N/A- atropine injection, 2 mg injection N/A- atropine sulfate injection usp, 1 mg/0.7 ml injection N/A- atropine sulfate injection usp, 0.5 mg/0.7 ml injection
N/A by
Drug Labeling and Warnings
N/A by is a Prescription medication manufactured, distributed, or labeled by Rafa Laboratories, Ltd.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ATROPINE safely and effectively. See full prescribing information for ATROPINE.
ATROPINE injection, for intramuscular use
Initial U.S. Approval: 1973INDICATIONS AND USAGE
(1)
(1)
Atropine, a cholinergic muscarinic antagonist, is indicated for the treatment of poisoning by susceptible organophosphorus nerve agents having anticholinesterase activity as well as organophosphorus or carbamate insecticides in adults and pediatric patients weighing more than 41 kg (90 pounds) (1). (1)
DOSAGE AND ADMINISTRATION
- Atropine is intended as an initial treatment as soon as symptoms appear; definitive medical care should be sought immediately. (2.1)
- Administer each dose of the 2 mg Atropine autoinjector into the patient’s mid-lateral outer thigh (2.1).
- Dosage for Mild Symptoms: If the patient experiences two or more mild symptoms, administer one injection intramuscularly into the mid-lateral thigh. If, at any time after the first dose, the patient develops any of the severe symptoms, administer two additional injections intramuscularly in rapid succession (2.2).
- Dosage for Severe Symptoms: If a patient has any of the severe symptoms, immediately administer three injections intramuscularly into the patient's mid-lateral thigh in rapid succession (2.2).
DOSAGE FORMS AND STRENGTHS
Injection: 1.67 mg/0.7 mL atropine base (equivalent to 2 mg atropine sulfate) in a single-dose prefilled autoinjector (3) (3)
CONTRAINDICATIONS
None (4) (4)
WARNINGS AND PRECAUTIONS
- Cardiovascular (CV) Risks: Tachycardia, palpitations, premature ventricular contractions, flutter, fibrillation, etc. Use caution in patients with known CV disease or conduction problems. (5.1)
- Heat Injury: May inhibit sweating and lead to hyperthermia; avoid excessive exercising and heat exposure. (5.2)
- Acute Glaucoma: May precipitate in susceptible individuals. (5.3)
- Urinary Retention: Administer with caution in patient with bladder outflow obstruction. (5.4)
- Pyloric Stenosis: May convert into complete obstruction. (5.5)
- Exacerbation of Chronic Lung Disease: Atropine may cause inspiration of bronchial secretions and formation of dangerous viscid plugs in individuals with chronic lung disease; monitor respiratory status. (5.6)
- Hypersensitivity: Atropine may cause hypersensitivity reactions, including anaphylaxis (5.7)
ADVERSE REACTIONS
Mild to moderate pain may be experienced at the site of injection. Common adverse reactions of atropine include dryness of the mouth, blurred vision, dry eyes, photophobia, confusion, headache, dizziness, tachycardia, palpitations, flushing, urinary hesitance or retention, constipation, abdominal pain, abdominal distention, nausea, vomiting, loss of libido, and impotency (6.1, 6.2). (6)
(6)
To report SUSPECTED ADVERSE REACTIONS, contact Rafa Laboratories at 1-386-418-7911 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch (6)
DRUG INTERACTIONS
Revised: 7/2019
- Table of Contents
- INDICATIONS & USAGE
-
DOSAGE & ADMINISTRATION
Important Administration Information
- Three (3) Atropine autoinjectors should be available for use in each patient at risk for nerve agent or organophosphate insecticide poisoning; one (1) for mild symptoms plus two (2) more for severe symptoms [see Dosage and Administration (2.2)].
- Only administer Atropine to patients experiencing symptoms of organophosphorus poisoning in a situation where exposure is known or suspected. The Atropine autoinjector is intended as an initial treatment of the muscarinic symptoms of insecticide or nerve agent poisonings as soon as symptoms appear; definitive medical care should be sought immediately.
- In general, atropine should not be used until cyanosis has been overcome since atropine may produce ventricular fibrillation and possible seizures in the presence of hypoxia.
- The Atropine autoinjector should be used by persons who have had adequate training in the recognition and treatment of nerve agent or insecticide intoxication, but may be administered by a caregiver or by self-administration if a trained provider is not available.
- Close supervision of all treated patients is indicated for at least 48 to 72 hours.
- In severe poisonings, concurrent administration of an anticonvulsant (preferably a benzodiazepine) may be warranted if seizure is suspected in the unconscious individual because overt jerking may not be apparent because of the effects of the poison [see Drug Interactions (7.2)].
- In poisonings caused by organophosphorous nerve agents and insecticides it may also be helpful to concurrently administer a cholinesterase reactivator such as pralidoxime chloride [see Drug Interactions (7.1)].
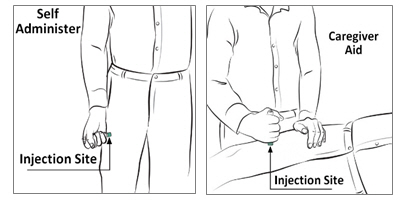
- The injection site is the mid-lateral thigh area. The Atropine autoinjector can inject through clothing. However, make sure pockets at the injection site are empty. People who may not have a lot of fat at the injection site should also be injected in the mid-lateral thigh, but before giving the injection, bunch up the thigh to provide a thicker area for injection.
Dosage InformationDosage for Mild Symptoms in Adults and Pediatric Patients Weighing More Than 41 kg (90 Pounds)
First Dose: If the patient experiences two or more mild symptoms of nerve agent (nerve gas) or insecticide exposure listed in Table 1, administer one (1) Atropine injection intramuscularly into the mid-lateral outer thigh.
Additional Doses: If, at any time after the first dose, the patient develops any of the severe symptoms listed in Table 1, administer two (2) additional Atropine injections intramuscularly in rapid succession.
Wait 10 to 15 minutes for Atropine to take effect. If, after 10 to 15 minutes, the patient does not develop any of the severe symptoms listed in Table 1, no additional Atropine injections are recommended.
If possible, a person other than the patient should administer the second and third 2 mg Atropine autoinjectors.
Dosage for Severe Symptoms in Adults and Pediatric Patients Weighing More Than 41 kg (90 Pounds)
If a patient is either unconscious or has any of the severe symptoms listed in Table 1, immediately administer three (3) Atropine injections intramuscularly into the patient’s mid-lateral outer thigh in rapid succession.
Table 1: Common Signs/Symptoms of Organophosphorus and/or Carbamate Poisoning MILD symptoms include:
- Blurred vision or miosis
- Unexplained excessive lacrimation
- Unexplained excessive nasopharyngeal secretions
- Increased salivation
- Chest tightness, difficulty breathing, wheezing, or coughing
- Tremors throughout the body or muscular twitching
- Nausea, vomiting, abdominal cramping, or diarrhea
- Tachycardia or bradycardia
SEVERE symptoms include:
- Altered mental status
- Loss of consciousness
- Respiratory distress
- Excessive secretions from the lungs/airway
- Severe muscular twitching, generalized weakness or paralysis
- Involuntary urination and/or defecation
- Convulsions or seizures
Additional Care Instructions
Environmental
All patients should be evacuated immediately from the contaminated environment.
Protective masks and clothing should be used when available.
Aggressive and safe decontamination procedures should be undertaken as soon as possible.
If dermal exposure has occurred, clothing should be removed and the hair and skin washed thoroughly with sodium bicarbonate or alcohol as soon as possible.
Physicians and/or other medical personnel assisting evacuated patients of nerve and insecticide poisoning should avoid exposing themselves to contamination by the patient’s clothing.Medical
Medical help should be sought immediately.
Emergency care of the severely poisoned individual should include removal of oral and bronchial secretions, maintenance of a patent airway, supplemental oxygen and, if necessary, artificial ventilation.
Severe difficulty in breathing requires artificial respiration in addition to the use of Atropine since Atropine is not dependable in reversing the weakness or paralysis of the respiratory muscles.Refer to the illustrated dose-specific Instructions for Use for autoinjector administration instructions.
Antidotes, such as Atropine, should not be relied upon solely to provide complete protection from chemical nerve agents and insecticide poisoning. - DOSAGE FORMS & STRENGTHS
- CONTRAINDICATIONS
-
WARNINGS AND PRECAUTIONS
Cardiovascular Risks
Cardiovascular adverse reactions reported in the literature for atropine include, but are not limited to, sinus tachycardia, palpitations, premature ventricular contractions, atrial flutter, atrial fibrillation, ventricular flutter, ventricular fibrillation, cardiac syncope, asystole, and myocardial infarction [see Adverse Reactions (6)]. In patients with a recent myocardial infarction and/or severe coronary artery disease, there is a possibility that atropine-induced tachycardia may cause ischemia, extend or initiate myocardial infarcts, and stimulate ventricular ectopy and fibrillation. Atropine should be used with caution in patients with known cardiovascular disease or cardiac conduction problems.
Heat Injury
Atropine may inhibit sweating which, in a warm environment or with excessive exercise, can lead to hyperthermia and heat injury. To the extent feasible, avoid excessive exercise and heat exposure [see Adverse Reactions (6)].
Acute Glaucoma
Atropine may cause acute glaucoma and should be administered with caution in patients at risk for acute glaucoma or who have severe narrow angle glaucoma. Monitor for signs and symptoms of intraocular pressure, as appropriate.
Urinary Retention
Atropine may cause urinary retention and should be administered with caution to patients with clinically significant bladder outflow obstruction.
Pyloric Stenosis
Atropine may cause complete pyloric obstruction in patients with partial pyloric stenosis. These patients should be monitored for gastrointestinal symptoms following administration of Atropine.
Exacerbation of Chronic Lung Disease
Atropine may cause thickening of bronchial secretions and formation of dangerous viscid plugs in individuals with chronic lung disease. Respiratory status should be monitored in individuals with chronic lung disease following administration of Atropine.
Hypersensitivity
Atropine can cause hypersensitivity reactions, including anaphylactic reactions [see Adverse Reactions (6)]. Medical supervision is necessary in patients who have had previous anaphylactic reactions to atropine and require treatment for organophosphorus or nerve agent poisoning.
-
ADVERSE REACTIONS
The following serious adverse reactions are described elsewhere in the labeling:
- Cardiovascular Risks [ see Warnings and Precautions ( 5.1)]
- Heat Injury [ see Warnings and Precautions ( 5.2)]
- Acute Glaucoma [ see Warnings and Precautions ( 5.3)]
- Urinary Retention [ see Warnings and Precautions ( 5.4)]
- Pyloric Stenosis [ see Warnings and Precautions ( 5.5)]
- Exacerbation of Chronic Lung Disease [ see Warnings and Precautions ( 5.6)]
- Hypersensitivity [ see Warnings and Precautions (5.7)]
The following adverse reactions associated with the use of atropine were identified in the literature. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Injection Site ReactionsMild to moderate pain may be experienced at the site of injection.
Adverse Reactions at Recommended Dosages
The major and most common side effects of atropine can be attributed to its antimuscarinic action. These include dryness of the mouth, blurred vision, dry eyes, photophobia, confusion, headache, dizziness, fatigue, tachycardia, palpitations, flushing, urinary hesitance or retention, constipation, abdominal pain, abdominal distention, nausea, vomiting, loss of libido, and impotency. Anhidrosis may produce heat intolerance and impairment of temperature regulation especially in a hot environment.
Hypersensitivity
Hypersensitivity reactions will occasionally occur with atropine; these are usually seen as skin rashes, on occasion progressing to exfoliation. Anaphylactic reactions have occurred.
Additional Adverse Reactions to Atropine by Organ SystemThe following adverse reactions were reported in published literature for atropine in both adults and pediatric patients:
Cardiovascular: Sinus tachycardia, supraventricular tachycardia, junctional tachycardia, ventricular tachycardia, bradycardia, palpitations, ventricular arrhythmia, ventricular flutter, ventricular fibrillation, atrial arrhythmia, atrial fibrillation, atrial ectopic beats, ventricular premature contractions, bigeminal beats, trigeminal beats, nodal extrasystole, ventricular extrasystole, supraventricular extrasystole, asystole, cardiac syncope, prolongation of sinus node recovery time, cardiac dilation, left ventricular failure, myocardial infarction, intermittent nodal rhythm (no P wave), prolonged P wave, shortened PR segment, R on T phenomenon, shortened RT duration, widening and flattening of QRS complex, prolonged QT interval, flattening of T wave, repolarization abnormalities, altered ST-T waves, retrograde conduction, transient AV dissociation, increased blood pressure, decreased blood pressure, labile blood pressure, weak or impalpable peripheral pulses.
Eye: Mydriasis, pupils poorly reactive to light, decreased contrast sensitivity, decreased visual acuity, decreased accommodation, cycloplegia, strabismus, heterophoria, cyclophoria, acute angle closure glaucoma, conjunctivitis, keratoconjunctivitis sicca, blindness, tearing, dry conjunctiva, irritated eyes, crusting of eyelid, blepharitis.
Gastrointestinal: Paralytic ileus, decreased bowel sounds, delayed gastric emptying, decreased food absorption, dysphagia.
General: Hyperpyrexia, lethargy, somnolence, chest pain, excessive thirst, weakness, syncope, insomnia, tongue chewing, dehydration, feeling hot.
Special Investigations: Leukocytosis, hyponatremia, elevated BUN, elevated hemoglobin, elevated erythrocytes, low hemoglobin, hypoglycemia, hyperglycemia, hypokalemia, increase in photic stimulation on EEG, signs of drowsiness on EEG, runs of alpha waves on EEG, alpha waves (EEG) blocked upon opening eyes.
Metabolic: Failure to feed.
Central Nervous System: Ataxia, hallucinations (visual or aural), seizures (generally tonic-clonic), abnormal movements, coma, stupor, amnesia, diminished tendon reflexes, hyperreflexia, muscle twitching, opisthotnos, Babinski's reflex/Chaddock's reflex, hypertonia, dysmetria, muscle clonus, sensation of intoxication, difficulty concentrating, vertigo, dysarthria.
Psychiatric: Agitation, restlessness, delirium, paranoia, anxiety, mental disorders, mania, withdrawn behavior, behavior changes.
Genitourinary: Difficulty in micturation, urine urgency, distended urinary bladder, bed-wetting.
Pulmonary: Tachypnea, slow respirations, shallow respirations, breathing difficulty, labored respirations, inspiratory stridor, laryngitis, laryngospasm, pulmonary edema, respiratory failure, subcostal recession.
Dermatologic: Dry mucous membranes, dry warm skin, oral lesions, dermatitis, petechiae, rash, macular rash, papular rash, maculopapular rash, scarlatiniform rash, erythematous rash, sweating/moist skin, cold skin, cyanosed skin, salivation.
Adverse Reactions Caused by Inadvertent Injection
Administering additional 2 mg Atropine autoinjectors by mistake in the absence of actual nerve agent or insecticide poisoning may cause an overdose of atropine which could result in temporary incapacitation (inability to walk properly, see clearly or think clearly for several or more hours). Patients with cardiac disease may be at risk for serious adverse events, including death.
Adverse Reactions Observed in Pediatric Patients after Inappropriate Administration of Atropine
Amitai et al. (JAMA 1990) evaluated the safety of an atropine autoinjector in a case series of 240 children who received the atropine inappropriately (i.e., no nerve agent exposure) during the 1990 Gulf War Period. Overall, severity of atropinization followed a nonlinear correlation with dose. Estimated doses up to 0.045 mg/kg produced no signs of atropinization. Estimated doses between 0.045 mg/kg to 0.175 mg/kg and even greater than 0.175 mg/kg were associated with mild and severe effects respectively. Actual dosage received by children may have been considerably lower than estimated since incomplete injection in many cases was suspected. Regardless, adverse events reported were generally mild and self-limited. Few children required hospitalization. Adverse reactions reported were dilated pupils (43%), tachycardia (39%), dry membranes (35%), flushed skin (20%), temperature 37.8° C or 100° F (4%), and neurologic abnormalities (5%). There was also local pain and swelling. In patients with electrocardiograms, 22 of 91 (24%) children had severe tachycardia of 160-190 bpm. Neurologic abnormalities consisted of irritability, agitation, confusion, lethargy, and ataxia. Atropine 2mg is only approved for pediatric patients weighing more than 41kg at the recommended dosing.
-
DRUG INTERACTIONS
Pralidoxime
When atropine and pralidoxime are used together, the signs of atropinization (flushing, mydriasis, tachycardia, dryness of the mouth and nose) may occur earlier than might be expected when atropine is used alone because pralidoxime may potentiate the effect of atropine. Excitement and manic behavior immediately following recovery of consciousness have been reported in several cases. However, similar behavior has occurred in cases of organophosphate poisoning that were not treated with pralidoxime.
Barbiturates
Barbiturates are potentiated by the anticholinesterases; therefore, barbiturates should be used cautiously in the treatment of convulsions resulting from exposure to Atropine.
-
USE IN SPECIFIC POPULATIONS
Pregnancy
Risk Summary
Atropine readily crosses the placental barrier and enters fetal circulation. There are no adequate data on the developmental risk associated with the use of atropine in pregnant women. Adequate animal reproduction studies have not been conducted with atropine.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Lactation
Risk Summary
Atropine has been reported to be excreted in human milk. There are no data on the effects of atropine on the breastfed infant or the effects of the drug on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Atropine and any potential adverse effects on the breastfed infant from Atropine or from the underlying maternal condition.
Pediatric Use
Safety and effectiveness of the 2 mg Atropine autoinjector in pediatric patients weighing less than or equal to 41 kg (90 pounds) have not been established.
Safety and effectiveness of atropine in patients weighing more than 41 kg (90 pounds) are supported by published literature. Adverse reactions seen in pediatric patients are similar to those that occur in adult patients. However, central nervous system effects are often seen earlier, and pediatric patients may be more susceptible to the pharmacologic effects of atropine [see Adverse Reactions (6)].
Although the 2 mg Atropine autoinjector is not approved for pediatric patients less than 41 kg, overheating (atropine fever) caused by suppression of sweat gland activity may be more pronounced in infants and small children. Extreme hyperthermia in a newborn has been reported with as little as 0.065 mg orally.
Geriatric Use
Geriatric patients may be more susceptible to the pharmacologic effects of atropine [see Adverse Reactions (6)].
-
OVERDOSAGE
Symptoms
Manifestations of atropine overdose are dose-related and include flushing, dry skin and mucous membranes, tachycardia, widely dilated pupils that are poorly responsive to light, blurred vision, and fever (which can sometimes be dangerously elevated). Locomotor difficulties, disorientation, hallucinations, delirium, confusion, agitation, coma, and central depression can occur and may last 48 hours or longer. In instances of severe atropine intoxication, respiratory depression, coma, circulatory collapse, and death may occur.
Treatment
Supportive treatment should be administered as indicated. If respiration is depressed, artificial respiration with oxygen is necessary. Ice bags, alcohol sponges, or a hypothermia blanket may be required to reduce fever, especially in pediatric patients. Catheterization may be necessary if urinary retention occurs. Since atropine elimination takes place through the kidney, urinary output must be maintained and increased if possible; however, dialysis has not been shown to be helpful in overdose situations. Intravenous fluids may be indicated. Because of atropine-induced photophobia, the room should be darkened.
A benzodiazepine may be needed to control marked excitement and convulsions. However, large doses for sedation should be avoided because the central nervous system depressant effect may coincide with the depressant effect occurring late in severe atropine poisoning. Barbiturates are potentiated by the anticholinesterases; therefore, barbiturates should be used cautiously in the treatment of convulsions. Central nervous system stimulants are not recommended.
-
DESCRIPTION
The Atropine prefilled autoinjector is a single dose, self-contained unit designed for self or caregiver administration.
Each 2 mg Atropine autoinjector delivers 1.67 mg atropine (equivalent to 2 mg atropine sulfate) in 0.7 mL of sterile pyrogen-free solution for intramuscular injection. Each 2 mg autoinjector also contains the following inactive ingredients: citric acid monohydrate (buffer), 12.47 mg glycerin, 2.8 mg phenol, and 3.05 mg sodium citrate dihydrate (buffer). The pH range is 4.1 - 4.5.
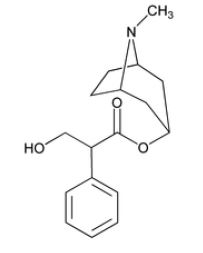
Atropine, a cholinergic muscarinic antagonist, occurs as white crystals, usually needle-like, or as a white, crystalline powder. It is highly soluble in water with a molecular weight of 289.38. Atropine, a naturally occurring belladonna alkaloid, is a racemic mixture of equal parts of d- and l-hyoscyamine; its activity is due almost entirely to the levo isomer of the drug.
Chemically, atropine is designated as 1αH,5αH-tropan-3–ol (±)-tropate (ester). Its empirical formula is C17H23NO3 and its structural formula is:
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Atropine competitively blocks the effects of acetylcholine, including excess acetylcholine due to organophosphorus poisoning, at muscarinic cholinergic receptors on smooth muscle, cardiac muscle, secretory gland cells, and in peripheral autonomic ganglia and the central nervous system.
Pharmacodynamics
Atropine reduces secretions in the mouth and respiratory passages, relieves the constriction and spasm of the respiratory passages, and may reduce the paralysis of respiration that results from toxic nerve agents which increase anticholinesterase activity in the central nervous system. Atropine- induced parasympathetic inhibition may be preceded by a transient phase of stimulation, especially on the heart where small doses first slow the rate before characteristic tachycardia develops because of paralysis of vagal control. Although mild vagal excitation occurs, the increased respiratory rate and occasionally increased depth of respiration produced by atropine are more probably the result of bronchiolar dilatation. Accordingly, atropine is an unreliable respiratory stimulant, and large or repeated doses may depress respiration.
Adequate doses of atropine can prevent or abolish various types of reflex vagal cardiac slowing or asystole. The drug also can prevent or abolish bradycardia or asystole produced by injection of choline esters, anticholinesterase agents or other parasympathomimetic drugs, and cardiac arrest produced by stimulation of the vagus. Atropine may also lessen the degree of partial heart block when vagal activity is an etiologic factor. In some individuals with complete heart block, the idioventricular rate may be accelerated by atropine; in others, the rate is stabilized. In some patients with conduction defects, atropine may cause paradoxical atrioventricular (A-V) block and nodal rhythm.
Systemic doses of atropine slightly raise systolic and lower diastolic pressures and can produce significant postural hypotension. Such doses also slightly increase cardiac output and decrease central venous pressure. Atropine can dilate cutaneous blood vessels, particularly in the “blush” area (atropine flush), and may cause overheating due to suppression of sweat gland activity [see Warnings and Precautions (5.2)].
Pharmacokinetics
Atropine is well absorbed after intramuscular administration. Atropine is distributed throughout the various body tissues and fluids. Much of the drug is metabolized by enzymatic hydrolysis, particularly in the liver; from 13 to 50% is excreted unchanged in the urine. Atropine has been reported to be excreted in human milk [see Use in Specific Populations (8.2)]. Atropine readily crosses the placental barrier and enters the fetal circulation.
The approximate Cmax of atropine following 1.67 mg atropine given intramuscularly to adults by the 2 mg AtroPen® delivery system was 9.6 ± 1.5 (mean ± SEM) ng/mL. The mean Tmax was 3 minutes. The T½ of intravenous atropine in pediatric subjects over 2 years is 2.5 ± 1.2 (mean ± SD) hours; in adults 16–58 years the T½ is 3.0 ± 0.9 (mean ± SD) hours; in geriatric patients 65–75 years it is 10.0 ± 7.3 (mean ± SD) hours. The protein binding of atropine is 14 to 22% in plasma. There are gender differences in the pharmacokinetics of atropine. The AUC(0-inf) and Cmax were 15% higher in females than males. The half-life of atropine is slightly shorter (approximately 20 minutes) in females than males.
-
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
No adequate studies regarding the carcinogenic potential of atropine have been conducted.
Mutagenesis
Studies to assess the mutagenic potential of atropine have not been conducted.
Impairment of Fertility
In studies in which male rats were orally administered atropine (62.5 to 125 mg/kg) for one week prior to mating and throughout a 5-day mating period with untreated females, a dose-related decrease in fertility was observed. A no-effect dose for male reproductive toxicity was not established. The lowest dose tested was approximately 300 times (on a mg/m2 basis) the dose of atropine in a single autoinjector application.
Fertility studies of atropine in females have not been conducted.
-
HOW SUPPLIED
How Supplied
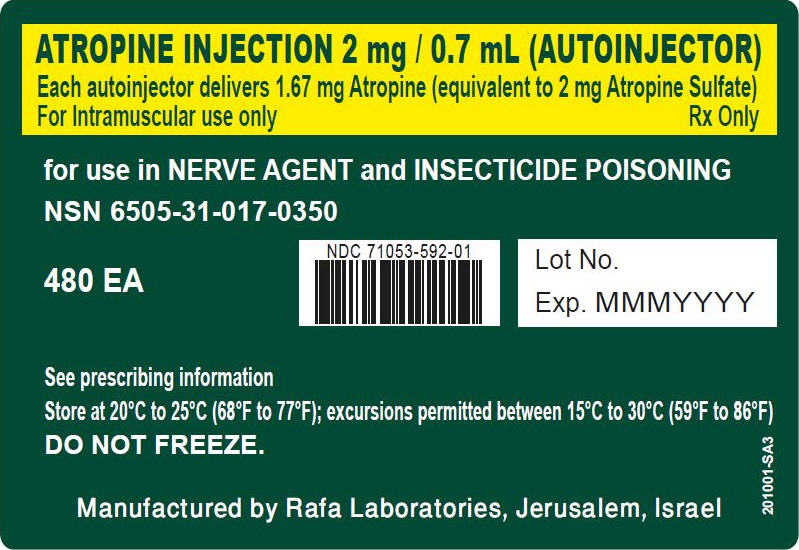
The 2 mg Atropine autoinjector provides atropine base 1.67 mg/0.7 mL (equivalent to atropine sulfate 2 mg/0.7 mL) in a sterile solution for intramuscular injection.
The 2 mg Atropine autoinjector is supplied as 480 self-contained single-dose autoinjectors per box (NDC: 71053-592-01).
Storage and Handling
Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
Do Not Freeze.
-
88436-1 - Section Title Not Found In Database
Advise the patient to read the FDA-approved patient labeling (Instructions for Use).
Administration
Ensure that users understand the indications for and use of Atropine, including review of symptoms of poisoning and operation of the Atropine autoinjector [see Dosage and Administration (2.2)].
Seek Definitive Medical Care
If feasible and appropriate, advise patients that Atropine is an initial emergency treatment, that they need additional care at a healthcare facility.
Avoid Overheating
If feasible and appropriate, advise the patient to avoid a hot environment and excessive physical activity since atropine can inhibit sweating which can lead to overheating and heat injury.
Manufactured by:
RAFA LABORATORIES, LTD.
JERUSALEM,ISRAEL
-
INSTRUCTIONS FOR USE
Instructions for Use
ATROPINE
injection, for intramuscular use
2 mg Atropine single-dose autoinjector
If possible, a healthcare provider or someone who has been trained to identify and treat the symptoms of exposure to nerve agents or insecticides should give (administer) the Atropine autoinjector. If a healthcare provider is not available during an emergency, a patient or a caregiver might need to give the Atropine injection.
Individuals should not rely only on Atropine for protection from nerve agent or insecticide poisoning.
Patients and caregivers need to wear clothing to protect their skin and goggles and masks to protect their face and eyes when available to avoid exposure.
Leave the exposed (contaminated) area as quickly as possible.
Get medical help right away after exposure.
Step 1: Decide if the 2 mg Atropine autoinjector is right to use based on weight and age.
- The 2 mg Atropine autoinjector is for use only in adults and children weighing over 90 pounds (41 kg) (generally over 10 years of age).
- Do not use the 2 mg Atropine autoinjector for children weighing 90 pounds (41 kg) and less (generally 10 years of age and younger). The dose of the 2 mg Atropine autoinjector cannot be changed.
Step 2: Decide if symptoms are mild or severe using Table 1 below. The number of injections needed depends on if there are 2 or more mild symptoms or if there are any severe symptoms.
Note: You may not see all of these symptoms in yourself or others exposed to a nerve agent or certain insecticide poisoning.
Table 1. Symptoms of Nerve Agent or Insecticide Poisoning Mild symptoms include:
- Blurred vision
- The black circle in the center of the colored part of the eye (pupil) is very small
- Unexplained excessive teary eyes
- Unexplained excessive runny nose
- Increased saliva or drooling
- Chest tightness, difficulty breathing, wheezing, or coughing
- Shaking (tremors) throughout the body or muscle twitching
- Nausea or vomiting
- Stomach cramps or diarrhea
- Fast heartbeat or pounding in your chest (tachycardia)
- Slow heartbeat (bradycardia)
Severe symptoms include:
- Strange or confused behavior
- Passing out (unconsciousness)
- Severe breathing problems such as short, quick breaths through the mouth (gasping for air)
- Large amount of fluid (secretions) coming from the mouth or nose
- Severe muscle twitching, general weakness, or paralysis
- Inability to control urine or stool (bowel movement)
- Sudden uncontrollable or irregular movements of parts of your body (convulsions or seizures)
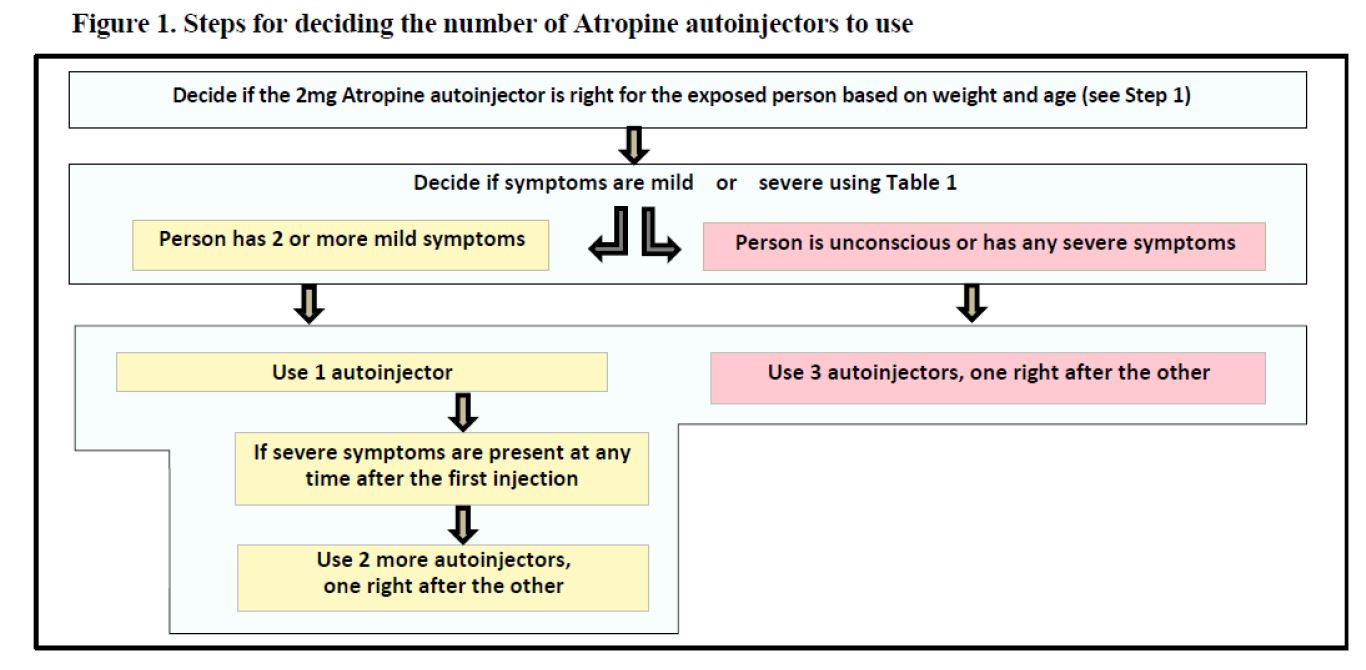
Step 3: Decide the number of Atropine autoinjectors to use based on if the symptoms are mild or severe. See Table 1 and Figure 1.
Mild Symptoms (see Table 1)
First Dose: If you have or see someone with 2 or more mild symptoms listed in Table 1 and exposure is known or suspected, give 1 injection of Atropine into the outer thigh using the Atropine autoinjector. You can inject through clothing, but make sure pockets at the injection site are empty. Keep checking to see if symptoms continue or get worse. Get medical help right away.
Additional Doses: If at any time after the first dose (1 injection) the person who was exposed starts to have any of the severe symptoms listed in Table 1, you will need to give 2 more injections quickly one right after the other using a new Atropine autoinjector for each injection. Do not use the same autoinjector more than one time. If you have given yourself the first injection, someone else should give you the second and third injections, if possible.
You can inject additional doses through clothing, but make sure pockets at the injection site are empty.
No more injections are needed if the person who was exposed does not get sever symptoms 10 to 15 minutes after the first dose (1 injection).
Severe Symptoms (see Table 1)
If you have or see someone with any of the severe symptoms listed in Table 1 and exposure is known or suspected, or you see an exposed person passed out (unconscious), give 3 injections into the outer thigh quickly one right after the other, using 3 new autoinjectors.
You can inject through clothing, but make sure pockets at the injection site are empty. Get medical help right away.
 Step 4: Instructions for how to use the Atropine autoinjector
Step 4: Instructions for how to use the Atropine autoinjector

A.) Hold the plastic sleeve on both sides of the dotted lines (perforation) and tear apart at the edge to open. Remove the autoinjector from the plastic sleeve.
Be careful not to place fingers on the green tip.

B.) Firmly hold the autoinjector with the green tip pointed down. 
C.) Pull off the yellow safety cap with your other hand. 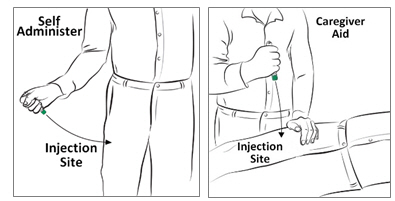
D.) Aim and firmly inject the green tip straight down (at a 90° angle) against the outer thigh. The autoinjector will give the medicine when you do this. You can inject through clothing, but make sure pockets at the injection site are empty.
Note: People who may not have a lot of fat at the injection site should also be injected in the outer thigh. Before giving the injection, pinch a fold of skin firmly on the outer thigh to provide a thicker area for the injection.
E.) Hold the autoinjector firmly in place for at least 10 seconds to allow the injection to finish.
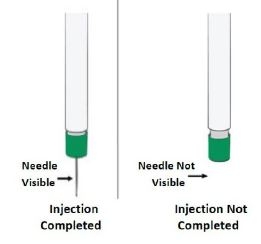
F.) After 10 seconds, remove the autoinjector from the outer thigh and massage the injection site in a circle motion for several seconds.
Note: If you do not see the needle after removing it from the outer thigh, the injection is not completed.
Check to be sure the yellow safety cap has been removed. If the yellow safety cap has been removed, repeat Step 4 D) to Step 4 E) pressing more firmly against the outer thigh to activate the autoinjector.
If you still do not see the needle, use a new autoinjector and start over again at Step 4 A).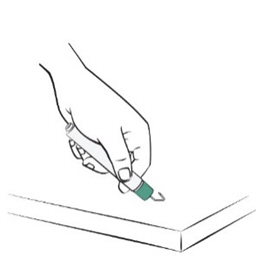
G.) After the injection, avoid contact with blood or the needle by carefully bending the needle back against the autoinjector using a hard surface. Use the bent needle as a hook to pin the used autoinjector to the clothing of the person who has been exposed. This will allow medical personnel to see the number of Atropine autoinjectors given. You can also put the used autoinjector back into the plastic sleeve and leave it next to the person or write the dose and number of autoinjectors used on a triage tag, hand, forehead, chest or other part of the body.
Move yourself and the exposed person away from the contaminated area right away. Get medical help right away.
Each autoinjector has only a single dose (1 injection) of medicine. If you need more than 1 injection, repeat the instructions in Step 4 using a new autoinjector for each injection.This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Rafa Laboratories, Ltd.
Jerusalem, Israel
Revised: 07/2019
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
N/A
atropine injection, 2 mg injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71053-592 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ATROPINE (UNII: 7C0697DR9I) (ATROPINE - UNII:7C0697DR9I) ATROPINE 2 mg in 0.7 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71053-592-01 480 in 1 BOX 07/09/2018 1 40 in 1 CARTON 1 0.7 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA212319 07/09/2018 N/A
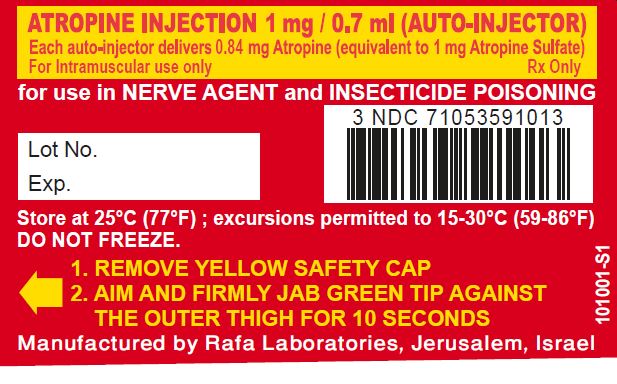
atropine sulfate injection usp, 1 mg/0.7 ml injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71053-591 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ATROPINE (UNII: 7C0697DR9I) (ATROPINE - UNII:7C0697DR9I) ATROPINE 1 mg in 0.7 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71053-591-01 0.7 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 03/09/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date unapproved drug other 03/09/2018 N/A
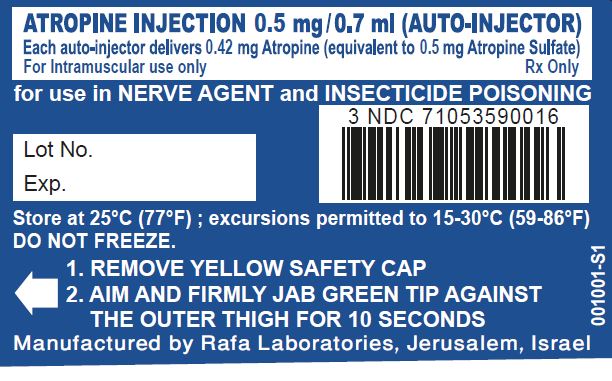
atropine sulfate injection usp, 0.5 mg/0.7 ml injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71053-590 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ATROPINE (UNII: 7C0697DR9I) (ATROPINE - UNII:7C0697DR9I) ATROPINE 0.5 mg in 0.7 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71053-590-01 0.7 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 03/09/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date unapproved drug other 03/09/2018 Labeler - Rafa Laboratories, Ltd. (600024855) Establishment Name Address ID/FEI Business Operations Rafa Laboratories, Ltd. 600024855 manufacture(71053-592, 71053-591, 71053-590)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.