These highlights do not include all the information needed to use Fusilev safely and effectively. See full prescribing information for Fusilev. Fusilev® (levoleucovorin) FOR INJECTION, POWDER, LYOPHILIZED, FOR SOLUTION for INTRAVENOUS use Fusilev® (levoleucovorin) INJECTION, SOLUTION for INTRAVENOUS useInitial U.S. Approval: 1952 (d,l-leucovorin), 2008 (levoleucovorin)
Fusilev by
Drug Labeling and Warnings
Fusilev by is a Prescription medication manufactured, distributed, or labeled by Spectrum Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
FUSILEV- levoleucovorin injection, powder, lyophilized, for solution
FUSILEV- levoleucovorin injection, solution
Spectrum Pharmaceuticals, Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use Fusilev safely and effectively. See full prescribing information for Fusilev. Fusilev® (levoleucovorin) FOR INJECTION, POWDER, LYOPHILIZED, FOR SOLUTION for INTRAVENOUS use Fusilev® (levoleucovorin) INJECTION, SOLUTION for INTRAVENOUS use
Initial U.S. Approval: 1952 (d,l-leucovorin), 2008 (levoleucovorin) RECENT MAJOR CHANGESIndications and Usage (1) 04/2011 Dosage and Administration, Fusilev Administration in Combination with 5-Fluorouracil (2.5) 04/2011 Dosage and Administration, Reconstitution and Infusion Instructions (2.6) 04/2011 INDICATIONS AND USAGEFusilev is a folate analog indicated for: (1)
Limitations of Use (1) Fusilev is not approved for pernicious anemia and megaloblastic anemias. Improper use may cause a hematologic remission while neurologic manifestations continue to progress. (1.1) (1) DOSAGE AND ADMINISTRATIONDo not administer intrathecally. (2.1) (2) Fusilev is dosed at one-half the usual dose of racemic d,l-leucovorin. (2.1) (2) Fusilev Rescue After High-Dose Methotrexate Therapy (2) Fusilev rescue recommendations are based on a methotrexate dose of 12 grams/m2 administered by intravenous infusion over 4 hours. Fusilev rescue at a dose of 7.5 mg (approximately 5 mg/m2) every 6 hours for 10 doses starts 24 hours after the beginning of the methotrexate infusion. Determine serum creatinine and methotrexate levels at least once daily. Continue Fusilev administration, hydration, and urinary alkalinization (pH of 7.0 or greater) until the methotrexate level is below 5 x 10-8 M (0.05 micromolar). The Fusilev dose may need to be adjusted. (2.3) (2) Fusilev Administration in Combination with 5-Fluorouracil (5-FU) (2) The following regimens have been used historically for the treatment of colorectal cancer: (2)
5-FU and Fusilev should be administered separately to avoid the formation of a precipitate. (2) Treatment is repeated daily for five days. This five-day treatment course may be repeated at 4 week (28-day) intervals, for 2 courses and then repeated at 4 to 5 week (28 to 35 day) intervals provided that the patient has completely recovered from the toxic effects of the prior treatment course. (2) In subsequent treatment courses, the dosage of 5-FU should be adjusted based on patient tolerance of the prior treatment course. The daily dosage of 5-FU should be reduced by 20% for patients who experienced moderate hematologic or gastrointestinal toxicity in the prior treatment course, and by 30% for patients who experienced severe toxicity. For patients who experienced no toxicity in the prior treatment course, 5-FU dosage may be increased by 10%. Fusilev dosages are not adjusted for toxicity. (2.5) (2) DOSAGE FORMS AND STRENGTHSFusilev for Injection: Each 50 mg single-use vial of Fusilev contains a sterile lyophilized powder consisting of 64 mg levoleucovorin calcium pentahydrate (equivalent to 50 mg levoleucovorin) and 50 mg mannitol. (3, 11, 16) It is intended for intravenous administration after reconstitution with 5.3 mL of sterile 0.9% Sodium Chloride Injection, USP. (2.6, 11) (3) Fusilev Injection: 17.5 mL of a sterile solution containing levoleucovorin calcium pentahydrate equivalent to 175 mg levoleucovorin and 0.83% sodium chloride. (3, 11, 16) (3) Fusilev Injection: 25 mL of a sterile solution containing levoleucovorin calcium pentahydrate equivalent to 250 mg levoleucovorin and 0.83% sodium chloride. (3, 11, 16) (3) CONTRAINDICATIONSFusilev is contraindicated for patients who have had previous allergic reactions attributed to folic acid or folinic acid. (4) (4) WARNINGS AND PRECAUTIONSDue to Ca++ content, no more than 16 mL (160 mg) of levoleucovorin solution should be injected intravenously per minute. (5.1) (5) Fusilev enhances the toxicity of fluorouracil. (5.2,7) (5) Concomitant use of d,l-leucovorin with trimethoprim-sulfamethoxazole for Pneumocystis carinii pneumonia in HIV patients was associated with increased rates of treatment failure in a placebo-controlled study. (5.3) (5) ADVERSE REACTIONSAllergic reactions were reported in patients receiving Fusilev. (6.3) (6) Vomiting (38%), stomatitis (38%) and nausea (19%) were reported in patients receiving Fusilev as rescue after high-dose methotrexate therapy. (6.1) (6) The most common adverse reactions (>50%) in patients with advanced colorectal cancer receiving Fusilev in combination with 5-FU were diarrhea, nausea and stomatitis. (6.2) (6) To report SUSPECTED ADVERSE REACTIONS, contact Spectrum Pharmaceuticals, Inc. at 1-877-387-4538 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch (6) DRUG INTERACTIONSFusilev may counteract the antiepileptic effect of phenobarbital, phenytoin and primidone, and increase the frequency of seizures in susceptible patients. (7) (7) Revised: 12/2019 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
- Fusilev® is a folate analog.
- Fusilev rescue is indicated after high-dose methotrexate therapy in osteosarcoma.
- Fusilev is also indicated to diminish the toxicity and counteract the effects of impaired methotrexate elimination and of inadvertent overdosage of folic acid antagonists.
- Fusilev is indicated for use in combination chemotherapy with 5-fluorouracil in the palliative treatment of patients with advanced metastatic colorectal cancer.
2 DOSAGE AND ADMINISTRATION
2.1 Administration Guidelines
Fusilev is dosed at one-half the usual dose of racemic d,l-leucovorin.
Fusilev is indicated for intravenous administration only. Do not administer intrathecally.
2.2 Co-administration of Fusilev with other agents
Due to the risk of precipitation, do not co-administer Fusilev with other agents in the same admixture.
2.3 Fusilev Rescue After High-Dose Methotrexate Therapy
The recommendations for Fusilev rescue are based on a methotrexate dose of 12 grams/m2 administered by intravenous infusion over 4 hours (see methotrexate package insert for full prescribing information). Fusilev rescue at a dose of 7.5 mg (approximately 5 mg/m2) every 6 hours for 10 doses starts 24 hours after the beginning of the methotrexate infusion.
Serum creatinine and methotrexate levels should be determined at least once daily. Fusilev administration, hydration, and urinary alkalinization (pH of 7.0 or greater) should be continued until the methotrexate level is below 5 x 10-8 M (0.05 micromolar). The Fusilev dose should be adjusted or rescue extended based on the following guidelines.
|
Clinical Situation |
Laboratory Findings |
Fusilev Dosage and Duration |
|
Normal Methotrexate Elimination |
Serum methotrexate level approximately 10 micromolar at 24 hours after administration, 1 micromolar at 48 hours, and less than 0.2 micromolar at 72 hours |
7.5 mg IV q 6 hours for 60 hours (10 doses starting at 24 hours after start of methotrexate infusion). |
|
Delayed Late Methotrexate Elimination |
Serum methotrexate level remaining above 0.2 micromolar at 72 hours, and more than 0.05 micromolar at 96 hours after administration. |
Continue 7.5 mg IV q 6 hours, until methotrexate level is less than 0.05 micromolar. |
|
Delayed Early Methotrexate Elimination and/or Evidence of Acute Renal Injury |
Serum methotrexate level of 50 micromolar or more at 24 hours, or 5 micromolar or more at 48 hours after administration, OR; a 100% or greater increase in serum creatinine level at 24 hours after methotrexate administration (e.g., an increase from 0.5 mg/dL to a level of 1 mg/dL or more). |
75 mg IV q 3 hours until methotrexate level is less than 1 micromolar; then 7.5 mg IV q 3 hours until methotrexate level is less than 0.05 micromolar. |
Patients who experience delayed early methotrexate elimination are likely to develop reversible renal failure. In addition to appropriate Fusilev therapy, these patients require continuing hydration and urinary alkalinization, and close monitoring of fluid and electrolyte status, until the serum methotrexate level has fallen to below 0.05 micromolar and the renal failure has resolved.
Some patients will have abnormalities in methotrexate elimination or renal function following methotrexate administration, which are significant but less severe than the abnormalities described in the table above. These abnormalities may or may not be associated with significant clinical toxicity. If significant clinical toxicity is observed, Fusilev rescue should be extended for an additional 24 hours (total of 14 doses over 84 hours) in subsequent courses of therapy. The possibility that the patient is taking other medications which interact with methotrexate (e.g., medications which may interfere with methotrexate elimination or binding to serum albumin) should always be reconsidered when laboratory abnormalities or clinical toxicities are observed.
Delayed methotrexate excretion may be caused by accumulation in a third space fluid collection (i.e., ascites, pleural effusion), renal insufficiency, or inadequate hydration. Under such circumstances, higher doses of Fusilev or prolonged administration may be indicated.
Although Fusilev may ameliorate the hematologic toxicity associated with high-dose methotrexate, Fusilev has no effect on other established toxicities of methotrexate such as the nephrotoxicity resulting from drug and/or metabolite precipitation in the kidney.
2.4 Dosing Recommendations for Inadvertent Methotrexate Overdosage
Fusilev rescue should begin as soon as possible after an inadvertent overdosage and within 24 hours of methotrexate administration when there is delayed excretion. As the time interval between antifolate administration [e.g., methotrexate] and Fusilev rescue increases, Fusilev’s effectiveness in counteracting toxicity may decrease. Fusilev 7.5 mg (approximately 5 mg/m2 ) should be administered IV every 6 hours until the serum methotrexate level is less than 10-8 M.
Serum creatinine and methotrexate levels should be determined at 24 hour intervals. If the 24 hour serum creatinine has increased 50% over baseline or if the 24 hour methotrexate level is greater than 5 x 10-6 M or the 48 hour level is greater than 9 x 10-7 M, the dose of Fusilev should be increased to 50 mg/m2 IV every 3 hours until the methotrexate level is less than 10-8 M. Hydration (3 L/day) and urinary alkalinization with NaHCO3 should be employed concomitantly. The bicarbonate dose should be adjusted to maintain the urine pH at 7.0 or greater.
2.5 Fusilev Administration in Combination with 5-Fluorouracil (5-FU)
The following regimens have been used historically for the treatment of colorectal cancer:
- 1. Fusilev is administered at 100 mg/m2 by slow intravenous injection over a minimum of 3 minutes, followed by 5-FU at 370 mg/m2 by intravenous injection.
- 2. Fusilev is administered at 10 mg/m2 by intravenous injection followed by 5-FU at 425 mg/m2 by intravenous injection.
5-FU and Fusilev should be administered separately to avoid the formation of a precipitate.
Treatment is repeated daily for five days. This five-day treatment course may be repeated at 4 week (28-day) intervals, for 2 courses and then repeated at 4 to 5 week (28 to 35 day) intervals provided that the patient has completely recovered from the toxic effects of the prior treatment course.
In subsequent treatment courses, the dosage of 5-FU should be adjusted based on patient tolerance of the prior treatment course. The daily dosage of 5-FU should be reduced by 20% for patients who experienced moderate hematologic or gastrointestinal toxicity in the prior treatment course, and by 30% for patients who experienced severe toxicity. For patients who experienced no toxicity in the prior treatment course, 5-FU dosage may be increased by 10%. Fusilev dosages are not adjusted for toxicity.
2.6 Reconstitution and Infusion Instructions
Fusilev for Injection
- Prior to intravenous injection, the 50 mg vial of Fusilev for Injection is reconstituted with 5.3 mL of 0.9% Sodium Chloride Injection, USP to yield a levoleucovorin concentration of 10 mg per mL. Reconstitution with Sodium Chloride solutions with preservatives (e.g. benzyl alcohol) has not been studied. The use of solutions other than 0.9% Sodium Chloride Injection, USP is not recommended.
- The reconstituted 10 mg per mL levoleucovorin contains no preservative. Observe strict aseptic technique during reconstitution of the drug product.
- Saline reconstituted levoleucovorin solutions may be further diluted, immediately, to concentrations of 0.5 mg/mL to 5 mg/mL in 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP. Initial reconstitution or further dilution using 0.9% Sodium Chloride Injection, USP may be held at room temperature for not more than a total of 12 hours. Dilutions in 5% Dextrose Injection, USP may be held at room temperature for not more than 4 hours.
- Visually inspect the reconstituted solution for particulate matter and discoloration, prior to administration. CAUTION: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if cloudiness or precipitate is observed.
- No more than 16 mL of reconstituted solutions (160 mg of levoleucovorin) should be injected intravenously per minute, because of the calcium content of the levoleucovorin solution.
Fusilev Injection
- Levoleucovorin contains no preservative. Observe strict aseptic technique during reconstitution of the drug product.
- Levoleucovorin solutions may be further diluted to concentrations of 0.5 mg/mL in 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP. The diluted solution using 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP may be held at room temperature for not more than 4 hours.
- Visually inspect the diluted solution for particulate matter and discoloration, prior to administration. CAUTION: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if cloudiness or precipitate is observed.
- No more than 16 mL of Fusilev Injection (160 mg of levoleucovorin) should be injected intravenously per minute, because of the calcium content of the levoleucovorin solution.
3 DOSAGE FORMS AND STRENGTHS
Fusilev for Injection is supplied in sterile, single-use vials containing 64 mg levoleucovorin calcium pentahydrate (equivalent to 50 mg levoleucovorin) and 50 mg mannitol.
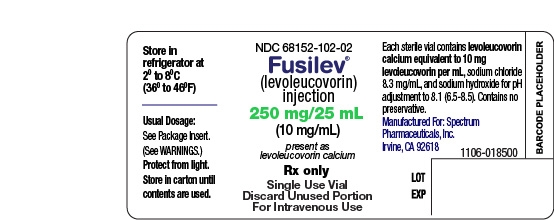
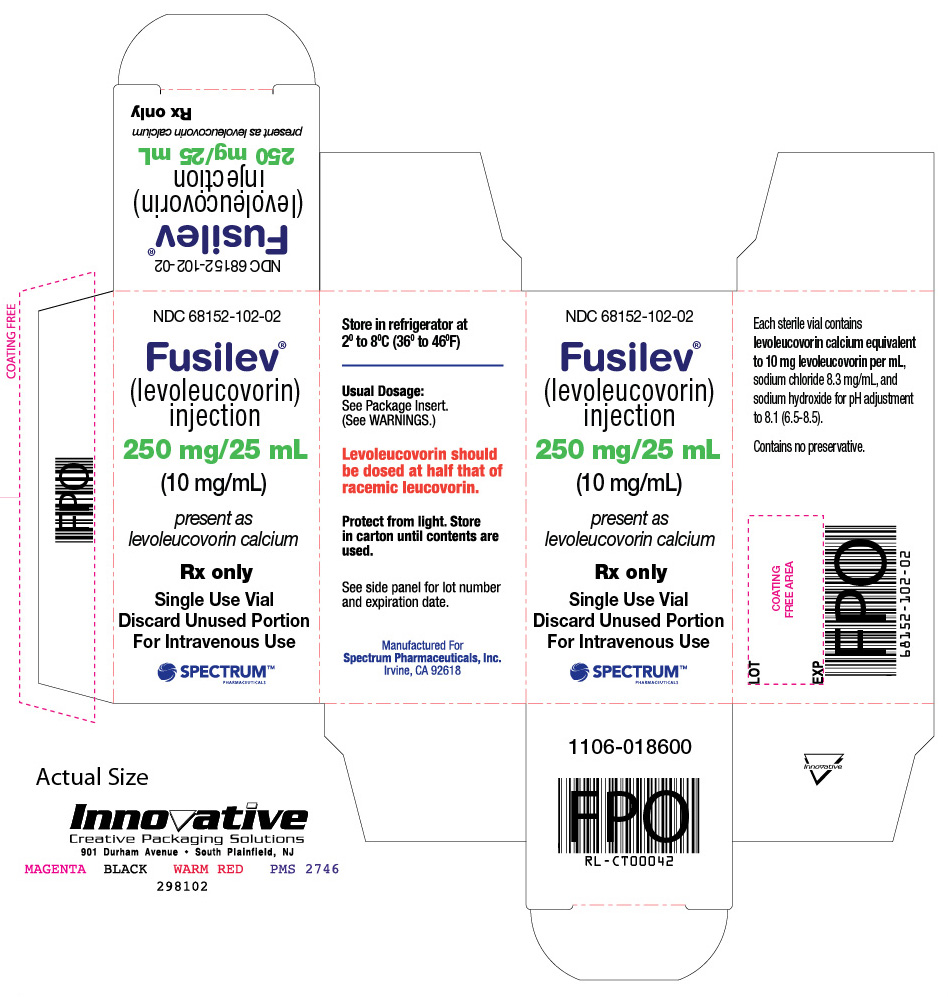
Fusilev Injection, 175 mg is supplied in a single-use vial containing 17.5 mL sterile solution. Each mL contains levoleucovorin calcium pentahydrate equivalent to 10 mg levoleucovorin and 8.3 mg sodium chloride.
Fusilev Injection, 250 mg is supplied in a single-use vial containing 25 mL sterile solution. Each mL contains levoleucovorin calcium pentahydrate equivalent to 10 mg levoleucovorin and 8.3 mg sodium chloride.
4 CONTRAINDICATIONS
Fusilev is contraindicated for patients who have had previous allergic reactions attributed to folic acid or folinic acid.
5 WARNINGS AND PRECAUTIONS
5.1 Rate of Administration
Because of the Ca++ content of the levoleucovorin solution, no more than 16 mL (160 mg of levoleucovorin) should be injected intravenously per minute.
5.2 Potential for Enhanced Toxicity with 5-Fluorouracil
Fusilev enhances the toxicity of 5-fluorouracil. Deaths from severe enterocolitis, diarrhea, and dehydration have been reported in elderly patients receiving weekly d,l-leucovorin and 5-fluorouracil. When these drugs are administered concurrently in the palliative treatment of advanced colorectal cancer, the dosage of 5-FU must be lower than usually administered. Although the toxicities observed in patients treated with the combination of Fusilev and 5-FU are qualitatively similar to those observed with 5-FU alone, gastrointestinal toxicities (particularly stomatitis and diarrhea) are observed more commonly and may be of greater severity and of prolonged duration in patients treated with the combination.
In the first Mayo/NCCTG controlled trial, toxicity, primarily gastrointestinal, resulted in 7% of patients requiring hospitalization when treated with 5-FU alone or 5-FU in combination with 200 mg/m2 of d,l-leucovorin and 20% when treated with 5-FU in combination with 20 mg/m2 of d,l-leucovorin. In the second Mayo/NCCTG trial, hospitalizations related to treatment toxicity also appeared to occur more often in patients treated with the low dose d,l-leucovorin/5-FU combination than in patients treated with the high dose combination – 11% versus 3%. Therapy with Fusilev and 5-FU must not be initiated or continued in patients who have symptoms of gastrointestinal toxicity of any severity, until those symptoms have completely resolved. Patients with diarrhea must be monitored with particular care until the diarrhea has resolved, as rapid clinical deterioration leading to death can occur. In an additional study utilizing higher weekly doses of 5-FU and d,l-leucovorin, elderly and/or debilitated patients were found to be at greater risk for severe gastrointestinal toxicity.
Seizures and/or syncope have been reported rarely in cancer patients receiving d,l-leucovorin, usually in association with fluoropyrimidine administration, and most commonly in those with CNS metastases or other predisposing factors. However, a causal relationship has not been established.
5.3 Potential for interaction with trimethoprim-sulfamethoxazole
The concomitant use of d,l-leucovorin with trimethoprim-sulfamethoxazole for the acute treatment of Pneumocystis carinii pneumonia in patients with HIV infection was associated with increased rates of treatment failure and morbidity in a placebo-controlled study.
6 ADVERSE REACTIONS
6.1 Clinical Studies in High-Dose Methotrexate Therapy
Since clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The following table presents the frequency of adverse reactions which occurred during the administration of 58 courses of high-dose methotrexate 12 grams/m2 followed by Fusilev rescue for osteosarcoma in 16 patients age 6-21. Most patients received Fusilev 7.5 mg every 6 hours for 60 hours or longer beginning 24 hours after completion of methotrexate.
|
Body System/Adverse Reactions |
Number (%) of Patients with Adverse Reactions |
Number (%) of Courses with Adverse Reactions |
||
|
(N =16) |
(N = 58) |
|||
|
All |
Grade 3+ |
All |
Grade 3+ |
|
|
Gastrointestinal | ||||
|
Stomatitis |
6 (37.5) |
1 (6.3) |
10 (17.2) |
1 (1.7) |
|
Vomiting |
6 (37.5) |
0 |
14 (24.1) |
0 |
|
Nausea |
3 (18.8) |
0 |
3 (5.2) |
0 |
|
Diarrhea |
1 (6.3) |
0 |
1 (1.7) |
0 |
|
Dyspepsia |
1 (6.3) |
0 |
1 (1.7) |
0 |
|
Typhlitis |
1 (6.3) |
1 (6.3) |
1 (1.7) |
1 (1.7) |
|
Respiratory | ||||
|
Dyspnea |
1 (6.3) |
0 |
1 (1.7) |
0 |
|
Skin and Appendages | ||||
|
Dermatitis |
1 (6.3) |
0 |
1 (1.7) |
0 |
|
Other | ||||
|
Confusion |
1 (6.3) |
0 |
1 (1.7) |
0 |
|
Neuropathy |
1 (6.3) |
0 |
1 (1.7) |
0 |
|
Renal function abnormal |
1 (6.3) |
0 |
3 (5.2) |
0 |
|
Taste perversion |
1 (6.3) |
0 |
1 (1.7) |
0 |
|
Total number of patients |
9 (56.3) |
2 (12.5) |
||
|
Total number of courses |
25 (43.1) |
2 (3.4) |
||
The incidence of adverse reactions may be underestimated because not all patients were fully evaluable for toxicity for all cycles in the clinical trials. Leukopenia and thrombocytopenia were observed, but could not be attributed to high-dose methotrexate with Fusilev rescue because patients were receiving other myelosuppressive chemotherapy.
6.2 Clinical Studies in Combination with 5-FU in Colorectal Cancer
A randomized controlled trial conducted by the North Central Cancer Treatment Group (NCCTG) in patients with advanced colorectal cancer failed to show superiority of a regimen of 5-FU + levoleucovorin to 5-FU + d,l-leucovorin in overall survival. Patients were randomized to 5-FU 370 mg/m2 intravenously and levoleucovorin 100 mg/m2 intravenously, both daily for 5 days, or with 5-FU 370 mg/m2 intravenously and d,l-leucovorin 200 mg/m2 intravenously, both daily for 5 days. Treatment was repeated week 4 and week 8, and then every 5 weeks until disease progression or unacceptable toxicity. The following table presents the most frequent adverse reactions which occurred in patients in the 2 treatment arms.
|
Adverse Reaction |
Levoleucovorin/5FU n=318 |
d,l-Leucovorin/5FU n=307 |
||
|
Adverse Event N (%) |
Grade 1-4 |
Grade 3-4 |
Grade 1-4 |
Grade 3-4 |
|
Gastrointestinal Disorders |
||||
|
Stomatitis |
229 (72%) |
37 (12%) |
221 (72%) |
44 (14%) |
|
Diarrhea |
222 (70%) |
61 (19%) |
201 (65%) |
51 (17%) |
|
Nausea |
197 (62%) |
25 (8%) |
186 (61%) |
26 (8%) |
|
Vomiting |
128 (40%) |
17 (5%) |
114 (37%) |
18 (6%) |
|
Abdominal Pain1 |
45 (14%) |
10 (3%) |
57 (19%) |
10 (3%) |
|
General Disorders |
||||
|
Asthenia/Fatigue/Malaise |
91 (29%) |
15 (5%) |
99 (32%) |
34 (11%) |
|
Metabolism and Nutrition |
||||
|
Anorexia/Decreased Appetite |
76 (24%) |
13 (4%) |
77 (25%) |
5 (2%) |
|
Skin Disorders |
||||
|
Dermatitis |
91 (29%) |
3 (1%) |
86 (28%) |
4 (1%) |
|
Alopecia |
83 (26%) |
1 (0.3%) |
87 (28%) |
3 (1%) |
1Includes abdominal pain, upper abdominal pain, lower abdominal pain, and abdominal tenderness
6.3 Postmarketing Experience
Since adverse reactions from spontaneous reports are provided voluntarily from a population of uncertain size, it is not always possible to estimate reliably their frequency or establish a causal relationship to drug exposure. Spontaneously reported adverse reactions collected by the WHO Collaborating Center for International Drug Monitoring in Uppsala Sweden have yielded seven cases where levoleucovorin was administered with a regimen of methotrexate. The events were dyspnea, pruritus, rash, temperature change and rigors. For 217 adverse reactions (108 reports) where levoleucovorin was a suspected or interacting medication, there were 40 occurrences of “possible allergic reactions.”
In an analysis where calcium levoleucovorin was reported as the primary suspect drug and fluorouracil (FU) was reported as a concomitant medication, possible allergic reactions were reported among 47 cases (67 events).
7 DRUG INTERACTIONS
Folic acid in large amounts may counteract the antiepileptic effect of phenobarbital, phenytoin and primidone, and increase the frequency of seizures in susceptible children. It is not known whether folinic acid has the same effects. However, both folic and folinic acids share some common metabolic pathways. Caution should be taken when taking folinic acid in combination with anticonvulsant drugs.
Preliminary human studies have shown that small quantities of systemically administered leucovorin enter the CSF, primarily as its major metabolite, 5-methyltetrahydrofolate (5-MTHFA). In humans, the CSF levels of 5-MTHFA remain 1-3 orders of magnitude lower than the usual methotrexate concentrations following intrathecal administration.
Fusilev increases the toxicity of 5-fluorouracil [see Warnings and Precautions (5.2)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C. Animal reproduction studies have not been conducted with Fusilev. It is not known whether Fusilev can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Fusilev should be given to a pregnant woman only if clearly needed.
8.3 Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, and because of the potential for serious adverse reactions in nursing infants from Fusilev, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
8.5 Geriatric Use
Clinical studies of Fusilev in the treatment of osteosarcoma did not include subjects aged 65 and over to determine whether they respond differently from younger subjects.
In the NCCTG clinical trial of Fusilev in combination with 5-FU in advanced colorectal cancer, adverse reactions were consistent with 5-FU related toxicity and were similar for patients age 65 and older and for patients younger than age 65.
11 DESCRIPTION
Levoleucovorin is the levo isomeric form of racemic d,l-leucovorin, present as the calcium salt. Levoleucovorin is the pharmacologically active isomer of leucovorin [(6-S)-leucovorin].
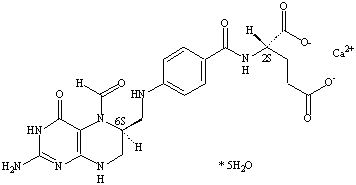
Fusilev for Injection and Fusilev Injection contain levoleucovorin calcium, which is one of several active, chemically reduced derivatives of folic acid. It is useful as antidote to the inhibition of dihydrofolate reductase by methotrexate. This compound has the chemical designation calcium (6S)-N-{4-[[(2-amino-5-formyl-1,4,5,6,7,8-hexahydro-4-oxo-6-pteridinyl)methyl] amino]benzoyl}-L-glutamate pentahydrate. The molecular weight is 601.6 and the structural formula is:
Its molecular formula is: C20H21CaN7O7 . 5 H2O.
Fusilev for Injection is supplied as a sterile lyophilized powder consisting of 64 mg levoleucovorin calcium pentahydrate (equivalent to 50 mg levoleucovorin) and 50 mg mannitol per 50 mg vial. Sodium hydroxide and/or hydrochloric acid are used to adjust the pH during manufacture. It is intended for intravenous administration after reconstitution with 5.3 mL of sterile 0.9% Sodium Chloride Injection, USP [See Dosage and Administration (2.6)]
Fusilev Injection is supplied as a sterile solution of either 175 mg levoleucovorin in 17.5 mL or 250 mg levoleucovorin in 25 mL. Each mL contains levoleucovorin calcium pentahydrate equivalent to 10 mg levoleucovorin and 8.3 mg sodium chloride. Sodium hydroxide is used for pH adjustment to pH 8.0 (6.5 to 8.5).
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.1.1 Levoleucovorin effects during high-dose methotrexate therapy
Levoleucovorin is the pharmacologically active isomer of 5-formyl tetrahydrofolic acid. Levoleucovorin does not require reduction by the enzyme dihydrofolate reductase in order to participate in reactions utilizing folates as a source of “one-carbon” moieties. Administration of levoleucovorin can counteract the therapeutic and toxic effects of folic acid antagonists such as methotrexate, which act by inhibiting dihydrofolate reductase.
12.1.2 Levoleucovorin effects in combination with 5-fluorouracil
Levoleucovorin can enhance the therapeutic and toxic effects of fluoropyrimidines used in cancer therapy such as 5-fluorouracil. 5-fluorouracil is metabolized to 5-fluoro-2'-deoxyuridine-5'-monophosphate (FdUMP), which binds to and inhibits thymidylate synthase (an enzyme important in DNA repair and replication). Levoleucovorin is readily converted to another reduced folate, 5,10-methylenetetrahydrofolate, which acts to stabilize the binding of FdUMP to thymidylate synthase and thereby enhances the inhibition of this enzyme.
12.2 Pharmacodynamics
Levoleucovorin is actively and passively transported across cell membranes. In vivo, levoleucovorin is converted to 5-methyltetrahydrofolic acid (5-methyl-THF), the primary circulating form of active reduced folate. Levoleucovorin and 5-methyl-THF are polyglutamated intracellularly by the enzyme folylpolyglutamate synthetase. Folylpolyglutamates are active and participate in biochemical pathways that require reduced folate.
12.3 Pharmacokinetics
The pharmacokinetics of levoleucovorin after intravenous administration of a 15 mg dose was studied in healthy male volunteers. After rapid intravenous administration, serum total tetrahydrofolate (total-THF) concentrations reached a mean peak of 1722 ng/mL. Serum (6S)-5-methyl-5,6,7,8-tetrahydrofolate concentrations reached a mean peak of 275 ng/mL and the mean time to peak was 0.9 hours. The mean terminal half-life for total-THF and (6S)-5-methyl-5,6,7,8-tetrahydrofolate was 5.1 and 6.8 hours, respectively.
A pharmacokinetic study was conducted in 40 healthy subjects who received a single intravenous dose of either Fusilev (200 mg/m2 ) or racemic d,l-leucovorin (400 mg/m2), each administered as a 2-hour infusion in a crossover design. Results indicate that the 90% confidence interval for the geometric mean ratios for both AUC0-inf and Cmax were within the standard limit of 80-125% for both l-leucovorin and l-5-methyl-THF. Therefore, the exposure to l-leucovorin and 5-methyl-THF (AUC0-inf and Cmax) was comparable whether it was administered as Fusilev or as d,l-leucovorin. The geometric mean AUC0-inf values for levoleucovorin were 30719 ng.h/mL and 31296 ng.h/mL for Fusilev and d,l-leucovorin, respectively. The geometric mean Cmax values for levoleucovorin were 10895 ng/mL and 11301 ng/mL for Fusilev and d,l-leucovorin, respectively. The geometric mean AUC0-inf values for 5-methyl-THF were 52105 ng.h/mL and 50137 ng.h/mL for Fusilev and d,l-leucovorin, respectively. The geometric mean Cmax values for 5-methyl-THF were 4930 ng/mL and 4658 ng/mL for Fusilev and d,l-leucovorin, respectively.
Use of Levoleucovorin in combination with 5-fluorouracil
A published cross study comparison showed that the mean dose-normalized steady-state plasma concentrations for both levoleucovorin and 5-methyl-THF were comparable whether 5-FU (370 mg/m2/day IV bolus) was given in combination with levoleucovorin (250 mg/m2 and 1000 mg/m2 as a continuous IV infusion for 5.5 days, N=9) or in combination with d,l-leucovorin (500 mg/m2 as a continuous IV infusion for 5.5 days, N=6).
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No studies have been conducted to evaluate the potential of levoleucovorin for carcinogenesis, mutagenesis and impairment of fertility.
13.2 Animal Toxicology and/or Pharmacology
The acute intravenous LD50 values in adult mice and rats were 575 mg/kg (1725 mg/m2) and 378 mg/kg (2268 mg/m2), respectively. Signs of sedation, tremors, reduced motor activity, prostration, labored breathing, and/or convulsion were observed in these studies. Anticipated human dose for each administration is approximately 5 mg/m2 for high-dose methotrexate therapy which represents a 3-log safety margin.
14 CLINICAL STUDIES
14.1 High-Dose Methotrexate Therapy
The safety and efficacy of Fusilev rescue following high-dose methotrexate were evaluated in 16 patients age 6-21 who received 58 courses of therapy for osteogenic sarcoma. High-dose methotrexate was one component of several different combination chemotherapy regimens evaluated across several trials. Methotrexate 12 g/m2 IV over 4 hours was administered to 13 patients, who received Fusilev 7.5 mg every 6 hours for 60 hours or longer beginning 24 hours after completion of methotrexate. Three patients received methotrexate 12.5 g/m2 IV over 6 hours, followed by Fusilev 7.5 mg every 3 hours for 18 doses beginning 12 hours after completion of methotrexate. The mean number of Fusilev doses per course was 18.2 and the mean total dose per course was 350 mg. The efficacy of Fusilev rescue following high-dose methotrexate was based on the adverse reaction profile. [See Adverse Reactions (6)]
14.2 Combination with 5-FU in Colorectal Cancer
In a randomized clinical study conducted by the Mayo Clinic and the North Central Cancer Treatment Group (Mayo/NCCTG) in patients with advanced metastatic colorectal cancer, three treatment regimens were compared: d,l-leucovorin (LV) 200 mg/m2 and 5-fluorouracil (5-FU) 370 mg/m2 versus LV 20 mg/m2 and 5-FU 425 mg/m2 versus 5-FU 500 mg/m2. All drugs were administered by slow intravenous infusion daily for 5 days repeated every 28 to 35 days. Response rates were 26% (p=0.04 versus 5-FU alone), 43% (p=0.001 versus 5-FU alone) and 10% for the high dose leucovorin, low dose leucovorin and 5-FU alone groups, respectively. Respective median survival times were 12.2 months (p=0.037), 12 months (p=0.050), and 7.7 months. The low dose LV regimen gave a statistically significant improvement in weight gain of more than 5%, relief of symptoms, and improvement in performance status. The high dose LV regimen gave a statistically significant improvement in performance status and trended toward improvement in weight gain and in relief of symptoms but these were not statistically significant.
In a second Mayo/NCCTG randomized clinical study the 5-FU alone arm was replaced by a regimen of sequentially administered methotrexate (MTX), 5-FU, and LV. Response rates with LV 200 mg/m2 and 5-FU 370 mg/m2 versus LV 20 mg/m2 and 5-FU 425 mg/m2 versus sequential MTX and 5-FU and LV were respectively 31% (p≤0.01), 42% (p≤0.01), and 14%. Respective median survival times were 12.7 months (p≤0.04), 12.7 months (p≤0.01), and 8.4 months. No statistically significant difference in weight gain of more than 5% or in improvement in performance status was seen between the treatment arms.
A randomized controlled trial conducted by the NCCTG in patients with advanced metastatic colorectal cancer failed to show superiority of a regimen of 5-FU + levoleucovorin to 5-FU + d,l-leucovorin in overall survival. Patients were randomized to 5-FU 370 mg/m2 intravenously and levoleucovorin 100 mg/m2 intravenously, both daily for 5 days, or with 5-FU 370 mg/m2 intravenously and d,l-leucovorin 200 mg/m2 intravenously, both daily for 5 days. Treatment was repeated week 4 and week 8, and then every 5 weeks until disease progression or unacceptable toxicity.
Fusilev is dosed at one-half the usual dose of racemic d,l-leucovorin.
16 HOW SUPPLIED/STORAGE AND HANDLING
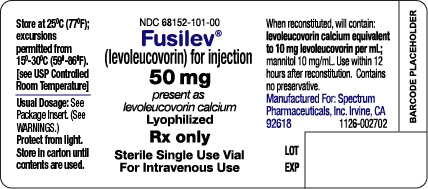
Each 50 mg single-use vial of Fusilev for Injection contains a sterile lyophilized powder consisting of 64 mg levoleucovorin calcium pentahydrate (equivalent to 50 mg levoleucovorin) and 50 mg mannitol.
50 mg vial of freeze-dried powder – NDC: 68152-101-00.
Store at 25° C (77 °F) in carton until contents are used. Excursions permitted from 15-30° C (59-86 °F). [See USP Controlled Room Temperature]. Protect from light.
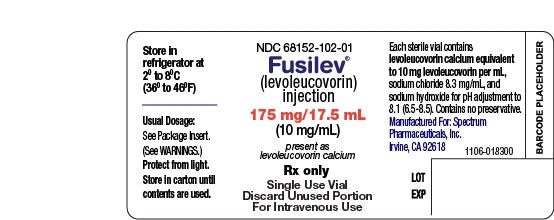
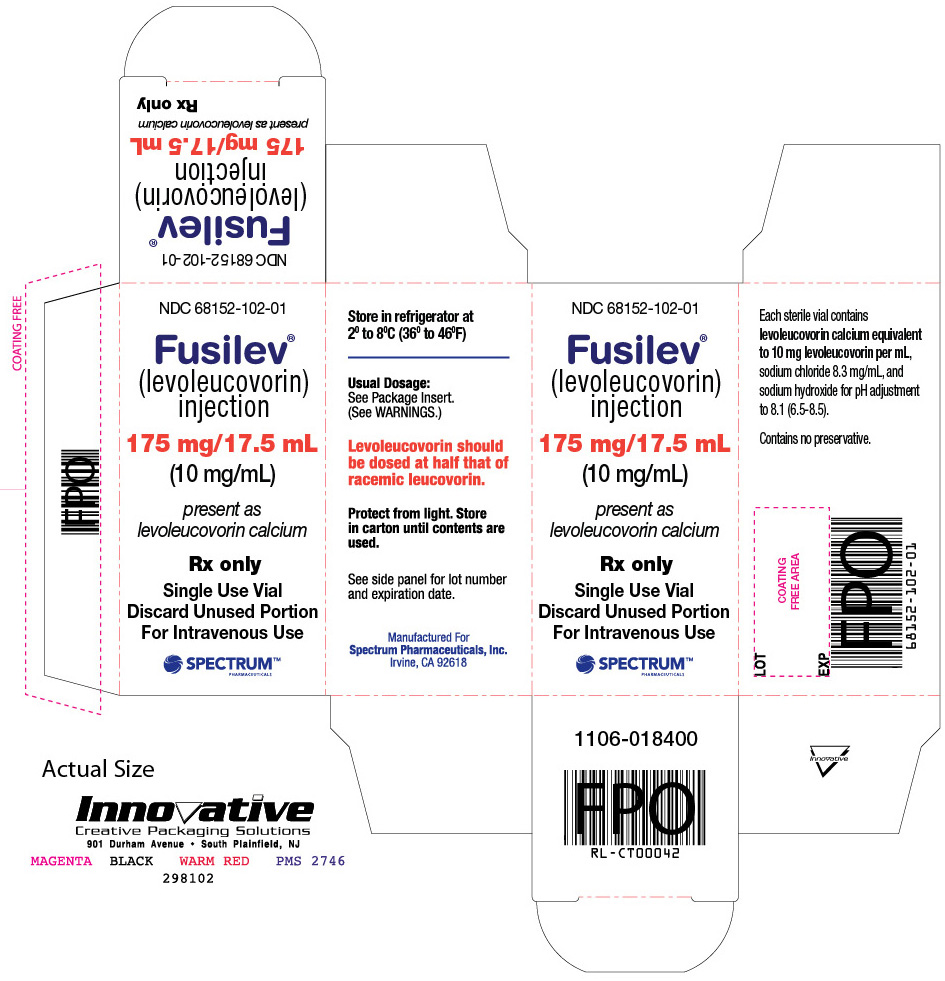
Fusilev Injection, 175 mg contains 17.5 mL sterile solution in a single-use vial. Each mL contains levoleucovorin calcium pentahydrate equivalent to 10 mg levoleucovorin and 8.3 mg sodium chloride.
175 mg/17.5 mL solution – NDC: 68152-102-01
Fusilev Injection, 250 mg contains 25 mL sterile solution in a single-use vial. Each mL contains levoleucovorin calcium pentahydrate equivalent to 10 mg levoleucovorin and 8.3 mg sodium chloride.
250 mg/25 mL solution – NDC: 68152-102-02
Store in refrigerator at 2°C to 8°C (36°F to 46°F). Protect from light. Store in carton until contents are used.
Manufactured for Spectrum Pharmaceuticals, Inc.
Irvine, CA 92618
Fusilev® is a registered trademark of Spectrum Pharmaceuticals, Inc.
| FUSILEV
levoleucovorin injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| FUSILEV
levoleucovorin injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Spectrum Pharmaceuticals, Inc. (790888002) |