LURASIDONE HYDROCHLORIDE tablet, film coated
Lurasidone Hydrochloride by
Drug Labeling and Warnings
Lurasidone Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by Exelan Pharmaceuticals Inc., InvaGen Pharmaceuticals, Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LURASIDONE HYDROCHLORIDE safely and effectively. See full prescribing information for LURASIDONE HYDROCHLORIDE.
LURASIDONE HYDROCHLORIDE tablets, for oral use
Initial U.S. Approval: 2010WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS; and SUICIDAL THOUGHTS AND BEHAVIORS
See full prescribing information for complete boxed warning.
- Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Lurasidone hydrochloride is not approved for the treatment of patients with dementia-related psychosis (5.1).
- Antidepressants increased the risk of suicidal thoughts and behavior in pediatric and young adult patients. Closely monitor for clinical worsening and emergence of suicidal thoughts and behaviors. (5.2).
RECENT MAJOR CHANGES
Warnings and Precautions (5.7)) 1/2025
INDICATIONS AND USAGE
Lurasidone hydrochloride is an atypical antipsychotic indicated for the treatment of:
- Schizophrenia in adults and adolescents (13 to 17 years) (1, 14.1)
- Depressive episode associated with Bipolar I Disorder (bipolar depression) in adults and pediatric patients (10-17 years) as monotherapy (1, 14.2)
- Depressive episode associated with Bipolar I Disorder (bipolar depression) in adults as adjunctive therapy with lithium or valproate (1, 14.2)
DOSAGE AND ADMINISTRATION
Lurasidone hydrochloride should be taken with food (at least 350 calories). Administration with food substantially increases the absorption of lurasidone hydrochloride (2.3, 12.3).
Indication Starting Dose Recommended Dose Schizophrenia - adults (2.1) 40 mg per day 40 mg to 160 mg per day Schizophrenia - adolescents (13 to 17 years) (2.1) 40 mg per day 40 mg to 80 mg per day Bipolar Depression - adults (2.2) 20 mg per day 20 mg to 120 mg per day Bipolar Depression - pediatric patients (10 to 17 years) (2.2) 20 mg per day 20 mg to 80 mg per day - Moderate and Severe Renal Impairment: Recommended starting dose is 20 mg per day, and the maximum recommended dose is 80 mg per day (2.4, 8.6).
- Moderate and Severe Hepatic Impairment: Recommended starting dose is 20 mg per day. The maximum recommended dose is 80 mg per day in moderate hepatic impairment and 40 mg per dayin severe hepatic impairment (2.5, 8.7).
- Concomitant Use of a Moderate CYP3A4 inhibitor (e.g., diltiazem):
Lurasidone hydrochloride dose should be reduced to half of the original dose level. Recommended starting dose is 20 mg per day. Maximum recommended dose is 80 mg per day (2.6, 7.1).
- Concomitant Use of a Moderate CYP3A4 Inducer:
It may be necessary to increase the dose of Lurasidone hydrochloride (2.6, 7.1).
DOSAGE FORMS AND STRENGTHS
Tablets: 20 mg, 40 mg, 60 mg, 80 mg and 120 mg (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Cerebrovascular Adverse Reactions in Elderly Patients with Dementia-Related Psychosis: Increased incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack) (5.3).
- Neuroleptic Malignant Syndrome: Manage with immediate discontinuation and close monitoring (5.4).
- Tardive Dyskinesia: Discontinue if clinically appropriate (5.5).
- Metabolic Changes: Monitor for hyperglycemia/diabetes mellitus, dyslipidemia and weight gain (5.6).
- Hyperprolactinemia: Prolactin elevations may occur (5.7).
- Leukopenia, Neutropenia, and Agranulocytosis: Perform complete blood counts (CBC) in patients with a pre-existing low white blood cell count (WBC) or a history of leukopenia or neutropenia. Consider discontinuing lurasidone hydrochloride if a clinically significant decline in WBC occurs in the absence of other causative factors (5.8).
- Orthostatic Hypotension and Syncope: Monitor heart rate and blood pressure and warn patients with known cardiovascular or cerebrovascular disease, and risk of dehydration or syncope (5.9).
ADVERSE REACTIONS
Commonly observed adverse reactions (incidence ≥ 5% and at least twice the rate for placebo) were (6.1):
- Adult patients with schizophrenia: somnolence, akathisia, extrapyramidal symptoms, and nausea
- Adolescent patients (13-17 years) with schizophrenia: somnolence, nausea, akathisia, EPS (non-akathisia), rhinitis (80 mg only), and vomiting
- Adult patients with bipolar depression: akathisia, extrapyramidal symptoms, and somnolence
- Pediatric patients (10-17 years) with bipolar depression: nausea, weight increase, and insomnia
To report SUSPECTED ADVERSE REACTIONS, contact Exelan Pharmaceuticals, Inc. at 1-866-604-3268 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
Pregnancy: May cause extrapyramidal and or/withdrawal symptoms in neonates with third trimester exposure (8.1).
See 17 for Medication Guide.
Revised: 3/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Schizophrenia
2.2 Depressive Episodes Associated with Bipolar I Disorder
2.3 Administration Information
2.4 Dose Modifications for Renal Impairment
2.5 Dose Modifications for Hepatic Impairment
2.6 Dose Modifications Due to Drug Interactions of CYP3A4 Inhibitors and CYP3A4 Inducers
3. DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5. WARNINGS AND PRECAUTIONS
5.1 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
5.2 Suicidal Thoughts and Behaviors in Pediatric and Young Adult Patients
5.3 Cerebrovascular Adverse Reactions, Including Stroke in Elderly Patients with Dementia Related Psychosis
5.4 Neuroleptic Malignant Syndrome
5.5 Tardive Dyskinesia
5.6 Metabolic Changes
5.7 Hyperprolactinemia
5.8 Leukopenia, Neutropenia and Agranulocytosis
5.9 Orthostatic Hypotension and Syncope
5.10 Falls
5.11 Seizures
5.12 Potential for Cognitive and Motor Impairment
5.13 Body Temperature Dysregulation
5.14 Activation of Mania/Hypomania
5.15 Dysphagia
5.16 Neurological Adverse Reactions in Patients with Parkinson’s Disease or Dementia with Lewy Bodies
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Drugs Having Clinically Important Interactions with lurasidone hydrochloride.
7.2 Drugs Having No Clinically Important Interactions with lurasidone hydrochloride
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Other Specific Populations
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
10 OVERDOSAGE
10.1 Human Experience
10.2 Management of Overdosage
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Schizophrenia
14.2 Depressive Episodes Associated with Bipolar I Disorder
16 HOW SUPPLIED/STORAGE AND HANDLING
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS; and SUICIDAL THOUGHTS AND BEHAVIORS
Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Lurasidone hydrochloride is not approved for the treatment of patients with dementia-related psychosis [see Warnings and Precautions (5.1)].
Suicidal Thoughts and Behaviors
Antidepressants increased the risk of suicidal thoughts and behavior in pediatric and young adults in short-term studies. Closely monitor all antidepressant-treated patients for clinical worsening, and for emergence of suicidal thoughts and behaviors [see Warnings and Precautions (5.2)].
-
1 INDICATIONS AND USAGE
Lurasidone hydrochloride tablets are indicated for:
- Treatment of adult and adolescent patients (13 to 17 years) with schizophrenia [see Clinical Studies (14.1)].
- Monotherapy treatment of adult and pediatric patients (10 to 17 years) with major depressive episode associated with bipolar I disorder (bipolar depression) [see Clinical Studies (14.2)].
- Adjunctive treatment with lithium or valproate in adult patients with major depressive episode associated with bipolar I disorder (bipolar depression) [see Clinical Studies (14.2)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Schizophrenia
Adults
The recommended starting dose of lurasidone hydrochloride is 40 mg once daily. Initial dose titration is not required. Lurasidone hydrochloride has been shown to be effective in a dose range of 40 mg per day to 160 mg per day [see Clinical Studies (14.1)]. The maximum recommended dose is 160 mg per day.
Adolescents (13 – 17 years)
The recommended starting dose of lurasidone hydrochloride is 40 mg once daily. Initial dose titration is not required. lurasidone hydrochloride has been shown to be effective in a dose range of 40 mg per day to 80 mg per day [see Clinical Studies (14.1)]. The maximum recommended dose is 80 mg per day.
2.2 Depressive Episodes Associated with Bipolar I Disorder
Adults
The recommended starting dose of lurasidone hydrochloride is 20 mg given once daily as monotherapy or as adjunctive therapy with lithium or valproate. Initial dose titration is not required. Lurasidone hydrochloride has been shown to be effective in a dose range of 20 mg per day to 120 mg per day as monotherapy or as adjunctive therapy with lithium or valproate [see Clinical Studies (14.2)]. The maximum recommended dose, as monotherapy or as adjunctive therapy with lithium or valproate, is 120 mg per day. In the monotherapy study, the higher dose range (80 mg to 120 mg per day) did not provide additional efficacy, on average, compared to the lower dose range (20 to 60 mg per day) [see Clinical Studies (14.2)].
Pediatric Patients (10 – 17 years)
The recommended starting dose of lurasidone hydrochloride is 20 mg given once daily as monotherapy. Initial dose titration is not required. The dose may be increased after one week based on clinical response. Lurasidone hydrochloride has been shown to be effective in a dose range of 20 mg per day to 80 mg per day as monotherapy. At the end of the clinical study, most of the patients (67%) received 20 mg or 40 mg once daily [see Clinical Studies (14.2)]. The maximum recommended dose is 80 mg per day. The efficacy of lurasidone hydrochloride in the treatment of mania associated with bipolar disorder has not been established.
2.3 Administration Information
Lurasidone hydrochloride should be taken with food (at least 350 calories). Administration with food substantially increases the absorption of lurasidone hydrochloride. Administration with food increases the AUC approximately 2-fold and increases the Cmax approximately 3-fold. In the clinical studies, lurasidone hydrochloride was administered with food [see Clinical Pharmacology (12.3)].
The effectiveness of lurasidone hydrochloride for longer-term use, that is, for more than 6 weeks, has not been established in controlled studies. Therefore, the physician who elects to use lurasidone hydrochloride for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient [see Dosage and Administration (2.1 and 2.2)].
2.4 Dose Modifications for Renal Impairment
Dose adjustment is recommended in moderate (creatinine clearance: 30 to <50 mL/min) and severe renal impairment (creatinine clearance <30 mL/min) patients. The recommended starting dose is 20 mg per day. The dose in these patients should not exceed 80 mg per day [see Use in Specific Populations (8.6)].
2.5 Dose Modifications for Hepatic Impairment
Dose adjustment is recommended in moderate (Child-Pugh Score = 7 to 9) and severe hepatic impairment (Child-Pugh Score = 10 to 15) patients. The recommended starting dose is 20 mg per day. The dose in moderate hepatic impairment patients should not exceed 80 mg per day and the dose in severe hepatic impairment patients should not exceed 40 per mg/day [see Use in Specific Populations (8.7)].
2.6 Dose Modifications Due to Drug Interactions of CYP3A4 Inhibitors and CYP3A4 Inducers
Concomitant Use with CYP3A4 Inhibitors
Lurasidone hydrochloride should not be used concomitantly with a strong CYP3A4 inhibitor (e.g., ketoconazole, clarithromycin, ritonavir, voriconazole, mibefradil, etc.) [see Contraindications (4)].
If lurasidone hydrochloride is being prescribed and a moderate CYP3A4 inhibitor (e.g. diltiazem, atazanavir, erythromycin, fluconazole, verapamil etc.) is added to the therapy, the lurasidone hydrochloride dose should be reduced to half of the original dose level. Similarly, if a moderate CYP3A4 inhibitor is being prescribed and lurasidone hydrochloride is added to the therapy, the recommended starting dose of lurasidone hydrochloride is 20 mg per day, and the maximum recommended dose of lurasidone hydrochloride is 80 mg per day [see Contraindications (4), Drug Interactions (7.1)].
Grapefruit and grapefruit juice should be avoided in patients taking lurasidone hydrochloride, since these may inhibit CYP3A4 and alter lurasidone hydrochloride concentrations [see Drug Interactions (7.1)].
Concomitant Use with CYP3A4 Inducers
Lurasidone hydrochloride should not be used concomitantly with a strong CYP3A4 inducer (e.g., rifampin, avasimibe, St. John’s wort, phenytoin, carbamazepine, etc.) [see Contraindications (4); Drug Interactions (7.1)]. If lurasidone hydrochloride is used concomitantly with a moderate CYP3A4 inducer, it may be necessary to increase the lurasidone hydrochloride dose after chronic treatment (7 days or more) with the CYP3A4 inducer.
-
3. DOSAGE FORMS AND STRENGTHS
Lurasidone hydrochloride tablets are available in the following shape and color (Table 1) with respective one-sided debossing.
Table 1: Lurasidone hydrochloride Tablet Presentations
Tablet Strength Tablet Color/Shape Tablet Markings 20 mg White to off-white round biconvex IG/ 522 40 mg White to off-white round biconvex IG/ 523 60 mg White to off-white oval biconvex IG/ 534 80 mg Pale green oval biconvex IG/ 524 120 mg White to off-white capsule shaped biconvex IG/ 525 -
4 CONTRAINDICATIONS
- Known hypersensitivity to lurasidone HCl or any components in the formulation. Angioedema has been observed with lurasidone [see Adverse Reactions (6.1)].
- Strong CYP3A4 inhibitors (e.g., ketoconazole, clarithromycin, ritonavir, voriconazole, mibefradil, etc.) [see Drug Interactions (7.1)].
- Strong CYP3A4 inducers (e.g., rifampin, avasimibe, St. John’s wort, phenytoin, carbamazepine, etc.) [see Drug Interactions (7.1)].
-
5. WARNINGS AND PRECAUTIONS
5.1 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of 17 placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6- to 1.7-times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Lurasidone hydrochloride is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning, Warnings and Precautions (5.3)].
5.2 Suicidal Thoughts and Behaviors in Pediatric and Young Adult Patients
In pooled analyses of placebo-controlled trials of antidepressant drugs (SSRIs and other antidepressant classes) that included approximately 77,000 adult patients, and over 4,400 pediatric patients, the incidence of suicidal thoughts and behaviors in pediatric and young adult patients was greater in antidepressant-treated patients than in placebo-treated patients. The drug-placebo differences in the number of cases of suicidal thoughts and behaviors per 1000 patients treated are provided in Table 2.
No suicides occurred in any of the pediatric studies. There were suicides in the adult studies, but the number was not sufficient to reach any conclusion about antidepressant drug effect on suicide
Table 2: Risk Differences of the Number of Cases of Suicidal Thoughts or Behaviors in the Pooled Placebo-Controlled Trials of Antidepressants in Pediatric and Adult Patients
Age Range Drug-Placebo Difference in Number of Patients of Suicidal Thoughts
or Behaviors per 1000 Patients TreatedIncreases Compared to Placebo <18 14 additional patients 18-24 5 additional patients Decreases Compared to Placebo 25-64 1 fewer patient ≥65 6 fewer patients It is unknown whether the risk of suicidal thoughts and behaviors in pediatric and young adult patients extends to longer-term use, i.e., beyond four months. However, there is substantial evidence from placebo controlled maintenance studies in adults with MDD that antidepressants delay the recurrence of depression. Monitor all antidepressant-treated patients for clinical worsening and emergence of suicidal thoughts and behaviors, especially during the initial few months of drug therapy and at times of dosage changes. Counsel family members or caregivers of patients to monitor for changes in behavior and to alert the healthcare provider. Consider changing the therapeutic regimen, including possibly discontinuing lurasidone hydrochloride, in patients whose depression is persistently worse, or who are experiencing emergent suicidal thoughts or behaviors.
5.3 Cerebrovascular Adverse Reactions, Including Stroke in Elderly Patients with Dementia Related Psychosis
In placebo-controlled trials with risperidone, aripiprazole, and olanzapine in elderly subjects with dementia, there was a higher incidence of cerebrovascular adverse reactions (cerebrovascular accidents and transient ischemic attacks), including fatalities, compared to placebo-treated subjects. Lurasidone hydrochloride is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning, Warnings and Precautions (5.1)].
5.4 Neuroleptic Malignant Syndrome
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) has been reported in association with administration of antipsychotic drugs, including lurasidone hydrochloride. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status, and evidence of autonomic instability. Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure.
If NMS is suspected, immediately discontinue lurasidone hydrochloride and provide intensive symptomatic treatment and monitoring.
5.5 Tardive Dyskinesia
Tardive dyskinesia is a syndrome consisting of potentially irreversible, involuntary, dyskinetic movements that can develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely upon prevalence estimates to predict, at the inception of antipsychotic treatment, which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
The risk of developing tardive dyskinesia and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses or may even arise after discontinuation of treatment.
The syndrome may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment, itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and thereby may possibly mask the underlying process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, lurasidone hydrochloride should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that (1) is known to respond to antipsychotic drugs, and (2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on lurasidone hydrochloride, drug discontinuation should be considered. However, some patients may require treatment with lurasidone hydrochloride despite the presence of the syndrome.
5.6 Metabolic Changes
Atypical antipsychotic drugs have been associated with metabolic changes that may increase cardiovascular/cerebrovascular risk. These metabolic changes include hyperglycemia, dyslipidemia, and body weight gain. While all of the drugs in the class have been shown to produce some metabolic changes, each drug has its own specific risk profile.
Hyperglycemia and Diabetes Mellitus
Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported in patients treated with atypical antipsychotics. Assessment of the relationship between atypical antipsychotic use and glucose abnormalities is complicated by the possibility of an increased background risk of diabetes mellitus in patients with schizophrenia and the increasing incidence of diabetes mellitus in the general population. Given these confounders, the relationship between atypical antipsychotic use and hyperglycemia-related adverse events is not completely understood. However, epidemiological studies suggest an increased risk of hyperglycemia-related adverse events in patients treated with the atypical antipsychotics.
Patients with an established diagnosis of diabetes mellitus who are started on atypical antipsychotics should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (e.g., obesity, family history of diabetes) who are starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic was discontinued; however, some patients required continuation of anti-diabetic treatment despite discontinuation of the suspect drug.
Schizophrenia
Adults
Pooled data from short-term, placebo-controlled schizophrenia studies are presented in Table 3.
Table 3: Change in Fasting Glucose in Adult Schizophrenia Studies
Placebo Lurasidone hydrochloride 20 mg/day 40 mg/day 80 mg/day 120 mg/day 160 mg/day Mean Change from Baseline (mg/dL) n=680 n=71 n=478 n=508 n=283 n=113 Serum Glucose -0.0 -0.6 +2.6 -0.4 +2.5 + 2.5 Proportion of Patients with Shifts to ≥ 126 mg/dL Serum Glucose
(≥ 126 mg/dL)8.3%
(52/628)11.7%
(7/60)12.7%
( 57/449)6.8%
(32/472)10.0%
(26/260)5.6%
(6/108)In the uncontrolled, longer-term schizophrenia studies (primarily open-label extension studies), lurasidone hydrochloride was associated with a mean change in glucose of +1.8 mg/dL at week 24 (n=355), +0.8 mg/dL at week 36 (n=299) and +2.3 mg/dL at week 52 (n=307).
Adolescents
In studies of adolescents and adults with schizophrenia, changes in fasting glucose were similar. In the short-term, placebo-controlled study of adolescents, fasting serum glucose mean values were -1.3 mg/ dL for placebo (n=95), +0.1 mg/dL for 40 mg/day (n=90), and +1.8 mg/dL for 80 mg/day (n=92).
Bipolar Depression
Adults
Monotherapy
Data from the adult short-term, flexible-dose, placebo-controlled monotherapy bipolar depression study are presented in Table 4.
Table 4: Change in Fasting Glucose in the Adult Monotherapy Bipolar Depression Study
Patients were randomized to flexibly dosed Lurasidone 20 to 60 mg/day, Lurasidone 80 to 120 mg/day, or placebo
Placebo Lurasidone 20 to 60 mg/day 80 to 120 mg/day Mean Change from Baseline (mg/dL) n=148 n=140 n=143 Serum Glucose +1.8 -0.8 +1.8 Proportion of Patients with Shifts to ≥ 126 mg/dL Serum Glucose
(≥ 126 mg/dL)4.3%
(6/141)2.2%
(3/138)6.4%
(9/141)In the uncontrolled, open-label, longer-term bipolar depression study, patients who received lurasidone hydrochloride as monotherapy in the short-term study and continued in the longer-term study, had a mean change in glucose of +1.2 mg/dL at week 24 (n=129).
Adjunctive Therapy with Lithium or Valproate
Data from the adult short-term, flexible-dosed, placebo-controlled adjunctive therapy bipolar depression studies are presented in Table 5.
Table 5: Change in Fasting Glucose in the Adult Adjunctive Therapy Bipolar Depression Studies
Patients were randomized to flexibly dosed Lurasidone 20 to 120 mg/day or placebo as adjunctive therapy with lithium or valproate.
Placebo Lurasidone 20 to 120 mg/day Mean Change from Baseline (mg/dL) n=302 n=319 Serum Glucose -0.9 +1.2 Proportion of Patients with Shifts to ≥ 126 mg/dL Serum Glucose
(≥ 126 mg/dL)1.0%
(3/290)1.3%
(4/316)In the uncontrolled, open-label, longer-term bipolar depression study, patients who received lurasidone hydrochloride as adjunctive therapy with either lithium or valproate in the short-term study and continued in the longer-term study, had a mean change in glucose of +1.7 mg/dL at week 24 (n=88).
Pediatric Patients (10 to 17 years)
In studies of pediatric patients 10 to 17 years and adults with bipolar depression, changes in fasting glucose were similar. In the 6-week, placebo-controlled study of pediatric patients with bipolar depression, mean change in fasting glucose was +1.6 mg/dL for lurasidone hydrochloride 20 to 80 mg/ day (n=145) and -0.5 mg/dL for placebo (n=145).
Pediatric Patients (6 to 17 years)
In a 104-week, open-label study in pediatric patients with schizophrenia, bipolar depression, or autistic disorder, 7 % of patients with a normal baseline fasting glucose experienced a shift to high at endpoint while taking lurasidone.
Dyslipidemia
Undesirable alterations in lipids have been observed in patients treated with atypical antipsychotics.
Schizophrenia
Adults
Pooled data from short-term, placebo-controlled schizophrenia studies are presented in Table 6
Table 6: Change in Fasting Lipids in Adult Schizophrenia Studies
Placebo Lurasidone 20 mg/day 40 mg/day 80 mg/day 120 mg/day 160 mg/day Mean Change from Baseline (mg/dL) n=660 n=71 n=466 n=499 n=268 n=115 Total Cholesterol -5.8 -12.3 -5.7 -6.2 -3.8 -6.9 Triglycerides -13.4 -29.1 -5.1 -13.0 -3.1 -10.6 Proportion of Patients with Shifts Total Cholesterol (≥ 240 mg/dL) 5.3%
(30/571)13.8%
(8/58)6.2%
(25/402)5.3%
(23/434)3.8%
(9/238)4.0%
(4/101)Triglycerides
(≥ 200 mg/dL)10.1%
(53/526)14.3%
(7/49)10.8%
(41/379)6.3%
(25/400)10.5%
(22/209)7.0%
(7/100)In the uncontrolled, longer-term schizophrenia studies (primarily open-label extension studies), lurasidone hydrochloride was associated with a mean change in total cholesterol and triglycerides of -3.8 (n=356) and -15.1 (n=357) mg/dL at week 24, -3.1 (n=303) and -4.8 (n=303) mg/dL at week 36 and -2.5 (n=307) and -6.9 (n=307) mg/dL at week 52, respectively.
Adolescents
In the adolescent short-term, placebo-controlled study, fasting serum cholesterol mean values were -9.6 mg/dL for placebo (n=95), -4.4 mg/dL for 40 mg/day (n=89), and +1.6 mg/dL for 80 mg/day (n=92), and fasting serum triglyceride mean values were +0.1 mg/dL for placebo (n=95), -0.6 mg/dL for 40 mg/day (n=89), and +8.5 mg/dL for 80 mg/day (n=92).
Bipolar Depression
Adults
Monotherapy
Data from the adult short-term, flexible-dosed, placebo-controlled, monotherapy bipolar depression study are presented in Table 7.
Table 7: Change in Fasting Lipids in the Adult Monotherapy Bipolar Depression Study
Patients were randomized to flexibly dosed Lurasidone 20 to 60 mg/day, Lurasidone 80 to 120 mg/day, or placebo
Placebo Lurasidone 20 to 60 mg/day 80 to 120 mg/day Mean Change from Baseline (mg/dL) n=147 n=140 n=144 Total cholesterol -3.2 +1.2 -4.6 Triglycerides +6.0 +5.6 +0.4 Proportion of Patients with Shifts Total cholesterol (≥ 240 mg/dL) 4.2%
(5/118)4.4%
(5/113)4.4%
(5/114)Triglycerides
(≥ 200 mg/dL)4.8%
(6/126)10.1%
(12/119)9.8%
(12/122)In the uncontrolled, open-label, longer-term bipolar depression study, patients who received lurasidone hydrochloride as monotherapy in the short-term and continued in the longer-term study had a mean change in total cholesterol and triglycerides of -0.5 mg/dL (n=130) and -1.0 mg/dL (n=130) at week 24, respectively.
Adjunctive Therapy with Lithium or Valproate
Data from the adult short-term, flexible-dosed, placebo-controlled, adjunctive therapy bipolar depression studies are presented in Table 8.
Table 8: Change in Fasting Lipids in the Adult Adjunctive Therapy Bipolar Depression Studies
Patients were randomized to flexibly dosed Lurasidone 20 to 120 mg/day or placebo as adjunctive therapy with lithium or valproate.
Placebo Lurasidone 20 to 120 mg/day Mean Change from Baseline (mg/dL) n=303 n=321 Total cholesterol -2.9 -3.1 Triglycerides -4.6 +4.6 Proportion of Patients with Shifts Total cholesterol
(≥ 240 mg/dL)5.7%
(15/263)5.4%
(15/276)Triglycerides
(≥ 200 mg/dL)8.6%
(21/243)10.8%
(28/260)In the uncontrolled, open-label, longer-term bipolar depression study, patients who received lurasidone hydrochloride, as adjunctive therapy with either lithium or valproate in the short-term study and continued in the longer-term study, had a mean change in total cholesterol and triglycerides of -0.9 (n=88) and +5.3 (n=88) mg/dL at week 24, respectively.
Pediatric Patients (10 to 17 years)
In the 6-week, placebo-controlled bipolar depression study with pediatric patients 10 to 17 years, mean change in fasting cholesterol was -6.3 mg/dL for lurasidone 20 to 80 mg/day (n=144) and -1.4 mg/dL for placebo (n=145), and mean change in fasting triglyceride was -7.6 mg/dL for lurasidone 20 to 80 mg/day (n=144) and +5.9 mg/dL for placebo (n=145).
Pediatric Patients (6 to 17 years)
In a 104-week, open-label study of pediatric patients with schizophrenia, bipolar depression, or autistic disorder, shifts in baseline fasting cholesterol from normal to high at endpoint were reported in 12% (total cholesterol), 3% (LDL cholesterol), and shifts in baseline from normal to low were reported in 27% (HDL cholesterol) of patients taking lurasidone. Of patients with normal baseline fasting triglycerides, 12% experienced shifts to high.
Weight Gain
Weight gain has been observed with atypical antipsychotic use. Clinical monitoring of weight is recommended.
Schizophrenia
Adults
Pooled data from short-term, placebo-controlled schizophrenia studies are presented in Table 9. The mean weight gain was +0.43 kg for lurasidone hydrochloride -treated patients compared to -0.02 kg for placebo-treated patients. Change in weight from baseline for olanzapine was +4.15 kg and for quetiapine extended-release was +2.09 kg in Studies 3 and 5 [see Clinical Studies (14.1)], respectively. The proportion of patients with a ≥ 7% increase in body weight (at Endpoint) was 4.8% for lurasidone hydrochloride -treated patients and 3.3% for placebo-treated patients.
Table 9: Mean Change in Weight (kg) from Baseline in Adult Schizophrenia Studies
Lurasidone Placebo
(n=696)20 mg/day
(n=71)40 mg/day
(n=484)80 mg/day
(n=526)120 mg/day
(n=291)160 mg/day
(n=114)All Patients -0.02 -0.15 +0.22 +0.54 +0.68 +0.60 In the uncontrolled, longer-term schizophrenia studies (primarily open-label extension studies), lurasidone hydrochloride was associated with a mean change in weight of -0.69 kg at week 24 (n=755), -0.59 kg at week 36 (n=443) and -0.73 kg at week 52 (n=377).
Adolescents
Data from the short-term, placebo-controlled adolescent schizophrenia study are presented in Table 10. The mean change in weight gain was +0.5 kg for lurasidone hydrochloride -treated patients compared to +0.2 kg for placebo-treated patients. The proportion of patients with a ≥7% increase in body weight (at Endpoint) was 3.3% for lurasidone hydrochloride -treated patients and 4.5% for placebo-treated patients.
Table 10: Mean Change in Weight (kg) from Baseline in the Adolescent Schizophrenia Study
Placebo
(n=111)Lurasidone 40 mg/day
(n=109)80 mg/day
(n=104)All Patients +0.2 +0.3 +0.7 Bipolar Depression
Adults
Monotherapy
Data from the adult short-term, flexible-dosed, placebo-controlled monotherapy bipolar depression study are presented in Table 11. The mean change in weight gain was +0.29 kg for lurasidone hydrochloride -treated patients compared to -0.04 kg for placebo-treated patients. The proportion of patients with a ≥ 7% increase in body weight (at Endpoint) was 2.4% for lurasidone hydrochloride -treated patients and 0.7% for placebo-treated patients.
Table 11: Mean Change in Weight (kg) from Baseline in the Adult Monotherapy Bipolar Depression Study
Patients were randomized to flexibly dosed Lurasidone 20 to 60 mg/day, Lurasidone 80 to 120 mg/day, or placebo
Placebo
(n=151)Lurasidone 20 to 60 mg/day
(n=143)80 to 120 mg/day
(n=147)All Patients -0.04 +0.56 +0.02 In the uncontrolled, open-label, longer-term bipolar depression study, patients who received lurasidone hydrochloride as monotherapy in the short-term and continued in the longer-term study had a mean change in weight of -0.02 kg at week 24 (n=130).
Adjunctive Therapy with Lithium or Valproate
Data from the adult short-term, flexible-dosed, placebo-controlled adjunctive therapy bipolar depression studies are presented in Table 12. The mean change in weight gain was +0.11 kg for lurasidone hydrochloride -treated patients compared to +0.16 kg for placebo-treated patients. The proportion of patients with a ≥ 7% increase in body weight (at Endpoint) was 3.1% for lurasidone hydrochloride -treated patients and 0.3% for placebo-treated patients.
Table 12: Mean Change in Weight (kg) from Baseline in the Adult Adjunctive Therapy Bipolar Depression Studies
Patients were randomized to flexibly dosed Lurasidone 20 to 120 mg/day or placebo as adjunctive therapy with lithium or valproate.
Placebo
(n=307)Lurasidone 20 to 120 mg/day
(n=327)All Patients +0.16 +0.11 In the uncontrolled, open-label, longer-term bipolar depression study, patients who were treated with lurasidone, as adjunctive therapy with either lithium or valproate in the short-term and continued in the longer-term study, had a mean change in weight of +1.28 kg at week 24 (n=86).
Pediatric Patients (10 to 17 years)
Data from the 6-week, placebo-controlled bipolar depression study in patients 10 to 17 years are presented in Table 13. The mean change in weight gain was +0.7 kg for lurasidone hydrochloride -treated patients compared to +0.5 kg for placebo-treated patients. The proportion of patients with a ≥7% increase in body weight (at Endpoint) was 4.0% for Lurasidone hydrochloride-treated patients and 5.3% for placebo-treated patients.
Table 13: Mean Change in Weight (kg) from Baseline in the Bipolar Depression Study in Pediatric Patients (10 to 17 years)
Placebo
(n=170)Lurasidone 20 to 80 mg/day
(n=175)All Patients +0.5 +0.7 Pediatric Patients (6 to 17 years)
In a long-term, open-label study that enrolled pediatric patients with schizophrenia, bipolar depression, or autistic disorder from three short-term, placebo-controlled trials, 54% (378/701) received lurasidone for 104 weeks. The mean increase in weight from open-label baseline to Week 104 was 5.85 kg. To adjust for normal growth, z-scores were derived (measured in standard deviations [SD]), which normalize for the natural growth of children and adolescents by comparisons to age- and sex-matched population standards. A z-score change <0.5 SD is considered not clinically significant. In this trial, the mean change in z-score from open-label baseline to Week 104 was -0.06 SD for body weight and -0.13 SD for body mass index (BMI), indicating minimal deviation from the normal curve for weight gain.
5.7 Hyperprolactinemia
As with other drugs that antagonize dopamine D2 receptors, lurasidone hydrochloride elevates prolactin levels. Hyperprolactinemia may suppress hypothalamic GnRH, resulting in reduced pituitary gonadotrophin secretion. This, in turn, may inhibit reproductive function by impairing gonadal steroidogenesis in both female and male patients. Galactorrhea, amenorrhea, gynecomastia, and impotence have been reported with prolactin-elevating compounds. Long-standing hyperprolactinemia, when associated with hypogonadism, may lead to decreased bone density in both female and male patients [see Adverse Reactions (6)].
Tissue culture experiments indicate that approximately one-third of human breast cancers are prolactin dependent in vitro, a factor of potential importance if the prescription of these drugs is considered in a patient with previously detected breast cancer. As is common with compounds which increase prolactin release, an increase in mammary gland neoplasia was observed in a carcinogenicity study conducted with lurasidone in rats and mice [see Nonclinical Toxicology (13)]. Published epidemiologic studies have shown inconsistent results when exploring the potential association between hyperprolactinemia and breast cancer.
Schizophrenia
Adults
In short-term, placebo-controlled schizophrenia studies, the median change from baseline to endpoint in prolactin levels for lurasidone hydrochloride -treated patients was +0.4 ng/mL and was -1.9 ng/mL in the placebo- treated patients. The median change from baseline to endpoint for males was +0.5 ng/mL and for females was -0.2 ng/mL. Median changes for prolactin by dose are shown in Table 14.
Table 14: Median Change in Prolactin (ng/mL) from Baseline in Adult Schizophrenia Studies
Placebo Lurasidone 20 mg/day 40 mg/day 80 mg/day 120 mg/day 160 mg/day All Patients -1.9
(n=672)-1.1
(n=70)-1.4
(n=476)-0.2
(n=495)+3.3
(n=284)+3.3
(n=115)Females -5.1
(n=200)-0.7
(n=19)-4.0
(n=149)-0.2
(n=150)+6.7
(n=70)+7.1
(n=36)Males -1.3
(n=472)-1.2
(n=51)-0.7
(n=327)-0.2
(n=345)+3.1
(n=214)+2.4
(n=79)The proportion of patients with prolactin elevations ≥ 5× upper limit of normal (ULN) was 2.8% for lurasidone hydrochloride -treated patients and = 1.0% for placebo-treated patients. The proportion of female patients with prolactin elevations ≥ 5x ULN was 5.7% for lurasidone hydrochloride -treated patients and = 2.0% for placebo- treated female patients. The proportion of male patients with prolactin elevations ≥ 5x ULN was 1.6% and 0.6% for placebo-treated male patients.
In the uncontrolled longer-term schizophrenia studies (primarily open-label extension studies), lurasidone hydrochloride was associated with a median change in prolactin of -0.9 ng/mL at week 24 (n=357), -5.3ng/mL at week 36 (n=190) and -2.2 ng/mL at week 52 (n=307).
Adolescents
In the short-term, placebo-controlled adolescent schizophrenia study, the median change from baseline to endpoint in prolactin levels for lurasidone hydrochloride -treated patients was +1.1 ng/mL and was +0.1 ng/mL for placebo-treated patients. For lurasidone hydrochloride -treated patients, the median change from baseline to endpoint for males was +1.0 ng/mL and for females was +2.6 ng/mL. Median changes for prolactin by dose are shown in Table 15.
Table 15: Median Change in Prolactin (ng/mL) from Baseline in the Adolescent Schizophrenia Study
PlaceboLurasidone
40 mg/dayLurasidone
80 mg/dayAll Patients +0.10
(n=103)+0.75
(n=102)+1.20
(n=99)Females +0.70
(n=39)+0.60
(n=42)+4.40
(n=33)Males 0.00
(n=64)+0.75
(n=60)+1.00
(n=66)The proportion of patients with prolactin elevations ≥5x ULN was 0.5% for lurasidone hydrochloride -treated patients and 1.0% for placebo-treated patients. The proportion of female patients with prolactin elevations ≥5x ULN was 1.3% for lurasidone hydrochloride -treated patients and 0% for placebo-treated female patients. The proportion of male patients with prolactin elevations ≥5x ULN was 0% for lurasidone hydrochloride treated patients and 1.6% for placebo-treated male patients.
Bipolar Depression
Adults
Monotherapy
The median change from baseline to endpoint in prolactin levels, in the adult short - term, flexible-dosed, placebo-controlled monotherapy bipolar depression study, was +1.7 ng/mL and +3.5 ng/mL with lurasidone hydrochloride 20 to 60 mg/day and 80 to 120 mg/day, respectively compared to +0.3 ng/mL with placebo treated patients. The median change from baseline to endpoint for males was +1.5 ng/mL and for females was +3.1 ng/mL. Median changes for prolactin by dose range are shown in Table 16.
Table 16: Median Change in Prolactin (ng/mL) from Baseline in the Adult Monotherapy Bipolar Depression Study
Patients were randomized to flexibly dosed Lurasidone 20 to 60 mg/day, Lurasidone 80 to 120 mg/day, or placebo
Placebo Lurasidone 20 to 60 mg/day 80 to 120 mg/day All Patients +0.3
(n=147)+1.7
(n=140)+3.5
(n=144)Females 0.0
(n=82)+1.8
(n=78)+5.3
(n=88)Males +0.4
(n=65)+1.2
(n=62)+1.9
(n=56)The proportion of patients with prolactin elevations ≥ 5x upper limit of normal (ULN) was 0.4% for lurasidone hydrochloride -treated patients and 0.0% for placebo-treated patients. The proportion of female patients with prolactin elevations ≥ 5x ULN was 0.6% for lurasidone hydrochloride -treated patients and 0% for placebo- treated female patients. The proportion of male patients with prolactin elevations ≥ 5x ULN was 0% and 0% for placebo-treated male patients.
In the uncontrolled, open-label, longer-term bipolar depression study, patients who were treated with lurasidone hydrochloride as monotherapy in the short-term and continued in the longer-term study, had a median change in prolactin of -1.15 ng/mL at week 24 (n=130).
Adjunctive Therapy with Lithium or Valproate
The median change from baseline to endpoint in prolactin levels, in the adult short-term, flexible-dosed, placebo-controlled adjunctive therapy bipolar depression studies was +2.8 ng/mL with lurasidone hydrochloride 20 to 120 mg/day compared to 0.0 ng/mL with placebo-treated patients. The median change from baseline to endpoint for males was +2.4 ng/mL and for females was +3.2 ng/mL. Median changes for prolactin across the dose range are shown in Table 17.
Table 17: Median Change in Prolactin (ng/mL) from Baseline in the Adult Adjunctive Therapy Bipolar Depression Studies
Patients were randomized to flexibly dosed Lurasidone 20 to 120 mg/day or placebo as adjunctive therapy with lithium or valproate.
Placebo Lurasidone 20 to 120 mg/day All Patients 0.0
(n=301)+2.8
(n=321)Females +0.4
(n=156)+3.2
(n=162)Males -0.1
(n=145)+2.4
(n=159)The proportion of patients with prolactin elevations ≥ 5x upper limit of normal (ULN) was 0.0% for lurasidone hydrochloride-treated patients and 0.0% for placebo-treated patients. The proportion of female patients with prolactin elevations ≥ 5x ULN was 0% for lurasidone hydrochloride -treated patients and 0% for placebo-treated female patients. The proportion of male patients with prolactin elevations ≥ 5x ULN was 0% and 0% for placebo-treated male patients.
In the uncontrolled, open-label, longer-term bipolar depression study, patients who were treated with lurasidone hydrochloride, as adjunctive therapy with either lithium or valproate, in the short-term and continued in the longer-term study, had a median change in prolactin of -2.9 ng/mL at week 24 (n=88).
Pediatric Patients (10 to 17 years)
In the 6-week, placebo-controlled bipolar depression study with pediatric patients 10 to 17 years, the median change from baseline to endpoint in prolactin levels for lurasidone hydrochloride -treated patients was +1.10 ng/mL and was +0.50 ng/mL for placebo-treated patients. For lurasidone hydrochloride -treated patients, the median change from baseline to endpoint for males was +0.85 ng/mL and for females was +2.50 ng/mL. Median changes for prolactin are shown in Table 18.
Table 18: Median Change in Prolactin (ng/mL) from Baseline in the Bipolar Depression Study in Pediatric Patients (10 to 17 years)
Placebo Lurasidone 20 to 80 mg/day All Patients +0.50
(n=157)+1.10
(n=165)Females +0.55
(n=78)+2.50
(n=83)Males +0.50
(n=79)+0.85
(n=82)The proportion of patients with prolactin elevations ≥5x ULN was 0% for lurasidone hydrochloride treated patients and 0.6% for placebo-treated patients. The proportion of female patients with prolactin elevations ≥5x ULN was 0% for lurasidone hydrochloride -treated patients and 1.3% for placebo-treated female patients. No male patients in the placebo or lurasidone hydrochloride treatment groups had prolactin elevations ≥5x ULN.
Pediatric Patients (6 to 17 years)
In a 104-week, open-label study of pediatric patients with schizophrenia, bipolar depression, or autistic disorder, the median changes from baseline to endpoint in serum prolactin levels were -0.20 ng/mL (all patients), -0.30 ng/mL (females), and -0.05 ng/mL (males). The proportions of patients with a markedly high prolactin level (≥5 times the upper limit of normal) at any time during open-label treatment were 2% (all patients), 3% (females), and 1% (males).
Adverse events among females in this trial that are potentially prolactin-related include galactorrhea (0.6%). Among male patients in this study, decreased libido was reported in one patient (0.2%) and there were no reports of impotence, gynecomastia, or galactorrhea.
5.8 Leukopenia, Neutropenia and Agranulocytosis
Leukopenia/neutropenia has been reported during treatment with antipsychotic agents. Agranulocytosis (including fatal cases) has been reported with other agents in the class.
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a pre-existing low WBC or a history of drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and lurasidone hydrochloride should be discontinued at the first sign of decline in WBC, in the absence of other causative factors.
Patients with neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue lurasidone hydrochloride and have their WBC followed until recovery.
5.9 Orthostatic Hypotension and Syncope
Lurasidone hydrochloride may cause orthostatic hypotension and syncope, perhaps due to its α1-adrenergic receptor antagonism. Associated adverse reactions can include dizziness, lightheadedness, tachycardia, and bradycardia. Generally, these risks are greatest at the beginning of treatment and during dose escalation. Patients at increased risk of these adverse reactions or at increased risk of developing complications from hypotension include those with dehydration, hypovolemia, treatment with antihypertensive medication, history of cardiovascular disease (e.g., heart failure, myocardial infarction, ischemia, or conduction abnormalities), history of cerebrovascular disease, as well as patients who are antipsychotic-naïve. In such patients, consider using a lower starting dose and slower titration, and monitor orthostatic vital signs.
Orthostatic hypotension, as assessed by vital sign measurement, was defined by the following vital sign changes: ≥ 20 mm Hg decrease in systolic blood pressure and ≥ 10 bpm increase in pulse from sitting to standing or supine to standing position.
Schizophrenia
Adults
The incidence of orthostatic hypotension and syncope reported as adverse events from short-term, placebo-controlled schizophrenia studies was (lurasidone hydrochloride incidence, placebo incidence): orthostatic hypotension [0.3% (5/1508), 0.1% (1/708)] and syncope [0.1% (2/1508), 0% (0/708)].
In short-term schizophrenia clinical studies, orthostatic hypotension, as assessed by vital signs, occurred with a frequency of 0.8% with lurasidone hydrochloride 40 mg, 2.1% with lurasidone hydrochloride 80 mg, 1.7% with lurasidone hydrochloride 120 mg and 0.8% with lurasidone hydrochloride 160 mg compared to 0.7% with placebo.
Adolescents
The incidence of orthostatic hypotension reported as adverse events from the short-term, placebo- controlled adolescent schizophrenia study was 0.5% (1/214) in lurasidone hydrochloride -treated patients and 0% (0/112) in placebo-treated patients. No syncope event was reported.
Orthostatic hypotension, as assessed by vital signs, occurred with a frequency of 0% with lurasidone hydrochloride 40 mg and 2.9% with lurasidone hydrochloride 80 mg, compared to 1.8% with placebo.
Bipolar Depression
Adults
Monotherapy
In the adult short-term, flexible-dose, placebo-controlled monotherapy bipolar depression study, there were no reported adverse events of orthostatic hypotension and syncope. Orthostatic hypotension, as assessed by vital signs, occurred with a frequency of 0.6% with lurasidone hydrochloride 20 to 60 mg and 0.6% with lurasidone hydrochloride 80 to 120 mg compared to 0% with placebo.
Adjunctive Therapy with Lithium or Valproate
In the adult short-term, flexible-dose, placebo-controlled adjunctive therapy bipolar depression therapy studies, there were no reported adverse events of orthostatic hypotension and syncope. Orthostatic hypotension, as assessed by vital signs, occurred with a frequency of 1.1% with lurasidone hydrochloride 20 to 120 mg compared to 0.9% with placebo.
Pediatric Patients (10 to 17 years)
In the 6-week, placebo-controlled bipolar depression study in pediatric patients 10 to 17 years, there were no reported adverse events of orthostatic hypotension or syncope. Orthostatic hypotension, as assessed by vital signs, occurred with a frequency of 1.1% with lurasidone 20 to 80 mg/day, compared to 0.6% with placebo.
5.10 Falls
Lurasidone hydrochloride may cause somnolence, postural hypotension, motor and sensory instability, which may lead to falls and, consequently, fractures or other injuries. For patients with diseases, conditions, or medications that could exacerbate these effects, complete fall risk assessments when initiating antipsychotic treatment and recurrently for patients on long-term antipsychotic therapy.
5.11 Seizures
As with other antipsychotic drugs, lurasidone hydrochloride should be used cautiously in patients with a history of seizures or with conditions that lower the seizure threshold, e.g., Alzheimer’s dementia. Conditions that lower the seizure threshold may be more prevalent in patients 65 years or older.
Schizophrenia
In adult short-term, placebo-controlled schizophrenia studies, seizures/convulsions occurred in 0.1% (2/1508) of patients treated with lurasidone hydrochloride compared to 0.1% (1/708) placebo-treated patients.
Bipolar Depression
Monotherapy
In the adult and pediatric 6-week, flexible-dose, placebo-controlled monotherapy bipolar depression studies, no patients experienced seizures/convulsions.
Adjunctive Therapy with Lithium or Valproate
In the adult short-term, flexible-dose, placebo-controlled adjunctive therapy bipolar depression studies, no patient experienced seizures/convulsions.
5.12 Potential for Cognitive and Motor Impairment
Lurasidone hydrochloride, like other antipsychotics, has the potential to impair judgment, thinking or motor skills. Caution patients about operating hazardous machinery, including motor vehicles, until they are reasonably certain that therapy with lurasidone hydrochloride does not affect them adversely. In clinical studies with lurasidone hydrochloride, somnolence included: hypersomnia, hypersomnolence, sedation and somnolence.
Schizophrenia
Adults
In short-term, placebo-controlled schizophrenia studies, somnolence was reported by 17.0% (256/1508) of patients treated with lurasidone hydrochloride (15.5% Lurasidone hydrochloride 20 mg, 15.6% lurasidone hydrochloride 40 mg, 15.2% lurasidone hydrochloride 80 mg, 26.5% lurasidone hydrochloride 120 mg and 8.3% lurasidone hydrochloride 160 mg/day) compared to 7.1% (50/708) of placebo patients.
Adolescents
In the short-term, placebo-controlled adolescent schizophrenia study, somnolence was reported by 14.5% (31/214) of patients treated with lurasidone hydrochloride (15.5% lurasidone hydrochloride 40 mg and 13.5% lurasidone hydrochloride 80 mg,/day) compared to 7.1% (8/112) of placebo patients.
Bipolar Depression
Adults
Monotherapy
In the adult short-term, flexible-dosed, placebo-controlled monotherapy bipolar depression study, somnolence was reported by 7.3% (12/164) and 13.8% (23/167) with lurasidone hydrochloride 20 to 60 mg and 80 to120 mg, respectively compared to 6.5% (11/168) of placebo patients.
Adjunctive Therapy with Lithium or Valproate
In the adult short-term, flexible-dosed, placebo-controlled adjunctive therapy bipolar depression studies, somnolence was reported by 11.4% (41/360) of patients treated with lurasidone hydrochloride 20 to120 mg compared to 5.1% (17/334) of placebo patients.
Pediatric Patients (10 to 17 years)
In the 6-week, placebo-controlled bipolar depression study in pediatric patients 10 to 17 years, somnolence was reported by 11.4% (20/175) of patients treated with lurasidone hydrochloride 20 to 80 mg/day compared to 5.8% (10/172) of placebo treated patients.
5.13 Body Temperature Dysregulation
Disruption of the body’s ability to reduce core body temperature has been attributed to antipsychotic agents. Appropriate care is advised when prescribing lurasidone hydrochloride for patients who will be experiencing conditions that may contribute to an elevation in core body temperature, e.g., exercising strenuously, exposure to extreme heat, receiving concomitant medication with anticholinergic activity, or being subject to dehydration.
5.14 Activation of Mania/Hypomania
Antidepressant treatment can increase the risk of developing a manic or hypomanic episode, particularly in patients with bipolar disorder. Monitor patients for the emergence of such episodes.
In the adult bipolar depression monotherapy and adjunctive therapy (with lithium or valproate) studies, less than 1% of subjects in the lurasidone hydrochloride and placebo groups developed manic or hypomanic episodes.
5.15 Dysphagia
Esophageal dysmotility and aspiration have been associated with antipsychotic drug use. Aspiration pneumonia is a common cause of morbidity and mortality in elderly patients, in particular those with advanced Alzheimer’s dementia. Lurasidone hydrochloride and other antipsychotic drugs should be used cautiously in patients at risk for aspiration pneumonia.
5.16 Neurological Adverse Reactions in Patients with Parkinson’s Disease or Dementia with Lewy Bodies
Patients with Parkinson’s Disease or Dementia with Lewy Bodies are reported to have an increased sensitivity to antipsychotic medication. Manifestations of this increased sensitivity include confusion, obtundation, postural instability with frequent falls, extrapyramidal symptoms, and clinical features consistent with the neuroleptic malignant syndrome.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in more detail in other sections of the labeling:
- Increased Mortality in Elderly Patients with Dementia-Related Psychosis [see Boxed Warning and Warnings and Precautions (5.1)]
- Suicidal Thoughts and Behaviors [see Boxed Warning and Warnings and Precautions (5.2)]
- Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients with Dementia-related Psychosis [see Warnings and Precautions (5.3)]
- Neuroleptic Malignant Syndrome [see Warnings and Precautions (5.4)]
- Tardive Dyskinesia [see Warnings and Precautions (5.5)]
- Metabolic Changes [see Warnings and Precautions (5.6)]
- Hyperprolactinemia [see Warnings and Precautions (5.7)]
- Leukopenia, Neutropenia, and Agranulocytosis [see Warnings and Precautions (5.8)]
- Orthostatic Hypotension and Syncope [see Warnings and Precautions (5.9)]
- Falls [see Warnings and Precautions (5.10)]
- Seizures [see Warnings and Precautions (5.11)]
- Potential for Cognitive and Motor Impairment [see Warnings and Precautions (5.12)]
- Body Temperature Dysregulation [see Warnings and Precautions (5.13)]
- Activation of Mania/Hypomania [see Warnings and Precautions (5.14)]
- Dysphagia [see Warnings and Precautions (5.15)]
- Neurological Adverse Reactions in Patients with Parkinson’s Disease or Dementia with Lewy Bodies [see Warnings and Precautions (5.16)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Adults
The information below is derived from an integrated clinical study database for lurasidone hydrochloride consisting of 3799 adult patients exposed to one or more doses of lurasidone hydrochloride for the treatment of schizophrenia, and bipolar depression in placebo-controlled studies. This experience corresponds with a total experience of 1250.9 patient-years. A total of 1106 lurasidone hydrochloride -treated patients had at least 24 weeks and 371 lurasidone hydrochloride -treated patients had at least 52 weeks of exposure.
Adverse events during exposure to study treatment were obtained by general inquiry and voluntarily reported adverse experiences, as well as results from physical examinations, vital signs, ECGs, weights and laboratory investigations. Adverse experiences were recorded by clinical investigators using their own terminology. In order to provide a meaningful estimate of the proportion of individuals experiencing adverse events, events were grouped in standardized categories using MedDRA terminology.
Schizophrenia
The following findings are based on the short-term, placebo-controlled premarketing adult studies for schizophrenia in which lurasidone hydrochloride was administered at daily doses ranging from 20 to 160 mg (n=1508).
Commonly Observed Adverse Reactions:The most common adverse reactions (incidence ≥ 5% and at least twice the rate of placebo) in patients treated with lurasidone hydrochloride were somnolence, akathisia, extrapyramidal symptoms, and nausea.
Adverse Reactions Associated with Discontinuation of Treatment: A total of 9.5% (143/1508) lurasidone hydrochloride treated patients and 9.3% (66/708) of placebo-treated patients discontinued due to adverse reactions. There were no adverse reactions associated with discontinuation in subjects treated with lurasidone hydrochloride that were at least 2% and at least twice the placebo rate.
Adverse Reactions Occurring at an Incidence of 2% or More in lurasidone hydrochloride -Treated Patients: Adverse reactions associated with the use of lurasidone hydrochloride (incidence of 2% or greater, rounded to the nearest percent and lurasidone hydrochloride incidence greater than placebo) that occurred during acute therapy (up to 6 weeks in patients with schizophrenia) are shown in Table 19.
Table 19: Adverse Reactions in 2% or More of Lurasidone hydrochloride-Treated Patients and That Occurred at Greater Incidence than in the Placebo-Treated Patients in Adult Short-term Schizophrenia Studies
Note: Figures rounded to the nearest integer
* Somnolence includes adverse event terms: hypersomnia, hypersomnolence, sedation, and somnolence
** Extrapyramidal symptoms include adverse event terms: bradykinesia, cogwheel rigidity, drooling, dystonia, extrapyramidal disorder, hypokinesia, muscle rigidity, oculogyric crisis, oromandibular dystonia, parkinsonism, psychomotor retardation, tongue spasm, torticollis, tremor, and trismus
Percentage of Patients Reporting Reaction Lurasidone Body System or
Organ ClassPlacebo
(N=708)
(%)20
mg/day
(N=71)
(%)40
mg/day
(N=487)
(%)80
mg/day
(N=538)
(%)120
mg/day
(N=291)
(%)160
mg/day
(N=121)
(%)All
Lurasidone
(N=1508)
(%)Gastrointestinal Disorders Nausea 5 11 10 9 13 7 10 Vomiting 6 7 6 9 9 7 8 Dyspepsia 5 11 6 5 8 6 6 Salivary
Hypersecretion<1 1 1 2 4 2 2 Musculoskeletal and Connective Tissue Disorders Back Pain 2 0 4 3 4 0 3 Nervous System Disorders Somnolence* 7 15 16 15 26 8 17 Akathisia 3 6 11 12 22 7 13 Extrapyramidal
Disorder**6 6 11 12 22 13 14 Dizziness 2 6 4 4 5 6 4 Psychiatric Disorders Insomnia 8 8 10 11 9 7 10 Agitation 4 10 7 3 6 5 5 Anxiety 4 3 6 4 7 3 5 Restlessness 1 1 3 1 3 2 2 Dose-Related Adverse Reactions in the Schizophrenia Studies
Akathisia and extrapyramidal symptoms were dose-related. The frequency of akathisia increased with dose up to 120 mg/day (5.6% for lurasidone hydrochloride 20 mg, 10.7% for lurasidone hydrochloride 40 mg, 12.3% for lurasidone hydrochloride 80 mg, and 22.0% for lurasidone hydrochloride 120 mg). Akathisia was reported by 7.4% (9/121) of patients receiving 160 mg/day. Akathisia occurred in 3.0% of subjects receiving placebo. The frequency of extrapyramidal symptoms increased with dose up to 120 mg/day (5.6% for lurasidone hydrochloride 20 mg, 11.5% for lurasidone hydrochloride 40 mg, 11.9% for lurasidone hydrochloride 80 mg, and 22.0% for lurasidone hydrochloride 120 mg).
Bipolar Depression (Monotherapy) The following findings are based on the adult short-term, placebo-controlled premarketing study for bipolar depression in which lurasidone hydrochloride was administered at daily doses ranging from 20 to 120 mg (n=331).
Commonly Observed Adverse Reactions:The most common adverse reactions (incidence ≥ 5%, in either dose group, and at least twice the rate of placebo) in patients treated with lurasidone hydrochloride were akathisia, extrapyramidal symptoms, somnolence, nausea, vomiting, diarrhea, and anxiety.
Adverse Reactions Associated with Discontinuation of Treatment: A total of 6.0% (20/331) lurasidone hydrochloride- treated patients and 5.4% (9/168) of placebo-treated patients discontinued due to adverse reactions. There were no adverse reactions associated with discontinuation in subjects treated with lurasidone hydrochloride that were at least 2% and at least twice the placebo rate.
Adverse Reactions Occurring at an Incidence of 2% or More in lurasidone hydrochloride -Treated Patients: Adverse reactions associated with the use of lurasidone hydrochloride (incidence of 2% or greater, rounded to the nearest percent and lurasidone hydrochloride incidence greater than placebo) that occurred during acute therapy (up to 6-week in patients with bipolar depression) are shown in Table 20.
Table 20: Adverse Reactions in 2% or More of Lurasidone hydrochloride-Treated Patients and That Occurred at Greater Incidence than in the Placebo-Treated Patients in the Adult Short-term Monotherapy Bipolar Depression Study
Note: Figures rounded to the nearest integer
*Extrapyramidal symptoms include adverse event terms: bradykinesia, cogwheel rigidity, drooling, dystonia, extrapyramidal disorder, glabellar reflex abnormal, hypokinesia, muscle rigidity, oculogyric crisis, oromandibular dystonia, parkinsonism, psychomotor retardation, tongue spasm, torticollis, tremor, and trismus
** Somnolence includes adverse event terms: hypersomnia, hypersomnolence, sedation, and somnolence
Percentage of Patients Reporting Reaction Body System or Organ Class
Dictionary-derived TermPlacebo
(N=168)
(%)Lurasidone
20-60 mg/day
(N=164)
(%)Lurasidone
80-120 mg/day
(N=167)
(%)All Lurasidone (N=331)
(%)Gastrointestinal Disorders Nausea 8 10 17 14 Dry Mouth 4 6 4 5 Vomiting 2 2 6 4 Diarrhea 2 5 3 4 Infections and Infestations Nasopharyngitis 1 4 4 4 Influenza 1 <1 2 2 Urinary Tract Infection <1 2 1 2 Musculoskeletal and Connective Tissue Disorders Back Pain <1 3 <1 2 Nervous System Disorders Extrapyramidal Symptoms* 2 5 9 7 Akathisia 2 8 11 9 Somnolence** 7 7 14 11 Psychiatric Disorders Anxiety 1 4 5 4 Dose-Related Adverse Reactions in the Monotherapy Study:
In the adult short-term, placebo-controlled study (involving lower and higher lurasidone hydrochloride dose ranges) [see Clinical Studies (14.2)] the adverse reactions that occurred with a greater than 5% incidence in the patients treated with lurasidone hydrochloride in any dose group and greater than placebo in both groups were nausea (10.4%, 17.4%), somnolence (7.3%, 13.8%), akathisia (7.9%, 10.8%), and extrapyramidal symptoms (4.9%, 9.0%) for lurasidone hydrochloride 20 to 60 mg/day and lurasidone hydrochloride 80 to 120 mg/day, respectively.
Bipolar Depression
Adjunctive Therapy with Lithium or Valproate
The following findings are based on two adult short-term, placebo-controlled premarketing studies for bipolar depression in which lurasidone hydrochloride was administered at daily doses ranging from 20 to 120 mg as adjunctive therapy with lithium or valproate (n=360).
Commonly Observed Adverse Reactions:The most common adverse reactions (incidence ≥ 5% and at least twice the rate of placebo) in subjects treated with lurasidone hydrochloride were akathisia and somnolence.
Adverse Reactions Associated with Discontinuation of Treatment:A total of 5.8% (21/360) lurasidone hydrochloride treated patients and 4.8% (16/334) of placebo-treated patients discontinued due to adverse reactions. There were no adverse reactions associated with discontinuation in subjects treated with lurasidone hydrochloride that were at least 2% and at least twice the placebo rate.
Adverse Reactions Occurring at an Incidence of 2% or More in lurasidone hydrochloride -Treated Patients: Adverse reactions associated with the use of lurasidone hydrochloride (incidence of 2% or greater, rounded to the nearest percent and lurasidone hydrochloride incidence greater than placebo) that occurred during acute therapy (up to 6 weeks in patients with bipolar depression) are shown in Table 21.
Table 21: Adverse Reactions in 2% or More of Lurasidone hydrochloride-Treated Patients and That Occurred at Greater Incidence than in the Placebo-Treated Patients in the Adult Short-term Adjunctive Therapy Bipolar Depression Studies
Note: Figures rounded to the nearest integer
*Extrapyramidal symptoms include adverse event terms: bradykinesia, cogwheel rigidity, drooling, dystonia, extrapyramidal disorder, glabellar reflex abnormal, hypokinesia, muscle rigidity, oculogyric crisis, oromandibular dystonia, parkinsonism, psychomotor retardation, tongue spasm, torticollis, tremor, and trismus
** Somnolence includes adverse event terms: hypersomnia, hypersomnolence, sedation, and somnolence
Percentage of Patients Reporting Reaction Body System or Organ Class
Dictionary-derived TermPlacebo
(N=334)
(%)Lurasidone
20 to 120 mg/day
(N=360)
(%)Gastrointestinal Disorders Nausea 10 14 Vomiting 1 4 General Disorders Fatigue 1 3 Infections and Infestations Nasopharyngitis 2 4 Investigations Weight Increased <1 3 Metabolism and Nutrition Disorders Increased Appetite 1 3 Nervous System Disorders Extrapyramidal Symptoms* 9 14 Somnolence** 5 11 Akathisia 5 11 Psychiatric Disorders Restlessness <1 4 Adolescents
Schizophrenia
The following findings are based on the short-term, placebo-controlled adolescent study for schizophrenia in which lurasidone hydrochloride was administered at daily doses ranging from 40 (N=110) to 80 mg (N=104).
Commonly Observed Adverse Reactions:The most common adverse reactions (incidence ≥5% and at least twice the rate of placebo) in adolescent patients (13 to 17 years) treated with lurasidone hydrochloride were somnolence, nausea, akathisia, extrapyramidal symptoms (non-akathisia, 40mg only), vomiting, and rhinorrhea/rhinitis (80mg only).
Adverse Reactions Associated with Discontinuation of Treatment: The incidence of discontinuation due to adverse reactions between lurasidone hydrochloride - and placebo-treated adolescent patients (13 to 17 years) was 4% and 8%, respectively.
Adverse Reactions Occurring at an Incidence of 2% or More in lurasidone hydrochloride -Treated Patients:Adverse reactions associated with the use of lurasidone hydrochloride (incidence of 2% or greater, rounded to the nearest percent and lurasidone hydrochloride incidence greater than placebo) that occurred during acute therapy (up to 6-weeks in adolescent patients with schizophrenia) are shown in Table 22.
Table 22: Adverse Reactions in 2% or More of Lurasidone hydrochloride-Treated Patients and That Occurred at Greater Incidence than in the Placebo-Treated Patients in the Adolescent Short-term Schizophrenia Study
Note: Figures rounded to the nearest integer
* Somnolence includes adverse event terms: hypersomnia, sedation, and somnolence
** Viral Infection includes adverse event terms: nasopharyngitis, influenza, viral infection, upper respiratory tract infection
*** Rhinitis incudes adverse event terms: rhinitis, allergic rhinitis, rhinorrhea, and nasal congestion
Percentage of Patients Reporting Reaction
Body System or Organ Class
Dictionary-derived Term
Placebo
(N=112)Lurasidone
40 mg/day
(N=110)Lurasidone
80 mg/day
(N=104)
All Lurasidone
(N=214)Gastrointestinal Disorders Nausea 3 13 14 14 Vomiting 2 8 6 8 Diarrhea 1 3 5 4 Dry Mouth 0 2 3 2 Infections and Infestations Viral Infection** 6 11 10 10 Rhinitis*** 2 <1 8 4 Oropharyngeal pain 0 <1 3 2 Tachycardia 0 0 3 1 Nervous System Disorders Somnolence* 7 15 13 15 Akathisia 2 9 9 9 Dizziness 1 5 5 5 Pediatric Patients (10 to 17 years)
Bipolar Depression
The following findings are based on the 6-week , placebo-controlled study for bipolar depression in pediatric patients 10 to 17 years in which lurasidone hydrochloride was administered at daily doses ranging from 20 to 80 mg (N=175).
Commonly Observed Adverse Reactions: The most common adverse reactions (incidence ≥5%, and at least twice the rate of placebo) in pediatric patients (10 to 17 years) treated with lurasidone hydrochloride were nausea, weight increase, and insomnia.
Adverse Reactions Associated with Discontinuation of Treatment:The incidence of discontinuation due to adverse reactions between lurasidone hydrochloride - and placebo-treated pediatric patients 10 to 17 years was 2% and 2%, respectively.
Adverse Reactions Occurring at an Incidence of 2% or More in lurasidone hydrochloride -Treated Patients: Adverse reactions associated with the use of lurasidone hydrochloride (incidence of 2% or greater, rounded to the nearest percent and lurasidone hydrochloride incidence greater than placebo) that occurred during acute therapy (up to 6 weeks in pediatric patients with bipolar depression) are shown in Table 23.
Table 23: Adverse Reactions in 2% or More of Lurasidone hydrochloride-Treated Patients and That Occurred at Greater Incidence than in the Placebo-Treated Patients in the 6-Week Bipolar Depression Study in Pediatric Patients (10 to 17 years)
Note: Figures rounded to the nearest integer
*Somnolence includes adverse event terms: hypersomnia, hypersomnolence, sedation, and somnolence
**EPS includes adverse event terms: akathisia, cogwheel rigidity, dyskinesia, dystonia, hyperkinesia, joint stiffness, muscle rigidity, muscle spasms, musculoskeletal stiffness, oculogyric crisis, parkinsonism, tardive dyskinesia, and tremor
Percentage of Patients Reporting Reaction Body System or Organ Class
Dictionary-derived TermPlacebo
(N=172)Lurasidone
20 to 80 mg/day
(N=175)Gastrointestinal Disorders Nausea 6 16 Vomiting 4 6 Abdominal Pain Upper 2 3 Diarrhea 2 3 Abdominal Pain 1 3 General Disorders And Administration Site Conditions Fatigue 2 3 Investigations Weight Increased 2 7 Metabolism and Nutrition Disorders Decreased Appetite 2 4 Nervous System Disorders Somnolence* 6 11 Extrapyramidal symptoms** 5 6 Dizziness 5 6 Psychiatric Disorders Insomnia 2 5 Abnormal Dreams 2 2 Respiratory, Thoracic and Mediastinal Disorders Oropharyngeal Pain 2 2 Extrapyramidal Symptoms
Schizophrenia
Adults
In the short-term, placebo-controlled schizophrenia studies, for lurasidone hydrochloride -treated patients, the incidence of reported events related to extrapyramidal symptoms (EPS), excluding akathisia and restlessness, was 13.5% and 5.8% for placebo-treated patients. The incidence of akathisia for lurasidone hydrochloride -treated patients was 12.9% and 3.0% for placebo-treated patients. Incidence of EPS by dose is provided in Table 24.
Table 24: Incidence of EPS Compared to Placebo in Adult Schizophrenia Studies
Note: Figures rounded to the nearest integer
* Dystonia includes adverse event terms: dystonia, oculogyric crisis, oromandibular dystonia, tongue spasm, torticollis, and trismus
** Parkinsonism includes adverse event terms: bradykinesia, cogwheel rigidity, drooling, extrapyramidal disorder, hypokinesia, muscle rigidity, parkinsonism, psychomotor retardation, and tremor
Adverse Event Term Placebo
(N=708)
(%)Lurasidone 20 mg/day
(N=71)
(%)40 mg/day
(N=487)
(%)80 mg/day
(N=538)
(%)120 mg/day
(N=291)
(%)160 mg/day
(N=121)
(%)All EPS events 9 10 21 23 39 20 All EPS events, excluding Akathisia/Restlessness 6 6 11 12 22 13 Akathisia 3 6 11 12 22 7 Dystonia* <1 0 4 5 7 2 Parkinsonism** 5 6 9 8 17 11 Restlessness 1 1 3 1 3 2 Adolescents
In the short-term, placebo-controlled, study of schizophrenia in adolescents, the incidence of EPS, excluding events related to akathisia, for lurasidone hydrochloride -treated patients was higher in the 40 mg (10%) and the 80 mg (7.7%) treatment groups vs. placebo (3.6%); and the incidence of akathisia related events for lurasidone hydrochloride -treated patients was 8.9% vs. 1.8% for placebo-treated patients. Incidence of EPS by dose is provided in Table 25.
Table 25: Incidence of EPS Compared to Placebo in the Adolescent Schizophrenia Study
Note: Figures rounded to the nearest integer
* Dystonia includes adverse event terms: dystonia, trismus, oculogyric crisis, oromandibular dystonia, tongue spasm, and torticollis
** Parkinsonism includes adverse event terms: bradykinesia, drooling, extrapyramidal disorder, glabellar reflex abnormal, hypokinesia, parkinsonism, and psychomotor retardation
Lurasidone Adverse Event Term Placebo
(N=112)
(%)40 mg/day
(N=110)
(%)80 mg/day
(N=104)
(%)All EPS events 5 14 14 All EPS events, excluding Akathisia/Restlessness 4 7 7 Akathisia 2 9 9 Parkinsonism** <1 4 0 Dyskinesia <1 <1 1 Dystonia* 0 <1 1 Bipolar Depression
Adults
Monotherapy
In the adult short-term, placebo-controlled monotherapy bipolar depression study, for lurasidone hydrochloride-treated patients, the incidence of reported events related to EPS, excluding akathisia and restlessness was 6.9% and 2.4% for placebo-treated patients. The incidence of akathisia for lurasidone hydrochloride-treated patients was 9.4% and 2.4% for placebo-treated patients. Incidence of EPS by dose groups is provided in Table 26.
Table 26: Incidence of EPS Compared to Placebo in the Adult Monotherapy Bipolar Depression Study
Note: Figures rounded to the nearest integer
* Dystonia includes adverse event terms: dystonia, oculogyric crisis, oromandibular dystonia, tongue spasm, torticollis, and trismus
** Parkinsonism includes adverse event terms: bradykinesia, cogwheel rigidity, drooling, extrapyramidal disorder, glabellar reflex abnormal, hypokinesia, muscle rigidity, parkinsonism, psychomotor retardation, and tremor
Lurasidone Adverse Event Term Placebo
(N=168)
(%)20 to 60 mg/day
(N=164)
(%)80 to 120 mg/day
(N=167)
(%)All EPS events 5 12 20 All EPS events, excluding Akathisia/Restlessness 2 5 9 Akathisia 2 8 11 Dystonia* 0 0 2 Parkinsonism** 2 5 8 Restlessness <1 0 3 Adjunctive Therapy with Lithium or Valproate
In the adult short-term, placebo-controlled adjunctive therapy bipolar depression studies, for lurasidone hydrochloride treated patients, the incidence of EPS, excluding akathisia and restlessness, was 13.9% and 8.7% for placebo. The incidence of akathisia for lurasidone hydrochloride-treated patients was 10.8% and 4.8% for placebo-treated patients. Incidence of EPS is provided in Table 27.Table 27: Incidence of EPS Compared to Placebo in the Adult Adjunctive Therapy Bipolar Depression Studies
Note: Figures rounded to the nearest integer
* Dystonia includes adverse event terms: dystonia, oculogyric crisis, oromandibular dystonia, tongue spasm, torticollis, and trismus
** Parkinsonism includes adverse event terms: bradykinesia, cogwheel rigidity, drooling, extrapyramidal disorder, glabellar reflex abnormal, hypokinesia, muscle rigidity, parkinsonism, psychomotor retardation, and tremor
Adverse Event Term Placebo
(N=334)
(%)Lurasidone
20 to 120 mg/day
(N=360)
(%)All EPS events 13 24 All EPS events, excluding Akathisia/Restlessness 9 14 Akathisia 5 11 Dystonia* <1 1 Parkinsonism** 8 13 Restlessness <1 4 In the short-term, placebo-controlled schizophrenia and bipolar depression studies, data was objectively collected on the Simpson Angus Rating Scale (SAS) for extrapyramidal symptoms (EPS), the Barnes Akathisia Scale (BAS) for akathisia and the Abnormal Involuntary Movement Scale (AIMS) for dyskinesias.
Pediatric Patients (10 to 17 years)
In the 6-week, placebo-controlled study of bipolar depression in pediatric patients 10 to 17 years, the incidence of EPS, excluding events related to akathisia, for lurasidone-treated patients was similar in the lurasidone 20 to 80 mg/day (3.4%) treatment group vs. placebo (3.5%); and the incidence of akathisia related events for lurasidone -treated patients was 2.9% vs. 3.5% for placebo-treated patients. Incidence of EPS by dose is provided in Table 28.
Table 28: Incidence of EPS Compared to Placebo in the Bipolar Depression Study in Pediatric Patients (10 to 17 years)
Note: Figures rounded to the nearest integer
* EPS include adverse event terms: akathisia, cogwheel rigidity, dyskinesia, dystonia, hyperkinesia, joint stiffness, muscle rigidity, muscle spasms, musculoskeletal stiffness, oculogyric crisis, parkinsonism, tardive dyskinesia, and tremor
** Parkinsonism includes adverse event terms: bradykinesia, drooling, extrapyramidal disorder, glabellar reflex abnormal, hypokinesia, parkinsonism, and psychomotor retardation
***Dystonia includes adverse event terms: dystonia, oculogyric crisis, oromandibular dystonia, tongue spasm, torticollis, and trismus
Adverse Event Term Placebo
(N=172)
(%)Lurasidone
20 to 80 mg/day
(N=175)
(%)All EPS events* 5 6 All EPS events, excluding Akathisia/Restlessness 4 3 Akathisia 4 3 Parkinsonism** <1 <1 Dystonia*** 1 <1 Salivary hypersecretion <1 <1 Psychomotor hyperactivity 0 <1 Tardive Dyskinesia <1 0 All EPS events* 5 6 All EPS events, excluding Akathisia/Restlessness 4 3 Schizophrenia
Adults
The mean change from baseline for lurasidone hydrochloride -treated patients for the SAS, BAS and AIMS was comparable to placebo-treated patients, with the exception of the Barnes Akathisia Scale global score (lurasidone hydrochloride , 0.1; placebo, 0.0). The percentage of patients who shifted from normal to abnormal was greater in lurasidone hydrochloride -treated patients and placebo for the BAS (lurasidone hydrochloride , 14.4%; placebo, 7.1%), the SAS (lurasidone hydrochloride , 5.0%; placebo, 2.3%) and the AIMS (lurasidone hydrochloride , 7.4%; placebo, 5.8%).
Adolescents
The mean change from baseline for lurasidone hydrochloride - treated patients with adolescent schizophrenia for the SAS, BAS and AIMS was comparable to placebo-treated patients. The percentage of patients who shifted from normal to abnormal was greater in lurasidone hydrochloride -treated patients and placebo for the BAS (lurasidone hydrochloride, 7.0%; placebo, 1.8%), the SAS (lurasidone hydrochloride, 8.3%; placebo, 2.7%) and the AIMS (lurasidone hydrochloride, 2.8%; placebo, 0.9%).
Bipolar Depression
Adults
Monotherapy
The mean change from baseline for lurasidone hydrochloride -treated adult patients for the SAS, BAS and AIMS was comparable to placebo-treated patients. The percentage of patients who shifted from normal to abnormal was greater in lurasidone hydrochloride -treated patients and placebo for the BAS (lurasidone hydrochloride, 8.4%; placebo, 5.6%), the SAS (lurasidone hydrochloride, 3.7%; placebo, 1.9%) and the AIMS (lurasidone hydrochloride, 3.4%; placebo, 1.2%).
Adjunctive Therapy with Lithium or Valproate
The mean change from baseline for lurasidone hydrochloride -treated adult patients for the SAS, BAS and AIMS was comparable to placebo-treated patients. The percentage of patients who shifted from normal to abnormal was greater in lurasidone hydrochloride -treated patients and placebo for the BAS (lurasidone hydrochloride, 8.7%; placebo, 2.1%), the SAS (lurasidone hydrochloride, 2.8%; placebo, 2.1%) and the AIMS (lurasidone hydrochloride, 2.8%; placebo, 0.6%).
Pediatric Patients (10 to 17 years)
The mean change from baseline for lurasidone hydrochloride - treated pediatric patients 10 to 17 years with bipolar depression for the SAS, BAS and AIMS was comparable to placebo-treated patients. The percentage of patients who shifted from normal to abnormal was greater in lurasidone hydrochloride -treated patients and placebo for the BAS (lurasidone hydrochloride, 4.6%; placebo, 2.4%), the SAS (lurasidone hydrochloride, 0.6%; placebo, 0%) and was the same for the AIMS (lurasidone hydrochloride, 0%; placebo, 0%).
Dystonia
Class Effect: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first-generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
Schizophrenia
Adults
In the short-term, placebo-controlled schizophrenia clinical studies, dystonia occurred in 4.2% of lurasidone hydrochloride -treated subjects (0.0% lurasidone hydrochloride 20 mg, 3.5% lurasidone hydrochloride 40 mg, 4.5% lurasidone hydrochloride 80 mg, 6.5% lurasidone hydrochloride 120 mg and 2.5% lurasidone hydrochloride 160 mg) compared to 0.8% of subjects receiving placebo. Seven subjects (0.5%, 7/1508) discontinued clinical trials due to dystonic events – four were receiving lurasidone hydrochloride 80 mg/day and three were receiving lurasidone hydrochloride 120 mg/day.
Adolescents
In the short-term, placebo-controlled, adolescent schizophrenia study, dystonia occurred in 1% of lurasidone-treated patients (1% lurasidone hydrochloride 40 mg and 1% lurasidone hydrochloride 80 mg) compared to 0% of patients receiving placebo. No patients discontinued the clinical study due to dystonic events.
Bipolar Depression
Adults
Monotherapy
In the adult short-term, flexible-dose, placebo-controlled monotherapy bipolar depression study, dystonia occurred in 0.9% of lurasidone hydrochloride -treated subjects (0.0% and 1.8% for lurasidone hydrochloride 20 to 60 mg/day and lurasidone hydrochloride 80 to 120 mg/day, respectively) compared to 0.0% of subjects receiving placebo. No subject discontinued the clinical study due to dystonic events.
Adjunctive Therapy with Lithium or Valproate
In the adult short-term, flexible-dose, placebo-controlled adjunctive therapy bipolar depression studies, dystonia occurred in 1.1% of lurasidone hydrochloride -treated subjects (20 to 120 mg) compared to 0.6% of subjects receiving placebo. No subject discontinued the clinical study due to dystonic events.
Pediatric Patients (10 to 17 years)
In the 6-week, placebo-controlled bipolar depression study in pediatric patients 10 to 17 years, dystonia occurred in 0.6% of lurasidone hydrochloride-treated patients compared to 1.2% of patients receiving placebo. No patients discontinued the clinical study due to dystonic events.
Other Adverse Reactions Observed During the Premarketing Evaluation of lurasidone hydrochloride
Following is a list of adverse reactions reported by adult patients treated with lurasidone hydrochloride at multiple doses of ≥ 20 mg once daily within the premarketing database of 2905 patients with schizophrenia. The reactions listed are those that could be of clinical importance, as well as reactions that are plausibly drug-related on pharmacologic or other grounds. Reactions listed in Table 19. or those that appear elsewhere in the lurasidone hydrochloride label are not included.
Reactions are further categorized by organ class and listed in order of decreasing frequency according to the following definitions: those occurring in at least 1/100 patients (frequent) (only those not already listed in the tabulated results from placebo-controlled studies appear in this listing); those occurring in 1/100 to 1/1000 patients (infrequent); and those occurring in fewer than 1/1000 patients (rare).
Blood and Lymphatic System Disorders: Infrequent: anemia
Cardiac Disorders: Frequent: tachycardia; Infrequent: AV block 1st degree, angina pectoris, bradycardia
Ear and Labyrinth Disorders: Infrequent: vertigo
Eye Disorders: Frequent: blurred vision
Gastrointestinal Disorders: Frequent: abdominal pain, diarrhea; Infrequent: gastritis
General Disorders and Administrative Site Conditions: Rare: sudden death Investigations: Frequent: CPK increased
Metabolism and Nutritional System Disorders: Frequent: decreased appetite
Musculoskeletal and Connective Tissue Disorders: Rare: rhabdomyolysis
Nervous System Disorders: Infrequent: cerebrovascular accident, dysarthria
Psychiatric Disorders: Infrequent: abnormal dreams, panic attack, sleep disorder
Renal and Urinary Disorders: Infrequent: dysuria; Rare: renal failure
Reproductive System and Breast Disorders: Infrequent: amenorrhea, dysmenorrhea; Rare: breast enlargement, breast pain, galactorrhea, erectile dysfunction, priapism
Skin and Subcutaneous Tissue Disorders: Frequent: rash, pruritus; Rare: angioedema
Vascular Disorders: Frequent: hypertension Clinical Laboratory Changes
Schizophrenia
Adults
Serum Creatinine: In short-term, placebo-controlled trials, the mean change from Baseline in serum creatinine was +0.05 mg/dL for lurasidone hydrochloride -treated patients compared to +0.02 mg/dL for placebo treated patients. A creatinine shift from normal to high occurred in 3.0% (43/1453) of lurasidone hydrochloride–treated patients and 1.6% (11/681) on placebo. The threshold for high creatinine value varied from > 0.79 to > 1.3 mg/dL based on the centralized laboratory definition for each study (Table 29).
Table 29: Serum Creatinine Shifts from Normal at Baseline to High at Study End-Point in Adult Schizophrenia Studies
Laboratory Parameter Placebo
(N=708)Lurasidone 20
mg/day
(N=71)Lurasidone 40
mg/day
(N=487)Lurasidone 80
mg/day
(N=538)Lurasidone 120 mg/day
(N=291)Lurasidone 160
mg/day
(N=121)Serum Creatinine Elevated 2% 1% 2% 2% 5% 7% Adolescents
Serum Creatinine: In the short-term, placebo-controlled, adolescent schizophrenia study, the mean change from Baseline in serum creatinine was -0.009 mg/dL for lurasidone-treated patients compared to +0.017 mg/dL for placebo-treated patients. A creatinine shift from normal to high (based on the centralized laboratory definition) occurred in 7.2% (14/194) of lurasidone-treated patients and 2.9% (3/103) on placebo (Table 30).
Table 30: Serum Creatinine Shifts from Normal at Baseline to High at Study End-Point in the Adolescent Schizophrenia Study
Laboratory Parameter Placebo
(N=103)Lurasidone
40 mg/day
(N=97)Lurasidone
80 mg/day
(N=97)Serum Creatinine Elevated 2.9% 7.2% 7.2% Bipolar Depression Adults Monotherapy Serum Creatinine: In the adult short-term, flexible-dose, placebo-controlled monotherapy bipolar depression study, the mean change from Baseline in serum creatinine was +0.01 mg/dL for lurasidone hydrochloride -treated patients compared to -0.02 mg/dL for placebo-treated patients. A creatinine shift from normal to high occurred in 2.8% (9/322) of lurasidone hydrochloride -treated patients and 0.6% (1/162) on placebo (Table 31).
Table 31: Serum Creatinine Shifts from Normal at Baseline to High at Study End-Point in the Adult Monotherapy Bipolar Depression Study
Laboratory Parameter Placebo
(N=168)Lurasidone
20 to 60 mg/day
(N=164)Lurasidone
80 to 120 mg/day
(N=167)Serum Creatinine Elevated <1% 2% 4% Adjunctive Therapy with Lithium or Valproate
Serum Creatinine: In adult short-term, placebo-controlled premarketing adjunctive studies for bipolar depression, the mean change from Baseline in serum creatinine was +0.04 mg/dL for lurasidone hydrochloride-treated patients compared to -0.01 mg/dL for placebo-treated patients. A creatinine shift from normal to high occurred in 4.3% (15/360) of lurasidone hydrochloride -treated patients and 1.6% (5/334) on placebo (Table 32).
Table 32: Serum Creatinine Shifts from Normal at Baseline to High at Study End-Point in the Adult Adjunctive Therapy Bipolar Depression Studies
Laboratory Parameter Placebo
(N=334)Lurasidone
20 to 120 mg/day
(N=360)Serum Creatinine Elevated 2% 4% Pediatric Patients (10 to 17 years)
Serum Creatinine: In the 6-week, placebo-controlled bipolar depression study in pediatric patients 10 to 17 years, the mean change from Baseline in serum creatinine was +0.021 mg/dL for lurasidone hydrochloride-treated patients compared to +0.009 mg/dL for placebo-treated patients. A creatinine shift from normal to high (based on the centralized laboratory definition) occurred in 6.7% (11/163) of lurasidone hydrochloride-treated patients and 4.5% (7/155) on placebo (Table 33).
Table 33: Serum Creatinine Shifts from Normal at Baseline to High at Study End-Point in the Bipolar Depression Study in Pediatric Patients (10 to 17 years)
Laboratory Parameter Placebo
(N=155)Lurasidone
20 to 80 mg/day
(N=163)Serum Creatinine Elevated 4.5% 6.7% Pediatric Patients (6 to 17 years)
In a 104-week, open-label study in pediatric patients with schizophrenia, bipolar depression, or autistic disorder, the mean change from baseline to Week 104 in serum creatinine was +0.07 mg/dL. In patients with a normal serum creatinine at baseline, 6% experienced a shift to high at endpoint
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of lurasidone hydrochloride. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Hypersensitivity Reactions: Urticaria, throat swelling, tongue swelling, dyspnea, and rash. Metabolism and Nutrition Disorders: Hyponatremia
-
7 DRUG INTERACTIONS
7.1 Drugs Having Clinically Important Interactions with lurasidone hydrochloride.
Table 34: Clinically Important Drug Interactions with Lurasidone Hydrochloride
Strong CYP3A4 Inhibitors Clinical Impact: Concomitant use of Lurasidone with strong CYP3A4 inhibitors increased the exposure of lurasidone compared to the use of Lurasidone alone [see Clinical Pharmacology (12.3)]. Intervention: Lurasidone should not be used concomitantly with strong CYP3A4 inhibitors [see Contraindications (4)]. Examples: Ketoconazole, clarithromycin, ritonavir, voriconazole, mibefradil Moderate CYP3A4 Inhibitors Clinical Impact: Concomitant use of Lurasidone with moderate CYP3A4 inhibitors increased the exposure of lurasidone compared to the use of Lurasidone alone [see Clinical Pharmacology (12.3)]. Intervention: Lrasidone dose should be reduced to half of the original level when used concomitantly with moderate inhibitors of CYP3A4 [see Dosage and Administration (2.6)]. Examples: Diltiazem, atazanavir, erythromycin, fluconazole, verapamil Strong CYP3A4 Inducers Clinical Impact: Concomitant use of Lurasidone with strong CYP3A4 inducers decreased the exposure of lurasidone compared to the use of Lurasidone alone [see Clinical Pharmacology (12.3)]. Intervention: Lurasidone should not be used concomitantly with strong CYP3A4 inducers [see Contraindications (4)]. Examples: Rifampin, avasimibe, St. John's wort, phenytoin, carbamazepine Moderate CYP3A4 Inducers Clinical Impact: Concomitant use of Lurasidone with moderate CYP3A4 inducers decreased the exposure of lurasidone compared to the use of Lurasidone alone [see Clinical Pharmacology (12.3)]. Intervention: Lurasidone dose should be increased when used concomitantly with moderate inducers of CYP3A4 [see Dosage and Administration (2.6)]. Examples: Bosentan, efavirenz, etravirine, modafinil, nafcillin 7.2 Drugs Having No Clinically Important Interactions with lurasidone hydrochloride
Based on pharmacokinetic studies, no dosage adjustment of lurasidone hydrochloride is required when administered concomitantly with lithium, valproate, or substrates of P-gp or CYP3A4 [see Clinical Pharmacology (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to lurasidone hydrochloride during pregnancy. For more information, contact the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or visit http://womensmentalhealth.org/ clinical-and-research- programs/pregnancyregistry/.
Risk Summary
Neonates exposed to antipsychotic drugs during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery [see Clinical Considerations].
There are no studies of lurasidone hydrochloride use in pregnant women. The limited available data are not sufficient to inform a drug-associated risk of birth defects or miscarriage. In animal reproduction studies, no teratogenic effects were seen in pregnant rats and rabbits given lurasidone during the period of organogenesis at doses approximately 1.5- and 6-times, the maximum recommended human dose (MRHD) of 160 mg/day, respectively based on mg/m2 body surface area [see Data].
The estimated background risk of major birth defects and miscarriage for the indicated population(s) is unknown. All pregnancies have a background risk of birth defect, loss or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder have been reported in neonates who were exposed to antipsychotic drugs during the third trimester of pregnancy. These symptoms have varied in severity. Some neonates recovered within hours or days without specific treatment; others required prolonged hospitalization. Monitor neonates for extrapyramidal and/or withdrawal symptoms and manage symptoms appropriately.
Data
Animal Data
Pregnant rats were treated with oral lurasidone at doses of 3, 10, and 25 mg/kg/day during the period of organogenesis. These doses are 0.2, 0.6, and 1.5 times the MRHD of 160 mg/day based on mg/m2 body surface area. No teratogenic or embryo-fetal effects were observed up to 1.5 times the MRHD of 160 mg/day, based on mg/m2.
Pregnant rabbits were treated with oral lurasidone at doses of 2, 10, and 50 mg/kg/day during the period of organogenesis. These doses are 0.2, 1.2 and 6 times the MRHD of 160 mg/day based on mg/m2. No teratogenic or embryo-fetal effects were observed up to 6 times the MRHD of 160 mg/day based on mg/m2. Pregnant rats were treated with oral lurasidone at doses of 0.4, 2, and 10 mg/kg/day during the periods of organogenesis and lactation. These doses are 0.02, 0.1 and 0.6 times the MRHD of 160 mg/day based on mg/m2. No pre- and postnatal developmental effects were observed up to 0.6 times the MRHD of 160 mg/day, based on mg/m2.
8.2 Lactation
Risk Summary
Lactation studies have not been conducted to assess the presence of lurasidone in human milk, the effects on the breastfed infant, or the effects on milk production. Lurasidone is present in rat milk. The development and health benefits of breastfeeding should be considered along with the mother’s clinical need for lurasidone hydrochloride and any potential adverse effects on the breastfed infant from lurasidone hydrochloride or from the underlying maternal condition.
8.4 Pediatric Use
Schizophrenia
The safety and effectiveness of lurasidone hydrochloride 40-mg/day and 80-mg/day for the treatment of schizophrenia in adolescents (13 to 17 years) was established in a 6-week, placebo-controlled clinical study in 326 adolescent patients [see Dosage and Administration (2.1), Adverse Reactions (6.1), and Clinical Studies (14.1)].
The safety and effectiveness of lurasidone hydrochloride has not been established in pediatric patients less than 13 years of age with schizophrenia.
Bipolar Depression
The safety and effectiveness of lurasidone hydrochloride has not been established in pediatric patients less than 13 years of age with schizophrenia 20 to 80 mg/day for the treatment of bipolar depression in pediatric patients (10 to 17 years) was established in a 6-week, placebo-controlled clinical study in 347 pediatric patients [see Dosage and Administration (2.2 ), Adverse Reactions ( 6.1 ), and Clinical Studies ( 14.2)].
The safety and effectiveness of lurasidone hydrochloride has not been established in pediatric patients less than 10 years of age with bipolar depression
Irritability Associated with Autistic Disorder
The effectiveness of lurasidone hydrochloride in pediatric patients for the treatment of irritability associated with autistic disorder has not been established.
Efficacy was not demonstrated in a 6-week study evaluating lurasidone hydrochloride 20 mg/day and 60 mg/day for the treatment of pediatric patients 6 to 17 years of age with irritability associated with autistic disorder diagnosed by Diagnostic and Statistical Manual of Mental Disorders, 4th Ed., Text Revision [DSM-IV-TR] criteria. The primary objective of the study as measured by improvement from Baseline in the irritability subscale of the Aberrant Behavior Checklist (ABC) at Endpoint (Week 6) was not met. A total of 149 patients were randomized to lurasidone hydrochloride or placebo. Vomiting occurred at a higher rate than reported in other lurasidone hydrochloride studies (4/49 or 8% for 20mg, 14/51 or 27% for 60mg, and 2/49 or 4% for placebo), particularly in children ages 6 to 12 (13 out of 18 patients on lurasidone hydrochloride with vomiting).
In a long-term, open-label study that enrolled pediatric patients (age 6 to 17 years) with schizophrenia, bipolar depression, or autistic disorder from three short-term, placebo-controlled trials, 54% (378/701) received lurasidone for 104 weeks. There was one adverse event in this trial that was considered possibly drug-related and has not been reported in adults receiving lurasidone: a 10 year old male experienced a prolonged, painful erection, consistent with priapism, that led to treatment discontinuation.
In this trial, the mean increase in height from open-label baseline to Week 104 was 4.94 cm. To adjust for normal growth, z-scores were derived (measured in standard deviations [SD]), which normalize for the natural growth of children and adolescents by comparisons to age- and sex-matched population standards. A z-score change <0.5 SD is considered not clinically significant. In this trial, the mean changein height z-score from open-label baseline to Week 104 was +0.05 SD, indicating minimal deviation from the normal growth curve.
Juvenile animal studies
Adverse effects were seen on growth, physical and neurobehavioral development at doses as low as 0.2 times the MRHD based on mg/m2. Lurasidone was orally administered to rats from postnatal days 21 through 91 (this period corresponds to childhood, adolescence, and young adulthood in humans) at doses of 3, 30, and 150 (males) or 300 (females) mg/kg/day which are 0.2 to 10 times (males) and 20 times (females) the maximum recommended adult human dose (MRHD) of 160 mg/day based on mg/m2. The adverse effects included dose-dependent decreases in femoral length, bone mineral content, body and brain weights at 2 times the MRHD in both sexes, and motor hyperactivity at 0.2 and 2 times the MRHD in both sexes based on mg/m2. In females, there was a delay in attainment of sexual maturity at 2 times the MRHD, associated with decreased serum estradiol. Mortality occurred in both sexes during early post-weaning period and some of the male weanlings died after only 4 treatments at doses as low as 2 times the MRHD based on mg/m2. Histopathological findings included increased colloid in the thyroids and inflammation of the prostate in males at 10 times MRHD based on mg/m2 and mammary gland hyperplasia, increased vaginal mucification, and increased ovarian atretic follicles at doses as low as 0.2 times the MRHD based on mg/m2. Some of these findings were attributed to transiently elevated serum prolactin which was seen in both sexes at all doses. However, there were no changes at any dose level in reproductive parameters (fertility, conception indices, spermatogenesis, estrous cycle, gestation length, parturition, number of pups born). The no effect dose for neurobehavioral changes in males is 0.2 times the MRHD based on mg/m2 and could not be determined in females. The no effect dose for growth and physical development in both sexes is 0.2 times the MRHD based on mg/m2.
8.5 Geriatric Use
Clinical studies with lurasidone hydrochloride did not include sufficient numbers of patients aged 65 and older to determine whether or not they respond differently from younger patients. In elderly patients with psychosis (65 to 85), lurasidone hydrochloride concentrations (20 mg/day) were similar to those in young subjects. It is unknown whether dose adjustment is necessary on the basis of age alone.
Elderly patients with dementia-related psychosis treated with lurasidone hydrochloride are at an increased risk of death compared to placebo. Lurasidone hydrochloride is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning, Warnings and Precautions (5.1, 5.3)].
8.6 Renal Impairment
Reduce the maximum recommended dosage in patients with moderate or severe renal impairment (CLcr<50 mL/minute). Patients with impaired renal function (CLcr<50 mL/minute) had higher exposure to lurasidone than patients with normal renal function [see Clinical Pharmacology (12.3)]. Greater exposure may increase the risk of lurasidone hydrochloride -associated adverse reactions [see Dosage and Administration (2.4)]
8.7 Hepatic Impairment
Reduce the maximum recommended dosage in patients with moderate to severe hepatic impairment (Child-Pugh score ≥7). Patients with moderate to severe hepatic impairment (Child- Pugh score ≥7) generally had higher exposure to lurasidone than patients with normal hepatic function [see Clinical Pharmacology (12.3)]. Greater exposure may increase the risk of lurasidone hydrochloride -associated adverse reactions [see Dosage and Administration (2.5)].
8.8 Other Specific Populations
No dosage adjustment for lurasidone hydrochloride is required on the basis of a patient’s sex, race, or smoking status [see Clinical Pharmacology (12.3)].
-
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
Lurasidone hydrochloride has not been systematically studied in humans for its potential for abuse or physical dependence or its ability to induce tolerance. While clinical studies with lurasidone hydrochloride did not reveal any tendency for drug-seeking behavior, these observations were not systematic and it is not possible to predict the extent to which a CNS-active drug will be misused, diverted and/or abused once it is marketed. Patients should be evaluated carefully for a history of drug abuse, and such patients should be observed carefully for signs of lurasidone hydrochloride misuse or abuse (e.g., development of tolerance, drug-seeking behavior, increases in dose).
-
10 OVERDOSAGE
10.1 Human Experience
In premarketing clinical studies, accidental or intentional overdosage of lurasidone hydrochloride was identified in one patient who ingested an estimated 560 mg of lurasidone hydrochloride. This patient recovered without sequelae. This patient resumed lurasidone hydrochloride treatment for an additional two months.
10.2 Management of Overdosage
No specific antidotes for lurasidone hydrochloride are known. In managing overdose, provide supportive care, including close medical supervision and monitoring, and consider the possibility of multiple drug involvement. If an overdose occurs, consult a Certified Poison Control Center (1-800-222-1222 or www. poison.org).
Cardiovascular monitoring should commence immediately, including continuous electrocardiographic monitoring for possible arrhythmias. If antiarrhythmic therapy is administered, disopyramide, procainamide, and quinidine carry a theoretical hazard of additive QT-prolonging effects when administered in patients with an acute overdose of lurasidone hydrochloride. Similarly, the alpha-blocking properties of bretylium might be additive to those of lurasidone hydrochloride, resulting in problematic hypotension.
Hypotension and circulatory collapse should be treated with appropriate measures. Epinephrine and dopamine should not be used, or other sympathomimetics with beta-agonist activity, since beta stimulation may worsen hypotension in the setting of lurasidone hydrochloride -induced alpha blockade. In case of severe extrapyramidal symptoms, anticholinergic medication should be administered.
Gastric lavage (after intubation if patient is unconscious) and administration of activated charcoal together with a laxative should be considered.
The possibility of obtundation, seizures, or dystonic reaction of the head and neck following overdose may create a risk of aspiration with induced emesis.
-
11 DESCRIPTION
Lurasidone hydrochloride is an atypical antipsychotic belonging to the chemical class of benzisothiazol derivatives.
Its chemical name is (3aR,4S,7R,7aS)-2-{(1R,2R)-2-[4-(1,2-benzisothiazol-3-yl)piperazin-1-ylmethyl] cyclohexylmethyl}hexahydro-4,7-methano-2H-isoindole-1,3-dione hydrochloride. Its molecular formula is C28H36N4O2SHCl and its molecular weight is 529.14.
The chemical structure is:
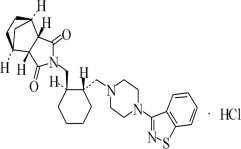
Lurasidone hydrochloride is a white to off-white powder. It is very slightly soluble in water, practically insoluble or insoluble in 0.1 N HCl, slightly soluble in ethanol, sparingly soluble in methanol, practically insoluble or insoluble in toluene and very slightly soluble in acetone.
Lurasidone hydrochloride tablets are intended for oral administration only. Each tablet contains 20 mg, 40 mg, 60 mg, 80 mg, or 120 mg of lurasidone hydrochloride.
Inactive ingredients are mannitol, pregelatinized starch, croscarmellose sodium, corn starch, hydroxy Propyl methyl cellulose, colloidal silicon dioxide, magnesium stearate, titanium dioxide, hypermellose, polyethelene glycol, polysorbate and additionally 80 mg tablets contains yellow iron oxide and FDC Blue #2/Indigotine Aluminum lake (12 to 14% dye).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of lurasidone in the treatment of schizophrenia and bipolar depression is unclear. However, its efficacy in schizophrenia and bipolar depression could be mediated through a combination of central dopamine D2 and serotonin Type 2 (5HT2A) receptor antagonism.
12.2 Pharmacodynamics
Lurasidone is an antagonist with high affinity binding at the dopamine D2 receptors (Ki of 1 nM) and the serotonin 5-HT2A (Ki of 0.5 nM) and 5-HT7 (Ki of 0.5 nM) receptors. It also binds with moderate affinity to the human α2C adrenergic receptors (Ki of 11 nM), is a partial agonist at serotonin 5-HT1A (Ki of 6.4 nM) receptors, and is an antagonist at the α2A adrenergic receptors (Ki of 41 nM). Lurasidone exhibits little or no affinity for histamine H1 and muscarinic M1 receptors (IC50 > 1,000 nM).
ECG Changes
The effects of lurasidone hydrochloride on the QTc interval were evaluated in a randomized, double-blind, multiple- dose, parallel-dedicated thorough QT study in 43 patients with schizophrenia or schizoaffective disorder, who were treated with lurasidone hydrochloride doses of 120 mg daily, 600 mg daily and completed the study. The maximum mean (upper 1-sided, 95% CI) increase in baseline-adjusted QTc intervals based on individual correction method (QTcI) was 7.5 (11.7) ms and 4.6 (9.5) ms, for the 120 mg and 600 mg dose groups respectively, observed at 2 to 4 hours after dosing. In this study, there was no apparent dose (exposure)-response relationship.
In short-term, placebo-controlled studies in schizophrenia and bipolar depression, no post-baseline QT prolongations exceeding 500 msec were reported in patients treated with lurasidone hydrochloride or placebo.
12.3 Pharmacokinetics
Adults
The activity of lurasidone hydrochloride is primarily due to the parent drug. The pharmacokinetics of lurasidone hydrochloride is dose-proportional within a total daily dose range of 20 mg to 160 mg. Steady-state concentrations of lurasidone hydrochloride are reached within 7 days of starting lurasidone hydrochloride.
Following administration of 40 mg of lurasidone hydrochloride, the mean (%CV) elimination half-life was 18 (7) hours.
Absorption and Distribution: Lurasidone hydrochloride is absorbed and reaches peak serum concentrations in approximately 1 to 3 hours. It is estimated that 9 to 19% of an administered dose is absorbed. Following administration of 40 mg of lurasidone hydrochloride, the mean (%CV) apparent volume of distribution was 6173 (17.2) L. lurasidone hydrochloride is highly bound (~99%) to serum proteins. In a food effect study, Lurasidone hydrochloride mean Cmax and AUC were about 3-times and 2-times, respectively, when administered with food compared to the levels observed under fasting conditions. Lurasidone hydrochloride exposure was not affected as meal size was increased from 350 to 1000 calories and was independent of meal fat content [see Dosage and Administration (2.3)].
In clinical studies, establishing the safety and efficacy of lurasidone hydrochloride, patients were instructed to take their daily dose with food [see Dosage and Administration (2.3)].
Metabolism and Elimination: Lurasidone hydrochloride is metabolized mainly via CYP3A4. The major biotransformation pathways are oxidative N-dealkylation, hydroxylation of norbornane ring, and S-oxidation. Lurasidone hydrochloride is metabolized into two active metabolites (ID-14283 and ID-14326) and two major non-active metabolites (ID-20219 and ID-20220). Based on in vitro studies, lurasidone hydrochloride is not a substrate of CYP1A1, CYP1A2, CYP2A6, CYP4A11, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6 or CYP2E1 enzymes. Because lurasidone hydrochloride is not a substrate for CYP1A2, smoking is not expected to have an effect on the pharmacokinetics of lurasidone hydrochloride. Transporter proteins: In vitro studies suggest lurasidone hydrochloride is not a substrate of OATP1B1 or OATP1B3, however, is probably a substrate of P-gp and BCRP. In vitro studies indicate that lurasidone hydrochloride is not expected to inhibit transporters OATP1B1, OATP1B3, OCT1, OCT2, OAT1, OAT3, MATE1, MATE2-K and BSEP at clinically relevant concentrations. Lurasidone hydrochloride is not a clinically significant inhibitor of P-gp. However, it may inhibit BCRP.
Total excretion of radioactivity in urine and feces combined was approximately 89%, with about 80% recovered in feces and 9% recovered in urine, after a single dose of [14C]-labeled lurasidone hydrochloride. Following administration of 40 mg of lurasidone hydrochloride, the mean (%CV) apparent clearance was 3902 (18.0) mL/min.
Drug Interaction Studies
Effects of other drugs on the exposure of lurasidone are summarized in Figure 5. A population PK analyses concluded that coadministration of lithium 300 to 2400 mg/day or valproate 300 to 2000 mg/day with lurasidone for up to 6 weeks has minimal effect on lurasidone exposure.
And the effects of lurasidone hydrochloride on the exposures of other drugs are summarized in Figure 2. A population PK analyses concluded that coadministration of lurasidone has minimal effect on lithium and valproate exposure when it is coadministered with lithium 300 to 2400 mg/day or valproate 300 to 2000 mg/day.
Figure 1: Impact of Other Drugs on Lurasidone Hydrochloride Pharmacokinetics
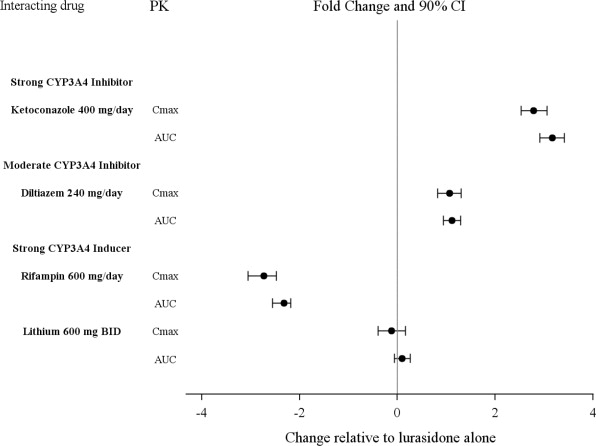
Figure 2: Impact of Lurasidone hydrochloride on Other Drugs
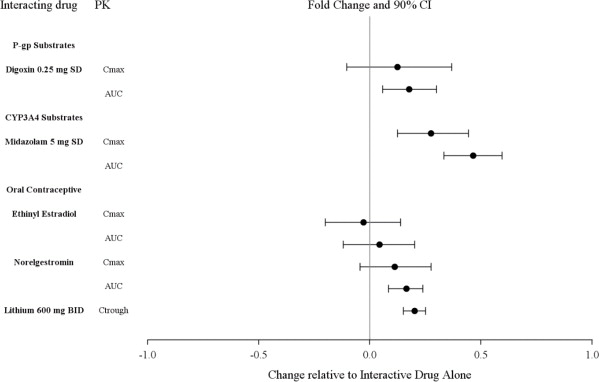
Studies in Specific Populations
The effect of intrinsic patient factors on the pharmacokinetics of lurasidone hydrochloride is presented in Figure 3.
Pediatric Patients
lurasidone hydrochloride exposure (i.e., steady-state Cmax and AUC) in children and adolescent patients (10 to 17 years of age) was generally similar to that in adults across the dose range from 40 to 160 mg, without adjusting for body weight.
Figure 3: Impact of Other Patient Factors on Lurasidone Hydrochloride Pharmacokinetics
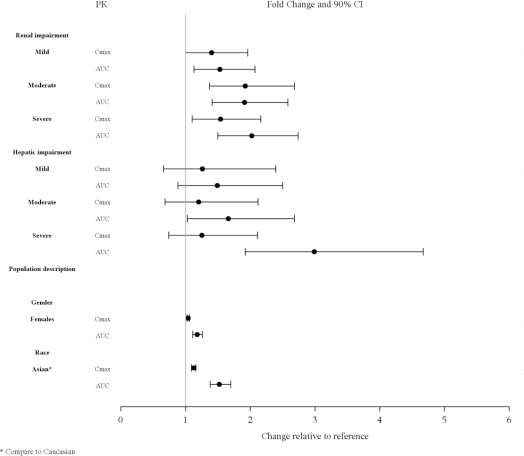
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis: Lurasidone increased incidences of malignant mammary gland tumors and pituitary gland adenomas in female mice orally dosed with 30, 100, 300, or 650 mg/kg/day. The lowest dose produced plasma levels (AUC) approximately equal to those in humans receiving the MRHD of 160 mg/day. No increases in tumors were seen in male mice up to the highest dose tested, which produced plasma levels (AUC) 14 times those in humans receiving the MRHD.
Lurasidone increased the incidence of mammary gland carcinomas in female rats orally dosed at 12 and 36 mg/kg/day: the lowest dose; 3 mg/kg/day is the no-effect dose which produced plasma levels (AUC) 0.4 times those in humans receiving the MRHD. No increases in tumors were seen in male rats up to the highest dose tested, which produced plasma levels (AUC) 6 times those in humans receiving the MRHD. Proliferative and/or neoplastic changes in the mammary and pituitary glands of rodents have been observed following chronic administration of antipsychotic drugs and are considered to be prolactin mediated [see Warnings and Precautions (5.7)].
Mutagenesis: Lurasidone did not cause mutation or chromosomal aberration when tested in vitro and in vivo test battery. Lurasidone was negative in the Ames gene mutation test, the Chinese Hamster Lung (CHL) cells, and in the in vivo mouse bone marrow micronucleus test up to 2000 mg/kg which is 61 times the MRHD of 160 mg/day based on mg/m2 body surface area.
Impairment of Fertility: Estrus cycle irregularities were seen in rats orally administered lurasidone at 1.5, 15 and 150 mg/kg/day for 15 consecutive days prior to mating, during the mating period, and through gestation day 7. No effect was seen at the lowest dose of 0.1 mg/kg which is approximately 0.006 times the MRHD of 160 mg/day based on mg/m2. Fertility was reduced only at the highest dose, which was reversible after a 14 day drug-free period. The no-effect dose for reduced fertility was approximately equal to the MRHD based on mg/m2.
Lurasidone had no effect on fertility in male rats treated orally for 64 consecutive days prior to mating and during the mating period at doses up to 9 times the MRHD based on mg/m2.
-
14 CLINICAL STUDIES
14.1 Schizophrenia
Adults
The efficacy of lurasidone hydrochloride for the treatment of schizophrenia was established in five short term (6- week), placebo-controlled studies in adult patients (mean age of 38.4 years, range 18 to 72) who met DSM-IV criteria for schizophrenia. An active-control arm (olanzapine or quetiapine extended-release) was included in two studies to assess assay sensitivity.
Several instruments were used for assessing psychiatric signs and symptoms in these studies:
- Positive and Negative Syndrome Scale (PANSS), is a multi-item inventory of general psychopathology used to evaluate the effects of drug treatment in schizophrenia. PANSS total scores may range from 30 to 210.
- Brief Psychiatric Rating Scale derived (BPRSd), derived from the PANSS, is a multi-item inventory primarily focusing on positive symptoms of schizophrenia, whereas the PANSS includes a wider range of positive, negative and other symptoms of schizophrenia. The BPRSd consists of 18 items rated on a scale of 1 (not present) to 7 (severe). BPRSd scores may range from 18 to 126.
- The Clinical Global Impression severity scale (CGI-S) is a clinician-rated scale that measures the subject’s current illness state on a 1- to 7-point scale.
The endpoint associated with each instrument is change from baseline in the total score to the end of week 6. These changes are then compared to placebo changes for the drug and control groups. The results of the studies follow:
- Study 1: In a 6-week, placebo-controlled trial (N=145) involving two fixed doses of lurasidone hydrochloride (40 or 120 mg/day), both doses of lurasidone hydrochloride at Endpoint were superior to placebo on the BPRSd total score, and the CGI-S.
- Study 2: In a 6-week, placebo-controlled trial (N=180) involving a fixed dose of lurasidone hydrochloride (80 mg/day), lurasidone hydrochloride at Endpoint was superior to placebo on the BPRSd total score, and the CGI-S.
- Study 3: In a 6-week, placebo- and active-controlled trial (N=473) involving two fixed doses of lurasidone hydrochloride (40 or 120 mg/day) and an active control (olanzapine), both lurasidone hydrochloride doses and the active control at Endpoint were superior to placebo on the PANSS total score, and the CGI-S.
- Study 4: In a 6-week, placebo-controlled trial (N=489) involving three fixed doses of lurasidone hydrochloride (40, 80 or 120 mg/day), only the 80 mg/day dose of lurasidone hydrochloride at Endpoint was superior to placebo on the PANSS total score, and the CGI-S.
- Study 5: In a 6-week, placebo- and active-controlled trial (N=482) involving two fixed doses of lurasidone hydrochloride (80 or 160 mg/day) and an active control (quetiapine extended-release), both lurasidone hydrochloride doses and the active control at Endpoint were superior to placebo on the PANSS total score, and the CGI-S.
Thus, the efficacy of lurasidone hydrochloride at doses of 40, 80, 120 and 160 mg/day has been established (Table 35).
Table 35: Primary Efficacy Results for Studies in Adult Patients with Schizophrenia (BPRSd or PANSS Scores)
SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: confidence interval, unadjusted for multiple comparisons.
a Difference (drug minus placebo) in least-squares mean change from baseline.
b Included for assay sensitivity.
* Doses statistically significantly superior to placebo.
Study Treatment Group Primary Efficacy Measure: BPRSd Mean Baseline Score (SD) LS Mean Change from Baseline (SE) Placebo-subtracted Differencea (95% CI) 1 Lurasidone (40 mg/day)* 54.2 (8.8) -9.4 (1.6) -5.6 (-9.8, -1.4) Lurasidone hydrochloride (120 mg/day)* 52.7 (7.6) -11.0 (1.6) -6.7 (-11.0, -2.5) Placebo 54.7 (8.1) -3.8 (1.6) – 2 Lurasidone (80 mg/day)* 55.1 (6.0) -8.9 (1.3) -4.7 (-8.3, -1.1) Placebo 56.1 (6.8) -4.2 (1.4) – Primary Efficacy Measure: PANSS 3 Lurasidone (40 mg/day)* 96.6 (10.7) -25.7 (2.0) -9.7 (-15.3, -4.1) Lurasidone hydrochloride (120 mg/day)* 97.9 (11.3) -23.6 (2.1) -7.5 (-13.4, -1.7) Olanzapine (15 mg/day)*b 96.3 (12.2) -28.7 (1.9) -12.6 (-18.2, -7.9) Placebo 95.8 (10.8) -16.0 (2.1) – 4 Lurasidone (40 mg/day) 96.5 (11.5) -19.2 (1.7) -2.1 (-7.0, 2.8) Lurasidone (80 mg/day)* 96.0 (10.8) -23.4 (1.8) -6.4 (-11.3, -1.5) Lurasidone (120 mg/day) 96.0 (9.7) -20.5 (1.8) -3.5 (-8.4, 1.4) Placebo 96.8 (11.1) -17.0 (1.8) – 5 Lurasidone (80 mg/day)* 97.7 (9.7) -22.2 (1.8) -11.9 (-16.9, -6.9) Lurasidone (160 mg/day)* 97.5 (11.8) -26.5 (1.8) -16.2 (-21.2, -11.2) Quetiapine Extended-release (600 mg/day)*b 97.7 (10.2) -27.8 (1.8) -17.5 (-22.5, -12.4) Placebo 96.6 (10.2) -10.3 (1.8) – Examination of population subgroups based on age (there were few patients over 65), gender and race did not reveal any clear evidence of differential responsiveness.
Adolescents (13-17 years)
The efficacy of lurasidone hydrochloride, was established in a 6-week, multicenter, randomized, double-blind, placebo-controlled study of adolescents (13 to 17 years) who met DSM-IV-TR criteria for schizophrenia (N=326). Patients were randomized to one of two fixed-doses of lurasidone hydrochloride (40 or 80 mg/day) or placebo.
The primary rating instrument used to assess psychiatric signs and symptoms was the PANSS. The key secondary instrument was the CGI-S.
For both dose groups, lurasidone hydrochloride was superior to placebo in reduction of PANSS and CGI-S scores at Week 6. On average, the 80 mg/day dose did not provide additional benefit compared to the 40 mg/day dose.
The primary efficacy results are provided in Table 36.
Table 36: Primary Efficacy Results (PANSS Total Score) for the Adolescent Schizophrenia Study
SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: confidence interval, unadjusted for multiple comparisons.
a Difference (drug minus placebo) in least-squares mean change from baseline.
* Doses statistically significantly superior to placebo.
Treatment Group Primary Efficacy Measure: PANSS Mean Baseline Score (SD) LS Mean Change from Baseline (SE) Placebo-subtracted Differencea(95% CI) Lurasidone (40 mg/day)* 94.5 (10.97) -18.6 (1.59) -8.0 (-12.4, -3.7) Lurasidone (80 mg/day)* 94.0 (11.12) -18.3 (1.60) -7.7 (-12.1, -3.4) Placebo 92.8 (11.08) -10.5 (1.59) – 14.2 Depressive Episodes Associated with Bipolar I Disorder
Adults
Monotherapy
The efficacy of lurasidone hydrochloride, as monotherapy, was established in a 6-week, multicenter, randomized, double-blind, placebo-controlled study of adult patients (mean age of 41.5 years, range 18 to 74) who met DSM-IV-TR criteria for major depressive episodes associated with bipolar I disorder, with or without rapid cycling, and without psychotic features (N=485). Patients were randomized to one of two flexible-dose ranges of lurasidone hydrochloride (20 to 60 mg/day, or 80 to 120 mg/day) or placebo. The primary rating instrument used to assess depressive symptoms in this study was the Montgomery Asberg Depression Rating Scale (MADRS), a 10-item clinician-rated scale with total scores ranging from 0 (no depressive features) to 60 (maximum score). The primary endpoint was the change from baseline in MADRS score at Week 6. The key secondary instrument was the Clinical Global Impression-Bipolar Severity of Illness scale (CGI-BP-S), a clinician-rated scale that measures the subject’s current illness state on a 7-point scale, where a higher score is associated with greater illness severity.
For both dose groups, lurasidone hydrochloride was superior to placebo in reduction of MADRS and CGI-BP-S scores at Week 6. The primary efficacy results are provided in Table 37. The high dose range (80 to 120 mg per day) did not provide additional efficacy on average, compared to the low dose range (20 to 60 mg per day).
Adjunctive Therapy with Lithium or Valproate
The efficacy of lurasidone hydrochloride, as an adjunctive therapy with lithium or valproate, was established in a 6-week, multicenter, randomized, double-blind, placebo-controlled study of adult patients (mean age of 41.7 years, range 18 to 72) who met DSM-IV-TR criteria for major depressive episodes associated with bipolar I disorder, with or without rapid cycling, and without psychotic features (N=340). Patients who remained symptomatic after treatment with lithium or valproate were randomized to flexibly dosed lurasidone hydrochloride 20 to 120 mg/day or placebo.
The primary rating instrument used to assess depressive symptoms in this study was the MADRS. The primary endpoint was the change from baseline in MADRS score at Week 6. The key secondary instrument was the CGI-BP-S scale.
Lurasidone hydrochloride was superior to placebo in reduction of MADRS and CGI-BP-S scores at Week 6, as an adjunctive therapy with lithium or valproate (Table 37).
Table 37: Primary Efficacy Results for Adult Studies in Depressive Episodes Associated with Bipolar I Disorder (MADRS Scores)
SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: confidence interval, unadjusted for multiple comparisons.
a Difference (drug minus placebo) in least-squares mean change from baseline.
* Treatment group statistically significantly superior to placebo.
Study Treatment Group Primary Efficacy Measure: MADRS Mean Baseline Score (SD) LS Mean Change from Baseline (SE) Placebo-subtracted Differencea (95% CI) Monotherapy study Lurasidone (20-60 mg/day)* 30.3 (5.0) -15.4 (0.8) -4.6 (-6.9, -2.3) Lurasidone (80-120 mg/day)* 30.6 (4.9) -15.4 (0.8) -4.6 (-6.9, -2.3) Placebo 30.5 (5.0) -10.7 (0.8) – Adjunctive Therapy study Lurasidone (20-120 mg/day)* + lithium or valproate 30.6 (5.3) -17.1 (0.9) -3.6 (-6.0, -1.1) Placebo + lithium or valproate 30.8 (4.8) -13.5 (0.9) – Pediatric Patients (10 to 17 years)
The efficacy of Lurasidone hydrochloride was established in a 6-week, multicenter, randomized, double blind, placebo-controlled study of pediatric patients (10 to 17 years) who met DSM-5 criteria for a major depressive episode associated with bipolar I disorder, with or without rapid cycling, and without psychotic features (N=343). Patients were randomized to flexibly dosed Lurasidone hydrochloride 20 to 80 mg/ day or placebo. At the end of the clinical study, most patients (67%) received 20 mg/day or 40 mg/day.
The primary rating scale used to assess depressive symptoms in this study was the Children’s Depression Rating Scale, Revised (CDRS-R) total score. The CDRS-R is a 17-item clinician-rated scale with total scores ranging from 17 to 113. The primary endpoint was the change from baseline in CDRS-R score at Week 6. The key secondary endpoint was the change from baseline in CGI BP-S depression score.
Lurasidone hydrochloride was superior to placebo in reduction of CDRS-R total score and CGI-BP-S depression score at Week 6. The primary efficacy results are provided in Table 38.
Table 38: Primary Efficacy Results for the Study in Depressive Episodes Associated with Bipolar I Disorder (CDRS-R Total Score) in Pediatric Patients (10 to 17 years)
SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: confidence interval, unadjusted for multiple comparisons.
a Difference (drug minus placebo) in least-squares mean change from baseline.
* Treatment group statistically significantly superior to placebo.
Treatment Group Primary Efficacy Measure: CDRS-R Mean Baseline Score (SD) LS Mean Change from Baseline (SE) Placebo-subtracted Differencea (95% CI) Lurasidone (20 to 80 mg/day)* 59.2 (8.24) -21.0 (1.06) -5.7 (-8.4, -3.0) Placebo 58.6 (8.26) -15.3 (1.08) – -
16 HOW SUPPLIED/STORAGE AND HANDLING
Lurasidone hydrochloride tablets 20 mg are White to off-white, Round, biconvex film-coated tablets de-bossed with IG on one side and 522 on the other side.
Lurasidone hydrochloride tablets 40 mg are White to off-white, Round, biconvex film-coated tablets de-bossed with IG on one side and 523 on the other side.
Lurasidone hydrochloride tablets 60 mg are White to off-white, Oval biconvex film-coated tablets de-bossed with IG on one side and 534 on the other side.
Lurasidone hydrochloride tablets 80 mg are Pale green, Oval biconvex film-coated tablets de-bossed with IG on one side and 524 on the other side.
Lurasidone hydrochloride tablets 120 mg are White to off-white, capsule shaped biconvex film-coated tablets de Bossed with IG on one side and 525 on the other side.Tablets are supplied in the following strengths and package configurations (Table 39).
Table 39: Package Configuration for Lurasidone hydrochloride Tablets
Tablet Strength Package Configuration NDC Code 20 mg Bottles of 30 76282-522-30 40 mg Bottles of 30 76282-523-30 60 mg Bottles of 30 76282-534-30 80 mg Bottles of 30 76282-524-30 120 mg Bottles of 30 76282-525-30 Storage
Store lurasidone hydrochloride tablets at 20°C to 25°C (68°F to 77°F) [See USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Suicidal Thoughts and Behavior
Advise patients and caregivers to look for the emergence of suicidality, especially early during treatment and when the dosage is adjusted up or down and instruct them to report such symptoms to the healthcare provider [see Boxed Warning, Warnings and Precautions (5.2)].
Neuroleptic Malignant Syndrome
Counsel patients about a potentially fatal adverse reaction referred to as Neuroleptic Malignant Syndrome (NMS). Advise patients, family members, or caregivers to contact healthcare provider or to report to the emergency room if they experience signs and symptoms of NMS [see Warnings and Precautions (5.4)].
Tardive Dyskinesia
Counsel patients on the signs and symptoms of tardive dyskinesia and to contact their healthcare provider if these abnormal movements occur [see Warnings and Precautions (5.5)].
Metabolic Changes
Educate patients about the risk of metabolic changes, how to recognize symptoms of hyperglycemia and diabetes mellitus, and the need for specific monitoring, including blood glucose, lipids, and weight [see Warnings and Precautions (5.6)].
Hyperprolactinemia
Counsel patients on signs and symptoms of hyperprolactinemia that may be associated with chronic use of lurasidone hydrochloride. Advise them to seek medical attention if they experience any of the following: amenorrhea or galactorrhea in females, erectile dysfunction or gynecomastia in males [see Warnings and Precautions (5.7)].
Leukopenia/Neutropenia
Advise patients with a pre-existing low WBC or a history of drug-induced leukopenia/neutropenia that they should have their CBC monitored while taking lurasidone hydrochloride [see Warnings and Precautions (5.8)].
Orthostatic Hypotension
Educate patients about the risk of orthostatic hypotension, particularly at the time of initiating treatment, re-initiating treatment, or increasing the dose [see Warnings and Precautions (5.9)].
Interference with Cognitive and Motor Performance
Caution patients about performing activities requiring mental alertness, such as operating hazardous machinery or operating a motor vehicle, until they are reasonably certain that lurasidone hydrochloride therapy does not affect them adversely [see Warnings and Precautions (5.12)].
Heat Exposure and Dehydration
Educate patients regarding appropriate care in avoiding overheating and dehydration [see Warnings and Precautions (5.13)]
Activation of Mania or Hypomania
Advise patients and their caregivers to observe for signs of activation of mania/hypomania [see Warnings and Precautions (5.14)].
Concomitant Medication
Advise patients to inform their physicians if they are taking, or plan to take, any prescription or over-the counter drugs, because there is a potential for drug interactions [see Drug Interactions (7)].
Pregnancy
Advise patients that lurasidone hydrochloride may cause extrapyramidal and/or withdrawal symptoms in a neonate. Advise patients to notify their healthcare provider with a known or suspected pregnancy [see Use in Specific Populations (8.1)]. Advise patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to lurasidone hydrochloride during pregnancy [see Use in Specific Populations (8.1)].
Revised: 03/2025
-
MEDICATION GUIDE
This Medication Guide has been approved by the U.S. Food and Drug Administration
Revised: 03/2025
MEDICATION GUIDE
Lurasidone hydrochloride tablets
loo-RAS-i-done HYE-droe-KLOR-ideWhat is the most important information I should know about lurasidone hydrochloride?
Lurasidone hydrochloride may cause serious side effects, including:- Increased risk of death in elderly people with dementia-related psychosis. Medicines like lurasidone hydrochloride can raise the risk of death in elderly people who have lost touch with reality (psychosis) due to confusion and memory loss (dementia). Lurasidone hydrochloride is not approved for the treatment of people with dementia-related psychosis.
- Increased risk of suicidal thoughts or actions in children and young adults.Antidepressant medicines may increase suicidal thoughts or actions in some children and young adults within the first few months of treatment and when the dose is changed.
- Depression and other serious mental illnesses are the most important causes of suicidal thoughts and actions. Some people may have a particularly high risk of having suicidal thoughts or actions. These include people who have (or have a family history of) depression, bipolar illness (also called manic-depressive illness), or a history of suicidal thoughts or actions.
How can I watch for and try to prevent suicidal thoughts and actions in myself or a family member?
- Pay close attention to any changes, especially sudden changes in mood, behaviors, thoughts, or feelings. This is very important when an antidepressant medicine is started or when the dose is changed.
- Call the healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings.
- Keep all follow-up visits with the healthcare provider as scheduled. Call the healthcare provider between visits as needed, especially if you have concerns about symptoms.
- Call a healthcare provider right away if you or your family member has any of the following symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling very agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
What is lurasidone hydrochloride?
Lurasidone hydrochloride is a prescription medicine used:
- To treat people 13 years of age or older with schizophrenia.
- Alone to treat people 10 years of age and older with depressive episodes that happen with Bipolar I Disorder (bipolar depression).
- With the medicine lithium or valproate to treat adults with depressive episodes that happen with Bipolar I Disorder (bipolar depression).
It is not known if lurasidone hydrochloride is safe and effective in children:
- less than 13 years of age with schizophrenia.
- less than 10 years of age with bipolar depression.
- for the treatment of irritability associated with autistic disorder.
Do not take lurasidone hydrochloride if you are:
- allergic to lurasidone hydrochloride or any of the ingredients in lurasidone hydrochloride tablets. See the end of this Medication Guide for a complete list of ingredients in Lurasidone hydrochloride tablets.
- taking certain other medicines called CYP3A4 inhibitors or inducers including ketoconazole, clarithromycin, ritonavir, voriconazole, mibefradil, rifampin, avasimibe, St. John's wort, phenytoin, or carbamazepine. Ask your healthcare provider if you are not sure if you are taking any of these medicines.
Before taking lurasidone hydrochloride, tell your healthcare provider about all of your medical conditions, including if you:
- have or have had heart problems or stroke
- have or have had low or high blood pressure
- haave or have had diabetes or high blood sugar, or have a family history of diabetes or high blood sugar.
- have or have had high levels of total cholesterol or triglycerides
- have or have had high levels of total cholesterol or triglycerides
- have or have had high prolactin levels
- have or have had low white blood cell count
- have or have had seizures
- have or have had kidney or liver problems
- are pregnant or plan to become pregnant. It is not known if lurasidone hydrochloride will harm your unborn baby. Talk to your healthcare provider about the risk to your unborn baby if you take lurasidone hydrochloride during pregnancy.
- Tell your healthcare provider if you become pregnant or think you are pregnant during treatment with lurasidone hydrochloride
- If you become pregnant during treatment with lurasidone hydrochloride, talk to your healthcare provider about registering with the National Pregnancy Registry for Atypical Antipsychotics. You can register by calling 1-866-961-2388 or go to http://womensmentalhealth.org/clinical-and-researchprograms/pregnancyregistry/.
- are breastfeeding or plan to breastfeed. It is not known if lurasidone hydrochloride passes into your breast milk. Talk to your healthcare provider about the best way to feed your baby during treatment with lurasidone hydrochloride.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Lurasidone hydrochloride and other medicines may affect each other causing possible serious side effects.
Lurasidone hydrochloride may affect the way other medicines work, and other medicines may affect how Lurasidone hydrochloride works.
Your healthcare provider can tell you if it is safe to take Lurasidone hydrochloride with your other medicines. Do not start or stop any other medicines during treatment with lurasidone hydrochloride without talking to your healthcare provider first.
Know the medicines you take. Keep a list of your medicines to show your healthcare provider and pharmacist when you get a new medicine.How should I take Lurasidone hydrochloride?
- Take lurasidone hydrochloride exactly as your healthcare provider tells you to take it. Do not change the dose or stop taking lurasidone hydrochloride without first talking to your healthcare provider.
- Take lurasidone hydrochloride by mouth, with food (at least 350 calories).
- If you take too much lurasidone hydrochloride, call your healthcare provider or poison control center or go to the nearest hospital emergency room right away.
What should I avoid while taking lurasidone hydrochloride?
- Do not drive, operate heavy machinery, or do other dangerous activities until you know how lurasidone hydrochloride affects you. Lurasidone hydrochloride may make you drowsy.
- Avoid eating grapefruit or drinking grapefruit juice during treatment with lurasidone hydrochloride. Grapefruit and grapefruit juice may affect the amount of lurasidone hydrochloride in your blood.
- Do not become too hot or dehydrated during treatment with lurasidone hydrochloride.
- Do not exercise too much.
- In hot weather, stay inside in a cool place if possible.
- Stay out of the sun.
- Do not wear too much clothing or heavy clothing.
- Drink plenty of water.
What are the possible side effects of Lurasidone hydrochloride?
Lurasidone hydrochloride may cause serious side effects, including:
- See “What is the most important information I should know about lurasidone hydrochloride?”
- Stroke (cerebrovascular problems) in elderly people with dementia-related psychosis that can lead to death.
- Neuroleptic malignant syndrome (NMS) a serious condition that can lead to death. Call your healthcare provider or go to the nearest hospital emergency room right away if you have some or all of the following signs and symptoms of NMS:
- high fever
- stiff muscles
- confusion
- increased sweating
- changes in your breathing, heart rate, and blood pressure
- Uncontrolled body movements (tardive dyskinesia). Lurasidone hydrochloride may cause movements that you cannot control in your face, tongue, or other body parts. Tardive dyskinesia may not go away, even if you stop taking lurasidone hydrochloride. Tardive dyskinesia may also start after you stop taking lurasidone hydrochloride.
-
Problems with your metabolism such as:
- high blood sugar (hyperglycemia) and diabetes. Increases in blood sugar can happen in some people who take lurasidone hydrochloride. Extremely high blood sugar can lead to coma or death. If you have diabetes or risk factors for diabetes (such as being overweight or a family history of diabetes), your healthcare provider should check your blood sugar before you start and during treatment with lurasidone hydrochloride.
Call your healthcare provider if you have any of these symptoms of high blood sugar during treatment with lurasidone hydrochloride:
- feel very thirsty
- feel very hungry
- feel sick to your stomach
- need to urinate more than usual
- feel weak or tired
- feel confused, or your breath smells fruity
- increased fat levels (cholesterol and triglycerides) in your blood.
- weight gain. You and your healthcare provider should check your weight regularly during treatment with lurasidone hydrochloride.
-
Increased prolactin levels in your blood (hyperprolactinemia).Your healthcare provider may do blood tests to check your prolactin levels during treatment with lurasidone hydrochloride. Tell your healthcare provider if you have any of the following signs and symptoms of hyperprolactinemia:
Females:
- absence of your menstrual cycle
- secretion of breast milk when you are not breastfeeding
Males:
- problems getting or maintaining an erection (erectile dysfunction)
- enlargement of breasts (gynecomastia)
- Low white blood cell count. Your healthcare provider may do blood tests during the first few months of treatment with lurasidone hydrochloride
- Decreased blood pressure (orthostatic hypotension). You may feel lightheaded or faint when you rise too quickly from a sitting or lying position.
- Falls. Lurasidone hydrochloride may make you sleepy or dizzy, may cause a decrease in your blood pressure when changing position (orthostatic hypotension), and can slow your thinking and motor skills which may lead to falls that can cause fractures or other injuries.
- Seizures (convulsions)
- Problems controlling your body temperature so that you feel too warm. See “What should I avoid while taking lurasidone hydrochloride?”
- Mania or hypomania (manic episodes) in people with a history of bipolar disorder. Symptoms may include:
- greatly increased energy
- racing thoughts
- unusually grand ideas
- talking more or faster than usual
- severe problems sleeping
- reckless behavior
- excessive happiness or irritability
- Difficulty swallowing
The most common side effects of lurasidone hydrochloride include:
-
Adults with schizophrenia:
- sleepiness or drowsiness
- restlessness and feeling like you need to move around (akathisia)
- difficulty moving, slow movements, muscle stiffness, or tremor
- nausea
-
Children 13 to 17 years of age with schizophrenia:
- sleepiness or drowsiness
- nausea
- restlessness and feeling like you need to move around (akathisia)
- difficulty moving, slow movements, muscle stiffness, or tremor
- runny nose
- vomiting
-
Adults with bipolar depression:
- restlessness and feeling like you need to move around (akathisia)
- difficulty moving, slow movements, muscle stiffness, or tremor
- sleepiness or drowsiness
-
Children 10 to 17 years of age with bipolar depression:
- nausea
- weight gain
- problems sleeping (insomnia)
These are not all of the possible side effects of lurasidone hydrochloride.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store lurasidone hydrochloride?
- Store lurasidone hydrochloride tablets at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep lurasidone hydrochloride and all medicines out of the reach of children.
General information about the safe and effective use of lurasidone hydrochloride.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use lurasidone hydrochloride for a condition for which it was not prescribed. Do not give lurasidone hydrochloride to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about lurasidone hydrochloride that is written for health professionals.What are the ingredients in lurasidone hydrochloride?
Active ingredient: Lurasidone hydrochloride
Inactive ingredients: mannitol, pregelatinized starch, croscarmellose sodium, corn starch, hydroxy Propyl methyl cellulose, colloidal silicon dioxide, magnesium stearate, titanium dioxide, hypermellose, polyethelene glycol, polysorbate and additionally 80 mg tablet contains yellow iron oxide and FDC Blue #2/Indigotine Aluminum lake (12 to 14% dye).
For more information, please call Exelan Pharmaceuticals, Inc. at 1-866-604-3268.
Manufactured by:
InvaGen Pharmaceuticals, Inc.
(a subsidiary of Cipla Ltd.)
Hauppauge, NY 11788
Manufactured for:
Exelan Pharmaceuticals Inc.
Boca Raton, FL 33432 -
PRINCIPAL DISPLAY PANEL
NDC: 76282-522-30
Lurasidone Hydrochloride Tablets
20 mg
30 Tablets
Rx Only
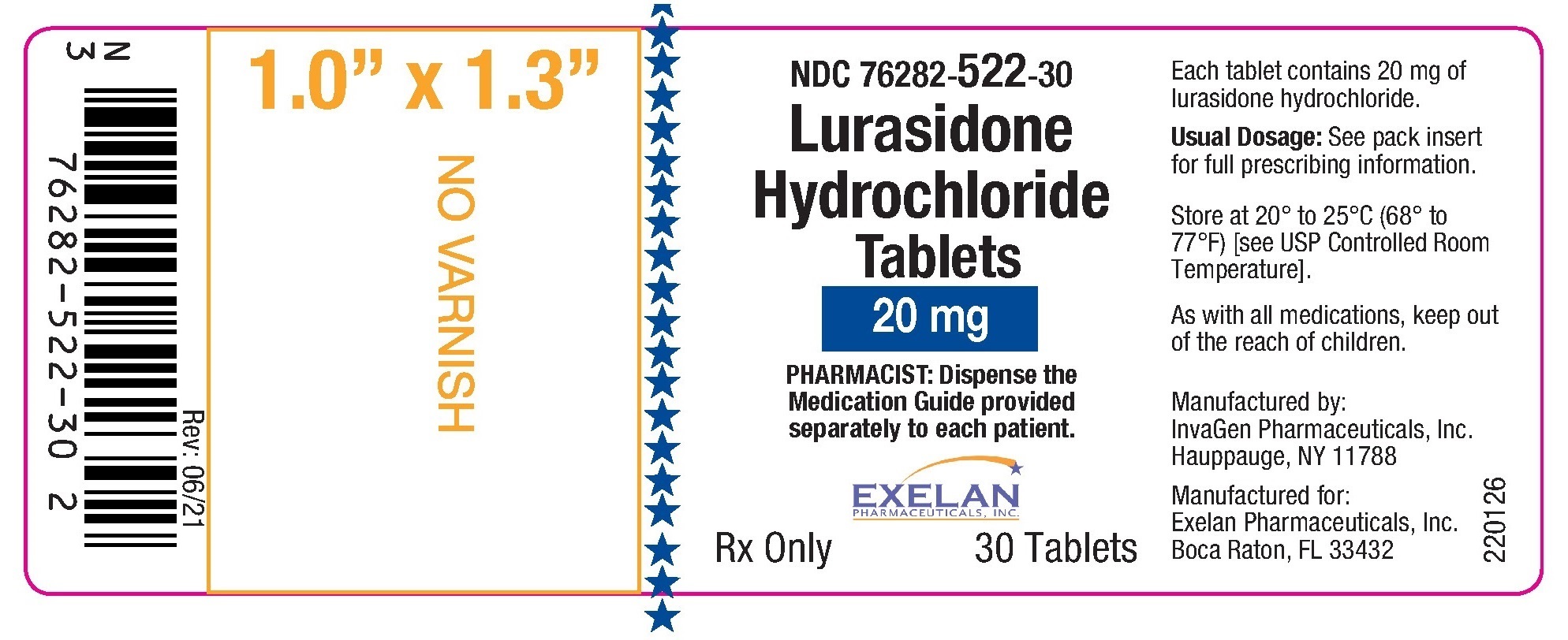
NDC: 76282-523-30
Lurasidone Hydrochloride Tablets
40 mg
30 Tablets
Rx Only
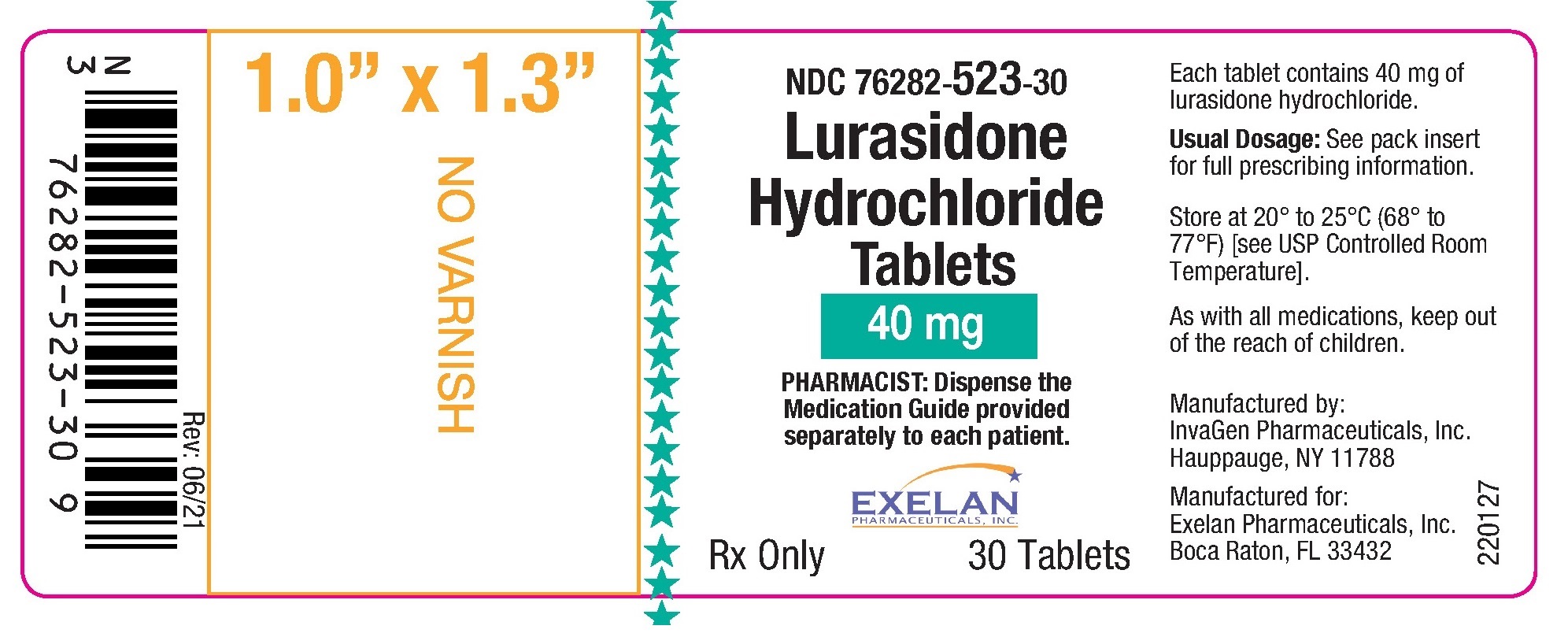
NDC: 76282-534-30
Lurasidone Hydrochloride Tablets
60 mg
30 Tablets
Rx Only
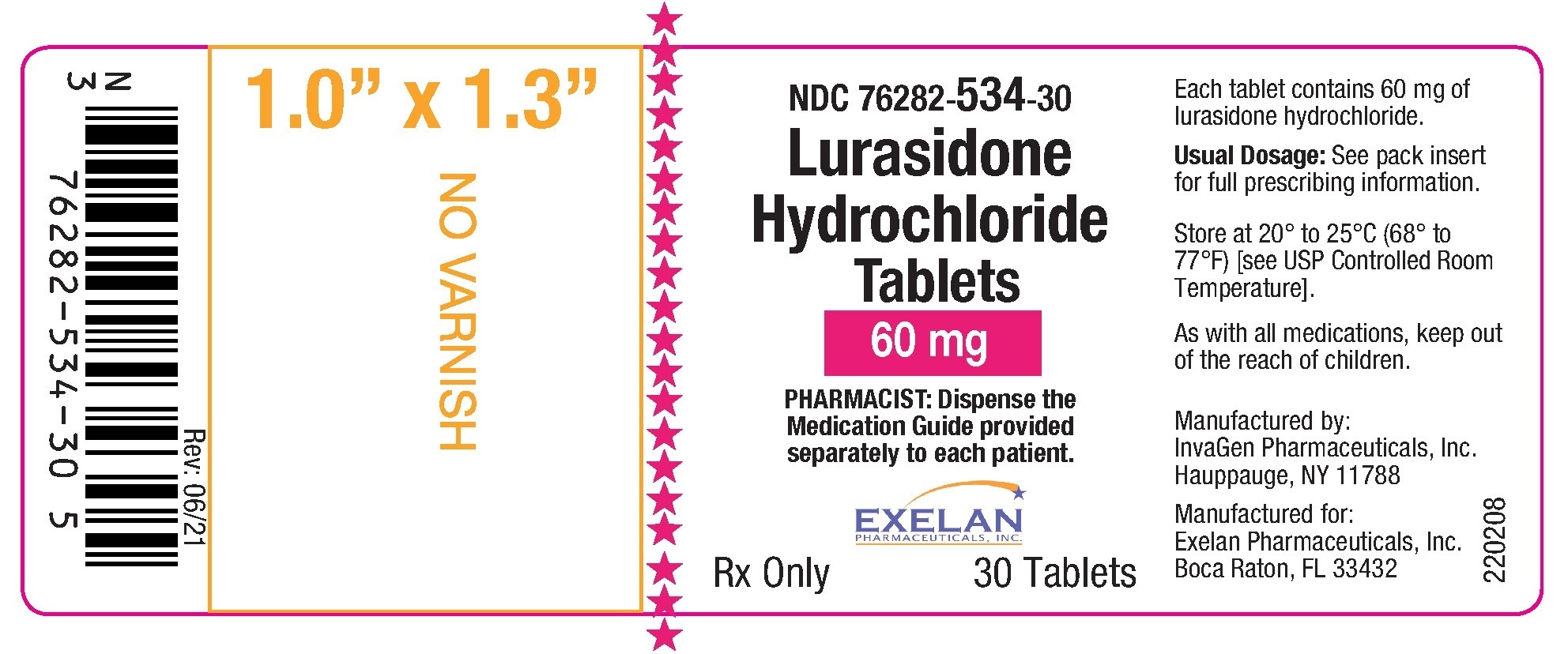
NDC: 76282-524-30
Lurasidone Hydrochloride Tablets
80 mg
30 Tablets
Rx Only
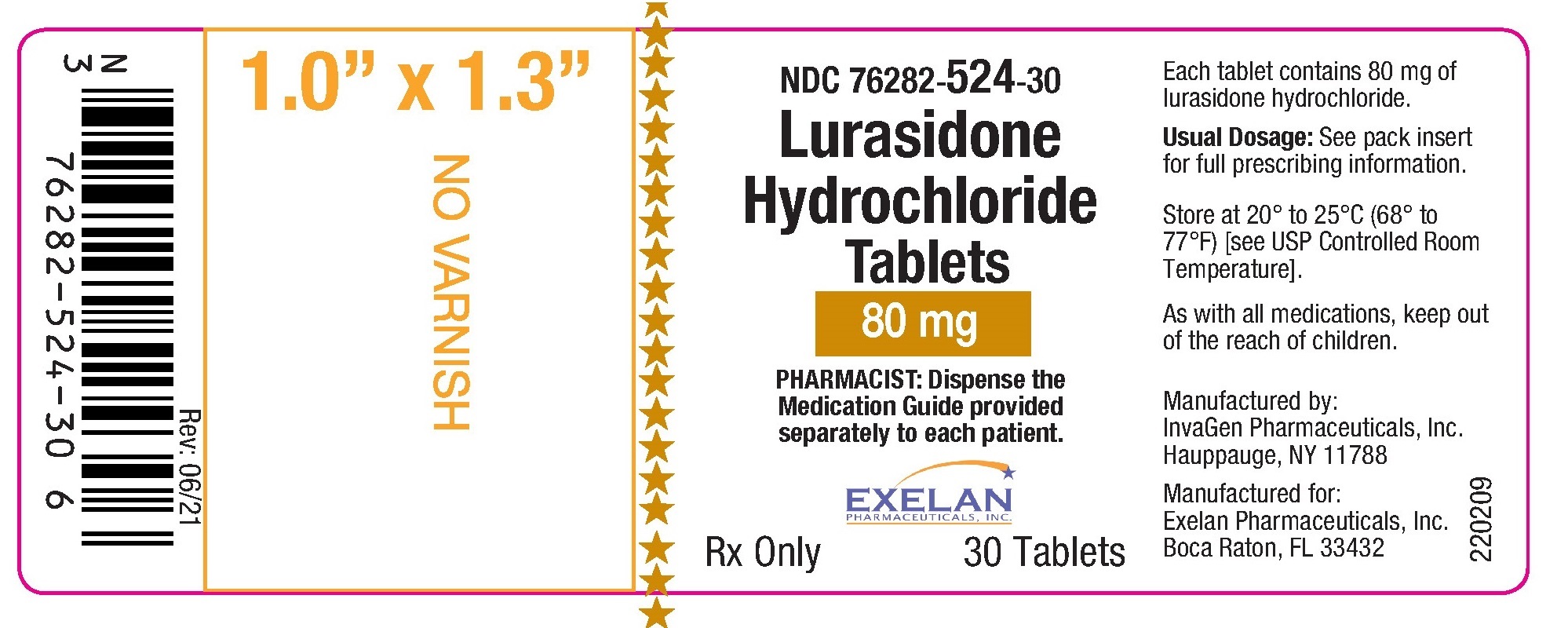
NDC: 76282-525-30
Lurasidone Hydrochloride Tablets
120 mg
30 Tablets
Rx Only
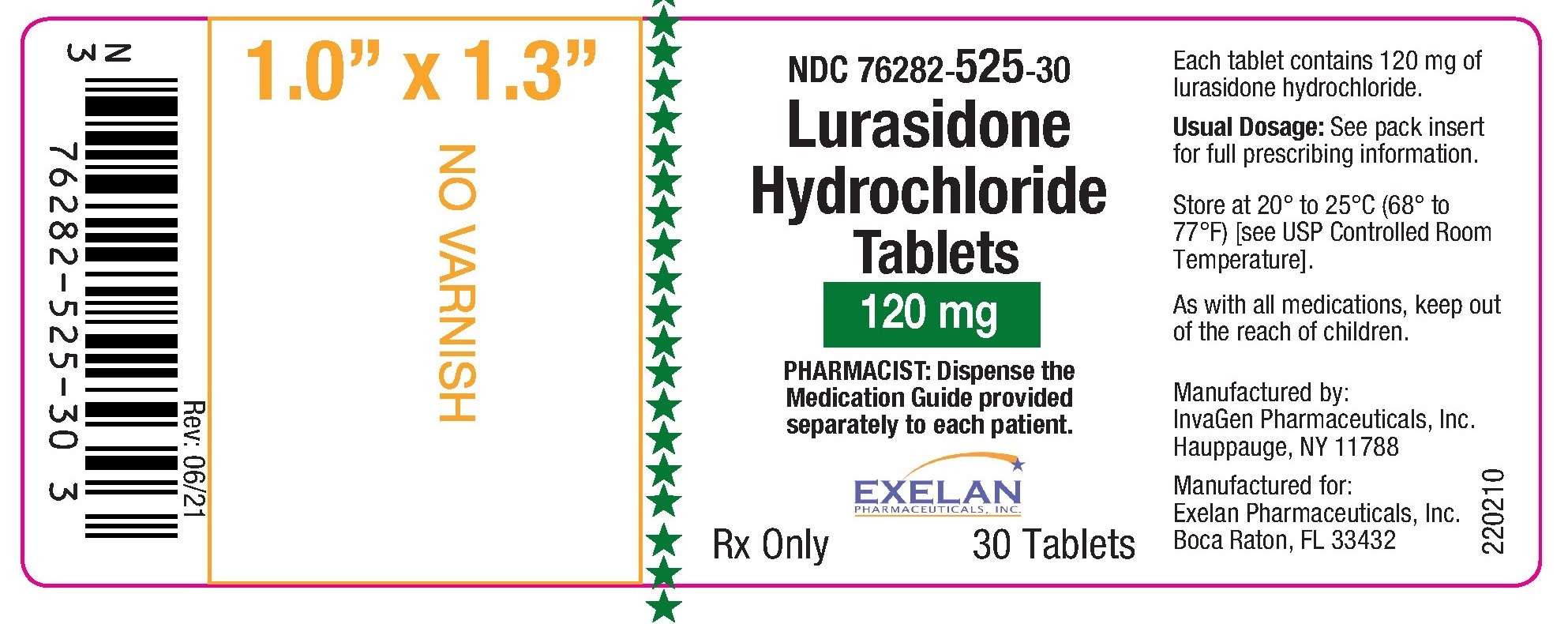
-
INGREDIENTS AND APPEARANCE
LURASIDONE HYDROCHLORIDE
lurasidone hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 76282-522 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LURASIDONE HYDROCHLORIDE (UNII: O0P4I5851I) (LURASIDONE - UNII:22IC88528T) LURASIDONE HYDROCHLORIDE 20 mg Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) STARCH, CORN (UNII: O8232NY3SJ) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLAWAX POLYSORBATE (UNII: Q504PL8E0V) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color white (White to off-white) Score no score Shape ROUND (ROUND) Size 6mm Flavor Imprint Code IG;522 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 76282-522-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 02/20/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA208028 02/20/2023 LURASIDONE HYDROCHLORIDE
lurasidone hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 76282-523 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LURASIDONE HYDROCHLORIDE (UNII: O0P4I5851I) (LURASIDONE - UNII:22IC88528T) LURASIDONE HYDROCHLORIDE 40 mg Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) STARCH, CORN (UNII: O8232NY3SJ) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLAWAX POLYSORBATE (UNII: Q504PL8E0V) Product Characteristics Color white (White to off-white) Score no score Shape ROUND (ROUND) Size 8mm Flavor Imprint Code IG;523 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 76282-523-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 02/20/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA208028 02/20/2023 LURASIDONE HYDROCHLORIDE
lurasidone hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 76282-534 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength lurasidone hydrochloride (UNII: O0P4I5851I) (lurasidone - UNII:22IC88528T) lurasidone hydrochloride 60 mg Inactive Ingredients Ingredient Name Strength mannitol (UNII: 3OWL53L36A) starch, corn (UNII: O8232NY3SJ) croscarmellose sodium (UNII: M28OL1HH48) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) magnesium stearate (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLAWAX POLYSORBATE (UNII: Q504PL8E0V) Product Characteristics Color white (White to off-white) Score no score Shape OVAL (Oval biconvex) Size 13mm Flavor Imprint Code IG;534 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 76282-534-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 02/20/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA208028 02/20/2023 LURASIDONE HYDROCHLORIDE
lurasidone hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 76282-524 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LURASIDONE HYDROCHLORIDE (UNII: O0P4I5851I) (LURASIDONE - UNII:22IC88528T) LURASIDONE HYDROCHLORIDE 80 mg Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) STARCH, CORN (UNII: O8232NY3SJ) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLAWAX POLYSORBATE (UNII: Q504PL8E0V) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FD&C BLUE NO. 2 ALUMINUM LAKE (UNII: 4AQJ3LG584) Product Characteristics Color green (Pale green) Score no score Shape OVAL (Oval biconvex) Size 14mm Flavor Imprint Code IG;524 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 76282-524-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 02/20/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA208028 02/20/2023 LURASIDONE HYDROCHLORIDE
lurasidone hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 76282-525 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LURASIDONE HYDROCHLORIDE (UNII: O0P4I5851I) (LURASIDONE - UNII:22IC88528T) LURASIDONE HYDROCHLORIDE 120 mg Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) STARCH, CORN (UNII: O8232NY3SJ) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLAWAX POLYSORBATE (UNII: Q504PL8E0V) Product Characteristics Color white (White to off-white) Score no score Shape CAPSULE (capsule shaped biconvex) Size 16mm Flavor Imprint Code IG;525 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 76282-525-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 02/20/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA208028 02/20/2023 Labeler - Exelan Pharmaceuticals Inc. (967795266) Registrant - InvaGen Pharmaceuticals, Inc (165104469) Establishment Name Address ID/FEI Business Operations InvaGen Pharmaceuticals, Inc 165104469 analysis(76282-523, 76282-534, 76282-525) , manufacture(76282-522, 76282-524) Establishment Name Address ID/FEI Business Operations InvaGen Pharmaceuticals, Inc 080334903 analysis(76282-523, 76282-534, 76282-525) , pack(76282-522, 76282-524)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.