PULMICORT FLEXHALER- budesonide aerosol, powder
PULMICORT by
Drug Labeling and Warnings
PULMICORT by is a Prescription medication manufactured, distributed, or labeled by AstraZeneca Pharmaceuticals LP, AstraZeneca PLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PULMICORT FLEXHALER™ safely and effectively. See full prescribing information for PULMICORT FLEXHALER.
PULMICORT FLEXHALER™ (budesonide) inhalation powder
Initial U.S. Approval: 2006INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
For oral inhalation only.
- Patients 18 Years of Age and Older: For patients 18 years of age and older, the recommended starting dosage is 360 mcg twice daily. In some adult patients, a starting dose of 180 mcg twice daily may be adequate. The maximum dosage should not exceed 720 mcg twice daily (2.1)
- Patients 6 to 17 Years of Age: The recommended starting dosage is 180 mcg twice daily. In some pediatric patients, a starting dose of 360 mcg twice daily may be appropriate. The maximum dosage should not exceed 360 mcg twice daily (2.1)
DOSAGE FORMS AND STRENGTHS
FLEXHALER device containing budesonide (90 mcg or 180 mcg) as an inhalation powder (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Localized Infections: Candida albicans infection of the mouth and throat may occur. Monitor patients periodically for signs of adverse effects on the oral cavity. Advise patients to rinse the mouth following inhalation (5.1)
- Deterioration of Asthma or Acute Episodes: PULMICORT FLEXHALER should not be used for relief of acute symptoms. Patients require immediate re-evaluation during rapidly deteriorating asthma (5.2)
- Hypersensitivity Reactions: Anaphylaxis, rash, contact dermatitis, urticaria, angioedema, and bronchospasm have been reported with use of PULMICORT FLEXHALER. Discontinue PULMICORT FLEXHALER if such reactions occur (5.3)
- Immunosuppression: Potential worsening of infections (e.g., existing tuberculosis, fungal, bacterial, viral, or parasitic infection; or ocular herpes simplex). Use with caution in patients with these infections. More serious or even fatal course of chickenpox or measles can occur in susceptible patients (5.4)
- Transferring Patients from Systemic Corticosteroid Therapy: Risk of impaired adrenal function when transferring from oral steroids. Taper patients slowly from systemic corticosteroids if transferring to PULMICORT FLEXHALER (5.5)
- Hypercorticism and Adrenal Suppression: May occur with very high dosages or at the regular dosage in susceptible individuals. If such changes occur, reduce PULMICORT FLEXHALER slowly (5.6)
- Reduction in Bone Mineral Density with Long term Administration: Monitor patients with major risk factors for decreased bone mineral content (5.8)
- Effects on Growth: Monitor growth of pediatric patients (5.9)
- Glaucoma and Cataracts: Close monitoring is warranted (5.10)
- Paradoxical Bronchospasm: Discontinue PULMICORT FLEXHALER and institute alternative therapy if paradoxical bronchospasm occurs (5.11)
- Eosinophilic Conditions and Churg-Strauss Syndrome: Be alert to eosinophilic conditions (5.12)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥1%) are nasopharyngitis, nasal congestion, pharyngitis, rhinitis allergic, viral upper respiratory tract infection, nausea, viral gastroenteritis, otitis media, oral candidiasis (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca at 1-800-236-9933 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 10/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Treatment of Asthma
2 DOSAGE AND ADMINISTRATION
2.1 Asthma
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Local Effects
5.2 Deterioration of Asthma or Acute Episodes
5.3 Hypersensitivity Reactions Including Anaphylaxis
5.4 Immunosuppression
5.5 Transferring Patients from Systemic Corticosteroid Therapy
5.6 Hypercorticism and Adrenal Suppression
5.7 Interactions with Strong Cytochrome P450 3A4 Inhibitors
5.8 Reduction in Bone Mineral Density
5.9 Effects on Growth
5.10 Glaucoma and Cataracts
5.11 Paradoxical Bronchospasm and Upper Airway Symptoms
5.12 Eosinophilic Conditions and Churg-Strauss Syndrome
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Inhibitors of Cytochrome P450 3A4
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Asthma
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Oral Candidiasis
17.2 Not for Acute Symptoms
17.3 Hypersensitivity Including Anaphylaxis
17.4 Immunosuppression
17.5 Hypercorticism and Adrenal Suppression
17.6 Reduction in Bone Mineral Density
17.7 Reduced Growth Velocity
17.8 Ocular Effects
17.9 Use Daily
17.10 How to Use Pulmicort Flexhaler
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
PULMICORT FLEXHALER should be administered twice daily by the orally inhaled route only. After inhalation, the patient should rinse the mouth with water without swallowing [see Patient Counseling Information (17.1)].
Patients should be instructed to prime PULMICORT FLEXHALER prior to its initial use, and instructed to inhale deeply and forcefully each time the device is used.
The safety and efficacy of PULMICORT FLEXHALER when administered in excess of recommended doses have not been established.
After asthma stability has been achieved, it is desirable to titrate to the lowest effective dosage to reduce the possibility of side effects. For patients who do not respond adequately to the starting dose after 1-2 weeks of therapy with PULMICORT FLEXHALER, increasing the dose may provide additional asthma control.
2.1 Asthma
If asthma symptoms arise in the period between doses, an inhaled, short-acting beta2-agonist should be taken for immediate relief.
Patients 18 Years of Age and Older: For patients 18 years of age and older, the recommended starting dosage is 360 mcg twice daily. In some adult patients, a starting dose of 180 mcg twice daily may be adequate. The maximum dosage should not exceed 720 mcg twice daily.
Patients 6 to 17 Years of Age: The recommended starting dosage is 180 mcg twice daily. In some pediatric patients, a starting dose of 360 mcg twice daily may be appropriate. The maximum dosage should not exceed 360 mcg twice daily.
For all patients, it is desirable to titrate to the lowest effective dose after adequate asthma stability is achieved.
Improvement in asthma control following inhaled administration of budesonide can occur within 24 hours of initiation of treatment, although maximum benefit may not be achieved for 1 to 2 weeks, or longer. Individual patients will experience a variable onset and degree of symptom relief.
If a previously effective dosage regimen of PULMICORT FLEXHALER fails to provide adequate control of asthma, the therapeutic regimen should be re-evaluated and additional therapeutic options (e.g., replacing the lower strength of PULMICORT FLEXHALER with the higher strength or initiating oral corticosteroids) should be considered.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
The use of PULMICORT FLEXHALER is contraindicated in the following conditions:
- Primary treatment of status asthmaticus or other acute episodes of asthma where intensive measures are required.
- Severe hypersensitivity to milk proteins or any ingredients of PULMICORT FLEXHALER [see Warnings and Precautions (5.3), Description (11)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Local Effects
In clinical studies, the development of localized infections of the mouth and pharynx with Candida albicans has occurred in patients treated with PULMICORT FLEXHALER. When such an infection develops, it should be treated with appropriate local or systemic (i.e., oral antifungal) therapy while treatment with PULMICORT FLEXHALER continues, but at times, therapy with PULMICORT FLEXHALER may need to be interrupted. Patients should rinse the mouth after inhalation of PULMICORT FLEXHALER.
5.2 Deterioration of Asthma or Acute Episodes
PULMICORT FLEXHALER is not a bronchodilator and is not indicated for the rapid relief of bronchospasm or other acute episodes of asthma. Patients should be instructed to contact their physician immediately if episodes of asthma not responsive to their usual doses of bronchodilators occur during the course of treatment with PULMICORT FLEXHALER. During such episodes, patients may require therapy with oral corticosteroids.
An inhaled short acting beta2-agonist, not PULMICORT FLEXHALER, should be used to relieve acute symptoms such as shortness of breath. When prescribing PULMICORT FLEXHALER, the physician must also provide the patient with an inhaled, short-acting beta2-agonist (e.g., albuterol) for treatment of acute symptoms, despite regular twice-daily (morning and evening) use of PULMICORT FLEXHALER.
5.3 Hypersensitivity Reactions Including Anaphylaxis
Hypersensitivity reactions including anaphylaxis, rash, contact dermatitis, urticaria, angioedema, and bronchospasm have been reported with use of PULMICORT FLEXHALER. Discontinue PULMICORT FLEXHALER if such reactions occur [see Contraindications (4), Adverse Reactions (6)].
PULMICORT FLEXHALER contains small amounts of lactose, which contains trace levels of milk proteins. It is possible that cough, wheezing, or bronchospasm may occur in patients who have a severe milk protein allergy [see Contraindications (4), Adverse Reactions (6.2)].
5.4 Immunosuppression
Patients who are on drugs that suppress the immune system are more susceptible to infection than healthy individuals. Chicken pox and measles, for example, can have a more serious or even fatal course in susceptible children or adults using corticosteroids. In children or adults who have not had these diseases or been properly immunized, particular care should be taken to avoid exposure. How the dose, route, and duration of corticosteroid administration affects the risk of developing a disseminated infection is not known. The contribution of the underlying disease and/or prior corticosteroid treatment to the risk is also not known. If exposed to chicken pox, therapy with varicella zoster immune globulin (VZIG) or pooled intravenous immunoglobulin (IVIG), as appropriate, may be indicated. If exposed to measles, prophylaxis with pooled intramuscular immunoglobulin (IG) may be indicated (see the respective package inserts for complete VZIG and IG prescribing information). If chicken pox develops, treatment with antiviral agents may be considered. The immune responsiveness to varicella vaccine was evaluated in pediatric patients with asthma ages 12 months to 8 years with budesonide inhalation suspension.
An open-label, nonrandomized clinical study examined the immune responsiveness to varicella vaccine in 243 asthma patients 12 months to 8 years of age who were treated with budesonide inhalation suspension 0.25 mg to 1 mg daily (n=151) or non-corticosteroid asthma therapy (n=92) (i.e., beta2-agonists, leukotriene receptor antagonists, cromones). The percentage of patients developing a seroprotective antibody titer of ≥5.0 (gpELISA value) in response to the vaccination was similar in patients treated with budesonide inhalation suspension (85%), compared to patients treated with non-corticosteroid asthma therapy (90%). No patient treated with budesonide inhalation suspension developed chicken pox as a result of vaccination.
Inhaled corticosteroids should be used with caution, if at all, in patients with active or quiescent tuberculosis infection of the respiratory tract, untreated systemic fungal, bacterial, viral or parasitic infections, or ocular herpes simplex.
5.5 Transferring Patients from Systemic Corticosteroid Therapy
Particular care is needed for patients who are transferred from systemically active corticosteroids to PULMICORT FLEXHALER because deaths due to adrenal insufficiency have occurred in asthmatic patients during and after transfer from systemic corticosteroids to less systemically available inhaled corticosteroids. After withdrawal from systemic corticosteroids, a number of months are required for recovery of hypothalamic-pituitary-adrenal (HPA) function.
Patients who have been previously maintained on 20 mg or more per day of prednisone (or its equivalent) may be most susceptible, particularly when their systemic corticosteroids have been almost completely withdrawn.
During this period of HPA suppression, patients may exhibit signs and symptoms of adrenal insufficiency when exposed to trauma, surgery, or infection (particularly gastroenteritis) or other conditions associated with severe electrolyte loss. Although PULMICORT FLEXHALER may provide control of asthma symptoms during these episodes, in recommended doses it supplies less than normal physiological amounts of glucocorticoid systemically and does NOT provide the mineralocorticoid activity that is necessary for coping with these emergencies.
During periods of stress or a severe asthma attack, patients who have been withdrawn from systemic corticosteroids should be instructed to resume oral corticosteroids (in large doses) immediately and to contact their physicians for further instruction. These patients should also be instructed to carry a medical identification card indicating that they may need supplementary systemic corticosteroids during periods of stress or a severe asthma attack.
Patients requiring oral corticosteroids should be weaned slowly from systemic corticosteroid use after transferring to PULMICORT FLEXHALER. Prednisone reduction can be accomplished by reducing the daily prednisone dose by 2.5 mg on a weekly basis during therapy with PULMICORT FLEXHALER. Lung function (mean forced expiratory volume in 1 second [FEV1] or morning peak expiratory flow [PEF]), beta-agonist use, and asthma symptoms should be carefully monitored during withdrawal of oral corticosteroids. In addition to monitoring asthma signs and symptoms, patients should be observed for signs and symptoms of adrenal insufficiency such as fatigue, lassitude, weakness, nausea and vomiting, and hypotension.
Transfer of patients from systemic corticosteroid therapy to PULMICORT FLEXHALER may unmask allergic conditions previously suppressed by the systemic corticosteroid therapy, (e.g., rhinitis, conjunctivitis, eczema, arthritis, eosinophilic conditions). Some patients may experience symptoms of systemically active corticosteroid withdrawal (e.g., joint and/or muscular pain, lassitude, depression) despite maintenance or even improvement of respiratory function.
5.6 Hypercorticism and Adrenal Suppression
PULMICORT FLEXHALER will often help control asthma symptoms with less suppression of HPA function than therapeutically equivalent oral doses of prednisone. Since budesonide is absorbed into the circulation and can be systemically active at higher doses, the beneficial effects of PULMICORT FLEXHALER in minimizing HPA dysfunction may be expected only when recommended dosages are not exceeded and individual patients are titrated to the lowest effective dose. Since individual sensitivity to effects on cortisol production exists, physicians should consider this information when prescribing PULMICORT FLEXHALER.
Because of the possibility of systemic absorption of inhaled corticosteroids, patients treated with PULMICORT FLEXHALER should be observed carefully for any evidence of systemic corticosteroid effects. Particular care should be taken in observing patients postoperatively or during periods of stress for evidence of inadequate adrenal response.
It is possible that systemic corticosteroid effects such as hypercorticism and adrenal suppression (including adrenal crisis) may appear in a small number of patients, particularly when budesonide is administered at higher than recommended doses over prolonged periods of time. If such effects occur, the dosage of PULMICORT FLEXHALER should be reduced slowly, consistent with accepted procedures for reducing systemic corticosteroids and for management of asthma symptoms.
5.7 Interactions with Strong Cytochrome P450 3A4 Inhibitors
Caution should be exercised when considering the co-administration of PULMICORT FLEXHALER with ketoconazole, and other known strong CYP3A4 inhibitors (e.g., ritonavir, atazanavir, clarithromycin, indinavir, itraconazole, nefazodone, nelfinavir, saquinavir, telithromycin) because adverse effects related to increased systemic exposure to budesonide may occur [see Drug Interactions (7.1), Clinical Pharmacology (12.3)].
5.8 Reduction in Bone Mineral Density
Decreases in bone mineral density (BMD) have been observed with long-term administration of products containing inhaled corticosteroids. The clinical significance of small changes in BMD with regard to long-term consequences such as fracture is unknown. Patients with major risk factors for decreased bone mineral content, such as prolonged immobilization, family history of osteoporosis, post menopausal status, tobacco use, advance age, poor nutrition, or chronic use of drugs that can reduce bone mass (e.g., anticonvulsants, oral corticosteroids) should be monitored and treated with established standards of care.
5.9 Effects on Growth
Orally inhaled corticosteroids, including budesonide, may cause a reduction in growth velocity when administered to pediatric patients. Monitor the growth of pediatric patients receiving PULMICORT FLEXHALER routinely (e.g., via stadiometry). To minimize the systemic effects of orally inhaled corticosteroids, including PULMICORT FLEXHALER, titrate each patient’s dose to the lowest dosage that effectively controls his/her symptoms [see Dosage and Administration (2.1), Use in Specific Populations (8.4)].
5.10 Glaucoma and Cataracts
Glaucoma, increased intraocular pressure, and cataracts have been reported following the long-term administration of inhaled corticosteroids, including budesonide. Therefore, close monitoring is warranted in patients with a change in vision or with a history of increased intraocular pressure, glaucoma, and/or cataracts.
5.11 Paradoxical Bronchospasm and Upper Airway Symptoms
As with other inhaled asthma medications, PULMICORT FLEXHALER can produce paradoxical bronchospasm, which may be life threatening. If paradoxical bronchospasm occurs following dosing with PULMICORT FLEXHALER, it should be treated immediately with an inhaled, short-acting beta2-bronchodilator. PULMICORT FLEXHALER should be discontinued immediately, and alternative therapy should be instituted.
5.12 Eosinophilic Conditions and Churg-Strauss Syndrome
In rare cases, patients on inhaled corticosteroids may present with systemic eosinophilic conditions. Some of these patients have clinical features of vasculitis consistent with Churg-Strauss syndrome, a condition that is often treated with systemic corticosteroid therapy. These events usually, but not always, have been associated with the reduction and/or withdrawal of oral corticosteroid therapy following the introduction of inhaled corticosteroids. Physicians should be alert to eosinophilia, vasculitic rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy presenting in their patients. A causal relationship between budesonide and these underlying conditions has not been established.
-
6 ADVERSE REACTIONS
Systemic and inhaled corticosteroid use may result in the following:
- Candida albicans Infection [see Warnings and Precautions (5.1)]
- Hypersensitivity Including Anaphylaxis [see Warnings and Precautions (5.3)]
- Immunosuppression [see Warnings and Precautions (5.4)]
- Hypercorticism and Adrenal Suppression [see Warnings and Precautions (5.6)]
- Reduction in Bone Mineral Density [see Warnings and Precautions (5.8)]
- Growth Effects [see Warnings and Precautions (5.9), Use in Specific Populations (8.4)]
- Glaucoma and Cataracts [see Warnings and Precautions (5.10)]
- Eosinophilic Conditions and Churg-Strauss [see Warnings and Precautions (5.12)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
PULMICORT FLEXHALER
Patients 6 years and older
The incidence of common adverse reactions in Table 1 is based upon pooled data reported in patients treated with PULMICORT FLEXHALER 180 or 90 mcg in two double-blind, placebo-controlled clinical trials in which 226 patients (106 females and 120 males) with mild to moderate asthma, previously receiving bronchodilators, inhaled corticosteroids, or both, were treated with PULMICORT FLEXHALER, administered as 360 mcg twice daily for 12 weeks. In these trials, the patients on PULMICORT FLEXHALER had a mean age of 28 years (range 6-80 years) and were predominantly Caucasian (59.7%) and Asian (31.4%). Table 1 includes all adverse reactions (regardless of investigator causality assessment) that occurred at a rate of ≥1% in the PULMICORT FLEXHALER group and more commonly than the placebo group.
Table 1 - Adverse Reactions occurring at an incidence of ≥1% and more commonly than placebo in the PULMICORT FLEXHALER group: pooled data from two 12-week, double-blind, placebo-controlled clinical asthma trials in patients 6 years and older Adverse Event
PULMICORT FLEXHALER
360 mcg twice daily
N=226
%
Placebo
N=230
%
Nasopharyngitis
9.3
8.3
Nasal congestion
2.7
0.4
Pharyngitis
2.7
1.7
Rhinitis allergic
2.2
1.3
Viral upper respiratory tract infection
2.2
1.3
Nausea
1.8
0.9
Viral gastroenteritis
1.8
0.4
Otitis media
1.3
0.9
Oral candidiasis
1.3
0.4
Average exposure duration (days)
76.2
68.2
Long-Term Safety in Patients 6 years of age and older
Non-placebo controlled long-term studies in children (at doses up to 360 mcg daily), and adolescent and adult subjects (at doses up to 720 mcg daily), treated for up to one year with PULMICORT FLEXHALER, revealed a similar pattern and incidence of adverse events.
PULMICORT TURBUHALER; a different PULMICORT DPI
The following adverse reactions occurred in placebo-controlled clinical trials with similar or lower doses with inhaled budesonide via a different PULMICORT dry powder inhaler with an incidence of ≥1% in the budesonide group and were more common than in the placebo group:
≥3%: respiratory infection, sinusitis, headache, pain, back pain, fever.
≥1-3%: neck pain, syncope, abdominal pain, dry mouth, vomiting, weight gain, fracture, myalgia, hypertonia, migraine, ecchymosis, insomnia, infection, taste perversion, voice alteration.
Higher doses of inhaled budesonide (800 mcg twice daily) via a different PULMICORT dry powder inhaler resulted in an increased incidence of voice alteration, flu syndrome, dyspepsia, gastroenteritis, nausea, and back pain, compared with doses of 400 mcg twice daily.
In a 20-week trial in adult asthmatics who previously required oral corticosteroids, the incidence of adverse reactions was evaluated with 400 mcg twice daily (N=53) and 800 mcg twice daily (N=53) of inhaled budesonide via a different PULMICORT dry powder inhaler and compared with placebo (N=53). In considering these data, the increased average duration of exposure for inhaled budesonide patients (78 days for inhaled budesonide vs. 41 days for placebo) should be taken into account. Adverse reactions, regardless of investigator causality assessment, reported in more than five patients in the budesonide group and which occurred more commonly than the placebo group in decreasing order of frequency include: respiratory infection, sinusitis, headache, oral candidiasis, pain, asthenia, dyspepsia, arthralgia, cough increased, nausea and rhinitis.
6.2 Postmarketing Experience
The following adverse reactions have been reported during post-approval use of PULMICORT FLEXHALER. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune system disorders: immediate and delayed hypersensitivity reactions including anaphylactic reaction, angioedema, bronchospasm, rash, contact dermatitis, urticaria, and cough, wheezing or bronchospasm in patients with severe milk protein hypersensitivity [see Warnings and Precautions (5.3), Contraindications (4)]
Endocrine disorders: symptoms of hypocorticism and hypercorticism [see Warnings and Precautions (5.6)]
Eye disorders: cataracts, glaucoma, increased intraocular pressure [see Warnings and Precautions (5.10)]
Psychiatric disorders: psychiatric symptoms including psychosis, depression, aggressive reactions, irritability, nervousness, restlessness, and anxiety
Respiratory, thoracic, and mediastinal disorders: throat irritation
Skin and subcutaneous tissue disorders: skin bruising
-
7 DRUG INTERACTIONS
7.1 Inhibitors of Cytochrome P450 3A4
The main route of metabolism of corticosteroids, including budesonide, is via cytochrome P450 (CYP) isoenzyme 3A4 (CYP3A4). After oral administration of ketoconazole, a strong inhibitor of CYP3A4, the mean plasma concentration of orally administered budesonide increased. Concomitant administration of CYP3A4 may inhibit the metabolism of, and increase the systemic exposure to, budesonide. Caution should be exercised when considering the co-administration of PULMICORT FLEXHALER with long-term ketoconazole and other known strong CYP3A4 inhibitors (e.g., ritonavir, atazanavir, clarithromycin, indinavir, itraconazole, nefazodone, nelfinavir, saquinavir, telithromycin) [see Warnings and Precautions (5.7)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate well-controlled studies of PULMICORT FLEXHALER in pregnant women. However, there are published studies on the use of budesonide, the active ingredient in PULMICORT FLEXHALER, in pregnant women. In animal reproduction studies, budesonide, administered by the subcutaneous route, caused structural abnormalities, was embryocidal, and reduced fetal weights in rats and rabbits at less than the maximum recommended human daily inhalation dose (MRHDID), but these effects were not seen in rats that received inhaled doses approximately 2 times the MRHDID (see Data). Studies of pregnant women have not shown that inhaled budesonide increases the risk of abnormalities when administered during pregnancy. Experience with oral corticosteroids suggests that rodents are more prone to structural abnormalities from corticosteroid exposure than humans.
The estimated background risk of major birth defects and miscarriage of the indicated populations is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal risk
In women with poorly or moderately controlled asthma, there is an increased risk of several perinatal adverse outcomes such as preeclampsia in the mother and prematurity, low birth weight, and small for gestational age in the neonate. Pregnant women with asthma should be closely monitored and medication adjusted as necessary to maintain optimal asthma control.
Labor or Delivery
There are no well-controlled human studies that have investigated the effects of PULMICORT FLEXHALER during labor and delivery.
Data
Human Data
Studies of pregnant women have not shown that inhaled budesonide increases the risk of abnormalities when administered during pregnancy. The results from a large population-based prospective cohort epidemiological study reviewing data from three Swedish registries covering approximately 99% of the pregnancies from 1995-1997 (i.e., Swedish Medical Birth Registry; Registry of Congenital Malformations; Child Cardiology Registry) indicate no increased risk for congenital malformations from the use of inhaled budesonide during early pregnancy. Congenital malformations were studied in 2014 infants born to mothers reporting the use of inhaled budesonide for asthma in early pregnancy (usually 10-12 weeks after the last menstrual period), the period when most major organ malformations occur. The rate of recorded congenital malformations was similar compared to the general population rate (3.8% vs. 3.5%, respectively). In addition, after exposure to inhaled budesonide, the number of infants born with orofacial clefts was similar to the expected number in the normal population (4 children vs. 3.3, respectively).
These same data were utilized in a second study bringing the total to 2534 infants whose mothers were exposed to inhaled budesonide. In this study, the rate of congenital malformations among infants whose mothers were exposed to inhaled budesonide during early pregnancy was not different from the rate for all newborn babies during the same period (3.6%).
Animal Data
In a fertility and reproduction study, male rats were subcutaneously dosed for 9 weeks and females for 2 weeks prior to pairing and throughout the mating period. Females were dosed up until weaning of their offspring. Budesonide caused a decrease in prenatal viability and viability in the pups at birth and during lactation, along with a decrease in maternal body-weight gain, at doses 0.1 times the MRHDID (on a mcg/m2 basis at maternal subcutaneous doses of 20 mcg/kg/day and above). No such effects were noted at a dose 0.03 times the MRHDID (on a mcg/m2 basis at a maternal subcutaneous dose of 5 mcg/kg/day).
In an embryo-fetal development study in pregnant rabbits dosed during the period of organogenesis from gestation days 6-18, budesonide produced fetal loss, decreased fetal weight, and skeletal abnormalities at doses 0.3 times the MRHDID (on a mcg/m2 basis at a maternal subcutaneous dose of 25 mcg/kg/day). In an embryo-fetal development study in pregnant rats dosed during the period of organogenesis from gestation days 6-15, budesonide produced similar adverse fetal effects at doses approximately 4 times the MRHDID (on a mcg/m2 basis at a maternal subcutaneous dose of 500 mcg/kg/day). In another embryo-fetal development study in pregnant rats, no structural abnormalities or embryocidal effects were seen at doses approximately 2 times the MRHDID (on a mcg/m2 basis at maternal inhalation doses up to 250 mcg/kg/day).
In a peri-and post-natal development study, rats dosed from gestation day 15 to postpartum day 21, budesonide had no effects on delivery, but did have an effect on growth and development of offspring. Offspring survival was reduced and surviving offspring had decreased mean body weights at birth and during lactation at doses 0.1 times the MRHDID and higher (on a mcg/m2 basis at maternal subcutaneous doses of 20 mcg/kg/day and higher). These findings occurred in the presence of maternal toxicity.
8.2 Lactation
Risk Summary
There are no available data on the effects of PULMICORT FLEXHALER on the breastfed child or on milk production. Budesonide, like other inhaled corticosteroids, is present in human milk [see Data]. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for PULMICORT FLEXHALER and any potential adverse effects on the breastfed infant from PULMICORT FLEXHALER or from the underlying maternal condition.
Data
Human data with budesonide delivered via dry powder inhaler indicates that the total daily oral dose of budesonide available in breast milk to the infant is approximately 0.3% to 1% of the dose inhaled by the mother [seeClinical Pharmacology (12.3)].
8.4 Pediatric Use
In a 12-week pivotal study, 204 patients 6 to 17 years of age were treated with PULMICORT FLEXHALER twice daily [see Clinical Studies (14.1)]. Efficacy results in this age group were similar to those observed in patients 18 years and older. There were no obvious differences in the type or frequency of adverse events reported in this age group compared with patients 18 years of age and older.
The safety and effectiveness of PULMICORT FLEXHALER in asthma patients below 6 years of age have not been established.
Controlled clinical studies have shown that orally inhaled corticosteroids, including budesonide, may cause a reduction in growth velocity in pediatric patients. This effect has been observed in the absence of laboratory evidence of hypothalamic-pituitary-adrenal (HPA) axis suppression, suggesting that growth velocity is a more sensitive indicator of systemic corticosteroid exposure in pediatric patients than some commonly used tests of HPA-axis function. The long-term effects of this reduction in growth velocity associated with orally inhaled corticosteroids including the impact on final adult height are unknown. The potential for “catch up” growth following discontinuation of treatment with orally inhaled corticosteroids has not been adequately studied.
In a study of asthmatic children 5-12 years of age, those treated with inhaled budesonide via a different PULMICORT dry powder inhaler 200 mcg twice daily (n=311) had a 1.1-centimeter reduction in growth compared with those receiving placebo (n=418) at the end of one year; the difference between these two treatment groups did not increase further over three years of additional treatment. By the end of four years, children treated with a different PULMICORT dry powder inhaler and children treated with placebo had similar growth velocities. Conclusions drawn from this study may be confounded by the unequal use of corticosteroids in the treatment groups and inclusion of data from patients attaining puberty during the course of the study.
The administration of inhaled budesonide via a different PULMICORT dry-powder inhaler in doses up to 800 mcg/day (mean daily dose 445 mcg/day) or via a pressurized metered-dose inhaler in doses up to 1200 mcg/day (mean daily dose 620 mcg/day) to 216 pediatric patients (age 3 to 11 years) for 2 to 6 years had no significant effect on statural growth compared with non-corticosteroid therapy in 62 matched control patients. However, the long-term effect of inhaled budesonide on growth is not fully known.
The growth of pediatric patients receiving orally inhaled corticosteroids, including PULMICORT FLEXHALER, should be monitored (e.g., via stadiometry). If a child or adolescent on any corticosteroid appears to have growth suppression, the possibility that he/she is particularly sensitive to this effect should be considered. The potential growth effects of prolonged treatment should be weighed against clinical benefits obtained. To minimize the systemic effects of inhaled corticosteroids, including PULMICORT FLEXHALER, each patient should be titrated to the lowest dose that effectively controls his/her asthma [see Dosage and Administration (2)].
8.5 Geriatric Use
Of the total number of patients in controlled clinical studies receiving inhaled budesonide, 153 (n=11 treated with PULMICORT FLEXHALER) were 65 years of age or older and one was age 75 years or older. No overall differences in safety were observed between these patients and younger patients. Clinical studies did not include sufficient numbers of patients aged 65 years and over to determine differences in efficacy between elderly and younger patients. Other reported clinical or medical surveillance experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Hepatic Impairment
Formal pharmacokinetic studies using PULMICORT FLEXHALER have not been conducted in patients with hepatic impairment. However, since budesonide is predominantly cleared by hepatic metabolism, impairment of liver function may lead to accumulation of budesonide in the plasma. Therefore, patients with hepatic disease should be closely monitored.
-
10 OVERDOSAGE
The potential for acute toxic effects following overdose of PULMICORT FLEXHALER is low. If used at excessive doses for prolonged periods, systemic corticosteroid effects such as hypercorticism may occur [see Warnings and Precautions (5.6)]. Another budesonide-containing dry powder inhaler at 3200 mcg daily administered for 6 weeks caused a significant reduction (27%) in the plasma cortisol response to a 6-hour infusion of ACTH compared with placebo (+1%). The corresponding effect of 10 mg prednisone daily was a 35% reduction in the plasma cortisol response to ACTH.
Postmarketing experience showed that acute overdose of inhaled budesonide commonly remained asymptomatic. The use of excessive doses (up to 6400 mcg daily) for prolonged periods showed systemic corticosteroid effects such as hypercorticism.
-
11 DESCRIPTION
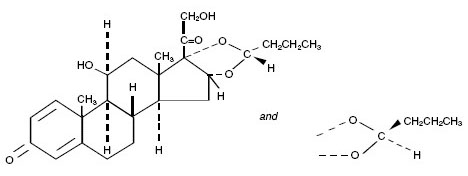
Budesonide, the active component of PULMICORT FLEXHALER, is a corticosteroid designated chemically as (RS)-11β, 16α, 17,21-Tetrahydroxypregna-1,4-diene-3,20-dione cyclic 16,17-acetal with butyraldehyde. Budesonide is provided as a mixture of two epimers (22R and 22S). The empirical formula of budesonide is C25H34O6 and its molecular weight is 430.5. Its structural formula is:
Budesonide is a white to off-white, tasteless, odorless powder that is practically insoluble in water and in heptane, sparingly soluble in ethanol, and freely soluble in chloroform. Its partition coefficient between octanol and water at pH 7.4 is 1.6 x 103.
PULMICORT FLEXHALER is an inhalation-driven multi-dose dry powder inhaler containing a formulation of 1 mg per actuation of micronized budesonide and micronized lactose monohydrate which contains trace levels of milk proteins [see Contraindications (4), Adverse Reactions (6.2)]. Each actuation of PULMICORT FLEXHALER 180 mcg delivers 160 mcg budesonide from the mouthpiece and each actuation of PULMICORT FLEXHALER 90 mcg delivers 80 mcg budesonide from the mouthpiece (based on in vitro testing at 60 L/min for 2 sec). Each PULMICORT FLEXHALER 180 mcg contains 120 actuations and each PULMICORT FLEXHALER 90 mcg contains 60 actuations.
In vitro testing has shown that the dose delivery for PULMICORT FLEXHALER is dependent on airflow through the device, as evidenced by a decrease in the fine particle dose at a flow rate of 30 L/min to a value that is approximately 40-50% of that produced at 60 L/min. At a flow rate of 40 L/min, the fine particle dose is approximately 70% of that produced at 60 L/min. Patient factors such as inspiratory flow rates will also affect the dose delivered to the lungs of patients in actual use [see Patient Information and Instructions for Use]. In asthmatic children age 6 to 17 (N=516, FEV1 2.29 [0.97– 4.28]) peak inspiratory flow (PIF) through PULMICORT FLEXHALER was 72.5 [19.1 – 103.6] L/min). Inspiratory flows were not measured in the adult pivotal study. Patients should be carefully instructed on the use of this drug product to assure optimal dose delivery.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Budesonide is an anti-inflammatory corticosteroid that exhibits potent glucocorticoid activity and weak mineralocorticoid activity. In standard in vitro and animal models, budesonide has approximately a 200-fold higher affinity for the glucocorticoid receptor and a 1000-fold higher topical anti-inflammatory potency than cortisol (rat croton oil ear edema assay). As a measure of systemic activity, budesonide is 40 times more potent than cortisol when administered subcutaneously and 25 times more potent when administered orally in the rat thymus involution assay. The clinical significance of this is unknown.
The activity of PULMICORT FLEXHALER is due to the parent drug, budesonide. In glucocorticoid receptor affinity studies, the 22R form was two times as active as the 22S epimer. In vitro studies indicated that the two forms of budesonide do not interconvert.
The precise mechanism of corticosteroid actions on inflammation in asthma is not known. Inflammation is an important component in the pathogenesis of asthma. Corticosteroids have a wide range of inhibitory activities against multiple cell types (e.g., mast cells, eosinophils, neutrophils, macrophages, and lymphocytes) and mediators (e.g., histamine, eicosanoids, leukotrienes, and cytokines) involved in allergic and non-allergic-mediated inflammation. These anti-inflammatory actions of corticosteroids may contribute to their efficacy in asthma.
Studies in asthmatic patients have shown a favorable ratio between topical anti-inflammatory activity and systemic corticosteroid effects over a wide range of doses of inhaled budesonide. This is explained by a combination of a relatively high local anti-inflammatory effect, extensive first pass hepatic degradation of orally absorbed drug (85-95%), and the low potency of formed metabolites (see below).
12.2 Pharmacodynamics
To confirm that systemic absorption is not a significant factor in the clinical efficacy of inhaled budesonide, a clinical study in patients with asthma was performed comparing 400 mcg budesonide administered via a pressurized metered-dose inhaler with a tube spacer to 1400 mcg of oral budesonide and placebo. The study demonstrated the efficacy of inhaled budesonide but not orally administered budesonide, even though systemic budesonide exposure was comparable for both treatments, indicating that the inhaled treatment is working locally in the lung. Thus, the therapeutic effect of conventional doses of orally inhaled budesonide are largely explained by its direct action on the respiratory tract.
Inhaled budesonide has been shown to decrease airway reactivity in various challenge models, including histamine, methacholine, sodium metabisulfite, and adenosine monophosphate in patients with hyperreactive airways. The clinical relevance of these models is not certain.
Pre-treatment with inhaled budesonide 1600 mcg daily (800 mcg twice daily) for 2 weeks reduced the acute (early-phase reaction) and delayed (late-phase reaction) decrease in FEV1 following inhaled allergen challenge.
HPA Axis effects: The effects of inhaled budesonide on the hypothalamic-pituitary-adrenal (HPA) axis were studied in 905 adults and 404 pediatric patients with asthma. For most patients, the ability to increase cortisol production in response to stress, as assessed by cosyntropin (ACTH) stimulation test, remained intact with inhaled budesonide treatment at recommended doses. For adult patients treated with 100, 200, 400, or 800 mcg twice daily for 12 weeks, 4%, 2%, 6%, and 13% respectively, had an abnormal stimulated cortisol response (peak cortisol <14.5 mcg/dL assessed by liquid chromatography following short-cosyntropin test) as compared with 8% of patients treated with placebo. Similar results were obtained in pediatric patients. In another study in adults, doses of 400, 800 and 1600 mcg of inhaled budesonide twice daily for 6 weeks were examined; 1600 mcg twice daily (twice the maximum recommended dose) resulted in a 27% reduction in stimulated cortisol (6-hour ACTH infusion) while 10 mg prednisone resulted in a 35% reduction. In this study, no patient taking doses of 400 and 800 mcg twice daily met the criterion for an abnormal stimulated cortisol response (peak cortisol <14.5 mcg/dL assessed by liquid chromatography) following ACTH infusion. An open-label, long-term follow-up of 1133 patients for up to 52 weeks confirmed the minimal effect on the HPA axis (both basal and stimulated plasma cortisol) of inhaled budesonide when administered at doses ranging from 100 to 800 mcg twice daily. In patients who had previously been oral steroid-dependent, use of inhaled budesonide at doses ranging from 100 to 800 mcg twice daily was associated with higher stimulated cortisol response compared with baseline following 1 year of therapy.
12.3 Pharmacokinetics
Absorption
After oral administration of budesonide, peak plasma concentration was achieved in about 1 to 2 hours and the absolute systemic availability was 6-13%. In contrast, most of budesonide delivered to the lungs is systemically absorbed. In healthy subjects, 34% of the metered dose was deposited in the lungs (as assessed by plasma concentration method and using a different budesonide containing dry-powder inhaler) with an absolute systemic availability of 39% of the metered dose. Peak steady-state plasma concentrations of budesonide delivered from PULMICORT FLEXHALER in adults with asthma (n=39) occurred at approximately 10 minutes post-dose and averaged 0.6 and 1.6 nmol/L at doses of 180 mcg once daily and 360 mcg twice daily, respectively.
In asthmatic patients, budesonide showed a linear increase in AUC and Cmax with increasing dose after both a single dose and repeated dosing of inhaled budesonide.
Distribution
The volume of distribution of budesonide was approximately 3 L/kg. It was 85-90% bound to plasma proteins. Protein binding was constant over the concentration range (1-100 nmol/L) achieved with, and exceeding, recommended doses of PULMICORT FLEXHALER. Budesonide showed little or no binding to corticosteroid binding globulin. Budesonide rapidly equilibrated with red blood cells in a concentration independent manner with a blood/plasma ratio of about 0.8.
Metabolism
In vitro studies with human liver homogenates have shown that budesonide is rapidly and extensively metabolized. Two major metabolites formed via cytochrome P450 (CYP) isoenzyme 3A4 (CYP3A4) catalyzed biotransformation have been isolated and identified as 16α-hydroxyprednisolone and 6β-hydroxybudesonide. The corticosteroid activity of each of these two metabolites is less than 1% of that of the parent compound. No qualitative differences between the in vitro and in vivo metabolic patterns have been detected. Negligible metabolic inactivation was observed in human lung and serum preparations.
Excretion/Elimination
The 22R form of budesonide was preferentially cleared by the liver with systemic clearance of 1.4 L/min vs. 1.0 L/min for the 22S form. The terminal half-life, 2 to 3 hours, was the same for both epimers and was independent of dose. Budesonide was excreted in urine and feces in the form of metabolites. Approximately 60% of an intravenous radiolabeled dose was recovered in the urine. No unchanged budesonide was detected in the urine.
Special Populations
No clinically relevant pharmacokinetic differences have been identified due to race, sex, or advanced age.
Geriatric
The pharmacokinetics of PULMICORT FLEXHALER in geriatric patients have not been specifically studied.
Pediatric
Following intravenous dosing in pediatric patients age 10-14 years, plasma half-life was shorter than in adults (1.5 hours vs. 2.0 hours in adults). In the same population following inhalation of budesonide via a pressurized metered-dose inhaler, absolute systemic availability was similar to that in adults.
Peak steady-state plasma concentrations of budesonide delivered via PULMICORT FLEXHALER in children and adolescents with asthma (n=14) occurred at approximately 15 to 30 minutes post-dose and averaged 0.4 and 1.5 nmol/L at doses of 180 mcg once daily and 360 mcg twice daily, respectively.
Nursing Mothers
The disposition of budesonide when delivered by inhalation from a dry powder inhaler at doses of 200 or 400 mcg twice daily for at least 3 months was studied in eight lactating women with asthma from 1 to 6 months postpartum. Systemic exposure to budesonide in these women appears to be comparable to that in non-lactating women with asthma from other studies. Breast milk obtained over eight hours post-dose revealed that the maximum concentration of budesonide for the 400 and 800 mcg doses was 0.39 and 0.78 nmol/L, respectively, and occurred within 45 minutes after dosing. The estimated oral daily dose of budesonide from breast milk to the infant is approximately 0.007 and 0.014 mcg/kg/day for the two dose regimens used in this study, which represents approximately 0.3% to 1% of the dose inhaled by the mother. Budesonide levels in plasma samples obtained from five infants at about 90 minutes after breastfeeding (and about 140 minutes after drug administration to the mother) were below quantifiable levels (<0.02 nmol/L in four infants and <0.04 nmol/L in one infant) [see Use In Specific Populations (8.2)].
Renal or Hepatic Insufficiency
There are no data regarding the specific use of PULMICORT FLEXHALER in patients with hepatic or renal impairment. Reduced liver function may affect the elimination of corticosteroids. The pharmacokinetics of budesonide were affected by compromised liver function as evidenced by a doubled systemic availability after oral ingestion. The intravenous pharmacokinetics of budesonide were, however, similar in cirrhotic patients and in healthy subjects.
Drug-Drug Interactions
Inhibitors of cytochrome P450 enzymes
Ketoconazole: Ketoconazole, a strong inhibitor of cytochrome P450 (CYP) isoenzyme 3A4 (CYP3A4), the main metabolic enzyme for corticosteroids, increased plasma levels of orally ingested budesonide [see Warnings and Precautions (5.7), Drug Interactions (7.1)].
Cimetidine: At recommended doses, cimetidine, a nonspecific inhibitor of CYP enzymes, had a slight but clinically insignificant effect on the pharmacokinetics of oral budesonide.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 104-week oral study in Sprague-Dawley rats, a statistically significant increase in the incidence of gliomas was observed in male rats receiving an oral dose of 50 mcg/kg/day (approximately 0.3 times the MRHDID in adults and children 6 to 17 years of age on a mcg/m2 basis). No tumorigenicity was seen in male rats at oral doses up to 25 mcg/kg (approximately 0.2 times the MRHDID in adults and children 6 to 17 years of age, on a mcg/m2 basis) and in female rats at oral doses up to 50 mc/kg (approximately 0.3 times, the MRHDID doses in adults and children 6 to 17 years of age, respectively, on a mcg/m2 basis). In two additional two-year studies in male Fischer and Sprague-Dawley rats, budesonide caused no gliomas at an oral dose of 50 mcg/kg (approximately 0.3 times the MRHDID in adults and children 6 to 17 years of age, respectively, on a mcg/m2 basis). However, in the male Sprague-Dawley rats, budesonide caused a statistically significant increase in the incidence of hepatocellular tumors at an oral dose of 50 mcg/kg (approximately 0.3 times the MRHDID in adults and children 6 to 17 years of age on a mcg/m2 basis). The concurrent reference corticosteroids (prednisone and triamcinolone acetonide) in these two studies showed similar findings.
There was no evidence of a carcinogenic effect when budesonide was administered orally for 91 weeks to mice at doses up to 200 mcg/kg/day (approximately 0.7 times the MRHDID in adults and children 6 to 17 years of age on a mcg/m2 basis). Budesonide was not mutagenic or clastogenic in six different test systems: Ames Salmonella/microsome plate test, mouse micronucleus test, mouse lymphoma test, chromosome aberration test in human lymphocytes, sex-linked recessive lethal test in Drosophila melanogaster, and DNA repair analysis in rat hepatocyte culture.
Fertility and reproductive performance were unaffected in rats at subcutaneous doses up to 80 mcg/kg (approximately 0.5 times the MRHDID in adults on a mcg/m2 basis). At a subcutaneous dose of 20 mcg/kg/day (approximately 0.1 times the maximum recommended daily inhalation dose in adults on a mcg/m2 basis), decreases in maternal body weight gain, prenatal viability, and viability of the young at birth and during lactation were observed. No such effects were noted at 5 mcg/kg (approximately 0.03 times the MRHDID in adults on a mcg/m2 basis).
-
14 CLINICAL STUDIES
14.1 Asthma
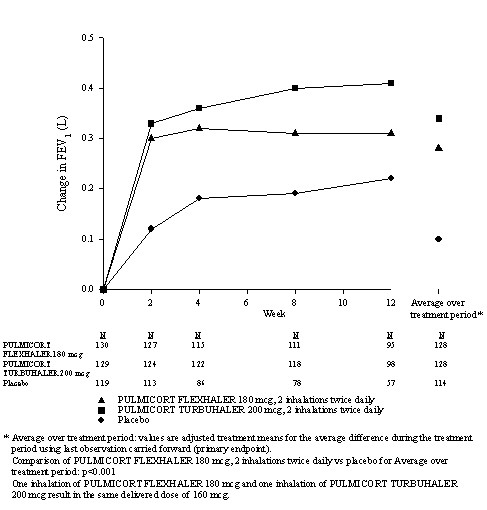
The safety and efficacy of PULMICORT FLEXHALER were evaluated in two 12-week, double-blind, randomized, parallel-group, placebo-controlled clinical studies conducted at sites in the United States and Asia involving 1137 patients aged 6 to 80 years with mild to moderate asthma. Study 1 evaluated PULMICORT FLEXHALER 180 mcg, PULMICORT TURBUHALER 200 mcg, and placebo, each administered as 1 inhalation once daily or 2 inhalations twice daily in patients 18 years of age and older with mild to moderate asthma previously treated with inhaled corticosteroids. The delivered dose of PULMICORT FLEXHALER 180 mcg and PULMICORT TURBUHALER 200 mcg are the same; each delivers 160 mcg from the mouthpiece. Study 2 evaluated PULMICORT FLEXHALER 90 mcg, 2 inhalations once daily or 4 inhalations twice daily, PULMICORT TURBUHALER 200 mcg, 1 inhalation once daily or 2 inhalations twice daily, and placebo in pediatric patients aged 6 to 17 years with mild to moderate asthma. Both of the studies had a 2-week placebo treatment run-in period followed by a 12-week randomized treatment period. The primary endpoint was the difference between baseline and the mean of the treatment-period FEV1 (adults) or FEV1 % predicted (children).
Patients ≥ 18 years of age and older (Study 1)
This study enrolled 621 patients aged ≥18 to 80 years with mild-to-moderate asthma (mean baseline % predicted FEV1 64.3%) whose symptoms were previously controlled on inhaled corticosteroids. Mean change from baseline in FEV1 in the PULMICORT FLEXHALER 180 mcg, 2 inhalations twice-daily group was 0.28 liters, as compared to 0.10 liters in the placebo group (p<0.001). Secondary endpoints of morning and evening peak expiratory flow rate, daytime asthma symptom severity, nighttime asthma symptom severity, daily rescue medication use, and the percentage of patients who met predefined asthma related withdrawal criteria showed differences from baseline favoring PULMICORT FLEXHALER over placebo (p<0.001).
12-Week Trial in Adult Patients with Mild to Moderate Asthma (Study 1) Mean Change from Baseline in FEV1 (L)
- Footnote: PULMICORT TURBUHALER; a different PULMICORT DPI. Statistical model is analysis of covariance with treatment and region (US/Asia) as factors and the baseline value as the covariate.
Patients 6 to 17 years of age (Study 2)
This study enrolled 516 patients aged 6 to 17 years with mild asthma (mean baseline % predicted FEV1 84.9%). The study population included patients previously treated with inhaled corticosteroids for no more than 30 days before the study began (4%) and patients who were naïve to inhaled corticosteroids (96%). Mean change from baseline in % predicted FEV1 during the 12-week treatment period in the PULMICORT FLEXHALER 90 mcg, 4 inhalations twice daily treatment group was 5.6 compared with 0.2 in the placebo group (p<0.001). Secondary endpoints of morning and evening PEF showed differences from baseline favoring PULMICORT FLEXHALER over placebo (p<0.001).
12-Week Trial in Pediatric Patients With Mild Asthma (Study 2) Mean Change from Baseline in Percent Predicted FEV1
- Footnote: PULMICORT TURBUHALER; a different PULMICORT DPI. Statistical model is analysis of covariance with treatment and region (US/Asia) as factors and the baseline value as the covariate.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
PULMICORT FLEXHALER is available as a dry powder for inhalation containing budesonide in the following 2 strengths: 90 mcg and 180 mcg. Each dosage strength contains 60 or 120 actuations per device. 180 mcg/dose (NDC: 0186-0916-12) with a target fill weight of 225 mg (range 200-250), and 90 mcg/dose, 60 dose (NDC: 0186-0917-06) with a target fill weight of 165 mg (range 140-190).
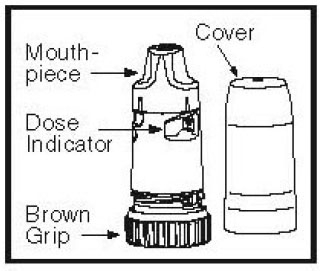
PULMICORT FLEXHALER consists of a number of assembled plastic details, the main parts being the dosing mechanism, the storage unit for drug substance, and the mouthpiece. The inhaler is protected by a white outer tubular cover screwed onto the inhaler. The body of the inhaler is white and the turning grip is brown. The PULMICORT FLEXHALER inhaler cannot be refilled and should be discarded when empty.
The number in the middle of the dose indicator window shows how many doses are left in the inhaler. The inhaler is empty when the number zero (“0”) on the red background reaches the middle of the window. If the unit is used beyond the point at which the zero reaches the middle of the window, the correct amount of medication may not be obtained and the unit should be discarded.
Store in a dry place at controlled room temperature 20-25°C (68-77°F) [see USP] with the cover tightly in place. Keep out of the reach of children.
-
17 PATIENT COUNSELING INFORMATION
Patients being treated with PULMICORT FLEXHALER should receive the following information and instructions. This information is intended to aid the patient in the safe and effective use of the medication. It is not a disclosure of all possible adverse or intended effects. For proper use of PULMICORT FLEXHALER and to attain maximum improvement, the patient should read and follow the accompanying FDA Approved Patient Labeling.
17.1 Oral Candidiasis
Patients should be advised that localized infections with Candida albicans occurred in the mouth and pharynx in some patients. If oropharyngeal candidiasis develops, it should be treated with appropriate local or systemic (i.e., oral) antifungal therapy while still continuing therapy with PULMICORT FLEXHALER, but at times therapy with PULMICORT FLEXHALER may need to be temporarily interrupted under close medical supervision. Rinsing the mouth after inhalation is advised [see Warnings and Precautions (5.1)].
17.2 Not for Acute Symptoms
PULMICORT FLEXHALER is not meant to relieve acute asthma symptoms and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled, short-acting beta2-agonist such as albuterol (the physician should provide the patient with such medication and instruct the patient in how it should be used).
Patients should be instructed to notify their physician immediately if they experience any of the following:
- Decreasing effectiveness of inhaled, short-acting beta2-agonists
- Need for more inhalations than usual of inhaled, short-acting beta2-agonists
- Significant decrease in lung function as outlined by the physician
Patients should not stop therapy with PULMICORT FLEXHALER without physician/provider guidance since symptoms may recur after discontinuation [see Warnings and Precautions (5.1)].
17.3 Hypersensitivity Including Anaphylaxis
Hypersensitivity reactions including anaphylaxis, rash, contact dermatitis, urticaria, angioedema, and bronchospasm have been reported with use of PULMICORT FLEXHALER. Discontinue PULMICORT FLEXHALER if such reactions occur [see Contraindications (4), Warnings and Precautions (5.3), Adverse Reactions (6)].
PULMICORT FLEXHALER contains small amounts of lactose, which contains trace levels of milk proteins. It is possible that cough, wheezing, or bronchospasm may occur in patients who have a severe milk protein allergy [see Contraindications (4)].
17.4 Immunosuppression
Patients who are on immunosuppressant doses of corticosteroids should be warned to avoid exposure to chickenpox or measles and, if exposed, to consult their physician without delay. Patients should be informed of potential worsening of existing tuberculosis, fungal, bacterial, viral, or parasitic infections, or ocular herpes simplex [see Warnings and Precautions (5.4)].
17.5 Hypercorticism and Adrenal Suppression
Patients should be advised that PULMICORT FLEXHALER may cause systemic corticosteroid effects of hypercorticism and adrenal suppression. Additionally, patients should be instructed that deaths due to adrenal insufficiency have occurred during and after transfer from systemic corticosteroids. Patients should taper slowly from systemic corticosteroids if transferring to PULMICORT FLEXHALER [see Warnings and Precautions (5.5, 5.6)].
17.6 Reduction in Bone Mineral Density
Patients who are at an increased risk for decreased BMD should be advised that the use of corticosteroids may pose an additional risk [see Warnings and Precautions (5.8)].
17.7 Reduced Growth Velocity
Patients should be informed that orally inhaled corticosteroids, including budesonide inhalation powder, may cause a reduction in growth velocity when administered to pediatric patients. Physicians should closely follow the growth of children and adolescents taking corticosteroids by any route [see Warnings and Precautions (5.9)].
17.8 Ocular Effects
Long-term use of inhaled corticosteroids may increase the risk of some eye problems (cataracts or glaucoma); regular eye examinations should be considered [see Warnings and Precautions (5.10)].
17.9 Use Daily
Patients should be advised to use PULMICORT FLEXHALER at regular intervals, since its effectiveness depends on regular use. Maximum benefit may not be achieved for 1 to 2 weeks or longer after starting treatment. If symptoms do not improve in that time frame or if the condition worsens, patients should be instructed to contact their physician.
17.10 How to Use Pulmicort Flexhaler
Patients should be carefully instructed on the use of this drug product to assure optimal dose delivery. The patient may not sense the presence of any medication entering their lungs when inhaling from PULMICORT FLEXHALER. This lack of sensation does not mean that they did not get the medication. They should not repeat their inhalation even if they did not feel the medication when inhaling [see Patient Information].
-
PATIENT PACKAGE INSERT
PULMICORT FLEXHALER™ (bew DEH so nide) 180 mcg
(budesonide inhalation powder, 180 mcg)
PULMICORT FLEXHALER™ 90 mcg
(budesonide inhalation powder, 90 mcg)
- Important Note: This medicine is to only be inhaled through the mouth (by oral inhalation only).
Read the Patient Information that comes with PULMICORT FLEXHALER before you start using it and each time you get a refill. There may be new information. This leaflet does not take the place of talking to your healthcare provider about your medical condition or treatment.
What is PULMICORT FLEXHALER?
PULMICORT FLEXHALER is an inhaled corticosteroid medicine. PULMICORT FLEXHALER is used for long-term (maintenance) treatment of asthma and to prevent asthma symptoms in adults and children 6 years of age and older.
Inhaled corticosteroids help to decrease inflammation in the lungs. Inflammation in the lungs can lead to asthma symptoms.
PULMICORT FLEXHALER helps reduce inflammation and helps keep the airways open to reduce asthma symptoms.
PULMICORT FLEXHALER does not treat the symptoms of a sudden asthma attack. Always have a short-acting beta2-agonist medicine (rescue inhaler) with you to treat sudden symptoms. If you do not have an inhaled, short-acting bronchodilator, call your healthcare provider to have one prescribed for you.
It is not known if PULMICORT FLEXHALER is safe and effective in children younger than 6 years of age.
Who should not use PULMICORT FLEXHALER?
Do not use PULMICORT FLEXHALER:
- to treat sudden severe symptoms of asthma.
- if you have a severe allergy to milk proteins. PULMICORT FLEXHALER contains a small amount of lactose (milk sugar). People with severe allergies to milk protein may have symptoms of an allergic reaction with PULMICORT FLEXHALER including: cough, wheezing, trouble breathing or feeling like your throat is closing.
What should I tell my healthcare provider before using PULMICORT FLEXHALER?
Before using PULMICORT FLEXHALER, tell your healthcare provider if you:
- have any allergies. See the section “Who should not use PULMICORT FLEXHALER”. There is a complete list of ingredients in PULMICORT FLEXHALER at the end of this leaflet.
- have or had chicken pox or measles, or have recently been near anyone with chicken pox or measles.
- have or had tuberculosis of your respiratory tract.
- have certain kinds of serious infections that have not been treated, including:
- fungal infections
- bacterial infections
- viral infections
- parasitic infections
- herpes simplex infection of the eye (ocular herpes simplex)
PULMICORT FLEXHALER may not be right for people who have or had any of these types of infections.
- have liver problems
- have decreased bone mineral density.
You are at risk for decreased bone mineral density if you:
- are inactive for a long period of time
- have a family history of osteoporosis
- are a woman going through menopause or are past menopause (“the change of life”)
- smoke or use tobacco
- do not eat well (poor nutrition)
- are elderly
- take bone thinning medicines (such as anticonvulsant medicines or corticosteroids) for a long time.
- have eye problems such as increased pressure in the eye, glaucoma, or cataracts
- are planning to have surgery
- are pregnant or plan to become pregnant. It is not known if PULMICORT FLEXHALER may harm your unborn baby
- are breast-feeding or plan to breast-feed. PULMICORT FLEXHALER can pass into breast milk. You and your healthcare provider should decide if you will use PULMICORT FLEXHALER or breast-feed
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Using PULMICORT FLEXHALER with certain other medicines may affect each other causing side effects.
Especially tell your healthcare provider if you take:
- a corticosteroid medicine
- anti-seizure medicine (anticonvulsants)
- medicines that suppress your immune system (immunosuppressant)
- ketoconazole (Nizoral), other medicines that affect how your liver works.
Ask your healthcare provider or pharmacist if you are not sure if your medicine is one listed above.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I use PULMICORT FLEXHALER?
Use PULMICORT FLEXHALER exactly as prescribed by your healthcare provider. You must use PULMICORT FLEXHALER regularly for it to work.
- PULMICORT FLEXHALER comes in two strengths. Your healthcare provider has prescribed the strength that is best for you.
- Be sure you know the difference between PULMICORT FLEXHALER and any other inhaled medicines that are prescribed for you, including what you use them for (prescribed use) and what they look like.
- Do not stop using PULMICORT FLEXHALER, even if your symptoms get better. Your healthcare provider will change your medicines as needed.
- Do not change or stop any medicines used to control or treat your breathing problems, unless your healthcare provider tells you to.
- Rinse your mouth with water and spit the water out after each dose of PULMICORT FLEXHALER. Do not swallow the water. This will lessen the chance of getting a fungal infection (thrush) in the mouth.
- If you miss a dose, just take your next regularly scheduled dose when it is due. Do not use PULMICORT FLEXHALER more often or use more puffs than you have been prescribed.
-
Make sure you always have a short-acting beta2-agonist medicine with you. Use your short acting beta2-agonist medicine if you have breathing problems between doses of PULMICORT FLEXHALER or if a sudden asthma attack happens. Call your healthcare provider right away if:
- ∘ your short-acting rescue medicine does not work as well for relieving asthma symptoms.
- ∘ you need to use your short-acting rescue medicines more often than usual.
- ∘ your breathing problems worsen with PULMICORT FLEXHALER.
If you use another inhaled medicine by mouth to treat your asthma, talk with your healthcare provider for instructions about when to use the other medicine and when to use your PULMICORT FLEXHALER.
- If you have used corticosteroid medicines for a long time and the dose is now being lowered or stopped, you should carry a medical alert card. The medical alert card should state that you may need increased corticosteroids during times of stress or during an asthma attack that does not get better with bronchodilator medicines.
- Your healthcare provider may check your breathing, do blood tests and eye exams during treatment with PULMICORT FLEXHALER.
- Be sure to read, understand and follow the detailed Patient Instructions for Use at the end of this leaflet. These Instructions for Use tell you how to prime and use your PULMICORT FLEXHALER the right way.
What are the possible side effects of PULMICORT FLEXHALER?
PULMICORT FLEXHALER can cause serious side effects, including:
- thrush (candida), a fungal infection in your mouth and throat. Tell your healthcare provider if you have any redness or white colored patches in your mouth or throat.
- worsening of asthma or sudden asthma attacks.
-
allergic reactions. Tell your healthcare provider or get medical help right away if you have:
- ∘ skin rash, redness or swelling
- ∘ severe itching
- ∘ swelling of the face, mouth, and tongue
- ∘ trouble breathing or swallowing
- ∘ chest pain
- ∘ anxiety (feeling of doom)
- Immune system effects and a higher chance of infections. You are more likely to get infections if you take medicines that weaken your immune system. Avoid contact with people who have contagious diseases such as chicken pox or measles while using PULMICORT FLEXHALER. Symptoms of infection may include: fever, pain, aches, chills, feeling tired, nausea and vomiting. Tell your healthcare provider about any signs of infection while you are using PULMICORT FLEXHALER.
- Adrenal insufficiency. Adrenal insufficiency is a condition in which the adrenal glands do not make enough steroid hormones. Symptoms of adrenal insufficiency include: tiredness, weakness, nausea and vomiting and low blood pressure.
- Decrease in bone mineral density. Your healthcare provider should check you for this during treatment with PULMICORT FLEXHALER.
- Slowed or delayed growth problems in children. A child’s growth should be checked regularly while using PULMICORT FLEXHALER.
- Eye problems, including glaucoma and cataracts. You should have regular eye exams while using PULMICORT FLEXHALER.
- Increased wheezing right after taking PULMICORT FLEXHALER. Always have a short-acting beta2-agonist medicine (rescue inhaler) with you to treat sudden wheezing.
Call your healthcare provider or get medical help right away if you have symptoms of any of the serious side effects listed above.
Common side effects reported by patients using PULMICORT FLEXHALER include:
- sore nose and throat
- stuffy nose
- runny nose
- nausea
- hay fever
- viral infections of the upper respiratory tract
- viral irritation and inflammation of the stomach and intestine (gastroenteritis). Symptoms may include stomach area pain, diarrhea, nausea and vomiting, loss of appetite, headaches, and weakness.
- ear infections
Tell your healthcare provider about any side effect that bothers you or that does not go away.
These are not all of the side effects of PULMICORT FLEXHALER. Ask your healthcare provider or pharmacist for more information.
Call your healthcare provider for medical advice about side effects. You may report side effects to AstraZeneca at 1-800-236-9933 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
How should I store PULMICORT FLEXHALER?
Store PULMICORT FLEXHALER at 68° to 77°F (20° to 25°C).
- Keep PULMICORT FLEXHALER dry.
- Keep your PULMICORT FLEXHALER with the cover tightly in place when not in use.
Keep your PULMICORT FLEXHALER and all medicines out of the reach of children.
General Information about PULMICORT FLEXHALER
Medicines are sometimes prescribed for conditions that are not mentioned in Patient Information Leaflets. Do not use PULMICORT FLEXHALER for a condition for which it was not prescribed. Do not give PULMICORT FLEXHALER to other people, even if they have the same symptoms that you have. It may harm them.
This Patient Information leaflet summarizes the most important information about PULMICORT FLEXHALER. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about PULMICORT FLEXHALER that is written for health professionals.
For more information, go to pulmicortflexhaler.com or call 1- 800-236-9933.
What are the ingredients in PULMICORT FLEXHALER?
Active ingredient: budesonide
Inactive ingredient: lactose
Patient Instructions for Use
How to use your PULMICORT FLEXHALER
Parts of your PULMICORT FLEXHALER
Figure 1
Priming PULMICORT FLEXHALER:
Before you use a new PULMICORT FLEXHALER for the first time, you must prime it.
To prime your PULMICORT FLEXHALER, follow the steps below:
- Hold the inhaler by the brown grip so that the white cover points upward (upright position). With the other hand, turn the white cover and lift it off (see Figure 2).
- Continue to hold your PULMICORT FLEXHALER upright as shown in Figure 1. Use your other hand to hold the inhaler in the middle. Do not hold the inhaler at the top of the mouthpiece.
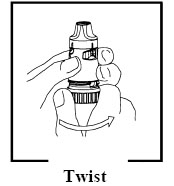
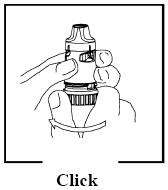
- Twist the brown grip as far as it will go in one direction and then fully back again in the other direction until it stops (it does not matter which way you turn it first). You will hear a “click” during one of the twisting movements (see Figures 3 and 4).
- Repeat Step 3. Your PULMICORT FLEXHALER is now primed. You are ready to load your first dose.
You do not have to prime your PULMICORT FLEXHALER again after this even if you do not use it for a long period of time.
1 Loading a dose
- Hold your PULMICORT FLEXHALER upright as described above. With your other hand, twist the white cover and lift it off (see Figure 2).
Figure 2
- Continue to hold your PULMICORT FLEXHALER upright to be sure that the right dose of medicine is loaded.
- Use your other hand to hold the inhaler in the middle. Do not hold the mouthpiece when you load the inhaler.
- Twist the brown grip fully in one direction as far as it will go. Twist it fully back again in the other direction as far as it will go (it does not matter which way you turn it first) [see Figure 3].
Figure 3
- You will hear a “click” during one of the twisting movements (see Figure 4).
Figure 4
- PULMICORT FLEXHALER will only give one dose at a time, no matter how often you click the brown grip, but the dose indicator will continue to move (advance). This means that if you continue to move the brown grip, it is possible for the indicator to show fewer doses or zero doses even if more doses are left in the inhaler.
- Do not shake the inhaler after loading it.
Figure 5
2 Inhaling a dose
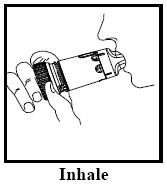
- Turn your head away from the inhaler and breathe out (exhale). If you accidentally blow into your inhaler after loading a dose, follow the instructions for loading a new dose.
- Place the mouthpiece in your mouth and close your lips around the mouthpiece. Breathe in (inhale) deeply and forcefully through the inhaler (see Figure 5).
- You may not sense the presence of any medication entering your lungs when inhaling from PULMICORT FLEXHALER. This lack of sensation does not mean that you did not get the medication. You should not repeat your inhalations even if you did not feel the medication when inhaling.
- Do not chew or bite on the mouthpiece.
- Remove the inhaler from your mouth and exhale. Do not blow or exhale into the mouthpiece.
- If more than one dose is prescribed repeat the steps above.
- When you are finished taking your dose place the white cover back on the inhaler and twist shut.
- Rinse your mouth with water after each dose to decrease your risk of getting thrush. Do not swallow the water.
Reading the Dose Indicator Window
- The label on the box or cover will tell you how many doses are in your PULMICORT FLEXHALER.
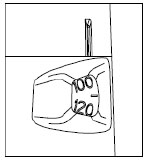
- Your PULMICORT FLEXHALER has a dose indicator window just below the mouthpiece. The dose indicator tells you about how many doses are left in the inhaler. Look at the middle of the window to find out about how many doses are left in your inhaler (see Figure 6).
Figure 6
- The dose indicator is connected to the turning grip and moves (counts down) every time a dose is loaded. It is not likely that you will see the dose indicator move with each dose. You can usually see the indicator move each time you use about 5 doses.
- The dose indicator starts with either the number 60 or 120 when full, depending upon the strength of the inhaler. The indicator is marked in intervals of 10 doses. Markings are either with numbers or dashes (alternating), counting down to “0”.
- 60 Dose Inhaler
- 120 Dose Inhaler
- 20
- 80
- Dose indicator starts at 60 or 120 depending on strength (90 mcg or 180 mcg) of the inhaler and counts down to 0.
- --
- --
- 40
- 100
- --
- --
- 60
- 120
- .
- The dose indicator will tell you about how many doses are left in your PULMICORT FLEXHALER.
- If you complete the instructions for loading the dose more than one time before you inhale the dose, you will only receive one dose. The dose indicator will move a small amount but it is not likely that you will see the dose indicator move with each dose.
- Your inhaler is empty when the number 0 on the red background reaches the middle of the dose indicator window. Throw away this inhaler. The inhaler may not give you the right amount of medicine, even though it may not feel completely empty and may seem like it continues to work (see Figure 7).
Figure 7
- Do not put your PULMICORT FLEXHALER in water (do not immerse it) to find out if it is empty. Check the dose indicator window to see how many doses are left.
- Refill your PULMICORT FLEXHALER prescription before your medicine runs out. You will get a new inhaler each time you refill your prescription.
Cleaning your PULMICORT FLEXHALER
- Keep your PULMICORT FLEXHALER clean and dry at all times. Do not immerse it in water.
- Wipe the outside of the mouthpiece one time each week with a dry tissue.
- Do not use water or liquids when cleaning the mouthpiece.
- Do not try to remove the mouthpiece or twist it.
Do not use your PULMICORT FLEXHALER if it has been damaged or if the mouthpiece has become detached. Talk to your healthcare provider or pharmacist if you have any problems with your PULMICORT FLEXHALER.
PULMICORT FLEXHALER is a trademark of the AstraZeneca group of companies.
©AstraZeneca 2007, 2008, 2010, 2016, 2019
Manufactured for: AstraZeneca Pharmaceuticals LP, Wilmington DE 19850
By: AstraZeneca AB, Södertälje, Sweden
Product of Sweden
-
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL – 90 mcg
NDC: 0186-0917-06
Pulmicort
Flexhaler™ 90 mcg
(budesonide inhalation
powder, 90 mcg)
90 mcg
For Oral Inhalation.
60 Metered Doses
Dispense with enclosed Patient
Information and Instructions for Use.
Rx only
AstraZeneca
-
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL – 180 mcg
NDC: 0186-0916-12
Pulmicort
Flexhaler™ 180 mcg
(budesonide inhalation
powder, 180 mcg)
180 mcg
For Oral Inhalation.
120 Metered Doses
Dispense with enclosed Patient
Information and Instructions for Use.
Rx only
AstraZeneca
-
INGREDIENTS AND APPEARANCE
PULMICORT FLEXHALER
budesonide aerosol, powderProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0186-0916 Route of Administration RESPIRATORY (INHALATION) Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BUDESONIDE (UNII: Q3OKS62Q6X) (BUDESONIDE - UNII:Q3OKS62Q6X) BUDESONIDE 180 ug Inactive Ingredients Ingredient Name Strength LACTOSE, UNSPECIFIED FORM (UNII: J2B2A4N98G) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0186-0916-12 1 in 1 CARTON 03/19/2007 1 120 in 1 INHALER; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021949 03/19/2007 PULMICORT FLEXHALER
budesonide aerosol, powderProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0186-0917 Route of Administration RESPIRATORY (INHALATION) Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BUDESONIDE (UNII: Q3OKS62Q6X) (BUDESONIDE - UNII:Q3OKS62Q6X) BUDESONIDE 90 ug Inactive Ingredients Ingredient Name Strength LACTOSE, UNSPECIFIED FORM (UNII: J2B2A4N98G) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0186-0917-06 1 in 1 CARTON 03/19/2007 1 60 in 1 INHALER; Type 0: Not a Combination Product 2 NDC: 0186-0917-65 1 in 1 CARTON 03/19/2007 2 60 in 1 INHALER; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021949 03/19/2007 Labeler - AstraZeneca Pharmaceuticals LP (938368834) Registrant - AstraZeneca PLC (230790719)
Trademark Results [PULMICORT]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 PULMICORT 78942523 3506648 Live/Registered |
AstraZeneca AB 2006-08-01 |
 PULMICORT 75001471 not registered Dead/Abandoned |
ASTRA AKTIEBOLAG 1995-10-04 |
 PULMICORT 73055022 1036567 Dead/Expired |
AKTIEBOLAGET ASTRA 1975-08-28 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.