LAZANDA- fentanyl citrate spray
LAZANDA by
Drug Labeling and Warnings
LAZANDA by is a Prescription medication manufactured, distributed, or labeled by Archimedes Pharma US Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LAZANDA safely and effectively. See full prescribing information for LAZANDA
Lazanda® (Fentanyl) Nasal Spray CII
Initial U.S. Approval: 1968WARNING: RISK OF RESPIRATORY DEPRESSION, MEDICATION ERRORS, ABUSE POTENTIAL
See full prescribing information for complete boxed warning.
- Due to the risk of fatal respiratory depression, Lazanda is contraindicated in opioid non-tolerant patients (1) and in management of acute or postoperative pain, including headache/migraines. (4)
- Keep out of reach of children. (5.3)
- Use with CYP3A4 inhibitors may cause fatal respiratory depression. (7)
- When prescribing, do not convert patients on a mcg per mcg basis from any other oral transmucosal fentanyl product to Lazanda. (2.1, 5.2)
- When dispensing, do not substitute with any other fentanyl products. (5.2)
- Contains fentanyl, a Schedule II controlled substance with abuse liability similar to other opioid analgesics. (9.1)
- Lazanda is available only through a restricted program called the TIRF REMS Access program. Outpatients, healthcare professionals who prescribe to outpatients, pharmacies, and distributors are required to enroll in the program. (5.10)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Lazanda is an opioid agonist indicated for the management of breakthrough pain in cancer patients 18 years of age and older who are already receiving and who are tolerant to opioid therapy for their underlying persistent cancer pain. [1]
Limitations of Use:
Lazanda may be dispensed only to patients enrolled in the TIRF REMS Access program.
DOSAGE AND ADMINISTRATION
- Patients must require and use around-the-clock opioids when taking Lazanda. (1)
- Initial dose of Lazanda for all patients is 100 mcg. [2.1]
- Individually titrate to an effective dose, from 100 mcg to 200 mcg to 400 mcg, and up to a maximum of 800 mcg, that provides adequate analgesia with tolerable side effects. [2.1]
- Dose is a single spray into one nostril or a single spray into each nostril (2 sprays). [2.1]
- Maximum dose is a single spray into one nostril or single spray into each nostril per episode; no more than four doses per 24 hours. [2.1]
- Wait at least 2 hours before treating another episode of breakthrough pain with Lazanda. [2.1]
- During any episode, if adequate pain relief is not achieved within 30 minutes, the patient may use a rescue medication as directed by their healthcare provider.[2]
DOSAGE FORMS AND STRENGTHS
- Nasal spray; each spray delivers 100 mcL of solution containing either 100 mcg or 400 mcg fentanyl base. [3] Supplied in a 5 mL bottle containing 8 sprays.
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Clinically significant respiratory and CNS depression can occur. Monitor patients accordingly. [5.1]
- Do not convert patients to Lazanda from other fentanyl products on a mcg per mcg basis, or substitute a Lazanda prescription for another fentanyl product, such substitution may result in fatal overdose. [5.2]
- Lazanda bottles contain medicine that can be fatal to a child. Ensure proper storage and disposal. [5.3, 16.2, 16.3]
- Use with other CNS depressants and potent CYP450 3A4 inhibitors may increase depressant effects including hypoventilation, hypotension, and profound sedation. Consider dosage adjustments if warranted. [5.2, 5.4]
- Titrate Lazanda cautiously in patients with chronic obstructive pulmonary disease or preexisting medical conditions predisposing them to respiratory depression and in patients susceptible to intracranial effects of CO2 retention. [5.2, 5.6, 5.7]
ADVERSE REACTIONS
- Most common (frequency ≥5%): vomiting, nausea, dizziness, pyrexia, and constipation. [6.1]
To report SUSPECTED ADVERSE REACTIONS, contact Archimedes Pharma at 1-866-435-6775 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
- Administer Lazanda with caution to patients with renal or hepatic impairment. [8.6]
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 7/2012
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF RESPIRATORY DEPRESSION, MEDICATION ERRORS, ABUSE POTENTIAL
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dose Titration
2.2 Maintenance Treatment
2.3 Dose Re-Adjustment
2.4 Administration of Lazanda
2.5 Discontinuation of Therapy
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Respiratory Depression
5.2 Lazanda and other Fentanyl Products
5.3 Information for Patients and Their Caregivers
5.4 Additive CNS Depressant Effects
5.5 Effects on Ability to Drive and Use Machines
5.6 Chronic Pulmonary Disease
5.7 Head Injuries and Increased Intracranial Pressure
5.8 Cardiac Disease
5.9 MAO Inhibitors
5.10 Transmucosal Immediate Release Fentanyl (TIRF) Risk Evaluation and Mitigation Strategy (REMS) Access Program
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
7 DRUG INTERACTIONS
7.1 Metabolic Drug Interactions
7.2 Non-metabolic Drug Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy – Category C
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients with Renal or Hepatic Impairment
8.7 Gender
8.8 Patients with Allergic (Seasonal) Rhinitis
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse and Addiction
9.3 Dependence
10 OVERDOSAGE
10.1 Clinical Presentation
10.2 Immediate Management
10.3 Treatment of Overdosage (Accidental Ingestion) in Opioid Non-Tolerant Patients
10.4 Treatment of Overdose in Opioid-Tolerant Patients
10.5 General Considerations for Overdose
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 Storage and Handling of Lazanda
16.2 Disposal of Lazanda
16.3 How Supplied
17 PATIENT COUNSELING INFORMATION
17.1 Patient/Caregiver Instructions
17.2 Disposal of Used Lazanda Bottles
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF RESPIRATORY DEPRESSION, MEDICATION ERRORS, ABUSE POTENTIAL
RESPIRATORY DEPRESSION
Fatal respiratory depression has occurred in patients treated with immediate-release transmucosal fentanyl, including following use in opioid non-tolerant patients and improper dosing. The substitution of Lazanda for any other fentanyl product may result in fatal overdose.
Due to the risk of respiratory depression, Lazanda is contraindicated in the management of acute or postoperative pain including headache/migraine and in opioid non-tolerant patients. [see Contraindications (4)]
Lazanda must be kept out of reach of children. [see Patient Counseling Information (17.1) and How Supplied/Storage and Handling (16.1)]
The concomitant use of Lazanda with CYP3A4 inhibitors may result in an increase in fentanyl plasma concentrations, and may cause potentially fatal respiratory depression [see Drug Interactions (7)].
MEDICATION ERRORS
Substantial differences exist in the pharmacokinetic profile of Lazanda compared to other fentanyl products that result in clinically important differences in the extent of absorption of fentanyl that could result in fatal overdose.
- When prescribing, do not convert patients on a mcg per mcg basis from any other fentanyl products to Lazanda. (2.1)
- When dispensing, do not substitute a Lazanda prescription for other fentanyl products.
ABUSE POTENTIAL
Lazanda contains fentanyl, an opioid agonist and a Schedule II controlled substance, with an abuse liability similar to other opioid analgesics. Lazanda can be abused in a manner similar to other opioid agonists, legal or illicit. This should be considered when prescribing or dispensing Lazanda in situations where the physician or pharmacist is concerned about an increased risk of misuse, abuse or diversion.
Because of the risk for misuse, abuse, addiction, and overdose, Lazanda is available only through a restricted program required by the Food and Drug Administration, called a Risk Evaluation and Mitigation Strategy (REMS). Under the Transmucosal Immediate Release Fentanyl (TIRF) REMS Access program, outpatients, healthcare professionals who prescribe to outpatients, pharmacies, and distributors must enroll in the program. [see Warnings and Precautions (5.10)] Further information is available at www.TIRFREMSaccess.com or by calling 1-866-822-1483.
-
1 INDICATIONS AND USAGE
Lazanda (fentanyl) nasal spray is indicated for the management of breakthrough pain in cancer patients 18 years of age and older who are already receiving and who are tolerant to opioid therapy for their underlying persistent cancer pain. Patients considered opioid tolerant are those who are taking at least: 60 mg of oral morphine/day, 25 mcg of transdermal fentanyl/hour, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, 25 mg oral oxymorphone/day, or an equianalgesic dose of another opioid for a week or longer. Patients must remain on around-the-clock opioids when taking Lazanda.
Lazanda is contraindicated for patients who are not already tolerant to opioids because life-threatening respiratory depression and death could occur in patients not taking chronic opioids. For this reason, Lazanda is contraindicated in the management of acute or postoperative pain, including headache/migraine, or dental pain. [4]
Lazanda is intended to be prescribed only by healthcare professionals who are knowledgeable of and skilled in the use of Schedule II opioids to treat cancer pain.
Limitations of Use:
As a part of the TIRF REMS Access program, Lazanda may be dispensed only to outpatients enrolled in the program. [see Warnings and Precautions (5.10)]. For inpatient administration of Lazanda (e.g. hospitals, hospices, and long-term care facilities that prescribe for inpatient use), patient enrollment is not required.
-
2 DOSAGE AND ADMINISTRATION
Healthcare professionals who prescribe Lazanda on an outpatient basis must enroll in the TIRF REMS Access program and comply with the requirements of the REMS to ensure safe use of Lazanda [see Warnings and Precautions (5.10)}.
As with all opioids, the safety of patients using such products is dependent on healthcare professionals prescribing them in strict conformity with their approved labeling with respect to patient selection, dosing, and proper conditions for use.
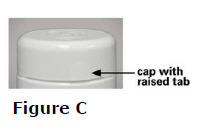
Open the child-resistant container just prior to product use and always replace the bottle in the child-resistant container between doses.
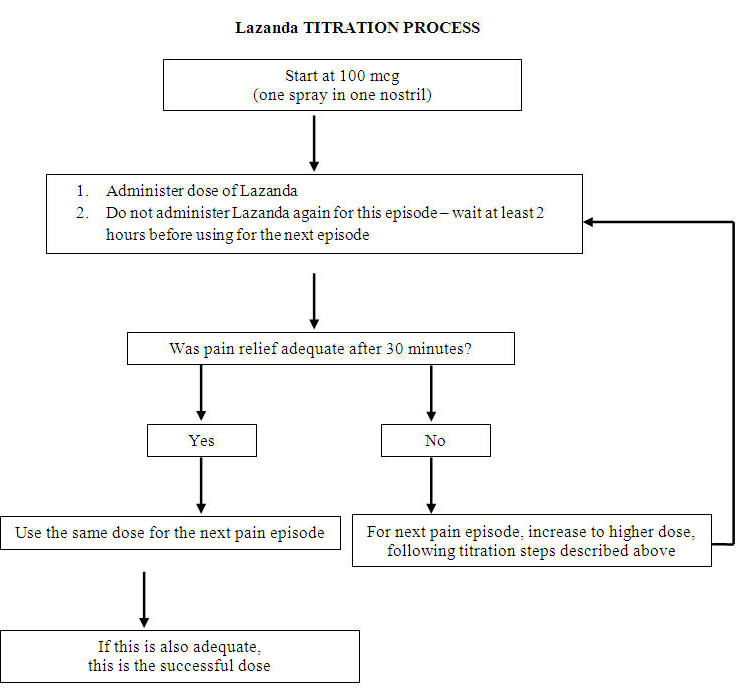
2.1 Dose Titration
The goal of dose titration is to find the individual patient's effective and tolerable dose. The dose of Lazanda is not predicted from the daily maintenance dose of opioid used to manage the persistent cancer pain and MUST be determined by dose titration.
Starting Dose: Individually titrate Lazanda to a dose that provides adequate analgesia with tolerable side effects. Begin treatment of all patients (including those switching from another fentanyl product) using ONE 100 mcg spray of Lazanda (1 spray in one nostril). Due to differences in pharmacokinetic properties and individual variability, do not switch patients on a mcg per mcg basis from any other fentanyl product to Lazanda as Lazanda is not equivalent with any other fentanyl product, nor is Lazanda a generic version of any other fentanyl product.
If adequate analgesia is obtained within 30 minutes of administration of the 100 mcg single spray, treat subsequent episodes of breakthrough pain with this dose.
Titration steps: If adequate analgesia is not achieved with the first 100 mcg dose, dose escalate in a step-wise manner over consecutive episodes of breakthrough pain until adequate analgesia with tolerable side effects is achieved.
Patients MUST wait at least 2 hours before treating another episode of breakthrough cancer pain with Lazanda.
The titration steps should be:
Lazanda Dose Using 100 mcg 1 × 100 mcg spray 200 mcg 2 × 100 mcg spray (1 in each nostril) 400 mcg 1 × 400 mcg 800 mcg 2 × 400 mcg (1 in each nostril) Patients should confirm the dose of Lazanda that works for them with a second episode of breakthrough pain and review their experience with their physicians to determine if that dose is appropriate, or whether a further adjustment is warranted.
The safety and efficacy of doses higher than 800 mcg have not been evaluated in clinical studies. There are no clinical data to support the use of a combination of dose strengths to treat an episode.
In order to minimize the risk of Lazanda-related adverse reactions and to identify the appropriate dose, it is imperative that patients be supervised closely by health professionals during the titration process.
2.2 Maintenance Treatment
Once an appropriate dose has been established, instruct patients to use that dose for each subsequent breakthrough cancer pain episode. Limit Lazanda use to four or fewer doses per day.
Patients MUST wait at least 2 hours before treating another episode of breakthrough cancer pain with Lazanda.
During any episode of breakthrough cancer pain, if there is inadequate pain relief after 30 minutes following Lazanda dosing or if a separate episode of breakthrough cancer pain occurs before the next dose of Lazanda is permitted (i.e. within 2 hours), the patients may use a rescue medication as directed by their healthcare provider.
2.3 Dose Re-Adjustment
If the response (analgesia or adverse reactions) to the titrated Lazanda dose markedly changes, an adjustment of dose may be necessary to ensure that an appropriate dose is maintained.
If more than four episodes of breakthrough pain are experienced per day, re-evaluate the dose of the long-acting opioid used for persistent underlying cancer pain. If the long-acting opioid or dose of long-acting opioid is changed, re-evaluate and re-titrate the Lazanda dose as necessary to ensure the patient is on an appropriate dose.
Limit the use of Lazanda to treat four or fewer episodes of breakthrough pain per day.
It is imperative that any dose re-titration is monitored carefully by a healthcare professional.
2.4 Administration of Lazanda
Instruct patients on the proper use of Lazanda.
- Prime the device before use by spraying into the pouch (4 sprays in total) following the instructions for use in the Medication Guide [17.3].
- Insert the nozzle of the Lazanda bottle a short distance (about ½ inch or 1 cm) into the nose and point towards the bridge of the nose, tilting the bottle slightly.
- Press down firmly on the finger grips until they hear a "click" and the number in the counting window advances by one.
Advise patients that the fine mist spray is not always felt on the nasal mucosal membrane and to rely on the audible click and the advancement of the dose counter to confirm a spray has been administered.
2.5 Discontinuation of Therapy
For patients no longer requiring opioid therapy, consider discontinuing Lazanda along with a gradual downward titration of other opioids to minimize possible withdrawal effects.
In patients who continue to take their chronic opioid therapy for persistent pain but no longer require treatment for breakthrough pain, Lazanda therapy can usually be discontinued immediately.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Lazanda is contraindicated in the management of pain in opioid non-tolerant patients, because life-threatening hypoventilation could occur at any dose in patients not already taking around-the-clock opioid therapy.
Patients considered opioid tolerant are those who are taking at least: 60 mg oral morphine/day, 25 mcg transdermal fentanyl/hour, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, 25 mg oral oxymorphone/day, or an equianalgesic dose of another opioid for a week or longer.
Lazanda is contraindicated in the management of acute or postoperative pain, including headache/migraine, or dental pain.
Lazanda is contraindicated in patients with known intolerance or hypersensitivity to any of its components or the drug fentanyl. Anaphylaxis and hypersensitivity have been reported in association with the use of other oral transmucosal fentanyl products.
-
5 WARNINGS AND PRECAUTIONS
5.1 Respiratory Depression
Serious or fatal respiratory depression can occur even at recommended doses in patients using Lazanda. Respiratory depression is more likely to occur in patients with underlying respiratory disorders and elderly or debilitated patients, in opioid non-tolerant patients, or when opioids are given in conjunction with other drugs that depress respiration.
Respiratory depression from opioids is manifested by a reduced urge to breathe and a decreased rate of respiration, often associated with a "sighing" pattern of breathing (deep breaths separated by abnormally long pauses). Carbon dioxide retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids. This makes overdoses involving drugs with sedative properties and opioids especially dangerous.
5.2 Lazanda and other Fentanyl Products
Lazanda is NOT equivalent to other fentanyl products used to treat breakthrough pain on a mcg per mcg basis. There are differences in the pharmacokinetics of Lazanda relative to other fentanyl products which could potentially result in clinically important differences in the amount of fentanyl absorbed and could result in a fatal overdose.
When prescribing Lazanda to a patient, DO NOT convert from other fentanyl products. Directions for safely converting patients to Lazanda from other fentanyl products are not currently available. (Note: This includes oral, transdermal, or parenteral formulations of fentanyl). Therefore, for opioid-tolerant patients starting treatment for breakthrough pain, the initial dose of Lazanda is 100 mcg. Individually titrate each patient's dose to provide adequate analgesia while minimizing side effects. [See Dosage and Administration (2.1)]
When dispensing Lazanda to a patient, DO NOT substitute it for any other fentanyl product prescription.
5.3 Information for Patients and Their Caregivers
Patients and their caregivers must be instructed that Lazanda contains medicine in an amount that could be fatal to a child.
Patients and their caregivers must be instructed to keep both used and unused bottles in their child-resistant container and out of the reach of children at all times. Partially used bottles represent a special risk to children. As soon as they are no longer required, all used, unopened or partially used bottles must be completely emptied of accessible fentanyl solution by spraying the remaining contents into the carbon-lined pouch. The sealed pouch and the empty bottle should be put into the child-resistant container before discarding in the trash. Hands must be washed with soap and water immediately after handling the pouch. [see Storage and Handling (16.2), Disposal of Lazanda (16.3), and Patient/Caregiver Instructions (17.1)].
Physicians and dispensing pharmacists must question patients and caregivers specifically about the presence of children in the home on a full-time or visiting basis and counsel accordingly regarding the dangers to children of inadvertent exposure to Lazanda.
Lazanda could be fatal to individuals for whom it is not prescribed and for those who are not opioid tolerant.
5.4 Additive CNS Depressant Effects
The concomitant use of Lazanda with other CNS depressants, including other opioids, sedatives or hypnotics, general anesthetics, phenothiazines, tranquilizers, skeletal muscle relaxants, sedating antihistamines, and alcoholic beverages may produce increased depressant effects (e.g., hypoventilation, hypotension, and profound sedation). Concomitant use with potent inhibitors of cytochrome P450 3A4 isoform (e.g., erythromycin, ketoconazole, and certain protease inhibitors) may increase fentanyl levels, resulting in increased depressant effects [see Metabolic Drug Interactions (7.1)].
Patients on concomitant CNS depressants must be monitored for a change in opioid effects and may require adjustment of the dose of Lazanda.
5.5 Effects on Ability to Drive and Use Machines
Opioid analgesics impair the mental and/or physical ability required for the performance of potentially dangerous tasks (e.g., driving a car or operating machinery). Warn patients taking Lazanda of these dangers and counsel them accordingly.
5.6 Chronic Pulmonary Disease
Because potent opioids can cause respiratory depression, cautiously adjust the dose of Lazanda in patients with chronic obstructive pulmonary disease or preexisting medical conditions predisposing them to respiratory depression. In such patients, even normal therapeutic doses of Lazanda may further decrease respiratory drive to the point of respiratory failure.
5.7 Head Injuries and Increased Intracranial Pressure
Administer Lazanda with extreme caution in patients who may be particularly susceptible to the intracranial effects of CO2 retention, such as those with evidence of increased intracranial pressure or impaired consciousness. Opioids may obscure the clinical course of a patient with a head injury; only use opioids if clinically warranted.
5.8 Cardiac Disease
Intravenous fentanyl may produce bradycardia. Use Lazanda with caution in patients with bradyarrhythmias.
5.9 MAO Inhibitors
Lazanda is not recommended for use in patients who have received MAO inhibitors within 14 days, because severe and unpredictable potentiation by MAO inhibitors has been reported with opioid analgesics. [see Non-metabolic Drug Interactions (7.2)].
5.10 Transmucosal Immediate Release Fentanyl (TIRF) Risk Evaluation and Mitigation Strategy (REMS) Access Program
Because of the risk of misuse, abuse, addiction, and overdose [see Drug Abuse and Dependence (9)], Lazanda is available only through a restricted program under a REMS called the TIRF REMS Access program. Under the TIRF REMS Access program, outpatients, healthcare professionals who prescribe to outpatients, pharmacies, and distributors must enroll in the program. For inpatient administration (e.g. hospitals, hospices, and long-term care facilities that prescribe for inpatient use) of Lazanda, patient and prescriber enrollment is not required.
Required components of the TIRF REMS Access program are:
- Healthcare professionals who prescribe Lazanda must review the prescriber educational materials for the TIRF REMS Access program, enroll in the program, and comply with the REMS requirements.
- To receive Lazanda, outpatients must understand the risks and benefits and sign a Patient-Prescriber Agreement.
- Pharmacies that dispense Lazanda must enroll in the program and agree to comply with the REMS requirements.
- Wholesalers and distributers that distribute Lazanda must enroll in the program and distribute only to authorized pharmacies.
Further information, including a list of qualified pharmacies/distributors, is available at www.tirfremsaccess.com or by calling 1-866-822-1483.
-
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse event rates observed in the clinical trials of a drug product cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of Lazanda has been evaluated in a total of 523 opioid-tolerant patients with breakthrough cancer pain. The average duration of therapy in patients in the long-term study was 73 days, with 153 patients being treated for over 3 months. Patients continuing into the open-label extension period of the safety study have been treated for up to 26 months.
The most commonly observed adverse events seen with Lazanda are typical of opioid side effects, such as nausea, constipation, somnolence, and headache. Expect opioid side effects and manage them accordingly.
The clinical trials of Lazanda were designed to evaluate safety and efficacy in treating breakthrough cancer pain; all patients were also taking concomitant opioids, such as sustained-release morphine, sustained-release oxycodone, or transdermal fentanyl, for their persistent cancer pain. The adverse reaction data presented in Table 1 reflect the actual percentage of patients experiencing each adverse effect among patients who received Lazanda for breakthrough cancer pain along with a concomitant opioid for persistent cancer pain. There has been no attempt to correct for concomitant use of other opioids, duration of Lazanda therapy, or cancer-related symptoms. Adverse events are included regardless of causality or severity. Table 1 lists adverse reactions with an overall frequency of 5% or greater within the total population that occurred during titration by maximum dose received. The ability to assign Lazanda a dose-response relationship to these adverse events is limited by the titration schemes used in these studies.
Table 1: Adverse Reactions That Occurred During Titration at a Frequency of ≥5% System Organ Class
MeDRA preferred term, n (%)100 mcg
(N=483)200 mcg
(N=380)400 mcg
(N=301)800 mcg
(N=161)Total
(N=516)Gastrointestinal disorders Nausea 19 (4) 6 (2) 6 (2) 5 (3) 35 (7) Vomiting 14 (3) 10 (3) 9 (3) 1 (1) 33 (6) Nervous system disorders Dizziness 14 (3) 11 (3) 6 (2) 4 (2) 31 (6) Table 2 lists, by dose, adverse reactions with an overall frequency of ≥5% within the total population that occurred after a final titrated dose had been determined.
Table 2: Adverse Reactions That Occurred During Maintenance Treatment at a Frequency of ≥5% System Organ Class
MeDRA preferred term, n (%)100 mcg
(N=61)200 mcg
(N=68)400 mcg
(N=109)800 mcg
(N=108)Total
(N=346)Gastrointestinal disorders Vomiting 8 (13) 5 (7) 9 (8) 12 (11) 34 (10) Nausea 4 (7) 6 (9) 4 (4) 9 (8) 23 (7) Constipation 6 (10) 1 (1) 8 (7) 5 (5) 20 (6) General disorders and administration site conditions Pyrexia 3 (5) 5 (7) 8 (7) 6 (6) 22 (6) The adverse reactions listed below represent those that occurred in ≥1% of patients from clinical trials while receiving Lazanda. Events are classified by system organ class.
Adverse Events (≥1%)
Eye disorders: dry eye, swelling, ptosis, strabismus
Blood and Lymphatic System Disorders: anemia, neutropenia
Cardiac Disorders: cardiorespiratory arrest
Gastrointestinal Disorders: vomiting, nausea, constipation, diarrhea, abdominal pain, gastritis, ascites, dry mouth, dyspepsia, mouth ulcer, proctalgia
General Disorders and Administration Site Conditions: pyrexia, fatigue, edema peripheral, asthenia, edema
Hepatobiliary Disorders: jaundice
Immune System Disorders: hypersensitivity
Infections and Infestations: urinary tract infection, pneumonia, nasopharyngitis, infection, rhinitis, upper respiratory tract infection, bronchitis
Injury, Poisoning and Procedural Complications: fall
Investigations: weight decreased, blood alkaline phosphatase increased
Metabolism and Nutrition Disorders: dehydration, decreased appetite, hyperglycemia, anorexia
Musculoskeletal and Connective Tissue Disorders: back pain, pain in extremity, arthralgia
Nervous System Disorders: dizziness, somnolence, headache, dysgeusia
Psychiatric Disorders: anxiety, insomnia, depression, confusional state, disorientation, agitation
Respiratory, Thoracic and Mediastinal Disorders: dyspnea, epistaxis, cough, pharyngolaryngeal pain, nasal discomfort, rhinorrhea, nasal congestion, postnasal drip, pulmonary embolism
Skin and Subcutaneous Tissue Disorders: pruritus, hyperhidrosis, decubitus ulcer, mouth ulceration
Vascular Disorders: hypertension, deep vein thrombosis -
7 DRUG INTERACTIONS
7.1 Metabolic Drug Interactions
Fentanyl is metabolized mainly via the human cytochrome P450 3A4 isoenzyme system (CYP3A4); therefore potential interactions may occur when Lazanda is given concurrently with agents that affect CYP3A4 activity.
CYP3A4 inhibitors
The concomitant use of Lazanda with CYP3A4 inhibitors (e.g., indinavir, nelfinavir, ritonavir, clarithromycin, itraconazole, ketoconazole, nefazodone, saquinavir, telithromycin, aprepitant, diltiazem, erythromycin, fluconazole, grapefruit juice, verapamil, or cimetidine) may result in a potentially dangerous increase in fentanyl plasma concentrations, which could increase or prolong adverse drug effects and may cause potentially fatal respiratory depression. Patients receiving Lazanda who begin therapy with, or increase the dose of, CYP3A4 inhibitors are to be carefully monitored for signs of opioid toxicity over an extended period of time. Increase dose conservatively [see Warnings and Precautions (5.4)].
CYP3A4 inducers
The concomitant use of Lazanda with CYP3A4 inducers (e.g., barbiturates, carbamazepine, efavirenz, glucocorticoids, modafinil, nevirapine, oxcarbazepine, phenobarbital, phenytoin, pioglitazone, rifabutin, rifampin, St. John's wort, or troglitazone) may result in a decrease in fentanyl plasma concentrations, which could decrease the efficacy of Lazanda. Patients receiving Lazanda who stop therapy with, or decrease the dose of, CYP3A4 inducers may experience sudden increase in fentanyl plasma concentrations and are to be monitored for signs of increased Lazanda activity. Adjust the dose of Lazanda accordingly.
7.2 Non-metabolic Drug Interactions
Agents used to treat Allergic Rhinitis
The presence of allergic rhinitis is not expected to affect Lazanda absorption. However, co-administration of a vasoconstrictive nasal decongestant such as oxymetazoline to treat allergic rhinitis leads to lower peak plasma concentrations and a delayed Tmax of fentanyl that may cause Lazanda to be less effective in patients with allergic rhinitis who use such decongestants, thus potentially impairing pain management. Additionally, in view of the possibility that the titration of a patient while they are experiencing an acute episode of rhinitis could lead to incorrect dose identification (particularly if they are using a vasoconstrictive decongestant), titration under these circumstances must be avoided [see Clinical Pharmacology (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy – Category C
There are no adequate and well-controlled studies in pregnant women.
Use Lazanda during pregnancy only if the potential benefit justifies the potential risk to the fetus. No epidemiological studies of congenital anomalies in infants born to women treated with fentanyl during pregnancy have been reported.
Chronic maternal treatment with fentanyl during pregnancy has been associated with transient respiratory depression, behavioral changes, or seizures in newborn infants characteristic of neonatal abstinence syndrome.
In women treated acutely with intravenous or epidural fentanyl during labor, symptoms of neonatal respiratory or neurological depression were no more frequent than would be expected in infants of untreated mothers.
Transient neonatal muscular rigidity has been observed in infants whose mothers were treated with intravenous fentanyl.
Fentanyl is embryocidal in rats as evidenced by increased resorptions in pregnant rats at doses of 30 mcg/kg IV or 160 mcg/kg SC. Conversion to human equivalent doses indicates this is within the range of the human recommended dosing for Lazanda.
Fentanyl citrate was not teratogenic when administered to pregnant animals. Published studies demonstrated that administration of fentanyl (10, 100, or 500 mcg/kg/day) to pregnant rats from day 7 to 21 of their 21 day gestation, via implanted microosmotic minipumps was not teratogenic. The high dose was approximately 3 times the human dose of 800 mcg per pain episode on a mg/m2 basis. Intravenous administration of fentanyl (10 or 30 mcg/kg) to pregnant female rats from gestation days 6 to 18 was embryo or fetal toxic and caused a slightly increased mean delivery time in the 30 mcg/kg/day group, but it was not teratogenic.
8.2 Labor and Delivery
Fentanyl readily passes across the placenta. Therefore do not use Lazanda during labor and delivery (including caesarean section) since it may cause respiratory depression in the fetus or in the newborn infant.
8.3 Nursing Mothers
Fentanyl is excreted in human milk; therefore, do not use Lazanda in women who are nursing because of the risk of sedation and/or respiratory depression in their infants. Symptoms of opioid withdrawal may occur in infants upon cessation of nursing by women using Lazanda.
8.4 Pediatric Use
The safety and efficacy of Lazanda have not been established in patients below the age of 18 years.
8.5 Geriatric Use
Of the 523 opioid tolerant cancer patients with breakthrough cancer pain in clinical studies of Lazanda, 148 (28%) were aged 60 years and over. No clinically meaningful difference was noted in the safety profile of the group aged over 60 years versus that of younger patients in Lazanda clinical trials.
Elderly patients have been shown to be more sensitive to the effects of fentanyl when administered intravenously compared with the younger population. Therefore, exercise caution when individually titrating Lazanda in elderly patients.
8.6 Patients with Renal or Hepatic Impairment
Insufficient information exists to make recommendations regarding the use of Lazanda in patients with impaired renal or hepatic function. Fentanyl is metabolized primarily via the human CYP3A4 isoenzyme system and the inactive metabolite is mostly eliminated in urine. If the drug is used in these patients, it is to be used with caution because of the hepatic metabolism and renal excretion of fentanyl.
It is recommended that Lazanda be titrated to clinical effect for all patients with special care taken in patients with severe renal or hepatic disease.
8.7 Gender
Both male and female opioid-tolerant cancer patients were studied for the treatment of breakthrough cancer pain. No clinically relevant gender differences were observed in adverse events.
8.8 Patients with Allergic (Seasonal) Rhinitis
The pharmacokinetic and safety profiles of Lazanda in individuals with known allergic (seasonal) rhinitis showed no clinically meaningful differences in rate or extent of exposure to fentanyl, or in local tolerability of Lazanda when compared to Asymptomatic (Unchallenged) state. However, when treated for their rhinitis with oxymetazoline, Lazanda absorption was compromised [see Pharmacokinetics (12.3)].
-
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Lazanda contains fentanyl, which is a Schedule II controlled substance. Schedule II substances such as fentanyl, hydromorphone, methadone, morphine, oxycodone, and oxymorphone have a high potential for abuse and addiction. Lazanda may be subject to misuse and criminal diversion.
9.2 Abuse and Addiction
Manage the handling of Lazanda to minimize the risk of abuse, including restriction of access and accounting procedures as appropriate to the clinical setting and as required by law [see How Supplied/Storage and Handling (16.1, 16.2)].
Concerns about abuse and addiction should not prevent the proper management of pain. However, all patients treated with opioids require careful monitoring for signs of abuse and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Addiction is a primary, chronic, neurobiologic disease, with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving. Drug addiction is a treatable disease, utilizing a multidisciplinary approach, but relapse is common. "Drug-seeking" behavior is very common in addicts and drug abusers.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of opioids can occur in the absence of addiction and is characterized by misuse for nonmedical purposes, often in combination with other psychoactive substances. Since Lazanda may be abused or diverted for nonmedical use, careful record keeping of prescribing information, including quantity, frequency, and renewal requests, is strongly advised.
Proper assessment of patients, proper prescribing practices, periodic reevaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
Contact your State Professional Licensing Board or State Controlled Substances Authority for information on how to prevent and detect abuse or diversion of this product.
9.3 Dependence
Physical dependence is not ordinarily a concern when treating a patient with cancer and chronic pain, and fear of tolerance and physical dependence should not deter using doses that adequately relieve the pain. Guide the administration of Lazanda by the response of the patient.
Opioid analgesics may cause physical dependence. Physical dependence results in withdrawal symptoms in patients who abruptly discontinue the drug. Withdrawal also may be precipitated through the administration of drugs with opioid antagonist activity, e.g., naloxone, nalmefene, or mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, buprenorphine, nalbuphine).
Physical dependence usually does not occur to a clinically significant degree until after several weeks of continued opioid usage. Tolerance, in which increasingly larger doses are required in order to produce the same degree of analgesia, initially manifests as a shortened duration of analgesic effect, and subsequently as decreases in the intensity of analgesia.
-
10 OVERDOSAGE
10.1 Clinical Presentation
The manifestations of overdosage with Lazanda are expected to be similar to those for intravenous fentanyl and other opioids, and are an extension of its pharmacological actions, with the most serious significant adverse effect being hypoventilation [see Clinical Pharmacology (12)].
10.2 Immediate Management
Immediate management of opioid overdose includes removal of the Lazanda pectin gel, if still in the nostril, ensuring a patent airway, physical and verbal stimulation of the patient, and assessment of level of consciousness, ventilatory status, and circulatory status.
10.3 Treatment of Overdosage (Accidental Ingestion) in Opioid Non-Tolerant Patients
Provide ventilatory support, obtain intravenous access, and administer naloxone or other opioid antagonists as clinically indicated. The duration of respiratory depression following overdose may be longer than the effects of the opioid antagonist's action (e.g., the half-life of naloxone ranges from 30 to 81 minutes) and repeated administration may be necessary. Consult the package insert of the individual opioid antagonist for details about such use.
10.4 Treatment of Overdose in Opioid-Tolerant Patients
Provide ventilatory support and obtain intravenous access as clinically indicated. Judicious use of naloxone or another opioid antagonist may be warranted in some instances, but it is associated with the risk of precipitating an acute withdrawal syndrome.
10.5 General Considerations for Overdose
Management of severe Lazanda overdose includes: securing a patent airway, assisting or controlling ventilation, and establishing intravenous access. In the presence of hypoventilation or apnea, assist or control ventilation, and administer oxygen as indicated.
Carefully observe and appropriately manage overdosed patients until their clinical condition is well controlled.
Although muscle rigidity interfering with respiration has not been observed following the use of Lazanda, this is possible with fentanyl and other opioids. If it occurs, manage by the use of assisted or controlled ventilation, by administration of an opioid antagonist, and, as a final alternative, by the administration of a neuromuscular blocking agent.
-
11 DESCRIPTION
Lazanda (fentanyl) nasal spray is a liquid formulation of fentanyl citrate intended for intranasal transmucosal administration. The product consists of a practically clear to clear, colorless, aqueous solution of fentanyl citrate in a glass multidose container to which is attached a metered-dose nasal spray pump with a visual and audible spray counter. Each actuation is designed to deliver a spray of 100 mcL of solution containing 100 mcg or 400 mcg fentanyl base, respectively. This enables doses of 100 mcg or 400 mcg to be administered using a single spray into one nostril (1 spray) and 200 mcg or 800 mcg to be administered using a single spray into both nostrils (2 sprays).
Active ingredient: Fentanyl citrate, USP is N-(l-phenethyl-4-piperidyl) propionanilide citrate (1:1). Fentanyl is a highly lipophilic compound (octanol-water partition coefficient at pH 7.4 is 816:1). Fentanyl citrate is sparingly soluble in water (1:40). The molecular weight of the free base and citrate salt are 336.5 and 528.6, respectively. The pKa is 8.4. The compound has the following structural formula:
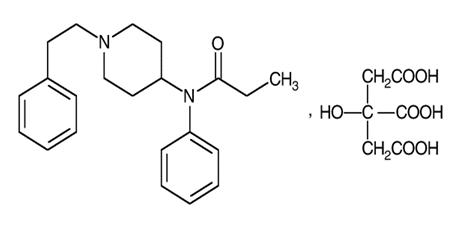
Lazanda is available in 2 strengths of nasal spray: 100 mcg fentanyl (yellow label) and 400 mcg fentanyl (violet label). The strength is expressed as the amount of fentanyl free base per spray, e.g., the 100 mcg strength provides 100 mcg of fentanyl free base per 100 mcL spray.
Inactive ingredients: mannitol, pectin, phenylethyl alcohol, propylparaben, sucrose, water. Sodium hydroxide and/or hydrochloric acid are added if required for pH adjustment.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Fentanyl is a pure opioid agonist whose principal therapeutic action is analgesia. Other members of the class known as opioid agonists include substances such as morphine, oxycodone, hydromorphone, codeine, and hydrocodone.
12.2 Pharmacodynamics
Pharmacological effects of opioid agonists include anxiolysis, euphoria, feelings of relaxation, respiratory depression, constipation, miosis, cough suppression, and analgesia. Like all pure opioid agonist analgesics, with increasing doses there is increasing analgesia, unlike with mixed agonist/antagonists or non-opioid analgesics, where there is a limit to the analgesic effect with increasing doses. With pure opioid agonist analgesics, there is no defined maximum dose; the ceiling to analgesic effectiveness is imposed only by side effects, the more serious of which may include somnolence, respiratory depression and death.
Analgesia: In general, the effective concentration and the concentration at which toxicity occurs increase with increasing tolerance to any and all opioids.
The rate of development of tolerance varies widely among individuals. As a result, individually titrate the dose of Lazanda to achieve the desired effect. [see Dosage and Administration (2)].
Central Nervous System: The precise mechanism of the analgesic action is unknown although fentanyl is known to be a mu-opioid receptor agonist. Specific CNS opioid receptors for endogenous compounds with opioid-like activity have been identified throughout the brain and spinal cord and play a role in the analgesic effects of this drug.
Fentanyl produces respiratory depression by direct action on brain stem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem to increases in carbon dioxide and to electrical stimulation.
Fentanyl causes miosis even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origin may produce similar findings).
Gastrointestinal System: Fentanyl causes a reduction in motility associated with an increase in smooth muscle tone in the antrum of the stomach and in the duodenum. Digestion of food is delayed in the small intestine and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone may be increased to the point of spasm resulting in constipation. Other opioid-induced effects may include a reduction in gastric, biliary, and pancreatic secretions, spasm of the sphincter of Oddi, and transient elevations in serum amylase.
Cardiovascular System: Fentanyl may produce release of histamine with or without associated peripheral vasodilation. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes, sweating, and/or orthostatic hypotension.
Endocrine System: Opioid agonists have been shown to have a variety of effects on the secretion of hormones. Opioids inhibit the secretion of ACTH, cortisol, and luteinizing hormone (LH) in humans. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon in humans and other species (e.g., rats and dogs). Thyroid stimulating hormone (TSH) has been shown to be both inhibited and stimulated by opioids.
Respiratory System: All opioid mu-receptor agonists, including fentanyl, produce dose-dependent respiratory depression. The risk of respiratory depression is less in patients receiving chronic opioid therapy who develop tolerance to respiratory depression and other opioid effects.
Serious or fatal respiratory depression can occur even at recommended doses. Fentanyl depresses the cough reflex as a result of its CNS activity. Although not observed with Lazanda, in clinical trials, fentanyl given rapidly by intravenous injection in large doses has interfered with respiration by causing rigidity in the muscles of respiration. Physicians and other healthcare providers should be aware of this potential complication. [see Boxed Warning - Warning: Risk of Respiratory Depression, Medication Errors, Abuse Potential, Contraindications (4), Warnings and Precautions (5), Adverse Reactions (6), and Overdosage (10) for additional information on hypoventilation].
12.3 Pharmacokinetics
Absorption: In a study that compared the relative bioavailability of Lazanda and an oral transmucosal fentanyl citrate product, the bioavailability of fentanyl from Lazanda was approximately 20% higher. Fentanyl is absorbed from the nasal mucosa following intranasal administration of Lazanda, with median Tmax values ranging from 15-21 min after administration of a single dose. Cmax and AUC values for fentanyl following administration of Lazanda increase linearly over the 100- to 800-mcg dose range.
Mean plasma concentration versus time profiles are presented in Figure 1. Mean pharmacokinetic parameters are presented in Table 3.
Figure 1.
Mean Plasma Fentanyl Concentration (pg/mL) in Normal Subjects Receiving 100, 200, 400 and 800 mcg Lazanda or 200 mcg OTFC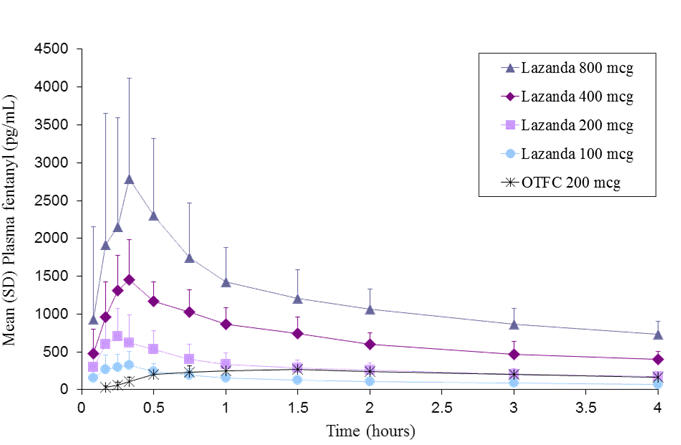
Table 3. Pharmacokinetic Parameters in Normal Subjects Receiving 100, 200, 400, and 800 mcg of Lazanda or 200 mcg OTFC Lazanda OTFC PHARMACOKINETIC PARAMETERS 100 mcg 200 mcg 400 mcg 800 mcg 200 mcg Tmax, hours
median (range)0.33
(0.08–1.50)0.25
(0.17–1.60)0.35
(0.25–0.75)0.34
(0.17–3.00)1.50
(0.50–8.00)Cmax, pg/mL
Mean (%CV)351.5
(51.3)780.8
(48.4)1552.1
(26.2)2844.0
(56.0)317.4
(29.9)AUCinf, pg.hour/mL
Mean (%CV)2460.5
(17.9)4359.9
(29.8)7513.4
(26.7)17272
(48.9)3735.0
(32.8)t1/2, hour
Mean (%CV)21.9
(13.6)24.9
(51.3)15.0
(24.7)24.9
(92.5)18.6
(31.4)In a pharmacokinetic study that evaluated multiple-dose pharmacokinetics of Lazanda when two doses of Lazanda are administered in the same nostril and are separated by a 1, 2 or 4 h time lapse, Cmax2 (Cmax after second administration) was greater than Cmax1 (Cmax after first administration), by 30% when Lazanda was administered 1 h apart, by 25% when Lazanda was administered 2 h apart and by 10% when Lazanda was administered 4 h apart. Based on these results and based on Tmax range of Lazanda observed across pharmacokinetic studies, and frequency of breakthrough pain episodes in a cancer population, a waiting period of 2 h between two consecutive doses of Lazanda is recommended [see Dosage and Administration (2)].
In a pharmacokinetic study to evaluate differences in Lazanda absorption in individuals with induced allergic (seasonal) rhinitis, no clinically meaningful differences were observed in rate or extent of exposure to fentanyl, when compared to the Asymptomatic (Unchallenged) state, indicating that presence of allergic rhinitis does not affect Lazanda absorption. This study also assessed differences in Lazanda absorption, if any, when co-administered with oxymetazoline, a nasal decongestant in subjects undergoing treatment for seasonal allergic rhinitis. Mean Cmax values for Treated arm (Rhinitis treated with oxymetazoline) were about 32% and 40% lower and mean AUCt values were about 10% and 17% lower for Ragweed and Tree pollen induced cohorts respectively as compared to the Asymptomatic arm in each cohort. In addition, mean Tmax of Lazanda in the Treated arm was 0.75 h (range 0.08-3 h) for the Ragweed pollen induced cohort and 1.25 h (range 0.08-3 h) for Tree pollen induced cohort as compared to 0.25 h (0.17-1 h) and 0.33 h (0.17-2 h) for the Asymptomatic arm in each cohort respectively. These results indicate that co-administration with oxymetazoline leads to lower peak plasma concentrations and delayed Tmax of Lazanda [see Drug Interactions (7.2)].
Distribution: Fentanyl is highly lipophilic. The plasma protein binding of fentanyl is 80% to 85%. The main binding protein is alpha-1-acid glycoprotein, but both albumin and lipoproteins contribute to some extent. The mean volume of distribution at steady state (Vss) was 4 L/kg.
Metabolism: The metabolic pathways following intranasal administration of Lazanda have not been characterized in clinical studies. The progressive decline of fentanyl plasma concentrations results from the uptake of fentanyl in the tissues and biotransformation in the liver. Fentanyl is metabolized in the liver and in the intestinal mucosa to norfentanyl by cytochrome P450 3A4 isoform. In animal studies, norfentanyl was not found to be pharmacologically active.
Elimination: The disposition of fentanyl following intranasal administration of Lazanda has not been characterized in a mass balance study. Fentanyl is primarily (more than 90%) eliminated by biotransformation to N-dealkylated and hydroxylated inactive metabolites. Less than 7% of the administered dose is excreted unchanged in the urine, and only about 1% is excreted unchanged in the feces. The metabolites are mainly excreted in the urine, while fecal excretion is less important.
The total plasma clearance of fentanyl following intravenous administration is approximately 42 L/h.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have not been performed to evaluate the carcinogenic potential of fentanyl.
Fentanyl citrate was not mutagenic in the in vitro Ames reverse mutation assay in S. typhimurium or E. coli, or the mouse lymphoma mutagenesis assay, and was not clastogenic in the in vivo mouse micronucleus assay.
Fentanyl has been shown to impair fertility in rats at doses of 30 mcg/kg subcutaneously. Conversion to human equivalent doses indicates this is within the range of the human recommended dosing for Lazanda.
-
14 CLINICAL STUDIES
The efficacy of Lazanda was evaluated in one clinical trial in opioid tolerant adult patients experiencing breakthrough cancer pain. Breakthrough cancer pain was defined as a transient flare of moderate-to-severe pain occurring in patients experiencing persistent cancer pain otherwise controlled with maintenance doses of opioid medications including at least 60 mg of oral morphine/day or an equianalgesic dose of another opioid (which could be fentanyl) for a week or longer. All patients were on stable doses of either long-acting oral opioids or transdermal fentanyl for their persistent cancer pain.
The clinical trial included an open-label titration phase where a dose was identified that provided adequate analgesia with tolerable side effects, within the range of 100 to 800 mcg. In the double-blind, placebo-controlled portion of the study, patients who were titrated to an adequate dose were randomized to a blinded sequence of 10 treatments with 7 being the identified dose of Lazanda and 3 being placebo.
Of the patients who enrolled in the study, 73% achieved an adequate dose during the titration phase, 6% withdrew for lack of effective pain relief, and 5% withdrew due to adverse events.
The distribution of final titrated doses is shown in Table 4. The final titrated dose of Lazanda for breakthrough pain was not predicted from the daily maintenance dose of opioid used to manage the persistent cancer pain and, therefore, the dose was determined by titration starting at 100 mcg.
Table 4. Dose of Lazanda Following Initial Titration (ITT population) Lazanda Dose (N=83) n (%) 100 mcg 12 (14) 200 mcg 7 (8) 400 mcg 27 (33) 800 mcg 37 (45) The primary outcome measure, the mean sum of the pain intensity difference at 30 minutes (SPID30), was statistically significantly higher for Lazanda than for placebo (see Figure 2).
Figure 2. Pain Intensity Differences (PID) following Lazanda or Placebo in Adult Patients with Breakthrough Cancer Pain 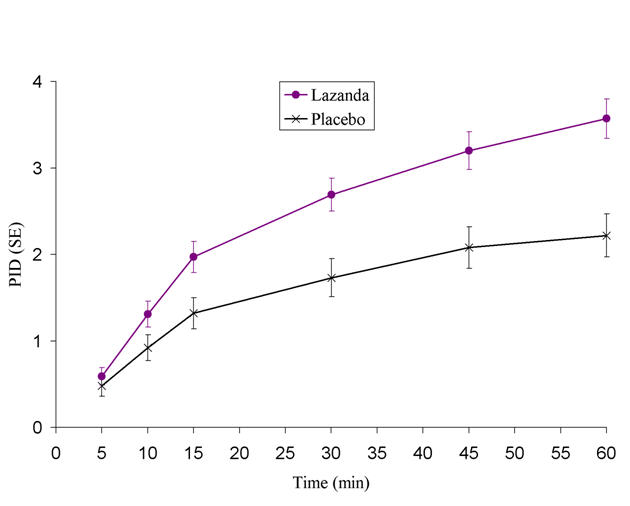
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 Storage and Handling of Lazanda
Lazanda is supplied in glass bottles, containing 8 sprays of 100 mcL containing 100 mcg/100 mcL or 400 mcg/100 mcL concentration solution. Each bottle is supplied in a child-resistant container.
The amount of fentanyl contained in Lazanda can be fatal to a child, individual for whom it is not prescribed or non-opioid tolerant adult. Patients and their caregivers must be instructed to keep Lazanda out of the reach of children [see Boxed Warning - Warning: Risk of Respiratory Depression, Medication Errors, Abuse Potential, Warnings and Precautions (5), and Patient Counseling Information (17.1)].
Store at up to 25°C. Do not freeze.
Return the bottle to the child-resistant container after each use. Put the bottle in its child-resistant container and the pouch in the cardboard carton and store securely out of the reach of children and protect from light.
Note: Carton and bottle label colors are a secondary aid in product identification. Confirm the printed dosage before dispensing.
16.2 Disposal of Lazanda
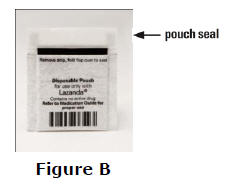
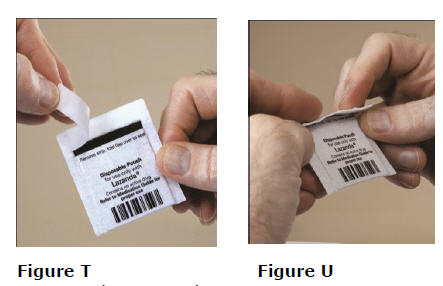
Patients and caregivers must be instructed to properly dispose of all unused, partially used and used Lazanda bottles. The remaining liquid in all bottles must be sprayed into the pouch, provided in the pack, for safe disposal as soon as possible.
The patient should be instructed how to do this correctly. If there are any unwanted therapeutic sprays remaining in the bottle, instruct the patient to spray these into the pouch until the number "8" appears in the counting window and there are no more full therapeutic sprays obtainable from the bottle. After the counter has advanced to "8", the patient should continue to push down on the finger grips a total of four times in order to expel any residual medicine from the bottle. After the 8 therapeutic sprays have been emitted, the patient will not hear a click and the counter will not advance beyond "8"; further sprays emitted will not be full sprays and should always be trapped in the pouch, not used therapeutically.
The patient and caregiver must be instructed to seal the pouch and place both it and the empty bottle into the child-resistant storage container. Hands must be washed with soap and water immediately after handling the pouch. The patient must discard the child-resistant container containing the pouch and the bottle in the trash.
The patient or caregiver must continue to store the Lazanda bottle in the specially provided child-resistant container and the pouch out of the reach of children until proper disposal, as described above, is possible.
Instruct the patient to dispose of the Lazanda bottle and start a new one if:
- it has been 5 days or more since they last used the bottle of Lazanda
- it has been 14 days or more since they primed the bottle.
In the event that caregivers or patients require additional assistance with the disposal of Lazanda bottles, call the Archimedes Pharma toll-free number (1-866-435-6775).
16.3 How Supplied
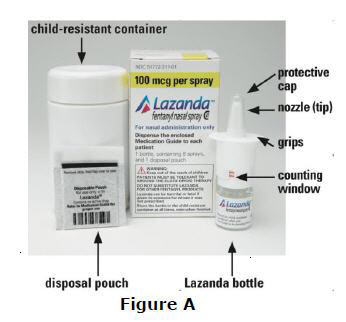
Lazanda is supplied in a 5.3 ml capacity clear glass bottle with an attached metered-dose nasal spray pump incorporating a visual and audible spray counter, and a protective dust cover. Each bottle contains a net fill weight of 1.57 grams and, after priming, delivers 8 sprays. The pump will remain primed for up to 5 days after priming or use. The nasal spray delivers 8 full sprays. There are 2 product strengths and each 100 mcL spray contains either 100 mcg or 400 mcg of fentanyl. Each bottle is supplied in a child-resistant container.
Bottles in their child-resistant containers are supplied in cartons containing 1 or 4 bottles with instructions for use.
Each carton contains one carbon-lined pouch per bottle for disposal of priming sprays, unwanted doses and residual fentanyl solution.
Lazanda Dosage Strength (fentanyl base) Number of Bottles per Carton NDC Number 100 mcg 1 51772-311-01 100 mcg 4 51772-311-04 400 mcg 1 51772-314-01 400 mcg 4 51772-314-04 -
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide)
17.1 Patient/Caregiver Instructions
- Before initiating treatment with Lazanda, explain the statements below to patients and/or caregivers. Instruct patients to read the Medication Guide each time Lazanda is dispensed because new information may be available.
- TIRF REMS Access Program
- Outpatients must be enrolled in the TIRF REMS Access program before they can receive Lazanda.
- Allow patients the opportunity to ask questions and discuss any concerns regarding Lazanda or the TIRF REMS Access program.
- As a component of the TIRF REMS Access program, prescribers must review the contents of the Lazanda Medication Guide with every patient before initiating treatment with Lazanda.
- Advise the patient that Lazanda is available only from pharmacies that are enrolled in the TIRF REMS Access program, and provide them with the telephone number and website for information on how to obtain the drug.
- Advise the patient that only enrolled health care providers may prescribe Lazanda.
- Patient must sign the Patient-Prescriber Agreement to acknowledge that they understand the risks of Lazanda.
- Advise patients that they may be requested to participate in a survey to evaluate the effectiveness of the TIRF REMS Access program.
- Instruct patients and their caregivers that the amount of fentanyl contained in a bottle can be fatal to a child. Patients and their caregivers must be instructed to keep Lazanda in its child-resistant container at all times and to store it and the pouch securely and out of the reach of children.
- Instruct patients how to safely dispose of the priming sprays and any remaining fentanyl solution in the pouch provided before disposing of both the empty bottle and the pouch inside the child-resistant container in the trash.
- Instruct patients not to take Lazanda for acute pain, postoperative pain, pain from injuries, headache, migraine, or any other short-term pain, even if they have taken other opioid analgesics for these conditions.
- Instruct patients on the meaning of opioid tolerance and Lazanda is only to be used as a supplemental pain medication for patients with pain requiring regular opioids, who have developed tolerance to the opioid medication and who need additional opioid treatment of breakthrough pain episodes.
- Instruct patients that if they are not taking an opioid medication on a regular around-the-clock basis, they must not take Lazanda.
- Instruct patients that they MUST wait at least 2 hours before treating another episode of breakthrough pain with Lazanda.
- Instruct patients NOT to share Lazanda and that sharing Lazanda with anyone else could result in the other individual's death due to overdose.
- Advise patients that Lazanda contains fentanyl, which is a pain medication similar to hydromorphone, methadone, morphine, oxycodone, and oxymorphone.
- Advise patients that the active ingredient in Lazanda, fentanyl, is a drug that some people abuse. Lazanda is to be taken only by the patient for whom it was prescribed, and protected from theft or misuse in the work or home environments.
- Instruct patients to talk to their doctor if breakthrough pain is not alleviated or worsens after taking Lazanda.
- Instruct patients to use Lazanda exactly as prescribed by their doctor and not to take Lazanda more often than prescribed.
- Caution patients that Lazanda can affect a person's ability to perform activities that require a high level of attention (such as driving or using heavy machinery). Warn patients taking Lazanda of these dangers and counsel accordingly.
- Warn patients not to combine Lazanda with alcohol, sleep aids, or tranquilizers except by order of the prescribing physician, because dangerous additive effects may occur resulting in serious injury or death.
- Inform female patients that if they become pregnant or plan to become pregnant during treatment with Lazanda to ask their doctor about the effects that Lazanda (or any medicine) may have on them and their unborn child.
- Instruct the patient to dispose of the Lazanda bottle and start a new one if:
- it has been 5 days or more since they last used the bottle of Lazanda
- it has been 14 days or more since they primed the bottle.
- Physicians and dispensing pharmacists must specifically question patients or caregivers about the presence of children in the home (on a full time or visiting basis) and counsel them regarding the dangers to children from inadvertent exposure.
17.2 Disposal of Used Lazanda Bottles
- Instruct patients and caregivers to properly dispose of all unused, partially used and used Lazanda bottles as soon as no longer needed.
- Instruct patients that, to dispose of Lazanda properly, the remaining liquid in all bottles must be sprayed into the pouch provided in the pack for safe disposal as soon as possible. This includes any unwanted therapeutic sprays remaining in the bottle. After the counter has advanced to "8", the patient should continue to push down on the finger grips a total of four times in order to expel any residual medicine from the bottle. After the 8 therapeutic sprays have been emitted, the patient will not hear a click and the counter will not advance beyond "8"; further sprays emitted will not be full sprays and should always be trapped in the pouch, not used therapeutically.
- Instruct the patient and caregiver to seal the pouch and to place both the empty bottle and the sealed pouch into the child-resistant storage container and discard in the trash. Lazanda must be stored in the specially provided child-resistant container out of the reach of children until proper disposal is possible.
- Instruct the patient and caregiver to wash their hands with soap and water immediately after handling the pouch.
- If the pouch is lost, instruct the patient and caregiver to use a pouch from another Lazanda pack to prime and dispose of unused medicine from the current bottle as well as from the next bottle. If they do not have an empty pouch available, the patient or caregiver can order one by calling 1-866-435-6775. They will receive the replacement pouch in the mail.
Rx Only.
Distributed by Archimedes Pharma US Inc.
One Crossroads Drive
Bedminster NJ 07921For information about this product call:
1- 866-435-6775U.S. Patent Nos. 6,432,440 and 8,216,604
Lazanda is a registered trademark of Archimedes Development Ltd.
© 2012 Archimedes Development Ltd.PIUS-300-4 ; PPIUS-300-4
-
MEDICATION GUIDE
Medication Guide
Lazanda® (La-ZAN-da) CII
(fentanyl)
nasal spray
100 mcg, 400 mcgIMPORTANT:
Do not use Lazanda unless you are regularly using another opioid pain medicine around-the-clock for your cancer pain and your body is used to these medicines (this means that you are opioid tolerant). You can ask your healthcare provider if you are opioid tolerant.
Keep Lazanda in a safe place away from children.
Get emergency medical help right away if:
- a child takes Lazanda. Lazanda can cause an overdose and death in any child who takes it
- an adult who has not been prescribed Lazanda takes it
- an adult who is not already taking opioids around-the-clock takes Lazanda
These are medical emergencies that can cause death.
Read this Medication Guide completely before you start taking Lazanda and each time you get a new prescription. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or your treatment. Be sure to share this important information with members of your household and other caregivers.
What is the most important information I should know about Lazanda?
Lazanda can cause life-threatening breathing problems that can lead to death:
- Do not take Lazanda if you are not opioid tolerant.
- If you stop taking your around-the-clock opioid pain medicine for your cancer, you must stop taking Lazanda. You may no longer be opioid tolerant. Talk to your healthcare provider about how to treat your pain.
-
Take Lazanda exactly as prescribed by your healthcare provider.
- You must not take more than 1 dose of Lazanda for each episode of breakthrough cancer pain.
- You must wait two hours before treating a new episode of breakthrough cancer pain with Lazanda. See the Medication Guide section "How should I use Lazanda?" and the "Instructions for Use" section at the end of this Medication Guide for detailed information about how to use Lazanda the right way.
- Do not switch from Lazanda to other medicines that contain fentanyl without talking with your healthcare provider. The amount of fentanyl in a dose of Lazanda is not the same as the amount of fentanyl in other medicines that contain fentanyl. Your healthcare provider will prescribe a starting dose of Lazanda that may be different than other fentanyl-containing medicine you may have been taking.
-
Do not take Lazanda for short-term pain that you would expect to go away in a few days, such as:
- pain after surgery
- headache or migraine
- dental pain
- Never give Lazanda to anyone else, even if they have the same symptoms you have. It may harm them or even cause death.
Lazanda is a federally controlled substance (CII) because it is a strong opioid (narcotic) pain medicine that can be misused by people who abuse prescription medicines or street drugs.
- Prevent theft, misuse or abuse. Keep Lazanda in a safe place to protect it from being stolen. Lazanda can be a target for people who abuse opioid (narcotic) medicines or street drugs.
- Selling or giving away this medicine is against the law.
Lazanda is available only through a program called the TIRF REMS ACCESS program. To receive Lazanda, you must:
- talk to your healthcare provider
- understand the benefits and risks of Lazanda
- agree to all of the instructions
- sign the Patient-Prescriber Agreement form
What is Lazanda®?
- Lazanda is a prescription medicine that contains the medicine fentanyl.
- Lazanda is used to manage breakthrough pain in adults with cancer (18 years of age and older) who are already routinely taking other opioid pain medicines around-the-clock for cancer pain.
- Lazanda is started only after you have been taking other opioid pain medicines and your body has become used to them (you are opioid tolerant). Do not use Lazanda if you are not opioid tolerant.
- You must stay under your healthcare provider's care while taking Lazanda.
- Lazanda is a nasal spray. You use Lazanda by placing the nozzle attached to the bottle in your nostril and spraying. See the Medication Guide section "How should I use Lazanda?"
- Lazanda is only:
- available through the TIRF REMS ACCESS program
- given to people who are opioid tolerant
It is not known if Lazanda is safe and effective in children under 18 years of age.
Who should not take Lazanda?
Do not take Lazanda:
- if you are not opioid tolerant. Opioid tolerant means that you are already taking other opioid (narcotic) pain medicines around-the-clock for your cancer pain and your body is used to these medicines
- for short-term pain that you would expect to go away in a few days, such as:
- pain after surgery
- headache or migraine
- dental pain
- if you are allergic to fentanyl or any of the ingredients in Lazanda. See the end of this Medication Guide for a complete list of other ingredients in Lazanda.
What should I tell my healthcare provider before taking Lazanda?
Before taking Lazanda, tell your healthcare provider if you:
- have trouble breathing or lung problems such as asthma, wheezing, or shortness of breath
- have or had a head injury or brain problem
- have liver or kidney problems
- have seizures
- have a slow heart rate or other heart problems
- have low blood pressure
- have mental health problems including major depression, schizophrenia, or hallucinations (seeing or hearing things that are not there)
- have a past or present drinking problem (alcoholism), or a family history of drinking problems
- have a past or present drug abuse problem or addiction problem, or a family history of a drug abuse problem or addiction problem
- have any other medical conditions
- are pregnant or planning to become pregnant. Lazanda may cause serious harm to your unborn baby
- are breastfeeding or plan to breastfeed. Lazanda can pass into your breast milk. It can cause serious harm to your baby. Do not use Lazanda while breastfeeding
Tell your healthcare provider about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. Some medicines may cause serious or life-threatening medical problems when taken with Lazanda. Sometimes, the doses of certain medicines and Lazanda need to be changed if used together.
- Do not take any medicine while using Lazanda until you have talked to your healthcare provider. Your healthcare provider will tell you if it is safe to take other medicines while you are using Lazanda.
- Be very careful about taking other medicines that may make you sleepy, such as other pain medicines, anti-depressants, sleeping pills, anti-anxiety medicines, anti-histamines, or tranquilizers.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
Before you can begin to use Lazanda:
- Your healthcare provider will explain the TIRF REMS ACCESS program to you.
- You will sign the TIRF REMS ACCESS program Patient-Prescriber Agreement form.
- Lazanda is only available at pharmacies that are part of the TIRF REMS ACCESS program. Your healthcare provider will let you know the pharmacy closest to your home where you can have your Lazanda prescription filled.
Using Lazanda:
- Use Lazanda exactly as your healthcare provider tells you to. Do not use Lazanda more often than prescribed.
- See the "Instructions for Use" section at the end of this Medication Guide for detailed information about the right way to use and throw away (dispose of) Lazanda.
- Lazanda comes in 2 strengths. When you are first prescribed Lazanda, your healthcare provider will start you with the lower strength medicine, and will change the dose until you and your healthcare provider find the right dose for you. Do not change your dose of Lazanda unless your healthcare provider tells you to.
- The beginning dose of Lazanda is always 1 spray in one of your nostrils.
-
Always use 1 dose of Lazanda for an episode of breakthrough cancer pain exactly as your healthcare provider tells you to. As your dose is adjusted, your healthcare provider will tell you whether your dose of Lazanda is 1 or 2 sprays:
- 1 spray is given by spraying 1 time into one of your nostrils
-
2 sprays are given by spraying 1 time into each nostril for a total of 2 sprays.
You must never use more than 2 sprays (1 spray in each nostril) for an episode of breakthrough pain.
- If an episode of breakthrough cancer pain continues for more than 30 minutes after you take a dose of Lazanda, follow your healthcare provider's instructions about taking a short-acting opioid pain medicine to manage your pain.
- Wait at least 2 hours before treating a new episode of breakthrough cancer pain with Lazanda.
- It is important for you to keep taking your around-the-clock opioid pain medicine while using Lazanda.
- Talk to your healthcare provider if your dose of Lazanda does not relieve your breakthrough cancer pain. Your healthcare provider will decide if your dose of Lazanda needs to be changed.
- Talk to your healthcare provider if you have more than 4 episodes of breakthrough cancer pain per day. The dose of your around-the-clock opioid pain medicine may need to be adjusted.
- The Lazanda nasal spray pump provides a total of 8 full sprays. When there is a red number "8" in the counting window, you have used all the medicine in the bottle. You may still see medicine in the bottle, but there is not enough for a full dose. Do not try to take more than 8 sprays from a bottle of Lazanda.
- If you use too much Lazanda or overdose, you or your caregiver should call for emergency medical help or have someone take you to the nearest hospital emergency room right away.
What should I avoid while using Lazanda?
- Do not drive, operate heavy machinery, or do other dangerous activities until you know how Lazanda affects you. Lazanda can make you sleepy. Ask your healthcare provider when it is okay to do these activities.
- Do not drink alcohol while using Lazanda. It can increase your chance of getting dangerous side effects.
- Avoid drinking grapefruit juice during treatment with Lazanda.
What are the possible side effects of Lazanda?
- 1.
Breathing problems that can become life-threatening. See "What is the most important information I should know about Lazanda?"
-
Call your healthcare provider or get emergency medical help right away if you:
- have trouble breathing
- have drowsiness with slowed breathing
- have shallow breathing (little chest movement with breathing)
- feel faint, very dizzy, confused, or have other unusual symptoms
-
Call your healthcare provider or get emergency medical help right away if you:
-
- These symptoms can be a sign that you have taken too much Lazanda or the dose is too high for you. These symptoms may lead to serious problems or death if not treated right away. If you have any of these symptoms, do not take any more Lazanda until you have talked to your healthcare provider.
- 2. Decreased blood pressure. This can make you feel dizzy or lightheaded if you get up too fast from sitting or lying down.
- 3. Physical dependence. Do not stop taking Lazanda or any other opioid without talking to your healthcare provider. You could become sick with uncomfortable withdrawal symptoms because your body has become used to these medicines. Physical dependency is not the same as drug addiction.
- 4. A chance of abuse or addiction. The chance is higher if you are or have ever been addicted to or abused other medicines, street drugs, or alcohol, or if you have a history of mental problems.
The most common side effects of Lazanda are:
- vomiting
- nausea
- constipation
- dizziness
- fever
Constipation (not often enough or hard bowel movements) is a very common side effect of pain medicines (opioids) including Lazanda and is unlikely to go away without treatment. Talk to your healthcare provider about dietary changes and the use of laxatives (medicines to treat constipation) and stool softeners to prevent or treat constipation while taking Lazanda.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Lazanda. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
- Always keep Lazanda in a safe place away from children and from anyone for whom it has not been prescribed. Protect Lazanda from theft.
- Store Lazanda at up to 77°F (25°C). Do not freeze Lazanda.
- Lazanda comes in a clear glass bottle with an attached nasal spray pump and a protective cap.
- Store Lazanda in the child-resistant container that comes with it at all times except when you are using it. Store the Lazanda child-resistant container and pouch in the cardboard box when not in use.
- Keep Lazanda away from light.
- See the "Instructions for Use" section at the end of this Medication Guide for information about the right way to dispose of Lazanda when no longer needed.
General information about Lazanda
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Use Lazanda only for the purpose for which it was prescribed. Do not give Lazanda to other people, even if they have the same symptoms you have. Lazanda can harm other people and even cause death. Sharing Lazanda is against the law.
This Medication Guide summarizes the most important information about Lazanda. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about Lazanda that is written for healthcare professionals.
For more information about the TIRF REMS ACCESS program, go to www.tirfremsaccess.com or call 1-866-822-1483.
What are the ingredients in Lazanda?
Active ingredient: fentanyl citrate
Inactive ingredients: mannitol, pectin, phenylethyl alcohol, propylparaben, sucrose, waterBefore you take Lazanda it is important that you read, understand, and follow the full Medication Guide, including these Instructions for Use. Ask your healthcare provider or pharmacist if you have any questions about the right way to prepare, use, or dispose of Lazanda. Wash your hands with soap and water before and after you use Lazanda.
What will I find in the Lazanda pack?
Each Lazanda pack contains a cardboard box that includes (See Figure A):- a Medication Guide (not shown)
- a disposal pouch (See Figure B)
- a child-resistant container, which holds 1 bottle of Lazanda.
Take the pouch and the Lazanda bottle in its child-resistant container out of the cardboard box when you are ready to use it. Keep the cardboard box and child-resistant container for storing your Lazanda. You will need to keep the pouch to safely dispose of any medicine left in the bottle. Do not remove the plastic strip from the pouch until you are ready to seal it.- Store the Lazanda bottle in the child-resistant container whenever it is not in use.
Preparing Lazanda for use
Before you use a new bottle of Lazanda for the first time, you will need to prime (prepare) the bottle. To prime the bottle:
- 1.
Remove the cap from the child-resistant container. To do this, squeeze the raised tabs on the cap and twist the cap to remove (See Figure C). Take the bottle of Lazanda out of the child-resistant container.
- 2. Remove the protective cap from the nozzle (tip) (See Figure D).
- 3. Place the tip of the Lazanda bottle into the opening of the pouch. Hold the Lazanda bottle upright so that the spray goes into the pouch (See Figure E).
- 2. Remove the protective cap from the nozzle (tip) (See Figure D).
- 4.
Look at the counting window. A new unused bottle of Lazanda will show 2 thin red lines in the counting window in the white plastic top on the bottle (See Figure F).
-
- Firmly press on the grips and then release. You will hear a "click" and you will see 1 wide red bar in the counting window (See Figure G).
- Keep pressing and releasing the grips 3 more times (for a total of 4 times). Each time, the red bar will become smaller until you see a green bar in the counting window (See Figures H, I, J).
- Firmly press on the grips and then release. You will hear a "click" and you will see 1 wide red bar in the counting window (See Figure G).
- 5.
When you see the green bar, this means that Lazanda is ready for use (See Figure K).
- 6. Remove the tip of the bottle from the pouch.
Do not seal the pouch. Do not throw the pouch away.
- 7. If you are not going to take your medicine right away
- Replace the protective cap
- Put the bottle in its child-resistant container. Put the child-resistant container and pouch in the cardboard box.
- Store the box securely out of the reach of children and pets
- 8. Wash your hands with soap and water.
- 6. Remove the tip of the bottle from the pouch.

Using Lazanda
- 1.
Check to be sure that the Lazanda bottle is ready for use. If the bottle is ready for use, you will see either a green bar (See Figure L) or a number (See Figure M) in the counting window.
- 2. If you have a runny nose, blow your nose now.
- 3. Remove the protective cap from the nozzle (tip).
- 4. Sit up with your head upright and hold the Lazanda bottle with your thumb on the bottom of the bottle and your first and middle fingers on the finger grips (See Figure N). Insert the tip a short distance (about ½ inch) into your nose, and point the tip toward the bridge of your nose. This will tilt the bottle slightly (See Figure O).
- 2. If you have a runny nose, blow your nose now.

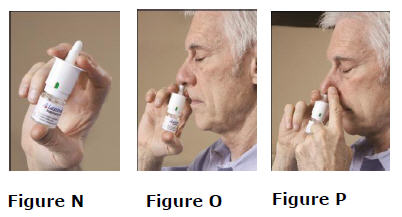
- 5.
Close off the other nostril with 1 finger (See Figure P).
- 6. Firmly press down on the finger grips until you hear a "click".
- 7. Breathe in gently through your nose and out through your mouth 1 time after spraying. Do not sniff after spraying the medicine into your nose.
- You may not feel the spray go into your nose. This is normal.
- After you hear the click, you will see that the number in the counting window has increased by 1. This tells you that a spray has been given.
- 8. If your healthcare provider has prescribed a second spray, repeat steps 4 through 7, but use the other nostril.
- 9. After each spray, the number in the counting window will increase by 1. When you see a red number "8" in the counting window, the bottle is finished and you will no longer be able to get a full dose from it. You may still see medicine in the bottle, but there is not enough for a full dose. Do not try to take another dose of Lazanda from this bottle.
- 6. Firmly press down on the finger grips until you hear a "click".
- 10.
Stay sitting down for at least 1 minute after using Lazanda.
- 11. Avoid blowing your nose for at least 30 minutes after each spray.
- 12. Replace the protective cap on the tip of the bottle (See Figure Q). Return the bottle to the child-resistant container after each use, and store securely out of the reach of children.
- 11. Avoid blowing your nose for at least 30 minutes after each spray.

Disposing of Lazanda
Dispose of the Lazanda bottle when no longer needed:
- If you have used 8 sprays from a bottle, or
- If it has been 5 days since you last used the bottle, or
- If it has been 14 days since you primed (prepared) your bottle
Before you throw away the Lazanda bottle, you must empty all the remaining medicine into the pouch. This is to protect others, especially children, from harm.
Disposal of any unused Lazanda
If you can see a number, other than 8 in the counting window, you have NOT used all 8 sprays in the bottle. There are still doses of Lazanda in the bottle.
- You must empty the remaining doses of Lazanda from the bottle
- Put tip in pouch and press and release the grips (See Figure R) until the red number "8" appears in the counting window (See Figure S).
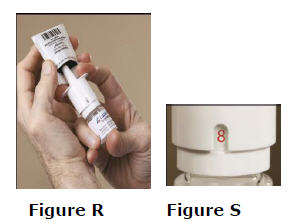
Disposal of Bottle and Pouch - 1.
Put the protective cap back on the spray bottle. Put the empty bottle back into the child-resistant container.
- 2. Seal the pouch by removing the plastic strip from the flap and folding the flap over (See Figures T and U). Put the sealed pouch into the child–resistant container with the empty bottle.
- 3. Place the cap back onto the child-resistant container and twist to close.
- 4. Throw the child-resistant container with the empty bottle and sealed pouch inside it into the trash.
- 5. Wash your hands with soap and water.
- 2. Seal the pouch by removing the plastic strip from the flap and folding the flap over (See Figures T and U). Put the sealed pouch into the child–resistant container with the empty bottle.
If you need help with disposal of unused Lazanda bottles, call Archimedes Pharma at 1-866-435-6775 or call your local Drug Enforcement Administration (DEA) office.
If you lose the pouch, use a pouch from another Lazanda pack to prime and dispose of unused medicine from this bottle as well as from the next bottle. If you do not have an empty pouch available, you can order one by calling 1-866-435-6775. You will receive the replacement pouch in the mail.
If you need to continue using Lazanda, open a new bottle and see the Instructions for Use section of this Medication Guide about "Preparing Lazanda for Use."
This Medication Guide has been approved by the US Food and Drug Administration.
Archimedes Pharma US Inc. One Crossroads Drive Bedminster NJ 07921
Revised: 12/2011Lazanda® is a registered trademark of Archimedes Development Ltd.
©2011 Archimedes Development Ltd.
All rights reserved.MGUS300
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL - 100 mcg Carton
NDC: 51772-311-04
100 mcg per spray
Lazanda™
fentanyl nasal spray CIIFor nasal administration only
Dispense the enclosed Medication Guide to each patient
4 bottles, containing 8 sprays each, and 4 disposal pouches
WARNING:
Keep out of the reach of childrenPATIENTS MUST BE TOLERANT TO
AROUND-THE-CLOCK OPIOID THERAPYDO NOT SUBSTITUTE LAZANDA
FOR OTHER FENTANYL PRODUCTSLazanda can be harmful or fatal if
given to someone for whom it was
not prescribedStore the bottle in the child resistant
container at all times, even when finished.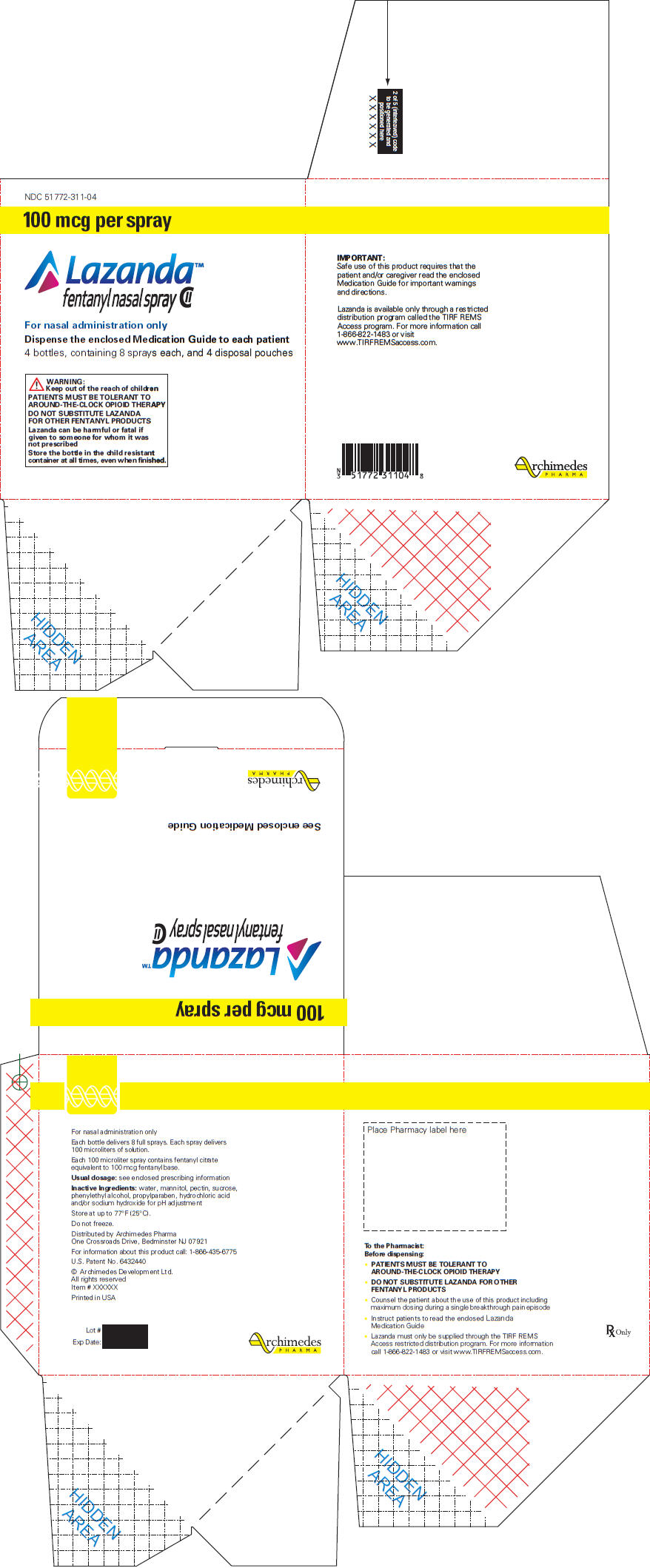
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL - 400 mcg Carton
NDC: 51772-314-04
400 mcg per spray
Lazanda™
fentanyl nasal spray CIIFor nasal administration only
Dispense the enclosed Medication Guide to each patient
4 bottles, containing 8 sprays each, and 4 disposal pouches
WARNING:
Keep out of the reach of childrenPATIENTS MUST BE TOLERANT TO
AROUND-THE-CLOCK OPIOID THERAPYDO NOT SUBSTITUTE LAZANDA
FOR OTHER FENTANYL PRODUCTSLazanda can be harmful or fatal if
given to someone for whom it was
not prescribedStore the bottle in the child resistant
container at all times, even when finished.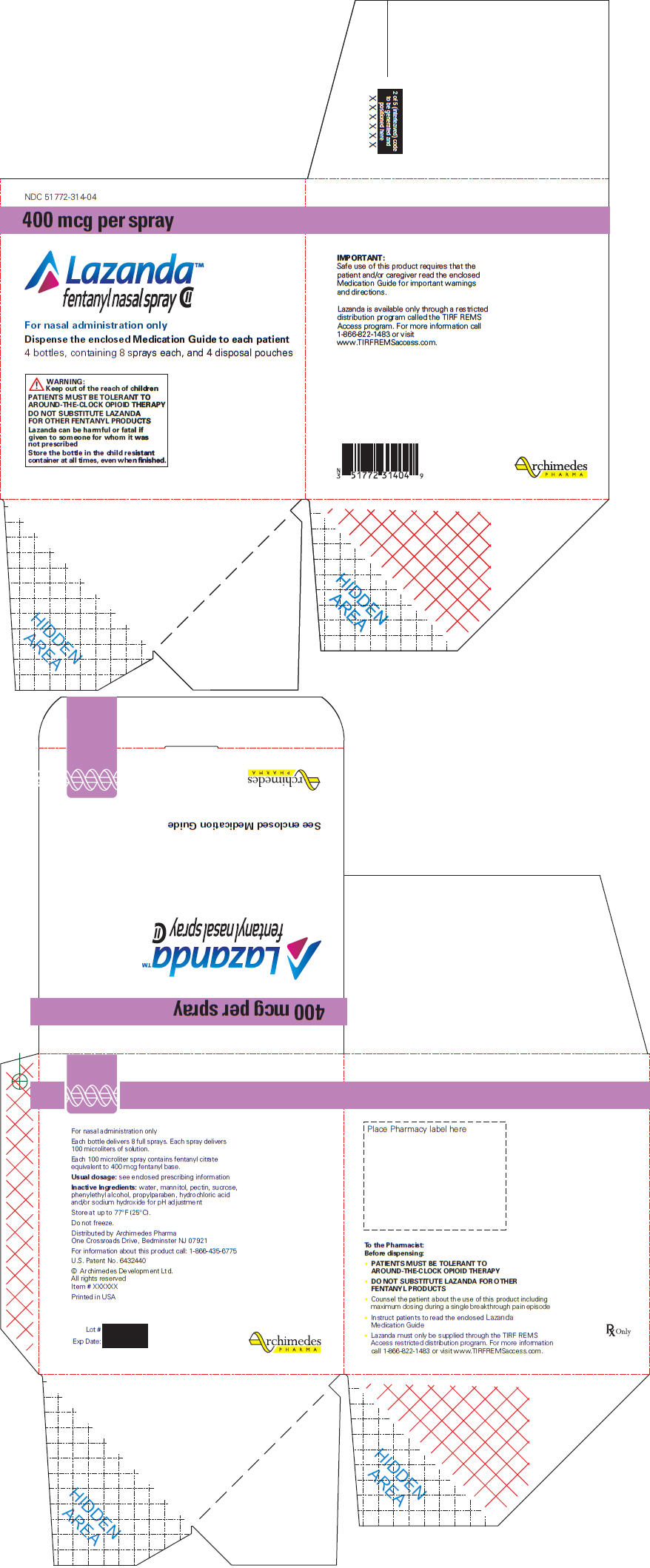
-
INGREDIENTS AND APPEARANCE
LAZANDA
fentanyl citrate sprayProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 51772-311 Route of Administration NASAL DEA Schedule CII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Fentanyl Citrate (UNII: MUN5LYG46H) (Fentanyl - UNII:UF599785JZ) Fentanyl 100 ug Inactive Ingredients Ingredient Name Strength Water (UNII: 059QF0KO0R) Mannitol (UNII: 3OWL53L36A) Pectin (UNII: 89NA02M4RX) Sucrose (UNII: C151H8M554) Phenylethyl alcohol (UNII: ML9LGA7468) Propylparaben (UNII: Z8IX2SC1OH) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 51772-311-01 1 in 1 CARTON 1 8 in 1 BOTTLE, SPRAY 2 NDC: 51772-311-04 4 in 1 CARTON 2 8 in 1 BOTTLE, SPRAY Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022569 10/17/2011 LAZANDA
fentanyl citrate sprayProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 51772-314 Route of Administration NASAL DEA Schedule CII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Fentanyl Citrate (UNII: MUN5LYG46H) (Fentanyl - UNII:UF599785JZ) Fentanyl 400 ug Inactive Ingredients Ingredient Name Strength Water (UNII: 059QF0KO0R) Mannitol (UNII: 3OWL53L36A) Pectin (UNII: 89NA02M4RX) Sucrose (UNII: C151H8M554) Phenylethyl alcohol (UNII: ML9LGA7468) Propylparaben (UNII: Z8IX2SC1OH) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 51772-314-01 1 in 1 CARTON 1 8 in 1 BOTTLE, SPRAY 2 NDC: 51772-314-04 4 in 1 CARTON 2 8 in 1 BOTTLE, SPRAY Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022569 10/17/2011 Labeler - Archimedes Pharma US Inc. (962751306)
Trademark Results [LAZANDA]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 LAZANDA 85302528 4104596 Live/Registered |
BTCP PHARMA, LLC 2011-04-22 |
 LAZANDA 85196387 not registered Dead/Abandoned |
Archimedes Development Limited 2010-12-13 |
 LAZANDA 85196378 4068538 Live/Registered |
BTCP PHARMA, LLC 2010-12-13 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.