CARDIOLITE (tetrakis(2-methoxyisobutylisocyanide)copper- i tetrafluoroborate injection, powder, lyophilized, for solution
Cardiolite by
Drug Labeling and Warnings
Cardiolite by is a Prescription medication manufactured, distributed, or labeled by Lantheus Medical Imaging, Inc., Jubilant HollisterStier LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use CARDIOLITE® safely and effectively. See full prescribing information for CARDIOLITE®.
CARDIOLITE®, Kit for the Preparation of Technetium Tc99m Sestamibi for Injection
Initial U.S. Approval: December, 1990INDICATIONS AND USAGE
CARDIOLITE® is a myocardial perfusion agent indicated for: (1)
- detecting coronary artery disease by localizing myocardial ischemia (reversible defects) and infarction (non-reversible defects)
- evaluating myocardial function and developing information for use in patient management decisions
DOSAGE AND ADMINISTRATION
- For Myocardial Imaging: The suggested dose range for I.V. administration of CARDIOLITE® in a single dose to be employed in the average patient (70 Kg) is 370 - 1110 MBq (10 - 30 mCi).
- For Breast Imaging: The recommended dose range for I.V. administration of MIRALUMA® is a single dose of 740 - 1110 MBq (20 - 30 mCi).
DOSAGE FORMS AND STRENGTHS
CARDIOLITE®, Kit for the Preparation of Technetium Tc99m Sestamibi for Injection is supplied as a lyophilized mixture in a 5 mL vial. (3)
CONTRAINDICATIONS
- None known.
WARNINGS AND PRECAUTIONS
- Pharmacologic induction of cardiovascular stress may be associated with serious adverse events such as myocardial infarction, arrhythmia, hypotension, bronchoconstriction and cerebrovascular events.
- CARDIOLITE® has been rarely associated with acute severe allergic and anaphylactic events of angioedema and generalized urticaria. In some patients the allergic symptoms developed on the second injection during CARDIOLITE® imaging.
- Caution should be exercised and emergency equipment should be available when administering CARDIOLITE®.
- Before administering CARDIOLITE® patients should be asked about the possibility of allergic reactions to either drug.
- The contents of the vial are intended only for use in the preparation of Technetium Tc99m Sestamibi and are not to be administered directly to the patient without first undergoing the preparative procedure.
ADVERSE REACTIONS
The following adverse reactions have been reported in ≤ 0.5% of patients: signs and symptoms consistent with seizure occurring shortly after administration of the agent; transient arthritis, angioedema, arrythmia, dizziness, syncope, abdominal pain, vomiting, and severe hypersensitivity characterized by dyspnea, hypotension, bradycardia, asthenia, and vomiting within two hours after a second injection of Technetium Tc99m Sestamibi. A few cases of flushing, edema, injection site inflammation, dry mouth, fever, pruritis, rash, urticaria and fatigue have also been attributed to administration of the agent. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Lantheus Medical Imaging, Inc. at 1-800-362-2668 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. (6)
DRUG INTERACTIONS
- Specific drug-drug interactions have not been studied.
USE IN SPECIFIC POPULATIONS
- In one study of 46 subjects who received CARDIOLITE® administration, the radioactivity in both children and adolescents exhibited blood PK profiles similar to those previously reported in adults.
- Lactation: Interruption of breastfeeding after exposure to Technetium Tc99m Sestamibi is not necessary, however, a lactating woman should be advised to consider restricting close contact with her breast fed infant to a maximum of 5 hours in the 24 hour period after Technetium Tc99m Sestamibi administration in order to minimize radiation exposure. (8.2)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1. INDICATIONS AND USAGE
2. DOSAGE AND ADMINISTRATION
2.1 Image Acquisition
2.2 Radiation Dosimetry
2.3 Instructions For Preparation
2.4 Determination of Radiochemical Purity in Technetium Tc99m Sestamibi
3. DOSAGE FORMS AND STRENGTHS
4. CONTRAINDICATIONS
5. WARNINGS AND PRECAUTIONS
5.1 Warnings
5.2 General Precautions
6. ADVERSE REACTIONS
7. DRUG INTERACTIONS
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10. OVERDOSAGE
11. DESCRIPTION
11.1 Physical Characteristics
11.2 External Radiation
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14. CLINICAL STUDIES
16. HOW SUPPLIED/STORAGE AND HANDLING
17. PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1. INDICATIONS AND USAGE
Myocardial Imaging: CARDIOLITE®, Kit for the Preparation of Technetium Tc99m Sestamibi for Injection, is a myocardial perfusion agent that is indicated for detecting coronary artery disease by localizing myocardial ischemia (reversible defects) and infarction (non-reversible defects), in evaluating myocardial function and developing information for use in patient management decisions. CARDIOLITE® evaluation of myocardial ischemia can be accomplished with rest and cardiovascular stress techniques (e.g., exercise or pharmacologic stress in accordance with the pharmacologic stress agent's labeling).
It is usually not possible to determine the age of a myocardial infarction or to differentiate a recent myocardial infarction from ischemia.
Breast Imaging: MIRALUMA®, Kit for the Preparation of Technetium Tc99m Sestamibi for Injection, is indicated for planar imaging as a second line diagnostic drug after mammography to assist in the evaluation of breast lesions in patients with an abnormal mammogram or a palpable breast mass.
MIRALUMA® is not indicated for breast cancer screening, to confirm the presence or absence of malignancy, and it is not an alternative to biopsy.
-
2. DOSAGE AND ADMINISTRATION
For Myocardial Imaging: The suggested dose range for I.V. administration of CARDIOLITE® in a single dose to be employed in the average patient (70 Kg) is 370 - 1110 MBq (10 - 30 mCi).
For Breast Imaging: The recommended dose range for I.V. administration of MIRALUMA® is a single dose of 740 - 1110 MBq (20 - 30 mCi).
2.1 Image Acquisition
Breast Imaging: It is recommended that images are obtained with a table overlay to separate breast tissue from the myocardium and liver, and to exclude potential activity that may be present in the opposite breast. For lateral images, position the patient prone with the isolateral arm comfortably above the head, shoulders flat against the table, head turned to the side and relaxed, with the breast imaged pendent through an overlay cutout. The breast should not be compressed on the overlay. For anterior images, position the patient supine with both arms behind the head. For either lateral or anterior images, shield the chest and abdominal organs, or remove them from the field of view.
For complete study, sets of images should be obtained five minutes after the injection, and in the following sequence:
Beginning five minutes after the injection of Technetium Tc99m Sestamibi:
- ten-minute lateral image of breast with abnormality
- ten-minute lateral image of contralateral breast
- ten-minute anterior image of both breasts
2.2 Radiation Dosimetry
The radiation doses to organs and tissues of an average patient (70 Kg) per 1110 MBq (30 mCi) of Technetium Tc99m Sestamibi injected intravenously are shown in Table 1.0.
Table 1.0. Radiation Absorbed Doses from Tc99m Sestamibi Estimated Radiation Absorbed Dose Radiation dosimetry calculations performed by Radiation Internal Dose Information Center, Oak Ridge Institute for Science and Education, PO Box 117, Oak Ridge, TN 37831-0117. REST 2.0 hour void 4.8 hour void Organ rads/
30 mCimGy/
1110 MBqrads/
30 mCimGy/
1110 MBqBreasts 0.2 2.0 0.2 1.9 Gallbladder Wall 2.0 20.0 2.0 20.0 Small Intestine 3.0 30.0 3.0 30.0 Upper Large Intestine Wall 5.4 55.5 5.4 55.5 Lower Large Intestine Wall 3.9 40.0 4.2 41.1 Stomach Wall 0.6 6.1 0.6 5.8 Heart Wall 0.5 5.1 0.5 4.9 Kidneys 2.0 20.0 2.0 20.0 Liver 0.6 5.8 0.6 5.7 Lungs 0.3 2.8 0.3 2.7 Bone Surfaces 0.7 6.8 0.7 6.4 Thyroid 0.7 7.0 0.7 7.0 Ovaries 1.5 15.5 1.6 15.5 Testes 0.3 3.4 0.4 3.9 Red Marrow 0.5 5.1 0.5 5.0 Urinary Bladder Wall 2.0 20.0 4.2 41.1 Total Body 0.5 4.8 0.5 4.8 STRESS 2.0 hour void 4.8 hour void Organ rads/
30 mCimGy/
1110 MBqrads/
30 mCimGy/
1110 MBqBreasts 0.2 2.0 0.2 1.8 Gallbladder Wall 2.8 28.9 2.8 27.8 Small Intestine 2.4 24.4 2.4 24.4 Upper Large Intestine Wall 4.5 44.4 4.5 44.4 Lower Large Intestine Wall 3.3 32.2 3.3 32.2 Stomach Wall 0.6 5.3 0.5 5.2 Heart Wall 0.5 5.6 0.5 5.3 Kidneys 1.7 16.7 1.7 16.7 Liver 0.4 4.2 0.4 4.1 Lungs 0.3 2.6 0.2 2.4 Bone Surfaces 0.6 6.2 0.6 6.0 Thyroid 0.3 2.7 0.2 2.4 Ovaries 1.2 12.2 1.3 13.3 Testes 0.3 3.1 0.3 3.4 Red Marrow 0.5 4.6 0.5 4.4 Urinary Bladder Wall 1.5 15.5 3.0 30.0 Total Body 0.4 4.2 0.4 4.2 2.3 Instructions For Preparation
Preparation of the Technetium Tc99m Sestamibi from the Kit for the Preparation of Technetium Tc99m Sestamibi is done by the following aseptic procedure:
General Procedure:
- a. Prior to adding the Sodium Pertechnetate Tc99m Injection to the vial, inspect the vial carefully for the presence of damage, particularly cracks, and do not use the vial if found. Tear off a radiation symbol and attach it to the neck of the vial.
- b. Waterproof gloves should be worn during the preparation procedure. Remove the plastic disc from the vial and swab the top of the vial closure with alcohol to sanitize the surface.
Boiling Water Bath Procedure:
- c. Place the vial in a suitable radiation shield with a fitted radiation cap.
- d. With a sterile shielded syringe, aseptically obtain additive-free, sterile, non-pyrogenic Sodium Pertechnetate Tc99m Injection [925 - 5550 MBq, (25 - 150 mCi)] in approximately 1 to 3 mL.
- e. Aseptically add the Sodium Pertechnetate Tc99m Injection to the vial in the lead shield. Without withdrawing the needle, remove an equal volume of headspace to maintain atmospheric pressure within the vial.
- f. Shake vigorously, about 5 to 10 quick upward-downward motions.
- g. Remove the vial from the lead shield and place upright in an appropriately shielded and contained boiling water bath, such that the vial is suspended above the bottom of the bath, and boil for 10 minutes. Timing for 10 minutes is begun as soon as the water begins to boil again. Do not allow the boiling water to come in contact with the aluminum crimp.
- h. Remove the vial from the water bath, place in the lead shield and allow to cool for fifteen minutes.
Recon-o-Stat (thermal cycler) Procedure:
- c. Place the vial in the thermal cycler radiation shield.
- d. With a sterile shielded syringe, aseptically obtain additive-free, sterile, non-pyrogenic Sodium Pertechnetate Tc99m Injection [925 - 5550 MBq, (25 - 150 mCi)] in approximately 1 to 3 mL.
- e. Aseptically add the Sodium Pertechnetate Tc99m Injection to the vial in the lead shield. Without withdrawing the needle, remove an equal volume of headspace to maintain atmospheric pressure within the vial.
- f. Shake vigorously, about 5 to 10 quick upward-downward motions.
- g. Place shield on sample block. While slightly pressing downward, give the shield a quarter turn to make certain there is a firm fit between the shield and the sample block.
- h. Press the proceed button to initiate the program (the thermal cycler automatically heats & cools the vial and contents). Please see the Recon-o-Stat Instruction Manual for further details.
General Procedure (cont.):
- i. Using proper shielding, the vial contents should be visually inspected. Use only if the solution is clear and free of particulate matter and discoloration.
- j. Assay the reaction vial using a suitable radioactivity calibration system. Record the Technetium Tc99m concentration, total volume, assay time and date, expiration time and lot number on the vial shield label and affix the label to the shield.
- k. Store the reaction vial containing the Technetium Tc99m Sestamibi at 15° to 25°C (59° - 77°F) until use; at such time the product should be aseptically withdrawn. Technetium Tc99m Sestamibi should be used within six hours of preparation. The vial contains no preservative.
Note: Adherence to the above product reconstitution instructions is recommended. The potential for cracking and significant contamination exists whenever vials containing radioactive material are heated. Product should be used within 6 hours after preparation. Final product with radiochemical purity of at least 90% was used in the clinical trials that established safety and effectiveness. The radiochemical purity was determined by the following method. 2.4 Determination of Radiochemical Purity in Technetium Tc99m Sestamibi
- Obtain a Baker-Flex Aluminum Oxide coated, plastic TLC plate, #1 B-F, pre-cut to 2.5 cm × 7.5 cm.
- Dry the plate or plates at 100°C for 1 hour and store in a desiccator. Remove pre-dried plate from the desiccator just prior to use.
- Apply 1 drop of ethanol1 using a 1 mL syringe with a 22-26 gauge needle, 1.5 cm from the bottom of the plate. THE SPOT SHOULD NOT BE ALLOWED TO DRY.
- Add 2 drops of Technetium Tc99m Sestamibi solution, side by side on top of the ethanol1 spot. Return the plate to a desiccator and allow the sample spot to dry (typically 15 minutes).
- The TLC tank is prepared by pouring ethanol1 to a depth of 3-4 mm. Cover the tank and let it equilibrate for ~10 minutes.
- Develop the plate in the covered TLC tank in ethanol1 for a distance of 5 cm from the point of application.
- Cut the TLC plate 4 cm from the bottom and measure the Tc99m activity in each piece by appropriate radiation detector.
- Calculate the % Tc99m Sestamibi as:
% Tc99m Sestamibi = µCi Top Piece × 100 µCi Both Pieces
Figure 1.0 TLC Plate Diagram 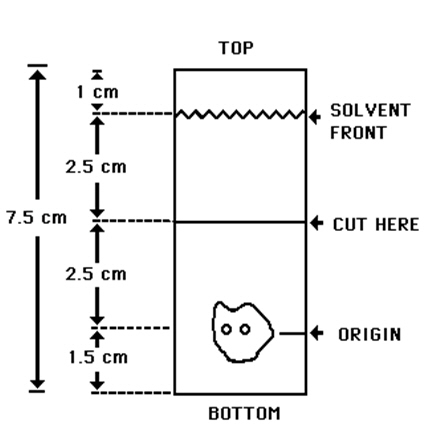
- 1 The ethanol used in this procedure should be 95% or greater. Absolute ethanol (99%) should remain at ≥ 95% ethanol content for one week after opening if stored tightly capped, in a cool dry place.
- 3. DOSAGE FORMS AND STRENGTHS
- 4. CONTRAINDICATIONS
-
5. WARNINGS AND PRECAUTIONS
5.1 Warnings
In studying patients in whom cardiac disease is known or suspected, care should be taken to assure continuous monitoring and treatment in accordance with safe, accepted clinical procedure. Infrequently, death has occurred 4 to 24 hours after Tc99m Sestamibi use and is usually associated with exercise stress testing (See Section 5.2 ).
Pharmacologic induction of cardiovascular stress may be associated with serious adverse events such as myocardial infarction, arrhythmia, hypotension, bronchoconstriction and cerebrovascular events. Caution should be used when pharmacologic stress is selected as an alternative to exercise; it should be used when indicated and in accordance with the pharmacologic stress agent's labeling.
Technetium Tc99m Sestamibi has been rarely associated with acute severe allergic and anaphylactic events of angioedema and generalized urticaria. In some patients the allergic symptoms developed on the second injection during CARDIOLITE® imaging. Patients who receive CARDIOLITE® or MIRALUMA® imaging are receiving the same drug. Caution should be exercised and emergency equipment should be available when administering Technetium Tc99m Sestamibi. Also, before administering either CARDIOLITE® or MIRALUMA®, patients should be asked about the possibility of allergic reactions to either drug.
5.2 General Precautions
The contents of the vial are intended only for use in the preparation of Technetium Tc99m Sestamibi and are not to be administered directly to the patient without first undergoing the preparative procedure.
Radioactive drugs must be handled with care and appropriate safety measures should be used to minimize radiation exposure to clinical personnel. Also, care should be taken to minimize radiation exposure to the patients consistent with proper patient management.
Contents of the kit before preparation are not radioactive. However, after the Sodium Pertechnetate Tc99m Injection is added, adequate shielding of the final preparation must be maintained. The components of the kit are sterile and non-pyrogenic. It is essential to follow directions carefully and to adhere to strict aseptic procedures during preparation.
Technetium Tc99m labeling reactions depend on maintaining the stannous ion in the reduced state. Hence, Sodium Pertechnetate Tc99m Injection containing oxidants should not be used.
Technetium Tc99m Sestamibi should not be used more than six hours after preparation.
Radiopharmaceuticals should be used only by physicians who are qualified by training and experience in the safe use and handling of radionuclides and whose experience and training have been approved by the appropriate government agency authorized to license the use of radionuclides.
Stress testing should be performed only under the supervision of a qualified physician and in a laboratory equipped with appropriate resuscitation and support apparatus.
The most frequent exercise stress test endpoints sufficient to stop the test reported during controlled studies (two-thirds were cardiac patients) were:
Fatigue 35% Dyspnea 17% Chest Pain 16% ST-depression 7% Arrhythmia 1% -
6. ADVERSE REACTIONS
Adverse events were evaluated in 3741 adults who were evaluated in clinical studies. Of these patients, 3068 (77% men, 22% women, and 0.7% of the patient's genders were not recorded) were in cardiac clinical trials and 673 (100% women) in breast imaging trials. Cases of angina, chest pain, and death have occurred (see Section 5 ). Adverse events reported at a rate of 0.5% or greater after receiving Technetium Tc99m Sestamibi administration are shown in the following table:
Table 2.0 Selected Adverse Events Reported in > 0.5% of Patients Who Received Technetium Tc99m Sestamibi in Either Breast or Cardiac Clinical Studies* Body System Breast Studies Cardiac Studies Women
n = 673Women
n = 685Men
n = 2361Total
n = 3046- * Excludes the 22 patients whose gender was not recorded.
Body as a Whole 21 (3.1%) 6 (0.9%) 17 (0.7%) 23 (0.8%) Headache 11 (1.6%) 2 (0.3%) 4 (0.2%) 6 (0.2%) Cardiovascular 9 (1.3%) 24 (3.5%) 75 (3.2%) 99 (3.3%) Chest Pain/Angina 0 (0%) 18 (2.6%) 46 (1.9%) 64 (2.1%) ST segment changes 0 (0%) 11 (1.6%) 29 (1.2%) 40 (1.3%) Digestive System 8 (1.2%) 4 (0.6%) 9 (0.4%) 13 (0.4%) Nausea 4 (0.6%) 1 (0.1%) 2 (0.1%) 3 (0.1%) Special Senses 132 (19.6%) 62 (9.1%) 160 (6.8%) 222 (7.3%) Taste Perversion 129 (19.2%) 60 (8.8%) 157 (6.6%) 217 (7.1%) Parosmia 8 (1.2%) 6 (0.9%) 10 (0.4%) 16 (0.5%) In the clinical studies for breast imaging, breast pain was reported in 12 (1.7%) of the patients. In 11 of these patients the pain appears to be associated with biopsy/surgical procedures.
The following adverse reactions have been reported in ≤ 0.5% of patients: signs and symptoms consistent with seizure occurring shortly after administration of the agent; transient arthritis, angioedema, arrythmia, dizziness, syncope, abdominal pain, vomiting, and severe hypersensitivity characterized by dyspnea, hypotension, bradycardia, asthenia, and vomiting within two hours after a second injection of Technetium Tc99m Sestamibi. A few cases of flushing, edema, injection site inflammation, dry mouth, fever, pruritis, rash, urticaria and fatigue have also been attributed to administration of the agent.
- 7. DRUG INTERACTIONS
-
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Limited available data with Technetium Tc99m Sestamibi use in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. Animal reproduction and teratogenicity studies have not been conducted with Technetium Tc99m Sestamibi. However, all radiopharmaceuticals have the potential to cause fetal harm depending on the fetal stage of development and the magnitude of the radiation dose. If considering Technetium Tc99m Sestamibi administration to a pregnant woman, inform the patient about the potential for adverse pregnancy outcomes based on the radiation dose from Technetium Tc99m Sestamibi and the gestational timing of exposure.
All pregnancies have a background risk of birth defects, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
8.2 Lactation
Risk Summary
Limited data in the scientific literature on the presence of Technetium Tc99m Sestamibi in human milk, demonstrate that between 0.01% and 0.03% of maternal injected activity of technetium Tc99m Sestamibi was excreted in human milk. Technetium Tc99m Sestamibi accumulates in the lactating breast [see Clinical Considerations]. There are limited data in the scientific literature on effects of Technetium Tc99m Sestamibi on the breastfed infant or on milk production The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Technetium Tc99m Sestamibi and any potential adverse effects on the breastfed infant from Technetium Tc99m Sestamibi or from the underlying maternal condition.
Clinical Considerations
Interruption of breastfeeding after exposure to Technetium Tc99m Sestamibi is not necessary because Technetium Tc99m Sestamibi excretion in breast milk is low. However, a lactating woman may restrict close contact with her breast fed infant to a maximum of 5 hours in the 24 hour period after Technetium Tc99m Sestamibi administration in order to minimize radiation exposure.
8.4 Pediatric Use
Safety and effectiveness in the pediatric population have not been established.
No evidence of diagnostic efficacy or clinical utility of CARDIOLITE® scan was found in clinical studies of children and adolescents with Kawasaki disease.
A prospective study of 445 pediatric patients with Kawasaki disease was designed to determine the predictive value of CARDIOLITE® rest and stress myocardial perfusion imaging to define a pediatric population with Kawasaki disease that was at risk of developing cardiac events. Cardiac events were defined as cardiac death, MI, hospitalization due to cardiac etiology, heart failure, CABG or coronary angioplasty. The standard of truth was defined as cardiac events occurring 6 months following the administration of CARDIOLITE®. Only three cardiac events were observed at six months in this study. In all three cases, the scan was negative. No clinically meaningful measurements of sensitivity, specificity or other diagnostic performance parameters could be demonstrated in this study.
A ten year retrospective case history study of pediatric Kawasaki disease patients who completed CARDIOLITE® myocardial perfusion imaging and who had coronary angiography within three months of the CARDIOLITE® scan was designed to measure sensitivity and specificity of CARDIOLITE® scan. Out of 72 patients who had both evaluable CARDIOLITE® scans and evaluable angiographic images, only one patient had both an abnormal angiogram and an abnormal CARDIOLITE® scan. No clinically meaningful measurements of sensitivity, specificity or other diagnostic performance parameters could be demonstrated in this study.
In a clinical pharmacology study, 46 pediatric patients with Kawasaki disease received CARDIOLITE® administration at the following doses: 0.1 - 0.2 mCi/kg for rest, 0.3 mCi/kg for stress in one day studies; 0.2 mCi/kg for rest and 0.2 mCi/kg for stress in two day studies.
The radioactivity both in younger children and in adolescents exhibited PK profiles similar to those previously reported in adults (See Section 12).
The radiation absorbed doses in adolescents, both at rest and stress, were similar to those observed in adults (see Section 2). When comparing weight-adjusted radioactivity (up to 0.3 mCi/kg) doses administered to adolescents and younger children to the recommended dose administered to adults (up to 30 mCi), the radiation absorbed doses in both adolescents and younger children were similar to those in adults.
Adverse events were evaluated in 609 pediatric patients from the three clinical studies described above. The frequency and the type of the adverse events were similar to the ones observed in the studies of CARDIOLITE® in adults. Two of the 609 had a serious adverse event: one patient received a CARDIOLITE® overdose but remained asymptomatic, and one patient had an asthma exacerbation following administration.
8.5 Geriatric Use
Of 3068 patients in clinical studies of CARDIOLITE®, Kit for the Preparation of Technetium Tc99m Sestamibi for Injection, 693 patients were 65 or older and 121 were 75 or older.
Of 673 patients in clinical studies of MIRALUMA®, Kit for the Preparation of Technetium Tc99m Sestamibi for Injection, 138 patients were 65 or older and 30 were 75 or older.
Based on the evaluation of the frequency of adverse events and review of vital signs data, no overall differences in safety were observed between these subjects and younger subjects. Although reported clinical experience has not identified differences in response between elderly and younger patients, greater sensitivity of some older individuals cannot be ruled out.
- 10. OVERDOSAGE
-
11. DESCRIPTION
Each 5 mL vial contains a sterile, non-pyrogenic, lyophilized mixture of:
- Tetrakis (2-methoxy isobutyl isonitrile) Copper (I) tetrafluoroborate - 1.0 mg
- Sodium Citrate Dihydrate - 2.6 mg
- L-Cysteine Hydrochloride Monohydrate - 1.0 mg
- Mannitol – 20 mg
- Stannous Chloride, Dihydrate, minimum (SnCl2∙2H2O) - 0.025 mg
- Stannous Chloride, Dihydrate, (SnCl2∙2H2O) - 0.075 mg
- Tin Chloride (stannous and stannic) Dihydrate, maximum (as SnCl2∙2H2O) - 0.086 mg
Prior to lyophilization the pH is 5.3 to 5.9. The contents of the vial are lyophilized and stored under nitrogen.
This drug is administered by intravenous injection for diagnostic use after reconstitution with sterile, non-pyrogenic, oxidant-free Sodium Pertechnetate Tc99m Injection. The pH of the reconstituted product is 5.5 (5.0 - 6.0). No bacteriostatic preservative is present.
The precise structure of the technetium complex is Tc99m[MIBI]6+ where MIBI is 2-methoxy isobutyl isonitrile.
11.1 Physical Characteristics
Technetium Tc99m decays by isomeric transition with a physical half-life of 6.02 hours2. Photons that are useful for detection and imaging studies are listed below in Table 3.0.
Table 3.0. Principal Radiation Emission Data Radiation Mean %/Disintegration Mean Energy (KeV) Gamma -2 89.07 140.5
- 2 Kocher, David, C., Radioactive Decay Data Tables, DOE/TIC-11026, 108(1981).
11.2 External Radiation
The specific gamma ray constant for Tc99m is 5.4 microcoulombs/Kg-MBq-hr (0.78R/mCi-hr) at 1 cm. The first half value layer is 0.017 cm of Pb. A range of values for the relative attenuation of the radiation emitted by this radionuclide that results from interposition of various thicknesses of Pb is shown in Table 4.0. To facilitate control of the radiation exposure from Megabequerel (millicurie) amounts of this radionuclide, the use of a 0.25 cm thickness of Pb will attenuate the radiation emitted by a factor of 1,000.
Table 4.0. Radiation Attenuation by Lead Shielding Shield Thickness (Pb) cm Coefficient of Attenuation 0.017 0.5 0.08 10-1 0.16 10-2 0.25 10-3 0.33 10-4 To correct for physical decay of this radionuclide, the fractions that remain at selected intervals after the time of calibration are shown in Table 5.0.
-
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Technetium Tc99m Sestamibi is a cationic Tc99m complex which has been found to accumulate in viable myocardial tissue in a manner analogous to that of thallous chloride Tl-201. Scintigraphic images obtained in humans after the intravenous administration of the drug have been comparable to those obtained with thallous chloride Tl-201 in normal and abnormal myocardial tissue.
Animal studies have shown that myocardial uptake is not blocked when the sodium pump mechanism is inhibited. Although studies of subcellular fractionation and electron micrographic analysis of heart cell aggregates suggest that Tc99m Sestamibi cellular retention occurs specifically within the mitochondria as a result of electrostatic interactions, the clinical relevance of these findings has not been determined.
The mechanism of Tc99m Sestamibi localization in various types of breast tissue (e.g., benign, inflammatory, malignant, fibrous) has not been established.
12.3 Pharmacokinetics
Pulmonary activity is negligible even immediately after injection. Blood clearance studies indicate that the fast clearing component clears with a t1/2 of 4.3 minutes at rest, and clears with a t1/2 of 1.6 minutes under exercise conditions. At five minutes post injection about 8% of the injected dose remains in circulation. There is less than 1% protein binding of Technetium Tc99m Sestamibi in plasma. The myocardial biological half-life is approximately six hours after a rest or exercise injection. The biological half-life for the liver is approximately 30 minutes after a rest or exercise injection. The effective half-life of clearance (which includes both the biological half-life and radionuclide decay) for the heart is approximately 3 hours, and for the liver is approximately 30 minutes, after a rest or exercise injection. The ideal imaging time reflects the best compromise between heart count rate and surrounding organ uptake.
Myocardial uptake which is coronary flow dependent is 1.2% of the injected dose at rest and 1.5% of the injected dose at exercise. Table 6.0 illustrates the biological clearance as well as effective clearance (which includes biological clearance and radionuclide decay) of Tc99m Sestamibi from the heart and liver.
[Organ concentrations expressed as percentage of injected dose; data based on an average of 5 subjects at rest and 5 subjects during exercise].
Table 6.0 Biological and Effective Clearance REST STRESS Heart Liver Heart Liver Time Biological Effective Biological Effective Biological Effective Biological Effective 5 min. 1.2 1.2 19.6 19.4 1.5 1.5 5.9 5.8 30 min. 1.1 1.0 12.2 11.5 1.4 1.3 4.5 4.2 1 hour 1.0 0.9 5.6 5.0 1.4 1.2 2.4 2.1 2 hours 1.0 0.8 2.2 1.7 1.2 1.0 0.9 0.7 4 hours 0.8 0.5 0.7 0.4 1.0 0.6 0.3 0.2 A study in a dog myocardial ischemia model reported that Technetium Tc99m Sestamibi undergoes myocardial distribution (redistribution), although more slowly and less completely than thallous chloride Tl-201. A study in a dog myocardial infarction model reported that the drug showed no redistribution of any consequence. Definitive human studies to demonstrate possible redistribution have not been reported. In patients with documented myocardial infarction, imaging revealed the infarct up to four hours post dose.
12.3.2 Elimination
The major pathway for clearance of Tc99m Sestamibi is the hepatobiliary system. Activity from the gall bladder appears in the intestines within one hour of injection. Twenty-seven percent of the injected dose is excreted in the urine, and approximately thirty-three percent of the injected dose is cleared through the feces in 48 hours.
-
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In comparison with most other diagnostic technetium labeled radiopharmaceuticals, the radiation dose to the ovaries (1.5 rads/30 mCi at rest, 1.2 rads/30 mCi at exercise) is high. Minimal exposure (ALARA) is necessary in women of childbearing capability. (See Section 2.)
The active intermediate, Cu(MIBI)4BF4, was evaluated for genotoxic potential in a battery of five tests. No genotoxic activity was observed in the Ames, CHO/HPRT and sister chromatid exchange tests (all in vitro). At cytotoxic concentrations (> 20 µg/mL), an increase in cells with chromosome aberrations was observed in the in vitro human lymphocyte assay. Cu(MIBI)4BF4 did not show genotoxic effects in the in vivo mouse micronucleus test at a dose which caused systemic and bone marrow toxicity (9 mg/kg, > 600 × maximal human dose).
-
14. CLINICAL STUDIES
CLINICAL TRIALS:
MYOCARDIAL IMAGING: In a trial of rest and stress CARDIOLITE® imaging, the relationship of normal or abnormal perfusion scans and long term cardiac events was evaluated in 521 patients (511 men, 10 women) with stable chest pain. There were 73.9% Caucasians, 25.9% Blacks and 0.2% Asians. The mean age was 59.6 years (range: 29 to 84 years). All patients had a baseline rest and exercise CARDIOLITE® scan and were followed for 13.2 ± 4.9 months (range: 1 to 24 months). Images were correlated with the occurrence of a cardiac event (cardiac death or non-fatal myocardial infarction). In this trial as summarized in Table 7.0, 24/521 (4.6%) had a cardiac event.
Table 7.0 Cardiac Events Baseline Scan* Proportion of patients with events by scan results * Proportion of scan result in patients with events;
N=24*Proportion of event-free patients by scan result * - * Note: Similar findings were found in two studies with patients who had pharmacologic stress CARDIOLITE® imaging.
- † p<0.01
Normal 1/206 (0.5%) 1/24 (4.2%) 205/206 (99.5%) Abnormal 23/315 (7.3%) † 23/24 (95.8%) † 292/315 (92.7%)† Although patients with normal images had a lower cardiac event rate than those with abnormal images, in all patients with abnormal images it was not possible to predict which patient would be likely to have further cardiac events; i.e., such individuals were not distinguishable from other patients with abnormal images.
The findings were not evaluated for defect location, disease duration, specific vessel involvement or intervening management.
In earlier trials, using a template consisting of the anterior wall, inferior-posterior wall and isolated apex, localization in the anterior or inferior-posterior wall in patients with suspected angina or coronary artery disease was shown. Disease localization isolated to the apex has not been established. In adults, Tc99m Sestamibi has not been studied or evaluated in cardiac disorders other than coronary artery disease.
BREAST IMAGING: MIRALUMA® was evaluated in two multicenter, clinical trials of a total of 673 woman patients. Overall the mean age was 52 (range 23 to 87 years). The racial and ethnic representation was 70% Caucasian, 15% African-American, 14% Hispanic and 1% Asian.
Both clinical studies evaluated women who were referred for further evaluation for either: 1) a mammographically detected (with varying degrees of malignant likelihood) but not palpable breast lesion (study A, n=387, mean age = 54 years), or 2) a palpable breast lesion (study B, n=286, mean age = 50 years). In both studies all patients were scheduled for biopsy.
MIRALUMA® (20 - 30 mCi) was injected intravenously in a vein that was contralateral to the breast lesion in question. Planar imaging was completed with a high resolution collimator with a 10% window centered at 140 KeV, and 128 × 128 matrix. An initial marker image, that was not used in the data analysis, was obtained using a cobalt Co57 point source as a marker of a palpable mass. Images were obtained 5 minutes after injection as follows: lateral image of the affected breast for 10 minutes, lateral image of the contralateral breast for 10 minutes, and an anterior image of both breasts for 10 minutes. For the lateral image the patients were positioned in a prone position. For the anterior image, the patients were supine. The MIRALUMA® scintigraphic images were read in a randomized method by two groups of three blinded readers. MIRALUMA® uptake was scored as: normal (no uptake), equivocal, low, moderate, or high uptake. The results of MIRALUMA® images and mammography were analyzed in comparison to histopathologic findings of malignant or non-malignant disease.
As shown in Table 8.0 for the 483 evaluable patients, the sensitivity and specificity of any degree of MIRALUMA® uptake appear to vary with the presence or absence of palpable mass.
TABLE 8.0 Overall MIRALUMA® Blinded Results of Target Lesions* Identified at Study Entry† STATISTIC Study A
Non-Palpable Mass and an Abnormal MammogramStudy B
Palpable Mass- * Excludes all discordant lesions not identified at entry and excludes 25 equivocal interpretations from Study A and 32 equivocal interpretations from Study B (see Tables 9.0 and 10.0)
- † Some patients had more than one target lesion
- ‡ Median and approximated 95% Confidence Interval
- § PPV= Positive Predict Value; NPV= Negative Predict Value
Number of Patients and Lesions N=277 Patients with 300 Lesions N=206 Patients with 240 Lesions Sensitivity 52(42,62)‡ 76(67,83) Specificity 94(89,96) 85(77,91) PPV§ 79(67,88) 83(74,89) NPV§ 80(74,85) 78(69,84) Agreement 80(75,85) 80(75,85) Prevalence 32(27,37) 49(43,56) In a separate retrospective subset analyses of 259 patients with dense (heterogeneously/extremely dense) and 275 patients with fatty (almost entirely fat/numerous vague densities) breast tissue, the MIRALUMA® results were similar. Overall, the studies were not designed to compare the performance of MIRALUMA® with the performance of mammography in patients with breast densities or other coexistent breast tissue disorders.
In general the histology seems to correlate with the degree of MIRALUMA® uptake. As shown in Tables 9.0 and 10.0, the majority of the normal MIRALUMA® images are associated with non-malignant tissue (78-81%) and the majority of low, moderate or high uptake MIRALUMA® images are associated with malignant disease (79-83%). In an individual patient, however, the intensity of MIRALUMA® uptake can not be used to confirm the presence or absence of malignancy. Equivocal results do not have a correlation with histology.
TABLE 9.0 Degree of MIRALUMA® Breast Imaging Uptake in Comparison to Histopathology Results in Patients with Mammographically Detected Non-Palpable Lesions* (Study A) Normal Uptake
N = 249 lesionsEquivocal Uptake
N = 25 lesionsLow, Moderate or High Uptake
N = 66 lesions- * Median finding for 3 blinded readers
- † Includes benign tissue, fibroadenoma, benign intramammary nodes, radial scar.
Non-malignant† 201 (81%) 14 (56%) 14 (21%) Malignant 48 (19%) 11 (44%) 52 (79%) TABLE 10.0 Degree of MIRALUMA® Breast Imaging Uptake in Comparison to Histopathology Results in Patients with Palpable Lesions* (Study B) Normal Uptake
N = 129 lesionsEquivocal Uptake
N = 32 lesionsLow, Moderate or High Uptake
N = 115 lesions- * Median finding for 3 blinded readers
- † Includes benign tissue, fibroadenoma, benign intramammary nodes, radial scar.
Non-malignant† 100 (78%) 19 (59%) 20 (17%) Malignant 29 (22%) 13 (41%) 95 (83%) An estimate of the likelihood of malignancy based on the MIRALUMA® uptake score in combination with the mammographic score has not been studied.
In these two studies approximately 150 additional, non-biopsied lesions were found to be positive after MIRALUMA® imaging. These lesions were identified in sites that did not physically correlate with identified entry criteria mammographic lesions and these lesions were not palpable. These lesions were not biopsied. Whether these lesions were benign or malignant is not known. MIRALUMA® uptake can occur in both benign and malignant disease. THE CLINICAL USEFULNESS OF A POSITIVE MIRALUMA® IMAGE IN THE ABSENCE OF AN ABNORMAL MAMMOGRAM OR A PALPABLE LESION IS NOT KNOWN.
-
16. HOW SUPPLIED/STORAGE AND HANDLING
CARDIOLITE®, Kit for the Preparation of Technetium Tc99m Sestamibi for Injection is supplied as a 5 mL vial in kits of five (5) vials (NDC # 11994-001-55) and twenty (20) vials (NDC # 11994-001-20), sterile and non-pyrogenic.
The patient dose should be measured by a suitable radioactivity calibration system immediately prior to patient administration. Radiochemical purity should be checked prior to patient administration.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
Prior to lyophilization the pH is between 5.3-5.9. The contents of the vial are lyophilized and stored under nitrogen. Store at 15-25°C (59-77° F) before and after reconstitution.
Technetium Tc99m Sestamibi contains no preservatives. Included in each five (5) vial kit is one (1) package insert, six (6) vial shield labels and six (6) radiation warning labels. Included in each twenty (20) vial kit is one (1) package insert, twenty four (24) vial shield labels and twenty four (24) radiation warning labels.
This reagent kit is approved for distribution to persons licensed pursuant to the Code of Massachusetts Regulations 105 CMR 120.500 for the uses listed in 105 CMR 120.547 or 120.552, or under equivalent regulations of the U.S. Nuclear Regulatory Commission, Agreement States or Licensing States.
-
17. PATIENT COUNSELING INFORMATION
CARDIOLITE® and MIRALUMA® are different names for the same drug. Patients should be advised to inform their health care provider if they had an allergic reaction to either drug or if they had an imaging study with either drug.
Lactation: Interruption of breastfeeding after exposure to Technetium Tc99m Sestamibi is not necessary, however, a lactating woman should be advised to consider restricting close contact with her breast fed infant to a maximum of 5 hours in the 24 hour period after Technetium Tc99m Sestamibi administration in order to minimize radiation exposure [see Use in Specific Populations (8.2)].
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - 5 Vial Box
Lantheus
Medical Imaging®Cardiolite®
Kit for the Preparation of Technetium Tc99m Sestamibi for Injection
CONTENTS AND STORAGE CONDITIONS:
1 Package Insert, 12 Radiation Labels and 5 Vials, each containing:
Tetrakis (2-methoxy isobutyl isonitrile) Copper (I) tetrafluoroborate - 1.0 mg
Stannous Chloride Dihydrate - 0.075 mg; L-Cysteine Hydrochloride
Monohydrate - 1.0 mg; Sodium Citrate Dihydrate - 2.6 mg; Mannitol - 20 mg
Store at 15-25°C (59-77°F).CONTAINS NO PRESERVATIVE. See Package Insert for dosage information.
Reconstitute with additive-free Tc99m and store at 15-25°C (59-77°F).
Use within 6 hours of reconstitution.
-
INGREDIENTS AND APPEARANCE
CARDIOLITE
tetrakis(2-methoxyisobutylisocyanide)copper(i) tetrafluoroborate injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 11994-001 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TETRAKIS(2-METHOXYISOBUTYLISOCYANIDE)COPPER(I) TETRAFLUOROBORATE (UNII: N6OU7HJ70P) (TETRAKIS(2-METHOXYISOBUTYLISOCYANIDE)COPPER(I) TETRAFLUOROBORATE - UNII:N6OU7HJ70P) TETRAKIS(2-METHOXYISOBUTYLISOCYANIDE)COPPER(I) TETRAFLUOROBORATE 1 mg in 1 mL Inactive Ingredients Ingredient Name Strength TRISODIUM CITRATE DIHYDRATE (UNII: B22547B95K) 2.6 mg in 1 mL CYSTEINE HYDROCHLORIDE (UNII: ZT934N0X4W) 1 mg in 1 mL MANNITOL (UNII: 3OWL53L36A) 20 mg in 1 mL STANNOUS CHLORIDE (UNII: 1BQV3749L5) 0.075 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 11994-001-52 2 in 1 BOX 12/20/1990 1 5 mL in 1 VIAL; Type 0: Not a Combination Product 2 NDC: 11994-001-55 5 in 1 BOX 12/20/1990 2 5 mL in 1 VIAL; Type 0: Not a Combination Product 3 NDC: 11994-001-20 20 in 1 BOX 02/28/2008 3 5 mL in 1 VIAL; Type 0: Not a Combination Product 4 NDC: 11994-001-00 5 mL in 1 SYRINGE; Type 0: Not a Combination Product 12/20/1990 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA019785 12/20/1990 Labeler - Lantheus Medical Imaging, Inc. (176786812) Establishment Name Address ID/FEI Business Operations Lantheus Medical Imaging, Inc. 176786812 RELABEL(11994-001) , REPACK(11994-001) , MANUFACTURE(11994-001) , LABEL(11994-001) , PACK(11994-001) , ANALYSIS(11994-001) Establishment Name Address ID/FEI Business Operations Jubilant HollisterStier LLC 069263643 ANALYSIS(11994-001) , MANUFACTURE(11994-001)
Trademark Results [Cardiolite]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 CARDIOLITE 73662052 1484982 Live/Registered |
E. I. DU PONT DE NEMOURS AND COMPANY 1987-05-21 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.