INDIUM IN 111 OXYQUINOLINE- indium in-111 oxyquinoline solution
Indium in 111 Oxyquinoline by
Drug Labeling and Warnings
Indium in 111 Oxyquinoline by is a Prescription medication manufactured, distributed, or labeled by Medi-Physics Inc. dba GE Healthcare., GE Healthcare Inc., Medi-Physics Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Indium In 111 oxyquinoline (oxine) is a diagnostic radiopharmaceutical intended for radiolabeling autologous leukocytes. It is supplied as a sterile, non-pyrogenic, isotonic aqueous solution with a pH range of 6.5 to 7.5. Each mL of the solution contains 37 MBq, 1 mCi of indium In 111 [no carrier added, >1.85 GBq/µg indium (>50 mCi/µg indium)] at calibration time, 50 µg oxyquinoline, 100 µg polysorbate 80, and 6 mg of HEPES (N-2-hydroxyethyl-piperazine-N'-2-ethane sulfonic acid) buffer in 0.75% sodium chloride solution. The drug is intended for single use only and contains no bacteriostatic agent. The radionuclidic impurity limit for indium 114m is not greater than 37 kBq, 1 µCi of indium 114m per 37 MBq, 1 mCi of indium In 111 at the time of calibration. The radionuclidic composition at expiration time is not less than 99.75% of indium In 111 and not more than 0.25% of indium In 114m/114.
Chemical name: Indium In 111 Oxyquinoline.
The precise structure of the indium In 111 oxyquinoline complex is unknown at this time. The empirical formula is (C9H6NO)3 In 111.
- PHYSICAL CHARACTERISTICS
-
EXTERNAL RADIATION
The exposure rate constant for 37 MBq, 1 mCi indium In 111 is 8.3 × 10-4 C/kg/h (3.21 R/h) at 1 cm. The first half value thickness of lead (Pb) for indium In 111 is 0.023 cm. A range of values for the relative attenuation of the radiation emitted by this radionuclide that results from the interposition of various thicknesses of Pb is shown in Table 2. For example, the use of 0.834 cm of lead will decrease the external radiation exposure by a factor of about 1,000.
Table 2. Radiation Attenuation by Lead Shielding* Shield Thickness
(Pb) cmCoefficient of
Attenuation- * Data supplied by Oak Ridge Associated Universities, Radiopharmaceutical Internal Dose Information Center, 1984.
0.023 0.5 0.203 10-1 0.513 10-2 0.834 10-3 1.12 10-4 These estimates of attenuation do not take into consideration the presence of longer-lived contaminants with higher energy photons, namely indium In 114m/114.
To allow correction for physical decay of indium In 111, the fractions that remain at selected intervals before and after the time of calibration are shown in Table 3.
-
CLINICAL PHARMACOLOGY
Indium forms a saturated (1:3) complex with oxyquinoline. The complex is neutral and lipid-soluble, which enables it to penetrate the cell membrane. Within the cell, indium becomes firmly attached to cytoplasmic components; the liberated oxyquinoline is released by the cell. It is thought likely that the mechanism of labeling cells with indium In 111 oxyquinoline involves an exchange reaction between the oxyquinoline carrier and subcellular components which chelate indium more strongly than oxyquinoline. The low stability constant of the oxyquinoline complex, estimated at approximately 10, supports this theory.
Following the recommended leukocyte cell labeling procedure, approximately 77% of the added indium In 111 oxyquinoline is incorporated in the resulting cell pellet (which represents approximately 3-4 × 108 WBC).
Cell clumping can occur and was found in about one fifth of the leukocyte preparations examined. The presence of red blood cells or plasma will lead to reduced leukocyte labeling efficiency. Transferrin in plasma competes for indium In 111 oxyquinoline.
After injection of labeled leukocytes into normal volunteers, about 30% of the dose is taken up by spleen and 30% by liver, reaching a plateau at 2-48 hours after injection. No significant clearance of radioactivity is observed at 72 hours in these two organs. Pulmonary uptake is 4-7.5% at 10 minutes but is lost rapidly; pulmonary radioactivity is usually visible in scans only up to about 4 hours after injection.
The human biodistribution studies in three normal subjects injected with indium In 111 oxyquinoline labeled leukocytes indicate a biexponential disappearance of indium In 111 from the blood when monitored for up to 72 hours. Between 9.5 to 24.4% of the injected dose remains in whole blood and clears with a biological half-time of 2.8 to 5.5 hours. The remainder (13-18%) clears from blood with a biological half-time of 64 to 116 hours.
Elimination from the body of injected indium In 111 oxyquinoline is probably mainly through decay to stable cadmium since only a negligible amount (less than 1%) of the dose is excreted in feces and urine in 24 hours.
Clearance from whole blood and biological distribution can vary considerably with the individual recipient, the condition of the injected cells and labeling techniques used.
Release of radioactivity from the labeled cells is about 3% at 1 hour and 24% at 24 hours.
Clearance from liver and spleen, for the purpose of calculating the radiation dose, is assumed to be equal to the physical half-life of indium In 111 (67.2 hours).
-
INDICATIONS AND USAGE
Indium In 111 oxyquinoline is indicated for radiolabeling autologous leukocytes.
Indium In 111 oxyquinoline labeled leukocytes may be used as an adjunct in the detection of inflammatory processes to which leukocytes migrate, such as those associated with abscesses or other infection, following reinjection and detection by appropriate imaging procedures. The degree of accuracy may vary with labeling techniques and with the size, location and nature of the inflammatory process.
Indium In 111 oxyquinoline labeled leukocyte imaging is not the preferred technique for the initial evaluation of patients with a high clinical probability of an abscess in a known location. Ultrasound or computed tomography may provide a better anatomical delineation of the infectious process and information may be obtained more quickly than with labeled leukocytes. If localization by these techniques is successful, labeled leukocytes should not be used as a confirmatory procedure. If localization or diagnosis by these methods fails or is ambiguous, indium In 111 oxyquinoline labeled leukocyte imaging may be appropriate.
- CONTRAINDICATIONS
-
WARNINGS
The content of the vial of indium In 111 oxyquinoline solution is intended only for use in the preparation of indium In 111 oxyquinoline labeled autologous leukocytes, and is not to be administered directly. Autologous leukocyte labeling is not recommended in leukopenic patients because of the small number of available leukocytes.
Due to radiation exposure, indium In 111 oxyquinoline labeled leukocytes could cause fetal harm when administered to pregnant women. If this radiopharmaceutical is used during pregnancy, the patient should be informed of the potential hazard to the fetus.
Indium In 111 oxyquinoline labeled autologous leukocytes should be used only when the benefit to be obtained exceeds the risks involved in children under eighteen years of age owing to the high radiation burden and the potential for delayed manifestation of long-term adverse effects.
-
PRECAUTIONS
Clumping of cells may produce focal accumulations of radioactivity in lungs which do not wash out in 24 hours and thus may lead to false positive results. This phenomenon can be detected by imaging the chest immediately after injection.
The normally high uptake of indium In 111 oxyquinoline labeled leukocytes by spleen and liver may mask inflammatory lesions in these organs. Labeled leukocytes have been observed to accumulate in the colon and accessory spleens of patients with or without disease.
Chemotaxis of granulocytes deteriorates during storage and loss of chemotaxis may cause false negative scans. The spontaneous release of indium In 111 has been reported to range from about 3% at one hour to 24% at 24 hours [ten Berge, R.J.M., Natarajan, A.T., Hardeman, M.R., et al, Labeling with indium In 111 has detrimental effects on human lymphocytes, Journal of Nuclear Medicine, 24, 615-620 (1983)]. The maximum amount of time recommended between drawing the blood and reinjection should not exceed 5 hours. It is recommended that the labeled cells be used within one hour of preparation, if possible and in no case more than three hours after preparation.
Plasma and red cell contamination impairs labeling efficiency of leukocytes. Hemolyzed blood in labeled leukocytes may produce heart pool activity and should be avoided.
Cell aggregates of various degrees have been reported. Cell labeling techniques and standing of cell preparation may be contributing factors.
Nuclear medicine procedures involving withdrawal and reinjection of blood have the potential for transmission of blood borne pathogens. Procedures should be implemented to avoid administration errors and viral contamination of personnel during blood product labeling. A system of checks similar to the ones used for administering blood transfusions should be routine.
General
Strict aseptic techniques should be used to maintain sterility throughout the procedures for using this product.
Do not use after the expiration time and date (5 days after calibration time) stated on the label.
The contents of the vial are radioactive. Adequate shielding of the preparation must be maintained at all times.
Indium In 111 oxyquinoline, like other radioactive drugs, must be handled with care and appropriate safety measures should be used to minimize radiation exposure to clinical personnel. Care should also be taken to minimize radiation exposure to the patient consistent with proper patient management.
Radiopharmaceuticals should be used only by physicians who are qualified by training and experience in the safe use and handling of radionuclides and whose experience and training have been approved by the appropriate governmental agency authorized to license the use of radio-nuclides.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Although earlier studies suggested that oxyquinoline (oxine) might have carcinogenic potential, recent studies have found no evidence of carcinogenicity in either rats or mice given oxyquinoline in feed at concentrations of 1,500 or 3,000 ppm for 103 weeks.
It has been reported [ten Berge, R.J.M., Natarajan, A.T., Hardeman, M.R., et al, Labeling with indium In 111 has detrimental effects on human lymphocytes, Journal of Nuclear Medicine, 24, 615-620 (1983)] that human lymphocytes labeled with recommended concentrations of indium In 111 oxyquinoline showed chromosome aberrations consisting of gaps, breaks and exchanges that appear to be radiation induced. At 555 kBq/107, 15 µCi/107 lymphocytes 93% of the cells were reported to be abnormal. The oncogenic potential of such lymphocytes has not been studied. It has been reported that the radiation dose to 108 leukocytes is 9 × 104 mGy (0.9 × 104 rads) from 18.5 MBq, 500 µCi [Goodwin, David A., Cell labeling with oxine chelates of radioactive metal ions: Techniques and clinical implications, Journal of Nuclear Medicine, 19, 557-559 (1978)].
Studies have not been performed to evaluate whether indium In 111 oxyquinoline affects fertility in male or female laboratory animals or humans.
Pregnancy Category C
Animal reproduction studies have not been conducted with Indium In 111 Oxyquinoline labeled leukocytes. It is also not known whether Indium In 111 Oxyquinoline labeled leukocytes can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity.
However, Indium Nitrate, a closely related compound, was teratogenic and embryopathic in hamsters. Indium In 111 Oxyquinoline labeled leukocytes should be given to a pregnant woman only if clearly needed.
Ideally, examinations using radiopharmaceuticals, especially those elective in nature, in women of childbearing capability should be performed during the first few (approximately ten) days following the onset of menses.
Nursing Mothers
It is reported that indium 111 is secreted in human milk following administration of indium In 111 labeled leukocytes. Therefore, formula feedings should be substituted for breast feedings.
Pediatric Use
Safety and effectiveness in pediatric patients below age 18 have not been established (See Warnings).
Geriatric Use
Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
- ADVERSE REACTIONS
-
DOSAGE AND ADMINISTRATION
The recommended adult (70 kg) dose of indium In 111 oxyquinoline labeled autologous leukocytes is 7.4 to 18.5 MBq, 200-500 µCi. Indium In 111 oxyquinoline solution is intended for the radiolabeling of autologous leukocytes. The indium In 111 oxyquinoline labeled autologous leukocytes are administered intravenously.
Imaging is recommended at approximately 24 hours post injection. Typically, anterior and posterior views of the chest, abdomen and pelvis should be obtained with other views as required.
Aseptic procedures and a shielded syringe should be employed in the withdrawal of indium In 111 oxyquinoline from the vial. Similar procedures should be employed during the labeling procedure and the administration of the labeled leukocytes to the patient. The user should wear waterproof gloves during the entire procedure. The patient's dose should be measured by a suitable radioactivity calibration system immediately before administration. At this time, the leukocyte preparation should be checked for gross clumping and red blood cell contamination.
-
RADIATION DOSIMETRY
The estimated absorbed radiation doses to an adult patient weighing 70 kg from an intravenous dose of 18.5 MBq, 500 µCi of indium In 111 oxyquinoline labeled leukocytes including contributions from indium In 114m/114 as a radionuclidic impurity are shown in Table 4.
Table 4. Radiation Dose Estimate in a 70 kg Human for 18.5 MBq, 500 µCi at Expiry of Indium In 111 (99.75%) Oxyquinoline labeled leukocytes with Indium In 114m/114 (0.25%) Assumptions: 30% to spleen, 30% to liver, 34% to red marrow, 6% to remainder of body, with no excretion. Organ mGy/18.5 MBq
In 111Rads/500 µCi
In 111Spleen 130 13 Liver 19 1.9 Red Marrow 13 1.3 Skeleton 3.64 0.364 Testes 0.1 0.01 Ovaries 1.9 0.19 Total Body 3.1 0.31 Organ mGy/46.25 kBq
In 114m/114Rads/1.25 µCi
In 114m/114Spleen 70 7 Liver 7.1 0.71 Red Marrow 6.9 0.69 Skeleton 0.85 0.085 Testes 0.04 0.004 Ovaries 0.06 0.006 Total Body 0.6 0.06 Organ Total Dose
in mGyTotal Dose
in RadsSpleen 200 20 Liver 26.6 2.66 Red Marrow 19.9 1.99 Skeleton 4.5 0.45 Testes 0.14 0.014 Ovaries 2.0 0.2 Total Body 3.7 0.37 The dose of radiation absorbed by the organs will vary with the distribution of the blood cells in the organs, which in turn will depend on the predominance of the cell types labeled and their condition.
-
LABELING PROCEDURE
Sterile technique must be used throughout. It is important that all equipment used for the preparation of reagents be thoroughly cleaned to assure the absence of trace metal impurities. The user should wear waterproof gloves during the handling and administration procedure.
- The following equipment is recommended:
One (1) 60 mL or two (2) 30 mL sterile disposable plastic syringes with a 19 or 20 gauge needle (NOTE: Do not use a smaller gauge needle).
Ring stand and clamp(s).
Three (3) 50 mL sterile conical plastic centrifuge tubes with screw caps. Label each set with patient ID and "WBC", "LPP" and "Wash" respectively (NOTE: 3 centrifuge tubes per patient).
Clinical Centrifuge with horizontal, 4 place rotor or equivalent.
Sodium Chloride 0.9% Injection, USP.
Three (3) disposable 5 or 10 mL syringes and 19 gauge needles.
Syringe shield to dispense indium In 111 oxyquinoline.
A dose calibrator.
Butterfly catheter infusion set.
Test tube rack.
Lab timer.
10 mL syringe with a 19 gauge or 20 gauge needle.
19 gauge needle with filter (optional). - Withdraw from the patient 30-50 mL blood [preferably fifty (50) mL] using aseptic venipuncture technique using the 60 mL syringe fitted with a 19 gauge or 20 gauge needle and containing approximately 1000-1500 units heparin in 1-2 mL. Blood withdrawal should be smooth and slow so as not to produce bubbles or foaming.
- Remove and dispose of the needle and replace with a syringe cap. Gently mix the contents of the syringe and label with the patient's ID, date and time.
- Upon receipt of the full syringe for processing, the contents should again be gently mixed.
- Clamp the syringe barrel to the ring stand in an upright (needle side up) position and tilt the syringe 10-20 degrees from its position perpendicular to the bench.
- Allow the red cells to sediment 30-60 minutes, depending upon when the supernatant [leukocyte rich plasma (LRP)] looks clear of red blood cells.
- Replace the syringe cap with an infusion set.
- Collect the plasma (LRP) in the centrifuge tube marked "WBC" by expressing the LRP through the catheter tubing making sure not to get any red cells into the WBC tube.
- Immediately centrifuge the capped WBC tube at 400-450 g for 5 minutes.
- Transfer the supernatant to the leukocyte poor plasma (LPP) tube leaving behind 0.5-1.0 mL supernatant to cover the white cell button (NOTE: the button often contains a small number of red cells and may appear red).
- Wash the white cell button with 4-6 mL Sodium Chloride (0.9%) Injection, USP. Resuspend the button by gentle swirling.
- Centrifuge the capped WBC tube at 400-450 g for 5 minutes (alternatively, 150 g for 8 minutes) and discard all but 0.5-1.0 mL of the supernate to cover the cells.
- Add 5.0 mL Sodium Chloride (0.9%) Injection, USP. Resuspend the cells by gentle swirling.
- With the shielded syringe, draw up approximately 22.2 MBq, 600 µCi indium In 111 oxyquinoline. Check the amount of radioactivity in a dose calibrator set for indium In 111 and record for labeling efficiency calculations.
Parenteral drug products should be inspected visually for particulate matter and discoloration before administration. - In several additions, add the indium In 111 oxyquinoline to the WBC tube, gently swirling after each addition.
- Set the lab timer for 15 minutes and allow the capped WBC tube to incubate. Swirl the cell preparation several times during the incubation.
- With a sterile plastic syringe, add half of the saved LPP (or about 8 mL) from the LPP tube. Cap and gently swirl the contents of WBC tube to resuspend the cells.
- Centrifuge the WBC tube at 450 g for 5 minutes (or 150 g for 8 minutes). Decant supernatant into the wash tube leaving behind about 0.5 mL of the supernate to cover the cells.
- Assay the activity in the WBC tube and in the wash tube in a dose calibrator and record.
- With a sterile plastic syringe add the remaining LPP to the cell button and gently resuspend by swirling. With a sterile syringe fitted with a 19 gauge needle, resuspend the cells by drawing the cells up into the syringe and expressing the suspension against the tube gently once or twice. Alternatively, draw up the cells into a syringe fitted with the filtered 19 gauge needle, and replace the needle with an unfiltered 19 or 20 gauge needle.
- Reserve in the WBC tube a minimum amount of white cell suspension for a WBC count. A microscopic examination should also be completed to observe for clumping. Draw up the patient's dose (7.4 to 18.5 MBq, 200-500 µCi) and check the syringe in the dose calibrator. Record the measurement.
- The following equipment is recommended:
-
QUALITY CONTROL
It is generally advantageous to record any observations on cell abnormalities (e.g., cell clumping). A trypan blue exclusion test may also be performed.
It is recommended that the preparation be used within one hour of labeling (See Precautions).
-
HOW SUPPLIED
Indium In 111 oxyquinoline solution is supplied in a vial as a single use only product containing 37 MBq, 1.0 mCi in 1.0 mL aqueous solution at the calibration date stated on the label. Vials are packaged in individual lead shields.
NDC: 17156-021-01
The contents of the vial are radioactive and adequate shielding and handling precautions must be maintained.
This preparation is approved for use by persons licensed by the Illinois Emergency Management Agency pursuant to 32 IL. Adm. Code Section 330.260(a) and 335.4010 or equivalent licenses of the Nuclear Regulatory Commission or an Agreement State.
-
SPECIAL HANDLING AND STORAGE
Indium In 111 oxyquinoline solution should be stored at room temperature (15-25°C, 59-77°F).
Indium In 111 oxyquinoline labeled autologous leukocytes should preferably be reinjected within one hour of labeling. The labeled cells may be stored at room temperature (15-25°C, 59-77°F) for up to three hours following completion of the cell labeling procedure. Reinjection of indium In 111 oxyquinoline labeled autologous leukocytes more than 5 hours after initial blood drawing is not recommended.
Sterile technique must be used throughout the collection, labeling and re-injection procedures.
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - 1 mL Vial Label
Indium In 111 Oxyquinoline Solution
For the radiolabeling of autologous
leukocytes. Each mL contains <0.1µg
Indium, 50µg 8-hydroxyquinoline,
~ 100µg polysorbate 80, 6mg
(N-2-hydroxyethylpiperazine-
N-2 ethane sulfonic acid). HEPES
buffer and 0.75% sodium chloride.
pH adjusted with NaOH/HCl.
Refer to package insert for further
details.
Rx ONLY
Mfd. by GE Healthcare, Medi-Physics, Inc.
Arlington Heights, IL 60004 U.S.A.IN15PA
Lot:
Expiry1mCi, 37 MBq
1mL at 0600hrs
CST on:41-8021
CAUTION
RADIOACTIVE
MATERIAL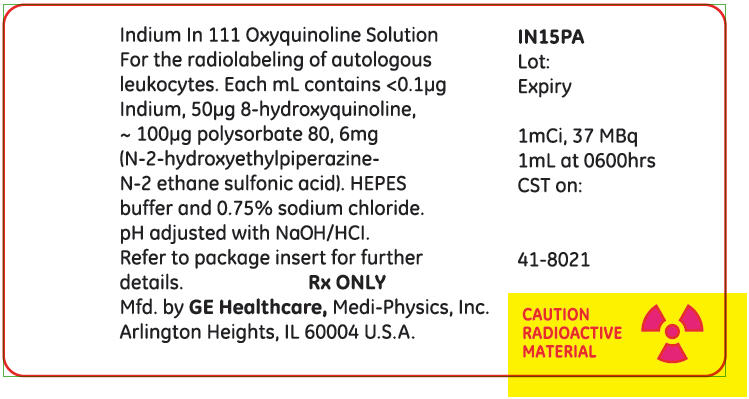
-
INGREDIENTS AND APPEARANCE
INDIUM IN 111 OXYQUINOLINE
indium in-111 oxyquinoline solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 17156-021 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Indium In-111 Oxyquinoline (UNII: LGX9OL562T) (Indium Cation In-111 - UNII:WJZ06C0H8L) Indium Cation In-111 1 ug in 1 mL Inactive Ingredients Ingredient Name Strength Polysorbate 80 (UNII: 6OZP39ZG8H) 100 ug in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 17156-021-01 1 in 1 BOX 12/01/1985 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA019044 12/01/1985 Labeler - Medi-Physics Inc. dba GE Healthcare. (095263729) Registrant - GE Healthcare Inc. (053046579) Establishment Name Address ID/FEI Business Operations Medi-Physics Inc. 095263729 MANUFACTURE(17156-021) , RELABEL(17156-021) , REPACK(17156-021) , ANALYSIS(17156-021) , API MANUFACTURE(17156-021)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.