AUCATZYL- obecabtagene autoleucel kit
AUCATZYL by
Drug Labeling and Warnings
AUCATZYL by is a Other medication manufactured, distributed, or labeled by Autolus Inc., Autolus Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use AUCATZYL safely and effectively. See full prescribing information for AUCATZYL.
AUCATZYL® (obecabtagene autoleucel) suspension for intravenous infusion
Initial U.S. Approval: 2024WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC TOXICITIES, and SECONDARY HEMATOLOGICAL MALIGNANCIES
See full prescribing information for complete boxed warning.
Cytokine Release Syndrome (CRS) occurred in patients receiving AUCATZYL. Do not administer AUCATZYL to patients with active infection or inflammatory disorders. Prior to administering AUCATZYL, ensure that healthcare providers have immediate access to medications and resuscitative equipment to manage CRS. (2.2, 2.3, 5.1).
Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS), including fatal or life-threatening reactions, occurred in patients receiving AUCATZYL, including concurrently with CRS or after CRS resolution. Monitor for neurologic signs and symptoms after treatment with AUCATZYL. Prior to administering AUCATZYL, ensure that healthcare providers have immediate access to medications and resuscitative equipment to manage neurologic toxicities (2.2, 2.3, 5.2).
T cell malignancies have occurred following treatment of hematologic malignancies with BCMA- and CD19-directed genetically modified autologous T cell immunotherapies (5.8).
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
AUCATZYL is a CD19-directed genetically modified autologous T cell immunotherapy indicated for the treatment of adults with relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL) (1).
DOSAGE AND ADMINISTRATION
For autologous use only. For intravenous use only.
Do NOT use a leukodepleting filter (2.4).
Prior to infusion
- Administer a lymphodepleting chemotherapy regimen of fludarabine/cyclophosphamide. (2.3).
- Ensure availability of bone marrow assessment results from a sample obtained within 7 days prior to start of lymphodepleting chemotherapy (2.3).
- Premedicate with acetaminophen (2.3).
- Confirm availability of tocilizumab prior to infusion (2.3).
AUCATZYL Dose and Administration
- Verify patient's identity prior to infusion (2.3).
- Dosing is based on the Dose Schedule Planner (2.3).
- The total recommended dose of AUCATZYL is 410 × 106 CD19 chimeric antigen receptor (CAR)-positive viable T cells (2.1).
- The treatment regimen consists of a split dose infusion to be administered on Day 1 and Day 10 (± 2 days) (2.1). Dose to be administered is determined by the patient bone marrow blast assessment.
- See Full Prescribing Information for important preparation and administration information (2.3, 2.4).
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
None (4).
WARNINGS AND PRECAUTIONS
- Prolonged Cytopenias: Patients may exhibit Grade 3 or higher cytopenias for several weeks following AUCATZYL infusion. Monitor complete blood counts (5.3).
- Infections: Monitor patients for signs and symptoms of infection; treat appropriately (5.4).
- Hypogammaglobulinemia: Monitor and consider immunoglobulin replacement therapy (5.5).
- Hemophagocytic Lymphohistiocytosis/ Macrophage Activation Syndrome: Administer treatment per institutional standards (5.6).
- Hypersensitivity Reactions: Monitor for hypersensitivity reactions during infusion (5.7).
- Secondary Malignancies: T cell malignancies have occurred following treatment of hematologic malignancies with BCMA- and CD19-directed genetically modified autologous T cell immunotherapies. In the event that a secondary malignancy occurs after treatment with AUCATZYL, contact Autolus Inc at 1-855-288-5227 (5.8).
ADVERSE REACTIONS
The most common (non-laboratory) adverse reactions (incidence ≥ 20%) are: CRS, infections - pathogen unspecified, musculoskeletal pain, viral infections, fever, nausea, bacterial infectious disorders, diarrhea, febrile neutropenia, ICANS, hypotension, pain, fatigue, headache, encephalopathy, and hemorrhage (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Autolus Inc at toll-free phone 1-855-288-5227 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch (17).
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 2/2026
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC TOXICITIES, and SECONDARY HEMATOLOGICAL MALIGNANCIES
1 INDICATION AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dose
2.2 Dosage Modification for Adverse Reactions
2.3 Administration
2.4 Infusion Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cytokine Release Syndrome
5.2 Neurologic Toxicities
5.3 Prolonged Cytopenias
5.4 Infections
5.5 Hypogammaglobulinemia
5.6 Hemophagocytic Lymphohistiocytosis/Macrophage Activation Syndrome
5.7 Hypersensitivity Reactions
5.8 Secondary Malignancies
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.6 Immunogenicity
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC TOXICITIES, and SECONDARY HEMATOLOGICAL MALIGNANCIES
- Cytokine Release Syndrome (CRS) occurred in patients receiving AUCATZYL. Do not administer AUCATZYL to patients with active infection or inflammatory disorders. Prior to administering AUCATZYL, ensure that healthcare providers have immediate access to medications and resuscitative equipment to manage CRS [see Dosage and Administration (2.2, 2.3), Warnings and Precautions (5.1)].
- Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS), including fatal or life-threatening reactions, occurred in patients receiving AUCATZYL, including concurrently with CRS or after CRS resolution. Monitor for neurologic signs and symptoms after treatment with AUCATZYL. Prior to administering AUCATZYL, ensure that healthcare providers have immediate access to medications and resuscitative equipment to manage neurologic toxicities. Provide supportive care and/or corticosteroids, as needed [see Dosage and Administration (2.2, 2.3), Warnings and Precautions (5.2)].
- T cell malignancies have occurred following treatment of hematologic malignancies with BCMA- and CD19-directed genetically modified autologous T cell immunotherapies [see Warnings and Precautions (5.8)].
- 1 INDICATION AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Dose
For autologous use only. For intravenous use only.
Strictly follow Administration instructions to minimize dosing errors [see Overdosage (10)].
The total recommended dose of AUCATZYL is 410 × 106 CD19 chimeric antigen receptor (CAR)-positive viable T cells supplied in three to five infusion bags. Bags are supplied in three color-coded bag configurations (10 × 106, 100 × 106, 300 × 106) for split dose administration.
Table 1: AUCATZYL Infusion Bag Configurations CAR-positive T Cell Dose (Bag Configuration) Color Code Volume Fully Infused 10 × 106 Blue 10 mL No (See Section 2.3) 100 × 106 Orange Variable Yes 300 × 106 Red Variable Yes The treatment regimen consists of a split dose infusion to be administered on Day 1 and Day 10 (± 2 days), see Figure 1 and Figure 3.
- The dosage regimen will be determined by the tumor burden assessed by bone marrow blast percentage from a sample obtained within 7 days prior to the start of lymphodepletion [see Dosing and Administration (2.3, 2.4), Figure 1 and Figure 3].
- See the Release for Infusion certificate and Dose Schedule Planner for the actual cell counts and volumes to be infused and to select the appropriate dosage regimen [see Dosage and Administration (2.4) and Dosage Forms and Strengths (3)].
2.2 Dosage Modification for Adverse Reactions
Table 2: Dosage Modifications Intended to Reduce the Risk of Adverse Reactions Adverse Event Severity * Actions
Second Split Dose
Day 10 (± 2 days)- * 1. Based on the Common Terminology Criteria for Adverse Events (CTCAE) v5.0. Grade 1 is mild, Grade 2 is moderate, Grade 3 is severe, and Grade 4 is life-threatening.
Cytokine Release Syndrome following the first split dose [see Warnings and Precautions (5.1)]. Grade 2 Consider postponing AUCATZYL infusion up to Day 21 to allow for the CRS to resolve to Grade ≤ 1. Grade ≥ 3 Discontinue treatment. Immune Effector Cell-associated Neurotoxicity Syndrome following the first split dose [see Warnings and Precautions (5.2)]. Grade 1 Consider postponing AUCATZYL infusion up to Day 21 to allow for the ICANS to completely resolve. Grade ≥ 2 Discontinue treatment. Pulmonary or cardiac toxicities following the first split dose. Grade ≥ 3 Discontinue treatment. Severe intercurrent infection at the time of AUCATZYL infusion [see Warnings and Precautions (5.4)]. Grade ≥ 3 Consider postponing AUCATZYL infusion up to Day 21 until the severe intercurrent infection is considered controlled. Requirement for supplementary oxygen. Grade ≥ 3 Consider postponing AUCATZYL treatment up to Day 21 to allow for the adverse reaction to resolve. Other clinically relevant adverse reactions following the first split dose [see Warnings and Precautions (5)]. Grade ≥ 3 Consider postponing AUCATZYL infusion up to Day 21 to allow for the adverse reaction to resolve. 2.3 Administration
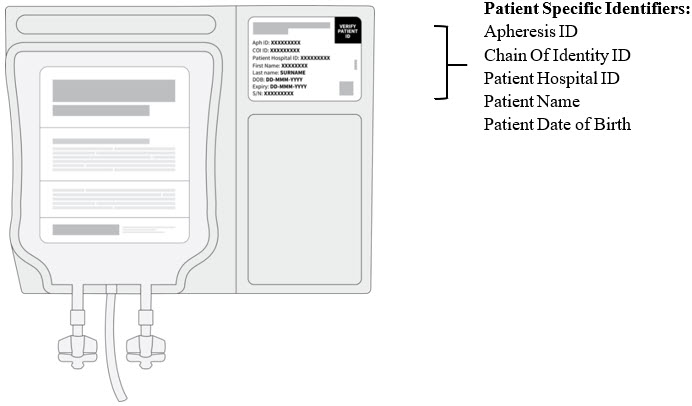
AUCATZYL is for autologous use only. The patient's identity must match the patient identifiers on the AUCATZYL infusion bag. Do not infuse AUCATZYL if the information on the patient-specific label does not match the intended patient.
Preparing the Patient for AUCATZYL Infusion
Bone marrow assessment
- A bone marrow assessment must be available from a sample obtained within 7 days prior to the commencement of the lymphodepleting chemotherapy treatment, see Figure 1.
Figure 1: AUCATZYL Treatment Schedule
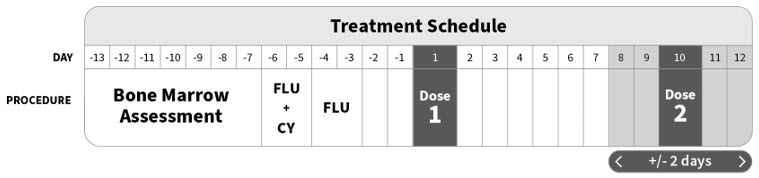
- The bone marrow assessment will be used to determine the AUCATZYL dosage regimen based on a Bone Marrow Blast of > 20% or ≤ 20%, see Figure 3.
- If the bone marrow assessment results are inconclusive:
- – Repeat biopsy or aspirate, NOTE a repeat biopsy or aspirate is only possible if lymphodepleting chemotherapy treatment has not started.
- – If results remain inconclusive, proceed with the Bone Marrow Blast of > 20% (i.e., administration of the 10 × 106 dose on Day 1) per the AUCATZYL Dose Schedule Planner.
- If the bone marrow assessment results are inconclusive:
Pretreatment
- Confirm availability of AUCATZYL prior to starting the lymphodepleting chemotherapy treatment.
- Administer the lymphodepleting chemotherapy regimen before infusion of AUCATZYL: fludarabine (FLU) 30 mg/m2/day intravenously (IV) for four days and cyclophosphamide (CY) 500 mg/m2/day IV for two days starting with the first dose of fludarabine. (total dose: FLU 120 mg/m2; CY 1000 mg/m2), see Figure 1. Infuse AUCATZYL 3 days (± 1 day) after completion of lymphodepleting chemotherapy treatment (Day 1), allowing a minimum 48-hour washout.
- Delay AUCATZYL treatment if the patient is experiencing severe intercurrent infection. If the patient requires supplementary oxygen AUCATZYL should only be infused if considered appropriate based on the treating physician's benefit/risk assessment.
A delay to the second split dose may be required to manage toxicities [see Dosage Modification for Adverse Reactions (2.2) and Warnings and Precautions (5)].
Receipt and storage of AUCATZYL
- AUCATZYL is supplied directly to the cellular therapy laboratory associated with the infusion center in the vapor phase of a liquid nitrogen shipper [see How Supplied/Storage and Handling (16)].
Confirm the patient's identity on the infusion bags with the patient identifiers on the shipper, see Figure 2.
Figure 2: Patient Specific Identifiers
- Keep the infusion bag(s) in the metal cassette(s) and transfer AUCATZYL to the onsite controlled-access vapor phase of liquid nitrogen for storage below minus 150°C until ready for thaw and administration.
- Time out of the vapor phase liquid nitrogen environment should be kept to an absolute minimum to avoid premature product thaw (recommend not to exceed 90 seconds).
Planning prior to AUCATZYL preparation
- The patient batch specific Release for Infusion certificate and Dose Schedule Planner will be provided in the shipper and via Autolus' Scheduling Portal.
- Confirm the patient identifiers on the Release for Infusion certificate and infusion bags match, see Figure 2.
- Ensure the patient's bone marrow assessment results are available.
NOTE: The patient's bone marrow assessment results will be used to select the appropriate dosing regimen based on a Bone Marrow Blast of > 20% or ≤ 20%, see Figure 3. - The AUCATZYL Dose Schedule Planner is provided with the Release for Infusion certificate and assists the determination of the appropriate dose regimen to be administered on Day 1 (3 days (± 1 day) after the completion of lymphodepleting chemotherapy) and Day 10 (± 2 days). Record the following information on the Dose Schedule Planner:
- The blast percentage from the patient's bone marrow assessment.
- The AUCATZYL bag serial number(s); number of bag type required for each dose; and the specified volume to administer via syringe (for the 10 × 106 dose, Blue Bag) transcribed from the Release for Infusion certificate.
- The completion of the AUCATZYL Dose Schedule Planner will guide the treating physician on the number of bags required and preparation of AUCATZYL for the Day 1 and Day 10 (± 2 days) dose, see Figure 3.
Dose Preparation
Do NOT irradiate. Do NOT use a leukodepleting filter.
- Confirm the patient's identity with the patient identifiers on the Release for Infusion certificate. Contact Autolus Inc at 1-855-288-5227 if there are any discrepancies between the labels and the patient identifiers.
- Confirm tocilizumab and emergency equipment are available prior to infusion and during the recovery period.
- Coordinate the timing of AUCATZYL thaw and infusion. Confirm the infusion time in advance and adjust the start time of AUCATZYL thaw such that it will be available for infusion when the patient is ready and will be infused within 60 minutes of thaw.
- Complete the AUCATZYL Dose Schedule Planner, as described above to identify the dose required for Day 1 and Day 10 (± 2 days) administration, see Figure 3.
- Follow the completed AUCATZYL Dose Schedule Planner and refer to the patient batch specific Release for Infusion certificate to verify the bag(s) required for Day 1 or Day 10 (± 2 days) dosing, see Figure 3.
Transfer and Thawing
- Using the completed Dose Schedule Planner for guidance, transfer ONLY the cassette(s)/ infusion bag(s) required for the given dosing day from the onsite vapor phase liquid nitrogen storage to an appropriate transfer vessel (i.e., a vapor phase liquid nitrogen shipper, maintaining a temperature below minus 150°C) for transport to the bag thaw location.
- Transfer the required cassette(s) one by one, confirming the AUCATZYL bag serial numbers and patient identifiers on each infusion bag label, see Figure 2.
- Time out of the vapor phase liquid nitrogen environment should be kept to an absolute minimum to avoid premature product thaw (recommend not to exceed 90 seconds).
- If more than one infusion bag is required on a given dosing day, thaw each infusion bag one at a time; Do NOT remove subsequent bags from the vapor phase liquid nitrogen storage (below minus 150°C) until the infusion of the previous bag is complete.
- AUCATZYL must be continuously monitored during thawing process.
- Leave the AUCATZYL infusion bag in its overwrap, thaw at 37°C using a water bath or dry thaw method until there are no visible frozen clumps left in the infusion bag. Each bag should be gently massaged until the cells have just thawed. Thawing of each infusion bag takes between 2 and 8 minutes. Remove from water bath or thaw device immediately after thawing is complete. Carefully remove the infusion bag from the overwrap taking care to avoid damage to the bag and ports.
- Gently mix the contents of the bag to disperse clumps of cellular material and administer immediately to the patient.
- Do not re-freeze or refrigerate thawed product.
Figure 3: AUCATZYL Dosage and Schedule
- * Refer to Release for Infusion Certificate for the exact volume to be administered via syringe. Withdraw ONLY the volume.
- † The 100 × 106 (Orange Bag) and 300 × 106 (Red Bag) doses will be suspended in one or more infusion bags.
Bone Marrow Blast > 20% Day 1 
Day 10 (± 2 days) 10 × 106 Dose administered via syringe* 100 × 106 Dose administered via bag infusion†
and
300 × 106 Dose administered via bag infusion†Bone Marrow Blast ≤ 20% Day 1 
Day 10 (± 2 days) 100 × 106 Dose administered via bag infusion† 10 × 106 Dose administered via syringe*
and
300 × 106 Dose administered via bag infusion†2.4 Infusion Instructions
AUCATZYL is for autologous and intravenous use only.
The patient's identity must match the patient identifiers on the Release for Infusion certificate and infusion bag. Contact Autolus Inc at 1-855-288-5227 if there are any discrepancies between the labels and the patient identifiers.
Dose administration for 10 × 106 CD19 CAR-positive viable T cell Dose (Blue Bag)
Withdrawal of the 10 × 106 dose into the syringe should be carried as follows:
- Prepare and administer AUCATZYL using aseptic technique.
- Gently mix the contents of the bag to disperse clumps of cellular material.
- The volume to be administered for the 10 × 106 dose (Blue Bag) is specified on the Release for Infusion certificate.
- Use the smallest Luer-lock tip syringe necessary (1, 3, 5, or 10 mL) with a Luer-lock bag spike to draw up the volume as specified on the Release for Infusion certificate.
- Do NOT use a leukodepleting filter.
- Do NOT use the syringe to mix the cells, see Figure 4.
Figure 4: Syringe Infusion Guidance for the 10 × 106 Dose (Blue Bag)

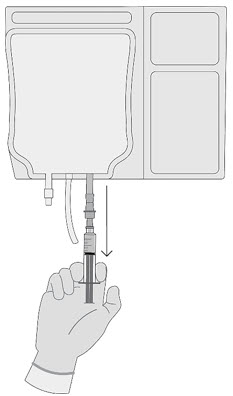
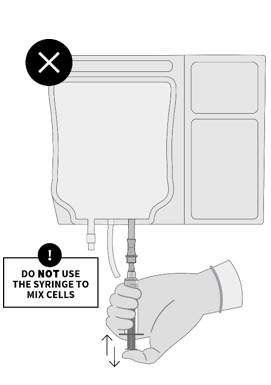
Withdraw the volume from the 10 × 106 Dose (Blue Bag) specified on the Release for Infusion certificate using a syringe fitted with a bag spike. Do not use the syringe to mix the cells Confirm withdrawal of the exact volume specified on the Release for Infusion certificate for the 10 × 106 Dose (Blue Bag). - Prime the tubing with normal saline prior to infusion.
- Once AUCATZYL has been drawn into the syringe, verify the volume and administer as an intravenous infusion as soon as possible as a slow push (approximately 0.5 mL/minute) through a central venous line (or large peripheral venous access line appropriate for blood products).
- Complete infusion at room temperature within 60 minutes post thaw and flush the tubing line with 60 mL of normal saline.
- Dispose of any unused portion of AUCATZYL (according to local biosafety guidelines).
Dose administration for 100 × 106 (Orange Bag) and/or 300 × 106 (Red Bag) CD19 CAR-positive viable T cells
Refer to the Release for Infusion certificate and Dose Schedule Planner for the following details:
- The volume and total CD19 CAR-positive viable T cell number contained in each infusion bag.
- The dose to be administered on the given dosing day and the number of bags required to deliver the specified CD19 CAR-positive viable T cell dose.
- If more than one bag is needed, thaw subsequent bags after the previous bag is fully administered.
- Prime the tubing with normal saline prior to infusion.
- Administer AUCATZYL via a gravity or peristaltic pump assisted IV infusion through a central venous line (or large peripheral venous access line appropriate for blood products).
- Do NOT use a leukodepleting filter.
- Aseptic techniques must be applied when performing a venepuncture, spiking the ports, and through the cell administration process.
- Gently mix the contents of the bag during AUCATZYL infusion to disperse cell clumps.
- Infuse the entire content of the AUCATZYL infusion bag at room temperature within 60 minutes post thaw (infusion rate within 0.1 to 27 mL/minute).
- After the entire content of the infusion bag is infused, rinse the bag with 30 mL of normal saline, then flush the tubing line with 60 mL of normal saline.
- Repeat steps 1 - 3 for any additional infusion bags required on the given dosing day. Do NOT initiate thaw of the next bag until infusion of the previous bag is complete.
AUCATZYL contains human blood cells that are genetically modified with replication-incompetent lentiviral vector. Follow universal precautions and local biosafety guidelines for handling and disposal of AUCATZYL to avoid potential transmission of infectious diseases.
Monitoring
- Monitor patients for signs and symptoms of CRS, neurologic toxicities/ICANS and other acute toxicities daily for at least 7 days following each infusion.
- Continue to monitor patients for at least 2 weeks following each infusion.
- Instruct patients to remain within proximity of a healthcare facility for at least 2 weeks following each infusion.
- Avoid driving for at least 2 weeks after each infusion.
-
3 DOSAGE FORMS AND STRENGTHS
AUCATZYL is a cell suspension for infusion.
AUCATZYL contains a total recommended dose of 410 × 106 CD19 CAR-positive viable T cells supplied in three to five infusion bags.
The infusion volume is variable and is calculated based on the concentration of CD19 CAR-positive viable T cells [see How Supplied/Storage and Handling (16)].
See the Release for Infusion certificate for actual cell counts. The Release for Infusion certificate and Dose Schedule Planner will be provided to the infusion site in the product shipper and via Autolus' Scheduling Portal.
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Cytokine Release Syndrome
Cytokine Release Syndrome (CRS) occurred following treatment with AUCATZYL. CRS was reported in 75% (75/100) of patients including Grade 3 CRS in 3% of patients.
The median time to onset of CRS was 8 days (range: 1 to 23 days) with a median duration of 5 days (range: 1 to 21 days). Sixty-eight percent of patients (51/75) experienced CRS after the first infusion, but prior to the second infusion of AUCATZYL with a median time to onset of 6 days (range: 1 to 10 days). Among patients with CRS, the most common manifestations of CRS included fever (100%), hypotension (35%) and hypoxia (19%) [see Adverse Reactions (6)].
The primary treatment for CRS was tocilizumab (73%; 55/75), with patients also receiving corticosteroids (21%; 16/75).
Prior to administering AUCATZYL, ensure that healthcare providers have immediate access to medications and resuscitative equipment to manage CRS. During and following treatment with AUCATZYL, closely monitor patients for signs and symptoms of CRS daily for at least 7 days following each infusion. Continue to monitor patients for CRS for at least 2 weeks following each infusion with AUCATZYL [see Dosage and Administration (2.1)]. Counsel patients to seek immediate medical attention should signs or symptoms of CRS occur at any time. At the first sign of CRS, immediately evaluate the patient for hospitalization and institute treatment with supportive care based on severity and consider further management per current practice guidelines.
5.2 Neurologic Toxicities
Neurologic toxicities including Immune Effector Cell-associated Neurotoxicity Syndrome (ICANS), which were fatal or life-threatening, occurred following treatment with AUCATZYL. Neurologic toxicities were reported in 64% (64/100) of patients, including Grade ≥ 3 in 12% of patients.
The median time to onset of neurologic toxicities was 10 days (range: 1 to 246 days) with a median duration of 13 days (range: 1 to 904 days). Fifty-five percent of patients (35/64) experienced neurologic toxicities after the first infusion but prior to the second infusion of AUCATZYL with a median time to onset of 6 days (range: 1 to 11 days). Among patients with neurologic toxicities, the most common symptoms (> 5%) included ICANS (38%), headache (34%), encephalopathy (33%), dizziness (22%), tremor (13%), anxiety (9%), insomnia (9%), and delirium (8%) [see Adverse Reactions (6)].
Immune Effector Cell-associated Neurotoxicity Syndrome (ICANS)
ICANS events occurred in 24% (24/100) of patients, including Grade ≥ 3 in 7% (7/100) of patients. Of the 24 patients who experienced ICANS, 33% (8/24) experienced an onset after the first infusion, but prior to the second infusion of AUCATZYL.
The median time to onset for ICANS events after the first infusion was 8 days (range: 1 to 10 days) and 6.5 days (range: 2 to 22 days) after the second infusion, with a median duration of 8.5 days (range: 1 to 53 days).
Eighty-eight percent (21/24) of patients received treatment for ICANS. All treated patients received high-dose corticosteroids and 42% (10/24) of patients received anti-epileptics prophylactically. Prior to administering AUCATZYL, ensure that healthcare providers have immediate access to medications and resuscitative equipment to manage ICANS.
During and following AUCATZYL administration, closely monitor patients for signs and symptoms of Neurologic Toxicity/ICANS. Following treatment with AUCATZYL, monitor patients daily for at least 7 days. Continue to monitor patients for at least 2 weeks following treatment with AUCATZYL. Avoid driving for at least 2 weeks after each infusion.
Counsel patients to seek medical attention should signs or symptoms of neurologic toxicity/ ICANS occur. At the first sign of Neurologic Toxicity/ICANS, immediately evaluate patients for hospitalization and institute treatment with supportive care based on severity and consider further management per current practice guidelines [see Dosage and Administration (2.1)].
5.3 Prolonged Cytopenias
Patients may exhibit cytopenias including anemia, neutropenia, and thrombocytopenia for several weeks after treatment with lymphodepleting chemotherapy and AUCATZYL. In patients who were responders to AUCATZYL, Grade ≥ 3 cytopenias that persisted beyond Day 30 following AUCATZYL infusion were observed in 71% (29/41) of patients and included neutropenia (66%, 27/41) and thrombocytopenia (54%, 22/41). Grade 3 or higher cytopenias that persisted beyond Day 60 following AUCATZYL infusion was observed in 27% (11/41) of patients and included neutropenia (17%, 7/41) and thrombocytopenia (15%, 6/41) [see Adverse Reactions (6)]. Monitor blood counts after AUCATZYL infusion.
5.4 Infections
Severe, including life-threatening and fatal infections occurred in patients after AUCATZYL infusion. Non-COVID-19 infections of all grades occurred in 67% (67/100) of patients. Grade 3 or higher non-COVID-19 infections occurred in 41% (41/100) of patients [see Adverse Reactions (6)].
AUCATZYL should not be administered to patients with clinically significant active systemic infections. Monitor patients for signs and symptoms of infection before and after AUCATZYL infusion and treat appropriately [see Dosage and Administration (2.2,2.3)]. Administer prophylactic antimicrobials according to local guidelines.
Grade 3 or higher febrile neutropenia was observed in 26% (26/100) of patients after AUCATZYL infusion and may be concurrent with CRS. In the event of febrile neutropenia, evaluate for infection and manage according to treatment guidelines as medically indicated.
Viral reactivation, potentially severe or life-threatening, can occur in patients treated with drugs directed against B cells. There is no experience with manufacturing AUCATZYL for patients with a positive test for human immunodeficiency virus (HIV) or with active hepatitis B virus (HBV) or active hepatitis C virus (HCV). Perform screening for HBV, HCV and HIV in accordance with clinical guidelines before collection of cells for manufacturing.
5.5 Hypogammaglobulinemia
Hypogammaglobulinemia and B-cell aplasia can occur in patients after treatment with AUCATZYL. Hypogammaglobulinemia was reported in 10% (10/100) of patients treated with AUCATZYL including Grade 3 events in 2 patients (2%) [see Adverse Reactions (6)].
Immunoglobulin levels should be monitored after treatment with AUCATZYL and managed per institutional guidelines including infection precautions, antibiotic or antiviral prophylaxis and immunoglobulin replacement.
The safety of immunization with live viral vaccines during or following treatment with AUCATZYL has not been studied. Vaccination with live viral vaccines is not recommended for at least 6 weeks prior to the start of lymphodepleting chemotherapy treatment, during AUCATZYL treatment, and until immune recovery following treatment AUCATZYL.
5.6 Hemophagocytic Lymphohistiocytosis/Macrophage Activation Syndrome
Hemophagocytic Lymphohistiocytosis/Macrophage Activation Syndrome (HLH/MAS), including fatal and life-threatening reactions occurred after treatment with AUCATZYL. HLH/MAS was reported in 2% (2/100) of patients and included Grade 3 and Grade 4 events with a time of onset at Day 22 and Day 41, respectively. One patient experienced a concurrent ICANS events after AUCATZYL infusion and died due to sepsis with ongoing HLH/MAS that had not resolved [see Adverse Reactions (6)].
Administer treatment for HLH/MAS according to institutional standards.
5.7 Hypersensitivity Reactions
Serious hypersensitivity reactions, including anaphylaxis, may occur due to dimethyl sulfoxide (DMSO), an excipient used in AUCATZYL. Observe patients for hypersensitivity reactions during and after AUCATZYL infusion.
5.8 Secondary Malignancies
Patients treated with AUCATZYL may develop secondary malignancies. T cell malignancies have occurred following treatment of hematologic malignancies with BCMA- and CD19-directed genetically modified autologous T cell immunotherapies. Mature T cell malignancies, including CAR-positive tumors, may present as soon as weeks following infusion, and may include fatal outcomes [see Adverse Reactions (6)].
Monitor lifelong for secondary malignancies. In the event that a secondary malignancy occurs, contact Autolus Inc at 1-855-288-5227 for reporting and to obtain instructions on the collection of patient samples for testing.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of AUCATZYL was evaluated in the FELIX study in which 100 patients with relapsed or refractory B-cell acute lymphoblastic leukemia (B-ALL) received AUCATZYL at a median dose of 410 × 106 CD19 CAR-positive viable T cells (range: 10 to 480 × 106 CD19 CAR-positive viable T cells with 90% of patients receiving the recommended dose of 410 × 106 ± 25%) [see Clinical Studies (14)].
The most common serious adverse reactions of any Grade (incidence ≥ 2%) included infections-pathogen unspecified, febrile neutropenia, ICANS, CRS, fever, bacterial infectious disorders, encephalopathy, fungal infections, hemorrhage, respiratory failure, hypotension, ascites, HLH/MAS, thrombosis and hypoxia.
Nine patients (9%) experienced fatal adverse reactions which included infections (sepsis, pneumonia, peritonitis), ascites, pulmonary embolism, acute respiratory distress syndrome, HLH/MAS and ICANS. Of the 9 patients, five patients who died from infections had pre-existing and ongoing neutropenia prior to receiving bridging therapy, lymphodepletion chemotherapy treatment and/or AUCATZYL.
Table 3 summarizes the adverse reactions (excluding laboratory abnormalities) that occurred in at least 10% of patients. Table 4 presents the most common Grade 3 or 4 laboratory abnormalities, occurring in at least 10% of patients.
Table 3: Adverse Reactions Occurring in ≥ 10% of Patients in FELIX Study (N=100) Adverse Reaction Any Grade (%) Grade 3 or Higher (%) - * Is a composite that includes multiple related terms.
- † Encephalopathy includes aphasia, cognitive disorder, confusional state, depressed level of consciousness, disturbance in attention, dysarthria, dysgraphia, encephalopathy, lethargy, memory impairment, mental status changes, posterior reversible encephalopathy syndrome, somnolence.
Blood and lymphatic system disorders Febrile neutropenia 26 26 Coagulopathy * 10 6 Cardiac disorders Tachycardia * 12 0 Gastrointestinal disorders Nausea 29 2 Diarrhea 26 0 Vomiting 18 0 Abdominal pain * 16 1 Constipation 11 0 General disorders and administration site conditions Fever 29 1 Pain * 23 0 Fatigue * 22 3 Edema * 12 0 Chills 11 0 Immune system disorders Cytokine release syndrome 75 3 Hypogammaglobulinemia 10 2 Infections and infestations Infections - pathogen unspecified * 44 31 Viral infections excluding COVID-19 * 16 1 COVID-19 * 18 6 Bacterial infections * 26 11 Fungal infections * 15 5 Investigations Weight decreased 11 2 Metabolism and nutrition disorders Decreased appetite 13 3 Musculoskeletal and connective tissue disorders Musculoskeletal pain * 36 4 Nervous system disorders Immune effector cell-associated neurotoxicity syndrome 24 7 Headache 22 0 Encephalopathy † 21 4 Dizziness * 14 0 Respiratory, thoracic and mediastinal disorders Cough * 14 0 Skin and subcutaneous tissue disorders Rash * 17 1 Vascular disorders Hypotension * 23 4 Hemorrhage * 20 4 Other clinically important adverse reactions that occurred in less than 10% of patients treated with AUCATZYL include the following:
- Cardiac disorders: arrhythmia (5%), palpitations (2%), cardiac failure (1%).
- Endocrine disorders: adrenal insufficiency (2%).
- Eye disorders: visual impairment (2%).
- Gastrointestinal disorders: stomatitis (5%), ascites (4%).
- Immune system disorders: graft versus host disease (4%), HLH/MAS (2%).
- Injury, poisoning and procedural complications: infusion related reaction (2%).
- Nervous system and psychiatric disorders: tremor (8%), motor dysfunction (6%), delirium (5%), seizure (2%).
- Renal disorders: renal impairment (7%).
- Respiratory disorders: respiratory failure (8%), pleural effusion (4%).
- Skin and subcutaneous tissue disorders: skin ulcer (2%).
- Vascular disorders: thrombosis (5%).
Table 4: Grade 3 or 4 * Laboratory Abnormalities that Worsened from Baseline † in ≥ 10% of Patients in FELIX Study (N=100) Laboratory Abnormality Grades 3 or 4 (%) - * Laboratory abnormalities graded using NCI Common Terminology Criteria for Adverse Events version 5.0.
- † Baseline laboratory values were assessed prior to lymphodepleting chemotherapy.
Lymphocytopenia 90 Leukopenia 87 Neutropenia 72 Thrombocytopenia 48 Anemia 43 Hyperferritinemia 13 Aspartate aminotransferase increased 10 6.2 Postmarketing Experience
Because adverse events to marketed products are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to product exposure. The following adverse event has been identified during postmarketing use of BCMA- or CD19-directed genetically modified autologous T cell immunotherapies:
Neoplasms: T cell malignancies.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are limited available data with AUCATZYL use in pregnant women. In the FELIX study, one patient became pregnant 6 months following treatment with AUCATZYL. The patient had a premature delivery at 30 weeks of pregnancy.
No animal reproductive and developmental toxicity studies have been conducted with AUCATZYL to assess whether AUCATZYL can cause fetal harm when administered to a pregnant woman.
It is not known if AUCATZYL has the potential to be transferred to the fetus and cause fetal toxicity. Based on the mechanism of action of AUCATZYL, if the transduced cells cross the placenta, they may cause fetal toxicity, including B-cell lymphocytopenia and hypogammaglobinemia. Therefore, AUCATZYL is not recommended for women who are pregnant. Pregnancy after AUCATZYL infusion should be discussed with the treating physician.
In the U.S. general population, the estimated background risk of major birth defects is 2% to 4% and of miscarriage is 15% to 20% of clinically recognized pregnancies.
8.2 Lactation
Risk Summary
There is no information regarding the presence of AUCATZYL in human milk, the effect on the breastfed infant, and the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for AUCATZYL and any potential adverse effects on the breastfed infant from AUCATZYL or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Pregnancy status of females with reproductive potential should be verified. Sexually active females of reproductive potential should have a negative pregnancy test before starting treatment with AUCATZYL.
Contraception
See the prescribing information for fludarabine and cyclophosphamide for information on the need for effective contraception in patients who receive lymphodepleting chemotherapy treatment.
There are insufficient exposure data to provide a recommendation concerning duration of contraception following treatment with AUCATZYL.
-
10 OVERDOSAGE
In FELIX study (all cohorts N=127), occurrences of overdose were observed at the administration of the first dose in 4% (5/127) of patients. All 5 patients had bone marrow blasts > 20% and should have received a first dose of 10 × 106 CAR-positive viable T cells but instead received a higher dose between 68 and 103 × 106 CAR-positive viable T cells. CRS, ICANS and HLH, including severe events, were observed in patients who received overdose of AUCATZYL.
In the event of a suspected overdose, closely monitor patients for any adverse reactions and administer treatment according to institutional practice and treatment guidelines.
-
11 DESCRIPTION
AUCATZYL (obecabtagene autoleucel) is a CD19-directed genetically modified autologous Tcell immunotherapy comprised of the patient's T cells that are transduced with a lentiviral vector to express an anti-CD19 chimeric antigen receptor (CAR). The CAR is composed of a murine anti-CD19 single chain variable fragment (scFv) linked to 4-1BB and CD3-zeta co-stimulatory domains.
AUCATZYL is prepared from the patient's own peripheral blood mononuclear cells, which are collected via a standard leukapheresis procedure. The mononuclear cells are enriched for T cells, activated and transduced with a replication-incompetent lentiviral vector containing the CD19 CAR transgene. The transduced T cells are expanded in cell culture, washed, formulated into a suspension, and then cryopreserved. AUCATZYL is frozen in patient-specific infusion bag(s) and thawed prior to infusion [see Dosage and Administration (2.3), How Supplied/Storage and Handling (16)]. The product must pass a sterility test before it is released to the treatment center. The thawed product is a colorless to pale yellow, very opalescent suspension that is essentially free from visible foreign particles.
In addition to T cells, AUCATZYL also contains non-transduced autologous T cells and non-T cells. The formulation contains phosphate-buffered saline (PBS) human serum albumin (HSA), ethylenediaminetetraacetic acid (EDTA) and 7.5% DMSO.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
AUCATZYL is a CD19-directed genetically modified autologous T cell immunotherapy consisting of the patient's own T cells expressing an anti-CD19 CAR. Engagement of anti-CD19 CAR-positive T cells with CD19 expressed on target cells, such as cancer cells and normal B cells, leads to activation of the anti-CD19 CAR-positive T cells and downstream signaling through the CD3-zeta domain. Proliferation and persistence by the anti-CD19 CAR-positive T cells following activation are enhanced by the presence of the 4-1BB co-stimulatory domain. This binding to CD19 results in anti-tumor activity and killing of CD19-expressing target cells.
12.2 Pharmacodynamics
Serum levels of cytokines such as IL-2, IL-5, IL-6, IL-7, IL-8, IL-10, IL-15, TNF-α, IFN-γ, and granulocyte-macrophage colony-stimulating factors were evaluated pre- and post-AUCATZYL infusion, over 3 months. Peak elevation of plasma cytokines was observed within the first month after infusion and levels returned to baseline by Month 3.
Due to the on-target effect of AUCATZYL, a period of B cell aplasia is expected. B cell aplasia was observed in 93.1% of patients at 3 months and 80.0% at 6 months.
12.3 Pharmacokinetics
The pharmacokinetics (PK) of AUCATZYL were assessed in 90 patients with relapsed or refractory CD19+ B-ALL receiving a median dose of 410 × 106 CD19 CAR-positive viable T cells (range: 10 to 480 × 106 CD19 CAR-positive viable T cells).
Following Day 1 infusion, levels of the AUCATZYL transgene in peripheral blood exhibited an initial rapid expansion. The median time of maximal expansion to peak (Tmax) occurred at Day 14 (range: Day 2-55), demonstrated by a geometric mean peak CAR T concentration (Cmax) of 115,193 copies/µg genomic DNA (gDNA; range: 129-600,000) and a geometric mean area under the curve between Days 0 and 28 (AUC0-28d) of 1,147,631 day*copies/μg DNA (range: 17,900-7,230,000 day*copies/μg DNA). A higher expansion was observed in patients with bone marrow blasts > 20% compared to patients with bone marrow blast ≤ 20%.
Table 5: Summary of Pharmacokinetics Parameters for Transgene Levels by ddPCR in Peripheral Blood by Dose Regimen Received Parameter Statistics Bone Marrow Blast * > 20% (N=59) Bone Marrow Blast † ≤ 20% (N=31) Total
(N=90)AUC0-28d=area under the concentration-time curve (exposure) from Day 0 to Day 28; Cmax = maximum serum concentration; ddPCR = droplet digital polymerase chain reaction; DNA = deoxyribonucleic acid; Geo-CV% = geometric mean coefficient of variation; Tmax = time to maximum concentration. - * Bone Marrow Blast > 20% = dosage regimen of 10 × 106 then 400 × 106 CD19 CAR-positive viable T cells.
- † Bone Marrow Blast ≤ 20% = dosage regimen 100 × 106 then 310 × 106 CD19 CAR-positive viable T cells.
Cmax (copies/µg DNA) n 59 31 90 Geometric Mean 146,314 73,074 115,193 (Geo-CV%) (294.4) (186.9) (267.0) Min–Max 129–600,000 9290–589,000 129–600,000 Tmax (days) n 59 31 90 Median 20 11 14 Min–Max 6–55 2–28 2–55 AUC0-28d (day*copies/µg DNA) n 52 29 81 Geometric Mean 1,521,310 692,307 1,147,631 (Geo-CV%) (191.3) (226.8) (219.5) Min–Max 17,900–6,730,000 70,400–7,230,000 17,900–7,230,000 No substantial differences in AUCATZYL expansion were observed between responding (CR/CRi) and non-responding (non-CR/CRi) patients. Furthermore, 75.9% (22/29) of patients who had ongoing remission had ongoing CAR T persistency at the last laboratory assessment, with a maximum observed persistency of 36.5 months.
Patients who received a first split dose of 10 × 106 cells (> 20% blast) demonstrated a higher expansion of CAR T cells (Cmax and AUC0-28d) compared to patients who received a first split dose of 100 × 106 cells (≤ 20% blast). Persistency was not impacted by tumor burden.
Patients who experience CRS had 1.8-fold higher mean bone marrow blast percentage and higher CAR T cell expansion (5.0-fold higher Cmax and 6.8-fold higher AUC0-28d [geometric mean]) compared to patients without CRS. Patients who experience ICANS had 1.8-fold higher mean bone marrow blast percentage and higher CAR T cell expansion (3.3-fold higher Cmax and 2.9-fold higher AUC0-28d [geometric mean]) compared to patients without ICANS.
12.6 Immunogenicity
The observed incidence of anti-drug antibodies is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of anti-drug antibodies in the studies described below with the incidence of anti-drug antibodies in other studies, including those of AUCATZYL or of other similar products.
The humoral immunogenicity of AUCATZYL was measured using an assay for the detection of anti-drug antibodies against AUCATZYL. In the FELIX study, 8.7% (11/127) of patients tested positive for anti-CD19 CAR antibodies pre-infusion. Treatment induced anti-CD19 CAR antibodies were detected in 1.6% (2/127) of patients.
The cellular immunogenicity of AUCATZYL was measured using an assay for the detection of T cell responses, measured by the production of interferon gamma (IFNγ) to the full length anti-CD19 CAR. Four percent (3/75) of patients tested positive in the cellular immunogenicity readout (IFNγ) post infusion.
There was no identified clinically significant effect of humoral and cellular immunogenicity on pharmacokinetics, pharmacodynamics, safety, or effectiveness of AUCATZYL.
- 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
The efficacy of AUCATZYL was evaluated in an open-label, multi-center, single-arm study (FELIX study; NCT04404660). The study enrolled patients with relapsed or refractory B-cell acute lymphoblastic leukemia (ALL). Eligible patients were adults with refractory ALL, first relapse following a remission lasting ≤ 12 months, relapsed or refractory ALL after two or more prior lines of systemic therapy, or relapsed or refractory ALL at least greater than 3 months after allogeneic stem cell transplantation (SCT) and had disease burden of ≥ 5% blasts in bone marrow at screening. The study excluded patients with isolated extramedullary disease, active or serious infections requiring systemic antimicrobials, active graft versus host disease, history or presence of central nervous system (CNS) disorders. Treatment was administered in the in-patient setting and consisted of lymphodepleting chemotherapy (fludarabine 30 mg/m2 IV daily for 4 days; cyclophosphamide 500 mg/m2 IV daily for 2 days starting with first dose of fludarabine) followed by AUCATZYL as a split dose infusion with a total recommended dose of 410 × 106 CD19 CAR-positive viable T cells.
A total of 112 patients were enrolled and underwent leukapheresis; 18 (16%) of whom discontinued without receiving AUCATZYL infusion due to the following: death (n=11), adverse event (n=1), physician decision (n=1), and manufacturing failure (n=5). Among the remaining 94 patients who received at least one infusion of AUCATZYL, 65 patients had ≥ 5% blasts in the bone marrow after screening and prior to the start of the lymphodepletion therapy, and received a conforming product, qualifying them as efficacy-evaluable patients.
The population characteristics of efficacy-evaluable patients were as follows: median age was 51 years (range: 20 to 77 years) with 7 patients (11%) ≤ 25 years of age and 14 patients (22%) ≥ 65 years of age, 35 patients (54%) were female, 47 patients (72%) were White, 8 patients (12%) were Asian and 1 patient (2%) was Black or African American. Twenty-one patients (32%) were of Hispanic or Latino ethnicity.
At enrollment, 35 patients (54%) were refractory to the last prior line of therapy, and 32 patients (49%) relapsed to first-line therapy within 12 months. The median number of prior lines of therapy was 2 (range: 1 to 6). Thirty-five patients (54%) received either blinatumomab or inotuzumab ozogamicin and 10 patients (15%) received both blinatumomab and inotuzumab ozogamicin, 22 (34%) patients received prior SCT therapy, 17 (26%) patients had Ph+ ALL and 13 (20%) patients had extramedullary disease. Fifty-nine patients (91%) received bridging therapy between leukapheresis and lymphodepleting chemotherapy.
The median dose was 410 × 106 CD19 CAR-positive viable T cells (range: 10 to 418 × 106 CD19 CAR-positive viable T cells). Fifty-eight patients (89%) received the target dose of 410 × 106 CD19 CAR-positive viable T cells (± 25%). Five patients (8%) only received the first dose, primarily due to adverse events (5%). The median time from leukapheresis to product release was 20 days (range: 17 to 23 days) and the median time from leukapheresis to AUCATZYL infusion was 35 days (range: 26 to 74 days).
The major efficacy outcome measures were rate and duration of complete remission within 3 months after infusion. Additional outcome measures were rate and duration of overall complete remission which includes complete remission and complete remission with incomplete hematologic recovery, at any time. The efficacy results are summarized in Table 6 below.
Table 6: Efficacy Results for FELIX Study Endpoint Efficacy-Evaluable
N=65
n (%)All Leukapheresed
N=112
n (%)CI=confidence interval; NR=not reached. - * Rate of Overall Complete Remission "At Anytime" includes Complete Remission and Complete Remission with incomplete hematologic recovery "At Anytime".
Complete Remission (within 3 months) rate n (%) 27 (42%) 40 (36%) [95% CI] [29%, 54%] (27%, 45%) Duration (months), median [95% CI] 14.1 [6.1, NR] 14.1 (6.2, NR) (Range in months) (0.5+, 21.2) (0.5+, 21.2) Overall Complete Remission (At Anytime) rate * n (%) 41 (63%) 60 (54%) [95% CI] [50%, 75%] [44%, 63%] Duration (months), median [95% CI] 14.1 [6.2, NR] 14.1 [8.1, NR] (Range in months) (0.03+, 21.2) (0.03+, 21.2) Among patients in the efficacy-evaluable population who achieved a best response of complete remission "At Anytime" (N=33; 51%), the median duration for remission was 14.1 months (95% confidence interval [CI]: 6.1, not reached [NR]). Among patients in the efficacy-evaluable population in whom best response was complete remission with incomplete hematologic recovery "At Anytime" (N=8; 12%), the median duration of remission was 10.5 months (95% CI: 1.8, NR).
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
AUCATZYL 410 × 106 CD19 CAR-positive viable T cells NDC (83047-410-04) is supplied in three to five infusion bags (see below) containing a frozen suspension of genetically modified autologous T cells in PBS, HSA, EDTA and 7.5% DMSO.
Each infusion bag of AUCATZYL is individually packed within an overwrap and then enclosed within a metal cassette. AUCATZYL is shipped from the manufacturing facility to the cellular therapy laboratory associated with the infusion center in a cryogenic shipper charged with liquid nitrogen. A Release for Infusion certificate is provided to the infusion site in the shipper and via the Autolus Scheduling Portal with the product.
Infusion bag configurations Color Code Fill Volume Range
(min – max)NDC Number 10 × 106 CD19 CAR-positive viable T cells in one 50 mL infusion bag Blue 10 mL 83047-010-10 100 × 106 CD19 CAR-positive viable T cells in one or more 50 mL infusion bags Orange 10 to 20 mL 83047-100-10 100 × 106 CD19 CAR-positive viable T cells in one 250 mL infusion bag Orange 30 to 70 mL 83047-100-30 300 × 106 CD19 CAR-positive viable T cells in one or more 250 mL infusion bags Red 30 to 70 mL 83047-300-30 - Match the identity of the patient with the patient identifiers on the infusion bag upon receipt [see Dosage and Administration (2.3)].
- Store AUCATZYL frozen in the vapor phase of liquid nitrogen (below minus 150°C) [see Dosage and Administration (Section 2.3)].
- Thaw AUCATZYL prior to infusion [see Dosage and Administration (2.3)].
- Do not re-freeze after thawing.
- Do not irradiate AUCATZYL, as this could lead to inactivation.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Discuss the following with the patient:
- Inform patients that there is a risk of manufacturing failure (4.5% [5/112 in clinical studies]). Therefore, a second manufacturing of AUCATZYL may be attempted, after a second leukapheresis collection.
- Inform patients that additional therapy (other than lymphodepletion) may be necessary before AUCATZYL manufacturing is completed. This may increase the risk of adverse events during the pre-infusion period, which could delay or prevent the administration of AUCATZYL.
- Advise patients to seek immediate attention if any of the following occur:
- Cytokine Release Syndrome: Inform patients that symptoms may include fever, hypotension and hypoxia [see Warnings and Precautions (5.1) and Adverse Reactions (6)].
- Neurologic Toxicity/ICANS: Inform patients that symptoms may include ICANS, headache, dizziness, anxiety, insomnia, delirium, tremor, and encephalopathy [see Warnings and Precautions (5.2) and Adverse Reactions (6)].
- Prolonged Cytopenias: Inform patients that symptoms may include neutropenia, anemia, thrombocytopenia, or bleeding [see Warnings and Precautions (5.3) and Adverse Reactions (6)].
- Severe Infections: Inform patients that they may exhibit signs or symptoms associated with infection, and that past infections can be reactivated following treatment with AUCATZYL [see Warnings and Precautions (5.4) and Adverse Reactions (6)].
- Secondary Malignancies: Secondary malignancies, including T cell malignancies, have occurred following treatment with BCMA- and CD19-directed genetically modified autologous T cell immunotherapies [see Boxed Warning, Warnings and Precautions (5.8), Adverse Reactions (6)].
Advise patients of the need to:
- Avoid driving for at least 2 weeks after each infusion.
- Have periodic monitoring of blood counts.
- Contact Autolus Inc at 1-855-288-5227 if they are diagnosed with a secondary malignancy [see Warnings and Precautions (5.8)].
-
MEDICATION GUIDE
MEDICATION GUIDE
AUCATZYL® [pronounced aw-kat-zil]
(obecabtagene autoleucel)Read this Medication Guide before you start your AUCATZYL treatment. The more you know about your treatment, the more active you can be in your care. Talk with your healthcare provider if you have questions about your health condition or treatment. Reading this Medication Guide does not take the place of talking with your healthcare provider about your treatment. What is the most important information I should know about AUCATZYL?
AUCATZYL may cause side effects that are life-threatening and can lead to death. Call or see your healthcare provider or get emergency help right away if you get any of the following:- Fever (100.4°F/38°C or higher)
- Severe nausea, vomiting, diarrhea
- Severe headache
- Dizziness or light-headedness
- Difficulty breathing
- Confusion
- Fast or irregular heartbeat
- Low blood pressure
- Chills/shivering
- Shaking or twitching (tremor)
What is AUCATZYL?
AUCATZYL is a treatment for adults with acute lymphoblastic leukemia. It is used following disease progression while on or after other treatment. AUCATZYL is a medicine made from your own white blood cells, which have been changed (genetically modified) to recognize and attack your leukemic cells.Before getting AUCATZYL, tell your healthcare provider about all of your medical problems, including if you have or have had: - Neurologic problems (such as seizures, stroke, new or worsening memory loss)
- Lung or breathing problems
- Heart problems
- A recent or active infection
- Past infections which can be reactivated following treatment with AUCATZYL
- Pregnancy, you think you may be pregnant, or plan to become pregnant
- Breastfeeding
How will I receive AUCATZYL? - AUCATZYL is made from your own white blood cells, so your blood will be collected by a process called "leukapheresis" (loo-kah-fur-ee-sis), which will concentrate your white blood cells.
- Your blood cells will be sent to a manufacturing center to make your AUCATZYL.
- While waiting for AUCATZYL to be made, you may get other medicines to stabilize your cancer. This is so that your acute lymphoblastic leukemia does not get worse.
- Within 7 days before you start treatment, a sample of your cells will be taken to confirm your disease burden, this will determine which infusion dose you are given first.
- Your infusion dose will be tailored to the burden of your disease. This will be provided as two separate infusions.
- Before you receive AUCATZYL, your healthcare provider will give you chemotherapy for a few days to make room in the bone marrow.
- When your AUCATZYL is ready, your healthcare provider will give it to you through a catheter (tube) placed into your vein (intravenous infusion).
- After you receive your AUCATZYL first infusion you will receive your second infusion 10 days (± 2 days) later.
- 30 minutes before you are given AUCATZYL, you may be given medicines for fever (such as acetaminophen).
- After AUCATZYL infusion, you will be monitored daily for at least 7 days after the infusion so that your healthcare team can closely monitor your recovery.
- You should plan to stay close to a healthcare facility for at least 2 weeks after getting AUCATZYL. Your healthcare provider will help you with any side effects that may occur.
- You may be hospitalized for side effects. Your healthcare provider will determine when you can go home.
- Your healthcare provider will want to do blood tests to follow your progress. It is important that you do have your blood tested. If you miss an appointment, call your healthcare provider as soon as possible to reschedule.
What should I avoid after receiving AUCATZYL? - Avoid driving for at least 2 weeks after you get AUCATZYL.
- Do not donate blood, organs, tissues, or cells for transplantation.
What are the possible side effects of AUCATZYL?
The most common side effects of AUCATZYL include:- Fever (100.4°F/38°C or higher)
- Nausea
- Diarrhea
- Infections
- Headache
- Muscle or joint pain
- Fatigue or feeling very tired
- Low blood pressure (dizziness or light-headedness, headache, fatigue, short of breath)
- Fast irregular heartbeat
- Confusion
- Difficulty speaking or slurred speech
- Low white blood cells (can occur with a fever)
- Bleeding
These are not all the side effects of AUCATZYL. Call your healthcare provider about any side effects that concern you. You may report side effects to FDA at 1-800-FDA-1088.General information about the safe and effective use of AUCATZYL.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide.
If you would like more information about AUCATZYL, talk with your healthcare provider. You can ask your healthcare provider for information about AUCATZYL that is written for health professionals. You can get additional information by contacting Autolus Inc at 1-855-288-5227 or at www.AUCATZYL.comWhat are the ingredients in AUCATZYL?
Active ingredients: obecabtagene autoleucel
Inactive ingredients: albumin (human); DMSOManufactured by: Autolus Limited, Marshgate, Stevenage, SG1 1FR, United Kingdom.
Manufactured for: Autolus Inc., Gaithersburg, MD, 20877
US License No 2339
AUCATZYL is a registered trademark of Autolus Limited.
© 2026 Autolus Limited. All Rights Reserved.This Medication Guide has been approved by the U.S. Food and Drug Administration.
Issued: 02/2026 -
PRINCIPAL DISPLAY PANEL - 10 mL Infusion Bag Label - 10 x 10
10x106 bag configuration
EXTRACT SPECIFIED VOLUME VIA SYRINGE
obecabtagene autoleucel
AUCATZYL®
FOR AUTOLOGOUS & INTRAVENOUS USE ONLY.
Dosage: See prescribing information and release for
infusion certificate. Discard unused portion.Contains: Up to 100x106 CD19 CAR-positive viable
T cells in 10mL suspension containing 7.5% DMSO USP.DO NOT USE A
LEUKODEPLETING FILTER
OR IRRADIATE.Storage: Ship and store
in vapor phase of liquid
nitrogen ≤ -150°C.Not evaluated for infectious substances.
Rx Only
US License 2339
A1001-01Autolus
Mfd by: Autolus Ltd, Stevenage, SG1 1FR, UK
Mfd for: Autolus Inc., Gaithersburg, MD, 20877
Phone: 1-855-288-5227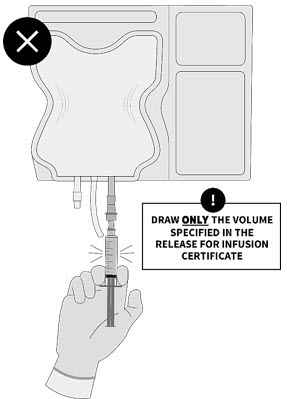
-
PRINCIPAL DISPLAY PANEL - 10 mL to 20 mL Infusion Bag Label - 100 x 10
100x106 bag configuration
obecabtagene autoleucel
AUCATZYL®
FOR AUTOLOGOUS & INTRAVENOUS USE ONLY.
Dosage: See prescribing information and the release for
infusion certificate.Contains: 100x106 CD19 CAR-positive viable T cells in
10mL to 20mL suspension containing 7.5% DMSO USP.Dose may be suspended in 1 or more infusion bag(s).
DO NOT USE A
LEUKODEPLETING FILTER
OR IRRADIATE.Storage: Ship and store
in vapor phase of liquid
nitrogen ≤ -150°C.Not evaluated for infectious substances.
Rx Only
US License 2339
D1001-01Autolus
Mfd by: Autolus Ltd, Stevenage, SG1 1FR, UK
Mfd for: Autolus Inc., Gaithersburg, MD, 20877
Phone: 1-855-288-5227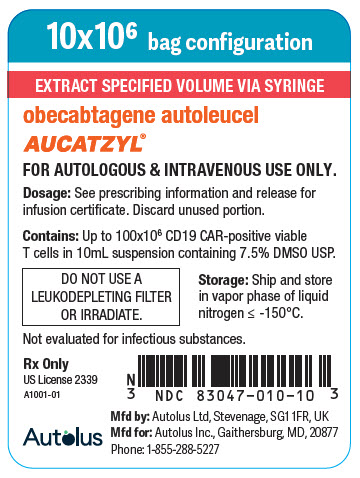
-
PRINCIPAL DISPLAY PANEL - 30 mL to 70 mL Infusion Bag Label - 100 x 10
100x106 bag configuration
obecabtagene autoleucel
AUCATZYL®
FOR AUTOLOGOUS & INTRAVENOUS USE ONLY.
Dosage: See prescribing information and the release for
infusion certificate.Contains: 100x106 CD19 CAR-positive viable T cells in
30mL to 70mL suspension containing 7.5% DMSO USP.DO NOT USE A
LEUKODEPLETING FILTER
OR IRRADIATE.Storage: Ship and store
in vapor phase of liquid
nitrogen ≤ -150°C.Not evaluated for infectious substances.
Rx Only
US License 2339
B1001-01Autolus
Mfd by: Autolus Ltd, Stevenage, SG1 1FR, UK
Mfd for: Autolus Inc., Gaithersburg, MD, 20877
Phone: 1-855-288-5227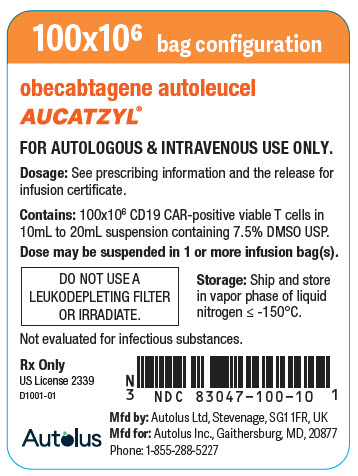
-
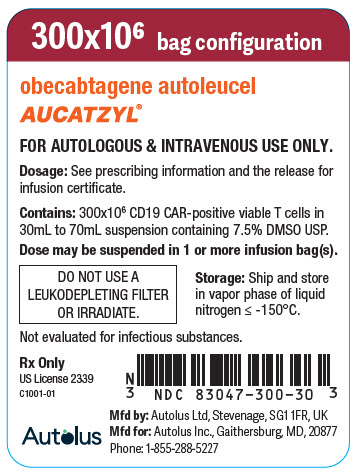
PRINCIPAL DISPLAY PANEL - 30 mL to 70 mL Infusion Bag Label - 300 x 10
300x106 bag configuration
obecabtagene autoleucel
AUCATZYL®
FOR AUTOLOGOUS & INTRAVENOUS USE ONLY.
Dosage: See prescribing information and the release for
infusion certificate.Contains: 300x106 CD19 CAR-positive viable T cells in
30mL to 70mL suspension containing 7.5% DMSO USP.Dose may be suspended in 1 or more infusion bag(s).
DO NOT USE A
LEUKODEPLETING FILTER
OR IRRADIATE.Storage: Ship and store
in vapor phase of liquid
nitrogen ≤ -150°C.Not evaluated for infectious substances.
Rx Only
US License 2339
C1001-01Autolus
Mfd by: Autolus Ltd, Stevenage, SG1 1FR, UK
Mfd for: Autolus Inc., Gaithersburg, MD, 20877
Phone: 1-855-288-5227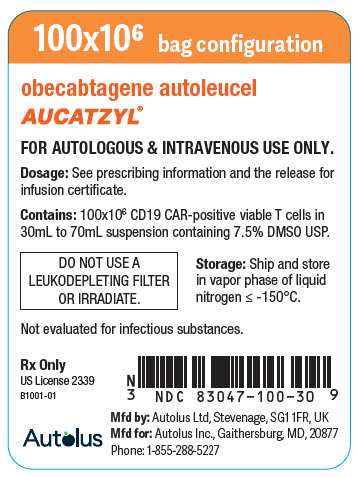
- PRINCIPAL DISPLAY PANEL - Patient Information Label
-
PRINCIPAL DISPLAY PANEL - Kit Label
obecabtagene autoleucel
AUCATZYL®FOR AUTOLOGOUS & INTRAVENOUS USE ONLY.
Dose: 410 x 106 CD19 CAR-positive viable T cells
Dosage: See prescribing information and the release for infusion certificate.
Contains: AUCATZYL is a frozen cell suspension containing 7.5% DMSO.
Supplied in three to five infusion bag(s) in one or two packs.Ship and store in vapor phase of liquid nitrogen ≤ -150°C.
Upon receipt, immediately transfer to a vapor phase liquid nitrogen
environment (≤ -150°C). Do not refreeze.DO NOT USE A LEUKODEPLETING FILTER OR IRRADIATE.
Rx Only
KIT NDC: 83047-410-04
Lot/COI ID :
Aph ID :
Expiry : DD-MMM-YYYY
1/X Pack
Autolus
M3001-01
Manufactured by Autolus Ltd, Stevenage, SG1 1FR, UK
Manufactured for Autolus Inc., Gaithersburg, MD, 20877
Phone: 1-855-288-5227
US License 2339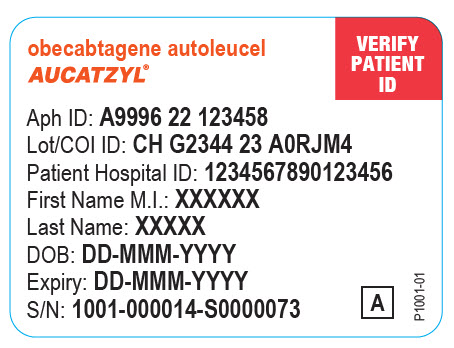
-
INGREDIENTS AND APPEARANCE
AUCATZYL
obecabtagene autoleucel kitProduct Information Product Type CELLULAR THERAPY Item Code (Source) NDC: 83047-410 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 83047-410-04 1 in 1 PACKAGE Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 BAG 1 Part 2 1 BAG 1 Part 3 1 BAG 1 Part 1 of 3 AUCATZYL
obecabtagene autoleucel suspensionProduct Information Item Code (Source) NDC: 83047-010 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Obecabtagene autoleucel (UNII: 760HJB0YRD) (Obecabtagene autoleucel - UNII:760HJB0YRD) Obecabtagene autoleucel 10000000 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 83047-010-10 1 in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125813 11/08/2024 Part 2 of 3 AUCATZYL
obecabtagene autoleucel suspensionProduct Information Item Code (Source) NDC: 83047-100 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Obecabtagene autoleucel (UNII: 760HJB0YRD) (Obecabtagene autoleucel - UNII:760HJB0YRD) Obecabtagene autoleucel 100000000 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 83047-100-10 1 in 1 BAG; Type 0: Not a Combination Product 2 NDC: 83047-100-30 1 in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125813 11/08/2024 Part 3 of 3 AUCATZYL
obecabtagene autoleucel suspensionProduct Information Item Code (Source) NDC: 83047-300 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Obecabtagene autoleucel (UNII: 760HJB0YRD) (Obecabtagene autoleucel - UNII:760HJB0YRD) Obecabtagene autoleucel 300000000 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 83047-300-30 1 in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125813 11/08/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125813 11/08/2024 Labeler - Autolus Inc. (118249238) Establishment Name Address ID/FEI Business Operations Autolus Limited 229442484 MANUFACTURE(83047-410) , ANALYSIS(83047-410) , LABEL(83047-410) , PACK(83047-410)
Trademark Results [AUCATZYL]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 AUCATZYL 79370753 not registered Live/Pending |
Autolus Limited 2023-04-27 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.