EVICEL FIBRIN SEALANT (HUMAN)- fibrinogen human and thrombin human kit
EVICEL Fibrin Sealant (Human) by
Drug Labeling and Warnings
EVICEL Fibrin Sealant (Human) by is a Other medication manufactured, distributed, or labeled by Ethicon Inc, Omrix Biopharmaceuticals Ltd. PFI, Omrix Biopharmaceuticals Ltd. JP. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use EVICEL® safely and effectively. See full prescribing information for EVICEL®.
EVICEL® (Fibrin Sealant [Human]) frozen solutions, for topical use only
Initial U.S. approval: 2003INDICATIONS AND USAGE
EVICEL® is a Fibrin Sealant (Human) indicated as an adjunct to hemostasis for use in patients undergoing surgery, when control of bleeding by standard surgical techniques (such as suture, ligature or cautery) is ineffective or impractical (1)
DOSAGE AND ADMINISTRATION
For Topical Use Only. Do not inject directly into the circulatory system (2, 4).
- After thawing, use the two components of EVICEL® (BAC2 and Thrombin) within 24 hours if stored at room temperature, or within 30 days if stored refrigerated (2.2).
- EVICEL® is applied onto the tissue surface using a variety of application tips and techniques. To reduce the risk of potentially life-threatening gas embolism when spraying EVICEL®, spray using only pressurized CO2 gas at the pressures and distances recommended for specific tips (2, 3).
- The amount of EVICEL® required depends upon the area of tissue to be treated and the method of application. Vials are for single use only. Discard unused contents (2.3, 16).
DOSAGE FORMS AND STRENGTHS
EVICEL® is supplied as a kit consisting of two separate packages (3):
- A package containing one vial each of BAC2 (55–85 mg/ml fibrinogen) and Thrombin (800–1200 IU/ml human thrombin) frozen solutions.
- A modular application device which includes a 6 cm yellow flexible tip. Optional accessory tips are distributed seperately.
The different EVICEL® dosage strengths include the following sizes (3):
BAC2 Vial Size Thrombin Vial Size Package Size 1.0 ml 1.0 ml 2.0 ml 2.0 ml 2.0 ml 4.0 ml 5.0 ml 5.0 ml 10.0 ml CONTRAINDICATIONS
- Do not inject directly into the circulatory system (4.1).
- Do not use in individuals known to have anaphylactic or severe systemic reaction to human blood products (4.2).
- Do not use for the treatment of severe or brisk arterial bleeding (4.3).
- Do not use EVICEL® for spraying in endoscopic or laparoscopic procedures in those instances where the minimum recommended distance from the applicator tip to the target site cannot be ensured (2.3, 4.4).
WARNINGS AND PRECAUTIONS
- Life-threatening air or gas embolism has occurred with the use of spray devices employing a pressure regulator to administer EVICEL®. This event appears to be related to the use of the spray device at pressures higher than recommended and/or at distances closer than recommended to the surface of the tissue (2.3, 5.1).
- Monitor changes in blood pressure, pulse, oxygen saturation and end-tidal CO2 when spraying EVICEL® because of the possibility of gas embolism (5.1).
- To reduce the risk of potentially life-threatening gas embolism, spray EVICEL® using only pressurized CO2 gas at the pressures and distances recommended for the specific tips.(2.3).
- Use EVICEL® spray application only if it is possible to accurately judge the spray distance, especially during endoscopic or laparoscopic procedures. (2.3, 4.4)
- Prior to applying EVICEL®, dry surface areas of the wound by standard techniques (e.g. intermittent application of compresses, swabs, use of suction devices). (2.3)
- Prepare and administer EVICEL® according to the instructions and with only devices recommended for this product. (2.3)
- May carry a risk of transmitting infectious agents e.g., viruses, the variant Creutzfeldt-Jakob disease (CJD) agent and, theoretically, the classic (CJD) agent (5.2).
ADVERSE REACTIONS
The most common adverse reactions reported in clinical trials are peripheral edema, abdominal abscess, infection, hematoma, incision site hemorrhage, vascular graft occlusion, postoperative wound complication and decreased hemoglobin (6.1).
The most common additional adverse reactions reported in postmarketing experience are, pyrexia, seroma, cardiac arrest, tachycardia, pulmonary embolism, dyspnea, and urticaria (6.2).
To report SUSPECTED ADVERSE REACTIONS, contact ETHICON Customer Support Center at (877) 384-4266 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 5/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Thawing
2.2 Preparation Prior to Application
2.3 Application Techniques
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Application Precautions
5.2 Infection Risk from Human Plasma
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
For topical use only. Do not inject.
2.1 Thawing
Thaw the two components of EVICEL® (BAC2 and Thrombin) in one of the following ways:
- 2°C to 8°C (refrigerator): vials thaw within 1 day; or
- 20°C to 25°C (room temperature): vials thaw within 1 hour; or
- 37°C (warm water bath): vials thaw within 10 minutes and must not be left at this temperature for longer than 10 minutes. The temperature must not exceed 37°C.
2.2 Preparation Prior to Application
Once thawed, use the components of EVICEL® (BAC2 and Thrombin) within 30 days if refrigerated or within 24 hours if stored at room temperature.
Do not use after the expiration date stated on the box, or after 30 days if refrigerated after thawing. Do not re-freeze EVICEL® once it has been thawed. Do not refrigerate EVICEL® after storage at room temperature. Discard unused product after 24 hours at room temperature.
Discard if the packaging of EVICEL® is damaged.
While maintaining a sterile surgical field, prepare the product assembly as follows:
- Draw the BAC2 and Thrombin into the application device (see diagram enclosed in the application device package).
- Fill both syringes of the application device with equal volumes. The solutions should not contain air bubbles.
- Carefully remove the vial assembly by rotating it in the direction indicated by the arrows to avoid leakage.
Prior to applying EVICEL®, dry surface areas of the wound by standard techniques (e.g. intermittent application of compresses, swabs, use of suction devices) [see Dosage and Administration (2.3)]. EVICEL®, the application device and accessory tips should only be used by persons trained in laparoscopic, laparoscopic-assisted, endoscopic or open surgical procedures.
Prepare and administer EVICEL® according to the instructions and with only devices recommended for this product.
2.3 Application Techniques
For topical use only. Apply EVICEL® to the surface of bleeding tissue only. Do not inject directly into the circulatory system or into tissues.
If the hemostatic effect is not complete, apply a second layer. The amount of EVICEL® required depends upon the area of tissue to be treated and the method of application. As an approximate guide, if a layer of 1 mm thickness is produced by spraying EVICEL®, the surface areas that can be covered by each of the kit sizes are given in Table 1.
Table 1: Area of Coverage of Each Kit Size BAC2 Vial Size Thrombin Vial Size Package Size Area of Coverage with Layer of 1 mm Thickness 1.0 ml 1.0 ml 2.0 ml 20 cm2 2.0 ml 2.0 ml 4.0 ml 40 cm2 5.0 ml 5.0 ml 10.0 ml 100 cm2 Use standard surgical techniques for hemorrhagic control, including suture, ligature and cautery prior to the application of EVICEL®. Remove excess blood from the site of application to the extent possible using standard techniques (e.g. intermittent application of compresses, swabs, use of suction devices). Apply EVICEL® with the approved application device and accessories supplied. EVICEL® forms a transparent layer on application through which specific bleeding points may be observed; these bleeding points may be sutured or electrocauterized through the layer of EVICEL®.
Vials are for single use only. Discard unused contents [see How supplied/ Storage and Handling (16)].
Application Instructions with the EVICEL® Application Device
Application by 4 cm Control Tip by Drip Method
- Grasp and bend tip to desired position. Tip will retain its shape.
- Keep the tip of the applicator as close as possible to the tissue surface without touching the tissue during application.
- Apply product to the surface area to be treated. As soon as product is applied, pull back the tip from the treated surface immediately.
- Control the coverage area by varying applied force on the plunger and tip distance from the tissue.
- If tip becomes clogged during use, wipe off or remove any visible clot at the end of the tip using sterile gauze. Do not trim the tip, which would expose the internal wire.
Application by CO2 Assisted Tips 6 cm, 35 cm and 45 cm Tips by Spray or Drip Methods
Apply by drip method, or spray method in short bursts (0.1-0.2 ml), onto the tissue to produce an even layer.
Drip Method
- Keep the tip of the applicator as close to the tissue surface as possible without touching the tissue during application.
- Apply individual drops to the surface area to be treated.
- Allow the drops to separate from each other and from the tip of the applicator. If the 6 cm or 45 cm catheter tip becomes blocked, wipe the tip clean or cut it back in 0.5 cm increments.
- Do not trim the 35 cm tip. If the tip should become clogged, wipe the tip clean with sterile gauze.
Spray Method (must only be used with CO2 as the gas); apply in short bursts (0.1-0.2 ml), onto the tissue to produce an even layer.
To reduce the risk of life-threatening gas embolism, spray EVICEL® using pressurized CO2 only at the pressures and distances indicated for each applicator tip. Reference Table 2 below for spray and distance parameters.
- Connect the short gas tube on the application device to the luer-lock end of the long gas hose.
- Connect the luer-lock of the gas tube (with the 0.2 µm filter) to a pressure regulator capable of delivering 15-25 psi (1.0-1.7 bar) of CO2 pressure.
- Ensure that gas pressure for open or laparoscopic/endoscopic procedures and specific accessory tips is set as indicated by the device manufacturer (Table 2).
- Carefully monitor insufflation pressure in all laparoscopic/endoscopic procedures.
- Ensure that the distance between the applicator tip head and the application bed is within the ranges indicated by the device manufacturer.
Table 2: Spray Application Parameters for the 6 cm, 35 cm and 45 cm Tips Surgery Applicator Tips to be used Distance from Target Tissue Spray Pressure Open surgery 6 cm Flexible Tip 10-15 cm
(4–6 inches)20-25 psi
(1.4-1.7 bar)35 cm Rigid Tip 45 cm Flexible Tip Laparoscopic procedures 35 cm Rigid Tip 4–10 cm
(1.6 – 4 inches)15–20 psi
(1.0-1.4 bar)45 cm Flexible Tip 4-10 cm
(1.6–4 in)20-25 psi
(1.4-1.7 bar)Application by Airless Spray Accessories
(Airless Spray Accessory and Laparoscopic Airless Spray Accessory 35 cm Rigid)
When using Airless Spray Accessories in either open or laparoscopic procedures, the need for connection to an external CO2 or other gas source has been eliminated.
- Once the Airless Spray Accessory and Laparoscopic Airless Spray Accessory (35 cm Rigid) is firmly attached, do not depress plungers to prime device until intended use because the two biologic components will pre-mix in the spray tip, forming a fibrin clot that prevents dispensing.
- Position the tip at least 2 cm away from the target tissue. Apply firm even pressure to the plunger to spray the fibrin sealant. Increase distance accordingly to achieve desired coverage of the target area.
- Following any pause in expression, replace the spray tip. Do not try and clear the fibrin clot within the tip by depressing the plunger otherwise the application device may become unusable.
- EVICEL™ Laparoscopic Airless Spray Accessory (35 cm Rigid) can be used for spraying as assembled.
- EVICEL™ Laparoscopic Airless Spray Accessory (35 cm Rigid) can be used for dripping. Remove the spray tip portion of the accessory and keep the tip of the applicator as close to the tissue surface as possible without touching the tissue during application. Apply individual drops to the surface area to be treated. Allow the drops to separate from each other and from the tip of the applicator.
For tip change instructions, refer to the assembly guide included with the Airless Spray Accessory or Laparoscopic Airless Spray Accessory (35 cm Rigid).
For all accessories, always reference the assembly guides enclosed in the application device and accessory packages.
-
3 DOSAGE FORMS AND STRENGTHS
EVICEL® is supplied as a kit consisting of two separate packages:
- A package containing one vial each of BAC2 (55–85 mg/ml fibrinogen) and Thrombin (800–1200 IU/ml human thrombin) frozen solutions.
- A modular application device which includes a 6 cm flexible yellow tip. Optional accessory tips are distributed separately.
The different EVICEL® dosage strengths include the following sizes (Table 3):
Table 3: EVICEL® package sizes BAC2 Vial Size Thrombin Vial Size Package Size 1.0 ml 1.0 ml 2.0 ml 2.0 ml 2.0 ml 4.0 ml 5.0 ml 5.0 ml 10.0 ml -
4 CONTRAINDICATIONS
Do not use EVICEL®:
- Directly into the circulatory system. Intravascular application of EVICEL® may result in life-threatening thromboembolic events [see Warnings and Precautions, (5.1) and Adverse Reactions, (6.2)].
- In individuals known to have anaphylactic or severe systemic reaction to human blood products [see Adverse Reactions (6.2)].
- For brisk arterial bleeding.
- For spraying in endoscopic or laparoscopic procedures in those instances where the minimum recommended distance from the applicator tip to the target site cannot be ensured. [see Dosage and Administration (2.3)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Application Precautions
Excessive product application thickness may negatively interfere with the product's efficacy and the wound healing process. Apply EVICEL® as a thin layer.
To reduce the risk of potentially life threatening air embolism, follow specific spray instructions for the pressure and distance from tissue recommended for each type of surgical procedure and length of application tip [see Dosage and Administration (2.2)].
- Spray EVICEL® using pressurized CO2 gas only.
- When using the Airless Spray Accessory and Laparoscopic Airless Spray Accessory (35 cm Rigid), the need for connection to an external CO2 or other gas source has been eliminated.
- Use EVICEL® spray application only if it is possible to accurately judge the distance from the spray tip to the tissue surface, especially during laparoscopic or endoscopic procedures.
- Monitor changes in blood pressure, pulse, oxygen saturation and end-tidal CO2 when spraying EVICEL® because of the possibility of gas embolism.
Prior to applying EVICEL®, dry surface areas of the wound by standard techniques (e.g. intermittent application of compresses, swabs, use of suction devices).
5.2 Infection Risk from Human Plasma
EVICEL® is made from human plasma and may carry a risk of transmitting infectious agents, e.g. viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent, and, theoretically, the Creutzfeldt-Jakob (CJD) agent. There is also the possibility that unknown infectious agents may be present in such products.
All infections thought by a physician to have been possibly transmitted by this product should be reported by the physician or other healthcare provider to ETHICON Customer Support Center at (877) 384-4266. The physician should discuss the risks and benefits of this product with the patient.
-
6 ADVERSE REACTIONS
The most common adverse reactions (0.5% of subjects) reported in clinical trials are peripheral edema, abdominal abscess, infection, hematoma, incision site hemorrhage, vascular graft occlusion, postoperative wound complication and decreased hemoglobin (6.1).
The most common additional adverse reactions reported in postmarketing experience are, pyrexia, seroma, cardiac arrest, tachycardia, pulmonary embolism, dyspnea, and urticaria (6.2).
6.1 Clinical Trials Experience
Clinical trials are conducted under widely varying conditions; therefore adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Vascular Surgery
In a controlled study involving 147 subjects undergoing vascular grafting procedures (75 treated with EVICEL® and 72 controls), nine subjects experienced 12 adverse reactions including graft or staphylococcal infection, hematoma, incision site hemorrhage, peripheral edema and decreased hemoglobin.
Retroperitoneal or Intra-Abdominal Surgery
Among 135 subjects undergoing retroperitoneal and intra-abdominal surgery (67 subjects treated with EVICEL® and 68 controls), one subject experienced an abdominal abscess in the EVICEL® group. In the control group, one subject experienced an abdominal abscess and one subject experienced a pelvic abscess.
Liver Surgery
In a controlled study involving 121 subjects undergoing liver surgery (58 treated with EVICEL® and 63 controls), no adverse reactions were observed.
Table 4 provides the adverse reactions of EVICEL® from three clinical trials. A total of 200 subjects were exposed to EVICEL® from these studies.
Table 4: Frequency of Adverse Reactions from Clinical Trials System organ class Adverse Reactions EVICEL
N=200GENERAL DISORDERS AND ADMINISTRATION SITE CONDITIONS Total 1 PERIPHERAL EDEMA 1 INFECTIONS AND INFESTATIONS Total 4 ABDOMINAL ABSCESS 1 GRAFT INFECTION 2 STAPHYLOCOCCAL INFECTION 1 INJURY, POISONING AND PROCEDURAL COMPLICATIONS Total 6 INCISION SITE HEMORRHAGE 1 INCISION SITE HEMATOMA 1 POST PROCEDURAL HEMATOMA 1 POSTOPERATIVE WOUND COMPLICATION 1 VASCULAR GRAFT OCCLUSION 1 POSTOPERATIVE WOUND INFECTION 1 INVESTIGATIONS Total 1 DECREASED HEMOGLOBIN 1 VASCULAR DISORDERS Total 1 HEMATOMA 1 6.2 Postmarketing Experience
The following adverse reactions are reported voluntarily from a population of uncertain size, therefore, it is not always possible to reliably estimate the frequency or establish a causal relationship to drug exposure.
Postmarketing fatalities attributable to air or gas embolism have been reported with the use of EVICEL® when applied using a spray device. These cases have occurred where EVICEL® was sprayed at a pressure higher than indicated for the device in use and when the spray tip was placed closer than the specified distance from the target site.
The following adverse reactions have been reported in postmarketing experience with EVICEL® in order of decreasing frequency (Table 5):
Table 5: Adverse Reactions Postmarketing Experience MedDRA System Organ Class Adverse Reactions GENERAL DISORDERS AND ADMINISTRATION SITE CONDITIONS PYREXIA INJURY, POISONING AND PROCEDURAL COMPLICATIONS SEROMA CARDIAC DISORDERS CARDIAC ARREST TACHYCARDIA RESPIRATORY, THORACIC AND MEDIASTINAL DISORDERS PULMONARY EMBOLISM DYSPNEA SKIN AND SUBCUTANEOUS TISSUE DISORDERS URTICARIA -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no data with EVICEL® use in pregnant women to inform a drug-associated risk. Animal reproduction studies have not been conducted with EVICEL®. It is not known whether EVICEL® can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. EVICEL® should be applied to a pregnant woman only if clearly needed.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
8.2 Lactation
Risk Summary
There is no information regarding the presence of any component of EVICEL® in human milk, the effect on the breastfed infant, and the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for EVICEL® and any potential adverse effects on the breastfed infant from EVICEL® or from the underlying maternal condition.
8.4 Pediatric Use
Limited data are available to support the safety and effectiveness of EVICEL® in children. No data is currently available for ages 0 to 6 months.
Of 135 subjects undergoing retroperitoneal and intra-abdominal surgery who were included in a controlled study of EVICEL®, four subjects treated with EVICEL® were age 16 years or younger. Of these, two were children age 2 to 11 years and two were adolescents age 12 to 16 years.
Pediatric patients for vascular surgery are rare and were therefore not included in the clinical trials involving vascular surgery.
Of the 155 subjects undergoing liver surgery who were treated in clinical trials, eight were pediatric subjects. Of these, five were less than 2 years old and three were between 2 and 12 years old.
Use of EVICEL® in pediatric patients above age 6 months is supported by these data and by extrapolation of efficacy in adults. Data can not be extrapolated to ages 0 to 6 months.
8.5 Geriatric Use
Clinical trials included 101 subjects age 65 years or older, of whom 30 underwent retroperitoneal or intra-abdominal surgery, 24 underwent liver surgery and 47 underwent vascular surgery.
No differences in safety or effectiveness were observed between the elderly and younger subjects.
-
11 DESCRIPTION
EVICEL® is manufactured from pooled human plasma. EVICEL® is provided as a single use kit consisting of two packages. One package contains one vial of Biological Active Component 2 (BAC2) and one vial of Thrombin. The second package contains a sterile spray application device.
The BAC2 and Thrombin components appear as white to slightly yellowish opaque masses when frozen and as clear to slightly opalescent and colorless to slightly yellowish solutions when thawed. The components contain no preservatives.
BAC2
BAC2 is a sterile solution, pH 6.7–7.2, which consists of concentrated human fibrinogen plus excipients. Fibrinogen is a protein from human blood that forms a clot when combined with thrombin. The composition of the BAC2 solution is as follows:
Active ingredient: Concentrate of human fibrinogen (55–85 mg/ml)
Other Ingredients: Arginine hydrochloride, glycine, sodium chloride, sodium citrate, calcium chloride, water for injection (WFI)
Thrombin
Thrombin is a sterile solution, pH 6.8–7.2, which contains purified human thrombin that activates clotting of the final combined product. Thrombin is a specific protease that transforms the fibrinogen contained in BAC2 into fibrin. The composition of the Thrombin solution is as follows:
Active Ingredient: Human thrombin (800–1200 IU/ml)
Other Ingredients: Calcium chloride, human albumin, mannitol, sodium acetate, WFI
Cryoprecipitate, which is the starting material for BAC2, and cryo-poor plasma, which is the starting material for the production of Thrombin, are both made from pooled human source plasma that is obtained from US licensed plasma collection centers.
Cryoprecipitate is manufactured in-house or supplied by either Octapharma AG (manufactured by Octapharma Pharmazeutika Produktionsges.m.b.H., Oberlaaer Strasse 235, Vienna, A-1100 Austria, License No. 1646) or Grifols Therapeutics Inc. (manufactured by Kedrion 155 Duryea Road, Melville, NY 11747, License No. 1906).
Viral Clearance
Individual plasma units which are obtained for the production of EVICEL® are evaluated by FDA-licensed serological tests for hepatitis B surface antigen (HBsAg), human immunodeficiency virus (HIV) 1 & 2 antibody and hepatitis C virus (HCV) antibody as well as with FDA-licensed nucleic acid testing (NAT) methods for HCV and HIV-1.
Some viruses such as hepatitis A virus (HAV) and parvovirus B19 are particularly difficult to remove or inactivate. Parvovirus B19 most seriously affects pregnant women or immune-compromised individuals. The plasma units are tested by NAT for HAV and hepatitis B virus (HBV). All tests for HIV, HCV, HBV and HAV must be negative (non-reactive). However, since the effectiveness of these test methods in detecting low levels of viral material is still under investigation, the significance of a negative result for these viruses is unknown. NAT for parvovirus B19 is also performed, and the level of contamination is not permitted to exceed 10,000 copies/ml. This limit is applied to restrict the viral load of parvovirus B19 in the starting plasma pool.
In addition to the screening of plasma, each manufacturing pool is tested for HBsAg, HIV-1 & 2 antibody, HCV by NAT and for parvovirus B19 by NAT. Manufacturing pool testing, however, has a lower sensitivity than that of individual unit testing.
The manufacturing procedure for EVICEL® includes processing steps which are designed to reduce the risk of viral transmission. Both BAC2 and Thrombin undergo two discrete virus inactivation/removal steps, summarized in Table 6:
Table 6: Steps for the Reduction of Viral Transmission Risk Step Component BAC2 Thrombin 1 Solvent/detergent treatment (1% TnBP, 1% Triton X-100) for 4 hours at 30°C Solvent/detergent treatment (1% TnBP, 1% Triton X-100) for 6 hours at 26°C 2 Pasteurization (10 hours at 60°C) Nanofiltration BAC2 is manufactured by treatment of cryoprecipitate with aluminum hydroxide gel to adsorb the Vitamin K dependent clotting factors and it is then incubated with a solvent detergent (SD) mixture (1% TnBP, 1% Triton X-100) for 4 hours at 30°C. The SD reagents are removed by castor oil extraction and reverse phase chromatography (C-18 column) and the preparation is subsequently treated by pasteurization.
Prior to pasteurization, sucrose and glycine are added as stabilizers. The solution is heated to 60±0.5°C and maintained at that temperature for 10 hours. After pasteurization, the stabilizers used for heat treatment are removed by diafiltration and the product is concentrated by ultrafiltration. An affinity chromatography step is then used to remove plasminogen from the product, after which it is concentrated. After concentration the solution is formulated, sterile filtered and aseptically filled and frozen.
Thrombin is manufactured by chromatographic purification of prothrombin from cryo-poor plasma followed by activation with calcium chloride. The manufacturing process includes two separate steps for inactivation or removal of viruses. The first of these is treatment with a SD mixture (1% TnBP, 1% Triton X-100) for 6 hours at 26°C to inactivate lipid enveloped viruses.
The SD reagents are removed by cation exchange chromatography. Mannitol and human albumin are used to stabilize the solution, which undergoes nanofiltration for removal of both enveloped and non-enveloped viruses. After nanofiltration, the solution is formulated with calcium chloride, sterile filtered and aseptically filled and frozen.
The efficiency of the virus inactivation/removal procedures in reducing the level of a range of viruses has been assessed using viruses with a range of physico-chemical characteristics. The results of virus removal/inactivation validation studies are summarized in Table 7:
Tables 7a,b: Results of Virus Removal/Inactivation in Validation Studies
Table 7a: BAC2 Virus HIV-1 BVDV PRV EMCV HAV CPV Reduction factor (log10) SD Treatment >4.4 >4.3 >3.8 Not Done Not Done 0 Pasteurization >4.4 >5.4 6.0 3.7 >5.8 1.3 Global Reduction Factor >8.8 >9.7 >9.8 3.7 >5.8 1.3 Table 7b: Thrombin Virus HIV-1 SBV BVDV PRV EMCV HAV MVM HIV-1: Human immunodeficiency virus Type 1;
SBV: Sindbis virus;
BVDV: Bovine viral diarrhea virus;
PRV: Pseudorabies virus;
EMCV: Encephalomyocarditis virus;
HAV: Hepatitis A virus;
CPV: Canine parvovirus;
MVM: Minute virus of mouse.Reduction factor (log10) SD Treatment >5.8 >5.0 >4.6 >4.2 Not Done Not Done Not Done Nanofiltration >4.6 Not Done >5.6 >5.7 >7.4 >7.5 >6.3 Global Reduction Factor >10.4 >5.0 >10.2 >9.9 >7.4 >7.5 >6.3 -
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The fibrin sealant system initiates the last phase of physiological blood coagulation. Thrombin activates the conversion of fibrinogen into fibrin, which occurs by the splitting of fibrinogen into fibrin monomers and fibrinopeptides. The fibrin monomers polymerize and form a fibrin clot. Factor XIIIa, which is activated from Factor XIII (FXIII) by thrombin, crosslinks fibrin. Calcium ions are required for FXIII activation by thrombin.
12.2 Pharmacodynamics
Pharmacodynamic studies were not conducted.
Clinical studies demonstrating hemostasis were conducted in a total of 167 subjects undergoing vascular surgery and in a total of 135 subjects undergoing retroperitoneal and intra-abdominal surgery. Efficacy data is provided in Section 14.
12.3 Pharmacokinetics
EVICEL® is for topical use only and intravascular administration is contraindicated [see Contraindication (4.1)], therefore pharmacokinetic studies were not performed.
Studies have been conducted in rabbits to evaluate the absorption and elimination of thrombin when applied to the cut surface of the liver resulting from partial hepatectomy. Using 125I-thrombin it was shown that a slow absorption of biologically inactive peptides resulting from the breakdown of thrombin occurred, reaching a C(max) in the plasma after 6–8 hours. At the C(max), the plasma concentration represented only 1–2% of the applied dose. The systemic exposure to thrombin when it is administered directly to a hepatic wound was estimated to be approximately equivalent to that generated by minor bleeding.
Fibrin sealants are metabolized in the same way as endogenous fibrin, by fibrinolysis and phagocytosis. As wound healing progresses, increased fibrinolytic activity is induced by plasmin and decomposition of fibrin to fibrin degradation products is initiated.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
- EVICEL® has been classified as non-irritant in the Primary Cutaneous Irritation test and slightly irritant in the Ocular Irritation test.
- No toxicological effects secondary to the solvent/detergent reagents (TnBP and Triton X-100) used in the virus inactivation procedure are expected based on acute and repeat toxicity studies and since the residual levels are less than 5 µg/ml.
- Long-term animal studies have not been performed to evaluate the carcinogenic potential of EVICEL® because of the human origin of both thrombin and fibrinogen contents.
- Neither BAC2 nor Thrombin solution induces mutagenic effects in the Ames test. Studies performed in bacteria to determine mutagenicity were negative for Thrombin alone, BAC (containing fibrinogen, citrate, glycine, tranexamic acid, and arginine hydrochloride), TnBP alone, and Triton X-100 alone at all concentrations tested. All concentrations of the combination of TnBP and Triton X-100 also tested negative in assays performed to determine mammalian cell mutagenicity, chromosomal aberrations and micronuclei induction.
- The effect of EVICEL® on fertility has not been evaluated in humans.
13.2 Animal Toxicology and/or Pharmacology
- Neurotoxicity studies performed with EVICEL® confirmed that subdural administration in the rabbit was not associated with any evidence of neurotoxicity.
- Reproductive studies performed in rats with the combination of TnBP and Triton X-100 at doses up to approximately 600-fold (TnBP, 900 µg/kg/day) and 3000-fold (Triton X-100, 4500 µg/kg/day) the human dose resulted in increased post-implantation loss and an increased number of late resorptions. No embryo-fetal adverse effects were observed at doses up to 200-fold (TnBP, 300 µg/kg/day) and 1000-fold (Triton X-100, 1500 µg/kg/day) the human dose. Other studies performed with the combination of TnBP at doses approximately 300-fold (TnBP, 450 µg/kg/day) and 1500-fold (Triton X-100, 2250 µg/kg/day) the human dose had increased resorption rates, decreased fetal body weights, and an increased number of runts. No embryo-fetal adverse effects were observed at doses up to 100-fold (TnBP, 150 µg/kg/day) and 500-fold (Triton X-100, 750 µg/kg/day) the human dose.
-
14 CLINICAL STUDIES
Retroperitoneal and Intra-Abdominal Surgery
In a prospective, randomized, controlled evaluation of the hemostatic efficacy of EVICEL® as an adjunct to hemostasis for soft tissue bleeding during retroperitoneal or intra-abdominal surgery, EVICEL® was shown to be superior to the control product (oxidized regenerated cellulose) in achieving hemostasis in less than 10 minutes (Table 8). Superiority was also established at 7 and 4 minutes.
Table 8: Efficacy Results in Retroperitoneal and Intra-Abdominal Surgery Variable EVICEL®
n = 66Control
n = 69Relative Risk (RR) 95% CI for RR Hemostasis at 10 min 63 (95.5%) 56 (81.2%) 1.18 1.04; 1.36 Hemostasis ≤7 min 60 (90.9%) 53 (76.8%) 1.18 1.02; 1.40 Hemostasis ≤4 min 50 (75.8%) 37 (53.6%) 1.41 1.10; 1.86 Vascular Surgery
A prospective, randomized study was performed to compare the hemostatic efficacy of EVICEL® versus manual compression during vascular surgical procedures utilizing polytetrafluoroethylene graft material on end-to-side femoral artery anastomosis or upper extremity vascular access arterial anastomosis.
A difference (p<0.001) in time to hemostasis was observed: 83.3% of the treatment subjects as compared to 39.7% of control subjects achieved hemostasis by 4 minutes (Table 9).
Table 9: Efficacy Results in Vascular Surgery Number (%) of patients achieving hemostasis EVICEL® Manual Compression n=72 n=68 At 4 minutes 60 (83.3%) 27 (39.7%) ≤7 minutes 63 (87.5%) 42 (61.8%) ≤10 minutes 66 (91.7%) 48 (70.6%) Liver Surgery
EVICEL® was compared in a prospective, randomized, parallel-group, multi-center study to FDA-approved control topical hemostatic agents in 121 subjects undergoing liver resection at 15 centers. Subjects were randomized (stratified by surgeon) at the conclusion of the liver resection surgery if general oozing was present that could not be controlled by further surgical methods and a topical hemostatic agent was needed to control the bleeding from the liver surface. For hemostatic efficacy, the EVICEL® was shown to be statistically superior to the control hemostatic agents (5.3 minutes for EVICEL® versus 7.7 minutes for control; one-sided p=0.011).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
EVICEL® is supplied as a kit consisting of two separate packages:
- A package containing one vial each of BAC2 (55–85 mg/ml fibrinogen) and Thrombin (800–1200 IU/ml human thrombin) frozen solutions.
- A modular application device.
The different EVICEL® dosage strengths include the following sizes (Table 10):
Table 10: EVICEL® Package Sizes BAC2 Vial Size Thrombin Vial Size Package Size 1.0 ml 1.0 ml 2.0 ml 2.0 ml 2.0 ml 4.0 ml 5.0 ml 5.0 ml 10.0 ml The vials must be stored in an upright position.
Store frozen vials at -18°C or colder (frozen) for up to 2 years.
Store unopened vials at 2°C to 8°C (refrigerated) for up to 30 days.
The two EVICEL® components, BAC2 and Thrombin, have been shown to be stable for up to 24 hours at room temperature.
Do not use after the expiration date stated on the box, or after 30 days if stored at 2°C to 8°C after thawing.
Do not re-freeze EVICEL® once it has been thawed.
Do not refrigerate EVICEL® once it has reached room temperature. Discard unused product after 24 hours at room temperature.
Discard if the packaging of EVICEL® is damaged.
Vials are for single use only. Discard unused contents.
-
17 PATIENT COUNSELING INFORMATION
- Inform patient that EVICEL® is made from human plasma
- Discuss the risks and benefits with the patient of being exposed to product made from human blood and explain risk of transmitting infectious agents that may be present in such products (e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent, and, theoretically, the classic CJD agent) as indicated in Section 5.2 Infection Risk from Human Plasma.
- Instruct the patient to consult their physician if symptoms of parvovirus B19 infection (fever, drowsiness, chills, and runny nose followed about two weeks later by a rash and joint pain) occur.
- Instruct the patient to consult their physician if symptoms of hepatitis A (several days to weeks of poor appetite, fatigue, and low-grade fever followed by nausea, vomiting and abdominal pain, dark urine, yellowed complexion) appear.
-
SPL UNCLASSIFIED SECTION
Distributed by:
Ethicon, Inc.
P.O. Box 151,
Somerville, NJ 08876-0151
USAManufactured by:
Omrix Biopharmaceuticals Ltd.
MDA Blood Bank, Sheba Hospital,
Ramat-Gan
POB 888, Kiryat Ono 5510801,
ISRAELU.S. License No. 1603
Ethicon, Inc. 2017
© Omrix Biopharmaceuticals Ltd. 2014
R6200Issued: 05/2018
Article No. 80FZ00M3-7 -
PRINCIPAL DISPLAY PANEL - Two Vial Carton
EVICEL®
Fibrin Sealant (Human)This package contains one (1)
vial of frozen sterile solution of
Biological Active Component 2 (BAC2)
[1 mL] and one (1) vial of Thrombin [1 mL].
The two components are mixed and
applied topically as described in the
Dosage and Administration Section of
the Complete Prescribing Information.Rx Only
1 mL
1 mL Biological
Active Component 2
(BAC2) and Thrombin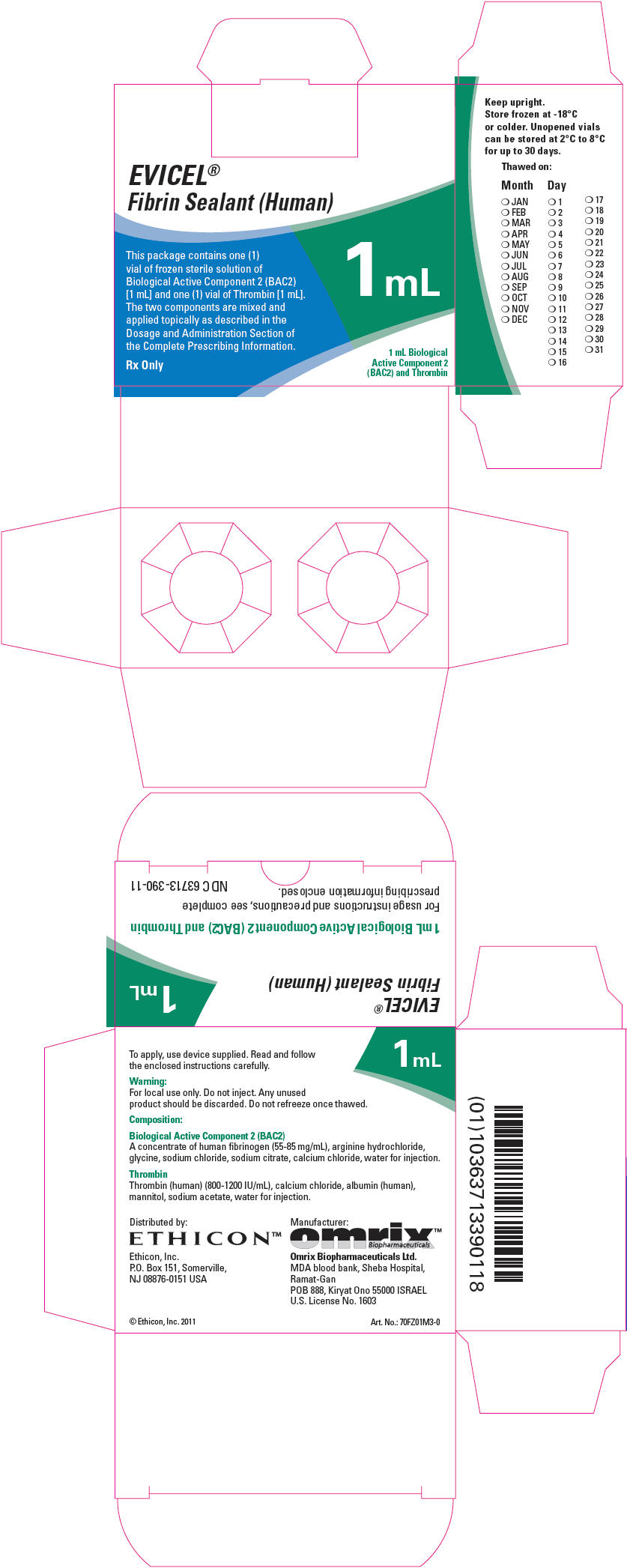
-
INGREDIENTS AND APPEARANCE
EVICEL FIBRIN SEALANT (HUMAN)
fibrinogen human and thrombin human kitProduct Information Product Type PLASMA DERIVATIVE Item Code (Source) NDC: 63713-390 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63713-390-11 1 in 1 PACKAGE, COMBINATION Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 VIAL, GLASS 1 mL Part 2 1 VIAL, GLASS 1 mL Part 1 of 2 BIOLOGICAL ACTIVE COMPONENT 2
fibrinogen human solutionProduct Information Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Fibrinogen Human (UNII: N94833051K) (Fibrinogen Human - UNII:N94833051K) Fibrinogen Human 85 mg in 1 mL Inactive Ingredients Ingredient Name Strength Arginine hydrochloride (UNII: F7LTH1E20Y) Glycine (UNII: TE7660XO1C) Sodium Citrate, Unspecified Form (UNII: 1Q73Q2JULR) Sodium chloride (UNII: 451W47IQ8X) Calcium chloride (UNII: M4I0D6VV5M) Water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 mL in 1 VIAL, GLASS; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125010 03/21/2003 Part 2 of 2 THROMBIN
thrombin solutionProduct Information Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Human Thrombin (UNII: 6K15ABL77G) (Human Thrombin - UNII:6K15ABL77G) Human Thrombin 1200 [iU] in 1 mL Inactive Ingredients Ingredient Name Strength Calcium Chloride (UNII: M4I0D6VV5M) Albumin Human (UNII: ZIF514RVZR) Mannitol (UNII: 3OWL53L36A) Sodium Acetate (UNII: 4550K0SC9B) Water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 mL in 1 VIAL, GLASS; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125010 03/21/2003 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125010 03/21/2013 Labeler - Ethicon Inc (002144145) Registrant - Omrix Biopharmaceuticals Ltd. PFI (514577949) Establishment Name Address ID/FEI Business Operations Omrix Biopharmaceuticals Ltd. PFI 514577949 API MANUFACTURE, ANALYSIS, LABEL, PACK
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.