AMPICILLIN injection, powder, for solution
Ampicillin by
Drug Labeling and Warnings
Ampicillin by is a Prescription medication manufactured, distributed, or labeled by WG Critical Care, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
SPL UNCLASSIFIED SECTION
Rx only
FOR INTRAMUSCULAR OR INTRAVENOUS USE
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Ampicillin and other antibacterial drugs, Ampicillin for Injection, USP should be used only to treat infections that are proven or strongly suspected to be caused by bacteria.
-
DESCRIPTION
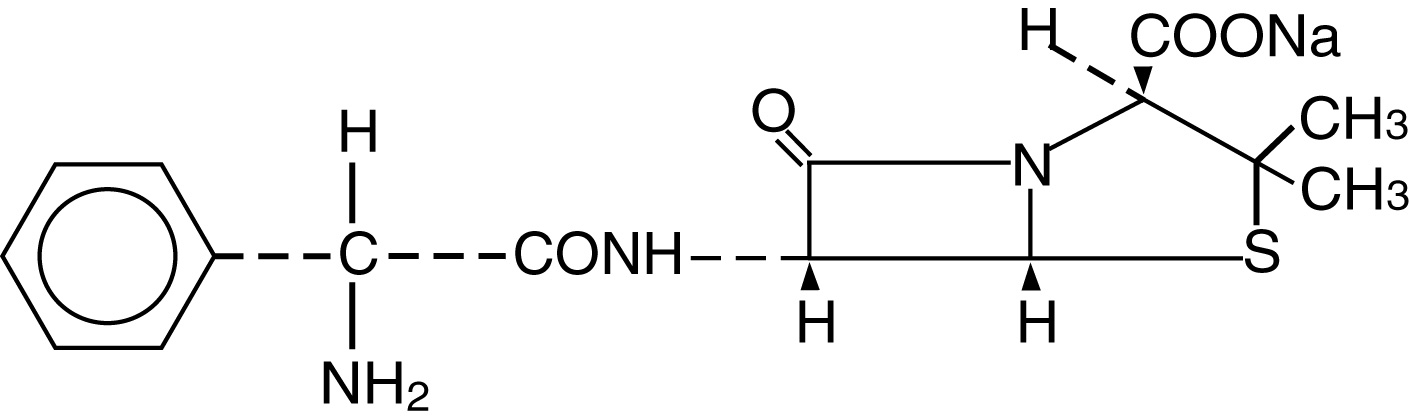
Ampicillin for Injection, USP the monosodium salt of [2S-[2a, 5a, 6b(S*)]]-6- [(aminophenylacetyl)amino]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo [3.2.0]heptane-2-carboxylic acid, is a synthetic penicillin. It is an antibacterial agent with a broad spectrum of bactericidal activity against both penicillin-susceptible Gram-positive organisms and many common Gram-negative pathogens. Ampicillin for Injection, USP is a dry, white to off-white powder. The reconstituted solution is clear, colorless and free from visible particulates. It has the following chemical structure:
The molecular formula is C16H18N3NaO4S, and the molecular weight is 371.39. The pH range of the reconstituted solution is 8.0 to 10.0. Ampicillin for Injection, USP contains 65.8 mg [2.9 mEq] sodium per gram ampicillin.
Ampicillin for Injection, USP is supplied in vials equivalent to 125 mg, 250 mg, 500 mg, 1 gram or 2 grams of ampicillin. It is to be administered by intravenous or intramuscular routes.
-
CLINICAL PHARMACOLOGY
Ampicillin for Injection, USP diffuses readily into most body tissues and fluids. However, penetration into the cerebrospinal fluid and brain occurs only when the meninges are inflamed. Ampicillin is excreted largely unchanged in the urine and its excretion can be delayed by concurrent administration of probenecid. Due to maturational changes in renal function, ampicillin half-life decreases as postmenstrual age (a sum of gestational age and postnatal age) increases for infants with postnatal age of less than 28 days. The active form appears in the bile in higher concentrations than those found in serum. Ampicillin is the least serum-bound of all the penicillins, averaging about 20% compared to approximately 60 to 90% for other penicillins. Ampicillin for Injection, USP is well tolerated by most patients and has been given in doses of 2 grams daily for many weeks without adverse reactions.
Microbiology:
While in vitro studies have demonstrated the susceptibility of most strains of the following organisms, clinical efficacy for infections other than those included in the INDICATIONS AND USAGE section has not been demonstrated.
Antibacterial Activity:
The following bacteria have been shown in in vitro studies to be susceptible to Ampicillin for Injection, USP:
Gram-positive Bacteria
Hemolytic and nonhemolytic streptococci
Streptococcus pneumoniae
Nonpenicillinase-producing staphylococci
Clostridium spp.
B. anthracis
Listeria monocytogenes
Most strains of enterococci.
Gram-negative Bacteria
H. influenzae
N. gonorrhoeae
N. meningitidis
Proteus mirabilis
Many strains of Salmonella, Shigella, and E. coli.
AMPICILLIN does not resist destruction by penicillinase.
Susceptibility Testing
For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see: https://www.fda.gov/STIC.
-
INDICATIONS AND USAGE
Ampicillin for Injection, USP is indicated in the treatment of infections caused by susceptible strains of the designated organisms in the following conditions:
Respiratory Tract Infections caused by S. pneumoniae, Staphylococcus aureus (penicillinase and non-penicillinase producing), H. influenzae and Group A beta-hemolytic Streptococci.
Bacterial Meningitis caused by E. coli, Group B Streptococci, and other Gram-negative bacteria (Listeria monocytogenes, N. meningitidis). The addition of an aminoglycoside with ampicillin may increase its effectiveness against Gram-negative bacteria.
Septicemia and Endocarditis caused by susceptible Gram-positive organisms including Streptococcus spp., penicillin-G-susceptible staphylococci and enterococci. Gram-negative sepsis caused by E. coli, Proteus mirabilis and Salmonella spp. responds to ampicillin. Endocarditis due to enterococcal strains usually respond to intravenous therapy. The addition of an aminoglycoside may enhance the effectiveness of ampicillin when treating streptococcal endocarditis.
Urinary Tract Infections caused by sensitive strains of E. coli and Proteus mirabilis.
Gastrointestinal Infections caused by Salmonella typhi (typhoid fever), other Salmonella spp. and Shigella spp. (dysentery) usually respond to oral or intravenous therapy.
Bacteriology studies to determine the causative organisms and their susceptibility to ampicillin should be performed. Therapy may be instituted prior to obtaining results of susceptibility testing.
It is advisable to reserve the parenteral form of this drug for moderately severe and severe infections and for patients who are unable to take the oral forms. A change to oral ampicillin may be made as soon as appropriate. Indicated surgical procedures should be performed.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Ampicillin for Injection, USP and other antibacterial drugs, Ampicillin for Injection, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
- CONTRAINDICATIONS
-
WARNINGS
Serious and occasionally fatal hypersensitivity (anaphylactoid) reactions have been reported in patients on penicillin therapy. Although anaphylaxis is more frequent following parenteral therapy, it has occurred in patients on oral penicillins. These reactions are more apt to occur in individuals with a history of penicillin hypersensitivity and/or a history of sensitivity to multiple allergens.
There have been well-documented reports of individuals with a history of penicillin hypersensitivity reactions who have experienced severe hypersensitivity reactions when treated with a cephalosporin. Before initiating therapy with a penicillin, careful inquiry should be made concerning previous hypersensitivity reactions to penicillins, cephalosporins, and other allergens. If an allergic reaction occurs, the drug should be discontinued and appropriate therapy instituted.
SERIOUS ANAPHYLACTOID REACTIONS REQUIRE IMMEDIATE EMERGENCY TREATMENT WITH EPINEPHRINE, OXYGEN, INTRAVENOUS STEROIDS, AND AIRWAY MANAGEMENT, INCLUDING INTUBATION, SHOULD ALSO BE ADMINISTERED AS INDICATED.
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Ampicillin for Injection, USP, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial drug use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibacterial drug use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
-
PRECAUTIONS
General
Prescribing Ampicillin for Injection, USP in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
The possibility of superinfections with mycotic organisms or bacterial pathogens should be kept in mind during therapy. In such cases, discontinue the drug and substitute appropriate treatment.
A high percentage (43 to 100 percent) of patients with infectious mononucleosis who receive ampicillin develop a skin rash. Typically, the rash appears 7 to 10 days after the start of oral ampicillin therapy and remains for a few days to a week after the drug is discontinued. In most cases, the rash is maculopapular; pruritic and generalized. Therefore, the administration of ampicillin is not recommended in patients with mononucleosis. It is not known whether these patients are truly allergic to ampicillin.
Information for Patients
Patients should be counseled that antibacterial drugs including Ampicillin for Injection, USP should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When Ampicillin for Injection, USP is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed.
Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Ampicillin for Injection, USP or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibacterials which usually ends when the antibacterial is discontinued. Sometimes after starting treatment with antibacterials, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibacterial. If this occurs, patients should contact their physician as soon as possible.
Laboratory Tests
As with any potent drug, periodic assessment of organ system function, including renal, hepatic and hematopoietic, should be made during prolonged therapy.
Transient elevation of serum transaminase has been observed following administration of ampicillin. The significance of this finding is not known.
Drug Interactions
The concurrent administration of allopurinol and ampicillin increases substantially the incidence of skin rashes in patients receiving both drugs as compared to patients receiving ampicillin alone. It is not known whether this potentiation of ampicillin rashes is due to allopurinol or the hyperuricemia present in these patients.
Drug/Laboratory Test Interactions
With high urine concentrations of ampicillin, false-positive glucose reactions may occur if Clinitest, Benedict’s Solution, or Fehling’s Solution are used. Therefore, it is recommended that glucose tests based on enzymatic glucose oxidase reactions (such as Clinistix or Tes-Tape) be used.
Carcinogenesis, Mutagenesis, and Impairment of Fertility
No long-term animal studies have been conducted with this drug.
Pregnancy Category B:
Reproduction studies have been performed in laboratory animals at doses several times the human dose and have revealed no evidence of adverse effects due to ampicillin. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Labor and Delivery
Oral ampicillin-class antibacterials are poorly absorbed during labor. Studies in guinea pigs showed that intravenous administration of ampicillin slightly decreased the uterine tone and frequency of contractions, but moderately increased the height and duration of contractions. However, it is not known whether use of these drugs in humans during labor or delivery has immediate or delayed adverse effects on the fetus, prolongs the duration of labor, or increases the likelihood that forceps delivery or other obstetrical intervention or resuscitation of the newborn will be necessary.
Nursing Mothers
Ampicillin is excreted in trace amounts in human milk. Therefore, caution should be exercised when ampicillin-class antibacterials are administered to a nursing woman.
Pediatric Use
Guidelines for the administration of these drugs to children, including neonates are presented in DOSAGE AND ADMINISTRATION.
-
ADVERSE REACTIONS
As with other penicillins, it may be expected that untoward reactions will be essentially limited to sensitivity phenomena. They are more likely to occur in individuals who have previously demonstrated hypersensitivity to penicillins and in those with a history of allergy, asthma, hay fever or urticaria. The following adverse reactions have been reported as associated with the use of ampicillin:
Gastrointestinal
Glossitis, stomatitis, black “hairy” tongue, nausea, vomiting, enterocolitis, pseudomembranous colitis, and diarrhea. (These reactions are usually associated with oral dosage forms.)
Hypersensitivity Reactions
Skin rashes and urticaria have been reported frequently. A few cases of exfoliative dermatitis and erythema multiforme have been reported. Anaphylaxis is the most serious reaction experienced and has usually been associated with the parenteral dosage form.
Note: Urticaria, other skin rashes, and serum sickness-like reactions may be controlled with antihistamines and, if necessary, systemic corticosteroids.
Whenever such reactions occur, ampicillin should be discontinued, unless, in the opinion of the physician, the condition being treated is life-threatening and amenable only to ampicillin therapy. Serious anaphylactic reactions require the immediate use of epinephrine, oxygen, and intravenous steroids.
Liver
A moderate rise in serum glutamic oxaloacetic transaminase (SGOT) has been noted, particularly in infants, but the significance of this finding is unknown. Mild transitory SGOT elevations have been observed in individuals receiving larger (two to four times) than usual and oft-repeated intramuscular injections. Evidence indicates that glutamic oxaloacetic transaminase (GOT) is released at the site of intramuscular injection of Ampicillin for Injection and that the presence of increased amounts of this enzyme in the blood does not necessarily indicate liver involvement.
Hemic and Lymphatic Systems
Anemia, thrombocytopenia, thrombocytopenic
purpura, eosinophilia, leukopenia, and agranulocytosis have been reported during therapy with the penicillins. These reactions are usually reversible on discontinuation of therapy and are believed to be hypersensitivity phenomena.
Central Nervous System
Seizures.
- OVERDOSAGE
-
DOSAGE AND ADMINISTRATION
Infections of the respiratory tract and soft tissues.
Patients weighing 40 kg (88 lbs) or more: 250 mg to 500 mg every 6 hours.
Patients weighing less than 40 kg (88 lbs): 25 to 50 mg/kg/day in equally divided doses at 6- to 8-hour intervals.
Infections of the gastrointestinal and genitourinary tracts (including those caused by Neisseria gonorrhoeae in females).
Patients weighing 40 kg (88 lbs) or more: 500 mg every 6 hours.
Patients weighing less than 40 kg (88 lbs): 50 mg/kg/day in equally divided doses at 6- to 8-hour intervals.
In the treatment of chronic urinary tract and intestinal infections, frequent bacteriological and clinical appraisal is necessary. Smaller doses than those recommended above should not be used. Higher doses should be used for stubborn or severe infections. In stubborn infections, therapy may be required for several weeks. It may be necessary to continue clinical and/or bacteriological follow-up for several months after cessation of therapy.
Urethritis in males due to N. gonorrhoeae:
Adults: Two doses of 500 mg each at an interval of 8 to 12 hours.
Treatment may be repeated if necessary or extended if required.
In the treatment of complications of gonorrheal urethritis, such as prostatitis and epididymitis, prolonged and intensive therapy is recommended. Cases of gonorrhea with a suspected primary lesion of syphilis should have darkfield examinations before receiving treatment. In all other cases where concomitant syphilis is suspected, monthly serological tests should be made for a minimum of four months.
The doses for the preceding infections may be given by either the intramuscular or intravenous route. A change to oral ampicillin may be made when appropriate.
Bacterial Meningitis.
Adults and children: 150 to 200 mg/kg/day in equally divided doses every 3 to 4 hours. (Treatment may be initiated with intravenous drip therapy and continued with intramuscular injections.) The doses for other infections may be given by either the intravenous or intramuscular route.
Neonates (less than or equal to 28 days of postnatal age): Dosage should be based on Gestational age and Postnatal age according to Table 1.
Table 1: Dosage in Neonates (less than or equal to 28 days of postnatal age) for Bacterial Meningitis and Septicemia
Gestational age (weeks)
Postnatal age (days)
Dosage
less than or equal to 34
less than or equal to 7
100 mg/kg/day in equally divided doses every 12 hours
less than or equal to 34
greater than or equal to 8 and less than 28
150 mg/kg/day in equally divided doses every 12 hours
greater than 34
less than or equal to 28
150 mg/kg/day in equally divided doses every 8 hours
Septicemia.
Adults and children: 150 to 200 mg/kg/day. Start with intravenous administration for at least three days and continue with the intramuscular route every 3 to 4 hours.
Neonates (less than or equal to 28 days of postnatal age): Dosage should be based on Gestational age and Postnatal age according to Table 1 (above).
Treatment of all infections should be continued for a minimum of 48 to 72 hours beyond the time that the patient becomes asymptomatic or evidence of bacterial eradication has been obtained. A minimum of 10 days treatment is recommended for any infection caused by Group A beta-hemolytic streptococci to help prevent the occurrence of acute rheumatic fever or acute glomerulonephritis.
DIRECTIONS FOR USE
Use only freshly prepared solutions. Intramuscular and intravenous injections should be administered within one hour after preparation, since the potency may decrease significantly after this period.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
For Intramuscular Use: Dissolve contents of a vial with the amount of Sterile Water for Injection, USP or Bacteriostatic Water for Injection, USP, listed in the table below:
NDC
Label Claim
Recommended Amount of Diluent
Withdrawable Volume
Concentration (in mg/mL)
44567-100-10
250 mg
1 mL
1 mL
250 mg
44567-101-10
500 mg
1.8 mL
2 mL
250 mg
44567-102-10
1 gram
3.5 mL
4 mL
250 mg
44567-103-10
2 grams
6.8 mL
8 mL
250 mg
While Ampicillin for Injection, USP 1 g and 2 g, are primarily for intravenous use, they may be administered intramuscularly when the 250 mg or 500 mg vials are unavailable. In such instances, dissolve in 3.5 or 6.8 mL Sterile Water for Injection, USP or Bacteriostatic Water for Injection, USP, respectively. The resulting solution will provide a concentration of 250 mg per mL.
Ampicillin for Injection, USP 125 mg, is intended primarily for pediatric use. It also serves as a convenient dosage form when small parenteral doses of the antibiotic are required.
Note: Bacteriostatic Water for Injection, USP is not to be used as a diluent when the product will be used in newborns.
For Direct Intravenous Use
Add 5 mL Sterile Water for Injection, USP, or Bacteriostatic Water for Injection, USP to the 125 mg, 250 mg, and 500 mg vials and administer slowly over a 3 to 5 minute period. Ampicillin for Injection, USP 1 g or 2 g, may also be given by direct intravenous administration. Dissolve in 7.4 or 14.8 mL Sterile Water for Injection, USP, or Bacteriostatic Water for Injection, USP, respectively, and administer slowly over at least 10 to 15 minutes. CAUTION: More rapid administration may result in convulsive seizures.
For Administration by Intravenous Drip:
Reconstitute as directed above (For Direct Intravenous Use) prior to diluting with Intravenous Solution. Stability studies on ampicillin sodium at several concentrations in various intravenous solutions indicate the drug will lose less than 10% activity at the temperatures noted for the time periods stated.
Room Temperature (25°C)
Diluent
Concentrations
Stability Periods
Sterile Water for Injection
up to 30 mg/mL
8 hours
0.9% Sodium Chloride Injection, USP
up to 30 mg/mL
8 hours
5% Dextrose Injection, USP
10 to 20 mg/mL
1 hour
5% Dextrose Injection, USP
up to 2 mg/mL
2 hours
5% Dextrose and 0.45% Sodium Chloride Injection, USP
up to 2 mg/mL
2 hours
Lactated Ringer’s Injection, USP
up to 30 mg/mL
8 hours
Refrigerated (4°C)
Sterile Water for Injection
30 mg/mL
48 hours
Sterile Water for Injection
up to 20 mg/mL
72 hours
0.9% Sodium Chloride Injection, USP
30 mg/mL
24 hours
0.9% Sodium Chloride Injection, USP
up to 20 mg/mL
48 hours
Lactated Ringer’s Injection, USP
up to 30 mg/mL
24 hours
5% Dextrose Injection, USP
up to 20 mg/mL
1 hour
5% Dextrose and 0.45% Sodium Chloride Injection, USP
up to 10 mg/mL
1 hour
Only those solutions listed above should be used for the intravenous infusion of Ampicillin for Injection, USP. The concentrations should fall within the range specified. The drug concentration and the rate and volume of the infusion should be adjusted so that the total dose of ampicillin is administered before the drug loses its stability in the solution in use.
Piggyback IV Package: These glass vials contain the labeled quantity of Ampicillin for Injection and are intended for intravenous administration. The diluent and volume are specified on the label of each package.
-
HOW SUPPLIED
Ampicillin for Injection, USP equivalent to 250 mg, 500 mg, 1 or 2 grams ampicillin as the sodium salt per vial is supplied as follows:
NDC: 44567-100-10
250 mg vial
(Tray of 10)
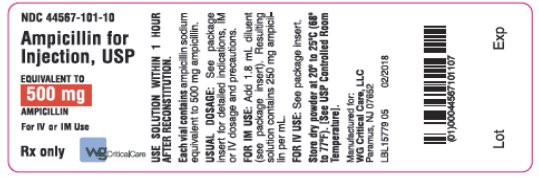
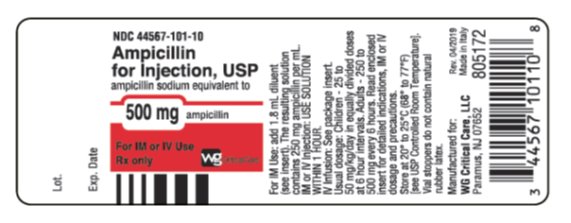
NDC: 44567-101-10
500 mg vial
(Tray of 10)
NDC: 44567-102-10
1 gram vial
(Tray of 10)
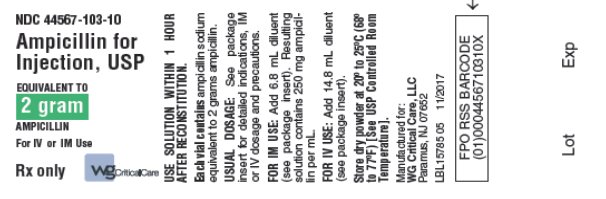
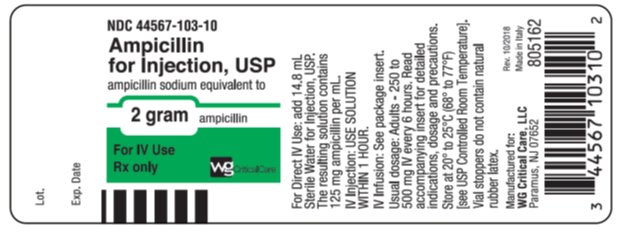
NDC: 44567-103-10
2 gram vial
(Tray of 10)
Ampicillin for Injection, USP dry powder should be stored at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
To report SUSPECTED ADVERSE REACTIONS, contact WG Critical Care, LLC at 1-866-562-4708 or the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Clinitest is a registered trademark of Miles, Inc.
Clinistix is a registered trademark of Bayer Corporation.
Tes-Tape is a registered trademark of Eli Lilly Company.
Manufactured for:
WG Critical Care, LLC
Paramus, NJ 07652
Made in Italy
805163/01
Revised: April 2019
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
- Package/Label Display Panel
- Package/Label Display Panel
-
INGREDIENTS AND APPEARANCE
AMPICILLIN
ampicillin injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44567-100 Route of Administration INTRAVENOUS, INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMPICILLIN SODIUM (UNII: JFN36L5S8K) (AMPICILLIN - UNII:7C782967RD) AMPICILLIN 250 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44567-100-10 10 in 1 TRAY 05/10/2012 03/31/2016 1 1 in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA062772 05/10/2012 03/31/2016 AMPICILLIN
ampicillin injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44567-101 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMPICILLIN SODIUM (UNII: JFN36L5S8K) (AMPICILLIN - UNII:7C782967RD) AMPICILLIN 500 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44567-101-10 10 in 1 TRAY 05/10/2012 1 1 in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA062772 05/10/2012 AMPICILLIN
ampicillin injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44567-102 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMPICILLIN SODIUM (UNII: JFN36L5S8K) (AMPICILLIN - UNII:7C782967RD) AMPICILLIN 1 g Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44567-102-10 10 in 1 TRAY 05/10/2012 1 1 in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA062772 05/10/2012 AMPICILLIN
ampicillin injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44567-103 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMPICILLIN SODIUM (UNII: JFN36L5S8K) (AMPICILLIN - UNII:7C782967RD) AMPICILLIN 2 g Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44567-103-10 10 in 1 TRAY 05/10/2012 1 1 in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA062772 05/10/2012 Labeler - WG Critical Care, LLC (829274633)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.