Methazolamide by Sandoz Inc METHAZOLAMIDE tablet
Methazolamide by
Drug Labeling and Warnings
Methazolamide by is a Prescription medication manufactured, distributed, or labeled by Sandoz Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
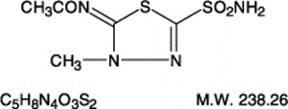
DESCRIPTION
Methazolamide, a sulfonamide derivative, is a white crystalline powder, weakly acidic, and slightly soluble in water, alcohol and acetone. It is available as 25 mg and 50 mg tablets. The chemical name for methazolamide is N -[5-(aminosulfonyl)-3-methyl-1,3,4-thiadiazol-2(3H)-ylidene]-acetamide and it has the following structural formula:
Methazolamide tablets, USP contain 25 mg or 50 mg of methazolamide. Inactive ingredients: croscarmellose sodium, hydroxypropyl methylcellulose, lactose (monohydrate), magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate.
-
CLINICAL PHARMACOLOGY
Methazolamide is a potent inhibitor of carbonic anhydrase.
Methazolamide is well absorbed from the gastrointestinal tract. Peak plasma concentrations are observed 1 to 2 hours after dosing. In a multiple-dose, pharmacokinetic study, administration of methazolamide 25 mg b.i.d., 50 mg b.i.d. and 100 mg b.i.d. demonstrated a linear relationship between plasma methazolamide levels and methazolamide dose. Peak plasma concentrations (Cmax) for the 25 mg, 50 mg and 100 mg b.i.d. regimens were 2.5 mcg/mL, 5.1 mcg/mL and 10.7 mcg/mL, respectively. The area under the plasma concentration-time curves (AUC) were 1130 mcg. min/mL, 2571 mcg. min/mL and 5418 mcg. min/mL for the 25 mg, 50 mg and 100 mg dosage regimens, respectively.
Methazolamide is distributed throughout the body including the plasma, cerebrospinal fluid, aqueous humor of the eye, red blood cells, bile and extracellular fluid. The mean apparent volume of distribution (Varea/F) ranges from 17 to 23 L. Approximately 55% is bound to plasma proteins. The steady-state methazolamide red blood cell: plasma ratio varies with dose and was found to be 27:1, 16:1 and 10:1 following the administration of methazolamide 25 mg b.i.d., 50 mg b.i.d. and 100 mg b.i.d., respectively.
The mean steady-state plasma elimination half-life for methazolamide is approximately 14 hours. At steady-state approximately 25% of the dose is recovered unchanged in the urine over the dosing interval. Renal clearance accounts for 20 to 25% of the total clearance of drug. After repeated b.i.d.-t.i.d. dosing, methazolamide accumulates to steady state concentrations in seven days.
Methazolamide’s inhibitory action on carbonic anhydrase decreases the secretion of aqueous humor and results in a decrease in intraocular pressure. The onset of the decrease in intraocular pressure generally occurs within two to four hours, has a peak effect in six to eight hours, and a total duration of ten to eighteen hours.
Methazolamide is a sulfonamide derivative; however, it does not have any clinically significant antimicrobial properties. Although methazolamide achieves a high concentration in the cerebrospinal fluid, it is not considered an effective anticonvulsant.
Methazolamide has a weak and transient diuretic effect, therefore use results in an increase in urinary volume, with excretion of sodium, potassium and chloride. The drug should not be used as a diuretic. Inhibition of renal bicarbonate reabsorption produces an alkaline urine. Plasma bicarbonate decreases, and a relative, transient metabolic acidosis may occur due to a disequilibrium in carbon dioxide transport in the red cell. Urinary citrate excretion is decreased by approximately 40% after doses of 100 mg every 8 hours. Uric acid output has been shown to decrease 36% in the first 24 hour period.
-
INDICATIONS AND USAGE
Methazolamide is indicated in the treatment of ocular conditions where lowering intraocular pressure is likely to be of therapeutic benefit, such as chronic open-angle glaucoma, secondary glaucoma, and preoperatively in acute angle-closure glaucoma where lowering the intraocular pressure is desired before surgery.
-
CONTRAINDICATIONS
Methazolamide therapy is contraindicated in situations in which sodium and/or potassium serum levels are depressed, in cases of marked kidney or liver disease or dysfunction, in adrenal gland failure, and in hyperchloremic acidosis. In patients with cirrhosis, use may precipitate the development of hepatic encephalopathy.
Long-term administration of methazolamide is contraindicated in patients with angle-closure glaucoma, since organic closure of the angle may occur in spite of lowered intraocular pressure.
-
WARNINGS
Fatalities have occurred, although rarely, due to severe reactions to sulfonamides including Stevens-Johnson syndrome, toxic epidermal necrolysis, fulminant hepatic necrosis, agranulocytosis, aplastic anemia, and other blood dyscrasias. Hypersensitivity reactions may recur when a sulfonamide is readministered, irrespective of the route of administration.
If hypersensitivity or other serious reactions occur, the use of this drug should be discontinued.
Caution is advised for patients receiving high-dose aspirin and methazolamide concomitantly, as anorexia, tachypnea, lethargy, coma and death have been reported with concomitant use of high-dose aspirin and carbonic anhydrase inhibitors.
-
PRECAUTIONS
General
Potassium excretion is increased initially upon administration of methazolamide and in patients with cirrhosis or hepatic insufficiency could precipitate a hepatic coma.
In patients with pulmonary obstruction or emphysema, where alveolar ventilation may be impaired methazolamide should be used with caution because it may precipitate or aggravate acidosis.
Information for Patients
Adverse reactions common to all sulfonamide derivatives may occur: anaphylaxis, fever, rash (including erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis), crystalluria, renal calculus, bone marrow depression, thrombocytopenic purpura, hemolytic anemia, leukopenia, pancytopenia and agranulocytosis. Precaution is advised for early detection of such reactions and the drug should be discontinued and appropriate therapy instituted.
Caution is advised for patients receiving high-dose aspirin and methazolamide concomitantly.
Laboratory Tests
To monitor for hematologic reactions common to all sulfonamides, it is recommended that a baseline CBC and platelet count be obtained on patients prior to initiating methazolamide therapy and at regular intervals during therapy. If significant changes occur, early discontinuance and institution of appropriate therapy are important. Periodic monitoring of serum electrolytes is also recommended.
Drug Interactions
Methazolamide should be used with caution in patients on steroid therapy because of the potential for developing hypokalemia. Caution is advised for patients receiving high-dose aspirin and methazolamide concomitantly, as anorexia, tachypnea, lethargy, coma and death have been reported with concomitant use of high-dose aspirin and carbonic anhydrase inhibitors (see WARNINGS).
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals to evaluate methazolamide’s carcinogenic potential and its effect on fertility have not been conducted. Methazolamide was not mutagenic in the Ames bacterial test.
Pregnancy
Teratogenic Effects
Pregnancy Category C
Methazolamide has been shown to be teratogenic (skeletal anomalies) in rats when given in doses approximately 40 times the human dose. There are no adequate and well controlled studies in pregnant women. Methazolamide should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from methazolamide, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
-
ADVERSE REACTIONS
Adverse reactions, occurring most often early in therapy, include paresthesias, particularly a “tingling” feeling in the extremities; hearing dysfunction or tinnitus; fatigue; malaise; loss of appetite; taste alteration; gastrointestinal disturbances such as nausea, vomiting and diarrhea; polyuria; and occasional instances of drowsiness and confusion.
Metabolic acidosis and electrolyte imbalance may occur.
Transient myopia has been reported. This condition invariably subsides upon diminution or discontinuance of the medication.
Other occasional adverse reactions include urticaria, melena, hematuria, glycosuria, hepatic insufficiency, flaccid paralysis, photosensitivity, convulsions, and, rarely, crystalluria and renal calculi. Also see PRECAUTIONS: Information for Patients for possible reactions common to sulfonamide derivatives. Fatalities have occurred, although rarely, due to severe reactions to sulfonamides including Stevens-Johnson syndrome, toxic epidermal necrolysis, fulminant hepatic necrosis, agranulocytosis, aplastic anemia, and other blood dyscrasias (see WARNINGS).
-
OVERDOSAGE
No data are available regarding methazolamide overdosage in humans as no cases of acute poisoning with this drug have been reported. Animal data suggest that even a high dose of methazolamide is nontoxic. No specific antidote is known. Treatment should be symptomatic and supportive.
Electrolyte imbalance, development of an acidotic state, and central nervous system effects might be expected to occur. Serum electrolyte levels (particularly potassium) and blood pH levels should be monitored.
Supportive measures may be required to restore electrolyte and pH balance.
- DOSAGE AND ADMINISTRATION
-
HOW SUPPLIED
Methazolamide tablets, USP for oral administration are available as:
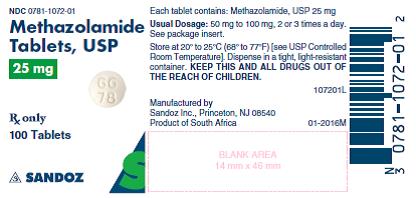
25 mg: Round, white, unscored tablets debossed GG 78 on one side and plain on the reverse side, and supplied as:
NDC: 0781-1072-01 bottles of 100
NDC: 0781-1072-10 bottles of 1000
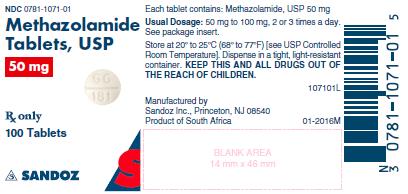
50 mg: Round, white, scored tablets debossed GG 181 on one side and plain on the reverse side, and supplied as:
NDC: 0781-1071-01 bottles of 100
NDC: 0781-1071-10 bottles of 1000
- SPL UNCLASSIFIED SECTION
- 25 mg Label
- 50 mg Label
-
INGREDIENTS AND APPEARANCE
METHAZOLAMIDE
methazolamide tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0781-1072 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METHAZOLAMIDE (UNII: W733B0S9SD) (METHAZOLAMIDE - UNII:W733B0S9SD) METHAZOLAMIDE 25 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSE 2910 (3 MPA.S) (UNII: 0VUT3PMY82) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SODIUM LAURYL SULFATE (UNII: 368GB5141J) Product Characteristics Color WHITE Score no score Shape ROUND Size 6mm Flavor Imprint Code GG78 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0781-1072-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 06/30/1993 03/31/2021 2 NDC: 0781-1072-10 1000 in 1 BOTTLE; Type 0: Not a Combination Product 06/30/1993 02/20/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA040036 06/30/1993 09/30/2021 METHAZOLAMIDE
methazolamide tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0781-1071 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METHAZOLAMIDE (UNII: W733B0S9SD) (METHAZOLAMIDE - UNII:W733B0S9SD) METHAZOLAMIDE 50 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSE 2910 (3 MPA.S) (UNII: 0VUT3PMY82) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SODIUM LAURYL SULFATE (UNII: 368GB5141J) Product Characteristics Color WHITE Score 2 pieces Shape ROUND Size 7mm Flavor Imprint Code GG181 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0781-1071-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 06/30/1993 09/30/2021 2 NDC: 0781-1071-10 1000 in 1 BOTTLE; Type 0: Not a Combination Product 06/30/1993 02/20/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA040036 06/30/1993 09/30/2021 Labeler - Sandoz Inc (110342024)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.