POLLENS - WEEDS AND GARDEN PLANTS, SHORT RAGWEED, AMBROSIA ARTEMISIIFOLIA- short ragweed, ambrosia artemisiifolia injection, solution POLLENS - WEEDS AND GARDEN PLANTS, RAGWEED, MIXED AMBROSIA- ragweed, mixed ambrosia injection, solution
Pollens - Weeds and Garden Plants, Ragweed, Mixed Ambrosia by
Drug Labeling and Warnings
Pollens - Weeds and Garden Plants, Ragweed, Mixed Ambrosia by is a Other medication manufactured, distributed, or labeled by Jubilant HollisterStier LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
WARNINGS
This product is intended for use only by licensed medical personnel experienced in administering allergenic extracts and trained to provide immediate emergency treatment in the event of a life-threatening reaction.
Allergenic extracts may potentially elicit a severe life-threatening systemic reaction, rarely resulting in death.1 Therefore, emergency measures and personnel trained in their use must be available immediately in the event of such a reaction. Patients should be instructed to recognize adverse reaction symptoms, be observed in the office for at least 30 minutes after skin testing or treatment, and be cautioned to contact the physician's office if symptoms occur. See ADVERSE REACTION section of this package insert regarding adverse event reporting.
This product should never be injected intravenously.
Patients with cardiovascular diseases and/or pulmonary diseases such as symptomatic unstable, steroid-dependent asthma, and/or those who are receiving cardiovascular drugs such as beta blockers, may be at higher risk for severe adverse reactions. These patients may also be more refractory to the normal allergy treatment regimen. Patients should be treated only if the benefit of treatment outweighs the risks.1
Patients on beta blockers may be more reactive to allergens given for testing or treatment and may be unresponsive to the actual doses of epinephrine used to treat allergic reactions. 2
Refer to the WARNINGS, PRECAUTIONS, ADVERSE REACTIONS and OVERDOSE Sections for further discussion.
-
DESCRIPTION
The sterile Short Ragweed or Giant and Short Ragweed Mix Allergenic Extract in this vial may be supplied for scratch, prick or puncture testing; intradermal testing; treatment; or as a "bulk" extract which is designed primarily for the physician equipped to prepare dilutions and mixtures as required.
Each concentrated lot of Short Ragweed and Giant and Short Ragweed Mix is assayed for Amb a 1 3 (also known as Antigen E) and submitted to the Center for Biologics Evaluation and Research for official release
The Amb a 1 concentrations for dilutions of extracts greater than 1:20 w/v have been obtained by calculation from the assayed value. The following is a brief description of the three expressions of concentration applied to these extracts.
1. Weight to volume (w:v). The amount of allergenic source material added to the extracting fluid. A 1:20 extract indicates that the solution contains the extractable material from one gram of raw material added to each 20 mL of extracting fluid. The amount and composition of extracted materials will vary with the kind of antigen, the extracting fluid, duration of extraction, pH, temperature, and other variables.
2. Protein Nitrogen Units (PNU). One protein nitrogen unit represents 0.00001 mg phosphotungstic acid precipitable protein nitrogen dissolved in one mL of antigen extract. The PNU content of extracts of the same antigen may vary according to the method of measuring the PNU. Thus, the PNU content of extracts from different manufacturers is not comparable unless the PNU method is known to be the same and is reproducible from lot to lot. Also, the amount of protein nitrogen extracted from an antigen is influenced by the same variables as the weight to volume extract. Allergenic materials make up a variable proportion of the total protein of an extract.
3. Of the many allergens from Short Ragweed which have been purified and characterized (Amb a 1, Amb a 2 3 (also known as Antigen K),Ra-34, Ra-4 (BPA-R)5, Ra-56, Ra6, Ra7and Ra87, and cytochrome C 8), Amb a 1 is considered the most important and has been selected as the basis for standardization. Extracts of Short Ragweed containing Amb a 1 are diffused in agar against standard anti-serum to Amb a 1, and compared to the diffusion of standard Amb a 1 solutions. The amount of Amb a 1 is expressed as units of Amb a 1 per mL of extract. Amb a 1 units are approximately equal to micrograms previously used to measure Amb a 1 concentration. The Amb a 1 assay therefore provides an absolute measure of extract potency related to the Amb a 1 antigen in Short Ragweed, rather than only an expression of extract strength.
Ingredients: Active ingredients are the allergen(s) noted on the vial label. Preservative is 50% (v/v) glycerin or 0.4% phenol, as indicated on the vial label. Glycerinated extracts contain 0.5% sodium chloride, 0.275% sodium bicarbonate and 50% glycerin (v/v) as a preservative. Non-glycerinated extracts contain 0.5% sodium chloride, 0.275% sodium bicarbonate and 0.4% phenol (w/v) as a preservative. -
CLINICAL PHARMACOLOGY
The mechanism by which hyposensitization is achieved is not known completely. It has been shown that repeated injections of appropriate allergenic extracts will ameliorate the intensity of allergic symptoms upon contact with the allergen.10, 11, 12, 13 Clinical studies which address the efficacy of immunotherapy are available. The allergens which have been studied are cat, mite, venoms, and some pollen extracts.9, 14, 15, 16, 17, 18, 19 IgE antibodies bound to receptors on mast cell membranes are required for the allergic reaction, and their level is probably related to serum IgE concentrations. Immunotherapy has been associated with decreased levels of IgE, and also with increases in allergen specific IgG "blocking" antibody.
The histamine release response of circulating basophils to a specific allergen is reduced in some patients by hyposensitization, but the mechanism of this change is not clear.
Further study and clarification of the relationships among changes in blocking antibody, reaginic antibody, and mediator-releasing cells, and between these three factors and successful immunotherapy, is needed.
-
INDICATIONS AND USAGE
20, 21, 22, 23 Allergenic extracts are indicated for use in diagnosis and immunotherapy of patients presenting symptoms of allergy (hay fever, rhinitis, etc.) to specific environmental allergens. The selection of allergenic extracts to be used should be based on a thorough and carefully taken history of hypersensitivity, and confirmed by skin testing.24, 25
The use of mixes of unrelated antigens for skin testing is not recommended since, in the case of a positive reaction, it does not indicate which component of the mix is responsible for the reaction; while, in the case of a negative reaction, it fails to indicate whether the individual antigens at full concentration would give a positive reaction. Utilization of such mixes for compounding a treatment may result, in the former case, in administering unnecessary antigens and, in the latter case, in the omission of a needed antigen.
Statistically controlled blind studies have demonstrated the effectiveness of therapy with Amb a 1.26 However, double blind studies have demonstrated a greater effectiveness for whole Short Ragweed extract when compared to Amb a 1 alone.27 Short Ragweed Extracts, standardized on the basis of Amb a 1 extract, would seem to be a logical choice for immunotherapy.
Allergens to which a patient is extremely sensitive should not be included in treatment mixes with allergens to which there is much less sensitivity, but should be administered separately. This allows individualized and better control of dosage increases, including adjustments in dosage becoming necessary after severe reactions which may occur to the highly reactive allergen.
-
CONTRAINDICATIONS
There are no known absolute contraindications to immunotherapy. See PRECAUTIONS and WARNINGS.
Patients with cardiovascular diseases and/or pulmonary diseases such as symptomatic unstable, steroid-dependent asthma, and/or those who are receiving cardiovascular drugs such as beta blockers, may be at higher risk for severe adverse reactions. These patients may also be more refractory to the normal allergy treatment regimen. Patients should be treated only if the benefit of treatment outweighs the risks.1
Treat patients only with allergens to which they are allergic by skin test reaction, have a history of symptoms on exposure, and are likely to be exposed to again.
Any injections, including immunotherapy, should be avoided in patients with a bleeding tendency.
Patients on beta blockers may be more reactive to allergens given for testing or treatment and may be unresponsive to the usual doses of epinephrine used to treat systemic reactions.2
Since there are differences of opinion concerning the possibility of routine immunizations exacerbating autoimmune diseases, immunotherapy should be given cautiously to patients with other immunologic diseases and only if the risk from exposure to the allergen is greater than the risk of exacerbating the underlying disorder. -
WARNINGS
See WARNINGS box at the beginning of this package insert. See also PRECAUTIONS.
Allergenic extracts must be temporarily withheld from patients or the dose adjusted downward if any of the following conditions exist: (1) severe symptoms of rhinitis and/or asthma; (2) infection or flu accompanied by fever; (3) any evidence of an excessively large local or generalized reaction during the initial stages of immunotherapy or during maintenance therapy, and/or (4) exposure to excessive amounts of clinically relevant allergen prior to a scheduled injection.
Do not administer immunotherapy during a period of symptoms due to exposure. Since the individual components of the extract are those to which the patient is allergic, and to which s/he will be exposed, typical allergic symptoms may follow shortly after the injection, particularly when the antigen load from exposure plus the injected antigen exceeds the patient's antigen tolerance.
THE CONCENTRATE MUST NOT BE INJECTED AT ANY TIME UNLESS TOLERANCE HAS BEEN ESTABLISHED. DILUTE CONCENTRATED EXTRACTS WITH STERILE DILUENT FOR INTRADERMAL TESTING AND IMMUNOTHERAPY.
INJECTIONS MUST NEVER BE GIVEN INTRAVENOUSLY. Subcutaneous injection is recommended. Intracutaneous or intramuscular injection may produce large local reactions or be excessively painful. AFTER INSERTING NEEDLE SUBCUTANEOUSLY, BUT BEFORE INJECTING, ALWAYS WITHDRAW THE PLUNGER SLIGHTLY. IF BLOOD APPEARS IN THE SYRINGE, CHANGE NEEDLE AND GIVE THE INJECTION IN ANOTHER SITE.
IF CHANGING TO A DIFFERENT LOT OF EXTRACT: All extracts lose potency over time, and a fresh extract could have an effective potency that is substantially greater than that of the old extract. Even though it is the same formula and concentration, the first dose from the new vial should not exceed 50% of the previous dose.
IF THE EXTRACT PREVIOUSLY USED WAS FROM ANOTHER MANUFACTURER: Since manufacturing processes and sources of raw materials differ among manufacturers, the interchangeability of extracts from different manufacturers cannot be insured. The starting dose of the extract therefore should be greatly decreased even though the extract is the same formula and dilution. In general, a dose reduction of 50% of the previous product dose should be adequate, but each situation must be evaluated separately considering the patient's history of sensitivity, tolerance of previous injections, and other factors. If the patient tolerates a 50% decrease, the next dose could be raised to the previous dose amount. If the decrease is greater than 50%, the next dose would need to be determined by the allergist, depending on the situation. Dose intervals should not exceed one week when rebuilding dose. See DOSAGE AND ADMINISTRATION.
IF A PROLONGED PERIOD OF TIME HAS ELAPSED SINCE THE LAST INJECTION: Patients may lose tolerance for allergen injections during prolonged periods between doses. The duration of tolerance is an individual characteristic and varies from patient to patient. In general, the longer the lapse in the injection schedule, the greater dose reduction required. If the interval since last dose is over four weeks, perform skin tests to determine starting dose. See DOSAGE AND ADMINISTRATION.
IF THE PREVIOUS EXTRACT WAS OUTDATED: The dating period for allergenic extracts indicates the time that they can be expected to remain potent under refrigerated storage conditions (2° - 8°C). During the storage of extracts, even under ideal conditions, some loss of potency occurs. For this reason, extracts should not be used beyond their expiration date. If a patient has been receiving injections of an outdated extract, s/he may experience excessive local or systemic reactions when changed to a new and possibly more potent extract. In general, the longer the material has been outdated, the greater the dose reduction necessary for the fresh extract.
IF CHANGING FROM ALUM-ADSORBED TO AQUEOUS OR GLYCERINATED EXTRACTS: When the patient previously has been receiving alum-adsorbed or alum-precipitated extract, the safest course is to start over as though the patient had not been receiving immunotherapy. See DOSAGE AND ADMINISTRATION and ADVERSE REACTIONS. IF ANY OTHER CHANGES HAVE BEEN MADE IN THE EXTRACT CONCENTRATE FORMULA: Changes other than those listed above may include situations such as a redistribution of component parts or percentages, a difference in extracting fluid (i.e., change from non-glycerin extracts to 50% glycerin extracts), combining two or more stock concentrates, or any other change.
It should be recognized that any change in formula can affect a patient's tolerance of the treatment. The usual 1/2 of the previous dose for a new extract may produce an adverse reaction: extra dilutions are recommended whenever starting a revised formula. The greater the change, the greater the number of dilutions required.Proper selection of the dose and careful injection should prevent most systemic reactions. It must be remembered, however, that allergenic extracts are highly potent in sensitive individuals, and that systemic reactions of varying degrees of severity may occur, including urticaria, rhinitis, conjunctivitis, wheezing, coughing, angioedema, hypotension, bradycardia, pallor, laryngeal edema, fainting, or even anaphylactic shock and death, as described underADVERSE REACTIONS. Patients should be informed of this, and the warnings and precautions should be discussed prior to immunotherapy. (See PRECAUTIONS.) Severe systemic reactions should be treated as indicated in ADVERSE REACTIONS.
-
PRECAUTIONS
1. General
The presence of asthmatic signs and symptoms appear to be an indicator for severe reactions following allergy injections. An assessment of airway obstruction either by measurement of peak flow or an alternate procedure may provide a useful indicator as to the advisability of administering an allergy injection.1, 28, 29, 30, 31
Concentrated extracts must not be injected unless tolerance has been established. Concentrated extracts must be diluted prior to use. See DOSAGE AND ADMINISTRATION for detailed instructions on the dilution of allergenic extracts.
Any evidence of a local or generalized reaction requires a reduction in dosage during the initial stages of immunotherapy, as well as during maintenance therapy. Allergenic extracts diluted with sterile Albumin Saline with Phenol (0.4%) may be more potent than extracts diluted with diluents which do not contain stabilizers. When changing from non-stabilized to stabilized diluent, consider weaker initial dilutions for both intradermal testing and immunotherapy. Dilutions for both intradermal testing and immunotherapy. Sterile solutions, vials, syringes, etc., should be used and aseptic precautions observed in making dilutions.
To avoid cross-contamination, do not use the same needle to withdraw materials from vials of more than one extract, or extract followed by diluent.
A sterile tuberculin syringe graduated in 0.01 mL units and with a needle at least 5/8" long should be used to measure each dose from the appropriate dilution. Aseptic techniques should always be employed when injections of allergenic extracts are being administered.
A separate sterile syringe should be used for each patient to prevent transmission of hepatitis and other infectious agents from one person to another. Patient reactions to previous injections should be reviewed before each new injection, so that dosage can be adjusted accordingly. See ADVERSE REACTIONS and WARNINGS.
Rarely, a patient is encountered who develops systemic reactions to minute doses of allergen and does not demonstrate increasing tolerance to injections after several months of treatment. If systemic reactions or excessive local responses occur persistently at very small doses, efforts at immunotherapy should be stopped. PATIENTS SHOULD BE OBSERVED IN THE OFFICE FOR AT LEAST 30 MINUTES AFTER SKIN TESTING AND EACH TREATMENT INJECTION. Most severe reactions will occur within this time period, and rapid treatment measures should be instituted. See ADVERSE REACTIONS for these treatment measures.
2. Information for Patients
Patients should be instructed in the recognition of adverse reactions to immunotherapy, and in particular, to the symptoms of shock. (See WARNINGS box at the beginning of this package insert.) Patients should be made to understand the importance of a 30 minute observation period following skin testing or therapeutic injections, and be cautioned to return to the office promptly if symptoms occur after leaving.
Patients should be instructed to report any symptoms of exposure to the allergen, so the physician can adjust the dosage appropriately.
3. Drug Interactions
Patients with cardiovascular diseases and/or pulmonary diseases such as symptomatic unstable, steroid-dependent asthma, and/or those who are receiving cardiovascular drugs such as beta blockers, may be at higher risk for severe adverse reactions. These patients may also be more refractory to the normal allergy treatment regimen. Patients should be treated only if the benefit of treatment outweighs the risks. 1
Patients on beta blockers may be more reactive to allergens given for testing or treatment and may be unresponsive to the usual doses of epinephrine used to treat allergic reactions.2 (See WARNINGS.)
Certain medications may lessen the skin test wheal and erythema responses elicited by allergens and histamine for varying time periods. Conventional antihistamines should be discontinued at least 5 days before skin testing. Long acting antihistamines should be discontinued for at least 3 weeks prior to skin testing. 32
Topical steroids should be discontinued at the skin test site for at least 2-3 weeks before skin testing.32, 33
Tricyclic antidepressants such as Doxepin should be withheld for at least 7 days before skin testing.34 Topical local anesthetics may suppress flare responses and should be avoided in skin test sites.35
When using other drugs in patients receiving allergenic extracts, always consult the product labeling of the other drugs to determine any possible interaction with use of allergenic extracts.4. Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have not been conducted with allergenic extracts to determine their potential for carcinogenicity, mutagenicity, or impairment of fertility.
5. Pregnancy
Animal reproduction studies have not been conducted with allergenic extracts. It is also not known whether allergenic extracts can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity.
Allergenic extracts should be given to a pregnant woman only if clearly needed. The physician must carefully consider the benefit-to-risk ratio to both patient and fetus, of performing skin testing or continuing immunotherapy during pregnancy. The recommended precautions (See WARNINGS and PRECAUTIONS) for preventing adverse reactions are especially important in the pregnant patient. Based on the physician's discretion, immunotherapy maintenance doses may be continued during pregnancy if the patient has not experienced adverse side effects. Immunotherapy is generally not initiated during pregnancy due to the risks associated with systemic reactions and their treatment.376. Nursing Mothers
There are no current studies on the secretion of allergenic extract components in human milk or their effect on the nursing infant. Because many drugs are excreted in human milk, caution should be exercised when allergenic extracts are administered to a nursing woman.
7. Pediatric Use
Since dosage for children is the same as for adults,38, 39 larger volumes of solution may produce excessive discomfort. Therefore, in order to achieve the total dose required, the volume of the dose may need to be divided into more than one injection per visit.
8. Geriatric Use
The reactions from immunotherapy can be expected to be the same in elderly patients as in younger ones. Elderly patients may be more likely to be on medication that could block the effect of epinephrine which could be used to treat serious reactions, or they could be more sensitive to the cardiovascular side effect of epinephrine because of pre-existing cardiovascular disease.40
-
ADVERSE REACTIONS
Physicians administering allergenic extract testing or treatment materials should be experienced in the treatment of severe systemic reactions. See WARNINGS box at the beginning of this package insert.
1. Local Reactions
Some erythema, swelling, or pruritus at the site of injection are common, the extent varying with the patient. Such reactions should not be considered significant unless they persist for at least 24 hours.
Local reactions (erythema or swelling) which exceed 4-5 cm in diameter are not only uncomfortable, but also indicate the possibility of a systemic reaction if dosage is increased. In such cases the dosage should be reduced to the last level not causing the reaction and maintained at this level for two or three treatments before cautiously increasing again.
Large, persistent local reactions may be treated by local cold, wet dressings and/or the use of oral antihistamines. They should be considered a warning of possible severe systemic reactions and the need for temporarily reduced dosages.
A mild burning immediately after the injection is to be expected; this usually subsides in 10 to 20 seconds.
2. Systemic Reactions
With careful attention to dosage and administration, systemic reactions occur infrequently, but it cannot be overemphasized that in sensitive individuals any injection could result in anaphylactic shock. Therefore, it is imperative that physicians administering allergenic extracts understand and be prepared for the treatment of severe reactions.
Most severe systemic reactions will begin within a 30 minute time period, but systemic reactions may occur at any time after skin tests or immunotherapy. Symptoms may range from mild to life-threatening (due to anaphylaxis) as described below.
Other possible systemic reaction symptoms which may occur in varying degrees of severity are laryngeal edema, fainting, pallor, bradycardia, hypotension, angioedema, cough, wheezing, conjunctivitis, rhinitis, and urticaria. Adverse reaction frequency data for allergenic extract administration for testing and treatment show that risk is low. 1, 41
If a systemic or anaphylactic reaction does occur, apply a tourniquet above the site of injection and inject 1:1000 epinephrine-hydrochloride intramuscularly into the opposite arm. Loosen the tourniquet at least every 10 minutes. Do not obstruct arterial blood flow with the tourniquet.
EPINEPHRINE DOSAGE
ADULT: 0.3 to 0.5 mL should be injected. Repeat in 5 to 10 minutes if necessary.
PEDIATRIC: The usual initial dose is 0.01 mg (mL) per kg body weight or 0.3 mg (mL) per square meter of body surface area. Suggested dosage for infants to 2 years of age is 0.05 mL to 0.1 mL; for children 2 to 6 years, 0.15 mL; and children 6 to 12 years, 0.2 mL. Single pediatric doses should not exceed 0.3 mg (mL). Doses may be repeated as frequently as every 20 minutes, depending on the severity of the condition and the response of the patient.After administration of epinephrine, profound shock or vasomotor collapse should be treated with intravenous fluids, and possibly vasoactive drugs. Airway patiency should be insured. Oxygen should be given by mask. Intravenous antihistamine, inhaled bronchodilators, theophylline, and/or adrenal corticosteroids may be used if necessary after adequate epinephrine and circulatory support have been given.
Emergency resuscitation measures and personnel trained in their use must be available immediately in the event of a serious systemic or anaphylactic reaction not responsive to the above measures [Ref. J. Allergy and Clinical Immunology 77(2): p. 271-273, 1986].
Rarely are all of the above measures necessary; the tourniquet and epinephrine usually produce prompt responses. However, the physician should be prepared in advance for all contingencies. Promptness in beginning emergency treatment measures is of utmost importance.Severe systemic reactions mandate a decrease of at least 50% in the next dose, followed by cautious increases. Repeated systemic reactions, even of a mild nature, are sufficient reason for the cessation of further attempts to increase the reaction-causing dose.
3. Adverse Event Reporting
Report all adverse events to Jubilant HollisterStier LLC, Customer Technical Services Department at 1(800) 992-1120. A voluntary adverse event reporting system for health professionals is available through the FDA MEDWATCH program. Preprinted forms (FDA Form 3500) are available from the FDA by calling 1(800) FDA-1088. Completed forms should be mailed to MEDWATCH, 5600 Fisher Lane, Rockville, MD 20852-9787 or Fax to: 1(800) FDA-0178. - OVERDOSAGE
-
DOSAGE AND ADMINISTRATION
21, 22, 23
1. General
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Sterile aqueous diluent containing human serum albumin [Albumin Saline with Phenol (0.4%)] or diluent of 50% glycerin may be used when preparing dilutions of the concentrate for immunotherapy. For intradermal testing dilutions, Albumin Saline with Phenol (0.4%) is recommended. Dilutions should be made accurately and aseptically, using sterile diluent, vials, syringes, etc. Mix thoroughly and gently by rocking or swirling. Maintain stock solutions and dilutions constantly at 2° - 8°C.2. Pediatric Use
The dose for the pediatric population is the same as for adults. (See PRECAUTIONS.)3. Geriatric Use
The dose for the elderly patients is the same as for adult patients under 65.404. Diagnosis
A positive reaction consists of an urticarial wheal with surrounding erythema (resembling somewhat a mosquito bite reaction) larger than the control site. The smallest reaction considered positive is erythema with a central papule at least 5 mm in diameter, however certain skin test devices may elicit a smaller positive reaction. Check the device manufacturer's recommendations. In some instances with no reaction at the control site, erythema may be considered an indication of sensitivity.A positive skin reaction to any allergen must be interpreted in light of the patient's history of symptoms, time of year, and known exposures. THE SKIN TESTS ARE IN NO WAY A SUBSTITUTE FOR A CAREFUL ALLERGIC HISTORY. THEY SERVE AS ADDITIONAL INFORMATION TO AID IN IDENTIFYING CAUSATIVE ALLERGENS IN PATIENTS WITH ALLERGIC DISORDERS.
Skin tests are graded in terms of the wheal and erythema response noted at 15 minutes. Wheal and erythema size may be recorded by actual measurement of the extent of both responses.
Refer to the following table to determine the skin test sensitivity class. The corresponding ∑E (sum of the longest diameter and the mid-point orthogonal diameters of erythema) is also presented.
Class
Wheal Diameter
Erythema Diameter
Corresponding ∑E
0
< 5 mm
<5 mm
<10 mm
±
5-10 mm
5-10 mm
10-20 mm
1+
5-10 mm
11-20 mm
20-40 mm
2+
5-10 mm
21-30 mm
40-60 mm
3+
10-15 mm a
31-40 mm
60-80 mm
4+
>15 mm b
>40 mm
>80 mm
a. or with pseudopods
b. or with many pseudopods
a. Scratch, Prick or Puncture Testing
To identify highly sensitive individuals and as a safety precaution, it is recommended that a scratch, prick or puncture test using a drop of the extract concentrate be performed prior to initiating intradermal testing. Short Ragweed extract at 1:20 w/v in 50% glycerin containing approximately 100 to 300 units of Amb a 1/mL or Giant and Short Ragweed Mix at 1:20 w/v in 50% glycerin containing approximately 50 to 150 units of Amb a 1/mL are usually used for scratch, prick or puncture testing.Scratch tests are performed by first scarifying the skin, then applying the extract to the scratch. Prick tests are performed by placing a drop of extract on the skin and piercing through the drop into the skin with a slight lifting motion. The prick is superficial and should not draw blood. Puncture tests are performed by placing a drop of extract on the skin and piercing through the drop perpendicular to the skin with a device such as a Prick Lancetter. After about 1 minute the extract may be wiped away with a dry sponge.
The diameter of wheal and erythema reactions are measured 15 minutes after the scratch, prick or puncture is made, and the sensitivity class of the patient determined by the table presented at the end of the diagnosis section. Less sensitive individuals (Class 0 to 1+) can be tested intradermally with the recommended dilutions of the extract concentrate (see Intradermal Testing)
b. Intradermal Testing
Intradermal tests should be done only on patients with a negative scratch, prick or puncture test. Patients who do not react to a valid scratch, prick or puncture test should be tested intradermally with 0.02 to 0.05 mL of extract solution. The intradermal strength for Short Ragweed extract is usually 500 PNU which by calculation contains approximately 0.7 to 3 units of Amb a 1/mL. For Giant and Short Ragweed mix, the suggested intradermal strength is 500 PNU which by calculation contains 0.4 to 1.5 units of Amb a 1/mL. These strengths are usually safe for testing patients previously having negative scratch, prick or puncture test reactions. A 1:10 dilution of the stock intradermal strength should be used in preliminary testing of patients not previously screened by scratch, prick or puncture tests. If the intradermal dilutions were prepared from glycerinated concentrate, the negative control used with this latter dilution should contain 5% glycerol. A site should be injected with 0.02 mL of the control solution. False positive reactions are sometimes encountered in intradermal testing and the possibility of irritation reactions should always be taken into consideration.
A study of ragweed sensitive patients, 42 indicates that intradermal tests, using 0.05 mL of extract, produce positive reactions (1+ to 2+) at Amb a 1 concentrations of 2.7x1-1 to 2.7x10-6 units per mL. The equivalent PNU range was 100 to 0.001 PNU per mL.
5. Immunotherapy
Dosage of allergenic extracts is a highly individualized matter and varies according to the degree of sensitivity of the patient, his or her clinical response, and tolerance to the extract administered during the early phases of an injection regimen.Allergen extracts should be administered using a sterile syringe with 0.01 mL gradations and a 25-27 gauge X 1/2" to 5/8" needle. The injections are given subcutaneously. The most common sites of injection are the lateral aspect of the upper arm or thigh. Intracutaneous or intramuscular injections may produce large local reactions which may be very painful.
To prepare dilutions for intradermal and therapeutic use, make a 1:10 dilution by adding 1.0 mL of the concentrate to 9.0 mL of the sterile aqueous diluent. Subsequent serial dilutions are made in a similar manner.
Following is a suggested schedule for average patients that will be satisfactory in most cases. However, the degree of sensitivity varies in many patients. The size of the dose should be adjusted and should be regulated by the patient's tolerance and reaction. Decrease the size of the dose if the previous injection resulted in marked local or the slightest general reaction. Another dose should never be given until all local reactions resulting from the previous dose have disappeared.
The starting dose should be based on skin tests of the extract to be used for immunotherapy. To determine the starting dose, begin intradermal testing with the most dilute extract preparation. Inject 0.02 mL and read the reaction after 15 minutes. Intradermal testing is continued with increasing concentrations of the extract until a reaction of 10-20 mm erythema (∑E 20-40 mm) and/or a 5 mm wheal occurs. This concentration at a dose of 0.03 mL then can serve as a starting dose for immunotherapy and be increased by 0.03 mL to as high as 0.12 mL increments each time until 0.3 mL is reached, at which time a dilution 10 times as strong can be used, starting with 0.03 mL. Proceed in this way until a tolerance dose is reached or symptoms are controlled. Suggested maintenance dose is 0.2 mL of the concentrate. Occasionally, higher doses are necessary to relieve symptoms. Special caution is required in administering doses greater than 0.2 mL. The interval between doses is normally 3 to 7 days during dose building regimen.
In some patients, the dosage may be increased more rapidly than called for in the schedule. In seasonal allergies, treatment should be started and the interval between doses regulated so that at least the first 20 doses will have been administered by the time symptoms are expected. Thus, the shorter the interval between the start of immunotherapy and the expected onset of symptoms, the shorter the interval between each dose. Some patients may even tolerate daily doses.
Should symptoms develop before the next injection is scheduled, the interval between doses should be decreased. Should allergic symptoms or local reactions develop shortly after the dose is administered, the size of the dose should be decreased. In seasonal allergies, it is often advisable to decrease the dose to one-half or one-quarter of the maximum dose previously attained if the patient has any seasonal symptoms.
A maintenance dose, the largest dose tolerated by the patient that relieves symptoms without producing undesirable local or general reactions, is recommended for most patients. The upper limits of dosage have not been established; however, doses larger than 0.2 mL of the glycerinated concentrate may be painful due to the glycerin content. The dosage of allergenic extract does not vary significantly with the respiratory allergic disease under treatment. The size of this dose and the interval between doses will vary and can be adjusted as necessary.
The interval between maintenance doses can be increased gradually from one week to 10 days, to two weeks, to three weeks, or even to four weeks, if tolerated. Repeat the doses at a given interval three or four times to check for untoward reactions before further increasing the interval. Protection is lost rapidly if the interval between doses is more than four weeks. (See WARNINGS Section.)
The usual duration of treatment has not been established. A period of two or three years of injection therapy constitutes an average minimum course of treatment.
In two hyposensitization studies using Amb a 1 27, 43 the amount administered over a pre-seasonal course of injections varied from 4 to 2,000 units of Amb a 1. The maximum individual dose attained ranged up to 170 units in one series.
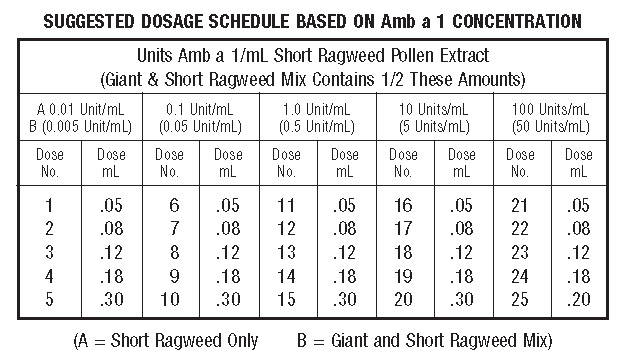
Short Ragweed pollen extracted at 1:20 (w/v) usually assays within a range of 50,000 to 70,000 PNU/mL and 100 to 300 units Amb a 1/mL. Most treatment programs use a w/v concentrate of 1:100 to 1:20 or a PNU/mL concentrate of 20,000 to 40,000. This would approximate a 100 units Amb a 1/mL average concentration of Short Ragweed extract (Giant and Short Ragweed mix would be one-half this value). The following suggested dose schedule is based on this average concentration of 100 Units/mL
The Amb a 1 content of different batches of Short Ragweed extract will vary so it will be necessary to dilute extract concentrate to the same Amb a 1 concentration when using a new lot of antigen.
Formula for calculating dilutions:
A1C1 = A2C2
A1 = Amount of extract you wish to prepare.
C1 = Concentration you wish to prepare.
A2 = Amount of extract you will need for dilution.
C2 = Concentration of extract you will use.
Formula for determining diluent required:
A1 minus A2 = Amount of diluent required.
-
HOW SUPPLIED
Scratch, Prick or Puncture Test extracts are supplied in 5 mL dropper bottles at 1:20 w/v and are preserved with glycerin. Intradermal extracts are supplied in multiple dose 5 mL vials at a concentration of 500 PNU/mL, and are preserved with phenol. Treatment sets are supplied as ordered by the physician. "Bulk" extracts are preserved with glycerin and are supplied in 10, 30 and 50 mL multidose vials at the w/v or PNU/mL ordered by the physician. Please see the current catalog or professional price
-
STORAGE
The expiration date is listed on the container label. To insure the maximum potency of Short Ragweed extract and its dilutions, it is recommended that the product be maintained at a temperature of 2° - 8°C at all times, even during use. Dilutions are less stable than the Concentrate. If loss of potency is suspected, the product should be checked by skin testing with equal units of a freshly prepared dilution on known ragweed pollen allergic individuals.
-
LIMITED WARRANTY SECTION
A number of factors beyond our control could reduce the efficacy of this product or even result in an ill effect following its use. These include storage and handling of the product after it leaves our hands, diagnosis, dosage, method of administration and biological differences in individual patients. Because of these factors, it is important that this product be stored properly and that the directions be followed carefully during use.
No warranty, express or implied, including any warranty of merchantability or fitness, is made. Representatives of the Company are not authorized to vary the terms or the contents of any printed labeling, including the package insert, for this product except by printed notice from the Company's headquarters. The prescriber and user of this product must accept the terms hereof.
-
REFERENCES
1. Lockey, R.F., L.M. Benedict, P.C. Turkeltaub, S.C. Bukantz. Fatalities from immunotherapy (IT) and skin testing (ST). J. Allergy Clin. Immunol. 79 (4): 660-677, April 1987.
2. Jacobs, R.L., G.W. Rake, Jr. et al. Potentiated anaphylaxis in patients with drug induced beta-adrenergic blockade. J. Allergy and Clin. Immunol. 68 (2): 125-127, August 1981.
3. Griffith, I.J., J. Pollock, D.G. Klapper, B.L. Rogers and A.K. Nault,. Sequence Polymorphism of Amb a I and Amb a II, the Major Allergens in Ambrosia artemisiifolia (Short Ragweed). Int. Arch. Allergy Apply. Immunol., 96: 296-304, 1991.
4. Underdown, B.J. and L. Goodfriend. Isolation and characterization of an allergen from short ragweed pollen. Biochem. 8 (3): 980-989, 1969.
5. Griffiths, B.W. and R. Brunet. Isolation of a basic protein antigen of low ragweed pollen. Can. J. Biochem. 49 (3): 396-400, 1971.
6. Lapkoff, C.B. and L. Goodfriend. Isolation of a low molecular weight ragweed allergen: Ra-5. Int. Arch. Allergy Appl. Immunol. 46 (2): 215-229, 1974.
7. Hussain, R. and D.G. Marsh. Characterization and allergenic activity of ragweed allergens Ra-6, Ra-7, Ra-8. J. Allergy Clin. Immunol. 65 (3): 230, abstr. 218, 1980.
8. Goodfriend, L., A.M. Choudhury, J. Del Carpio and T.P. King. Cytochrome C: New ragweed pollen allergen. Fed. Proc. 38 (3, part II): 1415, abstr. 6261, 1979.
9. Norman, P.S. Postgraduate Course Presentation. An overview of immunotherapy, implications for the future. J. Allergy Clin. Immunol. 65 (2): 87-96, 1980.
10. Lowell, F.C., W. Franklin. A "double-blind" study of treatment with aqueous allergenic extracts in cases of allergic rhinitis. J. Allergy 34 (2): 165-182, 1983.
11. Lowell, F.C., W. Franklin. A double-blind study of the effectiveness and specificity of injection therapy in ragweed hay fever. N. Eng. J. Med. 273 (13): 675-679, 1965.
12. Zavazal, V., A. Stajner. Immunologic changes during specific treatment of the atopic state. II. Acta. Allergol. 25 (1): 11-17, 1970.
13. Reisman, R.E., J.I. Wypych, E.E. Arbesman. Relationships of immunotherapy, seasonal pollen exposure and clinical response to serum concentrations of total IgE and ragweed-specific IgE. Int. Arch. Allergy Appl. Immunol. 48 (6): 721-730, 1975.
14. Chapman, M.D., T.A.E. Platts-Mills, M. Gabriel, H.K. Ng, W.G.L. Allen, L.E. Hill, A.J. Nunn. Antibody response following prolonged hyposensitization with Dermatophagoides pteronyssinus extract. Int. Arch. Allergy Appl. Immunol. 61: 431-440, 1980.
15. Norman, P.S., W.L. Winkenwerder. Maintenance immunotherapy in ragweed hay fever. J. Allergy 74: 273-282, 1971.
16. Norman, P.S., W.L. Winkenwerder, L.M. Lichtenstein. Immunotherapy of hay fever with ragweed Antigen E; comparisons with whole pollen extract and placebos. J.Allergy 42: 93-108, 1968.
17. Ohman, J.L., S.R. Findlay, K. Leiterman. Immunotherapy in cat-induced asthma: double-blind trial with evaluation of in vivo and vitro responses. J. Allergy Clin. Immunol. 74: 230, 1984.
18. Sundin, B., G. Lilja, V. Graff-Lonnevig, G. Hedlin, H. Heilborn, K. Norrlind, K-O Pegelow, and H. Lowenstein. Immunotherapy with partially purified and standardized animal dander extracts. I Clinical results from a double-blind study on patients with animal dander asthma. J. Allergy Clin. Immunol. 77: 478, 1986.
19. Hunt, K.J., Valentine, M.D., Sobotka, A.K., Benton, A.W., Amodio, F.J., and Lichtenstein, L.M. A controlled trial of immunotherapy in insect hypersensitivity. New Eng. J. Med. 299: 157-161, July 27, 1978.
20. Middleton, E., C.E. Reed and E.F. Ellis (Eds.). Allergy Principles and Practice. C.V. Mosby Co., St. Louis, 1978, pp. 877-898.
21. Sheldon, J.M., R.G. Lovell and K.P. Mathews. A Manual of Clinical Allergy, Second Edition, W.B. Saunders, Philadelphia, 1967, pp. 107-112.
22. Sherman, W.B. Hypersensitivity Mechanism and Management. W.B. Saunders, Philadelphia, 1968, pp. 169-172.
23. Swineford, O. Asthma and Hay Fever. Charles C. Thomas, Springfield, IL, 1971, pp. 148-155.
24. Pauli, G., J.D. Bessot, R. Thierry, and A. Lamensons. Correlation between skin tests, inhalation tests and specific IgE in a study of 120 subjects to house dust and D. pteronyssinus. Clin. Allergy 7:337, 1977.
25. Murray, A.B., A.C. Ferguson and B.J. Morrison. Diagnosis of house dust mite allergy in asthmatic children: What constitutes positive history. J. Allergy Clin. Immunol. 71:21, 1983.
26. Lichtenstein, L.M., P.S. Norman and W.L. Winkenwerder. Clinical and in vitro studies on the role of immunotherapy in ragweed hay fever. Amer. J. Med. 44 (4): 514-524, 1968.
27. Reisman, R.E., K. Wicher and C.E. Arbesman. Immunotherapy with Antigen E. J. Allergy 44 (2): 82-95, 1969.
28. Reid, M.J., R.F. Lockey, P.C. Turkletaub, T.A.E., Platts-Mills. Survey of fatalities from skin testing and immunotherapy. J. Allergy Clin. Immunol. 92 (1): 6-15, July 1993.
29. Reid, M.J., G. Gurka. Deaths associated with skin testing and immunotherapy. J.Allergy Clin. Immunol. 97(1) Part 3:231, Abstract 195, January 1996.
30. Thompson, R.A., et al, report of a WHO/IUIS working group. The current status of allergen immunotherapy (hyposensitization). Allergy. 44: 369-379, 1989.
31. Malling, H.J., B. Weeke, et al, The European Academy of Allergology and Clinical Immunology. Position Papers. Allergy. 48 (Supplement 14): 9-82, 1993.
32. Pipkorn, U. Pharmacological influence of anti-allergic medication on in Vivo allergen testing. Allergy 43: 81-86, 1988.
33. Andersson, M. and U. Pipkorn. Inhibition of the dermal immediate allergic reaction through prolonged treatment with topical glucocorticosteroids. J. Allergy Clinical Immunology 79 (2): 345-349, February 1987.
34. Rao, K.S., et al. Duration of suppressive effect of tricyclic antidepressants on histamine induced wheal and flare reactions on human skin. Allergy Clinical Immunology 82: 752-757, November 1988.
35. Pipkorn, U., and M. Andersson. Topical dermal anesthesia inhibits the flare but not the wheal response to allergen and histamine in the skin prick test. Clinical Allergy 17: 307-311, 1987.
36. Metzger, W.J., E. Turner and R. Patterson. The safety of immunotherapy during pregnancy. J. Allergy Clin. Immunol. 61 (4): 268-272, 1978.
37. Li, J.T., R.F. Lockey, I.L. Bernstein, J.M. Portnoy, R.A. Nicklas. Allergen Immunotherapy: A Practice Parameter. Ann. Allergy, Asthma and Immunotherapy 90 (1): 26, 2003.
38. Patterson, R., et al. Allergy Principles and Practice, 2nd ed. E. Middleton, Jr., C.E. Reed, E.F. Ellis, Ed., C.V. Mosby Co., St. Louis, MO, 1983, Chapter 52.
39. Levy, D.A., L.M. Lichtenstein, E.O. Goldstein, and K. Ishizaka. Immunologic and cellular changes accompanying the therapy of pollen allergy. J. Clinical Investigation 50: 360, 1971.
40. Peebles, R.S., Jr., B. Bochner, H.J. Zeitz, ed. Anaphylaxis in the elderly. Immunology and Allergy Clinics of North America. 13 (3): 627-646, August 1993.
41. Turkeltaub, P.C., MD, and P.J. Gergen, MD. The risk of adverse reactions from percutaneous prick-puncture allergen skin testing, venipuncture, and body measurements: Data from the second National Health and Nutrition Examination Survey 1976-80 (NHANES II). J. Allergy Clin. Immunol. 84 (6): 886-890, Dec. 1989.
42. Norman, P.S., L.M. Lichtenstein, and K. Ishizaka. Diagnostic tests in ragweed hay fever. J. Allergy Clin. Immunol. 52 (4): 212-224, 1973.
43. Lichtenstein, L.M., P.S. Norman and W.L. Winkenwerd. A single year of immunotherapy for ragweed hay fever. Immunologic and clinical studies. Ann. Int. Med. 75 (5): 663-671, 1971. - Ragweed Mix 5 mL, 1:20 w/v Carton Label
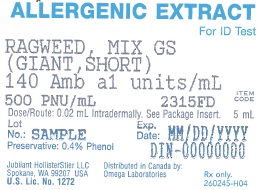
- Ragweed Mix 5 mL, 1:20 w/v Vial Label
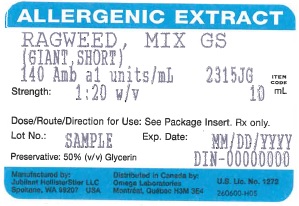
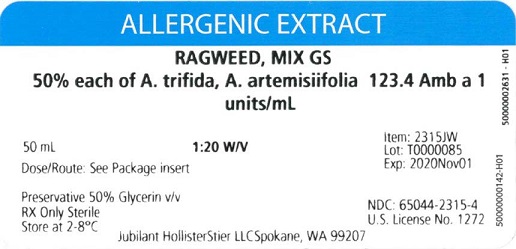
- Ragweed Mix 10 mL, 1:20 w/v Carton Label
- Ragweed Mix 10 mL, 1:20 w/v Vial Label
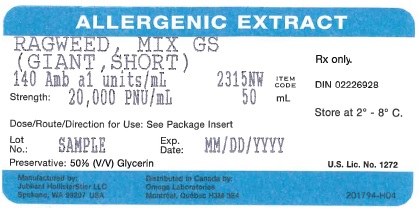
- Ragweed Mix 50 mL, 1:20 w/v Carton Label
- Ragweed Mix 50 mL, 1:20 w/v Vial Label
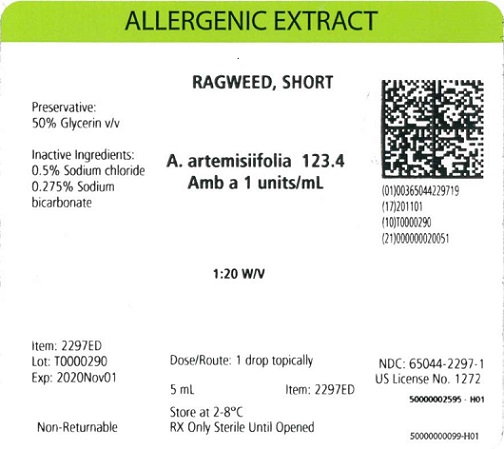
- Standardized Short Ragweed 5 mL, 1:20 w/v Carton Label
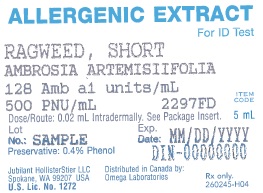
- Standardized Short Ragweed 5 mL, 1:20 w/v Vial Label
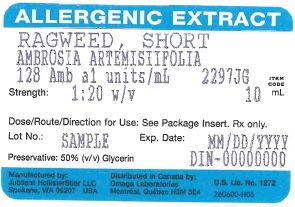
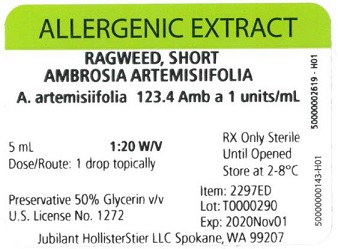
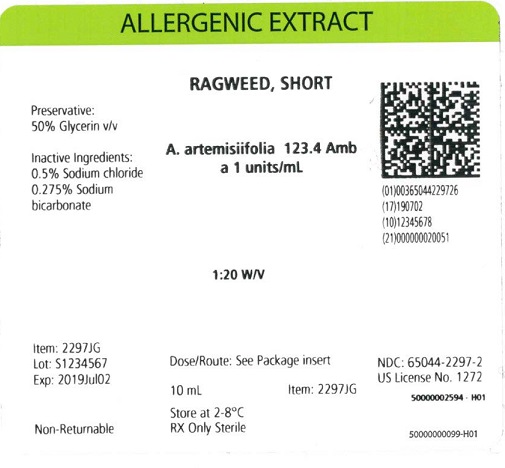
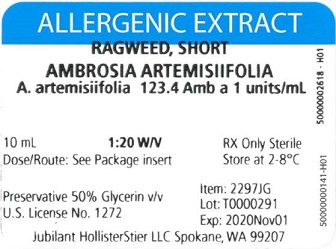
- Standardized Short Ragweed 10 mL, 1:20 w/v Carton Label
- Standardized Short Ragweed 10 mL, 1:20 w/v Vial Label
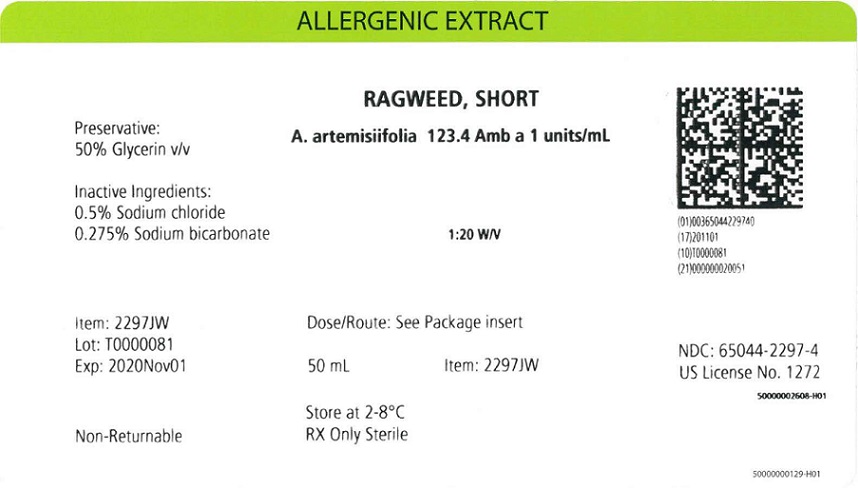
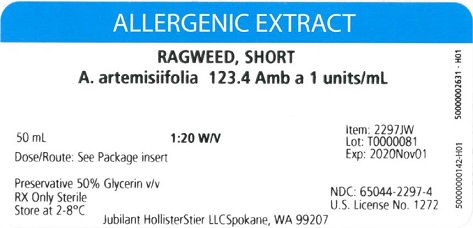
- Standardized Short Ragweed 50 mL, 1:20 w/v Carton Label
- Standardized Short Ragweed 50 mL, 1:20 w/v Vial Label
-
INGREDIENTS AND APPEARANCE
POLLENS - WEEDS AND GARDEN PLANTS, SHORT RAGWEED, AMBROSIA ARTEMISIIFOLIA
short ragweed, ambrosia artemisiifolia injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 65044-2297 Route of Administration PERCUTANEOUS, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMBROSIA ARTEMISIIFOLIA POLLEN (UNII: K20Y81ACO3) (AMBROSIA ARTEMISIIFOLIA POLLEN - UNII:K20Y81ACO3) AMBROSIA ARTEMISIIFOLIA POLLEN 0.05 g in 1 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM BICARBONATE (UNII: 8MDF5V39QO) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65044-2297-1 5 mL in 1 VIAL; Type 0: Not a Combination Product 2 NDC: 65044-2297-2 10 mL in 1 VIAL; Type 0: Not a Combination Product 3 NDC: 65044-2297-3 30 mL in 1 VIAL; Type 0: Not a Combination Product 4 NDC: 65044-2297-4 50 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103880 10/18/1977 POLLENS - WEEDS AND GARDEN PLANTS, SHORT RAGWEED, AMBROSIA ARTEMISIIFOLIA
short ragweed, ambrosia artemisiifolia injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 65044-2298 Route of Administration INTRADERMAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMBROSIA ARTEMISIIFOLIA POLLEN (UNII: K20Y81ACO3) (AMBROSIA ARTEMISIIFOLIA POLLEN - UNII:K20Y81ACO3) AMBROSIA ARTEMISIIFOLIA POLLEN 500 [PNU] in 1 mL Inactive Ingredients Ingredient Name Strength PHENOL (UNII: 339NCG44TV) SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM BICARBONATE (UNII: 8MDF5V39QO) GLYCERIN (UNII: PDC6A3C0OX) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65044-2298-5 5 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103880 10/18/1977 POLLENS - WEEDS AND GARDEN PLANTS, RAGWEED, MIXED AMBROSIA
ragweed, mixed ambrosia injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 65044-2315 Route of Administration PERCUTANEOUS, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMBROSIA TRIFIDA POLLEN (UNII: KU1V1898XX) (AMBROSIA TRIFIDA POLLEN - UNII:KU1V1898XX) AMBROSIA TRIFIDA POLLEN 0.05 g in 1 mL AMBROSIA ARTEMISIIFOLIA POLLEN (UNII: K20Y81ACO3) (AMBROSIA ARTEMISIIFOLIA POLLEN - UNII:K20Y81ACO3) AMBROSIA ARTEMISIIFOLIA POLLEN 0.05 g in 1 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM BICARBONATE (UNII: 8MDF5V39QO) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65044-2315-1 5 mL in 1 VIAL; Type 0: Not a Combination Product 2 NDC: 65044-2315-2 10 mL in 1 VIAL; Type 0: Not a Combination Product 3 NDC: 65044-2315-3 30 mL in 1 VIAL; Type 0: Not a Combination Product 4 NDC: 65044-2315-4 50 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103880 10/18/1977 POLLENS - WEEDS AND GARDEN PLANTS, RAGWEED, MIXED AMBROSIA
ragweed, mixed ambrosia injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 65044-2316 Route of Administration INTRADERMAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMBROSIA TRIFIDA POLLEN (UNII: KU1V1898XX) (AMBROSIA TRIFIDA POLLEN - UNII:KU1V1898XX) AMBROSIA TRIFIDA POLLEN 500 [PNU] in 1 mL AMBROSIA ARTEMISIIFOLIA POLLEN (UNII: K20Y81ACO3) (AMBROSIA ARTEMISIIFOLIA POLLEN - UNII:K20Y81ACO3) AMBROSIA ARTEMISIIFOLIA POLLEN 500 [PNU] in 1 mL Inactive Ingredients Ingredient Name Strength PHENOL (UNII: 339NCG44TV) SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM BICARBONATE (UNII: 8MDF5V39QO) GLYCERIN (UNII: PDC6A3C0OX) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65044-2316-5 5 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103880 10/18/1977 POLLENS - WEEDS AND GARDEN PLANTS, RAGWEED, MIXED AMBROSIA
ragweed, mixed ambrosia injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 65044-2317 Route of Administration PERCUTANEOUS, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMBROSIA TRIFIDA POLLEN (UNII: KU1V1898XX) (AMBROSIA TRIFIDA POLLEN - UNII:KU1V1898XX) AMBROSIA TRIFIDA POLLEN 20000 [PNU] in 1 mL AMBROSIA ARTEMISIIFOLIA POLLEN (UNII: K20Y81ACO3) (AMBROSIA ARTEMISIIFOLIA POLLEN - UNII:K20Y81ACO3) AMBROSIA ARTEMISIIFOLIA POLLEN 20000 [PNU] in 1 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM BICARBONATE (UNII: 8MDF5V39QO) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65044-2317-2 10 mL in 1 VIAL; Type 0: Not a Combination Product 2 NDC: 65044-2317-3 30 mL in 1 VIAL; Type 0: Not a Combination Product 3 NDC: 65044-2317-4 50 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103880 10/18/1977 Labeler - Jubilant HollisterStier LLC (069263643) Registrant - Jubilant HollisterStier LLC (069263643)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.