TENOFOVIR DISOPROXIL FUMARATE tablet
TENOFOVIR DISOPROXIL FUMARATE by
Drug Labeling and Warnings
TENOFOVIR DISOPROXIL FUMARATE by is a Prescription medication manufactured, distributed, or labeled by REMEDYREPACK INC.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use TENOFOVIR DISOPROXIL FUMARATE TABLETS safely and effectively. See full prescribing information for TENOFOVIR DISOPROXIL FUMARATE TABLETS.
TENOFOVIR DISOPROXIL FUMARATE tablets, for oral use
Initial U.S. Approval Date: 2001WARNINGS: POST TREATMENT EXACERBATION OF HEPATITIS
See full prescribing information for complete boxed warning.
Severe acute exacerbations of hepatitis have been reported in HBV-infected patients who have discontinued anti-hepatitis B therapy, including tenofovir disoproxil fumarate. Hepatic function should be monitored closely in these patients. If appropriate, resumption of anti-hepatitis B therapy may be warranted. (5.1)
RECENT MAJOR CHANGES
- Indications and Usage (1.1) 12/2017
- Boxed Warning,Lactic Acidosis/Severe Hepatomegaly With Steatosis Removed 12/2017
- Warnings and Precautions, Lactic Acidosis/Severe Hepatomegaly with Steatosis (5.3) 12/2017
- Warnings and Precautions, Coadministration with Other Products (5.4) 12/2017
- Warnings and Precautions, Fat Redistribution Removed 12/2017
INDICATIONS AND USAGE
Tenofovir disoproxil fumarate is a nucleotide analog HIV-1 reverse transcriptase inhibitor and an HBV reverse transcriptase inhibitor. (1)
- Tenofovir disoproxil fumarate is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection in adults and pediatric patients 2 years of age and older. (1)
- Tenofovir disoproxil fumarate is indicated for the treatment of chronic hepatitis B in adults and pediatric patients 12 years of age and older. (1)
DOSAGE AND ADMINISTRATION
- Recommended dose for the treatment of HIV-1 or chronic hepatitis B in adults and pediatric patients 12 years of ageand older (35 kg or more): 300 mg once daily taken orally without regard to food. (2.1)
- Recommended dose for the treatment of HIV-1 in pediatric patients (2 to less than 12 years of age):
- Tablets: for pediatric patients weighing greater than or equal to 17 kg who can swallow an intact tablet, one Tenofovir disoproxil fumarate tablet (300 mg based on body weight) once daily taken orally without regard to food. (2.2)
- Dose recommended in renal impairment in adults:
- Creatinine clearance 30-49 mL/min: 300 mg every 48 hours (2.3)
- Creatinine clearance 10-29 mL/min: 300 mg every 72 to 96 hours. (2.3)
- Hemodialysis: 300 mg every 7 days or after approximately 12 hours of dialysis. (2.3)
DOSAGE FORMS AND STRENGTHS
- Tablets: 300 mg (3)
CONTRAINDICATIONS
None. (4) (4)
WARNINGS AND PRECAUTIONS
- New onset or worsening renal impairment: Can include acute renal failure and Fanconi syndrome. Assess estimated creatinine clearance before initiating treatment with Tenofovir disoproxil fumarate. In patients at risk for renal dysfunction, assess estimated creatinine clearance, serum phosphorus, urine glucose and urine protein before initiating treatment with tenofovir disoproxil fumarate and periodically during treatment. Avoid administering tenofovir disoproxil fumarate with concurrent or recent use of nephrotoxic drugs. (5.2)
- Lactic acidosis/severe hepatomegaly with steatosis: Discontinue treatment in patients who develop symptoms or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity. (5.3)
- Coadministration with Other Products: Do not use with other tenofovir-containing products (e.g., ATRIPLA, COMPLERA, DESCOVY, GENVOYA, ODEFSEY, STRIBILD, TRUVAD or VEMLIDY). Do not administer in combination with HEPSERA. (5.4)
- HIV testing: HIV antibody testing should be offered to all HBV- infected patients before initiating therapy with tenofovir disoproxil fumarate. Tenofovir disoproxil fumarate should only be used as part of an appropriate antiretroviral combination regimen in HIV-infected patients with or without HBV coinfection. (5.5)
- Decreases in bone mineral density (BMD): Consider assessment of BMD in patients with a history of pathologic fracture or other risk factors for osteoporosis or bone loss.(5.6)
- Immune reconstitution syndrome: Observed in HIV-infected patients. May necessitate further evaluation and treatment.(5.7)
- Triple nucleoside-only regimens: Early virologic failure has been reported in HIV-infected patients. Monitor carefully and consider treatment modification. (5.8)
ADVERSE REACTIONS
- In HIV-infected adult subjects: Most common adverse reactions (incidence greater than or equal to 10%, Grades 2 - 4) are rash, diarrhea, headache, pain, depression, asthenia, and nausea.(6.1)
- In HBV-infected subjects with compensated liver disease: most common adverse reaction (all grades) was nausea (9%). (6.1)
- In pediatric subjects: Adverse reactions in pediatric subjects were consistent with those observed in adults. (6.1)
- In HBV–infected subjects with decompensated liver disease: most common adverse reactions (incidence greater than or equal to 10%, all grades) were abdominal pain, nausea, insomnia, pruritus, vomiting, dizziness, and pyrexia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Strides Pharma Inc. at 1877-244-9825 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch (6)
DRUG INTERACTIONS
- Didanosine: Coadministration increases didanosine concentrations. Use with caution and monitor for evidence of didanosine toxicity (e.g., pancreatitis, neuropathy). Consider dose reductions or discontinuations of didanosine if warranted. (7.1)
- HIV-1 protease inhibitors: Coadministration decreases atazanavir concentrations and increases tenofovir concentrations. When coadministered with tenofovir disoproxil fumarate, use atazanavir given with ritonavir. Coadministration of tenofovir disoproxil fumarate with atazanavir and ritonavir, darunavir and ritonavir, or lopinavir/ritonavir increases tenofovir concentrations. Monitor for evidence of tenofovir toxicity. (7.2)
USE IN SPECIFIC POPULATIONS
Nursing mothers: Women infected with HIV should be instructed not to breast feed. (8.3) (8)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 1/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
BOXED WARNING
1 INDICATIONS AND USAGE
1.1 HIV-1 Infection
1.2 Chronic Hepatitis B
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose in Adults and Pediatric Patients 12 Years of Age and Older (35 kg or more)
2.2 Recommended Dose in Pediatric Patients 2 Years to Less than 12 Years of Age
2.3 Dose Adjustment for Renal Impairment in Adults
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Exacerbation of Hepatitis after Discontinuation of Treatment
5.2 New Onset or Worsening Renal Impairment
5.3 Lactic Acidosis/Severe Hepatomegaly with Steatosis
5.4 Coadministration with Other Products
5.5 Patients Coinfected with HIV-1 and HBV
5.6 Bone Effects
5.7 Immune Reconstitution Syndrome
5.8 Early Virologic Failure
6 ADVERSE REACTIONS
6.1 Adverse Reactions from Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Didanosine
7.2 HIV-1 Protease Inhibitors
7.3 Hepatitis C Antiviral Agents
7.4 Drugs Affecting Renal Function
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients with Impaired Renal Function
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Clinical Efficacy in Adults with HIV-1 Infection
14.2 Clinical Efficacy in Adults with Chronic Hepatitis B
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
BOXED WARNING
WARNINGS: POST TREATMENT EXACERBATION OF HEPATITIS
Severe acute exacerbations of hepatitis have been reported in HBV-infected patients who have discontinued anti-hepatitis B therapy, including tenofovir disoproxil fumarate. Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients who dis continue anti-hepatitis B therapy, including tenofovir disoproxil fumarate. If appropriate, resumption of anti-hepatitis B therapy may be warranted. [See Warnings and Precautions (5.1)].
-
1 INDICATIONS AND USAGE
1.1 HIV-1 Infection
Tenofovir disoproxil fumarate is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection in adults and pediatric patients 2 years of age and older.
The following points should be considered when initiating therapy with tenofovir disoproxil fumarate for the treatment of HIV-1 infection:
- Tenofovir disoproxil fumarate should not be used in combination with ATRIPLA®, COMPLERA ®, DESCOVY ®, GENVOYA ®, ODEFSEY ®, STRIBILD ®, TRUVAD ®or VEMLIDY ®[ See Warnings and Precautions (5.4)].
1.2 Chronic Hepatitis B
Tenofovir disoproxil fumarate is indicated for the treatment of chronic hepatitis B in adults and pediatric patients 12 years of age and older.
The following points should be considered when initiating therapy with tenofovir disoproxil fumarate for the treatment of HBV infection:
- The indication in adults is based on safety and efficacy data from treatment of subjects who were nucleoside-treatment-naïve and subjects who were treatment-experienced with documented resistance to lamivudine. Subjects were adults with HBeAg-positive and HBeAg-negative chronic hepatitis B with compensated liver disease [See Clinical Studies (14.2)].
- Tenofovir disoproxil fumarate was evaluated in a limited number of subjects with chronic hepatitis B and decompensated liver disease. [See Adverse Reactions (6.1), Clinical Studies (14.2)].
- The number of subjects in clinical trials who had adefovir resistance-associated substitutions at baseline were too small to reach conclusions of efficacy [ See Microbiology (12.4), Clinical Studies (14.2)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose in Adults and Pediatric Patients 12 Years of Age and Older (35 kg or more)
For the treatment of HIV-1 or chronic hepatitis B: The dose is one 300 mg tenofovir disoproxil fumarate tablet once daily taken orally, without regard to food.
In the treatment of chronic hepatitis B, the optimal duration of treatment is unknown. Safety and efficacy in pediatric patients with chronic hepatitis B weighing less than 35 kg have not been established.
2.2 Recommended Dose in Pediatric Patients 2 Years to Less than 12 Years of Age
HIV-1 Infection
For the treatment of HIV-1 in pediatric patients 2 years of age and older, the recommended oral dose of tenofovir disoproxil fumarate tablet is 8 mg of tenofovir disoproxil fumarate per kilogram of body weight (up to a maximum of 300 mg) once daily administered as oral tablets.
Tenofovir disoproxil fumarate is available as tablets in 300 mg strengths for pediatric patients who weigh greater than or equal to 17 kg and who are able to reliably swallow intact tablets. The dose is one tablet once daily taken orally, without regard to food.
Tables 2 contain dosing recommendations for tenofovir disoproxil fumarate tablets based on body weight. Weight should be monitored periodically and the tenofovir disoproxil fumarate dose adjusted accordingly.
Table 2 Dosing Recommendations for Pediatric Patients ≥2 Years of Age and Weighing ≥17 kg Using Tenofovir disoproxil fumarate tablets.
Body Weight Kilogram (kg)
Tablets Once Daily
≥35
300 mg
2.3 Dose Adjustment for Renal Impairment in Adults
Significantly increased drug exposures occurred when tenofovir disoproxil fumarate was administered to subjects with moderate to severe renal impairment [see Clinical Pharmacology (12.3)]. Therefore, the dosing interval of tenofovir disoproxil fumarate tablets 300 mg should be adjusted in patients with baseline creatinine clearance below 50 mL/min using the recommendations in Table 3. These dosing interval recommendations are based on modeling of single-dose pharmacokinetic data in non-HIV and non-HBV infected subjects with varying degrees of renal impairment, including end-stage renal disease requiring hemodialysis.The safety and effectiveness of these dosing interval adjustment recommendations have not been clinically evaluated in patients with moderate or severe renal impairment: therefore, clinical response to treatment and renal function should be closely monitored inthese patients [See Warnings and Precautions (5.2)]. There are no data to recommend use of Tenofovir disoproxil fumarate tablets 300 mg in patients with renal impairment.
No dose adjustment of tenofovir disoproxil fumarate tablets 300 mg is necessary for patients with mild renal impairment (creatinine clearance 50-80 mL/min). Routine monitoring of estimated creatinine clearance, serum phosphorus, urine glucose, and urine protein should be performed in patients with mild renal impairment [See Warnings and Precautions (5.2)].
Table 3 Dosage Adjustment for Patients with Altered Creatinine Clearance a Calculated using ideal (lean) body weight.
bGenerally once weekly assuming three hemodialysis sessions a week of approximately 4 hours duration. Tenofovir disoproxil fumarate should be administered following completion of dialysis.
Creatinine Clearance
(mL/min) a
Hemodialysis Patients
≥50
30–49
10–29
Recommended 300 mg
Dosing interval
Every
24
hours
Every
48
hours
Every
72 to 96
hours
Every 7 days or after a total of approximately 12 hours of dialysis b
The pharmacokinetics of tenofovir have not been evaluated in non-hemodialysis patients with creatinine clearance below 10 mL/min; therefore, no dosing recommendation is available for these patients.
No data are available to make dose recommendations in pediatric patients with renal impairment.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Exacerbation of Hepatitis after Discontinuation of Treatment
Discontinuation of anti-HBV therapy, including tenofovir disoproxil fumarate, may be associated with severe acute exacerbations of hepatitis. Patients infected with HBV who discontinue tenofovir disoproxil fumarate should be closely monitored with both clinical and laboratory follow-up for at least several months after stopping treatment. If appropriate, resumption of anti-hepatitis B therapy may be warranted
5.2 New Onset or Worsening Renal Impairment
Tenofovir is principally eliminated by the kidney. Renal impairment, including cases of acute renal failure and Fanconi syndrome (renal tubular injury with severe hypophosphatemia), has been reported with the use of tenofovir disoproxil fumarate [see Adverse Reactions (6.2)].
It is recommended that estimated creatinine clearance be assessed in all patients prior to initiating therapy and as clinically appropriate during therapy with tenofovir disoproxil fumarate. In patients at risk of renal dysfunction, including patients who have previously experienced renal events while receiving HEPSERA®, it is recommended that estimated creatinine clearance, serum phosphorus, urine glucose, and urine protein be assessed prior to initiation of tenofovir disoproxil fumarate, and periodically during tenofovir disoproxil fumarate therapy.
Dosing interval adjustment of tenofovir disoproxil fumarate and close monitoring of renal function are recommended in all patients with creatinine clearance below 50 ml/min [See
Dosage and Administration (2.3)]. No safety or efficacy data are available in patients with renal impairment who received tenofovir disoproxil fumarate using these dosing guidelines, so the potential benefit of tenofovir disoproxil fumarate therapy should be assessed against the potential risk of renal toxicity.
Tenofovir disoproxil fumarate should be avoided with concurrent or recent use of a nephrotoxic agent (e.g., high-dose or multiple non-steroidal anti-inflammatory drugs (NSAIDs)) [See Drug Interactions (7.4)]. Cases of acute renal failure after initiation of high dose or multiple NSAIDs have been reported in HIV-infected patients with risk factors for renal dysfunction who appeared stable on tenofovir DF. Some patients required hospitalization and renal replacement therapy. Alternatives to NSAIDs should be considered, if needed, in patients at risk for renal dysfunction.
Persistent or worsening bone pain, pain in extremities, fractures and/or muscular pain or weakness may be manifestations of proximal renal tubulopathy and should prompt an evaluation of renal function in at-risk patients.
5.3 Lactic Acidosis/Severe Hepatomegaly with Steatosis
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogs, including tenofovir DF, alone or in combination with other antiretrovirals. Treatment with Tenofovir disoproxil fumarate should be suspended in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity (which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations).
5.4 Coadministration with Other Products
Tenofovir disoproxil fumarate should not be used in combination with other drugs containing tenofovir disoproxil fumurate or tenofovir alafenamide, including ATRIPLA, COMPLERA, DESCOVY, GENVOYA, ODEFSEY, STRIBILD, TRUVAD or VEMLIDY.
Tenofovir disoproxil fumarate should not be administered in combination with HEPSERA (adefovir dipivoxil) [See Drug Interactions (7.4)].
5.5 Patients Coinfected with HIV-1 and HBV
Due to the risk of development of HIV-1 resistance, tenofovir disoproxil fumarate should only be used in HIV-1 and HBV coinfected patients as part of an appropriate antiretroviral combination regimen.
HIV-1 antibody testing should be offered to all HBV- infected patients before initiating therapy with tenofovir disoproxil fumarate. It is also recommended that all patients with HIV-1 be tested for the presence of chronic hepatitis B before initiating treatment with tenofovir disoproxil fumarate.
5.6 Bone Effects
In clinical trials in HIV-1 infected adults, tenofovir disoproxil fumarate was associated with slightly greater decreases in bone mineral density (BMD) and increases in biochemical markers of bone metabolism, suggesting increased bone turnover relative to comparators. Serum parathyroid hormone levels and 1,25 Vitamin D levels were also higher in subjects receiving tenofovir disoproxil fumarate [See Adverse Reactions (6.1)].
Clinical trials evaluating tenofovir disoproxil fumarate in pediatric and adolescent subjects were conducted. Under normal circumstances, BMD increases rapidly in pediatric patients. In HIV-1 infected subjects aged 2 years to less than 18 years, bone effects were similar to those observed in adult subjects and suggest increased bone turnover. Total body BMD gain was less in the tenofovir disoproxil fumarate-treated HIV-1 infected pediatric subjects as compared to the control groups. Similar trends were observed in chronic hepatitis B infected adolescent subjects aged 12 years to less than 18 years. In all pediatric trials, skeletal growth (height) appeared to be unaffected [See Adverse Reactions (6.1)].
The effects of tenofovir disoproxil fumarate-associated changes in BMD and biochemical markers on long-term bone health and future fracture risk are unknown. Assessment of BMD should be considered for adult and pediatric patients who have a history of pathologic bone fracture or other risk factors for osteoporosis or bone loss. Although the effect of supplementation with calcium and vitamin D was not studied, such supplementation may be beneficial for all patients. If bone abnormalities are suspected then appropriate consultation should be obtained.
Mineralization Defects:
Cases of osteomalacia associated with proximal renal tubulopathy, manifested as bone pain or pain in extremities and which may contribute to fractures, have been reported in association with the use of tenofovir disoproxil fumarate [See Adverse Reactions (6.2)]. Arthralgias and muscle pain or weakness have also been reported in cases of proximal renal tubulopathy. Hypophosphatemia and osteomalacia secondary to proximal renal tubulopathy should be considered in patients at risk of renal dysfunction who present with persistent or worsening bone or muscle symptoms while receiving products containing tenofovir DF [See Warnings and Precautions (5.2)].
5.7 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in HIV-infected patients treated with combination antiretroviral therapy, including tenofovir disoproxil fumarate. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections [such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jirovecii pneumonia (PCP), or tuberculosis], which may necessitate further evaluation and treatment.
Autoimmune disorders (such as Graves' disease, polymyositis, and Guillain-Barr¡SR syndrome) have also been reported to occur in the setting of immune reconstitution, however, the time to onset is more variable, and can occur many months after initiation of treatment.
5.8 Early Virologic Failure
Clinical trials in HIV-infected subjects have demonstrated that certain regimens that only contain three nucleoside reverse transcriptase inhibitors (NRTI) are generally less effective than triple drug regimens containing two NRTIs in combination with either a non-nucleoside reverse transcriptase inhibitor or a HIV-1 protease inhibitor. In particular, early virological failure and high rates of resistance substitutions have been reported. Triple nucleoside regimens should therefore be used with caution. Patients on a therapy utilizing a triple nucleoside-only regimen should be carefully monitored and considered for treatment modification.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in other sections of the labeling:
- Severe Acute Exacerbation of Hepatitis [See Boxed Warning, Warnings and Precautions (5.1)] .
- New Onset or Worsening Renal Impairment [See Warnings and Precautions (5.2)] .
- Lactic Acidosis/Severe Hepatomegaly with Steatosis [See Boxed Warning, Warnings and Precautions (5.3)] .
- Bone Effects [See Warnings and Precautions (5.6)] .
- Immune Reconstitution Syndrome [See Warnings and Precautions (5.7)] .
6.1 Adverse Reactions from Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Trials in Adult Patients with HIV-1 Infection
More than 12,000 subjects have been treated with tenofovir disoproxil fumarate alone or in combination with other antiretroviral medicinal products for periods of 28 days to 215 weeks in clinical trials and expanded access programs. A total of 1,544 subjects have received tenofovir disoproxil fumarate 300 mg once daily in clinical trials; over 11,000 subjects have received tenofovir disoproxil fumarate in expanded access programs.
The most common adverse reactions (incidence greater than or equal to 10%, Grades 2-4) identified from any of the 3 large controlled clinical trials include rash, diarrhea, headache, pain, depression, asthenia, and nausea.
Treatment-Naïve Patients
Study 903 - Treatment-Emergent Adverse-Reactions: The most common adverse reactions seen in a double-blind comparative controlled trial in which 600 treatment-naïve subjects received tenofovir disoproxil fumarate (N=299) or stavudine (N=301) in combination with lamivudine and efavirenz for 144 weeks (Study 903) were mild to moderate gastrointestinal events and dizziness.
Mild adverse reactions (Grade 1) were common with a similar incidence in both arms, and included dizziness, diarrhea, and nausea. Selected treatment-emergent moderate to severe adverse reactions are summarized in Table 4.
Table 4 Selected Treatment-Emergent Adverse Reactions a (Grades 2–4) Reported in ≥5% in Any Treatment Group in Study 903 (0–144 Weeks) a Frequencies of adverse reactions are based on all treatment-emergent adverse events, regardless of relationship to study drug.
b Lipodystrophy represents a variety of investigator-described adverse events not a protocol-defined syndrome.
c Peripheral neuropathy includes peripheral neuritis and neuropathy.
d Rash event includes rash, pruritus, maculopapular rash, urticaria, vesiculobullous rash, and pustular rash.
Tenofovir disoproxil fumarate + 3TC + EFV
d4T + 3TC + EFV
N=299
N=301
Body as a Whole
Headache
14%
17%
Pain
13%
12%
Fever
8%
7%
Abdominal pain
7%
12%
Back pain
9%
8%
Asthenia
6%
7%
Digestive System
Diarrhea
11%
13%
Nausea
8%
9%
Dyspepsia
4%
5%
Vomiting
5%
9%
Metabolic Disorders
Lipodystrophy b
1%
8%
Musculoskeletal
Arthralgia
5%
7%
Myalgia
3%
5%
Nervous System
Depression
11%
10%
Insomnia
5%
8%
Dizziness
3%
6%
Peripheral neuropathy c
1%
5%
Anxiety
6%
6%
Respiratory
Pneumonia
5%
5%
Skin and Appendages
Rash event d
18%
12%
Laboratory Abnormalities: With the exception of fasting cholesterol and fasting triglyceride elevations that were more common in the stavudine group (40% and 9%) compared with tenofovir disoproxil fumarate (19% and 1%) respectively, laboratory abnormalities observed in this trial occurred with similar frequency in the tenofovir disoproxil fumarate and stavudine treatment arms. A summary of Grade 3-4 laboratory abnormalities is provided in Table 5.
Table 5 Grades 3-4 Laboratory Abnormalities Reported in ≥1% of Tenofovir Disoproxil Fumarate-Treated Subjects in Study 903 (0–144 Weeks)
Tenofovir disoproxil fumarate + 3TC + EFV
d4T + 3TC + EFV
N=299
N=301
Any ≥ Grade 3 Laboratory Abnormality
36%
42%
Fasting Cholesterol (>240 mg/dL)
19%
40%
Creatine Kinase (M: >990 U/L; F: >845 U/L)
12%
12%
Serum Amylase (>175 U/L)
9%
8%
AST (M: >180 U/L; F: >170 U/L)
5%
7%
ALT (M: >215 U/L; F: >170 U/L)
4%
5%
Hematuria (>100 RBC/HPF)
7%
7%
Neutrophils (<750/mm 3)
3%
1%
Fasting Triglycerides (>750 mg/dL)
1%
9%
Study 934 - Treatment Emergent Adverse Reactions: In Study 934, 511 antiretroviral-naïve subjects received either tenofovir disoproxil fumarate + EMTRIVA ® administered in combination with efavirenz (N=257) or zidovudine/lamivudine administered in combination with efavirenz (N=254). Adverse reactions observed in this trial were generally consistent with those seen in previous studies in treatment-experienced or treatment-naïve subjects (Table 6).
Changes in Bone Mineral Density:
In HIV-1 infected adult subjects in Study 903, there was a significantly greater mean percentage decrease from baseline in BMD at the lumbar spine in subjects receiving tenofovir disoproxil fumarate + lamivudine + efavirenz (-2.2% ± 3.9) compared with subjects receiving stavudine + lamivudine + efavirenz (-1.0% ± 4.6) through 144 weeks. Changes in BMD at the hip were similar between the two treatment groups (-2.8% ± 3.5 in the tenofovir disoproxil fumarate group vs. -2.4% ± 4.5 in the stavudine group). In both groups, the majority of the reduction in BMD occurred in the first 24–48 weeks of the trial and this reduction was sustained through Week 144. Twenty-eight percent of tenofovir disoproxil fumarate-treated subjects vs. 21% of the stavudine-treated subjects lost at least 5% of BMD at the spine or 7% of BMD at the hip. Clinically relevant fractures (excluding fingers and toes) were reported in 4 subjects in the tenofovir disoproxil fumarate group and 6 subjects in the stavudine group. In addition, there were significant increases in biochemical markers of bone metabolism (serum bone-specific alkaline phosphatase, serum osteocalcin, serum C telopeptide, and urinary N telopeptide) and higher serum parathyroid hormone levels and 1,25 Vitamin D levels in the tenofovir disoproxil fumarate group relative to the stavudine group; however, except for bone-specific alkaline phosphatase, these changes resulted in values that remained within the normal range [See Warnings and Precautions (5.6)].
Table 6 Selected Treatment-Emergent Adverse Reactions a (Grades 2–4) Reported in ≥5% in Any Treatment Group in Study 934 (0–144 Weeks) a Frequencies of adverse reactions are based on all treatment-emergent adverse events, regardless of relationship to study drug.
b From Weeks 96 to 144 of the trial, subjects received TRUVADA with efavirenz in place of tenofovir disoproxil fumarate + EMTRIVA with efavirenz.
c Rash event includes rash, exfoliative rash, rash generalized, rash macular, rash maculopapular, rash pruritic, and rash vesicular.
Tenofovir disoproxil fumarate b + FTC + EFV
AZT/3TC + EFV
N=257
N=254
Gastrointestinal Disorder
Diarrhea
9%
5%
Nausea
9%
7%
Vomiting
2%
5%
General Disorders and Administration Site Condition
Fatigue
9%
8%
Infections and Infestations
Sinusitis
8%
4%
Upper respiratory tract infections
8%
5%
Nasopharyngitis
5%
3%
Nervous System Disorders
Headache
6%
5%
Dizziness
8%
7%
Psychiatric Disorders
Depression
9%
7%
Insomnia
5%
7%
Skin and Subcutaneous Tissue Disorders
Rash event c
7%
9%
Laboratory Abnormalities: Laboratory abnormalities observed in this trial were generally consistent with those seen in previous trials (Table 7).
Table 7 Significant Laboratory Abnormalities Reported in ≥1% of Subjects in Any Treatment Group in Study 934 (0–144 Weeks) a From Weeks 96 to 144 of the trial, subjects received TRUVADA with efavirenz in place of tenofovir disoproxil fumarate + EMTRIVA with efavirenz.
Tenofovir disoproxil fumarate a + FTC + EFV
AZT/ 3TC + EFV
N=257
N=254
Any ≥ Grade 3 Laboratory
Abnormality
30%
26%
Fasting Cholesterol (>240 mg/dL)
22%
24%
Creatine Kinase
(M: >990 U/L; F: >845 U/L)
9%
7%
Serum Amylase (>175 U/L)
8%
4%
Alkaline Phosphatase (>550 U/L)
1%
0%
AST (M: >180 U/L, F: >170 U/L)
3%
3%
ALT (M: >215 U/L; F: >170 U/L)
2%
3%
Hemoglobin (<8.0 mg/dL)
0%
4%
Hyperglycemia (>250 mg/dL)
2%
1%
Hematuria (>75 RBC/HPF)
3%
2%
Glycosuria (≥3+)
<1%
1%
Neutrophils (<750/mm 3)
3%
5%
Fasting Triglycerides (>750 mg/dL)
4%
2%
Treatment-Experienced Patients
Treatment-Emergent Adverse Reactions: The adverse reactions seen in treatment experienced subjects were generally consistent with those seen in treatment naïve subjects including mild to moderate gastrointestinal events, such as nausea, diarrhea, vomiting, and flatulence. Less than 1% of subjects discontinued participation in the clinical trials due to gastrointestinal adverse reactions (Study 907).
A summary of moderate to severe, treatment-emergent adverse reactions that occurred during the first 48 weeks of Study 907 is provided in Table 8.
Table 8 Selected Treatment-Emergent Adverse Reactions a (Grades 2–4) Reported in ≥3% in Any Treatment Group in Study 907 (0–48 Weeks) a Frequencies of adverse reactions are based on all treatment-emergent adverse events, regardless of relationship to study drug.
b Peripheral neuropathy includes peripheral neuritis and neuropathy.
c Rash event includes rash, pruritus, maculopapular rash, urticaria, vesiculobullous rash, and pustular rash.
Tenofovir disoproxil fumarate
(N=368)
(Week 0–24)
Placebo
(N=182)
(Week 0–24)
Tenofovir disoproxil fumarate (N=368)
(Week 0–48)
Placebo Crossover to Tenofovir disoproxil fumarate (N=170)
(Week 24–48)
Body as a Whole
Asthenia
7%
6%
11%
1%
Pain
7%
7%
12%
4%
Headache
5%
5%
8%
2%
Abdominal pain
4%
3%
7%
6%
Back pain
3%
3%
4%
2%
Chest pain
3%
1%
3%
2%
Fever
2%
2%
4%
2%
Digestive System
Diarrhea
11%
10%
16%
11%
Nausea
8%
5%
11%
7%
Vomiting
4%
1%
7%
5%
Anorexia
3%
2%
4%
1%
Dyspepsia
3%
2%
4%
2%
Flatulence
3%
1%
4%
1%
Respiratory
Pneumonia
2%
0%
3%
2%
Nervous System
Depression
4%
3%
8%
4%
Insomnia
3%
2%
4%
4%
Peripheral neuropathy b
3%
3%
5%
2%
Dizziness
1%
3%
3%
1%
Skin and Appendage
Rash event c
5%
4%
7%
1%
Sweating
3%
2%
3%
1%
Musculoskeletal
Myalgia
3%
3%
4%
1%
Metabolic
Weight loss
2%
1%
4%
2%
Laboratory Abnormalities: Laboratory abnormalities observed in this trial occurred with similar frequency in the tenofovir disoproxil fumarate and placebo-treated groups. A summary of Grade 3-4 laboratory abnormalities is provided in Table 9.
Table 9 Grade 3-4 Laboratory Abnormalities Reported in ≥1% of Tenofovir Disoproxil Fumarate-Treated Subjects in Study 907 (0–48 Weeks) Tenofovir disoproxil fumarate (N=368)
(Week 0–24)
Placebo
(N=182)
(Week 0–24)
Tenofovir disoproxil fumarate (N=368)
(Week 0–48)
Placebo
Crossover to tenofovir disoproxil fumarate (N=170)
(Week 24–48)
Any ≥ Grade 3 Laboratory Abnormality
25%
38%
35%
34%
Triglycerides (>750 mg/dL)
8%
13%
11%
9%
Creatine Kinase
(M: >990 U/L; F: >845 U/L)
7%
14%
12%
12%
Serum Amylase (>175 U/L)
6%
7%
7%
6%
Glycosuria (≥3+)
3%
3%
3%
2%
AST
(M: >180 U/L; F: >170 U/L)
3%
3%
4%
5%
ALT
(M: >215 U/L; F: >170 U/L)
2%
2%
4%
5%
Serum Glucose (>250 U/L)
2%
4%
3%
3%
Neutrophils (<750/mm 3)
1%
1%
2%
1%
Clinical Trials in Pediatric Subjects 2 Years of Age and Older with HIV-1 Infection
Assessment of adverse reactions is based on two randomized trials (Studies 352 and 321) in 184 HIV-1 infected pediatric subjects (2 to less than 18 years of age) who received treatment with tenofovir disoproxil fumarate (N=93) or placebo/active comparator (N=91) in combination with other antiretroviral agents for 48 weeks. The adverse reactions observed in subjects who received treatment with tenofovir disoproxil fumarate were consistent with those observed in clinical trials in adults.
Eighty-nine pediatric subjects (2 to less than 12 years of age) received tenofovir disoproxil fumarate in Study 352 for a median exposure of 104 weeks. Of these, 4 subjects discontinued from the trial due to adverse reactions consistent with proximal renal tubulopathy. Three of these 4 subjects presented with hypophosphatemia and also had decreases in total body or spine BMD Z score [See Warnings and Precautions (5.6)].
Changes in Bone Mineral Density:
Clinical trials in HIV-1 infected children and adolescents evaluated BMD changes. In Study 321 (12 to less than 18 years), the mean rate of BMD gain at Week 48 was less in the tenofovir disoproxil fumarate compared to the placebo treatment group. Six tenofovir disoproxil fumarate treated subjects and one placebo treated subject had significant (greater than 4%) lumbar spine BMD loss at Week 48. Changes from baseline BMD Z-scores were -0.341 for lumbar spine and -0.458 for total body in the 28 subjects who were treated with tenofovir disoproxil fumarate for 96 weeks. In Study 352 (2 to less than 12 years), the mean rate of BMD gain in lumbar spine at Week 48 was similar between the tenofovir disoproxil fumarate and the d4Tor AZT treatment groups. Total body BMD gain was less in the tenofovir disoproxil fumarate compared to the d4T or AZT treatment groups. One tenofovir disoproxil fumarate -treated subject and none of the d4T or AZT-treated subjects experienced significant (greater than 4%) lumbar spine BMD loss at Week 48. Changes from baseline in BMD Z scores were -0.012 for lumbar spine and -0.338 for total body in the 64 subjects who were treated with tenofovir disoproxil fumarate for 96 weeks. In both trials, skeletal growth (height) appeared to be unaffected [See Warnings and Precautions (5.6)].
Clinical Trials in Adult Subjects with Chronic Hepatitis B and Compensated Liver Disease
Treatment-Emergent Adverse Reactions: In controlled clinical trials in 641 subjects with chronic hepatitis B (0102 and 0103), more subjects treated with tenofovir disoproxil fumarate during the 48-week double-blind period experienced nausea: 9% with tenofovir disoproxil fumarate versus 2% with HEPSERA. Other treatment-emergent adverse reactions reported in more than 5% of subjects treated with tenofovir disoproxil fumarate included: abdominal pain, diarrhea, headache, dizziness, fatigue, nasopharyngitis, back pain and skin rash.
During the open-label phase of treatment with tenofovir disoproxil fumarate (weeks 48–384) in Studies 0102 and 0103, 2% of subjects (13/585) experienced a confirmed increase in serum creatinine of 0.5 mg/dL from baseline. No significant change in the tolerability profile was observed with continued treatment for up to 384 weeks.
Laboratory Abnormalities: A summary of Grade 3-4 laboratory abnormalities through Week 48 is provided in Table 10. Grade 3-4 laboratory abnormalities were similar in subjects continuing tenofovir disoproxil fumarate treatment for up to 384 weeks in these trials.
Table 10 Grades 3-4 Laboratory Abnormalities Reported in ≥1% of Tenofovir Disoproxil Fumarate–Treated Subjects in Studies 0102 and 0103 (0-48 Weeks)
TENOFOVIR DISOPROXIL FUMARATE
(N=426)
HEPSERA
(N=215)
Any ≥ Grade 3 Laboratory Abnormality
19%
13%
Creatine Kinase
(M: >990 U/L; F: >845 U/L)
2%
3%
Serum Amylase (>175 U/L)
4%
1%
Glycosuria (≥3+)
3%
<1%
AST
(M: >180 U/L; F: >170 U/L)
4%
4%
ALT
(M: >215 U/L; F: >170 U/L)
10%
6%
The overall incidence of on-treatment ALT flares (defined as serum ALT greater than 2 × baseline and greater than 10 × ULN, with or without associated symptoms) was similar between tenofovir disoproxil fumarate (2.6%) and HEPSERA (2%). ALT flares generally occurred within the first 4-8 weeks of treatment and were accompanied by decreases in HBV DNA levels. No subject had evidence of decompensation. ALT flares typically resolved within 4 to 8 weeks without changes in study medication.
The adverse reactions observed in subjects with chronic hepatitis B and lamivudine resistance who received treatment with tenofovir disoproxil fumarate were consistent with those observed in other hepatitis B clinical trials in adults.
Clinical Trials in Adult Subjects with Chronic Hepatitis B and Decompensated Liver Disease
In a small randomized, double-blind, active-controlled trial (0108), subjects with CHB and decompensated liver disease received treatment with tenofovir disoproxil fumarate or other antiviral drugs for up to 48 weeks [See Clinical Studies (14.2)]. Among the 45 subjects receiving tenofovir disoproxil fumarate, the most frequently reported treatment-emergent adverse reactions of any severity were abdominal pain (22%), nausea (20%), insomnia (18%), pruritus (16%), vomiting (13%), dizziness (13%), and pyrexia (11%). Two of 45 (4%) subjects died through Week 48 of the trial due to progression of liver disease. Three of 45 (7%) subjects discontinued treatment due to an adverse event. Four of 45 (9%) subjects experienced a confirmed increase in serum creatinine of 0.5 mg dL (1 subject also had a confirmed serumphosphorus less than 2mg/dL through Week 48). Three of these subjects (each of whom had a Child-Pugh score greater than or equal to 10 and MELD score greater than or equal to 14 at entry) developed renal failure. Because both tenofovir disoproxil fumarate and decompensated liver disease may have an impact on renal function, the contribution of tenofovir disoproxil fumarate to renal impairment in this population is difficult to ascertain.
One of 45 subjects experienced as on-treatment hepatic flare during the 48 Week trial.
Clinical Trials in Pediatric Subjects 12 Years of Age and Older with Chronic Hepatitis B
Assessment of adverse reactions is based on one randomized study (Study GS-US-174-0115) in 106 pediatric subjects (12 to less than 18 years of age) infected with chronic hepatitis B receiving treatment with tenofovir disoproxil fumarate (N=52) or placebo (N=54) for 72 weeks. The adverse reactions observed in pediatric subjects who received treatment with tenofovir disoproxil fumarate were consistent with those observed in clinical trials of tenofovir disoproxil fumarate in adults.
In this study, both the tenofovir disoproxil fumarate and placebo treatment arms experienced an overall increase in mean lumbar spine BMD over 72 weeks, as expected for an adolescent population. The BMD gains from baseline to Week 72 in lumbar spine and total body BMD in tenofovir disoproxil fumarate-treated subjects (+5% and +3%, respectively) were less than the BMD gains observed in placebo-treated subjects (+8% and +5%, respectively). Three subjects in the tenofovir disoproxil fumarate group and two subjects in the placebo group had significant (greater than 4%) lumbar spine BMD loss at Week 72. At baseline, mean BMD Z-scores in subjects randomized to tenofovir disoproxil fumarate were −0.43 for lumbar spine and −0.20 for total body, and mean BMD Z-scores in subjects randomized to placebo were −0.28 for lumbar spine and −0.26 for total body. In subjects receiving tenofovir disoproxil fumarate for 72 weeks, the mean change in BMD Z-score was −0.05 for lumbar spine and −0.15 for total body compared to +0.07 and +0.06, respectively, in subjects receiving placebo. As observed in pediatric studies of HIV infected patients, skeletal growth (height) appeared to be unaffected [ See Warnings and Precautions (5.6)].
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of tenofovir disoproxil fumarate. Because postmarketing reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune System Disorders
allergic reaction, including angioedema
Metabolism and Nutrition Disorders
lactic acidosis, hypokalemia, hypophosphatemia
Respiratory, Thoracic, and Mediastinal Disorders
dyspnea
Gastrointestinal Disorders
pancreatitis, increased amylase, abdominal pain
Hepatobiliary Disorders
hepatic steatosis, hepatitis, increased liver enzymes (most commonly AST, ALT gamma GT)
Skin and Subcutaneous Tissue Disorders
rash
Musculoskeletal and Connective Tissue Disorders
rhabdomyolysis, osteomalacia (manifested as bone pain and which may contribute to fractures), muscular weakness, myopathy
Renal and Urinary Disorders
acute renal failure, renal failure, acute tubular necrosis, Fanconi syndrome, proximal renal tubulopathy, interstitial nephritis (including acute cases), nephrogenic diabetes insipidus, renal insufficiency, increased creatinine, proteinuria, polyuria
General Disorders and Administration Site Conditions
Asthenia
The following adverse reactions, listed under the body system headings above, may occur as a consequence of proximal renal tubulopathy: rhabdomyolysis, osteomalacia, hypokalemia, muscular weakness, myopathy, hypophosphatemia.
-
7 DRUG INTERACTIONS
This section describes clinically relevant drug interactions with tenofovir disoproxil fumarate. Drug interactions trials are described elsewhere in the labeling [See Clinical Pharmacology (12.3)].
7.1 Didanosine
Coadministration of tenofovir disoproxil fumarate and didanosine should be undertaken with caution and patients receiving this combination should be monitored closely for didanosine associated adverse reactions. Didanosine should be discontinued in patients who develop didanosine- associated adverse reactions.
When administered with tenofovir disoproxil fumarate, Cmax and AUC of didanosine increased significantly [See Clinical Pharmacology (12.3)]. The mechanism of this interaction is unknown. Higher didanosine concentrations could potentiate didanosine-associated adverse reactions, including pancreatitis and neuropathy. Suppression of CD4+ cell counts has been observed in patients receiving tenofovir disoproxil fumarate with didanosine 400 mg daily.
In patients weighing greater than 60 kg, the didanosine dose should be reduced to 250 mg once daily when it is coadministered with tenofovir disoproxil fumarate. In patients weighing less than60 kg, the didanosine dose should be reduced to 200 mg once daily when it is coadministered with tenofovir disoproxil fumarate. When coadministered, tenofovir disoproxil fumarate and didanosine EC may be taken under fasted conditions or with a light meal (less than 400 kcal, 20% fat). For additional information on coadministration of tenofovir disoproxil fumarate and didanosine, please refer to the full prescribing information for didanosine.
7.2 HIV-1 Protease Inhibitors
Tenofovir disoproxil fumarate decreases the AUC and Cmin of atazanavir [See Clinical Pharmacology (12.3)]. When coadministered with tenofovir disoproxil fumarate, it is recommended that atazanavir 300 mg is given with ritonavir 100 mg. Tenofovir disoproxil fumarate should not be coadministered with atazanavir without ritonavir.
Lopinavir/ritonavir, atazanavir coadministered with ritonavir, and darunavir coadministered with ritonavir have been shown to increase tenofovir concentrations [See Clinical Pharmacology (12.3)]. Tenofovir disoproxil fumarate is a substrate of P-glycoprotein (Pgp) and breast cancer resistance protein (BCRP) transporters. When tenofovir disoproxil fumarate is co-administered with an inhibitor of these transporters, an increase in absorption may be observed. Patients receiving tenofovir disoproxil fumarate concomitantly with lopinavir/ritonavir, ritonavir-boosted atazanavir, or ritonavir-boosted darunavir should be monitored for tenofovir disoproxil fumarate -associated adverse reactions. Tenofovir disoproxil fumarate should be discontinued in patients who develop tenofovir disoproxil fumarate-associated adverse reactions.
7.3 Hepatitis C Antiviral Agents
Coadministration of tenofovir disoproxil fumarate and EPCLUSA ® (sofosbuvir/velpatasvir) or HARVONI ® (ledipasvir/sofosbuvir) has been shown to increase tenofovir exposure [See Clinical Pharmacology (12.3)].
In patients receiving Tenofovir disoproxil fumarate concomitantly with EPCLUSA, monitor for adverse reactions associated with tenofovir DF.
In patients receiving tenofovir disoproxil fumarate concomitantly with HARVONI without an HIV-1 protease inhibitor/ritonavir or an HIV-1 protease inhibitor/cobicistat combination, monitor for adverse reactions associated with tenofovir disoproxil fumarate.
In patients receiving tenofovir disoproxil fumarate concomitantly with HARVONI and an HIV-1 protease inhibitor/ritonavir or an HIV-1 protease inhibitor/cobicistat combination, consider an alternative HCV or antiretroviral therapy, as the safety of increased tenofovir concentrations in this setting has not been established. If coadministration is necessary, monitor for adverse reactions associated with tenofovir disoproxil fumarate.
7.4 Drugs Affecting Renal Function
Since tenofovir is primarily eliminated by the kidneys [See Clinical Pharmacology (12.3)], coadministration of tenofovir disoproxil fumarate with drugs that reduce renal function or compete for active tubular secretion may increase serum concentrations of tenofovir and/or increase the concentrations of other renally eliminated drugs. Some examples include, but are not limited to cidofovir, acyclovir, valacyclovir, ganciclovir, valganciclovir, aminoglycosides (e.g., gentamicin), and high-dose or multiple NSAIDs [See Warnings and Precautions (5.2)].
In the treatment of chronic hepatitis B, tenofovir disoproxil fumarate should not be administered in combination with HEPSERA (adefovir dipivoxil).
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, tenofovir disoproxil fumarate should be used during pregnancy only if clearly needed.
Antiretroviral Pregnancy Registry: To monitor fetal outcomes of pregnant women exposed to tenofovir disoproxil fumarate, an Antiretroviral Pregnancy Registry has been established. Healthcare providers are encouraged to register patients by calling 1-800-258-4263.
Risk Summary
Animal Data
Reproduction studies have been performed in rats and rabbits at doses up to 14 and 19 times the human dose based on body surface area comparisons and revealed no evidence of impaired fertility or harm to the fetus due to tenofovir.
8.3 Nursing Mothers
Nursing Mothers: The Centers for Disease Control and Prevention recommend that HIV-1 infected mothers not breast-feed their infants to avoid risking postnatal transmission of HIV-1. Samples of breast milk obtained from five HIV-1 infected mothers in the first postpartum week show that tenofovir is secreted in human milk. The impact of this exposure in breastfed infants is unknown. Because of both the potential for HIV-1 transmission and the potential for serious adverse reactions in nursing infants, mothers should be instructed not to breast-feed if they are receiving tenofovir disoproxil fumarate.
8.4 Pediatric Use
Pediatric Patients 2 Years of Age and Older with HIV-1 infection
The safety of tenofovir disoproxil fumarate in pediatric patients aged 2 to less than 18 years is supported by data from two randomized trials in which tenofovir disoproxil fumarate was administered to HIV-1 infected treatment-experienced subjects. In addition, the pharmacokinetic profile of tenofovir in patients 2 to less than 18 years of age at the recommended doses was similar to that found to be safe and effective in adult clinical trials [See Clinical Pharmacology (12.3)].
In Study 352, 92 treatment-experienced subjects 2 to less than 12 years of age with stable, virologic suppression on stavudine-or zidovudine-containing regimen were randomized to either replace stavudine or zidovudine with tenofovir disoproxil fumarate (N=44) or continue their original regimen (N=48) for 48 weeks. Five additional subjects over the age of 12 were enrolled and randomized (Tenofovir disoproxil fumarate N=4, original regimen N=1) but are not included in the efficacy analysis. After 48 weeks, all eligible subjects were allowed to continue in the study receiving open-label tenofovir disoproxil fumarate. At Week 48, 89% of subjects in the tenofovir disoproxil fumarate treatment group and 90% of subjects in the stavudine or zidovudine treatment group had HIV-1 RNA concentrations less than 400 copies/mL. During the 48 week randomized phase of the study, 1 subject in the tenofovir disoproxil fumarate group discontinued the study prematurely because of virologic failure/lack of efficacy and 3 subjects (2 subjects in the tenofovir disoproxil fumarate group and 1 subject in the stavudine or zidovudine group) discontinued for other reasons.
In Study 321, 87 treatment-experienced subjects 12 to less than 18 years of age were treated with tenofovir disoproxil fumarate (N=45) or placebo (N=42) in combination with an optimized background regimen (OBR) for 48 weeks. The mean baseline CD4 cell count was 374 cells/mm 3 and the mean baseline plasma HIV-1 RNA was 4.6 log 10 copies/mL. At baseline, 90% of subjects harbored NRTI resistance-associated substitutions in their HIV-1 isolates. Overall, the trial failed to show a difference in virologic response between the tenofovir disoproxil fumarate and placebo treatment groups. Subgroup analyses suggest the lack of difference in virologic response may be attributable to imbalances between treatment arms in baseline viral susceptibility to tenofovir disoproxil fumarate and OBR.
Although changes in HIV-1 RNA in these highly treatment-experienced subjects were less than anticipated, the comparability of the pharmacokinetic and safety data to that observed in adults supports the use of tenofovir disoproxil fumarate in pediatric patients 12 years of age and older who weigh greater than or equal to 35 kg and whose HIV-1 isolate is expected to be sensitive to tenofovir disoproxil fumarate. [See Warnings and Precautions (5.6), Adverse Reactions (6.1), and Clinical Pharmacology (12.3)].
Safety and effectiveness of tenofovir disoproxil fumarate in pediatric patients younger than 2 years of age with HIV-1 infection have not been established.
Pediatric Patients 12 Years of Age and Older with Chronic Hepatitis B
In Study 115, 106 HBeAg negative (9%) and positive (91%) subjects aged 12 to less than 18 years with chronic HBV infection were randomized to receive blinded treatment with tenofovir disoproxil fumarate 300 mg (N=52) or placebo (N=54) for 72 weeks. At study entry, the mean HBV DNA was 8.1 log 10 copies/mL and mean ALT was 101 U/L. Of 52 subjects treated with tenofovir disoproxil fumarate, 20 subjects were nucleos (t)ide-naïve and 32 subjects were nucleos(t)ide experienced. Thirty-one of the 32 nucleos (t) ide-experienced subjects had prior lamivudine experience. At Week 72, 88% (46/52) of subjects in the tenofovir disoproxil fumarate group and 0% (0/54) of subjects in the placebo group had HBV DNA <400 copies/mL (69 IU/mL). Among subjects with abnormal ALT at baseline, 74% (26/35) of subjects receiving tenofovir disoproxil fumarate had normalized ALT at Week 72 compared to 31% (13/42) in the placebo group. One tenofovir disoproxil fumarate-treated subject experienced sustained HBsAg-loss and seroconversion to anti-HBs during the first 72 weeks of study participation.
Safety and effectiveness of tenofovir disoproxil fumarate in pediatric patients younger than 12 years of age or less than 35 kg with chronic hepatitis B have not been established.
8.5 Geriatric Use
Clinical trials of tenofovir disoproxil fumarate did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for the elderly patient should be cautious, keeping in mind the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Patients with Impaired Renal Function
It is recommended that the dosing interval for tenofovir disoproxil fumarate be modified in patients with estimated creatinine clearance below 50 mL/min or in patients with ESRD who require dialysis [See Dosage and Administration (2.3), Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
Limited clinical experience at doses higher than the therapeutic dose of tenofovir disoproxil fumarate 300 mg is available. In Study 901, 600 mg tenofovir disoproxil fumarate was administered to 8 subjects orally for 28 days. No severe adverse reactions were reported. The effects of higher doses are not known.
If overdose occurs the patient must be monitored for evidence of toxicity, and standard supportive treatment applied as necessary.
Tenofovir is efficiently removed by hemodialysis with an extraction coefficient of approximately 54%. Following a single 300 mg dose of tenofovir disoproxil fumarate, a four-hour hemodialysis session removed approximately 10% of the administered tenofovir dose.
-
11 DESCRIPTION
Tenofovir disoproxil fumarate (a prodrug of tenofovir) is a fumaric acid salt of bisisopropoxycarbonyloxymethyl ester derivative of tenofovir. In vivo tenofovir disoproxil fumarate is converted to tenofovir, an acyclic nucleoside phosphonate (nucleotide) analog of adenosine 5'-monophosphate. Tenofovir exhibits activity against HIV-1 reverse transcriptase.
The chemical name of tenofovir disoproxil fumarate is 9-[( R)-2-[[bis[[(isopropoxycarbonyl)oxy]methoxy]phosphinyl]methoxy]propyl]adenine fumarate (1:1). It has a molecular formula of C 19H 30N 5O 10P C 4H 4O 4 and a molecular weight of 635.52. It has the following structural formula:
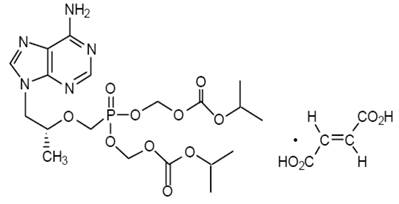
Tenofovir disoproxil fumarate is a white to off-white crystalline powder with a solubility of 13.4 mg/mL in distilled water at 25 °C. It has an octanol/phosphate buffer (pH 6.5) partition coefficient (log p) of 1.25 at 25 °C.
Tenofovir disoproxil fumarate is available as tablets.
Tenofovir disoproxil fumarate tablets are for oral administration in strength of 300 mg of tenofovir disoproxil fumarate, which is equivalent to 245 mg of tenofovir disoproxil. Each tablet contains the following inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate, microcrystalline cellulose, and pregelatinized starch. The tablets are coated with Opadry White Y-1-7000, which contains Hypromellose, Titanium dioxide USP & Polyethylene glycol 400 (Macrogol) USP.
In this insert, all dosages are expressed in terms of tenofovir disoproxil fumarate except where otherwise noted.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Tenofovir disoproxil fumarate is an antiviral drug [See Microbiology (12.4)].
12.3 Pharmacokinetics
The pharmacokinetics of tenofovir disoproxil fumarate have been evaluated in healthy volunteers and HIV-1 infected individuals. Tenofovir pharmacokinetics are similar between these populations.
Tenofovir disoproxil fumarate is a water soluble diester prodrug of the active ingredient tenofovir. The oral bioavailability of tenofovir from tenofovir disoproxil fumarate in fasted subjects is approximately 25%. Following oral administration of a single dose of tenofovir disoproxil fumarate 300 mg to HIV-1 infected subjects in the fasted state, maximum serum concentrations (C max) are achieved in 1.0 ± 0.4 hrs. C max and AUC values are 0.30 ± 0.09 µg/mL and 2.29 ± 0.69 µg ·hr/mL, respectively.
The pharmacokinetics of tenofovir are dose proportional over a tenofovir disoproxil fumarate dose range of 75 to 600 mg and are not affected by repeated dosing.
In a single-dose bioequivalence study conducted under non-fasted conditions (dose administered with 4 oz. applesauce) in healthy adult volunteers, the mean C max of tenofovir was 26% lower for the oral powder relative to the tablet formulation. Mean AUC of tenofovir was similar between the oral powder and tablet formulations.
In vitro binding of tenofovir to human plasma or serum proteins is less than 0.7 and 7.2%, respectively, over the tenofovir concentration range 0.01 to 25 µg/mL. The volume of distribution at steady-state is 1.3 ± 0.6 L/kg and 1.2 ± 0.4 L/kg, following intravenous administration of tenofovir 1.0 mg/kg and 3.0 mg/kg.
In vitro studies indicate that neither tenofovir disoproxil nor tenofovir are substrates of CYP enzymes.
Following IV administration of tenofovir, approximately 70-80% of the dose is recovered in the urine as unchanged tenofovir within 72 hours of dosing. Following single dose, oral administration of tenofovir disoproxil fumarate, the terminal elimination half-life of tenofovir is approximately 17 hours. After multiple oral doses of tenofovir disoproxil fumarate 300 mg once daily (under fed conditions), 32 ± 10% of the administered dose is recovered in urine over 24 hours.
Tenofovir is eliminated by a combination of glomerular filtration and active tubular secretion. There may be competition for elimination with other compounds that are also renally eliminated.
Effects of Food on Oral Absorption
Administration of tenofovir disoproxil fumarate 300 mg tablets following a high-fat meal (~700 to 1000 kcal containing 40 to 50% fat) increases the oral bioavailability, with an increase in tenofovir AUC 0-∞ of approximately 40% and an increase in C max of approximately 14%. However, administration of tenofovir disoproxil fumarate with a light meal did not have a significant effect on the pharmacokinetics of tenofovir when compared to fasted administration of the drug. Food delays the time to tenofovir C max by approximately 1 hour. C max and AUC of tenofovir are 0.33 ± 0.12 µg/mL and 3.32 ± 1.37 µg ·hr/mL following multiple doses of tenofovir disoproxil fumarate 300 mg once daily in the fed state, when meal content was not controlled.
Race: There were insufficient numbers from racial and ethnic groups other than Caucasian to adequately determine potential pharmacokinetic differences among these populations.
Gender: Tenofovir pharmacokinetics are similar in male and female subjects.
Pediatric Patients 2 Years of Age and Older: Steady-state pharmacokinetics of tenofovir were evaluated in 31 HIV-1 infected pediatric subjects 2 to less than 18 years (Table 11). Tenofovir exposure achieved in these pediatric subjects receiving oral once daily doses of tenofovir disoproxil fumarate 300 mg (tablet) or 8 mg/kg of body weight (powder) up to a maximum dose of 300 mg was similar to exposures achieved in adults receiving once-daily doses of tenofovir disoproxil fumarate 300 mg.
Caption: Table 11 Mean (± SD) Tenofovir Pharmacokinetic Parameters by Age Groups for HIV-1-infected Pediatric Patients
Dose and Formulation
300 mg Tablet
12 to <18 Years (N=8)
C max (μg/mL)
0.38 ± 0.13
AUC tau (μg hr/mL)
3.39 ± 1.22
Tenofovir exposures in 52 HBV-infected pediatric subjects (12 to less than 18 years of age) receiving oral once-daily doses of tenofovir disoproxil fumarate 300 mg tablet were comparable to exposures achieved in HIV- I-infected adults and adolescents receiving once-daily doses of 300 mg.
Geriatric Patients: Pharmacokinetic trials have not been performed in the elderly (65 years and older).
Patients with Impaired Renal Function: The pharmacokinetics of tenofovir are altered in subjects with renal impairment [See Warnings and Precautions (5.2)]. In subjects with creatinine clearance below 50 mL/min or with end-stage renal disease (ESRD) requiring dialysis, C max, and AUC 0-∞ of tenofovir were increased (Table 12). It is recommended that the dosing interval for tenofovir disoproxil fumarate be modified in patients with estimated creatinine clearance below 50 mL/min or in patients with ESRD who require dialysis [See Dosage and Administration (2.3)].
Table 12 Pharmacokinetic Parameters (Mean ± SD) of Tenofovir a in Subjects with Varying Degrees of Renal Function a 300 mg, single dose of tenofovir disoproxil fumarate
Baseline Creatinine
Clearance (mL/min)
>80
(N=3)
50–80
(N=10)
30–49
(N=8)
12–29
(N=11)
C max (µg/mL)
0.34 ± 0.03
0.33 ± 0.06
0.37 ± 0.16
0.60 ± 0.19
AUC 0-∞ (µg · hr/mL)
2.18 ± 0.26
3.06 ± 0.93
6.01 ± 2.50
15.98 ± 7.22
CL/F (mL/min)
1043.7 ± 115.4
807.7 ± 279.2
444.4 ± 209.8
177.0 ± 97.1
CL renal (mL/min)
243.5 ± 33.3
168.6 ± 27.5
100.6 ± 27.5
43.0 ± 31.2
Tenofovir is efficiently removed by hemodialysis with an extraction coefficient of approximately 54%. Following a single 300 mg dose of tenofovir disoproxil fumarate, a four-hour hemodialysis session removed approximately 10% of the administered tenofovir dose.
Patients with Hepatic Impairment: The pharmacokinetics of tenofovir following a 300 mg single dose of tenofovir disoproxil fumarate have been studied in non-HIV infected subjects with moderate to severe hepatic impairment. There were no substantial alterations in tenofovir pharmacokinetics in subjects with hepatic impairment compared with unimpaired subjects. No change in tenofovir disoproxil fumarate dosing is required in patients with hepatic impairment.
Assessment of Drug Interactions
At concentrations substantially higher (~300-fold) than those observed in vivo, tenofovir did not inhibit in vitro drug metabolism mediated by any of the following human CYP isoforms: CYP3A4, CYP2D6, CYP2C9, or CYP2E1. However, a small (6%) but statistically significant reduction in metabolism of CYP1A substrate was observed. Based on the results of in vitro experiments and the known elimination pathway of tenofovir, the potential for CYP mediated interactions involving tenofovir with other medicinal products is low.
Tenofovir disoproxil fumarate has been evaluated in healthy volunteers in combination with other antiretroviral and potential concomitant drugs. Tables 13 and 14 summarize pharmacokinetic effects of coadministered drug on tenofovir pharmacokinetics and effects of tenofovir disoproxil fumarate on the pharmacokinetics of coadministered drug. Coadministration of tenofovir disoproxil fumarate with didanosine results in changes in the pharmacokinetics of didanosine that may be of clinical significance. Concomitant dosing of tenofovir disoproxil fumarate with didanosine significantly increases the C max and AUC of didanosine. When didanosine 250 mg enteric-coated capsules were administered with tenofovir disoproxil fumarate, systemic exposures of didanosine were similar to those seen with the 400mg enteric-coated capsules alone under fasted conditions (Table 14). The mechanism of this interaction is unknown.
No clinically significant drug interactions have been observed between tenofovir disoproxil fumarate and efavirenz, methadone, nelfinavir, oral contraceptives, ribavirin, or sofosbuvir.
Table 13 Drug Interactions: Changes in Pharmacokinetic Parameters for Tenofovir a in the Presence of the Coadministered Drug a Subjects received tenofovir disoproxil fumarate 300 mg once daily.
b Increase = ↑; Decrease = ↓; No Effect = ↔ ; NC = Not Calculated
c Reyataz Prescribing Information
d Prezista Prescribing Information
e Data generated from simultaneous dosing with HARVONI (ledipasvir/sofosbuvir). Staggered administration (12 hours apart) provide similar results.
f Comparison based on exposures when administered as atazanavir/ritonavir + emtricitabine/tenofovir DF.
g Comparison based on exposures when administered as darunavir/ritonavir + emtricitabine/tenofovir DF.
h Study conducted with ATRIPLA (efavirenz/emtricitabine/tenofovir DF) coadministered with HARVONI.
i Study conducted with COMPLERA (emtricitabine/rilpivirine/tenofovir DF) coadministered with HARVONI.
j Study conducted with ATRIPLA coadministered with SOVALDI ® (sofosbuvir).
k Aptivus Prescribing Information.
l Study conducted with TRUVADA (emtricitabine/tenofovir DF) + dolutegravir coadministered with HARVONI.
m Comparison based on exposures when administered as atazanavir/ritonavir + emtricitabine/tenofovir DF.
n Comparison based on exposures when administered as darunavir/ritonavir + emtricitabine/tenofovir DF.
o Study conducted with ATRIPLA coadministered with EPCLUSA (sofosbuvir/velpatasvir).
p Study conducted with STRIBILD (elvitegravir/cobicistat/emtricitabine/tenofovir DF) coadministered with EPCLUSA.
q Study conduted with COMPLERA coadministered with EPCLUSA
r Administered as raltegravin +emtricitabine/tenofovir DF.
Coadministered Drug
Dose of Coadministere d Drug (mg)
N
% Change of Tenofovir Pharmacokinetic Parameters b
(90% CI)
C max
AUC
C min
Atazanavir c
400 once daily × 14 days
33
↑ 14
(↑ 8 to ↑ 20)
↑ 24
(↑ 21 to ↑ 28)
↑ 22
(↑ 15 to ↑ 30)
Atazanavir/ Ritonavir c
300/100 once daily
12
↑ 34
(↑ 20 to ↑ 51)
↑ 37
(↑ 30 to ↑ 45)
↑ 29
(↑ 21 to ↑ 36)
Darunavir/Ritonavir d
300/100 twice daily
12
↑ 24
(↑ 8 to ↑ 42)
↑ 22
(↑ 10 to ↑ 35)
↑ 37
(↑ 19 to ↑ 57)
Indinavir
800 three times daily × 7 days
13
↑ 14
(↓ 3 to ↑ 33)
↔
↔
Ledipasvir/ Sofosbuvir e,f
90/400 once daily x 10 days
24
↑ 47
(↑ 37 to ↑ 58)
↑ 35
(↑ 29 to ↑ 42 )
↑ 47
(↑ 38 to ↑ 57)
Ledipasvir/ Sofosbuvir e,g
23
↑ 64
(↑ 54 to ↑ 74)
↑ 50
(↑ 42 to ↑ 59)
↑ 59
(↑ 49 to ↑ 70)
Ledipasvir/ Sofosbuvir h
90/400 once daily x 14 days
15
↑ 79
(↑ 56 to ↑ 104)
↑ 98
(↑ 77 to ↑ 123)
↑ 163
(↑ 132 to↑197)
Ledipasvir/ Sofosbuvir i
90/400 once daily x 10 days
14
↑ 32
(↑ 25 to ↑ 39 )
↑ 40
(↑ 31 to ↑ 50 )
↑ 91
(↑ 74 to ↑ 110)
Ledipasvir/ Sofosbuvir l
90/400 once daily x 10 days
29
↑ 61
(↑ 51 to ↑ 72)
↑ 65
(↑ 59 to ↑ 71)
↑ 115
(↑ 105 to ↑
126)
Lopinavir/ Ritonavir
400/100 twice daily × 14 days
24
↔
↑ 32
(↑ 25 to ↑ 38)
↑ 51
(↑ 37 to ↑ 66)
Saquinavir/ Ritonavir
1000/100 twice daily × 14 days
35
↔
↔
↑ 23
(↑ 16 to ↑ 30)
Sofosbuvir j
400 single dose
16
↑ 25
(↑ 8 to ↑ 45)
↔
↔
Sofosbuvir/ Velpatasvir m
400/100 once daily
24
↑ 55
(↑ 43 to ↑ 68)
↑ 30
(↑ 24 to ↑ 36)
↑ 39
(↑ 31 to ↑ 48)
Sofosbuvir/ Velpatasvir n
400/100 once daily
29
↑ 55
(↑ 45 to ↑ 66)
↑ 39
(↑ 33 to ↑ 44)
↑ 52
(↑ 45 to ↑ 59)
Sofosbuvir/ Velpatasvir o
400/100 once daily
15
↑ 77
(↑ 53 to ↑ 104)
↑ 81
(↑ 68 to ↑ 94)
↑ 121
(↑ 100 to ↑ 143)
Sofosbuvir/ Velpatasvir p
400/100 once daily
24
↑ 36
(↑ 25 to ↑ 47)
↑ 35
(↑ 29 to ↑ 42)
↑ 45
(↑ 39 to ↑ 51)
Sofosbuvir/ Velpatasvir q
400/100 once daily
24
↑ 44
(↑ 33 to ↑ 55)
↑ 40
(↑ 34 to ↑ 46)
↑ 84
(↑ 76 to ↑ 92)
Sofosbuvir/ Velpatasvir r
400/100 once daily
30
↑ 46
(↑ 39 to ↑ 54)
↑ 40
(↑ 34 to ↑ 45)
↑ 70
(↑ 61 to ↑ 79)
Tacrolimus
0.05 mg/kg twice daily x 7 days
21
↑ 13
(↑ 1 to ↑ 27)
↔
↔
Tipranavir/ Ritonavir k
500/100 twice daily
22
↓ 23
(↓ 32 to ↓ 13)
↓ 2
(↓ 9 to ↑ 5)
↑ 7
(↓ 2 to ↑ 17)
750/200 twice daily (23 doses)
20
↓ 38
(↓ 46 to ↓ 29)
↑ 2
(↓ 6 to ↑ 10)
↑ 14
(↑ 1 to ↑ 27)
No effect on the pharmacokinetic parameters of the following coadministered drugs was observed with Tenofovir Disoproxil Fumarate: abacavir, didanosine (buffered tablets), emtricitabine, entecavir, and lamivudine.
Table 14 Drug Interactions: Changes in Pharmacokinetic Parameters for Co-Administered Drug in the Presence of Tenofovir Disoproxil Fumarate a Increase = ↑ ; Decrease = ↓ ; No Effect = ↔ ; NA = Not Applicable
b Reyataz Prescribing Information
c In HIV-infected subjects, addition of tenofovir DF to atazanavir 300 mg plus ritonavir 100 mg, resulted in AUC and Cmin values of atazanavir that were 2.3- and 4-fold higher than the respective values observed for atazanavir 400 mg when given alone.
d Prezista Prescribing Information
e Videx EC Prescribing Information. Subjects received didanosine enteric-coated capsules.
f 373 kcal, 8.2 g fat
g Compared with didanosine (enteric-coated) 400 mg administered alone under fasting conditions.
h Increases in AUC and Cmin are not expected to be clinically relevant; hence no dose adjustments are required when tenofovir DF and ritonavir-boosted saquinavir are coadministered.
i Aptivus Prescribing Information.
Coadministered Drug
Dose of
Coadministered
Drug (mg)
N
% Change of Coadministered Drug Pharmacokinetic Parameters a
(90% Cl)
C max
AUC
C min
Abacavir
300 once
8
↑ 12
(↓ 1 to ↑ 26)
↔
NA
Atazanavir b
400 once daily
× 14 days
34
↓ 21
(↓ 27 to ↓ 14)
↓ 25
(↓ 30 to ↓ 19)
↓ 40
(↓ 48 to ↓ 32)
Atazanavir b
Atazanavir/ Ritonavir
300/100 once daily
× 42 days
10
↓ 28
(↓ 50 to ↑ 5)
↓ 25 c
(↓ 42 to ↓ 3)
↓ 23 c
(↓ 46 to ↑ 10)
Darunavir d
Darunavir/Ritonavir 300/100 mg once daily
12
↑ 16
(↓ 6 to ↑ 42)
↑ 21
(↓ 5 to ↑ 54)
↑ 24
(↓ 10 to ↑ 69)
Didanosine e
250 once, simultaneously with tenofovir disoproxil fumarate and a light meal f
33
↓ 20 g
(↓32 to ↓7)
↔ g
NA
Emtricitabine
200 once daily
× 7 days
17
↔
↔
↑ 20
(↑ 12 to ↑ 29)
Entecavir
1 mg once daily x 10
days
28
↔
↑ 13
(↑ 11 to ↑ 15)
↔
Indinavir
800 three times
daily × 7 days
12
↓ 11
(↓ 30 to ↑ 12)
↔
↔
Lamivudine
150 twice daily
× 7 days
15
↓ 24
(↓ 34 to ↓ 12)
↔
↔
Lopinavir
Ritonavir
Lopinavir/Ritonavir 400/100 twice daily × 14 days
24
↔
↔
↔
↔
↔
↔
Saquinavir
Ritonavir
Saquinavir/Ritonavir 1000/100 twice
daily × 14 days
32
↑ 22
(↑ 6 to ↑ 41)
↔
↑ 29 h
(↑ 12 to ↑ 48)
↔
↑ 47 h
(↑ 23 to ↑ 76)
↑ 23
(↑ 3 to ↑ 46)
Tacrolimus
0.05 mg/kg twice daily
x 7 days
21
↔
↔
↔
Tipranavir i
Tipranavir/Ritonavir 500/100 twice daily
22
↓ 17
(↓ 26 to ↓ 6)
↓ 18
(↓ 25 to ↓ 9)
↓ 21
(↓ 30 to ↓ 10)
Tipranavir/Ritonavir 750/200 twice daily (23 doses)
20
↓ 11
(↓ 16 to ↓ 4)
↓ 9
(↓ 15 to ↓ 3)
↓ 12
(↓ 22 to 0)
12.4 Microbiology
Tenofovir disoproxil fumarate is an acyclic nucleoside phosphonate diester analog of adenosine monophosphate. Tenofovir disoproxil fumarate requires initial diester hydrolysis for conversion to tenofovir and subsequent phosphorylations by cellular enzymes to form tenofovir diphosphate, an obligate chain terminator. Tenofovir diphosphate inhibits the activity of HIV-1 reverse transcriptase and HBV reverse transcriptase by competing with the natural substrate deoxyadenosine 5'-triphosphate and, after incorporation into DNA, by DNA chain termination. Tenofovir diphosphate is a weak inhibitor of mammalian DNA polymerases α, β, and mitochondrial DNA polymerase γ.
Activity against HIV
Antiviral Activity
The antiviral activity of tenofovir against laboratory and clinical isolates of HIV-1 was assessed in lymphoblastoid cell lines, primary monocyte/macrophage cells and peripheral blood lymphocytes. The EC50 (50% effective concentration) values for tenofovir were in the range of 0.04 μM to 8.5 μM. In drug combination studies, tenofovir was not antagonistic with nucleoside reverse transcriptase inhibitors (abacavir, didanosine, lamivudine, stavudine, zalcitabine, zidovudine), non-nucleoside reverse transcriptase inhibitors (delavirdine, efavirenz, nevirapine), and protease inhibitors (amprenavir, indinavir, nelfinavir, ritonavir, saquinavir). Tenofovir displayed antiviral activity in cell culture against HIV-1 clades A, B, C, D, E, F, G, and O (EC50 values ranged from 0.5 μM to 2.2 μM) and strain specific activity against HIV-2 (EC50 values ranged from 1.6 μM to 5.5 μM).
Resistance
HIV-1 isolates with reduced susceptibility to tenofovir have been selected in cell culture. These viruses expressed a K65R substitution in reverse transcriptase and showed a 2 to 4-fold reduction in susceptibility to tenofovir. In addition, a K70E substitution in HIV-1 reverse transcriptase has been selected by tenofovir and results in low-level reduced susceptibility to tenofovir.
In Study 903 of treatment-naïve subjects (tenofovir disoproxil fumarate + lamivudine + efavirenz versus stavudine + lamivudine + efavirenz) [See Clinical Studies (14.1)], genotypic analyses of isolates from subjects with virologic failure through Week 144 showed development of efavirenz and lamivudine resistance-associated substitutions to occur most frequently and with no difference between the treatment arms. The K65R substitution occurred in 8/47 (17%) of analyzed patient isolates in the tenofovir disoproxil fumarate arm and in 2/49 (4%) of analyzed patient isolates in the stavudine arm. Of the 8 subjects whose virus developed K65R in the tenofovir disoproxil fumarate arm through 144 weeks, 7 occurred in the first 48 weeks of treatment and one at Week 96. One patient in the tenofovir disoproxil fumarate arm developed the K70E substitution in the virus. Other substitutions resulting in resistance to tenofovir disoproxil fumarate were not identified in this trial.
In Study 934 of treatment-naïve subjects (tenofovir disoproxil fumarate + EMTRIVA + efavirenz versus zidovudine (AZT)/lamivudine (3TC) + efavirenz) [See Clinical Studies (14.1)], genotypic analysis performed on HIV-1 isolates from all confirmed virologic failure subjects with greater than 400 copies/mL of HIV-1 RNA at Week 144 or early discontinuation showed development of efavirenz resistance-associated substitutions occurred most frequently and was similar between the two treatment arms The M184V substitution, associated with resistance to EMTRIVA and lamivudine, was observed in 2/19 of analyzed subject isolates in the tenofovir disoproxil fumarate + EMTRIVA group and in 10/29 analyzed subject isolates in the zidovudine/lamivudine group. Through 144 weeks of Study 934, no subjects have developed a detectable K65R substitution in their HIV-1 as analyzed through standard genotypic analysis.
Cross-Resistance
Cross-resistance among certain reverse transcriptase inhibitors has been recognized. The K65R and K70E substitutions selected by tenofovir are also selected in some HIV-1 infected subjects treated with abacavir or didanosine. HIV-1 isolates with this substitution also show reduced susceptibility to emtricitabine and lamivudine. Therefore, cross-resistance among these drugs may occur in patients whose virus harbors the K65R or K70E substitution. HIV-1 isolates from subjects (N=20) whose HIV-1 expressed a mean of three zidovudine-associated reverse transcriptase substitutions (M41L, D67N, K70R, L210W, T215Y/F, or K219Q/E/N), showed a 3.1-fold decrease in the susceptibility to tenofovir.
In Studies 902 and 907 conducted in treatment-experienced subjects (tenofovir disoproxil fumarate + Standard Background Therapy (SBT) compared to Placebo + SBT) [See Clinical Studies (14.1)], 14/304 (5%) of the tenofovir disoproxil fumarate-treated subjects with virologic failure through Week 96 had greater than 1.4-fold (median 2.7-fold) reduced susceptibility to tenofovir. Genotypic analysis of the baseline and failure isolates showed the development of the K65R substitution in the HIV-1 reverse transcriptase gene.
The virologic response to tenofovir disoproxil fumarate therapy has been evaluated with respect to baseline viral genotype (N=222) in treatment-experienced subjects participating in Studies 902 and 907.In these clinical trials, 94% of the participants evaluated had baseline HIV-1 isolates expressing at least one NRTI substitution. Virologic responses for subjects in the genotype substudy were similar to the overall trial results.
Several exploratory analyses were conducted to evaluate the effect of specific substitutions and substitutional patterns on virologic outcome. Because of the large number of potential comparisons, statistical testing was not conducted. Varying degrees of cross-resistance of tenofovir disoproxil fumarate to pre-existing zidovudine resistance-associated substitutions (M41L, D67N, K70R, L210W, T215Y/F, or K219Q/E/N) were observed and appeared to depend on the type and number of specific substitutions. Tenofovir disoproxil fumarate-treated subjects whose HIV-1 expressed 3 or more zidovudine resistance-associated substitutions that included either the M41L or L210W reverse transcriptase substitution showed reduced responses to tenofovir disoproxil fumarate therapy; however, these responses were still improved compared with placebo. The presence of the D67N, K70R, T215Y/F, or K219Q/E/N substitution did not appear to affect responses to tenofovir disoproxil fumarate therapy. Subjects whose virus expressed an L74V substitution without zidovudine resistance associated substitutions (N=8) had reduced response to tenofovir disoproxil fumarate. Limited data are available for subjects whose virus expressed a Y115F substitution (N=3), Q151M substitution (N=2), or T69 insertion (N=4), all of whom had a reduced response.
In the protocol defined analyses, virologic response to Tenofovir disoproxil fumarate was not reduced in subjects with HIV-1 that expressed the abacavir/emtricitabine/lamivudine resistance-associated M184V substitution. HIV-1 RNA responses among these subjects were durable through Week 48.
Studies 902 and 907 Phenotypic Analyses
Phenotypic analysis of baseline HIV-1 from treatment-experienced subjects (N=100) demonstrated a correlation between baseline susceptibility to tenofovir disoproxil fumarate and response to tenofovir disoproxil fumarate therapy. Table 15 summarizes the HIV-1 RNA response by baseline tenofovir disoproxil fumarate susceptibility.
Table 15 HIV-1 RNA Response at Week 24 by Baseline Tenofovir Disoproxil Fumarate Susceptibility (Intent- To-Treat) a a Tenofovir susceptibility was determined by recombinant phenotypic Antivirogram assay (Virco).
b Fold change in susceptibility from wild-type.
c Average HIV-1 RNA change from baseline through Week 24 (DAVG 24) in log 10 copies/mL.
Baseline Tenofovir Disoproxil Fumarate Susceptibility b
Change in HIV-1 RNA c (N)
<1
-0.74 (35)
>1 and 3
-0.56 (49)
>3 and 4
-0.3 (7)
>4
-0.12 (9)
Antiviral Activity
The antiviral activity of tenofovir against HBV was assessed in the HepG2 2.2.15 cell line. The EC 50 values for tenofovir ranged from 0.14 to 1.5 µM, with CC 50 (50% cytotoxicity concentration) values greater than 100 µM. In cell culture combination antiviral activity studies of tenofovir with the nucleoside HBV reverse transcriptase inhibitors entecavir, lamivudine, and telbivudine, and with the nucleoside HIV-1 reverse transcriptase inhibitor emtricitabine, no antagonistic activity was observed.
Resistance
Cumulative tenofovir disoproxil fumarate genotypic resistance has been evaluated annually for up to 384 weeks in Studies 0102, 0103, 0106 ,0108, and 0121 with the paired HBV reverse transcriptase amino acid sequences of the pre-treatment and on-treatment isolates from subjects who received at least 24 weeks of tenofovir disoproxil fumarate monotherapy and remained viremic with HBV DNA greater than or equal to 400 copies/mL (69 IU/mL) at the end of each study year (or at discontinuation of tenofovir disoproxil fumarate monotherapy) using an as-treated analysis. In the nucleotide-naïve population from Studies 0102 and 0103, HBeAg-positive subjects had a higher baseline viral load than HBeAg-negative subjects and a significantly higher proportion of the subjects remained viremic at their last time point on tenofovir disoproxil fumarate monotherapy (15% versus 5%, respectively).
HBV isolates from these subjects who remained viremic showed treatment-emergent substitutions (Table 16); however, no specific substitutions occurred at a sufficient frequency to be associated with resistance to tenofovir disoproxil fumarate (genotypic and phenotypic analyses).
Table 16 Amino Acid Substitutions in Viremic Subjects across HBV Trials of Tenofovir Disoproxil Fumarate a Nucleotide-naïve subjects from Studies 0102 (N=246) and 0103 (N=171) receiving up to 384 weeks of treatment with tenofovir disoproxil fumarate.
b HEPSERA-experienced subjects from Studies 0102/0103 (N=195) and 0106 (N=52) receiving up to 336 weeks of treatment with tenofovir disoproxil fumarate after switching to tenofovir disoproxil fumarate from HEPSERA. Study 0106, a randomized, double blind, 168-week Phase 2 trial, has been completed.
c Lamivudine-resistant subjects from Study 0121 (N=136) receiving up to 96 weeks of treatment with tenofovir disoproxil fumarate after switching to tenofovir disoproxil fumarate from lamivudine
d Subjects with decompensated liver disease from Study 0108 (N=39) receiving up to 48 weeks of treatment with tenofovir disoproxil fumarate.
e Denominator includes those subjects who were viremic at last time point on tenofovir disoproxil fumarate monotherapy and had evaluable paired genotypic data.
f Of the 18 subjects with treatment-emergent amino acid substitutions during Studies 0102 and 0103, 5 subjects had substitutions at conserved sites and 13 subjects had substitutions only at polymorphic sites, and 8 subjects had only transient substitutions that were not detected at the last time point on tenofovir disoproxil fumarate.
g Of the 11 HEPSERA-experienced subjects with treatment-emergent amino acid substitutions, 2 subjects had substitutions at conserved sites and 9 had substitutions only at polymorphic sites.
h Of the 6 lamivudine-resistant subjects with treatment-emergent substitutions during Study 0121, 3 subjects had substitutions at conserved sites and 3 had substitutions only at polymorphic sites.
Compensated Liver Disease
Decompensated Liver Disease (N=39) d
Nucleotide-Naïve
(N=417) a
HEPSERA-experienced
(N=247) b
Lamivudine-
Resistant
(N=136)c
Viremic at Last Time Point on tenofovir disoproxil fumarate
38/417 (9%)
37/247 (15%)
9/136 (7%)
7/39 (18%)
Treatment-Emergent Amino Acid Substitutions e
18 f/32 (56%)
11 g/31 (35%)
6 h/8 (75%)
3/5 (60%)
Cross-resistance has been observed between HBV nucleoside/nucleotide analogue reverse transcriptase inhibitors.
In cell based assays, HBV strains expressing the rtV173L, rtL180M, and rtM204I/V substitutions associated with resistance to lamivudine and telbivudine showed a susceptibility to tenofovir ranging from 0.7- to 3.4-fold that of wild type virus. The rtL180M and rtM204I/V double substitutions conferred 3.4-fold reduced susceptibility to tenofovir.
HBV strains expressing the rtL180M, rtT184G, rtS202G/I, rtM204V, and rtM250V substitutions associated with resistance to entecavir showed a susceptibility to tenofovir ranging from 0.6- to 6.9-fold that of wild type virus.
HBV strains expressing the adefovir resistance-associated substitutions rtA181V and/or rtN236T showed reductions in susceptibility to tenofovir ranging from 2.9- to 10-fold that of wild type virus. Strains containing the rtA181T substitution showed changes in susceptibility to tenofovir ranging from 0.9- to 1.5-fold that of wild type virus.
One hundred fifty-two subjects initiating tenofovir disoproxil fumarate therapy in Studies 0102, 0103, 0106, 0108, and 0121 harbored HBV with known resistance substitutions to HBV nucleos (t) ide analogue reverse transcriptase inhibitors: 14 with adefovir resistance-associated substitutions (rtA181S/T/V and/or rtN236T), 135 with lamivudine resistance-associated substitutions (rtM204I/V), and 3 with both adefovir and lamivudine resistance-associated substitutions. Following up to 384 weeks of tenofovir disoproxil fumarate treatment, 10 of the 14 subjects with adefovir-resistant HBV, 124 of the 135 subjects with lamivudine-resistant HBV, and 2 of the 3 subjects with both adefovir- and lamivudine-resistant HBV achieved and maintained virologic suppression (HBV DNA less than 400 copies/mL [69 IU/mL]). Three of the 5 subjects whose virus harbored both the rtA181T/V and rtN236T substitutions remained viremic.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term oral carcinogenicity studies of tenofovir disoproxil fumarate in mice and rats were carried out at exposures up to approximately 16 times (mice) and 5 times (rats) those observed in humans at the therapeutic dose for HIV-1 infection. At the high dose in female mice, liver adenomas were increased at exposures 16 times that in humans. In rats, the study was negative for carcinogenic findings at exposures up to 5 times that observed in humans at the therapeutic dose.
Tenofovir disoproxil fumarate was mutagenic in the in vitro mouse lymphoma assay and negative in an in vitro bacterial mutagenicity test (Ames test). In an in vivo mouse micronucleus assay, tenofovir disoproxil fumarate was negative when administered to male mice.
13.2 Animal Toxicology and/or Pharmacology
Tenofovir and tenofovir disoproxil fumarate administered in toxicology studies to rats, dogs, and monkeys at exposures (based on AUCs) greater than or equal to 6 fold those observed in humans caused bone toxicity. In monkeys the bone toxicity was diagnosed as osteomalacia. Osteomalacia observed in monkeys appeared to be reversible upon dose reduction or discontinuation of tenofovir. In rats and dogs, the bone toxicity manifested as reduced bone mineral density. The mechanism(s) underlying bone toxicity is unknown.
Evidence of renal toxicity was noted in 4 animal species. Increases in serum creatinine, BUN, glycosuria, proteinuria, phosphaturia, and/or calciuria and decreases in serum phosphate were observed to varying degrees in these animals. These toxicities were noted at exposures (based on AUCs) 2-20 times higher than those observed in humans. The relationship of the renal abnormalities, particularly the phosphaturia, to the bone toxicity is not known.
-
14 CLINICAL STUDIES
14.1 Clinical Efficacy in Adults with HIV-1 Infection
Treatment-Naïve Adult Patients
Data through 144 weeks are reported for Study 903, a double-blind, active-controlled multicenter trial comparing tenofovir disoproxil fumarate (300 mg once daily) administered in combination with lamivudine and efavirenz versus stavudine (d4T), lamivudine, and efavirenz in 600 antiretroviral-naïve subjects. Subjects had a mean age of 36 years (range 18-64), 74% were male, 64% were Caucasian and 20% were Black. The mean baseline CD4+ cell count was 279 cells/mm 3 (range 3-956) and median baseline plasma HIV-1 RNA was 77,600 copies/mL (range 417-5,130,000). Subjects were stratified by baseline HIV-1 RNA and CD4+ cell count. Forty-three percent of subjects had baseline viral loads >100,000 copies/mL and 39% had CD4+ cell counts <200 cells/mm 3. Treatment outcomes through 48 and 144 weeks are presented in Table 17.
Table 17 Outcomes of Randomized Treatment at Week 48 and 144 (Study 903) aSubjects achieved and maintained confirmed HIV-1 RNA <400 copies/mL through Week 48 and 144.
bIncludes confirmed viral rebound and failure to achieve confirmed <400 copies/mL through Week 48 and 144.
cIncludes lost to follow-up, subject's withdrawal, noncompliance, protocol violation and other reasons.
Outcomes
At Week 48
At Week 144
Tenofovir disoproxil fumarate +
3TC + EFV
(N=299)
d4T + 3TC +
EFV
(N=301)
Tenofovir disoproxil fumarate +
3TC + EFV
(N=299)
d4T + 3TC + EFV (N=301)
Responder a
79%
82%
68%
62%
Virologic failure b
6%
4%
10%
8%
Rebound
5%
3%
8%
7%
Never suppressed
0%
1%
0%
0%
Added an
antiretroviral agent
1%
1%
2%
1%
Death
<1%
1%
<1%
2%
Discontinued due to
adverse event
6%
6%
8%
13%
Discontinued
for other reasons c
8%
7%
14%
15%
Achievement of plasma HIV-1 RNA concentrations of less than 400 copies/mL at Week 144 was similar between the two treatment groups for the population stratified at baseline on the basis of HIV-1 RNA concentration (> or ≤100,000 copies/mL) and CD4 + cell count (< or ≥200 cells/mm 3). Through 144 weeks of therapy, 62% and 58% of subjects in the tenofovir disoproxil fumarate and stavudine arms, respectively achieved and maintained confirmed HIV-1 RNA <50 copies/mL. The mean increase from baseline in CD4 + cell count was 263 cells/mm 3 for the tenofovir disoproxil fumarate arm and 283 cells/mm 3 for the stavudine arm.
Through 144 weeks, 11 subjects in the tenofovir disoproxil fumarate group and 9 subjects in the stavudine group experienced a new CDC Class C event.
Data through 144 weeks are reported for Study 934, a randomized, open-label, active-controlled multicenter trial comparing emtricitabine + tenofovir disoproxil fumarate administered in combination with efavirenz versus zidovudine/lamivudine fixed-dose combination administered in combination with efavirenz in 511 antiretroviral-naïve subjects. From Weeks 96 to 144 of the trial, subjects received a fixed-dose combination of emtricitabine and tenofovir with efavirenz in place of emtricitabine + tenofovir disoproxil fumarate with efavirenz. Subjects had a mean age of 38 years (range 18-80), 86% were male, 59% were Caucasian and 23% were Black. The mean baseline CD4+ cell count was 245 cells/mm 3 (range 2-1191) and median baseline plasma HIV-1 RNA was 5.01 log 10 copies/mL (range 3.56-6.54). Subjects were stratified by baseline CD4+ cell count (< or ≥200 cells/mm 3); 41% had CD4+ cell counts <200 cells/mm 3 and 51% of subjects had baseline viral loads >100,000 copies/mL. Treatment outcomes through 48 and 144 weeks for those subjects who did not have efavirenz resistance at baseline are presented in Table 18.
Table 18 Outcomes of Randomized Treatment at Week 48 and 144 (Study 934) a Subjects who were responders at Week 48 or Week 96 (HIV-1 RNA <400 copies/mL) but did not consent to continue the trial after Week 48 or Week 96 were excluded from analysis.
b Subjects achieved and maintained confirmed HIV-1 RNA <400 copies/mL through Weeks 48 and 144.
c Includes confirmed viral rebound and failure to achieve confirmed <400 copies/mL through Weeks 48 and 144.
d Includes lost to follow-up, subject withdrawal, noncompliance, protocol violation and other reasons.
Outcomes
At Week 48
At Week 144
FTC +Tenofovir disoproxil fumarate + EFV
(N=244)
AZT/3TC+EFV
(N=243)
FTC +Tenofovir disoproxil fumarate + EFV
(N=227) a
AZT/3TC+EFV
(N=229) a
Responder b
84%
73%
71%
58%
Virologic failure c
2%
4%
3%
6%
Rebound
1%
3%
2%
5%
Never suppressed
0%
0%
0%
0%
Change in antiretroviral regimen
1%
1%
1%
1%
Death
<1%
1%
1%
1%
Discontinued due to adverse event
4%
9%
5%
12%
Discontinued for other reasons d
10%
14%
20%
22%
Through Week 48, 84% and 73% of subjects in the emtricitabine + tenofovir disoproxil fumarate group and the zidovudine/lamivudine group, respectively, achieved and maintained HIV-1 RNA <400 copies/mL (71% and 58% through Week 144). The difference in the proportion of subjects who achieved and maintained HIV-1 RNA <400 copies/mL through 48 weeks largely results from the higher number of discontinuations due to adverse events and other reasons in the zidovudine/lamivudine group in this open-label trial. In addition, 80% and 70% of subjects in the emtricitabine + tenofovir disoproxil fumarate group and the zidovudine/lamivudine group, respectively, achieved and maintained HIV-1 RNA <50 copies/mL through Week 48 (64% and 56% through Week 144). The mean increase from baseline in CD4+ cell count was 190 cells/mm 3 in the EMTRIVA + tenofovir disoproxil fumarate group and 158 cells/mm 3 in the zidovudine/lamivudine group at Week 48 (312 and 271 cells/mm 3 at Week 144).
Through 48 weeks, 7 subjects in the emtricitabine + tenofovir disoproxil fumarate group and 5 subjects in the zidovudine/lamivudine group experienced a new CDC Class C event (10 and 6 subjects through 144 weeks).
Treatment-Experienced Adult Patients
Study 907 was a 24-week, double-blind, placebo-controlled multicenter trial of tenofovir disoproxil fumarate added to a stable background regimen of antiretroviral agents in 550 treatment-experienced subjects. After 24 weeks of blinded trial treatment, all subjects continuing on trial were offered open-label tenofovir disoproxil fumarate for an additional 24 weeks. Subjects had a mean baseline CD4+ cell count of 427 cells/mm 3 (range 23-1385), median baseline plasma HIV-1 RNA of 2340 (range 50-75,000) copies/mL, and mean duration of prior HIV-1 treatment was 5.4 years. Mean age of the subjects was 42 years, 85% were male and 69% were Caucasian, 17% Black and 12% Hispanic.
The percent of subjects with HIV-1 RNA <400 copies/mL and outcomes of subjects through 48 weeks are summarized in Table 19.
Table 19 Outcomes of Randomized Treatment (Study 907) a Subjects with HIV-1 RNA <400 copies/mL and no prior study drug discontinuation at Week 24 and 48 respectively.
b Subjects with HIV-1 RNA ≥400 copies/mL efficacy failure or missing HIV-1 RNA at Week 24 and 48 respectively.
c Includes lost to follow-up, subject withdrawal, noncompliance, protocol violation and other reasons.
Outcomes
0-24 weeks
0-48 weeks
24-48 weeks
Tenofovir disoproxil fumarate (N=368)
Placebo
(N=182)
Tenofovir disoproxil fumarate
(N=368)
Placebo
Crossover
to tenofovir disoproxil fumarate
(N=170)
HIV-1 RNA <400 copies/mL a
40%
11%
28%
30%
Virologic failure b
53%
84%
61%
64%
Discontinued due to adverse event
3%
3%
5%
5%
Discontinued for other reasons c
3%
3%
5%
1%
At 24 weeks of therapy, there was a higher proportion of subjects in the tenofovir disoproxil fumarate arm compared to the placebo arm with HIV-1 RNA <50 copies/mL (19% and 1%, respectively). Mean change in absolute CD4+ cell counts by Week 24 was +11 cells/mm 3 for the tenofovir disoproxil fumarate group and -5 cells/mm 3 for the placebo group. Mean change in absolute CD4+ cell counts by Week 48 was +4 cells/mm 3 for the tenofovir disoproxil fumarate group.
Through Week 24, one subject in the tenofovir disoproxil fumarate group and no subjects in the placebo arm experienced a new CDC Class C event.
14.2 Clinical Efficacy in Adults with Chronic Hepatitis B
HBeAg-Negative Chronic Hepatitis B
Study 0102 was a Phase 3, randomized, double-blind, active-controlled trial of tenofovir disoproxil fumarate 300 mg compared to HEPSERA 10 mg in 375 HBeAg- (anti-HBe+) subjects with compensated liver function, the majority of whom were nucleoside-naïve. The mean age of subjects was 44 years, 77% were male, 25% were Asian, 65% were Caucasian, 17% had previously received alpha-interferon therapy and 18% were nucleoside-experienced (16% had prior lamivudine experience). At baseline, subjects had a mean Knodell necroinflammatory score of 7.8; mean plasma HBV DNA was 6.9 log10 copies/mL; and mean serum ALT was 140 U/L.
HBeAg-Positive Chronic Hepatitis B
Study 0103 was a Phase 3, randomized, double-blind, active-controlled trial of tenofovir disoproxil fumarate 300 mg compared to HEPSERA 10 mg in 266 HBeAg+ nucleoside-naïve subjects with compensated liver function. The mean age of subjects was 34 years, 69% were male, 36% were Asian, 52% were Caucasian, 16% had previously received alpha-interferon therapy, and <5% were nucleoside experienced. At baseline, subjects had a mean Knodell necroinflammatory score of 8.4; mean plasma HBV DNA was 8.7 log10 copies /mL; and mean serum ALT was 147 U/L.
The primary data analysis was conducted after all subjects reached 48 weeks of treatment and results are summarized below.
The primary efficacy endpoint in both trials was complete response to treatment defined as HBV DNA <400 copies/mL (69 IU/mL) and Knodell necroinflammatory score improvement of at least 2 points, without worsening in Knodell fibrosis at Week 48 (Table 20).
Table 20 Histological, Virological, Biochemical, and Serological Response at Week 48 a Knodell necroinflammatory score improvement of at least 2 points without worsening in Knodell fibrosis.
b The population used for analysis of ALT normalization included only subjects with ALT above ULN at baseline.
c NA = Not Applicable
0102 (HBeAg-)
0103 (HBeAg+)
Tenofovir disoproxil fumarate
(N=250)
HEPSERA
(N=125)
Tenofovir disoproxil fumarate
(N=176)
HEPSERA
(N=90)
Complete
Response
71%
49%
67%
12%
Histology
Histological
Response a
72%
69%
74%
68%
HBV DNA
<400 copies/mL
(<69 IU/mL)
93%
63%
76%
13%
ALT
Normalized ALT b
76%
77%
68%
54%
Serology
HBeAg Loss/
Seroconversion
NA c
NA c
20%/19%
16%/16%
HBsAg Loss/
Seroconversion
0/0
0/0
3%/1%
0/0
In Studies 0102 (HBeAg-negative) and 0103 (HBeAg-positive), subjects who completed double-blind treatment (389 and 196 subjects who were originally randomized to tenofovir disoproxil fumarate and HEPSERA, respectively) were eligible to roll over to open-label tenofovir disoproxil fumarate with no interruption in treatment.
In Study 0102, 266 of 347 subjects who entered the open-label period (77%) continued in the study through Week 384. Among subjects randomized to tenofovir disoproxil fumarate followed by open-label treatment with tenofovir disoproxil fumarate, 73% had HBV DNA <400 copies/ml (69 IU/ml), and 63% had ALT normalization at Week 384. Among subjects randomized to HEPSERA followed by open-label treatment with tenofovir disoproxil fumarate, 80% had HBV DNA <400 copies/mL (69 IU/mL) and 70% had ALT normalization through Week 384. At Week 384, both HBsAg loss and seroconversion were approximately 1% in both treatment groups.
In Study 0103, 146 of 238 subjects who entered the open-label period (61%) continued in the study through Week 384. Among subjects randomized to tenofovir disoproxil fumarate, 49% had HBV DNA <400 copies/mL (69 IU/mL), 42% had ALT normalization, and 20% had HBeAg loss (13% seroconversion to anti-HBe antibody) through Week 384. Among subjects randomized to HEPSERA followed by open-label treatment with tenofovir disoproxil fumarate, 56% had HBV DNA <400 copies/mL (69 IU/mL), 50% had ALT normalization, and 28% had HBeAg loss (19% seroconversion to anti-HBe antibody) through Week 384. At Week 384, HBsAg loss and seroconversion were 11% and 8% respectively, in subjects initially randomized to tenofovir disoproxil fumarate and 12% and 10%, respectively, in subjects initially randomized to HEPSERA.
Of the originally randomized and treated 641 subjects in the two studies, liver biopsy data from 328 subjects who received continuing open-label treatment with tenofovir disoproxil fumarate monotherapy were available for analysis at baseline, Week 48 and Week 240. There were no apparent differences between the subset of subjects who had liver biopsy data at Week 240 and those subjects remaining on open-label tenofovir disoproxil fumarate without biopsy data that would be expected to affect histological outcomes at Week 240. Among the 328 subjects evaluated, the observed histological response rates were 80% and 88% at Week 48 and Week 240, respectively. In the subjects without cirrhosis at baseline (Ishak fibrosis score 0-4), 92% (216/235) and 95% (223/235) had either improvement or no change in Ishak fibrosis score at Week 48 and Week 240, respectively. In subjects with cirrhosis at baseline (Ishak fibrosis score 5-6), 97% (90/93) and 99% (92/93) had either improvement or no change in Ishak fibrosis score at Week 48 and Week 240, respectively. Twenty-nine percent (27/93) and 72% (67/93) of subjects with cirrhosis at baseline experienced regression of cirrhosis by Week 48 and Week 240, respectively, with a reduction in Ishak fibrosis score of at least 2 points. No definitive conclusions can be established about the remaining study population who were not part of this subset analysis.
Patients with Lamivudine-Resistant Chronic Hepatitis B
Study 121 was a randomized, double-blind, active-controlled trial evaluating the safety and efficacy of tenofovir disoproxil fumarate compared to an unapproved antiviral regimen in subjects with chronic hepatitis B, persistent viremia (HBV DNA ≥1,000 IU/mL), and genotypic evidence of lamivudine resistance (rtM204I/V +/-rtL180M). One hundred forty-one adult subjects were randomized to the tenofovir disoproxil fumarate treatment arm. The mean age of subjects randomized to tenofovir disoproxil fumarate was 47 years (range 18-73), 74% were male, 59% were Caucasian, and 37% were Asian. At baseline, 54% of subjects were HBeAg-negative, 46% were HBeAg-positive, and 56% had abnormal ALT. Subjects had a mean HBV DNA of 6.4 log10 copies/mL and mean serum ALT of 71 U/L at baseline.
After 96 weeks of treatment, 126 of 141 subjects (89%) randomized to tenofovir disoproxil fumarate had HBV DNA <400 copies/mL (69 IU/mL), and 49 of 79 subjects (62%) with abnormal ALT at baseline had ALT normalization. Among the HBeAg-positive subjects randomized to tenofovir disoproxil fumarate, 10 of 65 subjects (15%) experienced HBeAg loss, and 7 of 65 subjects (11%) experienced anti-HBe seroconversion through Week 96. The proportion of subjects with HBV DNA concentrations below 400 copies/mL (69 IU/mL) at Week 96 was similar between the tenofovir disoproxil fumarate monotherapy and the comparator arms.
Across the combined chronic hepatitis B treatment trials, the number of subjects with adefovir-resistance associated substitutions at baseline was too small to establish efficacy in this subgroup.
Patients with Chronic Hepatitis B and Decompensated Liver Disease
Tenofovir disoproxil fumarate was studied in a small randomized, double-blind, active-controlled trial evaluating the safety of tenofovir disoproxil fumarate compared to other antiviral drugs in subjects with chronic hepatitis B and decompensated liver disease through 48 weeks (Study 0108).
Forty-five adult subjects (37 males and 8 females) were randomized to the tenofovir disoproxil fumarate treatment arm. At baseline, 69% subjects were HBeAg-negative, and 31% were HBeAg-positive. Subjects had a mean Child-Pugh score of 7, a mean MELD score of 12, mean HBV DNA of 5.8 log10 copies/mL and mean serum ALT of 61 U/L at baseline. Trial endpoints were discontinuation due to an adverse event and confirmed increase in serum creatinine ≥0.5 mg/dL or confirmed serum phosphorus of < 2 mg/dL. [See Adverse Reactions (6.1)].
At 48 weeks, 31/44 (70%) and 12/26 (46%) tenofovir disoproxil fumarate-treated subjects achieved an HBV DNA <400 copies/mL (69 IU/mL), and normalized ALT, respectively. The trial was not designed to evaluate treatment impact on clinical endpoints such as progression of liver disease, need for liver transplantation, or death.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Tenofovir Disoproxil Fumarate Tablets 300 mg, are white circular film-coated convex tablets containing 300 mg of tenofovir disoproxil fumarate, which is equivalent to 245 mg of tenofovir disoproxil, engraved TDF on one side and plain on other side and are available in a 40 cc/ 50 cc HDPE container containing a desiccant (silica gel sachet) and closed with child-resistant screw cap.:
- Bottle of 30 tablets (NDC: 64380-714-04)
Store tenofovir disoproxil fumarate tablets at 25°C (77°F), excursions permitted to 15-30°C (59-86°F) [see USP Controlled Room Temperature].
Keep the bottle tightly closed. Dispense only in original container. Do not use if seal over bottle opening is broken or missing.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
- Tenofovir disoproxil fumarate is not a cure for HIV-1 infection and patients may continue to experience illnesses associated with HIV-1 infection, including opportunistic infections. Patients should remain under the care of a physician when using tenofovir disoproxil fumarate.
Advice patients to avoid doing things that can spread HIV or HBV to others.
- Do not share needles or other injection equipment.
- Do not share personal items that can have blood or body fluids on them, like toothbrushes and razor blades.
- Do not have any kind of sex without protection. Always practice safer sex by using a latex or polyurethane condom to lower the chance of sexual contact with semen, vaginal secretions, or blood.
- Do not breastfeed. Tenofovir is excreted in breast milk and it is not known whether it can harm the baby. Mothers with HIV-1 should not breastfeed because HIV-1 can be passed to the baby in the breast milk.
-
PATIENT MEDICATION INFORMATION SECTION
Tenofovir Disoproxil Fumarate Tablets
( ten of' oh vir )
Read this Patient Information before you start taking tenofovir disoproxil fumarate tablets and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about tenofovir disoproxil fumarate tablets?
Tenofovir disoproxil fumarate tablets can cause serious side effects, including:
Worsening of your Hepatitis B infection. Your hepatitis B Virus (HBV) infection may become worse (flare-up) if you take tenofovir disoproxil fumarate tablets and then stop it. A "flare-up"is when your HBV infection suddenly returns in a worse way than before.
- Do not let your tenofovir disoproxil fumarate tablet run out. Refill your prescription or talk to your healthcare provider before your tenofovir disoproxil fumarate tablets are all gone.
- Do not stop taking tenofovir disoproxil fumarate tablet without first talking to your healthcare provider.
- If you stop taking tenofovir disoproxil fumarate, your healthcare provider will need to check your health often and do blood tests regularly to check your HBV infection. Tell your healthcare provider about any new or unusual symptoms you may have after you stop taking tenofovir disoproxil fumarate tablet.
Talk to your doctor about taking an HIV test before starting treatment with tenofovir disoproxil fumarate tablet for chronic hepatitis B. You should also get a test for HBV if you are taking tenofovir disoproxil fumarate tablet for treatment of HIV.
What is tenofovir disoproxil fumarate tablet?
Tenofovir disoproxil fumarate tablet is a prescription medicine used:
1.With other antiviral medicines to treat Human Immunodeficiency Virus-1 (HIV-1) in people 2 years of age and older. HIV is the virus that causes AIDS (Acquired Immune Deficiency Syndrome).
- When used with other HIV medicines, tenofovir disoproxil fumarate may reduce the amount of HIV in your blood (called "viral load"). Tenofovir disoproxil fumarate may also help to increase the number of CD4 (T) cells in your blood which help fight off other infections. Reducing the amount of HIV and increasing the CD4 (T) cell count may improve your immune system. This may reduce your risk of death or infections that can happen when your immune system is weak (opportunistic infections).
- Tenofovir disoproxil fumarate does not cure HIV infection or AIDS. People taking tenofovir disoproxil fumarate may still develop infections or other conditions associated with HIV infection.
- You must stay on continuous HIV therapy to control infection and decrease HIV-related illnesses.
- It is very important that you stay under the care of your healthcare provider.
- It is not known if tenofovir disoproxil fumarate is safe and effective for the treatment of HIV-1 infection in children under the age of 2 years.
2. to treat chronic (long-lasting) hepatitis B virus (HBV) in people 12 years of age and older.
- Tenofovir disoproxil fumarate will not cure HBV.
- Tenofovir disoproxil fumarate may lower the amount of HBV in your body.
- Tenofovir disoproxil fumarate may improve the condition of your liver.
- The long-term effects of taking tenofovir disoproxil fumarate for treatment of chronic hepatitis B infection are not known.
- It is not known if tenofovir disoproxil fumarate is safe and effective for treatment of chronic hepatitis B in children under the age of 12 years.
What should I tell my healthcare provider before taking tenofovir disoproxil fumarate tablet?
Before you take tenofovir disoproxil fumarate tablet, tell your healthcare provider if you:
- have liver problems, including hepatitis B (HBV) infection.
- have kidney problems.
- have bone problems.
- have any other medical conditions, including HIV infection.
- are pregnant or plan to become pregnant. It is not known if tenofovir disoproxil fumarate tablet will harm your unborn baby.
- Pregnancy Registry. There is a pregnancy registry for women who take antiviral medicines during pregnancy. Its purpose is to collect information about the health of you and your baby. Talk to your healthcare provider about how you can take part in this registry.
- are breastfeeding or plan to breastfeed. Do not breastfeed if you are taking tenofovir disoproxil fumarate tablets 300 mg . Tenofovir passes into your breast milk. You should not breastfeed because of the risk of passing HIV to your baby. Talk to your healthcare provider about the best way to feed your baby.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements.
Tenofovir disoproxil fumarate tablet may affect the way other medicines work, and other medicines may affect how tenofovir disoproxil fumarate tablet works.
Do not take tenofovir disoproxil fumarate tablet if you also take:
- other medicines that contain tenofovir (ATRIPLA®, COMPLERA®, DESCOVY®, GENVOYA®, ODEFSEY®, STRIBILD®, TRUVADA®, VEMLIDY®)
- adefovir (HEPSERA ®)
Especially tell your healthcare provider if you take the following medications.
- didanosine (Videx, Videx EC)
- atazanavir (Reyataz)
- darunavir (Prezista)
- lopinavir with ritonavir (Kaletra)
- ledipasvir with sofosbuvir (HARVONI®)
- sofosbuvir with velpatasvir (EPCLUSA®)
Know the medicines you take. Keep a list of them to show your healthcare provider or pharmacist when you get a new medicine.
How should I take tenofovir disoproxil fumarate tablet?
- See "What is the most important information I should know about tenofovir disoproxil fumarate tablet?"
- Take tenofovir disoproxil fumarate tablet exactly as your healthcare provider tells you to take it.
- Take tenofovir disoproxil fumarate tablet at the same time every day.
- Adults and children 12 years of age and older, the usual dose of tenofovir disoproxil fumarate is one 300 mg tablet each day.
- If you are an adult with kidney problems, your healthcare provider may tell you to take tenofovir disoproxil fumarate tablets less often.
- For children 2 to 12 years of age, your healthcare provider will prescribe the right dose of tenofovir disoproxil fumarate tablets based on your child's body weight.
- Tell your healthcare provider if your child has problems with swallowing tablets.
- Take tenofovir disoproxil fumarate tablets by mouth, with or without food.
- Do not miss a dose of tenofovir disoproxil fumarate tablet. If you miss a dose of tenofovir disoproxil fumarate tablet, take the missed dose as soon as you remember. If it is almost time for your next dose of tenofovir disoproxil fumarate tablet, do not take the missed dose. Take the next dose of tenofovir disoproxil fumarate tablet at your regular time.
- If you take too much tenofovir disoproxil fumarate tablet, call your local poison control center or go right away to the nearest hospital emergency room.
What are the possible side effects of tenofovir disoproxil fumarate tablet?
Tenofovir disoproxil fumarate tablet may cause serious side effects, including:
- See "What is the most important information I should know about tenofovir disoproxil fumarate tablet?
- New or worse kidney problems, including kidney failure, can happen in some people who take tenofovir disoproxil fumarate tablet. Your healthcare provider should do blood tests to check your kidneys before you start treatment with tenofovir disoproxil fumarate tablets. If you have had kidney problems in the past or need to take another medicine that can cause kidney problems, your healthcare provider may need to do blood tests to check your kidneys during your treatment with tenofovir disoproxil fumarate tablet.
- Too much lactic acid in your blood (lactic acidosis). Too much lactic acid is a serious but rare medical emergency that can lead to death. Tell your healthcare provider right away if you get these symptoms: weakness or being more tired than usual, unusual muscle pain, being short of breath or fast breathing, stomach pain with nausea and vomiting, cold or blue hands and feet, feel dizzy or lightheaded, or a fast or abnormal heartbeat.
- Severe liver problems. In rare cases, severe liver problems can happen that can lead to death. Tell your healthcare provider right away if you get these symptoms: skin or the white part of your eyes turns yellow, dark "tea-colored" urine, light-colored stools, loss of appetite for several days or longer, nausea, or stomach-area pain.
- Bone problems can happen in some people who take tenofovir disoproxil fumarate tablet. Bone problems include bone pain, softening or thinning (which may lead to fractures). Your healthcare provider may need to do additional tests to check your bones.
- Changes in your immune system (Immune Reconstitution Syndrome) can happen when you start taking HIV medicines. Your immune system may get stronger and begin to fight infections that have been hidden in your body for a long time. Tell your healthcare provider if you start having new symptoms after starting your HIV medicine.
The most common side effects in all people who take tenofovir disoproxil fumarate are:
- nausea
- rash
- diarrhea
- headache
- pain
- depression
- weakness
In some people with advanced HBV-infection, other common side effects may include:
- sleeping problems
- itching
- vomiting
- dizziness
- fever
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of tenofovir disoproxil fumarate tablet. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to Strides Pharma Inc at 1877-244-9825 or FDA at 1-800-FDA-1088.
How should I store tenofovir disoproxil fumarate tablet?
- Store tenofovir disoproxil fumarate tablets at room temperature between 68 °F to 77 °F (20 °C to 25 °C).
- Keep tenofovir disoproxil fumarate tablets in the original container.
- Do not use tenofovir disoproxil fumarate tablets if the seal over the bottle opening is broken or missing.
- Keep the bottle tightly closed.
Keep tenofovir disoproxil fumarate tablet and all medicines out of the reach of children.
General information about tenofovir disoproxil fumarate tablet:
Medicines are sometimes prescribed for purposes other than those listed in a patient information leaflet. Do not use tenofovir disoproxil fumarate tablet for a condition for which it was not prescribed. Do not give tenofovir disoproxil fumarate tablet to other people, even if they have the same condition you have. It may harm them.
Avoid doing things that can spread HIV-1 or HBV infection to others.
- Do not share or re-use needles or other injection equipment.
- Do not share personal items that can have blood or body fluids on them, like toothbrushes and razor blades.
- Do not have any kind of sex without protection . Always practice safe sex by using a latex or polyurethane condom to lower the chance of sexual contact with semen, vaginal secretions, or blood.
A vaccine is available to protect people at risk for becoming infected with HBV. You can ask your healthcare provider for information about this vaccine.
This leaflet summarizes the most important information about tenofovir disoproxil fumarate tablets. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about tenofovir disoproxil fumarate tablet that is written for health professionals.
You may report side effects to Strides Pharma Inc. at 1-877-244-9825 or go to www.stridesshasun.com or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
What are the ingredients in tenofovir disoproxil fumarate tablet?
Active Ingredient: tenofovir disoproxil fumarate
Inactive Ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate, microcrystalline cellulose, and pregelatinized starch. The tablets are coated with Opadry White Y-1-7000, which contains Hypromellose, Titanium dioxide USP & Polyethylene glycol 400 (Macrogol) USP.
This Patient Information has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Strides Shasun Limited
Bengaluru-560076, India
Distributed by:
Strides Pharma Inc.
East Brunswick, NJ 08816
Revised: 12/2017
COMPLERA, DESCOVY, GENVOYA, HARVONI, HEPSERA, ODEFSEY, STRIBILD, TRUVADA, VEMLIDY and VIREAD are registered trademarks of Gilead Sciences Inc., or its related companies. ATRIPLA is a registered trademark of Bristol-Myers Squibb & Gilead Sciences, LLC. All other trademarks herein are the property of their respective owners and are not trademarks of Strides Shasun Limited. The makers of these brands are not affiliated with and do not endorse Strides Shasun Limited. or its products.
-
PRINCIPAL DISPLAY PANEL
DRUG: TENOFOVIR DISOPROXIL FUMARATE
GENERIC: tenofovir disoproxil fumarate
DOSAGE: TABLET
ADMINSTRATION: ORAL
NDC: 70518-1002-0
NDC: 70518-1002-1
COLOR: white
SHAPE: ROUND
SCORE: No score
SIZE: 13 mm
IMPRINT: TDF
PACKAGING: 30 in 1 BLISTER PACK
PACKAGING: 4 in 1 BLISTER PACK
ACTIVE INGREDIENT(S):
- TENOFOVIR DISOPROXIL FUMARATE 300mg in 1
INACTIVE INGREDIENT(S):
- CROSCARMELLOSE SODIUM
- POLYETHYLENE GLYCOL 400
- MICROCRYSTALLINE CELLULOSE
- STARCH, PREGELATINIZED CORN
- HYPROMELLOSE 2910 (5 MPA.S)
- LACTOSE MONOHYDRATE
- MAGNESIUM STEARATE
- TITANIUM DIOXIDE
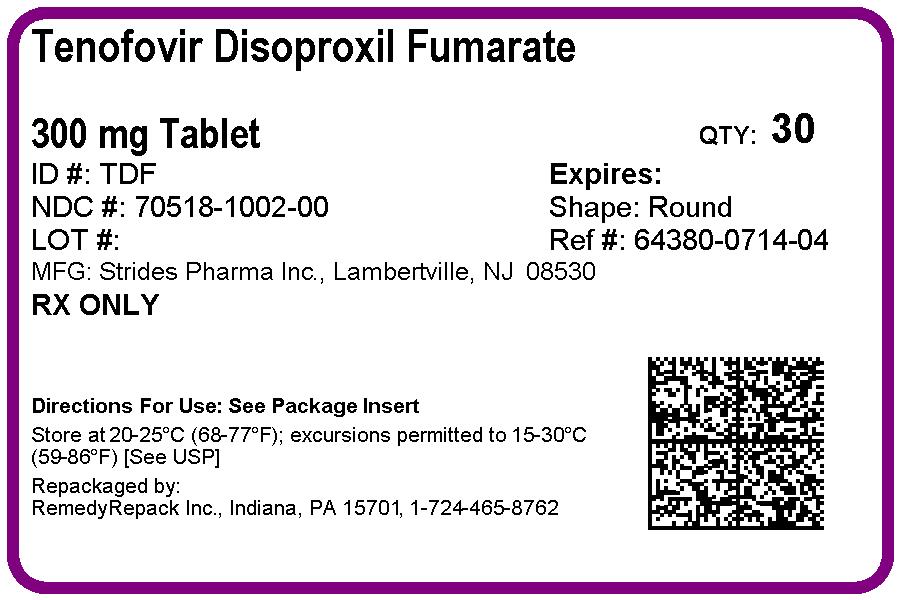
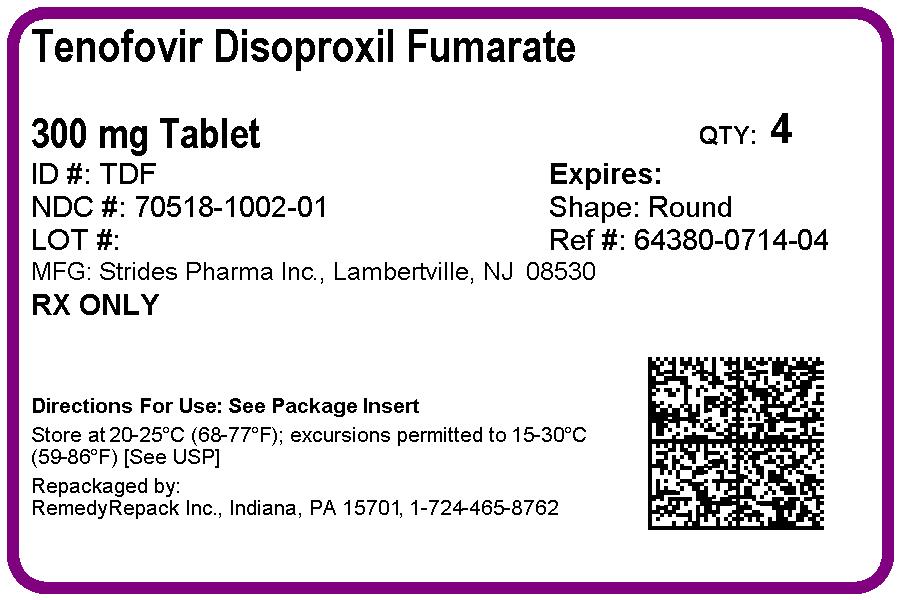
-
INGREDIENTS AND APPEARANCE
TENOFOVIR DISOPROXIL FUMARATE
tenofovir disoproxil fumarate tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70518-1002(NDC:64380-714) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TENOFOVIR DISOPROXIL FUMARATE (UNII: OTT9J7900I) (TENOFOVIR ANHYDROUS - UNII:W4HFE001U5) TENOFOVIR DISOPROXIL FUMARATE 300 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSE 2910 (5 MPA.S) (UNII: R75537T0T4) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL 400 (UNII: B697894SGQ) STARCH, PREGELATINIZED CORN (UNII: O8232NY3SJ) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color white Score no score Shape ROUND (convex) Size 13mm Flavor Imprint Code TDF Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70518-1002-0 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 02/02/2018 2 NDC: 70518-1002-1 4 in 1 BLISTER PACK; Type 0: Not a Combination Product 01/31/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090742 02/02/2018 Labeler - REMEDYREPACK INC. (829572556)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.