PREVNAR 13- pneumococcal 13-valent conjugate vaccine injection, suspension
PREVNAR 13 by
Drug Labeling and Warnings
PREVNAR 13 by is a Other medication manufactured, distributed, or labeled by Wyeth Pharmaceutical Division of Wyeth Holdings LLC, Pfizer Ireland Pharmaceuticals, Wyeth BioPharma Division of Wyeth Pharmaceuticals LLC, Pfizer Manufacturing Belgium NV, John Wyeth & Brother Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PREVNAR 13 safely and effectively. See full prescribing information for PREVNAR 13.
PREVNAR 13 (Pneumococcal 13-valent Conjugate Vaccine
[Diphtheria CRM197 Protein])
Suspension for intramuscular injection
Initial U.S. Approval: 2010INDICATIONS AND USAGE
In children 6 weeks through 5 years of age (prior to the 6th birthday), Prevnar 13 is indicated for:
- active immunization for the prevention of invasive disease caused by Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F. (1.1)
- active immunization for the prevention of otitis media caused by S. pneumoniae serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F. No otitis media efficacy data are available for serotypes 1, 3, 5, 6A, 7F, and 19A. (1.1)
In children 6 years through 17 years of age (prior to the 18th birthday), Prevnar 13 is indicated for:
- active immunization for the prevention of invasive disease caused by S. pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F. (1.2)
In adults 18 years of age and older, Prevnar 13 is indicated for:
- active immunization for the prevention of pneumonia and invasive disease caused by S. pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F. (1.3)
Limitations of Prevnar 13 Use and Effectiveness
- Prevnar 13 does not protect against disease caused by S. pneumoniae serotypes that are not in the vaccine. (1.4)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
0.5 mL suspension for intramuscular injection, supplied in a single-dose prefilled syringe. (3)
CONTRAINDICATIONS
Severe allergic reaction (e.g., anaphylaxis) to any component of Prevnar 13 or any diphtheria toxoid-containing vaccine. (4)
WARNINGS AND PRECAUTIONS
Apnea following intramuscular vaccination has been observed in some infants born prematurely. Decisions about when to administer an intramuscular vaccine, including Prevnar 13, to infants born prematurely should be based on consideration of the individual infant's medical status, and the potential benefits and possible risks of vaccination. (5.3)
ADVERSE REACTIONS
- In infants and toddlers vaccinated at 2, 4, 6, and 12–15 months of age in US clinical trials, the most commonly reported solicited adverse reactions (>5%) were irritability (>70%), injection site tenderness (>50%), decreased appetite (>40%), decreased sleep (>40%), increased sleep (>40%), fever (>20%), injection site redness (>20%), and injection site swelling (>20%). (6.1)
- In children aged 5 through 17 years, the most commonly reported solicited adverse reactions (>5%) were injection site tenderness (>80%), injection site redness (>30%), injection site swelling (>30%), irritability (>20%), decreased appetite (>20%), increased sleep (>20%), fever (>5%), and decreased sleep (>5%). (6.1)
- In adults aged 18 years and older, the most commonly reported solicited adverse reactions (>5%) were pain at the injection site (>50%), fatigue (>30%), headache (>20%), muscle pain (>20%), joint pain (>10%), decreased appetite (>10%), injection site redness (>10%), injection site swelling (>10%), limitation of arm movement (>10%), vomiting (>5%), fever (>5%), chills (>5%), and rash (>5%). (6.2)
To report SUSPECTED ADVERSE REACTIONS, contact Wyeth Pharmaceuticals LLC. at 1-800-438-1985 or VAERS at 1-800-822-7967 or http://vaers.hhs.gov.
USE IN SPECIFIC POPULATIONS
Pediatric Use: Safety and effectiveness of Prevnar 13 in children below the age of 6 weeks have not been established. (8.4)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 7/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Children 6 Weeks Through 5 Years of Age
1.2 Children 6 Years Through 17 Years of Age
1.3 Adults 18 Years of Age and Older
1.4 Limitations of Prevnar 13 Use and Effectiveness
2 DOSAGE AND ADMINISTRATION
2.1 Preparation for Administration
2.2 Administration Information
2.3 Vaccination Schedule for Infants and Toddlers
2.4 Vaccination Schedule for Unvaccinated Children 7 Months Through 5 Years of Age
2.5 Vaccination Schedule for Children 6 Years Through 17 Years of Age
2.6 Vaccination Schedule for Adults 18 Years of Age and Older
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Management of Allergic Reactions
5.2 Altered Immunocompetence
5.3 Apnea in Premature Infants
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience With Prevnar 13 in Children 6 Weeks Through 17 Years of Age
6.2 Clinical Trials Experience With Prevnar 13 in Adults ≥18 Years of Age
6.3 Post-marketing Experience With Prevnar 13 in Infants and Toddlers
7 DRUG INTERACTIONS
7.1 Concomitant Immunizations
7.2 Immunosuppressive Therapies
7.3 Antipyretics
7.4 Prior Vaccination with PPSV23
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 High Risk Populations
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Efficacy Data
14.2 Prevnar 13 Clinical Trials in Children 6 Weeks Through 17 Years of Age
14.3 Prevnar 13 Immunogenicity Clinical Trials in Adults
14.4 Concomitant Vaccine Administration
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Children 6 Weeks Through 5 Years of Age
In children 6 weeks through 5 years of age (prior to the 6th birthday), Prevnar 13® is indicated for:
- active immunization for the prevention of invasive disease caused by Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F.
- active immunization for the prevention of otitis media caused by S. pneumoniae serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F. No otitis media efficacy data are available for serotypes 1, 3, 5, 6A, 7F, and 19A.
1.2 Children 6 Years Through 17 Years of Age
In children 6 years through 17 years of age (prior to the 18th birthday), Prevnar 13 is indicated for:
- active immunization for the prevention of invasive disease caused by S. pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F.
-
2 DOSAGE AND ADMINISTRATION
2.1 Preparation for Administration
Since this product is a suspension containing an adjuvant, shake vigorously immediately prior to use to obtain a homogenous, white suspension in the vaccine container. Do not use the vaccine if it cannot be resuspended. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration [see Description (11)]. This product should not be used if particulate matter or discoloration is found.
Do not mix Prevnar 13 with other vaccines/products in the same syringe.
2.2 Administration Information
For intramuscular injection only.
Each 0.5 mL dose is to be injected intramuscularly using a sterile needle attached to the supplied prefilled syringe. The preferred sites for injection are the anterolateral aspect of the thigh in infants and the deltoid muscle of the upper arm in toddlers, children and adults. The vaccine should not be injected in the gluteal area or areas where there may be a major nerve trunk and/or blood vessel.
2.3 Vaccination Schedule for Infants and Toddlers
Prevnar 13 is to be administered as a four-dose series at 2, 4, 6, and 12–15 months of age.
Table 1: Vaccination Schedule for Infants and Toddlers Dose Dose 1*,† Dose 2† Dose 3† Dose 4‡ - * Dose 1 may be given as early as 6 weeks of age.
- † The recommended dosing interval is 4 to 8 weeks.
- ‡ The fourth dose should be administered at approximately 12–15 months of age, and at least 2 months after the third dose.
Age at Dose 2 months 4 months 6 months 12–15 months 2.4 Vaccination Schedule for Unvaccinated Children 7 Months Through 5 Years of Age
For children 7 months through 5 years of age who have not received Prevnar® or Prevnar 13, the catch-up schedule in Table 2 applies:
Table 2: Vaccination Schedule for Unvaccinated Children 7 Months of Age Through 5 Years of Age Age at First Dose Total Number of 0.5 mL Doses - * The first 2 doses at least 4 weeks apart; third dose after the one-year birthday, separated from the second dose by at least 2 months.
- † Two doses at least 2 months apart.
7–11 months of age 3* 12–23 months of age 2† 24 months through 5 years of age (prior to the 6th birthday) 1 The immune responses induced by this catch-up schedule may result in lower antibody concentrations for some serotypes, compared to antibody concentrations following 4 doses of Prevnar 13 (given at 2, 4, 6, and 12–15 months). In children 24 months through 5 years of age, lower antibody concentrations were observed for some serotypes, compared to antibody concentrations following 3 doses of Prevnar 13 (given at 2, 4, and 6 months).
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Severe allergic reaction (e.g., anaphylaxis) to any component of Prevnar 13 or any diphtheria toxoid-containing vaccine [see Description (11)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Management of Allergic Reactions
Epinephrine and other appropriate agents used to manage immediate allergic reactions must be immediately available should an acute anaphylactic reaction occur following administration of Prevnar 13.
5.2 Altered Immunocompetence
Individuals with altered immunocompetence, including those at higher risk for invasive pneumococcal disease (e.g., individuals with congenital or acquired splenic dysfunction, HIV infection, malignancy, hematopoietic stem cell transplant, nephrotic syndrome), may have reduced antibody responses to immunization with Prevnar 13 [see Use in Specific Populations (8.6)].
5.3 Apnea in Premature Infants
Apnea following intramuscular vaccination has been observed in some infants born prematurely. Decisions about when to administer an intramuscular vaccine, including Prevnar 13, to infants born prematurely should be based on consideration of the individual infant's medical status and the potential benefits and possible risks of vaccination.
-
6 ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse-reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
6.1 Clinical Trials Experience With Prevnar 13 in Children 6 Weeks Through 17 Years of Age
The safety of Prevnar 13 was evaluated in 13 clinical trials in which 4,729 infants (6 weeks through 11 months of age) and toddlers (12 months through 15 months of age) received at least one dose of Prevnar 13 and 2,760 infants and toddlers received at least one dose of Prevnar active control. Safety data for the first three doses are available for all 13 infant studies; dose 4 data are available for 10 studies; and data for the 6-month follow-up are available for 7 studies. The vaccination schedule and concomitant vaccinations used in these infant trials were consistent with country-specific recommendations and local clinical practice. There were no substantive differences in demographic characteristics between the vaccine groups. By race, 84.0% of subjects were White, 6.0% were Black or African-American, 5.8% were Asian and 3.8% were of 'Other' race (most of these being biracial). Overall, 52.3% of subjects were male infants.
Three studies in the US (Studies 1, 2 and 3)1,2,3 evaluated the safety of Prevnar 13 when administered concomitantly with routine US pediatric vaccinations at 2, 4, 6, and 12–15 months of age. Solicited local and systemic adverse reactions were recorded daily by parents/guardians using an electronic diary for 7 consecutive days following each vaccination. For unsolicited adverse events, study subjects were monitored from administration of the first dose until one month after the infant series, and for one month after the administration of the toddler dose. Information regarding unsolicited and serious adverse events, newly diagnosed chronic medical conditions, and hospitalizations since the last visit were collected during the clinic visit for the fourth-study dose and during a scripted telephone interview 6 months after the fourth-study dose. Serious adverse events were also collected throughout the study period. Overall, the safety data show a similar proportion of Prevnar 13 and Prevnar subjects reporting serious adverse events. Among US study subjects, a similar proportion of Prevnar 13 and Prevnar recipients reported solicited local and systemic adverse reactions as well as unsolicited adverse events.
Serious Adverse Events in All Infant and Toddler Clinical Studies
Serious adverse events were collected throughout the study period for all 13 clinical trials. This reporting period is longer than the 30-day post-vaccination period used in some vaccine trials. The longer reporting period may have resulted in serious adverse events being reported in a higher percentage of subjects than for other vaccines. Serious adverse events reported following vaccination in infants and toddlers occurred in 8.2% among Prevnar 13 recipients and 7.2% among Prevnar recipients. Serious adverse events observed during different study periods for Prevnar 13 and Prevnar respectively were: 1) 3.7% and 3.5% from dose 1 to the blood draw approximately 1 month after the infant series; 2) 3.6% and 2.7% from the blood draw after the infant series to the toddler dose; 3) 0.9% and 0.8% from the toddler dose to the blood draw approximately 1 month after the toddler dose and 4) 2.5% and 2.8% during the 6 month follow-up period after the last dose.
The most commonly reported serious adverse events were in the 'Infections and infestations' system organ class including bronchiolitis (0.9%, 1.1%), gastroenteritis, (0.9%, 0.9%), and pneumonia (0.9%, 0.5%) for Prevnar 13 and Prevnar respectively.
There were 3 (0.063%) deaths among Prevnar 13 recipients, and 1 (0.036%) death in Prevnar recipients, all as a result of sudden infant death syndrome (SIDS). These SIDS rates are consistent with published age specific background rates of SIDS from the year 2000.
Among 6,839 subjects who received at least 1 dose of Prevnar 13 in clinical trials conducted globally, there was 1 hypotonic-hyporesponsive episode adverse reaction reported (0.015%). Among 4,204 subjects who received at least 1 dose of Prevnar in clinical trials conducted globally, there were 3 hypotonic-hyporesponsive episode adverse reactions reported (0.071%). All 4 events occurred in a single clinical trial in Brazil in which subjects received whole cell pertussis vaccine at the same time as Prevnar 13 or Prevnar.
Solicited Adverse Reactions in the Three US Infant and Toddler Studies
A total of 1,907 subjects received at least 1 dose of Prevnar 13 and 701 subjects received at least 1 dose of Prevnar in the three US studies (Studies 1, 2 and 3)1,2,3. Most subjects were White (77.3%), 14.2% were Black or African-American, and 1.7% were Asian; 79.1% of subjects were non-Hispanic and non-Latino and 14.6% were Hispanic or Latino. Overall, 53.6% of subjects were male infants.
The incidence and severity of solicited adverse reactions that occurred within 7 days following each dose of Prevnar 13 or Prevnar administered to US infants and toddlers are shown in Tables 3 and 4.
Table 3: Percentage of US Infant and Toddler Subjects Reporting Solicited Local Reactions at the Prevnar 13 or Prevnar Injection Sites Within 7 Days After Each Vaccination at 2, 4, 6, and 12–15 Months of Age* Dose 1 Dose 2 Dose 3 Dose 4 Graded Local Reaction Prevnar 13
(N†=1375–1612)
%Prevnar
(N†=516–606)
%Prevnar 13
(N†=1069–1331)
%Prevnar
(N†=405–510)
%Prevnar 13
(N†=998–1206)
%Prevnar
(N†=348–446)
%Prevnar 13
(N†=874–1060)
%Prevnar
(N†=283–379)
%- * Data are from three primary US safety studies (the US Phase 2 infant study [National Clinical Trial (NCT) number NCT00205803] Study 1, the US noninferiority study [NCT00373958] Study 2, and the US lot consistency study [NCT00444457] Study 3). All infants received concomitant routine infant immunizations. Concomitant vaccines and pneumococcal conjugate vaccines were administered in different limbs.
- † Number of subjects reporting Yes for at least 1 day or No for all days.
- ‡ Diameters were measured in caliper units of whole numbers from 1 to 14 or 14+. One caliper unit = 0.5 cm. Measurements were rounded up to the nearest whole number. Intensity of induration and erythema were then characterized as Mild (0.5–2.0 cm), Moderate (2.5–7.0 cm), or Severe (>7.0 cm).
- § Statistically significant difference p <0.05. No adjustments for multiplicity.
Redness‡ Any 24.3 26.0 33.3 29.7 37.1 36.6 42.3 45.5 Mild 23.1 25.2 31.9 28.7 35.3 35.3 39.5 42.7 Moderate 2.2 1.5 2.7 2.2 4.6 5.1 9.6 13.4§ Severe 0 0 0 0 0 0 0 0 Swelling‡ Any 20.1 20.7 25.2 22.5 26.8 28.4 31.6 36.0§ Mild 17.2 18.7 23.8 20.5 25.2 27.5 29.4 33.8 Moderate 4.9 3.9 3.7 4.9 3.8 5.8 8.3 11.2§ Severe 0 0 0.1 0 0 0 0 0 Tenderness Any 62.5 64.5 64.7 62.9 59.2 60.8 57.8 62.5 Interferes with limb movement 10.4 9.6 9.0 10.5 8.4 9.0 6.9 5.7 Table 4: Percentage of US Infant and Toddler Subjects Reporting Solicited Systemic Adverse Reactions Within 7 Days After Each Vaccination at 2, 4, 6, and 12–15 Months of Age*,† Dose 1 Dose 2 Dose 3 Dose 4 Graded Systemic Events Prevnar 13
(N*=1360 – 1707)
%Prevnar
(N*=497–640)
%Prevnar 13
(N*=1084–1469)
%Prevnar
(N*=409–555)
%Prevnar 13
(N*=997–1361)
%Prevnar
(N*=354–521)
%Prevnar 13
(N*=850–1227)
%Prevnar
(N*=278–436)
%- * Number of subjects reporting Yes for at least 1 day or No for all days.
- † Data are from three primary US safety studies (the US Phase 2 infant study [NCT00205803] Study 1, the US noninferiority study [NCT00373958] Study 2, and the US lot consistency study [NCT00444457] Study 3). All infants received concomitant routine infant immunizations. Concomitant vaccines and pneumococcal conjugate vaccines were administered in different limbs.
- ‡ Fever gradings: Mild (≥38°C but ≤39°C), Moderate (>39°C but ≤40°C), and Severe (>40°C). No other systemic event other than fever was graded. Parents reported the use of antipyretic medication to treat or prevent symptoms in 62 to 75% of subjects after any of the 4 doses. There were no statistical differences in frequencies of adverse reactions reported between the Prevnar 13 and Prevnar groups.
Fever‡ Any 24.3 22.1 36.5 32.8 30.3 31.6 31.9 30.6 Mild 23.6 21.7 34.9 31.6 29.1 30.2 30.3 30.0 Moderate 1.1 0.6 3.4 2.8 4.2 3.3 4.4 4.6 Severe 0.1 0.2 0.1 0.3 0.1 0.7 1.0 0 Decreased appetite 48.3 43.6 47.8 43.6 47.6 47.6 51.0 49.4 Irritability 85.6 83.6 84.8 80.4 79.8 80.8 80.4 77.8 Increased sleep 71.5 71.5 66.6 63.4 57.7 55.2 48.7 55.1 Decreased sleep 42.5 40.6 45.6 43.7 46.5 47.7 45.3 40.3 The incidence rates of any fever (≥38.0°C) were similar on days 1 and 2 following each dose of Prevnar 13 compared to after each dose of Prevnar administered to US infants and toddlers (day 1 = day of vaccination). After dose 1, fever was reported in 11.0–12.7% on day 1 and 6.4–6.8% on day 2. After dose 2, fever was reported in 12.3–13.1% on day 1 and 12.5–12.8% on day 2. After dose 3, fever was reported in 8.0–9.6% on day 1 and 9.1–10.5% on day 2. And after dose 4, fever was reported in 6.3–6.4% on day 1 and 7.3–9.7% on day 2.
Unsolicited Adverse Reactions in the Three US Infant and Toddler Safety Studies
The following were determined to be adverse drug reactions based on experience with Prevnar 13 in clinical trials.
Reactions occurring in greater than 1% of infants and toddlers: diarrhea, vomiting, and rash.
Reactions occurring in less than 1% of infants and toddlers: crying, hypersensitivity reaction (including face edema, dyspnea, and bronchospasm), seizures (including febrile seizures), and urticaria or urticaria-like rash.
Safety Assessments in the Catch-Up Studies in Infants and Children Through 5 Years of Age
In a catch-up study4 conducted in Poland (Study 4), 354 children (7 months through 5 years of age) receiving at least one dose of Prevnar 13 were also monitored for safety. All subjects in this study were White and non-Hispanic. Overall, 49.6% of subjects were male infants. The incidence and severity of solicited adverse reactions that occurred within 4 days following each dose of Prevnar 13 administered to pneumococcal-vaccine naïve children 7 months through 5 years of age are shown in Tables 5 and 6.
Table 5: Percentage of Subjects 7 Months Through 5 Years of Age Reporting Solicited Local Reactions Within 4 Days After Each Catch-Up Prevnar 13 Vaccination* 7 through 11 months 12 through 23 months 24 months through 5 years Graded Local Reaction Dose 1
N†=86
%Dose 2
N†=86–87
%Dose 3
N†=78–82
%Dose 1
N†=108–110
%Dose 2
N†=98–106
%Dose 1
N†=147–149
%- * Study conducted in Poland (NCT00452452) Study 4.
- † Number of subjects reporting Yes for at least 1 day or No for all days.
- ‡ Diameters were measured in caliper units of whole numbers from 1 to 14 or 14+. One caliper unit = 0.5 cm. Measurements were rounded up to the nearest whole number. Intensity of redness and swelling were then characterized as Mild (0.5–2.0 cm), Moderate (2.5–7.0 cm), or Severe (>7.0 cm).
Redness‡ Any 48.8 46.0 37.8 70.0 54.7 50.0 Mild 41.9 40.2 31.3 55.5 44.7 37.4 Moderate 16.3 9.3 12.5 38.2 25.5 25.7 Severe 0.0 0.0 0.0 0.0 0.0 0.0 Swelling‡ Any 36.0 32.2 25.0 44.5 41.0 36.9 Mild 32.6 28.7 20.5 36.7 36.2 28.2 Moderate 11.6 14.0 11.3 24.8 12.1 20.3 Severe 0.0 0.0 0.0 0.0 0.0 0.0 Tenderness Any 15.1 15.1 15.2 33.3 43.7 42.3 Interferes with limb movement 1.2 3.5 6.4 0.0 4.1 4.1 Table 6: Percentage of Subjects 7 Months Through 5 Years of Age Reporting Solicited Systemic Adverse Reactions Within 4 Days After Each Catch-Up Prevnar 13 Vaccination* 7 through 11 months 12 through 23 months 24 months through 5 years Systemic Reaction Dose 1
N†=86–87
%Dose 2
N†=86–87
%Dose 3
N†=78–81
%Dose 1
N†=108
%Dose 2
N†=98–100
%Dose 1
N†=147–148
%- * Study conducted in Poland (NCT00452452) Study 4.
- † Number of subjects reporting Yes for at least 1 day or No for all days.
- ‡ Fever gradings: Mild (≥38°C but ≤39°C), Moderate (>39°C but ≤40°C), and Severe (>40°C). No other systemic event other than fever was graded.
Fever‡ Mild 3.4 8.1 5.1 3.7 5.1 0.7 Moderate 1.2 2.3 1.3 0.9 0.0 0.7 Severe 0.0 0.0 0.0 0.0 0.0 0.0 Decreased appetite 19.5 17.2 17.5 22.2 25.5 16.3 Irritability 24.1 34.5 24.7 30.6 34.0 14.3 Increased sleep 9.2 9.3 2.6 13.0 10.1 11.6 Decreased sleep 24.1 18.4 15.0 19.4 20.4 6.8 A US study5 (Study 5) evaluated the use of Prevnar 13 in children previously immunized with Prevnar. In this open label trial, 596 healthy children 15 through 59 months of age previously vaccinated with at least 3 doses of Prevnar, received 1 or 2 doses of Prevnar 13. Children 15 months through 23 months of age (group 1) received 2 doses, and children 24 months through 59 months of age (group 2) received one dose. Most subjects were White (74.3%), 14.9% were Black or African-American, and 1.2% were Asian; 89.3% of subjects were non-Hispanic and non-Latino and 10.7% were Hispanic or Latino. Overall, 52.2% of subjects were male.
The incidence and severity of solicited adverse reactions that occurred within 7 days following one dose of Prevnar 13 administered to children 15 months through 59 months of age are shown in Tables 7 and 8.
Table 7: Percentage of Subjects 15 Months Through 59 Months of Age, Previously Vaccinated With 3 or 4 Prior Infant Doses of Prevnar, Reporting Solicited Local Reactions Within 7 Days After One Supplemental Prevnar 13 Vaccination* 15 months through 23 months† 24 months through 59 months‡ Graded Local Reaction 1 dose Prevnar 13
3 prior Prevnar doses
N§=67–72
%1 dose Prevnar 13
4 prior Prevnar doses
N§=154–184
%1 dose Prevnar 13
3 or 4 prior Prevnar doses
N§=209–238
%- * Study conducted in US NCT00761631 (Study 5).
- † Dose 2 data not shown.
- ‡ The data for this age group are only represented as a single result as 95% of children received 4 doses of Prevnar prior to enrollment.
- § Number of subjects reporting Yes for at least 1 day or No for all days.
- ¶ Diameters were measured in caliper units of whole numbers from 1 to 14 or 14+. One caliper unit = 0.5 cm. Measurements were rounded up to the nearest whole number. Intensity of redness and swelling were then characterized as Mild (0.5–2.0 cm), Moderate (2.5–7.0 cm), or Severe (>7.0 cm).
Redness¶ Any 26.4 28.2 35.4 Mild 18.8 24.3 31.1 Moderate 11.4 7.5 12.1 Severe 1.5 0.0 0.0 Swelling¶ Any 23.9 19.6 20.7 Mild 18.6 16.4 17.2 Moderate 8.8 8.1 7.5 Severe 0.0 0.0 0.0 Tenderness Any 48.6 47.3 62.6 Interferes with limb movement 5.9 6.4 10.7 Table 8: Percentage of Subjects 15 Months Through 59 Months of Age, Previously Vaccinated With 3 or 4 Prior Infant Prevnar Doses, Reporting Solicited Systemic Adverse Reactions Within 7 Days After One Supplemental Prevnar 13 Vaccination* 15 through 23 months† 24 months through 59 months‡ Systemic Reaction 1 dose Prevnar 13
3 prior Prevnar doses
N§=66–75
%1 dose Prevnar 13
4 prior Prevnar doses
N§=154–189
%1 dose Prevnar 13
3 or 4 prior Prevnar doses
N§=209–236
%- * Study conducted in US NCT00761631 (Study 5).
- † Dose 2 data not shown.
- ‡ The data for this age group are only represented as a single result as 95% of children received 4 doses of Prevnar prior to enrollment.
- § Number of subjects reporting Yes for at least 1 day or No for all days.
- ¶ Fever gradings: Mild (≥38°C but ≤39°C), Moderate (>39°C but ≤40°C), and Severe (>40°C). No other systemic event other than fever was graded.
Fever¶ Any 19.1 19.9 8.1 Mild 16.2 17.4 7.6 Moderate 6.1 3.9 1.9 Severe 0.0 0.0 0.5 Decreased appetite 44.4 39.3 28.1 Irritability 73.3 65.1 45.8 Increased sleep 35.2 35.3 18.8 Decreased sleep 25.0 29.7 14.8 Clinical Trials Experience With Prevnar 13 in Children 5 Through 17 Years of Age
In a US study5 (Study 5), the safety of Prevnar 13 was evaluated in children 5 through 9 years of age previously immunized with at least one dose of Prevnar, and in children 10 through 17 years of age with no prior pneumococcal vaccination. In this open label trial, 592 children, including those with asthma, received a single dose of Prevnar 13. The percentage of children 5 through 9 years of age who received 3 and 4 prior doses of Prevnar was 29.1% and 54.5% respectively.
Most subjects were White (72.8%), 21.8% were Black or African-American, and 1.5% were Asian; 91.4% of subjects were non-Hispanic and non-Latino and 8.6% were Hispanic or Latino. Overall, 51.2% of subjects were male.
The incidence and severity of solicited adverse reactions that occurred within 7 days following one dose of Prevnar 13 administered to children 5 through 17 years of age are shown in Tables 9 and 10.
Table 9: Percentage of Subjects 5 Through 17 Years of Age, Reporting Solicited Local Reactions Within 7 Days After Prevnar 13 Vaccination * Vaccine Group (as Administered) Prevnar 13
(5 Through 9 Years)Prevnar 13
(10 Through 17 Years)Local Reaction N† n‡ % N† n‡ % - * Study conducted in US NCT00761631 (Study 5).
- † N = number of subjects reporting Yes for at least 1 day or No for all days.
- ‡ n = Number of subjects reporting the specific characteristic.
- § Mild, 0.5 – 2.0 cm; moderate, 2.5 – 7.0 cm; severe, >7.0 cm.
- ¶ Significant = present and interfered with limb movement.
Redness Any 233 100 42.9 232 70 30.2 Mild§ 226 63 27.9 226 48 21.2 Moderate§ 218 48 22.0 221 31 14.0 Severe§ 212 7 3.3 213 4 1.9 Swelling Any 226 85 37.6 233 86 36.9 Mild§ 220 48 21.8 221 50 22.6 Moderate§ 219 48 21.9 226 48 21.2 Severe§ 211 7 3.3 214 4 1.9 Tenderness Any 265 230 86.8 283 252 89.0 Significant¶ 221 43 19.5 242 106 43.8 Table 10: Percentage of Subjects 5 Through 17 Years of Age, Reporting Solicited Systemic Adverse Reactions Within 7 Days After Prevnar 13 Vaccination* Vaccine Group (as Administered) Prevnar 13
(5 Through 9 Years)Prevnar 13
(10 Through 17 Years)Systemic Event N† n‡ % N† n‡ % - * Study conducted in US NCT00761631 (Study 5).
- † N = number of subjects reporting Yes for at least 1 day or No for all days.
- ‡ n = Number of subjects reporting the event.
- § Fever gradings: Mild (≥38°C but ≤39°C), Moderate (>39°C but ≤40°C), and Severe (>40°C). No other systemic event other than fever was graded. Parents reported the use of antipyretic medication to treat or prevent symptoms in 45.1% and 33.1% of subjects 5 through 9 years of age and 10 through 17 years of age, respectively.
Any fever ≥38°C 214 13 6.1 214 12 5.6 Mild§ 212 9 4.2 214 11 5.1 Moderate§ 212 5 2.4 212 1 0.5 Severe§ 210 1 0.5 212 1 0.5 Decreased appetite 227 52 22.9 223 51 22.9 Irritability 234 73 31.2 234 59 25.2 Increased sleep 226 48 21.2 229 61 26.6 Decreased sleep 212 12 5.7 224 42 18.8 Hives (urticaria) 213 4 1.9 214 3 1.4 6.2 Clinical Trials Experience With Prevnar 13 in Adults ≥18 Years of Age
The safety of Prevnar 13 was assessed in 7 clinical studies (Studies 6–12) 6–12 conducted in the US and Europe which included 91,593 adults (48,806 received Prevnar 13) ranging in age from 18 through 101 years.
The 48,806 Prevnar 13 recipients included 899 adults who were aged 18 through 49 years, 2,616 adults who were aged 50 through 64 years, 45,291 adults aged 65 years and older. Of the 48,806 Prevnar 13 recipients, 46,890 adults had not previously received Pneumovax® 23 (pneumococcal polysaccharide vaccine [23-valent], PPSV23) ("PPSV23 unvaccinated") and 1,916 adults were previously vaccinated ("PPSV23 previously vaccinated") with PPSV23 at least 3 years prior to enrollment.
Safety and Immunogenicity Studies
Safety and immunogenicity of Prevnar 13 is supported by 6 clinical studies. Study 66 evaluated the safety and immunogenicity of Prevnar 13 in adults 18 through 64 years of age who had not received a previous dose of pneumococcal vaccine. Adults 18 through 59 years of age received a single dose of Prevnar 13, and adults 60 through 64 years of age received a single dose of Prevnar 13 or PPSV23.
Study 7 was randomized and compared the safety and immunogenicity of Prevnar 13 with PPSV23 as a single dose in adults ≥70 years vaccinated with PPSV23 (≥5 years prior to enrollment).7 Study 8 was randomized and evaluated the safety and immunogenicity of Prevnar 13 and PPSV23 in different sequential order in PPSV23 naive adults aged 60 through 64 years8.
One clinical safety study9 (Study 9) of Prevnar 13, conducted in PPSV23 previously vaccinated (≥3 years prior to enrollment) adults aged ≥68 years was a single arm study. Two studies, one in the US10 (Study 10) in adults aged 50 through 59 years and the other in Europe11 (Study 11) in adults aged ≥65 years, evaluated the concomitant administration of Prevnar 13 with inactivated influenza vaccine, trivalent (Fluarix®, A/H1N1, A/H3N2, and B, Fall 2007/Spring 2008: IIV3) in these two age groups in PPSV23 unvaccinated adults.
The total safety population in the 6 safety and immunogenicity studies was 7,097. In 5 of the 6 safety and immunogenicity studies, more females than males were enrolled (50.2% – 61.8%). Across the 6 studies the racial distribution included: >85% White; 0.2%–10.7% Black or African American; 0%–1.7% Asian; <1% Native Hawaiian or other Pacific Islander; ≤1%, American Indian or Alaskan Native. Ethnicity data were not collected in Study 11; in the 5 other studies 0.6%–4.8% were Hispanic or Latino.
In five studies,6–8,10,11 subjects with pre-existing underlying diseases were enrolled if the medical condition was stable (did not require a change in therapy or hospitalization for worsening disease for 12 weeks before receipt of study vaccine) except in Study 9 where subjects were enrolled if the medical condition was stable for 6 or more weeks before receipt of study vaccine.
In the 6 safety and immunogenicity studies,6–11 subjects were excluded from study participation due to prior receipt of diphtheria toxoid-containing vaccines within 6 months of study vaccine. However, the time of prior receipt of a diphtheria toxoid-containing vaccine was not recorded.
Solicited adverse reactions for Prevnar 13 in the safety and immunogenicity studies were monitored by subjects recording local adverse reactions and systemic reactions daily using an electronic diary for 14 consecutive days following vaccination. Unsolicited serious and non-serious adverse events were collected for one month after each vaccination. In addition, serious adverse events were collected for an additional 5 months after each vaccination (at the 6-month follow-up phone contact) in all studies except Study 11.
Following licensure of Prevnar 13 in adults ≥50 years of age, a randomized, double-blind, placebo-controlled US study (Study 13) was conducted to evaluate concomitant administration of Prevnar 13 with inactivated influenza vaccine, quadrivalent (Fluzone® Quadrivalent, A/H1N1, A/H3N2, B/Brisbane, and B/Massachusetts, Fall 2014/Spring 2015: IIV4) in PPSV23 previously vaccinated adults ≥50 years of age. Unsolicited serious and non-serious adverse events were collected as described above for Studies 6–10.
Efficacy Study
Study 1212 was a randomized double-blind placebo-controlled study conducted in the Netherlands in community-dwelling adults aged 65 years and older with no prior pneumococcal vaccination history. A total of 84,496 subjects received either a single dose of Prevnar 13 (42,240) or placebo (42,256) in a 1:1 randomization. Among the 84,496 subjects, 58,072 (68.7%) were ≥65 to <75 years of age, 23,481 (27.8%) were ≥75 and <85 years of age, and 2,943 (3.5%) were ≥85 years of age. In the total safety population, more males (55.9%) were enrolled than females. The racial distribution was 98.5% White, 0.3% Black, 0.7% Asian, 0.5% Other, with <0.1% having missing data.
Adults with immunocompromising conditions or receiving immunosuppressive therapy and adults residing in a long-term care facility or requiring semiskilled nursing care were excluded. Adults with pre-existing medical conditions, as well as subjects with a history of smoking were eligible for enrollment. In the safety population, 42.3% of subjects had pre-existing medical conditions including heart disease (25.4%), lung disease or asthma (15.1%) and type 1 and type 2 diabetes mellitus (12.5%). Smoking was reported at baseline by 12.3% of the subjects.
For a subset of 2,011 subjects (1,006 Prevnar 13 recipients and 1,005 placebo recipients), solicited adverse reactions were monitored by recording local and systemic events using electronic diaries for 7 days after vaccination; unsolicited adverse events were collected for 28 days after vaccination, and serious adverse events were collected for 6 months after vaccination. For the remaining 41,231 Prevnar 13 and 41,250 placebo vaccinated subjects, serious adverse events were collected for 28 days after vaccination.
Serious Adverse Events in Adult Clinical Studies
Safety and Immunogenicity Studies
Across the 6 safety and immunogenicity studies,6–11 serious adverse events within 1 month of vaccination were reported after an initial study dose in 0.2%–1.4% of 5,057 subjects vaccinated with Prevnar 13, and in 0.4%–1.7% of 1,124 subjects vaccinated after an initial study dose of PPSV23. From 1 month to 6 months after an initial study dose, serious adverse events were reported in 0.2%–5.8% of subjects vaccinated during the studies with Prevnar 13 and in 2.4%–5.5% of subjects vaccinated with PPSV23. One case of erythema multiforme occurred 34 days after receipt of a second dose of Prevnar 13.
Twelve of 5,667 (0.21%) Prevnar 13 recipients and 4 of 1,391 (0.29 %) PPSV23 recipients died. Deaths occurred between Day 3 and Day 309 after study vaccination with Prevnar 13 or PPSV23. Two of 12 deaths occurred within 30 days of vaccination and both deaths were in subjects >65 years of age. One death due to cardiac failure occurred 3 days after receiving placebo. This subject had received Prevnar 13 and IIV3 one month earlier. The other death was due to peritonitis 20 days after receiving Prevnar 13. The reported causes of the 10 remaining deaths occurring greater than 30 days after receiving Prevnar 13 were cardiac disorders (4), neoplasms (4), Mycobacterium avium complex pulmonary infection (1) and septic shock (1).
Efficacy Study
In Study 1212 (subjects 65 years and older), serious adverse events within 1 month of vaccination were reported in 327 of 42,237 (0.8%) Prevnar 13 recipients (352 events) and in 314 of 42,225 (0.7%) placebo recipients (337 events). In the subset of subjects where serious adverse events were monitored for 6 months, 70 of 1,006 (7%) Prevnar 13 vaccinated subjects (90 events) and 60 of 1,005 (6%) placebo vaccinated subjects (69 events) reported serious adverse events.
During the follow-up period (average of 4 years) for case accumulation there were 3,006 deaths (7.1%) in the Prevnar 13 group and 3,005 deaths (7.1%) in the placebo group. There were 10 deaths (<0.1%) in the Prevnar 13 group and 10 deaths (<0.1%) in the placebo group within 28 days of vaccination. There were 161 deaths (0.4%) in the Prevnar 13 group and 144 deaths (0.3%) in the placebo group within 29 days – 6 months following vaccination. These data do not provide evidence for a causal relationship between deaths and vaccination with Prevnar 13.
Solicited Adverse Reactions in Adult Clinical Studies
The incidence and severity of solicited adverse reactions that occurred within 7 or 14 days following each dose of Prevnar 13, PPSV23, or placebo administered to adults in 5 studies are shown in Tables 11, 12, 13, and 14.
The commonly reported local adverse reactions after Prevnar 13 vaccination in PPSV23 unvaccinated and PPSV23 previously vaccinated adults were redness, swelling and pain at the injection site, or limitation of arm movement (Tables 11 and 12). The commonly reported systemic adverse reactions in PPSV23 unvaccinated and PPSV23 previously vaccinated adults were fatigue, headache, chills, rash, decreased appetite, or muscle pain and joint pain (Tables 13 and 14).
Table 11 - Percentage of Subjects With Solicited Local Adverse Reactions Within 7 or 14 Days in PPSV23 Unvaccinated Adults* Study 6 Study 8 Study 12 Age in Years 18–49 50–59 60–64 60–64 ≥65 Local Reaction Prevnar 13†
N‡=266–787
%Prevnar 13†
N‡=152–322
%Prevnar 13
N‡=193–331
%PPSV23
N‡=190–301
%Prevnar 13
N‡=270–370
%PPSV23
N‡=134–175
%Prevnar 13
N‡=886–914
%Placebo
N‡=859–865
%- * Studies conducted in US NCT00427895 (Study 6) and NCT00574548 (Study 8) reported local reactions within 14 days. Study conducted in the Netherlands NCT00744263 (Study 12) reported local reactions within 7 days.
- † Open label administration of Prevnar 13.
- ‡ Number of subjects with known values (number of subjects reporting yes for at least one day or no for all days).
- § Diameters were measured in caliper units of whole numbers from 1 to 21 or 21+. One caliper unit = 0.5 cm. Measurements were rounded up to the nearest whole number. Intensity of redness and swelling were then characterized as Mild = 2.5 to 5.0 cm, Moderate = 5.1 to 10.0 cm, and Severe is >10.0 cm.
- ¶ Statistically significant difference p <0.05. No adjustments for multiplicity.
- # Mild = awareness of symptom but easily tolerated, Moderate = discomfort enough to cause interference with usual activity, Severe = incapacitating with inability to do usual activity.
- Þ Mild = some limitation of arm movement, Moderate = unable to move arm above head but able to move arm above shoulder, and Severe = unable to move arm above shoulder.
Redness§ Any 30.5 15.8 20.2 14.2 12.2 11.2 4.9¶ 1.2 Mild 26.4 15.2 15.9 11.2 8.3 9.7 3.7¶ 0.8 Moderate 11.9 5.0 8.6 4.9 6.4 3.9 1.7¶ 0.3 Severe 2.8 0.7 1.7 0.0 1.2 0.8 0.5 0.1 Swelling§ Any 39.4 21.7 19.3 13.1 10.0 10.4 6.8¶ 1.2 Mild 37.2 20.6 15.6 10.1 8.2 6.1 5.5¶ 0.7 Moderate 15.1 4.3 8.2 4.4 3.8 7.6 2.6¶ 0.6 Severe 1.4 0.0 0.6 1.1 0.0 0.0 0.1 0.1 Pain# Any 96.7 88.8 80.1 73.4 69.2¶ 58.3 36.1¶ 6.1 Mild 93.2 85.9 78.6¶ 68.6 66.1¶ 52.9 32.9¶ 5.6 Moderate 77.1 39.5 23.3 30.0 20.1 21.7 7.7¶ 0.6 Severe 16.0 3.6 1.7 8.6¶ 2.3 0.8 0.3 0.1 Limitation of arm movementÞ Any 75.2 40.7 28.5 30.8 23.5 28.2 14.1¶ 3.2 Mild 71.5 38.6 26.9 29.3 22.7 26.1 12.4¶ 2.5 Moderate 18.5 2.9 2.2 3.8 1.2 3.1 1.7¶ 0.5 Severe 15.6 2.9 1.7 4.3 1.1 2.3 1.2 0.7 Table 12 - Percentage of Subjects With Solicited Local Adverse Reactions in PPSV23 Previously Vaccinated Adults* Study 7 Study 9 Age in Years ≥70 ≥68 Local Reaction Prevnar 13
N†=306–362
%PPSV23
N†=324–383
%Prevnar 13‡
N†=664–777
%- * Study conducted in US and Sweden NCT00546572 (Study 7) reported local reactions within 14 days. Study conducted in US, Sweden and Germany NCT00500266 (Study 9) reported local reactions within 14 days.
- † Number of subjects with known values.
- ‡ Open label administration of Prevnar 13.
- § Diameters were measured in caliper units of whole numbers from 1 to 21 or 21+. One caliper unit = 0.5 cm. Measurements were rounded up to the nearest whole number. Intensity of redness and swelling were then characterized as Mild = 2.5 to 5.0 cm, Moderate = 5.1 to 10.0 cm, and Severe is >10.0 cm.
- ¶ Statistically significant difference p <0.05. No adjustments for multiplicity.
- # Mild = awareness of symptom but easily tolerated, Moderate = discomfort enough to cause interference with usual activity, Severe = incapacitating with inability to do usual activity.
- Þ Mild = some limitation of arm movement, Moderate = unable to move arm above head but able to move arm above shoulder, and Severe = unable to move arm above shoulder.
Redness§ Any 10.8 22.2¶ 14.3 Mild 9.5 13.5 12.6 Moderate 4.7 11.5¶ 6.5 Severe 1.7 4.8¶ 1.1 Swelling§ Any 10.4 23.1¶ 12.8 Mild 8.9 14.0¶ 10.9 Moderate 4.0 13.6¶ 5.5 Severe 0.0 4.8¶ 0.6 Pain# Any 51.7 58.5 51.0 Mild 50.1 54.1 49.4 Moderate 7.5 23.6¶ 9.0 Severe 1.3 2.3 0.2 Limitation of arm movementÞ Any 10.5 27.6¶ 16.2 Mild 10.3 25.2¶ 14.8 Moderate 0.3 2.6¶ 1.6 Severe 0.7 3.0¶ 1.6 Table 13 - Percentage of Subjects With Solicited Systemic Events in PPSV23 Unvaccinated Adults* Study 6 Study 8 Study 12 Age in Years 18–49 50–59 60–64 60–64 ≥65 Prevnar 13†
N‡=221–561
%Prevnar 13†
N‡=137–248
%Prevnar 13
N‡=174–277
%PPSV23
N‡=176–273
%Prevnar 13
N‡=261–328
%PPSV23
N‡=127–173
%Prevnar 13
N‡=881–896
%Placebo
N‡=860–878
%- * Studies conducted in US NCT00427895 (Study 6) and NCT00574548 (Study 8) reported systemic events within 14 days. Study conducted in the Netherlands NCT00744263 (Study 12) reported systemic events within 7 days.
- † Open label administration of Prevnar 13.
- ‡ Number of subjects with known values (number of subjects reporting yes for at least one day or no for all days).
- § Statistically significant difference p <0.05. No adjustments for multiplicity.
- ¶ Fevers >40.0°C were confirmed to be data entry errors and remain in the table for the following: 1 case in the 18- to 49- year-old cohort (Study 6), and 7 cases in the Prevnar 13 group and 3 cases in placebo group (Study 12). For the other cohorts in Study 6 and for Study 8, data entry errors were removed.
Systemic Event Fever ≥38.0°C 7.2 1.5 4.0 1.1 4.2 1.6 2.9§ 1.3 38.0°C to 38.4°C 4.2 1.5 4.0 1.1 3.8 0.8 1.1 0.6 38.5°C to 38.9°C 1.9 0.0 0.6 0.0 0.8 0.0 0.6 0.2 39.0°C to 40.0°C 1.4 0.0 0.0 0.0 0.4 0.8 0.7 0.2 >40.0°C¶ 0.5 0.0 0.0 0.0 0.0 0.0 0.8 0.3 Fatigue 80.5 63.3 63.2 61.5 50.5 49.1 18.8§ 14.8 Headache 81.4 65.9 54.0 54.4 49.7 46.1 15.9 14.8 Chills 38.1 19.6 23.5 24.1 19.9 26.9 9.4 8.4 Rash 21.3 14.2 16.5 13.0 8.6 13.4 3.3§ 0.8 Vomiting 15.0 6.9 3.9 5.4 3.1 3.1 0.3 0.9 Decreased appetite 55.6 25.3 21.3 21.7 14.7 23.0§ 5.3 3.7 Generalized new muscle pain 82.0 61.8 56.2 57.8 46.9 51.5 18.4§ 8.4 Generalized aggravated muscle pain 55.9 39.9 32.6 37.3 22.0 32.5§ 9.1§ 4.4 Generalized new joint pain 41.7 31.5 24.4 30.1 15.5 23.8§ 7.4 5.4 Generalized aggravated joint pain 28.6 25.6 24.9 21.4 14.0 21.1 5.2 4.2 Table 14 - Percentage of Subjects With Systemic Events in PPSV23 Previously Vaccinated Adults* Study 7 Study 9 Age in Years ≥70 ≥68 Prevnar 13
N†=299–350
%PPSV23
N†=303–367
%Prevnar 13‡
N†=635–733
%- * Study conducted in US and Sweden NCT00546572 (Study 7) reported systemic events within 14 days. Study conducted in US, Sweden and Germany NCT00500266 (Study 9) reported systemic events within 14 days.
- † Number of subjects with known values.
- ‡ Open label administration of Prevnar 13.
- § Statistically significant difference p <0.05. No adjustments for multiplicity.
Systemic Event Fever ≥38.0°C 1.0 2.3 1.1 38.0°C to 38.4°C 1.0 2.0 0.8 38.5°C to 38.9°C 0.0 0.0 0.0 39.0°C to 40.0°C 0.0 0.3 0.3 >40.0°C 0.0 0.0 0.0 Fatigue 34.0 43.3§ 34.4 Headache 23.7 26.0 26.1 Chills 7.9 11.2 7.5 Rash 7.3 16.4§ 8.4 Vomiting 1.7 1.3 0.9 Decreased appetite 10.4 11.5 11.2 Generalized new muscle pain 36.8 44.7§ 25.3 Generalized aggravated muscle pain 20.6 27.5§ 12.3 Generalized new joint pain 12.6 14.9 12.8 Generalized aggravated joint pain 11.6 16.5 9.7 Safety Results from Adult Clinical Study of Concomitant Administration of Prevnar 13 and IIV4 (Fluzone Quadrivalent) (Study 13)
The safety profile of Prevnar 13 when administered concomitantly with seasonal inactivated influenza vaccine, quadrivalent, to PPSV23 previously vaccinated adults ≥50 years of age was generally consistent with the known safety profile of Prevnar 13.
6.3 Post-marketing Experience With Prevnar 13 in Infants and Toddlers
The following adverse events have been reported through passive surveillance since market introduction of Prevnar 13. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to the vaccine. The following adverse events were included based on one or more of the following factors: severity, frequency of reporting, or strength of evidence for a causal relationship to Prevnar 13 vaccine.
Administration site conditions: Vaccination-site dermatitis, vaccination-site pruritus, vaccination-site urticaria
Blood and lymphatic system disorders: Lymphadenopathy localized to the region of the injection site
Cardiac disorders: Cyanosis
Immune system disorders: Anaphylactic/anaphylactoid reaction including shock
Nervous system disorders: Hypotonia
Skin and subcutaneous tissue disorders: Angioneurotic edema, erythema multiforme
Respiratory: Apnea
Vascular disorders: Pallor
-
7 DRUG INTERACTIONS
7.1 Concomitant Immunizations
In clinical trials with infants and toddlers, Prevnar 13 was administered concomitantly with the following US-licensed vaccines: Pediarix [Diphtheria and Tetanus Toxoids and Acellular Pertussis Adsorbed, Hepatitis B (Recombinant) and Inactivated Poliovirus Vaccine Combined] (DTaP-HBV-IPV) and ActHIB [Haemophilus b Conjugate Vaccine (Tetanus Toxoid Conjugate)] (PRP-T) for the first three doses and with PedvaxHIB [Haemophilus b Conjugate Vaccine (Meningococcal Protein Conjugate)] (PRP-OMP), M-M-R II [Measles, Mumps, Rubella Virus Vaccine Live] (MMR) and Varivax [Varicella Virus Vaccine Live], or ProQuad [Measles, Mumps, Rubella and Varicella Virus Vaccine Live] (MMRV) and VAQTA [Hepatitis A vaccine, Inactivated] (HepA) for dose 4 [see Clinical Studies (14.2) and Adverse Reactions (6.1)].
In children and adolescents, data are insufficient to assess the concomitant administration of Prevnar 13 with Human Papillomavirus Vaccine (HPV), Meningococcal Conjugate Vaccine (MCV4) and Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine, Adsorbed (Tdap).
In adults, Prevnar 13 was administered concomitantly with US-licensed inactivated influenza vaccines, trivalent and quadrivalent (Studies 10, 11 and 13)[see Clinical Studies (14.4) and Adverse Reactions (6.2)]. There are no data on the concomitant administration of Prevnar 13 with diphtheria toxoid-containing vaccines and other vaccines licensed for use in adults 50 years of age and older.
When Prevnar 13 is administered at the same time as another injectable vaccine(s), the vaccines should always be administered with different syringes and given at different injection sites.
Do not mix Prevnar 13 with other vaccines/products in the same syringe.
7.2 Immunosuppressive Therapies
Individuals with impaired immune responsiveness due to the use of immunosuppressive therapy (including irradiation, corticosteroids, antimetabolites, alkylating agents, and cytotoxic agents) may not respond optimally to active immunization.
7.3 Antipyretics
A post-marketing clinical study conducted in Poland using a non-US vaccination schedule (2, 3, 4, and 12 months of age) evaluated the impact of prophylactic oral acetaminophen on antibody responses to Prevnar 13. The data show that 3 doses of acetaminophen (the first dose administered at the time of each vaccination and the subsequent doses at 6 to 8 hour intervals) reduced the antibody response to some serotypes following the third dose of Prevnar 13, compared with responses among infants who received antipyretics only as needed for treatment. Reduced antibody responses were not observed after the fourth dose of Prevnar 13 when acetaminophen was administered prophylactically.
7.4 Prior Vaccination with PPSV23
Prior receipt of PPSV23 within 1 year results in diminished immune responses to Prevnar 13 compared to PPSV23 naïve individuals [see Clinical Studies (14.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Available data on Prevnar 13 administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.
A developmental toxicity study has been performed in female rabbits administered Prevnar 13 prior to mating and during gestation. Each dose was approximately 20 times the human dose. This study revealed no evidence of harm to the fetus due to Prevnar 13 (see 8.1 Data).
Data
Animal
In a developmental toxicity study, female rabbits were administered Prevnar 13 by intramuscular injection twice prior to mating (17 days and 3 days prior to mating) and twice during gestation (gestation days 10 and 24), 0.5 mL/rabbit/occasion (each dose approximately 20 times the human dose). No adverse effects on pre-weaning development were observed. There were no vaccine-related fetal malformations or variations.
8.2 Lactation
Risk Summary
Data are not available to assess the effects of Prevnar 13 on the breastfed infant or on milk production/excretion. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Prevnar 13 and any potential adverse effects on the breastfed child from Prevnar 13 or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to disease prevented by the vaccine.
8.4 Pediatric Use
Safety and effectiveness of Prevnar 13 in children below the age of 6 weeks have not been established.
8.5 Geriatric Use
Of the total number of Prevnar 13 recipients aged 50 years and older in clinical studies (N=47,907), 94.5% (45,291 of 47,907 ) were 65 years and older and 30.3 % (14,498 of 47,907) were 75 years and older [see Clinical Studies (14.1) and (14.3)].
8.6 High Risk Populations
Individuals with the diseases or conditions listed below are at increased risk of pneumococcal disease. Immunogenicity and safety data in these populations are limited.
Infants Born Prematurely
Immune responses elicited by Prevnar 13 administered on a US schedule to preterm infants have not been studied. When preterm infants (<37 weeks gestational age, N=100) were administered 4 doses of Prevnar 13 on a non-US schedule, the serotype-specific IgG antibody responses after the third and fourth dose were lower compared to responses among term infants (≥37 weeks gestational age, N=100) for some serotypes; the effectiveness of Prevnar 13 in preterm infants cannot be established from this study.
Children with Sickle Cell Disease
In an open-label, single-arm, descriptive study, 2 doses of Prevnar 13 were administered 6 months apart to children ≥6 to <18 years of age with sickle cell disease who previously received PPSV23 at least 6 months prior to enrollment. Children with a prior history of pneumococcal conjugate vaccination were excluded. For all vaccine serotypes, anti-pneumococcal opsonophagocytic activity (OPA) geometric mean antibody titers (GMTs) were higher after the first dose compared to pre-vaccination (N=95–131); OPA GMTs following the first and second dose were comparable. The effectiveness of Prevnar 13 in this specific population has not been established.
Individuals with Hematopoietic Stem Cell Transplant
In an open-label, single-arm, descriptive study, 4 doses of Prevnar 13 were administered to subjects ≥2 years of age (range 2 to 71 years) who had received an allogeneic hematopoietic stem cell transplant 3 to 6 months prior to enrollment. All subjects had a history of stable engraftment (absolute neutrophil count>1000/µL, platelet count >50,000/µL), and did not have uncontrolled graft versus host disease. The first three doses of Prevnar 13 were administered one month apart, followed by a fourth dose of Prevnar 13 six months after the third dose. Sera were obtained approximately one month after each vaccination. Immune responses (IgG GMCs) after the first dose of Prevnar 13 were numerically higher for all serotypes compared with baseline. In addition, after each subsequent dose of Prevnar 13, IgG GMCs for all serotypes were numerically higher than responses after the previous dose. A post hoc analysis of the immune responses as measured by OPA antibody assay showed the pattern of functional antibody responses to be consistent with IgG responses for each serotype. The effectiveness of Prevnar 13 in this specific population has not been established.
Individuals with HIV Infection
In an open-label, single-arm, descriptive study, 3 doses of Prevnar 13 were administered 6 months apart to HIV-infected adults ≥18 years of age (median age 48 years), with CD4 counts ≥200 cells/µL and serum HIV RNA titer <50,000 copies/mL. All subjects had been vaccinated previously with PPSV23 at least 6 months prior to enrollment. For all vaccine serotypes anti-pneumococcal OPA GMTs were numerically higher after the first dose compared to pre-vaccination (N=227–253); OPA GMTs following the first, second and third dose were generally comparable. The effectiveness of Prevnar 13 in this specific population has not been established.
In an open-label, single-arm, descriptive study, 3 doses of Prevnar 13 were administered 1 month apart to HIV-infected subjects ≥6 years of age with CD4 counts ≥200 cells/µL, and serum HIV RNA titer <50,000 copies/mL. Subjects had not previously been vaccinated with a pneumococcal vaccine. For all vaccine serotypes anti-pneumococcal OPA GMTs were numerically higher after the first dose compared to pre-vaccination (N=197–257); OPA GMTs following the first, second and third dose were generally comparable. The effectiveness of Prevnar 13 in this specific population has not been established.
-
11 DESCRIPTION
Prevnar 13, Pneumococcal 13-valent Conjugate Vaccine (Diphtheria CRM197 Protein) is a sterile suspension of saccharides of the capsular antigens of Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, and 23F, individually linked to non-toxic diphtheria CRM197 protein. Each serotype is grown in soy peptone broth. The individual polysaccharides are purified through centrifugation, precipitation, ultrafiltration, and column chromatography. The polysaccharides are chemically activated to make saccharides, which are directly conjugated by reductive amination to the protein carrier CRM197, to form the glycoconjugate. CRM197 is a nontoxic variant of diphtheria toxin isolated from cultures of Corynebacterium diphtheriae strain C7 (β197) grown in a casamino acids and yeast extract-based medium or in a chemically-defined medium. CRM197 is purified through ultrafiltration, ammonium sulfate precipitation, and ion-exchange chromatography. The individual glycoconjugates are purified by ultrafiltration and column chromatography and analyzed for saccharide to protein ratios, molecular size, free saccharide, and free protein.
The individual glycoconjugates are compounded to formulate Prevnar 13. Potency of the formulated vaccine is determined by quantification of each of the saccharide antigens and by the saccharide to protein ratios in the individual glycoconjugates. Each 0.5 mL dose of the vaccine is formulated to contain approximately 2.2 µg of each of Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 7F, 9V, 14, 18C, 19A, 19F, 23F saccharides, 4.4 μg of 6B saccharides, 34 µg CRM197 carrier protein, 100 µg polysorbate 80, 295 µg succinate buffer and 125 µg aluminum as aluminum phosphate adjuvant.
The tip cap and rubber plunger of the prefilled syringe are not made with natural rubber latex.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Prevnar 13, comprised of pneumococcal polysaccharides conjugated to a carrier protein (CRM197), elicits a T-cell dependent immune response. Protein carrier-specific T-cells provide the signals needed for maturation of the B-cell response.
Nonclinical and clinical data support opsonophagocytic activity, as measured by opsonophagocytic activity (OPA) antibody assay, as a contributor to protection against pneumococcal disease. The OPA antibody assay provides an in vitro measurement of the ability of serum antibodies to eliminate pneumococci by promoting complement-mediated phagocytosis and is believed to reflect relevant in vivo mechanisms of protection against pneumococcal disease. OPA antibody titers are expressed as the reciprocal of the highest serum dilution that reduces survival of the pneumococci by at least 50%.
In infants that have received Prevnar 13, opsonophagocytic activity correlates well with serotype specific anti-capsular polysaccharide IgG levels as measured by ELISA. A serum anti-capsular polysaccharide antibody concentration of 0.35 µg/mL as measured by ELISA one month after the third dose as a single antibody reference concentration was used to estimate the effectiveness of Prevnar 13 against invasive pneumococcal disease (IPD) in infants and children. The assay used for this determination is a standardized ELISA involving pre-absorption of the test sera with pneumococcal C-polysaccharide and serotype 22F polysaccharide to reduce non-specific background reactivity. The single antibody reference value was based on pooled efficacy estimates from three placebo-controlled IPD efficacy trials with either Prevnar or the investigational 9-valent CRM197 conjugate pneumococcal polysaccharide vaccine. This reference concentration is only applicable on a population basis and cannot be used to predict protection against IPD on an individual basis. Functional antibodies elicited by the vaccine (as measured by a dribble opsonophagocytic activity [dOPA] antibody assay) were also evaluated in infants.
In adults, an antipolysaccharide binding antibody IgG level to predict protection against invasive pneumococcal disease or non-bacteremic pneumonia has not been defined. Noninferiority trials for Prevnar 13 were designed to show that functional OPA antibody responses (as measured by a microcolony OPA [mcOPA] antibody assay) for the Prevnar 13 serotypes are noninferior and for some serotypes superior to the common serotypes in the currently licensed pneumococcal polysaccharide vaccine (PPSV23). OPA antibody titers measured in the mcOPA antibody assay cannot be compared directly to titers measured in the dOPA antibody assay.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Prevnar 13 has not been evaluated for the potential to cause carcinogenicity, genotoxicity, or impairment of male fertility. In a study in rabbits, no vaccine-related effects were found regarding reproductive performance including female fertility [see Use in Specific Populations (8.1)].
-
14 CLINICAL STUDIES
14.1 Efficacy Data
Prevnar Efficacy Data
Invasive Pneumococcal Disease (IPD)
Prevnar (Pneumococcal 7-valent Conjugate Vaccine [Diphtheria CRM'197 Protein]) was licensed in the US for infants and children in 2000, following a randomized, double-blind clinical trial in a multiethnic population at Northern California Kaiser Permanente (NCKP) from October 1995 through August 20, 1998, in which 37,816 infants were randomized to receive either Prevnar or a control vaccine (an investigational meningococcal group C conjugate vaccine [MnCC]) at 2, 4, 6, and 12–15 months of age. In this study, the efficacy of Prevnar against invasive disease due to S. pneumoniae in cases accrued during this period was 100% in both the per-protocol and intent-to-treat analyses (95% confidence interval [CI]: 75.4%, 100% and 81.7%, 100%, respectively). Data accumulated through an extended follow-up period to April 20, 1999, resulted in similar efficacy estimates of 97.4% in the per-protocol analysis and 93.9% in the intent-to-treat analysis (95% CI: 82.7%, 99.9% and 79.6%, 98.5%, respectively).
Acute Otitis Media (AOM)
The efficacy of Prevnar against otitis media was assessed in two clinical trials: a trial in Finnish infants at the National Public Health Institute and the efficacy trial in US infants at Northern California Kaiser Permanente (NCKP).
The Finnish Otitis Media (FinOM) trial was a randomized, double-blind trial in which 1,662 infants were equally randomized to receive either Prevnar or a control vaccine Recombivax HB (Hepatitis B vaccine (Recombinant) [Hep B]) at 2, 4, 6, and 12–15 months of age. In this study, conducted between December 1995 and March 1999, parents of study participants were asked to bring their children to the study clinics if the child had respiratory infections or symptoms suggesting acute otitis media (AOM). If AOM was diagnosed, tympanocentesis was performed, and the middle-ear fluid was cultured. If S. pneumoniae was isolated, serotyping was performed; the primary endpoint was efficacy against AOM episodes caused by vaccine serotypes in the per-protocol population. In the NCKP trial, the efficacy of Prevnar against otitis media was assessed from the beginning of the trial in October 1995 through April 1998. The otitis media analysis included 34,146 infants randomized to receive either Prevnar (N=17,070), or the control vaccine (N=17,076), at 2, 4, 6, and 12–15 months of age. In this trial, no routine tympanocentesis was performed, and no standard definition of otitis media was used by study physicians. The primary otitis media endpoint was efficacy against all otitis media episodes in the per-protocol population.
The vaccine efficacy against AOM episodes due to vaccine serotypes assessed in the Finnish trial, was 57% (95% CI: 44%, 67%) in the per-protocol population and 54% (95% CI: 41%, 64%) in the intent-to-treat population. The vaccine efficacy against AOM episodes due to vaccine-related serotypes (6A, 9N, 18B, 19A, 23A), also assessed in the Finnish trial, was 51% (95% CI: 27, 67) in the per-protocol population and 44% (95% CI: 20, 62) in the intent-to-treat population. There was a nonsignificant increase in AOM episodes caused by serotypes unrelated to the vaccine in the per-protocol population, compared to children who received the control vaccine, suggesting that children who received Prevnar appeared to be at increased risk of otitis media due to pneumococcal serotypes not represented in the vaccine. However, vaccination with Prevnar reduced pneumococcal otitis media episodes overall. In the NCKP trial, in which the endpoint was all otitis media episodes regardless of etiology, vaccine efficacy was 7% (95% CI: 4%, 10%) and 6% (95% CI: 4%, 9%), respectively, in the per-protocol and intent-to-treat analyses. Several other otitis media endpoints were also assessed in the two trials.
Recurrent AOM, defined as 3 episodes in 6 months or 4 episodes in 12 months, was reduced by 9% in both the per-protocol and intent-to-treat populations (95% CI: 3%, 15% in per-protocol and 95% CI: 4%, 14% in intent-to-treat) in the NCKP trial; a similar trend was observed in the Finnish trial. The NCKP trial also demonstrated a 20% reduction (95% CI: 2, 35) in the placement of tympanostomy tubes in the per-protocol population and a 21% reduction (95% CI: 4, 34) in the intent-to-treat population. Data from the NCKP trial accumulated through an extended follow-up period to April 20, 1999, in which a total of 37,866 children were included (18,925 in Prevnar group and 18,941 in MnCC control group), resulted in similar otitis media efficacy estimates for all endpoints.
Prevnar 13 Adult Efficacy Data
The efficacy of Prevnar 13 against vaccine-type (VT) pneumococcal community-acquired pneumonia (CAP) and IPD was assessed in a randomized, double-blind, placebo-controlled study conducted over ~ 4 years in the Netherlands12 (Study 12). A total of 84,496 subjects 65 years and older received a single dose of either Prevnar 13 or placebo in a 1:1 randomization; 42,240 subjects were vaccinated with Prevnar 13 and 42,256 subjects were vaccinated with placebo.
The primary objective was to demonstrate the efficacy of Prevnar 13 in the prevention of a first episode of confirmed VT-CAP (defined as presence of ≥2 specified clinical criteria; chest X-ray consistent with CAP as determined by a central committee of radiologists; and positive VT-specific Urinary Antigen Detection assay (UAD) or isolation of VT S. pneumoniae from blood or other sterile site). The secondary objectives were to demonstrate the efficacy of Prevnar 13 in the prevention of a first episode of 1) confirmed nonbacteremic/noninvasive (NB/NI) VT-CAP (an episode of VT-CAP for which the blood culture result and any other sterile site culture results were negative for S. pneumoniae) and 2) VT-IPD (the presence of S. pneumoniae in a sterile site).
Surveillance for suspected pneumonia and IPD began immediately after vaccination and continued through identification of a prespecified number of cases. Subjects who had a CAP or IPD episode with symptom onset less than 14 days after vaccination were excluded from all analyses.
The median duration of follow-up per subject was 3.93 years. Prevnar 13 demonstrated statistically significant vaccine efficacy (VE) in preventing first episodes of VT pneumococcal CAP, nonbacteremic/noninvasive (NB/NI) VT pneumococcal CAP, and VT-IPD (Table 15).
Table 15 - Vaccine Efficacy for the Primary and Secondary Efficacy Endpoints – Per-Protocol Population Vaccine Group Prevnar 13 Placebo N=42240 N=42256 Efficacy Endpoint Total Number of Episodes n n VE (%) (95.2% CI) Abbreviations: CAP = community-acquired pneumonia; CI = confidence interval; NB/NI = nonbacteremic/noninvasive; IPD = invasive pneumococcal disease; VE = vaccine efficacy; VT = vaccine-type. Primary endpoint:
First case of confirmed VT pneumococcal CAP139 49 90 45.6 (21.8, 62.5) Secondary endpoint:
First episode of confirmed NB/NI VT pneumococcal CAP93 33 60 45 (14.2, 65.3) Secondary endpoint:
First episode of VT-IPD35 7 28 75 (41.1, 90.9) 14.2 Prevnar 13 Clinical Trials in Children 6 Weeks Through 17 Years of Age
Infants and Children 6 Weeks Through 17 Months of Age
Prevnar 13 effectiveness against invasive pneumococcal disease was inferred from comparative studies to a US-licensed 7-valent pneumococcal conjugate vaccine, Prevnar, in which Prevnar 13 elicited antipolysaccharide binding and functional OPA antibodies, as measured by ELISA and dOPA assays, respectively. These studies were designed to evaluate immunologic noninferiority of Prevnar 13 to Prevnar.
Clinical trials have been conducted in the US using a 2, 4, 6, and 12–15 month schedule.
The US noninferiority study2 (Study 2) was a randomized, double-blind, active-controlled trial in which 2 month-old infants were randomly assigned to receive either Prevnar 13 or Prevnar in a 1:1 ratio. The two vaccine groups were well balanced with respect to race, ethnicity, and age and weight at enrollment. Most subjects were White (69.1%), 19.6% were Black or African-American, and 2.4% were Asian; 82.1% of subjects were non-Hispanic and non-Latino and 17.3% were Hispanic or Latino. Overall, 54.0% of subjects were male infants.
In Study 2, immune responses were compared in subjects receiving either Prevnar 13 or Prevnar using a set of noninferiority criteria. Co-primary endpoints included the percentage of subjects with serum pneumococcal anti-capsular polysaccharide IgG ≥0.35 µg/mL measured one month after the third dose and serum pneumococcal anti-capsular polysaccharide IgG geometric mean concentrations (GMCs) one month after the fourth dose. The assay used for this determination was a standardized ELISA involving pre-absorption of the test sera with pneumococcal C-polysaccharide and serotype 22F polysaccharide to reduce non-specific background reactivity. Responses to the 7 common serotypes in Prevnar 13 and Prevnar recipients were compared directly. Responses to the 6 additional serotypes in Prevnar 13 recipients were each compared to the lowest response observed among the Prevnar serotypes in Prevnar recipients.
Pneumococcal Immune Responses Following Three Doses
In Study 2, the noninferiority criterion for the proportion of subjects with pneumococcal anti-capsular polysaccharide IgG antibody concentrations ≥0.35 μg/mL one month after the third dose was met for 10 of the 13 serotypes. The exceptions were serotypes 6B, 9V, and 3. Although the response to serotypes 6B and 9V did not meet the pre-specified noninferiority criterion, the differences were marginal.
The percentage of infants achieving pneumococcal anti-capsular polysaccharide IgG antibody concentrations ≥0.35 μg/mL one month after the third dose is shown below (Table 16).
Table 16: Percentage of Subjects With Anti-capsular Antibody Concentration ≥0.35 µg/mL One Month After a Three Dose Series Administered at 2, 4 and 6 Months of Age, Study 2*,†,‡,§ Serotype Prevnar 13
N=249–252
(95% CI)Prevnar
N=250–252
(95% CI)Difference in % responders
(95% CI)- * Studies conducted in US NCT00373958 (Study 2).
- † Evaluable Immunogenicity Population.
- ‡ Noninferiority was met when the lower limit of the 95% CI for the difference between groups (Prevnar 13 minus Prevnar) was greater than -10%.
- § Antibody measured by a standardized ELISA involving pre-absorption of the test sera with pneumococcal C-polysaccharide and serotype 22F polysaccharide to reduce non-specific background reactivity.
- ¶ Comparison for the 6 additional serotypes was to the lowest responder of the 7 common serotypes in Prevnar recipients, which for this analysis was serotype 6B (92.8%; 95% CI: 88.9, 95.7).
Prevnar Serotypes 4 94.4 (90.9, 96.9) 98.0 (95.4, 99.4) -3.6 (-7.3, -0.1) 6B 87.3 (82.5, 91.1) 92.8 (88.9, 95.7) -5.5 (-10.9, -0.1) 9V 90.5 (86.2, 93.8) 98.4 (96.0, 99.6) -7.9 (-12.4, -4.0) 14 97.6 (94.9, 99.1) 97.2 (94.4, 98.9) 0.4 (-2.7, 3.5) 18C 96.8 (93.8, 98.6) 98.4 (96.0, 99.6) -1.6 (-4.7, 1.2) 19F 98.0 (95.4, 99.4) 97.6 (99.4, 99.1) 0.4 (-2.4, 3.4) 23F 90.5 (86.2, 93.8) 94.0 (90.4, 96.6) -3.6 (-8.5, 1.2) Additional Serotypes¶ 1 95.6 (92.3, 97.8) ¶ 2.8 (-1.3, 7.2) 3 63.5 (57.1, 69.4) ¶ -29.3 (-36.2, -22.4) 5 89.7 (85.2, 93.1) ¶ -3.1 (-8.3, 1.9) 6A 96.0 (92.8, 98.1) ¶ 3.2 (-0.8, 7.6) 7F 98.4 (96.0, 99.6) ¶ 5.6 (1.9, 9.7) 19A 98.4 (96.0, 99.6) ¶ 5.6 (1.9, 9.7) Functional dOPA antibody responses were elicited for all 13 serotypes, as shown in Table 17.
Table 17: Pneumococcal dOPA Antibody Geometric Mean Titers One Month After a Three Dose Series Administered at 2, 4 and 6 Months of Age, Study 2*,†,‡ Serotype Prevnar 13
N=91–94
(95% CI)Prevnar
N=89–94
(95% CI)- * Studies conducted in US NCT00373958 (Study 2).
- † The dOPA (opsonophagocytic activity) antibody assay measures the ability of immune sera, in conjunction with complement, to mediate the uptake and killing of S. pneumoniae by phagocytic cells.
- ‡ Evaluable Immunogenicity Population.
Prevnar Serotypes 4 359 (276, 468) 536 (421, 681) 6B 1055 (817, 1361) 1514 (1207, 1899) 9V 4035 (2933, 5553) 3259 (2288, 4641) 14 1240 (935, 1646) 1481 (1133, 1934) 18C 276 (210, 361) 376 (292, 484) 19F 54 (40, 74) 45 (34, 60) 23F 791 (605, 1034) 924 (709, 1204) Additional Serotypes 1 52 (39, 69) 4 (4, 5) 3 121 (92, 158) 7 (5, 9) 5 91 (67, 123) 4 (4, 4) 6A 980 (783, 1226) 100 (66, 152) 7F 9494 (7339, 12281) 128 (80, 206) 19A 152 (105, 220) 7 (5, 9) Pneumococcal Immune Responses Following Four Doses
In Study 2, post-dose 4 antibody concentrations were higher for all 13 serotypes than those achieved after the third dose. The noninferiority criterion for pneumococcal anti-capsular polysaccharide GMCs after 4 doses was met for 12 of the 13 pneumococcal serotypes. The noninferiority criterion was not met for the response to serotype 3 (Table 18).
Table 18: Pneumococcal IgG GMCs (µg/mL) One Month After a Four Dose Series Administered at 2, 4, 6 and 12–15 Months, Study 2*,†,‡,§ Serotype Prevnar 13
N=232–236
(95% CI)Prevnar
N=222–223
(95% CI)GMC Ratio
(95% CI)- * Studies conducted in US NCT00373958 (Study 2).
- † Evaluable Immunogenicity Population.
- ‡ Noninferiority was declared if the lower limit of the 2-sided 95% CI for Geometric Mean Ratio (Prevnar 13:Prevnar) was greater than 0.5.
- § Antibody measured by a standardized ELISA involving pre-absorption of the test sera with pneumococcal C-polysaccharide and serotype 22F polysaccharide to reduce non-specific background reactivity.
- ¶ Comparison for the 6 additional serotypes was to the lowest responder of the 7 common serotypes in Prevnar recipients, which for this analysis was serotype 9V (3.63; 95% CI 3.25, 4.05).
Prevnar Serotypes 4 3.73 (3.28, 4.24) 5.49 (4.91, 6.13) 0.68 (0.57, 0.80) 6B 11.53 (9.99, 13.30) 15.63 (13.80, 17.69) 0.74 (0.61, 0.89) 9V 2.62 (2.34, 2.94) 3.63 (3.25, 4.05) 0.72 (0.62, 0.85) 14 9.11 (7.95, 10.45) 12.72 (11.22, 14.41) 0.72 (0.60, 0.86) 18C 3.20 (2.82, 3.64) 4.70 (4.18, 5.28) 0.68 (0.57, 0.81) 19F 6.60 (5.85, 7.44) 5.60 (4.87, 6.43) 1.18 (0.98, 1.41) 23F 5.07 (4.41, 5.83) 7.84 (6.91, 8.90) 0.65 (0.54, 0.78) Additional Serotypes¶ 1 5.06 (4.43, 5.80) ¶ 1.40 (1.17, 1.66) 3 0.94 (0.83, 1.05) ¶ 0.26 (0.22, 0.30) 5 3.72 (3.31, 4.18) ¶ 1.03 (0.87, 1.20) 6A 8.20 (7.30, 9.20) ¶ 2.26 (1.93, 2.65) 7F 5.67 (5.01, 6.42) ¶ 1.56 (1.32, 1.85) 19A 8.55 (7.64, 9.56) ¶ 2.36 (2.01, 2.76) Following the fourth dose, the functional dOPA antibody response for each serotype was quantitatively greater than the response following the third dose (see Table 19).
Table 19: Pneumococcal dOPA Antibody Geometric Mean Titers One Month After the Fourth Dose-Evaluable Toddler Immunogenicity Population, Study 2*,† Serotype Prevnar 13
N=88–92
(95% CI)Prevnar
N=92–96
(95% CI)- * Studies conducted in US NCT00373958 (Study 2).
- † The dOPA (opsonophagocytic activity) antibody assay measures the ability of immune sera, in conjunction with complement, to mediate the uptake and killing of S. pneumoniae by phagocytic cells.
Prevnar Serotypes 4 1180 (847, 1643) 1492 (1114, 1999) 6B 3100 (2337, 4111) 4066 (3243, 5098) 9V 11856 (8810, 15955) 18032 (14125, 23021) 14 2002 (1453, 2760) 2366 (1871, 2992) 18C 993 (754, 1308) 1722 (1327, 2236) 19F 200 (144, 276) 167 (121, 230) 23F 2723 (1961, 3782) 4982 (3886, 6387) Additional Serotypes 1 164 (114, 237) 5 (4, 6) 3 380 (300, 482) 12 (9, 16) 5 300 (229, 393) 5 (4, 6) 6A 2242 (1707, 2945) 539 (375, 774) 7F 11629 (9054, 14938) 268 (164, 436) 19A 1024 (774, 1355) 29 (19, 44) Previously Unvaccinated Older Infants and Children 7 Months Through 5 Years of Age
In an open-label descriptive study of Prevnar 13 in Poland4 (Study 4), children 7 months through 11 months of age, 12 months through 23 months of age and 24 months through 5 years of age (prior to the 6th birthday) who were naïve to pneumococcal conjugate vaccine, were given 3, 2 or 1 dose of Prevnar 13 respectively, according to the age-appropriate schedules in Table 2. Serum IgG concentrations were measured one month after the final dose in each age group and the data are shown in Table 20.
Table 20: Pneumococcal Anti-capsular Polysaccharide IgG Antibody Geometric Mean Concentrations (μg/mL) One Month After the Final Prevnar 13 Catch-Up Dose in Pneumococcal Vaccine Naïve Children 7 Months Through 5 Years of Age by Age Group, Study 4*,† Serotype 3 doses Prevnar 13
7 through 11 months
N=83–84
(95% CI)2 doses Prevnar 13
12 through 23 months
N=104–110
(95% CI)1 dose Prevnar 13
24 months through 5 years
N=135–152
(95% CI)Note – ClinicalTrials.gov NCT number is as follows: NCT00452452 (Poland). - * Studies conducted in Poland NCT00452452 (Study 4).
- † Open label administration of Prevnar 13.
1 2.88 (2.44, 3.39) 2.74 (2.37, 3.16) 1.78 (1.52, 2.08) 3 1.94 (1.68, 2.24) 1.86 (1.60, 2.15) 1.42 (1.23, 1.64) 4 3.63 (3.11, 4.23) 4.28 (3.78, 4.86) 3.37 (2.95, 3.85) 5 2.85 (2.34, 3.46) 2.16 (1.89, 2.47) 2.33 (2.05, 2.64) 6A 3.72 (3.12, 4.45) 2.62 (2.25, 3.06) 2.96 (2.52, 3.47) 6B 4.77 (3.90, 5.84) 3.38 (2.81, 4.06) 3.41 (2.80, 4.16) 7F 5.30 (4.54, 6.18) 5.99 (5.40, 6.65) 4.92 (4.26, 5.68) 9V 2.56 (2.21, 2.96) 3.08 (2.69, 3.53) 2.67 (2.32, 3.07) 14 8.04 (6.95, 9.30) 6.45 (5.48, 7.59) 2.24 (1.71, 2.93) 18C 2.77 (2.39, 3.23) 3.71 (3.29, 4.19) 2.56 (2.17, 3.03) 19A 4.77 (4.28, 5.33) 4.94 (4.31, 5.65) 6.03 (5.22, 6.97) 19F 2.88 (2.35, 3.54) 3.07 (2.68, 3.51) 2.53 (2.14, 2.99) 23F 2.16 (1.82, 2.55) 1.98 (1.64, 2.39) 1.55 (1.31, 1.85) Children 15 Months Through 59 Months of Age Previously Vaccinated with Prevnar
In an open-label descriptive study in the US5 (Study 5), children 15 months through 59 months previously vaccinated with 3 or 4 doses of Prevnar, received 2 doses of Prevnar 13 (children >15 through 23 months of age) or 1 dose of Prevnar 13 (children 24 months through 59 months of age). The data following one dose of Prevnar 13 in children 24 months through 59 months of age are shown in Table 21.
Table 21: Pneumococcal Anti-capsular Polysaccharide IgG Antibody Geometric Mean Concentrations (μg/mL) One Month After One Prevnar 13 Catch-Up Dose in Children 24 Through 59 Months of Age With 3 or 4 Prior Doses of Prevnar, US Catch-Up Study 5*,† Serotype 1 dose Prevnar 13
24 months through 59 months
N=173–175
(95% CI)- * Studies conducted in US NCT00761631 (Study 5).
- † Open label administration of Prevnar 13.
1 2.43 (2.15, 2.75) 3 1.38 (1.17, 1.61) 5 2.13 (1.89, 2.41) 6A 12.96 (11.04, 15.21) 7F 4.22 (3.74, 4.77) 19A 14.18 (12.37, 16.25) Children 5 Through 17 Years of Age
In a US study5 (Study 5), a single dose of Prevnar 13 was administered to children 5 through 9 years of age, who were previously vaccinated with at least one dose of Prevnar, and to pneumococcal vaccine-naïve children 10 through 17 years of age.
In children 5 through 9 years of age, serotype-specific IgG concentrations measured 1 month after vaccination were noninferior (i.e., the lower limit of the 2-sided 95% CI for the geometric mean ratio [GMR] of >0.5) to the corresponding IgG concentrations in toddlers (Study 3) 1 month after a fourth pneumococcal vaccination (after the 4th dose of Prevnar for the 7 common serotypes and after the 4th dose of Prevnar 13 for the 6 additional serotypes) as shown in Tables 22 and 23 respectively.
Table 22: Pneumococcal IgG GMCs (µg/mL) One Month After Vaccination for 7 Common Serotypes, Prevnar 13 in Children 5 through 9 Years of Age in Study 5 Relative to Prevnar in Study 3 (Post-toddler)*,†,‡ Vaccine Group (as Enrolled/Randomized) Prevnar 13
5 Through 9 Years
(Study 5)Prevnar
Post-Toddler Dose
(Study 3)Serotype n§ GMC¶ (95% CI#) n§ GMC¶ (95% CI#) GMC RatioÞ (95% CIß) - * Studies conducted in US NCT00761631 (Study 5) and NCT00444457 (Study 3).
- † Evaluable Immunogenicity Population.
- ‡ Noninferiority was declared if the lower limit of the 2-sided 95% CI for geometric mean ratio was greater than 0.5.
- § n = Number of subjects with a determinate antibody concentration for the specified serotype.
- ¶ Geometric mean concentrations (GMCs) were calculated using all subjects with available data for the specified blood draw. GMC after a 4-dose vaccination series with Prevnar (Study 3, post-toddler).
- # Confidence intervals (CIs) are back transformations of a confidence interval based on the Student t distribution for the mean logarithm of the concentrations.
- Þ Ratio of GMCs: Prevnar 13 (Study 5) to Prevnar (Study 3) reference.
- ß CIs for the ratio are back transformations of a confidence interval based on the Student t distribution for the mean difference of the logarithms of the measures [Prevnar 13 (Study 5) – Prevnar (Study 3)].
Common 4 169 8.45 (7.24, 9.87) 173 2.79 (2.45, 3.18) 3.03 (2.48, 3.71) 6B 171 53.56 (45.48, 63.07) 173 9.47 (8.26, 10.86) 5.66 (4.57, 6.99) 9V 171 9.51 (8.38, 10.78) 172 1.97 (1.77, 2.19) 4.83 (4.10, 5.70) 14 169 29.36 (24.78, 34.78) 173 8.19 (7.31, 9.18) 3.58 (2.93, 4.39) 18C 171 8.23 (7.13, 9.51) 173 2.33 (2.05, 2.65) 3.53 (2.91, 4.29) 19F 171 17.58 (14.95, 20.67) 173 3.31 (2.87, 3.81) 5.31 (4.29, 6.58) 23F 169 11.26 (9.79, 12.95) 173 4.49 (3.86, 5.23) 2.51 (2.04, 3.08) Table 23: Pneumococcal IgG GMCs (µg/mL) One Month After Vaccination for Additional 6 Serotypes, Prevnar 13 in Children 5 through 9 Years of Age in Study 5 Relative to Prevnar 13 in Study 3 (Post-toddler)*,†.‡ Vaccine Group (as Enrolled/Randomized) Prevnar 13
5 Through 9 Years
(Study 5)Prevnar 13
Post-Toddler Dose
(Study 3)Serotype n§ GMC¶ (95% CI#) n§ GMC¶ (95% CI#) GMC
RatioÞ(95% CIß) - * Studies conducted in US NCT00761631 (Study 5) and NCT00444457 (Study 3).
- † Evaluable Immunogenicity Population.
- ‡ Noninferiority was declared if the lower limit of the 2-sided 95% CI for geometric mean ratio was greater than 0.5.
- § n = Number of subjects with a determinate antibody concentration for the specified serotype.
- ¶ Geometric mean concentrations (GMCs) were calculated using all subjects with available data for the specified blood draw. GMC after a 4-dose vaccination series with Prevnar 13 (Study 3, post-toddler).
- # Confidence intervals (CIs) are back transformations of a confidence interval based on the Student t distribution for the mean logarithm of the concentrations.
- Þ Ratio of GMCs: Prevnar 13 (Study 5) to Prevnar 13 (Study 3).
- ß CIs for the ratio are back transformations of a confidence interval based on the Student t distribution for the mean difference of the logarithms of the measures [Prevnar 13 (Study 5) – Prevnar 13 (Study 3)].
Additional 1 171 3.57 (3.05, 4.18) 1068 2.90 (2.75, 3.05) 1.23 (1.07, 1.42) 3 171 2.38 (2.07, 2.74) 1065 0.75 (0.72, 0.79) 3.17 (2.78, 3.62) 5 171 5.52 (4.82, 6.32) 1068 2.85 (2.72, 2.98) 1.94 (1.71, 2.20) 6A 169 21.51 (18.15, 25.51) 1063 7.11 (6.78, 7.46) 3.03 (2.64, 3.47) 7F 170 6.24 (5.49, 7.08) 1067 4.39 (4.18, 4.61) 1.42 (1.24, 1.62) 19A 170 17.18 (15.01, 19.67) 1056 8.44 (8.05, 8.86) 2.03 (1.78, 2.32) In children 10 through 17 years of age OPA GMTs, as measured by the mcOPA assay, 1 month after vaccination were noninferior (i.e., the lower limit of the 2-sided 95% CI for the GMR of >0.5) to mcOPA GMTs in the 5 through 9 year old group for 12 of 13 serotypes (except for serotype 3), as shown in Table 24.
Table 24: Comparison of Pneumococcal mcOPA GMTs One Month After Vaccination, Prevnar 13, in Children 10 through 17 Years of Age Relative to Prevnar 13 in Children 5 through 9 Years of Age*,†,‡,§ Vaccine Group (as Enrolled) Prevnar 13
(10 through 17 Years)Prevnar 13
(5 through 9 Years)Serotype n¶ GMT# (95% CIÞ) n¶ GMT# (95% CIÞ) GMT Ratioß (95% CIà) - * Studies conducted in US NCT00761631 (Study 5).
- † Evaluable Immunogenicity Population.
- ‡ Noninferiority was declared if the lower limit of the 2-sided 95% CI for geometric mean ratio was greater than 0.5.
- § Individual mcOPA antibody assay values below the assay LLOQ (lower limit of quantitation) were set at 0.50*LLOQ for the purpose of calculating the mcOPA antibody GMT.
- ¶ n= Number of subjects with a determinate antibody titer for the specified serotype.
- # Geometric mean titers (GMTs) were calculated using all subjects with available data for the specified blood draw.
- Þ Confidence intervals (CIs) are back transformations of a confidence interval based on the Student t distribution for the mean logarithm of the titers.
- ß Ratio of GMTs: Prevnar 13(10 through 17 years of age) to Prevnar 13 (5 through 9 years of age).
- à CIs for the ratio are back transformations of a confidence interval based on the Student t distribution for the mean difference of the logarithms of the measures [Prevnar 13(10 through 17 years of age) – Prevnar 13(5 through 9 years of age)] Study 5.
Common 4 188 6912 (6101, 7831) 181 4629 (4017, 5334) 1.5 (1.24, 1.80) 6B 183 14224 (12316, 16427) 178 14996 (13164, 17083) 0.9 (0.78, 1.15) 9V 186 4485 (4001, 5028) 180 4733 (4203, 5328) 0.9 (0.80, 1.12) 14 187 6894 (6028, 7884) 176 4759 (4120, 5497) 1.4 (1.19, 1.76) 18C 182 6263 (5436, 7215) 175 8815 (7738, 10041) 0.7 (0.59, 0.86) 19F 184 2280 (1949, 2668) 178 1591 (1336, 1893) 1.4 (1.14, 1.81) 23F 187 3808 (3355, 4323) 176 3245 (2819, 3736) 1.2 (0.97, 1.42) Additional 1 189 322 (275, 378) 179 191 (165, 221) 1.7 (1.36, 2.10) 3 181 114 (101, 130) 178 203 (182, 226) 0.6 (0.48, 0.67) 5 183 360 (298, 436) 178 498 (437, 568) 0.7 (0.57, 0.91) 6A 182 9928 (8457, 11655) 178 7514 (6351, 8891) 1.3 (1.05, 1.67) 7F 185 6584 (5829, 7436) 178 10334 (9099, 11737) 0.6 (0.53, 0.76) 19A 187 1276 (1132, 1439) 180 1180 (1048, 1329) 1.1 (0.91, 1.28) 14.3 Prevnar 13 Immunogenicity Clinical Trials in Adults
Six Phase 3 or Phase 4 clinical trials6–8,10,11,13 were conducted in the US and Europe evaluating the immunogenicity of Prevnar 13 in different adult age groups, in individuals who were either not previously vaccinated with PPSV23 (PPSV23 unvaccinated) or who had received one dose of PPSV23 (PPSV23 previously vaccinated).
Each study included healthy adults and immunocompetent adults with stable underlying conditions including chronic cardiovascular disease, chronic pulmonary disease, renal disorders, diabetes mellitus, chronic liver disease, and medical risk conditions and behaviors (e.g., alcoholism and smoking) that are known to increase the risk of serious pneumococcal pneumonia and invasive pneumococcal disease. A stable medical condition was defined as a medical condition not requiring significant change in therapy (i.e., change to new therapy category due to worsening disease) or hospitalization for worsening disease 6–12 weeks prior to receipt of the study vaccine.
Immune responses elicited by Prevnar 13 and PPSV23 were measured by a mcOPA antibody assay for the 13 pneumococcal serotypes contained in Prevnar 13. Serotype-specific mcOPA antibody GMTs measured 1 month after each vaccination were calculated. For the 12 serotypes in common to both vaccines, noninferiority between vaccines was met if the lower limit of the 2-sided 95% confidence interval (CI) of the GMT ratio (Prevnar 13/PPSV23) was greater than 0.5.
The response to the additional serotype 6A, which is contained in Prevnar 13 but not in PPSV23, was assessed by demonstration of a ≥4-fold increase in the anti-6A mcOPA antibody titer above preimmunization levels. A statistically significantly greater response for Prevnar 13 was defined, for the difference in percentages (Prevnar 13 minus PPSV23) of adults achieving a ≥4-fold increase in anti-6A mcOPA antibody titer, as the lower limit of the 2-sided 95% CI greater than zero. For comparison of mcOPA antibody GMTs, a statistically greater response for serotype 6A was defined as the lower limit of the 2-sided 95% CI of the GMT ratio (Prevnar 13/PPSV23) greater than 2.
Of the 6 Phase 3 or Phase 4 clinical trials, 2 noninferiority trials6,7 were conducted in which the immune responses to Prevnar 13 were compared with the immune responses to PPSV23; one in PPSV23 unvaccinated adults aged 18 through 64 years6 (Study 6), and one in PPSV23 previously vaccinated adults aged ≥70 years7 (Study 7). A third study compared immune responses to a single dose of Prevnar 13 to the response to Prevnar 13 administered one year after a dose of PPSV23 in adults aged 60 through 64 years who were PPSV23 unvaccinated at enrollment8 (Study 8). The study also compared immune responses of PPSV23 as a single dose to the responses to PPSV23 administered one year after a dose of Prevnar 13. Two studies assessed the concomitant administration of Prevnar 13 with seasonal inactivated Fluarix (IIV3) in the US10 (Study 10) and Europe11 (Study 11). One study (Study 13) assessed the concomitant administration of Prevnar 13 with seasonal inactivated Fluzone Quadrivalent (IIV4) in PPSV23 previously vaccinated adults ≥50 years of age in the US.
Overall across the clinical studies evaluating the immunogenicity of Prevnar 13 in adults, persons 18 through 64 years of age responded at least as well as persons 65 years and older, the age group evaluated in a clinical endpoint efficacy trial.
Clinical Trials Conducted in PPSV23 Unvaccinated Adults
In an active-controlled modified1 double-blind clinical trial6 (Study 6) of Prevnar 13 in the US, PPSV23 unvaccinated adults aged 60 through 64 years were randomly assigned (1:1) to receive Prevnar 13 or PPSV23. In addition, adults aged 18 through 49 years and 50 through 59 years were enrolled and received one dose of Prevnar 13 (open-label).
In adults aged 60 through 64 years, the mcOPA antibody GMTs elicited by Prevnar 13 were noninferior to those elicited by PPSV23 for the 12 serotypes in common to both vaccines (see Table 24). In addition, the lower limit of the 95% confidence interval for the mcOPA antibody GMT ratio (Prevnar 13/PPSV23) was greater than 1 for 8 of the serotypes in common.
For serotype 6A, which is unique to Prevnar 13, the proportion of subjects with a ≥4-fold increase after Prevnar 13 (88.5%) was statistically significantly greater than after PPSV23 (49.3%) in PPSV23-unvaccinated adults aged 60 through 64 years. OPA antibody GMTs for serotype 6A were statistically significantly greater after Prevnar 13 compared with after PPSV23 (see Table 25).
The mcOPA antibody GMTs elicited by Prevnar 13 in adults aged 50 through 59 years were noninferior to the corresponding mcOPA antibody GMTs elicited by Prevnar 13 in adults aged 60 through 64 years for all 13 serotypes (see Table 25).
In adults aged 18 through 49 years, the mcOPA antibody GMTs elicited by Prevnar 13 were noninferior to those elicited by Prevnar 13 in adults aged 60 through 64 years for all 13 serotypes (see Table 25).
Table 25: mcOPA Antibody GMTs in PPSV23-Unvaccinated Adults Aged 18 Through 49 Years or Aged 50 Through 59 Years Given Prevnar 13 and in Adults Aged 60 Through 64 Years Given Prevnar 13 or PPSV23 (Study 6)*,†,‡,§,¶ Prevnar 13 Prevnar 13 Prevnar 13 PPSV23 Prevnar 13
18–49 Relative to 60–64 YearsPrevnar 13
50–59 Relative to 60–64 YearsPrevnar 13 Relative to PPSV23, 60–64 Years# Serotype 18–49 YearsÞ
N=836–86650–59 YearsÞ
N=350–38460–64 Years
N=359–40460–64 Years
N=367–402GMT GMT GMT GMT GMT Ratio
(95% CI)GMT Ratio
(95% CI)GMT Ratio
(95% CI)GMT, Geometric Mean Titer. - * Study conducted in US NCT00427895 (Study 6).
- † Noninferiority was defined for the 13 serotypes in adults aged 18 to 49 years, for the 12 common serotypes in adults aged 60 to 64 years and for the 13 serotypes in adults aged 50 to 59 years as the lower limit of the 2-sided 95% CI for GMT ratio greater than 0.5.
- ‡ mcOPA antibody for the 11 serotypes unique to PPSV23 but not contained in Prevnar 13 were not measured.
- § Individual mcOPA antibody assay values below the assay LLOQ (lower limit of quantitation) were set at 0.50*LLOQ for the purpose of calculating the mcOPA antibody GMT.
- ¶ Evaluable Immunogenicity Population.
- # For serotype 6A, which is unique to Prevnar 13, a statistically significantly greater response was defined for analysis in cohort 1 as the lower limit of the 2-sided 95% CI for the GMT ratio (Prevnar 13/PPSV23) greater than 2.
- Þ Open label administration of Prevnar 13.
- ß 6A is a serotype unique to Prevnar 13 but not contained in PPSV23.
1 353 211 158 119 2.4
(2.03, 2.87)1.3
(1.07, 1.65)1.3
(1.07, 1.65)3 91 94 96 90 1.0
(0.84, 1.13)1.0
(0.82, 1.18)1.1
(0.89, 1.29)4 4747 2904 2164 1405 2.3
(1.92, 2.76)1.3
(1.06, 1.70)1.5
(1.18, 2.00)5 386 322 236 198 1.9
(1.55, 2.42)1.4
(1.08, 1.74)1.2
(0.95, 1.50)6Aß 5746 4469 2766 343 2.2
(1.84, 2.67)1.6
(1.28, 2.03)8.1
(6.11, 10.67)6B 9813 3350 2212 998 4.9
(4.13, 5.93)1.5
(1.20, 1.91)2.2
(1.70, 2.89)7F 3249 1807 1535 829 2.9
(2.41, 3.49)1.2
(0.98, 1.41)1.9
(1.52, 2.26)9V 3339 2190 1701 1012 2.9
(2.34, 3.52)1.3
(1.08, 1.53)1.7
(1.40, 2.02)14 2983 1078 733 819 4.9
(4.01, 5.93)1.5
(1.14, 1.89)0.9
(0.69, 1.16)18C 3989 2077 1834 1074 2.3
(1.91, 2.79)1.1
(0.89, 1.44)1.7
(1.32, 2.21)19A 1580 968 691 368 2.3
(2.02, 2.66)1.4
(1.17, 1.68)1.9
(1.53, 2.30)19F 1533 697 622 636 3.0
(2.44, 3.60)1.1
(0.89, 1.41)1.0
(0.78, 1.23)23F 1570 531 404 87 4.2
(3.31, 5.31)1.3
(0.96, 1.80)4.6
(3.37, 6.38)
- 1 Modified double-blind means that the site staff dispensing and administering the vaccine were unblinded, but all other study personnel including the principal investigator and subject were blinded.
Clinical Trials Conducted in PPSV23 Previously Vaccinated Adults
In a Phase 3 active-controlled, modified double-blind clinical trial7 (Study 7) of Prevnar 13 in the US and Sweden, PPSV23 previously vaccinated adults aged ≥70 years who had received one dose of PPSV23 ≥5 years prior were randomly assigned (1:1) to receive either Prevnar 13 or PPSV23.
The mcOPA antibody GMTs elicited by Prevnar 13 were noninferior to those elicited by PPSV23 for the 12 serotypes in common, when Prevnar 13 or PPSV23 were administered at a minimum of 5 years after a prior dose of PPSV23. In addition, the lower limit of the 95% confidence interval for the mcOPA antibody GMT ratio (Prevnar 13/PPSV23) was greater than 1 for 9 of the serotypes in common.
For serotype 6A, which is unique to Prevnar 13, the proportion of subjects with a ≥4-fold increase in mcOPA antibody titers after Prevnar 13 (71.1%) was statistically significantly greater than after PPSV23 (27.3%) in PPSV23 previously vaccinated adults aged ≥70 years. mcOPA antibody GMTs for serotype 6A were statistically significantly greater after Prevnar 13 compared with after PPSV23.
This clinical trial demonstrated that in adults aged ≥70 years and previously vaccinated with PPSV23 ≥5 years prior, vaccination with Prevnar 13 elicited noninferior immune responses as compared with re-vaccination with PPSV23 (see Table 26).
Table 26: mcOPA Antibody GMTs in PPSV23-Previously Vaccinated Adults Aged ≥70 Years Given Prevnar 13 or PPSV23 (Study 7)*,†,‡,§,¶,# Serotype Prevnar 13
N=400–426PPSV23
N=395–445Prevnar 13
Relative to PPSV23GMT GMT GMT Ratio (95% CI) GMT, Geometric Mean Titer. - * Study conducted in US and Sweden NCT00546572 (Study 7).
- † For the 12 common serotypes, noninferiority was defined as the lower limit of the 2-sided 95% CI for GMT ratio (Prevnar 13/PPSV23) greater than 0.5.
- ‡ For serotype 6A, which is unique to Prevnar 13, a statistically significantly greater response was defined as the lower limit of the 2-sided 95% CI for the GMT ratio (Prevnar 13/PPSV23) greater than 2.
- § mcOPA antibody for the 11 serotypes unique to PPSV23 but not contained in Prevnar 13 were not measured.
- ¶ Individual mcOPA antibody assay values below the assay LLOQ (lower limit of quantitation) were set at 0.50*LLOQ for the purpose of calculating the mcOPA antibody GMT.
- # Evaluable Immunogenicity Population.
- Þ 6A is a serotype unique to Prevnar 13 but not contained in PPSV23.
1 93 66 1.4 (1.14, 1.72) 3 59 53 1.1 (0.92, 1.31) 4 613 263 2.3 (1.76, 3.10) 5 100 61 1.6 (1.35, 2.00) 6AÞ 1056 160 6.6 (5.14, 8.49) 6B 1450 565 2.6 (2.00, 3.29) 7F 559 481 1.2 (0.97, 1.39) 9V 622 491 1.3 (1.08, 1.49) 14 355 366 1.0 (0.76, 1.23) 18C 972 573 1.7 (1.33, 2.16) 19A 366 216 1.7 (1.40, 2.07) 19F 422 295 1.4 (1.16, 1.77) 23F 177 53 3.3 (2.49, 4.47) Clinical Trial of Sequential Vaccination of Prevnar 13 and PPSV23 in PPSV23 Unvaccinated Adults
In a randomized clinical trial conducted in PPSV23-unvaccinated adults 60 through 64 years of age8 (Study 8), 223 subjects received PPSV23 followed by Prevnar 13 one year later (PPSV23/Prevnar 13), and 478 received only Prevnar 13. mcOPA antibody titers were measured 1 month after vaccination with Prevnar 13 and are shown in Table 26. mcOPA antibody GMTs in those that received Prevnar 13 one year after PPSV23 were diminished when compared to those who received Prevnar 13 alone. Similarly, in exploratory analyses in PPSV23 previously vaccinated adults ≥70 years of age in Study 7, diminished mcOPA antibody GMTs were observed in those that received Prevnar 13 one year after PPSV23 when compared to those who received Prevnar 13 alone.
Table 27: mcOPA Antibody GMTs for the Prevnar 13 Serotypes in PPSV23 Unvaccinated Adults Aged 60 Through 64 Years Given Prevnar 13 Alone or Prevnar 13 One Year After PPSV23 (Study 8) (PPSV23/Prevnar 13)*,†,‡,§ Prevnar 13
N=410–457PPSV23/Prevnar 13
N=180–196Serotype GMT (95% CI) GMT (95% CI) GMT =Geometric Mean Titer. - * Study conducted in US NCT00574548 (Study 8).
- † Evaluable Immunogenicity Population.
- ‡ mcOPA antibody for the 11 serotypes unique to PPSV23 but not contained in Prevnar 13 were not measured.
- § Individual mcOPA antibody assay values below the assay LLOQ (lower limit of quantitation) were set at 0.50*LLOQ for the purpose of calculating the mcOPA antibody GMT.
- ¶ 6A is a serotype unique to Prevnar 13 but not contained in PPSV23.
1 219 (191, 252) 88 (72, 109) 3 78 (69, 88) 54 (45, 65) 4 2590 (2257, 2973) 988 (802, 1218) 5 258 (218, 305) 112 (90, 139) 6A¶ 2947 (2536, 3426) 1210 (962, 1522) 6B 2165 (1845, 2540) 832 (654, 1059) 7F 1518 (1339, 1721) 407 (342, 485) 9V 1279 (1142, 1432) 495 (426, 575) 14 790 (663, 941) 515 (402, 659) 18C 1683 (1437, 1971) 650 (504, 839) 19A 717 (629, 818) 299 (248, 361) 19F 812 (702, 939) 360 (293, 442) 23F 384 (312, 472) 142 (104, 193) Also in Study 8, 266 subjects received Prevnar 13 followed by PPSV23 one year later (Prevnar 13/PPSV23). mcOPA antibody GMTs following PPSV23 administered one year after Prevnar 13 (Prevnar 13/PPSV23) were noninferior to those following a single dose of PPSV23 (N=237) for the 12 common serotypes [the lower limit of the 95% CI for the GMT ratio [Prevnar 13/PPSV23 relative to PPSV23] was >0.5] (see Table 27). In Study 6, which was conducted in PPSV23-unvaccinated adults 60 through 64 years of age, 108 subjects received PPSV23 3.5 to 4 years after Prevnar 13 (Prevnar 13/PPSV23) and 414 received a single dose of PPSV23. Higher serotype-specific mcOPA antibody GMT ratios [(Prevnar 13/PPSV23) / PPSV23] were generally observed compared to the one year dosing interval in Study 8.
Table 28: mcOPA Antibody GMTs for the Prevnar 13 Serotypes in PPSV23-Unvaccinated Adults Aged 60 Through 64 Years Given PPSV23 One Year After Prevnar 13 Relative to PPSV23 Alone (Study 8)*,†,‡,§ Prevnar 13/PPSV23
N=216–233PPSV23
N=214–229GMT Ratio (Prevnar 13/PPSV23) / PPSV23 Serotype GMT 95% CI GMT 95% CI Ratio 95% CI GMT =Geometric Mean Titer. - * Study conducted in US NCT00574548 (Study 8).
- † Evaluable Immunogenicity Population.
- ‡ mcOPA antibody for the 11 serotypes unique to PPSV23 but not contained in Prevnar 13 were not measured.
- § Individual mcOPA antibody assay values below the assay LLOQ (lower limit of quantitation) were set at 0.50*LLOQ for the purpose of calculating the mcOPA antibody GMT.
- ¶ 6A is a serotype unique to Prevnar 13 but not contained in PPSV23. Anti-6A mcOPA antibody GMTs were descriptive in nature.
1 155 (131, 182) 161 (131, 198) 1.0 (0.74, 1.25) 3 127 (111, 145) 83 (71, 98) 1.5 (1.23, 1.87) 4 1409 (1202, 1651) 1468 (1139, 1893) 1.0 (0.71, 1.29) 5 220 (184, 264) 178 (144, 222) 1.2 (0.93, 1.64) 6A¶ 1366 (1122, 1663) 400 (306, 524) 3.4 (2.45, 4.77) 6B 1345 (1113, 1625) 875 (689, 1111) 1.5 (1.14, 2.08) 7F 748 (653, 857) 719 (598, 865) 1.0 (0.83, 1.31) 9V 848 (731, 984) 824 (694, 977) 1.0 (0.82, 1.29) 14 711 (580, 872) 869 (677, 1115) 0.8 (0.59, 1.13) 18C 1115 (925, 1344) 912 (707, 1177) 1.2 (0.89, 1.67) 19A 471 (408, 543) 390 (318, 477) 1.2 (0.94, 1.55) 19F 819 (697, 963) 626 (504, 779) 1.3 (1.00, 1.71) 23F 216 (169, 277) 84 (62, 114) 2.6 (1.74, 3.79) 14.4 Concomitant Vaccine Administration
Infants and Toddlers
The concomitant administration of routine US infant vaccines [see Drug Interactions (7.1)] with Prevnar 13 was evaluated in two studies: Study 2 [see Clinical Studies (14.2)], Pneumococcal Immune Responses Following Three Doses2, and the US lot consistency study3 (Study 3). In Study 3, subjects were randomly assigned to receive one of 3 lots of Prevnar 13 or Prevnar in a 2:2:2:1 ratio. The total number of infants vaccinated was 6632 (Study 2) and 16993 (Study 3). Immune responses to concomitant vaccine antigens were compared in infants receiving Prevnar and Prevnar 13. Responses to diphtheria toxoid, tetanus toxoid, pertussis, polio types 1, 2, and 3, hepatitis B, PRP-T, PRP-OMP, measles, and varicella antigens in Prevnar 13 recipients were similar to those in Prevnar recipients. Based on limited data, responses to mumps and rubella antigens in Prevnar 13 recipients were similar to those in Prevnar recipients.
Adults ≥50 Years of Age
Concomitant Administration with QIV
Prevnar 13 was administered to PPSV23 previously vaccinated adults ≥50 years of age concomitantly with a US-licensed inactivated influenza vaccine, quadrivalent (IIV4) (Fluzone Quadrivalent) for the 2014/2015 influenza season (Study 13) [see Adverse Reactions (6.2) and Drug Interactions (7.1)]. One study group received Prevnar 13 and IIV4 concurrently, followed approximately one month later by placebo. A second study group received IIV4 and placebo concurrently, followed approximately one month later by Prevnar 13.
Serotype-specific pneumococcal antibody responses were measured one month after Prevnar 13 vaccination as OPA GMTs. Noninferiority was demonstrated for each pneumococcal serotype if the lower limit of the 2-sided 95% CI for the GMT ratio (Prevnar 13 + IIV4 relative to Prevnar 13 alone) was >0.5. Although OPA antibody responses to Prevnar 13 generally appeared to be slightly lower when Prevnar 13 was administered concomitantly with IIV4 compared to Prevnar 13 administered alone, noninferiority was demonstrated for all Prevnar 13 pneumococcal serotypes evaluated in Study 13.
Strain-specific influenza antibody responses were measured one month after IIV4 as hemagglutinin inhibition assay (HAI) titers. HAI GMTs were evaluated for each IIV4 strain in Study 13. Noninferiority was demonstrated if the lower limit of the 2-sided 95% CI for the HAI GMT ratio (Prevnar 13 + IIV4 relative to IIV4 + Placebo) was >0.5. Noninferiority was demonstrated for each IIV4 vaccine strain evaluated in Study 13.
Concomitant Administration with TIV
Two randomized, double-blind clinical trials evaluated the immunogenicity of Prevnar 13 given with IIV3 (Fall 2007/ Spring 2008 Fluarix, A/H1N1, A/H3N2, and B strains) in PPSV23 unvaccinated adults aged 50 through 59 years10 (Study 10, conducted in the US) and in adults ≥65 years11 (Study 11, conducted in Europe). Based on analysis of the primary pre-specified comparison of serotype specific anti-capsular polysaccharide IgG GMCs, noninferiority was met for all serotypes in adults 50–59 years of age and for 12 of 13 serotypes in adults ≥65years of age.
-
15 REFERENCES
ClinicalTrials.gov identifiers for studies included below:
- Study 1 NCT00205803
- Study 2 NCT00373958
- Study 3 NCT00444457
- Study 4 NCT00452452
- Study 5 NCT00761631
- Study 6 NCT00427895
- Study 7 NCT00546572
- Study 8 NCT00574548
- Study 9 NCT00500266
- Study 10 NCT00521586
- Study 11 NCT00492557
- Study 12 NCT00744263
- Study 13 NCT02124161
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Prefilled Syringe, 1 Dose (10 per package) – NDC: 0005-1971-02.
Prefilled Syringe, 1 Dose (1 per package) – NDC: 0005-1971-05.
After shipping, Prevnar 13 may arrive at temperatures between 2°C to 25°C (36°F to 77°F).
Upon receipt, store refrigerated at 2°C to 8°C (36°F to 46°F).
Do not freeze. Discard if the vaccine has been frozen.
Prevnar 13 is stable at temperatures up to 25°C (77°F) for 4 days. These data are not recommendations for shipping or storage, but may guide decisions for use in case of temporary temperature excursions.
The tip cap and rubber plunger of the prefilled syringe are not made with natural rubber latex.
-
17 PATIENT COUNSELING INFORMATION
Prior to administration of this vaccine, inform the individual, parent, guardian, or other responsible adult of the following:
- The potential benefits and risks of immunization with Prevnar 13 [see Warnings and Precautions (5) and Adverse Reactions (6)].
- The importance of completing the immunization series unless contraindicated.
- Any suspected adverse reactions should be reported to their healthcare professional.
Provide the Vaccine Information Statements, which are available free of charge at the Centers for Disease Control and Prevention (CDC) website (www.cdc.gov/vaccines).
This product's label may have been updated. For current full prescribing information, please visit www.pfizer.com.
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Label
NDC: 0005-1971-01
Rx onlyPneumococcal 13-valent Conjugate
Vaccine
(Diphtheria CRM197 Protein)Prevnar 13®
One Dose (0.5 mL)
FOR IM USE ONLYREFRIGERATE
DO NOT FREEZE
SHAKE WELLWyeth Pharm. LLC
US Govt. License No. 3PAA133492
LOT:
EXP:
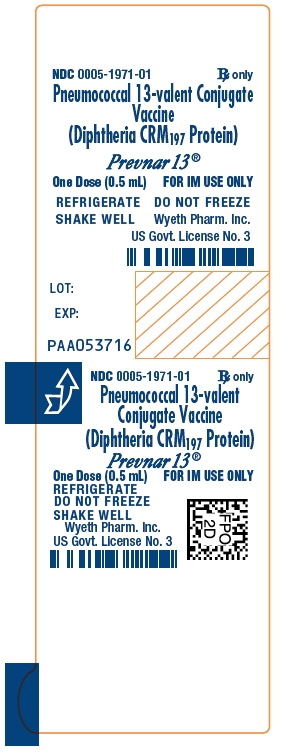
-
PRINCIPAL DISPLAY PANEL - 10 Syringe Carton
NDC: 0005-1971-02
Rx onlyPneumococcal 13-valent Conjugate Vaccine
(Diphtheria CRM197 Protein)Prevnar 13®
10 One-Dose (0.5 mL)
Disposable Syringes
FOR INTRAMUSCULAR USE ONLY
Pfizer
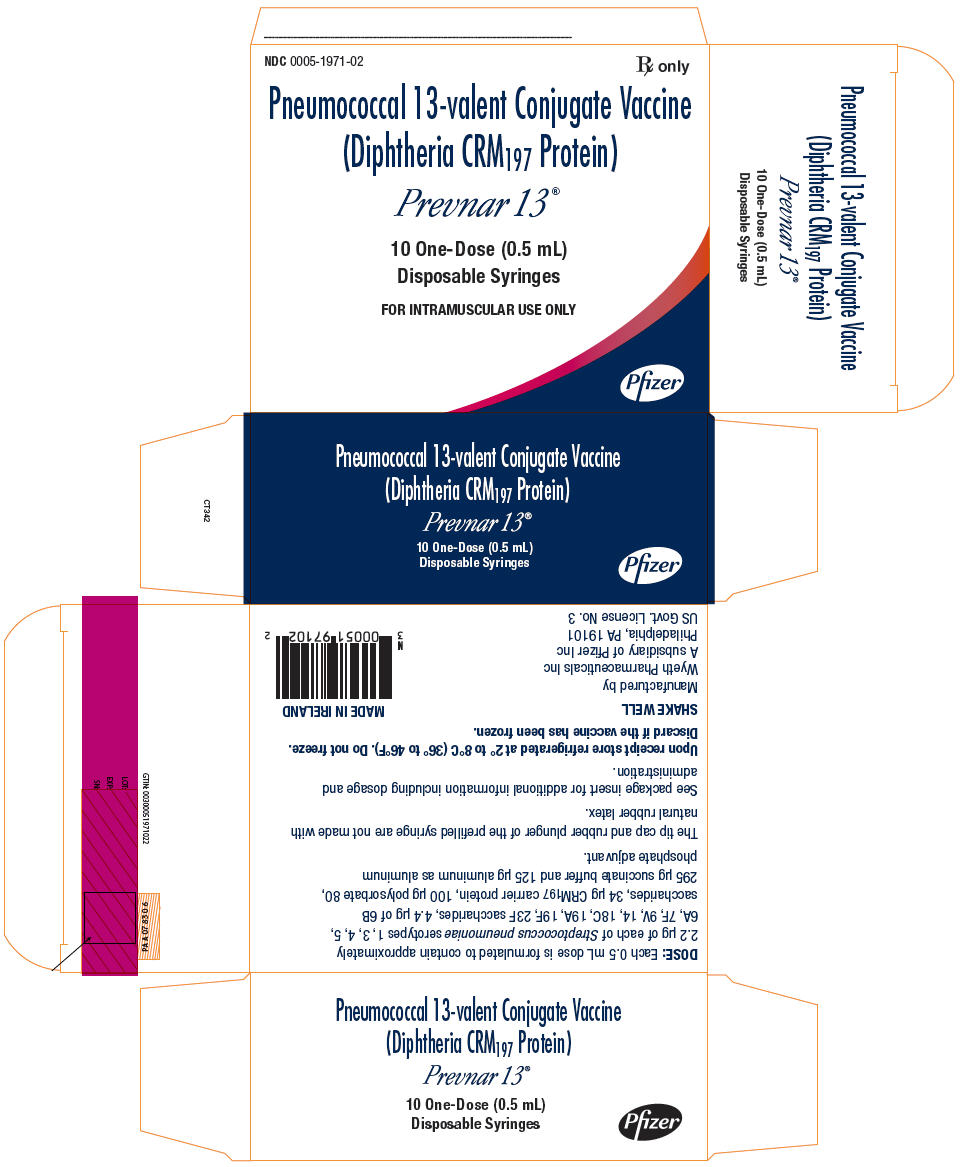
-
PRINCIPAL DISPLAY PANEL - 1 Syringe Carton
NDC: 0005-1971-05
Rx only
Pneumococcal 13-valent Conjugate Vaccine
(Diphtheria CRM197 Protein)Prevnar 13®
One Dose (0.5 mL)
Disposable SyringeFOR INTRAMUSCULAR USE ONLY
Pfizer
-
INGREDIENTS AND APPEARANCE
PREVNAR 13
pneumococcal 13-valent conjugate vaccine injection, suspensionProduct Information Product Type VACCINE Item Code (Source) NDC: 0005-1971 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength STREPTOCOCCUS PNEUMONIAE TYPE 1 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 54EC0SE5PZ) (STREPTOCOCCUS PNEUMONIAE TYPE 1 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:54EC0SE5PZ) STREPTOCOCCUS PNEUMONIAE TYPE 1 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 3 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 2VF3V7175U) (STREPTOCOCCUS PNEUMONIAE TYPE 3 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:2VF3V7175U) STREPTOCOCCUS PNEUMONIAE TYPE 3 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 4 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: TGJ6YZC4W7) (STREPTOCOCCUS PNEUMONIAE TYPE 4 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:TGJ6YZC4W7) STREPTOCOCCUS PNEUMONIAE TYPE 4 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 5 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 5SKG37872O) (STREPTOCOCCUS PNEUMONIAE TYPE 5 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:5SKG37872O) STREPTOCOCCUS PNEUMONIAE TYPE 5 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 6A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: Z9HK08690W) (STREPTOCOCCUS PNEUMONIAE TYPE 6A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:Z9HK08690W) STREPTOCOCCUS PNEUMONIAE TYPE 6A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 6B CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 4M543JVT7G) (STREPTOCOCCUS PNEUMONIAE TYPE 6B CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:4M543JVT7G) STREPTOCOCCUS PNEUMONIAE TYPE 6B CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 4.4 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 7F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 0K0S2P98ZJ) (STREPTOCOCCUS PNEUMONIAE TYPE 7F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:0K0S2P98ZJ) STREPTOCOCCUS PNEUMONIAE TYPE 7F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 9V CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 5Q768OY0GI) (STREPTOCOCCUS PNEUMONIAE TYPE 9V CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:5Q768OY0GI) STREPTOCOCCUS PNEUMONIAE TYPE 9V CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 14 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: SK54I0S386) (STREPTOCOCCUS PNEUMONIAE TYPE 14 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:SK54I0S386) STREPTOCOCCUS PNEUMONIAE TYPE 14 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 18C CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: XK87D9J012) (STREPTOCOCCUS PNEUMONIAE TYPE 18C CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:XK87D9J012) STREPTOCOCCUS PNEUMONIAE TYPE 18C CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 23F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 25N8E57V6T) (STREPTOCOCCUS PNEUMONIAE TYPE 23F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:25N8E57V6T) STREPTOCOCCUS PNEUMONIAE TYPE 23F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 19A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: B970MQT365) (STREPTOCOCCUS PNEUMONIAE TYPE 19A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:B970MQT365) STREPTOCOCCUS PNEUMONIAE TYPE 19A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 19F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 2E1M7F958B) (STREPTOCOCCUS PNEUMONIAE TYPE 19F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:2E1M7F958B) STREPTOCOCCUS PNEUMONIAE TYPE 19F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength POLYSORBATE 80 (UNII: 6OZP39ZG8H) 100 ug in 0.5 mL ALUMINUM PHOSPHATE (UNII: F92V3S521O) 125 ug in 0.5 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0005-1971-02 10 in 1 CARTON 1 NDC: 0005-1971-01 0.5 mL in 1 SYRINGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 2 NDC: 0005-1971-05 1 in 1 CARTON 2 NDC: 0005-1971-01 0.5 mL in 1 SYRINGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125324 03/12/2010 Labeler - Wyeth Pharmaceutical Division of Wyeth Holdings LLC (054065909) Establishment Name Address ID/FEI Business Operations Pfizer Ireland Pharmaceuticals 985586408 ANALYSIS(0005-1971) , API MANUFACTURE(0005-1971) , MANUFACTURE(0005-1971) Establishment Name Address ID/FEI Business Operations Wyeth BioPharma Division of Wyeth Pharmaceuticals LLC 174350868 ANALYSIS(0005-1971) Establishment Name Address ID/FEI Business Operations Wyeth Pharmaceutical Division of Wyeth Holdings LLC 883534067 ANALYSIS(0005-1971) , API MANUFACTURE(0005-1971) Establishment Name Address ID/FEI Business Operations Wyeth Pharmaceutical Division of Wyeth Holdings LLC 054065909 ANALYSIS(0005-1971) , API MANUFACTURE(0005-1971) Establishment Name Address ID/FEI Business Operations Pfizer Manufacturing Belgium NV 370156507 LABEL(0005-1971) , PACK(0005-1971) Establishment Name Address ID/FEI Business Operations John Wyeth & Brother Limited 215193306 LABEL(0005-1971) , PACK(0005-1971)
Trademark Results [PREVNAR 13]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 PREVNAR 13 88389585 not registered Live/Pending |
Wyeth LLC 2019-04-17 |
 PREVNAR 13 77631362 not registered Dead/Abandoned |
Wyeth 2008-12-11 |
 PREVNAR 13 77018369 3811235 Live/Registered |
WYETH LLC 2006-10-11 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.