ATROPINE SULFATE injection
Atropine Sulfate by
Drug Labeling and Warnings
Atropine Sulfate by is a Prescription medication manufactured, distributed, or labeled by Hikma Pharmaceuticals USA Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ATROPINE SULFATE INJECTION safely and effectively. See full prescribing information for ATROPINE SULFATE INJECTION.
ATROPINE SULFATE injection, for intravenous, intramuscular, subcutaneous, intraosseous or endotracheal use.
Initial U.S. Approval: 1960INDICATIONS AND USAGE
Atropine is a muscarinic antagonist indicated for temporary blockade of severe or life threatening muscarinic effects. (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Injection: 8 mg per 20 mL (0.4 mg per mL) multiple dose glass vial (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
Most adverse reactions are directly related to atropine’s antimuscarinic action. Dryness of the mouth, blurred vision, photophobia and tachycardia commonly occur with chronic administration of therapeutic doses. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Hikma Pharmaceuticals USA Inc. at 1-877-845-0689 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Mexiletine: Decreases rate of mexiletine absorption. (7.1)
Revised: 1/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 General Administration
2.2 Adult Dosage
2.3 Pediatric Dosage
2.4 Dosing in Patients with Ischemic Heart Disease
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity
5.2 Worsening of Ischemic Heart Disease
5.3 Acute Glaucoma
5.4 Pyloric Obstruction
5.5 Complete Urinary Retention
5.6 Viscid Plugs
5.7 Benzyl Alcohol
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
7.1 Mexiletine
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis and Mutagenesis and Impairment of Fertility
16 HOW SUPPLIED
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 General Administration
Inspect parenteral drug products for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not administer unless solution is clear and seal is intact.
After initial use, discard unused portion within 24 hours.
Intravenous administration is usually preferred, but subcutaneous, intramuscular, endotracheal, and intraosseous administration are possible.
2.2 Adult Dosage
Table 1: Recommended Dosage in Adult Patients
Use
Initial Dose
Continued Treatment
Antisialagogue or
0.5 to 1 mg IV/IM/SC
Repeat as needed every 4 to 6 hours.
other antivagal
30 to 60 minutes
(preanesthesia and
preoperatively
Maximum Total Dose
during surgery)
3 mg
Organophosphorus, carbamate, or muscarinic mushroom poisoning
1 to 6 mg IV/IM/ET depending on severity of symptoms
Repeat as needed every 3 to 5 minutes
Dose may be doubled with each administration until response (reduced bronchospasm, improved oxygenation and drying of pulmonary secretions).
Maintenance Dose: Administer 10% to 20% of the loading dose required for response as a continuous infusion per hour and titrate.
Maximum Total Dose: No maximum total dose.
Symptomatic
0.5 mg IV/IM or 1 to 2 mg
As needed every 3 to 5 minutes
bradycardia*
ET by diluting in no more than 10 mL sterile water for injection or 0.9% sodium chloride
Maximum Total Dose 3 mg
IV=intravenous; IM=intramuscular; SC=subcutaneous; ET=endotracheal
*Do not rely on atropine in type II second-degree or third-degree AV block with wide QRS complexes because these bradyarrhythmias are not likely to be responsive to reversal of cholinergic effects by atropine. Atropine has no effect on bradycardia in patients with transplanted hearts.
2.3 Pediatric Dosage
Table 2: Recommended Dosage in Pediatric Patients
Use
Initial Dose
Continued Treatment
Antisialagogue or other antivagal (preanesthesia and during surgery)*
0.02 mg/kg IV/IM/SC 30 to 60 minutes preoperatively
Repeat as needed every 4 to 6 hours.
Maximum Single Dose
Less than 12 years old: 0.5 mg
12 years and older: 1 mg
Maximum Total Dose
Less than 12 years old: 1 mg
12 years and older: 2 mg
Organophosphorus,
0.02 to 0.06 mg/kg
Repeat as needed every 5 minutes
carbamate or
IV/IM/IO/ET
muscarinic
Dose may be doubled with each administration until response
mushroom poisoning
(reduced bronchospasm, improved oxygenation and drying of pulmonary secretions).
Maintenance Dose: Administer 10% to 20% of the loading dose required for response as a continuous infusion per hour and titrate as needed.
Maximum Total Dose: No maximum total dose.
Symptomatic
0.02 mg/kg IV/IO or
Repeat as needed every 5 minutes
bradycardia due to
0.04 to 0.06 mg/kg via
increased vagal tone
endotracheal tube
Maximum Single Dose
or primary AV
followed by 1 to 5 mL
Less than 12 years old: 0.5 mg
conduction block
flush of normal saline
12 years and older: 1 mg
(not secondary to
followed by 5
hypoxia) **
ventilations
IV=intravenous; IM=intramuscular; SC=subcutaneous; IO=intraosseous; ET=endotracheal;
*Available evidence does not support the routine use of atropine in emergency intubation of critically ill infants and children except in specific emergency intubations when there is higher risk of bradycardia
** Atropine has no effect on bradycardia in patients with transplanted hearts.
2.4 Dosing in Patients with Ischemic Heart Disease
Limit the total dose of atropine sulfate to 0.03 to 0.04 mg/kg [see Warnings and Precautions (5.2)].
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.2 Worsening of Ischemic Heart Disease
In patients with ischemic heart disease, the total dose should be restricted to 2 to 3 mg (maximum 0.03 to 0.04 mg/kg) to avoid atropine-induced tachycardia, increased myocardial oxygen demand and the potential for worsening cardiac ischemia or increasing infarction size.
5.4 Pyloric Obstruction
Atropine may convert partial organic pyloric stenosis into complete obstruction.
5.5 Complete Urinary Retention
Atropine may lead to complete urinary retention in patients with prostatic hypertrophy.
5.6 Viscid Plugs
Atropine may cause thickening of bronchial secretions and formation of viscid plugs in patients with chronic lung disease.
5.7 Benzyl Alcohol
The preservative benzyl alcohol has been associated with serious adverse events and death in neonates. The “gasping syndrome” (characterized by central nervous system depression, metabolic acidosis, gasping respirations, and high levels of benzyl alcohol and its metabolites found in the blood and urine) has been associated with benzyl alcohol dosages >99 mg/kg/day in neonates and low-birth weight infants. Additional symptoms may include gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse.
Although normal therapeutic doses of this product deliver amounts of benzyl alcohol that are substantially lower than those reported in association with the “gasping syndrome”, the minimum amount of benzyl alcohol at which toxicity may occur is not known. Premature and low-birth weight infants may be more likely to develop toxicity. Practitioners administering this and other medications containing benzyl alcohol should consider the combined daily metabolic load of benzyl alcohol from all sources.
-
6 ADVERSE REACTIONS
The following adverse reactions are described elsewhere in labeling:
- Hypersensitivity (5.1)
- Worsening of Ischemic Heart Disease (5.2)
- Acute Glaucoma (5.3)
- Pyloric Obstruction (5.4)
- Complete Urinary Retention (5.5)
- Viscid Plugs (5.6)
The following adverse reactions have been identified during post-approval use of atropine sulfate.
Because these reactions are reported voluntarily from a population of uncertain size, it is not always
possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Most of the side effects of atropine are directly related to its antimuscarinic action. Dryness of the
mouth, blurred vision, photophobia and tachycardia commonly occur. Anhidrosis can produce heat
intolerance. Constipation and difficulty in micturition may occur. Occasional hypersensitivity
reactions have been observed, including serious skin rashes. Paralytic ileus may occur. Exacerbation
of reflux has been reported. Larger or toxic doses may produce such central effects as restlessness,
tremor, fatigue, locomotor difficulties, delirium, followed by hallucinations, depression, and
ultimately, medullary paralysis and death. Large doses can also lead to circulatory collapse. In such
cases, blood pressure declines and death due to respiratory failure may ensue following paralysis and
coma.
- 7 DRUG INTERACTIONS
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Limited available data with Atropine Sulfate Injection use in pregnant women are insufficient to
inform a drug associated risk of adverse developmental outcomes (see Data). There are risks to the
mother and fetus associated with untreated severe or life-threatening muscarinic events (see Clinical
Considerations). Animal reproduction studies have not been conducted with Atropine Sulfate
Injection.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Severe or life-threatening muscarinic events such as acute organophosphate poisoning and symptomatic bradycardia are medical emergencies in pregnancy which can be fatal if left untreated. Life-sustaining therapy for the pregnant woman should not be withheld due to potential concerns regarding the effects of atropine on the fetus.
Data
Human Data
No adequate and well-controlled studies are available regarding use of atropine in pregnant women. In a cohort study of 401 pregnancies in the first trimester and 797 pregnancies in the second or third trimester, atropine use was not associated with an increased risk of congenital malformation. In a surveillance study, 381 newborns were exposed to atropine during the first trimester; 18 major birth defects were observed when 16 were expected. No specific pattern of major birth defects was identified. In another surveillance study of 50 pregnancies in the first trimester, atropine use was not associated with an increased risk of malformations. Methodological limitations of these observational studies including the inability to control for the dosage and timing of atropine exposure, underlying maternal disease, or concomitant maternal drug use, cannot definitively establish or exclude any drug- associated risk during pregnancy.
8.2 Lactation
Risk Summary
Trace amounts of atropine have been reported in human milk after oral intake. There are no available data on atropine levels in human milk after intravenous injection, the effects on the breastfed infant, or the effects on milk production. The lack of clinical data during lactation precludes a clear determination of the risk of atropine to an infant during lactation.
Clinical Considerations
Minimizing exposure
The elimination half-life of atropine is more than doubled in children less than 2 years of age [see Clinical Pharmacology (12.3)]. To minimize potential infant exposure to Atropine Sulfate Injection, a woman may pump and discard her milk for 24 hours after use before resuming to breastfeed her infant.
8.5 Geriatric Use
An evaluation of current literature revealed no clinical experience identifying differences in response between elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
-
10 OVERDOSAGE
Excessive dosing may cause palpitation, dilated pupils, difficulty in swallowing, hot dry skin, thirst, dizziness, restlessness, tremor, fatigue and ataxia. Toxic doses lead to restlessness and excitement, hallucinations, delirium and coma. Depression and circulatory collapse occur only with severe intoxication. In such cases, blood pressure declines and death due to respiratory failure may ensue following paralysis and coma.
The fatal adult dose of atropine is not known. In pediatric populations, 10 mg or less may be fatal.
In the event of toxic overdosage, a short acting barbiturate or diazepam may be given as needed to control marked excitement and convulsions. Large doses for sedation should be avoided because central depressant action may coincide with the depression occurring late in atropine poisoning.
Central stimulants are not recommended.
Physostigmine, given as an atropine antidote by slow intravenous injection of 1 to 4 mg (0.5 to 1 mg in pediatric populations), rapidly abolishes delirium and coma caused by large doses of atropine. Since physostigmine is rapidly destroyed, the patient may again lapse into coma after one to two hours, and repeated doses may be required.
Artificial respiration with oxygen may be necessary. Ice bags and alcohol sponges help to reduce fever, especially in pediatric populations.
Atropine is not removed by dialysis.
-
11 DESCRIPTION
Atropine Sulfate Injection, USP is a sterile, nonpyrogenic, isotonic, clear solution of atropine sulfate in water for injection with sodium chloride sufficient to render the solution isotonic. It is administered parenterally by subcutaneous, intramuscular or intravenous injection.
Each mL contains atropine sulfate, 0.4 mg; benzyl alcohol, 9 mg; sodium chloride 9 mg. May contain sulfuric acid for pH adjustment. pH 3.5 (3.0 to 3.8).
Sodium chloride added to render the solution isotonic for injection of the active ingredient is present in amounts insufficient to affect serum electrolyte balance of sodium (Na+) and chloride (Cl-) ions.
Atropine Sulfate, USP is chemically designated lα H, 5α H-Tropan-3-α-ol (±)-tropate (ester), sulfate (2:1) (salt) monohydrate, (C17H23NO3)2 · H2SO4 · H2O, colorless crystals or white crystalline powder very soluble in water. It has the following structural formula: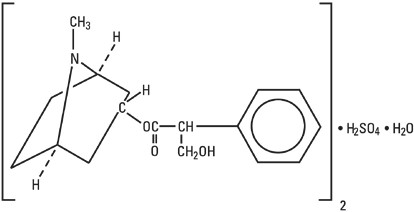
Atropine Sulfate Structural Formula
Atropine, a naturally occurring belladonna alkaloid, is a racemic mixture of equal parts of d- and 1-hyocyamine, whose activity is due almost entirely to the levo isomer of the drug.
Sodium Chloride, USP is chemically designated NaCl, a white crystalline powder freely soluble in water.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Atropine is an antimuscarinic agent since it antagonizes the muscarine-like actions of acetylcholine and other choline esters.
Atropine inhibits the muscarinic actions of acetylcholine on structures innervated by postganglionic cholinergic nerves, and on smooth muscles which respond to endogenous acetylcholine but are not so innervated. As with other antimuscarinic agents, the major action of atropine is a competitive or surmountable antagonism which can be overcome by increasing the concentration of acetylcholine at receptor sites of the effector organ (e.g., by using anticholinesterase agents which inhibit the enzymatic destruction of acetylcholine). The receptors antagonized by atropine are the peripheral structures that are stimulated or inhibited by muscarine (i.e., exocrine glands and smooth and cardiac muscle). Responses to postganglionic cholinergic nerve stimulation also may be inhibited by atropine but this occurs less readily than with responses to injected (exogenous) choline esters.
12.2 Pharmacodynamics
Atropine-induced parasympathetic inhibition may be preceded by a transient phase of stimulation, especially on the heart where small doses first slow the rate before characteristic tachycardia develops due to paralysis of vagal control. Atropine exerts a more potent and prolonged effect on heart, intestine and bronchial muscle than scopolamine, but its action on the iris, ciliary body and certain secretory glands is weaker than that of scopolamine. Unlike the latter, atropine in clinical doses does not depress the central nervous system but may stimulate the medulla and higher cerebral centers. Although mild vagal excitation occurs, the increased respiratory rate and (sometimes) increased depth of respiration produced by atropine are more probably the result of bronchiolar dilatation. Accordingly, atropine is an unreliable respiratory stimulant and large or repeated doses may depress respiration.
Adequate doses of atropine abolish various types of reflex vagal cardiac slowing or asystole. The drug also prevents or abolishes bradycardia or asystole produced by injection of choline esters, anticholinesterase agents or other parasympathomimetic drugs, and cardiac arrest produced by stimulation of the vagus. Atropine also may lessen the degree of partial heart block when vagal activity is an etiologic factor. In some patients with complete heart block, the idioventricular rate may be accelerated by atropine; in others, the rate is stabilized. Occasionally a large dose may cause atrioventricular (A-V) block and nodal rhythm.
Atropine in clinical doses counteracts the peripheral dilatation and abrupt decrease in blood pressure produced by choline esters. However, when given by itself, atropine does not exert a striking or uniform effect on blood vessels or blood pressure. Systemic doses slightly raise systolic and lower diastolic pressures and can produce significant postural hypotension. Such doses also slightly increase cardiac output and decrease central venous pressure. Occasionally, therapeutic doses dilate cutaneous blood vessels, particularly in the “blush” area (atropine flush), and may cause atropine “fever” due to suppression of sweat gland activity in infants and small children.
The effects of intravenous atropine on heart rate (maximum heart rate) and saliva flow (minimum flow) after I.V. administration (rapid, constant infusion over 3 min.) are delayed by 7 to 8 minutes after drug administration and both effects are non-linearly related to the amount of drug in the peripheral compartment. Changes in plasma atropine levels following intramuscular administration (0.5 to 4 mg doses) and heart rate are closely overlapped but the time course of the changes in atropine levels and behavioral impairment indicates that pharmacokinetics is not the primary rate-limiting mechanism for the central nervous system effect of atropine.
12.3 Pharmacokinetics
Absorption
After intramuscular administration, atropine is absorbed with peak concentration occurring at 30 min following injection.
Effects of exercise:
Exercise following intramuscular administration of atropine significantly increases the absorption of atropine due to increased perfusion in the muscle, with an increase in AUC by approximately 20% and Cmax by approximately 80%.
Distribution
Atropine is distributed throughout the body. Atropine’s plasma protein binding is about 44% and saturable in the 2 to 20 mcg/mL concentration range.
Elimination
The pharmacokinetics of atropine is nonlinear after intravenous administration of 0.5 to 4 mg. Atropine disappears from the blood following injection with a plasma half-life of about 2 to 4 hours. Much of the drug is destroyed by enzymatic hydrolysis, particularly in the liver, with 13 to 50% is excreted unchanged in the urine.
Metabolism
The major metabolites of atropine are noratropine, atropin-n-oxide, tropine, and tropic acid. The metabolism of atropine is inhibited by organophosphate pesticides.
Specific Populations
Pregnant Women
Atropine readily crosses the placental barrier and enters the fetal circulation, but is not found in amniotic fluid.
Nursing Mother
Traces are found in various secretions, including milk.
Pediatric and Geriatric Patients
The elimination half-life of atropine is more than doubled in children under two years, and the elderly (> 65 years old) compared to other age groups.
- 13 NONCLINICAL TOXICOLOGY
-
16 HOW SUPPLIED
Atropine Sulfate Injection, USP is a non-pyrogenic, isotonic, clear solution and is supplied as follows:
Presentation
Single Vial
10 Vial Pack
NDC#
0641-6251-01
0641-6251-10
Description
8 mg per 20 mL (0.4 mg per mL) Multiple-dose vial
20 mL multiple-dose vial, packaged in a carton containing 10 vials.
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. After initial use, store between 20° to 25°C (68° to 77°F) and discard within 24 hours.
Manufactured by:
Hikma Pharmaceuticals USA Inc.
Berkeley Heights, NJ 07922
Revised: December 2021
462-917-00
-
PRINCIPAL DISPLAY PANEL
NDC: 0641-6251-01 Rx only
Atropine Sulfate Injection, USP
8 mg per 20 mL (0.4 mg/mL)
For intravenous, intramuscular, subcutaneous, intraosseous, or endotracheal use.
20 mL Multiple Dose Vial
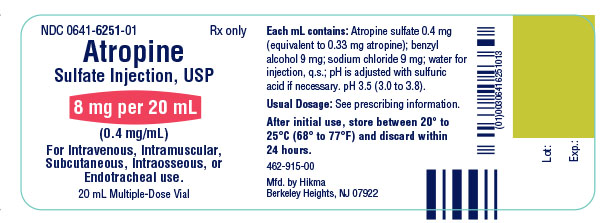
Atropine Sulfate Injection, USP 8 mg per 20 mL Container Label
NDC: 0641-6251-10 Rx only
Atropine Sulfate Injection, USP
8 mg per 20 mL (0.4 mg/mL)
For intravenous, intramuscular, subcutaneous, intraosseous, or endotracheal use.
10 x 20 mL Multiple Dose Vial

Atropine Sulfate Injection, USP 8 mg per 20 mL Carton Label
-
INGREDIENTS AND APPEARANCE
ATROPINE SULFATE
atropine sulfate injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0641-6251 Route of Administration ENDOTRACHEAL, INTRAMEDULLARY, INTRAMUSCULAR, INTRAVENOUS, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ATROPINE SULFATE (UNII: 03J5ZE7KA5) (ATROPINE - UNII:7C0697DR9I) ATROPINE SULFATE 0.4 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 9 mg in 1 mL BENZYL ALCOHOL (UNII: LKG8494WBH) 9 mg in 1 mL SULFURIC ACID (UNII: O40UQP6WCF) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0641-6251-10 10 in 1 CARTON 12/01/2021 1 20 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA213561 12/01/2021 Labeler - Hikma Pharmaceuticals USA Inc. (946499746)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.