ASTAGRAF XL- tacrolimus extended-release capsules capsule, coated, extended release
ASTAGRAF XL by
Drug Labeling and Warnings
ASTAGRAF XL by is a Prescription medication manufactured, distributed, or labeled by Astellas Pharma US, Inc., Astellas Ireland Co., Ltd., Astellas Pharma Tech Co., Ltd.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ASTAGRAF XL® safely and effectively. See full prescribing information for ASTAGRAF XL.
ASTAGRAF XL (tacrolimus extended-release capsules), for oral use
Initial U.S. Approval: 1994WARNING: MALIGNANCIES AND SERIOUS INFECTIONS IN TRANSPLANT PATIENTS; and INCREASED MORTALITY IN FEMALE LIVER TRANSPLANT PATIENTS
See full prescribing information for complete boxed warning.
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
- Capsules must be taken whole. (2.1)
- Take consistently every morning at the same time on an empty stomach at least 1 hour before a meal or at least 2 hours after a meal. (2.1)
- Avoid eating grapefruit or drinking grapefruit juice or alcohol. (2.1)
- African-American patients and patients with severe hepatic impairment may require dosing adjustments. (2.3)
- Frequent monitoring of trough concentrations is recommended. (2.4)
- For complete dosing information, see full prescribing information.
MMF = Mycophenolate mofetil Recommended ASTAGRAF XL Initial Dosage
Patient Population
Initial Oral Dosage
Whole Blood Trough Concentration Range
ADULT
With basiliximab, MMF and steroids
0.15 to 0.2 mg/kg once daily prior to reperfusion or within 48 hours of completion of transplant
- Month 1: 7-15 ng/mL
- Months 2-6: 5-15 ng/mL
- > 6 Months: 5-10 ng/mL
With MMF and steroids, without basiliximab induction
-
First dose
(pre-operative):
0.1 mg/kg, within 12 hours prior to reperfusion - Subsequent doses (post-operative): 0.2 mg/kg once daily at least 4 hours after pre-operative dose and within 12 hours after reperfusion
- Month 1: 10-15 ng/mL
- Months 2-6: 5-15 ng/mL
- > 6 Months: 5-10 ng/mL
PEDIATRIC
With basiliximab, MMF and steroids
0.3 mg/kg once daily, administered within 24 hours following reperfusion
- Month 1: 10-20 ng/mL
- > Month 1: 5-15 ng/mL
DOSAGE FORMS AND STRENGTHS
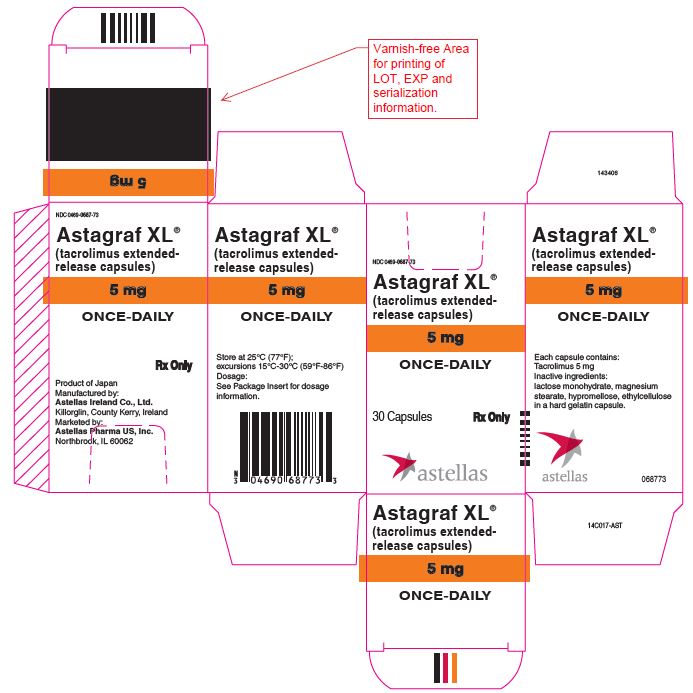
Capsules: 0.5 mg, 1 mg, 5 mg (3)
CONTRAINDICATIONS
Known hypersensitivity to tacrolimus. (4)
WARNINGS AND PRECAUTIONS
- Not Interchangeable with Other Tacrolimus Products-Medication Errors: Instruct patients or caregivers to recognize the appearance of ASTAGRAF XL capsules. (5.4)
- New onset diabetes after transplant: Monitor blood glucose. (5.5)
- Nephrotoxicity (acute and/or chronic): May occur due to ASTAGRAF XL, drug interactions, concomitant nephrotoxic drugs. Monitor renal function; consider dosage reduction. (5.6)
- Neurotoxicity: Including risk of posterior reversible encephalopathy syndrome (PRES), monitor for neurologic abnormalities; reduce dosage or discontinue ASTAGRAF XL. (5.7)
- Hyperkalemia: Risk may be increased with other agents associated with hyperkalemia; monitor serum potassium levels. (5.8)
- Hypertension: May require antihypertensive therapy; monitor relevant drug interactions. (5.9)
- QT prolongation: Consider obtaining electrocardiograms and monitoring electrolytes in patients at high risk. (5.11)
- Immunizations: Avoid live vaccines. (5.12)
- Pure red cell aplasia: Consider discontinuation of ASTAGRAF XL. (5.13)
ADVERSE REACTIONS
The most common adverse reactions (≥ 30%) are: diarrhea, constipation, nausea, peripheral edema, tremor and anemia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Astellas Pharma US, Inc. at 1-800-727-7003 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: MALIGNANCIES AND SERIOUS INFECTIONS IN TRANSPLANT PATIENTS; and INCREASED MORTALITY IN FEMALE LIVER TRANSPLANT PATIENTS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 Dosing for Kidney Transplant Patients
2.3 Dosage Adjustments: African-American Patients, Patients with Hepatic Impairment, Drug Interactions
2.4 Therapeutic Drug Monitoring
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Lymphoma and Other Malignancies
5.2 Serious Infections
5.3 Increased Mortality in Female Liver Transplant Patients
5.4 Not Interchangeable with Other Tacrolimus Products - Medication Errors
5.5 New Onset Diabetes After Transplant
5.6 Nephrotoxicity due to ASTAGRAF XL and Drug Interactions
5.7 Neurotoxicity
5.8 Hyperkalemia
5.9 Hypertension
5.10 Risk of Rejection with Strong CYP3A Inducers and Risk of Serious Adverse Reactions with Strong CYP3A Inhibitors
5.11 QT Prolongation
5.12 Immunizations
5.13 Pure Red Cell Aplasia
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Mycophenolic Acid
7.2 Effects of Other Drugs on ASTAGRAF XL
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Race or Ethnicity
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 ASTAGRAF XL with Basiliximab Induction
14.2 Clinical Study of ASTAGRAF XL without Induction
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Administration
17.2 Development of Lymphoma and Other Malignancies
17.3 Increased Risk of Infection
17.4 New Onset Diabetes After Transplant
17.5 Nephrotoxicity
17.6 Neurotoxicity
17.7 Hyperkalemia
17.8 Hypertension
17.9 Drug Interactions
17.10 Pregnancy, Lactation and Infertility
17.11 Immunizations
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: MALIGNANCIES AND SERIOUS INFECTIONS IN TRANSPLANT PATIENTS; and INCREASED MORTALITY IN FEMALE LIVER TRANSPLANT PATIENTS
- Increased risk for developing serious infections and malignancies with ASTAGRAF XL® or other immunosuppressants that may lead to hospitalization or death. [see Warnings and Precautions (5.1, 5.2)]
- Increased mortality in female liver transplant patients with ASTAGRAF XL. ASTAGRAF XL is not approved for use in liver transplantation. [see Warnings and Precautions (5.3)]
-
1 INDICATIONS AND USAGE
ASTAGRAF XL® is indicated for the prophylaxis of organ rejection in kidney transplant patients in combination with other immunosuppressants in adult and pediatric patients who can swallow capsules intact [see Use in Specific Populations (8.4) and Clinical Studies (14.1), (14.2)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
- ASTAGRAF XL should not be used without the supervision by a physician with experience in immunosuppressive therapy.
- ASTAGRAF XL (tacrolimus extended-release capsules) is not interchangeable or substitutable for tacrolimus extended-release tablets, tacrolimus immediate-release capsules or tacrolimus for oral suspension. Under or overexposure to tacrolimus may result in graft rejection or other serious adverse reactions. Changes between tacrolimus immediate-release and extended-release dosage forms must occur under physician supervision [see Warnings and Precautions (5.4)].
- Advise patients to swallow ASTAGRAF XL capsules whole with liquid; patients must not chew, divide, or crush the capsules.
- ASTAGRAF XL should be taken consistently every morning at the same time to ensure consistent and maximum possible drug exposure, on an empty stomach at least 1 hour before a meal, or at least 2 hours after a meal [see Clinical Pharmacology (12.3)].
- If a dose is missed, the dose may be taken up to 14 hours after the scheduled time (i.e., for a missed 8:00 AM dose, a dose may be taken by 10:00 PM). Beyond the 14-hour time frame, the patient should wait until the usual scheduled time the following morning to take the next regular daily dose. Instruct the patient not to double the next dose.
- Advise patients to avoid eating grapefruit or drinking grapefruit juice or alcoholic beverages while taking ASTAGRAF XL [see Drug Interactions (7.2)].
- Therapeutic drug monitoring is recommended for all patients receiving ASTAGRAF XL [see Dosage and Administration (2.4)].
2.2 Dosing for Kidney Transplant Patients
Table 1 includes the recommended starting ASTAGRAF XL dosages and whole blood trough concentration ranges; the observed trough concentrations are shown in another section of the Full Prescribing Information [see Clinical Studies (14)]. Titrate the ASTAGRAF XL dosage based on clinical assessments of rejection and tolerability, and to achieve target trough concentration ranges [see Dosage and Administration (2.4) and Warnings and Precautions (5.6, 5.7, 5.10, 5.11)].
Table 1: Recommended Starting Daily Dosage Regimen of ASTAGRAF XL MMF = mycophenolate mofetil Recommended ASTAGRAF XL Initial Dosage*
Patient Population
Initial Oral Dosage
Whole Blood Trough Concentration Range
ADULT
With basiliximab, MMF and steroids
0.15 to 0.2 mg/kg once daily prior to reperfusion or within 48 hours of completion of transplant
Month 1: 7-15 ng/mL
Months 2-6: 5-15 ng/mL
> 6 Months: 5-10 ng/mL
With MMF and steroids, without basiliximab induction
First dose (pre-operative): 0.1 mg/kg, within 12 hours prior to reperfusion
Subsequent doses (post-operative): 0.2 mg/kg once daily at least 4 hours after pre-operative dose and within 12 hours after reperfusion
Month 1: 10-15 ng/mL
Months 2-6: 5-15 ng/mL
> 6 Months: 5-10 ng/mL
PEDIATRIC
With basiliximab, MMF and steroids
0.3 mg/kg once daily, administered within 24 hours following reperfusion.
Month 1: 10-20 ng/mL
> Month 1: 5-15 ng/mL
2.3 Dosage Adjustments: African-American Patients, Patients with Hepatic Impairment, Drug Interactions
African-American patients, compared to Caucasian patients, may need to be titrated to higher ASTAGRAF XL dosages to attain comparable trough concentrations [see Clinical Pharmacology (12.3) and Clinical Studies (14)].
Patients with severe hepatic impairment (Child-Pugh ≥ 10) may require a lower starting dosage of ASTAGRAF XL, due to the reduced clearance and prolonged half-life [see Clinical Pharmacology (12.3)].
Dose adjustments of ASTAGRAF XL may be necessary when administered concomitantly with CYP3A inducers or CYP3A inhibitors [see Warnings and Precautions (5.10) and Drug Interactions (7.2)].
2.4 Therapeutic Drug Monitoring
Measure tacrolimus whole blood trough concentrations at least two times on separate days during the first week after initiation of dosing and after a change in dosage, after a change in coadministration of CYP3A4 inducers and/or inhibitors, or after a change in renal or hepatic function. When interpreting measured concentrations, consider that the time to achieve tacrolimus steady state is approximately 7 days after initiating or changing the ASTAGRAF XL dose.
Monitor tacrolimus whole blood trough concentrations using a validated assay [e.g., immunoassays or high performance liquid chromatography with tandem mass spectrometric detection (HPLC/MS/MS)]. The immunosuppressive activity of tacrolimus is mainly due to the parent drug rather than to its metabolites. Immunoassays may react with metabolites as well as the parent drug. Therefore, whole blood tacrolimus trough concentrations obtained with immunoassays may be numerically higher than concentrations obtained with an assay using HPLC/MS/MS. Comparison of the whole blood tacrolimus trough concentrations of patients to those described in the prescribing information and other published literature must be made with knowledge of the assay method(s) employed.
-
3 DOSAGE FORMS AND STRENGTHS
ASTAGRAF XL CAPSULES:
0.5 mg: light yellow cap and orange body branded with red “
 647” on the capsule body and “0.5 mg” on the capsule cap.
647” on the capsule body and “0.5 mg” on the capsule cap.1 mg: white cap and orange body branded with red “
 677” on the capsule body and “1 mg” on the capsule cap.
677” on the capsule body and “1 mg” on the capsule cap.5 mg: grayish-red cap and orange body branded with red “
 687” on the capsule body and “5 mg” on the capsule cap.
687” on the capsule body and “5 mg” on the capsule cap. -
4 CONTRAINDICATIONS
ASTAGRAF XL is contraindicated in patients with known hypersensitivity to tacrolimus [see Adverse Reactions (6.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Lymphoma and Other Malignancies
Immunosuppressants, including ASTAGRAF XL, increase the risk of developing lymphomas and other malignancies, particularly of the skin [see Boxed Warning]. The risk appears to be related to the intensity and duration of immunosuppression rather than to the use of any specific agent. Examine patients for skin changes and advise to avoid or limit exposure to sunlight and UV light by wearing protective clothing and using a broad spectrum sunscreen with a high protection factor.
Post-transplant lymphoproliferative disorder (PTLD), associated with Epstein-Barr Virus (EBV), has been reported in immunosuppressed organ transplant patients. The risk of PTLD appears greatest in patients who are EBV seronegative, a population which includes many young children. Monitor EBV serology during treatment.
5.2 Serious Infections
Immunosuppressants, including ASTAGRAF XL, increase the risk of developing bacterial, viral, fungal, and protozoal infections, including opportunistic infections. These infections may lead to serious, including fatal, outcomes. Serious viral infections reported include:
- Polyomavirus-associated nephropathy (especially due to BK virus infection)
- JC virus-associated progressive multifocal leukoencephalopathy (PML)
- Cytomegalovirus (CMV) infections: CMV seronegative transplant patients who receive an organ from a CMV seropositive donor are at highest risk of CMV viremia and CMV disease.
Monitor for the development of infection and adjust the immunosuppressive regimen to balance the risk of rejection with the risk of infection [see Adverse Reactions (6.1, 6.2)].
5.3 Increased Mortality in Female Liver Transplant Patients
In a clinical trial of 471 liver transplant patients randomized to ASTAGRAF XL or tacrolimus immediate-release product, mortality at 12 months was 10% higher among the 76 female patients (18%) treated with ASTAGRAF XL compared to the 64 female patients (8%) treated with tacrolimus immediate-release product. ASTAGRAF XL is not approved for the prophylaxis of organ rejection in patients who received a liver transplant.
5.4 Not Interchangeable with Other Tacrolimus Products - Medication Errors
Medication errors, including substitution and dispensing errors, between tacrolimus immediate-release products and ASTAGRAF XL (tacrolimus extended-release capsules) were reported outside the U.S. This led to serious adverse reactions, including graft rejection, or other adverse reactions due to under- or over-exposure to tacrolimus. ASTAGRAF XL is not interchangeable or substitutable for tacrolimus extended-release tablets, tacrolimus immediate-release capsules or tacrolimus for oral suspension. Changes between tacrolimus immediate-release and extended-release dosage forms must occur under physician supervision. Instruct patients and caregivers to recognize the appearance of ASTAGRAF XL capsules [see Dosage Forms and Strengths (3)] and to confirm with the healthcare provider if a different product is dispensed or if dosing instructions have changed.
5.5 New Onset Diabetes After Transplant
ASTAGRAF XL caused new onset diabetes after transplant (NODAT) in kidney transplant patients, which may be reversible in some patients. African-American and Hispanic kidney transplant patients are at an increased risk. Monitor blood glucose concentrations and treat appropriately [see Adverse Reactions (6.1) and Use in Specific Populations (8.8)].
5.6 Nephrotoxicity due to ASTAGRAF XL and Drug Interactions
ASTAGRAF XL, like other calcineurin-inhibitors, can cause acute or chronic nephrotoxicity. Consider dosage reduction in patients with elevated serum creatinine and tacrolimus whole blood trough concentrations greater than the recommended range.
The risk for nephrotoxicity may increase when ASTAGRAF XL is concomitantly administered with CYP3A inhibitors (by increasing tacrolimus whole blood concentrations) or drugs associated with nephrotoxicity (e.g., aminoglycosides, ganciclovir, amphotericin B, cisplatin, nucleotide reverse transcriptase inhibitors, protease inhibitors) [see Adverse Reactions (6.1, 6.2) and Drug Interactions (7.2)]. Monitor renal function and consider dosage reduction if nephrotoxicity occurs.
5.7 Neurotoxicity
ASTAGRAF XL may cause a spectrum of neurotoxicities. The most severe neurotoxicities include posterior reversible encephalopathy syndrome (PRES), delirium, seizure and coma; others include tremors, paresthesias, headache, mental status changes, and changes in motor and sensory functions [see Adverse Reactions (6.1, 6.2)]. As symptoms may be associated with tacrolimus whole blood trough concentrations at or above the recommended range, monitor for neurologic symptoms and consider dosage reduction or discontinuation of ASTAGRAF XL if neurotoxicity occurs.
5.8 Hyperkalemia
Mild to severe hyperkalemia, which may require treatment, has been reported with tacrolimus including ASTAGRAF XL. Concomitant use of agents associated with hyperkalemia (e.g., potassium-sparing diuretics, ACE inhibitors, angiotensin receptor blockers) may increase the risk for hyperkalemia [see Adverse Reactions (6.1)]. Monitor serum potassium levels periodically during treatment.
5.9 Hypertension
Hypertension is a common adverse reaction of ASTAGRAF XL therapy and may require antihypertensive therapy [see Adverse Reactions (6.1)]. Some antihypertensive drugs can increase the risk for hyperkalemia [see Warnings and Precautions (5.8)]. Calcium-channel blocking agents may increase tacrolimus blood concentrations and require dosage reduction of ASTAGRAF XL [see Drug Interactions (7.2)].
5.10 Risk of Rejection with Strong CYP3A Inducers and Risk of Serious Adverse Reactions with Strong CYP3A Inhibitors
The concomitant use of strong CYP3A inducers may increase the metabolism of tacrolimus, leading to lower whole blood trough concentrations and greater risk of rejection. In contrast, the concomitant use of strong CYP3A inhibitors may decrease the metabolism of tacrolimus, leading to higher whole blood trough concentrations and greater risk of serious adverse reactions (e.g., neurotoxicity, QT prolongation) [see Warnings and Precautions (5.7, 5.11)]. Therefore, adjust ASTAGRAF XL dose and monitor tacrolimus whole blood trough concentrations when coadministering ASTAGRAF XL with strong CYP3A inhibitors (e.g., including, but not limited to, telaprevir, boceprevir, ritonavir, ketoconazole, itraconazole, voriconazole, clarithromycin) or strong CYP3A inducers (e.g., including, but not limited to, rifampin, rifabutin) [see Dosage and Administration (2.4) and Drug Interactions (7.2)].
5.11 QT Prolongation
ASTAGRAF XL may prolong the QT/QTc interval and cause Torsade de Pointes. Avoid ASTAGRAF XL in patients with congenital long QT syndrome. Consider obtaining electrocardiograms and monitoring electrolytes (magnesium, potassium, calcium) periodically during treatment in patients with congestive heart failure, bradyarrhythmias, those taking certain antiarrhythmic medications or other products that lead to QT prolongation, and those with electrolyte disturbances (e.g., hypokalemia, hypocalcemia, or hypomagnesemia).
When coadministering ASTAGRAF XL with other substrates and/or inhibitors of CYP3A, especially those that also have the potential to prolong the QT interval, a reduction in ASTAGRAF XL dosage, monitoring of tacrolimus whole blood concentrations, and monitoring for QT prolongation is recommended [see Dosage and Administration (2.4) and Drug Interactions (7.2)].
5.12 Immunizations
Whenever possible, administer the complete complement of vaccines before transplantation and treatment with ASTAGRAF XL.
Avoid the use of live attenuated vaccines during treatment with ASTAGRAF XL (e.g., intranasal influenza, measles, mumps, rubella, oral polio, BCG, yellow fever, varicella, and TY21a typhoid vaccines).
Inactivated vaccines noted to be safe for administration after transplantation may not be sufficiently immunogenic during treatment with ASTAGRAF XL.
5.13 Pure Red Cell Aplasia
Cases of pure red cell aplasia (PRCA) have been reported in patients treated with tacrolimus. All of these patients reported risk factors for PRCA such as parvovirus B19 infection, underlying disease, or concomitant medications associated with PRCA. A mechanism for tacrolimus-induced PRCA has not been elucidated. If PRCA is diagnosed, consider discontinuation of ASTAGRAF XL.
-
6 ADVERSE REACTIONS
The following clinically significant adverse drug reactions are discussed in greater detail in other sections of labeling:
- Lymphoma and Other Malignancies [see Boxed Warning, Warnings and Precautions (5.1)]
- Serious Infections [see Boxed Warnings, Warnings and Precautions (5.2)]
- Increased Mortality in Female Liver Transplant Patients [see Warnings and Precautions (5.3)]
- New Onset Diabetes after Transplant [see Warnings and Precautions (5.5)]
- Nephrotoxicity due to ASTAGRAF XL and Drug Interactions [see Warnings and Precautions (5.6)]
- Neurotoxicity [see Warnings and Precautions (5.7)]
- Hyperkalemia [see Warnings and Precautions (5.8)]
- Hypertension [see Warnings and Precautions (5.9)]
- QT Prolongation [see Warnings and Precautions (5.11)]
- Pure Red Cell Aplasia [see Warnings and Precautions (5.13)]
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. In addition, the clinical trials were not designed to establish comparative differences across study arms with regards to the adverse reactions discussed below.
Kidney transplant patients were treated with ASTAGRAF XL (N=214) or tacrolimus immediate-release product (N=212) and concomitant immunosuppressants (median duration of exposure of 12 months) in a randomized, open-label, active-controlled trial of mostly U.S. patients (Study 1) [see Clinical Studies (14.1)]. The types of adverse reactions seen in Study 1 were similar to the adverse reactions seen in Study 2 [non-U.S. trial in kidney transplant patients treated with ASTAGRAF XL (N=331) or tacrolimus immediate-release product (N=336) and concomitant immunosuppressants] [see Clinical Studies (14.2)].
In Study 1, the proportion of patients who discontinued treatment due to adverse reactions was 9% and 11% in the ASTAGRAF XL and tacrolimus immediate-release treatment groups, respectively, through 12 months of treatment. The most common adverse reactions leading to discontinuation in ASTAGRAF XL-treated patients were related to infections or renal/urinary disorders.
Infections
The overall incidence of infections, serious infections, and infections with identified etiology reported in patients treated with the ASTAGRAF XL or tacrolimus immediate-release product in Study 1 are shown in Table 2.Table 2: Percentage of Patients with Infections in Study 1* Through One Year Post-Kidney Transplant - * Study 1 was not designed to support comparative claims of ASTAGRAF XL compared to tacrolimus immediate-release product for the adverse reactions reported in this table.
ASTAGRAF XL, MMF,
steroids, basiliximabinduction
N=214Tacrolimus immediate-release
product, MMF, steroids,
basiliximab inductionN=212
All Infections
69%
69%
Respiratory Infections
34%
31%
Urinary Tract Infections
16%
25%
Cytomegalovirus Infections
10%
11%
Bacterial Infections
8%
12%
Gastroenteritis
7%
3%
Polyomavirus Infections
3%
5%
Serious Infections
22%
23%
New Onset Diabetes After Transplant (NODAT)
The incidence of new onset diabetes after transplantation (defined by the composite occurrence of ≥ 2 fasting plasma glucose values that were > 126 mg/dL at ≥ 30 days apart, insulin use for ≥ 30 consecutive days, oral hypoglycemic use for ≥ 30 consecutive days, and/or HbA1C ≥ 6.5%) is summarized in Table 3 below for Study 1 through one year post-transplant [see Warnings and Precautions (5.5)].Table 3: Percentage of Patients with NODAT Through One Year Post-Kidney Transplant in Study 1* ASTAGRAF XL, MMF, steroids, basiliximab induction
N=162Tacrolimus immediate-release product, MMF, steroids, basiliximab induction
N=151- * Study 1 was not designed to support comparative claims of ASTAGRAF XL compared to tacrolimus immediate-release product for the adverse reactions reported in this table.
Composite NODAT
36%
35%
≥ 2 Fasting Plasma Glucose Values
≥ 126 mg/dL ≥ 30 days apart
26%
23%
HbA1C ≥ 6.5%
19%
22%
Oral hypoglycemic use ≥ 30 consecutive days
14%
9%
Insulin use ≥ 30 consecutive days
6%
8%
Hyperkalemia
In Study 1 [see Clinical Studies (14.1)], 73 of 214 (34.1%) patients on ASTAGRAF XL had a serum potassium level greater than 5.4 up to 6.4 mEq/L, and 8 out of 214 (3.7%) patients had a serum potassium level greater than 6.4 mEq/L [see Warnings and Precautions (5.8)].Common Adverse Reactions
The most common (≥ 30%) adverse reactions observed with ASTAGRAF XL in Study 1 were: diarrhea, constipation, nausea, peripheral edema, tremor, and anemia. The incidence of adverse reactions that occurred in ≥ 15% of ASTAGRAF XL-treated patients compared to tacrolimus immediate-release product through one year of treatment in Study 1 is shown by treatment groups in Table 4.Table 4: Adverse Reactions (≥ 15%) in Kidney Transplant Patients Through One Year Post-Transplant in Study 1* - * Study 1 was not designed to support comparative claims of ASTAGRAF XL compared to tacrolimus immediate-release for the adverse reactions reported in this table.
ASTAGRAF XL, MMF,
steroids, basiliximab
induction
N=214
Tacrolimus immediate-release
product, MMF, steroids,
basiliximab induction
N=212
Diarrhea
45%
44%
Constipation
40%
32%
Nausea
36%
35%
Peripheral Edema
36%
34%
Tremor
35%
34%
Anemia
33%
29%
Hypertension
28%
30%
Vomiting
25%
25%
Hypomagnesemia
24%
27%
Insomnia
24%
28%
Hypophosphatemia
23%
28%
Headache
22%
24%
Hyperkalemia
20%
23%
Increased Blood Creatinine
19%
23%
Fatigue
16%
10%
Leukopenia
16%
16%
Hyperlipidemia
16%
17%
Hyperglycemia
16%
18%
Less Frequently Reported Adverse Reactions (< 15% in ASTAGRAF XL-treated patients) by System Organ Class
The following adverse reactions were reported in clinical studies of kidney transplant patients who were treated with ASTAGRAF XL, MMF, and steroids (Studies 1 and 2):
- Blood and Lymphatic System Disorders: Hemolytic anemia, leukocytosis, neutropenia, thrombocytopenia, thrombotic microangiopathy
- Cardiac Disorders: Atrial fibrillation, atrial flutter, tachycardia
- Ear Disorders: Tinnitus
- Eye Disorders: Vision blurred, conjunctivitis
- Gastrointestinal Disorders: Abdominal distension, abdominal pain, aphthous stomatitis, dyspepsia, esophagitis, flatulence, gastritis, gastroesophageal reflux disease
- General Disorders and Administration Site Conditions: Anasarca, asthenia, edema, pyrexia
- Hepatobiliary Disorders: Abnormal hepatic function, cholestasis, hepatitis (acute and chronic), hepatotoxicity
- Infections and Infestations: Condyloma acuminatum, tinea versicolor
- Injury: Fall
- Investigations: Increased blood lactate dehydrogenase, increased blood urea, increased hepatic enzyme
- Metabolism and Nutrition Disorders: Anorexia, hyperphosphatemia, hyperuricemia, hypokalemia, hyponatremia, metabolic acidosis
- Musculoskeletal and Connective Tissue Disorders: Arthralgia, osteopenia, osteoporosis
- Neoplasms: Kaposi’s sarcoma
- Nervous System Disorders: Convulsion, dizziness, hypoesthesia, neurotoxicity, paresthesia, peripheral neuropathy
- Psychiatric Disorders: Agitation, anxiety, confusional state, depression, hallucination, mood swings, nightmare
- Renal and Urinary Disorders: Anuria, oliguria, proteinuria, renal failure, renal tubular necrosis, toxic nephropathy
- Respiratory, Thoracic and Mediastinal Disorders: Acute respiratory distress syndrome, dyspnea, pulmonary edema, productive cough
- Skin and Subcutaneous Tissue Disorders: Acne, alopecia, dermatitis, hyperhidrosis, hypotrichosis, pruritus, rash
- Vascular Disorders: Deep vein thrombosis, flushing
Pediatrics
De Novo Pediatric Transplant Patients
A study was conducted in 44 de novo pediatric transplant patients (including 25 kidney transplant patients; 13 randomized to ASTAGRAF XL and 12 randomized to Prograf), who were started on 0.3 mg/kg daily of tacrolimus product, given once daily for ASTAGRAF XL and divided into two doses for Prograf. Two kidney transplant patients on Prograf discontinued the study (withdrawn consent, sapovirus enteritis). Thirteen (13) pediatric kidney transplant patients completed 52 weeks on ASTAGRAF XL. The most common adverse reactions were diarrhea [7/13 (54%)], increased blood creatinine [6/13 (46%)], hypertension [3/13 (23%)], cough [4/13 (31%)], and upper respiratory tract infection [4/13 (31%)].
Stable Pediatric Transplant Patients
Another study was conducted in 81 stable pediatric allograft recipients (including 48 kidney transplant patients) 5 to 16 years of age converted 1:1 (mg:mg) from Prograf to ASTAGRAF XL. Seventy-six (76) pediatric patients completed at least one year of ASTAGRAF XL-based treatment. Treatment-related adverse reactions were reported in 35%, including 13% serious adverse reactions. The most frequent adverse reactions by system organ class were infections (55.7%), followed by gastrointestinal disorders (27.8%), skin and subcutaneous tissue disorders (21.5%), respiratory, thoracic and mediastinal disorders (20.3% each). The most common adverse reactions were diarrhea (13.9%), headache (13.9%) and cough (11.4%).
6.2 Postmarketing Experience
The following adverse reactions have been reported from marketing experience with tacrolimus in the U.S. and outside the U.S. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These reactions have been chosen for inclusion due to either their seriousness, frequency of reporting or causal connection to ASTAGRAF XL:
- Blood and Lymphatic System Disorders: Agranulocytosis, disseminated intravascular coagulation, hemolytic uremic syndrome, febrile neutropenia, pancytopenia, pure red cell aplasia [see Warnings and Precautions (5.13)], coagulopathy, thrombotic thrombocytopenic purpura, prolonged activated partial thromboplastin time, decreased blood fibrinogen
- Cardiac Disorders: Cardiac arrest, myocardial infarction, ventricular fibrillation, congestive cardiac failure, hypertrophic cardiomyopathy, pericardial effusion, angina pectoris, supraventricular extrasystoles, supraventricular tachycardia, bradycardia, Torsade de Pointes, QT prolongation
- Ear Disorders: Hearing loss
- Eye Disorders: Blindness, optic neuropathy, optic atrophy, photophobia
- Gastrointestinal Disorders: Gastrointestinal hemorrhage, gastrointestinal perforation, pancreatitis, peritonitis, stomach ulcer, intestinal obstruction, ascites, colitis, ileus, impaired gastric emptying, dysphagia
- Hepatobiliary Disorders: Hepatic failure, hepatic necrosis, cirrhosis, cholangitis, venoocclusive liver disease, bile duct stenosis, hepatic steatosis, jaundice
- Hypersensitivity Reactions: Hypersensitivity, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
- Immune System Disorders: Graft versus host disease (acute and chronic)
- Investigations: Increased international normalized ratio
- Metabolism and Nutrition Disorders: Hypoproteinemia
- Musculoskeletal and Connective Tissue Disorders: Rhabdomyolysis, myalgia, polyarthritis, pain in extremity including Calcineurin-Inhibitor Induced Pain Syndrome (CIPS)
- Neoplasms: Lymphoma including EBV-associated lymphoproliferative disorder, hepatosplenic T-cell lymphoma, PTLD [see Warnings and Precautions (5.1)], leukemia, melanoma
- Nervous System Disorders: Cerebral infarction, progressive multifocal leukoencephalopathy (PML) sometimes fatal [see Warnings and Precautions (5.2)], posterior reversible encephalopathy syndrome (PRES) [see Warnings and Precautions (5.7)], coma, status epilepticus, quadriplegia, flaccid paralysis, hemiparesis, aphasia, syncope, carpal tunnel syndrome, nerve compression, mutism, dysarthria, somnolence
- Psychiatric Disorders: Mental status changes
- Renal and Urinary Disorders: Hemorrhagic cystitis, hematuria, urinary retention, urinary incontinence
- Respiratory, Thoracic and Mediastinal Disorders: Interstitial lung disease, pulmonary hypertension, lung infiltration, rhinitis allergic, hiccups
- Skin and Subcutaneous Tissue Disorders: Hyperpigmentation, photosensitivity
- Vascular Disorders: Hemorrhage
-
7 DRUG INTERACTIONS
7.1 Mycophenolic Acid
When ASTAGRAF XL is prescribed with a given dose of a mycophenolic acid (MPA) product, exposure to MPA is higher with ASTAGRAF XL coadministration than with cyclosporine coadministration with MPA, because cyclosporine interrupts the enterohepatic recirculation of MPA while tacrolimus does not. Monitor for MPA-associated adverse reactions and reduce the dose of concomitantly administered mycophenolic acid products as needed.
7.2 Effects of Other Drugs on ASTAGRAF XL
Table 5 displays the effects of other drugs on ASTAGRAF XL.
Table 5: Effects of Other Drugs/Substances on ASTAGRAF XL* - * ASTAGRAF XL dosage adjustment recommendation based on observed effect of coadministered drug on tacrolimus exposures [see Clinical Pharmacology (12.3)], literature reports of altered tacrolimus exposures, or the other drug’s known CYP3A inhibitor/inducer status.
- † High dose or double strength grapefruit juice is a strong CYP3A inhibitor; low dose or single strength grapefruit juice is a moderate CYP3A inhibitor.
- ‡ Strong CYP3A inhibitor/inducer, based on reported effect on exposures to tacrolimus along with supporting in vitro CYP3A inhibitor/inducer data, or based on drug-drug interaction studies with midazolam (sensitive CYP3A probe substrate).
Drug/Substance Class or Name
Drug Interaction Effect
Recommendations
Grapefruit or grapefruit juice†
May increase tacrolimus whole blood trough concentrations and increase the risk of serious adverse reactions (e.g., neurotoxicity, QT prolongation) [see Warnings and Precautions (5.7, 5.10, 5.11)].
Avoid grapefruit or grapefruit juice.
Alcohol
May increase the rate of tacrolimus release and increase the risk of serious adverse reactions (e.g., neurotoxicity, QT prolongation ) [see Warnings and Precautions (5.7, 5.10, 5.11)].
Avoid alcoholic beverages.
Strong CYP3A Inducers‡:
Antimycobacterials (e.g., rifampin, rifabutin), anticonvulsants (e.g., phenytoin, carbamazepine and phenobarbital), St John’s Wort
May decrease tacrolimus whole blood trough concentrations and increase the risk of rejection [see Warnings and Precautions (5.10)].
Increase ASTAGRAF XL dose and monitor tacrolimus whole blood trough concentrations [see Dosage and Administration (2.3, 2.4) and Clinical Pharmacology (12.3)].
Strong CYP3A Inhibitors‡:
Protease inhibitors (e.g, nelfinavir, telaprevir, boceprevir, ritonavir), azole antifungals (e.g., voriconazole, posaconazole, itraconazole, ketoconazole), antibiotics (e.g., clarithromycin, troleandomycin, chloramphenicol), nefazodone, letermovir, Schisandra sphenanthera extracts
May increase tacrolimus whole blood trough concentrations and increase the risk of serious adverse reactions (e.g., neurotoxicity, QT prolongation) [see Warnings and Precautions (5.7, 5.10, 5.11)].
Reduce ASTAGRAF XL dose (for voriconazole and posaconazole, give one-third of the original dose) and adjust dose based on tacrolimus whole blood trough concentrations [see Dosage and Administration (2.3, 2.4) and Clinical Pharmacology (12.3)].
Mild or Moderate CYP3A Inhibitors:
Clotrimazole, antibiotics (e.g., erythromycin, fluconazole), calcium channel blockers (e.g., verapamil, diltiazem, nifedipine, nicardipine), amiodarone, danazol, ethinyl estradiol, cimetidine, lansoprazole and omeprazole
May increase tacrolimus whole blood trough concentrations and increase the risk of serious adverse reactions (e.g., neurotoxicity, QT prolongation) [see Warnings and Precautions (5.7, 5.10, 5.11)].
Monitor tacrolimus whole blood trough concentrations and reduce ASTAGRAF XL dose if needed [see Dosage and Administration (2.3, 2.4) and Clinical Pharmacology (12.3)].
Other drugs, such as:
Magnesium and aluminum hydroxide antacids
MetoclopramideMay increase tacrolimus whole blood trough concentrations and increase the risk of serious adverse reactions (e.g., neurotoxicity, QT prolongation) [see Warnings and Precautions (5.7, 5.10, 5.11)].
Monitor tacrolimus whole blood trough concentrations and reduce ASTAGRAF XL dose if needed [see Dosage and Administration (2.3, 2.4) and Clinical Pharmacology (12.3)].
Mild or Moderate CYP3A Inducers
Methylprednisolone, prednisone
May decrease tacrolimus concentrations.
Monitor tacrolimus whole blood trough concentrations and adjust ASTAGRAF XL dose if needed [see Dosage and Administration (2.3, 2.4)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy registry that monitors pregnancy outcomes in women exposed to ASTAGRAF XL during pregnancy. The Transplantation Pregnancy Registry International (TPRI) is a voluntary pregnancy exposure registry that monitors outcomes of pregnancy in female transplant recipients and those fathered by male transplant recipients exposed to immunosuppressants including tacrolimus. Healthcare providers are encouraged to advise their patients to register by contacting the Transplantation Pregnancy Registry International at 1-877-955-6877 or https://www.transplantpregnancyregistry.org/.
Risk Summary
Tacrolimus can cause fetal harm when administered to a pregnant woman. Data from postmarketing surveillance and TPRI suggest that infants exposed to tacrolimus in utero are at a risk of prematurity, birth defects/congenital anomalies, low birth weight, and fetal distress [see Human Data]. Advise pregnant women of the potential risk to the fetus.
Administration of oral tacrolimus to pregnant rabbits and rats throughout the period of organogenesis was associated with maternal toxicity/lethality, and an increased incidence of abortion, malformation and embryofetal death at clinically relevant doses [0.5 the maximum recommended clinical dose (0.2 mg/kg/day), on a mg/m2 basis]. Administration of oral tacrolimus to pregnant rats after organogenesis and throughout lactation produced maternal toxicity, effects on parturition, reduced pup viability and reduced pup weight at clinically relevant doses (0.8 the maximum recommended clinical dose, on a mg/m2 basis). Administration of oral tacrolimus to rats prior to mating, and throughout gestation and lactation produced maternal toxicity/lethality, marked effects on parturition, embryofetal loss, malformations, and reduced pup viability at clinically relevant doses (0.8 times the maximum recommended clinical dose, on a mg/m2 basis). Interventricular septal defects, hydronephrosis, craniofacial malformations and skeletal effects were observed in offspring that died [see Animal Data].
The background risk of major birth defects and miscarriage in the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo-Fetal Risk
Risks during pregnancy are increased in organ transplant recipients. The risk of premature delivery following transplantation is increased. Pre-existing hypertension and diabetes confer additional risk to the pregnancy of an organ transplant recipient. Pre-gestational and gestational diabetes are associated with birth defects/congenital anomalies, hypertension, low birth weight and fetal death.
Cholestasis of pregnancy (COP) was reported in 7% of liver or liver-kidney (LK) transplant recipients, compared with approximately 1% of pregnancies in the general population. However, COP symptoms resolved postpartum and no long-term effects on the offspring were reported.
Maternal Adverse Reactions
ASTAGRAF XL may increase hyperglycemia in pregnant women with diabetes (including gestational diabetes). Monitor maternal blood glucose levels regularly [see Warnings and Precautions (5.5)].
ASTAGRAF XL may exacerbate hypertension in pregnant women and increase pre-eclampsia. Monitor and control blood pressure [see Warnings and Precautions (5.8, 5.9)].
Fetal/Neonatal Adverse Reactions
Renal dysfunction, transient neonatal hyperkalemia and low birth weight have been reported at the time of delivery in infants of mothers taking ASTAGRAF XL.
Labor or Delivery
There is an increased risk for premature delivery (< 37 weeks) following transplantation and maternal exposure to ASTAGRAF XL.
Data
Human Data
There are no adequate and well-controlled studies on the effects of tacrolimus in human pregnancy. Safety data from the TPRI and postmarketing surveillance suggest infants exposed to tacrolimus in utero have an increased risk for miscarriage, pre-term delivery (< 37 weeks), low birth weight (< 2500 g), birth defects/congenital anomalies and fetal distress.TPRI reported 450 and 241 total pregnancies in kidney and liver transplant recipients exposed to tacrolimus, respectively. The TPRI pregnancy outcomes are summarized in Table 6. In the table below, the number of recipients exposed to tacrolimus concomitantly with mycophenolic acid (MPA) products during the preconception and first trimester periods is high (27% and 29% for kidney and liver transplant recipients, respectively). Because MPA products may also cause birth defects, the birth defect rate may be confounded and this should be taken into consideration when reviewing the data, particularly for birth defects. Birth defects observed include cardiac malformations, craniofacial malformations, renal/urogenital disorders, skeletal abnormalities, neurological abnormalities and multiple malformations.
Table 6: TPRI-Reported Pregnancy Outcomes in Transplant Recipients with Exposure to Tacrolimus - * Includes multiple births and terminations.
- † Birth defect rate confounded by concomitant MPA products exposure in over half of offspring with birth defects.
Kidney
Liver
Pregnancy Outcomes*
462
253
Miscarriage
24.5%
25%
Live births
331
180
Pre-term delivery (< 37 weeks)
49%
42%
Low birth weight (< 2500 g)
42%
30%
Birth defects
8%†
5%
Additional information reported by TPRI in pregnant transplant patients receiving tacrolimus included diabetes during pregnancy in 9% of kidney recipients and 13% of liver recipients and hypertension during pregnancy in 53% of kidney recipients and 16.2% of liver recipients.
Animal Data
Administration of oral tacrolimus to pregnant rabbits throughout organogenesis produced maternal toxicity and abortion at 0.32 mg/kg (0.5 times the maximum recommended clinical dose [0.2 mg/kg/day], on a mg/m2 basis). At 1 mg/kg (1.6 times the maximum recommended clinical dose), embryofetal lethality and fetal malformations (ventricular hypoplasia, interventricular septal defect, bulbous aortic arch, stenosis of ductus arteriosus, omphalocele, gallbladder agenesis, skeletal anomalies) were observed. Administration of 3.2 mg/kg oral tacrolimus (2.6 times the maximum recommended clinical dose) to pregnant rats throughout organogenesis produced maternal toxicity/lethality, embryofetal lethality and decreased fetal body weight in the offspring of C-sectioned dams; and decreased pup viability and interventricular septal defect in offspring of dams that delivered.
In a peri-/postnatal development study, oral administration of tacrolimus to pregnant rats during late gestation (after organogenesis) and throughout lactation produced maternal toxicity, effects on parturition, and reduced pup viability at 3.2 mg/kg (2.6 times the maximum recommended clinical dose); among these pups that died early, an increased incidence of kidney hydronephrosis was observed. Reduced pup weight was observed at 1.0 mg/kg (0.8 times the maximum recommended clinical dose).
Administration of oral tacrolimus to rats prior to mating, and throughout gestation and lactation produced maternal toxicity/lethality, embryofetal loss and reduced pup viability at 3.2 mg/kg (2.6 times the maximum recommended clinical dose range). Interventricular septal defects, hydronephrosis, craniofacial malformations and skeletal effects were observed in offspring that died. Effects on parturition (incomplete delivery of nonviable pups) were observed at 1 mg/kg (0.8 times the maximum recommended clinical dose) [see Nonclinical Toxicology (13.1)].
8.2 Lactation
Risk Summary
Controlled lactation studies have not been conducted in humans; however, tacrolimus has been reported to be present in human milk. The effects of tacrolimus on the breastfed infant, or on milk production, have not been assessed. Tacrolimus is excreted in rat milk and in peri-/postnatal rat studies; exposure to tacrolimus during the postnatal period was associated with developmental toxicity in the offspring at clinically relevant doses [see Pregnancy (8.1) and Nonclinical Toxicology (13.1)].The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for ASTAGRAF XL and any potential adverse effects on the breastfed child from ASTAGRAF XL or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Contraception
ASTAGRAF XL can cause fetal harm when administered to pregnant women. Advise female and male patients of reproductive potential to speak to their healthcare provider on family planning options including appropriate contraception prior to starting treatment with ASTAGRAF XL [see Use in Specific Populations (8.1) and Nonclinical Toxicology (13.1)].Infertility
Based on findings in animals, male and female fertility may be compromised by treatment with ASTAGRAF XL [see Nonclinical Toxicology (13.1)].8.4 Pediatric Use
The safety and effectiveness of ASTAGRAF XL in de novo pediatric kidney transplant patients have been established. Use of ASTAGRAF XL in pediatric kidney transplant patients is based on adequate and well-controlled studies of ASTAGRAF XL in adult kidney transplant patients [see Clinical Studies (14.1, 14.2)] and supported by pharmacokinetic and safety data of ASTAGRAF XL in pediatric transplant patients 4 years of age and older who are able to swallow capsules intact and Prograf (tacrolimus) capsules in adult and pediatric transplant patients [see Clinical Pharmacology (12.3)].
De Novo Pediatric Kidney Transplant Patients
A pharmacokinetic and safety study included 25 de novo pediatric kidney transplant patients, 4 to 15 years of age, randomized to Prograf (N=12) or ASTAGRAF XL (N=13). Tacrolimus exposures for the two drug products were comparable on Days 7 and 28 [see Clinical Pharmacology (12.3)]. Among the 13 pediatric kidney transplant patients who completed 52 weeks on ASTAGRAF XL, there were no graft loss, deaths or episodes of biopsy-proven acute rejection [see Dosage and Administration (2.2) and Adverse Reactions (6.1)].Stable Pediatric Kidney Transplant Patients
Another pharmacokinetic and safety study included 48 stable pediatric kidney transplant patients, 5 to 16 years of age, who were converted from a Prograf-based regimen to ASTAGRAF XL. Tacrolimus systemic exposures for the two drug products were comparable [see Clinical Pharmacology (12.3)]. Acute rejections were reported in 2/48 kidney pediatric patients that responded to subsequent treatment. There were no graft failures or deaths following use of ASTAGRAF XL during the 54-week follow up [see Adverse Reactions (6.1)].8.5 Geriatric Use
Clinical studies of ASTAGRAF XL did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients. In Studies 1 and 2, 29 patients were 65 years of age and older, and 3 patients were 75 years of age and over [see Clinical Studies (14)]. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment
The pharmacokinetics of tacrolimus in patients with renal impairment was similar to that in healthy subjects with normal renal function. However, due to its potential for nephrotoxicity, monitoring of renal function in patients with renal impairment is recommended; tacrolimus dosage should be reduced if indicated [see Warnings and Precautions (5.6) and Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
The mean clearance of tacrolimus was substantially lower in patients with severe hepatic impairment (mean Child-Pugh score: > 10) compared to healthy subjects with normal hepatic function [see Clinical Pharmacology (12.3)]. With greater tacrolimus whole blood trough concentrations in patients with severe hepatic impairment, there is a greater risk of adverse reactions and dosage reduction is recommended [see Dosage and Administration (2.3)]. For patients with moderate hepatic impairment, monitor tacrolimus whole blood trough concentrations. For patients with mild hepatic impairment, no dosage adjustments are needed.
8.8 Race or Ethnicity
African-American patients may need to be titrated to higher dosages to attain comparable trough concentrations compared to Caucasian patients [see Dosage and Administration (2.3), Clinical Pharmacology (12.3), and Clinical Studies (14)].
African-American and Hispanic patients are at increased risk for new onset diabetes after transplant. Monitor blood glucose concentrations and treat appropriately [see Warnings and Precautions (5.5)].
-
10 OVERDOSAGE
Postmarketing cases of overdose with tacrolimus have been reported. Overdosage adverse reactions included:
- nervous system disorders (tremor, headache, confusional state, balance disorders, encephalopathy, lethargy and somnolence)
- gastrointestinal disturbances (nausea, vomiting, and diarrhea)
- abnormal renal function (increased blood urea nitrogen and elevated serum creatinine)
- urticaria
- hypertension
- peripheral edema, and
- infections [one fatal postmarketing case of bilateral pneumopathy and CMV infection was attributed to tacrolimus (extended-release) overdose].
Based on the poor aqueous solubility and extensive erythrocyte and plasma protein binding, it is anticipated that tacrolimus is not dialyzable to any significant extent; there is no experience with charcoal hemoperfusion. The oral use of activated charcoal has been reported in treating acute overdoses, but experience has not been sufficient to warrant recommending its use. General supportive measures and treatment of specific symptoms should be followed in all cases of overdosage.
-
11 DESCRIPTION
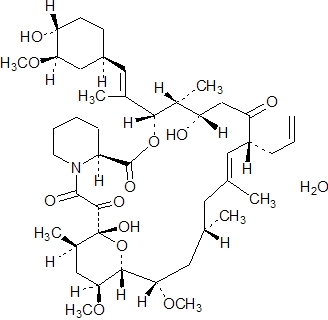
Tacrolimus is the active ingredient in ASTAGRAF XL. Tacrolimus is a calcineurin-inhibitor immunosuppressant produced by Streptomyces tsukubaensis. Chemically, tacrolimus is designated as [3S – [3R*[E(1S*, 3S*, 4S*)], 4S*, 5R*, 8S*, 9E, 12R*, 14R*, 15S*, 16R*, 18S*, 19S*, 26aR*]] – 5, 6, 8, 11, 12, 13, 14, 15, 16, 17, 18, 19, 24, 25, 26, 26a – hexadecahydro – 5, 19 – dihydroxy – 3 – [2 – (4 – hydroxy – 3 – methoxycyclo – hexyl) – 1 – methylethenyl] – 14, 16 – dimethoxy – 4, 10, 12, 18 – tetramethyl – 8 – (2 – propenyl) – 15, 19 – epoxy – 3H – pyrido[2, 1 – c][1, 4]oxaazacyclotricosine – 1, 7, 20, 21(4H, 23H) – tetrone, monohydrate.
The chemical structure of tacrolimus is:
Tacrolimus has an empirical formula of C44H69NO12H2O and a formula weight of 822.03. Tacrolimus appears as white crystals or crystalline powder. It is practically insoluble in water, freely soluble in ethanol, and very soluble in methanol and chloroform.
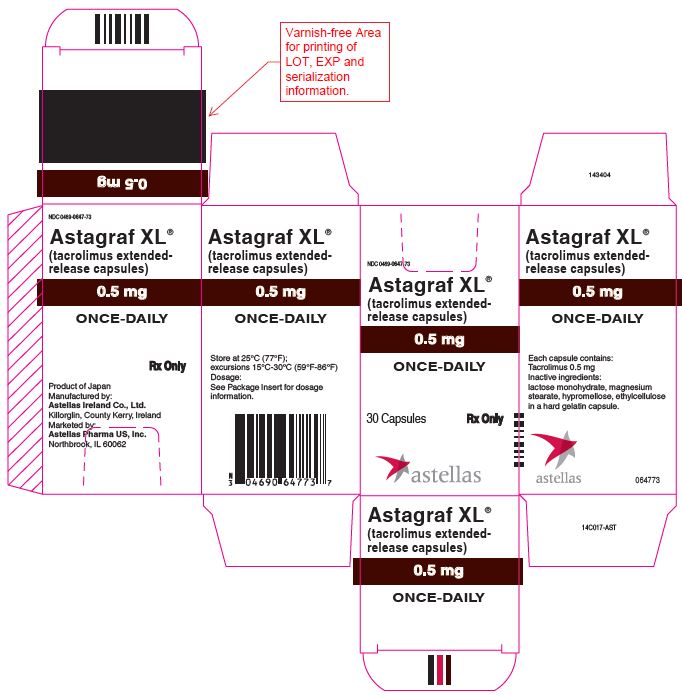
ASTAGRAF XL is available for oral administration as hard gelatin capsules (tacrolimus extended-release capsules) containing the equivalent of 0.5 mg, 1 mg or 5 mg of anhydrous tacrolimus, USP. Inactive ingredients include ethylcellulose NF, hypromellose USP, magnesium stearate NF and lactose monohydrate NF. The ingredients are directly proportional across all capsule strengths. The capsule shell contains gelatin NF, titanium dioxide USP, ferric oxide NF, and sodium lauryl sulfate.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Tacrolimus binds to an intracellular protein, FKBP-12. A complex of tacrolimus-FKBP-12, calcium, calmodulin, and calcineurin (a ubiquitous mammalian intracellular enzyme) is then formed and the phosphatase activity of calcineurin is inhibited. Such inhibition prevents the dephosphorylation and translocation of various factors such as the nuclear factor of activated T-cells (NF-AT), and nuclear factor kappa-light-chain-enhancer of activated B-cells (NF-κB).
Tacrolimus inhibits the expression and/or production of several cytokines that include interleukin (IL)-1 beta, IL‑2, IL-3, IL-4, IL-5, IL-6, IL-8, IL-10, gamma interferon, tumor necrosis factor-alpha, and granulocyte macrophage colony-stimulating factor. Tacrolimus also inhibits IL-2 receptor expression and nitric oxide release, induces apoptosis and production of transforming growth factor-beta that can lead to immunosuppressive activity. The net result is the inhibition of T-lymphocyte activation and proliferation as well as T-helper-cell-dependent B-cell response (i.e., immunosuppression).
12.3 Pharmacokinetics
Table 7 summarizes the pharmacokinetic (PK) parameters of tacrolimus following oral administration of ASTAGRAF XL in healthy subjects and in kidney transplant patients. Whole blood tacrolimus concentrations in these PK studies were measured using validated HPLC/MS/MS assays.
Table 7: Pharmacokinetic Parameters of ASTAGRAF XL (Given Once Daily) in Healthy Subjects and in Kidney Transplant Patients (Under Fasted Conditions) - * Healthy adult subjects (actual administered dose of ASTAGRAF XL); adult de novo kidney transplant patients (actual group mean dose of ASTAGRAF XL).
- † Day of ASTAGRAF XL treatment and PK profiling.
- ‡ Arithmetic means ± S.D.
- § Median [range].
- ¶ Tacrolimus trough concentration before the next dose.
- # “De novo” refers to immunosuppression starting at the time of transplantation; data from PK substudy of Study 2.
- Þ Same daily dose of ASTAGRAF XL for 14-day period.
- ß Correlation coefficient of AUC24 to Cmin r = 0.88.
Population
ASTAGRAF XL Dose*
Day†
PK Parameters of ASTAGRAF XL
Cmax‡
(ng/mL)
Tmax§
(hr)
AUC24‡
(nghr/mL)
C24¶
(ng/mL)
Healthy Subjects
(N=24)
4 mg
4 mg
Day 1
Day 10
6.2 ± 2.1
11.6 ± 3.4
2.0 [1.0-5.0]
2.0 [1.0-3.0]
74 ± 22
155 ± 46
2.3 ± 0.8
4.7 ± 1.5
Adult Kidney
De novo#
(N=17)0.20 mg/kg
0.19 mg/kg
0.18 mg/kg
0.18 mg/kg
Day 1
Day 3
Day 7
Day 14
26.0 ± 13.7
31.0 ± 13.9
32.2 ± 10.2
32.7 ± 9.0
3.0 [2-24]
2.0 [0.5-2.0]
2.0 [1-6]
2.0 [1-4]
372 ± 202
437 ± 175
405 ± 117
412 ± 109
12.1 ± 7.2
13.5 ± 5.6
11.4 ± 4.0
11.2 ± 3.9
Adult Kidney
(6 months or greater post-transplant)
(N=60)5.2 mg/dayÞ
Day 14Þ
16.1 ± 5.3
2.0 [1.0 - 6.0]
222 ± 64
6.7 ± 1.9ß
In de novo adult kidney transplant patients, the tacrolimus systemic exposure, as assessed by AUC24, for ASTAGRAF XL 0.2 mg/kg once daily on Day 1 post-transplant was 18% (Ratio [SD]: 0.822 [1.647]) lower when compared with Prograf (tacrolimus immediate-release) 0.2 mg/kg/day given twice daily. By Day 3 post-transplant, the AUC24 was similar between the two formulations. On Day 14 (steady state), the AUC24 for ASTAGRAF XL was 21% (Ratio [SD]: 1.207 [1.326]) higher than that of Prograf (tacrolimus immediate-release), at comparable trough concentrations (C24).
Due to intersubject variability in tacrolimus PK, individualization of dosing regimen is necessary for optimal therapy [see Dosage and Administration (2.3, 2.4)].
Pharmacokinetic data indicate that whole blood concentrations rather than plasma concentrations serve as the more appropriate sampling compartment to describe tacrolimus PK.
Absorption
In healthy subjects, the administration of escalating ASTAGRAF XL doses ranging from 1.5 mg to 10 mg resulted in dose-proportional increases in tacrolimus AUC and C24h, and no change in elimination half-life.Food Effects
The presence of a meal affects the absorption of tacrolimus; the rate and extent of absorption is greatest under fasted conditions. In 24 healthy subjects, administration of ASTAGRAF XL immediately following a high-fat meal (150 protein calories, 250 carbohydrate calories, and 500 to 600 fat calories) reduced the Cmax, AUCt, and AUCinf of tacrolimus by approximately 25% compared with fasting values. Food delayed the median Tmax from 2 hours in the fasted state to 4 hours in the fed state; however, the terminal half-life remained 36 hours regardless of dosing conditions. The time when a meal is consumed also affected tacrolimus bioavailability. In 24 healthy subjects, when ASTAGRAF XL was administered 1.5 hours after consumption of a high-fat breakfast, tacrolimus exposure was decreased approximately 35%. Administration of ASTAGRAF XL 1 hour prior to a high-fat breakfast reduced tacrolimus exposure by 10%. ASTAGRAF XL capsules should be taken, preferably on an empty stomach, at least 1 hour before a meal or at least 2 hours after a meal.Chronopharmacokinetic Effect
In 23 healthy subjects, a diurnal effect on the absorption of tacrolimus was observed. Evening dosing of ASTAGRAF XL reduced AUCinf by 35% relative to morning dosing. ASTAGRAF XL capsules should be taken consistently at the same time every morning.
Distribution
The plasma protein binding of tacrolimus is approximately 99% and is independent of concentration over a range of 5-50 ng/mL. Tacrolimus is bound mainly to albumin and alpha-1-acid glycoprotein, and has a high level of association with erythrocytes. The distribution of tacrolimus between whole blood and plasma depends on several factors, such as hematocrit, temperature at the time of plasma separation, drug concentration, and plasma protein concentration. In a U.S. trial in which tacrolimus was administered as tacrolimus immediate-release, the ratio of whole blood concentration to plasma concentration averaged 35 (range 12 to 67).Elimination
Metabolism
The desired pharmacological activity of tacrolimus is primarily due to the parent drug. Tacrolimus is extensively metabolized by the mixed-function oxidase system, primarily the cytochrome P-450 system (CYP3A). A metabolic pathway leading to the formation of 8 possible metabolites has been proposed. Demethylation and hydroxylation were identified as the primary mechanisms of biotransformation in vitro. The major metabolite identified in incubations with human liver microsomes is 13-demethyl tacrolimus. In in vitro studies, a 31-demethyl metabolite has been reported to have the same activity as tacrolimus.Excretion
In a mass balance study of orally-administered radiolabeled tacrolimus to 6 healthy subjects, the mean recovery of the radiolabel was 94.9 ± 30.7%. Fecal elimination accounted for 92.6 ± 30.7% and urinary elimination accounted for 2.3 ± 1.1% of the total radiolabel administered. The elimination half-life based on radioactivity was 31.9 ± 10.5 hours, whereas it was 48.4 ± 12.3 hours based on tacrolimus concentrations. The mean clearance of radiolabel was 0.226 ± 0.116 L/hr/kg and the mean clearance of tacrolimus was 0.172 ± 0.088 L/hr/kg.The elimination half-life of tacrolimus after oral administration of 4 mg ASTAGRAF XL daily for 10 days was 38 ± 3 hours in 24 healthy subjects.
Specific Populations
Pediatric Patients
De Novo Pediatric Transplant Patients
A PK study to compare ASTAGRAF XL to Prograf capsules was conducted in 44 de novo pediatric transplant patients, including 25 pediatric de novo kidney transplant patients, 4 to 15 years of age (mean age of 10.6 years). These patients were administered a starting daily dose of 0.3 mg/kg/day of Prograf capsules divided into two daily doses or ASTAGRAF XL once daily. Overall, the tacrolimus PK parameters AUC24 and C24 are comparable among Prograf and ASTAGRAF XL on Days 7 and 28 (Table 8).Table 8: Tacrolimus Pharmacokinetic Parameters Following Daily Doses of Prograf Capsules or ASTAGRAF XL in Pediatric De Novo Kidney Transplant Patients 4 to 15 Years of Age - * Study Visit Day on which PK profiles were collected following administration of Prograf capsules or ASTAGRAF XL.
- † PK estimates following the morning Prograf capsules dose are reported for Tmax and Cmax.
- ‡ Observed whole blood tacrolimus trough levels at 12 hours following the evening dose of Prograf capsules or 24 hours after the morning dose of ASTAGRAF XL.
- § Tmax - Reported as median (range).
Study Visit*Mean ± SD (Range) PK Parameters for Prograf Capsules and ASTAGRAF XL
PK Parameters
Prograf Capsules†
(N=10)ASTAGRAF XL
(N=10)Day 1
AUC24 (ng∙hr/mL)
280.4 ± 164.4
(145.0 – 688.4)
211.4 ± 128.2
(76.9 – 459.8)
Cmax (ng/mL)
23.1 ± 14.4
(8.2 – 55.7)
17.7 ± 11.1
(5.0 – 44.9)
C24 (ng/mL)‡
8.5 ± 5.4
(3.2 – 16.7)
6.7 ± 4.3
(2.0 – 16.5)
Tmax (hr)§
2.0
(0.9 – 4.0)
2.0
(1.0 – 12.0)
Day 7
AUC24 (ng∙hr/mL)
347.2 ± 124.2
(153.7 – 561.8)
350.6 ± 92.7
(149.0 – 493.0)
Cmax (ng/mL)
28.7 ± 14.6
(10.5 – 49.0)
37.7 ± 13.9
(15.1 – 62.6)
C24 (ng/mL)‡
9.6 ±2.8
(5.9 – 16.0)
8.4 ± 2.7
(4.3 – 14.4)
Tmax (hr)§
1.0
(1.0 – 2.3)
1.0
(1.0 – 2.0)
Day 28
AUC24 (ng∙hr/mL)
323.6 ± 114.5
(234.5 – 614.0)
322.4 ± 78.1
(240.3 – 516.4)
Cmax (ng/mL)
28.5 ± 17.1
(17.5 – 70.1)
24.7 ± 4.8
(14.2 – 32.5)
C24 (ng/mL)‡
9.8 ± 3.1
(5.4 – 16.0)
9.2 ± 3.0
(5.1 – 15.9)
Tmax (hr)§
1.0
(1.0 – 4.0)
1.5
(1.0 – 4.0)
Stable Pediatric Transplant Patients
Another PK study to compare ASTAGRAF XL to Prograf capsules was conducted in 81 stable pediatric transplant patients, including 48 pediatric kidney transplant patients, 5 to 16 years of age (mean age of 11.0 years). Pediatric kidney transplant patients who had been administered Prograf for at least 3 months prior to treatment were converted on a 1:1 (mg:mg) basis from Prograf, given in two divided doses, to ASTAGRAF XL once-daily. Overall, the tacrolimus AUC24, Cmax, and C24 are comparable upon conversion from Prograf to ASTAGRAF XL on a 1:1 (mg:mg) basis in stable pediatric kidney transplant patients (Table 9).Table 9: Tacrolimus Pharmacokinetic Parameters at Steady State Following 1:1 (mg:mg) Total Daily Dose Conversion from Prograf Capsules to ASTAGRAF XL in Stable Pediatric Kidney Transplant Patients 5 to 16 Years of Age - * Observed whole blood tacrolimus trough levels at 12 hours following the evening dose of Prograf capsules and at 24 hours after the morning dose of ASTAGRAF XL once daily under steady-state conditions.
Organ Transplant
Population
Mean ± SD (Range) PK Parameters for Prograf Capsules
and ASTAGRAF XLPediatric Kidney
(N=45)PK Parameters
Prograf Capsules
ASTAGRAF XL
AUC24 (ng∙hr/mL)
188.8 ± 53.5
(102.3 – 406.8)
173.2 ± 44.6
(80.9 – 262.5)
Cmax (ng/mL)
14.9 ± 5.8
(4.9 – 34.4)
12.5 ± 4.5
(5.4 – 24.4)
C24*(ng/mL)
5.6 ± 1.9
(2.9 – 13.8)
5.1 ± 1.4
(2.0 – 8.4)
Patients with Renal Impairment
Tacrolimus pharmacokinetics following a single administration of tacrolimus immediate-release injection (administered as a continuous IV infusion) were determined in 12 patients (7 not on dialysis and 5 on dialysis, serum creatinine of 3.9 ± 1.6 and 12.0 ± 2.4 mg/dL, respectively) prior to their kidney transplant. The mean clearance of tacrolimus in patients with renal dysfunction given tacrolimus IV was similar to that in healthy subjects given tacrolimus IV and in healthy subjects given oral tacrolimus immediate-release [see Use in Specific Populations (8.6)].Patients with Hepatic Impairment
Tacrolimus pharmacokinetics have been determined in six patients with mild hepatic impairment (mean Child-Pugh score: 6.2) following single oral administration of tacrolimus immediate-release. The mean clearance of tacrolimus in patients with mild hepatic impairment was not substantially different from that in healthy subjects. Tacrolimus pharmacokinetics were studied in six patients with severe hepatic impairment (mean Child-Pugh score: > 10). The mean clearance was substantially lower in patients with severe hepatic impairment [see Dosage and Administration (2.3) and Use in Specific Populations (8.7)].Racial or Ethnic Groups
The pharmacokinetics of tacrolimus was studied following single oral administration of tacrolimus immediate-release (5 mg) in 10 African-American, 12 Latino-American, and 12 Caucasian healthy subjects [see Dosage and Administration (2.2), Use in Specific Populations (8.8) and Clinical Studies (14)]:- The mean (± SD) tacrolimus Cmax in African-Americans (23.6 ± 12.1 ng/mL) was lower than in Caucasians (40.2 ± 12.6 ng/mL) and Latino-Americans (36.2 ± 15.8 ng/mL).
- Mean AUC0-inf tended to be lower in African-Americans (203 ± 115 ng∙hr/mL) than Caucasians (344 ± 186 ng∙hr/mL) and Latino-Americans (274 ± 150 ng∙hr/mL).
- The mean (± SD) absolute oral bioavailability (F) in African-Americans (12 ± 4.5%) and Latino-Americans (14 ± 7.4%) was lower than in Caucasians (19 ± 5.8%).
- There was no significant difference in mean terminal half-life among the three ethnic groups (range from approximately 25 to 30 hours).
Male and Female Patients
A formal trial to evaluate the effect of gender on tacrolimus pharmacokinetics has not been conducted; however, there was no difference in total mg daily dosages between male and female patients receiving ASTAGRAF XL in the kidney transplant trials. A retrospective comparison of pharmacokinetics in healthy subjects, and in kidney transplant patients indicated no gender-based differences.Drug Interaction Studies
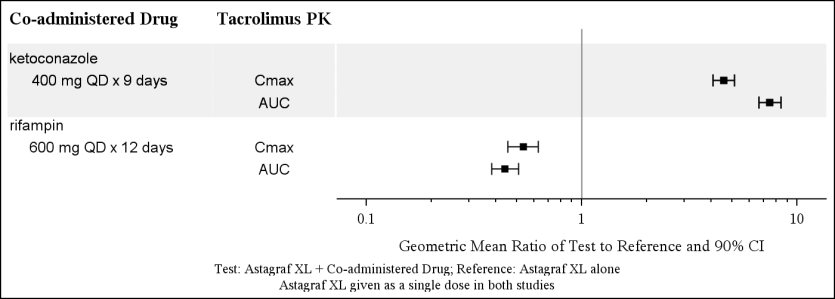
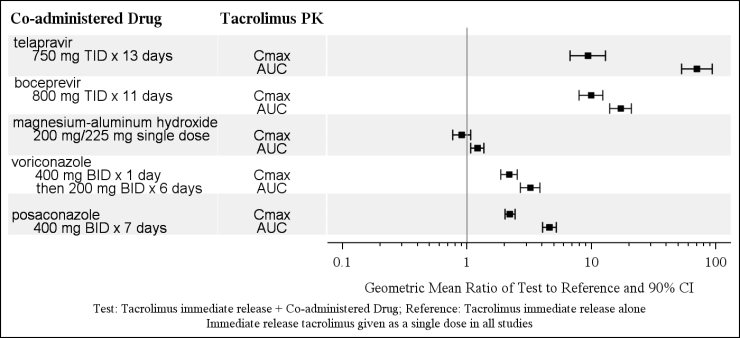
Because tacrolimus is metabolized mainly by CYP3A enzymes, drugs or substances known to inhibit these enzymes and/or are known CYP3A substrates may increase tacrolimus whole blood concentrations. Drugs known to induce CYP3A enzymes may decrease tacrolimus whole blood concentrations [see Warnings and Precautions (5.10) and Drug Interactions (7.2)].Figures 1 and 2 summarize the PK data from drug interaction studies of ASTAGRAF XL or tacrolimus immediate-release capsules. These studies assessed the effect of co-administered drugs on tacrolimus PK in healthy subjects. Dosing adjustments, when using drugs that inhibit or increase CYP3A enzymes, may be necessary [see Drug Interactions (7.2)].
Figure 1: Effect of Co-administered Drugs on the Pharmacokinetics of Tacrolimus (when Given as ASTAGRAF XL)
Figure 2: Effect of Co-administered Drugs on the Pharmacokinetics of Tacrolimus (when Given as Immediate-Release Tacrolimus)
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Carcinogenicity studies were conducted in male and female rats and mice. In the 80-week mouse oral study and in the 104-week rat oral study, no relationship of tumor incidence to tacrolimus dosage was found. The highest dose used in the mouse was 3 mg/kg/day (0.49 times the AUC at the maximum clinical dose of 0.2 mg/kg/day) and in the rat was 5 mg/kg/day (0.14 times the AUC at the maximum clinical dose of 0.2 mg/kg/day) [see Boxed Warning and Warnings and Precautions (5.1)].A 104-week dermal carcinogenicity study was performed in mice with tacrolimus ointment (0.03%-3%), equivalent to tacrolimus doses of 1.1-118 mg/kg/day or 3.3-354 mg/m2/day. In the study, the incidence of skin tumors was minimal and the topical application of tacrolimus was not associated with skin tumor formation under ambient room lighting. However, a statistically significant elevation in the incidence of pleomorphic lymphoma in high-dose male (25/50) and female animals (27/50), and in the incidence of undifferentiated lymphoma in high-dose female animals (13/50), was noted in the mouse dermal carcinogenicity study. Lymphomas were noted in the mouse dermal carcinogenicity study at a daily dose of 3.5 mg/kg (0.1% tacrolimus ointment; 2.4-fold the human exposure in stable adult kidney transplant patients > 6 months post-transplant). No drug-related tumors were noted in the mouse dermal carcinogenicity study at a daily dose of 1.1 mg/kg (0.03% tacrolimus ointment). The relevance of topical administration of tacrolimus in the setting of systemic tacrolimus use is unknown.
The implications of these carcinogenicity studies are limited; doses of tacrolimus were administered that likely induced immunosuppression in these animals, impairing their immune system’s ability to inhibit unrelated carcinogenesis.
Mutagenesis
No evidence of genotoxicity was seen in bacterial (Salmonella and E. coli) or mammalian (Chinese hamster lung-derived cells) in vitro assays of mutagenicity, the in vitro CHO/HGPRT assay of mutagenicity, or in vivo clastogenicity assays performed in mice; tacrolimus did not cause unscheduled DNA synthesis in rodent hepatocytes.Impairment of Fertility
Tacrolimus subcutaneously administered to male rats at paternally toxic doses of 2 mg/kg/day [1.6 times the maximum recommended clinical dose (0.2 mg/kg/day) on a mg/m2 basis] or 3 mg/kg/day (2.4 times the maximum recommended clinical dose) resulted in a dose-related decrease in sperm count.Tacrolimus administered orally at 1.0 mg/kg (0.8 times the maximum clinical dose) to male and female rats, prior to and during mating, as well as to dams during gestation and lactation, was associated with embryolethality and adverse effects on female reproduction. Effects on female reproductive function (parturition) and embryolethal effects were indicated by a higher rate of pre- and post-implantation loss and increased numbers of undelivered and nonviable pups. When administered at 3.2 mg/kg (2.6 times the maximum clinical dose range based on body surface area), tacrolimus was associated with maternal and paternal toxicity as well as reproductive toxicity including marked adverse effects on estrus cycles, parturition, pup viability, and pup malformations.
-
14 CLINICAL STUDIES
14.1 ASTAGRAF XL with Basiliximab Induction
Study 1 was a 12-month, randomized, open-label trial of ASTAGRAF XL (N=214) compared to active-control of tacrolimus (Prograf) immediate-release (N=212), conducted primarily in the U.S. in patients who were a recipient of a primary or retransplanted non-HLA-identical living or deceased donor kidney transplant. All patients received basiliximab induction and concomitant mycophenolate mofetil (MMF) and corticosteroids. The study population was 17 to 77 years of age, the mean age was 48 years; 64% were male and 36% were female; 73% were Caucasian, 22% were African-American, 2% were Asian, and 3% were categorized as other races. Living donors provided 49% of the organs and 51% of patients received a kidney transplant from a deceased donor with a mean cold ischemia time of 19 hours. The most frequent diseases leading to transplantation were balanced between the groups and included nephrosclerosis/hypertensive nephropathy, diabetic nephropathy, glomerulonephritis, and polycystic kidney disease. In the study, 97% of patients had no previous transplant and 3% had a previous transplant.
Study Medications
ASTAGRAF XL or Control [Prograf (tacrolimus) capsules]
The initial dose of ASTAGRAF XL was administered prior to reperfusion or within 48 hours after completion of the transplant procedure. The protocol-defined initial post-operative daily doses were 0.15 to 0.20 mg per kg given as a single dose in the morning for ASTAGRAF XL and 0.075 to 0.10 mg per kg twice daily for control. The ASTAGRAF XL and control dosage was then adjusted on the basis of safety and efficacy and a target whole blood tacrolimus trough concentration range of 7 to 16 ng/mL for the first 90 days post-transplant and 5 to 15 ng/mL thereafter.The average recorded starting tacrolimus daily dose, given any time up to day 2 post-transplant, was higher for ASTAGRAF XL than for control (0.14 mg per kg per day versus 0.10 mg per kg per day). Thereafter, to achieve comparable mean tacrolimus trough concentrations, on average 15% higher total mean daily doses of tacrolimus were required for ASTAGRAF XL than for control.
Tacrolimus whole blood trough concentrations were monitored on Days 3, 7, 10, 14, and 21, then Months 1, 2, 4, 6, 8, 10, and 12. Table 10 shows the tacrolimus whole blood trough concentrations measured at protocol-specified time points for ASTAGRAF XL. Approximately 80% of ASTAGRAF XL-treated patients maintained tacrolimus whole trough blood concentrations between 5 to 17 ng/mL during months 1 through 2 and between 4 to 12 ng/mL from months 3 through 12.
Table 10: Observed Tacrolimus Whole Blood Trough Concentrations in ASTAGRAF XL-Treated Kidney Transplant Patients in Study 1 - * Immunoassay was used in most laboratories.
Scheduled Visit
Tacrolimus Whole Blood Trough Concentrations (ng/mL)*
[Median (10th to 90th Percentile)]
Day 3
9.6 (4.9 to 20.2)
Day 7
9.1 (4.4 to 16.8)
Day 14
10.0 (5.7 to 16.9)
Month 1
10.5 (5.6 to 17.1)
Month 2
9.4 (6.1 to 14.2)
Month 6
7.7 (4.4 to 11.5)
Month 12
7.2 (3.8 to 10.4)
African-American patients required higher ASTAGRAF XL dosages to attain similar trough concentrations as Caucasian patients (see Table 11).
Table 11: ASTAGRAF XL Dosages and Mean Whole Blood Trough Concentrations in African-American and Caucasian Kidney Transplant Patients in Study 1 Time After Transplant
Caucasian Patients
N=160
African-American Patients
N=41
Dose
(mg/kg)
Mean Trough
Concentration
(ng/mL)
Dose
(mg/kg)
Mean Trough
Concentration
(ng/mL)
Day 7
0.14
10.65
0.14
7.78
Month 1
0.14
11.11
0.17
10.92
Month 6
0.10
7.95
0.13
8.42
Month 12
0.09
7.53
0.12
7.33
MMF
The initial dose of MMF was 1 gram administered orally or intravenously prior to or within 48 hours of completion of the transplant procedure. Subsequent MMF was administered orally 1 gram twice daily or up to 1.5 grams twice daily in African-American patients. Dose-equivalent three times daily or four times daily dosing was permitted if MMF tolerability was a concern.The MMF dosages administered by time period in ASTAGRAF XL-treated patients are shown in Table 12. The MMF dosage was reduced to less than 2 grams per day by month 12 in 56% of ASTAGRAF XL-treated patients. Approximately 57% of the MMF dose reductions were because of adverse reactions in the ASTAGRAF XL group [see Adverse Reactions (6.1)].
Table 12: Proportion of Patients Who Received 2 grams (or less than or more than 2 grams) of MMF by Time Period in ASTAGRAF XL-Treated Patients in Study 1 - * Time-averaged MMF dosage is the total MMF dosage per day divided by the duration of treatment. A time-averaged MMF dosage of 2 grams per day means that the MMF dosage was not reduced in those patients during the time period.
Time period
(Days)
Patients on MMF
Time-averaged MMF dosage*
N
Less than
2 grams per day
2 grams per
day
Greater than
2 grams per day
1-30
211
30%
64%
6%
31-90
208
38%
57%
5%
91-180
205
49%
48%
3%
181-365
201
51%
47%
3%
Basiliximab Induction
All patients were administered 2 doses of basiliximab induction therapy (20 mg intravenously) with the first dose on day 0 before skin closure and the second dose between days 3 and 5.Steroids
All patients were administered an intravenous bolus of 500 to 1000 mg of methylprednisolone (or an equivalent steroid dose) on day 0 followed by oral administration of 200 mg methylprednisolone (or an equivalent dose of steroid) on day 1 and subsequent tapering to achieve a targeted mean prednisone dose of 5 to 10 mg/day after the first 3 months.Efficacy Results
The efficacy failure rate, defined as the percentage of patients with biopsy-proven acute rejection (BPAR), graft failure, death, and/or lost to follow at 12 months, is shown in Table 13 for the intent-to-treat population, as well as the rates of the individual events.Table 13: Incidence of BPAR, Graft Loss, Death or Lost to Follow-up at 12 Months in Kidney Transplant Patients in Study 1 - * 95% confidence interval calculated using normal approximation.
ASTAGRAF XL + MMF,
steroids, basiliximab induction
(N=214)Prograf + MMF,
steroids, basiliximab
induction
(N=212)Efficacy Failure
30 (14.0%)
32 (15.1%)
Treatment Difference (95% CI*)
-1.1% (-7.8%, +5.6%)
Efficacy Failure Endpoints
Biopsy-Proven Acute Rejection
22 (10.3%)
16 (7.5%)
Graft Loss
5 (2.3%)
9 (4.2%)
Death
3 (1.4%)
9 (4.2%)
Lost to follow-up
3 (1.4%)
4 (1.9%)
Glomerular Filtration Rate
The estimated mean glomerular filtration rates, using the Modification of Diet in Renal Disease (MDRD) formula, by treatment group at Month 12 in the intent-to-treat population is shown in Table 14.Table 14: Estimated Glomerular Filtration Rate (mL/min/1.73m2) by MDRD Formula at 12 Months Post-Transplant in Study 1 - * Last observation carried forward (LOCF); patients who died, lost the graft, or were lost to follow-up are imputed as zeroes.
- † Results from analysis of covariance model with Month 1 baseline as a covariate.
ASTAGRAF XL + MMF,
steroids, basiliximab
induction
(N=201)
Prograf + MMF,
steroids, basiliximabinduction
(N=202)
Month 1 Baseline Mean (SD)
Month 12 LOCF*
Mean (Standard deviation)
Mean Difference XL minus
Prograf (tacrolimus
immediate-release)†
56 (20)
58 (21)
+2.3 (-1.2, +5.8)
56 (21)
56 (23)
14.2 Clinical Study of ASTAGRAF XL without Induction
Study 2 was a 12-month, randomized, double-blind trial of ASTAGRAF XL (N=331) compared to active control of tacrolimus (Prograf) immediate-release (N=336), in non-U.S. patients who received a primary or retransplanted non-HLA-identical living or deceased donor kidney transplant. This trial was designed to remain double-blind until the last patient enrolled had completed 24 weeks on study treatment. Patients with a high immunologic risk defined as a panel reactive antibody (PRA) grade > 50% in the previous 6 months and/or with a previous graft survival of less than 12 months due to immunologic reasons were excluded, as were patients of donor kidneys with cold ischemia time > 30 hours, or donor kidneys from a non heart-beating donor. The patient treatment assignments remained blinded for 12 months for 96% of the patients participating in the trial.
All patients received concomitant MMF and corticosteroids without induction. The population was 18 to 65 years of age; the mean age was 48 years; 63% of the study population was male; 82% were Caucasian, 5% were African-American, 2% were Asian, and 11% were categorized as other races. Living donors provided 27% of the organs and 73% of patients received a kidney transplant from a deceased donor with a mean cold ischemia time of 17 hours. The most frequent diseases leading to transplantation were balanced between the groups and included nephrosclerosis/hypertensive nephropathy, diabetic nephropathy, glomerulonephritis, and polycystic kidney disease.
Study Medication
ASTAGRAF XL or Control [Prograf (tacrolimus) capsules]
The protocol-specified initial preoperative dose for both ASTAGRAF XL and control was 0.1 mg per kg given orally in one dose within 12 hours prior to reperfusion, given at any time of the day. The initial post-operative tacrolimus daily dose (0.2 mg per kg per day) was given orally in one dose, preferably in the morning for ASTAGRAF XL, and was given as 0.1 mg/kg twice daily for control. Subsequent doses of ASTAGRAF XL and control were adjusted on the basis of clinical evidence of efficacy, occurrence of adverse events and according to whole blood tacrolimus trough concentration target ranges of 10 to 15 ng/mL for the first 28 days post-transplant, 5 to 15 ng/mL from Day 29 to Day 168, 5 to 10 ng/mL thereafter.The actual tacrolimus doses on day 0 (0.1 mg per kg per day preoperative) and day 1 (0.2 mg per kg per day post-operative) were comparable between ASTAGRAF XL and control. Thereafter, to achieve comparable mean tacrolimus trough concentrations, on average, 25% higher total mean daily doses of tacrolimus were required for ASTAGRAF XL than for control.
Tacrolimus whole blood trough concentrations were monitored on Days 1, 3, 7, 14, then Months 1, 2, 3, 6, 11, 12, and then every 3 months.
Table 15 shows the tacrolimus whole blood trough concentrations measured at protocol-specified time points for ASTAGRAF XL. Approximately 80% of ASTAGRAF XL-treated patients maintained tacrolimus whole trough blood concentrations between 6 to 20 ng/mL during months 1 through 2, and between 6 to 14 ng/mL from months 3 through 12.
Table 15: Observed Tacrolimus Whole Blood Trough Concentrations for ASTAGRAF XL Kidney Transplant Patients Evaluated in Study 2 - * Immunoassay was used in most laboratories.
Scheduled Visit
Tacrolimus Whole Blood Trough Concentrations (ng/mL)*
[Median (10th to 90th Percentile)]
Day 3
13.8 (6.5 to 25.5)
Day 7
10.1 (5.5 to 17.3)
Day 14
10.8 (6.7 to 17.9)
Month 1
12.0 (7.5 to 17.6)
Month 2
11.1 (6.6 to 17.3)
Month 6
9.2 (5.7 to 13.5)
Month 12
8.0 (5.1 to 13.8)
MMF
The initial dose of MMF was 1 gram orally twice daily starting preoperatively and given for the first 14 days of the study. Thereafter the MMF dose was reduced to 0.5 grams twice daily to be maintained throughout the study.The MMF dosages administered by time period in ASTAGRAF XL-treated patients are shown in Table 16. The MMF dosage was reduced to 0.5 grams twice daily starting after day 14 in the majority of patients.
Table 16: Distribution (%) of ASTAGRAF XL-Treated Patients by Average Daily Dosage of MMF Received by Time Period in Study 2 - * Time-averaged MMF dosage is the total MMF dosage per day divided by the duration of treatment. A time-averaged MMF dosage of 2 grams per day means that the MMF dosage was not reduced in those patients during the time period.
- † One patient had a time-averaged dose during the first and last period of > 2 gm/day.
Time period
(Days)
Patients on
MMF
N
Less than 1 gram
per day
1 gram to less than
2 grams per day2 grams per
day
1-30
331
1%
78%
21%
31-90
303
8%
87%
6%
91-180
281
12%
85%
3%
181-365
258
15%
83%
2%
Steroids
An intravenous (IV) bolus of up to 1000 mg methylprednisolone (or equivalent) was administered perioperatively (Day 0) with a second IV bolus of 125 mg being administered 1 day after reperfusion (Day 1). On Day 2, oral prednisone was started at 20 mg per day. Thereafter, the dose of oral prednisone (or equivalent) was tapered to a dose of 0 to 5 mg/day.No Antibody Induction
Antibody induction therapy was not allowed.Efficacy Results
The efficacy failure rate, defined as the percentage of patients with biopsy-proven acute rejection (BPAR), graft failure, death, and/or lost to follow at 12 months, is shown in Table 17 for the intent-to-treat population, as well as the rates of the individual events. About 1% of randomized patients were not transplanted and were not included in the ITT analysis.Table 17: Incidence of BPAR, Graft Loss, Death or Lost to Follow-up at 12 Months in Kidney Transplant Patients in Study 2 - * 95% confidence interval calculated using normal approximation.
ASTAGRAF XL + MMF
and steroids(N=331)
Prograf + MMF
and steroids(N=336)
Efficacy Failure
93 (28.1%)
78 (23.2%)
Treatment Difference (95% CI*)
+4.9% (-1.7%, +11.5%)
Efficacy Failure Endpoints
Biopsy-Proven Acute Rejection
68 (20.5%)
54 (16.1%)
Graft loss
28 (8.5%)
24 (7.1%)
Death
10 (3%)
8 (2.4%)
Lost to follow-up
4 (1.2%)
7 (2.1%)
Glomerular Filtration Rate
The estimated mean glomerular filtration rates, using the Modification of Diet in Renal Disease (MDRD) formula, by treatment group at Month 12 in the intent-to-treat population in Study 2 is shown in Table 18.Table 18: Estimated Glomerular Filtration Rate (mL/min/1.73m2) by MDRD Formula at 12 Months Post-Kidney Transplant in Study 2 - * Last observation carried forward (LOCF); patients who died, lost the graft or were lost to follow-up are imputed as zeroes.
- † Results from analysis of covariance model with Month 1 baseline as a covariate.
ASTAGRAF XL + MMF
and steroids
(N=287)
Prograf + MMF
and steroids(N=300)
Month 1 Baseline Mean (SD)
Month 12 LOCF*
Mean (Standard deviation)
Mean Difference ASTAGRAF XL minus
Prograf (tacrolimus immediate-release)†
51 (19)
52 (20)
-1.8 (-4.6, +0.8)
52 (20)
55 (19)
-
16 HOW SUPPLIED/STORAGE AND HANDLING
ASTAGRAF XL (tacrolimus) extended-release capsules are supplied in short, square bottles (see Table 19).
Table 19: Strengths of ASTAGRAF XL 0.5 mg
Oblong capsule with a light yellow cap and orange body. Capsule is branded with red “
 647” on capsule body and “0.5 mg” on the capsule cap. The bottle packaging is branded with a brown stripe.
647” on capsule body and “0.5 mg” on the capsule cap. The bottle packaging is branded with a brown stripe.-
30-count in short, square bottles with a brown cap
(NDC: 0469-0647-73)
1 mg
Oblong capsule with a white cap and orange body. Capsule is branded with red “
 677” on capsule body and “1 mg” on the capsule cap. The bottle packaging is branded with a blue stripe.
677” on capsule body and “1 mg” on the capsule cap. The bottle packaging is branded with a blue stripe.-
30-count in short, square bottles with a blue cap
(NDC: 0469-0677-73)
5 mg
Oblong capsule with a grayish-red cap and orange body. Capsule is branded with red “
 687” on capsule body and “5 mg” on the capsule cap. The bottle packaging is branded with an orange stripe.
687” on capsule body and “5 mg” on the capsule cap. The bottle packaging is branded with an orange stripe.-
30-count in short, square bottles with an orange cap
(NDC: 0469-0687-73)
Store and Dispense
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
-
30-count in short, square bottles with a brown cap
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
17.1 Administration
Advise patients or caregivers to:
- Inspect their ASTAGRAF XL medicine when they receive a new prescription and before taking it. If the appearance of the capsule is not the same as usual, or if dosage instructions have changed, advise patients to contact their healthcare provider as soon as possible to make sure that they have the right medicine. Other tacrolimus products cannot be substituted for ASTAGRAF XL [see Warnings and Precautions (5.4)].
- Take ASTAGRAF XL at the same time every day to achieve consistent blood concentrations.
- Take ASTAGRAF XL in the morning, on an empty stomach at least 1 hour before or at least 2 hours after breakfast, to achieve maximum possible blood concentrations of the drug.
- Swallow capsule whole with liquid. Do not chew, divide or crush capsule.
- Avoid alcoholic beverages, grapefruit, and grapefruit juice while on ASTAGRAF XL [see Dosage and Administration (2.1) and Drug Interactions (7.2)].
- Take a missed dose of ASTAGRAF XL as soon as possible but not more than 14 hours after the scheduled time (i.e., for a missed 8 AM dose, take by 10 PM). Beyond the 14-hour timeframe, instruct the patient to wait until the usual scheduled time the following morning to take the next scheduled dose. Do not take 2 doses at the same time.
17.2 Development of Lymphoma and Other Malignancies
Inform patients that they are at an increased risk of developing lymphomas and other malignancies, particularly of the skin, due to immunosuppression. Advise patients to limit exposure to sunlight and ultraviolet (UV) light by wearing protective clothing and using a broad spectrum sunscreen with a high protection factor [see Boxed Warning and Warnings and Precautions (5.1)].
17.3 Increased Risk of Infection
Inform patients that they are at an increased risk of developing a variety of infections, including opportunistic infections, due to immunosuppression and to contact their physician if they develop any symptoms of infection such as fever, sweats or chills, cough or flu-like symptoms, muscle aches, or warm, red, painful areas of the skin [see Boxed Warning and Warnings and Precautions (5.2)].
17.4 New Onset Diabetes After Transplant
Inform patients that ASTAGRAF XL can cause diabetes mellitus and should be advised to contact their physician if they develop frequent urination, increased thirst or hunger [see Warnings and Precautions (5.5)].
17.5 Nephrotoxicity
Inform patients that ASTAGRAF XL can have toxic effects on the kidney that should be monitored. Advise patients to attend all visits and complete all blood tests ordered by their medical team [see Warnings and Precautions (5.6)].
17.6 Neurotoxicity
Inform patients that they are at risk of developing adverse neurologic reactions including seizure, altered mental status, and tremor. Advise patients to contact their physician should they develop vision changes, delirium, or tremors [see Warnings and Precautions (5.7)].
17.7 Hyperkalemia
Inform patients that ASTAGRAF XL can cause hyperkalemia. Monitoring of potassium levels may be necessary, especially with concomitant use of other drugs known to cause hyperkalemia [see Warnings and Precautions (5.8)].
17.8 Hypertension
Inform patients that ASTAGRAF XL can cause high blood pressure which may require treatment with anti-hypertensive therapy [see Warnings and Precautions (5.9)]. Advise patients to monitor their blood pressure.
17.9 Drug Interactions
Instruct patients to tell their healthcare providers when they start or stop taking any medicines, including prescription and nonprescription medicines, herbal and dietary supplements. Some medications could alter tacrolimus concentrations in the blood and thus may require the adjustment of the dosage of ASTAGRAF XL. Advise patients to avoid grapefruit, grapefruit juice and alcoholic beverages [see Warnings and Precautions (5.10) and Drug Interactions (7)].
17.10 Pregnancy, Lactation and Infertility
Inform women of childbearing potential that ASTAGRAF XL can harm the fetus. Instruct male and female patients to discuss with their healthcare provider family planning options including appropriate contraception. Also, discuss with pregnant patients the risks and benefits of breastfeeding their infant [see Use in Specific Populations (8.1, 8.2, 8.3)].
Encourage female transplant patients who become pregnant and male patients who have fathered a pregnancy, exposed to immunosuppressants including tacrolimus, to enroll in the voluntary Transplantation Pregnancy Registry International. To enroll or register, patients can call the toll free number 1-877-955-6877 or https://www.transplantpregnancyregistry.org/ [see Use in Specific Populations (8.1)].
Based on animal studies, ASTAGRAF XL may affect fertility in males and females [see Nonclinical Toxicology (13.1)].
17.11 Immunizations
Inform patients that ASTAGRAF XL can interfere with the usual response to immunizations and that they should avoid live vaccines [see Warnings and Precautions (5.12)].
Product of JapanManufactured by:
Astellas Ireland Co., Limited
Killorglin, County Kerry, IrelandMarketed by:
Astellas Pharma US, Inc.
Northbrook, IL 60062ASTAGRAF XL® is a registered trademark of Astellas Pharma Inc.
Prograf® is a registered trademark of Astellas Pharma Inc.222293-AST
-
MEDICATION GUIDE
MEDICATION GUIDEASTAGRAF XL® [as' tah graf ex el']
(tacrolimus)
extended-release capsules
Read this Medication Guide before you start taking ASTAGRAF XL and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment. If you have any questions about ASTAGRAF XL, ask your healthcare provider or pharmacist.
What is the most important information I should know about ASTAGRAF XL?
ASTAGRAF XL can cause serious side effects, including:
- Increased risk of cancer. People who take ASTAGRAF XL have an increased risk of getting some kinds of cancer, including skin and lymph gland cancer (lymphoma).
- Increased risk of infection. ASTAGRAF XL is a medicine that affects your immune system. ASTAGRAF XL can lower the ability of your immune system to fight infections. Serious infections can happen in people receiving ASTAGRAF XL that can cause death. Call your healthcare provider right away if you have symptoms of an infection such as:
- fever
- sweats or chills
- cough or flu-like symptoms
- muscle aches
- warm, red, or painful areas on your skin
- Increased risk of death in females who have had a liver transplant. You should not take ASTAGRAF XL if you have had a liver transplant without talking to your healthcare provider.
What is ASTAGRAF XL?
- ASTAGRAF XL is a prescription medicine used with other medicines to help prevent organ rejection in people who have had a kidney transplant.
- ASTAGRAF XL is an extended-release capsule and is not the same as tacrolimus immediate-release capsules, tacrolimus for oral suspension or tacrolimus extended-release tablets. Your healthcare provider should decide what medicine is right for you.
Who should not take ASTAGRAF XL?
- Do not take ASTAGRAF XL if you are allergic to tacrolimus or any of the ingredients in ASTAGRAF XL. See the end of this leaflet for a complete list of ingredients in ASTAGRAF XL.
What should I tell my healthcare provider before taking ASTAGRAF?
Before you take ASTAGRAF XL tell your healthcare provider if you:
- plan to receive any live vaccines. Ask your healthcare provider if you are not sure if your vaccine is a live vaccine.
- have or have had liver, kidney, or heart problems or any other medical conditions.
-
are pregnant or plan to become pregnant. ASTAGRAF XL may harm your unborn baby.
- o If you are able to become pregnant, you should use effective birth control before and during treatment with ASTAGRAF XL. Talk to your healthcare provider before starting treatment with ASTAGRAF XL about birth control methods that may be right for you.
- o Males who have female partners that are able to become pregnant should also use effective birth control before and during treatment with ASTAGRAF XL. Talk to your healthcare provider before starting treatment with ASTAGRAF XL about birth control methods that may be right for you.
- o There is a pregnancy registry for females who become pregnant and males who have fathered a pregnancy during treatment with ASTAGRAF XL. The purpose of this registry is to collect information about your health and of your baby. To enroll in this voluntary registry, call 1-877-955-6877 or go to https://www.transplantpregnancyregistry.org/
- are breastfeeding or plan to breastfeed. ASTAGRAF XL passes into your breast milk. You and your healthcare provider should decide if you will breastfeed while taking ASTAGRAF XL.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, natural, herbal or nutritional supplements. ASTAGRAF XL may affect the way other medicines work, and other medicines may affect how ASTAGRAF XL works.
How should I take ASTAGRAF XL?
- Take ASTAGRAF XL exactly as your healthcare provider tells you to take it.
- Your healthcare provider may change your dose if needed. Do not stop taking or change your dose of ASTAGRAF XL without talking to your healthcare provider.
- Take ASTAGRAF XL capsules whole. Do not break, crush, chew, or dissolve ASTAGRAF XL capsules before swallowing. If you cannot swallow ASTAGRAF XL capsules whole, tell your healthcare provider.
- Take ASTAGRAF XL at the same time each morning, preferably on an empty stomach at least 1 hour before, or at least 2 hours after, you have eaten a meal.
- If you miss your dose of ASTAGRAF XL, it should be taken as soon as possible, but no longer than 14 hours after your regularly scheduled time. If it is longer than 14 hours, the missed dose should be skipped and the next dose should be taken the following morning at your regularly scheduled time. Do not take 2 doses at the same time.
- If you take too much ASTAGRAF XL, call your healthcare provider or go to the nearest hospital emergency room right away.
What should I avoid while taking ASTAGRAF XL?
- Live vaccines such as flu vaccine through your nose, measles, mumps, rubella, polio by mouth, BCG (TB vaccine), yellow fever, chicken pox (varicella) or typhoid.
- Exposure to sunlight and UV light such as tanning machines. Wear protective clothing and use a sunscreen.
- You should not eat grapefruit or drink grapefruit juice while taking ASTAGRAF XL.
- You should not drink alcohol when taking ASTAGRAF XL.
What are the possible side effects of ASTAGRAF XL?
ASTAGRAF XL may cause serious side effects, including:
- See “What is the most important information I should know about ASTAGRAF XL?”
-
Problems from medication errors such as graft rejection and other serious reactions. People who take ASTAGRAF XL have sometimes been given the wrong medicine because some medicines have the same ingredient (tacrolimus) as ASTAGRAF XL. Serious reactions have happened including graft rejection. Check your ASTAGRAF XL when you get a new prescription to make sure you have received the right medicine.
- o Call your healthcare provider right away if you think you were given the wrong medicine.
- o Ask your healthcare provider or pharmacist if you are not sure what ASTAGRAF XL should look like.
- high blood sugar (diabetes). Your healthcare provider may do certain tests to check for diabetes while you take ASTAGRAF XL. Call your healthcare provider right away if you have:
- o frequent urination
- o increased thirst or hunger
- o blurred vision
- o confusion
- o drowsiness
- o loss of appetite
- o fruity smell on your breath
- o nausea, vomiting, or stomach pain
- kidney problems. Kidney problems are serious and common side effects of ASTAGRAF XL. Your healthcare provider may do certain tests to check your kidney function while you take ASTAGRAF XL.
- nervous system problems. Nervous system problems are a serious and common side effect of ASTAGRAF XL. Call your healthcare provider or go to the nearest hospital emergency room right away if you get any of these symptoms while taking ASTAGRAF XL. These could be signs of serious nervous system problems:
- o confusion
- o changes in alertness
- o muscle tremors
- o numbness and tingling
- o headache
- o seizures
- o vision changes
- high levels of potassium in your blood. Your healthcare provider may do certain tests to check your potassium level while you take ASTAGRAF XL.
- high blood pressure. High blood pressure is a serious and common side effect of ASTAGRAF XL. Your healthcare provider will monitor your blood pressure while you take ASTAGRAF XL and may ask you to check your blood pressure at home.
- changes in the electrical activity of your heart (QT prolongation).
- severe low blood cell count (anemia).
The most common side effects of ASTAGRAF XL are diarrhea, constipation, nausea, swelling of the hands, ankles, or legs, and tremors (shaking of the body).
These are not all the possible side effects of ASTAGRAF XL. For more information, ask your healthcare provider or pharmacist.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store ASTAGRAF XL?
- Store ASTAGRAF XL at room temperature between 68°F to 77°F (20°C to 25°C).
- Safely throw away medicine that is out of date or no longer needed.
- Keep ASTAGRAF XL and all medicines out of reach of children.
General information about the safe and effective use of ASTAGRAF XL.
- Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use ASTAGRAF XL for a condition for which it was not prescribed. Do not give ASTAGRAF XL to other people, even if they have the same symptoms that you have. It may harm them.
- This Medication Guide summarizes the most important information about ASTAGRAF XL. If you would like more information, talk to your healthcare provider. You can ask your pharmacist or healthcare provider for information about ASTAGRAF XL that is written for health professionals.
What are the ingredients in ASTAGRAF XL?
Active ingredient: tacrolimus.
Inactive ingredients:
- The capsule contains: ethylcellulose NF, hypromellose USP, magnesium stearate NF, and lactose monohydrate NF
- The capsule shell contains: gelatin NF, titanium dioxide USP, ferric oxide NF, and sodium lauryl sulfate
Manufactured by: Astellas Ireland Co., Limited, Killorglin, County Kerry, Ireland
Marketed by: Astellas Pharma US, Inc., Northbrook, IL 60062
ASTAGRAF XL® is a registered trademark of Astellas Pharma Inc.
222293-AST-MG
This Medication Guide has been approved by the U.S. Food and Drug Administration. Issued: June 2019
- PACKAGE/LABEL PRINCIPAL DISPLAY PANEL – 0.5 mg carton label
- PACKAGE/LABEL PRINCIPAL DISPLAY PANEL – 1 mg carton label
- PACKAGE/LABEL PRINCIPAL DISPLAY PANEL – 5 mg carton label
-
INGREDIENTS AND APPEARANCE
ASTAGRAF XL
tacrolimus extended-release capsules capsule, coated, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0469-0647 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TACROLIMUS (UNII: WM0HAQ4WNM) (TACROLIMUS ANHYDROUS - UNII:Y5L2157C4J) TACROLIMUS ANHYDROUS 0.5 mg Product Characteristics Color YELLOW, ORANGE Score no score Shape CAPSULE Size 11mm Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0469-0647-73 1 in 1 CARTON 07/19/2013 1 30 in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA204096 07/19/2013 ASTAGRAF XL
tacrolimus extended-release capsules capsule, coated, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0469-0677 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TACROLIMUS (UNII: WM0HAQ4WNM) (TACROLIMUS ANHYDROUS - UNII:Y5L2157C4J) TACROLIMUS ANHYDROUS 1 mg Product Characteristics Color WHITE, ORANGE Score no score Shape CAPSULE Size 14mm Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0469-0677-73 1 in 1 CARTON 07/19/2013 1 30 in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA204096 07/19/2013 ASTAGRAF XL
tacrolimus extended-release capsules capsule, coated, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0469-0687 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TACROLIMUS (UNII: WM0HAQ4WNM) (TACROLIMUS ANHYDROUS - UNII:Y5L2157C4J) TACROLIMUS ANHYDROUS 5 mg Product Characteristics Color GRAY, RED, ORANGE Score no score Shape CAPSULE Size 22mm Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0469-0687-73 1 in 1 CARTON 07/19/2013 1 30 in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA204096 07/19/2013 Labeler - Astellas Pharma US, Inc. (605764828) Establishment Name Address ID/FEI Business Operations Astellas Ireland Co., Ltd. 985098269 ANALYSIS(0469-0647, 0469-0677, 0469-0687) , MANUFACTURE(0469-0647, 0469-0677, 0469-0687) Establishment Name Address ID/FEI Business Operations Astellas Pharma Tech Co., Ltd. 691336904 ANALYSIS(0469-0647, 0469-0677, 0469-0687) , MANUFACTURE(0469-0647, 0469-0677, 0469-0687)
Trademark Results [ASTAGRAF XL]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ASTAGRAF XL 85925271 4480263 Live/Registered |
Astellas Pharma Inc. 2013-05-07 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.