TIMOLOL MALEATE solution
Timolol Maleate by
Drug Labeling and Warnings
Timolol Maleate by is a Prescription medication manufactured, distributed, or labeled by A-S Medication Solutions. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
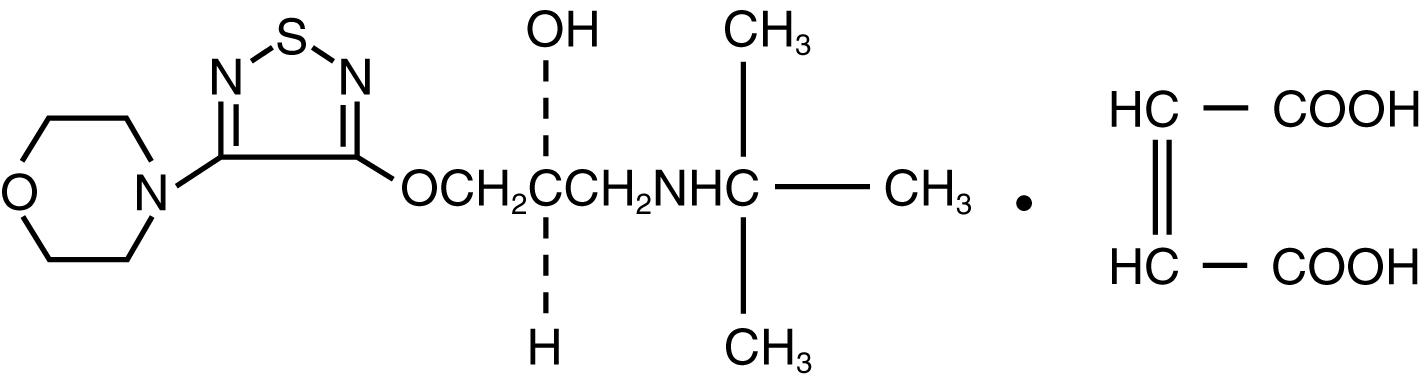
Timolol maleate ophthalmic solution, USP is a non-selective beta-adrenergic receptor blocking agent. Its chemical name is (-)-1-(tert-butylamino)-3-[(4-morpholino-1,2,5-thiadiazol-3-yl)oxy]-2-propanol maleate (1:1) (salt). Timolol maleate possesses an asymmetric carbon atom in its structure and is provided as the levo-isomer. The optical rotation of timolol maleate is:
- 25°
- [α] in 1.0N HCl (C = 5%) = -12.2° (-11.7° to -12.5°)
- 405 nm
Its molecular formula is C13H24N4O3SC4H4O4 and its structural formula is:
Timolol maleate has a molecular weight of 432.50. It is a white, odorless, crystalline powder which is soluble in water, methanol, and alcohol. Timolol maleate ophthalmic solution, USP is stable at room temperature.
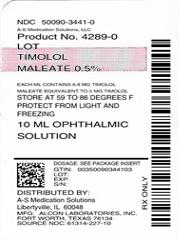
Timolol maleate ophthalmic solution, USP is supplied as a sterile, isotonic, buffered, aqueous solution of timolol maleate in two dosage strengths. Each mL of timolol maleate ophthalmic solution 0.25% contains 2.5 mg of timolol (3.4 mg of timolol maleate). Each mL of timolol maleate ophthalmic solution 0.5% contains 5.0 mg of timolol (6.8 mg of timolol maleate). Inactive ingredients: monobasic and dibasic sodium phosphate, sodium hydroxide and/or hydrochloric acid to adjust pH (6.5 to 7.5), and purified water. Benzalkonium chloride 0.01% is added as preservative.
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Timolol maleate is a beta1 and beta2 (non-selective) adrenergic receptor blocking agent that does not have significant intrinsic sympathomimetic, direct myocardial depressant, or local anesthetic (membrane-stabilizing) activity.
Beta-adrenergic receptor blockade reduces cardiac output in both healthy subjects and patients with heart disease. In patients with severe impairment of myocardial function, beta-adrenergic receptor blockade may inhibit the stimulatory effect of the sympathetic nervous system necessary to maintain adequate cardiac function.
Beta-adrenergic receptor blockade in the bronchi and bronchioles results in increased airway resistance from unopposed parasympathetic activity. Such an effect in patients with asthma or other bronchospastic conditions is potentially dangerous.
Timolol maleate ophthalmic solution, when applied topically on the eye, has the action of reducing elevated as well as normal intraocular pressure, whether or not accompanied by glaucoma. Elevated intraocular pressure is a major risk factor in the pathogenesis of glaucomatous visual field loss. The higher the level of intraocular pressure, the greater the likelihood of glaucomatous visual field loss and optic nerve damage.
The onset of reduction in intraocular pressure following administration of timolol maleate ophthalmic solution can usually be detected within one-half hour after a single dose. The maximum effect usually occurs in one to two hours and significant lowering of intraocular pressure can be maintained for periods as long as 24 hours with a single dose. Repeated observations over a period of one year indicate that the intraocular pressure-lowering effect of timolol is well maintained.
The precise mechanism of the ocular hypotensive action of timolol is not clearly established at this time. Tonography and fluorophotometry studies in man suggest that its predominant action may be related to reduced aqueous formation. However, in some studies a slight increase in outflow facility was also observed.
Pharmacokinetics
In a study of plasma drug concentration in six subjects, the systemic exposure to timolol was determined following twice daily administration of timolol maleate ophthalmic solution 0.5%. The mean peak plasma concentration following morning dosing was 0.46 ng/mL and following afternoon dosing was 0.35 ng/mL.
Clinical Studies
In controlled multiclinic studies in patients with untreated intraocular pressures of 22 mmHg or greater, timolol maleate ophthalmic solution 0.25% or 0.5% administered twice a day produced a greater reduction in intraocular pressure than 1, 2, 3, or 4% pilocarpine solution administered four times a day or 0.5, 1, or 2% epinephrine hydrochloride solution administered twice a day.
In these studies, timolol was generally well tolerated and produced fewer and less severe side effects than either pilocarpine or epinephrine. A slight reduction of resting heart rate in some patients receiving timolol (mean reduction 2.9 beats/minute standard deviation 10.2) was observed.
- INDICATIONS AND USAGE
-
CONTRAINDICATIONS
Timolol maleate is contraindicated in patients with (1) bronchial asthma; (2) a history of bronchial asthma; (3) severe chronic obstructive pulmonary disease [see Warnings]; (4) sinus bradycardia; (5) second or third degree atrioventricular block; (6) overt cardiac failure [see Warnings]; (7) cardiogenic shock; or (8) hypersensitivity to any component of this product.
-
WARNINGS
As with many topically applied ophthalmic drugs, this drug is absorbed systemically.
The same adverse reactions found with systemic administration of beta-adrenergic blocking agents may occur with topical administration. For example, severe respiratory reactions and cardiac reactions, including death due to bronchospasm in patients with asthma, and rarely death in association with cardiac failure, have been reported following systemic or ophthalmic administration of timolol maleate [see Contraindications].
Cardiac Failure
Sympathetic stimulation may be essential for support of the circulation in individuals with diminished myocardial contractility, and its inhibition of beta-adrenergic receptor blockade may precipitate more severe failure.
In Patients Without a History of Cardiac Failure continued depression of the myocardium with beta-blocking agents over a period of time can, in some cases, lead to cardiac failure. At the first sign or symptom of cardiac failure, timolol should be discontinued.
Obstructive Pulmonary Disease
Patients with chronic obstructive pulmonary disease (e.g., chronic bronchitis, emphysema) of mild or moderate severity, bronchospastic disease, or a history of bronchospastic disease (other than bronchial asthma or a history of bronchial asthma, in which timolol is contraindicated [see Contraindications]) should, in general, not receive beta-blockers, including timolol.
Major Surgery
The necessity or desirability of withdrawal of beta-adrenergic blocking agents prior to major surgery is controversial. Beta-adrenergic receptor blockade impairs the ability of the heart to respond to beta-adrenergically mediated reflex stimuli. This may augment the risk of general anesthesia in surgical procedures. Some patients receiving beta-adrenergic receptor blocking agents have experienced protracted severe hypotension during anesthesia. Difficulty in restarting and maintaining the heartbeat has also been reported. For these reasons, in patients undergoing elective surgery, some authorities recommend gradual withdrawal of beta-adrenergic receptor blocking agents.
If necessary during surgery, the effects of beta-adrenergic blocking agents may be reversed by sufficient doses of adrenergic agonists.
-
Diabetes Mellitus
Beta-adrenergic blocking agents should be administered with caution in patients subject to spontaneous hypoglycemia or to diabetic patients (especially those with labile diabetes) who are receiving insulin or oral hypoglycemic agents. Beta-adrenergic receptor blocking agents may mask the signs and symptoms of acute hypoglycemia.
-
PRECAUTIONS
General
Because of potential effects of beta-adrenergic blocking agents on blood pressure and pulse, these agents should be used with caution in patients with cerebrovascular insufficiency. If signs or symptoms suggesting reduced cerebral blood flow develop following initiation of therapy with timolol, alternative therapy should be considered.
There have been reports of bacterial keratitis associated with the use of multiple-dose containers of topical ophthalmic products. These containers had been inadvertently contaminated by patients who, in most cases, had a concurrent corneal disease or a disruption of the ocular epithelial surface [see Precautions, Information for Patients].
Choroidal detachment after filtration procedures has been reported with the administration of aqueous suppressant therapy (e.g., timolol).
Angle-closure glaucoma
In patients with angle-closure glaucoma, the immediate objective of treatment is to reopen the angle. This requires constricting the pupil. Timolol maleate has little or no effect on the pupil. Timolol maleate should not be used alone in the treatment of angle-closure glaucoma.
Anaphylaxis
While taking beta-blockers, patients with a history of atopy or a history of severe anaphylactic reactions to a variety of allergens may be more reactive to repeated accidental, diagnostic, or therapeutic challenge with such allergens. Such patients may be unresponsive to the usual doses of epinephrine used to treat anaphylactic reactions.
Muscle Weakness
Beta-adrenergic blockade has been reported to potentiate muscle weakness consistent with certain myasthenic symptoms (e.g., diplopia, ptosis, and generalized weakness). Timolol has been reported rarely to increase muscle weakness in some patients with myasthenia gravis or myasthenic symptoms.
Information for Patients
Patients should be instructed to avoid allowing the tip of the dispensing container to contact the eye or surrounding structures.
Patients should also be instructed that ocular solutions, if handled improperly or if the tip of the dispensing container contacts the eye or surrounding structures, can become contaminated by common bacteria known to cause ocular infections. Serious damage to the eye and subsequent loss of vision may result from using contaminated solutions [see Precautions, General].
Patients should also be advised that if they have ocular surgery or develop an intercurrent ocular condition (e. g., trauma or infection), they should immediately seek their physician's advice concerning the continued use of the present multidose container.
Patients with bronchial asthma, a history of bronchial asthma, severe chronic obstructive pulmonary disease, sinus bradycardia, second or third degree atrioventricular block, or cardiac failure should be advised not to take this product [see Contraindications].
Patients should be advised that timolol maleate ophthalmic solution contains benzalkonium chloride which may be absorbed by soft contact lenses. Contact lenses should be removed prior to administration of the solution. Lenses may be reinserted 15 minutes following timolol maleate ophthalmic solution administration.
Drug Interactions
Although timolol used alone has little or no effect on pupil size, mydriasis resulting from concomitant therapy with timolol and epinephrine has been reported occasionally.
Beta-adrenergic blocking agents
Patients who are receiving a beta-adrenergic blocking agent orally and timolol should be observed for potential additive effects of beta-blockade, both systemic and on intraocular pressure. The concomitant use of two topical beta-adrenergic blocking agents is not recommended.
Calcium antagonists
Caution should be used in the coadministration of beta-adrenergic blocking agents, such as timolol, and oral or intravenous calcium antagonists because of possible atrioventricular conduction disturbances, left ventricular failure, and hypotension. In patients with impaired cardiac function, coadministration should be avoided.
Catecholamine-depleting drugs
Close observation of the patient is recommended when a beta blocker is administered to patients receiving catecholamine-depleting drugs such as reserpine, because of possible additive effects and the production of hypotension and/or marked bradycardia, which may result in vertigo, syncope, or postural hypotension.
Digitalis and calcium antagonists
The concomitant use of beta-adrenergic blocking agents with digitalis and calcium antagonists may have additive effects in prolonging atrioventricular conduction time.
CYP2D6 inhibitors
Potentiated systemic beta-blockade (e.g., decreased heart rate, depression) has been reported during combined treatment with CYP2D6 inhibitors (e.g., quinidine, SSRIs) and timolol.
Clonidine
Oral beta-adrenergic blocking agents may exacerbate the rebound hypertension which can follow the withdrawal of clonidine. There have been no reports of exacerbation of rebound hypertension with ophthalmic timolol maleate.
Injectable epinephrine
Carcinogenesis, Mutagenesis, Impairment of Fertility
In a two-year study of timolol maleate administered orally to rats, there was a statistically significant increase in the incidence of adrenal pheochromocytomas in male rats administered 300 mg/kg/day (approximately 42,000 times the systemic exposure following the maximum recommended human ophthalmic dose). Similar differences were not observed in rats administered oral doses equivalent to approximately 14,000 times the maximum recommended human ophthalmic dose.
In a lifetime oral study in mice, there were statistically significant increases in the incidence of benign and malignant pulmonary tumors, benign uterine polyps and mammary adenocarcinomas in female mice at 500 mg/kg/day, (approximately 71,000 times the systemic exposure following the maximum recommended human ophthalmic dose), but not at 5 or 50 mg/kg/day (approximately 700 or 7,000, respectively, times the systemic exposure following the maximum recommended human ophthalmic dose). In a subsequent study in female mice, in which post-mortem examinations were limited to the uterus and the lungs, a statistically significant increase in the incidence of pulmonary tumors was again observed at 500 mg/kg/day.
The increased occurrence of mammary adenocarcinomas was associated with elevations in serum prolactin which occurred in female mice administered oral timolol at 500 mg/kg/day, but not at doses of 5 or 50 mg/kg/day. An increased incidence of mammary adenocarcinomas in rodents has been associated with administration of several other therapeutic agents that elevate serum prolactin, but no correlation between serum prolactin levels and mammary tumors has been established in humans. Furthermore, in adult human female subjects who received oral dosages of up to 60 mg of timolol maleate (the maximum recommended human oral dosage), there were no clinically meaningful changes in serum prolactin.
Timolol maleate was devoid of mutagenic potential when tested in vivo (mouse) in the micronucleus test and cytogenetic assay (doses up to 800 mg/kg) and in vitro in a neoplastic cell transformation assay (up to 100 mcg/mL). In Ames tests the highest concentrations of timolol employed, 5,000 or 10,000 mcg/plate, were associated with statistically significant elevations of revertants observed with tester strain TA100 (in seven replicate assays), but not in the remaining three strains. In the assays with tester strain TA100, no consistent dose response relationship was observed, and the ratio of test to control revertants did not reach 2. A ratio of 2 is usually considered the criterion for a positive Ames test.
Reproduction and fertility studies in rats demonstrated no adverse effect on male or female fertility at doses up to 21,000 times the systemic exposure following the maximum recommended human ophthalmic dose.
Pregnancy
Teratogenic effects
Teratogenicity studies with timolol in mice, rats, and rabbits at oral doses up to 50 mg/kg/day (7,000 times the systemic exposure following the maximum recommended human ophthalmic dose) demonstrated no evidence of fetal malformations. Although delayed fetal ossification was observed at this dose in rats, there were no adverse effects on postnatal development of offspring. Doses of 1000 mg/kg/day (142,000 times the systemic exposure following the maximum recommended human ophthalmic dose) were maternotoxic in mice and resulted in an increased number of fetal resorptions. Increased fetal resorptions were also seen in rabbits at doses of 14,000 times the systemic exposure following the maximum recommended human ophthalmic dose, in this case without apparent maternotoxicity.
There are no adequate and well-controlled studies in pregnant women. Timolol should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
Timolol maleate has been detected in human milk following oral and ophthalmic drug administration. Because of the potential for serious adverse reactions from timolol in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness of timolol maleate ophthalmic solution have been established when administered in pediatric patients aged 2 years and older. Use of timolol maleate ophthalmic solution in these children is supported by evidence from adequate and well controlled studies in children and adults. Safety and efficacy in pediatric patients below the age of 2 years have not been established.
-
ADVERSE REACTIONS
The most frequently reported adverse experiences have been burning and stinging upon instillation (approximately one in eight patients).
The following additional adverse experiences have been reported less frequently with ocular administration of this or other timolol maleate formulations:
Body as a Whole
Headache, asthenia/fatigue, and chest pain.
Cardiovascular
Bradycardia, arrhythmia, hypotension, hypertension, syncope, heart block, cerebral vascular accident, cerebral ischemia, cardiac failure, worsening of angina pectoris, palpitation, cardiac arrest, pulmonary edema, edema, claudication, Raynaud's phenomenon, and cold hands and feet.
Digestive
Nausea, diarrhea, dyspepsia, anorexia, and dry mouth.
Immunologic
Systemic lupus erythematosus.
Nervous System/Psychiatric
Dizziness, increase in signs and symptoms of myasthenia gravis, paresthesia, somnolence, insomnia, nightmares, behavioral changes and psychic disturbances including depression, confusion, hallucinations, anxiety, disorientation, nervousness, and memory loss.
Skin
Alopecia and psoriasiform rash or exacerbation of psoriasis.
Hypersensitivity
Signs and symptoms of systemic allergic reactions, including anaphylaxis, angioedema, urticaria, and localized and generalized rash.
Respiratory
Bronchospasm (predominantly in patients with preexisting bronchospastic disease), respiratory failure, dyspnea, nasal congestion, cough and upper respiratory infections.
Endocrine
Masked symptoms of hypoglycemia in diabetic patients [see Warnings].
Special Senses
Signs and symptoms of ocular irritation including conjunctivitis, blepharitis, keratitis, ocular pain, discharge (e.g., crusting), foreign body sensation, itching and tearing, and dry eyes; ptosis; decreased corneal sensitivity; cystoid macular edema; visual disturbances including refractive changes and diplopia; pseudopemphigoid; choroidal detachment following filtration surgery [see Precautions, General]; and tinnitus.
Urogenital
Retroperitoneal fibrosis, decreased libido, impotence, and Peyronie's disease.
The following additional adverse effects have been reported in clinical experience with ORAL timolol maleate or other ORAL beta-blocking agents and may be considered potential effects of ophthalmic timolol maleate: Allergic: Erythematous rash, fever combined with aching and sore throat, laryngospasm with respiratory distress; Body as a Whole: Extremity pain, decreased exercise tolerance, weight loss; Cardiovascular: Worsening of arterial insufficiency, vasodilatation; Digestive: Gastrointestinal pain, hepatomegaly, vomiting, mesenteric arterial thrombosis, ischemic colitis; Hematologic: Nonthrombocytopenic purpura; thrombocytopenic purpura, agranulocytosis; Endocrine: Hyperglycemia, hypoglycemia; Skin: Pruritus, skin irritation, increased pigmentation, sweating; Musculoskeletal: Arthralgia; Nervous System/Psychiatric: Vertigo, local weakness, diminished concentration, reversible mental depression progressing to catatonia, an acute reversible syndrome characterized by disorientation for time and place, emotional lability, slightly clouded sensorium, and decreased performance on neuropsychometrics; Respiratory: Rales, bronchial obstruction; Urogenital: Urination difficulties.
To report SUSPECTED ADVERSE REACTIONS, contact Sandoz Inc., at 1-800-525-8747 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
-
OVERDOSAGE
There have been reports of inadvertent overdosage with timolol maleate ophthalmic solution resulting in systemic effects similar to those seen with systemic beta-adrenergic blocking agents such as dizziness, headache, shortness of breath, bradycardia, bronchospasm, and cardiac arrest [see also Adverse Reactions].
Overdosage has been reported with timolol maleate tablets. A 30-year-old female ingested 650 mg of timolol maleate tablets (maximum recommended oral daily dose is 60 mg) and experienced second and third degree heart block. She recovered without treatment but approximately two months later developed irregular heartbeat, hypertension, dizziness, tinnitus, faintness, increased pulse rate, and borderline first degree heart block.
An in vitro hemodialysis study, using 14C timolol added to human plasma or whole blood, showed that timolol was readily dialyzed from these fluids; however, a study of patients with renal failure showed that timolol did not dialyze readily.
-
DOSAGE AND ADMINISTRATION
Timolol maleate ophthalmic solution is available in concentrations of 0.25 and 0.5%. The usual starting dose is one drop of 0.25% timolol maleate ophthalmic solution in the affected eye(s) twice a day. If the clinical response is not adequate, the dosage may be changed to one drop of 0.5% solution in the affected eye(s) twice a day.
Since in some patients the pressure-lowering response to timolol may require a few weeks to stabilize, evaluation should include a determination of intraocular pressure after approximately 4 weeks of treatment with timolol.
If the intraocular pressure is maintained at satisfactory levels, the dosage schedule may be changed to one drop once a day in the affected eye(s). Because of diurnal variations in intraocular pressure, satisfactory response to the once-a-day dose is best determined by measuring the intraocular pressure at different times during the day.
Dosages above one drop of 0.5% timolol maleate ophthalmic solution twice a day generally have not been shown to produce further reduction in intraocular pressure. If the patient's intraocular pressure is still not at a satisfactory level on this regimen, concomitant therapy with other agent(s) for lowering intraocular pressure can be instituted. The concomitant use of two topical beta-adrenergic blocking agents is not recommended [see Precautions, Drug Interactions, Beta-adrenergic blocking agents].
- HOW SUPPLIED
-
Instructions for Use
Timolol (tye-MOE-lawl) Maleate
Ophthalmic Solution
Read this Instructions for Use that comes with timolol maleate ophthalmic solution before you start using it and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or treatment.
Important information about timolol maleate ophthalmic solution:
- Use timolol maleate ophthalmic solution exactly as your doctor tells you to use it. Your doctor will tell you how much timolol maleate ophthalmic solution to use and when to use it.
- If you use other medicines in your eye, wait at least 10 minutes between using timolol maleate ophthalmic solution and your other eye medicines.
- Do not touch your eye or areas around your eye with the tip of the timolol maleate ophthalmic solution bottle. You may get bacteria on the tip of the bottle that can cause you to get an eye infection that can lead to serious eye damage or vision loss.
How should I use timolol maleate ophthalmic solution?
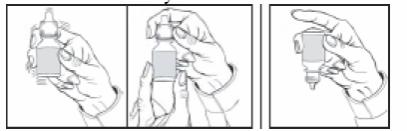
The DROP-TAINER* bottle is designed to assure the delivery of a precise dose of medication. Before using your DROP-TAINER bottle, read the complete instructions carefully.
1. If you use other topically applied ophthalmic medications, they should be administered at least 10 minutes before or after Timolol Maleate Ophthalmic Solution.
2. Wash hands before each use.
3. Before using the medication for the first time, be sure the Safety Seal on the bottle is unbroken.
4. Tear off the Safety Seal to break the seal.
5. Before each use, shake once and remove the screw cap.
6. Invert the bottle and hold the bottle between your thumb and middle finger, with the tips of the fingers pointing towards you.
7. Tilt your head back and position the bottle above the affected eye.
DO NOT TOUCH THE EYE WITH THE TIP OF THE DROPPER.
8. With the opposite hand, place a finger under the eye. Gently pull down until a "V" pocket is made between your eye and lower lid.
9. With the hand holding the bottle, place your index finger on the bottom of the bottle. Push the bottom of the bottle to dispense one drop of medication.
DO NOT SQUEEZE THE SIDES OF THE BOTTLE.
10. Repeat 6, 7, 8, & 9 with other eye if instructed to do so.
11. Replace screw cap by turning until firmly touching the bottle.
If you have any questions about the use of timolol maleate ophthalmic solutions, please consult your doctor.
Ophthalmic medications, if handled improperly, can become contaminated by common bacteria known to cause eye infections. Serious damage to the eye and subsequent loss of vision may result from using contaminated ophthalmic medications. If you think that your medication may be contaminated, or if you develop an eye infection, contact your doctor immediately concerning continued use of this bottle.
The dispenser tip is designed to provide a pre-measured drop; therefore, do NOT enlarge the hole of the dispenser tip.
After you have used all doses, there will be some Timolol Maleate Ophthalmic Solution left in the bottle. You should not be concerned since an extra amount of Timolol Maleate Ophthalmic Solution has been added and you will get the full amount of Timolol Maleate Ophthalmic Solution that your doctor prescribed. Do not attempt to remove excess medicine from the bottle.
How should I store Timolol Maleate Ophthalmic Solution?
- Store Timolol Maleate Ophthalmic Solution at room temperature between 59°F to 86°F (15°C to 30°C) in an upright position.
- Do not freeze Timolol Maleate Ophthalmic Solution.
- Keep Timolol Maleate Ophthalmic Solution out of light.
Keep Timolol Maleate Ophthalmic Solution and all medicines out of the reach of children.
If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for more information about Timolol Maleate Ophthalmic Solution that is written for health professionals.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
* DROP-TAINER is a registered trademark of Alcon Research, LLC.
Manufactured by
Alcon Laboratories, Inc.
Fort Worth, Texas 76134 for
Sandoz Inc., Princeton, NJ 08540
Revised: August 2019
- Timolol Maleate
-
INGREDIENTS AND APPEARANCE
TIMOLOL MALEATE
timolol maleate solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50090-3441(NDC:61314-227) Route of Administration OPHTHALMIC Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TIMOLOL MALEATE (UNII: P8Y54F701R) (TIMOLOL ANHYDROUS - UNII:5JKY92S7BR) TIMOLOL ANHYDROUS 5 mg in 1 mL Inactive Ingredients Ingredient Name Strength BENZALKONIUM CHLORIDE (UNII: F5UM2KM3W7) SODIUM PHOSPHATE, MONOBASIC, UNSPECIFIED FORM (UNII: 3980JIH2SW) SODIUM PHOSPHATE, DIBASIC, UNSPECIFIED FORM (UNII: GR686LBA74) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50090-3441-0 10 mL in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 04/20/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA074262 01/15/1996 Labeler - A-S Medication Solutions (830016429) Establishment Name Address ID/FEI Business Operations A-S Medication Solutions 830016429 RELABEL(50090-3441)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.