These highlights do not include all the information needed to use FAMOTIDINE TABLETS safely and effectively. See full prescribing information for FAMOTIDINE TABLETS.FAMOTIDINE tablets, for oral useInitial U.S. Approval: 1986
Famotidine by
Drug Labeling and Warnings
Famotidine by is a Prescription medication manufactured, distributed, or labeled by Preferred Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
FAMOTIDINE- famotidine tablet, film coated
Preferred Pharmaceuticals Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use FAMOTIDINE TABLETS safely and effectively. See full prescribing information for FAMOTIDINE TABLETS.
FAMOTIDINE tablets, for oral use Initial U.S. Approval: 1986 INDICATIONS AND USAGEFamotidine is a histamine-2 (H2) receptor antagonist indicated (1): In adult and pediatric patients 40 kg and greater for the treatment of:
In adults for the:
DOSAGE AND ADMINISTRATION
Administration (2.3):
DOSAGE FORMS AND STRENGTHSTablets: 20 mg, 40 mg (3) CONTRAINDICATIONSHistory of serious hypersensitivity reactions (e.g., anaphylaxis) to famotidine or other H2 receptor antagonists. (4) WARNINGS AND PRECAUTIONSADVERSE REACTIONSThe most common adverse reactions are: headache, dizziness, constipation and diarrhea. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Zydus Pharmaceuticals (USA) Inc. at 1-877-993-8779 at 1-800-321-4576 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONSSee 17 for PATIENT COUNSELING INFORMATION. Revised: 4/2024 |
|||||||||||||||||||
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Famotidine tablets are indicated in adult and pediatric patients 40 kg and greater for the treatment of:
- active duodenal ulcer (DU).
- active gastric ulcer (GU).
- symptomatic nonerosive gastroesophageal reflux disease (GERD).
- erosive esophagitis due to GERD, diagnosed by biopsy.
Famotidine tablets are indicated in adults for the:
- treatment of pathological hypersecretory conditions (e.g., Zollinger-Ellison syndrome, multiple endocrine neoplasias).
- reduction of the risk of duodenal ulcer recurrence.
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
Table 1 shows the recommended dosage of famotidine 20 mg and 40 mg tablets in adult and pediatric patients weighing 40 kg and greater with normal renal function. The use of famotidine 20 mg and 40 mg tablets is not recommended in pediatric patients weighing less than 40 kg because the lowest available strength (20 mg) exceeds the recommended dose for these patients. Use another famotidine formulation for pediatric patients weighing less than 40 kg.
| a Both dosages demonstrated effectiveness in clinical trials [see Clinical Studies (14)]. | ||
| b In clinical trials, the majority of patients healed within 4 weeks. For patients who do not heal after 4 weeks, consider an additional 2 weeks to 4 weeks of treatment [see Clinical Studies (14.1)]. | ||
| c Longer treatment durations have not been studied in clinical trials [see Clinical Studies (14.1, 14.2, 14.3)]. | ||
| d In pediatric patients, the safety and effectiveness of famotidine have not been established for the reduction of the risk of duodenal ulcer recurrence or for treatment of pathological hypersecretory conditions [see Use in Specific Populations (8.4)]. | ||
|
Indication
|
Recommended Dosage
|
Recommended Duration
|
|
Active duodenal ulcer (DU)
|
40 mg once daily; or 20 mg twice dailya
|
Up to 8 weeksb,c
|
|
Active gastric ulcer
|
40 mg once daily |
Up to 8 weeksc
|
|
Symptomatic nonerosive
|
20 mg twice daily |
Up to 6 weeksc
|
|
Erosive esophagitis
|
20 mg twice daily; or 40 mg twice dailya
|
Up to 12 weeks |
|
Pathological hypersecretory conditionsd
|
Starting dosage: 20 mg every 6 hours; adjust dosage to individual patient needs Maximum dosage 160 mg every 6 hours |
As clinically indicated |
|
Reduction of the risk of DU recurrenced
|
20 mg once daily |
1 yearc or as clinically indicated |
2.2 Dosage in Renal Impairment
Dosage adjustments of famotidine are recommended for patients with moderate to severe renal impairment (creatinine clearance less than 60 mL/min) [see Use in Specific Populations (8.6)]. Table 2 shows the recommended maximum dosage of famotidine 20 mg or 40 mg tablets for patients with renal impairment, by indication. Use the lowest effective dose. Some dosage adjustments may require switching to other formulations of famotidine (e.g., oral suspension, lower dose tablet).
| a An alternate dosage regimen is 10 mg once daily. Since 20 mg or 40 mg tablet strength cannot be used for this dosage regimen, use an alternate famotidine formulation. | ||
| b Dosage adjustments for renal impairment are provided for both dosing regimens (20 mg twice daily and 40 mg twice daily) which showed effectiveness for the treatment of erosive esophagitis in clinical trials [see Clinical Studies (14.4)] . | ||
| c In pediatric patients, the safety and effectiveness of famotidine have not been established for the reduction of the risk of duodenal ulcer recurrence or for treatment of pathological hypersecretory conditions [see Use in Specific Populations (8.4)] . | ||
| d Doses required to treat pathological hypersecretory conditions may exceed the maximum doses evaluated in patients with impaired renal function. The risk for increased adverse reactions in renally impaired patients treated with famotidine for pathological hypersecretory conditions is unknown. | ||
| e Recommended dosage regimen is 10 mg every other day. Since 20 mg or 40 mg tablet strength cannot be used for this dosage regimen, use an alternate famotidine formulation. | ||
|
Indication
|
Recommended Maximum Dosages
|
|
|
Creatinine clearance
|
Creatinine clearance
|
|
|
Active duodenal ulcer (DU)
|
20 mg once daily; or |
20 mg every other daya
|
|
Active gastric ulcer
|
20 mg once daily; or |
20 mg every other daya
|
|
Symptomatic nonerosive GERD
|
20 mg once daily |
20 mg every other daya
|
|
Erosive esophagitis diagnosed by endoscopyb
|
20 mg once daily; or |
20 mg every other daya,b
|
|
40 mg once dailyb
|
20 mg once dailyb
|
|
|
Pathological hypersecretory conditionsc
|
Avoid used
|
|
|
Reduction of the risk of DU recurrencec
|
20 mg every other daya
|
(see footnote)e
|
2.3 Administration Instructions
- Take famotidine tablets once daily before bedtime or twice daily in the morning and before bedtime, as recommended.
- Famotidine tablets may be taken with or without food [see Clinical Pharmacology (12.3)].
- Famotidine tablets may be given with antacids.
3 DOSAGE FORMS AND STRENGTHS
- Famotidine Tablets USP, 20 mg are white to off-white, round, biconvex film-coated tablets debossed with "Z21" on one side and plain on other side.
- Famotidine Tablets USP, 40 mg are white to off-white, round, biconvex film-coated tablets debossed with "Z41" on one side and plain on other side.
4 CONTRAINDICATIONS
Famotidine is contraindicated in patients with a history of serious hypersensitivity reactions (e.g., anaphylaxis) to famotidine or other histamine-2 (H2) receptor antagonists.
5 WARNINGS AND PRECAUTIONS
5.1 Central Nervous System Adverse Reactions
Central nervous system (CNS) adverse reactions, including confusion, delirium, hallucinations, disorientation, agitation, seizures and lethargy, have been reported in elderly patients and patients with moderate and severe renal impairment treated with famotidine. Since famotidine blood levels are higher in patients with renal impairment than in patients with normal renal function, dosage adjustments are recommended in patients with renal impairment [see Dosage and Administration (2.2), Clinical Pharmacology (12.3)].
5.2 Concurrent Gastric Malignancy
In adults, symptomatic response to therapy with famotidine does not preclude the presence of gastric malignancy. Consider evaluation for gastric malignancy in adult patients who have a suboptimal response or an early symptomatic relapse after completing treatment with famotidine.
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Famotidine was studied in 7 US and international placebo- and active-controlled trials in approximately 2,500 patients [see Clinical Studies (14)]. A total of 1,442 patients were treated with famotidine, including 302 treated with 40 mg twice daily, 456 treated with 20 mg twice daily, 461 treated with 40 mg once daily and 396 treated with 20 mg once daily. The population was 17 years to 91 years old, fairly well distributed between gender and race; however, the predominant race treated was Caucasian.
The following adverse reactions occurred in greater than or equal to 1% of famotidine-treated patients: headache, dizziness and constipation.
The following other adverse reactions were reported in less than 1% of patients in clinical trials:
Body as a Whole: fever, asthenia, fatigue
Cardiovascular: palpitations
Gastrointestinal: elevated liver enzymes, vomiting, nausea, abdominal discomfort, anorexia, dry mouth
Hematologic: thrombocytopenia
Hypersensitivity: orbital edema, rash, conjunctival injection, bronchospasm
Musculoskeletal: musculoskeletal pain, arthralgia
Nervous System/Psychiatric: seizure, hallucinations, depression, anxiety, decreased libido, insomnia, somnolence
Skin: pruritus, dry skin, flushing
Special Senses: tinnitus, taste disorder
Other: impotence
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of famotidine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiovascular: arrhythmia, AV block, prolonged QT interval
Gastrointestinal: cholestatic jaundice, hepatitis
Hematologic: agranulocytosis, pancytopenia, leukopenia
Hypersensitivity: anaphylaxis, angioedema, facial edema, urticaria
Musculoskeletal: rhabdomyolysis, muscle cramps
Nervous System/Psychiatric: confusion, agitation, paresthesia
Respiratory: interstitial pneumonia
Skin: toxic epidermal necrolysis/Stevens-Johnson syndrome
7 DRUG INTERACTIONS
7.1 Drugs Dependent on Gastric pH for Absorption
Famotidine can reduce the absorption of other drugs, due to its effect on reducing intragastric acidity, leading to loss of efficacy of the concomitant drug.
Concomitant administration of famotidine with dasatinib, delavirdine mesylate, cefditoren and fosamprenavir is not recommended.
See the prescribing information for other drugs dependent on gastric pH for absorption for administration instructions, including atazanavir, erlotinib, ketoconazole, itraconazole, ledipasvir/sofosbuvir, nilotinib and rilpivirine.
7.2 Tizanidine (CYP1A2 Substrate)
Although not studied clinically, famotidine is considered a weak CYP1A2 inhibitor and may lead to substantial increases in blood concentrations of tizanidine, a CYP1A2 substrate. Avoid concomitant use with famotidine. If concomitant use is necessary, monitor for hypotension, bradycardia or excessive drowsiness. Refer to the full prescribing information for tizanidine.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data with H2-receptor antagonists, including famotidine, in pregnant women are insufficient to establish a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. In animal reproduction studies, no adverse development effects were observed with oral administration of famotidine at doses up to approximately 243 times and 122 times, respectively, the recommended human dose of 80 mg per day for the treatment of erosive esophagitis (see Data).
The estimated background risk for major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss or other adverse outcomes. In the U.S. general population, the background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
Reproductive studies have been performed in rats and rabbits at oral doses of up to 2,000 mg/kg/day and 500 mg/kg/day, respectively and in both species at intravenous doses of up to 200 mg/kg/day and have revealed no significant evidence of impaired fertility or harm to the fetus due to famotidine. While no direct fetotoxic effects have been observed, sporadic abortions occurring only in mothers displaying marked decreased food intake were seen in some rabbits at oral doses of 200 mg/kg/day (about 49 times the recommended human dose of 80 mg per day, based on body surface area) or higher. There are, however, no adequate or well-controlled studies in pregnant women. Because animal reproductive studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
8.2 Lactation
Risk Summary
There are limited data available on the presence of famotidine in human breast milk. There were no effects on the breastfed infant. There are no data on famotidine effects on milk production. Famotidine is present in the milk of lactating rats (see Data).
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for famotidine and any potential adverse effects on the breastfed child from famotidine or from the underlying maternal condition.
Data
Animal Data
Transient growth depression was observed in young rats suckling from mothers treated with maternotoxic doses of famotidine at least 600 times the usual human dose.
8.4 Pediatric Use
The safety and effectiveness of famotidine have been established in pediatric patients for the treatment of peptic ulcer disease (i.e., duodenal ulcer, gastric ulcer) and GERD (i.e., symptomatic nonerosive GERD, erosive esophagitis as diagnosed by endoscopy). The use of famotidine and the recommended dosage of famotidine in these pediatric patients is supported by evidence from adequate and well-controlled studies of famotidine in adults and published pharmacokinetic and pharmacodynamic data in pediatric patients [see Dosage and Administration (2.1), Clinical Pharmacology (12.2, 12.3)]. In pediatric patients, the safety and effectiveness for the treatment of pathological hypersecretory conditions and reduction of risk of duodenal ulcer recurrence have not been established.
Famotidine 20 mg and 40 mg tablets are not recommended for use in pediatric patients weighing less than 40 kg because these tablet strengths exceed the recommended dose for these patients [see Dosage and Administration (2.1)]. For pediatric patients weighing less than 40 kg, consider another famotidine formulation (e.g., oral suspension, lower dose tablet).
8.5 Geriatric Use
Of the 1,442 famotidine-treated patients in clinical studies, approximately 10% were 65 and older. In these studies, no overall differences in safety or effectiveness were observed between elderly and younger patients. In postmarketing experience, CNS adverse reactions have been reported in elderly patients with and without renal impairment receiving famotidine [see Warnings and Precautions (5.1)].
Famotidine is known to be substantially excreted by the kidney and the risk of adverse reactions to famotidine may be greater in elderly patients, particularly those with impaired renal function [see Use in Specific Populations (8.6)].
In general, use the lowest effective dose of famotidine for an elderly patient and monitor renal function [see Dosage and Administration (2.2)].
8.6 Renal Impairment
CNS adverse reactions and prolonged QT intervals have been reported in patients with moderate and severe renal impairment [see Warnings and Precautions (5.1)]. The clearance of famotidine is reduced in adults with moderate and severe renal impairment compared to adults with normal renal function [see Clinical Pharmacology (12.3)]. No dosage adjustment is needed in patients with mild renal impairment (creatinine clearance greater than or equal to 60 mL/minute). Dosage reduction is recommended in adult and pediatric patients greater than or equal to 40 kg with moderate or severe renal impairment (creatinine clearance less than 60 mL/minute) [see Dosage and Administration (2.2)].
10 OVERDOSAGE
The types of adverse reactions in overdosage of famotidine are similar to the adverse reactions encountered with use of recommended dosages [see Adverse Reactions (6.1)].
In the event of overdosage, treatment should be symptomatic and supportive. Unabsorbed material should be removed from the gastrointestinal tract, the patient should be monitored and supportive therapy should be employed.
Due to low binding to plasma proteins, famotidine is eliminated by hemodialysis. There is limited experience on the usefulness of hemodialysis as a treatment for famotidine overdosage.
11 DESCRIPTION
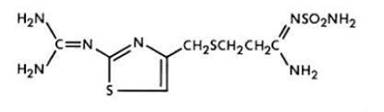
The active ingredient in famotidine tablets is a histamine-2 (H2) receptor antagonist. Famotidine is N'-(aminosulfonyl)-3-[[[2-[(diaminomethylene)amino]-4-thiazolyl]methyl]thio]propanimidamide. The molecular formula of famotidine is C8H15N7O2S3 and its molecular weight is 337.45. Its structural formula is:
Each famotidine tablet for oral administration contains either 20 mg or 40 mg of famotidine and the following inactive ingredients: colloidal silicon dioxide, hypromellose, magnesium stearate, microcrystalline cellulose, polyethylene glycol, pregelatinized starch (source: maize), sodium starch glycolate, talc and titanium dioxide.
Famotidine, USP is a white to pale yellowish-white crystalline powder that is freely soluble in dimethyl formamide and glacial acetic acid, slightly soluble in methanol, very slightly soluble in water, practically insoluble in acetone, in alcohol, in chloroform, in ether and ethyl acetate.
FDA approved dissolution test specifications differ from USP.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Famotidine is a competitive inhibitor of histamine-2 (H2) receptors. The primary clinically important pharmacologic activity of famotidine is inhibition of gastric secretion. Both the acid concentration and volume of gastric secretion are suppressed by famotidine, while changes in pepsin secretion are proportional to volume output.
12.2 Pharmacodynamics
Adults
Famotidine inhibited both basal and nocturnal gastric secretion, as well as secretion stimulated by food and pentagastrin. After oral administration of famotidine, the onset of the antisecretory effect occurred within one hour; the maximum effect was dose-dependent, occurring within one hour to three hours. Duration of inhibition of secretion by doses of 20 mg and 40 mg was 10 hours to 12 hours.
Single evening oral doses of 20 mg and 40 mg inhibited basal and nocturnal acid secretion in all subjects; mean nocturnal gastric acid secretion was inhibited by 86% and 94%, respectively, for a period of at least 10 hours. The same doses given in the morning suppressed food-stimulated acid secretion in all subjects. The mean suppression was 76% and 84%, respectively, 3 hours to 5 hours after administration and 25% and 30%, respectively, 8 hours to 10 hours after administration. In some subjects who received the 20 mg dose, however, the antisecretory effect was dissipated within 6 hours to 8 hours. There was no cumulative effect with repeated doses. The nocturnal intragastric pH was raised by evening doses of 20 mg and 40 mg of famotidine to mean values of 5 and 6.4, respectively. When famotidine was given after breakfast, the basal daytime interdigestive pH at 3 hours and 8 hours after 20 mg or 40 mg of famotidine was raised to about 5.
Famotidine had little or no effect on fasting or postprandial serum gastrin levels. Gastric emptying and exocrine pancreatic function were not affected by famotidine.
In clinical pharmacology studies, systemic effects of famotidine in the CNS, cardiovascular, respiratory or endocrine systems were not noted. Also, no anti-androgenic effects were noted. Serum hormone levels, including prolactin, cortisol, thyroxine (T4) and testosterone, were not altered after treatment with famotidine.
Pediatric Patients
Pharmacodynamics of famotidine, assessed by gastric pH, were evaluated in 5 pediatric patients 2 years to 13 years of age using the sigmoid Emax model. These data suggest that the relationship between serum concentration of famotidine and gastric acid suppression is similar to that observed in adults (see Table 3).
| a Using the Sigmoid Emax model, serum concentrations of famotidine associated with 50% maximum gastric acid reduction are presented as means ± SD. | |
|
EC50 (ng/mL)a
|
|
|
Pediatric Patients |
26 ± 13 |
|
Adults | |
|
Healthy adult subjects |
26.5 ± 10.3 |
|
Adult patients with upper GI bleeding |
18.7 ± 10.8 |
In a study examining the effect of famotidine on gastric pH and duration of acid suppression in pediatric patients, four pediatric patients ages 11 years to 15 years of age using the oral formulation at a dose of 0.5 mg/kg, maintained a gastric pH above 5 for 13.5 hours ± 1.8 hours.
12.3 Pharmacokinetics
Absorption
Famotidine is incompletely absorbed. The bioavailability of oral doses is 40% to 45%. Bioavailability may be slightly increased by food or slightly decreased by antacids; however, these effects are of no clinical consequence.
Peak famotidine plasma levels occur in 1 hour to 3 hours. Plasma levels after multiple dosages are similar to those after single doses.
Distribution
Fifteen to 20% of famotidine in plasma is protein bound.
Elimination
Metabolism
Famotidine undergoes minimal first-pass metabolism. Twenty-five to 30% of an oral dose was recovered in the urine as unchanged compound. The only metabolite identified in humans is the S-oxide.
Excretion
Famotidine has an elimination half-life of 2.5 hours to 3.5 hours. Famotidine is eliminated by renal (65% to 70%) and metabolic (30% to 35%) routes. Renal clearance is 250 mL/minute to 450 mL/minute, indicating some tubular excretion.
Specific Populations
Pediatric Patients
Bioavailability studies of 8 pediatric patients (11 years to 15 years of age) showed a mean oral bioavailability of 0.5 compared to adult values of 0.42 to 0.49. Oral doses of 0.5 mg per kg achieved AUCs of 580 nghr/mL ± 60 nghr/mL in pediatric patients 11 years to 15 years of age, compared to 482 nghr/mL ± 181 nghr/mL in adults treated with 40 mg orally.
Patients with Renal Impairment
In adult patients with severe renal impairment (creatinine clearance less than 30 mL/minute), the systemic exposure (AUC) of famotidine increased at least 5-fold. In patients with moderate renal impairment (creatinine clearance between 30 mL/minute to 60 mL/minute), the AUC of famotidine increased at least 2-fold [see Dosage and Administration (2.2), Use in Specific Population (8.6)].
Drug Interaction Studies
Human Organic Anion Transporter (OAT) 1 and 3
In vitro studies indicate that famotidine is a substrate for OAT1 and OAT3. Following coadministration of probenecid (1,500 mg), an inhibitor of OAT1 and OAT3, with a single oral 20 mg dose of famotidine in 8 healthy subjects, the serum AUC0-10h of famotidine increased from 424 nghr/mL to 768 nghr/mL and the maximum serum concentration (Cmax) increased from 73 ng/mL to 113 ng/mL. Renal clearance, urinary excretion rate and amount of famotidine excreted unchanged in urine were decreased. The clinical relevance of this interaction is unknown.
Multidrug and Toxin Extrusion Protein 1 (MATE-1)
An in vitro study showed that famotidine is an inhibitor of MATE-1. However, no clinically significant interaction with metformin, a substrate for MATE-1, was observed.
CYP1A2
Famotidine is a weak CYP1A2 inhibitor.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenic potential of famotidine was assessed in a 106 week oral carcinogenicity study in rats and a 92 week oral carcinogenicity study in mice. In the 106 week study in rats and the 92 week study in mice at oral doses of up to 2,000 mg/kg/day (approximately 243 times and 122 times, respectively, based on body surface area, the recommended human dose of 80 mg per day for the treatment of erosive esophagitis), there was no evidence of carcinogenic potential for famotidine.
Famotidine was negative in the microbial mutagen test (Ames test) using Salmonella typhimurium and Escherichia coli with or without rat liver enzyme activation at concentrations up to 10,000 mcg/plate. In in vivo studies in mice, with a micronucleus test and a chromosomal aberration test, no evidence of a mutagenic effect was observed.
In studies with rats given oral doses of up to 2,000 mg/kg/day (approximately 243 times, based on body surface area, the recommended human dose of 80 mg per day) fertility and reproductive performance were not affected.
14 CLINICAL STUDIES
14.1 Active Duodenal Ulcer
In a U.S. multicenter, double-blind trial in adult outpatients with endoscopically confirmed duodenal ulcer (DU), orally administered famotidine was compared to placebo. As shown in Table 4, 70% of patients treated with famotidine 40 mg at bedtime were healed by Week 4. Most patients' DU healed within 4 weeks.
Patients not healed by Week 4 were continued in the trial. By Week 8, 83% of patients treated with famotidine had healed DU, compared to 45% of patients treated with placebo. The incidence of DU healing with famotidine was greater than with placebo at each time point based on proportion of endoscopically confirmed healed DUs. Trials have not assessed the safety of famotidine in uncomplicated active DU for periods of more than 8 weeks.
| ap<0.001 vs. placebo | |||
|
Famotidine
|
Famotidine
|
Placebo
|
|
|
Week 2 |
32%a
|
38%a
|
17% |
|
Week 4 |
70%a
|
67%a
|
31% |
In this study, time to relief of daytime and nocturnal pain was shorter for patients receiving famotidine than for patients receiving placebo; patients receiving famotidine also took less antacid than patients receiving placebo.
14.2 Active Gastric Ulcer
In both a U.S. and an international multicenter, double-blind trials in patients with endoscopically confirmed active gastric ulcer (GU), orally administered famotidine 40 mg at bedtime was compared to placebo. Antacids were permitted during the trials, but consumption was not significantly different between the famotidine and placebo groups.
As shown in Table 5, the incidence of GU healing confirmed by endoscopy (dropouts counted as unhealed) with famotidine was greater than placebo at Weeks 6 and Weeks 8 in the U.S. trial and at Weeks 4, Weeks 6 and Weeks 8 in the international trial. In these trials, most famotidine-treated patients healed within 6 weeks. Trials have not assessed the safety of famotidine in uncomplicated active GU for periods of more than 8 weeks.
| a p≤0.01 vs. placebo | ||||
| b p≤0.05 vs. placebo | ||||
|
U.S. Study (N=149)
|
International Study (N=294)
|
|||
|
Famotidine
|
Placebo
|
Famotidine
|
Placebo
|
|
|
Week 4 |
45% |
39% |
47%a
|
31% |
|
Week 6 |
66%a
|
44% |
65%a
|
46% |
|
Week 8 |
78%b
|
64% |
80%a
|
54% |
Time to complete relief of daytime and nighttime pain was statistically significantly shorter for patients receiving famotidine than for patients receiving placebo; however, neither trial demonstrated a statistically significant difference in the proportion of patients whose pain was relieved by the end of the trial (Week 8).
14.3 Symptomatic Gastroesophageal Reflux Disease (GERD)
Orally administered famotidine was compared to placebo in a U.S. trial that enrolled patients with symptoms of GERD and without endoscopic evidence of esophageal erosion or ulceration. As shown in Table 6, patients treated with famotidine 20 mg twice daily had greater improvement in symptomatic GERD than patients treated with 40 mg at bedtime or placebo.
| a p≤0.01 vs. placebo | |||
|
Famotidine
|
Famotidine
|
Placebo
|
|
|
Week 6 |
82%a
|
69% |
62% |
14.4 Erosive Esophagitis due to GERD
Healing of endoscopically verified erosion and symptomatic improvement were studied in a U.S. and an international double-blind trials. Healing was defined as complete resolution of all erosions visible with endoscopy. The U.S. trial comparing orally administered famotidine 40 mg twice daily to placebo and orally administered famotidine 20 mg twice daily showed a significantly greater percentage of healing of erosive esophagitis for famotidine 40 mg twice daily at Weeks 6 and Weeks 12 (Table 7).
| a p≤0.01 vs. placebo | |||
| b p≤0.01 vs. famotidine 20 mg twice daily | |||
| c p≤0.05 vs. famotidine 20 mg twice daily | |||
|
Famotidine
|
Famotidine
|
Placebo
|
|
|
Week 6 |
48%a,b
|
32% |
18% |
|
Week 12 |
69%a,c
|
54%a
|
29% |
As compared to placebo, patients in the U.S. trial who received famotidine had faster relief of daytime and nighttime heartburn and a greater percentage of famotidine-treated patients experienced complete relief of nighttime heartburn. These differences were statistically significant.
In the international trial, when orally administered famotidine 40 mg twice daily was compared to orally administered ranitidine 150 mg twice daily, a statistically significantly greater percentage of healing of erosive esophagitis was observed with famotidine 40 mg twice daily at Week 12 (Table 8). There was, however, no significant difference in symptom relief among treatment groups.
| ap≤0.05 vs. ranitidine 150 mg twice daily | |||
|
Famotidine
|
Famotidine
|
Ranitidine
|
|
|
Week 6 |
48% |
52% |
42% |
|
Week 12 |
71%a
|
68% |
60% |
14.5 Pathological Hypersecretory Conditions
In trials of patients with pathological hypersecretory conditions such as Zollinger-Ellison syndrome with or without multiple endocrine neoplasias, famotidine significantly inhibited gastric acid secretion and controlled associated symptoms. Orally administered famotidine dosages from 20 mg to 160 mg every 6 hours maintained basal acid secretion below 10 mEq/hour; initial dosages were titrated to the individual patient need and subsequent adjustments were necessary with time in some patients.
14.6 Risk Reduction of Duodenal Ulcer Recurrence
Two randomized, double-blind, multicenter trials in patients with endoscopically confirmed healed DUs demonstrated that patients receiving treatment with orally administered famotidine 20 mg at bedtime had lower rates of DU recurrence, as compared with placebo.
- In the U.S. trial, DU recurrence within 12 months was 2.4 times greater in patients treated with placebo than in the patients treated with famotidine. The 89 famotidine-treated patients had a cumulative observed DU recurrence rate of 23%, compared to a 57% in the 89 patients receiving placebo (p<0.01).
- In the international trial, the cumulative observed DU recurrence within 12 months in the 307 famotidine-treated patients was 36%, compared to 76% in the 325 patients who received placebo (p<0.01).
Controlled trials have not extended beyond one year.
16 HOW SUPPLIED/STORAGE AND HANDLING
Famotidine Tablets USP, 20 mg are white to off white, round, biconvex film-coated tablets debossed with "Z21" on one side and plain on other side and are supplied as follows:
NDC: 68788-8269-4 in bottle of 14 tablets with child-resistant closure
NDC: 68788-8269-3 in bottle of 30 tablets with child-resistant closure
NDC: 68788-8269-6 in bottle of 60 tablets with child-resistant closure
NDC: 68788-8269-9 in bottle of 90 tablets with child-resistant closure
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
Dispense in a USP tight, light-resistant container.
17 PATIENT COUNSELING INFORMATION
Central Nervous System (CNS) Adverse Reactions
Advise elderly patients and those with moderate and severe renal impairment of the risk of CNS adverse reactions, including confusion, delirium, hallucinations, disorientation, agitation, seizures and lethargy [see Warnings and Precautions (5.1)]. Report symptoms immediately to a healthcare provider.
QT Prolongation
Advise patients with moderate and severe renal impairment of the risk of QT interval prolongation [see Use in Specific Populations (8.6)]. Report new cardiac symptoms, such as palpitations, fainting and dizziness or lightheadedness immediately to a healthcare provider.
Administration
Advise patients:
- Take famotidine tablets once daily before bedtime or twice daily in the morning and before bedtime, as recommended.
- Famotidine tablets may be taken with or without food.
- Famotidine tablets may be given with antacids.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
For more information, go to MedicalAffairs@zydususa.com or Tel. 1-877-993-8779.
Manufactured by:
Zydus Lifesciences Ltd.
Ahmedabad, India
Distributed by:
Zydus Pharmaceuticals (USA) Inc.
Pennington, NJ 08534
Rev.: 06/23
Repackaged By: Preferred Pharmaceuticals Inc.
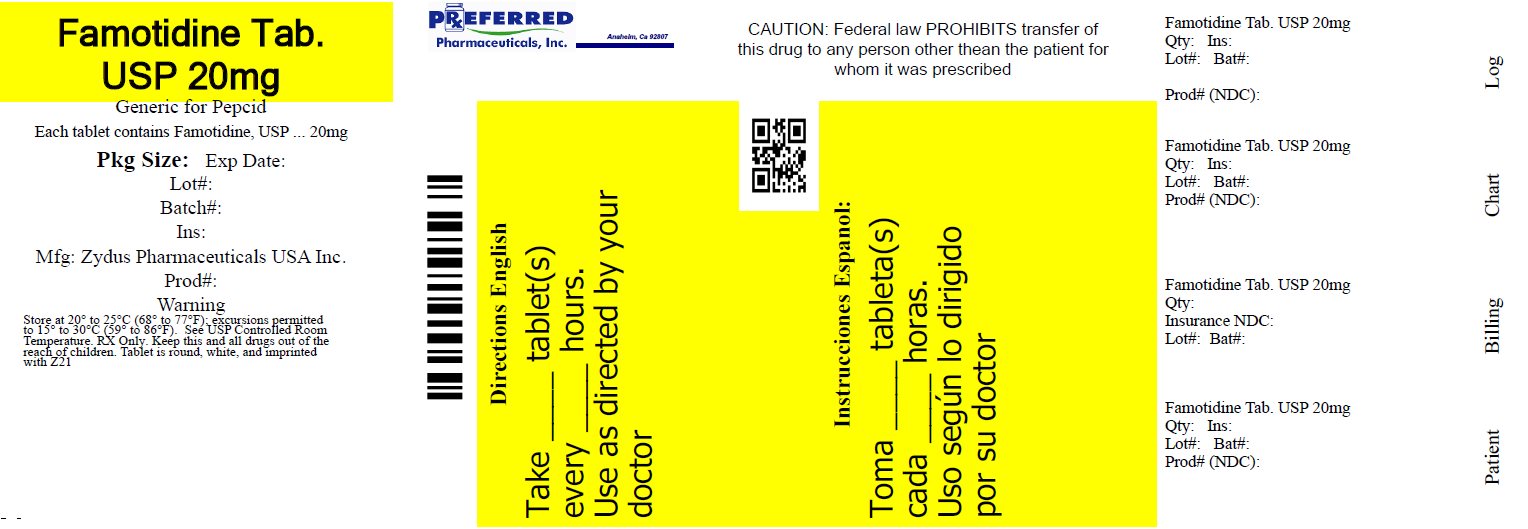
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC: 68788-8269
Famotidine Tablets USP, 20 mg
Rx only
Zydus
Repackaged By: Preferred Pharmaceuticals Inc.
| FAMOTIDINE
famotidine tablet, film coated |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Preferred Pharmaceuticals Inc. (791119022) |
| Registrant - Preferred Pharmaceuticals Inc. (791119022) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Preferred Pharmaceuticals Inc. | 791119022 | REPACK(68788-8269) | |