AMIODARONE HYDROCHLORIDE injection, solution
Amiodarone Hydrochloride by
Drug Labeling and Warnings
Amiodarone Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by Henry Schein, Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use a
AMIODARONE HYDROCHLORIDE INJECTION safely and effectively. See full prescribing information for AMIODARONE HYDROCHLORIDE INJECTION. AMIODARONE HYDROCHLORIDE injection, for intravenous use Initial U.S. Approval: 1985INDICATIONS AND USAGE
Amiodarone hydrochloride injection is an antiarrhythmic agent indicated for initiation of treatment and prophylaxis of frequently recurring ventricular fibrillation (VF) and hemodynamically unstable ventricular tachycardia (VT) in patients refractory to other therapy. (1)
DOSAGE AND ADMINISTRATION
- The recommended starting dose is about 1000 mg over the first 24 hours of therapy, delivered by the following infusion regimen (2):
- Initial Load: 150 mg per 100 mL (in D5W) infused over 10 minutes
- Followed by: 1 mg/min for 6 hours
- Followed by: 0.5 mg/min thereafter - For breakthrough episodes of VF or hemodynamically unstable VT, repeat the initial Load (2)
DOSAGE FORMS AND STRENGTHS
Injection, 50 mg/mL (3)
CONTRAINDICATIONS
Amiodarone is contraindicated in patients with: (4)
- Known hypersensitivity to any of the components of amiodarone, including iodine.
- Cardiogenic shock
- Marked sinus bradycardia
- Second- or third-degree atrio-ventricular (AV) block unless a functioning pacemaker is available.
WARNINGS AND PRECAUTIONS
Hypotension: Slow the infusion; as needed, add vasopressor drugs, positive inotropic agents, and volume expansion. (5.1)
Bradycardia and AV block: Slow the infusion or discontinue. (5.2) (5)ADVERSE REACTIONS
(6)
- The most common adverse reactions (1-2%) leading to discontinuation of intravenous amiodarone therapy are hypotension, asystole/cardiac arrest/pulseless electrical activity, VT, and cardiogenic shock.
- Other important adverse reactions are, torsade de pointes (TdP), congestive heart failure, and liver function test abnormalities.
To report SUSPECTED ADVERSE REACTIONS, contact Mylan Institutional at 1-877-446-3679 (1-877-4-INFO-RX) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. (6)
DRUG INTERACTIONS
Amiodarone is a substrate for CYP3A and CYP2C8, so inhibitors and inducers affect amiodarone exposure (7)
Amiodarone inhibits p-glycoprotein and CYP1A2, CYP2C9, CYP2D6, and CYP3A, increasing exposure to other drugs (7) (7)USE IN SPECIFIC POPULATIONS
(8)
- Pregnancy: Use amiodarone during pregnancy only if the potential benefit to the mother justifies the risk to the fetus (8.1).
- Nursing mothers: Amiodarone and one of its major metabolites, desethylamiodarone (DEA), are excreted in human milk, suggesting that breastfeeding could expose the nursing infant to a significant dose of the drug. Advise mothers to discontinue breastfeeding (8.3).
- Pediatric use: The safety and efficacy of amiodarone in the pediatric population have not been established (8.4).
See 17 for PATIENT COUNSELING INFORMATION. (8)
Revised: 7/2020 (8)
Revised: 9/2025
- The recommended starting dose is about 1000 mg over the first 24 hours of therapy, delivered by the following infusion regimen (2):
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 Warnings and Precautions
6 ADVERSE REACTIONS
7 Drug Interactions
8 Use in Specific Populations
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
7 NONCLINICAL TECHNOLOGY
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Amiodarone injection is indicated for initiation of treatment and prophylaxis of frequently recurring ventricular fibrillation (VF) and hemodynamically unstable ventricular tachycardia (VT) in patients refractory to other therapy. Amiodarone also can be used to treat patients with VT/VF for whom oral amiodarone is indicated, but who are unable to take oral medication. During or after treatment with amiodarone, patients may be transferred to oral amiodarone therapy [see Dosage and Administration (2)].
Use amiodarone for acute treatment until the patient's ventricular arrhythmias are stabilized. Most patients will require this therapy for 48 to 96 hours, but amiodarone may be safely administered for longer periods if necessary.
-
2 DOSAGE AND ADMINISTRATION
Amiodarone shows considerable interindividual variation in response. Although a starting dose adequate to suppress life-threatening arrhythmias is needed, close monitoring with adjustment of dose is essential. The recommended starting dose of amiodarone is about 1000 mg over the first 24 hours of therapy, delivered by the following infusion regimen:
Table 1: AMIODARONE DOSE RECOMMENDATIONS: FIRST 24 HOURSLoading infusions First Rapid: 150 mg over the FIRST 10 minutes (15 mg/min). Add 3 mL of amiodarone (150 mg) to 100 mL D5W (concentration = 1.5 mg/mL). Infuse 100 mL over 10 minutes. Followed by Slow: 360 mg over the NEXT 6 hours (1 mg/min). Add 18 mL of amiodarone (900 mg) to 500 mL D5W (concentration = 1.8 mg/mL) Infuse 200mL at a rate of 0.556mL/min. Maintenance infusion 540 mg over the REMAINING 18 hours (0.5 mg/min). Decrease the rate of the slow loading infusion to 0.278mL/min. After the first 24 hours, continue the maintenance infusion rate of 0.5 mg/min (720 mg per 24 hours) utilizing a concentration of 1 to 6 mg/mL (Use a central venous catheter for amiodarone concentrations greater than 2 mg/mL). The rate of the maintenance infusion may be increased to achieve effective arrhythmia suppression.
In the event of breakthrough episodes of VF or hemodynamically unstable VT, use 150 mg supplemental infusions of amiodarone (mixed in 100 mL of D5W and infused over 10 minutes to minimize the potential for hypotension).
The first 24-hour dose may be individualized for each patient; however, in controlled clinical trials, mean daily doses above 2100 mg were associated with an increased risk of hypotension. Do not exceed an initial infusion rate of 30 mg/min.
Based on the experience from clinical studies of intravenous amiodarone, a maintenance infusion of up to 0.5 mg/min can be continued for 2 to 3 weeks regardless of the patient's age, renal function, or left ventricular function. There has been limited experience in patients receiving intravenous amiodarone for longer than 3 weeks.
The surface properties of solutions containing injectable amiodarone are altered such that the drop size may be reduced. This reduction may lead to underdosage of the patient by up to 30% if drop counter infusion sets are used. Amiodarone must be delivered by a volumetric infusion pump.
Administer amiodarone, whenever possible, through a central venous catheter dedicated to that purpose. Use an in-line filter during administration.
Intravenous amiodarone loading infusions at much higher concentrations and rates of infusion much faster than recommended have resulted in hepatocellular necrosis and acute renal failure, leading to death[see Warnings and Precautions (5.3)].
Intravenous amiodarone concentrations greater than 3 mg/mL in D5W have been associated with a high incidence of peripheral vein phlebitis; however, concentrations of 2.5 mg/mL or less appear to be less irritating. Therefore, for infusions longer than 1 hour, do not exceed amiodarone concentrations of 2 mg/mL, unless a central venous catheter is used[see Adverse Reactions (6.2)].
Amiodarone infusions exceeding 2 hours must be administered in glass or polyolefin bottles containing D5W. Do not use evacuated glass containers for admixing, as incompatibility with a buffer in the container may cause precipitation.
Amiodarone absorbs to polyvinyl chloride (PVC) tubing, but all of the clinical experience has been with PVC tubing and the concentrations and rates of infusion provided in DOSAGE AND ADMINISTRATION reflect dosing in these studies.
Amiodarone has been found to leach out plasticizers, including DEHP [di-(2-ethylhexyl)phthalate] from intravenous tubing (including PVC tubing). The degree of leaching increases when infusing amiodarone at higher concentrations and lower flow rates than provided in DOSAGE AND ADMINISTRATION. Polysorbate 80, a component of amiodarone injection, is also known to leach DEHP from PVC[see Description (11)].
Amiodarone does not need to be protected from light during administration.
NOTE: Inspect parenteral drug products for particulate matter and discoloration prior to administration, whenever solution and container permit solution should be clear.CAUTION: Do not use plastic containers in series connections. Such use could result in air embolism due to residual air being drawn from the primary container before the administration of the fluid from the secondary container is complete.
Discard unused portion.
Table 2: AMIODARONE HCL SOLUTION STABILITYSolution Concentration
(mg/mL)Container Comments 5% Dextrose in Water (D5W) 1.0 to 6.0 PVC Physically compatible, with amiodarone loss <10% at 2 hours at room temperature. 5% Dextrose in Water (D5W) 1.0 to 6.0 Polyolefin, Glass Physically compatible, with no amiodarone loss at 24 hours at room temperature. Admixture Incompatibility
Amiodarone in D5W Injection forms precipitates with the drugs shown in Table 3. If coadministration of the following drugs is necessary, use separate intravenous administration lines.
Table 3: Y-SITE INJECTION INCOMPATIBILITYDrug Vehicle Amiodarone Concentration Aminophylline D5W;NS 4mg/mL Amoxillin Sodium-Clavulanic unknown 12.5mg/mL Ampicillin Sodium-Sulbactam Sodium NS 6mg/mL Argatroban D5W 1.8mg/mL Bivalirudin D5W 4mg/mL Cefamandole Nafate D5W 4mg/mL Cefaolin Sodium D5W 4mg/mL Ceftazidime D5W 6mg/mL Digoxin D5W 6mg/mL Furosemide (10mg/mL)
D5W 6mg/mL Mezlocillin Sodium D5W 4mg/mL Heparin Sodium
D5W -- Imipenem-Cilastin Sodium D5W 6mg/mL Magnesium Sulfate (500mg/mL) D5W 6mg/mL Micafungin NS 4mg/mL Piperacillin Sodium-Tazobactam D5W 6mg/mL Potassium Phosphates D5W 6mg/mL Sodium Bicarbonate D5W 3mg/mL Sodium Nitroprusside D5W 1.5mg/mL, 6mg/mL and 15mg/mL Sodium Phosphates D5W 6mg/mL D5W = Dextrose 5% in Sterile Water, NS = Normal Saline
Intravenous to Oral Transition
Patients whose arrhythmias have been suppressed by amiodarone may be switched to oral amiodarone. The optimal dose for changing from intravenous to oral administration of amiodarone will depend on the dose of intravenous amiodarone already administered, as well as the bioavailability of oral amiodarone. When changing to oral amiodarone therapy, clinical monitoring is recommended, particularly for elderly patients. See package insert for oral amiodarone.
Since grapefruit juice is known to inhibit CYP3A-mediated metabolism of oral amiodarone in the intestinal mucosa, resulting in increased plasma levels of amiodarone, do not drink grapefruit juice during treatment with oral amiodarone [see DRUG INTERACTIONS (7)].
Table 4 provides suggested doses of oral amiodarone to be initiated after varying durations of amiodarone administration. These recommendations are made on the basis of a similar total body amount of amiodarone delivered by the intravenous and oral routes, based on 50% bioavailability of oral amiodarone.
Table 4: RECOMMENDATIONS FOR ORAL DOSAGE AFTER INTRAVENOUS INFUSION
Duration of Amiodarone Infusion Initial Daily Dose of Oral Amiodarone < than 1 week 800 to 1600 mg 1-3 weeks 600 to 800 mg > than 3 weeks * 400 mg *Assuming a 720 mg/day infusion (0.5 mg/min).
†Intravenous amiodarone is not intended for maintenance treatment.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Amiodarone is contraindicated in patients with:
- Known hypersensitivity to any of the components of amiodarone, including iodine. Hypersensitivity reactions may involve rash, angioedema, cutaneous/mucosal hemorrhage (bleeding), fever, arthralgias (joint pains), eosinophilia (abnormal blood counts), urticaria (hives), thrombotic thrombocytopenic purpura, or severe periarteritis (inflammation around blood vessels).
- Cardiogenic shock.
- Marked sinus bradycardia.
- Second- or third-degree atrio-ventricular (AV) block unless a functioning pacemaker is available.
-
5 Warnings and Precautions
Amiodarone should be administered only by physicians who are experienced in the treatment of life-threatening arrhythmias, who are thoroughly familiar with the risks and benefits of amiodarone therapy, and who have access to facilities adequate for monitoring the effectiveness and side effects of treatment.
Because of the long half-life of amiodarone and its metabolite desethylamiodarone, the potential for adverse reactions or interactions, as well as observed adverse effects, can persist following amiodarone withdrawal.
5.1 Hypotension
Hypotension is the most common adverse reaction seen with intravenous amiodarone. In clinical trials, treatment-emergent, drug-related hypotension was reported as an adverse effect in 288 (16%) of 1836 patients treated with intravenous amiodarone. Clinically significant hypotension during infusions was seen most often in the first several hours of treatment and was not dose related, but appeared to be related to the rate of infusion. Hypotension necessitating alterations in intravenous amiodarone therapy was reported in 3% of patients, with permanent discontinuation required in less than 2% of patients.Treat hypotension initially by slowing the infusion; additional standard therapy may be needed, including the following: vasopressor drugs, positive inotropic agents, and volume expansion. Monitor the initial rate of infusion closely and do not exceed the recommended rate [see DOSAGE AND ADMINISTRATION (2)].
In some cases, hypotension may be refractory and result in a fatal outcome [see ADVERSE REACTIONS (6.2)].
5.2 Bradycardia and Atrio-ventricular Block
In 90 (4.9%) of 1836 patients in clinical trials, drug-related bradycardia that was not dose-related occurred while they were receiving intravenous amiodarone for life-threatening VT/VF. Treat bradycardia by slowing the infusion rate or discontinuing amiodarone. In some patients, a pacemaker is required. Despite such measures, bradycardia was progressive and terminal in 1 patient during the controlled trials. Treat patients with a known predisposition to bradycardia or AV block with amiodarone in a setting where a temporary pacemaker is available.5.3 Hepatic Injury
Elevations of blood hepatic enzyme values [alanine aminotransferase (ALT), aspartate aminotransferase (AST), and gamma-glutamyl transferase (GGT)] are commonly seen in patients with immediately life-threatening VT/VF. Interpreting elevated AST activity can be difficult because the values may be elevated in patients who have had recent myocardial infarction, congestive heart failure, or multiple electrical defibrillations. Approximately 54% of patients receiving intravenous amiodarone in clinical studies had baseline liver enzyme elevations, and 13% had clinically significant elevations. In 81% of patients with both baseline and on-therapy data available, the liver enzyme elevations either improved during therapy or remained at baseline levels. Baseline abnormalities in hepatic enzymes are not a contraindication to treatment. Elevated bilirubin levels have been reported in patients administered intravenous amiodarone.Acute, centrolobular confluent hepatocellular necrosis leading to hepatic coma, acute renal failure, and death has been associated with the administration of intravenous amiodarone [see DOSAGE AND ADMINISTRATION (2)].
In patients with life-threatening arrhythmias, the potential risk of hepatic injury should be weighed against the potential benefit of amiodarone therapy. Carefully monitor patients receiving amiodarone for evidence of progressive hepatic injury. In such cases, consider reducing the rate of administration or withdrawing amiodarone.
5.4 Proarrhythmia
Like all antiarrhythmic agents, amiodarone may cause a worsening of existing arrhythmias or precipitate a new arrhythmia sometimes leading to fatal outcomes [see ADVERSE REACTIONS (6.2)]. Proarrhythmia, primarily torsade de pointes (TdP), has been associated with prolongation, by intravenous amiodarone, of the QTc interval to 500 ms or greater. Although QTc prolongation occurred frequently in patients receiving intravenous amiodarone, TdP or new-onset VF occurred infrequently (less than 2%). Monitor patients for QTc prolongation during infusion with amiodarone. Reserve the combination of amiodarone with other antiarrhythmic therapies that prolong the QTc to patients with life-threatening ventricular arrhythmias who are incompletely responsive to a single agent.Correct hypokalemia, hypomagnesemia or hypocalcemia whenever possible before initiating treatment with amiodarone, as these disorders can exaggerate the degree of QTc prolongation and increase the potential for TdP. Give special attention to electrolyte and acid-base balance in patients experiencing severe or prolonged diarrhea or in patients receiving concomitant diuretics and laxatives.
Amiodarone causes thyroid dysfunction in some patients, which may lead to potentially fatal breakthrough or exacerbated arrhythmias.
5.5 Pulmonary Injury
Early-onset Pulmonary Toxicity
There have been postmarketing reports of acute-onset (days to weeks) pulmonary injury in patients treated with intravenous amiodarone. Findings have included pulmonary infiltrates and masses on X-ray, bronchospasm, wheezing, fever, dyspnea, cough, hemoptysis, and hypoxia. Some cases have progressed to respiratory failure or death.ARDS
Two percent (2%) of patients were reported to have adult respiratory distress syndrome (ARDS) during clinical studies involving 48 hours of therapy.Pulmonary Fibrosis
There have been reports of early development of pulmonary fibrosis (within 1 to 3 months) following initiation of amiodarone treatment. Only 1 of more than 1000 patients treated with intravenous amiodarone in clinical studies developed pulmonary fibrosis. In that patient, the condition was diagnosed 3 months after treatment with intravenous amiodarone, during which time the patient received oral amiodarone. Pulmonary toxicity is a well-recognized complication of long-term amiodarone use (see package insert for oral amiodarone).5.6 Loss of Vision
Cases of optic neuropathy and optic neuritis, usually resulting in visual impairment, have been reported in patients treated with oral amiodarone or intravenous amiodarone. In some cases, visual impairment has progressed to permanent blindness. Optic neuropathy and neuritis may occur at any time following initiation of therapy. A causal relationship to the drug has not been clearly established. Perform an ophthalmic examination if symptoms of visual impairment appear, such as changes in visual acuity and decreases in peripheral vision. Re-evaluate the necessity of amiodarone therapy if optic neuropathy or neuritis is suspected. Perform regular ophthalmic examination, including fundoscopy and slit-lamp examination, during administration of amiodarone.5.7 Thyroid Abnormalities
Amiodarone inhibits peripheral conversion of thyroxine (T4) to triiodothyronine (T3) and may cause increased T4 levels, decreased T3 levels, and increased levels of inactive reverse T3 (rT3) in clinically euthyroid patients. Amiodarone is also a potential source of large amounts of inorganic iodine and can cause either hypothyroidism or hyperthyroidism. Evaluate thyroid function prior to treatment and periodically thereafter, particularly in elderly patients, and in any patient with a history of thyroid nodules, goiter, or other thyroid dysfunction. Because of the slow elimination of amiodarone and its metabolites, high plasma iodide levels, altered thyroid function, and abnormal thyroid-function tests may persist for months following amiodarone withdrawal.There have been postmarketing reports of thyroid nodules/thyroid cancer in patients treated with amiodarone. In some instances hyperthyroidism was also present.
Hyperthyroidism and Thyrotoxicosis
Amiodarone causes hyperthyroidism in about 2% of patients. Thyrotoxicosis and arrhythmia with fatal outcome has been reported in the presence of pre-existing hyperthyroidism even following a single intravenous amiodarone dose. Consider the possibility of hyperthyroidism if any new signs of arrhythmia appear.Hyperthyroidism may result from iodine load (type 1 amiodarone-induced thyrotoxicosis [type 1 AIT]; in particular in patients with underlying autonomous thyroid nodules or latent Grave’s disease). Hyperthyroidism may also result from direct amiodarone-induced destructive thyroiditis that occurs in individuals with no underlying thyroid disease (type 2 AIT), resulting in the release of preformed thyroid hormone into the bloodstream from damaged thyroid follicular epithelium. Mixed forms of hyperthyroidism as a result of both pathogenic mechanisms (excessive thyroid hormone production and thyroid destruction) can also occur. The risk of hyperthyroidism may be higher among patients with prior inadequate dietary iodine intake.
Identify hyperthyroidism by relevant clinical signs and symptoms, subnormal serum levels of thyroid stimulating hormone (TSH), abnormally elevated serum free T4, and elevated or normal serum T3. Since arrhythmia breakthroughs may accompany amiodarone-induced hyperthyroidism, aggressive medical treatment is indicated, including, if possible, dose reduction or withdrawal of amiodarone. Amiodarone hyperthyroidism may be followed by a transient period of hypothyroidism.
The institution of antithyroid drugs, β-adrenergic blockers or temporary corticosteroid therapy may be necessary. The action of antithyroid drugs may be especially delayed in amiodarone-induced thyrotoxicosis because of substantial quantities of preformed thyroid hormones stored in the gland. Radioactive iodine therapy is not recommended because of the low radioiodine uptake associated with amiodarone-induced hyperthyroidism.
When aggressive treatment of amiodarone-induced thyrotoxicosis has failed or amiodarone cannot be discontinued because it is the only drug effective against the resistant arrhythmia, surgical management may be an option. Experience with thyroidectomy as a treatment for amiodarone-induced thyrotoxicosis is limited, and this form of therapy could induce thyroid storm. Therefore, surgical and anesthetic management require careful planning.
Hypothyroidism
Hypothyroidism has been reported in 2% to 10% of patients receiving amiodarone and may be primary or subsequent to resolution of preceding amiodarone-induced hyperthyroidism. This condition may be identified by clinical symptoms and elevated serum TSH levels. Cases of severe hypothyroidism and myxedema coma, sometimes fatal, have been reported in association with amiodarone therapy. In some clinically hypothyroid amiodarone-treated patients, free thyroxine index values may be normal. Manage hypothyroidism by reducing the dose of or discontinuing amiodarone and considering the need for thyroid hormone supplement.5.8 Neonatal Injury
Amiodarone can cause fetal harm when administered to a pregnant woman. Fetal exposure may increase the potential for adverse experiences including cardiac, thyroid, neurodevelopmental, neurological and growth effects in neonates. Inform the patient of the potential hazard to the fetus if amiodarone is administered during pregnancy or if the patient becomes pregnant while taking amiodarone [see PREGNANCY (8.1)].5.9 Exaggerated Effects of Perisurgical Therapy
Perform close perioperative monitoring in patients undergoing general anesthesia who are on amiodarone therapy as they may be more sensitive to the myocardial depressant and conduction defects of halogenated inhalational anesthetics.5.10 Interference with Corneal Refractive Laser Surgery
Advise patients that most manufacturers of corneal refractive laser surgery devices contraindicate corneal refractive laser surgery in patients taking amiodarone.5.11 Hypersensitivity Reactions
Anaphylactic/anaphylactoid reactions have been reported with intravenous amiodarone including shock (sometimes fatal), cardiac arrest, and the following manifestations: hypotension, tachycardia, hypoxia, cyanosis, rash, flushing, hyperhidrosis and cold sweat. -
6 ADVERSE REACTIONS
The following adverse reactions are described elsewhere in labeling:
Hypotension [see WARNINGS AND PRECAUTIONS (5.1)]
Hepatic injury [see WARNINGS AND PRECAUTIONS (5.3)]
Rhythm disturbances [see WARNINGS AND PRECAUTIONS (5.4)]
Pulmonary injury [see WARNINGS AND PRECAUTIONS (5.5)]
Thyroid injury [see WARNINGS AND PRECAUTIONS (5.7)]
Hypersensitivity [see WARNINGS AND PRECAUTIONS (5.11)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.In a total of 1836 patients in controlled and uncontrolled clinical trials, 14% of patients received intravenous amiodarone for at least one week, 5% received it for at least 2 weeks, 2% received it for at least 3 weeks, and 1% received it for more than 3 weeks, without an increased incidence of severe adverse reactions. The mean duration of therapy in these studies was 5.6 days; median exposure was 3.7 days.
The most important adverse reactions were hypotension, asystole/cardiac arrest/pulseless electrical activity (PEA), cardiogenic shock, congestive heart failure, bradycardia, liver function test abnormalities, VT, and AV block. Overall, treatment was discontinued for about 9% of the patients because of adverse reactions. The most common adverse reactions leading to discontinuation of intravenous amiodarone therapy were hypotension (1.6%), asystole/cardiac arrest/PEA (1.2%), VT (1.1%), and cardiogenic shock (1%).
Table 5 lists the most common (incidence 2%) adverse reactions during intravenous amiodarone therapy considered at least possibly drug-related. These data were collected in clinical trials involving 1836 patients with life-threatening VT/VF. Data from all assigned treatment groups are pooled because none of the adverse reactions appeared to be dose-related.
Table 5: ADVERSE REACTIONS IN PATIENTS RECEIVING INTRAVENOUS AMIODARONE IN CONTROLLED AND OPEN-LABEL STUDIES ( 2% INCIDENCE)
Study Event Controlled Studies (n=814) Open-Label Studies (n=1022) Total (n=1836) Body as a whole Fever 24 9(2.9%) 13 (1.2%) 37 (2.0%) Cardiovascular System Bradycardia 49 (6.0%) 41(4.0%) 90(4.9%) Congestive heart failure 18 (2.2%) 21 (2.0%) 39 (2.1%) Heart arrest 29 (3.5%) 26 (2.5%) 55 (2.9%) Hypotension 165 (20.2%) 123 (12.0%) 288 (15.6%) Ventricular tachycardia 15 (1.8%) 30 (2.9%) 45 (2.4%) Digestive System Liver function tests abnormal 35 (4.2%) 29 (2.8%) 64 (3.4%) Nausea 29 (3.5%) 43 (4.2%) 72 (3.9%) Other adverse reactions reported in less than 2% of patients receiving intravenous amiodarone in controlled and uncontrolled studies included the following: abnormal kidney function, atrial fibrillation, diarrhea, increased ALT, increased AST, lung edema, nodal arrhythmia, prolonged QT interval, respiratory disorder, shock, sinus bradycardia, Stevens-Johnson syndrome, thrombocytopenia, VF, and vomiting.
6.2 Post-Marketing Experience
The following adverse reactions have been reported in the post-marketing experience during or in close temporal relationship to intravenous amiodarone administration. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.Blood and Lymphatic System Disorders: pancytopenia, neutropenia, hemolytic anemia, aplastic anemia, thrombocytopenia, and agranulocytosis.
Cardiac Disorders: sinus node dysfunction (sinus arrest, sinoatrial block), intraventricular conduction disorders including bundle branch block and infra-HIS block, bradycardia (sometimes fatal), ventricular extrasystoles, and antegrade conduction via an accessory pathway.
Endocrine Disorders: syndrome of inappropriate antidiuretic hormone secretion (SIADH).
Eye Disorders: visual field defect and blurred vision.
Gastrointestinal Disorders: pancreatitis.
General Disorders and Administration Site Conditions: infusion site reactions, including thrombosis, phlebitis, thrombophlebitis, cellulitis, pain, induration, edema, inflammation, urticaria, pruritus, erythema, pigment changes, hypoesthesia, skin sloughing, extravasation possibly leading to venous/infusion site necrosis, intravascular amiodarone deposition/mass (developed in the superior vena cava around a central venous catheter after long-term [28 days] amiodarone therapy administered through a central line), and granuloma.
Hepatobiliary Disorders: cholestasis, cirrhosis, jaundice, alkaline phosphatase and blood lactate dehydrogenase increase.
Musculoskeletal and Connective Tissue Disorders: myopathy, muscle weakness, rhabdomyolysis, muscle spasms, and back pain.
Neoplasms Benign, Malignant and Unspecified (incl Cysts and Polyps) Disorders: thyroid nodules/thyroid cancer.
Nervous System Disorders: intracranial pressure increased, pseudotumor cerebri, tremor, dizziness and hypoesthesia.
Psychiatric Disorders: confusional state, hallucination, disorientation, and delirium.
Renal and Urinary Disorders: acute renal failure (sometimes fatal), renal impairment, renal insufficiency, and blood creatinine increased.
Reproductive Disorders and Breast Disorders: Epididymitis
Respiratory, Thoracic and Mediastinal Disorders: interstitial pneumonitis, bronchiolitis obliterans organizing pneumonia (possibly fatal), pulmonary alveolar hemorrhage, pulmonary phospholipidoisis, pleural effusion, bronchospasm, dyspnea, cough, hemoptysis, wheezing, and hypoxia.
Skin and Subcutaneous Tissue Disorders: toxic epidermal necrolysis (sometimes fatal), Stevens-Johnson syndrome, exfoliative dermatitis, erythema multiforme, skin cancer, pruritus, angioedema, and urticaria.
Vascular Disorders: vasculitis and flushing.
-
7 Drug Interactions
7.1 Pharmacodynamic Interactions
Drugs Prolonging the QT Interval
Co-administration of drugs prolonging the QT interval (such as class I and III antiarrhythmics, lithium, certain phenothiazines, tricyclic antidepressants, certain fluoroquinolone and macrolide antibiotics, azole antifungals, halogenated inhalation anesthetic agents) increases the risk of Torsade de Pointes. In general, avoid concomitant use of drugs that prolong the QT interval [see WARNINGS AND PRECAUTIONS (5.4)].Drugs That Slow Heart Rate
Concomitant use of drugs with depressant effects on the sinus and AV nodes (e.g., digoxin, beta blockers, verapamil, diltiazem, ivabradine, clonidine) can potentiate the electrophysiologic and hemodynamic effects of amiodarone, resulting in bradycardia, sinus arrest, and AV block. Monitor heart rate in patients on amiodarone and concomitant drugs that slow heart rate.7.2 Pharmacokinetic Interactions
Effect of Other Drugs on Amiodarone
Amiodarone is metabolized to the active metabolite desethylamiodarone (DEA) by the cytochrome P450 (CYP450) enzyme group, specifically CYP3A and CYP2C8.Amiodarone has the potential for interactions with drugs or substances that may be substrates, inhibitors or inducers of CYP450 enzymes (e.g., inhibitors such as protease inhibitors, grapefruit juice, certain fluoroquinolone and macrolide antibiotics, azole antifungals and inducers such as St. John’s Wort) or P-glycoprotein. In view of the long and variable half- life of amiodarone, potential for drug interactions exists not only with concomitant medications but also with drugs administered after discontinuation of amiodarone [see CLINICAL PHARMACOLOGY (12.3)].
Patients should avoid grapefruit juice beverages while taking amiodarone because exposure to amiodarone is significantly increased [see CLINICAL PHARMACOLOGY (12.3)].
Antiarrhythmics
The metabolism of quinidine, procainamide, and flecainide can be inhibited by amiodarone. In general, initiate any added antiarrhythmic drug at a lower than usual dose and monitor the patient carefully.During transfer to oral amiodarone, reduce the dose levels of previously administered antiarrhythmic agents by 30% to 50% several days after the addition of oral amiodarone. Review the continued need for the other antiarrhythmic agent after the effects of amiodarone have been established, and attempt discontinuation [see CLINICAL PHARMACOLOGY (12.3)].
Digoxin
In patients receiving digoxin therapy, administration of oral amiodarone results in an increase in serum digoxin concentration. Reduce dose of digoxin by half or discontinue digoxin. If digitalis treatment is continued, monitor serum levels closely and observe patients for clinical evidence of toxicity [see CLINICAL PHARMACOLOGY (12.3)].HMG-CoA Reductase Inhibitors
Limit the dose of simvastatin in patients on amiodarone to 20 mg daily. Limit the daily dose of lovastatin to 40 mg. Lower starting and maintenance doses of other CYP3A4 substrates (e.g., atorvastatin) may be required as amiodarone may increase the plasma concentration of these drugs.Anticoagulants
Potentiation of warfarin-type (CYP2C9 and CYP3A substrate) anticoagulant response is almost always seen in patients receiving amiodarone and can result in serious or fatal bleeding. Since the concomitant administration of warfarin with amiodarone increases INR by 100% after 3 to 4 days, reduce the dose of the anticoagulant by one-third to one-half, and monitor INR closely.Cyclosporine (CYP3A Substrate)
Administered in combination with oral amiodarone has been reported to produce persistently elevated plasma concentrations of cyclosporine resulting in elevated creatinine, despite reduction in dose of cyclosporine. Monitor cyclosporine drug levels and renal function in patients taking both drugs.Increased steady-state levels of phenytoin during concomitant therapy with amiodarone have been reported. Monitor phenytoin levels in patients taking both drugs.
7.3 Serious Symptomatic Bradycardia When Co-administered with Ledipasvir/Sofosbuvir or with Sofosbuvir with Simeprevir
Postmarketing cases of symptomatic bradycardia, some requiring pacemaker insertion and at least one fatal, have been reported when ledipasvir/sofosbuvir or sofosbuvir with simeprevir were initiated in patients on amiodarone. Bradycardia generally occurred within hours to days, but in some cases up to 2 weeks after initiating antiviral treatment. Bradycardia generally resolved after discontinuation of antiviral treatment. The mechanism for this effect is unknown. Monitor heart rate in patients taking or recently discontinuing amiodarone when starting antiviral treatment.CLOSE
-
8 Use in Specific Populations
8.1 Pregnancy
Pregnancy Category D [see WARNINGS AND PRECAUTIONS (5.8)].Teratogenic Effects
Amiodarone and desethylamiodarone cross the placenta.Reported risks include:
neonatal bradycardia, QT prolongation, and periodic ventricular extrasystoles
neonatal hypothyroidism (with or without goiter) detected antenatally or in the newborn and reported even after a few days of exposure
neonatal hyperthyroxinemia
neurodevelopmental abnormalities independent of thyroid function, including speech delay and difficulties with written language and arithmetic, delayed motor development, and ataxia.
jerk nystagmus with synchronous head titubation
fetal growth retardation
premature birth
Amiodarone has caused a variety of adverse effects in animals.Amiodarone was given intravenously to rabbits at dosages of 5 mg/kg per day, 10 mg/kg per day, or 25 mg/kg per day (about 0.1, 0.3, and 0.7 times the human intravenous maintenance dose of 0.5 mg/min on a body surface area basis), during gestation days 8 to 16 (organogenesis). The incidence of maternal deaths increased with increasing dose and occurred in all treated groups, and controls. Mean fetal weights were significantly decreased in the low and middle dose groups and embryotoxicity (as manifested by fewer full- term fetuses and increased resorptions) occurred at dosages of 10 mg/kg and above. There were no significant differences in the number of minor fetal abnormalities and no major fetal abnormalities were observed.
Amiodarone was administered by continuous intravenous infusion to rats at dosages of 25 mg/kg per day, 50 mg/kg per day, or 100 mg/kg per day (about 0.3, 0.7, and 1.3 times the human intravenous maintenance dose of 0.5 mg/min on a body surface area basis) during gestation days 8 to 16 (organogenesis). Maternal toxicity (manifest as reduced weight gain and food consumption) and embryotoxicity (manifest as increased resorptions, decreased live litter size and fetal body weights, and delayed sternal and metacarpal ossification) were observed in the 100 mg/kg group. The delayed ossification was reversible and related to decreased fetal weight. Fetal thyroid tissues appeared normal in all groups.
Nonteratogenic Effects
Very high concentrations of amiodarone and desethylamiodarone may be found in testes. Elevated follicle-stimulating hormone and luteinizing hormone levels, suggestive of testicular dysfunction, have been reported in men on long-term amiodarone treatment.While planning pregnancy after discontinuation of amiodarone treatment, consider the long half-life of amiodarone and its metabolite DEA.
8.2 Labor and Delivery
It is not known whether the use of amiodarone during labor or delivery has any immediate or delayed adverse effects. Preclinical studies in rodents have not shown any effect on the duration of gestation or on parturition.8.3 Nursing Mothers
Amiodarone and one of its major metabolites, desethylamiodarone (DEA), are excreted in human milk, suggesting that breast-feeding could expose the nursing infant to a significant dose of the drug. Nursing offspring of lactating rats administered amiodarone have demonstrated reduced viability and reduced body weight gains. The risk of exposing the infant to amiodarone must be weighed against the potential benefit of arrhythmia suppression in the mother. Advise the mother to discontinue nursing.8.4 Pediatric Use
The safety and effectiveness of amiodarone in pediatric patients have not been established; therefore, the use of amiodarone in pediatric patients is not recommended. In a pediatric trial of 61 patients, aged 30 days to 15 years, hypotension (36%), bradycardia (20%), and AV block (15%) were common dose-related adverse reactions and were severe or life-threatening in some cases. Injection site reactions were seen in 5 (25%) of the 20 patients receiving intravenous amiodarone through a peripheral vein irrespective of dose regimen.Amiodarone hydrochloride injection contains the preservative benzyl alcohol [see DESCRIPTION (11)]. There have been reports of fatal "gasping syndrome" in neonates (children less than one month of age) following the administration of intravenous solutions containing the preservative benzyl alcohol. Symptoms include a striking onset of gasping respiration, hypotension, bradycardia, and cardiovascular collapse.
8.5 Geriatric Use
Clinical studies of amiodarone did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. Carefully consider dose selection in an elderly patient. In general, start at the low end of the dosing range in the elderly to reflect the greater frequency of decreased hepatic, renal, or cardiac function, and concomitant disease or other drug therapy.CLOSE
10 OVERDOSAGE
There have been cases, some fatal, of amiodarone overdose. Effects of an inadvertent overdose of intravenous amiodarone include hypotension, cardiogenic shock, bradycardia, AV block, and hepatotoxicity. Treat hypotension and cardiogenic shock by slowing the infusion rate or with standard therapy: vasopressor drugs, positive inotropic agents, and volume expansion. Bradycardia and AV block may require temporary pacing. Monitor hepatic enzyme concentrations closely. Neither amiodarone nor DEA is dialyzable. -
10 OVERDOSAGE
There have been cases, some fatal, of amiodarone overdose. Effects of an inadvertent overdose of intravenous amiodarone include hypotension, cardiogenic shock, bradycardia, AV block, and hepatotoxicity. Treat hypotension and cardiogenic shock by slowing the infusion rate or with standard therapy: vasopressor drugs, positive inotropic agents, and volume expansion. Bradyardia and AV block may require temporary pacing. Monitor hepatic enzyme concentrations closely. Amiodarone is not dialyzable.
-
11 DESCRIPTION
Amiodarone hydrochloride injection, USP contains amiodarone hydrochloride, USP (C25H29I2NO3HCl), a class III antiarrhythmic drug. Amiodarone hydrochloride is (2-butyl-3-benzo-furanyl)[4-[2-(diethylamino)ethoxy]-3,5-diiodophenyl]methanone hydrochloride.
Amiodarone hydrochloride has the following structural formula:


Amiodarone hydrochloride is a white to slightly yellow crystalline powder, and is very slightly soluble in water. It has a molecular weight of 681.78 and contains 37.3% iodine by weight. Amiodarone hydrochloride injection is a sterile clear, pale-yellow micellar solution visually free from particulates. Each milliliter of the amiodarone formulation contains 50 mg of amiodarone hydrochloride, 20.2 mg of benzyl alcohol, 100 mg of polysorbate 80, and water for injection.
Amiodarone hydrochloride injection contains polysorbate 80, which is known to leach di-(2-ethylhexyl)phthalate (DEHP) from polyvinylchloride (PVC) [see DOSAGE AND ADMINISTRATION (2)].
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Amiodarone is generally considered a class III antiarrhythmic drug, but it possesses electrophysiologic characteristics of all four Vaughan Williams classes. Like class I drugs, amiodarone blocks sodium channels at rapid pacing frequencies, and like class II drugs, amiodarone exerts a noncompetitive antisympathetic action. One of its main effects, with prolonged administration, is to lengthen the cardiac action potential, a class III effect. The negative chronotropic effect of amiodarone in nodal tissues is similar to the effect of class IV drugs. In addition to blocking sodium channels, amiodarone blocks myocardial potassium channels, which contributes to slowing of conduction and prolongation of refractoriness. The antisympathetic action and the block of calcium and potassium channels are responsible for the negative dromotropic effects on the sinus node and for the slowing of conduction and prolongation of refractoriness in the atrioventricular (AV) node. Its vasodilatory action can decrease cardiac workload and consequently myocardial oxygen consumption.Intravenous amiodarone administration prolongs intranodal conduction (Atrial-His, AH) and refractoriness of the atrioventricular node (ERP AVN), but has little or no effect on sinus cycle length (SCL), refractoriness of the right atrium and right ventricle (ERP RA and ERP RV), repolarization (QTc), intraventricular conduction (QRS), and infra-nodal conduction (His-ventricular, HV). A comparison of the electrophysiologic effects of intravenous amiodarone and oral amiodarone is shown in the table below.
Table 6: EFFECTS OF INTRAVENOUS AND ORAL AMIODARONE ON ELECTROPHYSIOLOGIC PARAMETERS
Formulation SCL QRS QTc AH HV ERP
RA
ERP
RV
ERP
AVN
Intravenous Oral -
7 NONCLINICAL TECHNOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity studies were conducted with intravenous administration of amiodarone. However, oral amiodarone caused a statistically significant, dose-related increase in the incidence of thyroid tumors (follicular adenoma and carcinoma) in rats. The incidence of thyroid tumors in rats was greater than the incidence in controls even at the lowest dose level tested, i.e., 5 mg/kg/day (much less, on a body surface area basis, than the maximum recommended human maintenance dose of 600 mg/day).Mutagenicity studies conducted with amiodarone HCl (Ames, micronucleus, and lysogenic induction tests) were negative.
No fertility studies were conducted with intravenous administration of amiodarone. However, in a study in which amiodarone HCl was orally administered to male and female rats, beginning 9 weeks prior to mating, reduced fertility was observed at a dose level of 90 mg/kg/day (approximately 1.4 times the maximum recommended human maintenance dose of 600 mg/day).
-
14 CLINICAL STUDIES
Apart from studies in patients with VT or VF, described below, there are two other studies of amiodarone showing an antiarrhythmic effect before significant levels of DEA could have accumulated. A placebo-controlled study of intravenous amiodarone (300 mg over 2 hours followed by 1200 mg/day) in post-coronary artery bypass graft patients with supraventricular and 2- to 3-consecutive-beat ventricular arrhythmias showed a reduction in arrhythmias from 12 hours on. A baseline-controlled study using a similar IV regimen in patients with recurrent, refractory VT/VF also showed rapid onset of antiarrhythmic activity; amiodarone therapy reduced episodes of VT by 85% compared to baseline.
The acute effectiveness of intravenous amiodarone in suppressing recurrent VF or hemodynamically unstable VT is supported by two randomized, parallel, dose-response studies of approximately 300 patients each. In these studies, patients with at least two episodes of VF or hemodynamically unstable VT in the preceding 24 hours were randomly assigned to receive doses of approximately 125 mg or 1000 mg over the first 24 hours, an 8-fold difference. In one study, a middle dose of approximately 500 mg was evaluated. The dose regimen consisted of an initial rapid loading infusion, followed by a slower 6-hour loading infusion, and then an 18-hour maintenance infusion. The maintenance infusion was continued up to hour 48. Additional 10-minute infusions of 150 mg intravenous amiodarone were given for "breakthrough" VT/VF more frequently to the 125 mg dose group, thereby considerably reducing the planned 8-fold differences in total dose to 1.8- and 2.6-fold, respectively, in the two studies.
The prospectively defined primary efficacy end point was the rate of VT/VF episodes per hour. For both studies, the median rate was 0.02 episodes per hour in patients receiving the high dose and 0.07 episodes per hour in patients receiving the low dose, or approximately 0.5 versus 1.7 episodes per day (p = 0.07, 2-sided, in both studies). In one study, the time to first episode of VT/VF was significantly prolonged (approximately 10 hours in patients receiving the low dose and 14 hours in patients receiving the high dose). In both studies, significantly fewer supplemental infusions were given to patients in the high-dose group. At the end of double-blind therapy or after 48 hours, all patients were given open access to whatever treatment (including intravenous amiodarone) was deemed necessary. Mortality was not affected in these studies.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Amiodarone Hydrochloride Injection USP, 50 mg/mL, is available in:
150 mg/3 mL - single-dose vial - NDC: 67457-153-03, packages of 10.
450 mg/9 mL - single-dose vial - NDC: 67457-153-09, packages of 10.
900 mg/18 mL - single-dose vial - NDC: 67457-153-18, packages of 1.
Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.]
Protect from light and excessive heat.
Use carton to protect contents from light until used.
Discard unused portion.
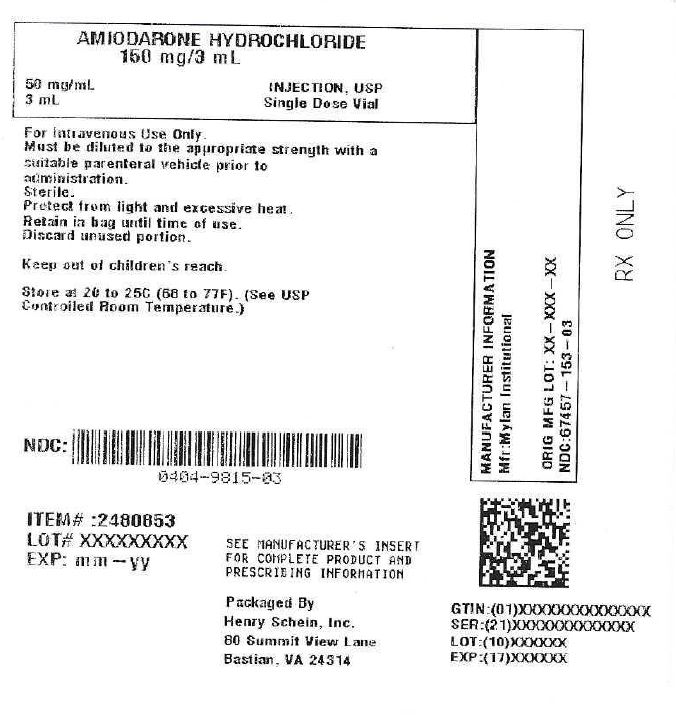
Stoppers are not made with natural rubber latex.Product repackaged by: Henry Schein, Inc., Bastian, VA 24314 From Original Manufacturer/Distributor's NDC and Unit of Sale To Henry Schein Repackaged Product NDC and Unit of Sale Total Strength/Total Volume (Concentration) per unit NDC: 67457-153-03
Packages of 10NDC: 0404-9815-03
1 single-dose vial in a bag
(Vial bears NDC: 67457-153-00)150 mg/3 mL
(50 mg/mL) -
17 PATIENT COUNSELING INFORMATION
Amiodarone has the potential to cause serious side effects that limit its use to life-threatening and hemodynamically unstable cardiac arrhythmias. Advise female patients to discontinue nursing while being treated with amiodarone, as breast-feeding could expose the nursing infant to a significant dose of the drug. Recommend that patients avoid grapefruit juice, over-the-counter cough medicines (which commonly contain dextromethorphan), and St. John's Wort. Inform patients that most manufacturers of corneal refractive laser surgery devices contraindicate corneal refractive laser surgery in patients taking amiodarone. Discuss the symptoms of hypo- and hyper-thyroidism, particularly if patients will be transitioned to oral amiodarone.
Manufactured for:
Mylan Institutional LLC
Morgantown, WV 26505 U.S.A.Manufactured by:
Mylan Institutional
Galway, Ireland0920L103
Revised: 7/2020
MI:AMDRIJ:R6 - Sample Package Label
-
INGREDIENTS AND APPEARANCE
AMIODARONE HYDROCHLORIDE
amiodarone hydrochloride injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0404-9815(NDC:67457-153) Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Amiodarone Hydrochloride (UNII: 976728SY6Z) (Amiodarone - UNII:N3RQ532IUT) Amiodarone Hydrochloride 50 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0404-9815-03 1 in 1 BAG 01/08/2022 03/31/2026 1 3 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076217 01/08/2022 03/31/2026 Labeler - Henry Schein, Inc (012430880)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.