TOPIRAMATE tablet, film coated
TOPIRAMATE by
Drug Labeling and Warnings
TOPIRAMATE by is a Prescription medication manufactured, distributed, or labeled by Rebel Distributors Corp. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
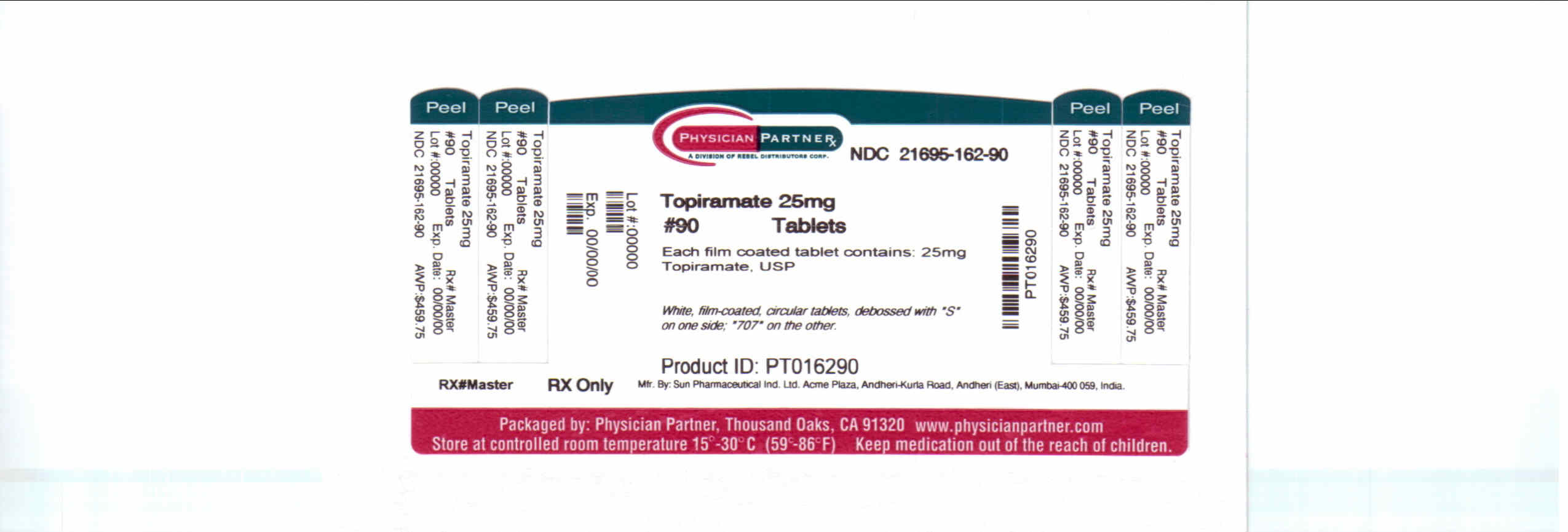
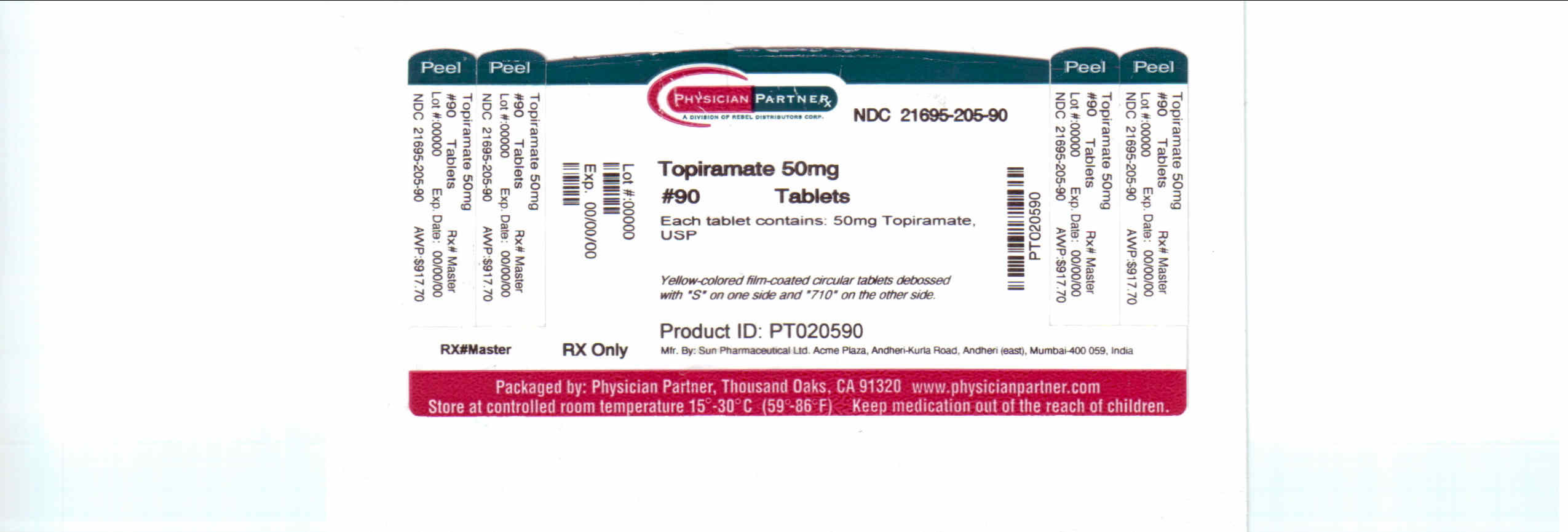
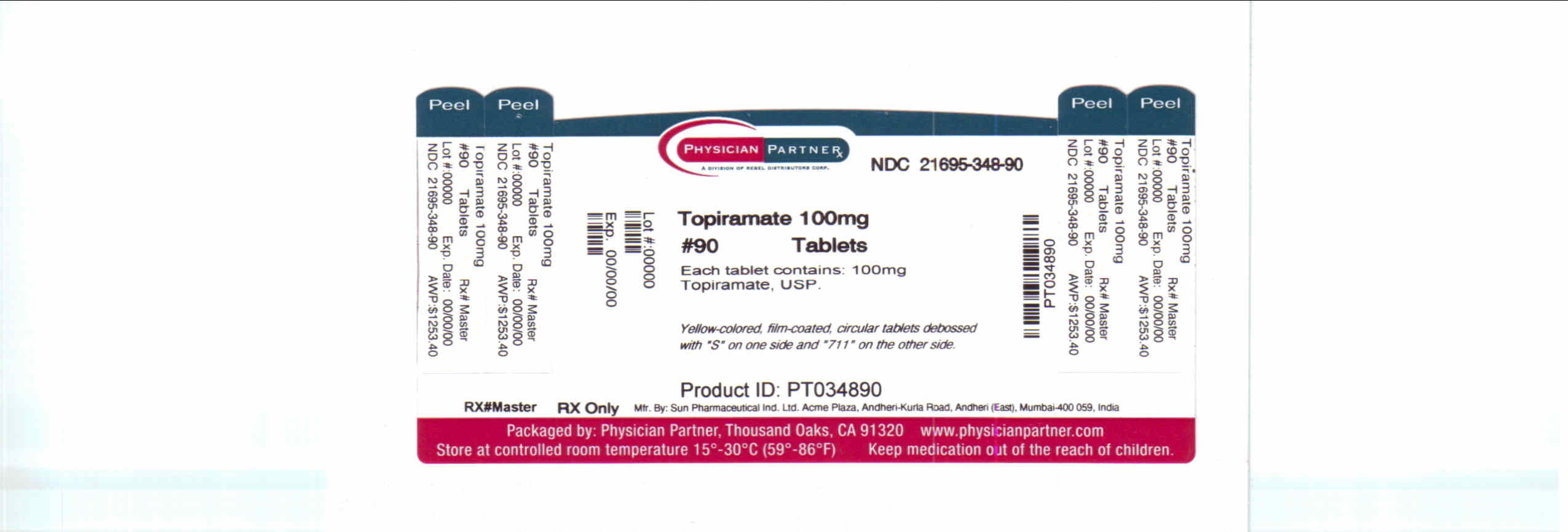
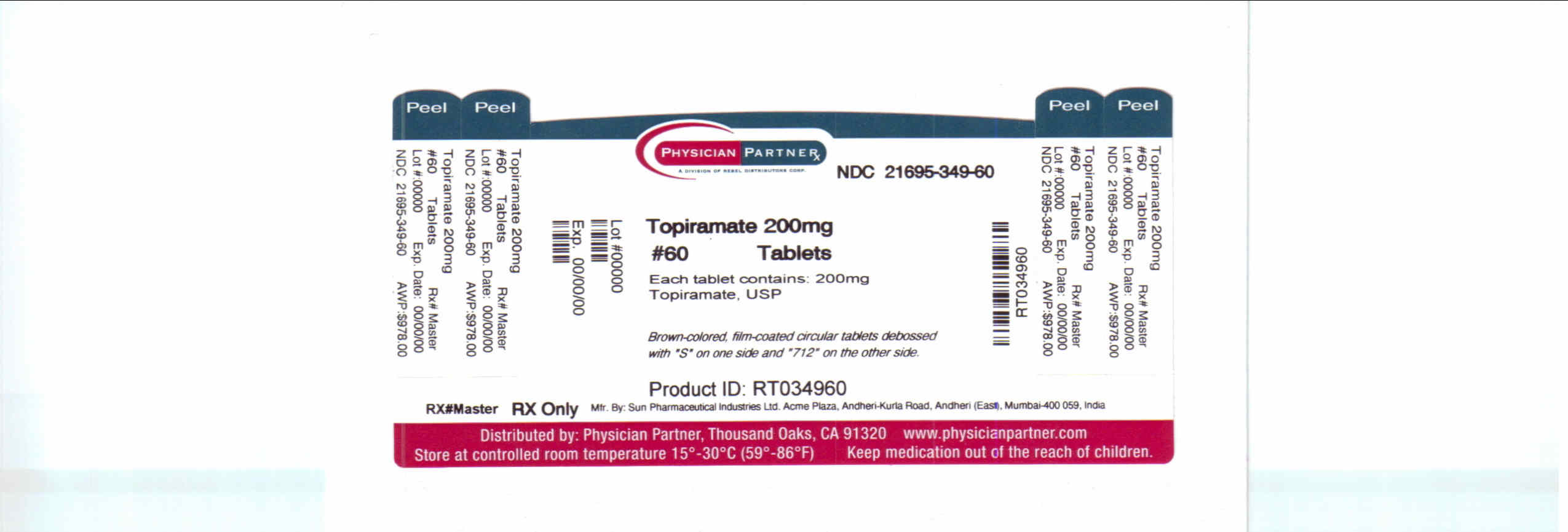
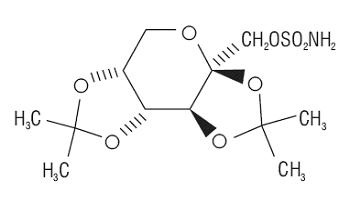
Topiramate is a sulfamate-substituted monosaccharide. Topiramate tablets are available as 25 mg, 50 mg, 100 mg, and 200 mg circular tablets for oral administration.
Topiramate is a white crystalline powder with a bitter taste. Topiramate USP is most soluble in alkaline solutions containing sodium hydroxide or sodium phosphate and having a pH of 9 to 10. It is freely soluble in acetone, chloroform, dimethylsulfoxide, and ethanol. The solubility in water is 9.8 mg/mL. Its saturated solution has a pH of 6.3. Topiramate has the molecular formula C12H21NO8S and a molecular weight of 339.37. Topiramate is designated chemically as 2,3:4,5-Di-O-isopropylidene-β-D-fructopyranose sulfamate and has the following structural formula:
Topiramate tablets contain the following inactive ingredients: anhydrous lactose, microcrystalline cellulose, pregelatinized starch, sodium starch glycolate, magnesium stearate, purified water, polyvinyl alcohol, titanium dioxide, polyethylene glycol and talc.
In addition, individual tablets contain:
50 mg tablets: iron oxide yellow
100 mg tablets: iron oxide yellow, and D&C Yellow # 10 Aluminum Lake
200 mg tablets: iron oxide red, lecithin (soya), and iron oxide black
-
CLINICAL PHARMACOLOGY
Mechanism of Action:
The precise mechanisms by which topiramate exerts its anticonvulsant effects are unknown; however, preclinical studies have revealed four properties that may contribute to topiramate's efficacy for epilepsy. Electrophysiological and biochemical evidence suggests that topiramate, at pharmacologically relevant concentrations, blocks voltage-dependent sodium channels, augments the activity of the neurotransmitter gamma-aminobutyrate at some subtypes of the GABA-A receptor, antagonizes the AMPA/kainate subtype of the glutamate receptor, and inhibits the carbonic anhydrase enzyme, particularly isozymes II and IV.
Pharmacodynamics:
Topiramate has anticonvulsant activity in rat and mouse maximal electroshock seizure (MES) tests. Topiramate is only weakly effective in blocking clonic seizures induced by the GABAA receptor antagonist, pentylenetetrazole. Topiramate is also effective in rodent models of epilepsy, which include tonic and absence-like seizures in the spontaneous epileptic rat (SER) and tonic and clonic seizures induced in rats by kindling of the amygdala or by global ischemia.
Pharmacokinetics:
The sprinkle formulation is bioequivalent to the immediate release tablet formulation and, therefore, may be substituted as a therapeutic equivalent.
Absorption of topiramate is rapid, with peak plasma concentrations occurring at approximately 2 hours following a 400 mg oral dose. The relative bioavailability of topiramate from the tablet formulation is about 80% compared to a solution. The bioavailability of topiramate is not affected by food.
The pharmacokinetics of topiramate are linear with dose proportional increases in plasma concentration over the dose range studied (200 to 800 mg/day). The mean plasma elimination half-life is 21 hours after single or multiple doses. Steady state is thus reached in about 4 days in patients with normal renal function. Topiramate is 15 to 41% bound to human plasma proteins over the blood concentration range of 0.5 to 250 mcg/mL. The fraction bound decreased as blood concentration increased.
Carbamazepine and phenytoin do not alter the binding of topiramate. Sodium valproate, at 500 mcg/mL (a concentration 5 to 10 times higher than considered therapeutic for valproate) decreased the protein binding of topiramate from 23% to 13%. Topiramate does not influence the binding of sodium valproate.
Metabolism and Excretion:
Topiramate is not extensively metabolized and is primarily eliminated unchanged in the urine (approximately 70% of an administered dose). Six metabolites have been identified in humans, none of which constitutes more than 5% of an administered dose. The metabolites are formed via hydroxylation, hydrolysis, and glucuronidation. There is evidence of renal tubular reabsorption of topiramate. In rats, given probenecid to inhibit tubular reabsorption, along with topiramate, a significant increase in renal clearance of topiramate was observed. This interaction has not been evaluated in humans. Overall, oral plasma clearance (CL/F) is approximately 20 to 30 mL/min in humans following oral administration.
Pharmacokinetic Interactions
(see also Drug Interactions):
Antiepileptic Drugs
Potential interactions between topiramate and standard AEDs were assessed in controlled clinical pharmacokinetic studies in patients with epilepsy. The effect of these interactions on mean plasma AUCs are summarized under PRECAUTIONS (Table 4).
Special Populations:
Renal Impairment:
The clearance of topiramate was reduced by 42% in moderately renally impaired (creatinine clearance 30 to 69 mL/min/1.73m2) and by 54% in severely renally impaired subjects (creatinine clearance <30 mL/min/1.73m2) compared to normal renal function subjects (creatinine clearance >70 mL/min/1.73m2). Since topiramate is presumed to undergo significant tubular reabsorption, it is uncertain whether this experience can be generalized to all situations of renal impairment. It is conceivable that some forms of renal disease could differentially affect glomerular filtration rate and tubular reabsorption resulting in a clearance of topiramate not predicted by creatinine clearance. In general, however, use of one-half the usual starting and maintenance dose is recommended in patients with moderate or severe renal impairment (see PRECAUTIONS: Adjustment of Dose in Renal Failure and DOSAGE AND ADMINISTRATION).
Hemodialysis:
Topiramate is cleared by hemodialysis. Using a high efficiency, counterflow, single pass-dialysate hemodialysis procedure, topiramate dialysis clearance was 120 mL/min with blood flow through the dialyzer at 400 mL/min. This high clearance (compared to 20 to 30 mL/min total oral clearance in healthy adults) will remove a clinically significant amount of topiramate from the patient over the hemodialysis treatment period. Therefore, a supplemental dose may be required (see DOSAGE AND ADMINISTRATION).
Hepatic Impairment:
In hepatically impaired subjects, the clearance of topiramate may be decreased; the mechanism underlying the decrease is not well understood.
Age, Gender, and Race:
The pharmacokinetics of topiramate in elderly subjects (65 to 85 years of age, N=16) were evaluated in a controlled clinical study. The elderly subject population had reduced renal function [creatinine clearance (-20%)] compared to young adults. Following a single oral 100 mg dose, maximum plasma concentration for elderly and young adults was achieved at approximately 1 to 2 hours. Reflecting the primary renal elimination of topiramate, topiramate plasma and renal clearance were reduced 21% and 19%, respectively, in elderly subjects, compared to young adults. Similarly, topiramate half-life was longer (13%) in the elderly. Reduced topiramate clearance resulted in slightly higher maximum plasma concentration (23%) and AUC (25%) in elderly subjects than observed in young adults. Topiramate clearance is decreased in the elderly only to the extent that renal function is reduced. As recommended for all patients, dosage adjustment may be indicated in the elderly patient when impaired renal function (creatinine clearance rate ≤70 mL/min/1.73 m2) is evident. It may be useful to monitor renal function in the elderly patient (see Special Populations: Renal Impairment, PRECAUTIONS: Adjustment of Dose in Renal Failure and DOSAGE AND ADMINISTRATION).
Clearance of topiramate in adults was not affected by gender or race.
Pediatric Pharmacokinetics:
Pharmacokinetics of topiramate were evaluated in patients ages 4 to 17 years receiving one or two other antiepileptic drugs. Pharmacokinetic profiles were obtained after one week at doses of 1, 3, and 9 mg/kg/day. Clearance was independent of dose.
Pediatric patients have a 50% higher clearance and consequently shorter elimination half-life than adults. Consequently, the plasma concentration for the same mg/kg dose may be lower in pediatric patients compared to adults. As in adults, hepatic enzyme-inducing antiepileptic drugs decrease the steady state plasma concentrations of topiramate.
-
CLINICAL STUDIES
The studies described in the following sections were conducted using topiramate tablets.
Epilepsy
Monotherapy Controlled Trial
The effectiveness of topiramate as initial monotherapy in adults and children 10 years of age and older with partial onset or primary generalized seizures was established in a multicenter, randomized, double-blind, parallel-group trial.
The trial was conducted in 487 patients diagnosed with epilepsy (6 to 83 years of age) who had 1 or 2 well-documented seizures during the 3-month retrospective baseline phase who then entered the study and received topiramate 25 mg/day for 7 days in an open-label fashion. Forty-nine percent of subjects had no prior AED treatment and 17% had a diagnosis of epilepsy for greater than 24 months. Any AED therapy used for temporary or emergency purposes was discontinued prior to randomization. In the double-blind phase, 470 patients were randomized to titrate up to 50 mg/day or 400 mg/day. If the target dose could not be achieved, patients were maintained on the maximum tolerated dose. Fifty eight percent of patients achieved the maximal dose of 400 mg/day for ≥ 2 weeks, and patients who did not tolerate 150 mg/day were discontinued. The primary efficacy assessment was a between group comparison of time to first seizure during the double-blind phase. Comparison of the Kaplan-Meier survival curves of time to first seizure favored the topiramate 400 mg/day group over the topiramate 50 mg/day group (p=0.0002, log rank test; Figure 1). The treatment effects with respect to time to first seizure were consistent across various patient subgroups defined by age, sex, geographic region, baseline body weight, baseline seizure type, time since diagnosis, and baseline AED use.
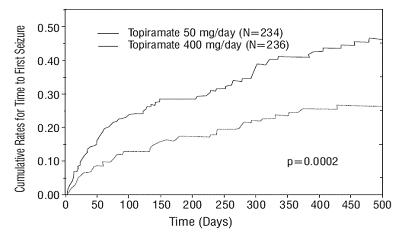
Figure 1: Kaplan-Meier Estimates of Cumulative Rates for Time to First Seizure
Adjunctive Therapy Controlled Trials in Patients With Partial Onset Seizures
The effectiveness of topiramate as an adjunctive treatment for adults with partial onset seizures was established in six multicenter, randomized, double-blind, placebo-controlled trials, two comparing several dosages of topiramate and placebo and four comparing a single dosage with placebo, in patients with a history of partial onset seizures, with or without secondarily generalized seizures.
Patients in these studies were permitted a maximum of two antiepileptic drugs (AEDs) in addition to topiramate tablets or placebo. In each study, patients were stabilized on optimum dosages of their concomitant AEDs during baseline phase lasting between 4 and 12 weeks. Patients who experienced a prespecified minimum number of partial onset seizures, with or without secondary generalization, during the baseline phase (12 seizures for 12-week baseline, 8 for 8-week baseline, or 3 for 4-week baseline) were randomly assigned to placebo or a specified dose of topiramate tablets in addition to their other AEDs.
Following randomization, patients began the double-blind phase of treatment. In five of the six studies, patients received active drug beginning at 100 mg per day; the dose was then increased by 100 mg or 200 mg/day increments weekly or every other week until the assigned dose was reached, unless intolerance prevented increases. In the sixth study (119), the 25 or 50 mg/day initial doses of topiramate were followed by respective weekly increments of 25 or 50 mg/day until the target dose of 200 mg/day was reached. After titration, patients entered a 4, 8, or 12-week stabilization period. The numbers of patients randomized to each dose, and the actual mean and median doses in the stabilization period are shown in Table 1.
Adjunctive Therapy Controlled Trial in Pediatric Patients Ages 2 to 16 Years With Partial Onset Seizures
The effectiveness of topiramate as an adjunctive treatment for pediatric patients ages 2 to 16 years with partial onset seizures was established in a multicenter, randomized, double-blind, placebo-controlled trial, comparing topiramate and placebo in patients with a history of partial onset seizures, with or without secondarily generalized seizures.
Patients in this study were permitted a maximum of two antiepileptic drugs (AEDs) in addition to topiramate tablets or placebo. In this study, patients were stabilized on optimum dosages of their concomitant AEDs during an 8-week baseline phase. Patients who experienced at least six partial onset seizures, with or without secondarily generalized seizures, during the baseline phase were randomly assigned to placebo or topiramate tablets in addition to their other AEDs.
Following randomization, patients began the double-blind phase of treatment. Patients received active drug beginning at 25 or 50 mg per day; the dose was then increased by 25 mg to 150 mg/day increments every other week until the assigned dosage of 125, 175, 225, or 400 mg/day based on patients' weight to approximate a dosage of 6 mg/kg per day was reached, unless intolerance prevented increases. After titration, patients entered an 8-week stabilization period.
Adjunctive Therapy Controlled Trial in Patients With Primary Generalized Tonic-Clonic Seizures
The effectiveness of topiramate as an adjunctive treatment for primary generalized tonic-clonic seizures in patients 2 years old and older was established in a multicenter, randomized, double-blind, placebo-controlled trial, comparing a single dosage of topiramate and placebo.
Patients in this study were permitted a maximum of two antiepileptic drugs (AEDs) in addition to topiramate or placebo. Patients were stabilized on optimum dosages of their concomitant AEDs during an 8-week baseline phase. Patients who experienced at least three primary generalized tonic-clonic seizures during the baseline phase were randomly assigned to placebo or topiramate in addition to their other AEDs.
Following randomization, patients began the double-blind phase of treatment. Patients received active drug beginning at 50 mg per day for four weeks; the dose was then increased by 50 mg to 150 mg/day increments every other week until the assigned dose of 175, 225, or 400 mg/day based on patients' body weight to approximate a dosage of 6 mg/kg per day was reached, unless intolerance prevented increases. After titration, patients entered a 12-week stabilization period.
Adjunctive Therapy Controlled Trial in Patients With Lennox-Gastaut Syndrome
The effectiveness of topiramate as an adjunctive treatment for seizures associated with Lennox-Gastaut syndrome was established in a multicenter, randomized, double-blind, placebo-controlled trial comparing a single dosage of topiramate with placebo in patients 2 years of age and older.
Patients in this study were permitted a maximum of two antiepileptic drugs (AEDs) in addition to topiramate or placebo. Patients who were experiencing at least 60 seizures per month before study entry were stabilized on optimum dosages of their concomitant AEDs during a 4-week baseline phase. Following baseline, patients were randomly assigned to placebo or topiramate in addition to their other AEDs. Active drug was titrated beginning at 1 mg/kg per day for a week; the dose was then increased to 3 mg/kg per day for one week then to 6 mg/kg per day. After titration, patients entered an 8-week stabilization period. The primary measures of effectiveness were the percent reduction in drop attacks and a parental global rating of seizure severity.
Table 1: Topiramate Dose Summary During the Stabilization Periods of Each of Six Double-Blind, Placebo-Controlled, Add-On Trials in Adults with Partial Onset Seizuresb Target Topiramate Dosage (mg/day) Protocol Stabilization Dose Placeboa 200 400 600 800 1,000 a Placebo dosages are given as the number of tablets. Placebo target dosages were as follows: Protocol Y1, 4 tablets/day; Protocols YD and Y2, 6 tablets/day; Protocol Y3 and 119, 8 tablets/day; Protocol YE, 10 tablets/day.
b Dose-response studies were not conducted for other indications or pediatric partial onset seizures.
YD N 42 42 40 41 -- -- Mean Dose 5.9 200 390 556 -- -- Median Dose 6.0 200 400 600 -- -- YE N 44 -- -- 40 45 40 Mean Dose 9.7 -- -- 544 739 796 Median Dose 10.0 -- -- 600 800 1,000 Y1 N 23 -- 19 -- -- -- Mean Dose 3.8 -- 395 -- -- -- Median Dose 4.0 -- 400 -- -- -- Y2 N 30 -- -- 28 -- -- Mean Dose 5.7 -- -- 522 -- -- Median Dose 6.0 -- -- 600 -- -- Y3 N 28 -- -- -- 25 -- Mean Dose 7.9 -- -- -- 568 -- Median Dose 8.0 -- -- -- 600 -- 119 N 90 157 -- -- -- -- Mean Dose 8 200 -- -- -- -- Median Dose 8 200 -- -- -- -- In all add-on trials, the reduction in seizure rate from baseline during the entire double-blind phase was measured. The median percent reductions in seizure rates and the responder rates (fraction of patients with at least a 50% reduction) by treatment group for each study are shown below in Table 2. As described above, a global improvement in seizure severity was also assessed in the Lennox-Gastaut trial.
Table 2: Efficacy Results in Double-Blind, Placebo-Controlled, Add-On Epilepsy Trials Target Topiramate Dosage (mg/day) Protocol Efficacy Results Placebo 200 400 600 800 1,000 ≈6
mg/kg/day*Comparisons with placebo: a p=0.080; b p<0.010; c p<0.001; d p<0.050; e p=0.065; f p<0.005;g p=0.071;
h Median % reduction and % responders are reported for PGTC Seizures;
i Median % reduction and % responders for drop attacks, i.e., tonic or atonic seizures;
j Percent of subjects who were minimally, much, or very much improved from baseline
* For Protocols YP and YTC, protocol-specified target dosages (<9.3 mg/kg/day) were assigned based on subject's weight to approximate a dosage of 6 mg/kg per day; these dosages corresponded to mg/day dosages of 125, 175, 225, and 400 mg/day.
Partial Onset Seizures Studies in Adults YD N 45 45 45 46 -- -- -- Median % Reduction 11.6 27.2a 47.5b 44.7c -- -- -- % Responders 18 24 44d 46d -- -- -- YE N 47 -- -- 48 48 47 -- Median % Reduction 1.7 -- -- 40.8c 41.0c 36.0c -- % Responders 9 -- -- 40c 41c 36d -- Y1 N 24 -- 23 -- -- -- -- Median % Reduction 1.1 -- 40.7e -- -- -- -- % Responders 8 -- 35d -- -- -- -- Y2 N 30 -- -- 30 -- -- -- Median % Reduction -12.2 -- -- 46.4f -- -- -- % Responders 10 -- -- 47c -- -- -- Y3 N 28 -- -- -- 28 -- -- Median % Reduction -20.6 -- -- -- 24.3c -- -- % Responders 0 -- -- -- 43c -- -- 119 N 91 168 -- -- -- -- -- Median % Reduction 20.0 44.2c -- -- -- -- -- % Responders 24 45c -- -- -- -- -- Studies in Pediatric Patients YP N 45 -- -- -- -- -- 41 Median % Reduction 10.5 -- -- -- -- -- 33.1d % Responders 20 -- -- -- -- -- 39 Primary Generalized Tonic-Clonich YTC N 40 -- -- -- -- -- 39 Median % Reduction 9.0 -- -- -- -- -- 56.7d % Responders 20 -- -- -- -- -- 56c Lennox-Gastaut Syndromei YL N 49 -- -- -- -- -- 46 Median % Reduction -5.1 -- -- -- -- -- 14.8d % Responders 14 -- -- -- -- -- 28g Improvement in Seizure Severityj 28 -- -- -- -- -- 52d Subset analyses of the antiepileptic efficacy of topiramate tablets in these studies showed no differences as a function of gender, race, age, baseline seizure rate, or concomitant AED.
-
INDICATIONS AND USAGE
Monotherapy Epilepsy
Topiramate tablets are indicated as initial monotherapy in patients 10 years of age and older with partial onset or primary generalized tonic-clonic seizures.
Effectiveness was demonstrated in a controlled trial in patients with epilepsy who had no more than 2 seizures in the 3 months prior to enrollment. Safety and effectiveness in patients who were converted to monotherapy from a previous regimen of other anticonvulsant drugs have not been established in controlled trials.
Adjunctive Therapy Epilepsy
Topiramate tablets are indicated as adjunctive therapy for adults and pediatric patients ages 2 to 16 years with partial onset seizures, or primary generalized tonic-clonic seizures, and in patients 2 years of age and older with seizures associated with Lennox-Gastaut syndrome.
- CONTRAINDICATIONS
-
WARNINGS
Acute Myopia and Secondary Angle Closure Glaucoma
A syndrome consisting of acute myopia associated with secondary angle closure glaucoma has been reported in patients receiving topiramate. Symptoms include acute onset of decreased visual acuity and/or ocular pain. Ophthalmologic findings can include myopia, anterior chamber shallowing, ocular hyperemia (redness) and increased intraocular pressure. Mydriasis may or may not be present. This syndrome may be associated with supraciliary effusion resulting in anterior displacement of the lens and iris, with secondary angle closure glaucoma. Symptoms typically occur within 1 month of initiating topiramate therapy. In contrast to primary narrow angle glaucoma, which is rare under 40 years of age, secondary angle closure glaucoma associated with topiramate has been reported in pediatric patients as well as adults. The primary treatment to reverse symptoms is discontinuation of topiramate as rapidly as possible, according to the judgment of the treating physician. Other measures, in conjunction with discontinuation of topiramate, may be helpful.
Elevated intraocular pressure of any etiology, if left untreated, can lead to serious sequelae including permanent vision loss.
Oligohidrosis and Hyperthermia
Oligohidrosis (decreased sweating), infrequently resulting in hospitalization, has been reported in association with topiramate use. Decreased sweating and an elevation in body temperature above normal characterized these cases. Some of the cases were reported after exposure to elevated environmental temperatures.
The majority of the reports have been in children. Patients, especially pediatric patients, treated with topiramate should be monitored closely for evidence of decreased sweating and increased body temperature, especially in hot weather. Caution should be used when topiramate is prescribed with other drugs that predispose patients to heat-related disorders; these drugs include, but are not limited to, other carbonic anhydrase inhibitors and drugs with anticholinergic activity.
Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including topiramate, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5 to 100 years) in the clinical trials analyzed.
Table 3 shows absolute and relative risk by indication for all evaluated AEDs.
Table 3 Risk by Indication for Antiepileptic Drugs in the Pooled Analysis Indication Placebo Patients with Events Per 1000 Patients Drug Patients with Events Per 1000 Patients Relative Risk: Incidence of Events in Drug Patients/Incidence in Placebo Patients Risk Difference: Additional Drug Patients with Events Per 1000 Patients Epilepsy 1.0 3.4 3.5 2.4 Psychiatric 5.7 8.5 1.5 2.9 Other 1.0 1.8 1.9 0.9 Total 2.4 4.3 1.8 1.9 The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing topiramate or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior or the emergence of suicidal thoughts, behavior or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Metabolic Acidosis
Hyperchloremic, non-anion gap, metabolic acidosis (i.e., decreased serum bicarbonate below the normal reference range in the absence of chronic respiratory alkalosis) is associated with topiramate treatment. This metabolic acidosis is caused by renal bicarbonate loss due to the inhibitory effect of topiramate on carbonic anhydrase. Such electrolyte imbalance has been observed with the use of topiramate in placebo-controlled clinical trials and in the post-marketing period. Generally, topiramate-induced metabolic acidosis occurs early in treatment although cases can occur at any time during treatment. Bicarbonate decrements are usually mild-moderate (average decrease of 4 mEq/L at daily doses of 400 mg in adults and at approximately 6 mg/kg/day in pediatric patients); rarely, patients can experience severe decrements to values below 10 mEq/L. Conditions or therapies that predispose to acidosis (such as renal disease, severe respiratory disorders, status epilepticus, diarrhea, surgery, ketogenic diet, or drugs) may be additive to the bicarbonate lowering effects of topiramate.
In adults, the incidence of persistent treatment-emergent decreases in serum bicarbonate (levels of <20 mEq/L at two consecutive visits or at the final visit) in controlled clinical trials for adjunctive treatment of epilepsy was 32% for 400 mg/day, and 1% for placebo. Metabolic acidosis has been observed at doses as low as 50 mg/day. The incidence of persistent treatment-emergent decreases in serum bicarbonate in adults in the epilepsy controlled clinical trial for monotherapy was 15% for 50 mg/day and 25% for 400 mg/day. The incidence of a markedly abnormally low serum bicarbonate (i.e., absolute value <17 mEq/L and >5 mEq/L decrease from pretreatment) in the adjunctive therapy trials was 3% for 400 mg/day, and 0% for placebo and in the monotherapy trial was 1% for 50 mg/day and 7% for 400 mg/day. Serum bicarbonate levels have not been systematically evaluated at daily doses greater than 400 mg/day.
In pediatric patients (<16 years of age), the incidence of persistent treatment-emergent decreases in serum bicarbonate in placebo-controlled trials for adjunctive treatment of Lennox-Gastaut syndrome or refractory partial onset seizures was 67% for topiramate (at approximately 6 mg/kg/day), and 10% for placebo. The incidence of a markedly abnormally low serum bicarbonate (i.e., absolute value <17 mEq/L and >5 mEq/L decrease from pretreatment) in these trials was 11% for topiramate and 0% for placebo. Cases of moderately severe metabolic acidosis have been reported in patients as young as 5 months old, especially at daily doses above 5 mg/kg/day.
In pediatric patients (10 years up to 16 years of age), the incidence of persistent treatment-emergent decreases in serum bicarbonate in the epilepsy controlled clinical trial for monotherapy was 7% for 50 mg/day and 20% for 400 mg/day. The incidence of a markedly abnormally low serum bicarbonate (i.e., absolute value <17 mEq/L and >5 mEq/L decrease from pretreatment) in this trial was 4% for 50 mg/day and 4% for 400 mg/day.
Some manifestations of acute or chronic metabolic acidosis may include hyperventilation, nonspecific symptoms such as fatigue and anorexia, or more severe sequelae including cardiac arrhythmias or stupor. Chronic, untreated metabolic acidosis may increase the risk for nephrolithiasis or nephrocalcinosis, and may also result in osteomalacia (referred to as rickets in pediatric patients) and/or osteoporosis with an increased risk for fractures. Chronic metabolic acidosis in pediatric patients may also reduce growth rates. A reduction in growth rate may eventually decrease the maximal height achieved. The effect of topiramate on growth and bone-related sequelae has not been systematically investigated.
Measurement of baseline and periodic serum bicarbonate during topiramate treatment is recommended. If metabolic acidosis develops and persists, consideration should be given to reducing the dose or discontinuing topiramate (using dose tapering). If the decision is made to continue patients on topiramate in the face of persistent acidosis, alkali treatment should be considered.
Cognitive/Neuropsychiatric Adverse Events
Adults
Adverse events most often associated with the use of topiramate were related to the central nervous system and were observed in the epilepsy population. In adults, the most frequent of these can be classified into three general categories: 1) Cognitive-related dysfunction (e.g. confusion, psychomotor slowing, difficulty with concentration/attention, difficulty with memory, speech or language problems, particularly word-finding difficulties); 2) Psychiatric/behavioral disturbances (e.g. depression or mood problems); and 3) Somnolence or fatigue.
Cognitive-Related Dysfunction
The majority of cognitive-related adverse events were mild to moderate in severity, and they frequently occurred in isolation. Rapid titration rate and higher initial dose were associated with higher incidences of these events. Many of these events contributed to withdrawal from treatment [see ADVERSE REACTIONS, Table 5 and Table 7].
In the original add-on epilepsy controlled trials (using rapid titration such as 100 to 200 mg/day weekly increments), the proportion of patients who experienced one or more cognitive-related adverse events was 42% for 200 mg/day, 41% for 400 mg/day, 52% for 600 mg/day, 56% for 800 and 1000 mg/day, and 14% for placebo. These dose-related adverse reactions began with a similar frequency in the titration or in the maintenance phase, although in some patients the events began during titration and persisted into the maintenance phase. Some patients who experienced one or more cognitive-related adverse events in the titration phase had a dose-related recurrence of these events in the maintenance phase.
In the monotherapy epilepsy controlled trial, the proportion of patients who experienced one or more cognitive-related adverse events was 19% for topiramate 50 mg/day and 26% for 400 mg/day.
Psychiatric/Behavioral Disturbances
Psychiatric/behavioral disturbances (depression or mood problems) were dose-related for the epilepsy population.
Somnolence/Fatigue
Somnolence and fatigue were the adverse events most frequently reported during clinical trials of topiramate for adjunctive epilepsy. For the adjunctive epilepsy population, the incidence of somnolence did not differ substantially between 200 mg/day and 1000 mg/day, but the incidence of fatigue was dose-related and increased at dosages above 400 mg/day. For the monotherapy epilepsy population in the 50 mg/day and 400 mg/day groups, the incidence of somnolence was dose-related (9% for the 50 mg/day group and 15% for the 400 mg/day group) and the incidence of fatigue was comparable in both treatment groups (14% each).
Additional nonspecific CNS events commonly observed with topiramate in the add-on epilepsy population include dizziness or ataxia.
Pediatric Patients
In double-blind adjunctive therapy and monotherapy epilepsy clinical studies, the incidences of cognitive/neuropsychiatric adverse events in pediatric patients were generally lower than observed in adults. These events included psychomotor slowing, difficulty with concentration/attention, speech disorders/related speech problems and language problems. The most frequently reported neuropsychiatric events in pediatric patients during adjunctive therapy double-blind studies were somnolence and fatigue. The most frequently reported neuropsychiatric events in pediatric patients in the 50 mg/day and 400 mg/day groups during the monotherapy double-blind study were headache, dizziness, anorexia, and somnolence.
No patients discontinued treatment due to any adverse events in the adjunctive epilepsy double-blind trials. In the monotherapy epilepsy double-blind trial, 1 pediatric patient (2%) in the 50 mg/day group and 7 pediatric patients (12%) in the 400 mg/day group discontinued treatment due to any adverse events. The most common adverse event associated with discontinuation of therapy was difficulty with concentration/attention; all occurred in the 400 mg/day group.
Withdrawal of AEDs
Antiepileptic drugs, including topiramate, should be withdrawn gradually to minimize the potential of increased seizure frequency.
Sudden Unexplained Death in Epilepsy (SUDEP)
During the course of premarketing development of topiramate tablets, 10 sudden and unexplained deaths were recorded among a cohort of treated patients (2,796 subject years of exposure). This represents an incidence of 0.0035 deaths per patient year. Although this rate exceeds that expected in a healthy population matched for age and sex, it is within the range of estimates for the incidence of sudden unexplained deaths in patients with epilepsy not receiving topiramate (ranging from 0.0005 for the general population of patients with epilepsy, to 0.003 for a clinical trial population similar to that in the topiramate program, to 0.005 for patients with refractory epilepsy).
-
PRECAUTIONS
Hyperammonemia and Encephalopathy Associated with Concomitant Valproic Acid Use
Concomitant administration of topiramate and valproic acid has been associated with hyperammonemia with or without encephalopathy in patients who have tolerated either drug alone. Clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy or vomiting. In most cases, symptoms and signs abated with discontinuation of either drug. This adverse event is not due to a pharmacokinetic interaction.
It is not known if topiramate monotherapy is associated with hyperammonemia.
Patients with inborn errors of metabolism or reduced hepatic mitochondrial activity may be at an increased risk for hyperammonemia with or without encephalopathy. Although not studied, an interaction of topiramate and valproic acid may exacerbate existing defects or unmask deficiencies in susceptible persons.
In patients who develop unexplained lethargy, vomiting, or changes in mental status, hyperammonemic encephalopathy should be considered and an ammonia level should be measured.
Kidney Stones
A total of 32/2,086 (1.5%) of adults exposed to topiramate during its adjunctive epilepsy therapy development reported the occurrence of kidney stones, an incidence about 2 to 4 times greater than expected in a similar, untreated population. In the double-blind monotherapy epilepsy study, a total of 4/319 (1.3%) of adults exposed to topiramate reported the occurrence of kidney stones. As in the general population, the incidence of stone formation among topiramate treated patients was higher in men. Kidney stones have also been reported in pediatric patients.
An explanation for the association of topiramate and kidney stones may lie in the fact that topiramate is a carbonic anhydrase inhibitor. Carbonic anhydrase inhibitors, e.g., acetazolamide or dichlorphenamide, promote stone formation by reducing urinary citrate excretion and by increasing urinary pH. The concomitant use of topiramate with other carbonic anhydrase inhibitors or potentially in patients on a ketogenic diet may create a physiological environment that increases the risk of kidney stone formation, and should therefore be avoided.
Increased fluid intake increases the urinary output, lowering the concentration of substances involved in stone formation. Hydration is recommended to reduce new stone formation.
Paresthesia
Paresthesia (usually tingling of the extremities), an effect associated with the use of other carbonic anhydrase inhibitors, appears to be a common effect of topiramate. Paresthesia was more frequently reported in the monotherapy epilepsy trials versus the adjunctive therapy epilepsy trials. In the majority of instances, paresthesia did not lead to treatment discontinuation.
Adjustment of Dose in Renal Failure
The major route of elimination of unchanged topiramate and its metabolites is via the kidney. Dosage adjustment may be required in patients with reduced renal function (see DOSAGE AND ADMINISTRATION).
Decreased Hepatic Function
In hepatically impaired patients, topiramate should be administered with caution as the clearance of topiramate may be decreased.
Information for Patients
Patients and their caregivers should be informed of the availability of a Medication Guide, and they should be instructed to read the Medication Guide prior to taking topiramate tablets. Patients should be instructed to take topiramate tablets only as prescribed.
Patients taking topiramate should be told to seek immediate medical attention if they experience blurred vision or periorbital pain.
Patients, especially pediatric patients, treated with topiramate should be monitored closely for evidence of decreased sweating and increased body temperature, especially in hot weather.
Patients, their caregivers, and families should be counseled that AEDs, including topiramate, may increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior or the emergence of suicidal thoughts, behavior or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Patients, particularly those with predisposing factors, should be instructed to maintain an adequate fluid intake in order to minimize the risk of renal stone formation (see PRECAUTIONS: Kidney Stones, for support regarding hydration as a preventative measure).
Patients should be warned about the potential for somnolence, dizziness, confusion, and difficulty concentrating, and advised not to drive or operate machinery until they have gained sufficient experience on topiramate to gauge whether it adversely affects their mental performance and/or motor performance.
Additional food intake may be considered if the patient is losing weight while on this medication.
Patients should be encouraged to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant. This registry is collecting information about the safety of antiepileptic drugs during pregnancy. To enroll, patients can call the toll free number, 1-888-233-2334 (see PRECAUTIONS: Pregnancy: Pregnancy Category C).
Laboratory Tests:
Measurement of baseline and periodic serum bicarbonate during topiramate treatment is recommended (see WARNINGS).
Drug Interactions:
In vitro studies indicate that topiramate does not inhibit enzyme activity for CYP1A2, CYP2A6, CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP2E1 and CYP3A4/5 isozymes.
Antiepileptic Drugs
Potential interactions between topiramate and standard AEDs were assessed in controlled clinical pharmacokinetic studies in patients with epilepsy. The effects of these interactions on mean plasma AUCs are summarized in Table 4.
In Table 4, the second column (AED concentration) describes what happens to the concentration of the AED listed in the first column when topiramate is added.
The third column (topiramate concentration) describes how the coadministration of a drug listed in the first column modifies the concentration of topiramate in experimental settings when topiramate was given alone.
Table 4: Summary of AED Interactions with Topiramate AED
Co-administeredAED
ConcentrationTopiramate
Concentrationa = Plasma concentration increased 25% in some patients, generally those on a b.i.d. dosing regimen of phenytoin.
b = Is not administered but is an active metabolite of carbamazepine.
NC = Less than 10% change in plasma concentration.
AED = Antiepileptic drug.
NE = Not Evaluated.
TPM = Topiramate
Phenytoin NC or 25% increasea 48% decrease Carbamazepine (CBZ) NC 40% decrease CBZ epoxideb NC NE Valproic acid 11% decrease 14% decrease Phenobarbital NC NE Primidone NC NE Lamotrigine NC at TPM doses up to 400 mg/day 15% increase In addition to the pharmacokinetic interaction described in the above table, concomitant administration of valproic acid and topiramate has been associated with hyperammonemia with and without encephalopathy (see PRECAUTIONS, Hyperammonemia and Encephalopathy Associated with Concomitant Valproic Acid Use).
Other Drug Interactions
Digoxin
In a single-dose study, serum digoxin AUC was decreased by 12% with concomitant topiramate administration. The clinical relevance of this observation has not been established.
CNS Depressants
Concomitant administration of topiramate and alcohol or other CNS depressant drugs has not been evaluated in clinical studies. Because of the potential of topiramate to cause CNS depression, as well as other cognitive and/or neuropsychiatric adverse events, topiramate should be used with extreme caution if used in combination with alcohol and other CNS depressants.
Oral Contraceptives
In a pharmacokinetic interaction study in healthy volunteers with a concomitantly administered combination oral contraceptive product containing 1 mg norethindrone (NET) plus 35 mcg ethinyl estradiol (EE), topiramate given in the absence of other medications at doses of 50 to 200 mg/day was not associated with statistically significant changes in mean exposure (AUC) to either component of the oral contraceptive. In another study, exposure to EE was statistically significantly decreased at doses of 200, 400, and 800 mg/day (18%, 21%, and 30%, respectively) when given as adjunctive therapy in patients taking valproic acid. In both studies, topiramate (50 mg/day to 800 mg/day) did not significantly affect exposure to NET. Although there was a dose dependent decrease in EE exposure for doses between 200 to 800 mg/day, there was no significant dose dependent change in EE exposure for doses of 50 to 200 mg/day. The clinical significance of the changes observed is not known. The possibility of decreased contraceptive efficacy and increased breakthrough bleeding should be considered in patients taking combination oral contraceptive products with topiramate. Patients taking estrogen containing contraceptives should be asked to report any change in their bleeding patterns. Contraceptive efficacy can be decreased even in the absence of breakthrough bleeding.
Hydrochlorothiazide (HCTZ)
A drug-drug interaction study conducted in healthy volunteers evaluated the steady-state pharmacokinetics of HCTZ (25 mg q24h) and topiramate (96 mg q12h) when administered alone and concomitantly. The results of this study indicate that topiramate Cmax increased by 27% and AUC increased by 29% when HCTZ was added to topiramate. The clinical significance of this change is unknown. The addition of HCTZ to topiramate therapy may require an adjustment of the topiramate dose. The steady-state pharmacokinetics of HCTZ were not significantly influenced by the concomitant administration of topiramate. Clinical laboratory results indicated decreases in serum potassium after topiramate or HCTZ administration, which were greater when HCTZ and topiramate were administered in combination.
Pioglitazone
A drug-drug interaction study conducted in healthy volunteers evaluated the steady-state pharmacokinetics of topiramate and pioglitazone when administered alone and concomitantly. A 15% decrease in the AUCτ,ss of pioglitazone with no alteration in Cmax,ss was observed. This finding was not statistically significant. In addition, a 13% and 16% decrease in Cmax,ss and AUCτ,ss respectively, of the active hydroxy-metabolite was noted as well as a 60% decrease in Cmax,ss and AUCτ,ss of the active keto-metabolite. The clinical significance of these findings is not known. When topiramate is added to pioglitazone therapy or pioglitazone is added to topiramate therapy, careful attention should be given to the routine monitoring of patients for adequate control of their diabetic disease state.
Lithium
Multiple dosing of topiramate 100 mg every 12 hrs decreased the AUC and cmax of Lithium (300 mg every 8 hrs) by 20% (N=12, 6 M; 6 F).
Haloperidol
The pharmacokinetics of a single dose of haloperidol (5 mg) were not affected following multiple dosing of topiramate (100 mg every 12 hr) in 13 healthy adults (6 M, 7 F).
Amitriptyline
There was a 12% increase in AUC and Cmax for amitriptyline (25 mg per day) in 18 normal subjects (9 male; 9 female) receiving 200 mg/day of topiramate. Some subjects may experience a large increase in amitriptyline concentration in the presence of topiramate and any adjustments in amitriptyline dose should be made according to the patient's clinical response and not on the basis of plasma levels.
Sumatriptan
Multiple dosing of topiramate (100 mg every 12 hrs) in 24 healthy volunteers (14 M, 10 F) did not affect the pharmacokinetics of single dose sumatriptan either orally (100 mg) or subcutaneously (6 mg).
Risperidone
There was a 25% decrease in exposure to risperidone (2 mg single dose) in 12 healthy volunteers (6 M, 6 F) receiving 200 mg/day of topiramate. Therefore, patients receiving risperidone in combination with topiramate should be closely monitored for clinical response.
Propranolol
Multiple dosing of topiramate (200 mg/day) in 34 healthy volunteers (17 M, 17 F) did not affect the pharmacokinetics of propranolol following daily 160 mg doses. Propranolol doses of 160 mg/day in 39 volunteers (27M, 12F) had no effect on the exposure to topiramate at a dose of 200 mg/day of topiramate.
Dihydroergotamine
Multiple dosing of topiramate (200 mg/day) in 24 healthy volunteers (12 M, 12 F) did not affect the pharmacokinetics of a 1 mg subcutaneous dose of dihydroergotamine. Similarly, a 1 mg subcutaneous dose of dihydroergotamine did not affect the pharmacokinetics of a 200 mg/day dose of topiramate in the same study.
Drug/Laboratory Tests Interactions
There are no known interactions of topiramate with commonly used laboratory tests.
Carcinogenesis, Mutagenesis, Impairment of Fertility:
An increase in urinary bladder tumors was observed in mice given topiramate (20, 75, and 300 mg/kg) in the diet for 21 months. The elevated bladder tumor incidence, which was statistically significant in males and females receiving 300 mg/kg, was primarily due to the increased occurrence of a smooth muscle tumor considered histomorphologically unique to mice. Plasma exposures in mice receiving 300 mg/kg were approximately 0.5 to 1 times steady-state exposures measured in patients receiving topiramate monotherapy at the recommended human dose (RHD) of 400 mg, and 1.5 to 2 times steady-state topiramate exposures in patients receiving 400 mg of topiramate plus phenytoin. The relevance of this finding to human carcinogenic risk is uncertain. No evidence of carcinogenicity was seen in rats following oral administration of topiramate for 2 years at doses up to 120 mg/kg (approximately 3 times the RHD on a mg/m2 basis).
Topiramate did not demonstrate genotoxic potential when tested in a battery of in vitro and in vivo assays. Topiramate was not mutagenic in the Ames test or the in vitro mouse lymphoma assay; it did not increase unscheduled DNA synthesis in rat hepatocytes in vitro; and it did not increase chromosomal aberrations in human lymphocytes in vitro or in rat bone marrow in vivo.
No adverse effects on male or female fertility were observed in rats at doses up to 100 mg/kg (2.5 times the RHD on a mg/m2 basis).
Pregnancy: Pregnancy Category C.
Topiramate has demonstrated selective developmental toxicity, including teratogenicity, in experimental animal studies. When oral doses of 20, 100, or 500 mg/kg were administered to pregnant mice during the period of organogenesis, the incidence of fetal malformations (primarily craniofacial defects) was increased at all doses. The low dose is approximately 0.2 times the recommended human dose (RHD=400 mg/day) on a mg/m2 basis. Fetal body weights and skeletal ossification were reduced at 500 mg/kg in conjunction with decreased maternal body weight gain.
In rat studies (oral doses of 20, 100, and 500 mg/kg or 0.2, 2.5, 30, and 400 mg/kg), the frequency of limb malformations (ectrodactyly, micromelia, and amelia) was increased among the offspring of dams treated with 400 mg/kg (10 times the RHD on a mg/m2 basis) or greater during the organogenesis period of pregnancy. Embryotoxicity (reduced fetal body weights, increased incidence of structural variations) was observed at doses as low as 20 mg/kg (0.5 times the RHD on a mg/m2 basis). Clinical signs of maternal toxicity were seen at 400 mg/kg and above, and maternal body weight gain was reduced during treatment with 100 mg/kg or greater.
In rabbit studies (20, 60, and 180 mg/kg or 10, 35, and 120 mg/kg orally during organogenesis), embryo/fetal mortality was increased at 35 mg/kg (2 times the RHD on a mg/m2 basis) or greater, and teratogenic effects (primarily rib and vertebral malformations) were observed at 120 mg/kg (6 times the RHD on a mg/m2 basis). Evidence of maternal toxicity (decreased body weight gain, clinical signs, and/or mortality) was seen at 35 mg/kg and above.
When female rats were treated during the latter part of gestation and throughout lactation (0.2, 4, 20, and 100 mg/kg or 2, 20, and 200 mg/kg), offspring exhibited decreased viability and delayed physical development at 200 mg/kg (5 times the RHD on a mg/m2 basis) and reductions in pre- and/or postweaning body weight gain at 2 mg/kg (0.05 times the RHD on a mg/m2 basis) and above. Maternal toxicity (decreased body weight gain, clinical signs) was evident at 100 mg/kg or greater.
In a rat embryo/fetal development study with a postnatal component (0.2, 2.5, 30, or 400 mg/kg during organogenesis; noted above), pups exhibited delayed physical development at 400 mg/kg (10 times the RHD on a mg/m2 basis) and persistent reductions in body weight gain at 30 mg/kg (1 times the RHD on a mg/m2 basis) and higher.
There are no studies using topiramate in pregnant women. Topiramate should be used during pregnancy only if the potential benefit outweighs the potential risk to the fetus.
In post-marketing experience, cases of hypospadias have been reported in male infants exposed in utero to topiramate, with or without other anticonvulsants; however, a causal relationship with topiramate has not been established.
To provide information regarding the effects of in utero exposure to topiramate tablets, physicians are advised to recommend that pregnant patients taking topiramate tablets enroll in the NAAED Pregnancy Registry. This can be done by calling the toll free number, 1-888-233-2334, and must be done by patients themselves. Information on the registry can also be found at the website http://www.aedpregnancyregistry.org/.
Labor and Delivery:
In studies of rats where dams were allowed to deliver pups naturally, no drug-related effects on gestation length or parturition were observed at dosage levels up to 200 mg/kg/day.
The effect of topiramate on labor and delivery in humans is unknown.
Nursing Mothers:
Topiramate is excreted in the milk of lactating rats. The excretion of topiramate in human milk has not been evaluated in controlled studies. Limited observations in patients suggest an extensive secretion of topiramate into breast milk. Since many drugs are excreted in human milk, and because the potential for serious adverse reactions in nursing infants to topiramate is unknown, the potential benefit to the mother should be weighed against the potential risk to the infant when considering recommendations regarding nursing.
Pediatric Use:
Safety and effectiveness in patients below the age of 2 years have not been established for the adjunctive therapy treatment of partial onset seizures, primary generalized tonic-clonic seizures, or seizures associated with Lennox-Gastaut syndrome. Safety and effectiveness in patients below the age of 10 years have not been established for the monotherapy treatment of epilepsy. Topiramate is associated with metabolic acidosis. Chronic untreated metabolic acidosis in pediatric patients may cause osteomalacia/rickets and may reduce growth rates. A reduction in growth rate may eventually decrease the maximal height achieved. The effect of topiramate on growth and bone-related sequelae has not been systematically investigated (see WARNINGS).
Geriatric Use:
In clinical trials, 3% of patients were over 60. No age related difference in effectiveness or adverse effects were evident. However, clinical studies of topiramate did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently than younger subjects. Dosage adjustment may be necessary for elderly with impaired renal function (creatinine clearance rate ≤70 mL/min/1.73 m2) due to reduced clearance of topiramate (see CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
-
ADVERSE REACTIONS
The data described in the following section were obtained using topiramate tablets.
Monotherapy Epilepsy
The adverse events in the controlled trial that occurred most commonly in adults in the 400 mg/day group and at a rate higher than the 50 mg/day group were: paresthesia, weight decrease, somnolence, anorexia, dizziness, and difficulty with memory NOS [see Table 5].
The adverse events in the controlled trial that occurred most commonly in children (10 years up to 16 years of age) in the 400 mg/day group and at a rate higher than the 50 mg/day group were: weight decrease, upper respiratory tract infection, paresthesia, anorexia, diarrhea, and mood problems [see Table 6].
Approximately 21% of the 159 adult patients in the 400 mg/day group who received topiramate as monotherapy in the controlled clinical trial discontinued therapy due to adverse events. Adverse events associated with discontinuing therapy (≥2%) included depression, insomnia, difficulty with memory (NOS), somnolence, paresthesia, psychomotor slowing, dizziness, and nausea.
Approximately 12% of the 57 pediatric patients in the 400 mg/day group who received topiramate as monotherapy in the controlled clinical trial discontinued therapy due to adverse events. Adverse events associated with discontinuing therapy (≥5%) included difficulty with concentration/attention.
The prescriber should be aware that these data cannot be used to predict the frequency of adverse events in the course of usual medical practice where patient characteristics and other factors may differ from those prevailing during the clinical study. Similarly, the cited frequencies cannot be directly compared with data obtained from other clinical investigations involving different treatments, uses, or investigators. Inspection of these frequencies, however, does provide the prescribing physician with a basis to estimate the relative contribution of drug and non-drug factors to the adverse event incidences in the population studied.
Table 5: Incidence of Treatment-Emergent Adverse Events in the Monotherapy Epilepsy Trial in Adultsa Where Rate Was at Least 2% in the 400 mg/day Topiramate Group and Greater Than the Rate in the 50 mg/day Topiramate Group Topiramate Dosage (mg/day) Body System/
Adverse Event50
(N= 160)400
(N=159)a Values represent the percentage of patients reporting a given adverse event. Patients may have reported more than one adverse event during the study and can be included in more than one adverse event category.
Body as a Whole-General Disorders Asthenia 4 6 Leg Pain 2 3 Chest Pain 1 2 Central & Peripheral Nervous System Disorders Paresthesia 21 40 Dizziness 13 14 Hypoaesthesia 4 5 Ataxia 3 4 Hypertonia 0 3 Gastro-Intestinal System Disorders Diarrhea 5 6 Constipation 1 4 Gastritis 0 3 Dry Mouth 1 3 Gastroesophageal Reflux 1 2 Liver and Biliary System Disorders Gamma-GT Increased 1 3 Metabolic and Nutritional Disorders Weight Decrease 6 16 Psychiatric Disorders Somnolence 9 15 Anorexia 4 14 Difficulty with Memory NOS 5 10 Insomnia 8 9 Depression 7 9 Difficulty with Concentration/Attention 7 8 Anxiety 4 6 Psychomotor Slowing 3 5 Mood Problems 2 5 Confusion 3 4 Cognitive Problem NOS 1 4 Libido Decreased 0 3 Reproductive Disorders, Female Vaginal Hemorrhage 0 3 Red Blood Cell Disorders Anemia 1 2 Resistance Mechanism Disorders Infection Viral 6 8 Infection 2 3 Respiratory System Disorders Bronchitis 3 4 Rhinitis 2 4 Dyspnea 1 2 Skin and Appendages Disorders Rash 1 4 Pruritus 1 4 Acne 2 3 Special Senses Other, Disorders Taste Perversion 3 5 Urinary System Disorders Cystitis 1 3 Renal Calculus 0 3 Urinary Tract Infection 1 2 Dysuria 0 2 Micturition Frequency 0 2 Table 6: Incidence of Treatment-Emergent Adverse Events in the Monotherapy Epilepsy Trial in Children Ages 10 up to 16 Yearsa Where Rate Was at Least 5% in the 400 mg/day Topiramate Group and Greater Than the Rate in the 50 mg/day Topiramate Group Topiramate Dosage (mg/day) Body System/
Adverse Event50
(N=57)400
(N=57)a Values represent the percentage of patients reporting a given adverse event. Patients may have reported more than one adverse event during the study and can be included in more than one adverse event category.
Body as a Whole-General Disorders Fever 0 9 Central & Peripheral Nervous System Disorders Paresthesia 2 16 Gastro-Intestinal System Disorders Diarrhea 5 11 Metabolic and Nutritional Disorders Weight Decrease 7 21 Psychiatric Disorders Anorexia 11 14 Mood Problems 2 11 Difficulty with Concentration/Attention 4 9 Cognitive Problems NOS 0 7 Nervousness 4 5 Resistance Mechanism Disorders Infection Viral 4 9 Infection 2 7 Respiratory System Disorders Upper Respiratory Tract Infection 16 18 Rhinitis 2 7 Bronchitis 2 7 Sinusitis 2 5 Skin and Appendages Disorders Alopecia 2 5 Adjunctive Therapy Epilepsy
The most commonly observed adverse events associated with the use of topiramate at dosages of 200 to 400 mg/day in controlled trials in adults with partial onset seizures, primary generalized tonic-clonic seizures, or Lennox-Gastaut syndrome, that were seen at greater frequency in topiramate-treated patients and did not appear to be dose-related were: somnolence, dizziness, ataxia, speech disorders and related speech problems, psychomotor slowing, abnormal vision, difficulty with memory, paresthesia and diplopia [see Table 7]. The most common dose-related adverse events at dosages of 200 to 1,000 mg/day were: fatigue, nervousness, difficulty with concentration or attention, confusion, depression, anorexia, language problems, anxiety, mood problems, and weight decrease [see Table 9].
Adverse events associated with the use of topiramate at dosages of 5 to 9 mg/kg/day in controlled trials in pediatric patients with partial onset seizures, primary generalized tonic-clonic seizures, or Lennox-Gastaut syndrome, that were seen at greater frequency in topiramate-treated patients were: fatigue, somnolence, anorexia, nervousness, difficulty with concentration/attention, difficulty with memory, aggressive reaction, and weight decrease [see Table 10].
In controlled clinical trials in adults, 11% of patients receiving topiramate 200 to 400 mg/day as adjunctive therapy discontinued due to adverse events. This rate appeared to increase at dosages above 400 mg/day. Adverse events associated with discontinuing therapy included somnolence, dizziness, anxiety, difficulty with concentration or attention, fatigue, and paresthesia and increased at dosages above 400 mg/day. None of the pediatric patients who received topiramate adjunctive therapy at 5 to 9 mg/kg/day in controlled clinical trials discontinued due to adverse events.
Approximately 28% of the 1,757 adults with epilepsy who received topiramate at dosages of 200 to 1,600 mg/day in clinical studies discontinued treatment because of adverse events; an individual patient could have reported more than one adverse event. These adverse events were: psychomotor slowing (4%), difficulty with memory (3.2%), fatigue (3.2%), confusion (3.1%), somnolence (3.2%), difficulty with concentration/attention (2.9%), anorexia (2.7%), depression (2.6%), dizziness (2.5%), weight decrease (2.5%), nervousness (2.3%), ataxia (2.1%), and paresthesia (2%). Approximately 11% of the 310 pediatric patients who received topiramate at dosages up to 30 mg/kg/day discontinued due to adverse events. Adverse events associated with discontinuing therapy included aggravated convulsions (2.3%), difficulty with concentration/attention (1.6%), language problems (1.3%), personality disorder (1.3%), and somnolence (1.3%).
Incidence in Epilepsy Controlled Clinical Trials - Adjunctive Therapy – Partial Onset Seizures, Primary Generalized Tonic-Clonic Seizures, and Lennox-Gastaut Syndrome
Table 7 lists treatment-emergent adverse events that occurred in at least 1% of adults treated with 200 to 400 mg/day topiramate in controlled trials that were numerically more common at this dose than in the patients treated with placebo. In general, most patients who experienced adverse events during the first eight weeks of these trials no longer experienced them by their last visit. Table 10 lists treatment-emergent adverse events that occurred in at least 1% of pediatric patients treated with 5 to 9 mg/kg topiramate in controlled trials that were numerically more common than in patients treated with placebo.
The prescriber should be aware that these data were obtained when topiramate was added to concurrent antiepileptic drug therapy and cannot be used to predict the frequency of adverse events in the course of usual medical practice where patient characteristics and other factors may differ from those prevailing during clinical studies. Similarly, the cited frequencies cannot be directly compared with data obtained from other clinical investigations involving different treatments, uses, or investigators. Inspection of these frequencies, however, does provide the prescribing physician with a basis to estimate the relative contribution of drug and non-drug factors to the adverse event incidences in the population studied.
Other Adverse Events Observed During Double-Blind Epilepsy Adjunctive Therapy Trials
Other events that occurred in more than 1% of adults treated with 200 to 400 mg of topiramate in placebo-controlled epilepsy trials but with equal or greater frequency in the placebo group were: headache, injury, anxiety, rash, pain, convulsions aggravated, coughing, fever, diarrhea, vomiting, muscle weakness, insomnia, personality disorder, dysmenorrhea, upper respiratory tract infection, and eye pain.
Table 7: Incidence of Treatment-Emergent Adverse Events in Placebo-Controlled, Add-On Epilepsy Trials in Adultsa,b Where Rate Was > 1% in Any Topiramate Group and Greater Than the Rate in Placebo-Treated Patients Topiramate Dosage (mg/day) Body System/
Adverse EventcPlacebo
(N=291)200 to 400
(N=183)600 to 1,000
(N=414)a Patients in these add-on trials were receiving 1 to 2 concomitant antiepileptic drugs in addition to topiramate or placebo.
b Values represent the percentage of patients reporting a given adverse event. Patients may have reported more than one adverse event during the study and can be included in more than one adverse event category.
c Adverse events reported by at least 1% of patients in the topiramate 200 to 400 mg/day group and more common than in the placebo group are listed in this table.
Body as a Whole-General Disorders Fatigue 13 15 30 Asthenia 1 6 3 Back Pain 4 5 3 Chest Pain 3 4 2 Influenza-Like Symptoms 2 3 4 Leg Pain 2 2 4 Hot Flushes 1 2 1 Allergy 1 2 3 Edema 1 2 1 Body Odor 0 1 0 Rigors 0 1 <1 Central & Peripheral Nervous System Disorders Dizziness 15 25 32 Ataxia 7 16 14 Speech Disorders/Related Speech Problems 2 13 11 Paresthesia 4 11 19 Nystagmus 7 10 11 Tremor 6 9 9 Language Problems 1 6 10 Coordination Abnormal 2 4 4 Hypoaesthesia 1 2 1 Gait Abnormal 1 3 2 Muscle Contractions Involuntary 1 2 2 Stupor 0 2 1 Vertigo 1 1 2 Gastro-Intestinal System Disorders Nausea 8 10 12 Dyspepsia 6 7 6 Abdominal Pain 4 6 7 Constipation 2 4 3 Gastroenteritis 1 2 1 Dry Mouth 1 2 4 Gingivitis <1 1 1 GI Disorder <1 1 0 Hearing and Vestibular Disorders Hearing Decreased 1 2 1 Metabolic and Nutritional Disorders Weight Decrease 3 9 13 Muscle-Skeletal System Disorders Myalgia 1 2 2 Skeletal Pain 0 1 0 Platelet, Bleeding, & Clotting Disorders Epistaxis 1 2 1 Psychiatric Disorders Somnolence 12 29 28 Nervousness 6 16 19 Psychomotor Slowing 2 13 21 Difficulty with Memory 3 12 14 Anorexia 4 10 12 Confusion 5 11 14 Depression 5 5 13 Difficulty with Concentration/Attention 2 6 14 Mood Problems 2 4 9 Agitation 2 3 3 Aggressive Reaction 2 3 3 Emotional Lability 1 3 3 Cognitive Problems 1 3 3 Libido Decreased 1 2 <1 Apathy 1 1 3 Depersonalization 1 1 2 Reproductive Disorders, Female Breast Pain 2 4 0 Amenorrhea 1 2 2 Menorrhagia 0 2 1 Menstrual Disorder 1 2 1 Reproductive Disorders, Male Prostatic Disorder <1 2 0 Resistance Mechanism Disorders Infection 1 2 1 Infection Viral 1 2 <1 Moniliasis <1 1 0 Respiratory System Disorders Pharyngitis 2 6 3 Rhinitis 6 7 6 Sinusitis 4 5 6 Dyspnea 1 1 2 Skin and Appendages Disorders Skin Disorder <1 2 1 Sweating Increased <1 1 <1 Rash Erythematous <1 1 <1 Special Sense Other, Disorders Taste Perversion 0 2 4 Urinary System Disorders Hematuria 1 2 <1 Urinary Tract Infection 1 2 3 Micturition Frequency 1 1 2 Urinary Incontinence <1 2 1 Urine Abnormal 0 1 <1 Vision Disorders Vision Abnormal 2 13 10 Diplopia 5 10 10 White Cell and RES Disorders Leukopenia 1 2 1 Incidence in Study 119 – Add-On Therapy– Adults with Partial Onset Seizures
Study 119 was a randomized, double-blind, placebo-controlled, parallel group study with 3 treatment arms: 1) placebo; 2) topiramate 200 mg/day with a 25 mg/day starting dose, increased by 25 mg/day each week for 8 weeks until the 200 mg/day maintenance dose was reached; and 3) topiramate 200 mg/day with a 50 mg/day starting dose, increased by 50 mg/day each week for 4 weeks until the 200 mg/day maintenance dose was reached. All patients were maintained on concomitant carbamazepine with or without another concomitant antiepileptic drug.
The incidence of adverse events (Table 8) did not differ significantly between the 2 topiramate regimens. Because the frequencies of adverse events reported in this study were markedly lower than those reported in the previous epilepsy studies, they cannot be directly compared with data obtained in other studies.
Table 8: Incidence of Treatment-Emergent Adverse Events in Study 119a,b Where Rate Was ≥ 2% in the Topiramate Group and Greater Than the Rate in Placebo-Treated Patients Topiramate Dosage (mg/day) Body System/
Adverse EventcPlacebo
(N=92)200
(N=171)a Patients in these add-on trials were receiving 1 to 2 concomitant antiepileptic drugs in addition to topiramate or placebo.
b Values represent the percentage of patients reporting a given adverse event. Patients may have reported more than one adverse event during the study and can be included in more than one adverse event category.
c Adverse events reported by at least 2% of patients in the topiramate 200 mg/day group and more common than in the placebo group are listed in this table.
Body as a Whole-General Disorders Fatigue 4 9 Chest Pain 1 2 Cardiovascular Disorders, General Hypertension 0 2 Central & Peripheral Nervous System Disorders Paresthesia 2 9 Dizziness 4 7 Tremor 2 3 Hypoasthesia 0 2 Leg Cramps 0 2 Language Problems 0 2 Gastro-Intestinal System Disorders Abdominal Pain 3 5 Constipation 0 4 Diarrhea 1 2 Dyspepsia 0 2 Dry Mouth 0 2 Hearing and Vestibular Disorders Tinnitus 0 2 Metabolic and Nutritional Disorders Weight Decrease 4 8 Psychiatric Disorders Somnolence 9 15 Anorexia 7 9 Nervousness 2 9 Difficulty with Concentration/Attention 0 5 Insomnia 3 4 Difficulty with Memory 1 2 Aggressive Reaction 0 2 Respiratory System Disorders Rhinitis 0 4 Urinary System Disorders Cystitis 0 2 Vision Disorders Diplopia 0 2 Vision Abnormal 0 2 Table 9: Incidence (%) of Dose-Related Adverse Events From Placebo-Controlled, Add-On Trials in Adults with Partial Onset Seizuresa Topiramate Dosage (mg/day)
Adverse EventPlacebo
(N = 216)200
(N = 45)400
(N = 68)600 to 1,000
(N = 414)a Dose-response studies were not conducted for other adult indications or for pediatric indications.
Fatigue 13 11 12 30 Nervousness 7 13 18 19 Difficulty with Concentration/Attention 1 7 9 14 Confusion 4 9 10 14 Depression 6 9 7 13 Anorexia 4 4 6 12 Language problems <1 2 9 10 Anxiety 6 2 3 10 Mood problems 2 0 6 9 Weight decrease 3 4 9 13 Table 10: Incidence (%) of Treatment-Emergent Adverse Events in Placebo-Controlled, Add-On Epilepsy Trials in Pediatric Patients Ages 2 to 16 Yearsa,b (Events that Occurred in at Least 1% of Topiramate-Treated Patients and Occurred More Frequently in Topiramate-Treated Than Placebo-Treated Patients) Body System/
Adverse EventPlacebo
(N=101)Topiramate
(N=98)a Patients in these add-on trials were receiving 1 to 2 concomitant antiepileptic drugs in addition to topiramate or placebo.
b Values represent the percentage of patients reporting a given adverse event. Patients may have reported more than one adverse event during the study and can be included in more than one adverse event category.
Body as a Whole - General Disorders Fatigue 5 16 Injury 13 14 Allergic Reaction 1 2 Back Pain 0 1 Pallor 0 1 Cardiovascular Disorders, General Hypertension 0 1 Central & Peripheral Nervous System Disorders Gait Abnormal 5 8 Ataxia 2 6 Hyperkinesia 4 5 Dizziness 2 4 Speech Disorders/Related Speech Problems 2 4 Hyporeflexia 0 2 Convulsions Grand Mal 0 1 Fecal Incontinence 0 1 Paresthesia 0 1 Gastro-Intestinal System Disorders Nausea 5 6 Saliva Increased 4 6 Constipation 4 5 Gastroenteritis 2 3 Dysphagia 0 1 Flatulence 0 1 Gastroesophageal Reflux 0 1 Glossitis 0 1 Gum Hyperplasia 0 1 Heart Rate and Rhythm Disorders Bradycardia 0 1 Metabolic and Nutritional Disorders Weight Decrease 1 9 Thirst 1 2 Hypoglycemia 0 1 Weight Increase 0 1 Platelet, Bleeding, & Clotting Disorders Purpura 4 8 Epistaxis 1 4 Hematoma 0 1 Prothrombin Increased 0 1 Thrombocytopenia 0 1 Psychiatric Disorders Somnolence 16 26 Anorexia 15 24 Nervousness 7 14 Personality Disorder (Behavior Problems) 9 11 Difficulty with Concentration/Attention 2 10 Aggressive Reaction 4 9 Insomnia 7 8 Difficulty with Memory NOS 0 5 Confusion 3 4 Psychomotor Slowing 2 3 Appetite Increased 0 1 Neurosis 0 1 Reproductive Disorders, Female Leukorrhoea 0 2 Resistance Mechanism Disorders Infection Viral 3 7 Respiratory System Disorders Pneumonia 1 5 Respiratory Disorder 0 1 Skin and Appendages Disorders Skin Disorder 2 3 Alopecia 1 2 Dermatitis 0 2 Hypertrichosis 1 2 Rash Erythematous 0 2 Eczema 0 1 Seborrhoea 0 1 Skin Discoloration 0 1 Urinary System Disorders Urinary Incontinence 2 4 Nocturia 0 1 Vision Disorders Eye Abnormality 1 2 Vision Abnormal 1 2 Diplopia 0 1 Lacrimation Abnormal 0 1 Myopia 0 1 White Cell and RES Disorders Leukopenia 0 2 Other Adverse Events Observed During All Epilepsy Clinical Trials
Topiramate has been administered to 2,246 adults and 427 pediatric patients with epilepsy during all clinical studies, only some of which were placebo controlled. During these studies, all adverse events were recorded by the clinical investigators using terminology of their own choosing. To provide a meaningful estimate of the proportion of individuals having adverse events, similar types of events were grouped into a smaller number of standardized categories using modified WHOART dictionary terminology. The frequencies presented represent the proportion of patients who experienced an event of the type cited on at least one occasion while receiving topiramate. Reported events are included except those already listed in the previous tables or text, those too general to be informative, and those not reasonably associated with the use of the drug.
Events are classified within body system categories and enumerated in order of decreasing frequency using the following definitions: frequent occurring in at least 1/100 patients; infrequent occurring in 1/100 to 1/1000 patients; rare occurring in fewer than 1/1000 patients.
Autonomic Nervous System Disorders: Infrequent: vasodilation.
Body as a Whole: Frequent: syncope. Infrequent: abdomen enlarged. Rare: alcohol intolerance.
Cardiovascular Disorders, General: Infrequent: hypotension, postural hypotension, angina pectoris.
Central & Peripheral Nervous System Disorders: Infrequent : neuropathy, apraxia, hyperaesthesia, dyskinesia, dysphonia, scotoma, ptosis, dystonia, visual field defect, encephalopathy, EEG abnormal. Rare: upper motor neuron lesion, cerebellar syndrome, tongue paralysis.
Gastrointestinal System Disorders: Infrequent: hemorrhoids, stomatitis, melena, gastritis, esophagitis. Rare: tongue edema.
Heart Rate and Rhythm Disorders: Infrequent: AV block.
Liver and Biliary System Disorders: Infrequent: SGPT increased, SGOT increased.
Metabolic and Nutritional Disorders: Infrequent: dehydration, hypokalemia, alkaline phosphatase increased, hypocalcemia, hyperlipemia, hyperglycemia, xerophthalmia, diabetes mellitus. Rare: hyperchloremia, hypernatremia, hyponatremia, hypocholesterolemia, hypophosphatemia, creatinine increased.
Musculoskeletal System Disorders: Frequent: arthralgia. Infrequent: arthrosis.
Neoplasms: Infrequent: thrombocythemia. Rare: polycythemia.
Platelet, Bleeding, and Clotting Disorders: Infrequent: gingival bleeding, pulmonary embolism.
Psychiatric Disorders: Frequent: impotence, hallucination, psychosis, suicide attempt. Infrequent: euphoria, paranoid reaction, delusion, paranoia, delirium, abnormal dreaming. Rare: libido increased, manic reaction.
Red Blood Cell Disorders: Frequent: anemia. Rare: marrow depression, pancytopenia.
Reproductive Disorders, Male: Infrequent: ejaculation disorder, breast discharge.
Skin and Appendages Disorders: Infrequent: urticaria, photosensitivity reaction, abnormal hair texture. Rare: chloasma.
Special Senses Other, Disorders: Infrequent: taste loss, parosmia.
Urinary System Disorders: Infrequent: urinary retention, face edema, renal pain, albuminuria, polyuria, oliguria.
Vascular (Extracardiac) Disorders: Infrequent: flushing, deep vein thrombosis, phlebitis. Rare: vasospasm.
Vision Disorders: Frequent: conjunctivitis. Infrequent: abnormal accommodation, photophobia, strabismus. Rare: mydriasis, iritis.
White Cell and Reticuloendothelial System Disorders: Infrequent: lymphadenopathy, eosinophilia, lymphopenia, granulocytopenia. Rare: lymphocytosis.
Postmarketing and Other Experience
In addition to the adverse experiences reported during clinical testing of topiramate, the following adverse experiences have been reported worldwide in patients receiving topiramate post-approval.
These adverse experiences have not been listed above and data are insufficient to support an estimate of their incidence or to establish causation. The listing is alphabetized: bullous skin reactions (including erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis), hepatic failure (including fatalities), hepatitis, maculopathy, pancreatitis, pemphigus, and renal tubular acidosis.
- DRUG ABUSE AND DEPENDENCE
-
OVERDOSAGE
Overdoses of topiramate have been reported. Signs and symptoms included convulsions, drowsiness, speech disturbance, blurred vision, diplopia, mentation impaired, lethargy, abnormal coordination, stupor, hypotension, abdominal pain, agitation, dizziness and depression. The clinical consequences were not severe in most cases, but deaths have been reported after poly-drug overdoses involving topiramate.
Topiramate overdose has resulted in severe metabolic acidosis (see WARNINGS).
A patient who ingested a dose between 96 and 110 g topiramate was admitted to hospital with coma lasting 20 to 24 hours followed by full recovery after 3 to 4 days.
In acute topiramate overdose, if the ingestion is recent, the stomach should be emptied immediately by lavage or by induction of emesis. Activated charcoal has been shown to adsorb topiramate in vitro. Treatment should be appropriately supportive. Hemodialysis is an effective means of removing topiramate from the body.
-
DOSAGE AND ADMINISTRATION
Epilepsy
In the controlled add-on trials, no correlation has been demonstrated between trough plasma concentrations of topiramate and clinical efficacy. No evidence of tolerance has been demonstrated in humans. Doses above 400 mg/day (600, 800, or 1000 mg/day) have not been shown to improve responses in dose-response studies in adults with partial onset seizures.
It is not necessary to monitor topiramate plasma concentrations to optimize topiramate therapy. On occasion, the addition of topiramate to phenytoin may require an adjustment of the dose of phenytoin to achieve optimal clinical outcome. Addition or withdrawal of phenytoin and/or carbamazepine during adjunctive therapy with topiramate may require adjustment of the dose of topiramate. Because of the bitter taste, tablets should not be broken.
Topiramate tablets can be taken without regard to meals.
Monotherapy Use
The recommended dose for topiramate monotherapy in adults and children 10 years of age and older is 400 mg/day in two divided doses. Approximately 58% of patients randomized to 400 mg/day achieved this maximal dose in the monotherapy controlled trial; the mean dose achieved in the trial was 275 mg/day. The dose should be achieved by titrating according to the following schedule:
Morning Dose Evening Dose Week 1 25 mg 25 mg Week 2 50 mg 50 mg Week 3 75 mg 75 mg Week 4 100 mg 100 mg Week 5 150 mg 150 mg Week 6 200 mg 200 mg Adjunctive Therapy Use
Adults (17 Years of Age and Over) - Partial Seizures, Primary Generalized Tonic-Clonic Seizures, or Lennox-Gastaut Syndrome
The recommended total daily dose of topiramate as adjunctive therapy in adults with partial seizures is 200 to 400 mg/day in two divided doses, and 400 mg/day in two divided doses as adjunctive treatment in adults with primary generalized tonic-clonic seizures. It is recommended that therapy be initiated at 25 to 50 mg/day followed by titration to an effective dose in increments of 25 to 50 mg/week. Titrating in increments of 25 mg/week may delay the time to reach an effective dose. Daily doses above 1,600 mg have not been studied.
In the study of primary generalized tonic-clonic seizures the initial titration rate was slower than in previous studies; the assigned dose was reached at the end of 8 weeks (see CLINICAL STUDIES, Adjunctive Therapy Controlled Trials in Patients With Primary Generalized Tonic-Clonic Seizures).
Pediatric Patients (Ages 2 to 16 Years)– Partial Seizures, Primary Generalized Tonic-Clonic Seizures, or Lennox-Gastaut Syndrome
The recommended total daily dose of topiramate as adjunctive therapy for patients with partial seizures, primary generalized tonic-clonic seizures, or seizures associated with Lennox-Gastaut syndrome is approximately 5 to 9 mg/kg/day in two divided doses. Titration should begin at 25 mg (or less, based on a range of 1 to 3 mg/kg/day) nightly for the first week. The dosage should then be increased at 1- or 2-week intervals by increments of 1 to 3 mg/kg/day (administered in two divided doses), to achieve optimal clinical response. Dose titration should be guided by clinical outcome.
In the study of primary generalized tonic-clonic seizures the initial titration rate was slower than in previous studies; the assigned dose of 6 mg/kg/day was reached at the end of 8 weeks (see CLINICAL STUDIES, Adjunctive Therapy Controlled Trials in Patients With Primary Generalized Tonic-Clonic Seizures).
Patients with Renal Impairment:
In renally impaired subjects (creatinine clearance less than 70 mL/min/1.73 m2), one half of the usual adult dose is recommended. Such patients will require a longer time to reach steady-state at each dose.
Geriatric Patients (Ages 65 Years and Over):
Dosage adjustment may be indicated in the elderly patient when impaired renal function (creatinine clearance rate ≤70 mL/min/1.73 m2) is evident (see DOSAGE AND ADMINISTRATION: Patients with Renal Impairment and CLINICAL PHARMACOLOGY: Special Populations: Age, Gender, and Race).
Patients Undergoing Hemodialysis:
Topiramate is cleared by hemodialysis at a rate that is 4 to 6 times greater than a normal individual. Accordingly, a prolonged period of dialysis may cause topiramate concentration to fall below that required to maintain an anti-seizure effect. To avoid rapid drops in topiramate plasma concentration during hemodialysis, a supplemental dose of topiramate may be required. The actual adjustment should take into account 1) the duration of dialysis period, 2) the clearance rate of the dialysis system being used, and 3) the effective renal clearance of topiramate in the patient being dialyzed.
-
HOW SUPPLIED
Topiramate tablets are available as debossed, film-coated, circular tablets in the following strengths and colors:
25 mg white (coded "S" on one side; "707" on the other)
50 mg yellow (coded "S" on one side; "710" on the other)
100 mg yellow (coded "S" on one side; "711" on the other)
200 mg brown (coded "S" on one side; "712" on the other)They are supplied as follows:
25 mg tablets Bottles of 30's with Child Resistant Cap… …………NDC: 21695-162-30
Bottles of 60's with Child Resistant Cap… …………NDC: 21695-162-60
50 mg tablets Bottles of 30's with Child Resistant Cap… ……… …NDC: 21695-205-30 Bottles of 60's with Child Resistant Cap… ……… NDC: 21695-205-60
Bottles of 90's with Child Resistant Cap… … … …NDC: 21695-205-90
100 mg tablets Bottles of 30's with Child Resistant Cap… ………… NDC: 21695-348-30
Bottles of 60's with Child Resistant Cap… …………NDC: 21695-348-60
Bottles of 90's with Child Resistant Cap… … … … NDC: 21695-348-90
200 mg tablets Bottles of 30's with Child Resistant Cap… …………NDC: 21695-349-30
Bottles of 60's with Child Resistant Cap… …………NDC: 21695-349-60
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [See USP Controlled Room Temperature]. Protect from moisture. Dispense in a tight container.
-
MEDICATION GUIDE
Topiramate Tablets
Read this Medication Guide before you start taking topiramate tablets and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment. If you have any questions about topiramate tablets, talk to your healthcare provider or pharmacist.
What is the most important information I should know about topiramate tablets?
-
Topiramate tablets may cause eye problems. Serious eye problems include:
- .
- any sudden decrease in vision with or without eye pain and redness
- a blockage of fluid in the eye causing increased pressure in the eye (secondary angle closure glaucoma).
- These eye problems can lead to permanent loss of vision if not treated. You should call your healthcare provider right away if you have any new eye symptoms.
- Topiramate tablets may cause decreased sweating and increased body temperature (fever). People, especially children, should be watched for signs of decreased sweating and fever, especially in hot temperatures. Some people may need to be hospitalized for this condition.
- Like other antiepileptic drugs, topiramate tablets may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
Do not stop topiramate tablets without first talking to a healthcare provider.
- Stopping topiramate tablets suddenly can cause serious problems.
- Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
How can I watch for early symptoms of suicidal thoughts and actions?
- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
- Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
What is topiramate tablet?
Topiramate tablet is a prescription medicine used:
- to treat certain types of seizures (partial onset seizures and primary generalized tonic-clonic seizures) in people 10 years and older
- with other medicines to treat certain types of seizures (partial onset seizures, primary generalized tonic-clonic seizures, and seizures associated with Lennox-Gastaut syndrome) in adults and children 2 years and older
What should I tell my healthcare provider before taking topiramate tablets?
Before taking topiramate tablets, tell your healthcare provider about all your medical conditions, including if you:
- have or have had depression, mood problems or suicidal thoughts or behavior
- have kidney problems, kidney stones, or are getting kidney dialysis
- have a history of metabolic acidosis (too much acid in the blood)
- have liver problems
- have osteoporosis, soft bones, or decreased bone density
- have lung or breathing problems
- have eye problems, especially glaucoma
- have diarrhea
- have a growth problem
- are on a diet high in fat and low in carbohydrates, which is called a ketogenic diet
- are having surgery
- are pregnant or plan to become pregnant. It is not known if topiramate tablets will harm your unborn baby. If you become pregnant while taking topiramate tablets, talk to your healthcare provider about registering with the North American Antiepileptic Drug Pregnancy Registry. You can enroll in this registry by calling 1-888-233-2334. The purpose of this registry is to collect information about the safety of antiepileptic medicine during pregnancy.
- are breastfeeding. It is not known if topiramate passes into breast milk and if it can harm your baby. Talk to your healthcare provider about the best way to feed your baby if you take topiramate tablets.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Topiramate tablets and other medicines may affect each other causing side effects.
Especially, tell your healthcare provider if you take:
- Valproic acid
- any medicines that impair or decrease your thinking, concentration, or muscle coordination.
- birth control pills. Topiramate tablets may make your birth control pills less effective. Tell your healthcare provider if your menstrual bleeding changes while you are taking birth control pills and topiramate tablets.
Ask you healthcare provider if you are not sure if your medicine is listed above.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist each time you get a new medicine. Do not start a new medicine without talking with your healthcare provider.
How should I take topiramate tablets?
- Take topiramate tablets exactly as prescribed.
- Your healthcare provider may change your dose. Do not change your dose without talking to your healthcare provider.
- Topiramate tablets should be swallowed whole. Do not chew the tablets. They may leave a bitter taste.
- Do not store any medicine and food mixture for later use.
- Topiramate tablets can be taken before, during, or after a meal. Drink plenty of fluids during the day. This may help prevent kidney stones while taking topiramate tablets.
- If you take too many topiramate tablets, call your healthcare provider or poison control center right away or go to the nearest emergency room.
- If you miss a single dose of topiramate tablets, take it as soon as you can. However, if you are within 6 hours of taking your next scheduled dose, wait until then to take your usual dose of topiramate tablets, and skip the missed dose. Do not double your dose. If you have missed more than one dose, you should call your healthcare professional for advice.
- Do not stop taking topiramate tablets without talking to your healthcare provider. Stopping topiramate tablets suddenly may cause serious problems. If you have epilepsy and you stop taking topiramate tablets suddenly, you may have seizures that do not stop. Your healthcare provider will tell you how to stop taking topiramate tablets slowly.
- Your healthcare provider may do blood tests while you take topiramate tablets.
What should I avoid while taking topiramate tablets?
- Do not drink alcohol while taking topiramate tablets. Topiramate tablets and alcohol can affect each other causing side effects such as sleepiness and dizziness.
- Do not drive a car or operate heavy machinery until you know how topiramate tablets affect you. Topiramate tablets can slow your thinking and motor skills.
What are the possible side effects of topiramate tablets?
Topiramate tablets may cause serious side effects including:
See “What is the most important information I should know about topiramate tablets?”
- Metabolic Acidosis. Metabolic acidosis can cause:
- .
- tiredness
- loss of appetite
- irregular heartbeat
- impaired consciousness
- High blood ammonia levels. High ammonia in the blood can affect your mental activities, slow your alertness, make you feel tired, or cause vomiting. This has happened when topiramate tablets are taken with a medicine called valproic acid.
- Kidney stones. Drink plenty of fluids when taking topiramate tablets to decrease your chances of getting kidney stones.
- Effects on Thinking and Alertness. Topiramate tablets may affect how you think, and cause confusion, problems with concentration, attention, memory, or speech. Topiramate tablets may cause depression or mood problems, tiredness, and sleepiness.
- Dizziness or Loss of Muscle Coordination.
Call your healthcare provider right away if you have any of the symptoms above.
The most common side effects of topiramate tablets include:
- tingling of the arms and legs (paresthesia)
- not feeling hungry
- nausea
- a change in the way foods taste
- diarrhea
- weight loss
- nervousness
- upper respiratory tract infection
Tell your healthcare provider about any side effect that bothers you or that does not go away.
These are not all the possible side effects of topiramate tablets. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store topiramate tablets?
- Store topiramate tablets at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F).
- Keep topiramate tablets in a tightly closed container
- Keep topiramate tablets dry and away from moisture
- Keep topiramate tablets and all medicines out of the reach of children.
General information about topiramate tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use topiramate tablet for a condition for which it was not prescribed. Do not give topiramate tablets to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about topiramate tablets. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about topiramate tablets that is written for health professionals.
For more information, call 1-800-818-4555
What are the ingredients in topiramate tablets?
Active ingredient: topiramate
Inactive ingredients: anhydrous lactose, microcrystalline cellulose, pregelatinized starch, sodium starch glycolate, magnesium stearate, purified water, polyvinyl alcohol, titanium dioxide, polyethylene glycol and talc.
In addition, individual tablets contain:
50 mg tablets: iron oxide yellow
100 mg tablets: iron oxide yellow, and D&C Yellow # 10 Aluminum Lake
200 mg tablets: iron oxide red, lecithin (soya), and iron oxide blackThis Medication Guide has been approved by the U.S. Food and Drug Administration.
Distributed by:
Caraco Pharmaceutical Laboratories, Ltd.
1150 Elijah McCoy Drive, Detroit, MI 48202Manufactured by:
Sun Pharmaceutical Industries Ltd.
Acme Plaza, Andheri-Kurla Road,
Andheri (East), Mumbai - 400 059, India.ISS. 07/2009
PGPI0101A -
Topiramate tablets may cause eye problems. Serious eye problems include:
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - Label - 25 mg
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - Label - 50 mg
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - Label - 100 mg
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - Label - 200 mg
-
INGREDIENTS AND APPEARANCE
TOPIRAMATE
topiramate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 21695-162(NDC:62756-707) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TOPIRAMATE (UNII: 0H73WJJ391) (TOPIRAMATE - UNII:0H73WJJ391) TOPIRAMATE 25 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) Product Characteristics Color white Score no score Shape ROUND (circular) Size 6mm Flavor Imprint Code S;707 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 21695-162-30 30 in 1 BOTTLE 2 NDC: 21695-162-60 60 in 1 BOTTLE 3 NDC: 21695-162-90 90 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090278 03/27/2009 TOPIRAMATE
topiramate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 21695-205(NDC:62756-710) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TOPIRAMATE (UNII: 0H73WJJ391) (TOPIRAMATE - UNII:0H73WJJ391) TOPIRAMATE 50 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color yellow Score no score Shape ROUND (circular) Size 7mm Flavor Imprint Code S;710 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 21695-205-30 30 in 1 BOTTLE 2 NDC: 21695-205-60 60 in 1 BOTTLE 3 NDC: 21695-205-90 90 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090278 03/27/2009 TOPIRAMATE
topiramate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 21695-348(NDC:62756-711) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TOPIRAMATE (UNII: 0H73WJJ391) (TOPIRAMATE - UNII:0H73WJJ391) TOPIRAMATE 100 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) Product Characteristics Color yellow Score no score Shape ROUND (circular) Size 10mm Flavor Imprint Code S;711 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 21695-348-30 30 in 1 BOTTLE 2 NDC: 21695-348-60 60 in 1 BOTTLE 3 NDC: 21695-348-90 90 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090278 03/27/2009 TOPIRAMATE
topiramate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 21695-349(NDC:62756-712) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TOPIRAMATE (UNII: 0H73WJJ391) (TOPIRAMATE - UNII:0H73WJJ391) TOPIRAMATE 200 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE RED (UNII: 1K09F3G675) LECITHIN, SOYBEAN (UNII: 1DI56QDM62) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color brown Score no score Shape ROUND (circular) Size 12mm Flavor Imprint Code S;712 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 21695-349-30 30 in 1 BOTTLE 2 NDC: 21695-349-60 60 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090278 03/27/2009 Labeler - Rebel Distributors Corp (118802834) Establishment Name Address ID/FEI Business Operations Rebel Distributors Corp 118802834 RELABEL, REPACK
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.