REZENOPY- naloxone hydrochloride spray
Rezenopy by
Drug Labeling and Warnings
Rezenopy by is a Prescription medication manufactured, distributed, or labeled by Summit Biosciences Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use REZENOPY nasal spray safely and effectively. See full prescribing information for REZENOPY nasal spray.
REZENOPY (naloxone hydrochloride) nasal spray
Initial U.S. Approval: 1971INDICATIONS AND USAGE
REZENOPY nasal spray is an opioid antagonist for the emergency treatment of known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression in adult and pediatric patients. (1)
REZENOPY nasal spray is intended for immediate administration as emergency therapy in settings where opioids may be present. (1)
REZENOPY nasal spray is not a substitute for emergency medical care. (1)
DOSAGE AND ADMINISTRATION
- REZENOPY nasal spray is for intranasal use only. (2.1)
- Seek emergency medical care immediately after use. (2.1)
- Administration of a single spray of REZENOPY nasal spray intranasally into one nostril in adult and pediatric patients. (2.2)
- If the patient does not respond within 2 to 3 minutes or responds and then relapses into respiratory depression, an additional dose of REZENOPY nasal spray may be given into the other nostril with a new device. (2.2)
- Do not administer more than 2 sprays of REZENOPY nasal spray per day. (2.2)
- Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance. (2.2)
DOSAGE FORMS AND STRENGTHS
Nasal spray: 10 mg of naloxone hydrochloride in 0.11 mL. (3)
CONTRAINDICATIONS
Hypersensitivity to naloxone hydrochloride. (4)
WARNINGS AND PRECAUTIONS
- Risk of Recurrent Respiratory and CNS Depression: Due to the duration of action of naloxone relative to the opioid, keep patient under continued surveillance and administer additional doses of REZENOPY nasal spray, as necessary, using a new nasal spray device while awaiting emergency medical assistance. (5.1)
- Risk of Limited Efficacy with Partial Agonists or Mixed Agonists/Antagonists: Reversal of respiratory depression caused by partial agonists or mixed agonists/antagonists, such as buprenorphine and pentazocine, may be incomplete. Larger or repeat doses may be required. (5.2)
- Precipitation of Severe Opioid Withdrawal: Use in patients who are opioid dependent may precipitate opioid withdrawal. In neonates, opioid withdrawal may be life- threatening if not recognized and properly treated. Monitor for the development of opioid withdrawal. (5.3)
- Risk of Cardiovascular (CV) Effects: Abrupt postoperative reversal of opioid depression may result in adverse CV effects. These events have primarily occurred in patients who had pre-existing CV disorders or received other drugs that may have similar adverse CV effects. Monitor these patients closely in an appropriate healthcare setting after use of naloxone hydrochloride. (5.3)
ADVERSE REACTIONS
The following adverse reactions were observed in a REZENOPY nasal spray clinical study: abdominal pain upper, nasopharyngitis, and dysgeusia. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Summit Biosciences Inc. at 1-859-254-0180 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 4/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 Dosing in Adult and Pediatric Patients
2.3 Dosing Modifications due to Partial Agonists or Mixed Agonist/Antagonists
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Recurrent Respiratory and Central Nervous System Depression
5.2 Risk of Limited Efficacy with Partial Agonists or Mixed Agonist/Antagonists
5.3 Precipitation of Severe Opioid Withdrawal
6 ADVERSE REACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
REZENOPY nasal spray is indicated for the emergency treatment of known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression in adult and pediatric patients.
REZENOPY nasal spray is intended for immediate administration as emergency therapy in settings where opioids may be present.
REZENOPY nasal spray is not a substitute for emergency medical care.
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
REZENOPY nasal spray is for intranasal use only.
All approved naloxone hydrochloride products achieve plasma concentrations that have been shown to be efficacious in reversing the effects of opioid overdose. Comparing different products on a nominal mg-for-mg basis may be misleading [see Clinical Pharmacology (12.3)].
Because treatment of suspected opioid overdose must be performed by someone other than the patient, instruct the prescription recipient to inform those around them about the presence of REZENOPY nasal spray and the Instructions for Use.
Instruct the patient or caregiver to read the Instructions for Use at the time they receive a prescription for REZENOPY nasal spray.
Emphasize the following instructions to the patient or caregiver:
- Seek medical care immediately after use. Since the duration of action of most opioids exceeds that of naloxone hydrochloride and the suspected opioid overdose may occur outside of supervised medical settings, seek immediate emergency medical assistance, keep the patient under continued surveillance until emergency personnel arrive, and administer additional doses of REZENOPY nasal spray, as necessary. Always seek emergency medical assistance in the event of a suspected, potentially life-threatening opioid emergency after administration of the first dose of REZENOPY nasal spray.
- Additional doses of REZENOPY nasal spray may be required before emergency medical assistance becomes available.
- Do not attempt to reuse REZENOPY nasal spray. Each REZENOPY nasal spray contains a single dose of naloxone.
- Re-administer REZENOPY nasal spray, using a new nasal spray, if the patient does not respond within 2 to 3 minutes or responds and then relapses into respiratory depression.
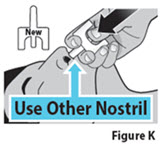
- Administer REZENOPY nasal spray in alternate nostrils with each dose.
- Administer REZENOPY nasal spray according to the printed instructions on the device label and the Instructions for Use.
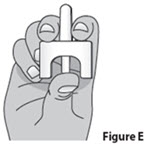
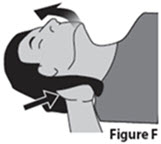
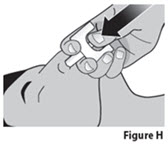
- Place the patient in the supine position on their back. Prior to administration, be sure the device nozzle is inserted in either nostril of the patient, support the back of the neck and tilt the patient’s head back. Do not prime or test the device prior to administration.
- To administer the dose firmly press the bottom of the device plunger.
- Remove the device nozzle from the nostril after use.
- Turn patient on their side as shown in the Instructions for Use and call for emergency medical assistance immediately after administration of the first dose of REZENOPY nasal spray.
2.2 Dosing in Adult and Pediatric Patients
Initial Dosing
The recommended initial dose of REZENOPY nasal spray in adults and pediatric patients is one spray delivered by intranasal administration. Administer REZENOPY nasal spray as quickly as possible because prolonged respiratory depression may result in damage to the central nervous system or death.
Repeat Dosing
Seek emergency medical assistance as soon as possible after administering the first dose of REZENOPY nasal spray.
The requirement for repeat doses of REZENOPY nasal spray depends upon the amount, type, and route of administration of the opioid being antagonized.
Administer REZENOPY nasal spray in alternate nostrils with each dose.
If the desired response is not obtained after 2 to 3 minutes, administer a second dose of REZENOPY nasal spray using a new REZENOPY nasal spray device. If there is still no response and additional doses are available, administer additional doses of REZENOPY every 2 to 3 minutes, alternating nostrils and using a new REZENOPY, until emergency medical assistance arrives. Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance.
If the patient responds to REZENOPY nasal spray and relapses back into respiratory depression before emergency assistance arrives, administer an additional dose of REZENOPY nasal spray using a new REZENOPY nasal spray device and continue surveillance of the patient.
2.3 Dosing Modifications due to Partial Agonists or Mixed Agonist/Antagonists
Reversal of respiratory depression by partial agonists or mixed agonist/antagonists, such as buprenorphine and pentazocine, may be incomplete and require higher doses of naloxone hydrochloride or repeat administration of REZENOPY nasal spray using a new nasal spray device [see Warnings and Precautions (5.2)].
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Recurrent Respiratory and Central Nervous System Depression
The duration of action of most opioids may exceed that of REZENOPY nasal spray resulting in a return of respiratory and/or central nervous system depression after an initial improvement in symptoms. Therefore, it is necessary to seek emergency medical assistance immediately after administration of the first dose of REZENOPY nasal spray and to keep the patient under continued surveillance. Administer additional doses of REZENOPY nasal spray if the patient does not adequately respond or responds and then relapses back into respiratory depression, as necessary [see DOSAGE AND ADMINISTRATION (2.2)]. Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance.
5.2 Risk of Limited Efficacy with Partial Agonists or Mixed Agonist/Antagonists
Reversal of respiratory depression by partial agonists or mixed agonist/antagonists such as buprenorphine and pentazocine, may be incomplete. Larger or repeat doses of naloxone hydrochloride may be required to antagonize buprenorphine because the latter has a long duration of action due to its slow rate of binding and subsequent slow dissociation from the opioid receptor [see Dosage and Administration (2.2)].
Buprenorphine antagonism is characterized by a gradual onset of the reversal effects and a decreased duration of action of the normally prolonged respiratory depression.
5.3 Precipitation of Severe Opioid Withdrawal
The use of REZENOPY nasal spray in patients who are opioid-dependent may precipitate opioid withdrawal characterized by the following signs and symptoms: body aches, diarrhea, tachycardia, fever, runny nose, sneezing, piloerection, sweating, yawning, nausea or vomiting, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure. In neonates, opioid withdrawal may be life-threatening if not recognized and properly treated and may include the following signs and symptoms: convulsions, excessive crying, and hyperactive reflexes. Monitor the patient for the development of the signs and symptoms of opioid withdrawal.
Abrupt postoperative reversal of opioid depression after using naloxone hydrochloride may result in nausea, vomiting, sweating, tremulousness, tachycardia, hypotension, hypertension, seizures, ventricular tachycardia and fibrillation, pulmonary edema, and cardiac arrest. Death, coma, and encephalopathy have been reported as sequelae of these events. These events have primarily occurred in patients who had pre-existing cardiovascular disorders or received other drugs that may have similar adverse cardiovascular effects. Although a direct cause and effect relationship has not been established, after use of naloxone hydrochloride, monitor patients with pre-existing cardiac disease or patients who have received medications with potential adverse cardiovascular effects for hypotension, ventricular tachycardia or fibrillation, and pulmonary edema in an appropriate healthcare setting. It has been suggested that the pathogenesis of pulmonary edema associated with the use of naloxone hydrochloride is similar to neurogenic pulmonary edema, i.e., a centrally mediated massive catecholamine response leading to a dramatic shift of blood volume into the pulmonary vascular bed resulting in increased hydrostatic pressures.
There may be clinical settings, particularly the postpartum period in neonates with known or suspected exposure to maternal opioid use, where it is preferable to avoid the abrupt precipitation of opioid withdrawal symptoms. In these settings, consider use of an alternative, naloxone-containing product that can be titrated to effect and, where applicable, dosed according to weight [see Use in Specific Population (8.4)].
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed elsewhere in the labeling:
- Precipitation of Severe Opioid Withdrawal [see Warnings and Precautions (5.3)].
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to the rates in the clinical studies of another drug and may not reflect the rates observed in practice.
The following adverse reactions were observed in a REZENOPY nasal spray clinical study.
In a pharmacokinetic study of 30 healthy adult volunteers exposed to one spray of REZENOPY nasal spray, adverse reactions of abdominal pain upper, nasopharngitis and dysgeusia were observed.
The following adverse reactions have been identified primarily during post-approval use of naloxone hydrochloride in the post-operative setting. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: Hypotension, hypertension, ventricular tachycardia and fibrillation, dyspnea, pulmonary edema, and cardiac arrest. Death, coma, and encephalopathy have been reported as sequelae of these events. Excessive doses of naloxone hydrochloride in post-operative patients have resulted in significant reversal of analgesia, and have caused agitation.
Abrupt reversal of opioid effects in persons who were physically dependent on opioids has precipitated an acute withdrawal syndrome. Signs and symptoms have included: body aches, fever, sweating, runny nose, sneezing, piloerection, yawning, weakness, shivering or trembling, nervousness, restlessness or irritability, diarrhea, nausea or vomiting, abdominal cramps, increased blood pressure, tachycardia. In some patients, there may be aggressive behavior upon abrupt reversal of an opioid overdose. In the neonate, opioid withdrawal signs and symptoms also included convulsions, excessive crying, and hyperactive reflexes.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Life-sustaining therapy for opioid overdose should not be withheld (see Clinical Considerations). Available data from retrospective cohort studies on naloxone use in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage, or other adverse maternal or fetal outcomes. In animal reproduction studies, no embryotoxic or teratogenic effects were observed in mice and rats administered naloxone hydrochloride during organogenesis at doses equivalent to 2-times and 4-times, respectively, a human dose of 20 mg/day (2 sprays of REZENOPY) (see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
An opioid overdose is a medical emergency and can be fatal for the pregnant woman and fetus if left untreated. Treatment with REZENOPY for opioid overdose should not be withheld because of potential concerns regarding the effects of REZENOPY on the fetus.
Data
Animal Data
Naloxone hydrochloride was administered during organogenesis to mice and rats at doses 2-times and 4-times, respectively, a human dose of 20 mg (two REZENOPY nasal sprays) based on body surface area comparison. These studies demonstrated no embryotoxic or teratogenic effects due to naloxone hydrochloride.
8.2 Lactation
Risk Summary
There is no information available on the presence of naloxone in human or animal milk, the effects of the drug on the breastfed infant, or the effects of the drug on milk production.
Published studies in lactating women have shown that naloxone does not effect prolactin and oxytocin hormone levels. Naloxone is minimally orally bioavailable.
8.4 Pediatric Use
The safety and effectiveness of REZENOPY for known or suspected opioid overdose as manifested by respiratory and/or central nervous system depression have been established in pediatric patients Use of naloxone hydrochloride in pediatric patients is supported by adult bioequivalence studies coupled with evidence from the safe and effective use of other naloxone hydrochloride drug products. No pediatric studies were conducted for REZENOPY nasal spray.
Absorption of naloxone hydrochloride following intranasal administration in pediatric patients may be erratic or delayed. Even when the opiate-intoxicated pediatric patient responds appropriately to naloxone hydrochloride, he/she must be carefully monitored for at least 24 hours, as a relapse may occur as naloxone hydrochloride is metabolized.
In opioid-dependent pediatric patients, (including neonates), administration of naloxone hydrochloride may result in an abrupt and complete reversal of opioid effects, precipitating an acute opioid withdrawal syndrome. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening if not recognized, and should be treated according to protocols developed by neonatology experts [see Warnings and Precautions (5.3)].
In settings such as in neonates with known or suspected exposure to maternal opioid use, where it may be preferable to avoid the abrupt precipitation of opioid withdrawal symptoms, consider use of an alternate naloxone-containing product that can be dosed according to weight and titrated to effect.
Also, in situations where the primary concern is for infants at risk for opioid overdose, consider whether the availability of alternate naloxone-containing products may be better suited than REZENOPY nasal spray.
8.5 Geriatric Use
Geriatric patients have a greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy. Therefore, the systemic exposure of naloxone hydrochloride can be higher in these patients.
Clinical studies of naloxone hydrochloride did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
-
11 DESCRIPTION
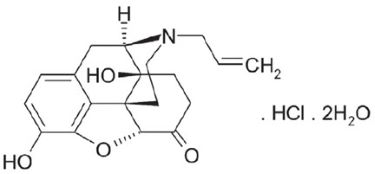
REZENOPY (naloxone hydrochloride) nasal spray is a pre-filled, single dose intranasal spray. Chemically, naloxone hydrochloride is the hydrochloride salt of 17-Allyl-4,5α-epoxy- 3,14-dihydroxymorphinan-6-one hydrochloride with the following structure:
Molecular Formula: C19H21N04HCl2H20
Relative Molecular Mass: 399.87Naloxone hydrochloride, an opioid antagonist, occurs as a white, to slightly off-white powder or almost white crystalline powder and contains two molecules of water of hydration. It is freely soluble in water, in dilute acids, and in strong alkali; slightly soluble in ethanol. pKa values (proton on Nitrogen) are respectively 7.94 at 20°C and 7.82 at 37°C.
Each REZENOPY nasal spray delivers 10 mg naloxone hydrochloride (equivalent to 9 mg of naloxone) in a 0.11 mL aqueous solution.
Inactive ingredients include glycerin, trisodium citrate dihydrate, hydrochloric acid and sodium hydroxide to adjust pH, and purified water. The pH range is 3.9 to 4.5.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Naloxone hydrochloride is an opioid antagonist that antagonizes opioid effects by competing for the same receptor sites.
Naloxone hydrochloride reverses the effects of opioids, including respiratory depression, sedation, and hypotension. It can also reverse the psychotomimetic and dysphoric effects of agonist-antagonists such as pentazocine.
12.2 Pharmacodynamics
When naloxone hydrochloride is administered intravenously, the onset of action is generally apparent within two minutes. The time to onset of action is shorter for intravenous compared to subcutaneous or intramuscular routes of administration. The duration of action is dependent upon the dose and route of administration of naloxone hydrochloride.
12.3 Pharmacokinetics
In a pharmacokinetic study in 30 healthy adult subjects, the relative bioavailability (BA) of one nasal spray of a 10 mg total dose (0.11 mL of 91 mg/mL naloxone hydrochloride solution) was compared to a single dose of 0.4 mg naloxone hydrochloride intramuscular injection and a single dose of 2 mg naloxone hydrochloride intravenous injection. For intranasal administration, the subjects were instructed not to breathe through the nose during administration of the nasal spray and remained fully supine for approximately one-hour post-dose. For intramuscular administration, naloxone was administered as a single injection in the gluteus maximus muscle. For intravenous administration, naloxone was administered as an intravenous bolus. The pharmacokinetic parameters obtained in the study are shown in Table 1.
Table 1 Mean Pharmacokinetic Parameters (CV%) for REZENOPY nasal spray, Intramuscular and Intravenous Injections of Naloxone HCl to Healthy Subjects Parameter REZENOPY nasal spray 10 mg
(n=29)Naloxone HCl 0.4 mg Intramuscular Injection
(n=30)Naloxone HCl 2 mg Intravenous Injection (n=23) † tmax reported as median (minimum, maximum)
†† N=22 and N=23, respectively for REZENOPY nasal spray 10 mg and Naloxone HCl 0.4 mg Intramuscular Injection for Dose normalized absolute BA vs. IVtmax (h)†
0.75 (0.25, 1.03)
0.50 (0.17, 2.00)
0.08 (0.02, 0.18)
Cmax (ng/mL)
9.11 (35.45)
0.74 (36.63)
18.41 (46.08)
AUCt
(h·ng/mL)
19.19 (24.81)
1.92 (19.75)
12.18 (24.30)
AUC0-∞
(h·ng/mL)
19.52 (24.78)
1.98 (19.18)
12.25 (24.22)
t1/2 (h)
1.33 (16.09)
1.22 (18.48)
1.18 (11.59)
Dose normalized absolute BA vs. IV††
0.34 (30.53)
0.84 (29.06)
-
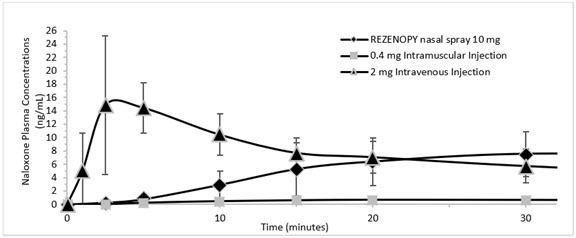
Figure 1 Mean ± SD Plasma Concentration of Naloxone 0-30 minutes Following Intranasal, Intramuscular and Intravenous Administration.
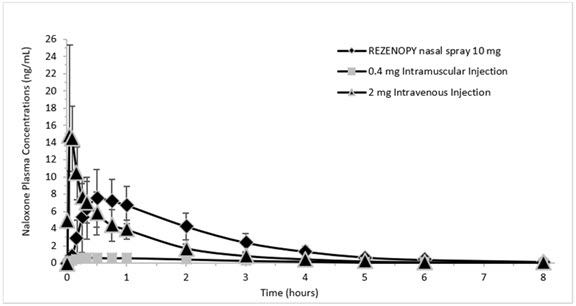
Figure 2 Mean ± SD Plasma Concentration of Naloxone 0-8 hours Following Intranasal, Intramuscular and Intravenous Administration.
Absorption
REZENOPY nasal spray showed median Tmax 0.75 hour. The median Tmax for the 0.4 mg naloxone hydrochloride intramuscular injection was 0.5 hour. The dose normalized absolute bioavailability of one dose (10 mg) of REZENOPY nasal spray and 0.4 mg of naloxone HCl intramuscular injection compared to 2 mg of naloxone HCl intravenous injection was 34% and 84% respectively.
Distribution
Following parenteral administration, naloxone is distributed in the body and readily crosses the placenta. Plasma protein binding occurs but is relatively weak. Plasma albumin is the major binding constituent, but significant binding of naloxone also occurs to plasma constituents other than albumin. It is not known whether naloxone is excreted into human milk.
Elimination
Following a single intranasal administration of REZENOPY nasal spray (10 mg dose of naloxone hydrochloride), the mean plasma half-life of naloxone in healthy adults was approximately 1.33 hours (16.09% CV) hours. Following the administrations of a 0.4 mg naloxone hydrochloride intramuscular injection and a 2 mg naloxone hydrochloride intravenous injection, the half-life was 1.22 hours (18.48% CV) and 1.18 hours (11.59% CV), respectively. In a neonatal study of naloxone hydrochloride injection, the mean (± SD) plasma half-life was observed to be 3.1 (± 0.5) hours.
Metabolism
Naloxone hydrochloride is metabolized in the liver, primarily by glucuronide conjugation, with naloxone-3-glucoronide as the major metabolite.
Excretion
After an oral or intravenous dose, about 25-40% of naloxone is excreted as metabolites in urine within 6 hours, about 50% in 24 hours, and 60-70% in 72 hours.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term animal studies to evaluate the carcinogenic potential of naloxone have not been completed.
Mutagenesis
Naloxone was weakly positive in the Ames mutagenicity and in the in vitro human lymphocyte chromosome aberration test but was negative in the in vitro Chinese hamster V79 cell HGPRT mutagenicity assay and in the in vivo rat bone marrow chromosome aberration study.
Impairment of Fertility
Reproductive studies conducted in mice and rats at doses 2-times and 4-times, respectively, a human dose of 20 mg/day (from two nasal sprays of REZENOPY) based on body surface area comparison, demonstrated no adverse effects on fertility of naloxone hydrochloride.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
REZENOPY nasal spray 10 mg is supplied as a carton containing two (2) blister packages (NDC: 43674-004-02) each with a single spray device.
REZENOPY nasal spray is not made with natural rubber latex.
16.2 Storage and Handling
Store REZENOPY nasal spray in the blister and cartons provided.
Store between 2°C to 25°C (36°F to 77°F). Excursions permitted up to 40°C (104°F). Do not freeze or expose to excessive heat above 40°C (104°F). Protect from light.
REZENOPY nasal spray may freeze at cold temperatures. If this happens, the device will not spray. If REZENOPY nasal spray is frozen and is needed in an emergency, do NOT wait for REZENOPY nasal spray to thaw. Get emergency medical help right away.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Recognition of Opioid Overdose
Instruct patients and their family members or caregivers about how to recognize the signs and symptoms of an opioid overdose such as the following:
- Extreme somnolence - inability to awaken a patient verbally or upon a firm sternal rub.
- Respiratory depression - this can range from slow or shallow respiration to no respiration in a patient who is unarousable.
-
Other signs and symptoms that may accompany somnolence and respiratory depression include the following:
- o Miosis
- o Bradycardia and/or hypotension
Risk of Recurrent Respiratory and Central Nervous System Depression
Instruct patients and their family members or caregivers that, since the duration of action of most opioids may exceed that of REZENOPY nasal spray, they must seek immediate emergency medical assistance after the first dose of REZENOPY nasal spray and keep the patient under continued surveillance [see Dosage and Administration (2.2), Warnings and Precautions (5.2)].
Limited Efficacy for/with Partial Agonists or Mixed Agonist/Antagonists
Instruct patients and their family members or caregivers that the reversal of respiratory depression caused by partial agonists or mixed agonist/antagonists, such as buprenorphine and pentazocine, may be incomplete and may require higher doses of naloxone hydrochloride or repeat administration of REZENOPY nasal spray, using a new nasal spray [see Dosage and Administration (2.2), Warnings and Precautions (5.2)].
Precipitation of Severe Opioid Withdrawal
Instruct patients and their family members or caregivers that the use of REZENOPY nasal spray in patients who are opioid dependent may precipitate opioid withdrawal [see Warnings and Precautions (5.3), Adverse Reactions (6)].
Administration Instructions
Instruct patients and their family members or caregivers to:
- Ensure REZENOPY nasal spray is present whenever persons may be intentionally or accidentally exposed to an opioid overdose (i.e., opioid emergencies).
- Administer REZENOPY nasal spray as quickly as possible if a patient is unresponsive and an opioid overdose is suspected, even when in doubt, because prolonged respiratory depression may result in damage to the central nervous system or death. REZENOPY nasal spray is not a substitute for emergency medical care [see Dosage and Administration (2.1)].
- Lay the patient on their back, tilt the patient’s head back while supporting the neck and administer REZENOPY nasal spray into one nostril. [see Dosage and Administration (2.1)].
- Use each nasal spray only one time [see Dosage and Administration (2.1)].
- Turn patient on their side as shown in the Instructions for Use and call for emergency medical assistance immediately after administration of the first dose of REZENOPY nasal spray. Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance [see Dosage and Administration (2.1)].
- Monitor the patient and administer an additional dose of REZENOPY nasal spray using a new REZENOPY nasal spray every 2 to 3 minutes, if the patient is not responding or responds and then relapses back into respiratory depression. Administer REZENOPY nasal spray in alternate nostrils with each dose [see Dosage and Administration (2.1)].
- Replace REZENOPY nasal spray before its expiration date.
Manufactured by: Summit Biosciences Inc., Lexington, KY 40511
5121XX
-
INSTRUCTIONS FOR USE
REZENOPY (reh zeh' noe pee)
(naloxone hydrochloride)
nasal spray10 mg
You and your family members or caregivers should read the Instructions for Use that comes with REZENOPY nasal spray before using it. Talk to your healthcare provider if you and your family members or caregivers have any questions about the use of REZENOPY nasal spray.
Use REZENOPY nasal spray for known or suspected opioid overdose in adults and children. Use REZENOPY nasal spray exactly as prescribed by your healthcare provider.
Important Information You Need to Know Before Giving REZENOPY nasal spray:
- For use in the nose only.
- Do not remove REZENOPY nasal spray from package until ready to use.
- Each REZENOPY nasal spray device has 1 dose and cannot be reused.
- Do not test or prime REZENOPY nasal spray before use.
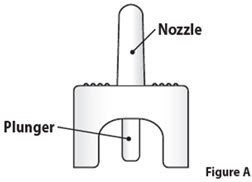
REZENOPY nasal spray Parts (Figure A)
Storing REZENOPY nasal spray
- Store REZENOPY nasal spray between 2°C to 25°C (36°F to 77°F). Excursions permitted up to 40°C (104°F).
- Do not freeze. Do not expose to excessive heat above 40°C (104°F).
- Keep REZENOPY nasal spray in its box until ready to use. Protect from light.
- Replace REZENOPY nasal spray before the expiration date on the box.
Keep REZENOPY nasal spray and all medicines out of the reach of children.
For more information, go to www.summitbiosciences.com or call 1-859-254-0180.
This Instructions for Use leaflet has been approved by the U.S. Food and Drug Administration. Issued: 4/2024
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
REZENOPY (reh zeh' noe pee)
(Naloxone Hydrochloride)
nasal sprayYou and your family members or caregivers should read this Patient Information leaflet before an opioid emergency happens. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about REZENOPY nasal spray?
REZENOPY nasal spray is used to temporarily reverse the effects of opioid medicines. The medicine in REZENOPY nasal spray has no effect in people who are not taking opioid medicines. Always carry REZENOPY nasal spray with you in case of an opioid emergency.
- 1.
Use REZENOPY nasal spray right away if you or your caregiver think signs or symptoms of an opioid emergency are present, even if you are not sure, because an opioid emergency can cause severe injury or death. Signs and symptoms of an opioid emergency may include:
unusual sleepiness and you are not able to awaken the person with a loud voice or rubbing firmly on the middle of their chest (sternum)
breathing problems including slow or shallow breathing in someone difficult to awaken or who looks like they are not breathing
the black circle in the center of the colored part of the eye (pupil) is very small, sometimes called “pinpoint pupils”, in someone difficult to awaken - 2. Family members, caregivers, or other people who may have to use REZENOPY nasal spray in an opioid emergency should know where REZENOPY nasal spray is stored and how to give it before an opioid emergency happens.
- 3. Call 911 or get emergency medical help right away after giving the first dose of REZENOPY nasal spray. Rescue breathing or CPR (cardiopulmonary resuscitation) may be given while waiting for emergency medical help.
- 4. The signs and symptoms of an opioid emergency can return after REZENOPY nasal spray is given. If this happens, give another dose every 2 to 3 minutes using a new REZENOPY nasal spray and watch the person closely until emergency help is received.
What is REZENOPY nasal spray?
- REZENOPY nasal spray is a prescription medicine used in adults and children for the treatment of an opioid emergency such as an overdose or a possible opioid overdose with signs of breathing problems and severe sleepiness or not being able to respond.
- REZENOPY nasal spray is to be given right away and does not take the place of emergency medical care. Get emergency medical help right away after giving the first dose of REZENOPY nasal spray, even if the person wakes up.
- REZENOPY nasal spray is safe and effective in children for known or suspected opioid overdose.
Do not use REZENOPY nasal spray if you are allergic to naloxone hydrochloride or any of the ingredients in REZENOPY nasal spray. See the end of this leaflet for a complete list of ingredients in REZENOPY nasal spray.
Before using REZENOPY nasal spray, tell your healthcare provider about all your medical conditions, including if you:
- have heart problems
- are breastfeeding or plan to breastfeed. It is not known if REZENOPY nasal spray passes into your breast milk.
Tell your healthcare provider about the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
How should I use REZENOPY nasal spray?
Read the “Instructions for Use” at the end of this Patient Information leaflet for detailed information about the right way to use REZENOPY nasal spray.
- Use REZENOPY nasal spray exactly as prescribed by your healthcare provider.
- Each REZENOPY nasal spray contains 1 dose of medicine and cannot be reused.
- Lay the person on their back. Support their neck with your hand and allow the head to tilt back before giving REZENOPY nasal spray.
- REZENOPY nasal spray should be given into one nostril.
- If additional doses are needed, give REZENOPY nasal Spray in the other nostril.
What are the possible side effects of REZENOPY nasal spray?
REZENOPY nasal spray may cause serious side effects, including:
- Sudden opioid withdrawal symptoms. In someone who has been using opioids regularly, opioid withdrawal symptoms can happen suddenly after receiving REZENOPY nasal spray and may include:
- o body aches
- o diarrhea
- o increased heart rate
- o fever
- o runny nose
- o sneezing
- o goose bumps
- o sweating
- o yawning
- o nausea or vomiting
- o nervousness
- o restlessness or irritability
- o shivering or trembling
- o stomach cramping
- o weakness
- o increased blood pressure
In infants under 4 weeks old who have been receiving opioids regularly, sudden opioid withdrawal may be life-threatening if not treated the right way. Signs and symptoms include: seizures, crying more than usual, and increased reflexes.
The most common side effects of REZENOPY nasal spray include: upper stomach-area (abdominal) pain, the common cold, and changes in sense of taste.
These are not all the possible side effects of REZENOPY nasal spray.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1 800-FDA-1088.
How should I store REZENOPY nasal spray?
- Store REZENOPY nasal spray between 2°C to 25°C (36°F to 77°F).
- Do not freeze. Do not expose to excessive heat above 40°C (104°F).
- Keep REZENOPY nasal spray in its box until ready to use. Protect from light.
- Replace REZENOPY nasal spray before the expiration date on the box.
Keep REZENOPY nasal spray and all medicines out of the reach of children.
General Information about the safe and effective use of REZENOPY nasal spray.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use REZENOPY nasal spray for a condition for which it was not prescribed. You can ask your pharmacist or healthcare provider for information about REZENOPY nasal spray that is written for health professionals.
What are the ingredients in REZENOPY nasal spray?
Active ingredients: naloxone hydrochloride
Inactive ingredients: glycerin, trisodium citrate dihydrate, hydrochloric acid and sodium hydroxide to adjust pH, and purified water.
REZENOPY nasal spray is not made with natural rubber latex.
Manufactured by: Summit Biosciences Inc., Lexington, KY 40511 USA.
For more information, go to www.summitbiosciences.com or call 1-859-254-0180
This Patient Information has been approved by the U.S. Food and Drug Administration
Issued: 4/2024 - 1.
Use REZENOPY nasal spray right away if you or your caregiver think signs or symptoms of an opioid emergency are present, even if you are not sure, because an opioid emergency can cause severe injury or death. Signs and symptoms of an opioid emergency may include:
-
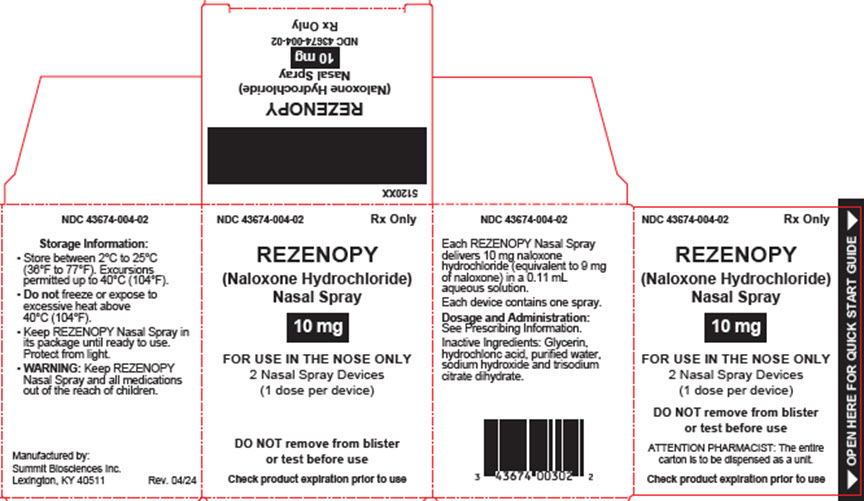
PRINCIPAL DISPLAY PANEL - Carton
NDC: 43674-004-02 Rx Only
REZENOPY
(Naloxone Hydrochloride)
Nasal Spray10 mg
FOR USE IN THE NOSE ONLY
2 Nasal Spray Devices
(1 dose per device)DO NOT remove from blister
or test before useATTENTION PHARMACIST: The entire
carton is to be dispensed as a unit.Check product expiration prior to use
-
INGREDIENTS AND APPEARANCE
REZENOPY
naloxone hydrochloride sprayProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 43674-004 Route of Administration NASAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NALOXONE HYDROCHLORIDE (UNII: F850569PQR) (NALOXONE - UNII:36B82AMQ7N) NALOXONE HYDROCHLORIDE 10 mg in 0.11 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) TRISODIUM CITRATE DIHYDRATE (UNII: B22547B95K) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 43674-004-02 2 in 1 CARTON 02/10/2025 1 1 in 1 BLISTER PACK 1 0.11 mL in 1 VIAL, SINGLE-DOSE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA215487 02/10/2025 Labeler - Summit Biosciences Inc (832920081)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.