ZOLPIDEM TARTRATE tablet, film coated
Zolpidem Tartrate by
Drug Labeling and Warnings
Zolpidem Tartrate by is a Prescription medication manufactured, distributed, or labeled by NuCare Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ZOLPIDEM TARTRATE TABLETS safely and effectively. See full prescribing information for ZOLPIDEM TARTRATE TABLETS.
ZOLPIDEM TARTRATE tablets, for oral use CIV
Initial U.S. Approval: 1992RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Zolpidem tartrate tablets, a gamma-aminobutyric acid (GABA) A agonist, are indicated for the short-term treatment of insomnia characterized by difficulties with sleep initiation. ( 1)
DOSAGE AND ADMINISTRATION
- Use the lowest dose effective for the patient and must not exceed a total of 10 mg daily ( 2.1)
- Recommended initial dose is a single dose of 5 mg for women and a single dose of 5 or 10 mg for men, immediately before bedtime with at least 7 to 8 hours remaining before the planned time of awakening ( 2.1)
- Geriatric patients and patients with hepatic impairment: Recommended dose is 5 mg for men and women ( 2.2)
- Lower doses of CNS depressants may be necessary when taken concomitantly with zolpidem tartrate tablets ( 2.3)
- The effect of zolpidem tartrate tablets may be slowed if taken with or immediately after a meal ( 2.4)
DOSAGE FORMS AND STRENGTHS
5 mg and 10 mg tablets. Tablets not scored. ( 3)
CONTRAINDICATIONS
Known hypersensitivity to zolpidem ( 4)
WARNINGS AND PRECAUTIONS
- CNS depressant effects: Impairs alertness and motor coordination. Instruct patients on correct use. ( 5.1)
- Need to evaluate for co-morbid diagnosis: Reevaluate if insomnia persists after 7 to 10 days of use. ( 5.2)
- Severe anaphylactic/anaphylactoid reactions: Angioedema and anaphylaxis have been reported. Do not rechallenge if such reactions occur. ( 5.3)
- “Sleep-driving” and other complex behaviors while not fully awake. Risk increases with dose and use with other CNS depressants and alcohol. Immediately evaluate any new onset behavioral changes. ( 5.4)
- Depression: Worsening of depression or suicidal thinking may occur. Prescribe the least amount of tablets feasible to avoid intentional overdose. ( 5.5)
- Respiratory Depression: Consider this risk before prescribing in patients with compromised respiratory function ( 5.6)
- Withdrawal effects: Symptoms may occur with rapid dose reduction or discontinuation ( 5.7, 9.3)
- Severe Injuries: Drowsiness may lead to fall including severe injuries ( 5.8)
ADVERSE REACTIONS
Most commonly observed adverse reactions were:
Short-term (< 10 nights): Drowsiness, dizziness, and diarrhea
Long-term (28 to 35 nights): Dizziness and drugged feelings ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact TEVA USA, PHARMACOVIGILANCE at 1-866-832-8537 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- CNS depressants, including alcohol: Possible adverse additive CNS-depressant effects ( 5.1, 7.1)
- Imipramine: Decreased alertness observed ( 7.1)
- Chlorpromazine: Impaired alertness and psychomotor performance observed ( 7.1)
- CYP3A4 inducers (e.g. rifampin): Combination use may decrease effect ( 7.2)
- CYP3A4 inhibitors (e.g. ketoconazole): Combination use may increase effect ( 7.2)
USE IN SPECIFIC POPULATIONS
- Pregnancy: Based on animal data, may cause fetal harm ( 8.1)
- Pediatric use: Safety and effectiveness not established. Hallucinations (incidence rate 7%) and other psychiatric and/or nervous system adverse reactions were observed frequently in a study of pediatric patients with Attention-Deficit/Hyperactivity Disorder ( 5.4, 8.4)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 8/2016
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosage in Adults
2.2 Special Populations
2.3 Use with CNS Depressants
2.4 Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 CNS Depressant Effects and Next-Day Impairment
5.2 Need to Evaluate for Co-Morbid Diagnoses
5.3 Severe Anaphylactic and Anaphylactoid Reactions
5.4 Abnormal Thinking and Behavioral Changes
5.5 Use in Patients with Depression
5.6 Respiratory Depression
5.7 Withdrawal Effects
5.8 Severe Injuries
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 CNS-active Drugs
7.2 Drugs That Affect Drug Metabolism via Cytochrome P450
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Gender Difference in Pharmacokinetics
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
10.1 Signs and Symptoms
10.2 Recommended Treatment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Transient Insomnia
14.2 Chronic Insomnia
14.3 Studies Pertinent to Safety Concerns for Sedative/Hypnotic Drugs
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
Zolpidem Tartrate Tablets USP 10 mg CIV 100s Label Text
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Zolpidem tartrate tablets are indicated for the short-term treatment of insomnia characterized by difficulties with sleep initiation. Zolpidem tartrate tablets have been shown to decrease sleep latency for up to 35 days in controlled clinical studies [see Clinical Studies ( 14)] .
The clinical trials performed in support of efficacy were 4 to 5 weeks in duration with the final formal assessments of sleep latency performed at the end of treatment.
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosage in Adults
Use the lowest effective dose for the patient. The recommended initial dose is 5 mg for women and either 5 or 10 mg for men, taken only once per night immediately before bedtime with at least 7 to 8 hours remaining before the planned time of awakening. If the 5 mg dose is not effective, the dose can be increased to 10 mg. In some patients, the higher morning blood levels following use of the 10 mg dose increase the risk of next day impairment of driving and other activities that require full alertness [see Warnings and Precautions ( 5.1)] . The total dose of zolpidem tartrate tablets should not exceed 10 mg once daily immediately before bedtime. Zolpidem tartrate tablets should be taken as a single dose and should not be readministered during the same night.
The recommended initial doses for women and men are different because zolpidem clearance is lower in women.
2.2 Special Populations
Elderly or debilitated patients may be especially sensitive to the effects of zolpidem tartrate. Patients with hepatic insufficiency do not clear the drug as rapidly as normal subjects. The recommended dose of zolpidem tartrate tablets in both of these patient populations is 5 mg once daily immediately before bedtime [see Warnings and Precautions ( 5.1); Use in Specific Populations ( 8.5)] .
2.3 Use with CNS Depressants
Dosage adjustment may be necessary when zolpidem tartrate tablets are combined with other CNS depressant drugs because of the potentially additive effects [see Warnings and Precautions ( 5.1)] .
-
3 DOSAGE FORMS AND STRENGTHS
Zolpidem tartrate tablets USP are available in 5 mg and 10 mg strength tablets for oral administration. Tablets are not scored.
Zolpidem tartrate tablets USP, 5 mg are pink, film-coated, round tablets; debossed "TEVA" on one side and "73" on the other.
Zolpidem tartrate tablets USP, 10 mg are white to off-white, film-coated, round tablets; debossed "TEVA" on one side and "74" on the other.
-
4 CONTRAINDICATIONS
Zolpidem tartrate is contraindicated in patients with known hypersensitivity to zolpidem. Observed reactions include anaphylaxis and angioedema [see Warnings and Precautions ( 5.3)] .
-
5 WARNINGS AND PRECAUTIONS
5.1 CNS Depressant Effects and Next-Day Impairment
Zolpidem tartrate, like other sedative-hypnotic drugs, has central nervous system (CNS) depressant effects. Coadministration with other CNS depressants (e.g., benzodiazepines, opioids, tricyclic antidepressants, alcohol) increases the risk of CNS depression. Dosage adjustments of zolpidem tartrate and of other concomitant CNS depressants may be necessary when zolpidem tartrate is administered with such agents because of the potentially additive effects. The use of zolpidem tartrate with other sedative-hypnotics (including other zolpidem products) at bedtime or the middle of the night is not recommended . Zolpidem tartrate, like other sedative-hypnotic drugs, has central nervous system (CNS) depressant effects. Coadministration with other CNS depressants (e.g., benzodiazepines, opioids, tricyclic antidepressants, alcohol) increases the risk of CNS depression. Dosage adjustments of zolpidem tartrate and of other concomitant CNS depressants may be necessary when zolpidem tartrate is administered with such agents because of the potentially additive effects. The use of zolpidem tartrate with other sedative-hypnotics (including other zolpidem products) at bedtime or the middle of the night is not recommended [see Dosage and Administration ( 2.3)] .
The risk of next-day psychomotor impairment, including impaired driving, is increased if zolpidem tartrate is taken with less than a full night of sleep remaining (7 to 8 hours); if a higher than the recommended dose is taken; if coadministered with other CNS depressants or alcohol; or if coadministered with other drugs that increase the blood levels of zolpidem. Patients should be warned against driving and other activities requiring complete mental alertness if zolpidem tartrate is taken in these circumstances [see Dosage and Administration (2) and Clinical Studies ( 14.3)] .
Vehicle drivers and machine operators should be warned that, as with other hypnotics, there may be a possible risk of adverse reactions including drowsiness, prolonged reaction time, dizziness, sleepiness, blurred/double vision, reduced alertness and impaired driving the morning after therapy. In order to minimize this risk a full night of sleep (7 to 8 hours) is recommended.
5.2 Need to Evaluate for Co-Morbid Diagnoses
Because sleep disturbances may be the presenting manifestation of a physical and/or psychiatric disorder, symptomatic treatment of insomnia should be initiated only after a careful evaluation of the patient. The failure of insomnia to remit after 7 to 10 days of treatment may indicate the presence of a primary psychiatric and/or medical illness that should be evaluated. Worsening of insomnia or the emergence of new thinking or behavior abnormalities may be the consequence of an unrecognized psychiatric or physical disorder. Such findings have emerged during the course of treatment with sedative/hypnotic drugs, including zolpidem.
5.3 Severe Anaphylactic and Anaphylactoid Reactions
Cases of angioedema involving the tongue, glottis or larynx have been reported in patients after taking the first or subsequent doses of sedative-hypnotics, including zolpidem. Some patients have had additional symptoms such as dyspnea, throat closing or nausea and vomiting that suggest anaphylaxis. Some patients have required medical therapy in the emergency department. If angioedema involves the throat, glottis or larynx, airway obstruction may occur and be fatal. Patients who develop angioedema after treatment with zolpidem should not be rechallenged with the drug.
5.4 Abnormal Thinking and Behavioral Changes
Abnormal thinking and behavior changes have been reported in patients treated with sedative/hypnotics, including zolpidem tartrate. Some of these changes included decreased inhibition (e.g., aggressiveness and extroversion that seemed out of character), bizarre behavior, agitation and depersonalization. Visual and auditory hallucinations have been reported.
In controlled trials of zolpidem tartrate 10 mg taken at bedtime < 1% of adults with insomnia reported hallucinations. In a clinical trial, 7% of pediatric patients treated with zolpidem tartrate 0.25 mg/kg taken at bedtime reported hallucinations versus 0% treated with placebo [see Use in Specific Populations ( 8.4)] .
Complex behaviors such as “sleep-driving” (i.e., driving while not fully awake after ingestion of a sedative-hypnotic, with amnesia for the event) have been reported in sedative-hypnotic-naive as well as in sedative-hypnotic-experienced persons. Although behaviors such as “sleep-driving” have occurred with zolpidem tartrate alone at therapeutic doses, the coadministration of zolpidem tartrate with alcohol and other CNS depressants increases the risk of such behaviors, as does the use of zolpidem tartrate at doses exceeding the maximum recommended dose. Due to the risk to the patient and the community, discontinuation of zolpidem tartrate should be strongly considered for patients who report a “sleep-driving” episode.
Other complex behaviors (e.g., preparing and eating food, making phone calls, or having sex) have been reported in patients who are not fully awake after taking a sedative-hypnotic. As with “sleep-driving”, patients usually do not remember these events. Amnesia, anxiety and other neuro-psychiatric symptoms may also occur.
It can rarely be determined with certainty whether a particular instance of the abnormal behaviors listed above is drug induced, spontaneous in origin, or a result of an underlying psychiatric or physical disorder. Nonetheless, the emergence of any new behavioral sign or symptom of concern requires careful and immediate evaluation.
5.5 Use in Patients with Depression
In primarily depressed patients treated with sedative-hypnotics, worsening of depression, and suicidal thoughts and actions (including completed suicides), have been reported. Suicidal tendencies may be present in such patients and protective measures may be required. Intentional overdosage is more common in this group of patients; therefore, the lowest number of tablets that is feasible should be prescribed for the patient at any one time.
5.6 Respiratory Depression
Although studies with 10 mg zolpidem tartrate did not reveal respiratory depressant effects at hypnotic doses in healthy subjects or in patients with mild-to-moderate chronic obstructive pulmonary disease (COPD), a reduction in the Total Arousal Index, together with a reduction in lowest oxygen saturation and increase in the times of oxygen desaturation below 80% and 90%, was observed in patients with mild-to-moderate sleep apnea when treated with zolpidem compared to placebo. Since sedative-hypnotics have the capacity to depress respiratory drive, precautions should be taken if zolpidem tartrate is prescribed to patients with compromised respiratory function. Postmarketing reports of respiratory insufficiency in patients receiving 10 mg of zolpidem tartrate, most of whom had preexisting respiratory impairment, have been reported. The risk of respiratory depression should be considered prior to prescribing zolpidem tartrate in patients with respiratory impairment including sleep apnea and myasthenia gravis.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in other sections of the labeling:
- CNS-depressant effects and next-day impairment [see Warnings and Precautions ( 5.1)]
- Serious anaphylactic and anaphylactoid reactions [see Warnings and Precautions ( 5.3)]
- Abnormal thinking and behavior changes, and complex behaviors [see Warnings and Precautions ( 5.4)]
- Withdrawal effects [see Warnings and Precautions ( 5.7)]
6.1 Clinical Trials Experience
Associated with discontinuation of treatment: Approximately 4% of 1,701 patients who received zolpidem at all doses (1.25 to 90 mg) in U.S. premarketing clinical trials discontinued treatment because of an adverse reaction. Reactions most commonly associated with discontinuation from U.S. trials were daytime drowsiness (0.5%), dizziness (0.4%), headache (0.5%), nausea (0.6%), and vomiting (0.5%).
Approximately 4% of 1,959 patients who received zolpidem at all doses (1 to 50 mg) in similar foreign trials discontinued treatment because of an adverse reaction. Reactions most commonly associated with discontinuation from these trials were daytime drowsiness (1.1%), dizziness/vertigo (0.8%), amnesia (0.5%), nausea (0.5%), headache (0.4%), and falls (0.4%).
Data from a clinical study in which selective serotonin reuptake inhibitor (SSRI)-treated patients were given zolpidem revealed that four of the seven discontinuations during double-blind treatment with zolpidem (n = 95) were associated with impaired concentration, continuing or aggravated depression, and manic reaction; one patient treated with placebo (n = 97) was discontinued after an attempted suicide.
Most commonly observed adverse reactions in controlled trials: During short-term treatment (up to 10 nights) with zolpidem tartrate at doses up to 10 mg, the most commonly observed adverse reactions associated with the use of zolpidem and seen at statistically significant differences from placebo-treated patients were drowsiness (reported by 2% of zolpidem patients), dizziness (1%), and diarrhea (1%). During longer-term treatment (28 to 35 nights) with zolpidem at doses up to 10 mg, the most commonly observed adverse reactions associated with the use of zolpidem and seen at statistically significant differences from placebo-treated patients were dizziness (5%) and drugged feelings (3%).
Adverse reactions observed at an incidence of ≥ 1% in controlled trials: The following tables enumerate treatment-emergent adverse reactions frequencies that were observed at an incidence equal to 1% or greater among patients with insomnia who received zolpidem tartrate and at a greater incidence than placebo in U.S. placebo-controlled trials. Events reported by investigators were classified utilizing a modified World Health Organization (WHO) dictionary of preferred terms for the purpose of establishing event frequencies. The prescriber should be aware that these figures cannot be used to predict the incidence of side effects in the course of usual medical practice, in which patient characteristics and other factors differ from those that prevailed in these clinical trials. Similarly, the cited frequencies cannot be compared with figures obtained from other clinical investigators involving related drug products and uses, since each group of drug trials is conducted under a different set of conditions. However, the cited figures provide the physician with a basis for estimating the relative contribution of drug and nondrug factors to the incidence of side effects in the population studied.
The following table was derived from results of 11 placebo-controlled short-term U.S. efficacy trials involving zolpidem in doses ranging from 1.25 to 20 mg. The table is limited to data from doses up to and including 10 mg, the highest dose recommended for use.
Incidence of Treatment-Emergent Adverse Experiences in Placebo-Controlled Clinical Trials Lasting up to 10 Nights (Percentage of patients reporting) Body System/
Adverse Event *Zolpidem
(≤ 10 mg)
(N = 685)Placebo
(N = 473)- * Reactions reported by at least 1% of patients treated with zolpidem tartrate and at a greater frequency than placebo.
Central and Peripheral Nervous System
Headache
7
6
Drowsiness
2
–
Dizziness
1
–
Gastrointestinal System
Diarrhea
1
-
The following table was derived from results of three placebo-controlled long-term efficacy trials involving zolpidem tartrate. These trials involved patients with chronic insomnia who were treated for 28 to 35 nights with zolpidem at doses of 5, 10, or 15 mg. The table is limited to data from doses up to and including 10 mg, the highest dose recommended for use. The table includes only adverse events occurring at an incidence of at least 1% for zolpidem patients.
Incidence of Treatment-Emergent Adverse Experiences in Placebo-Controlled Clinical Trials Lasting up to 35 Nights (Percentage of patients reporting) Body System/
Adverse Event *Zolpidem
(≤ 10 mg)
(N = 152)Placebo
(N = 161)- * Reactions reported by at least 1% of patients treated with zolpidem tartrate and at a greater frequency than placebo.
Autonomic Nervous System
Dry mouth
3
1
Body as a Whole
Allergy
4
1
Back Pain
3
2
Influenza-like symptoms
2
-
Chest pain
1
-
Cardiovascular System
Palpitation
2
-
Central and Peripheral Nervous System
Drowsiness
8
5
Dizziness
5
1
Lethargy
3
1
Drugged feeling
3
-
Lightheadedness
2
1
Depression
2
1
Abnormal dreams
1
-
Amnesia
1
-
Sleep disorder
1
-
Gastrointestinal System
Diarrhea
3
2
Abdominal pain
2
2
Constipation
2
1
Respiratory System
Sinusitis
4
2
Pharyngitis
3
1
Skin and Appendages
Rash
2
1
Dose relationship for adverse reactions: There is evidence from dose comparison trials suggesting a dose relationship for many of the adverse reactions associated with zolpidem use, particularly for certain CNS and gastrointestinal adverse events.
Adverse event incidence across the entire preapproval database: Zolpidem tartrate was administered to 3,660 subjects in clinical trials throughout the U.S., Canada, and Europe. Treatment-emergent adverse events associated with clinical trial participation were recorded by clinical investigators using terminology of their own choosing. To provide a meaningful estimate of the proportion of individuals experiencing treatment-emergent adverse events, similar types of untoward events were grouped into a smaller number of standardized event categories and classified utilizing a modified World Health Organization (WHO) dictionary of preferred terms.
The frequencies presented, therefore, represent the proportions of the 3,660 individuals exposed to zolpidem, at all doses, who experienced an event of the type cited on at least one occasion while receiving zolpidem. All reported treatment-emergent adverse events are included, except those already listed in the table above of adverse events in placebo-controlled studies, those coding terms that are so general as to be uninformative, and those events where a drug cause was remote. It is important to emphasize that, although the events reported did occur during treatment with zolpidem tartrate, they were not necessarily caused by it.
Adverse events are further classified within body system categories and enumerated in order of decreasing frequency using the following definitions: frequent adverse events are defined as those occurring in greater than 1/100 subjects; infrequent adverse events are those occurring in 1/100 to 1/1,000 patients; rare events are those occurring in less than 1/1,000 patients.
Autonomic nervous system: Infrequent: increased sweating, pallor, postural hypotension, syncope. Rare: abnormal accommodation, altered saliva, flushing, glaucoma, hypotension, impotence, increased saliva, tenesmus.
Body as a whole: Frequent: asthenia. Infrequent: edema, falling, fatigue, fever, malaise, trauma. Rare: allergic reaction, allergy aggravated, anaphylactic shock, face edema, hot flashes, increased ESR, pain, restless legs, rigors, tolerance increased, weight decrease.
Cardiovascular system: Infrequent: cerebrovascular disorder, hypertension, tachycardia. Rare: angina pectoris, arrhythmia, arteritis, circulatory failure, extrasystoles, hypertension aggravated, myocardial infarction, phlebitis, pulmonary embolism, pulmonary edema, varicose veins, ventricular tachycardia.
Central and peripheral nervous system: Frequent: ataxia, confusion, euphoria, headache, insomnia, vertigo. Infrequent: agitation, anxiety, decreased cognition, detached, difficulty concentrating, dysarthria, emotional lability, hallucination, hypoesthesia, illusion, leg cramps, migraine, nervousness, paresthesia, sleeping (after daytime dosing), speech disorder, stupor, tremor. Rare: abnormal gait, abnormal thinking, aggressive reaction, apathy, appetite increased, decreased libido, delusion, dementia, depersonalization, dysphasia, feeling strange, hypokinesia, hypotonia, hysteria, intoxicated feeling, manic reaction, neuralgia, neuritis, neuropathy, neurosis, panic attacks, paresis, personality disorder, somnambulism, suicide attempts, tetany, yawning.
Gastrointestinal system: Frequent: dyspepsia, hiccup, nausea. Infrequent: anorexia, constipation, dysphagia, flatulence, gastroenteritis, vomiting. Rare: enteritis, eructation, esophagospasm, gastritis, hemorrhoids, intestinal obstruction, rectal hemorrhage, tooth caries.
Hematologic and lymphatic system: Rare: anemia, hyperhemoglobinemia, leukopenia, lymphadenopathy, macrocytic anemia, purpura, thrombosis.
Immunologic system: Infrequent: infection. Rare: abscess herpes simplex herpes zoster, otitis externa, otitis media.
Liver and biliary system: Infrequent: abnormal hepatic function, increased SGPT. Rare: bilirubinemia, increased SGOT.
Metabolic and nutritional: Infrequent: hyperglycemia, thirst. Rare: gout, hypercholesteremia, hyperlipidemia, increased alkaline phosphatase, increased BUN, periorbital edema.
Musculoskeletal system: Frequent: arthralgia, myalgia. Infrequent: arthritis. Rare: arthrosis, muscle weakness, sciatica, tendinitis.
Reproductive system: Infrequent: menstrual disorder, vaginitis. Rare: breast fibroadenosis, breast neoplasm, breast pain.
Respiratory system: Frequent: upper respiratory infection, lower respiratory infection. Infrequent: bronchitis, coughing, dyspnea, rhinitis. Rare: bronchospasm, respiratory depression, epistaxis, hypoxia, laryngitis, pneumonia.
Skin and appendages: Infrequent: pruritus. Rare: acne, bullous eruption, dermatitis, furunculosis, injection-site inflammation, photosensitivity reaction, urticaria.
Special senses: Frequent: diplopia, vision abnormal. Infrequent: eye irritation, eye pain, scleritis, taste perversion, tinnitus. Rare: conjunctivitis, corneal ulceration, lacrimation abnormal, parosmia, photopsia.
Urogenital system: Frequent: urinary tract infection. Infrequent: cystitis, urinary incontinence. Rare: acute renal failure, dysuria, micturition frequency, nocturia, polyuria, pyelonephritis, renal pain, urinary retention.
-
7 DRUG INTERACTIONS
7.1 CNS-active Drugs
Coadministration of zolpidem with other CNS depressants increases the risk of CNS depression. Concomitant use of zolpidem with these drugs may increase drowsiness and psychomotor impairment, including impaired driving ability [see Warnings and Precautions ( 5.1)] . Zolpidem tartrate was evaluated in healthy volunteers in single-dose interaction studies for several CNS drugs.
Imipramine, Chlorpromazine
Imipramine in combination with zolpidem produced no pharmacokinetic interaction other than a 20% decrease in peak levels of imipramine, but there was an additive effect of decreased alertness. Similarly, chlorpromazine in combination with zolpidem produced no pharmacokinetic interaction, but there was an additive effect of decreased alertness and psychomotor performance [see Clinical Pharmacology ( 12.3)] .
Haloperidol
A study involving haloperidol and zolpidem revealed no effect of haloperidol on the pharmacokinetics or pharmacodynamics of zolpidem. The lack of a drug interaction following single-dose administration does not predict the absence of an effect following chronic administration [see Clinical Pharmacology ( 12.3)] .
Alcohol
An additive adverse effect on psychomotor performance between alcohol and oral zolpidem was demonstrated [see Warnings and Precautions ( 5.1)] .
Sertraline
Concomitant administration of zolpidem and sertraline increases exposure to zolpidem [see Clinical Pharmacology ( 12.3)] .
Fluoxetine
After multiple doses of zolpidem tartrate and fluoxetine an increase in the zolpidem half-life (17%) was observed. There was no evidence of an additive effect in psychomotor performance [see Clinical Pharmacology ( 12.3)] .
7.2 Drugs That Affect Drug Metabolism via Cytochrome P450
Some compounds known to induce or inhibit CYP3A may affect exposure to zolpidem. The effect of drugs that induce or inhibit other P450 enzymes on the exposure to zolpidem is not known.
CYP3A4 Inducers
Rifampin, a CYP3A4 inducer, significantly reduced the exposure to and the pharmacodynamic effects of zolpidem. Use of CYP3A4 inducers in combination with zolpidem may decrease the efficacy of zolpidem [see Clinical Pharmacology ( 12.3)] .
CYP3A4 Inhibitors
Ketoconazole, a potent CYP3A4 inhibitor, increased the exposure to and pharmacodynamic effects of zolpidem. Consideration should be given to using a lower dose of zolpidem when a potent CYP3A4 inhibitor and zolpidem are given together [see Clinical Pharmacology ( 12.3)] .
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies of zolpidem tartrate in pregnant women.
Studies in children to assess the effects of prenatal exposure to zolpidem have not been conducted; however, cases of severe neonatal respiratory depression have been reported when zolpidem was used at the end of pregnancy, especially when taken with other CNS-depressants. Children born to mothers taking sedative-hypnotic drugs may be at risk for withdrawal symptoms during the postnatal period. Neonatal flaccidity has also been reported in infants born to mothers who received sedative-hypnotic drugs during pregnancy. Zolpidem tartrate should be used during pregnancy only if the potential benefit outweighs the potential risk to the fetus.
Administration of zolpidem to pregnant rats and rabbits resulted in adverse effects on offspring development at doses greater than the zolpidem tartrate maximum recommended human dose (MRHD) of 10 mg/day (approximately 8 mg/day zolpidem base); however, teratogenicity was not observed.
When zolpidem was administered at oral doses of 4, 20, and 100 mg base/kg/day to pregnant rats during the period of organogenesis, dose-related decreases in fetal skull ossification occurred at all but the lowest dose, which is approximately 5 times the MRHD on a mg/m 2 basis. In rabbits treated during organogenesis with zolpidem at oral doses of 1, 4, and 16 mg base/kg/day increased embryo-fetal death and incomplete fetal skeletal ossification occurred at the highest dose tested. The no-effect dose for embryo-fetal toxicity in rabbits is approximately 10 times the MRHD on a mg/m 2 basis. Administration of zolpidem to rats at oral doses of 4, 20, and 100 mg base/kg/day during the latter part of pregnancy and throughout lactation produced decreased offspring growth and survival at all but the lowest dose, which is approximately 5 times the MRHD on a mg/m 2 basis.
8.2 Labor and Delivery
Zolpidem tartrate has no established use in labor and delivery [see Pregnancy ( 8.1)] .
8.3 Nursing Mothers
Zolpidem is excreted in human milk. Caution should be exercised when zolpidem tartrate is administered to a nursing woman.
8.4 Pediatric Use
Zolpidem tartrate is not recommended for use in children. Safety and effectiveness of zolpidem in pediatric patients below the age of 18 years have not been established.
In an 8-week study, in pediatric patients (aged 6 to 17 years) with insomnia associated with attention-deficit/hyperactivity disorder (ADHD) an oral solution of zolpidem tartrate dosed at 0.25 mg/kg at bedtime did not decrease sleep latency compared to placebo. Psychiatric and nervous system disorders comprised the most frequent (> 5%) treatment emergent adverse reactions observed with zolpidem versus placebo and included dizziness (23.5% vs. 1.5%), headache (12.5% vs. 9.2%), and hallucinations were reported in 7% of the pediatric patients who received zolpidem; none of the pediatric patients who received placebo reported hallucinations [see Warnings and Precautions ( 5.4)] . Ten patients on zolpidem (7.4%) discontinued treatment due to an adverse reaction.
8.5 Geriatric Use
A total of 154 patients in U.S. controlled clinical trials and 897 patients in non-U.S. clinical trials who received zolpidem were ≥ 60 years of age. For a pool of U.S. patients receiving zolpidem at doses of ≤ 10 mg or placebo, there were three adverse reactions occurring at an incidence of at least 3% for zolpidem and for which the zolpidem incidence was at least twice the placebo incidence (i.e., they could be considered drug related).
Adverse Event Zolpidem Placebo Dizziness
3%
0%
Drowsiness
5%
2%
Diarrhea
3%
1%
A total of 30/1,959 (1.5%) non-U.S. patients receiving zolpidem reported falls, including 28/30 (93%) who were ≥ 70 years of age. Of these 28 patients, 23 (82%) were receiving zolpidem doses > 10 mg. A total of 24/1,959 (1.2%) non-U.S. patients receiving zolpidem reported confusion, including 18/24 (75%) who were ≥ 70 years of age. Of these 18 patients, 14 (78%) were receiving zolpidem doses > 10 mg.The dose of zolpidem tartrate in elderly patients is 5 mg to minimize adverse effects related to impaired motor and/or cognitive performance and unusual sensitivity to sedative/hypnotic drugs [see Warnings and Precautions ( 5.1)].
8.6 Gender Difference in Pharmacokinetics
Women clear zolpidem tartrate from the body at a lower rate than men. C max and AUC parameters of zolpidem were approximately 45% higher at the same dose in female subjects compared with male subjects. Given the higher blood levels of zolpidem tartrate in women compared to men at a given dose, the recommended initial dose of zolpidem tartrate for adult women is 5 mg, and the recommended dose for adult men is 5 or 10 mg.
In geriatric patients, clearance of zolpidem is similar in men and women. The recommended dose of zolpidem tartrate in geriatric patients is 5 mg regardless of gender.
-
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Zolpidem tartrate is classified as a Schedule IV controlled substance by federal regulation.
9.2 Abuse
Abuse and addiction are separate and distinct from physical dependence and tolerance. Abuse is characterized by misuse of the drug for non-medical purposes, often in combination with other psychoactive substances. Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug effects over time. Tolerance may occur to both desired and undesired effects of drugs and may develop at different rates for different effects.
Addiction is a primary, chronic, neurobiological disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving. Drug addiction is a treatable disease, using a multidisciplinary approach, but relapse is common.
Studies of abuse potential in former drug abusers found that the effects of single doses of zolpidem tartrate 40 mg were similar, but not identical, to diazepam 20 mg, while zolpidem tartrate 10 mg was difficult to distinguish from placebo.
Because persons with a history of addiction to, or abuse of, drugs or alcohol are at increased risk for misuse, abuse and addiction of zolpidem, they should be monitored carefully when receiving zolpidem or any other hypnotic.
9.3 Dependence
Physical dependence is a state of adaptation that is manifested by a specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist.
Sedative/hypnotics have produced withdrawal signs and symptoms following abrupt discontinuation. These reported symptoms range from mild dysphoria and insomnia to a withdrawal syndrome that may include abdominal and muscle cramps, vomiting, sweating, tremors, and convulsions. The following adverse events which are considered to meet the DSM-III-R criteria for uncomplicated sedative/hypnotic withdrawal were reported during U.S. clinical trials following placebo substitution occurring within 48 hours following last zolpidem treatment: fatigue, nausea, flushing, lightheadedness, uncontrolled crying, emesis, stomach cramps, panic attack, nervousness, and abdominal discomfort. These reported adverse events occurred at an incidence of 1% or less. However, available data cannot provide a reliable estimate of the incidence, if any, of dependence during treatment at recommended doses. Postmarketing reports of abuse, dependence and withdrawal have been received.
-
10 OVERDOSAGE
10.1 Signs and Symptoms
In postmarketing experience of overdose with zolpidem tartrate alone, or in combination with CNS-depressant agents, impairment of consciousness ranging from somnolence to coma, cardiovascular and/or respiratory compromise, and fatal outcomes have been reported.
10.2 Recommended Treatment
General symptomatic and supportive measures should be used along with immediate gastric lavage where appropriate. Intravenous fluids should be administered as needed. Zolpidem’s sedative hypnotic effect was shown to be reduced by flumazenil and therefore may be useful; however, flumazenil administration may contribute to the appearance of neurological symptoms (convulsions). As in all cases of drug overdose, respiration, pulse, blood pressure, and other appropriate signs should be monitored and general supportive measures employed. Hypotension and CNS depression should be monitored and treated by appropriate medical intervention. Sedating drugs should be withheld following zolpidem overdosage, even if excitation occurs. The value of dialysis in the treatment of overdosage has not been determined, although hemodialysis studies in patients with renal failure receiving therapeutic doses have demonstrated that zolpidem is not dialyzable.
As with the management of all overdosage, the possibility of multiple drug ingestion should be considered. The physician may wish to consider contacting a poison control center for up-to-date information on the management of hypnotic drug product overdosage.
-
11 DESCRIPTION
Zolpidem tartrate, USP is a gamma-aminobutyric acid (GABA) A agonist of the imidazopyridine class and is available in 5 mg and 10 mg strength tablets for oral administration.
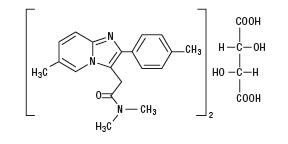
Chemically, zolpidem tartrate, USP is N, N,6-Trimethyl-2- p-tolylimidazo[1,2-α]pyridine-3-acetamide L-(+)-tartrate. It has the following structure:
(C 19H 21N 3O) 2C 4H 6O 6 M.W. 764.87
Zolpidem tartrate, USP is a white to off-white crystalline powder that is sparingly soluble in water, alcohol, and propylene glycol.
Each zolpidem tartrate tablet USP includes the following inactive ingredients: hypromellose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polysorbate 80, sodium starch glycolate, and titanium dioxide; the 5 mg tablet also contains iron oxide red.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Zolpidem, the active moiety of zolpidem tartrate, is a hypnotic agent with a chemical structure unrelated to benzodiazepines, barbiturates, or other drugs with known hypnotic properties. It interacts with a GABA-BZ receptor complex and shares some of the pharmacological properties of the benzodiazepines. In contrast to the benzodiazepines, which non-selectively bind to and activate all BZ receptor subtypes, zolpidem in vitro binds the BZ 1 receptor preferentially with a high affinity ratio of the α 1/α 5 subunits. This selective binding of zolpidem on the BZ 1 receptor is not absolute, but it may explain the relative absence of myorelaxant and anticonvulsant effects in animal studies as well as the preservation of deep sleep (stages 3 and 4) in human studies of zolpidem tartrate at hypnotic doses.
12.3 Pharmacokinetics
The pharmacokinetic profile of zolpidem tartrate is characterized by rapid absorption from the gastrointestinal tract and a short elimination half-life (T 1/2) in healthy subjects.
In a single-dose crossover study in 45 healthy subjects administered 5 and 10 mg zolpidem tartrate tablets, the mean peak concentrations (C max) were 59 (range: 29 to 113) and 121 (range: 58 to 272) ng/mL, respectively, occurring at a mean time (T max) of 1.6 hours for both. The mean zolpidem tartrate elimination half-life was 2.6 (range: 1.4 to 4.5) and 2.5 (range: 1.4 to 3.8) hours, for the 5 and 10 mg tablets, respectively. Zolpidem tartrate is converted to inactive metabolites that are eliminated primarily by renal excretion. Zolpidem tartrate demonstrated linear kinetics in the dose range of 5 to 20 mg. Total protein binding was found to be 92.5 ± 0.1% and remained constant, independent of concentration between 40 and 790 ng/mL. Zolpidem did not accumulate in young adults following nightly dosing with 20 mg zolpidem tartrate tablets for 2 weeks.
A food-effect study in 30 healthy male subjects compared the pharmacokinetics of zolpidem tartrate 10 mg when administered while fasting or 20 minutes after a meal. Results demonstrated that with food, mean AUC and C max were decreased by 15% and 25%, respectively, while mean T max was prolonged by 60% (from 1.4 to 2.2 hr). The half-life remained unchanged. These results suggest that, for faster sleep onset, zolpidem tartrate should not be administered with or immediately after a meal.
Special Populations
Elderly:
In the elderly, the dose for zolpidem tartrate should be 5 mg [see Warnings and Precautions ( 5) and Dosage and Administration ( 2)] . This recommendation is based on several studies in which the mean C max, T 1/2, and AUC were significantly increased when compared to results in young adults. In one study of eight elderly subjects (> 70 years), the means for C max, T 1/2, and AUC significantly increased by 50% (255 vs. 384 ng/mL), 32% (2.2 vs. 2.9 hr), and 64% (955 vs. 1,562 nghr/mL), respectively, as compared to younger adults (20 to 40 years) following a single 20 mg oral dose. Zolpidem tartrate did not accumulate in elderly subjects following nightly oral dosing of 10 mg for 1 week.
Hepatic Impairment:
The pharmacokinetics of zolpidem tartrate in eight patients with chronic hepatic insufficiency were compared to results in healthy subjects. Following a single 20 mg oral zolpidem tartrate dose, mean C max and AUC were found to be two times (250 vs. 499 ng/mL) and five times (788 vs. 4,203 nghr/mL) higher, respectively, in hepatically-compromised patients. T max did not change. The mean half-life in cirrhotic patients of 9.9 hr (range: 4.1 to 25.8 hr) was greater than that observed in normal subjects of 2.2 hr (range: 1.6 to 2.4 hr). Dosing should be modified accordingly in patients with hepatic insufficiency [see Dosage and Administration ( 2.2)] .
Renal Impairment:
The pharmacokinetics of zolpidem tartrate were studied in 11 patients with end-stage renal failure (mean Cl Cr = 6.5 ± 1.5 mL/min) undergoing hemodialysis three times a week, who were dosed with zolpidem tartrate 10 mg orally each day for 14 or 21 days. No statistically significant differences were observed for C max, T max, half-life, and AUC between the first and last day of drug administration when baseline concentration adjustments were made. Zolpidem was not hemodialyzable. No accumulation of unchanged drug appeared after 14 or 21 days. Zolpidem pharmacokinetics were not significantly different in renally impaired patients. No dosage adjustment is necessary in patients with compromised renal function.
Drug Interactions
CNS-depressants
Coadministration of zolpidem with other CNS depressants increases the risk of CNS depression [see Warnings and Precautions ( 5.1)] . Zolpidem tartrate was evaluated in healthy volunteers in single-dose interaction studies for several CNS drugs. Imipramine in combination with zolpidem produced no pharmacokinetic interaction other than a 20% decrease in peak levels of imipramine, but there was an additive effect of decreased alertness. Similarly, chlorpromazine in combination with zolpidem produced no pharmacokinetic interaction, but there was an additive effect of decreased alertness and psychomotor performance.
A study involving haloperidol and zolpidem revealed no effect of haloperidol on the pharmacokinetics or pharmacodynamics of zolpidem. The lack of a drug interaction following single-dose administration does not predict the absence of an effect following chronic administration.
An additive adverse effect on psychomotor performance between alcohol and oral zolpidem was demonstrated [see Warnings and Precautions ( 5.1)].
Following five consecutive nightly doses at bedtime of oral zolpidem tartrate 10 mg in the presence of sertraline 50 mg (17 consecutive daily doses, at 7:00 am, in healthy female volunteers), zolpidem C max was significantly higher (43%) and T max was significantly decreased (-53%). Pharmacokinetics of sertraline and N-desmethylsertraline were unaffected by zolpidem.
A single-dose interaction study with zolpidem tartrate 10 mg and fluoxetine 20 mg at steady-state levels in male volunteers did not demonstrate any clinically significant pharmacokinetic or pharmacodynamic interactions. When multiple doses of zolpidem and fluoxetine were given at steady state and the concentrations evaluated in healthy females, an increase in the zolpidem half-life (17%) was observed. There was no evidence of an additive effect in psychomotor performance.
Drugs that Affect Drug Metabolism via Cytochrome P450
Some compounds known to inhibit CYP3A may increase exposure to zolpidem. The effect of inhibitors of other P450 enzymes on the pharmacokinetics of zolpidem is unknown.
A single-dose interaction study with zolpidem tartrate 10 mg and itraconazole 200 mg at steady-state levels in male volunteers resulted in a 34% increase in AUC 0-∞ of zolpidem tartrate. There were no pharmacodynamic effects of zolpidem detected on subjective drowsiness, postural sway, or psychomotor performance.
A single-dose interaction study with zolpidem tartrate 10 mg and rifampin 600 mg at steady-state levels in female subjects showed significant reductions of the AUC (-73%), C max (-58%), and T 1/2 (-36 %) of zolpidem together with significant reductions in the pharmacodynamic effects of zolpidem tartrate. Rifampin, a CYP3A4 inducer, significantly reduced the exposure to and the pharmacodynamic effects of zolpidem [see Drug Interactions ( 7.2)] .
A single-dose interaction study with zolpidem tartrate 5 mg and ketoconazole, a potent CYP3A4 inhibitor, given as 200 mg twice daily for 2 days increased C max of zolpidem (30%) and the total AUC of zolpidem (70%) compared to zolpidem alone and prolonged the elimination half-life (30%) along with an increase in the pharmacodynamic effects of zolpidem [see Drug Interactions ( 7.2)] .
Additionally, fluvoxamine (a strong inhibitor of CYP1A2 and a weak inhibitor of CYP3A4 and CYP2C9) and ciprofloxacin (a strong inhibitor of CYP1A2 and a moderate inhibitor of CYP3A4) are also likely to inhibit zolpidem’s metabolic pathways, potentially leading to an increase in zolpidem exposure.
Other Drugs with No Interactions with Zolpidem
A study involving cimetidine/zolpidem tartrate and ranitidine/zolpidem tartrate combinations revealed no effect of either drug on the pharmacokinetics or pharmacodynamics of zolpidem.
Zolpidem tartrate had no effect on digoxin pharmacokinetics and did not affect prothrombin time when given with warfarin in healthy subjects.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis: Zolpidem was administered to mice and rats for 2 years at oral doses of 4, 18, and 80 mg base/kg. In mice, these doses are approximately 2.5, 10, and 50 times the maximum recommended human dose (MRHD) of 10 mg/day (8 mg zolpidem base) on mg/m 2 basis. In rats, these doses are approximately 5, 20, and 100 times the MRHD on a mg/m 2 basis. No evidence of carcinogenic potential was observed in mice. In rats, renal tumors (lipoma, liposarcoma) were seen at the mid- and high doses.
Mutagenesis: Zolpidem was negative in in vitro (bacterial reverse mutation, mouse lymphoma, and chromosomal aberration) and in vivo (mouse micronucleus) genetic toxicology assays.
Impairment of fertility: Oral administration of zolpidem (doses of 4, 20, and 100 mg base/kg/day) to rats prior to and during mating, and continuing in females through postpartum day 25, resulted in irregular estrus cycles and prolonged precoital intervals at the highest dose tested. The no-effect dose for these findings is approximately 24 times the MRHD on a mg/m 2 basis. There was no impairment of fertility at any dose tested.
-
14 CLINICAL STUDIES
14.1 Transient Insomnia
Normal adults experiencing transient insomnia (n = 462) during the first night in a sleep laboratory were evaluated in a double-blind, parallel group, single-night trial comparing two doses of zolpidem (7.5 and 10 mg) and placebo. Both zolpidem doses were superior to placebo on objective (polysomnographic) measures of sleep latency, sleep duration, and number of awakenings.
Normal elderly adults (mean age 68) experiencing transient insomnia (n = 35) during the first two nights in a sleep laboratory were evaluated in a double-blind, crossover, 2 night trial comparing four doses of zolpidem (5, 10, 15 and 20 mg) and placebo. All zolpidem doses were superior to placebo on the two primary PSG parameters (sleep latency and efficiency) and all four subjective outcome measures (sleep duration, sleep latency, number of awakenings, and sleep quality).
14.2 Chronic Insomnia
Zolpidem was evaluated in two controlled studies for the treatment of patients with chronic insomnia (most closely resembling primary insomnia, as defined in the APA Diagnostic and Statistical Manual of Mental Disorders, DSM-IV™). Adult outpatients with chronic insomnia (n = 75) were evaluated in a double-blind, parallel group, 5 week trial comparing two doses of zolpidem tartrate and placebo. On objective (polysomnographic) measures of sleep latency and sleep efficiency, zolpidem 10 mg was superior to placebo on sleep latency for the first 4 weeks and on sleep efficiency for weeks 2 and 4. Zolpidem was comparable to placebo on number of awakenings at both doses studied.
Adult outpatients (n = 141) with chronic insomnia were also evaluated, in a double-blind, parallel group, 4 week trial comparing two doses of zolpidem and placebo. Zolpidem 10 mg was superior to placebo on a subjective measure of sleep latency for all 4 weeks, and on subjective measures of total sleep time, number of awakenings, and sleep quality for the first treatment week.
Increased wakefulness during the last third of the night as measured by polysomnography has not been observed in clinical trials with zolpidem tartrate.
14.3 Studies Pertinent to Safety Concerns for Sedative/Hypnotic Drugs
Next-day residual effects: Next-day residual effects of zolpidem tartrate were evaluated in seven studies involving normal subjects. In three studies in adults (including one study in a phase advance model of transient insomnia) and in one study in elderly subjects, a small but statistically significant decrease in performance was observed in the Digit Symbol Substitution Test (DSST) when compared to placebo. Studies of zolpidem tartrate in non-elderly patients with insomnia did not detect evidence of next-day residual effects using the DSST, the Multiple Sleep Latency Test (MSLT), and patient ratings of alertness.
Rebound effects: There was no objective (polysomnographic) evidence of rebound insomnia at recommended doses seen in studies evaluating sleep on the nights following discontinuation of zolpidem tartrate. There was subjective evidence of impaired sleep in the elderly on the first post-treatment night at doses above the recommended elderly dose of 5 mg.
Memory impairment: Controlled studies in adults utilizing objective measures of memory yielded no consistent evidence of next-day memory impairment following the administration of zolpidem tartrate. However, in one study involving zolpidem doses of 10 and 20 mg, there was a significant decrease in next-morning recall of information presented to subjects during peak drug effect (90 minutes post-dose), i.e., these subjects experienced anterograde amnesia. There was also subjective evidence from adverse event data for anterograde amnesia occurring in association with the administration of zolpidem tartrate, predominantly at doses above 10 mg.
Effects on sleep stages: In studies that measured the percentage of sleep time spent in each sleep stage, zolpidem tartrate has generally been shown to preserve sleep stages. Sleep time spent in stages 3 and 4 (deep sleep) was found comparable to placebo with only inconsistent, minor changes in REM (paradoxical) sleep at the recommended dose.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
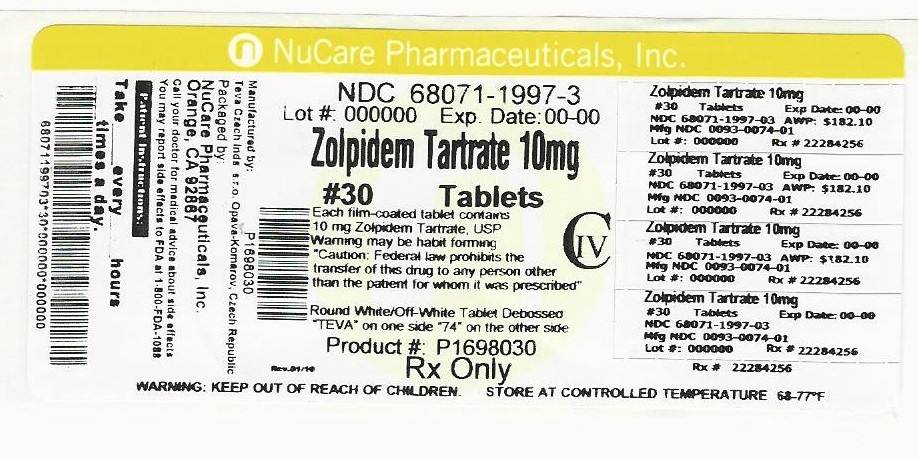
10 mg: white to off-white, film-coated, round, unscored tablets, debossed "TEVA" on one side of the tablet and “74” on the other. They are available in bottles of
bottles of 10 NDC: 68071-1997-1
bottles of 14 NDC: 68071-1997-4
bottles of 15 NDC: 68071-1997-5
bottles of 20 NDC: 68071-1997-2
bottles of 28 NDC: 68071-1997-2
bottles of 30 NDC: 68071-1997-3
bottles of 60 NDC: 68071-1997-6
bottles of 90 NDC: 68071-1997-9
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
-
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide).
Inform patients and their families about the benefits and risks of treatment with zolpidem tartrate tablets. Inform patients of the availability of a Medication Guide and instruct them to read the Medication Guide prior to initiating treatment with zolpidem tartrate tablets and with each prescription refill. Review the zolpidem tartrate tablets Medication Guide with every patient prior to initiation of treatment. Instruct patients or caregivers that zolpidem tartrate tablets should be taken only as prescribed.
CNS Depressant Effects and Next-Day Impairment
Tell patients that zolpidem tartrate has the potential to cause next-day impairment, and that this risk is increased if dosing instructions are not carefully followed. Tell patients to wait for at least 8 hours after dosing before driving or engaging in other activities requiring full mental alertness. Inform patients that impairment can be present despite feeling fully awake.
Severe Anaphylactic and Anaphylactoid Reactions
Inform patients that severe anaphylactic and anaphylactoid reactions have occurred with zolpidem. Describe the signs/symptoms of these reactions and advise patients to seek medical attention immediately if any of them occur.
Sleep-driving and Other Complex Behaviors
Instruct patients and their families that sedative hypnotics can cause abnormal thinking and behavior change, including “sleep driving” and other complex behaviors while not being fully awake (preparing and eating food, making phone calls, or having sex). Tell patients to call you immediately if they develop any of these symptoms.
Suicide
Tell patients to immediately report any suicidal thoughts.
Alcohol and Other Drugs
Ask patients about alcohol consumption, medicines they are taking, and drugs they may be taking without a prescription. Advise patients not to use zolpidem tartrate tablets if they drank alcohol that evening or before bed.
Tolerance, Abuse, and Dependence
Tell patients not to increase the dose of zolpidem tartrate tablets on their own, and to inform you if they believe the drug “does not work”.
Administration Instructions
Patients should be counseled to take zolpidem tartrate tablets right before they get into bed and only when they are able to stay in bed a full night (7 to 8 hours) before being active again. Zolpidem tartrate tablets should not be taken with or immediately after a meal. Advise patients NOT to take zolpidem tartrate tablets if they drank alcohol that evening.
Manufactured In Czech Republic By:
Teva Czech Industries, s.r.o.
Opava-Komarov, Czech RepublicManufactured For:
Teva Pharmaceuticals USA, Inc.
North Wales, PA 19454Rev. J 8/2016
-
MEDICATION GUIDE
ZOLPIDEM TARTRATE (zol PI dem tar trate) Tablets USP CIV
Read the Medication Guide that comes with zolpidem tartrate tablets before you start taking them and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or treatment.
What is the most important information I should know about zolpidem tartrate tablets?
- Do not take more zolpidem tartrate tablets than prescribed.
- Do not take zolpidem tartrate tablets unless you are able to stay in bed a full night (7 to 8 hours) before you must be active again.
- Take zolpidem tartrate tablets right before you get in bed, not sooner.
Zolpidem tartrate tablets may cause serious side effects, including:
-
After taking zolpidem tartrate tablets, you may get up out of bed while not being fully awake and do an activity that you do not know you are doing. The next morning, you may not remember that you did anything during the night. You have a higher chance for doing these activities if you drink alcohol or take other medicines that make you sleepy with zolpidem tartrate tablet
s. Reported activities include:
- driving a car (“sleep-driving”)
- making and eating food
- talking on the phone
- having sex
- sleep-walking
Call your healthcare provider right away if you find out that you have done any of the above activities after taking zolpidem tartrate tablets.
Do not take zolpidem tartrate tablets if you:
- drank alcohol that evening or before bed
- took another medicine to help you sleep
What is zolpidem tartrate?
Zolpidem tartrate is a sedative-hypnotic (sleep) medicine. Zolpidem tartrate is used in adults for the short-term treatment of a sleep problem called insomnia (trouble falling asleep).
It is not known if zolpidem tartrate is safe and effective in children under the age of 18 years.
Zolpidem tartrate is a federally controlled substance (CIV) because it can be abused or lead to dependence. Keep zolpidem tartrate in a safe place to prevent misuse and abuse. Selling or giving away zolpidem tartrate may harm others, and is against the law. Tell your healthcare provider if you have ever abused or have been dependent on alcohol, prescription medicines or street drugs.
Who should not take zolpidem tartrate tablets?
- Do not take zolpidem tartrate tablets if you are allergic to zolpidem or any other ingredients in zolpidem tartrate. See the end of this Medication Guide for a complete list of ingredients in zolpidem tartrate.
- Do not take zolpidem tartrate tablets if you have had an allergic reaction to drugs containing zolpidem, such as zolpidem tartrate extended-release tablets, Edluar, Zolpimist, or Intermezzo.
Symptoms of a serious allergic reaction to zolpidem can include:
- swelling of your face, lips, and throat that may cause difficulty breathing or swallowing
What should I tell my healthcare provider before taking zolpidem tartrate tablets?
Zolpidem tartrate tablets may not be right for you. Before starting zolpidem tartrate tablets, tell your healthcare provider about all of your health conditions, including if you:
- have a history of depression, mental illness, or suicidal thoughts
- have a history of drug or alcohol abuse or addiction
- have kidney or liver disease
- have a lung disease or breathing problems
- are pregnant, planning to become pregnant. It is not known if zolpidem tartrate tablets will harm your unborn baby
- are breastfeeding or plan to breastfeed. Zolpidem tartrate can pass into your breast milk. It is not known if zolpidem tartrate tablets will harm your baby. Talk to your healthcare provider about the best way to feed your baby while you take zolpidem tartrate tablets.
Tell your healthcare provider about all of the medicines you take, including prescription and nonprescription medicines, vitamins and herbal supplements.
Medicines can interact with each other, sometimes causing serious side effects. Do not take zolpidem tartrate tablets with other medicines that can make you sleepy unless your healthcare provider tells you to.
Know the medicines you take. Keep a list of your medicines with you to show your healthcare provider and pharmacist each time you get a new medicine.
How should I take zolpidem tartrate tablets?
- See “ What is the most important information I should know about zolpidem tartrate tablets?”
- Take zolpidem tartrate tablets exactly as prescribed. Only take 1 zolpidem tartrate tablet a night if needed.
- Do not take zolpidem tartrate tablets if you drank alcohol that evening or before bed.
- You should not take zolpidem tartrate tablets with or right after a meal. Zolpidem tartrate tablets may help you fall asleep faster if you take them on an empty stomach.
- Call your healthcare provider if your insomnia worsens or is not better within 7 to 10 days. This may mean that there is another condition causing your sleep problem.
- If you take too many zolpidem tartrate tablets or overdose, get emergency treatment.
What are the possible side effects of zolpidem tartrate tablets?
Zolpidem tartrate tablets may cause serious side effects, including:
- getting out of bed while not being fully awake and do an activity that you do not know you are doing. See “ What is the most important information I should know about zolpidem tartrate tablets?”
- abnormal thoughts and behavior. Symptoms include more outgoing or aggressive behavior than normal, confusion, agitation, hallucinations, worsening of depression, and suicidal thoughts or actions.
- memory loss
- anxiety
- severe allergic reactions. Symptoms include swelling of the tongue or throat, and trouble breathing. Get emergency medical help if you get these symptoms after taking zolpidem tartrate tablets.
- falls, which may lead to severe injuries
Call your healthcare provider right away if you have any of the above side effects or any other side effects that worry you while using zolpidem tartrate tablets.
The most common side effects of zolpidem tartrate tablets are:
- drowsiness
- dizziness
- diarrhea
- grogginess or feeling as if you have been drugged
After you stop taking a sleep medicine, you may have symptoms for 1 to 2 days such as:
- trouble sleeping
- nausea
- flushing
- lightheadedness
- uncontrolled crying
- vomiting
- stomach cramps
- panic attack
- nervousness
- stomach area pain
These are not all the side effects of zolpidem tartrate tablets. Ask your healthcare provider or pharmacist for more information.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1–800–FDA–1088.
How should I store zolpidem tartrate tablets?
- Store zolpidem tartrate tablets at room temperature, 68° to 77°F (20° to 25°C).
Keep zolpidem tartrate tablets and all medicines out of reach of children.
General Information about the safe and effective use of zolpidem tartrate tablets
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use zolpidem tartrate tablets for a condition for which they were not prescribed. Do not share zolpidem tartrate tablets with other people, even if they have the same symptoms that you have. They may harm them and it is against the law.
This Medication Guide summarizes the most important information about zolpidem tartrate tablets. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about zolpidem tartrate tablets that is written for healthcare professionals.
For more information, call Teva Pharmaceuticals at 1-888-838-2872.
What are the ingredients in zolpidem tartrate tablets?
Active Ingredient: Zolpidem tartrate USP
Inactive Ingredients: hypromellose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polysorbate 80, sodium starch glycolate, and titanium dioxide; the 5 mg tablet also contains iron oxide red.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured In Czech Republic By:
TEVA Czech Industries, s.r.o.
Opava-Komarov, Czech RepublicManufactured For:
TEVA PHARMACEUTICALS USA, INC.
North Wales, PA 19454Rev. C 10/2014
- Package/Label Display Panel
-
INGREDIENTS AND APPEARANCE
ZOLPIDEM TARTRATE
zolpidem tartrate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 68071-1997(NDC:0093-0074) Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ZOLPIDEM TARTRATE (UNII: WY6W63843K) (ZOLPIDEM - UNII:7K383OQI23) ZOLPIDEM TARTRATE 10 mg Inactive Ingredients Ingredient Name Strength HYPROMELLOSE 2910 (5 MPA.S) (UNII: R75537T0T4) HYPROMELLOSE 2910 (3 MPA.S) (UNII: 0VUT3PMY82) HYPROMELLOSE 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL 400 (UNII: B697894SGQ) POLYSORBATE 80 (UNII: 6OZP39ZG8H) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color white (white to off-white) Score no score Shape ROUND Size 7mm Flavor Imprint Code TEVA;74 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 68071-1997-3 30 in 1 BOTTLE; Type 0: Not a Combination Product 12/23/2016 2 NDC: 68071-1997-2 20 in 1 BOTTLE; Type 0: Not a Combination Product 12/23/2016 3 NDC: 68071-1997-6 60 in 1 BOTTLE; Type 0: Not a Combination Product 12/23/2016 4 NDC: 68071-1997-9 90 in 1 BOTTLE; Type 0: Not a Combination Product 12/23/2016 5 NDC: 68071-1997-5 15 in 1 BOTTLE; Type 0: Not a Combination Product 12/23/2016 6 NDC: 68071-1997-1 10 in 1 BOTTLE; Type 0: Not a Combination Product 12/23/2016 7 NDC: 68071-1997-4 14 in 1 BOTTLE; Type 0: Not a Combination Product 12/23/2016 8 NDC: 68071-1997-8 28 in 1 BOTTLE; Type 0: Not a Combination Product 12/23/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076410 04/23/2007 Labeler - NuCare Pharmaceuticals, Inc. (010632300) Establishment Name Address ID/FEI Business Operations NuCare Pharmaceuticals, Inc. 010632300 repack(68071-1997)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.