Ciclopirox by Taro Pharmaceuticals, Inc. / Taro Pharmaceuticals Inc. CICLOPIROX shampoo
Ciclopirox by
Drug Labeling and Warnings
Ciclopirox by is a Prescription medication manufactured, distributed, or labeled by Taro Pharmaceuticals, Inc., Taro Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Ciclopirox Shampoo 1% contains the synthetic antifungal agent, ciclopirox.
Each gram (equivalent to 0.96 mL) of Ciclopirox Shampoo contains 10 mg ciclopirox in a shampoo base consisting of disodium laureth sulfosuccinate, laureth-2, purified water USP, sodium chloride USP and sodium laureth sulfate.
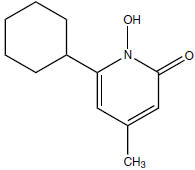
Ciclopirox Shampoo is a colorless to yellowish, translucent solution. The chemical name for ciclopirox is 6-cyclohexyl-1-hydroxy-4-methyl-2(1H)-pyridone, with the empirical formula C12H17NO2 and a molecular weight of 207.27. The CAS Registry Number is [29342-05-0]. The chemical structure is:
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Ciclopirox is a hydroxypyridone antifungal agent although the relevance of this property for the indication of seborrheic dermatitis is not known. Ciclopirox acts by chelation of polyvalent cations (Fe3+ or Al3+), resulting in the inhibition of the metal-dependent enzymes that are responsible for the degradation of peroxides within the fungal cell.
Pharmacokinetics and Pharmacodynamics
In a study in patients with seborrheic dermatitis of the scalp, application of 5 mL ciclopirox shampoo 1% twice weekly for 4 weeks, with an exposure time of 3 minutes per application, resulted in detectable serum concentrations of ciclopirox in 6 out of 18 patients. The serum concentrations measured throughout the dosing interval on Days 1 and 29 ranged from 10.3 ng/mL to 13.2 ng/mL. Total urinary excretion of ciclopirox was less than 0.5% of the administered dose.
CLINICAL STUDIES
In two randomized, double-blind clinical trials, patients 16 years and older with seborrheic dermatitis of the scalp applied Ciclopirox Shampoo or its vehicle two times per week for 4 weeks. Patients who were immunocompromised, those with psoriasis or atopic dermatitis, women of childbearing potential not using adequate contraception, and pregnant or lactating women were excluded from the clinical studies. An evaluation of the overall status of the seborrheic dermatitis, and the presence and severity of erythema or inflammation, and scaling, was made at week 4, using a scale of 0 = none, 1 = slight, 2 = mild, 3 = moderate, 4 = pronounced, and 5 = severe. Effective treatment was defined as achieving a score of 0 (or a score of 1 if the baseline score was ≥ 3) simultaneously for status of the seborrheic dermatitis, erythema or inflammation, and scaling at Week 4. Ciclopirox shampoo was shown to be statistically significantly more effective than vehicle in both studies. Efficacy results for the two studies are presented in the following table.
Effective Treatment Rates at Week 4 in Studies 1 and 2 Ciclopirox Shampoo Vehicle Study 1 220/380 (58%) 60/192 (31%) Study 2 65/250 (26%) 32/249 (13%) Efficacy for black patients was not demonstrated, although only 53 black patients were enrolled in the two pivotal studies.
Microbiology
Ciclopirox is fungicidal in vitro against Malassezia furfur (Pityrosporum spp.), P. ovale, and P. orbiculare. Ciclopirox acts by chelation of polyvalent cations (Fe3+ or Al3+), resulting in the inhibition of the metal-dependent enzymes that are responsible for the degradation of peroxides within the fungal cell.
The clinical significance of antifungal activity in the treatment of seborrheic dermatitis is not known.
- INDICATIONS AND USAGE
- CONTRAINDICATIONS
- WARNINGS
-
PRECAUTIONS
General
If a reaction suggesting sensitivity or irritation should occur with the use of Ciclopirox Shampoo, treatment should be discontinued and appropriate therapy instituted.
Contact of Ciclopirox Shampoo with the eyes should be avoided. If contact occurs, rinse thoroughly with water.
Seborrheic dermatitis may appear at puberty, however, no clinical studies have been done in patients younger than 16 years.
In patients with lighter hair color, hair discoloration has been rarely reported.
There is no relevant clinical experience with patients who have a history of immunosuppression (e.g., extensive, persistent, or unusual distribution of dermatomycoses, recent or recurring herpes zoster, or persistent herpes simplex), who are immunocompromised (e.g., HIV-infected patients and transplant patients), or who have a diabetic neuropathy.
Information for Patients
The patient should be instructed to:
- Use Ciclopirox Shampoo as directed by the physician. Avoid contact with the eyes and mucous membranes. If contact occurs, rinse thoroughly with water. Ciclopirox Shampoo is for external use on the scalp only. Do not swallow.
- Use the medication for seborrheic dermatitis for the full treatment time even though symptoms may have improved. Notify the physician if there is no improvement after 4 weeks.
- Inform the physician if the area of application shows signs of increased irritation (redness, itching, burning, blistering, swelling, or oozing) indicative of possible allergic reaction.
- Not use the medication for any disorder other than that for which it is prescribed.
Carcinogenesis, Mutagenesis, and Impairment of Fertility
Long-term animal studies have not been performed to evaluate the carcinogenic potential of Ciclopirox Shampoo or ciclopirox.
The following in vitro genotoxicity tests have been conducted with ciclopirox: evaluation of gene mutation in the Ames Salmonella and E. coli assays (negative); chromosome aberration assays in V79 Chinese hamster lung fibroblast cells, with and without metabolic activation (positive); chromosome aberration assays in V79 Chinese hamster lung fibroblast cells in the presence of supplemental Fe3+, with and without metabolic activation (negative); gene mutation assays in the HGPRT-test with V79 Chinese hamster lung fibroblast cells (negative); and a primary DNA damage assay (i.e., unscheduled DNA synthesis assay in A549 human cells) (negative). An in vitro cell transformation assay in BALB/c 3T3 cells was negative for cell transformation. In an in vivo Chinese hamster bone marrow cytogenetic assay, ciclopirox was negative for chromosome aberrations at a dosage of 5000 mg/kg body weight.
A combined oral fertility and embryofetal developmental study was conducted in rats with ciclopirox olamine. No effect on fertility or reproductive performance was noted at the highest dose tested of 3.85 mg/kg/day ciclopirox (approximately 1.3 times the maximum recommended human dose based on body surface area comparisons).
Pregnancy
Teratogenic effects
Pregnancy Category B
Oral embryofetal developmental studies were conducted in mice, rats, rabbits and monkeys. Ciclopirox or ciclopirox olamine was orally administered during the period of organogenesis. No maternal toxicity, embryotoxicity or teratogenicity were noted at the highest doses of 77, 125, 80 and 38.5 mg/kg/day ciclopirox in mice, rats, rabbits and monkeys, respectively (approximately 13, 42, 54 and 26 times the maximum recommended human dose based on body surface area comparisons, respectively).
Dermal embryofetal developmental studies were conducted in rats and rabbits with ciclopirox olamine dissolved in PEG 400. Ciclopirox olamine was topically administered during the period of organogenesis. No maternal toxicity, embryotoxicity or teratogenicity were noted at the highest doses of 92 mg/kg/day and 77 mg/kg/day ciclopirox in rats and rabbits, respectively (approximately 31 and 54 times the maximum recommended human dose based on body surface area comparisons, respectively).
There are no adequate or well-controlled studies of topically applied ciclopirox in pregnant women. Because animal reproduction studies are not always predictive of human response, Ciclopirox Shampoo should be used during pregnancy only if clearly needed.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Ciclopirox Shampoo is administered to a nursing woman.
Pediatric Use
Seborrheic dermatitis may appear at puberty, however, no clinical studies have been done in patients younger than 16 years.
Geriatric Use
In clinical studies, the safety and tolerability of Ciclopirox Shampoo in the population 65 years and older was comparable to that of younger subjects. Results of the efficacy analysis in those patients 65 years and older showed effectiveness in 25 of 85 (29%) patients treated with Ciclopirox Shampoo, and in 15 of 61 (25%) patients treated with the vehicle; due to the small sample size, a statistically significant difference was not demonstrated. Other reported clinical experience has not identified differences in responses between the elderly and younger subjects, but greater sensitivity to adverse effects in some older individuals cannot be ruled out.
-
ADVERSE REACTIONS
In 626 patients treated with Ciclopirox Shampoo twice weekly in the two pivotal clinical studies, the most frequent adverse events were increased itching in 1% of patients, and application site reactions, such as burning, erythema, and itching, also in 1% of patients. Other adverse events occurred in individual patients only.
Adverse events that led to early study medication termination in clinical trials occurred in 1.5% (26/1738) of patients treated with Ciclopirox Shampoo and 2.0% (12/661) of patients treated with shampoo vehicle. The most common adverse events leading to termination of study medication in either group was seborrhea. In the Ciclopirox Shampoo group, other adverse events included rash, pruritus, headache, ventricular tachycardia, and skin disorder. In the shampoo vehicle group, other adverse events included skin disorder and rash.
-
DOSAGE AND ADMINISTRATION
Wet hair and apply approximately 1 teaspoon (5 mL) of Ciclopirox Shampoo to the scalp. Up to 2 teaspoons (10 mL) may be used for long hair. Lather and leave on hair and scalp for 3 minutes. A timer may be used. Avoid contact with eyes. Rinse off. Treatment should be repeated twice per week for 4 weeks, with a minimum of 3 days between applications.
If a patient with seborrheic dermatitis shows no clinical improvement after 4 weeks of treatment with Ciclopirox Shampoo, the diagnosis should be reviewed.
-
HOW SUPPLIED
Ciclopirox Shampoo, 1% is supplied in 120 mL plastic bottles (NDC: 51672-1351-8). Discard unused product after initial treatment duration. Store at 20° - 25°C (68° - 77°F) [See USP Controlled Room Temperature].
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - 120 mL Carton
120 mL
NDC: 51672-1351-8
Ciclopirox
Shampoo
1%FOR TOPICAL USE ONLY
NOT FOR OPHTHALMIC,
ORAL OR INTRAVAGINAL
USEKeep this and all
medication out of the
reach of childrenThis package is not
child resistantRx only
TARO

-
INGREDIENTS AND APPEARANCE
CICLOPIROX
ciclopirox shampooProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 61360-1351 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ciclopirox (UNII: 19W019ZDRJ) (ciclopirox - UNII:19W019ZDRJ) ciclopirox 10 mg in 0.96 mL Inactive Ingredients Ingredient Name Strength disodium laureth sulfosuccinate (UNII: D6DH1DTN7E) laureth-2 (UNII: D4D38LT1L5) water (UNII: 059QF0KO0R) sodium chloride (UNII: 451W47IQ8X) sodium laureth sulfate (UNII: BPV390UAP0) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 61360-1351-8 1 in 1 CARTON 1 120 mL in 1 BOTTLE, PLASTIC Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090269 02/23/2011 Labeler - Taro Pharmaceuticals, Inc. (206263295) Establishment Name Address ID/FEI Business Operations Taro Pharmaceuticals Inc. 206263295 MANUFACTURE(61360-1351)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.