XEOMIN- incobotulinumtoxina injection, powder, lyophilized, for solution
Xeomin by
Drug Labeling and Warnings
Xeomin by is a Prescription medication manufactured, distributed, or labeled by Merz North America, Inc., Merz Pharma GmbH & Co. KGaA. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use XEOMIN® safely and effectively. See full prescribing information for XEOMIN.
XEOMIN (incobotulinumtoxinA) for injection, for intramuscular or intraglandular use
Initial U.S. Approval: 2010WARNING: DISTANT SPREAD OF TOXIN EFFECT
See full prescribing information for complete boxed warning.
The effects of XEOMIN and all botulinum toxin products may spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can also occur in adults, particularly in those patients who have underlying conditions that would predispose them to these symptoms. (5.1)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
XEOMIN is an acetylcholine release inhibitor and neuromuscular blocking agent indicated for the treatment or improvement of adult patients with:
DOSAGE AND ADMINISTRATION
Chronic Sialorrhea: the recommended total dose is 100 Units per treatment session consisting of 30 Units per parotid gland and 20 Units per submandibular gland, no sooner than every 16 weeks (2.2)
Upper limb spasticity, cervical dystonia, and blepharospasm: the optimum dose, frequency, and number of injection sites in the treated muscle(s) should be based on severity and prior treatment response; individualize dosing for each patient:
- Upper Limb Spasticity in Adults: the recommended total dose is up to 400 Units no sooner than every 12 weeks (2.3)
- Cervical Dystonia: the recommended initial total dose is 120 Units per treatment session (2.4)
- Blepharospasm: the recommended initial total dose is 50 Units (25 Units per eye) (2.5)
Glabellar Lines: the recommended dose is 20 Units per treatment session divided into five equal intramuscular injections of 4 Units each (two injections in each corrugator muscle and one injection in the procerus muscle; wait a minimum of three months before retreatment (2.6)
Reconstituted XEOMIN:
- is intended for intramuscular or intraglandular injection in the parotid and submandibular glands only (2.7)
- use for only one injection session and for only one patient (2.7)
- instructions are specific for 50 Unit, 100 Unit, and 200 Unit vials (2.7)
- store in a refrigerator (2°C to 8°C) and use within 24 hours (2.7)
DOSAGE FORMS AND STRENGTHS
- For injection: 50 Units, 100 Units, or 200 Units lyophilized powder in a single-dose vial (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Respiratory, speech, or swallowing difficulties: Increased risk if bilateral neck muscle injections are needed or with pre-existing muscular disorders; immediate medical attention may be required (5.1, 5.4)
- The potency Units of XEOMIN are not interchangeable with other preparations of botulinum toxin products (5.2)
- Corneal exposure and ulceration: protective measures may be required (5.5)
- Risk of ptosis: follow dosage recommendations (5.6)
ADVERSE REACTIONS
The most commonly observed adverse reactions at rates specified below and greater than placebo are:
- Chronic Sialorrhea: (≥4% of patients) tooth extraction, dry mouth, diarrhea, and hypertension (6.1)
- Upper Limb Spasticity: (≥2% of patients) seizure, nasopharyngitis, dry mouth, upper respiratory tract infection (6.1)
- Cervical Dystonia: (≥5% of patients) dysphagia, neck pain, muscle weakness, injection site pain, and musculoskeletal pain (6.1)
- Blepharospasm: (≥10% of patients) eyelid ptosis, dry eye, visual impairment, and dry mouth (6.1)
- Glabellar Lines: (>1% of patients) headache (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Merz Pharmaceuticals, LLC at 888-493-6646 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Aminoglycosides or other agents that interfere with neuromuscular transmission may potentiate the effect of XEOMIN; co-administer only with caution and close observation (7)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 5/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: DISTANT SPREAD OF TOXIN EFFECT
1 INDICATIONS AND USAGE
1.1 Chronic Sialorrhea
1.2 Upper Limb Spasticity
1.3 Cervical Dystonia
1.4 Blepharospasm
1.5 Glabellar Lines
2 DOSAGE AND ADMINISTRATION
2.1 Instructions for Safe Use
2.2 Chronic Sialorrhea
2.3 Upper Limb Spasticity
2.4 Cervical Dystonia
2.5 Blepharospasm
2.6 Glabellar Lines
2.7 Preparation and Reconstitution Technique
2.8 Administration
2.9 Monitoring to Assess Effectiveness
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Spread of Toxin Effect
5.2 Lack of Interchangeability between Botulinum Toxin Products
5.3 Hypersensitivity Reactions
5.4 Dysphagia and Breathing Difficulties
5.5 Corneal Exposure, Corneal Ulceration, and Ectropion in Patients Treated for Blepharospasm
5.6 Risk of Ptosis in Patients Treated for Glabellar Lines
5.7 Human Albumin and Transmission of Viral Diseases
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Immunogenicity
6.3 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Aminoglycosides and Other Agents Interfering with Neuromuscular Transmission
7.2 Anticholinergic Drugs
7.3 Other Botulinum Neurotoxin Products
7.4 Muscle Relaxants
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Chronic Sialorrhea
14.2 Upper Limb Spasticity
14.3 Cervical Dystonia
14.4 Blepharospasm
14.5 Glabellar Lines
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: DISTANT SPREAD OF TOXIN EFFECT
Postmarketing reports indicate that the effects of XEOMIN and all botulinum toxin products may spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These may include asthenia, generalized muscle weakness, diplopia, blurred vision, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses, including spasticity in children and in approved indications, cases of spread of effect have been reported at doses comparable to those used to treat cervical dystonia and at lower doses [see Warnings and Precautions (5.1)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Instructions for Safe Use
The potency Units of XEOMIN (incobotulinumtoxinA) for injection are specific to the preparation and assay method utilized. They are not interchangeable with other preparations of botulinum toxin products and, therefore, units of biological activity of XEOMIN cannot be compared to or converted into Units of any other botulinum toxin products assessed with any other specific assay method [see Warnings and Precautions (5.2) and Description (11)]. Reconstituted XEOMIN is intended for intramuscular or intra-salivary gland injection only.
The recommended maximum cumulative dose for any indication should not exceed 400 Units in a treatment session.
2.2 Chronic Sialorrhea
XEOMIN is injected into the parotid and submandibular glands on both sides (i.e., 4 injection sites per treatment session). The recommended total dose per treatment session is 100 Units. The dose is divided with a ratio of 3:2 between the parotid and submandibular glands (Table 1).
Figure 1: Glands for Injection in Chronic Sialorrhea
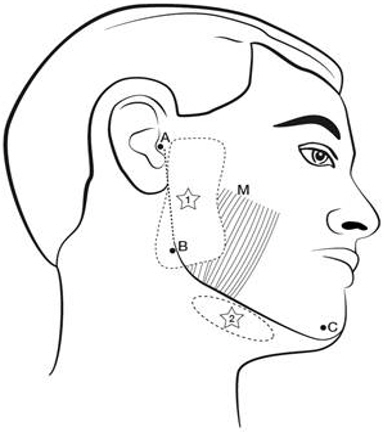
M = Masseter Use the following guidelines if locating salivary glands using anatomic landmarks:
- 1) To inject the parotid gland, find the midpoint on the line connecting the tragus and mandible angle (Site A and B, respectively, Figure 1), approximately at the height of the ear lobe. Deliver the injection one finger breadth anterior to this site (Star 1, Figure 1).
- 2) To inject the submandibular gland, find the midpoint between the angle of the mandible and the tip of the chin (Site B and C, respectively, Figure 1). Deliver the injection one finger breadth medial to the inferior surface of the mandible at this site (Star 2, Figure 1).
Table 1: Dosing by Gland for Treatment of Chronic Sialorrhea Gland(s) Units Per Side Total Parotid gland(s) 30 Units 60 Units Submandibular gland(s) 20 Units 40 Units Both Glands 50 Units 100 Units The concentration used in the clinical study after reconstitution is 5 Units/0.1mL. The timing for repeat treatment should be determined based on the actual clinical need of the individual patient, and no sooner than every 16 weeks.
2.3 Upper Limb Spasticity
The dosage, frequency, and number of injection sites should be tailored to the individual patient based on the size, number, and location of muscles to be treated, severity of spasticity, presence of local muscle weakness, patient's response to previous treatment, and adverse event history with XEOMIN. The frequency of XEOMIN treatments should be no sooner than every 12 weeks. In spasticity patients not previously treated with botulinum toxins, initial dosing should begin at the low end of the recommended dosing range and titrated as clinically necessary. Most patients in clinical studies were retreated between 12-14 weeks.
Table 2: XEOMIN Dosing by Muscle for Treatment of Upper Limb Spasticity Clinical Pattern
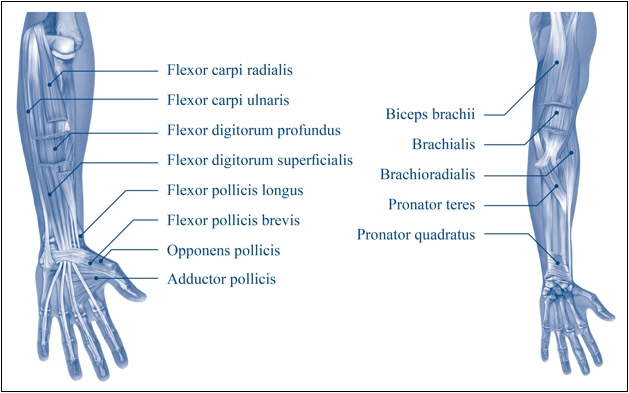
MuscleUnits (Range) Number of injection sites per muscle Clenched Fist Flexor digitorum superficialis 25 Units-100 Units 2 Flexor digitorum profundus 25 Units-100 Units 2 Flexed Wrist Flexor carpi radialis 25 Units-100 Units 1-2 Flexor carpi ulnaris 20 Units-100 Units 1-2 Flexed Elbow Brachioradialis 25 Units-100 Units 1-3 Biceps 50 Units-200 Units 1-4 Brachialis 25 Units-100 Units 1-2 Pronated Forearm Pronator quadratus 10 Units-50 Units 1 Pronator teres 25 Units-75 Units 1-2 Thumb-in-Palm Flexor pollicis longus 10 Units-50 Units 1 Adductor pollicis 5 Units-30 Units 1 Flexor pollicis brevis/Opponens pollicis 5 Units-30 Units 1 Figure 2: Muscles Involved In Adult Upper Limb Spasticity
2.4 Cervical Dystonia
The recommended initial total dose of XEOMIN for cervical dystonia is 120 Units. In a placebo-controlled trial utilizing initial XEOMIN doses of 120 Units and 240 Units, no meaningful difference in effectiveness was demonstrated between the doses [see Clinical Studies (14.3)]. In previously treated patients, their past dose, response to treatment, duration of effect, and adverse event history should be taken into consideration when determining the XEOMIN dose.
In the treatment of cervical dystonia, XEOMIN is usually injected into the sternocleidomastoid, levator scapulae, splenius capitis, scalenus, and/or the trapezius muscle(s). This list is not exhaustive, as any of the muscles responsible for controlling head position may require treatment [see Clinical Studies (14.3)]. The dose and number of injection sites in each treated muscle should be individualized based on the number and location of the muscle(s) to be treated, the degree of spasticity/dystonia, muscle mass, body weight, and response to any previous botulinum toxin injections.
The frequency of XEOMIN repeat treatments should be determined by clinical response, but should generally be no more frequent than every 12 weeks [see Clinical Studies (14.3)].
2.5 Blepharospasm
In treatment-naïve patients, the recommended initial total dose of XEOMIN is 50 Units (25 Units per eye). In patients previously treated with a botulinum toxin A, their past dose, response to treatment, duration of effect, and adverse event history should be taken into consideration when determining the XEOMIN dose.
The total dose of XEOMIN should not exceed 100 Units per treatment session (50 Units per eye).
XEOMIN is injected into the lateral and medial orbicularis oculi muscle of the upper lid; lateral canthus and the lateral orbicularis oculi muscle of the lower lid; and the corrugator muscle, if necessary (see Figure 3). The number and location of injections may be changed in response to adverse reactions or based on the patient's response to treatment, but the total dose should not exceed 50 Units per eye.
Figure 3: Injection Sites for Blepharospasm
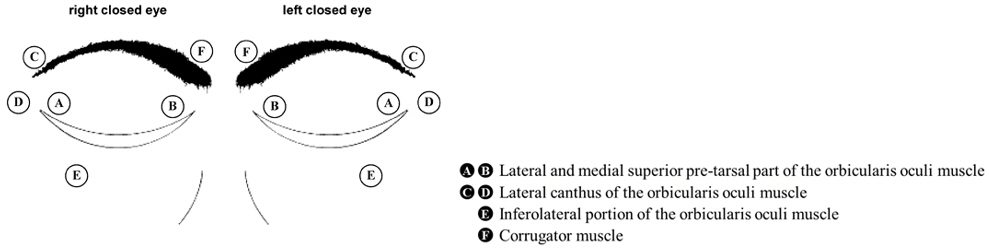
The frequency of XEOMIN repeat treatments should be determined by clinical response but should generally be no more frequent than every 12 weeks [see Clinical Studies (14.4)].
2.6 Glabellar Lines
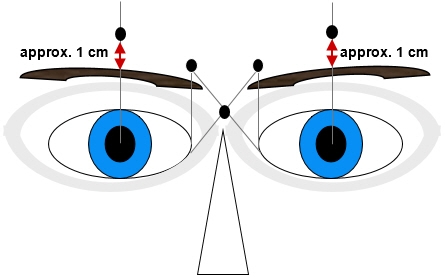
The total recommended XEOMIN dose is 20 Units per treatment session divided into five equal intramuscular injections of 4 Units each. The five injection sites are: two injections in each corrugator muscle and one injection in the procerus muscle.
Retreatment with XEOMIN should be administered no more frequently than every three months.
Figure 4: Injection Sites for Glabellar Lines
2.7 Preparation and Reconstitution Technique
Prior to injection, reconstitute each vial of XEOMIN with sterile, preservative-free 0.9% Sodium Chloride Injection, USP [see Dosage Form and Strengths (3)]. A 20-27 gauge short bevel needle is recommended for reconstitution. Draw up an appropriate amount of preservative-free 0.9% Sodium Chloride Injection, USP into a syringe (see Table 3). Clean the exposed portion of the rubber stopper of the vial with alcohol (70%) prior to insertion of the needle. After vertical insertion of the needle through the rubber stopper, the vacuum will draw the saline into the vial. Gently inject any remaining saline into the vial to avoid foam formation. If the vacuum does not pull the saline into the vial, then XEOMIN must be discarded. Remove the syringe from the vial and mix XEOMIN with the saline by carefully swirling and inverting/flipping the vial – do not shake vigorously. Reconstituted XEOMIN is a clear, colorless solution free of particulate matter. XEOMIN should not be used if the reconstituted solution has a cloudy appearance or contains floccular or particulate matter.
After reconstitution, XEOMIN should be used for only one injection session and for only one patient. Reconstituted XEOMIN solution should be administered within 24 hours after dilution. During this time period, unused reconstituted XEOMIN may be stored in the original container in a refrigerator 2°C -8°C (36°F -46°F) for up to 24 hours until time of use. XEOMIN vials are for single-dose only. Discard any unused portion.
Diluent volumes for reconstitution of XEOMIN are indicated in Table 3.
Table 3: Diluent Volumes for Reconstitution of XEOMIN Volume of Preservative-free 0.9% Sodium Chloride Injection, USP 50 Unit Vial:
Resulting dose in Units per 0.1 mL100 Unit Vial:
Resulting dose in Units per 0.1 mL200 Unit Vial:
Resulting dose in Units per 0.1 mL0.25 mL 20 Units - - 0.5 mL 10 Units 20 Units 40 Units 1 mL 5 Units 10 Units 20 Units 1.25 mL 4 Units 8 Units 16 Units 2 mL 2.5 Units 5 Units 10 Units 2.5 mL 2 Units 4 Units 8 Units 4 mL 1.25 Units 2.5 Units 5 Units 5 mL 1 Unit 2 Units 4 Units 2.8 Administration
Reconstituted XEOMIN is intended for intramuscular or intra-salivary gland injection only.
If proposed injection sites are marked with a pen, the product must not be injected through the pen marks; otherwise a permanent tattooing effect may occur.
For intramuscular injections, the number of injection sites is dependent upon the size of the muscle to be treated and the volume of reconstituted XEOMIN injected.
XEOMIN should be injected carefully when injected at sites close to sensitive structures, such as the carotid artery, lung apices, and esophagus. Before administering XEOMIN, the physician should be familiar with the patient's anatomy and any anatomic alterations, e.g., due to prior surgical procedures.
Chronic Sialorrhea
A sterile needle (e.g., 27-30 gauge (0.30-0.40 mm diameter), 12.5 mm length) should be used for intra-salivary gland administration for the treatment of chronic sialorrhea.
The salivary glands can be located using ultrasound imaging or surface anatomical landmarks [see Dosage and Administration (2.2)].
Upper Limb Spasticity and Cervical Dystonia
A sterile needle (e.g., 26-gauge (0.45 mm diameter), 37 mm length for superficial muscles; or 22-gauge (0.70 mm diameter), 75 mm length for injections into deeper muscles) should be used in the intramuscular administration in the treatment of upper limb spasticity and cervical dystonia.
Localization of the involved muscles with electromyographic guidance or nerve stimulation techniques may be useful.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
XEOMIN is contraindicated in patients with:
- Known hypersensitivity to any botulinum toxin product or to any of the components in the formulation [see Warnings and Precautions (5.3) and Description (11)].
- Infection at the proposed injection site(s) because it could lead to severe local or disseminated infection.
-
5 WARNINGS AND PRECAUTIONS
5.1 Spread of Toxin Effect
Postmarketing safety data from XEOMIN and other approved botulinum toxins suggest that botulinum toxin effects may, in some cases, be observed beyond the site of local injection. The symptoms are consistent with the mechanism of action of botulinum toxin and may include asthenia, generalized muscle weakness, diplopia, blurred vision, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence, and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening and there have been reports of death related to the spread of toxin effects. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can occur in adults treated for spasticity and other conditions, and particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses, including spasticity in children, and in approved indications, symptoms consistent with spread of toxin effect have been reported at doses comparable to or lower than doses used to treat cervical dystonia.
Patients or caregivers should be advised to seek immediate medical care if swallowing, speech, or respiratory disorders occur.
5.2 Lack of Interchangeability between Botulinum Toxin Products
The potency Units of XEOMIN are specific to the preparation and assay method utilized. They are not interchangeable with the other preparations of botulinum toxin products and, therefore, Units of biological activity of XEOMIN cannot be compared to or converted into Units of any other botulinum toxin products assessed with any other specific assay method [see Description (11)].
5.3 Hypersensitivity Reactions
Serious hypersensitivity reactions have been reported with botulinum toxin products. Hypersensitivity reactions include anaphylaxis, serum sickness, urticaria, soft tissue edema, and dyspnea. If serious and/or immediate hypersensitivity reactions occur, discontinue further injection of XEOMIN and institute appropriate medical therapy immediately. The use of XEOMIN in patients with a known hypersensitivity to any botulinum neurotoxin or to any of the excipients (human albumin, sucrose), could lead to a life-threatening allergic reaction [see Contraindications (4)].
5.4 Dysphagia and Breathing Difficulties
Treatment with XEOMIN and other botulinum toxin products can result in swallowing or breathing difficulties. Patients with pre-existing swallowing or breathing difficulties may be more susceptible to these complications. In most cases, this is a consequence of weakening of muscles in the area of injection that are involved in breathing or swallowing. When distant effects occur, additional respiratory muscles may be involved [See Warnings and Precautions (5.1)].
Deaths as a complication of severe dysphagia have been reported after treatment with botulinum toxin. Dysphagia may persist for several months, and require use of a feeding tube to maintain adequate nutrition and hydration. Aspiration may result from severe dysphagia and is a particular risk when treating patients in whom swallowing or respiratory function is already compromised.
Treatment of cervical dystonia with botulinum toxins may weaken neck muscles that serve as accessory muscles of ventilation. This may result in critical loss of breathing capacity in patients with respiratory disorders who may have become dependent upon these accessory muscles. There have been post-marketing reports of serious breathing difficulties, including respiratory failure, in patients with cervical dystonia treated with botulinum toxin products.
Patients with smaller neck muscle mass and patients who require bilateral injections into the sternocleidomastoid muscles have been reported to be at greater risk of dysphagia. In general, limiting the dose injected into the sternocleidomastoid muscle may decrease the occurrence of dysphagia.
Patients treated with botulinum toxin may require immediate medical attention should they develop problems with swallowing, speech or respiratory disorders. These reactions can occur within hours to weeks after injection with botulinum toxin [See Warnings and Precautions (5.1) and Adverse Reactions (6.1)].
Patients with neuromuscular disorders with peripheral motor neuropathic diseases, amyotrophic lateral sclerosis, or neuromuscular junctional disorders (e.g., myasthenia gravis or Lambert-Eaton syndrome) may be at increased risk for severe dysphagia and respiratory compromise from typical doses of XEOMIN.
5.5 Corneal Exposure, Corneal Ulceration, and Ectropion in Patients Treated for Blepharospasm
Reduced blinking from injection of botulinum toxin products in the orbicularis muscle can lead to corneal exposure, persistent epithelial defect, and corneal ulceration, especially in patients with VII nerve disorders. As patients with previous eye surgery may have reduced corneal sensation, carefully assess corneal sensation before treatment. Vigorous treatment of any corneal epithelial defect should be employed. This may require protective drops, ointment, therapeutic soft contact lenses, or closure of the eye by patching or other means. Because of its anticholinergic effects, XEOMIN should be used with caution in patients at risk of developing narrow angle glaucoma. To decrease the risk for ectropion, XEOMIN should not be injected into the medial lower eyelid area.
Ecchymosis easily occurs in the soft tissues of the eyelid. Immediate gentle pressure at the injection site can limit the size.
5.6 Risk of Ptosis in Patients Treated for Glabellar Lines
Do not exceed the recommended dosage and frequency of administration of XEOMIN.
In order to reduce the complication of ptosis the following steps should be taken:
- Avoid injection near the levator palpebrae superioris, particularly in patients with larger brow depressor complexes.
- Corrugator injections should be placed at least 1 cm above the bony supraorbital ridge.
5.7 Human Albumin and Transmission of Viral Diseases
This product contains albumin, a derivative of human blood. Based on effective donor screening and product manufacturing processes, it carries an extremely remote risk for transmission of viral diseases and variant Creutzfeldt-Jakob disease (vCJD). There is a theoretical risk for transmission of Creutzfeldt-Jakob disease (CJD), but if that risk actually exists, the risk of transmission would also be considered extremely remote. No cases of transmission of viral diseases, CJD, or vCJD have ever been identified for licensed albumin or albumin contained in other licensed products.
-
6 ADVERSE REACTIONS
The following adverse reactions to XEOMIN are discussed in greater detail in other sections of the labeling:
- Spread of Effects from Toxin [see Warnings and Precautions (5.1)]
- Lack of Interchangeability between Botulinum Toxin Products [see Warnings and Precautions (5.2)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.3)]
- Dysphagia and Breathing Difficulties [see Warnings and Precautions (5.4)]
- Corneal Exposure, Corneal Ulceration, and Ectropion in Patients Treated with XEOMIN for Blepharospasm [see Warnings and Precautions (5.5)]
- Risk of Ptosis in Patients Treated for Glabellar Lines [see Warnings and Precautions (5.6)]
- Human Albumin and Transmission of Viral Diseases [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Chronic Sialorrhea
Table 4 lists the adverse reactions that occurred in ≥3% of XEOMIN-treated patients in the double-blind, placebo-controlled phase of the study in patients with chronic sialorrhea [see Clinical Studies (14.1)]. The most common adverse reactions (≥4%) were tooth extraction, dry mouth, diarrhea, and hypertension. In the controlled portion of this study, 74 patients received 100 Units of XEOMIN and 36 patients received placebo. XEOMIN-treated patients were 21-80 years old (mean 65 years), and were predominantly male (71%) and white (99.5%).
Table 4: Adverse Reactions (≥3%) and Greater for XEOMIN than Placebo: Double-Blind Phase of the Placebo-Controlled Chronic Sialorrhea Study Adverse Reaction XEOMIN 100 Units
(N = 74)
%Placebo
(N = 36)
%Tooth extraction 5 0 Dry mouth 4 0 Diarrhea 4 3 Hypertension 4 3 Fall 3 0 Bronchitis 3 0 Dysphonia 3 0 Back pain 3 0 Dry eye 3 0 Upper Limb Spasticity
Table 5 lists the adverse reactions that occurred in ≥2% of XEOMIN-treated patients in two placebo-controlled, Phase 3 studies in patients with upper limb spasticity. Study 1 and Study 2 were both double-blind, placebo-controlled studies, with an open-label extension [see Clinical Studies (14.2)]. In the controlled portion of these studies, 283 patients received ≥120 Units to 400 Units, of which 217 patients received at least 400 units of XEOMIN, and 182 patients received placebo. XEOMIN-treated patients were 20-79 years old (mean 56 years), and were predominantly male (58%) and white (84%).
Table 5: Adverse Reactions (≥2%) and Greater for XEOMIN than Placebo: Double-Blind Phase of Placebo-Controlled Upper Limb Spasticity Study 1 and Study 2 Adverse Reaction XEOMIN 400 Units
(N = 217)
%Placebo
(N = 182)
%Seizure 3 0 Nasopharyngitis 2 0 Dry mouth 2 1 Upper respiratory tract infection 2 1 Cervical Dystonia
The data described below reflect exposure to a single intramuscular dose of XEOMIN in a placebo-controlled, Phase 3 trial in patients with cervical dystonia [see Clinical Studies (14.3)]. In this study, 159 patients received XEOMIN (78 were randomized to receive a total dose of 120 Units, and 81 were randomized to receive a total dose of 240 Units). XEOMIN-treated patients were 18 to 79 years old (mean 53 years), and were predominantly female (66%) and Caucasian (91%). At study baseline, approximately 25% had mild, 50% had moderate, and 25% had severe cervical dystonia. Approximately 61% of XEOMIN-treated patients had previously received another botulinum toxin type A product. Table 6 lists adverse reactions that occurred in ≥5% of XEOMIN-treated patients (in any treatment group) and greater than placebo.
Table 6: Adverse Reactions (≥5%) and Greater for XEOMIN than Placebo: Double-Blind Phase of the Placebo-Controlled Cervical Dystonia Study Adverse Reaction XEOMIN 120 Units
(N=77)
%XEOMIN 240 Units
(N=82)
%Placebo
(N=74)
%Musculoskeletal and connective tissue disorders 23 32 11 Neck pain 7 15 4 Muscular weakness 7 11 1 Musculoskeletal pain 7 4 1 Gastrointestinal disorders 18 24 4 Dysphagia 13 18 3 Nervous system disorders 16 17 7 General disorders and administration site conditions 16 11 11 Injection site pain 9 4 7 Infections and infestations 14 13 11 Respiratory, thoracic and mediastinal disorders 13 10 3 Blepharospasm
Study 1 was a randomized, double-blind, placebo-controlled study that only included treatment-naïve patients [see Clinical Studies (14.3)]. In the controlled portion, 22 patients received XEOMIN 25 Units, 19 patients received 50 Units, and 20 patients received placebo. XEOMIN-treated patients were 23 to 78 years of age (mean 55 years). Fifty-nine percent of the patients were women, 77% were Asian, and 23% White. No patients withdrew prematurely because of an adverse event. Table 7 lists the adverse reactions that occurred in ≥6% of XEOMIN-treated patients and greater than placebo.
Table 7: Adverse Reactions (≥6%) and Greater for XEOMIN than Placebo: Double-Blind Phase of the Placebo-Controlled Blepharospasm Study 1 Adverse Reaction XEOMIN 50 U
(N=19)
%Placebo
(N=20)
%Eye disorders 21 10 Eyelid ptosis 16 0 Study 2 was a double-blind, placebo-controlled, flexible dose study with an open-label extension (OLEX) period. The study only included patients previously treated with onabotulinumtoxinA (Botox) [see Clinical Studies (14.4)]. In the controlled portion, 74 patients received XEOMIN at a mean dose of approximately 33 Units per eye (minimum 10 Units, maximum 50 Units). XEOMIN-treated patients were 22 to 79 years of age (mean 62 years), predominantly female (65%), and Caucasian (60%). Table 8 lists the adverse reactions that occurred in ≥5% of XEOMIN-treated patients and greater than placebo.
Table 8: Adverse Reactions (≥5%) and Greater for XEOMIN than Placebo: Double-Blind Phase of the Placebo-Controlled Blepharospasm Study 2 Adverse Reaction XEOMIN
(N=74)
%Placebo
(N=34)
%- * including vision blurred
Eye disorders 38 21 Eyelid ptosis 19 9 Dry eye 16 12 Visual impairment* 12 6 Gastrointestinal disorders 30 15 Dry mouth 16 3 Diarrhea 8 0 Infections and infestations 20 15 Nasopharyngitis 5 3 Respiratory tract infection 5 3 Nervous system disorders 14 9 Headache 7 3 General disorders and administration site conditions 11 9 Respiratory, thoracic and mediastinal disorders 11 3 Dyspnea 5 3 Glabellar Lines
In three placebo-controlled trials in 803 subjects with glabellar lines, 535 subjects received a single dose of 20 Units XEOMIN and 268 subjects received placebo. XEOMIN-treated subjects were 24 to 74 years old, and were predominantly female (88%). The most frequent adverse reactions in XEOMIN-treated subjects were: headache (5%), facial paresis (0.7%), injection site hematoma (0.6%) and eyelid edema (0.4%). Four serious adverse events occurred in two placebo-treated subjects. Six XEOMIN treated subjects experienced six serious adverse events. All serious adverse events were assessed as unrelated to study drug.
The adverse reactions below reflect exposure to XEOMIN with glabellar lines in placebo-controlled studies. Adverse reactions are adverse events in which there is some basis to believe there is a causal relationship between the drug and the occurrence of the adverse event.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Table 9: Adverse Reactions in Placebo-Controlled Glabellar Lines Trials Adverse Reaction XEOMIN
(N=535)
%Placebo
(N=268)
%Nervous system disorders 6 2 Headache 5 2 Facial paresis (brow ptosis) 0.7 0 General disorders and administration site conditions 0.9 0.7 Injection site hematoma 0.6 0 Injection site pain 0.2 0 Facial pain 0.2 0 Injection site swelling 0 0.4 Sensation of pressure 0 0.4 Eye disorders 0.9 0 Eyelid edema 0.4 0 Blepharospasm 0.2 0 Eye disorder 0.2 0 Eyelid ptosis 0.2 0 In open-label, multiple-dose trials, adverse reactions were reported for 105 of the 800 subjects (13%). Headache was the most common adverse reaction, reported in 7% of subjects, followed by injection site hematoma (1%). Adverse reactions reported in less than 1% of subjects were: facial paresis (brow ptosis), muscle disorder (elevation of eyebrow), injection site pain, and eyelid edema.
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity.
The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other botulinumtoxinA products may be misleading.
Of the 1490 patients treated with XEOMIN in placebo-controlled clinical trials supporting approved indications [see Clinical Studies (14)], 5 (0.3%) patients were positive for neutralizing antibodies after treatment whose antibody status at baseline was unknown and 4 (0.2%) additional patients developed neutralizing antibodies after treatment. No patients demonstrated a secondary lack of treatment response due to neutralizing antibodies.
Chronic Sialorrhea
Of the 180 patients treated with XEOMIN in the main phase and extension period of the chronic sialorrhea clinical trial [see Clinical Studies (14.1)], 1 (0.6%) patient was positive for neutralizing antibodies after treatment. The patient had an antibody status unknown at baseline, and had not received a botulinum toxin treatment in the 12 months prior to enrollment in the study. No patients demonstrated a secondary lack of treatment response due to neutralizing antibodies.
Upper Limb Spasticity
Of the 456 patients treated with XEOMIN in the main phase and open-label extension period of the upper limb spasticity clinical trials (Study 1 and Study 2) [see Clinical Studies (14.2)], 4 patients were positive for neutralizing antibodies at baseline, and 2 (0.4%) additional patients (with unknown antibody status at baseline) were positive after treatment. Both patients had not received a botulinum toxin treatment in the 12 months prior to enrollment in the studies. No patients demonstrated a secondary lack of treatment response due to neutralizing antibodies.
Cervical Dystonia
Of the 227 patients treated with XEOMIN in the main phase and open-label extension period of the cervical dystonia clinical trial [see Clinical Studies (14.3)], 5 patients were positive for neutralizing antibodies at baseline, 1 (0.4%) patient (with unknown antibody status at baseline) was positive after treatment, and 4 (1.8%) additional patients developed neutralizing antibodies after treatment. All of these patients were pre-treated with onabotulinumtoxinA prior to enrollment in the study. No patients demonstrated a secondary lack of treatment response due to neutralizing antibodies.
Blepharospasm
Of the 163 patients treated with XEOMIN in the main phase and open-label extension period of the blepharospasm clinical trials (Study 1 and Study 2) [see Clinical Studies (14.4)], 1 (0.6%) patient (with unknown antibody status at baseline) was positive for neutralizing antibodies after treatment. The patient had not received a botulinum toxin treatment in the 12 months prior to enrollment in the studies. No patients demonstrated a secondary lack of treatment response due to neutralizing antibodies.
Glabellar Frown Lines
Of the 464 patients treated with XEOMIN in the main phase and open-label extension period of the glabellar frown lines clinical trials (GL-1 and GL-2) [see Clinical Studies (14.5)], no patients developed neutralizing antibodies after treatment. No patients demonstrated a secondary lack of treatment response due to neutralizing antibodies.
6.3 Postmarketing Experience
The following adverse reactions have been reported during post-approval use of XEOMIN. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: eye swelling, eyelid edema, dysphagia, nausea, flu-like symptoms, injection site pain, injection site reaction, allergic dermatitis, localized allergic reactions like swelling, edema, erythema, pruritus or rash, herpes zoster, muscular weakness, muscle spasm, dysarthria, myalgia and hypersensitivity.
-
7 DRUG INTERACTIONS
7.1 Aminoglycosides and Other Agents Interfering with Neuromuscular Transmission
Co-administration of XEOMIN and aminoglycosides or other agents interfering with neuromuscular transmission (e.g., tubocurarine-type muscle relaxants) should only be performed with caution as these agents may potentiate the effect of the toxin.
7.2 Anticholinergic Drugs
Use of anticholinergic drugs after administration of XEOMIN may potentiate systemic anticholinergic effects.
7.3 Other Botulinum Neurotoxin Products
The effect of administering different botulinum toxin products at the same time or within several months of each other is unknown. Excessive neuromuscular weakness may be exacerbated by administration of another botulinum toxin prior to the resolution of the effects of a previously administered botulinum toxin.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate data on the developmental risk associated with the use of XEOMIN in pregnant women. XEOMIN should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. XEOMIN was embryotoxic in rats and increased abortions in rabbits when given at doses higher than the maximum recommended human dose (MRHD) for cervical dystonia (120 Units), on a body weight basis.
In the U.S. general population, the estimated background risk of major birth defects and miscarriages in clinically recognized pregnancies is 2-4% and 15-20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Data
Animal Data
When XEOMIN was administered intramuscularly to pregnant rats during organogenesis (3 Units/kg, 10 Units/kg, or 30 Units/kg on gestational days [GDs] 6, 12, and 19; or 7 Units/kg on GDs 6 to 19; or 2 Units/kg, 6 Units/kg, or 18 Units/kg on GDs 6, 9, 12, 16, and 19), decreases in fetal body weight and skeletal ossification were observed at doses that were also maternally toxic. The no-effect level for embryotoxicity in rats was 6 Units/kg (3 times the MRHD for cervical dystonia on a body weight basis). Intramuscular administration to pregnant rabbits during organogenesis (1.25 Units/kg, 2.5 Units/kg, or 5.0 Units/kg on GDs 6, 18, and 28) resulted in an increased rate of abortion at the highest dose, which was also maternally toxic. In rabbits, the no-effect level for increased abortion was 2.5 Units/kg (similar to the MRHD for cervical dystonia on a body weight basis).
8.2 Lactation
Risk Summary
There are no data on the presence of XEOMIN in human milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for XEOMIN and any potential adverse effects on the breastfed infant from XEOMIN or from the underlying maternal conditions.
8.4 Pediatric Use
Safety and effectiveness of XEOMIN in patients less than 18 years of age have not been established [see Warnings and Precautions (5.1)].
8.5 Geriatric Use
Chronic Sialorrhea
Of the total number of 184 patients in the placebo-controlled study in chronic sialorrhea [see Clinical Studies (14.1)], 107 were 65 years of age and over (46 treated with XEOMIN 100 Units, 44 treated with XEOMIN 75 Units, and 17 received placebo). No differences in safety or effectiveness were observed between older and younger patients. Other clinical studies have not identified differences in responses between older and younger patients, but increased sensitivity in older patients cannot be ruled out.
Upper Limb Spasticity
Of the total number of 283 patients in the placebo-controlled studies in upper limb spasticity [see Clinical Studies (14.2)], 118 were 65 years of age and over (70 treated with XEOMIN and 48 received placebo), which included 12 patients 75 years of age and over (7 treated with XEOMIN and 5 received placebo). No overall differences in safety or effectiveness were observed between older and younger patients. Other clinical studies have not identified differences in responses between older and younger patients, but increased sensitivity in older patients cannot be ruled out.
Cervical Dystonia
Of the total number of 233 patients in the placebo-controlled study in cervical dystonia [see Clinical Studies (14.3)], 29 were 65 years of age and over (19 treated with XEOMIN and 10 received placebo). Of these, ten XEOMIN-treated patients and four placebo-treated patients experienced an adverse event. For patients 65 years of age and over treated with XEOMIN, the most common adverse events were dysphagia (21%) and asthenia (11%).
Blepharospasm
Of the total number of 169 patients in the placebo-controlled studies in blepharospasm [see Clinical Studies (14.4)], 61 were 65 years of age and over (45 treated with XEOMIN and 16 received placebo). No overall difference in effectiveness was observed between older and younger patients.
Glabellar Lines
There are limited clinical data with XEOMIN in subjects 65 years of age and over in clinical studies with glabellar lines. Of the total number of 547 subjects in the placebo-controlled clinical studies [see Clinical Studies (14.5)], 21 subjects were 65 years of age and over. Efficacy was observed in 20% (3/15) of XEOMIN subjects 65 years of age and over. For the entire safety database of geriatric subjects, there was no increase in the incidence of adverse events related to treatment with XEOMIN.
-
10 OVERDOSAGE
Excessive doses of XEOMIN may be expected to produce neuromuscular weakness with a variety of symptoms, particularly when treated intramuscularly. Respiratory support may be required where excessive doses cause paralysis of the respiratory muscles. In the event of overdose, the patient should be medically monitored for symptoms of excessive muscle weakness or muscle paralysis [See Warnings and Precautions (5.1, 5.4)]. Symptomatic treatment may be necessary.
Symptoms of overdose are not likely to be present immediately following injection. Should accidental injection or oral ingestion occur, the person should be medically supervised for several weeks for signs and symptoms of excessive muscle weakness or paralysis.
There is no significant information regarding overdose from clinical studies of XEOMIN.
In the event of overdose, antitoxin raised against botulinum toxin is available from the Centers for Disease Control and Prevention (CDC) in Atlanta, GA. However, the antitoxin will not reverse any botulinum toxin-induced effects already apparent by the time of antitoxin administration. In the event of suspected or actual cases of botulinum toxin poisoning, please contact your local or state Health Department to process a request for antitoxin through the CDC. If you do not receive a response within 30 minutes, please contact the CDC directly at 770-488-7100. More information can be obtained at http://www.cdc.gov/ncidod/srp/drugs/formulary.html#1a.
-
11 DESCRIPTION
The active ingredient of XEOMIN is botulinum toxin type A produced from fermentation of Hall strain Clostridium botulinum serotype A. The botulinum toxin complex is purified from the culture supernatant and then the active ingredient is separated from the proteins (hemagglutinins and non-hemagglutinins) through a series of steps yielding the active neurotoxin with molecular weight of 150 kDa, without accessory proteins. XEOMIN is a sterile white to off-white lyophilized powder intended for intramuscular or intra-salivary gland injection after reconstitution with preservative-free 0.9% Sodium Chloride Injection, USP (3). One vial of XEOMIN contains 50 Units, 100 Units, or 200 Units of incobotulinumtoxinA, human albumin (1 mg), and sucrose (4.7 mg).
The primary release procedure for XEOMIN uses a cell-based potency assay to determine the potency relative to a reference standard. One Unit corresponds to the median intraperitoneal lethal dose (LD50) in mice. As the method for conducting the assay is specific to XEOMIN, Units of biological activity of XEOMIN cannot be converted into Units of any other botulinum toxin assessed with other specific assays.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
XEOMIN blocks cholinergic transmission at the neuromuscular and salivary neuroglandular junction by inhibiting the release of acetylcholine from peripheral cholinergic nerve endings. This inhibition occurs according to the following sequence: neurotoxin binding to cholinergic nerve terminals, internalization of the neurotoxin into the nerve terminal, translocation of the light-chain part of the molecule into the cytosol of the nerve terminal, and enzymatic cleavage of SNAP25, a presynaptic target protein essential for the release of acetylcholine. In both muscles and glands, impulse transmission is re-established by the formation of new nerve endings.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Impairment of Fertility
In a fertility and early embryonic development study in rabbits, males and females were dosed with XEOMIN (1.25 Units/kg, 2.5 Units/kg, or 3.5 Units/kg) intramuscularly every two weeks for 5 and 3 doses, respectively, beginning 2 weeks prior to mating. No effects on mating or fertility were observed. The highest dose tested is approximately twice the maximum recommended human dose for cervical dystonia (120 Units) on a body weight basis.
-
14 CLINICAL STUDIES
14.1 Chronic Sialorrhea
The efficacy and safety of XEOMIN for the treatment of chronic sialorrhea were evaluated in a double-blind, placebo-controlled clinical trial that enrolled a total of 184 patients with chronic sialorrhea resulting from Parkinson's disease, atypical parkinsonism, stroke, or traumatic brain injury, that was present for at least three months. Patients with a history of aspiration pneumonia, amyotrophic lateral sclerosis, salivary gland or duct malformation, and gastroesophageal reflux disease were excluded. The study consisted of a 16-week main phase, followed by an extension period of dose-blinded treatment with XEOMIN.
In the main phase, a fixed total dose of XEOMIN (100 Units or 75 Units) or placebo was administered into the parotid and submandibular salivary glands in a 3:2 dose ratio. The co-primary efficacy variables were the change in unstimulated Salivary Flow Rate (uSFR, Table 10) and the change in Global Impression of Change Scale (GICS, Table 11) at Week 4 post-injection. A total of 173 treated patients completed the main phase of the study. For both the uSFR and GICS, XEOMIN 100 Units was significantly better than placebo (see Table 10 and Table 11). XEOMIN 75 Units was not significantly better than placebo.
Table 10: Change in uSFR (g/min) from Baseline at Week 4, 8, 12, and 16 of Main Phase XEOMIN
100 UnitsPlacebo N = 73 N=36 - * p=0.004
Week 4* -0.13 -0.04 Week 8 -0.13 -0.02 Week 12 -0.12 -0.03 Week 16 -0.11 -0.01 Table 11: Mean GICS at Week 4, 8, 12, and 16 of Main Phase XEOMIN
100 UnitsPlacebo N = 74 N=36 - * p=0.002
Week 4* 1.25 0.67 Week 8 1.30 0.47 Week 12 1.21 0.56 Week 16 0.93 0.41 In the extension period, patients received up to 3 additional treatments with XEOMIN 100 Units or 75 Units every 16±2 weeks, for a total exposure duration of up to 64 weeks. Patients had periodic dental examinations to monitor for changes in dentition and oral mucosa. A total of 151 patients completed the extension period.
14.2 Upper Limb Spasticity
The efficacy and safety of XEOMIN for the treatment of upper limb spasticity were evaluated in two Phase 3, randomized, multi-center, double-blind studies.
Study 1 and Study 2 were both prospective, double-blind, placebo-controlled, randomized, multi-center trials with an open-label extension period (OLEX) to investigate the efficacy and safety of XEOMIN in the treatment of post-stroke spasticity of the upper limb. For patients who had previously received botulinum toxin treatment in any body region, Study 1 and Study 2 required that ≥ 12 months and ≥ 4 months, respectively, had passed since the most recent botulinum toxin administration.
Study 1 consisted of a 12-week main phase followed by three 12-week OLEX treatment cycles for a total exposure duration of 48 weeks. The study included 317 treatment-naïve patients who were at least three months post-stroke in the main study period (210 XEOMIN and 107 placebo). During the main period, XEOMIN (fixed total dose of 400 Units) and placebo were administered intramuscularly to the defined primary target clinical pattern chosen from among the flexed elbow, flexed wrist, or clenched fist patterns and to other affected muscle groups. 296 treated patients completed the main phase and participated in the first OLEX cycle. Each OLEX cycle consisted of a single treatment session (XEOMIN 400 Units total dose, distributed among all affected muscles) followed by a 12 week observation period.
Study 2 consisted of a 12 - 20 week main phase followed by an OLEX period of 48 – 69 weeks for up to 89 weeks of exposure to XEOMIN. The study included 148 treatment-naïve and pre-treated patients with a confirmed diagnosis of post-stroke spasticity of the upper limb who were at least six months post-stroke (73 XEOMIN and 75 placebo). During the main period, for each patient, the clinical patterns of flexed wrist and clenched fist were treated with fixed doses (90 Units and 80 Units, respectively). Additionally, if other upper limb spasticity patterns were present, the elbow, forearm and thumb muscles could be treated with fixed doses of XEOMIN per muscle. 145 patients completed the main phase and participated in the OLEX period, during which time the dosing of each involved muscle could be adapted individually. During the main and OLEX periods, the maximum total dose per treatment session and 12-week interval was 400 Units.
The average XEOMIN doses injected into specific muscles and the number of injection sites per muscle in Study 1 and Study 2 are presented in Table 12.
Table 12: Doses Administered to Individual Muscles (Main Period) in Study 1 and Study 2 Intent to Treat (ITT) Muscle Group Muscle Study 1
Units InjectedInjection Site Per Muscle Study 2
Units InjectedInjection Site Per Muscle XEOMIN
(N=210)
Mean±SDXEOMIN
Median
(Min; Max)XEOMIN
(N=73)
Mean±SDXEOMIN
Median
(Min; Max)All Overall 400 ± 2 Units -- 307 ± 77 Units -- Elbow flexors Overall 151 ± 50 Units 5 (1; 11) 142 ± 30 Units 5 (2; 9) Biceps 90 ± 21 Units 3 (1; 4) 80 ± 0 Units 3 (2; 4) Brachialis 52 ± 26 Units 2 (1; 4) 50 ± 0 Units 2 (1; 2) Brachioradialis 43 ± 16 Units 2 (1; 3) 60 ± 2Units 2 (1; 3) Wrist flexors Overall 112 ± 43 Units 4 (1; 6) 90 ± 0 Units 4 (4; 4) Flexor carpi radialis 58 ± 22 Units 2 (1; 3) 50 ± 0 Units 2 (2; 2) Flexor carpi ulnaris 56 ± 22 Units 2 (1; 3) 40 ± 0 Units 2 (2; 2) Finger flexors Overall 104 ± 35 Units 4 (1; 4) 80 ± 0 Units 4 (4; 4) Flexor digitorum profundus 54 ± 19 Units 2 (1; 2) 40 ± 0 Units 2 (2; 2) Flexor digitorum superficialis 54 ± 19 Units 2 (1; 2) 40 ± 0 Units 2 (2; 2) Forearm pronators Overall 52 ± 24 Units 2 (1; 3) 47 ± 16 Units 2 (1; 3) Pronator quadratus 26 ± 13 Units 1 (1; 1) 25 ± 0 Units 1 (1; 1) Pronator teres 42 ± 13 Units 1 (1; 2) 40 ± 0 Units 1.5 (1; 2) Thumb flexors/adductors Overall 37 ± 25 Units 2 (1; 4) 25 ± 10 Units 1.5 (1; 3) Adductor pollicis 14 ± 8 Units 1 (1; 1) 10 ± 0 Units 1 (1; 1) Flexor pollicis brevis / opponens pollicis 14 ± 9 Units 1 (1; 1) 10 ± 0 Units 1 (1; 1) Flexor pollicis longus 26 ± 16 Units 1 (1; 2) 20 ± 0 Units 1 (1; 1) In Study 1, the primary efficacy variable was the change from baseline in Ashworth Scale (AS) score of the primary target clinical pattern determined by the investigator at the Week 4 visit. The Ashworth Scale is a clinical measure of the severity of spasticity by judging resistance to passive movement. The spasticity of the elbow flexors, wrist flexors, finger flexors, and thumb muscles as well as the forearm pronators was assessed on the 0 to 4-point Ashworth scale at each visit.
Table 13: Efficacy Results by Patterns of Spasticity in Study 1, Week 4 Mean Change in Ashworth Scale XEOMIN
(N=171)Placebo
(N=88)The analysis is based on Last Observation Carried Forward in the Intent To Treat population. p<0.001 Total Primary Target Clinical Pattern (flexed wrist, flexed elbow, and clenched fist) -0.9 -0.5 The co-primary efficacy variable of Study 1 was the Investigator's Global Impression of Change Scales (GICS) after 4 Weeks of treatment with XEOMIN or placebo. The GICS is a global measure of a subject's functional improvement. Investigators were asked to evaluate the subject's global change in spasticity of the upper limb due to treatment, compared to the condition before the last injection. The response was assessed using a 7-point Likert scale that ranges from –3 (very much worse) to +3 (very much improved). A greater percentage of XEOMIN-treated subjects (43%) than placebo-treated subjects (23%) reported 'very much improved' and 'much improved' in their spasticity (see Figure 5).
Figure 5: Investigator's GICS in Study 1
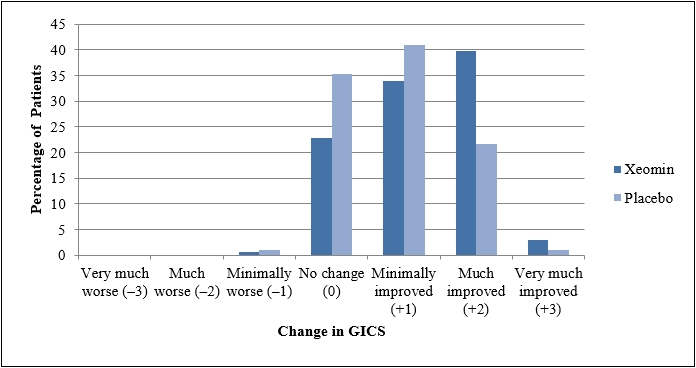
XEOMIN was considered to be superior to placebo in Study 1 only if statistical significance was reached in both the AS and GICS variables.
14.3 Cervical Dystonia
XEOMIN has been investigated in a Phase 3, randomized, double-blind, placebo-controlled, multi-center trial in a total of 233 patients with cervical dystonia. Patients had a clinical diagnosis of predominantly rotational cervical dystonia, with baseline Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) total score ≥20, TWSTRS severity score ≥10, TWSTRS disability score ≥3, and TWSTRS pain score ≥1. For patients who had previously received a botulinum toxin treatment for cervical dystonia, the trial required that ≥10 weeks had passed since the most recent botulinum toxin administration. Patients with swallowing disorders or any significant neuromuscular disease that might interfere with the study were excluded from enrollment. Patients were randomized (1:1:1) to receive a single administration of XEOMIN 240 Units (n=81), XEOMIN 120 Units (n=78), or placebo (n=74). Each patient received a single administration of 4.8 mL of reconstituted study agent (XEOMIN 240 Units, XEOMIN 120 Units, or placebo). The investigator at each site decided which muscles would receive injections of the study agent, the number of injection sites, and the volume at each site. The muscles most frequently injected were the splenius capitis/semispinalis, trapezius, sternocleidomastoid, scalene, and levator scapulae muscles. Table 14 indicates the average XEOMIN dose, and percentage of total dose, injected into specific muscles in the pivotal clinical trial.
Table 14: XEOMIN 120 Units Initial Dose (Units and % of the Total Dose) by Unilateral Muscle Injected During Double Blind Pivotal Phase 3 Study XEOMIN Dose Injected Number of Patients Injected Per Muscle Median XEOMIN Units 75th percentile XEOMIN Units Sternocleidomastoid 63 25 35 Splenius capitis/ Semispinalis capitis 78 48 63 Trapezius 55 25 38 Levator scapulae 49 25 25 Scalenus (medius and anterior) 27 20 25 Most patients received a total of 2-10 injections into the selected muscles. Patients were assessed by telephone at one week post-injection, during clinic visits at Weeks 4 and 8, and then by telephone assessments or clinic visits every two weeks up to Week 20.
The mean age of the study patients was 53 years, and 66% of the patients were women. At study baseline, 61% of patients had previously received a botulinum toxin as treatment for cervical dystonia. The study was completed by 94% of study patients. Three patients discontinued the study prematurely due to adverse events: two patients in the 240 Unit group experienced musculoskeletal pain and muscle weakness, and one patient in the 120 Unit group experienced nausea and dizziness.
The primary efficacy endpoint was the change in the TWSTRS total score from baseline to Week 4 post-injection, in the intent-to-treat (ITT) population, with missing values replaced by the patient's baseline value. In the ITT population, the difference between the XEOMIN 240 Unit group and the placebo group in the change of the TWSTRS total score from baseline to Week 4 was -9.0 points, 95% confidence interval (CI) -12.0; -5.9 points; the difference between the XEOMIN 120 Unit group and the placebo group in the change of the TWSTRS total score from baseline to Week 4 was -7.5 points, 95% CI -10.4; -4.6 points.
Figure 6 illustrates the cumulative percentage of patients from each of the three treatment groups who had attained the specified change in TWSTRS Score from baseline versus 4 weeks post-injection. Three change scores have been identified for illustrative purposes, and the percent of patients in each group achieving that result is shown.
Figure 6: Cumulative Percentage of Patients with Specified Changes from Baseline TWSTRS Total Score at Week 4
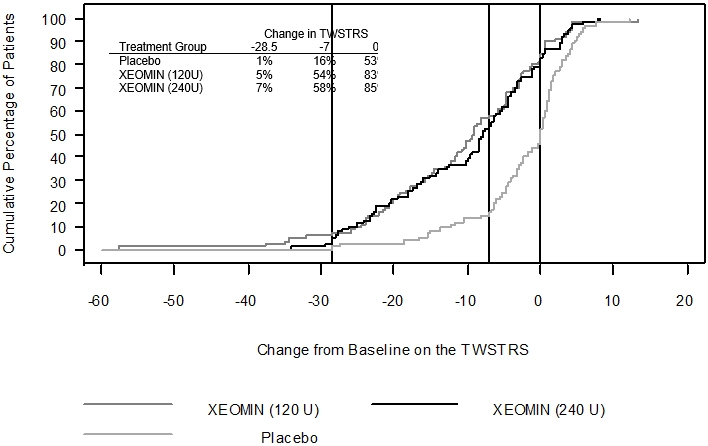
The curves demonstrate that both patients assigned to placebo and XEOMIN have a wide range of responses, but that the active treatment groups are more likely to show greater improvements. A curve for an effective treatment would be shifted to the left of the curve for placebo, while an ineffective or deleterious treatment would be superimposed upon or shifted to the right of the curve for placebo.
Comparison of each XEOMIN group to the placebo group was statistically significant at p<0.001. Initial XEOMIN doses of 120 Units and 240 Units demonstrated no significant difference in effectiveness between the doses. The efficacy of XEOMIN was similar in patients who were botulinum toxin naïve and those who had received botulinum toxin prior to this study.
Examination of age and gender subgroups did not identify differences in response to XEOMIN among these subgroups. There were too few non-white patients enrolled to adequately assess efficacy in other racial populations.
14.4 Blepharospasm
Treatment-Naïve Patients
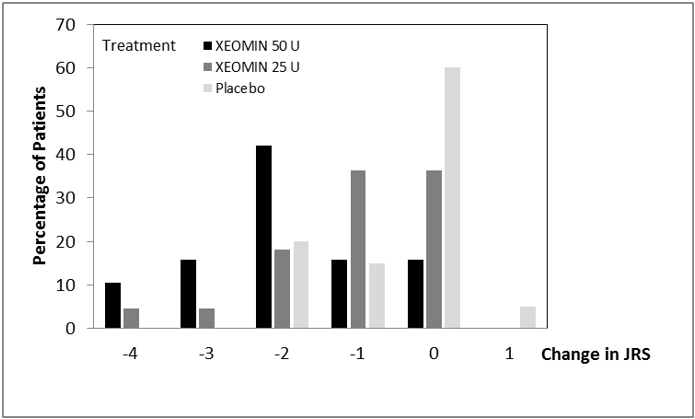
The efficacy and safety of XEOMIN for the treatment of blepharospasm in treatment-naïve patients were evaluated in Study 1, a randomized, double-blind, placebo-controlled, multi-center trial in a total of 61 patients. Patients had a clinical diagnosis of blepharospasm, with a baseline Jankovic Rating Scale (JRS) severity subscore ≥2. Patients were defined as treatment-naïve if at least 12 months had passed since their last botulinum toxin treatment for blepharospasm. During the placebo-controlled phase, a fixed total dose of 25 Units XEOMIN (n=22), 50 Units XEOMIN (n=19), or placebo (n=20) was administered intramuscularly at 6 injection sites per eye (Figure 3). Of the 61 patients randomized, 55 patients completed the placebo-controlled phase. Patients only continued to the open-label extension (OLEX) period if they had a confirmed need for a re-injection by week 20 of the placebo-controlled phase. A total of 39 patients entered and completed the OLEX phase.
The primary efficacy variable was the change from baseline in JRS Severity subscore determined at Week 6 after the injection. The 50 Unit treatment group demonstrated statistically significant improvements compared to placebo, with a difference of -1.2 (p=0.0004). The change from baseline in the JRS Severity subscore for the 25 Unit treatment group 6 weeks after the injection was not statistically significant, with a difference of -0.5 (p=0.1452) compared to placebo (see Figure 7).
Figure 7: Frequency Distribution of Changes from Baseline JRS Severity Subscore at Week 6 for Treatment-Naïve Patients
Pre-Treated Patients
The efficacy and safety of XEOMIN for the treatment of blepharospasm patients pre-treated with onabotulinumtoxinA (Botox) were evaluated in Study 2, a randomized, double-blind, placebo-controlled, multi-center trial in a total of 109 patients. Patients had a clinical diagnosis of benign essential blepharospasm, with baseline JRS Severity subscore ≥2, and a stable satisfactory therapeutic response to previous administrations of onabotulinumtoxinA (Botox). At least 10 weeks had to have elapsed since the most recent onabotulinumtoxinA administration. Patients with any significant neuromuscular disease that might interfere with the study were excluded from enrollment. Patients were randomized (2:1) to receive a single administration of XEOMIN (n=75) or placebo (n=34). Each patient in the XEOMIN group received a XEOMIN treatment (dose, volume, dilution, and injection sites per muscle) that was similar to the most recent onabotulinumtoxinA injection sessions prior to study entry. The highest dose permitted in this study was 100 Units (50 Units per eye); the mean XEOMIN dose was 33 Units per eye.
In Table 15 the most frequently injected sites, the median dose per injection site, and the median number (and range) of injection sites per eye are presented.
Table 15: Median Dose and Median Number of Injection Sites per Eye (Blepharospasm) Injection Area Median Units XEOMIN Median Number of Injection Sites
(Min-Max)Temporal Area 13 2 (1 – 6) Eyebrow Area 5 1 (1 – 4) Upper Lid Area 10 2 (1 – 4) Lower Lid Area 8 2 (1 – 3) Orbital Rim 5 1 (1 – 3) Patients were assessed during clinic visits at Weeks 3 and 6, and then by telephone or at clinic visits every two weeks up to Week 20.
The mean age of the study patients was 62 years, and 65% of the patients were women. The study was completed by 94% of study patients. Approximately one third of patients had other dystonic phenomena; in all but 1% this was limited to facial, cervical, perioral and mandibular muscles. No patients discontinued the study prematurely due to adverse events.
The primary efficacy endpoint was the change in the JRS Severity subscore from baseline to Week 6 post-injection, in the intent-to-treat (ITT) population, with missing values replaced by the patient's most recent value (i.e., last observation carried forward). In the ITT population, the difference between the XEOMIN group and the placebo group in the change of the JRS Severity subscore from baseline to Week 6 was -1.0 (95% CI -1.4; -0.5) points. Comparison of the XEOMIN group to the placebo group was statistically significant at p<0.001.
Figure 8: Frequency Distribution of Changes from Baseline JRS Severity Subscore at Week 6
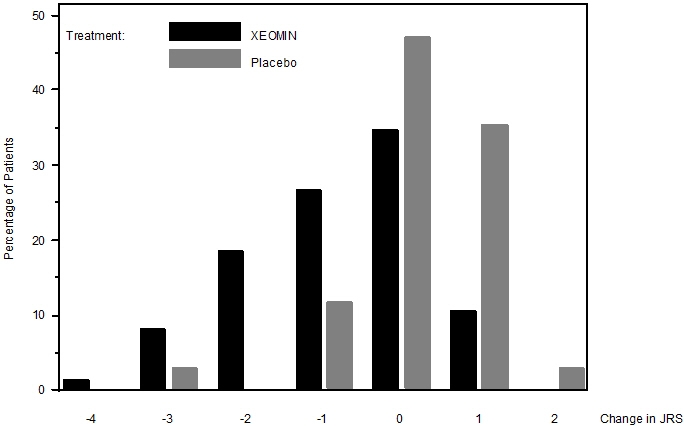
Examination of age and gender subgroups did not identify substantial differences in response to XEOMIN among these subgroups. There were too few non-white patients enrolled to adequately assess efficacy in other racial populations.
14.5 Glabellar Lines
Two identically designed randomized, double-blind, multi-center, placebo controlled clinical trials (Studies GL-1 and GL-2) were conducted to evaluate XEOMIN for use in the temporary improvement of moderate to severe glabellar lines. The studies enrolled 547 healthy patients (≥18 years old) with glabellar lines of at least moderate severity at maximum frown. Three hundred sixty six subjects were treated with 20 Units of XEOMIN and 181 subjects were treated with placebo. Subjects were excluded if they had marked ptosis, deep dermal scarring, or an inability to lessen glabellar lines, even by physically spreading them apart. The mean age of study subjects was 46 years. The majority of patients were female (86% and 93% in Studies GL-1 and GL-2, respectively), and predominantly Caucasian (89% and 65% respectively). The study subjects received either 20 Units of XEOMIN or an equal amount of placebo. The total dose was delivered in 5 equally divided intramuscular injections of 4 Units each to specific sites (see Figure 4). Subjects were followed up for 120 days.
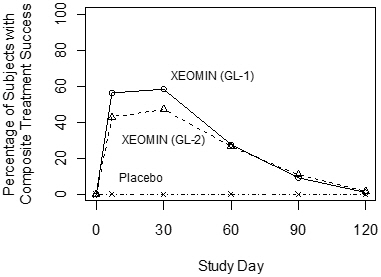
Investigators and subjects assessed efficacy at maximum frown on Day 30 of treatment using a 4-point scale (0=none, 1=mild, 2=moderate, 3=severe). Composite treatment success was defined as a 2-grade improvement on this scale compared to baseline for both the investigator's and subject's assessments on Day 30. The percentage of subjects with treatment success was greater on the XEOMIN arm than the placebo arm at Day 30 in both studies (see Table 16). The percentage of subjects with composite treatment success at each visit are presented in Figure 9.
Table 16: Treatment Success at Day 30 (at Least 2 Grades Improvement from Baseline at Maximum Frown) GL-1 GL-2 XEOMIN
(N=184)Placebo
(N=92)XEOMIN
(N=182)Placebo
(N=89)- * Success on both the Investigator and Subject Assessments
Composite Treatment Success* 111 (60%) 0 (0%) 87 (48%) 0 (0%) Investigator Assessment 141 (77%) 0 (0%) 129 (71%) 0 (0%) Subject Assessment 120 (65%) 0 (0%) 101 (55%) 1 (1%) Figure 9: Percentage of Subjects with Composite Treatment Success by Visit – Observed Cases (GL-1 and GL-2)
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
XEOMIN (incobotulinumtoxinA) for injection is a sterile white to off-white lyophilized powder supplied in Type 1 borosilicate glass single-dose vials with tamper-proof aluminum seals and bromobutyl rubber closures that are not made with natural rubber latex in the following pack sizes:
Upper Limb Spasticity and Cervical Dystonia
Package XEOMIN 50 Units XEOMIN 100 Units XEOMIN 200 Units Carton with one single-dose vial NDC: 0259-1605-01 NDC: 0259-1610-01 NDC: 0259-1620-01 Chronic Sialorrhea and Blepharospasm
Package XEOMIN 50 Units XEOMIN 100 Units Carton with one single-dose vial NDC: 0259-1605-01 NDC: 0259-1610-01 Glabellar Lines
Package XEOMIN 50 Units XEOMIN 100 Units Carton with one single-dose vial NDC: 46783-161-01 NDC: 46783-160-01 16.2 Storage and Handling
Unopened vials of XEOMIN should be stored at or below 25°C (77°F). Refrigeration of unopened vials is not required. Do not use after the expiration date on the vial. Reconstituted XEOMIN may be stored in a refrigerator at 2°C to 8°C (36°F to 46°F) for up to 24 hours until time of use [see Dosage and Administration (2.7)].
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Swallowing, Speaking, or Breathing Difficulties or Other Unusual Symptoms
Advise patients to inform their healthcare provider if they develop any unusual symptoms, including difficulty with swallowing, speaking, or breathing, or if any existing symptom worsens [see Boxed Warning and Warnings and Precautions (5.1, 5.4)]. Inform patients of the risk of aspiration.
Ability to Operate Machinery or Vehicles
Counsel patients that if loss of strength, muscle weakness, blurred vision, or drooping eyelids occur, they should avoid driving a car or engaging in other potentially hazardous activities.
Corneal Exposure, Corneal Ulceration, and Ectropion in Patients Treated for Blepharospasm
Inform patients that injections of XEOMIN may cause reduced blinking or effectiveness of blinking, and that they should seek immediate medical attention if eye pain or irritation occurs following treatment [see Warnings and Precautions (5.5)].
-
SPL UNCLASSIFIED SECTION
Manufactured by:
Merz Pharmaceuticals GmbH
Eckenheimer Landstrasse 100
Frankfurt Germany
U.S. License Number 1830Distributed by:
Merz Pharmaceuticals, LLC
6501 Six Forks Road
Raleigh, NC 27615and
Merz North America, Inc.
4133 Courtney Street, Suite 10
Franksville, WI 53126© 2019 Merz Pharmaceuticals, LLC
XEOMIN® is a registered trademark of Merz Pharma GmbH & Co KGaA.
All trademarks are the property of their respective owners.
Patent www.merzusa.com/patents/EM00451-05
-
MEDICATION GUIDE
This Medication Guide has been approved by the U. S. Food and Drug Administration. Revised: 5/2019 MEDICATION GUIDE
XEOMIN® (Zeo-min)
(incobotulinumtoxinA) for injection, for intramuscular or intraglandular useWhat is the most important information I should know about XEOMIN?
XEOMIN may cause serious side effects that can be life-threatening. Call your doctor or get medical help right away if you have any of these problems after treatment with XEOMIN:-
Problems with swallowing, speaking, or breathing. These problems can happen hours to weeks after an injection of XEOMIN if the muscles that you use to breathe and swallow become weak after the injection. Death can happen as a complication if you have severe problems with swallowing or breathing after treatment with XEOMIN.
- People with certain breathing problems may need to use muscles in their neck to help them breathe. These people may be at greater risk for serious breathing problems with XEOMIN.
- Swallowing problems may last for several months. People who cannot swallow well may need a feeding tube to receive food and water. If swallowing problems are severe, food or liquids may go into your lungs. People who already have swallowing or breathing problems before receiving XEOMIN have the highest risk of getting these problems.
- Spread of toxin effects. In some cases, the effect of botulinum toxin may affect areas of the body away from the injection site and cause symptoms of a serious condition called botulism. The symptoms of botulism include:
- loss of strength and muscle weakness all over the body
- double vision
- blurred vision and drooping eyelids
- hoarseness or change or loss of voice
- trouble saying words clearly
- loss of bladder control
- trouble breathing
- trouble swallowing
These symptoms can happen hours to weeks after you receive an injection of XEOMIN..
These problems could make it unsafe for you to drive a car or do other dangerous activities. See "What should I avoid while receiving XEOMIN?"What is XEOMIN?
XEOMIN is a prescription medicine used in adults:- that is injected into glands that make saliva and is used to treat long-lasting (chronic) drooling (sialorrhea).
- that is injected into muscles and used to:
- treat increased muscle stiffness in the arm because of upper limb spasticity.
- treat the abnormal head position and neck pain with cervical dystonia (CD).
- treat abnormal spasm of the eyelids (blepharospasm).
- improve the look of moderate to severe frown lines between the eyebrows (glabellar lines) for a short period of time (temporary).
Do not take XEOMIN if you: - are allergic to XEOMIN or any of the ingredients in XEOMIN. See the end of this Medication Guide for a list of ingredients in XEOMIN.
- had an allergic reaction to any other botulinum toxin products such as rimabotulinumtoxinB (MYOBLOC), onabotulinumtoxinA (BOTOX, BOTOX COSMETIC), or abobotulinumtoxinA (DYSPORT).
- have a skin infection at the planned injection site.
Before receiving XEOMIN, tell your doctor about all of your medical conditions, including if you: - have a disease that affects your muscles and nerves (such as amyotrophic lateral sclerosis [ALS or Lou Gehrig's disease], myasthenia gravis or Lambert-Eaton syndrome). See "What is the most important information I should know about XEOMIN?"
- have had any side effect from any other botulinum toxin in the past.
- have a breathing problem, such as asthma or emphysema.
- have a history of swallowing problems or inhaling food or fluid into your lungs (aspiration).
- have bleeding problems.
- have drooping eyelids.
- plan to have surgery.
- have had surgery on your face.
- are pregnant or plan to become pregnant. It is not known if XEOMIN can harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if XEOMIN passes into your breast milk.
Using XEOMIN with certain other medicines may cause serious side effects. Do not start any new medicines until you have told your doctor that you have received XEOMIN in the past. Especially tell your doctor if you:- have received any other botulinum toxin product in the last four months.
- have received injections of botulinum toxin such as rimabotulinumtoxinB (MYOBLOC), onabotulinumtoxinA (BOTOX, BOTOX COSMETIC) or abobotulinumtoxinA (DYSPORT) in the past. Be sure your doctor knows exactly which product you received. The dose of XEOMIN may be different from other botulinum toxin products that you have received.
- have recently received an antibiotic by injection or inhalation.
- take muscle relaxants.
- take an allergy or cold medicine.
- take a sleep medicine.
Know the medicines you take. Keep a list of your medicines with you to show your doctor and pharmacist each time you get a new medicine.How will I receive XEOMIN? - XEOMIN is a shot (injection) that your doctor will give you.
- XEOMIN is injected into your affected muscles or glands.
- Your doctor may change your dose of XEOMIN during treatment.
What should I avoid while taking XEOMIN?
XEOMIN may cause loss of strength or general muscle weakness, blurred vision, or drooping eyelids within hours to weeks of taking XEOMIN. If this happens, do not drive a car, operate machinery, or do other dangerous activities. See "What is the most important information I should know about XEOMIN? "What are the possible side effects of XEOMIN?
XEOMIN may cause serious side effects, including:
See "What is the most important information I should know about XEOMIN?"- Injury to the cornea (the clear front surface of the eye) in people treated for blepharospasm. People who receive XEOMIN to treat spasm of the eyelid may have reduced blinking that can cause a sore on their cornea or other problems of the cornea. Call your healthcare provider or get medical care right away if you have eye pain or irritation after treatment with XEOMIN.
- XEOMIN may cause other serious side effects including allergic reactions. Symptoms of an allergic reaction to XEOMIN may include: itching, rash, redness, swelling, wheezing, trouble breathing, or dizziness or feeling faint. Tell your doctor or get medical help right away if you get wheezing or trouble breathing, or if you get dizzy or faint.
- needing to have a tooth pulled (extracted)
- dry mouth
- diarrhea
- high blood pressure
The most common side effects of XEOMIN in people with upper limb spasticity include: - seizure
- nasal congestion, sore throat and runny nose
- dry mouth
- upper respiratory infection
The most common side effects of XEOMIN in people with cervical dystonia include: - difficulty swallowing
- neck pain
- muscle weakness
- pain at the injection site
- muscle and bone pain
The most common side effects of XEOMIN in people with blepharospasm include: - drooping of the eyelid
- dry eye
- vision problems
- dry mouth
The most common side effect of XEOMIN in people with glabellar lines include: - headache
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.General information about the safe and effective use of XEOMIN.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. You can ask your pharmacist or doctor for information about XEOMIN that is written for health professionals.What are the ingredients in XEOMIN?
Active ingredient: botulinum toxin type A
Inactive ingredients: human albumin and sucrose
Manufactured by: Merz Pharmaceuticals GmbH, Eckenheimer Landstrasse 100, Frankfurt Germany U.S. License Number 1830
Distributed by: Merz Pharmaceuticals, LLC, 6501 Six Forks Road, Raleigh, NC 27615 and Merz North America, Inc. 4133 Courtney Street, Suite 10, Franksville, WI 53126
© 2019 Merz Pharmaceuticals, LLC, XEOMIN® is a registered trademark of Merz Pharma GmbH & Co KGaA.
All trademarks are the property of their respective owners.
Patent www.merzusa.com/patents/
EM00674-04 -
Problems with swallowing, speaking, or breathing. These problems can happen hours to weeks after an injection of XEOMIN if the muscles that you use to breathe and swallow become weak after the injection. Death can happen as a complication if you have severe problems with swallowing or breathing after treatment with XEOMIN.
-
PRINCIPAL DISPLAY PANEL - 50 Unit Vial Carton
1 vial
Rx Only
NDC: 46783-161-01incobotulinumtoxinA
XEOMIN®
FOR INJECTIONFor Intramuscular Use
Dispense the enclosed Medication
Guide to each patient.
One single-dose vial per carton.
Discard Unused Portion.50 units/vial
WARNING: Dosing units of botulinum
toxins are not interchangeable between
commercial products.MERZ AESTHETICS®
-
PRINCIPAL DISPLAY PANEL - 100 Unit Vial Carton
1 vial
Rx Only
NDC: 46783-160-10incobotulinumtoxinA
XEOMIN®
FOR INJECTIONFor Intramuscular Use
Dispense the enclosed Medication
Guide to each patient.
One single-dose vial per carton.
Discard Unused Portion.100 units/vial
WARNING: Dosing units of botulinum
toxins are not interchangeable between
commercial products.MERZ AESTHETICS®

-
PRINCIPAL DISPLAY PANEL - 50 Unit Vial Carton - NDC: 46783-165-01
1 vial
Rx Only
NDC: 46783-165-01incobotulinumtoxinA
XEOMIN®
FOR INJECTIONFor Intramuscular Use
Dispense the enclosed Medication
Guide to each patient.
One single-dose vial per carton.
Discard Unused Portion.50 units/vial
WARNING: Dosing units of botulinum
toxins are not interchangeable between
commercial products.MERZ AESTHETICS®
-
INGREDIENTS AND APPEARANCE
XEOMIN
incobotulinumtoxina injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 46783-161 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Botulinum Toxin Type A (UNII: E211KPY694) (Botulinum Toxin Type A - UNII:E211KPY694) Botulinum Toxin Type A 50 [USP'U] Inactive Ingredients Ingredient Name Strength Albumin Human (UNII: ZIF514RVZR) Sucrose (UNII: C151H8M554) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 46783-161-01 1 in 1 CARTON 08/01/2011 1 1 in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125360 08/01/2011 XEOMIN
incobotulinumtoxina injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 46783-160 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Botulinum Toxin Type A (UNII: E211KPY694) (Botulinum Toxin Type A - UNII:E211KPY694) Botulinum Toxin Type A 100 [USP'U] Inactive Ingredients Ingredient Name Strength Albumin Human (UNII: ZIF514RVZR) Sucrose (UNII: C151H8M554) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 46783-160-01 1 in 1 CARTON 08/01/2011 1 1 in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product 2 NDC: 46783-160-10 1 in 1 CARTON 08/01/2011 2 1 in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125360 08/01/2011 XEOMIN
incobotulinumtoxina injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 46783-165 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Botulinum Toxin Type A (UNII: E211KPY694) (Botulinum Toxin Type A - UNII:E211KPY694) Botulinum Toxin Type A 50 [USP'U] Inactive Ingredients Ingredient Name Strength Albumin Human (UNII: ZIF514RVZR) Sucrose (UNII: C151H8M554) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 46783-165-01 1 in 1 CARTON 08/01/2011 1 1 in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125360 08/01/2011 Labeler - Merz North America, Inc. (028147846) Establishment Name Address ID/FEI Business Operations Merz Pharma GmbH & Co. KGaA 342543051 MANUFACTURE(46783-160, 46783-161, 46783-165)
Trademark Results [Xeomin]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 XEOMIN 79371939 not registered Live/Pending |
Merz Pharma GmbH & Co. KGaA 2023-02-22 |
 XEOMIN 77910865 3898981 Live/Registered |
MERZ PHARMA GmbH & Co. KGaA 2010-01-13 |
 XEOMIN 76533879 2918539 Dead/Cancelled |
Merz Pharma GmbH & Co. KGaA 2003-08-01 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.