EPRONTIA- topiramate solution
Eprontia by
Drug Labeling and Warnings
Eprontia by is a Prescription medication manufactured, distributed, or labeled by Praxis, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to topiramate during pregnancy. Patients should be encouraged to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant. This registry is collecting information about the safety of antiepileptic drugs during pregnancy. To enroll, patients can call the toll-free number 1-888-233-2334. Information about the North American Drug Pregnancy Registry can be found at http://www.aedpregnancyregistry.org/.
Risk Summary
Topiramate can cause fetal harm when administered to a pregnant woman. Data from pregnancy registries indicate that infants exposed to topiramate in uterohave an increased risk of major congenital malformations, including but not limited to cleft lip and/or cleft palate (oral clefts), and of being small for gestational age (SGA) [see Human Data] . SGA has been observed at all doses and appears to be dose-dependent. The prevalence of SGA is greater in infants of women who received higher doses of topiramate during pregnancy. In addition, the prevalence of SGA in infants of women who continued topiramate use until later in pregnancy is higher compared to the prevalence in infants of women who stopped topiramate use before the third trimester.
In multiple animal species, topiramate produced developmental toxicity, including increased incidences of fetal malformations, in the absence of maternal toxicity at clinically relevant doses [see Animal Data] .
All pregnancies have a background risk of birth defects, loss, or other adverse outcomes. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risks of major birth defects and miscarriage in clinically recognized pregnancies are 2-4% and 15-20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Consider the benefits and risks of topiramate when prescribing this drug to women of childbearing potential, particularly when topiramate is considered for a condition not usually associated with permanent injury or death. Because of the risk of oral clefts to the fetus, which occur in the first trimester of pregnancy, all women of childbearing potential should be informed of the potential risk to the fetus from exposure to topiramate. Women who are planning a pregnancy should be counseled regarding the relative risks and benefits of topiramate use during pregnancy, and alternative therapeutic options should be considered for these patients.
Labor or Delivery
Although the effect of topiramate on labor and delivery in humans has not been established, the development of topiramate-induced metabolic acidosis in the mother and/or in the fetus might affect the fetus' ability to tolerate labor.
Topiramate treatment can cause metabolic acidosis [see Warnings and Precautions ( 5.4)] . The effect of topiramate-induced metabolic acidosis has not been studied in pregnancy; however, metabolic acidosis in pregnancy (due to other causes) can cause decreased fetal growth, decreased fetal oxygenation, and fetal death, and may affect the fetus' ability to tolerate labor. Pregnant patients should be monitored for metabolic acidosis and treated as in the nonpregnant state [see Warnings and Precautions ( 5.4)] . Newborns of mothers treated with topiramate should be monitored for metabolic acidosis because of transfer of topiramate to the fetus and possible occurrence of transient metabolic acidosis following birth.
Based on limited information, topiramate has also been associated with pre-term labor and premature delivery.
Data
Human Data
Data from pregnancy registries indicate an increased risk of major congenital malformations, including but not limited to oral clefts in infants exposed to topiramate during the first trimester of pregnancy. Other than oral clefts, no specific pattern of major congenital malformations or grouping of major congenital malformation types were observed. In the NAAED pregnancy registry, when topiramate-exposed infants with only oral clefts were excluded, the prevalence of major congenital malformations (4.1%) was higher than that in infants exposed to a reference AED (1.8%) or in infants with mothers without epilepsy and without exposure to AEDs (1.1%). The prevalence of oral clefts among topiramate-exposed infants (1.4%) was higher than the prevalence in infants exposed to a reference AED (0.3%) or the prevalence in infants with mothers without epilepsy and without exposure to AEDs (0.11%). It was also higher than the background prevalence in United States (0.17%) as estimated by the Centers for Disease Control and Prevention (CDC). The relative risk of oral clefts in topiramate-exposed pregnancies in the NAAED Pregnancy Registry was 12.5 (95% Confidence Interval [CI] 5.9 – 26.37) as compared to the risk in a background population of untreated women. The UK Epilepsy and Pregnancy Register reported a prevalence of oral clefts among infants exposed to topiramate monotherapy (3.2%) that was 16 times higher than the background rate in the UK (0.2%).
Data from the NAAED pregnancy registry and a population-based birth registry cohort indicate that exposure to topiramate in uterois associated with an increased risk of SGA newborns (birth weight <10th percentile). In the NAAED pregnancy registry, 19.7% of topiramate-exposed newborns were SGA compared to 7.9% of newborns exposed to a reference AED and 5.4% of newborns of mothers without epilepsy and without AED exposure. In the Medical Birth Registry of Norway (MBRN), a population-based pregnancy registry, 25% of newborns in the topiramate monotherapy exposure group were SGA compared to 9 % in the comparison group unexposed to AEDs. The long-term consequences of the SGA findings are not known.
Animal Data
When topiramate (0, 20, 100, or 500 mg/kg/day) was administered to pregnant mice during the period of organogenesis, incidences of fetal malformations (primarily craniofacial defects) were increased at all doses. Fetal body weights and skeletal ossification were reduced at the highest dose tested in conjunction with decreased maternal body weight gain. A no-effect dose for embryofetal developmental toxicity in mice was not identified. The lowest dose tested, which was associated with increased malformations, is less than the maximum recommended human dose (MRHD) for epilepsy (400 mg/day) or migraine (100 mg/day) on a body surface area (mg/m 2) basis.
In pregnant rats administered topiramate (0, 20, 100, and 500 mg/kg/day or 0, 0.2, 2.5, 30, and 400 mg/kg/day) orally during the period of organogenesis, the frequency of limb malformations (ectrodactyly, micromelia, and amelia) was increased in fetuses at 400 and 500 mg/kg/day. Embryotoxicity (reduced fetal body weights, increased incidences of structural variations) was observed at doses as low as 20 mg/kg/day. Clinical signs of maternal toxicity were seen at 400 mg/kg/day and above, and maternal body weight gain was reduced at doses of 100 mg/kg/day or greater. The no-effect dose (2.5 mg/kg/day) for embryofetal developmental toxicity in rats is less than the MRHD for epilepsy or migraine on a mg/m 2basis.
In pregnant rabbits administered topiramate (0, 20, 60, and 180 mg/kg/day or 0, 10, 35, and 120 mg/kg/day) orally during organogenesis, embryofetal mortality was increased at 35 mg/kg/day, and increased incidences of fetal malformations (primarily rib and vertebral malformations) were observed at 120 mg/kg/day. Evidence of maternal toxicity (decreased body weight gain, clinical signs, and/or mortality) was seen at 35 mg/kg/day and above. The no-effect dose (20 mg/kg/day) for embryofetal developmental toxicity in rabbits is equivalent to the MRHD for epilepsy and approximately 4 times the MRHD for migraine on a mg/m 2basis.
When topiramate (0, 0.2, 4, 20, and 100 mg/kg/day or 0, 2, 20, and 200 mg/kg/day) was administered orally to female rats during the latter part of gestation and throughout lactation, offspring exhibited decreased viability and delayed physical development at 200 mg/kg/day and reductions in pre- and/or postweaning body weight gain at 2 mg/kg/day and above. Maternal toxicity (decreased body weight gain, clinical signs) was evident at 100 mg/kg/day or greater. In a rat embryofetal development study which included postnatal assessment of offspring, oral administration of topiramate (0, 0.2, 2.5, 30, and 400 mg/kg) to pregnant animals during the period of organogenesis resulted in delayed physical development in offspring at 400 mg/kg/day and persistent reductions in body weight gain in offspring at 30 mg/kg/day and higher. The no-effect dose (0.2 mg/kg/day) for pre- and postnatal developmental toxicity in rats is less than the MRHD for epilepsy or migraine on a mg/m 2basis.
8.2 Lactation
Risk Summary
Topiramate is excreted in human milk [ see Data] . The effects of topiramate on milk production are unknown. Diarrhea and somnolence have been reported in breastfed infants whose mothers receive topiramate treatment. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for topiramate and any potential adverse effects on the breastfed infant from topiramate or from the underlying maternal condition.
8.4 Pediatric Use
Adjunctive Treatment for Epilepsy
Pediatric Patients 2 Years of Age and Older
The safety and effectiveness of EPRONTIA as adjunctive therapy for the treatment of partial-onset seizures, primary generalized tonic-clonic seizures, or seizures associated with Lennox-Gastaut syndrome have been established in pediatric patients 2 years of age and older [see Adverse Reactions ( 6.1) and Clinical Studies ( 14.2)] .
Pediatric Patients Below the Age of 2 YearsSafety and effectiveness in patients below the age of 2 years have not been established for the adjunctive therapy treatment of partial-onset seizures, primary generalized tonic-clonic seizures, or seizures associated with Lennox-Gastaut syndrome. In a single randomized, double-blind, placebo-controlled investigational trial, the efficacy, safety, and tolerability of topiramate oral liquid and sprinkle formulations as an adjunct to concurrent antiepileptic drug therapy in pediatric patients 1 to 24 months of age with refractory partial-onset seizures were assessed. After 20 days of double-blind treatment, topiramate (at fixed doses of 5, 15, and 25 mg/kg/day) did not demonstrate efficacy compared with placebo in controlling seizures.
In general, the adverse reaction profile for topiramate in this population was similar to that of older pediatric patients, although results from the above controlled study and an open-label, long-term extension study in these pediatric patients 1 to 24 months old suggested some adverse reactions/toxicities (not previously observed in older pediatric patients and adults; i.e., growth/length retardation, certain clinical laboratory abnormalities, and other adverse reactions/toxicities that occurred with a greater frequency and/or greater severity than had been recognized previously from studies in older pediatric patients or adults for various indications).
These very young pediatric patients appeared to experience an increased risk for infections (any topiramate dose 12%, placebo 0%) and of respiratory disorders (any topiramate dose 40%, placebo 16%). The following adverse reactions were observed in at least 3% of patients on topiramate and were 3% to 7% more frequent than in patients on placebo: viral infection, bronchitis, pharyngitis, rhinitis, otitis media, upper respiratory infection, cough, and bronchospasm. A generally similar profile was observed in older pediatric patients [see Adverse Reactions ( 6)] .
Topiramate resulted in an increased incidence of patients with increased creatinine (any topiramate dose 5%, placebo 0%), BUN (any topiramate dose 3%, placebo 0%), and protein (any topiramate dose 34%, placebo 6%), and an increased incidence of decreased potassium (any topiramate dose 7%, placebo 0%). This increased frequency of abnormal values was not dose-related. Creatinine was the only analyte showing a noteworthy increased incidence (topiramate 25 mg/kg/day 5%, placebo 0%) of a markedly abnormal increase. The significance of these findings is uncertain.
Topiramate treatment also produced a dose-related increase in the percentage of patients who had a shift from normal at baseline to high/increased (above the normal reference range) in total eosinophil count at the end of treatment. The incidence of these abnormal shifts was 6 % for placebo, 10% for 5 mg/kg/day, 9% for 15 mg/kg/day, 14% for 25 mg/kg/day, and 11% for any topiramate dose. There was a mean dose-related increase in alkaline phosphatase. The significance of these findings is uncertain.
Topiramate produced a dose-related increased incidence of hyperammonemia [see Warnings and Precautions (5.12)].
Treatment with topiramate for up to 1 year was associated with reductions in Z SCORES for length, weight, and head circumference [see Warnings and Precautions ( 5.4), Adverse Reactions ( 6)] .
In open-label, uncontrolled experience, increasing impairment of adaptive behavior was documented in behavioral testing over time in this population. There was a suggestion that this effect was dose-related. However, because of the absence of an appropriate control group, it is not known if this decrement in function was treatment-related or reflects the patient's underlying disease (e.g., patients who received higher doses may have more severe underlying disease) [see Warnings and Precautions ( 5.6)] .
In this open-label, uncontrolled study, the mortality was 37 deaths/1000 patient years. It is not possible to know whether this mortality rate is related to topiramate treatment, because the background mortality rate for a similar, significantly refractory, young pediatric population (1-24 months) with partial epilepsy is not known.
Monotherapy Treatment for Epilepsy
Pediatric Patients 2 Years of Age and Older
The safety and effectiveness of EPRONTIA as monotherapy for the treatment of partial-onset seizures or primary generalized tonic-clonic seizures have been established in pediatric patients aged 2 years and older [see Clinical Trials Experience ( 6.1), Clinical Studies ( 14.1)] .
A one-year, active-controlled, open-label study with blinded assessments of bone mineral density (BMD) and growth in pediatric patients 4 to 15 years of age, including 63 patients with recent or new onset of epilepsy, was conducted to assess effects of topiramate (N=28, 6-15 years of age) versus levetiracetam (N=35, 4-15 years of age) monotherapy on bone mineralization and on height and weight, which reflect growth. Effects on bone mineralization were evaluated via dual-energy X-ray absorptiometry and blood markers. Table 10summarizes effects of topiramate at 12 months for key safety outcomes including BMD, height, height velocity, and weight. All Least Square Mean values for topiramate and the comparator were positive. Therefore, the Least Square Mean treatment differences shown reflect a topiramate-induced attenuation of the key safety outcomes. Statistically significant effects were observed for decreases in BMD (and bone mineral content) in lumbar spine and total body less head and in weight. Subgroup analyses according to age demonstrated similar negative effects for all key safety outcomes (i.e., BMD, height, weight).
Table 10: Summary of Topiramate Treatment Difference Results at 12 Months for Key Safety Outcomes - * TBLH=total body less head
- † Whereas no patients were randomized to 2-5 year age subgroup for topiramate, 5 patients (4-5 years) were randomized to the active control group.
Safety Parameter
Treatment Difference in Least Square Means (95 % Confidence Interval)
Annual Change in BMD Lumbar Spine (g/cm 2)
-0.036 (-0.058, -0.014)
Annual Change in BMD TBLH *(g/cm 2)
-0.026 (-0.039, -0.012)
Annual Change in Height (cm) (4-9 years, Primary Analysis Population for Height) †
-0.84 (-2.67, 0.99)
Annual Change in Height (cm) (4-15 years)
-0.75 (-2.21, 0.71)
Annual Change in Height (cm) (10-15 years)
-1.01 (-3.64, 1.61)
Height Velocity (cm/year) (4-9 years)
-1.00 (-2.76, 0.76)
Height Velocity (cm/year) (4-15 years)
-0.98 (-2.33, 0.37)
Height Velocity (cm/year) (10-15 years)
-0.96 (-3.24, 1.32)
Annual Change in Weight (kg)
-2.05 (-3.66, -0.45)
Metabolic acidosis (serum bicarbonate < 20 mEq/L) was observed in all topiramate-treated patients at some time in the study [see Warnings and Precautions ( 5.4)] . Over the whole study, 76% more topiramate-treated patients experienced persistent metabolic acidosis (i.e. 2 consecutive visits with or final serum bicarbonate < 20 mEq/L) compared to levetiracetam-treated patients. Over the whole study, 35% more topiramate-treated patients experienced a markedly abnormally low serum bicarbonate (i.e., absolute value < 17 mEq/L and ≥ 5 mEq/L decrease from pre-treatment), indicating the frequency of more severe metabolic acidosis, compared to levetiracetam-treated patients. The decrease in BMD at 12 months was correlated with decreased serum bicarbonate, suggesting that metabolic acidosis was at least a partial factor contributing to this adverse effect on BMD.
Topiramate-treated patients exhibited an increased risk for developing an increased serum creatinine and an increased serum glucose above the normal reference range compared to control patients.
Pediatric Patients Below the Age of 2 Years
Safety and effectiveness in patients below the age of 2 years have not been established for the monotherapy treatment of epilepsy.Preventive Treatment of Migraine
Pediatric Patients 12 to 17 Years of Age
Safety and effectiveness of topiramate for the preventive treatment of migraine was studied in 5 double-blind, randomized, placebo-controlled, parallel-group trials in a total of 219 pediatric patients, at doses of 50 to 200 mg/day, or 2 to 3 mg/kg/day. These comprised a fixed dose study in 103 pediatric patients 12 to 17 years of age [see Clinical Studies ( 14.3)] , a flexible dose (2 to 3 mg/kg/day), placebo-controlled study in 157 pediatric patients 6 to 16 years of age (including 67 pediatric patients 12 to 16 years of age), and a total of 49 pediatric patients 12 to 17 years of age in 3 studies for the preventive treatment of migraine primarily in adults. Open-label extension phases of 3 studies enabled evaluation of long-term safety for up to 6 months after the end of the double-blind phase.
Efficacy of topiramate for the preventive treatment of migraine in pediatric patients 12 to 17 years of age is demonstrated for a 100 mg daily dose in Study 13 [see Clinical Studies ( 14.3)] . Efficacy of topiramate (2 to 3 mg/kg/day) for the preventive treatment of migraine was not demonstrated in a placebo-controlled trial of 157 pediatric patients (6 to 16 years of age) that included treatment of 67 pediatric patients (12 to 16 years of age) for 20 weeks.
In the pediatric trials (12 to 17 years of age) in which patients were randomized to placebo or a fixed daily dose of topiramate, the most common adverse reactions with topiramate that were seen at an incidence higher (≥5%) than in the placebo group were: paresthesia, upper respiratory tract infection, anorexia, and abdominal pain [see Adverse Reactions ( 6)] .
The most common cognitive adverse reaction in pooled double-blind studies in pediatric patients 12 to 17 years of age was difficulty with concentration/attention [see Warnings and Precautions ( 5.6)] .
Markedly abnormally low serum bicarbonate values indicative of metabolic acidosis were reported in topiramate-treated pediatric migraine patients [see Warnings and Precautions ( 5.4)] .
In topiramate-treated pediatric patients (12 to 17 years of age) compared to placebo-treated patients, abnormally increased results were more frequent for creatinine, BUN, uric acid, chloride, ammonia, total protein, and platelets. Abnormally decreased results were observed with topiramate vs placebo treatment for phosphorus and bicarbonate [see Clinical Trials Experience ( 6.1)] .
Notable changes (increases and decreases) from baseline in systolic blood pressure, diastolic blood pressure, and pulse were observed occurred more commonly in pediatric patients treated with topiramate compared to pediatric patients treated with placebo [see Clinical Pharmacology ( 12.2)] .
Pediatric Patients Below the Age of 12 Years
Safety and effectiveness in pediatric patients below the age of 12 years have not been established for the preventive treatment of migraine.
In a double-blind study in 90 pediatric patients 6 to 11 years of age (including 59 topiramate-treated and 31 placebo patients), the adverse reaction profile was generally similar to that seen in pooled double-blind studies of pediatric patients 12 to 17 years of age. The most common adverse reactions that occurred in topiramate -treated pediatric patients 6 to 11 years of age, and at least twice as frequently than placebo, were gastroenteritis (12% topiramate, 6% placebo), sinusitis (10% topiramate, 3% placebo), weight loss (8% topiramate, 3% placebo) and paresthesia (7% topiramate, 0% placebo). Difficulty with concentration/attention occurred in 3 topiramate-treated patients (5%) and 0 placebo-treated patients (0%).
The risk for cognitive adverse reaction was greater in younger patients (6 to 11 years of age) than in older patients (12 to 17 years of age) [see Warnings and Precautions ( 5.6)] .
Juvenile Animal Studies
When topiramate (0, 30, 90, and 300 mg/kg/day) was administered orally to rats during the juvenile period of development (postnatal days 12 to 50), bone growth plate thickness was reduced in males at the highest dose. The no-effect dose (90 mg/kg/day) for adverse developmental effects is approximately 2 times the maximum recommended pediatric dose (9 mg/kg/day) on a body surface area (mg/m 2) basis.
8.5 Geriatric Use
In clinical trials, 3% of patients were over age 60. No age-related differences in effectiveness or adverse effects were evident. However, clinical studies of topiramate did not include sufficient numbers of subjects age 65 and over to determine whether they respond differently than younger subjects. Dosage adjustment may be necessary for elderly with age-related renal impairment (creatinine clearance rate <70 mL/min/1.73 m 2) resulting in reduced clearance [see Dosage and Administration ( 2.5), Clinical Pharmacology ( 12.3)] .
8.6 Renal Impairment
The clearance of topiramate is reduced in patients with moderate (creatinine clearance 30 to 69 mL/min/1.73 m 2) and severe (creatinine clearance <30 mL/min/1.73 m 2) renal impairment. A dosage adjustment is recommended in patients with moderate or severe renal impairment [see Dosage and Administration ( 2.5), Clinical Pharmacology ( 12.3)] .
-
10 OVERDOSAGE
Overdoses of topiramate have been reported. Signs and symptoms included convulsions, drowsiness, speech disturbance, blurred vision, diplopia, impaired mentation, lethargy, abnormal coordination, stupor, hypotension, abdominal pain, agitation, dizziness and depression. The clinical consequences were not severe in most cases, but deaths have been reported after overdoses involving topiramate.
Topiramate overdose has resulted in severe metabolic acidosis [see Warnings and Precautions ( 5.4)] .
A patient who ingested a dose of topiramate between 96 and 110 g was admitted to a hospital with a coma lasting 20 to 24 hours followed by full recovery after 3 to 4 days.
In the event of overdose, EPRONTIA should be discontinued and general supportive treatment given until clinical toxicity has been diminished or resolved. Hemodialysis is an effective means of removing topiramate from the body.
-
11 DESCRIPTION
EPRONTIA (topiramate) oral solution is available as a 25 mg/mL solution for oral administration.
Topiramate has the molecular formula C 12H 21NO 8S and a molecular weight of 339.36. Topiramate is designated chemically as 2,3:4,5-Di- O-isopropylidene-β-D-fructopyranose sulfamate and has the following structural formula:
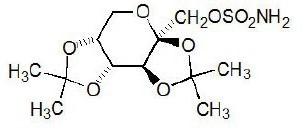
Topiramate is a white crystalline powder with a bitter taste. Topiramate is a sulfamate-substituted monosaccharide. Topiramate is most soluble in alkaline solutions containing sodium hydroxide or sodium phosphate and having a pH of 9 to 10. It is freely soluble in acetone, chloroform, dimethylsulfoxide, and ethanol. The solubility in water is 9.8 mg/mL. Its saturated solution has a pH of 6.3.
EPRONTIA oral solution is colorless to slightly yellow colored clear viscous liquid. EPRONTIA contains the following inactive ingredients: glycerin, methylparaben, mixed berry flavor, polyethylene glycol, propylparaben, and sucralose.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The precise mechanisms by which topiramate exerts its anticonvulsant and preventive migraine effects are unknown; however, preclinical studies have revealed four properties that may contribute to topiramate's efficacy for epilepsy and the preventive treatment of migraine. Electrophysiological and biochemical evidence suggests that topiramate, at pharmacologically relevant concentrations, blocks voltage-dependent sodium channels, augments the activity of the neurotransmitter gamma-aminobutyrate at some subtypes of the GABA-A receptor, antagonizes the AMPA/kainate subtype of the glutamate receptor, and inhibits the carbonic anhydrase enzyme, particularly isozymes II and IV.
12.2 Pharmacodynamics
Topiramate has anticonvulsant activity in rat and mouse maximal electroshock seizure (MES) tests. Topiramate is only weakly effective in blocking clonic seizures induced by the GABA A receptor antagonist, pentylenetetrazole. Topiramate is also effective in rodent models of epilepsy, which include tonic and absence-like seizures in the spontaneous epileptic rat (SER) and tonic and clonic seizures induced in rats by kindling of the amygdala or by global ischemia.
Changes (increases and decreases) from baseline in vital signs (systolic blood pressure-SBP, diastolic blood pressure-DBP, pulse) occurred more frequently in pediatric patients (6 to 17 years) treated with various daily doses of topiramate (50 mg, 100 mg, 200 mg, 2 to 3 mg/kg) than in patients treated with placebo in controlled trials for the preventive treatment of migraine. The most notable changes were SBP <90 mm Hg, DBP <50 mm Hg, SBP or DBP increases or decreases ≥20 mm Hg, and pulse increases or decreases ≥30 beats per minute. These changes were often dose-related and were most frequently associated with the greatest treatment difference at the 200 mg dose level. Systematic collection of orthostatic vital signs has not been conducted. The clinical significance of these various changes in vital signs has not been clearly established.
12.3 Pharmacokinetics
Peak topiramate plasma concentrations (C max) occurred at approximately 0.5 hour after oral administration of EPRONTIA in healthy male subjects under fasting conditions. Oral administration of EPRONTIA with a high-fat and high calorie meal did not affect topiramate AUC 0-tand AUC 0-∞, but lowered the C maxby 28% and delayed the T maxby 5 hours. Overall, the impact of food-intake on topiramate pharmacokinetics is not expected to be clinically significant, and therefore, EPRONTIA can be administered without regard to food.
The pharmacokinetics of topiramate are linear with dose proportional increases in plasma concentration over the dose range studied (200 to 800 mg/day). The mean plasma elimination half-life is 21 hours after single or multiple doses. Steady-state is thus reached in about 4 days in patients with normal renal function. Topiramate is 15% to 41% bound to human plasma proteins over the blood concentration range of 0.5 to 250 μg/mL. The fraction bound decreased as blood concentration increased.
Carbamazepine and phenytoin do not alter the binding of topiramate. Sodium valproate, at 500 μg/mL (a concentration 5 to 10 times higher than considered therapeutic for valproate) decreased the protein binding of topiramate from 23% to 13%. Topiramate does not influence the binding of sodium valproate.
Metabolism and Excretion
Topiramate is not extensively metabolized and is primarily eliminated unchanged in the urine (approximately 70% of an administered dose). Six metabolites have been identified in humans, none of which constitutes more than 5% of an administered dose. The metabolites are formed via hydroxylation, hydrolysis, and glucuronidation. There is evidence of renal tubular reabsorption of topiramate. In rats, given probenecid to inhibit tubular reabsorption, along with topiramate, a significant increase in renal clearance of topiramate was observed. This interaction has not been evaluated in humans. Overall, oral plasma clearance (CL/F) is approximately 20 to 30 mL/min in adults following oral administration.
Specific Populations
Renal Impairment
The clearance of topiramate was reduced by 42% in subjects with moderate renal impairment (creatinine clearance 30 to 69 mL/min/1.73 m 2) and by 54% in subjects with severe renal impairment (creatinine clearance <30 mL/min/1.73 m 2) compared to subjects with normal renal function (creatinine clearance >70 mL/min/1.73 m 2) [see Dosage and Administration ( 2.4) and ( 2.5)] .
Hemodialysis
Topiramate is cleared by hemodialysis. Using a high-efficiency, counterflow, single pass-dialysate hemodialysis procedure, topiramate dialysis clearance was 120 mL/min with blood flow through the dialyzer at 400 mL/min. This high clearance (compared to 20 to 30 mL/min total oral clearance in healthy adults) will remove a clinically significant amount of topiramate from the patient over the hemodialysis treatment period [see Dosage and Administration ( 2.6), Use in Specific Populations ( 8.7)] .
Hepatic Impairment
Plasma clearance of topiramate decreased a mean of 26% in patients with moderate to severe hepatic impairment.
Age, Gender, and Race
The pharmacokinetics of topiramate in elderly subjects (65 to 85 years of age, N=16) were evaluated in a controlled clinical study. The elderly subject population had reduced renal function (creatinine clearance [-20%]) compared to young adults. Following a single oral 100 mg dose, maximum plasma concentration for elderly and young adults was achieved at approximately 1 to 2 hours. Reflecting the primary renal elimination of topiramate, topiramate plasma and renal clearance were reduced 21% and 19%, respectively, in elderly subjects, compared to young adults. Similarly, topiramate half-life was longer (13%) in the elderly. Reduced topiramate clearance resulted in slightly higher maximum plasma concentration (23%) and AUC (25%) in elderly subjects than observed in young adults. Topiramate clearance is decreased in the elderly only to the extent that renal function is reduced [see Dosage and Administration ( 2.4) and Use in Specific Populations ( 8.5)] .
Clearance of topiramate in adults was not affected by gender or race.
Pediatric Pharmacokinetics
Pharmacokinetics of topiramate were evaluated in patients age 2 to <16 years. Patients received either no or a combination of other antiepileptic drugs. A population pharmacokinetic model was developed on the basis of pharmacokinetic data from relevant topiramate clinical studies. This dataset contained data from 1217 subjects including 258 pediatric patients age 2 to <16 years (95 pediatric patients <10 years of age).
Pediatric patients on adjunctive treatment exhibited a higher oral clearance (L/h) of topiramate compared to patients on monotherapy, presumably because of increased clearance from concomitant enzyme-inducing antiepileptic drugs. In comparison, topiramate clearance per kg is greater in pediatric patients than in adults and in young pediatric patients (down to 2 years) than in older pediatric patients. Consequently, the plasma drug concentration for the same mg/kg/day dose would be lower in pediatric patients compared to adults and also in younger pediatric patients compared to older pediatric patients. Clearance was independent of dose.
As in adults, hepatic enzyme-inducing antiepileptic drugs decrease the steady state plasma concentrations of topiramate.
Pediatric Patients with Obesity
A population PK analysis of topiramate was conducted in 129 children <21 years of age with and without obesity to evaluate the potential impact of obesity on plasma topiramate exposures. Obesity was defined as BMI ≥ 95th percentile for age and sex based on CDC-recommended BMI-for-age growth charts for males and females. Using the currently recommended dosing regimens, children with obesity are likely to have median values of average concentration at steady-state and trough concentration at steady-state that are up to 20% lower, and 19% lower, respectively, compared to children without obesity. Dosage adjustment according to obesity status is not necessary.
Drug Interactions
In vitrostudies indicate that topiramate does not inhibit CYP1A2, CYP2A6, CYP2B6, CYP2C9, CYP2D6, CYP2E1, or CYP3A4/5 isozymes. In vitrostudies indicate that topiramate is a mild inhibitor of CYP2C19 and a mild inducer of CYP3A4.
Antiepileptic Drugs
Potential interactions between topiramate and standard AEDs were assessed in controlled clinical pharmacokinetic studies in patients with epilepsy. The effects of these interactions on mean plasma AUCs are summarized in Table 11.
In Table 11, the second column (AED concentration) describes what happens to the concentration of the co-administered AED listed in the first column when topiramate is added. The third column (topiramate concentration) describes how the co-administration of a drug listed in the first column modifies the concentration of topiramate when compared to topiramate given alone.
Table 11: Summary of AED Interactions with Topiramate - * Plasma concentration increased 25% in some patients, generally those on a twice a day dosing regimen of phenytoin.
- † Is not administered but is an active metabolite of carbamazepine.
AED
Co-administeredAED
ConcentrationTopiramate
ConcentrationPhenytoin
NC or 25% increase *
48% decrease
Carbamazepine (CBZ)
NC
40% decrease
CBZ epoxide †
NC
NE
Valproic acid
11% decrease
14% decrease
Phenobarbital
NC
NE
Primidone
NC
NE
Lamotrigine
NC at TPM doses up to 400 mg/day
13% decrease
NC = Less than 10% change in plasma concentration.
AED = Antiepileptic drug.
NE = Not Evaluated.
TPM = Topiramate
Oral Contraceptives
In a pharmacokinetic interaction study in healthy volunteers with a concomitantly administered combination oral contraceptive product containing 1 mg norethindrone (NET) plus 35 mcg ethinyl estradiol (EE), topiramate, given in the absence of other medications at doses of 50 to 200 mg/day, was not associated with statistically significant changes in mean exposure (AUC) to either component of the oral contraceptive. In another study, exposure to EE was statistically significantly decreased at doses of 200, 400, and 800 mg/day (18%, 21%, and 30%, respectively) when given as adjunctive therapy in patients taking valproic acid. In both studies, topiramate (50 mg/day to 800 mg/day) did not significantly affect exposure to NET and there was no significant dose-dependent change in EE exposure for doses of 50 to 200 mg/day. The clinical significance of the changes observed is not known [see Drug Interactions ( 7.4)] .
Digoxin
In a single-dose study, serum digoxin AUC was decreased by 12% with concomitant topiramate administration. The clinical relevance of this observation has not been established.
Hydrochlorothiazide
A drug interaction study conducted in healthy volunteers evaluated the steady-state pharmacokinetics of hydrochlorothiazide (HCTZ) (25 mg every 24 hours) and topiramate (96 mg every 12 hours) when administered alone and concomitantly. The results of this study indicate that topiramate C maxincreased by 27% and AUC increased by 29% when HCTZ was added to topiramate. The clinical significance of this change is unknown. The steady-state pharmacokinetics of HCTZ were not significantly influenced by the concomitant administration of topiramate. Clinical laboratory results indicated decreases in serum potassium after topiramate or HCTZ administration, which were greater when HCTZ and topiramate were administered in combination.
Metformin
A drug interaction study conducted in healthy volunteers evaluated the steady-state pharmacokinetics of metformin (500 mg every 12 hours) and topiramate in plasma when metformin was given alone and when metformin and topiramate (100 mg every 12 hours) were given simultaneously. The results of this study indicated that the mean metformin C maxand AUC 0-12hincreased by 18% and 25%, respectively, when topiramate was added. Topiramate did not affect metformin t max. The clinical significance of the effect of topiramate on metformin pharmacokinetics is not known. Oral plasma clearance of topiramate appears to be reduced when administered with metformin. The clinical significance of the effect of metformin on topiramate pharmacokinetics is unclear.
Pioglitazone
A drug interaction study conducted in healthy volunteers evaluated the steady-state pharmacokinetics of topiramate and pioglitazone when administered alone and concomitantly. A 15% decrease in the AUC t,ssof pioglitazone with no alteration in C max,sswas observed. This finding was not statistically significant. In addition, a 13% and 16% decrease in C max,ssand AUC t,ssrespectively, of the active hydroxy-metabolite was noted as well as a 60% decrease in C max,ssand AUC t,ssof the active keto-metabolite. The clinical significance of these findings is not known.
Glyburide
A drug-drug interaction study conducted in patients with type 2 diabetes evaluated the steady-state pharmacokinetics of glyburide (5 mg/day) alone and concomitantly with topiramate (150 mg/day). There was a 22% decrease in C maxand a 25% reduction in AUC 24for glyburide during topiramate administration. Systemic exposure (AUC) of the active metabolites, 4- trans-hydroxy-glyburide (M1) and 3- cis-hydroxyglyburide (M2), was also reduced by 13% and 15%, and C maxwas reduced by 18% and 25%, respectively. The steady-state pharmacokinetics of topiramate were unaffected by concomitant administration of glyburide.
Lithium
In patients, the pharmacokinetics of lithium were unaffected during treatment with topiramate at doses of 200 mg/day; however, there was an observed increase in systemic exposure of lithium (27% for C maxand 26% for AUC) following topiramate doses up to 600 mg/day [see Drug Interactions ( 7.7)] .
Haloperidol
The pharmacokinetics of a single dose of haloperidol (5 mg) were not affected following multiple dosing of topiramate (100 mg every 12 hr) in 13 healthy adults (6 males, 7 females).
Amitriptyline
There was a 12% increase in AUC and C maxfor amitriptyline (25 mg per day) in 18 healthy subjects (9 males, 9 females) receiving 200 mg/day of topiramate.
Sumatriptan
Multiple dosing of topiramate (100 mg every 12 hours) in 24 healthy volunteers (14 males, 10 females) did not affect the pharmacokinetics of single-dose sumatriptan either orally (100 mg) or subcutaneously (6 mg).
Risperidone
When administered concomitantly with topiramate at escalating doses of 100, 250, and 400 mg/day, there was a reduction in risperidone systemic exposure (16% and 33% for steady-state AUC at the 250 and 400 mg/day doses of topiramate). No alterations of 9-hydroxyrisperidone levels were observed. Co-administration of topiramate 400 mg/day with risperidone resulted in a 14% increase in C maxand a 12% increase in AUC 12of topiramate. There were no clinically significant changes in the systemic exposure of risperidone plus 9-hydroxyrisperidone or of topiramate; therefore, this interaction is not likely to be of clinical significance.
Propranolol
Multiple dosing of topiramate (200 mg/day) in 34 healthy volunteers (17 males, 17 females) did not affect the pharmacokinetics of propranolol following daily 160 mg doses. Propranolol doses of 160 mg/day in 39 volunteers (27 males, 12 females) had no effect on the exposure to topiramate, at a dose of 200 mg/day of topiramate.
Dihydroergotamine
Multiple dosing of topiramate (200 mg/day) in 24 healthy volunteers (12 males, 12 females) did not affect the pharmacokinetics of a 1 mg subcutaneous dose of dihydroergotamine. Similarly, a 1 mg subcutaneous dose of dihydroergotamine did not affect the pharmacokinetics of a 200 mg/day dose of topiramate in the same study.
Diltiazem
Co-administration of diltiazem (240 mg Cardizem CD ®) with topiramate (150 mg/day) resulted in a 10% decrease in C maxand a 25% decrease in diltiazem AUC, a 27% decrease in C maxand an 18% decrease in des-acetyl diltiazem AUC, and no effect on N-desmethyl diltiazem. Co-administration of topiramate with diltiazem resulted in a 16% increase in C maxand a 19% increase in AUC 12of topiramate.
Venlafaxine
Multiple dosing of topiramate (150 mg/day) in healthy volunteers did not affect the pharmacokinetics of venlafaxine or O-desmethyl venlafaxine. Multiple dosing of venlafaxine (150 mg) did not affect the pharmacokinetics of topiramate.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
An increase in urinary bladder tumors was observed in mice given topiramate (0, 20, 75, and 300 mg/kg/day) in the diet for 21 months. The increase in the incidence of bladder tumors in males and females receiving 300 mg/kg/day was primarily due to the increased occurrence of a smooth muscle tumor considered histomorphologically unique to mice. The higher of the doses not associated with an increase in tumors (75 mg/kg/day) is equivalent to the maximum recommended human dose (MRHD) for epilepsy (400 mg), and approximately 4 times the MRHD for migraine (100 mg) on a mg/m 2basis. The relevance of this finding to human carcinogenic risk is uncertain. No evidence of carcinogenicity was seen in rats following oral administration of topiramate for 2 years at doses up to 120 mg/kg/day (approximately 3 times the MRHD for epilepsy and 12 times the MRHD for migraine on a mg/m 2basis).
Mutagenesis
Topiramate did not demonstrate genotoxic potential when tested in a battery of in vitroand in vivoassays. Topiramate was not mutagenic in the Ames test or the in vitromouse lymphoma assay; it did not increase unscheduled DNA synthesis in rat hepatocytes in vitro; and it did not increase chromosomal aberrations in human lymphocytes in vitroor in rat bone marrow in vivo.
Impairment of Fertility
No adverse effects on male or female fertility were observed in rats administered topiramate orally at doses up to 100 mg/kg/day (2.5 times the MRHD for epilepsy and 10 times the MRHD for migraine on a mg/m 2basis) prior to and during mating and early pregnancy.
-
14 CLINICAL STUDIES
The safety and efficacy of EPRONTIA are based on the relative bioavailability of EPRONTIA compared to topiramate sprinkle capsules in healthy subjects [see Clinical Pharmacology ( 12.3)] . Topiramate sprinkle capsules have comparable bioavailability to topiramate tablets.
The studies described in the following subsections were conducted using topiramate tablets or sprinkle capsules.
14.1 Monotherapy Epilepsy
Patients with Partial-Onset or Primary Generalized Tonic-Clonic Seizures
Adults and Pediatric Patients 10 Years of Age and Older
The effectiveness of topiramate as initial monotherapy in adults and pediatric patients 10 years of age and older with partial-onset or primary generalized tonic-clonic seizures was established in a multicenter, randomized, double-blind, parallel-group trial (Study 1).
Study 1 was conducted in 487 patients diagnosed with epilepsy (6 to 83 years of age) who had 1 or 2 well-documented seizures during the 3-month retrospective baseline phase who then entered the study and received topiramate 25 mg/day for 7 days in an open-label fashion. Forty-nine percent of patients had no prior AED treatment and 17% had a diagnosis of epilepsy for greater than 24 months. Any AED therapy used for temporary or emergency purposes was discontinued prior to randomization. In the double-blind phase, 470 patients were randomized to titrate up to 50 mg/day or 400 mg/day. If the target dose could not be achieved, patients were maintained on the maximum tolerated dose. Fifty-eight percent of patients achieved the maximal dose of 400 mg/day for >2 weeks, and patients who did not tolerate 150 mg/day were discontinued.
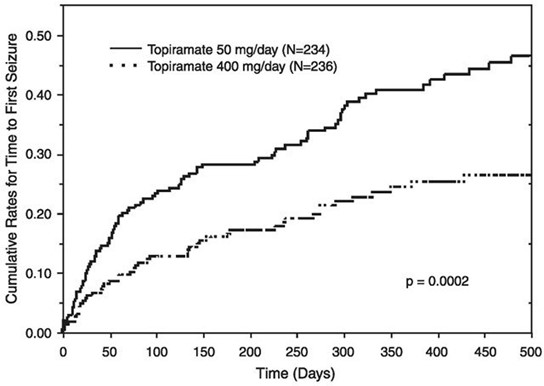
The primary efficacy assessment was a between-group comparison of time to first seizure during the double-blind phase. Comparison of the Kaplan-Meier survival curves of time to first seizure favored the topiramate 400 mg/day group over the topiramate 50 mg/day group ( Figure 1). The treatment effects with respect to time to first seizure were consistent across various patient subgroups defined by age, sex, geographic region, baseline body weight, baseline seizure type, time since diagnosis, and baseline AED use.
Figure 1: Kaplan-Meier Estimates of Cumulative Rates for Time to First Seizure in Study 1
Pediatric Patients 2 to 9 Years of Age
The conclusion that topiramate is effective as initial monotherapy in pediatric patients 2 to 9 years of age with partial-onset or primary generalized tonic-clonic seizures was based on a pharmacometric bridging approach using data from the controlled epilepsy trials described in labeling. This approach consisted of first showing a similar exposure-response relationship between pediatric patients down to 2 years of age and adults when topiramate was given as adjunctive therapy. Similarity of exposure response was also demonstrated in pediatric patients 6 to less than 16 years of age and adults when topiramate was given as initial monotherapy. Specific dosing in pediatric patients 2 to 9 years of age was derived from simulations utilizing plasma exposure ranges observed in pediatric and adult patients treated with topiramate initial monotherapy [see Dosage and Administration ( 2.1)] .
14.2 Adjunctive Therapy Epilepsy
Adult Patients with Partial-Onset Seizures
The effectiveness of topiramate as an adjunctive treatment for adults with partial-onset seizures was established in six multicenter, randomized, double-blind, placebo-controlled trials (Studies 2, 3, 4, 5, 6, and 7), two comparing several dosages of topiramate and placebo and four comparing a single dosage with placebo, in patients with a history of partial-onset seizures, with or without secondarily generalized seizures.
Patients in these studies were permitted a maximum of two antiepileptic drugs (AEDs) in addition to topiramate tablets or placebo. In each study, patients were stabilized on optimum dosages of their concomitant AEDs during baseline phase lasting between 4 and 12 weeks. Patients who experienced a pre-specified minimum number of partial-onset seizures, with or without secondary generalization, during the baseline phase (12 seizures for 12-week baseline, 8 for 8-week baseline or 3 for 4-week baseline) were randomly assigned to placebo or a specified dose of topiramate tablets in addition to their other AEDs.
Following randomization, patients began the double-blind phase of treatment. In five of the six studies, patients received active drug beginning at 100 mg per day; the dose was then increased by 100 mg or 200 mg/day increments weekly or every other week until the assigned dose was reached, unless intolerance prevented increases. In the sixth study (Study 7), the 25 or 50 mg/day initial doses of topiramate were followed by respective weekly increments of 25 or 50 mg/day until the target dose of 200 mg/day was reached. After titration, patients entered a 4, 8 or 12-week stabilization period. The numbers of patients randomized to each dose and the actual mean and median doses in the stabilization period are shown in Table 12.
Pediatric Patients 2 to 16 Years of Age with Partial-Onset Seizures
The effectiveness of topiramate as an adjunctive treatment for pediatric patients 2 to 16 years of age with partial-onset seizures was established in a multicenter, randomized, double-blind, placebo-controlled trial (Study 8), comparing topiramate and placebo in patients with a history of partial-onset seizures, with or without secondarily generalized seizures (see Table 13).
Patients in this study were permitted a maximum of two antiepileptic drugs (AEDs) in addition to topiramate tablets or placebo. In this study, patients were stabilized on optimum dosages of their concomitant AEDs during an 8-week baseline phase. Patients who experienced at least six partial-onset seizures, with or without secondarily generalized seizures, during the baseline phase were randomly assigned to placebo or topiramate tablets in addition to their other AEDs.
Following randomization, patients began the double-blind phase of treatment. Patients received active drug beginning at 25 or 50 mg/day; the dose was then increased by 25 mg to 150 mg/day increments every other week until the assigned dosage of 125, 175, 225, or 400 mg/day based on patients' weight to approximate a dosage of 6 mg/kg/day was reached, unless intolerance prevented increases. After titration, patients entered an 8-week stabilization period.
Patients With Primary Generalized Tonic-Clonic Seizures
The effectiveness of topiramate as an adjunctive treatment for primary generalized tonic-clonic seizures in patients 2 years of age and older was established in a multicenter, randomized, double-blind, placebo-controlled trial (Study 9), comparing a single dosage of topiramate and placebo (see Table 13).
Patients in Study 9 were permitted a maximum of two antiepileptic drugs (AEDs) in addition to topiramate or placebo. Patients were stabilized on optimum dosages of their concomitant AEDs during an 8-week baseline phase. Patients who experienced at least three primary generalized tonic-clonic seizures during the baseline phase were randomly assigned to placebo or topiramate in addition to their other AEDs.
Following randomization, patients began the double-blind phase of treatment. Patients received active drug beginning at 50 mg/day for four weeks; the dose was then increased by 50 mg to 150 mg/day increments every other week until the assigned dose of 175, 225, or 400 mg/day based on patients' body weight to approximate a dosage of 6 mg/kg/day was reached, unless intolerance prevented increases. After titration, patients entered a 12-week stabilization period.
Patients With Lennox-Gastaut Syndrome
The effectiveness of topiramate as an adjunctive treatment for seizures associated with Lennox- Gastaut syndrome was established in a multicenter, randomized, double-blind, placebo-controlled trial (Study 10) comparing a single dosage of topiramate with placebo in patients 2 years of age and older (see Table 13).
Patients in Study 10 were permitted a maximum of two antiepileptic drugs (AEDs) in addition to topiramate or placebo. Patients who were experiencing at least 60 seizures per month before study entry were stabilized on optimum dosages of their concomitant AEDs during a 4-week baseline phase. Following baseline, patients were randomly assigned to placebo or topiramate in addition to their other AEDs. Active drug was titrated beginning at 1 mg/kg/day for a week; the dose was then increased to 3 mg/kg/day for one week, then to 6 mg/kg/day. After titration, patients entered an 8-week stabilization period.
The primary measures of effectiveness were the percent reduction in drop attacks and a parental global rating of seizure severity.
Table 12: Topiramate Dose Summary During the Stabilization Periods of Each of Six Double-Blind, Placebo-Controlled, Adjunctive Trials in Adults with Partial-Onset Seizures * - * Dose-response studies were not conducted for other indications or pediatric partial-onset seizures.
- † Placebo dosages are given as the number of tablets. Placebo target dosages were as follows: Protocol 3 4 tablets/day; Protocols 1 and 4, 6 tablets/day; Protocols 5 and 6, 8 tablets/day; Protocol 2, 10 tablets/day.
Study
Stabilization Dose
Placebo†
Target TOPIRAMATE Dosage (mg/day)
200
400
600
800
1,000
2
N
Mean Dose
Median Dose
42
5.9
6.0
42
200
200
40
390
400
41
556
600
--
--
3
N
Mean Dose
Median Dose
44
9.7
10.0
--
--
40
544
600
45
739
800
40
796
1,000
4
N
Mean Dose
Median Dose
23
3.8
4.0
--
19
395
400
--
--
--
5
N
Mean Dose
Median Dose
30
5.7
6.0
--
--
28
522
600
--
--
6
N
Mean Dose
Median Dose
28
7.9
8.0
--
--
--
25
568
600
--
7
N
Mean Dose
Median Dose
90
8
8
157
200
200
--
--
--
--
In all adjunctive trials, the reduction in seizure rate from baseline during the entire double-blind phase was measured. The median percent reductions in seizure rates and the responder rates (fraction of patients with at least a 50% reduction) by treatment group for each study are shown below in Table 13. As described above, a global improvement in seizure severity was also assessed in the Lennox-Gastaut trial.
Table 13: Efficacy Results in Double-Blind, Placebo-Controlled, Adjunctive Epilepsy Trials - * For Studies 8 and 9, specified target dosages (<9.3 mg/kg/day) were assigned based on subject's weight to approximate a dosage of 6mg/kg per day; these dosages corresponded to mg/day dosages of 125, 175, 225, and 400 mg/day.
Study#
#
Target TOPIRAMATE Dosage (mg per day)
Placebo
200
400
600
800
1,000
≈6mg/kg/day*
Partial-Onset Seizures Studies in Adults
2
N
45
45
45
46
--
--
--
Median % Reduction
12
27 a
48 b
45 c
--
--
--
% Responders
18
24
44 d
46 d
--
--
--
3
N
47
--
--
48
48
47
--
Median % Reduction
2
--
--
41 c
41 c
36 c
% Responders
9
--
--
40 c
41 c
36 d
4
N
24
--
23
--
--
--
--
Median % Reduction
1
--
41 e
--
--
--
--
% Responders
8
--
35 d
--
--
--
--
5
N
30
--
--
30
--
--
--
Median % Reduction
-12
--
--
46 f
--
--
--
% Responders
10
--
--
47 c
--
--
--
6
N
28
--
--
--
28
--
--
Median % Reduction
-21
--
--
--
24 c
--
--
% Responders
0
--
--
--
43 c
--
--
7
N
91
168
--
--
--
--
--
Median % Reduction
20
44 c
--
--
--
--
--
% Responders
24
45 c
Partial-Onset Seizures Studies in Pediatric Patients
8
N
45
--
--
--
--
--
41
Median % Reduction
11
--
--
--
--
--
33 d
% Responders
20
--
--
--
--
--
39
Primary Generalized Tonic-Clonic h
9
N
40
--
--
--
--
--
39
Median % Reduction
9
--
--
--
--
--
57 d
% Responders
20
--
--
--
--
--
56 c
Lennox-Gastaut Syndrome i
10
N
49
--
--
--
--
--
46
Median % Reduction
-5
--
--
--
--
--
15 d
% Responders
14
28 g
Improvement in Seizure Severity j
28
52 d
Comparisons with placebo: ap=0.080; bp ≤ 0.010; cp ≤ 0.001; dp ≤ 0.050; ep=0.065; fp≤0.005; gp=0.071;
hMedian % reduction and % responders are reported for PGTC seizures;
iMedian % reduction and % responders for drop attacks, i.e., tonic or atonic seizures;
jPercentage of subjects who were minimally, much, or very much improved from baseline.
Subset analyses of the antiepileptic efficacy of topiramate tablets in these studies showed no differences as a function of gender, race, age, baseline seizure rate, or concomitant AED.
In clinical trials for epilepsy, daily dosages were decreased in weekly intervals by 50 to 100 mg/day in adults and over a 2- to 8-week period in pediatric patients; transition was permitted to a new antiepileptic regimen when clinically indicated.
14.3 Preventive Treatment of Migraine
Adult Patients
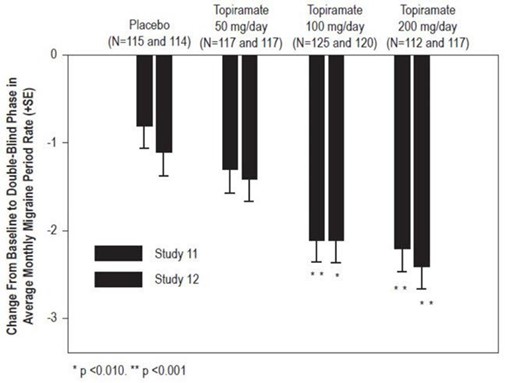
The results of 2 multicenter, randomized, double-blind, placebo-controlled, parallel-group clinical trials established the effectiveness of topiramate in the preventive treatment of migraine. The design of both trials (Study 11 was conducted in the U.S. and Study 12 was conducted in the U.S. and Canada) was identical, enrolling patients with a history of migraine, with or without aura, for at least 6 months, according to the International Headache Society (IHS) diagnostic criteria. Patients with a history of cluster headaches or basilar, ophthalmoplegic, hemiplegic, or transformed migraine headaches were excluded from the trials. Patients were required to have completed up to a 2-week washout of any prior migraine preventive medications before starting the baseline phase.
Patients who experienced 3 to 12 migraine headaches over the 4 weeks in the baseline phase were randomized to either topiramate 50 mg/day, 100 mg/day, 200 mg/day, or placebo and treated for a total of 26 weeks (8-week titration period and 18-week maintenance period). Treatment was initiated at 25 mg/day for one week, and then the daily dosage was increased by 25 mg increments each week until reaching the assigned target dose or maximum tolerated dose (administered twice daily).
Effectiveness of treatment was assessed by the reduction in migraine headache frequency, as measured by the change in 4-week migraine rate (according to migraines classified by IHS criteria) from the baseline phase to double-blind treatment period in each topiramate treatment group compared to placebo in the Intent-To-Treat (ITT) population.
In Study 11, a total of 469 patients (416 females, 53 males), ranging in age from 13 to 70 years, were randomized and provided efficacy data. Two hundred sixty-five patients completed the entire 26-week double-blind phase. The median average daily dosages were 48 mg/day, 88 mg/day, and 132 mg/day in the target dose groups of topiramate 50, 100, and 200 mg/day, respectively.
The mean migraine headache frequency rate at baseline was approximately 5.5 migraine headaches/28 days and was similar across treatment groups. The change in the mean 4-week migraine headache frequency from baseline to the double-blind phase was -1.3, -2.1, and -2.2 in the topiramate 50, 100, and 200 mg/day groups, respectively, versus -0.8 in the placebo group (see Figure 2). The treatment differences between the topiramate 100 and 200 mg/day groups versus placebo were similar and statistically significant (p<0.001 for both comparisons).
In Study 12, a total of 468 patients (406 females, 62 males), ranging in age from 12 to 65 years, were randomized and provided efficacy data. Two hundred fifty-five patients completed the entire 26-week double-blind phase. The median average daily dosages were 47 mg/day, 86 mg/day, and 150 mg/day in the target dose groups of topiramate 50, 100, and 200 mg/day, respectively.
The mean migraine headache frequency rate at baseline was approximately 5.5 migraine headaches/28 days and was similar across treatment groups. The change in the mean 4-week migraine headache period frequency from baseline to the double-blind phase was -1.4, -2.1, and -2.4 in the topiramate 50, 100, and 200 mg/day groups, respectively, versus -1.1 in the placebo group (see Figure 2). The differences between the topiramate 100 and 200 mg/day groups versus placebo were similar and statistically significant (p=0.008 and p <0.001, respectively).
In both studies, there were no apparent differences in treatment effect within age or gender subgroups. Because most patients were Caucasian, there were insufficient numbers of patients from different races to make a meaningful comparison of race.
For patients withdrawing from topiramate, daily dosages were decreased in weekly intervals by 25 to 50 mg/day.
Figure 2: Reduction in 4-Week Migraine Headache Frequency
(Studies 11 and 12 for Adults and Adolescents)
Pediatric Patients 12 to 17 Years of Age
The effectiveness of topiramate for the preventive treatment of migraine in pediatric patients 12 to 17 years of age was established in a multicenter, randomized, double-blind, parallel-group trial (Study 13). The study enrolled 103 patients (40 male, 63 female) 12 to 17 years of age with episodic migraine headaches with or without aura. Patient selection was based on IHS criteria for migraines (using proposed revisions to the 1988 IHS pediatric migraine criteria [IHS-R criteria]).
Patients who experienced 3 to 12 migraine attacks (according to migraines classified by patient reported diaries) and ≤14 headache days (migraine and non-migraine) during the 4-week prospective baseline period were randomized to either topiramate 50 mg/day, 100 mg/day, or placebo and treated for a total of 16 weeks (4-week titration period followed by a 12-week maintenance period). Treatment was initiated at 25 mg/day for one week, and then the daily dosage was increased by 25 mg increments each week until reaching the assigned target dose or maximum tolerated dose (administered twice daily). Approximately 80% or more patients in each treatment group completed the study. The median average daily dosages were 45 and 79 mg/day in the target dose groups of topiramate 50 and 100 mg/day, respectively.
Effectiveness of treatment was assessed by comparing each topiramate treatment group to placebo (ITT population) for the percent reduction from baseline to the last 12 weeks of the double-blind phase in the monthly migraine attack rate (primary endpoint). The percent reduction from baseline to the last 12 weeks of the double-blind phase in average monthly migraine attack rate is shown in Table 14.
The 100 mg topiramate dose produced a statistically significant treatment difference relative to placebo of 28% reduction from baseline in the monthly migraine attack rate.
The mean reduction from baseline to the last 12 weeks of the double-blind phase in average monthly attack rate, a key secondary efficacy endpoint in Study 13 (and the primary efficacy endpoint in Studies 11 and 12, of adults) was 3.0 for 100 mg topiramate dose and 1.7 for placebo. This 1.3 treatment difference in mean reduction from baseline of monthly migraine rate was statistically significant (p = 0.0087).
Table 14: Percent Reduction from Baseline to the Last 12 Weeks of Double-Blind Phase in Average Monthly Attack Rate: Study 13 (Intent-to-Treat Analysis Set) - * P-values (two-sided) for comparisons relative to placebo are generated by applying an ANCOVA model on ranks that includes subject's stratified age at baseline, treatment group, and analysis center as factors and monthly migraine attack rate during baseline period as a covariate.
- † P-values for the dose groups are the adjusted p-value according to the Hochberg multiple comparison procedure.
- ‡ Indicates p-value is <0.05 (two-sided).
Category
Placebo
(N=33)TOPIRAMATE
50 mg/day
(N=35)TOPIRAMATE
100 mg/day
(N=35)Baseline
Median
3.6
4.0
4.0
Last 12 Weeks of Double-Blind Phase
Median
2.3
2.3
1.0
Percent Reduction (%)
Median
44.4
44.6
72.2
0.7975
0.0164 ‡
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
EPRONTIA oral solution 25 mg/mL is supplied as a colorless to slightly yellow colored clear viscous liquid in white HDPE bottles. It is available as follows:
NDC
Size
NDC: 52652-9001-3
120 mL
NDC: 52652-9001-2
240 mL
NDC: 52652-9001-1
473 mL
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Eye Disorders
Instruct patients taking EPRONTIA to seek immediate medical attention if they experience blurred vision, visual disturbances, or periorbital pain [see Warnings and Precautions ( 5.1, 5.2)] .
Oligohidrosis and Hyperthermia
Closely monitor EPRONTIA treated patients, especially pediatric patients, for evidence of decreased sweating and increased body temperature, especially in hot weather. Counsel patients to contact their healthcare professionals immediately if they develop a high or persistent fever, or decreased sweating [see Warnings and Precautions ( 5.3)] .
Metabolic Acidosis
Warn patients about the potential significant risk for metabolic acidosis that may be asymptomatic and may be associated with adverse effects on kidneys (e.g., kidney stones, nephrocalcinosis), bones (e.g., osteoporosis, osteomalacia, and/or rickets in children), and growth (e.g., growth delay/retardation) in pediatric patients, and on the fetus [see Warnings and Precautions ( 5.4), Use in Specific Populations ( 8.1)] .
Suicidal Behavior and Ideation
Counsel patients, their caregivers, and families that AEDs, including EPRONTIA, may increase the risk of suicidal thoughts and behavior, and advise of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior or the emergence of suicidal thoughts, or behavior or thoughts about self-harm. Instruct patients to immediately report behaviors of concern to their healthcare providers [see Warnings and Precautions ( 5.5)] .
Interference with Cognitive and Motor Performance
Warn patients about the potential for somnolence, dizziness, confusion, difficulty concentrating, or visual effects, and advise patients not to drive or operate machinery until they have gained sufficient experience on EPRONTIA to gauge whether it adversely affects their mental performance, motor performance, and/or vision [see Warnings and Precautions ( 5.6)] .
Even when taking EPRONTIA or other anticonvulsants, some patients with epilepsy will continue to have unpredictable seizures. Therefore, advise all patients taking EPRONTIA for epilepsy to exercise appropriate caution when engaging in any activities where loss of consciousness could result in serious danger to themselves or those around them (including swimming, driving a car, climbing in high places, etc.). Some patients with refractory epilepsy will need to avoid such activities altogether. Discuss the appropriate level of caution with patients before patients with epilepsy engage in such activities.
Fetal Toxicity
Inform pregnant women and women of childbearing potential that use of EPRONTIA during pregnancy can cause fetal harm. EPRONTIA increases the risk of major congenital malformations, including but not limited to cleft lip and/or cleft palate (oral clefts), which occur early in pregnancy before many women know they are pregnant. Also inform patients that infants exposed to topiramate monotherapy in uteromay be SGA [see Use in Specific Populations ( 8.1)] . There may also be risks to the fetus from chronic metabolic acidosis with use of EPRONTIA during pregnancy [see Warnings and Precautions ( 5.7), Use in Specific Populations ( 8.1)] . When appropriate, counsel pregnant women and women of childbearing potential about alternative therapeutic options.
Advise women of childbearing potential who are not planning a pregnancy to use effective contraception while using EPRONTIA, keeping in mind that there is a potential for decreased contraceptive efficacy when using estrogen-containing or progestin-only contraceptives with topiramate [see Drug Interactions ( 7.4)] .
Encourage pregnant women using EPRONTIA, to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry. The registry is collecting information about the safety of antiepileptic drugs during pregnancy [see Use in Specific Populations ( 8.1)] .
Decrease in Bone Mineral Density
Inform the patient or caregiver that long-term treatment with EPRONTIA can decrease bone formation and increase bone resorption in children [see Warnings and Precautions ( 5.9)].
Negative Effects on Growth (Height and Weight)
Discuss with the patient or caregiver that long-term EPRONTIA treatment may attenuate growth as reflected by slower height increase and weight gain in pediatric patients [see Warnings and Precautions ( 5.10)].
Serious Skin Reactions
Inform patients about the signs of serious skin reactions. Instruct patients to immediately inform their healthcare provider at the first appearance of skin rash [see Warnings and Precautions (5.11)].
Hyperammonemia and Encephalopathy
Warn patients about the possible development of hyperammonemia with or without encephalopathy. Although hyperammonemia may be asymptomatic, clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy and/or vomiting. This hyperammonemia and encephalopathy can develop with EPRONTIA treatment alone or with EPRONTIA treatment with concomitant valproic acid (VPA).
Instruct patients to contact their physician if they develop unexplained lethargy, vomiting, or changes in mental status [see Warnings and Precautions (5.12)].
Kidney Stones
Instruct patients, particularly those with predisposing factors, to maintain an adequate fluid intake in order to minimize the risk of kidney stone formation [see Warnings and Precautions (5.13)].
Administration Instructions
Counsel patients that EPRONTIA may be taken with or without food. Advise patients that the dosage of EPRONTIA should be measured using a calibrated measuring device and not a household teaspoon and they may ask their pharmacist for an oral dosing syringe if you do not have one. Instruct patients to discard any unused EPRONTIA after 90 days of first opening the bottle [see Dosage and Administration ( 2.4)] .
Instructions for a Missing Dose
Instruct patients that if they miss a single dose of EPRONTIA, it should be taken as soon as possible. However, if a patient is within 6 hours of taking the next scheduled dose, tell the patient to wait until then to take the usual dose of EPRONTIA, and to skip the missed dose. Tell patients that they should not take a double dose in the event of a missed dose. Advise patients to contact their healthcare provider if they have missed a dose.
-
SPL UNCLASSIFIED SECTION
EPRONTIA is a registered trademark of Azurity Pharmaceuticals, Inc.
Manufactured for:
Azurity Pharmaceuticals, Inc.
Woburn, MA 01801Patent: https://azurity.com/patents_and_trademarks/
This product's labeling may have been updated. For current Full Prescribing Information, please visit www.eprontia.com
PN: 65628-00603
REV #: 09
-
Medication Guide
MEDICATION GUIDE
EPRONTIA ® [ee-pron-tee-ah]
(topiramate) oral solution
What is the most important information I should know about EPRONTIA?
EPRONTIA may cause eye problems.Serious eye problems include:
- any sudden decrease in vision with or without eye pain and redness.
- a blockage of fluid in the eye causing increased pressure in the eye (secondary angle closure glaucoma).
- These eye problems can lead to permanent loss of vision if not treated.
- You should call your healthcare provider right away if you have any new eye symptoms, including any new problems with your vision.
EPRONTIA may cause decreased sweating and increased body temperature (fever).People, especially children, should be watched for signs of decreased sweating and fever, especially in hot temperatures. Some people may need to be hospitalized for this condition. If a high fever, a fever that does not go away, or decreased sweating develops, call your healthcare provider right away.
EPRONTIA can increase the level of acid in your blood (metabolic acidosis). If left untreated, metabolic acidosis can cause brittle or soft bones (osteoporosis, osteomalacia, osteopenia), kidney stones, can slow the rate of growth in children, and may possibly harm your baby if you are pregnant. Metabolic acidosis can happen with or without symptoms. Sometimes people with metabolic acidosis will:
- feel tired
- not feel hungry (loss of appetite)
- feel changes in heartbeat
- have trouble thinking clearly
Your healthcare provider should do a blood test to measure the level of acid in your blood before and during your treatment with EPRONTIA. If you are pregnant, you should talk to your healthcare provider about whether you have metabolic acidosis.
Like other antiepileptic drugs, EPRONTIA may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- new or worse depression
- feeling agitated or restless
- trouble sleeping (insomnia)
- acting aggressive, being angry, or violent
- an extreme increase in activity and talking (mania)
- attempts to commit suicide
- new or worse anxiety
- panic attacks
- new or worse irritability
- acting on dangerous impulses
- other unusual changes in behavior or mood
Do not stop EPRONTIA without first talking to a healthcare provider.
- Stopping EPRONTIA suddenly can cause serious problems.
- Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
How can I watch for early symptoms of suicidal thoughts and actions?
- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
- Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
EPRONTIA can harm your unborn baby.
- If you take EPRONTIA during pregnancy, your baby has a higher risk for birth defects including cleft lip and cleft palate. These defects can begin early in pregnancy, even before you know you are pregnant.
- Birth defects may happen even in children born to women who are not taking any medicines and do not have other risk factors.
- There may be other medicines to treat your condition that have a lower chance of birth defects.
- All women of childbearing age should talk to their healthcare providers about using other possible treatments instead of EPRONTIA. If the decision is made to use EPRONTIA, you should use effective birth control (contraception) unless you are planning to become pregnant. You should talk to your doctor about the best kind of birth control to use while you are taking EPRONTIA.
- Tell your healthcare provider right away if you become pregnant while taking EPRONTIA. You and your healthcare provider should decide if you will continue to take EPRONTIA while you are pregnant.
- If you take EPRONTIA during pregnancy, your baby may be smaller than expected at birth. The long-term effects of this are not known. Talk to your healthcare provider if you have questions about this risk during pregnancy.
- Metabolic acidosis may have harmful effects on your baby. Talk to your healthcare provider if EPRONTIA has caused metabolic acidosis during your pregnancy.
- Pregnancy Registry: If you become pregnant while taking EPRONTIA, talk to your healthcare provider about registering with the North American Antiepileptic Drug Pregnancy Registry. You can enroll in this registry by calling 1-888-233-2334. The purpose of this registry is to collect information about the safety of EPRONTIA and other antiepileptic drugs during pregnancy.
EPRONTIA may decrease the density of bones when used over a long period.
EPRONTIA may slow height increase and weight gain in children and adolescents when used over a long period.
What is EPRONTIA?
EPRONTIA is a prescription medicine used:
to treat certain types of seizures (partial-onset seizures and primary generalized tonic-clonic seizures) in adults and children 2 years and older.
with other medicines to treat certain types of seizures (partial-onset seizures, primary generalized tonic-clonic seizures, and seizures associated with Lennox-Gastaut syndrome) in adults and children 2 years and older.
to prevent migraine headaches in adults and adolescents 12 years and older.
Before taking EPRONTIA, tell your healthcare provider about all of your medical conditions, including if you:
- have or have had depression, mood problems, or suicidal thoughts or behavior.
- have kidney problems, have kidney stones, or are getting kidney dialysis.
- have a history of metabolic acidosis (too much acid in the blood).
- have liver problems.
- have weak, brittle, or soft bones (osteomalacia, osteoporosis, osteopenia, or decreased bone density).
- have lung or breathing problems.
- have eye problems, especially glaucoma.
- have diarrhea.
- have a growth problem.
- are on a diet high in fat and low in carbohydrates, which is called a ketogenic diet.
- are having surgery.
- are pregnant or plan to become pregnant.
- are breastfeeding or plan to breastfeed. EPRONTIA passes into breast milk. Breastfed babies may be sleepy or have diarrhea. It is not known if the EPRONTIA that passes into breast milk can cause other serious harm to your baby. Talk to your healthcare provider about the best way to feed your baby if you take EPRONTIA.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. EPRONTIA and other medicines may affect each other causing side effects.
Especially tell your healthcare provider if you take:
- Valproic acid (such as DEPAKOTE).
- any medicines that impair or decrease your thinking, concentration, or muscle coordination.
- birth control that contains hormones (such as pills, implants, patches, or injections). EPRONTIA may make your birth control less effective. Tell your healthcare provider if your menstrual bleeding changes while you are using birth control and EPRONTIA.
Ask your healthcare provider if you are not sure if your medicine is listed above.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist each time you get a new medicine. Do not start a new medicine without talking with your healthcare provider.
How should I take EPRONTIA?
- Take EPRONTIA Oral Solution exactly as prescribed.
- Your healthcare provider may change your dose. Do not change your dose without talking to your healthcare provider.
- EPRONTIA can be taken with or without food. Drink plenty of fluids during the day. This may help prevent kidney stones while taking EPRONTIA.
- Take EPRONTIA using a marked (calibrated) measuring device. Ask your pharmacist to recommend a measuring device and for instructions on how to measure the correct dose. Do not use a household teaspoon or tablespoon.
- If you take too much EPRONTIA, call your healthcare provider right away or go to the nearest emergency room.
- If you miss a single dose of EPRONTIA, take it as soon as you can. However, if you are within 6 hours of taking your next scheduled dose, wait until then to take your usual dose of EPRONTIA, and skip the missed dose. Do not double your dose. If you have missed more than 1 dose, you should call your healthcare provider for advice.
- Do not stop taking EPRONTIA without talking to your healthcare provider. Stopping EPRONTIA suddenly may cause serious problems. If you have epilepsy and you stop taking EPRONTIA suddenly, you may have seizures that do not stop. Your healthcare provider will tell you how to stop taking EPRONTIA slowly. Your healthcare provider may do blood tests while you take EPRONTIA.
What should I avoid while taking EPRONTIA?
- You should not drink alcohol while taking EPRONTIA. EPRONTIA and alcohol can affect each other causing side effects such as sleepiness and dizziness.
- Do not drive a car or operate machinery until you know how EPRONTIA affects you. EPRONTIA can slow your thinking and motor skills and may affect vision.
What are the possible side effects of EPRONTIA? EPRONTIA may cause serious side effects including:
See " What is the most important information I should know about EPRONTIA?"
- High blood ammonia levels. High ammonia in the blood can affect your mental activities, slow your alertness, make you feel tired, or cause vomiting. This has happened when EPRONTIA is taken with a medicine called valproic acid (DEPAKOTE). Call your healthcare provider right away if you develop unexplained tiredness, vomiting, slowing of your thinking or reaction time, or changes in your mental activities.
- Effects on thinking and alertness. EPRONTIA may affect how you think and cause confusion, problems with concentration, attention, memory, or speech. EPRONTIA may cause depression or mood problems, tiredness, and sleepiness.
- Dizziness or loss of muscle coordination.
- Serious skin reactions. EPRONTIA may cause a severe rash with blisters and peeling skin, especially around the mouth, nose, eyes, and genitals (Stevens-Johnson syndrome). EPRONTIA may also cause a rash with blisters and peeling skin over much of the body that may cause death (toxic epidermal necrolysis). Call your healthcare provider right away if you develop a skin rash or blisters.
- Kidney stones. Drink plenty of fluids when taking EPRONTIA to decrease your chances of getting kidney stones.
- Low body temperature. Taking EPRONTIA when you are also taking valproic acid can cause a drop in body temperature to less than 95°F, or can cause tiredness, confusion, or coma.
Call your healthcare provider right away if you have any of the symptoms above.
The most common side effects of EPRONTIA include:
o tingling of the arms and legs (paresthesia)
o nausea
o diarrhea
o nervousness
o speech problems
o dizziness
o slow reactions
o pain in the abdomen
o decreased feeling or sensitivity, especially in the skino not feeling hungry
o a change in the way foods taste
o weight loss
o upper respiratory tract infection
o tiredness
o sleepiness/drowsiness
o difficulty with memory
o fever
o abnormal vision
Tell your healthcare provider about any side effect that bothers you or that does not go away. These are not all the possible side effects of EPRONTIA. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1- 800-FDA-1088. You may also report side effects to Azurity Pharmaceuticals, Inc. at 1-800-461-7449.
How should I store EPRONTIA?
- Store EPRONTIA at room temperature between 68°F to 77°F (20°C to 25°C).
- Throw away (discard) unused portion 90 days after first opening.
- Avoid freezing and excessive heat.
- Keep container tightly closed
Keep EPRONTIA and all medicines out of the reach of children.
General information about the safe and effective use of EPRONTIA.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use EPRONTIA for a condition for which it was not prescribed. Do not give EPRONTIA to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about EPRONTIA that is written for health professionals.
What are the ingredients in EPRONTIA?
Active ingredient:Topiramate
Inactive ingredients: glycerin, methylparaben, mixed berry flavor, polyethylene glycol, propylparaben, and sucralose.
Manufactured for:
Azurity Pharmaceuticals, Inc.
Woburn, MA 01801This Medication Guide has been approved by the U.S. Food and Drug Administration
Approved: May 2024
-
PRINCIPAL DISPLAY PANEL - Carton Label
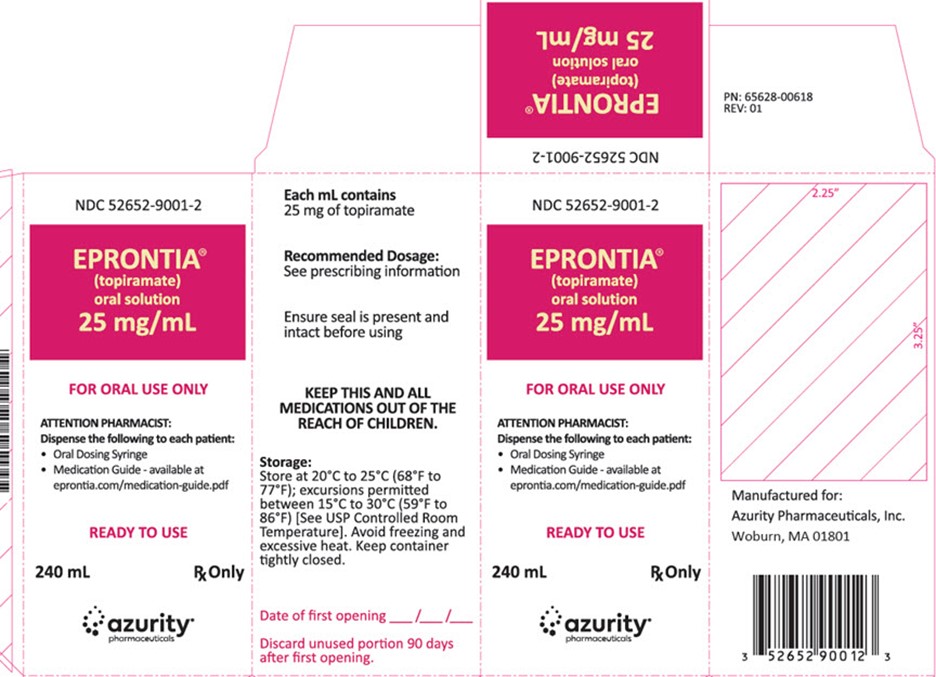
Carton Label
NDC: 52652-9001-2
EPRONTIA ®(topiramate)
oral solution25 mg/mL
FOR ORAL USE ONLY
ATTENTION PHARMACIST:
Dispense the following to each patient:
Oral Dosing Syringe
Medication Guide - available at
eprontia.com/medication-guide.pdfREADY TO USE
240 mL Rx Only
azurity ®pharmaceuticals
Manufactured for:
Azurity Pharmaceuticals, Inc.
Woburn, MA 01801 -
INGREDIENTS AND APPEARANCE
EPRONTIA
topiramate solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59368-405 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TOPIRAMATE (UNII: 0H73WJJ391) (TOPIRAMATE - UNII:0H73WJJ391) TOPIRAMATE 25 mg in 1 mL Inactive Ingredients Ingredient Name Strength POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) METHYLPARABEN (UNII: A2I8C7HI9T) PROPYLPARABEN (UNII: Z8IX2SC1OH) SUCRALOSE (UNII: 96K6UQ3ZD4) GLYCERIN (UNII: PDC6A3C0OX) Product Characteristics Color Score Shape Size Flavor BERRY (Mixed) Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59368-405-02 1 in 1 CARTON 01/02/2023 1 240 mL in 1 BOTTLE; Type 0: Not a Combination Product 2 NDC: 59368-405-01 1 in 1 CARTON 01/02/2023 2 120 mL in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA214679 12/06/2021 Labeler - Praxis, LLC (016329513) Establishment Name Address ID/FEI Business Operations Praxis, LLC 016329513 manufacture(59368-405) , label(59368-405) , pack(59368-405)
Trademark Results [Eprontia]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 EPRONTIA 90690878 not registered Live/Pending |
Azurity Pharmaceuticals, Inc. 2021-05-05 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.