n = 107)
Male (n = 58)
4.2 ± 2.6
Female (n = 49)
4.6 ± 1.5
<65 years (n = 52)
4.1 ± 1.4
≥65 years (n = 55)
4.7 ± 2.7
Plasma concentrations increase proportionately with dose up to the highest dose tested (1200 mg single oral dose). The mean (± SD) elimination half-life from plasma is 12 ± 1.3 hours; steady-state is achieved after at least three days with a 400 mg once daily regimen.
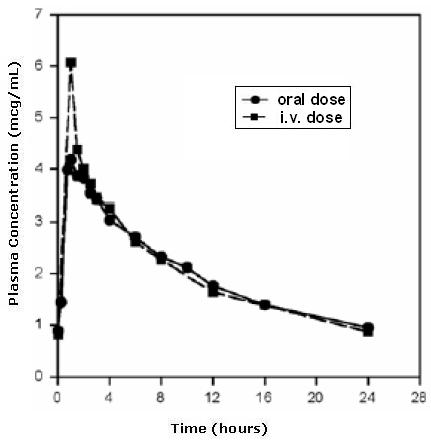
Mean Steady-State Plasma Concentrations of Moxifloxacin Obtained With Once Daily Dosing of 400 mg Either Orally (n=10) or by IV Infusion (n=12)
Distribution
Moxifloxacin is approximately 30 to 50% bound to serum proteins, independent of drug concentration. The volume of distribution of moxifloxacin ranges from 1.7 to 2.7 L/kg. Moxifloxacin is widely distributed throughout the body, with tissue concentrations often exceeding plasma concentrations. Moxifloxacin has been detected in the saliva, nasal and bronchial secretions, mucosa of the sinuses, skin blister fluid, subcutaneous tissue, skeletal muscle, and abdominal tissues and fluids following oral or intravenous administration of 400 mg. Moxifloxacin concentrations measured post-dose in various tissues and fluids following a 400 mg oral or IV dose are summarized in Table 7. The rates of elimination of moxifloxacin from tissues generally parallel the elimination from plasma.Table 7: Moxifloxacin Concentrations (mean ± SD) in Tissues and the Corresponding Plasma Concentrations After a Single 400 mg Oral or Intravenous Dose a a) All moxifloxacin concentrations were measured 3 hours after a single 400 mg dose, except the abdominal tissue and exudate concentrations which were measured at 2 hours post-dose and the sinus concentrations which were measured 3 hours post-dose after 5 days of dosing.
b) N = 5
c) N = 7
d) N = 12
e) Reflects only non-protein bound concentrations of drug.
Tissue or Fluid
N
Plasma
Concentration
(mcg/mL)
Tissue or Fluid
Concentration
(mcg/mL or
mcg/g)
Tissue Plasma
Ratio
Respiratory
Alveolar Macrophages
5
3.3 ± 0.7
61.8 ± 27.3
21.2 ± 10
Bronchial Mucosa
8
3.3 ± 0.7
5.5 ± 1.3
1.7 ± 0.3
Epithelial Lining Fluid
5
3.3 ± 0.7
24.4 ± 14.7
8.7 ± 6.1
Sinus
Maxillary Sinus Mucosa
4
3.7 ± 1.1 b
7.6 ± 1.7
2 ± 0.3
Anterior Ethmoid Mucosa
3
3.7 ± 1.1 b
8.8 ± 4.3
2.2 ± 0.6
Nasal Polyps
4
3.7 ± 1.1 b
9.8 ± 4.5
2.6 ± 0.6
Skin, Musculoskeletal
Blister Fluid
5
3 ± 0.5 c
2.6 ± 0.9
0.9 ± 0.2
Subcutaneous Tissue
6
2.3 ± 0.4 d
0.9 ± 0.3 e
0.4 ± 0.6
Skeletal Muscle
6
2.3 ± 0.4 d
0.9 ± 0.2 e
0.4 ± 0.1
Intra-Abdominal
Abdominal tissue
8
2.9 ± 0.5
7.6 ± 2
2.7 ± 0.8
Abdominal exudate
10
2.3 ± 0.5
3.5 ± 1.2
1.6 ± 0.7
Abscess fluid
6
2.7 ± 0.7
2.3 ± 1.5
0.8 ± 0.4
Metabolism
Approximately 52% of an oral or intravenous dose of moxifloxacin is metabolized via glucuronide and sulfate conjugation. The cytochrome P450 system is not involved in moxifloxacin metabolism, and is not affected by moxifloxacin. The sulfate conjugate (M1) accounts for approximately 38% of the dose, and is eliminated primarily in the feces. Approximately 14% of an oral or intravenous dose is converted to a glucuronide conjugate (M2), which is excreted exclusively in the urine. Peak plasma concentrations of M2 are approximately 40% those of the parent drug, while plasma concentrations of M1 are generally less than 10% those of moxifloxacin.
In vitro studies with cytochrome (CYP) P450 enzymes indicate that moxifloxacin does not inhibit CYP3A4, CYP2D6, CYP2C9, CYP2C19, or CYP1A2, suggesting that moxifloxacin is unlikely to alter the pharmacokinetics of drugs metabolized by these enzymes.
Excretion
Approximately 45% of an oral or intravenous dose of moxifloxacin is excreted as unchanged drug (~20% in urine and ~25% in feces). A total of 96% ± 4% of an oral dose is excreted as either unchanged drug or known metabolites. The mean (± SD) apparent total body clearance and renal clearance are 12 ± 2 L/hr and 2.6 ± 0.5 L/hr, respectively.
Pharmacokinetics in Specific Populations
Geriatric
Following oral administration of 400 mg moxifloxacin for 10 days in 16 elderly (8 male; 8 female) and 17 young (8 male; 9 female) healthy volunteers, there were no age-related changes in moxifloxacin pharmacokinetics. In 16 healthy male volunteers (8 young; 8 elderly) given a single 200 mg dose of oral moxifloxacin, the extent of systemic exposure (AUC and C max) was not statistically different between young and elderly males and elimination half-life was unchanged. No dosage adjustment is necessary based on age. In large phase III studies, the concentrations around the time of the end of the infusion in elderly patients following intravenous infusion of 400 mg were similar to those observed in young patients. [see Use In Specific Populations (8.5).]
Pediatric
The pharmacokinetics of moxifloxacin in pediatric subjects has not been studied [see Use in Specific Populations (8.4)] .
Gender
Following oral administration of 400 mg moxifloxacin daily for 10 days to 23 healthy males (19 to 75 years) and 24 healthy females (19 to 70 years), the mean AUC and C max were 8% and 16% higher, respectively, in females compared to males. There are no significant differences in moxifloxacin pharmacokinetics between male and female subjects when differences in body weight are taken into consideration.
A 400 mg single dose study was conducted in 18 young males and females. The comparison of moxifloxacin pharmacokinetics in this study (9 young females and 9 young males) showed no differences in AUC or C max due to gender. Dosage adjustments based on gender are not necessary.
Race
Steady-state moxifloxacin pharmacokinetics in male Japanese subjects were similar to those determined in Caucasians, with a mean C max of 4.1 mcg/mL, an AUC 24 of 47 mcgh/mL, and an elimination half-life of 14 hours, following 400 mg p.o. daily.
Renal Insufficiency
The pharmacokinetic parameters of moxifloxacin are not significantly altered in mild, moderate, severe, or end-stage renal disease. No dosage adjustment is necessary in patients with renal impairment, including those patients requiring hemodialysis (HD) or continuous ambulatory peritoneal dialysis (CAPD).
In a single oral dose study of 24 patients with varying degrees of renal function from normal to severely impaired, the mean peak concentrations (C max) of moxifloxacin were reduced by 21% and 28% in the patients with moderate (CL CR≥30 and ≤ 60 mL/min) and severe (CL CR<30 mL/min) renal impairment, respectively. The mean systemic exposure (AUC) in these patients was increased by 13%. In the moderate and severe renally impaired patients, the mean AUC for the sulfate conjugate (M1) increased by 1.7-fold (ranging up to 2.8-fold) and mean AUC and C max for the glucuronide conjugate (M2) increased by 2.8-fold (ranging up to 4.8-fold) and 1.4-fold (ranging up to 2.5-fold), respectively. [See Use in Specific Populations (8.6).]
The pharmacokinetics of single dose and multiple dose moxifloxacin were studied in patients with CL CR<20 mL/min on either hemodialysis or continuous ambulatory peritoneal dialysis (8 HD, 8 CAPD). Following a single 400 mg oral dose, the AUC of moxifloxacin in these HD and CAPD patients did not vary significantly from the AUC generally found in healthy volunteers. C max values of moxifloxacin were reduced by about 45% and 33% in HD and CAPD patients, respectively, compared to healthy, historical controls. The exposure (AUC) to the sulfate conjugate (M1) increased by 1.4- to 1.5-fold in these patients. The mean AUC of the glucuronide conjugate (M2) increased by a factor of 7.5, whereas the mean C max values of the glucuronide conjugate (M2) increased by a factor of 2.5 to 3, compared to healthy subjects. The sulfate and the glucuronide conjugates of moxifloxacin are not microbiologically active, and the clinical implication of increased exposure to these metabolites in patients with renal disease including those undergoing HD and CAPD has not been studied.
Oral administration of 400 mg QD moxifloxacin for 7 days to patients on HD or CAPD produced mean systemic exposure (AUC ss) to moxifloxacin similar to that generally seen in healthy volunteers. Steady-state C max values were about 22% lower in HD patients but were comparable between CAPD patients and healthy volunteers. Both HD and CAPD removed only small amounts of moxifloxacin from the body (approximately 9% by HD, and 3% by CAPD). HD and CAPD also removed about 4% and 2% of the glucuronide metabolite (M2), respectively.
Hepatic Insufficiency
No dosage adjustment is recommended for mild, moderate, or severe hepatic insufficiency (Child-Pugh Classes A, B, or C). However, due to metabolic disturbances associated with hepatic insufficiency, which may lead to QT prolongation, moxifloxacin hydrochloride should be used with caution in these patients [see Warnings and Precautions (5.3), Use in Specific Populations (8.7)].
In 400 mg single oral dose studies in 6 patients with mild (Child-Pugh Class A) and 10 patients with moderate (Child-Pugh Class B) hepatic insufficiency, moxifloxacin mean systemic exposure (AUC) was 78% and 102%, respectively, of 18 healthy controls and mean peak concentration (C max) was 79% and 84% of controls.
The mean AUC of the sulfate conjugate of moxifloxacin (M1) increased by 3.9-fold (ranging up to 5.9-fold) and 5.7-fold (ranging up to 8-fold) in the mild and moderate groups, respectively. The mean C max of M1 increased by approximately 3-fold in both groups (ranging up to 4.7- and 3.9-fold). The mean AUC of the glucuronide conjugate of moxifloxacin (M2) increased by 1.5-fold (ranging up to 2.5-fold) in both groups. The mean C max of M2 increased by 1.6- and 1.3-fold (ranging up to 2.7- and 2.1-fold), respectively. The clinical significance of increased exposure to the sulfate and glucuronide conjugates has not been studied. In a subset of patients participating in a clinical trial, the plasma concentrations of moxifloxacin and metabolites determined approximately at the moxifloxacin T max following the first intravenous or oral moxifloxacin dose in the Child-Pugh Class C patients (n=10) were similar to those in the Child-Pugh Class A/B patients (n=5), and also similar to those observed in healthy volunteer studies.
Photosensitivity Potential
A study of the skin response to ultraviolet (UVA and UVB) and visible radiation conducted in 32 healthy volunteers (8 per group) demonstrated that moxifloxacin hydrochloride does not show phototoxicity in comparison to placebo. The minimum erythematous dose (MED) was measured before and after treatment with moxifloxacin (200 mg or 400 mg once daily), lomefloxacin (400 mg once daily), or placebo. In this study, the MED measured for both doses of moxifloxacin were not significantly different from placebo, while lomefloxacin significantly lowered the MED.
It is difficult to ascribe relative photosensitivity/phototoxicity among various fluoroquinolones during actual patient use because other factors play a role in determining a subject’s susceptibility to this adverse event such as: a patient’s skin pigmentation, frequency and duration of sun and artificial ultraviolet light (UV) exposure, wearing of sunscreen and protective clothing, the use of other concomitant drugs and the dosage and duration of fluoroquinolone therapy [see Warnings and Precautions (5.11), Adverse Reactions ( 6.3), and Patient Counseling Information (17)] .
Drug-Drug Interactions
The following drug interactions were studied in healthy volunteers or patients.
Antacids and iron significantly reduced bioavailability of moxifloxacin, as observed with other quinolones [see Drug Interactions (7.1)] .
Calcium, digoxin, itraconazole, morphine, probenecid, ranitidine, theophylline and warfarin did not significantly affect the pharmacokinetics of moxifloxacin. These results and the data from in vitro studies suggest that moxifloxacin is unlikely to significantly alter the metabolic clearance of drugs metabolized by CYP3A4, CYP2D6, CYP2C9, CYP2C19, or CYP1A2 enzymes.
Moxifloxacin had no clinically significant effect on the pharmacokinetics of atenolol, digoxin, glyburide, itraconazole, oral contraceptives, theophylline, cyclosporine and warfarin [see Drug Interactions (7.2)].
Antacids
When moxifloxacin (single 400 mg tablet dose) was administered two hours before, concomitantly, or 4 hours after an aluminum/magnesium-containing antacid (900 mg aluminum hydroxide and 600 mg magnesium hydroxide as a single oral dose) to 12 healthy volunteers there was a 26%, 60% and 23% reduction in the mean AUC of moxifloxacin, respectively. Moxifloxacin should be taken at least 4 hours before or 8 hours after antacids containing magnesium or aluminum, as well as sucralfate, metal cations such as iron, and multivitamin preparations with zinc, or VIDEX ® (didanosine) chewable/ buffered tablets or the pediatric powder for oral solution. [See Dosage and Administration (2.2), Drug Interactions (7.1).]
Atenolol
In a crossover study involving 24 healthy volunteers (12 male; 12 female), the mean atenolol AUC following a single oral dose of 50 mg atenolol with placebo was similar to that observed when atenolol was given concomitantly with a single 400 mg oral dose of moxifloxacin. The mean C max of single dose atenolol decreased by about 10% following co-administration with a single dose of moxifloxacin.
Calcium
Twelve healthy volunteers were administered concomitant moxifloxacin (single 400 mg dose) and calcium (single dose of 500 mg Ca ++ dietary supplement) followed by an additional two doses of calcium 12 and 24 hours after moxifloxacin administration. Calcium had no significant effect on the mean AUC of moxifloxacin. The mean C max was slightly reduced and the time to maximum plasma concentration was prolonged when moxifloxacin was given with calcium compared to when moxifloxacin was given alone (2.5 hours versus 0.9 hours). These differences are not considered to be clinically significant.
Digoxin
No significant effect of moxifloxacin (400 mg once daily for two days) on digoxin (0.6 mg as a single dose) AUC was detected in a study involving 12 healthy volunteers. The mean digoxin C max increased by about 50% during the distribution phase of digoxin. This transient increase in digoxin C max is not viewed to be clinically significant. Moxifloxacin pharmacokinetics were similar in the presence or absence of digoxin. No dosage adjustment for moxifloxacin or digoxin is required when these drugs are administered concomitantly.
Glyburide
In diabetics, glyburide (2.5 mg once daily for two weeks pretreatment and for five days concurrently) mean AUC and C max were 12% and 21% lower, respectively, when taken with moxifloxacin (400 mg once daily for five days) in comparison to placebo. Nonetheless, blood glucose levels were decreased slightly in patients taking glyburide and moxifloxacin in comparison to those taking glyburide alone, suggesting no interference by moxifloxacin on the activity of glyburide. These interaction results are not viewed as clinically significant.
Iron
When moxifloxacin tablets were administered concomitantly with iron (ferrous sulfate 100 mg once daily for two days), the mean AUC and C max of moxifloxacin was reduced by 39% and 59%, respectively. Moxifloxacin should only be taken more than 4 hours before or 8 hours after iron products. [See Dosage and Administration (2.2), Drug Interactions (7.1).]
Itraconazole
In a study involving 11 healthy volunteers, there was no significant effect of itraconazole (200 mg once daily for 9 days), a potent inhibitor of cytochrome P4503A4, on the pharmacokinetics of moxifloxacin (a single 400 mg dose given on the 7 th day of itraconazole dosing). In addition, moxifloxacin was shown not to affect the pharmacokinetics of itraconazole.
Morphine
No significant effect of morphine sulfate (a single 10 mg intramuscular dose) on the mean AUC and C max of moxifloxacin (400 mg single dose) was observed in a study of 20 healthy male and female volunteers.
Oral Contraceptives
A placebo-controlled study in 29 healthy female subjects showed that moxifloxacin 400 mg daily for 7 days did not interfere with the hormonal suppression of oral contraception with 0.15 mg levonorgestrel/0.03 mg ethinylestradiol (as measured by serum progesterone, FSH, estradiol, and LH), or with the pharmacokinetics of the administered contraceptive agents.
Probenecid
Probenecid (500 mg twice daily for two days) did not alter the renal clearance and total amount of moxifloxacin (400 mg single dose) excreted renally in a study of 12 healthy volunteers.
Ranitidine
No significant effect of ranitidine (150 mg twice daily for three days as pretreatment) on the pharmacokinetics of moxifloxacin (400 mg single dose) was detected in a study involving 10 healthy volunteers.
Theophylline
No significant effect of moxifloxacin (200 mg every twelve hours for 3 days) on the pharmacokinetics of theophylline (400 mg every twelve hours for 3 days) was detected in a study involving 12 healthy volunteers. In addition, theophylline was not shown to affect the pharmacokinetics of moxifloxacin. The effect of co-administration of a 400 mg dose of moxifloxacin with theophylline has not been studied, but it is not expected to be clinically significant based on in vitro metabolic data showing that moxifloxacin does not inhibit the CYP1A2 isoenzyme.
Warfarin
No significant effect of moxifloxacin (400 mg once daily for eight days) on the pharmacokinetics of R- and S-warfarin (25 mg single dose of warfarin sodium on the fifth day) was detected in a study involving 24 healthy volunteers. No significant change in prothrombin time was observed. [See Adverse Reactions (6.2), Drug Interactions (7.2).]12.4 Microbiology
Mechanism of Action
The bactericidal action of moxifloxacin results from inhibition of the topoisomerase II (DNA gyrase) and topoisomerase IV required for bacterial DNA replication, transcription, repair, and recombination. It appears that the C8-methoxy moiety contributes to enhanced activity and lower selection of resistant mutants of Gram-positive bacteria compared to the C8-H moiety. The presence of the bulky bicycloamine substituent at the C-7 position prevents active efflux, associated with the NorA or pmrA genes seen in certain Gram-positive bacteria.
Mechanism of Resistance
The mechanism of action for fluoroquinolones, including moxifloxacin, is different from that of macrolides, beta-lactams, aminoglycosides, or tetracyclines; therefore, microorganisms resistant to these classes of drugs may be susceptible to moxifloxacin. Resistance to fluoroquinolones occurs primarily by a mutation in topoisomerase II (DNA gyrase) or topoisomerase IV genes, decreased outer membrane permeability or drug efflux. In vitro resistance to moxifloxacin develops slowly via multiple-step mutations. Resistance to moxifloxacin occurs in vitro at a general frequency of between 1.8 x 10 -9 to < 1 x 10 -11 for Gram-positive bacteria.
Cross Resistance
Cross-resistance has been observed between moxifloxacin and other fluoroquinolones against Gram-negative bacteria. Gram-positive bacteria resistant to other fluoroquinolones may, however, still be susceptible to moxifloxacin. There is no known cross-resistance between moxifloxacin and other classes of antimicrobials.
Moxifloxacin has been shown to be active against most isolates of the following bacteria, both in vitro and in clinical infections [see Indications and Usage (1)].
Gram-positive bacteria
- Enterococcus faecalis
- Staphylococcus aureus
- Streptococcus anginosus
- Streptococcus constellatus
- Streptococcus pneumoniae (including multi-drug resistant isolates [MDRSP]**)
- Streptococcus pyogenes
**MDRSP, Multi-drug resistant Streptococcus pneumoniae includes isolates previously known as PRSP (Penicillin-resistant S. pneumoniae), and are isolates resistant to two or more of the following antibiotics: penicillin (MIC) ≥2 mcg/mL), 2 nd generation cephalosporins (for example, cefuroxime), macrolides, tetracyclines, and trimethoprim/sulfamethoxazole.
Gram-negative bacteria
- Enterobacter cloacae
- Escherichia coli
- Haemophilus influenzae
- Haemophilus parainfluenzae
- Klebsiella pneumoniae
- Moraxella catarrhalis
- Proteus mirabilis
Anaerobic bacteria
- Bacteroides fragilis
- Bacteroides thetaiotaomicron
- Clostridium perfringens
- Peptostreptococcus species
Other microorganisms
- Chlamydophila pneumoniae
- Mycoplasma pneumoniae
The following in vitro data are available, but their clinical significance is unknown. At least 90 percent of the following bacteria exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for moxifloxacin. However, the efficacy of moxifloxacin hydrochloride in treating clinical infections due to these bacteria has not been established in adequate and well controlled clinical trials.
Gram-positive bacteria
- Staphylococcus epidermidis
- Streptococcus agalactiae
- Streptococcus viridans group
Gram-negative bacteria
- Citrobacter freundii
- Klebsiella oxytoca
- Legionella pneumophila
Anaerobic bacteria
- Fusobacterium species
- Prevotella species
Susceptibility Tests Methods
When available, the clinical microbiology laboratory should provide the results of in vitro susceptibility test results for antimicrobial drug products used in resident hospitals to the physician as periodic reports that describe the susceptibility profile of nosocomial and community acquired pathogens. These reports should aid the physician in selecting an antibacterial drug product for treatment.
- Dilution Techniques:
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method (broth and/or agar). 1 The MIC values should be interpreted according to the criteria in Table 8.
- Diffusion Techniques:
Quantitative methods that require measurement of zone diameters can also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. The zone size provides an estimate of the susceptibility of bacteria to antimicrobial compounds. The zone size prove should be determined using a standardized test method. 2,3 This procedure uses paper disks impregnated with 5 mcg moxifloxacin to test the susceptibility of bacteria to moxifloxacin. The disc diffusion interpretive criteria are provided in Table 8.
- Anaerobic Techniques:
For anaerobic bacteria, the susceptibility to moxifloxacin can be determined by a standardized test method. 4 The MIC values obtained should be interpreted according to the criteria provided in Table 8.
Table 8: Susceptibility Test Interpretive Criteria for Moxifloxacin S=Susceptible, I=Intermediate, and R=Resistant.
a) The current absence of data on moxifloxacin-resistant isolates precludes defining any results other than “Susceptible”.
Isolates yielding test results (MIC or zone diameter) other than susceptible, should be submitted to a reference laboratory for additional testing.
MIC (mcg/mL)
Zone Diameter (mm)
Species
S
I
R
S
I
R
Enterobacteriacae
≤2
4
≥8
≥19
16–18
≤15
Enterococcus faecalis
≤1
2
≥4
≥18
15–17
≤14
Staphylococcus aureus
≤2
4
≥8
≥19
16–18
≤15
Haemophilus influenzae
≤1
a
a
≥18
a
a
Haemophilus parainfluenzae
≤1
a
a
≥18
a
a
Streptococcus pneumoniae
≤1
2
≥4
≥18
15–17
≤14
Streptococcus species
≤1
2
≥4
≥18
15–17
≤14
Anaerobic bacteria
≤2
4
≥8
-
-
-
A report of “Susceptible” indicates that the antimicrobial is likely to inhibit growth of the pathogen if the antimicrobial compound reaches the concentrations at the infection site necessary to inhibit growth of the pathogen. A report of “Intermediate” indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where a high dosage of the drug product can be used. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of “Resistant” indicates that the antimicrobial is not likely to inhibit growth of the pathogen if the antimicrobial compound reaches the concentrations usually achievable at the infection site; other therapy should be selected.
- Quality Control
Standardized susceptibility test procedures require the use of laboratory controls to monitor and ensure the accuracy and precision of supplies and reagents used in the assay and the techniques of the individuals performing the test. 1,2,3,4 Standard moxifloxacin powder should provide the following range of MIC values noted in Table 9. For the diffusion technique using the 5 mcg moxifloxacin disk, the criteria in Table 9 should be achieved.
Table 9: Acceptable Quality Control Ranges for Moxifloxacin Strains
MIC range (mcg/mL)
Zone Diameter (mm)
Enterococcus faecalis ATCC 29212
0.06–0.5
-
Escherichia coli ATCC 25922
0.008–0.06
28–35
Haemophilus influenzae ATCC 49247
0.008–0.03
31–39
Staphylococcus aureus ATCC 29213
0.015–0.06
-
Staphylococcus aureus ATCC 25923
-
28–35
Streptococcus pneumoniae ATCC 49619
0.06–0.25
25–31
Bacteroides fragilis ATCC 25285
0.125–0.5
-
Bacteroides thetaiotaomicron ATCC 29741
1–4
-
Eubacterium lentum ATCC 43055
0.125–0.5
-
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long term studies in animals to determine the carcinogenic potential of moxifloxacin have not been performed.
Moxifloxacin was not mutagenic in 4 bacterial strains (TA 98, TA 100, TA 1535, TA 1537) used in the Ames Salmonella reversion assay. As with other quinolones, the positive response observed with moxifloxacin in strain TA 102 using the same assay may be due to the inhibition of DNA gyrase. Moxifloxacin was not mutagenic in the CHO/HGPRT mammalian cell gene mutation assay. An equivocal result was obtained in the same assay when v79 cells were used. Moxifloxacin was clastogenic in the v79 chromosome aberration assay, but it did not induce unscheduled DNA synthesis in cultured rat hepatocytes. There was no evidence of genotoxicity in vivo in a micronucleus test or a dominant lethal test in mice.
Moxifloxacin had no effect on fertility in male and female rats at oral doses as high as 500 mg/kg/day, approximately 12 times the maximum recommended human dose based on body surface area (mg/m 2), or at intravenous doses as high as 45 mg/kg/day, approximately equal to the maximum recommended human dose based on body surface area (mg/m 2). At 500 mg/kg orally there were slight effects on sperm morphology (head-tail separation) in male rats and on the estrous cycle in female rats.13.2 Animal Toxicology and/or Pharmacology
Quinolones have been shown to cause arthropathy in immature animals. In studies in juvenile dogs oral doses of moxifloxacin ≥ 30 mg/kg/day (approximately 1.5 times the maximum recommended human dose based upon systemic exposure) for 28 days resulted in arthropathy. There was no evidence of arthropathy in mature monkeys and rats at oral doses up to 135 and 500 mg/kg/day, respectively.
Moxifloxacin at an oral dose of 300 mg/kg did not show an increase in acute toxicity or potential for CNS toxicity (for example, seizures) in mice when used in combination with NSAIDs such as diclofenac, ibuprofen, or fenbufen. Some quinolones have been reported to have proconvulsant activity that is exacerbated with concomitant use of non-steroidal anti-inflammatory drugs (NSAIDs).
A QT-prolonging effect of moxifloxacin was found in dog studies, at plasma concentrations about five times the human therapeutic level. The combined infusion of sotalol, a Class III antiarrhythmic agent, with moxifloxacin induced a higher degree of QTc prolongation in dogs than that induced by the same dose (30 mg/kg) of moxifloxacin alone. Electrophysiological in vitro studies suggested an inhibition of the rapid activating component of the delayed rectifier potassium current (I Kr) as an underlying mechanism.
No signs of local intolerability were observed in dogs when moxifloxacin was administered intravenously. After intraarterial injection, inflammatory changes involving the peri-arterial soft tissue were observed suggesting that intra-arterial administration of moxifloxacin hydrochloride should be avoided. -
14 CLINICAL STUDIES
14.1 Acute Bacterial Exacerbation of Chronic Bronchitis
Moxifloxacin hydrochloride tablets (400 mg once daily for five days) were evaluated for the treatment of acute bacterial exacerbation of chronic bronchitis in a randomized, double-blind, controlled clinical trial conducted in the U.S. This study compared moxifloxacin hydrochloride with clarithromycin (500 mg twice daily for 10 days) and enrolled 629 patients. Clinical success was assessed at 7 to 17 days post-therapy. The clinical success for moxifloxacin hydrochloride was 89% (222/250) compared to 89% (224/251) for clarithromycin.
Table 10: Clinical Success Rates at Follow-Up Visit for Clinically Evaluable Patients by Pathogen (Acute Bacterial Exacerbation of Chronic Bronchitis) Pathogen Moxifloxacin Hydrochloride Clarithromycin Streptococcus pneumoniae
16/16 (100%)
20/23 (87%)
Haemophilus influenzae
33/37 (89%)
36/41 (88%)
Haemophilus parainfluenzae
16/16 (100%)
14/14 (100%)
Moraxella catarrhalis
29/34 (85%)
24/24 (100%)
Staphylococcus aureus
15/16 (94%)
6/8 (75%)
Klebsiella pneumoniae
18/20 (90%)
10/11 (91%)
The microbiological eradication rates (eradication plus presumed eradication) in moxifloxacin hydrochloride treated patients were Streptococcus pneumoniae 100%, Haemophilus influenzae 89%, Haemophilus parainfluenzae 100%, Moraxella catarrhalis 85%, Staphylococcus aureus 94%, and Klebsiella pneumoniae 85%.
14.2 Community Acquired Pneumonia
A randomized, double-blind, controlled clinical trial was conducted in the U.S. to compare the efficacy of moxifloxacin hydrochloride tablets (400 mg once daily) to that of high-dose clarithromycin (500 mg twice daily) in the treatment of patients with clinically and radiologically documented community acquired pneumonia. This study enrolled 474 patients (382 of whom were valid for the efficacy analysis conducted at the 14 to 35 day follow-up visit). Clinical success for clinically evaluable patients was 95% (184/194) for moxifloxacin hydrochloride and 95% (178/188) for high dose clarithromycin.
A randomized, double-blind, controlled trial was conducted in the U.S. and Canada to compare the efficacy of sequential IV/PO moxifloxacin 400 mg QD for 7 to 14 days to an IV/PO fluoroquinolone control (trovafloxacin or levofloxacin) in the treatment of patients with clinically and radiologically documented community acquired pneumonia. This study enrolled 516 patients, 362 of whom were valid for the efficacy analysis conducted at the 7 to 30 day post-therapy visit. The clinical success rate was 86% (157/182) for moxifloxacin hydrochloride therapy and 89% (161/180) for the fluoroquinolone comparators.
An open-label ex-U.S. study that enrolled 628 patients compared moxifloxacin hydrochloride to sequential IV/PO amoxicillin/clavulanate (1.2 g IV q 8 h/625 mg PO q 8 h) with or without high-dose IV/PO clarithromycin (500 mg BID). The intravenous formulations of the comparators are not FDA approved. The clinical success rate at Day 5 to 7 for moxifloxacin hydrochloride therapy was 93% (241/258) and demonstrated superiority to amoxicillin/clavulanate ± clarithromycin (85%, 239/280) [95% C.I. of difference in success rates between moxifloxacin and comparator (2.9%, 13.2%)]. The clinical success rate at the 21 to 28 days post-therapy visit for moxifloxacin hydrochloride was 84% (216/258), which also demonstrated superiority to the comparators (74%, 208/280) [95% C.I. of difference in success rates between moxifloxacin and comparator (2.6%, 16.3%)].
The clinical success rates by pathogen across four CAP studies are presented in Table 11.
Table 11: Clinical Success Rates By Pathogen (Pooled CAP Studies) Pathogen Moxifloxacin Hydrochloride Streptococcus pneumoniae
80/85
(94%)
Staphylococcus aureus
17/20
(85%)
Klebsiella pneumoniae
11/12
(92%)
Haemophilus influenzae
56/61
(92%)
Chlamydophila pneumoniae
119/128
(93%)
Mycoplasma pneumoniae
73/76
(96%)
Moraxella catarrhalis
11/12
(92%)
14.3 Community Acquired Pneumonia caused by Multi-Drug Resistant Streptococcus pneumoniae (MDRSP)*
Moxifloxacin hydrochloride was effective in the treatment of community acquired pneumonia (CAP) caused by multi-drug resistant Streptococcus pneumoniae MDRSP* isolates. Of 37 microbiologically evaluable patients with MDRSP isolates, 35 patients (95%) achieved clinical and bacteriological success post-therapy. The clinical and bacteriological success rates based on the number of patients treated are shown in Table 12.
* MDRSP, Multi-drug resistant Streptococcus pneumoniae includes isolates previously known as PRSP (Penicillin-resistant S. pneumoniae), and are isolates resistant to two or more of the following antibiotics: penicillin (MIC ≥ 2 mcg/mL), 2 nd generation cephalosporins (for example, cefuroxime), macrolides, tetracyclines, and trimethoprim/sulfamethoxazole.Table 12: Clinical and Bacteriological Success Rates for Moxifloxacin Hydrochloride-Treated MDRSP CAP Patients (Population: Valid for Efficacy) a) n = number of patients successfully treated; N = number of patients with MDRSP (from a total of 37 patients)
b) n = number of patients successfully treated (presumed eradication or eradication); N = number of patients with MDRSP (from a total of 37 patients)
c) One patient had a respiratory isolate that was resistant to penicillin and cefuroxime but a blood isolate that was intermediate to penicillin and cefuroxime. The patient is included in the database based on the respiratory isolate.
d) Azithromycin, clarithromycin, and erythromycin were the macrolide antimicrobials tested.
Screening Susceptibility
Clinical Success
Bacteriological Success
n/N a
%
n/N b
%
Penicillin-resistant
21/21
100% c
21/21
100% c
2 nd generation cephalosporin-resistant
25/26
96% c
25/26
96% c
Macrolide-resistant d
22/23
96%
22/23
96%
Trimethoprim/sulfamethoxazole-resistant
28/30
93%
28/30
93%
Tetracycline-resistant
17/18
94%
17/18
94%
Not all isolates were resistant to all antimicrobial classes tested. Success and eradication rates are summarized in Table 13.
Table 13: Clinical Success Rates and Microbiological Eradication Rates for Resistant Streptococcus pneumoniae (Community Acquired Pneumonia) a) One patient had a respiratory isolate resistant to 5 antimicrobials and a blood isolate resistant to 3 antimicrobials. The patient was included in the category resistant to 5 antimicrobials.
S. pneumoniae with
MDRSP
Clinical Success
Bacteriological Eradication Rate
Resistant to 2 antimicrobials
12/13 (92.3%)
12/13 (92.3%)
Resistant to 3 antimicrobials
10/11 (90.9%) a
10/11 (90.9%) a
Resistant to 4 antimicrobials
6/6 (100%)
6/6 (100%)
Resistant to 5 antimicrobials
7/7 (100%) a
7/7 (100%) a
Bacteremia with MDRSP
9/9 (100%)
9/9 (100%)
14.4 Acute Bacterial Sinusitis
In a controlled double-blind study conducted in the U.S., moxifloxacin hydrochloride tablets (400 mg once daily for ten days) were compared with cefuroxime axetil (250 mg twice daily for ten days) for the treatment of acute bacterial sinusitis. The trial included 457 patients valid for the efficacy analysis. Clinical success (cure plus improvement) at the 7 to 21 day post-therapy test of cure visit was 90% for moxifloxacin hydrochloride and 89% for cefuroxime.
An additional non-comparative study was conducted to gather bacteriological data and to evaluate microbiological eradication in adult patients treated with moxifloxacin 400 mg once daily for seven days. All patients (n = 336) underwent antral puncture in this study. Clinical success rates and eradication/presumed eradication rates at the 21 to 37 day follow-up visit were 97% (29 out of 30) for Streptococcus pneumoniae, 83% (15 out of 18) for Moraxella catarrhalis, and 80% (24 out of 30) for Haemophilus influenzae.14.5 Uncomplicated Skin and Skin Structure Infections
A randomized, double-blind, controlled clinical trial conducted in the U.S. compared the efficacy of moxifloxacin 400 mg once daily for seven days with cephalexin hydrochloride 500 mg three times daily for seven days. The percentage of patients treated for uncomplicated abscesses was 30%, furuncles 8%, cellulitis 16%, impetigo 20%, and other skin infections 26%. Adjunctive procedures (incision and drainage or debridement) were performed on 17% of the moxifloxacin hydrochloride treated patients and 14% of the comparator treated patients. Clinical success rates in evaluable patients were 89% (108/122) for moxifloxacin hydrochloride and 91% (110/121) for cephalexin hydrochloride.
14.6 Complicated Skin and Skin Structure Infections
Two randomized, active controlled trials of cSSSI were performed. A double-blind trial was conducted primarily in North America to compare the efficacy of sequential IV/PO moxifloxacin 400 mg QD for 7 to 14 days to an IV/PO beta-lactam/beta-lactamase inhibitor control in the treatment of patients with cSSSI. This study enrolled 617 patients, 335 of which were valid for the efficacy analysis. A second open-label International study compared moxifloxacin 400 mg QD for 7 to 21 days to sequential IV/PO beta-lactam/beta-lactamase inhibitor control in the treatment of patients with cSSSI. This study enrolled 804 patients, 632 of which were valid for the efficacy analysis. Surgical incision and drainage or debridement was performed on 55% of the moxifloxacin hydrochloride treated and 53% of the comparator treated patients in these studies and formed an integral part of therapy for this indication. Success rates varied with the type of diagnosis ranging from 61% in patients with infected ulcers to 90% in patients with complicated erysipelas. These rates were similar to those seen with comparator drugs. The overall success rates in the evaluable patients and the clinical success by pathogen are shown in Tables 14 and 15.
Table 14: Overall Clinical Success Rates in Patients with Complicated Skin and Skin Structure Infections Study Moxifloxacin Hydrochloride
n/N (%)Comparator
n/N (%)95% Confidence Interval* * of difference in success rates between moxifloxacin and comparator (moxifloxacin – comparator)
North America
125/162 (77.2%)
141/173 (81.5%)
(-14.4%, 2%)
International
254/315 (80.6%)
268/317 (84.5%)
(-9.4%, 2.2%)
Table 15: Clinical Success Rates by Pathogen in Patients with Complicated Skin and Skin Structure Infections Pathogen Moxifloxacin Hydrochloride
n/N (%)Comparator
n/N (%)a) methicillin susceptibility was only determined in the North American Study
Staphylococcus aureus
(methicillin-susceptible isolates) a
106/129 (82.2%)
120/137 (87.6%)
Escherichia coli
31/38 (81.6 %)
28/33 (84.8 %)
Klebsiella pneumoniae
11/12 (91.7 % )
7/10 (70%)
Enterobacter cloacae
9/11 (81.8%)
4/7 (57.1%)
14.7 Complicated Intra-Abdominal Infections
Two randomized, active controlled trials of cIAI were performed. A double-blind trial was conducted primarily in North America to compare the efficacy of sequential IV/PO moxifloxacin 400 mg QD for 5 to 14 days to IV/piperacillin/tazobactam followed by PO amoxicillin/clavulanic acid in the treatment of patients with cIAI, including peritonitis, abscesses, appendicitis with perforation, and bowel perforation. This study enrolled 681 patients, 379 of which were considered clinically evaluable. A second open-label international study compared moxifloxacin 400 mg QD for 5 to 14 days to IV ceftriaxone plus IV metronidazole followed by PO amoxicillin/clavulanic acid in the treatment of patients with cIAI. This study enrolled 595 patients, 511 of which were considered clinically evaluable. The clinically evaluable population consisted of subjects with a surgically confirmed complicated infection, at least 5 days of treatment and a 25 to 50 day follow-up assessment for patients at the Test of Cure visit. The overall clinical success rates in the clinically evaluable patients are shown in Table 16.
Table 16: Clinical Success Rates in Patients with Complicated Intra-Abdominal Infections Study Moxifloxacin Hydrochloride
n/N (%)Comparator
n/N (%)95% Confidence Interval a a) of difference in success rates between moxifloxacin hydrochloride and comparator (moxifloxacin hydrochloride – comparator)
b) Excludes 2 patients who required additional surgery within the first 48 hours.
c) NA - not applicable
North America (overall)
146/183 (79.8%)
153/196 (78.1%)
(-7.4%, 9.3%)
Abscess
40/57 (70.2%)
49/63 (77.8%) b
NA c
Non-abscess
106/126 (84.1%)
104/133 (78.2%)
NA
International (overall)
199/246 (80.9%)
218/265 (82.3%)
(-8.9%, 4.2%)
Abscess
73/93 (78.5%)
86/99 (86.9%)
NA
Non-abscess
126/153 (82.4%)
132/166 (79.5%)
NA
-
15 REFERENCES
- Clinical and Laboratory Standards Institute (CLSI), Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically 9 th edition. Approved Standard CLSI Document M7-A9, CLSI, 950 West Valley Rd., Suite 2500, Wayne, PA 19087, 2012.
- CLSI, Performance Standards for Antimicrobial Susceptibility Testing 22 Informational Supplement. CLSI Document M100-S22, 2012.
- CLSI, Performance Standards for Antimicrobial Disk Susceptibility Tests 11 th edition. Approved Standard CLSI Document M2-A11, 2012.
- CLSI, Methods for Antimicrobial Susceptibility Testing of Anaerobic Bacteria 8 th edition ; Approved Standard CLSI Document M11-A8, 2012.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 Moxifloxacin Hydrochloride Tablets
Moxifloxacin Hydrochloride Tablets are available as modified capsule shaped, dull red film-coated tablets containing 400 mg moxifloxacin. The tablet is debossed with E-18 on one side and plain on the other side.
NDC: 50268-576-13 10 Tablets per card, 3 cards per carton.
Dispensed in Unit Dose Package. For Institutional Use Only.
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. Avoid high humidity. -
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Medication Guide
Antibacterial Resistance
Antibacterial drugs including moxifloxacin hydrochloride should only be used to treat bacterial infections. They do not treat viral infections (for example, the common cold). When moxifloxacin hydrochloride is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by moxifloxacin hydrochloride or other antibacterial drugs in the future.
Administration With Food, Fluids, and Drug Products Containing Multivalent Cations
Patients should be informed that moxifloxacin hydrochloride tablets may be taken with or without food. Patients should be advised to drink fluids liberally.
Moxifloxacin hydrochloride tablets should be taken at least 4 hours before or 8 hours after multivitamins (containing iron or zinc), antacids (containing magnesium or aluminum), sucralfate, or VIDEX ® (didanosine) chewable/buffered tablets or the pediatric powder for oral solution.
Serious and Potentially Serious Adverse Reactions
To assure safe and effective use of moxifloxacin hydrochloride, patients should be informed of the following serious adverse reactions that have been associated with moxifloxacin hydrochloride and other fluoroquinolone use:- Tendon Disorders: Patients should contact their healthcare provider if they experience pain, swelling, or inflammation of a tendon, or weakness or inability to use one of their joints; rest and refrain from exercise; and discontinue moxifloxacin hydrochloride treatment. The risk of severe tendon disorder with fluoroquinolones is higher in older patients usually over 60 years of age, in patients taking corticosteroid drugs, and in patients with kidney, heart or lung transplants.
- Exacerbation of Myasthenia Gravis: Fluoroquinolones like moxifloxacin hydrochloride may cause worsening of myasthenia gravis symptoms, including muscle weakness and breathing problems. Patients should call their healthcare provider right away if they have any worsening muscle weakness or breathing problems.
- Prolongation of the QT interval: Moxifloxacin hydrochloride may produce changes in the electrocardiogram (QTc interval prolongation). Moxifloxacin hydrochloride should be avoided in patients receiving Class IA (for example quinidine, procainamide) or Class III (for example amiodarone, sotalol) antiarrhythmic agents. Moxifloxacin hydrochloride may add to the QTc prolonging effects of other drugs such as cisapride, erythromycin, antipsychotics, and tricyclic antidepressants. The patients should inform their physician of any personal or family history of QTc prolongation or proarrhythmic conditions such as recent hypokalemia, significant bradycardia, and acute myocardial ischemia. Patients should contact their physician if they experience palpitations or fainting spells while taking moxifloxacin hydrochloride.
- Hypersensitivity Reactions: Patients should be advised that moxifloxacin hydrochloride may be associated with hypersensitivity reactions, including anaphylactic reactions, even following a single dose. Patients should discontinue moxifloxacin hydrochloride at the first sign of a skin rash or other signs of an allergic reaction.
- Convulsions: Convulsions have been reported in patients receiving quinolones, and they should notify their physician before taking moxifloxacin hydrochloride if there is a history of this condition. Patients should also inform their physician if they are taking NSAIDs concurrently with moxifloxacin hydrochloride.
- Neurologic Adverse Effects (for example, dizziness, lightheadedness): Moxifloxacin hydrochloride may cause dizziness, lightheadedness, and vision disorders; therefore, patients should know how they react to this drug before they operate an automobile or machinery or engage in activities requiring mental alertness or coordination.
- Psychotic Reaction: Psychotic reactions sometimes resulting in self-injurious behavior have been reported in patients receiving quinolones. Patients should notify their physician if they have a history of psychiatric illness before taking moxifloxacin hydrochloride.
- Peripheral Neuropathies: Patients should be informed that peripheral neuropathy has been associated with moxifloxacin hydrochloride use. Symptoms may occur soon after initiation of therapy and may be irreversible. If symptoms of peripheral neuropathy including pain, burning, tingling, numbness, and/or weakness develop, patients should immediately discontinue moxifloxacin hydrochloride and contact their physician.
- Blood Glucose Disturbances: Inform the patients that if they are diabetic and are being treated with insulin or an oral hypoglycemic agent and a hypoglycemic reaction occurs, they should discontinue moxifloxacin hydrochloride and consult a physician.
- Photosensitivity/Phototoxicity: Patients should be informed that photosensitivity/ phototoxicity has been reported in patients receiving quinolones. Patients should minimize or avoid exposure to natural or artificial sunlight (tanning beds or UVA/B treatment) while taking quinolones. If patients need to be outdoors while using quinolones, they should wear loose-fitting clothes that protect skin from sun exposure and discuss other sun protection measures with their physician. If a sunburn-like reaction or skin eruption occurs, patients should contact their physician .
- Diarrhea: Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Manufactured for:
AvKARE, Inc.
Pulaski, TN 38478
Mfg. Rev. 08/15
AV 07/16 (P)
AvPAK -
FDA-Approved Medication Guide
MEDICATION GUIDE
Moxifloxacin Hydrochloride Tablets
(mox'' i flox' a sin hye'' droe klor' ide)
Rx only
Read the Medication Guide that comes with moxifloxacin hydrochloride tablets before you start taking them and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about moxifloxacin hydrochloride tablets?
Moxifloxacin hydrochloride tablets belong to a class of antibiotics called fluoroquinolones. Moxifloxacin hydrochloride tablets can cause side effects that may be serious or even cause death. If you get any of the following serious side effects, get medical help right away. Talk with your healthcare provider about whether you should continue to take moxifloxacin hydrochloride tablets.
1. Tendon rupture or swelling of the tendon (tendinitis).
- Tendon problems can happen in people of all ages who take moxifloxacin hydrochloride tablets. Tendons are tough cords of tissue that connect muscles to bones. Symptoms of tendon problems may include:
- Pain, swelling, tears and inflammation of tendons including the back of the ankle (Achilles), shoulder, hand, or other tendon sites.
-
The risk of getting tendon problems while you take moxifloxacin hydrochloride tablets is higher if you:
- Are over 60 years of age
- Are taking steroids (corticosteroids)
- Have had a kidney, heart or lung transplant
Tendon problems can happen in people who do not have the above risk factors when they take moxifloxacin hydrochloride tablets.
- Other reasons that can increase your risk of tendon problems can include:
- Physical activity or exercise
- Kidney failure
- Tendon problems in the past, such as in people with rheumatoid arthritis (RA).
- Call your healthcare provider right away at the first sign of tendon pain, swelling or inflammation. Stop taking moxifloxacin hydrochloride tablets until tendinitis or tendon rupture has been ruled out by your healthcare provider. Avoid exercise and using the affected area. The most common area of pain and swelling is in the Achilles tendon at the back of your ankle. This can also happen with other tendons.
- Talk to your healthcare provider about the risk of tendon rupture with continued use of moxifloxacin hydrochloride tablets. You may need a different antibiotic that is not a fluoroquinolone to treat your infection.
- Tendon rupture can happen while you are taking or after you have finished taking moxifloxacin hydrochloride tablets. Tendon ruptures have happened up to several months after patients have finished taking their fluoroquinolone.
-
Get medical help right away if you get any of the following signs or symptoms of a tendon rupture:
- Hear or feel a snap or pop in a tendon area
- Bruising right after an injury in a tendon area
- Unable to move the affected area or bear weight.
2. Worsening of myasthenia gravis (a disease which causes muscle weakness).
Fluoroquinolones like moxifloxacin hydrochloride tablets may cause worsening of myasthenia gravis symptoms, including muscle weakness and breathing problems. Call your healthcare provider right away if you have any worsening muscle weakness or breathing problems.
See the section “What are the possible side effects of moxifloxacin hydrochloride tablets?” for more information about side effects.
What are moxifloxacin hydrochloride tablets?
Moxifloxacin hydrochloride tablets are a fluoroquinolone antibiotic medicine used to treat certain types of infections caused by certain germs called bacteria in adults 18 years or older. It is not known if moxifloxacin hydrochloride tablets are safe and work in people under 18 years of age. Children have a higher chance of getting bone, joint, and tendon (musculoskeletal) problems while taking fluoroquinolone antibiotic medicines.
Sometimes infections are caused by viruses rather than by bacteria. Examples include viral infections in the sinuses and lungs, such as the common cold or flu. Antibiotics, including moxifloxacin hydrochloride tablets, do not kill viruses.
Call your healthcare provider if you think your condition is not getting better while you are taking moxifloxacin hydrochloride tablets.
Who should not take moxifloxacin hydrochloride tablets?
Do not take moxifloxacin hydrochloride tablets if you have ever had a severe allergic reaction to an antibiotic known as a fluoroquinolone, or if you are allergic to any of the ingredients in moxifloxacin hydrochloride tablets. Ask your healthcare provider if you are not sure. See the list of ingredients in moxifloxacin hydrochloride tablets at the end of this Medication Guide.
What should I tell my healthcare provider before taking moxifloxacin hydrochloride tablets?
See “What is the most important information I should know about moxifloxacin hydrochloride tablets?”
Tell your healthcare provider about all your medical conditions, including if you:
- Have tendon problems
- Have a disease that causes muscle weakness (myasthenia gravis)
- Have central nervous system problems (such as epilepsy)
- Have nerve problems
- Have or anyone in your family has an irregular heartbeat, especially a condition called “QT prolongation”
- Have low blood potassium (hypokalemia)
- Have a slow heartbeat (bradycardia)
- Have a history of seizures
- Have kidney problems
- Have rheumatoid arthritis (RA) or other history of joint problems
- Are pregnant or planning to become pregnant. It is not known if moxifloxacin hydrochloride tablets will harm your unborn child
- Are breast-feeding or planning to breast-feed. It is not known if moxifloxacin hydrochloride passes into breast milk. You and your healthcare provider should decide whether you will take moxifloxacin hydrochloride tablets or breast-feed.
- Have diabetes or problems with low blood sugar (hypoglycemia)
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, herbal, and dietary supplements. Moxifloxacin hydrochloride tablets and other medicines can affect each other causing side effects. Especially tell your healthcare provider if you take:
- An NSAID (Non-Steroidal Anti-Inflammatory Drug). Many common medicines for pain relief are NSAIDs. Taking an NSAID while you take moxifloxacin hydrochloride tablets or other fluoroquinolones may increase your risk of central nervous system effects and seizures. See “What are the possible side effects of moxifloxacin hydrochloride tablets?”
- A blood thinner (warfarin, Coumadin, Jantoven).
- A medicine to control your heart rate or rhythm (antiarrhythmic). See “What are the possible side effects of moxifloxacin hydrochloride tablets?”
- An anti-psychotic medicine.
- A tricyclic antidepressant.
- An oral anti-diabetes medicine or insulin.
- Erythromycin.
- A water pill (diuretic).
- A steroid medicine. Corticosteroids taken by mouth or by injection may increase the chance of tendon injury. See “What is the most important information I should know about moxifloxacin hydrochloride tablets?”
- Certain medicines may keep moxifloxacin hydrochloride tablets from working correctly. Take moxifloxacin hydrochloride tablets either 4 hours before or 8 hours after taking these products:
- An antacid, multivitamin, or other product that has magnesium, aluminum, iron, or zinc
- Sucralfate (Carafate ®)
- Didanosine (Videx ®, Videx EC ®)
Ask your healthcare provider if you are not sure if any of your medicines are listed above.
Know the medicines you take. Keep a list of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I take moxifloxacin hydrochloride tablets?
- Take moxifloxacin hydrochloride tablets once a day exactly as prescribed by your healthcare provider.
- Take moxifloxacin hydrochloride tablets at about the same time each day.
- Moxifloxacin hydrochloride tablets should be swallowed.
- Moxifloxacin hydrochloride tablets can be taken with or without food.
- Drink plenty of fluids while taking moxifloxacin hydrochloride tablets.
- Do not skip any doses, or stop taking moxifloxacin hydrochloride tablets even if you begin to feel better, until you finish your prescribed treatment, unless:
- You have tendon effects (see “What is the most important information I should know about moxifloxacin hydrochloride tablets?”).
- You have a serious allergic reaction (see “What are the possible side effects of moxifloxacin hydrochloride tablets?”), or your healthcare provider tells you to stop.
- This will help make sure that all of the bacteria are killed and lower the chance that the bacteria will become resistant to moxifloxacin hydrochloride tablets. If this happens, moxifloxacin hydrochloride tablets and other antibiotic medicines may not work in the future.
- If you miss a dose of moxifloxacin hydrochloride tablets, take it as soon as you remember. Do not take more than 1 dose of moxifloxacin hydrochloride tablets in one day.
- If you take too much, call your healthcare provider or get medical help immediately.
What should I avoid while taking moxifloxacin hydrochloride tablets?
- Moxifloxacin hydrochloride tablets can make you feel dizzy and lightheaded. Do not drive, operate machinery, or do other activities that require mental alertness or coordination until you know how moxifloxacin hydrochloride tablets affect you.
- Avoid sunlamps, tanning beds, and try to limit your time in the sun. Moxifloxacin hydrochloride tablets can make your skin sensitive to the sun (photosensitivity) and the light from sunlamps and tanning beds. You could get severe sunburn, blisters or swelling of your skin. If you get any of these symptoms while taking moxifloxacin hydrochloride tablets, call your healthcare provider right away. You should use a sunscreen and wear a hat and clothes that cover your skin if you have to be in sunlight.
What are the possible side effects of moxifloxacin hydrochloride tablets?
Moxifloxacin hydrochloride tablets can cause side effects that may be serious or even cause death. See “What is the most important information I should know about moxifloxacin hydrochloride tablets?”
Other serious side effects of moxifloxacin hydrochloride tablets include:
- Central Nervous System effects
Seizures have been reported in people who take fluoroquinolone antibiotics including moxifloxacin hydrochloride tablets. Tell your healthcare provider if you have a history of seizures. Ask your healthcare provider whether taking moxifloxacin hydrochloride tablets will change your risk of having a seizure.
Central Nervous System (CNS) side effects may happen as soon as after taking the first dose of moxifloxacin hydrochloride tablets. Talk to your healthcare provider right away if you have any of these side effects, or other changes in mood or behavior:
- Feeling dizzy
- Seizures
- Hear voices, see things, or sense things that are not there (hallucinations)
- Feel restless
- Tremors
- Feel anxious or nervous
- Confusion
- Depression
- Trouble sleeping
- Feel more suspicious (paranoia)
- Suicidal thoughts or acts
- Nightmares
- Vision Loss
- Serious allergic reactions
Allergic reactions can happen in people taking fluoroquinolones, including moxifloxacin hydrochloride tablets, even after only one dose. Stop taking moxifloxacin hydrochloride tablets and get emergency medical help right away if you get any of the following symptoms of a severe allergic reaction:
- Hives
- Trouble breathing or swallowing
- Swelling of the lips, tongue, face
- Throat tightness, hoarseness
- Rapid heartbeat
- Faint
- Yellowing of the skin or eyes. Stop taking moxifloxacin hydrochloride tablets and tell your healthcare provider right away if you get yellowing of your skin or white part of your eyes, or if you have dark urine. These can be signs of a serious reaction to moxifloxacin hydrochloride tablets (a liver problem).
- Skin rash
Skin rash may happen in people taking moxifloxacin hydrochloride tablets even after only one dose. Stop taking moxifloxacin hydrochloride tablets at the first sign of a skin rash and call your healthcare provider. Skin rash may be a sign of a more serious reaction to moxifloxacin hydrochloride tablets.
- Serious heart rhythm changes (QT prolongation and torsade de pointes)
Tell your healthcare provider right away if you have a change in your heart beat (a fast or irregular heartbeat), or if you faint. Moxifloxacin hydrochloride tablets may cause a rare heart problem known as prolongation of the QT interval. This condition can cause an abnormal heartbeat and can be very dangerous. The chances of this event are higher in people:
- Who are elderly
- With a family history of prolonged QT interval
- With low blood potassium (hypokalemia)
- Who take certain medicines to control heart rhythm (antiarrhythmics)
- Intestine infection (Pseudomembranous colitis)
Pseudomembranous colitis can happen with most antibiotics, including moxifloxacin hydrochloride tablets. Call your healthcare provider right away if you get watery diarrhea, diarrhea that does not go away, or bloody stools. You may have stomach cramps and a fever. Pseudomembranous colitis can happen 2 or more months after you have finished your antibiotic.
- Changes in sensation and nerve damage (Peripheral Neuropathy)
Damage to the nerves in arms, hands, legs, or feet can happen in people taking fluoroquinolones, including moxifloxacin hydrochloride tablets. Stop moxifloxacin and talk with your healthcare provider right away if you get any of the following symptoms of peripheral neuropathy in your arms, hands, legs, or feet:
- Pain
- Burning
- Tingling
- Numbness
- Weakness
The nerve damage may be permanent.
- Changes in blood sugar
People who take moxifloxacin hydrochloride tablets and other fluoroquinolone medicines with oral anti-diabetes medicines or with insulin can get low blood sugar (hypoglycemia) and high blood sugar (hyperglycemia). Follow your healthcare provider's instructions for how often to check your blood sugar. If you have diabetes and you get low blood sugar while taking moxifloxacin hydrochloride tablets, stop taking moxifloxacin hydrochloride tablets and call your healthcare provider right away. Your antibiotic medicine may need to be changed.
- Sensitivity to sunlight (photosensitivity)
See “What should I avoid while taking moxifloxacin hydrochloride tablets?” The most common side effects of moxifloxacin hydrochloride tablets include nausea and diarrhea.
These are not all the possible side effects of moxifloxacin hydrochloride tablets. Tell your healthcare provider about any side effect that bothers you or that does not go away. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store moxifloxacin hydrochloride tablets?
- Store moxifloxacin hydrochloride tablets at 20° to 25°C (68° to 77°F).
- Keep moxifloxacin hydrochloride tablets away from moisture (humidity).
Keep moxifloxacin hydrochloride tablets and all medicines out of the reach of children.
General information about moxifloxacin hydrochloride tablets
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use moxifloxacin hydrochloride tablets for a condition for which it is not prescribed. Do not give moxifloxacin hydrochloride tablets to other people, even if they have the same symptoms that you have. They may harm them.
This Medication Guide summarizes the most important information about moxifloxacin hydrochloride tablets. If you would like more information about moxifloxacin hydrochloride tablets, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about moxifloxacin hydrochloride tablets that is written for healthcare professionals. For more information call AvKARE, Inc. at 1-855-361-3993..
What are the ingredients in moxifloxacin hydrochloride tablets?
- Active ingredient: moxifloxacin hydrochloride
- Inactive ingredients: hypromellose, iron oxide red, magnesium stearate, microcrystalline cellulose, polyethylene glycol, povidone, sodium starch glycolate, and titanium dioxide.
All brands listed are the trademarks of their respective owners and are not trademarks of AvKARE, Inc.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured for:
AvKARE, Inc.
Pulaski, TN 38478
Mfg. Rev. 08/15
AV 07/16 (P)
AvPAK -
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC 50268-576-13
Moxifloxacin Hydrochloride Tablets
400 mg*
30 Tablets (3 X 10) Unit Dose
5026857613
NDC 50268-576-13
Moxifloxacin Hydrochloride Tablets
400 mg*
30 Tablets (3 X 10) Unit Dose
5026857613
PHARMACIST: Dispense the Medication Guide provided separately to each patient.
* Each film-coated tablet contains:
Moxifloxacin hydrochloride USP equivalent to moxifloxacin 400 mg.
Usual Dosage: See accompanying literature for complete information on dosage and administration.Store at 20° to 25°C (68° to 77°F). [see USP Controlled Room Temperature]. Avoid high humidity.
Manufactured for:
AvKARE, Inc.
Pulaski, TN 38478AvPAK
A PRODUCT OF AvKARE
Mfg. Rev. 08/15 AV 07/16 (P)
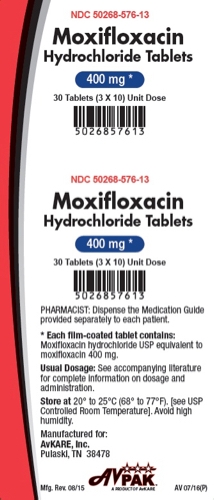
-
INGREDIENTS AND APPEARANCE
MOXIFLOXACIN HYDROCHLORIDE
moxifloxacin hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50268-576(NDC:65862-603) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MOXIFLOXACIN HYDROCHLORIDE (UNII: C53598599T) (MOXIFLOXACIN - UNII:U188XYD42P) MOXIFLOXACIN 400 mg Inactive Ingredients Ingredient Name Strength HYPROMELLOSE 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) FERRIC OXIDE RED (UNII: 1K09F3G675) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL 4000 (UNII: 4R4HFI6D95) POVIDONE K30 (UNII: U725QWY32X) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color red (Dull Red) Score no score Shape CAPSULE (Modified Capsule Shaped) Size 17mm Flavor Imprint Code E;18 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50268-576-13 30 in 1 BOX, UNIT-DOSE 07/22/2016 1 NDC: 50268-576-11 1 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA202632 07/22/2016 Labeler - AvPAK (832926666)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.