These highlights do not include all the information needed to use VANCOMYCIN INJECTION safely and effectively. See full prescribing information for VANCOMYCIN INJECTION. VANCOMYCIN injection, for intravenous use or oral use Initial U.S. Approval: 1958
Vancomycin by
Drug Labeling and Warnings
Vancomycin by is a Prescription medication manufactured, distributed, or labeled by Xellia Pharmaceuticals USA LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
VANCOMYCIN- vancomycin injection, solution
Xellia Pharmaceuticals USA LLC
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use VANCOMYCIN INJECTION safely and effectively. See full prescribing information for VANCOMYCIN INJECTION.
VANCOMYCIN injection, for intravenous use or oral use Initial U.S. Approval: 1958 WARNING: POTENTIAL RISK OF EXPOSURE TO EXCIPIENT DURING THE FIRST OR SECOND TRIMESTER OF PREGNANCYSee full prescribing information for complete boxed warning.If use of vancomycin is needed during the first or second trimester of pregnancy, use other available formulations of vancomycin. This formulation of Vancomycin Injection contains the excipient polyethylene glycol (PEG 400), which resulted in fetal malformations in animal reproduction studies. (5.1, 8.1) INDICATIONS AND USAGEVancomycin Injection is a glycopeptide antibacterial indicated in adult and pediatric patients less than 18 years of age as follows:
Limitations of Use (1.8):
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Vancomycin Injection and other antibacterial drugs, Vancomycin Injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. (1.9) DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSVancomycin Injection 5 g/100 mL (50 mg/mL): Pharmacy Bulk Package bottle containing 5 g vancomycin in 100 mL (3) CONTRAINDICATIONSHypersensitivity to vancomycin (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSThe common adverse reactions following intravenously, and orally administered vancomycin were acute kidney injury, hearing loss, neutropenia, anaphylaxis, vancomycin infusion reaction. (6.1) The most common adverse reactions following orally administered vancomycin (≥ 10%) were nausea, abdominal pain, and hypokalemia (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Xellia Pharmaceuticals USA, LLC at 1-833-295-6953 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION. Revised: 8/2021 |
FULL PRESCRIBING INFORMATION
WARNING: POTENTIAL RISK OF EXPOSURE TO EXCIPIENT DURING THE FIRST OR SECOND TRIMESTER OF PREGNANCY
If use of vancomycin is needed during the first or second trimester of pregnancy, use other available formulations of vancomycin. This formulation of Vancomycin Injection contains the excipient polyethylene glycol (PEG 400) which resulted in fetal malformations in animal reproduction studies [see Warnings and Precautions (5.1) and Use in Specific Populations (8.1)].
1 INDICATIONS AND USAGE
1.1 Septicemia
Vancomycin Injection administered intravenously is indicated in adults and pediatric patients less than 18 years of age for the treatment of septicemia due to:
- Susceptible isolates of methicillin-resistant Staphylococcus aureus (MRSA) and coagulase negative staphylococci.
- Methicillin-susceptible staphylococci in penicillin-allergic patients, or those patients who cannot receive or who have failed to respond to other drugs, including penicillins or cephalosporins.
1.2 Infective Endocarditis
Vancomycin Injection administered intravenously is indicated in adults and pediatric patients less than 18 years of age for the treatment of infective endocarditis due to:
- Susceptible isolates of MRSA.
- Viridans group streptococci Streptococcus gallolyticus (previously known as Streptococcus bovis), Enterococcus species and Corynebacterium species. For enterococcal endocarditis, use Vancomycin Injection in combination with an aminoglycoside.
- Methicillin-susceptible staphylococci in penicillin-allergic patients, or those patients who cannot receive or who have failed to respond to other drugs, including penicillins or cephalosporins.
Vancomycin Injection administered intravenously is indicated in adults and pediatric patients for the treatment of early-onset prosthetic valve endocarditis caused by Staphylococcus epidermidis in combination with rifampin and an aminoglycoside.
1.3 Skin and Skin Structure Infections
Vancomycin Injection administered intravenously is indicated in adults and pediatric patients less than 18 years of age for the treatment of skin and skin structure infections due to:
- Susceptible isolates of MRSA and coagulase negative staphylococci.
- Methicillin-susceptible staphylococci in penicillin-allergic patients, or those patients who cannot receive or who have failed to respond to other drugs, including penicillins or cephalosporins.
1.4 Bone Infections
Vancomycin Injection administered intravenously is indicated in adults and pediatric patients less than 18 years of age for the treatment of bone infections due to:
- Susceptible isolates of MRSA and coagulase negative staphylococci.
- Methicillin-susceptible staphylococci in penicillin-allergic patients, or those patients who cannot receive or who have failed to respond to other drugs, including penicillins or cephalosporins.
1.5 Lower Respiratory Tract Infections
Vancomycin Injection administered intravenously is indicated in adults and pediatric patients less than 18 years of age for the treatment of lower respiratory tract infections due to:
- Susceptible isolates of MRSA
- Methicillin-susceptible staphylococci in penicillin-allergic patients, or those patients who cannot receive or who have failed to respond to other drugs, including penicillins or cephalosporins.
1.6 Clostridioides difficile-Associated Diarrhea
Vancomycin Injection administered orally is indicated for the treatment of C. difficile-associated diarrhea (CDAD) in adult and pediatric patients less than 18 years of age.
1.7 Enterocolitis Caused by S. aureus (including methicillin-resistant strains)
Vancomycin Injection administered orally is indicated for the treatment of enterocolitis caused by susceptible isolates of Staphylococcus aureus in adults and pediatric patients less than 18 years of age.
1.8 Limitations of Use
Vancomycin Injection administered intravenously is not approved for the treatment of the following conditions because it is not effective:
- C. difficile-associated diarrhea
- Enterocolitis caused by susceptible isolates of Staphylococcus aureus
Vancomycin Injection administered orally is not approved for the treatment of the following conditions because it is not effective:
- Septicemia due to susceptible isolates of MRSA or methicillin-susceptible staphylococci
- Infective endocarditis due to susceptible isolates of MRSA, methicillin-susceptible staphylococci, Viridans group streptococci Streptococcus gallolyticus, Enterococcus species and Corynebacterium species, or for the treatment of early-onset prosthetic valve endocarditis caused by Staphylococcus epidermidis in combination with rifampin and an aminoglycoside
- Skin and skin structure infections due to susceptible isolates of MRSA and methicillin- susceptible staphylococci
- Bone infections due to susceptible isolates of MRSA and lower respiratory tract infections due to susceptible isolates of MRSA and methicillin-susceptible staphylococci
1.9 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Vancomycin Injection and other antibacterial drugs, Vancomycin Injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions for Intravenous and Oral Use
- Obtain a pregnancy test in females of reproductive potential prior to initiating treatment with Vancomycin Injection [see Warnings and Precautions (5.1), and Use in Specific Populations (8.1, 8.3)].
- Vancomycin Injection is supplied in pharmacy bulk packages. A pharmacy bulk package is a sterile dosage form containing many single doses. The contents of Vancomycin Injection pharmacy bulk package are intended for use by a pharmacy admixture service for addition to suitable parenteral fluids in the preparation of admixtures for intravenous infusion. The Pharmacy Bulk Package is NOT for direct infusion. Further dilution is required before use [see Dosage and Administration (2.5)].
- To reduce the risk of infusion related adverse reactions, administer diluted Vancomycin Injection by intravenous infusion over 60 minutes or greater [see Warnings and Precautions (5.6) and Adverse Reactions (6.1)].
- Diluted Vancomycin Injection concentrations of no more than 5 mg/mL are recommended in adults [see Dosage and Administration (2.2)]. See also age-specific recommendations [see Dosage and Administration (2.2, 2.3)]. In selected patients in need of fluid restriction, a concentration up to 10 mg/mL may be used. Infusion related events may occur, however, at any rate or concentration [see Warnings and Precautions (5.6)].
- Other drugs should not be added to the Vancomycin Injection Pharmacy Bulk Package or the diluted Vancomycin Injection [see Dosage and Administration (2.6)].
- Administer diluted Vancomycin Injection prior to intravenous anesthetic agents to reduce the risk of infusion related adverse reactions [see Warnings and Precautions (5.6)].
- Administer diluted Vancomycin Injection by a secure intravenous route of administration to avoid local irritation and phlebitis reactions [see Warnings and Precautions (5.7)].
2.2 Intravenous Dosage in Adult and Pediatric Patients with Normal Renal Function
Dosage in Adult Patients
The usual daily intravenous dose is 2 g divided either as 500 mg every 6 hours or 1 g every 12 hours. Administer each dose by intravenous infusion over a period of 60 minutes or greater. Other patient factors, such as age or obesity, may call for modification of the usual intravenous daily dose.
Dosage in Pediatric Patients Aged 1 Month and Older
The usual intravenous dosage of vancomycin is 10 mg/kg per dose given every 6 hours. Each dose should be administered over a period of at least 60 minutes. Close monitoring of serum concentrations of vancomycin may be warranted in these patients.
Dosage in Pediatric Patients Younger than 1 Month of Age
In pediatric patients up to the age of 1 month, the total daily intravenous dosage may be lower. In neonates, an initial dose of 15 mg/kg is suggested, followed by 10 mg/kg every 12 hours for neonates in the 1st week of life and every 8 hours thereafter up to the age of 1 month. Each dose should be administered over 60 minutes. In premature infants, vancomycin clearance decreases as postconceptional age decreases. Therefore, longer dosing intervals may be necessary in premature infants. Close monitoring of serum concentrations of vancomycin is recommended in these patients.
2.3 Orally Administered Dosage in Adult and Pediatric Patients
2.4 Intravenous Dosage in Patients with Renal Impairment
Dosage adjustment must be made in adult and pediatric patients with renal impairment. The initial dose should be no less than 15 mg/kg in adult patients with any degree of renal impairment.
In premature infants and the elderly, greater dosage reductions than expected may be necessary because of decreased renal function. Measure trough vancomycin serum concentrations to guide therapy, especially in seriously ill patients with changing renal function.
For functionally anephric patients, an initial dose of 15 mg/kg of body weight should be given to achieve a prompt therapeutic serum concentration. A dose of 1.9 mg/kg/24 h should be given after the initial dose of 15 mg/kg.
2.5 Directions for the Preparation, Dilution and Storage of the Pharmacy Bulk Package for Intravenous Use
Preparation
- Vancomycin Injection pharmacy bulk package is not for direct intravenous infusion. Prior to intravenous administration, contents of the Vancomycin Injection pharmacy bulk package must be further diluted.
- Prepare Vancomycin Injection pharmacy bulk package for use in a pharmacy admixture service only in a suitable work area, such as a laminar flow hood. They should be hung by the integral hanger provided and suspended as a unit in the laminar flow hood.
- Using aseptic technique, penetrate the container closure only one time utilizing a suitable sterile dispensing set or transfer device which allows measured dispensing of the contents.
- Use of a syringe and needle is not recommended as it may cause leakage. Swab bottle stopper with an antiseptic solution prior to inserting the dispensing set into the bottle using aseptic technique.
- Once the sterile dispensing set has been inserted into the container, withdrawal of the contents from the Vancomycin Injection pharmacy bulk package should be accomplished without delay immediately. However, if this is not possible, a maximum time of 4 hours from the initial closure entry may be permitted to complete fluid transfer operations.
- Discard any unused portion in the container no later than 4 hours after the container closure has been penetrated.
Dilution and Storage
- Vancomycin Injection solution in the pharmacy bulk package contains vancomycin equivalent to 5 g/100 mL (50 mg/mL). After withdrawing the contents of the Vancomycin Injection Pharmacy Bulk Package, further dilution is required using one of the compatible intravenous diluents listed below [see Dosage and Administration (2.6)], prior to intravenous administration.
- For doses of 500 mg, 10 mL of solution of Vancomycin Injection must be further diluted in at least 100 mL of a suitable infusion solution.
- For doses of 1 gram (20 mL), at least 250 mL of solution must be used.
- The desired dose diluted in this manner should be administered by intravenous infusion over a period of at least 60 minutes [see Dosage and Administration (2.2)]
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- The diluted solutions may be stored in a refrigerator for 14 days or at 25°C for up to 7 days.
2.6 Compatibility with Intravenous Fluids for Intravenous Use
The following diluents are physically and chemically compatible with up to 5 g/L of vancomycin:
5% Dextrose Injection, USP
5% Dextrose Injection and 0.9% Sodium Chloride Injection, USP
Lactated Ringer's Injection, USP
5% Dextrose and Lactated Ringer's Injection, USP
0.9 % Sodium Chloride Injection, USP
2.7 Incompatibilities for Intravenous Use
Vancomycin Injection solution has a low pH and may cause chemical or physical instability when it is mixed with other compounds.
Mixtures of solutions of vancomycin and beta-lactam antibacterial drugs have been shown to be physically incompatible. The likelihood of precipitation increases with higher concentrations of vancomycin. It is recommended to adequately flush the intravenous lines between the administration of these antibacterial drugs. It is also recommended to dilute solutions of vancomycin to 5 mg/mL or less.
2.8 Preparation of Vancomycin Injection Pharmacy Bulk Package for Oral Administration
The appropriate oral dose [see Dosage and Administration (2.3)] may be taken undiluted or may be diluted in 30 mL (1 oz) of water and given to the patient to drink. SyrSpend PH4 cherry flavored syrup may be added to the solution to improve the taste for oral administration. Only the diluted solution may be administered via a nasogastric tube.
Discard the diluted solution after 24 hours if stored at room temperature and 14 days if stored refrigerated.
3 DOSAGE FORMS AND STRENGTHS
Vancomycin Injection, 5 g/100 mL (50 mg/mL), in a Pharmacy Bulk Package bottle is sterile, nonpyrogenic 100 mL clear, colorless to light yellow or light brown solution containing 5 g vancomycin.
4 CONTRAINDICATIONS
Vancomycin Injection is contraindicated in patients with known hypersensitivity to vancomycin.
5 WARNINGS AND PRECAUTIONS
5.1 Potential Risk of Exposure to Excipient During the First or Second Trimester of Pregnancy
If use of vancomycin is needed during the first or second trimester of pregnancy, use other available formulations of vancomycin. This formulation of Vancomycin Injection contains the excipient polyethylene glycol (PEG 400) which caused fetal malformations in animal reproduction studies. In a rabbit reproduction study, fetal spinal malformations occurred when the excipient PEG 400 was administered intravenously at dose exposures approximately 13 times the exposure at the maximum daily human dose. Based on uncertainty with the oral bioavailability of PEG 400, the potential adverse developmental effect of PEG 400 with oral administration is unknown The active ingredient vancomycin is not known to be associated with embryo-fetal toxicity [see Use in Specific Populations (8.1)].
5.2 Nephrotoxicity
Vancomycin Injection administered intravenously or orally can result in acute kidney injury (AKI), including acute renal failure, mainly due to interstitial nephritis or less commonly acute tubular necrosis. AKI is manifested by increasing blood urea nitrogen (BUN) and serum creatinine (Cr). The risk of AKI increases with higher vancomycin serum levels, prolonged exposure, concomitant administration of other nephrotoxic drugs, concomitant administration of piperacillin-tazobactam [see Drug Interactions (7.2)], volume depletion, pre-existing renal impairment and in critically ill patients and patients with co-morbid conditions that predispose to renal impairment.
Monitor serum vancomycin concentrations and renal function in all patients receiving Vancomycin Injection intravenously.
Nephrotoxicity (e.g., reports of renal failure, renal impairment, blood creatinine increased) has occurred following oral vancomycin hydrochloride capsule therapy in randomized controlled clinical studies and can occur either during or after completion of therapy. The risk of nephrotoxicity is increased in patients >65 years of age [see Adverse Reactions (6.1) and Use in Specific Populations (8.5)]. In patients over 65 years of age, including those with normal renal function prior to treatment, renal function should be monitored during and following treatment with orally administered Vancomycin Injection to detect potential vancomycin induced nephrotoxicity.
More frequent monitoring is recommended in patients with comorbidities that predispose to impairment in renal function or are concomitantly receiving other nephrotoxic drugs, in critically ill patients, in patients with changing renal function, and in patients requiring higher therapeutic vancomycin levels. If acute kidney injury occurs, discontinue Vancomycin Injection or reduce the dose.
5.3 Ototoxicity
Ototoxicity has occurred in patients administered vancomycin intravenously or orally. It may be transient or permanent. Ototoxicity manifests as tinnitus, hearing loss, dizziness or vertigo. The risk is higher in older patients, patients who are receiving higher doses, who have an underlying hearing loss, who are receiving concomitant therapy with another ototoxic agent, such as an aminoglycoside or who have underlying renal impairment. Monitor for signs and symptoms of ototoxicity during oral or intravenous therapy with Vancomycin Injection. Discontinue Vancomycin Injection if ototoxicity occurs. Serial tests of auditory function may be helpful in order to minimize the risk of ototoxicity.
5.4 Severe Dermatologic Reactions
Severe dermatologic reactions such as toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome (SJS), drug reaction with eosinophilia and systemic symptoms (DRESS), acute generalized exanthematous pustulosis (AGEP), and linear IgA bullous dermatosis (LABD) have been reported in association with the use of vancomycin. Cutaneous signs or symptoms reported include skin rashes, mucosal lesions, and blisters. Discontinue Vancomycin Injection at the first appearance of signs and symptoms of TEN, SJS, DRESS, AGEP, or LABD.
5.5 Neutropenia
Reversible neutropenia has been reported in patients administered vancomycin intravenously or orally. Patients who will undergo prolonged therapy with Vancomycin Injection or those who are receiving concomitant drugs which may cause neutropenia should have periodic monitoring of the leukocyte count.
5.6 Infusion Reactions
Hypotension, including shock and cardiac arrest, wheezing, dyspnea, urticaria, muscular and chest pain may occur with rapid Vancomycin Injection intravenous administration. The reactions may be more severe in younger patients, particularly children, and in patients receiving concomitant muscle relaxant anesthetics. Rapid intravenous administration of Vancomycin Injection may also be associated with vancomycin infusion reaction which manifests as pruritus and erythema that involves the face, neck and upper torso. Infusion-related adverse reactions are related to both the concentration and the rate of administration of vancomycin. Infusion-related adverse reactions may occur, however, at any rate or concentration.
Administer Vancomycin Injection over a period of 60 minutes or greater to reduce the risk of infusion-related adverse reactions. In selected patients in need of fluid restriction, a concentration up to 10 mg/mL may be used; use of such higher concentrations may increase the risk of infusion-related adverse reactions. Administer prior to intravenous anesthetic agents when feasible. Stop the infusion if a reaction occurs.
5.7 Phlebitis and Adverse Reactions with Unapproved Routes of Administration
Inflammation at the site of injection of vancomycin has been reported. Vancomycin is irritating to tissue and must be given by a secure intravenous route of administration to reduce the risk of local irritation and phlebitis. Thrombophlebitis may occur, the frequency and severity of which can be minimized by slow infusion of the drug and by rotation of venous access sites.
Administration of vancomycin by intramuscular (IM), intraperitoneal, intrathecal, intraventricular, or intravitreal routes has not been approved and is not recommended. The safety and efficacy of vancomycin administered by these routes of administration have not been established by adequate and well controlled trials. Pain, tenderness, and necrosis occur with IM injection of vancomycin or with inadvertent extravasation. Intraperitoneal administration during continuous ambulatory peritoneal dialysis (CAPD) can result in chemical peritonitis. Manifestations range from cloudy dialysate alone to a cloudy dialysate accompanied by variable degrees of abdominal pain and fever. This syndrome appears to be resolved after discontinuation of intraperitoneal vancomycin.
About 60% of an intraperitoneal dose of vancomycin administered during peritoneal dialysis is absorbed systemically in 6 hours. Serum concentrations of about 10 mcg/mL are achieved by intraperitoneal injection of 30 mg/kg of vancomycin. However, the safety and efficacy of the intraperitoneal use of vancomycin has not been established in adequate and well-controlled trials.
5.8 Clostridioides difficile-Associated Diarrhea (CDAD)
Clostridioides difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including intravenous administration of vancomycin and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents. If CDAD is suspected or confirmed, ongoing antibacterial use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Clinically significant serum concentrations of vancomycin have been reported in some patients being treated for active C. difficile-induced pseudomembranous colitis after multiple oral doses of vancomycin [see Warning sand Precautions (5.11)].
Prolonged use of Vancomycin Injection may result in the overgrowth of non-susceptible microorganisms. Careful observation of the patient is essential. If superinfection occurs during therapy, appropriate measures should be taken. There have been reports of pseudomembranous colitis due to C. difficile developing in patients who received intravenous vancomycin.
5.9 Hemorrhagic Occlusive Retinal Vasculitis (HORV)
Hemorrhagic occlusive retinal vasculitis, including permanent loss of vision, occurred in patients receiving intracameral or intravitreal administration of vancomycin during or after cataract surgery. The safety and efficacy of vancomycin administered by the intracameral or the intravitreal route have not been established by adequate and well-controlled trials. Vancomycin Injection (intravenously and orally administered) is not indicated for the prophylaxis of endophthalmitis.
5.10 Development of Drug-Resistant Bacteria
Prescribing Vancomycin Injection (intravenously and orally administered) in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
5.11 Potential for Systemic Absorption after Oral Administration
Clinically significant serum concentrations have been reported in some patients who have taken multiple oral doses of oral vancomycin for active C. difficile-associated diarrhea. Some patients with inflammatory disorders of the intestinal mucosa also may have significant systemic absorption of vancomycin. These patients may be at risk for the development of adverse reactions associated with higher doses of oral vancomycin; therefore, monitoring of serum concentrations of vancomycin may be appropriate in some instances, e.g., in patients with renal insufficiency and/or colitis or in those receiving concomitant therapy with an aminoglycoside antibacterial drug.
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
Nephrotoxicity [see Warnings and Precautions (5.2)]
Ototoxicity [see Warnings and Precautions (5.3)]
Severe Dermatologic Reactions [see Warnings and Precautions (5.4)]
Neutropenia [see Warnings and Precautions (5.5)]
Infusion Reactions [see Warnings and Precautions (5.6)]
Clostridioides difficile-Associated Diarrhea [see Warnings and Precautions (5.8)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adverse Reactions in Patients Receiving Intravenously and Orally Administered Vancomycin
The following adverse reactions associated with the use of intravenously and orally administered vancomycin were identified in clinical trials:
Renal and Urinary Disorders: Acute kidney injury and interstitial nephritis [see Warnings and Precautions (5.2)]
Ear and Labyrinth Disorders: Tinnitus, hearing loss, vertigo [see Warnings and Precautions (5.3)]
Skin and Subcutaneous Tissue Disorders: Erythema (especially of the face, neck and upper torso) and pruritus which are manifestations of rashes including exfoliative dermatitis, toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome (SJS), linear IgA bullous dermatosis (LABD) [see Warnings and Precautions (5.4)].
Blood and Lymphatic System Disorders: Agranulocytosis, neutropenia, pancytopenia, leukopenia, thrombocytopenia, eosinophilia [see Warnings and Precautions (5.5)]
Immune System Disorders: Hypersensitivity reactions including anaphylaxis and vancomycin infusion reaction [see Warnings and Precautions (5.6)]
General Disorders and Administration Site Conditions: General discomfort, fever, chills, phlebitis, injection site irritation, injection site pain and necrosis following intramuscular injection, chemical peritonitis following intraperitoneal administration. Vancomycin Injection is not approved for intramuscular and intraperitoneal administration [see Warnings and Precautions (5.7)]
Gastrointestinal Disorders: Pseudomembranous colitis [see Warnings and Precautions (5.8)]
Cardiac Disorders: Cardiac arrest, chest pain
Laboratory Abnormalities: Elevated blood urea nitrogen, elevated serum creatinine
Musculoskeletal and Connective Tissue Disorders: Muscle pain
Nervous System Disorders: Dizziness
Respiratory, Thoracic and Mediastinal Disorders: Wheezing, dyspnea
Vascular Disorders: Hypotension, shock, vasculitis
Adverse Reactions in Patients Receiving Oral Administration of Vancomycin Hydrochloride Capsules
The data described below reflect exposure to vancomycin hydrochloride capsules in 260 adult subjects in two Phase 3 clinical trials for the treatment of diarrhea associated with C. difficile. In both trials, subjects received vancomycin hydrochloride capsules 125 mg orally four times daily. The mean duration of treatment was 9.4 days. The median age of patients was 67, ranging between 19 and 96 years of age. Patients were predominantly Caucasian (93%) and 52% were male.
Adverse reactions occurring in ≥5% of vancomycin hydrochloride capsules-treated subjects are shown in Table 1. The most common adverse reactions associated with vancomycin hydrochloride capsules (≥10%) were nausea, abdominal pain, and hypokalemia.
| System /Organ Class | Adverse Reaction | Vancomycin Hydrochloride Capsules % (n=260) |
|---|---|---|
|
|
||
| Gastrointestinal disorders | Nausea Abdominal pain Vomiting Diarrhea Flatulence | 17 15 9 9 8 |
| General disorders and administration site conditions | Pyrexia Edema peripheral Fatigue | 9 6 5 |
| Infections and infestations | Urinary tract infection | 8 |
| Metabolism and nutrition disorders | Hypokalemia | 13 |
| Musculoskeletal and connective tissue disorders | Back pain | 6 |
| Nervous system disorders | Headache | 7 |
Nephrotoxicity (e.g., reports of renal failure, renal impairment, blood creatinine increased) occurred in 5% of subjects treated with oral vancomycin. Nephrotoxicity following oral vancomycin typically first occurred within one week after completion of treatment (median day of onset was Day 16). Nephrotoxicity following oral vancomycin occurred in 6% of subjects >65 years of age and 3% of subjects ≤65 years of age [see Warnings and Precautions (5.2)].
The incidences of hypokalemia, urinary tract infection, peripheral edema, insomnia, constipation, anemia, depression, vomiting, and hypotension were higher among subjects >65 years of age than in subjects ≤65 years of age [see Use in Specific Populations (8.5)].
Discontinuation of study drug due to adverse events occurred in 7% of subjects treated with oral vancomycin. The most common adverse events leading to discontinuation of oral vancomycin were C. difficile colitis (<1%), nausea (<1%), and vomiting (<1%).
6.2 Postmarketing Experience
The following adverse reactions have been identified during postmarketing use of vancomycin (administered orally and intravenously). Because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Skin and Subcutaneous Tissue Disorders: Drug reaction with eosinophilia and systemic symptoms (DRESS), acute generalized exanthematous pustulosis (AGEP) [see Warnings and Precautions (5.4)].
Ototoxicity: Cases of hearing loss associated with intravenously administered vancomycin have been reported. Most of these patients had kidney dysfunction or a preexisting hearing loss or were receiving concomitant treatment with an ototoxic drug [see Warnings and Precautions (5.3)]. Vertigo, dizziness, and tinnitus have been reported.
Hematopoietic: Reversible neutropenia, usually starting 1 week or more after onset of intravenous therapy with vancomycin or after a total dose of more than 25 g, has been reported for several dozen patients. Neutropenia appears to be promptly reversible when vancomycin is discontinued. Thrombocytopenia has been reported.
Miscellaneous: Patients have been reported to have had anaphylaxis, drug fever, chills, nausea, eosinophilia, rashes (including exfoliative dermatitis), Stevens-Johnson syndrome, toxic epidermal necrolysis, and rare cases of vasculitis in association with the administration of vancomycin.
A condition has been reported with oral vancomycin that is similar to the IV-induced syndrome with symptoms consistent with anaphylactoid reactions, including hypotension, wheezing, dyspnea, urticaria, pruritus, flushing of the upper body ("vancomycin infusion reaction"), pain and muscle spasm of the chest and back. These reactions usually resolve within 20 minutes but may persist for several hours.
7 DRUG INTERACTIONS
7.1 Anesthetic Agents
Concomitant administration of vancomycin and anesthetic agents has been associated with erythema and histamine-like flushing [see Warnings and Precautions (5.6) and Use in Specific Populations (8.4)].
7.2 Piperacillin-Tazobactam
Studies have detected an increased incidence of acute kidney injury in patients administered concomitant piperacillin/tazobactam and vancomycin as compared to vancomycin alone. Monitor kidney function in patients receiving concomitant piperacillin/tazobactam and Vancomycin Injection. No pharmacokinetic interactions have been noted between piperacillin/tazobactam and vancomycin.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
This formulation of Vancomycin Injection administered intravenously or orally is not recommended for use during the first or second trimester of pregnancy because it contains the excipient, PEG 400, which caused fetal malformations in animal reproduction studies following intravenous administration (see Data). Advise pregnant women of the potential risk to the fetus. If therapy with Vancomycin Injection is needed during the first or second trimester of pregnancy, use other available formulations of vancomycin free of PEG 400.
There are no available data on use of this formulation of Vancomycin Injection (with the excipient PEG 400) in pregnant women to inform a drug-associated risk of major birth defects, miscarriage, or other adverse maternal or infant outcomes. Available published data on use of vancomycin (without the excipient PEG 400) administered intravenously in pregnancy during the second and third trimesters have not shown an association with adverse pregnancy related outcomes (see Data). There are no available data on first trimester use of vancomycin in pregnant women to assess the risk of major birth defects or miscarriage. Systemic absorption of vancomycin is low following oral administration of vancomycin hydrochloride capsules; however, absorption may vary depending on various factors [see Clinical Pharmacology (12.3)].
A reproduction study in rabbits with intravenous doses of PEG 400 during organogenesis, at approximately 13 times the maximum daily human dose of vancomycin, resulted in fetal spinal malformations. Vancomycin alone did not show adverse developmental effects when administered intravenously to pregnant rats and rabbits during organogenesis at doses less than or equal to the recommended maximum human dose (see Data).
There were no oral embryo-fetal toxicity studies conducted in animals with this formulation of Vancomycin Injection. Based on the uncertainty with oral bioavailability of PEG 400, the potential adverse developmental effect of PEG 400 with oral administration is unknown.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data
There are no available data on first trimester use of vancomycin, including vancomycin with the excipients PEG 400 and N-acetyl D-alanine (NADA), in pregnant women to assess a risk of major birth defects or miscarriage.
A published study evaluated hearing loss and nephrotoxicity in infants of 10 pregnant intravenous drug users treated with intravenously administered vancomycin (formulation did not include the excipients PEG 400 and NADA) for suspected or documented methicillin-resistant Staphylococcus aureus in the second or third trimester. The comparison groups were 10 uninfected non-intravenous drug-dependent patients, and 10 uninfected intravenous drug-dependent patients who served as substance abuse controls. No infant in the vancomycin exposed group had abnormal sensorineural hearing at 3 months of age or nephrotoxicity.
A published prospective study assessed outcomes in 55 pregnant women with a positive Group B streptococcus (GBS) culture and a high-risk penicillin allergy with resistance to clindamycin or unknown sensitivity who were administered vancomycin intravenously (formulation did not include the excipients PEG 400 and NADA) at the time of delivery. Vancomycin dosing ranged from the standard 1 g intravenously every 12 hours to 20 mg/kg intravenous every 8 hours (maximum individual dose 2 g). No major adverse reactions were recorded either in the mothers or their newborns. None of the newborns had sensorineural hearing loss. Neonatal renal function was not examined, but all of the newborns were discharged in good condition.
Animal Data
Vancomycin did not cause fetal malformations when administered during organogenesis to pregnant rats (gestation days 6 to 15) and rabbits (gestation days 6 to 18) at the equivalent recommended maximum human dose (based on body surface area comparisons) of 200 mg/kg/day IV to rats or 120 mg/kg/day IV to rabbits1. No effects on fetal weight or development were seen in rats at the highest dose tested or in rabbits given 80 mg/kg/day (approximately 1 and 0.8 times the recommended maximum human dose based on body surface area, respectively). Maternal toxicity was observed in rats (at doses 120 mg/kg and above) and rabbits (at 80 mg/kg and above).
The excipient, PEG 400, administered intravenously to pregnant rabbits at 2000 mg/kg (approximately 13 times higher AUC levels of PEG 400 than in the maximum daily human dose of vancomycin) during organogenesis (gestation days 6 to 19) resulted in fetal scoliosis (thoracic and lumbar) and increased incidence of delayed or incomplete ossification of the pubes, epiphyses, and talus bones when compared with controls. No maternal toxicity was observed up to the maximum dose tested.
In animal reproduction studies conducted in pregnant rabbits (gestation days 6 to 19) and pregnant rats (gestation days 6 to 17) administered the excipient NADA intravenously at 1680 and 3780 mg/kg, respectively (approximately 96 times or more higher AUC levels of NADA than in the maximum daily human dose of vancomycin) resulted in fetal scoliosis and a spectrum of cardiovascular anomalies in rabbits when compared with controls and no adverse effects on fetuses in rats. Increased incidence of delayed or incomplete ossifications of the metacarpals/metatarsals/phalanges and increased ossification (fused jugal/maxilla bones) were observed in rabbits at 1680 mg/kg. Minor non adverse fetal skeletal abnormalities were observed in rats at 3780 mg/kg which was also associated with maternal toxicity including increased incidence of litter loss [see Clinical Pharmacology (12.6)].
There were no oral embryo-fetal toxicity studies conducted in animals with this Vancomycin Injection product. The oral bioavailability of PEG 400 in humans is uncertain. The oral bioavailability of NADA is unknown.
No animal studies have been conducted to evaluate the potential reproductive and embryo-fetal effects of Vancomycin Injection with the excipients PEG 400 and NADA.
8.2 Lactation
Risk Summary
Vancomycin is present in human milk following intravenous administration, however, there are insufficient data to inform the levels. There are no available data on vancomycin presence in milk following oral administration. Systemic absorption of vancomycin is low following oral administration of vancomycin hydrochloride capsules; however, absorption may vary depending on various factors [see Clinical Pharmacology (12.3)]. There are no data on the effects of vancomycin on the breastfed infant or milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Vancomycin Injection and any potential adverse effects on the breastfed infant from Vancomycin Injection or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Perform a pregnancy test in females of reproductive potential prior to prescribing this formulation of Vancomycin Injection for intravenous or oral administration [see Warnings and Precautions (5.1) and Use in Specific Populations (8.1)].
8.4 Pediatric Use
Vancomycin Injection administered intravenously is indicated in pediatric patients less than 18 years of age for the treatment of septicemia, infective endocarditis, skin and skin structure infections, bone infections and lower respiratory tract infections [see Indications and Usage (1.1 to 1.5) and Dosage and Administration (2.2)].
Vancomycin Injection administered orally is indicated in pediatric patients less than 18 years of age for the treatment of Clostridioides difficile-associated diarrhea and enterocolitis caused by Staphylococcus aureus (including methicillin-resistant strains) [see Indications and Usage (1.6, 1.7) and Dosage and Administration (2.3)].
In pediatric patients, monitor vancomycin serum concentration and renal function when administering Vancomycin Injection intravenously [see Dosage and Administration (2.12.3) and Warnings and Precautions (5.2)]. More severe infusion related reactions related to vancomycin administration may occur in pediatric patients. Concomitant administration of vancomycin and intravenous anesthetic agents has been associated with erythema and histamine-like flushing in all patients including pediatric patients [see Warnings and Precautions (5.6)].
8.5 Geriatric Use
Clinical studies with another vancomycin hydrochloride drug product in C. difficile-associated diarrhea have demonstrated that geriatric subjects are at increased risk of developing nephrotoxicity following treatment with oral vancomycin hydrochloride, which may occur during or after completion of therapy. In patients over 65 years of age, including those with normal renal function prior to treatment, renal function should be monitored during and following treatment with Vancomycin Injection to detect potential vancomycin induced nephrotoxicity [see Warnings and Precautions (5.2) and Adverse Reactions (6.1)].
Patients over 65 years of age may take longer to respond to therapy compared to patients 65 years of age and younger. Clinicians should be aware of the importance of appropriate duration of Vancomycin Injection treatment in patients over 65 years of age and not discontinue or switch to alternative treatment prematurely.
Vancomycin is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection [see Dosage and Administration (2.4)], and it may be useful to monitor renal function [see Warnings and Precautions (5.2)].
8.6 Renal Impairment
Dosage adjustment must be made in patients with impaired renal function [see Dosage and Administration (2.3)]. Measure trough vancomycin serum concentrations to guide intravenous therapy, especially in seriously ill patients with changing renal function.
10 OVERDOSAGE
Supportive care is advised, with maintenance of glomerular filtration. Vancomycin is poorly removed by dialysis. Hemofiltration and hemoperfusion with polysulfone resin have been reported to result in increased vancomycin clearance.
For current information on the management of overdosage, contact the National Poison Control Center at 1-800-222-1222 or www.poison.org.
11 DESCRIPTION
Vancomycin Injection, 5 g/100 mL (50 mg/mL), in a Pharmacy Bulk Package bottle, is supplied as a clear, colorless to light yellow or light brown solution containing 5 g /100 mL (50 mg/mL) vancomycin.
A pharmacy bulk package is a sterile dosage form containing many single doses. The contents of this pharmacy bulk package are intended for use by a pharmacy admixture service for addition to suitable parenteral fluids in the preparation of admixtures for intravenous infusion. Vancomycin Injection is for intravenous or oral administration. Vancomycin Injection must be diluted with an appropriate diluent prior to intravenous administration [see Dosage and Administration (2.5)]. Vancomycin Injection may also be diluted with water and SyrSpend PH4 cherry flavored syrup added for oral administration [see Dosage and Administration (2.8)].
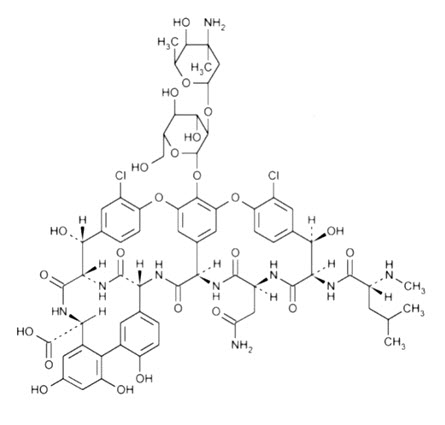
Vancomycin is a tricyclic glycopeptide antibacterial drug derived from Amycolatopsis orientalis (formerly Nocardia orientalis). The molecular formula is C66H75Cl2N9O24 and the molecular weight is 1,449.265 g/mol. The chemical name of vancomycin is (Sa)-(3S,6R,7R, 22R,23S,26S,36R,38aR)-44-{[2-O-(3-amino-2,3,6-trideoxy-3-C-methyl-α-L-lyxo-hexopyranosyl)-β-D-glucopyranosyl]-oxy}-3-(carbamoylmethyl)-10,19-dichloro-2,3,4,5,6,7,23,24,25,26,36,37,38,38a-tetradecahydro-7,22,28,30,32-pentahydroxy-6-[(2R)-4-methyl-2-(methylamino]valeramido]-2,5,24,38,39-pentaoxo-22H-8,11:18,21-dietheno-23,36(iminometha-no)-13,16:31,35-dimetheno-1H,16H-[1,6,9]-oxadiazacyclohexadecino-[4,5-m][10,2,16]-benzoxa-diazacyclotetracosine-26-carboxylic acid. Vancomycin has the following structural formula:
Vancomycin Injection, 5 g/100 mL, in a Pharmacy Bulk Package bottle is sterile, nonpyrogenic 100 mL solution containing 5 g vancomycin, 11.3 g polyethylene glycol 400, 4.52 g N-acetyl-D-alanine, 1.26 g L-lysine hydrochloride (monochloride) in water for injection. Sodium hydroxide is used for pH adjustment. The pH is 3.9 to 4.3.
12 CLINICAL PHARMACOLOGY
12.3 Pharmacokinetics
General Pharmacokinetics
In subjects with normal kidney function, multiple intravenous dosing of 1 g of vancomycin (15 mg/kg) infused over 60 minutes produces mean plasma concentrations of approximately 63 mcg/mL immediately after the completion of infusion, mean plasma concentrations of approximately 23 mcg/mL 2 hours after infusion, and mean plasma concentrations of approximately 8 mcg/mL 11 hours after the end of the infusion. Multiple dosing of 500 mg infused over 30 minutes produces mean plasma concentrations of about 49 mcg/mL at the completion of infusion, mean plasma concentrations of about 19 mcg/mL 2 hours after infusion, and mean plasma concentrations of about10 mcg/mL 6 hours after infusion. The plasma concentrations during multiple dosing are like those after a single dose.
Absorption
Vancomycin is poorly absorbed after oral administration. During multiple dosing of 250 mg every 8 hours for 7 doses, fecal concentrations of vancomycin in volunteers exceeded 100 mg/kg in the majority of samples. No blood concentrations were detected and urinary recovery did not exceed 0.76%. In anephric subjects with no inflammatory bowel disease who received vancomycin oral solution 2 g for 16 days, blood concentrations of vancomycin were less than or equal to 0.66 mcg/mL in 2 of 5 subjects. No measurable blood concentrations were attained in the other 3 subjects. Following doses of 2 g daily, concentrations of drug were >3100 mg/kg in the feces and <1 mcg/mL in the serum of subjects with normal renal function who had C. difficile-associated diarrhea. After multiple-dose oral administration of vancomycin, measurable serum concentrations may occur in patients with active C. difficile-associated diarrhea, and, in the presence of renal impairment, the possibility of accumulation exists. It should be noted that the total systemic and renal clearances of vancomycin are reduced in the elderly [see Use in Specific Populations (8.5)].
Distribution
The volume of distribution ranges from 0.3 to 0.43 L/kg after intravenous administration. Vancomycin is approximately 55% serum protein bound as measured by ultrafiltration at vancomycin serum concentrations of 10 to 100 mcg/mL. After intravenous administration of vancomycin, inhibitory concentrations are present in pleural, pericardial, ascitic, and synovial fluids; in urine; in peritoneal dialysis fluid; and in atrial appendage tissue. Vancomycin does not readily diffuse across normal meninges into the spinal fluid; but, when the meninges are inflamed, penetration into the spinal fluid occurs.
Elimination
Mean plasma clearance is about 0.058 L/kg/h, and mean renal clearance is about 0.048 L/kg/h. The mean elimination half-life of vancomycin from plasma is 4 to 6 hours in subjects with normal renal function. In anephric patients, the mean elimination half-life is 7.5 days. Total body and renal clearance of vancomycin may be reduced in the elderly.
12.4 Microbiology
Mechanism of Action
The bactericidal action of vancomycin results primarily from inhibition of cell-wall biosynthesis. In addition, vancomycin alters bacterial-cell-membrane permeability and RNA synthesis.
Resistance
Vancomycin is not active in vitro against gram-negative bacilli, mycobacteria, or fungi. There is no cross-resistance between vancomycin and other antibacterials.
C. difficile
Isolates of C. difficile generally have vancomycin minimal inhibitory concentrations (MICs) of < 1 mcg/mL; however, vancomycin MICs ranging from 4 mcg/mL to 16 mcg/mL have been reported. The mechanism which mediates C. difficile's decreased susceptibility to vancomycin has not been fully elucidated.
Interaction with Other Antimicrobials
The combination of vancomycin and an aminoglycoside acts synergistically in vitro against many isolates of Staphylococcus aureus, Streptococcus gallolyticus (previously known as Streptococcus bovis), Enterococcus spp, and the viridans group streptococci.
Antimicrobial Activity
Vancomycin has been shown to be active against most isolates of the following bacteria, both in vitro and in clinical infections [see Indications and Usage (1)].
Aerobic bacteria
Gram-positive bacteria
Corynebacterium spp.
Enterococcus spp. (including Enterococcus faecalis)
Staphylococcus aureus (including methicillin-resistant and methicillin-susceptible isolates)
Coagulase negative staphylococci (including S. epidermidis and methicillin-resistant isolates)
Streptococcus gallolyticus (previously known as Streptococcus bovis)
Viridans group streptococci
Anaerobic bacteria
Gram-positive bacteria
Clostridioides difficile isolates associated with C. difficile associated diarrhea
The following in vitro data are available, but their clinical significance is unknown.
At least 90 percent of the following bacteria exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for vancomycin against isolates of similar genus or organism group. However, the efficacy of vancomycin in treating clinical infections caused by these bacteria has not been established in adequate and well-controlled clinical trials.
12.6 Pharmacokinetics of Polyethylene Glycol 400 and N-acetyl D-alanine
Because fetal malformations were observed with PEG 400 and NADA in animal reproduction studies [see Use in Specific Populations (8.1)], NADA and PEG 400 pharmacokinetics following a single intravenous administration of Vancomycin injection 1 g were studied in healthy adults.
The geometric mean (95% prediction interval) of simulated steady-state AUC0-24hr in healthy adults administered a 1g Vancomycin Injection over 1.5 hours every 12 hours was 128 (92.5-182) and 408 (306-552) mcg∙h/mL for NADA and PEG 400, respectively.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term carcinogenesis studies in animals have been conducted.
At concentrations up to 1000 mcg/mL, vancomycin had no mutagenic effect in vitro in the mouse lymphoma forward mutation assay or the primary rat hepatocyte unscheduled DNA synthesis assay. The concentrations tested in vitro were above the peak plasma vancomycin concentrations of 20 to 40 mcg/mL usually achieved in humans after slow infusion of the maximum recommended dose of 1 g intravenously. Vancomycin had no mutagenic effect in vivo in the Chinese hamster sister chromatid exchange assay (400 mg/kg IP) or the mouse micronucleus assay (800 mg/kg IP).
No definitive fertility studies have been conducted.
15 REFERENCES
1. Byrd RA., Gries CL, Buening M.: Developmental Toxicology Studies of Vancomycin Hydrochloride Administered Intravenously to Rats and Rabbits. Fundam Appl Toxicol 1994; 23: 590-597.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Vancomycin Injection, 5g /100 mL (50 mg/mL), in a Pharmacy Bulk Package bottle, is supplied as a clear, colorless to light yellow or light brown solution containing 50 mg/mL of vancomycin. The solution is supplied in a 100 mL clear glass bottle with rubber stopper and aluminum seals with a dark blue flip off cap. The vial stopper is not made with natural rubber latex
| NDC number | Packaging configuration |
|---|---|
| 70594-040-01 | Vancomycin Injection, 5 g/100 mL (50 mg/mL), in a Pharmacy Bulk Package bottle, packed individually |
16.2 Storage
Store at 15°C to 25°C (59°F to 77°F), in original package, protected from light. Do not refrigerate or freeze. Storage after reconstitution and dilution is described elsewhere in the labeling [see Dosage and Administration (2.5, 2.8)].
17 PATIENT COUNSELING INFORMATION
Potential Risk of Exposure to Excipient During the First or Second Trimester of Pregnancy
Advise patients to notify their healthcare provider if they are pregnant prior to treatment with this formulation of vancomycin [see Warnings and Precautions (5.1) and Use in Specific Populations (8.1)].
Acute Kidney Injury
Advise patients that Vancomycin Injection can result in kidney damage and that blood tests are required to monitor vancomycin blood levels and kidney function during therapy [see Warnings and Precautions (5.2)].
Hearing Loss or Balance Problems
Advise patients that Vancomycin Injection may result in decreased hearing and to report hearing loss or balance problems to their health care provider [see Warnings and Precautions (5.3)].
Severe Dermatologic Reactions
Advise patients about the signs and symptoms of serious skin manifestations. Instruct patients to stop Vancomycin Injection immediately and promptly report the first signs or symptoms of skin rash, mucosal lesions or blisters, [see Warnings and Precautions (5.4)].
Infusion Reactions During or After Intravenous Use
Advise patients that generalized skin redness, skin rash, itching, flushing, muscle pain, chest pain, shortness of breath, wheezing, or dizziness may occur during Vancomycin Injection infusion [see Warnings and Precautions (5.6)].
Diarrhea
Diarrhea is a common problem caused by antibacterial drugs, including Vancomycin Injection, which usually ends when the antibacterial drug is discontinued. Sometimes after starting treatment with antibacterial drugs, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibacterial drug. If this occurs, patients should contact their physician as soon as possible [see Warnings and Precautions (5.8)].
Antibacterial Resistance
Patients should be counseled that antibacterial drugs including Vancomycin Injection, should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When Vancomycin Injection is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Vancomycin Injection or other antibacterial drugs in the future.
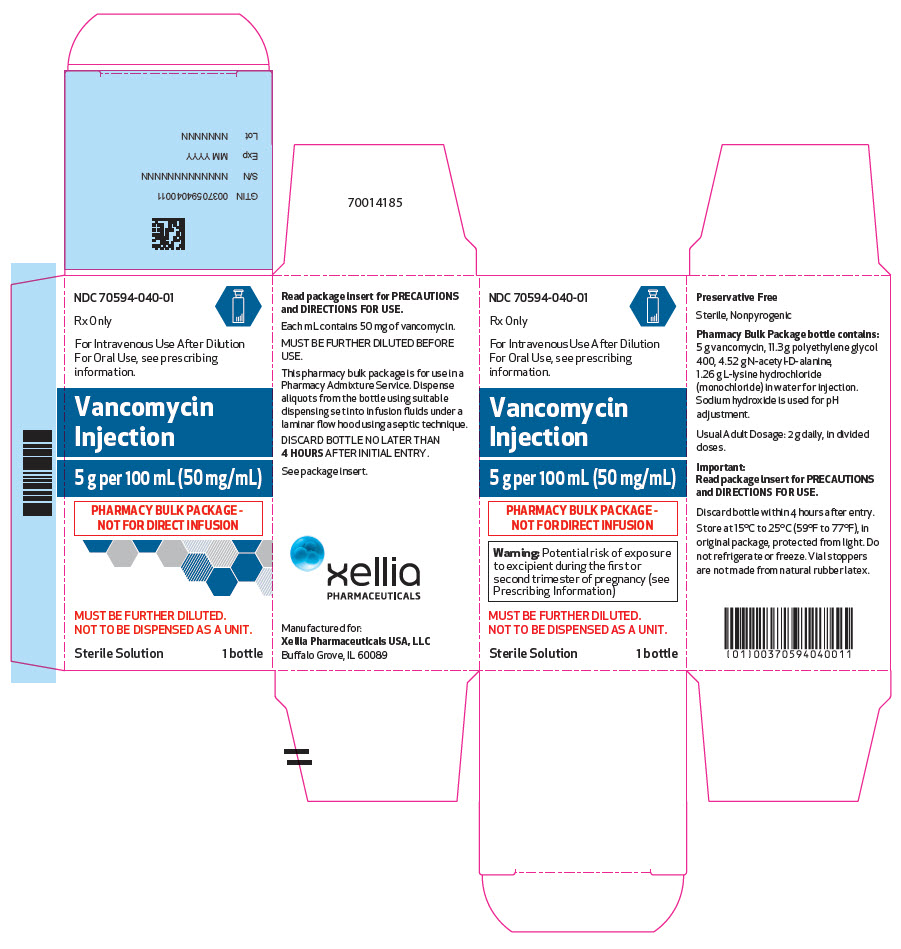
PRINCIPAL DISPLAY PANEL - 100 mL Vial Carton
NDC: 70594-040-01
Rx Only
For Intravenous Use After Dilution
For Oral Use, see prescribing
information.
Vancomycin
Injection
5 g per 100 mL (50 mg/mL)
PHARMACY BULK PACKAGE -
NOT FOR DIRECT INFUSION
Warning: Potential risk of exposure
to excipient during the first or
second trimester of pregnancy (see
Prescribing Information)
MUST BE FURTHER DILUTED.
NOT TO BE DISPENSED AS A UNIT.
Sterile Solution
1 bottle
| VANCOMYCIN
vancomycin injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Xellia Pharmaceuticals USA LLC (116768762) |