XERESE- acyclovir and hydrocortisone cream
Xerese by
Drug Labeling and Warnings
Xerese by is a Prescription medication manufactured, distributed, or labeled by Bausch Health US LLC, Contract Pharmaceuticals Limited Canada, Bausch Health Companies Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use XERESE safely and effectively. See full prescribing information for XERESE.
XERESE® (acyclovir and hydrocortisone) cream, for topical use
Initial U.S. Approval: 2009INDICATIONS AND USAGE
XERESE, a combination of acyclovir, a herpes simplex virus deoxynucleoside analog DNA polymerase inhibitor, and hydrocortisone, a corticosteroid, is indicated for the early treatment of recurrent herpes labialis (cold sores) to reduce the likelihood of ulcerative cold sores and to shorten the lesion healing time in adults and children (6 years of age and older). (1)
DOSAGE AND ADMINISTRATION
Topically apply XERESE 5 times per day for 5 days. Therapy should be initiated as early as possible after the first signs and symptoms (i.e., during the prodrome or when lesions appear). (2)
DOSAGE FORMS AND STRENGTHS
Cream: 50 mg (equivalent to 5%, w/w) acyclovir and 10 mg (equivalent to 1%, w/w) hydrocortisone. (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
- Only for topical use for recurrent herpes labialis on the lips and around the mouth. (5)
ADVERSE REACTIONS
The following most common adverse reactions (<1%) were local skin reactions:
Drying or flaking of the skin; burning or tingling, erythema; pigmentation changes; application site reactions including signs and symptoms of inflammation. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Bausch Health US, LLC at 1-800-321-4576 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
No drug interaction studies have been performed with XERESE. (7)
USE IN SPECIFIC POPULATIONS
Immunocompromised Patients: Benefit has not been adequately assessed. (8.6)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 12/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 General
6 ADVERSE REACTIONS
6.1 Adverse Reactions in Clinical Trials
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Immunocompromised Subjects
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Clinical Trial Experience in Adults
14.2 Clinical Trial Experience in Pediatric Subjects
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
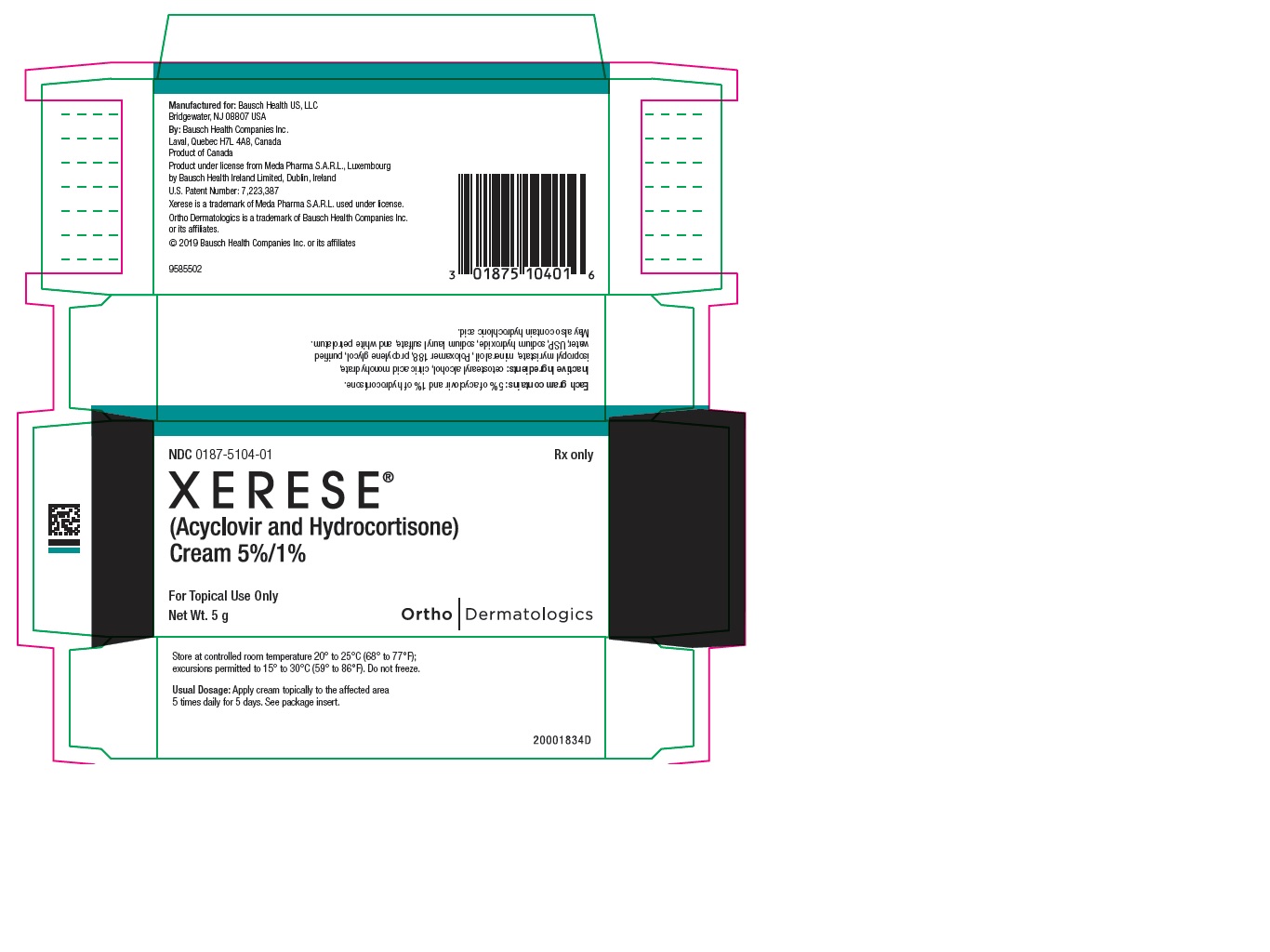
Principal Display Panel - 5 g Carton
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
XERESE, a combination of acyclovir, a herpes simplex virus deoxynucleoside analog DNA polymerase inhibitor, and hydrocortisone, a corticosteroid, is indicated for the early treatment of recurrent herpes labialis (cold sores) to reduce the likelihood of ulcerative cold sores and to shorten the lesion healing time in adults and children (6 years of age and older).
-
2 DOSAGE AND ADMINISTRATION
Topically apply XERESE 5 times per day for 5 days. Therapy should be initiated as early as possible after the first signs and symptoms (i.e., during the prodrome or when lesions appear).
For each dose, topically apply a quantity of XERESE sufficient to cover the affected area, including the outer margin. Avoid unnecessary rubbing of the affected area to avoid aggravating or transferring the infection. For children 6 years of age and older, the dosage is the same as in adults.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 General
XERESE is intended for cutaneous use only for herpes labialis of the lips and around the mouth. XERESE should not be used in the eye, inside the mouth or nose, or on the genitals.
There are other orofacial lesions, including bacterial and fungal infections, which may be difficult to distinguish from a cold sore. Patients should be encouraged to seek medical advice when a cold sore fails to heal within 2 weeks.
XERESE has a potential for irritation and contact sensitization [see Adverse Reactions (6.1)].
-
6 ADVERSE REACTIONS
6.1 Adverse Reactions in Clinical Trials
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other clinical trials and may not reflect the rates observed in clinical practice.
The safety data derived from XERESE clinical trials reflect exposure to XERESE in 1,056 subjects with recurrent herpes labialis treated 5 times daily for 5 days.
The most common adverse reactions (<1%) were local skin reactions, and occurred in the area of the application site, including:
- Drying or flaking of the skin; burning or tingling following application; erythema; pigmentation changes; application site reaction including signs and symptoms of inflammation.
Contact dermatitis following application has been observed when applied under occlusion in dermal safety trials. Where contact sensitivity tests have been conducted, the reactive substances were hydrocortisone or a component of the cream base.
A trial enrolling 225 healthy adults was conducted to evaluate the contact sensitization potential of XERESE using repeat insult patch testing methodology. Of 205 evaluable subjects, one confirmed case (0.5%) of sensitization to hydrocortisone and 2 additional cases (1.0%) of possible sensitization to the XERESE base were identified. Additionally, one subject developed a contact allergy in the photosafety study to propylene glycol, one of the inactive ingredients of the cream base.
Dermal tolerance was assessed in a 21-day cumulative irritation trial in 36 healthy subjects. XERESE, its cream base and Zovirax® (acyclovir) Cream 5% all showed a high and cumulative irritation potential under occlusive and semiocclusive conditions.
Photoallergic potential and phototoxicity were assessed in two trials in 50 and 30 healthy volunteers, respectively. No photoallergic or phototoxicity potential was identified for XERESE.
- 7 DRUG INTERACTIONS
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on XERESE use in pregnant women. However, published observational studies over decades of use of topical acyclovir and low and medium potency topical corticosteroids during pregnancy have not established any association between use of these products and major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data).
Animal reproduction studies have not been conducted with XERESE. Systemic exposure of acyclovir and hydrocortisone following topical administration of XERESE is expected to be minimal. Animal reproduction studies with systemic exposure of acyclovir and hydrocortisone have been conducted. Refer to acyclovir and hydrocortisone prescribing information for additional details.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data
While available studies cannot definitively establish the absence of risk, published data from multiple large observational studies have not established an association with the use of topical acyclovir or low and medium potency topical corticosteroids (including hydrocortisone) during pregnancy and major birth defects, miscarriage, or adverse maternal or fetal outcomes. Available studies have methodological limitations including whether women who filled a prescription actually took the medication, non-randomized design, retrospective data collection, and the inability to control for confounders such as underlying maternal disease and use of concomitant medications.
8.2 Lactation
- Risk Summary
- There are no data on the presence of acyclovir or hydrocortisone in human milk following topical administration. There are no data on the effects of acyclovir or hydrocortisone on the breastfed infant or on milk production. Systemic exposure following topical administration of either drug is expected to be minimal. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for XERESE and any potential adverse effects on the breastfed child from XERESE or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness in pediatric subjects less than 6 years of age have not been established.
8.5 Geriatric Use
In clinical studies, there were insufficient subjects above 65 years of age to reach a firm conclusion regarding safety and efficacy of XERESE in this group, although the available results were similar to lower age subjects.
8.6 Immunocompromised Subjects
Even though the safety of XERESE has been studied in immunocompromised subjects, data are insufficient to support use in this population. Immunocompromised subjects should be encouraged to consult a physician concerning the treatment of any infection.
Benefit has not been adequately assessed in immunocompromised patients. A randomized, double-blind trial was conducted in 107 immunocompromised subjects with stable HIV infection and recurrent herpes labialis. Subjects had on average 3.7 episodes of herpes labialis in the previous 12 months. The median age was 30 years (range 19 to 64 years), 46% were female, and all Caucasian. Median CD4+ T-cell count at screening was 344/mm3 (range 100-500/mm3). Subjects were treated with XERESE or 5% acyclovir in XERESE vehicle. The primary objective was to exclude a doubling of the healing time in either treatment arm. The mean healing time for cold sores was similar between the two treatment groups: 6.6 days for XERESE and 6.9 days for 5% acyclovir in XERESE vehicle.
-
10 OVERDOSAGE
Overdosage by topical application of XERESE is unlikely because of minimal systemic exposure [seeClinical Pharmacology (12.3)].
-
11 DESCRIPTION
XERESE contains acyclovir, a synthetic nucleoside analogue active against herpes viruses, and hydrocortisone, an anti-inflammatory corticosteroid, combined in a cream for topical administration. Each gram of XERESE contains 50 mg (equivalent to 5%, w/w) of acyclovir, 10 mg (equivalent to 1%, w/w) of hydrocortisone and the following inactive ingredients: cetostearyl alcohol, citric acid monohydrate, isopropyl myristate, mineral oil, Poloxamer 188, propylene glycol, purified water, USP, sodium hydroxide, sodium lauryl sulfate, and white petrolatum. Sodium hydroxide or hydrochloric acid may have been added to adjust the pH to approximately pH 5.
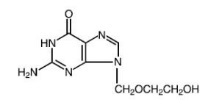
Acyclovir, 2-Amino-9-[(2-hydroxyethoxy)methyl]-1,9-dihydro-6H-purin-6-one, is a synthetic nucleoside analogue active against herpes viruses. The maximum solubility of acyclovir in water at 37°C is 2.5 mg/mL. The pKa’s of acyclovir are 2.27 and 9.25. Its empirical formula is C8H11N5O3. The structural formula is provided in Figure 1:
Figure 1: Structural Formula of Acyclovir
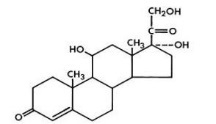
Hydrocortisone, pregn-4-ene-3,20-dione, 11,17,21-trihydroxy- (11β), is an anti-inflammatory corticosteroid. Its empirical formula is C21H30O5. The structural formula is provided in Figure 2:
Figure 2: Structural Formula of Hydrocortisone
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Acyclovir is an antiviral drug active against α-herpesviruses and hydrocortisone is an anti-inflammatory drug [see Microbiology (12.4)].
12.3 Pharmacokinetics
The plasma concentrations of acyclovir and hydrocortisone were not measured following topical administration of XERESE on cold sores.
The extent of percutaneous absorption of topical corticosteroids is determined by many factors including the vehicle, the integrity of the epidermal barrier, and the use of occlusive dressings.
Topical corticosteroids can be absorbed from normal intact skin and can have systemic side effects depending on both the potency of the corticosteroid and the surface area of application. Inflammation and/or other disease processes in the skin that disrupt the skin barrier can increase percutaneous absorption.
Once absorbed through the skin, topical corticosteroids are handled through pharmacokinetic pathways similar to systemically administered corticosteroids. Corticosteroids are bound to plasma proteins in varying degrees. They are metabolized primarily in the liver and are then excreted by the kidneys. Some of the topical corticosteroids and their metabolites are also excreted into the bile.
12.4 Microbiology
- Mechanism of Action
- Acyclovir is a synthetic purine deoxynucleoside analogue with inhibitory activity against herpes simplex viruses type 1 (HSV-1) and type 2 (HSV-2) DNA polymerases. It inhibits HSV-1 and HSV-2 replication in cell culture and in vivo.
- The inhibitory activity of acyclovir is selective due to its affinity for the enzyme thymidine kinase (TK) encoded by HSV. This viral enzyme converts acyclovir into acyclovir monophosphate, a deoxynucleotide analogue. The monophosphate is further converted into diphosphate by cellular guanylate kinase and into triphosphate by a number of cellular enzymes. In biochemical assays, acyclovir triphosphate inhibits replication of α-herpes viral DNA. This inhibition is accomplished in 3 ways: 1) competitive inhibition of viral DNA polymerase, 2) incorporation into and termination of the growing viral DNA chain, and 3) inactivation of the viral DNA polymerase.
- Hydrocortisone is the main glucocorticoid secreted by the adrenal cortex. It is used topically for its anti-inflammatory effects which suppress the clinical manifestations of the disease in a wide range of disorders where inflammation is a prominent feature.
- Antiviral Activity
- The quantitative relationship between the susceptibility of herpes viruses to antivirals in cell culture and the clinical response to therapy has not been established in humans, and virus sensitivity testing has not been standardized. Sensitivity testing results, expressed as the concentration of drug required to inhibit by 50% the growth of virus in cell culture (EC50 value), vary greatly depending upon a number of factors. Using plaque-reduction assays on Vero cells, the EC50 value of acyclovir against herpes virus isolates ranged from 0.09 to 60 µM (0.02 to 13.5 µg/mL) for HSV-1 and from 0.04 to 44 µM (0.01 to 9.9 µg/mL) for HSV-2.
- Resistance
- In Cell Culture
- Acyclovir-resistant HSV-1 and HSV-2 strains were isolated in cell culture. Acyclovir-resistant HSV resulted from mutations in the viral thymidine kinase (TK; pUL23) and DNA polymerase (POL; pUL30) genes. Frameshifts were commonly isolated and result in premature truncation of the HSV TK product with consequent decreased susceptibility to acyclovir. Mutations in the viral TK gene may lead to complete loss of TK activity (TK negative), reduced levels of TK activity (TK partial), or alteration in the ability of viral TK to phosphorylate the drug without an equivalent loss in the ability to phosphorylate thymidine (TK altered). In cell culture the following resistance-associated substitutions in TK of HSV-1 and HSV-2 were observed (Table 1).
Table 1: Summary of Acyclovir (ACV) Resistance-associated Amino Acid Substitutions in Cell Culture HSV-1
TK
P5A, H7Q, L50V, G56V, G59A, G61A, K62N, T63A, E83K, P84S, D116N, P131S, R163H, A167V, P173L, Q185R, R216S, R220H, T245M, R281stop, T287M, M322K
HSV-2
TK
L69P, C172R, T288M
HSV-1
POL
D368A, Y557S, E597D, V621S, L702H, N815S, V817M, G841C
HSV-2
POL
-
- In HSV-Infected Patients
- Clinical HSV-1 and HSV-2 isolates obtained from patients who failed treatment for their α-herpesvirus infections were evaluated for genotypic changes in the TK and POL genes and for phenotypic resistance to acyclovir (Table 2). HSV isolates with frameshift mutations and resistance-associated substitutions in TK and POL were identified. The listing of substitutions in HSV TK and POL leading to decreased susceptibility to acyclovir is not all inclusive and additional changes will likely be identified in HSV variants isolated from patients who fail acyclovir-containing regimens. The possibility of viral resistance to acyclovir should be considered in patients who fail to respond or experience recurrent viral shedding during therapy.
Table 2: Summary of ACV Resistance-associated Amino Acid Substitutions Observed in Treated Patients HSV-1
TK
G6C, R32H, R41H, R51W, Y53C/D/H, Y53stop, D55N, G56D/S, P57H, H58/N/R/Y, G59R, G61A, K62N, T63I, Q67stop, S74stop, Y80N, E83K, P84L, Y87H, W88R, R89Q/W, E95stop, T103P, Q104H, Q104stop, H105P, D116N, M121L/R, S123R, Q125H, M128L, G129D, I143V, A156V, D162A/H/N, R163G/H, L170P, Y172C, P173L, A174P, A175V, R176Q/W, R176stop, L178R, S181N, V187M, A189V, V192A, G200C/D/S, T201P, V204G, A207P, L208F/H, R216C/H, R220C/H, R221H, R222C/H, L227F, T245M/P, L249P, Q250Stop, C251G, R256W, E257K, Q261R, T287M, L288Stop, L291P/R, L297S, L315S, L327R, C336Y, Q342Stop, T354P, L364P, A365T
HSV-2
TK
R34C, G39E, R51W, Y53N, G59P, G61W, S66P, A72S, D78N, P85S, A94V, N100H, I101S, Q105P, T131P, D137stop, F140L, L158P, S169P, R177W, S182N, M183I, V192M, G201D, R217H, R221C/H, Q222stop, R223H, Y239stop, R271V, P272S, D273R, T287M, C337Y
HSV-1
POL
K532T, Q570R, L583V, A605V, A657T, D672N, V715G, A719T/V, S724N, F733C, E771Q, S775N, L778M, E798K, V813M, N815S, G841S, I890M, G901V, V958L H1228D
HSV-2
POL
E250Q, D307N, K533E, A606V, C625R, R628C, E678G, A724V, S725G, S729N, I731F, Q732R, M789K/T, V818A, N820S, Y823C, Q829R, T843A, M910T, D912N/V, A915V, F923L, T934A, R964H
Note: Additional substitutions to acyclovir resistance may exist.
- Cross-resistance
- Cross-resistance has been observed among HSV isolates carrying frameshift mutations and resistance-associated substitutions, which confer reduced susceptibility to penciclovir (PCV), famciclovir (FCV), and foscarnet (FOS) [Table 3].
Table 3: Summary of Amino Acid Substitutions Conferring Cross-Resistance to PCV, FCV or FOS Cross-resistant to PCV/FCV
HSV-1 TK
G6C, R32H, R51W, Y53C/H, H58N, G61A, S74Stop, E83K, P84L, T103P, Q104Stop, D116N, M121R, I143V, R163H, L170P, Y172C, A174P, R176Q/W, Q185R, A189V, G200D, L208H, R216C, R220H, R222C/H, T245M, Q250Stop, R256W, R281Stop, T287M, L315S, M322K, C336Y
Cross-resistant to PCV/FCV
HSV-1 POL
A657T, D672N, V715G, A719V, S724N, E798K, N815S, G841S
Cross-resistant to PCV/FCV
HSV-2 TK
G39E, R51W, Y53N, R177W, R221H, T288M
Cross-resistant to PCV/FCV
HSV-2 POL
K533E, A606V, C625R, R628C, S729N, Q732R, M789K/T, V818A, N820S, F923L, T934A
Cross-resistant to FOS
HSV-1 POL
D368A, A605V, D672N, L702H, V715G, A719T/V, S724N, L778M, E798K, V813M, N815S, V817M, G841C/S, I890M,
Cross-resistant to FOS
HSV-2 POL
K533E, A606V, C625R, R628C, A724V, S725G, S729N, I731F, Q732R, M789K/T, V818A, Y823C, D912V, F923L, T934A, R964H
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Systemic exposure following topical administration of acyclovir is minimal. Results from previous studies of carcinogenesis, mutagenesis and fertility for acyclovir and hydrocortisone are not included in the full prescribing information for XERESE due to the minimal exposures that result from dermal application. Information on these studies following systemic exposure is available in the full prescribing information for acyclovir and hydrocortisone products approved for oral or parenteral administration. Dermal carcinogenicity studies have not been conducted.
-
14 CLINICAL STUDIES
14.1 Clinical Trial Experience in Adults
In a double-blind, clinical trial, 1,443 subjects with recurrent labial herpes were randomized to receive XERESE, 5% acyclovir in XERESE vehicle or vehicle alone. Subjects had, on average, 5.6 episodes of herpes labialis in the previous 12 months. The median age was 44 years (range 18 to 80 years), 72% were female, and 91% were Caucasian. Subjects were instructed to initiate treatment within 1 hour of noticing signs or symptoms and continue treatment for 5 days, with application of study medication 5 times per day. Ulcerative cold sores occurred in 58% of the subjects treated with XERESE compared to 74% in subjects treated with vehicle and 65% in subjects treated with 5% acyclovir in XERESE vehicle. The mean time to skin normalization was approximately 1.6 days shorter in the subjects treated with XERESE compared to vehicle. Clinical signs in terms of size of the cold sore and symptoms such as tenderness were reduced with XERESE as compared to vehicle.
14.2 Clinical Trial Experience in Pediatric Subjects
An open-label safety trial in adolescents with recurrent herpes labialis was conducted in 134 subjects. Subjects had, on average, 4 episodes of herpes labialis in the previous 12 months. The median age was 14 years (range 12 to 17 years); 50% were female and all were Caucasian. XERESE was applied using the same dosing regimen as in adults and subjects were monitored for adverse events and selected efficacy parameters. The safety profile of XERESE appeared similar to that observed in adults.
An open-label safety trial in children with recurrent herpes labialis was conducted in 54 subjects, who averaged an episode of herpes labialis 2 months prior to trial entry. The mean age was 9 years (range 6 to 11 years); 57% were female and 90% were Caucasian. XERESE was applied using the same dosing regimen as in adolescents and adults and subjects were monitored for adverse events and select efficacy parameters. The safety profile of XERESE appeared similar to that observed in adults.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
XERESE is supplied in a plastic-laminated aluminum tube containing 5 g of XERESE. Each gram of XERESE contains 50 mg (equivalent to 5%, w/w) acyclovir and 10 mg (equivalent to 1%, w/w) hydrocortisone in an aqueous cream base.
NDC: 0187-5104-01: 5 g tubes
Store at controlled room temperature 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F). Do not freeze.
-
17 PATIENT COUNSELING INFORMATION
- Advise the patient to read the FDA-approved patient labeling (Patient Information).
- General
- Patients should be informed that XERESE is not a cure for cold sores. Patients should be instructed that XERESE is intended for cutaneous use only for herpes labialis of the lips and around the mouth. Patients should be advised that XERESE should not be used in the eye, inside the mouth or nose, or on the genitals.
- Instructions for Use
- Advise patients to apply XERESE topically 5 times per day for 5 days. Instruct patients to topically apply a quantity of XERESE sufficient to cover the affected area, including the outer margin. Advise patients to avoid unnecessary rubbing of the affected area to avoid aggravating or transferring the infection.
- Distributed by:
- Bausch Health US, LLC
- Bridgewater, NJ 08807 USA
- Manufactured by:
- Contract Pharmaceuticals Limited (CPL)
- Mississauga, Ontario L5N 6L6, Canada
- Product under license from Meda Pharma S.A.R.L., Luxembourg by Bausch Health Ireland Limited, Dublin, Ireland
- U.S. Patent Number: 7,223,387
- XERESE is a trademark of Meda Pharma S.A.R.L. used under license.
- Zovirax is a registered trademark of the GlaxoSmithKline group of companies.
- © 2019 Bausch Health Companies Inc. or its affiliates
-
PATIENT PACKAGE INSERT
FDA-Approved Patient LabelingPATIENT INFORMATION
XERESE® (sûr-eeze)
(acyclovir and hydrocortisone) Cream 5%/1%Important information: XERESE is for use on cold sores on the lips and around the mouth only. XERESE should not be used in your eyes, mouth, nose or on your genitals.
What is XERESE?
- XERESE is a prescription medicine used in people 6 years of age and older to shorten the healing time of cold sores (herpes labialis) and lower the chance of a cold sore becoming worse (ulcerating).
- XERESE is not a cure for cold sores.
It is not known if XERESE is safe and effective in children less than 6 years of age.
What should I tell my healthcare provider before using XERESE?
Before using XERESE, tell your healthcare provider about all of your medical conditions, including if you:
- become sick very easily (have a weak immune system)
- are pregnant or plan to become pregnant. It is not known if XERESE will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if XERESE passes into your breast milk. Talk with your healthcare provider about the best way to feed your baby if you use XERESE.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
How should I use XERESE?
- Use XERESE exactly as your healthcare provider tells you to use it.
- Use XERESE as soon as you have the first symptom of a cold sore such as itching, redness, burning or tingling or when the cold sore appears.
- Apply XERESE over the affected area, including the outer edge of the cold sore.
- Do not rub the cold sore because this may cause the cold sore to spread to other areas around your mouth or make your cold sore worse.
- Do not cover the cold sore or the area around the cold sore with a bandage.
- Do not use other skin products (such as make-up, sun screen or lip balm) or other skin medicine on the cold sore or the area around the cold sore.
- Tell your healthcare provider if your cold sore is not better in 2 weeks.
What are the possible side effects of XERESE?
The most common side effects of XERESE are skin reactions at the treatment site and may include:- drying or flaking, tingling or burning after you apply XERESE, redness, changes in skin color where the cream is applied, and swelling.
These are not all the possible side effects of XERESE. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store XERESE?
- Store XERESE at room temperature between 68° to 77°F (20° to 25°C). Do not freeze XERESE.
Keep XERESE and all medicines out of the reach of children.
General information about the safe and effective use of XERESE.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use XERESE for a condition for which it was not prescribed. Do not give XERESE to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about XERESE that is written for healthcare professionals.
What are the ingredients in XERESE?
Active ingredients: acyclovir and hydrocortisone
Inactive ingredients: cetostearyl alcohol, citric acid monohydrate, isopropyl myristate, mineral oil, Poloxamer 188, propylene glycol, sodium lauryl sulfate, purified water, USP, sodium hydroxide, and white petrolatum. May also contain hydrochloric acid.
Distributed by:
Bausch Health US, LLC
Bridgewater, NJ 08807 USA
Manufactured by:
Contract Pharmaceuticals Limited (CPL)
Mississauga, Ontario L5N 6L6, Canada
Product under license from Meda Pharma S.A.R.L., Luxembourg by Bausch Health Ireland Limited, Dublin, Ireland
U.S. Patent Number: 7,223,387
XERESE is a trademark of Meda Pharma S.A.R.L. used under license.
Zovirax is a registered trademark of the GlaxoSmithKline group of companies.
© 2019 Bausch Health Companies Inc. or its affiliates
-
For more information call 1-800-321-4576.
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 12/2019
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
XERESE
acyclovir and hydrocortisone creamProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0187-5104 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ACYCLOVIR (UNII: X4HES1O11F) (ACYCLOVIR - UNII:X4HES1O11F) ACYCLOVIR 50 mg in 1 g HYDROCORTISONE (UNII: WI4X0X7BPJ) (HYDROCORTISONE - UNII:WI4X0X7BPJ) HYDROCORTISONE 10 mg in 1 g Inactive Ingredients Ingredient Name Strength cetostearyl alcohol (UNII: 2DMT128M1S) mineral oil (UNII: T5L8T28FGP) Poloxamer 188 (UNII: LQA7B6G8JG) propylene glycol (UNII: 6DC9Q167V3) isopropyl myristate (UNII: 0RE8K4LNJS) sodium lauryl sulfate (UNII: 368GB5141J) petrolatum (UNII: 4T6H12BN9U) citric acid monohydrate (UNII: 2968PHW8QP) sodium hydroxide (UNII: 55X04QC32I) water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0187-5104-01 1 in 1 CARTON 07/31/2009 1 5 g in 1 TUBE; Type 0: Not a Combination Product 2 NDC: 0187-5104-02 20 in 1 CARTON 07/31/2009 2 0.5 g in 1 PACKET; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022436 07/31/2009 Labeler - Bausch Health US LLC (831922488) Establishment Name Address ID/FEI Business Operations Contract Pharmaceuticals Limited Canada 248761249 MANUFACTURE(0187-5104) Establishment Name Address ID/FEI Business Operations Bausch Health Companies Inc. 245141858 MANUFACTURE(0187-5104)
Trademark Results [Xerese]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 XERESE 77918965 3975430 Live/Registered |
MEDA PHARMA S. A.R.L. 2010-01-25 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.