NATEGLINIDE tablet, coated
Nateglinide by
Drug Labeling and Warnings
Nateglinide by is a Prescription medication manufactured, distributed, or labeled by AvKARE. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
Nateglinide Tablets, USP are an oral antidiabetic agent used in the management of Type 2 diabetes mellitus [also known as non-insulin dependent diabetes mellitus (NIDDM) or adult-onset diabetes]. Nateglinide,(-)-N-[(trans-4-isopropylcyclohexane)carbonyl]-D-phenylalanine, is structurally unrelated to the oral sulfonylurea insulin secretagogues.
The structural formula is as shown
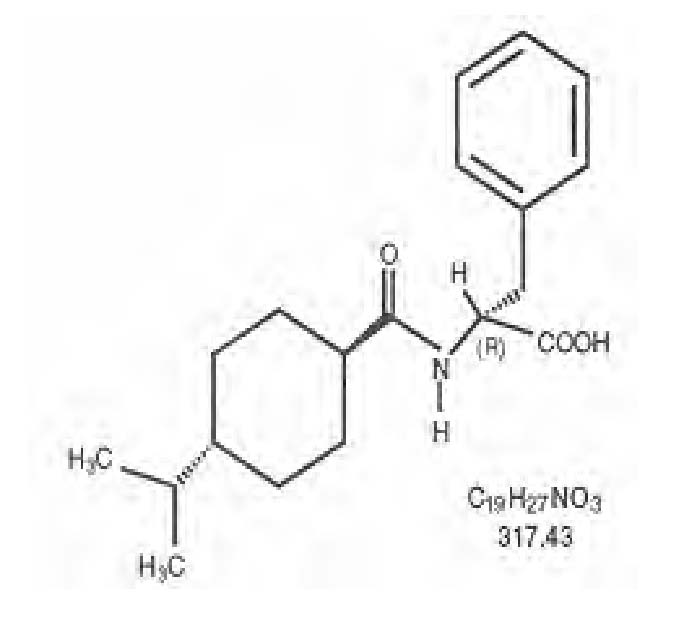
Nateglinide is a white powder with a molecular weight of 317.43. It is freely soluble in methanol, ethanol, and chloroform, soluble in ether, sparingly soluble in acetonitrile and octanol, and practically insoluble in water. Nateglinide biconvex tablets contain 60 mg, or 120 mg, of nateglinide for oral administration.
Inactive Ingredients: colloidal silicon dioxide, croscarmellose sodium, lactose monohydrate, magnesium stearate, microcrystalline cellulose, povidone, pregelatinized starch. The 60 mg also contains iron oxide red, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide. In addition, the 120 mg contains FD&C Yellow #6/Sunset Yellow Aluminum Lake, iron oxide yellow.
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Nateglinide is an amino-acid derivative that lowers blood glucose levels by stimulating insulin secretion from the pancreas. This action is dependent upon functioning beta-cells in the pancreatic islets. Nateglinide interacts with the ATP-sensitive potassium (K+ ATP) channel on pancreatic beta-cells. The subsequent depolarization of the beta cell opens the calcium channel, producing calcium influx and insulin secretion. The extent of insulin release is glucose dependent and diminishes at low glucose levels. Nateglinide is highly tissue selective with low affinity for heart and skeletal muscle.
Pharmacokinetics
Absorption
Following oral administration immediately prior to a meal, nateglinide is rapidly absorbed with mean peak plasma drug concentrations (C max) generally occurring within 1 hour (T max) after dosing. When administered to patients with Type 2 diabetes over the dosage range 60 mg to 240 mg three times a day for one week, nateglinide demonstrated linear pharmacokinetics for both AUC (area under the time/plasma concentration curve) and C max. T max was also found to be independent of dose in this patient population. Absolute bioavailability is estimated to be approximately 73%. When given with or after meals, the extent of nateglinide absorption (AUC) remains unaffected. However, there is a delay in the rate of absorption characterized by a decrease in C max and a delay in time to peak plasma concentration (T max). Plasma profiles are characterized by multiple plasma concentration peaks when nateglinide is administered under fasting conditions. This effect is diminished when nateglinide is taken prior to a meal.
Distribution
Based on data following intravenous (IV) administration of nateglinide, the steady-state volume of distribution of nateglinide is estimated to be approximately 10 liters in healthy subjects. Nateglinide is extensively bound (98%) to serum proteins, primarily serum albumin, and to a lesser extent α 1 acid glycoprotein. The extent of serum protein binding is independent of drug concentration over the test range of 0.1 to 10 mcg/mL.
Metabolism
Nateglinide is metabolized by the mixed-function oxidase system prior to elimination. The major routes of metabolism are hydroxylation followed by glucuronide conjugation. The major metabolites are less potent antidiabetic agents than nateglinide. The isoprene minor metabolite possesses potency similar to that of the parent compound nateglinide.
In vitro data demonstrate that nateglinide is predominantly metabolized by cytochrome P450 isoenzymes CYP2C9 (70%) and CYP3A4 (30%).
Excretion
Nateglinide and its metabolites are rapidly and completely eliminated following oral administration. Within 6 hours after dosing, approximately 75% of the administered 14C-nateglinide was recovered in the urine. Eighty-three percent of the 14C-nateglinide was excreted in the urine with an additional 10% eliminated in the feces. Approximately 16% of the 14C-nateglinide was excreted in the urine as parent compound. In all studies of healthy volunteers and patients with Type 2 diabetes, nateglinide plasma concentrations declined rapidly with an average elimination half-life of approximately 1.5 hours. Consistent with this short elimination half-life, there was no apparent accumulation of nateglinide upon multiple dosing of up to 240 mg three times daily for 7 days.
Drug Interactions
In vitro drug metabolism studies indicate that nateglinide is predominantly metabolized by the cytochrome P450 isozyme CYP2C9 (70%) and to a lesser extent CYP3A4 (30%). Nateglinide is a potential inhibitor of the CYP2C9 isoenzyme in vivo as indicated by its ability to inhibit the in vitro metabolism of tolbutamide. Inhibition of CYP3A4 metabolic reactions was not detected in in vitro experiments.
Glyburide: In a randomized, multiple-dose crossover study, patients with Type 2 diabetes were administered 120 mg nateglinide three times a day before meals for 1 day in combination with glyburide 10 mg daily. There were no clinically relevant alterations in the pharmacokinetics of either agent.
Metformin: When nateglinide 120 mg three times daily before meals was administered in combination with metformin 500 mg three times daily to patients with Type 2 diabetes, there were no clinically relevant changes in the pharmacokinetics of either agent.
Digoxin: When nateglinide 120 mg before meals was administered in combination with a single 1 mg dose of digoxin to healthy volunteers, there were no clinically relevant changes in the pharmacokinetics of either agent.
Warfarin: When healthy subjects were administered nateglinide 120 mg three times daily before meals for four days in combination with a single dose of warfarin 30 mg on day 2, there were no alterations in the pharmacokinetics of either agent. Prothrombin time was not affected.
Diclofenac: Administration of morning and lunch doses of nateglinide 120 mg in combination with a single 75 mg dose of diclofenac in healthy volunteers resulted in no significant changes to the pharmacokinetics of either agent.
Special Populations
Geriatric: Age did not influence the pharmacokinetic properties of nateglinide. Therefore, no dose adjustments are necessary for elderly patients.
Gender: No clinically significant differences in nateglinide pharmacokinetics were observed between men and women. Therefore, no dose adjustment based on gender is necessary.
Race: Results of a population pharmacokinetic analysis including subjects of Caucasian, Black, and other ethnic origins suggest that race has little influence on the pharmacokinetics of nateglinide.
Renal Impairment: Compared to healthy matched subjects, patients with Type 2 diabetes and moderate-to-severe renal insufficiency (CrCl 15 to 50 mL/min) not on dialysis displayed similar apparent clearance, AUC and C max. Patients with Type 2 diabetes and renal failure on dialysis exhibited reduced overall drug exposure. However, hemodialysis patients also experienced reductions in plasma protein binding compared to the matched healthy volunteers.
Hepatic Impairment: The peak and total exposure of nateglinide in non-diabetic subjects with mild hepatic insufficiency were increased by 30% compared to matched healthy subjects. Nateglinide should be used with caution in patients with chronic liver disease. (See PRECAUTIONS, Hepatic Impairment.)
Pharmacodynamics
Nateglinide is rapidly absorbed and stimulates pancreatic insulin secretion within 20 minutes of oral administration. When nateglinide is dosed three times daily before meals there is a rapid rise in plasma insulin, with peak levels approximately 1 hour after dosing and a fall to baseline by 4 hours after dosing.
In a double-blind, controlled clinical trial in which nateglinide was administered before each of three meals, plasma glucose levels were determined over a 12-hour, daytime period after 7 weeks of treatment. Nateglinide was administered 10 minutes before meals. The meals were based on standard diabetic weight maintenance menus with the total caloric content based on each subject’s height. Nateglinide produced statistically significant decreases in fasting and postprandial glycemia compared to placebo.
CLINICAL STUDIES
A total of 3,566 patients were randomized in nine double-blind, placebo-or active-controlled studies 8 to 24 weeks in duration to evaluate the safety and efficacy of nateglinide. 3,513 patients had efficacy values beyond baseline. In these studies nateglinide was administered up to 30 minutes before each of three main meals daily.
Nateglinide Monotherapy Compared to Placebo
In a randomized, double-blind, placebo-controlled, 24-week study, patients with Type 2 diabetes with HbA1c ≥6.8% on diet alone were randomized to receive either nateglinide (60 mg or 120 mg three times daily before meals) or placebo. Baseline HbA1c ranged from 7.9% to 8.1% and 77.8% of patients were previously untreated with oral antidiabetic therapy. Patients previously treated with antidiabetic medications were required to discontinue that medication for at least 2 months before randomization. The addition of nateglinide before meals resulted in statistically significant reductions in mean HbA1c and mean fasting plasma glucose (FPG) compared to placebo (see Table 1). The reductions in HbA1c and FPG were similar for patients naïve to, and those previously exposed to, antidiabetic medications.
In this study, one episode of severe hypoglycemia (plasma glucose <36 mg/dL) was reported in a patient treated with nateglinide 120 mg three times daily before meals. No patients experienced hypoglycemia that required third party assistance. Patients treated with nateglinide had statistically significant mean increases in weight compared to placebo (see Table 1).
In another randomized, double-blind, 24-week, active-and placebo-controlled study, patients with Type 2 diabetes were randomized to receive nateglinide (120 mg three times daily before meals), metformin 500 mg (three times daily), a combination of nateglinide 120 mg (three times daily before meals) and metformin 500 mg (three times daily), or placebo. Baseline HbA1c ranged from 8.3% to 8.4%. Fifty-seven percent of patients were previously untreated with oral antidiabetic therapy. Nateglinide monotherapy resulted in significant reductions in mean HbA1c and mean FPG compared to placebo that were similar to the results of the study reported above (see Table 2).
Table 1: Endpoint results for a 24-week, fixed dose study of Nateglinide monotherapy HbA1c (%) Placebo N=168 Nateglinide 60 mg three times daily before meals N=167 Nateglinide 120 mg three times daily before meals N=168 Baseline (mean) Change from baseline (mean) Difference from placebo (mean 8.0 +0.2 7.9 -0.3 -0.5 a 8.1 -0.5 -0.7 a FPG (mg/dL) N=172 N=171 N=169 Baseline (mean) Change from baseline (mean) Difference from placebo (mean) 167.9 +9.1 161.0 +0.4 -8.7 a 166.5 -4.5 -13.6 a Weight (kg) N=170 N=169 N=166 Baseline (mean) Change from baseline (mean) Difference from placebo (mean) 85.8 -0.7 83.7 +0.3 +1.0 a 86.3 +0.9 +1.6 a Nateglinide Monotherapy Compared to Other Oral Antidiabetic Agents
In a 24-week, double-blind, active-controlled trial, patients with Type 2 diabetes who had been on a sulfonylurea for ≥ 3 months and who had a baseline HbA 1c ≥6.5% were randomized to receive nateglinide (60 mg or 120 mg three times daily before meals) or glyburide 10 mg once daily. Patients randomized to nateglinide had significant increases in mean HbA 1c and mean FPG at endpoint compared to patients randomized to glyburide.
In another randomized, double-blind, 24-week, active- and placebo-controlled study, patients with Type 2 diabetes were randomized to receive nateglinide (120 mg three times daily before meals), metformin 500 mg (three times daily), a combination of nateglinide 120 mg (three times daily before meals) and metformin 500 mg (three times daily), or placebo. Baseline HbA 1c ranged from 8.3% to 8.4%. Fifty-seven percent of patients were previously untreated with oral antidiabetic therapy. Patients previously treated with antidiabetic medications were required to discontinue medication for at least 2 months before randomization. The reductions in mean HbA 1c and mean FPG at endpoint with metformin monotherapy were significantly greater than the reductions in these variables with nateglinide monotherapy (see Table 2). Relative to placebo, nateglinide monotherapy was associated with significant increases in mean weight whereas metformin monotherapy was associated with significant decreases in mean weight. Among the subset of patients naïve to antidiabetic therapy, the reductions in mean HbA 1c and mean FPG for nateglinide monotherapy were similar to those for metformin monotherapy (see Table 2). Among the subset of patients previously treated with other antidiabetic agents, primarily glyburide, HbA 1c in the nateglinide monotherapy group increased slightly from baseline, whereas HbA 1c was reduced in the metformin monotherapy group (see Table 2).
Nateglinide Combination Therapy
In the active and placebo-controlled study of metformin and nateglinide described above, the combination of nateglinide and metformin resulted in statistically significantly greater reductions in HbA 1c and FPG compared to either nateglinide or metformin monotherapy (see Table 2). Nateglinide, alone or in combination with metformin, significantly reduced the prandial glucose elevation form pre-meal to 2-hours post-meal compared to placebo and metformin alone.
In this study, one episode of severe hypoglycemia (plasma glucose ≤36 mg/dL) was reported in a patient receiving the combination of nateglinide and metformin and four episodes of severe hypoglycemia were reported in a single patient in the metformin treatment arm. No patient experienced an episode of hypoglycemia that required third party assistance. Compared to placebo, nateglinide monotherapy was associated with a statistically significant increase in weight, while no significant change in weight was observed with combined nateglinide and metformin therapy (see Table 2).
In another 24-week, double-blind, placebo-controlled trial, patients with Type 2 diabetes with HbA1c ≥6.8% after treatment with metformin (≥1500 mg daily for ≥1 month) were first entered into a four-week run-in period of metformin monotherapy (2000 mg daily) and then randomized to receive nateglinide (60 mg or 120 mg three times daily before meals) or placebo in addition to metformin. Combination therapy with nateglinide and metformin was associated with statistically significantly greater reductions in HbA1c compared to metformin monotherapy (-0.4% and -0.6% for nateglinide 60 mg and nateglinide 120 mg plus metformin, respectively).
Table 2: Endpoint results for a 24-week study of Nateglinide monotherapy and combination with metformin HbA1c (%) All Placebo N=160 Nateglinide 120 mg three times daily before meals N=171 Metformin 500 mg three times daily N=172 Nateglinide 120 mg before meals plus Metformin* N=162 Baseline (mean) Change from baseline (mean) Difference from placebo Naïve 8.3 +0.4 N=98 8.3 -0.4 bc -0.8 a N=99 8.4 -0.8 c -1.2 a N=98 .4 -1.5 -1.9 a N=81 Baseline (mean) Change from baseline (mean) Difference from placebo Non-Naïve 8.2 +0.3 N=62 8.1 -0.7 c -1.0 a N=72 8.3 -0.8 c -1.1 a N=74 8.2 -1.6 -1.9 a N=81 Baseline (mean) Change from baseline (mean) Difference from placebo FPG (mg/dL) All 8.3 +0.6 N=166 8.5 +0.004 bc -0.6 a N=173 8.7 -0.8 c -1.4 a N=174 8.7 -1.4 -2.0 a N=167 Baseline (mean) Change from baseline (mean) Difference from placebo Weight (kg) All 194.0 +8.0 N=160 196.5 -13.1 bc -21.1 a N=169 196.0 -30.0 c -38.0 a N=169 197.7 -44.9 -52.9 a N=160 Baseline (mean) Change from baseline (mean) Difference from placebo 85.0-0.4 85.0 +0.9 bc +1.3 a 86.0 -0.1 +0.3 87.4 +0.2 +0.6 A 24-week, double blind multicenter, placebo-controlled trial was performed in patients with Type 2 diabetes not adequately controlled after a therapeutic response to rosiglitazone monotherapy 8 mg daily. The addition of nateglinide (120 mg three times per day with meals) was associated with statistically significantly greater reductions in HbA 1c compared to rosiglitazone monotherapy. The difference was -0.77% at 24 weeks. The mean change in weight from baseline was about +3 kg for patients treated with nateglinide plus rosiglitazone vs about +1 kg for patients treated with placebo plus rosiglitazone.
In a 12-week study of patients with Type 2 diabetes inadequately controlled on glyburide 10 mg once daily, the addition of nateglinide (60 mg or 120 mg three times daily before meals) did not produce any additional benefit.
- INDICATIONS AND USAGE
- CONTRAINDICATIONS
-
PRECAUTIONS
Macrovascular Outcomes: There have been no clinical studies establishing conclusive evidence of macrovascular risk reduction with nateglinide or any other antidiabetic drug.
Hypoglycemia: All oral blood glucose lowering drugs that are absorbed systemically are capable of producing hypoglycemia. The frequency of hypoglycemia is related to the severity of the diabetes, the level of glycemic control, and other patient characteristics. Geriatric patients, malnourished patients, and those with adrenal or pituitary insufficiency or severe renal impairment are more susceptible to the glucose lowering effect of these treatments. The risk of hypoglycemia may be increased by strenuous physical exercise, ingestion of alcohol, insufficient caloric intake on an acute or chronic basis, or combinations with other oral antidiabetic agents. Hypoglycemia may be difficult to recognize in patients with autonomic neuropathy and/or those who use beta-blockers. Nateglinide should be administered prior to meals to reduce the risk of hypoglycemia. Patients who skip meals should also skip their scheduled dose of nateglinide to reduce the risk of hypoglycemia.
Hepatic Impairment: Nateglinide should be used with caution in patients with moderate-to-severe liver disease because such patients have not been studied.
Transient loss of glycemic control may occur with fever, infection, trauma, or surgery. Insulin therapy may be needed instead of nateglinide therapy at such times. Secondary failure, or reduced effectiveness of nateglinide over a period of time, may occur.
Information for Patients
Patients should be informed of the potential risks and benefits of nateglinide and of alternative modes of therapy. The risks and management of hypoglycemia should be explained. Patients should be instructed to take nateglinide 1 to 30 minutes before ingesting a meal, but to skip their scheduled dose if they skip the meal so that the risk of hypoglycemia will be reduced. Drug interactions should be discussed with patients. Patients should be informed of potential drug-drug interactions with nateglinide.
Laboratory Tests
Response to therapies should be periodically assessed with glucose values and HbA 1c levels.
Drug Interactions
Nateglinide is highly bound to plasma proteins (98%), mainly albumin. In vitro displacement studies with highly protein-bound drugs such as furosemide, propranolol, captopril, nicardipine, pravastatin, glyburide, warfarin, phenytoin, acetylsalicylic acid, tolbutamide, and metformin showed no influence on the extent of nateglinide protein binding. Similarly, nateglinide had no influence on the serum protein binding of propranolol, glyburide, nicardipine, warfarin, phenytoin, acetylsalicylic acid and tolbutamide in vitro. However, prudent evaluation of individual cases is warranted in the clinical setting.
Certain drugs, including nonsteroidal anti-inflammatory agents (NSAIDs), salicylates, monoamine oxidase inhibitors, and non-selective beta-adrenergic-blocking agents, guanethidine, and CYP2C9 inhibitors (e.g., fluconazole, amiodarone, miconazole, oxandrolone) may potentiate the hypoglycemic action of nateglinide and other oral antidiabetic drugs.
Certain drugs including thiazides, corticosteroids, thyroid products, sympathomimetics, somatropin, rifampin, phenytoin and dietary supplements (St. John’s wort) may reduce the hypoglycemic action of nateglinide and other oral antidiabetic drugs. Somatostatin analogues may potentiate or attenuate the hypoglycemic action of nateglinide.
When these drugs are administered to or withdrawn from patients receiving nateglinide, the patient should be observed closely for changes in glycemic control.
Drug/Food Interactions
The pharmacokinetics of nateglinide were not affected by the composition of a meal (high protein, fat, or carbohydrate). However, peak plasma levels were significantly reduced when nateglinide was administered 10 minutes prior to a liquid meal. Nateglinide did not have any effect on gastric emptying in healthy subjects as assessed by acetaminophen testing.
Carcinogenesis and Mutagenesis and Impairment of Fertility
Carcinogenicity: A two-year carcinogenicity study in Sprague-Dawley rats was performed with oral doses of nateglinide up to 900 mg/kg/day, which produced AUC exposures in male and female rats approximately 30 and 40 times the human therapeutic exposure respectively with a recommended nateglinide dose of 120 mg, three times daily before meals. A two-year carcinogenicity study in B6C3F1 mice was performed with oral doses of nateglinide up to 400 mg/kg/day, which produced AUC exposures in male and female mice approximately 10 and 30 times the human therapeutic exposure with a recommended nateglinide dose of 120 mg, three times daily before meals. No evidence of a tumorigenic response was found in either rats or mice.
Mutagenesis: Nateglinide was not genotoxic in the in vitro Ames test, mouse lymphoma assay, chromosome aberration assay in Chinese hamster lung cells, or in the in vivo mouse micronucleus test.
Impairment of Fertility: Fertility was unaffected by administration of nateglinide to rats at doses up to 600 mg/kg (approximately 16 times the human therapeutic exposure with a recommended nateglinide dose of 120 mg three times daily before meals).
Pregnancy
Pregnancy Category C:
Nateglinide was not teratogenic in rats at doses up to 1000 mg/kg (approximately 60 times the human therapeutic exposure with a recommended nateglinide dose of 120 mg, three times daily before meals). In the rabbit, embryonic development was adversely affected and the incidence of gallbladder agenesis or small gallbladder was increased at a dose of 500 mg/kg (approximately 40 times the human therapeutic exposure with a recommended nateglinide dose of 120 mg, three times daily before meals). There are no adequate and well-controlled studies in pregnant women. Nateglinide should not be used during pregnancy.
Nursing Mothers
Studies in lactating rats showed that nateglinide is excreted in the milk; the AUC 0-48h ratio in milk to plasma was approximately 1:4. During the peri- and postnatal period body weights were lower in offspring of rats administered nateglinide at 1000 mg/kg (approximately 60 times the human therapeutic exposure with a recommended nateglinide dose of 120 mg, three times daily before meals). It is not known whether nateglinide is excreted in human milk. Because many drugs are excreted in human milk, nateglinide should not be administered to a nursing woman.
-
ADVERSE REACTIONS
In clinical trials, approximately 2,600 patients with Type 2 diabetes were treated with nateglinide. Of these, approximately 1,335 patients were treated for 6 months or longer and approximately 190 patients for one year or longer.
Hypoglycemia was relatively uncommon in all treatment arms of the clinical trials. Only 0.3% of nateglinide patients discontinued due to hypoglycemia. Symptoms suggestive of hypoglycemia have been observed after administration of nateglinide. These symptoms included sweating, trembling, dizziness, increased appetite, palpitations, nausea, fatigue and weakness.
Gastrointestinal symptoms, especially diarrhea and nausea, were no more common in patients using the combination of nateglinide and metformin than in patients receiving metformin alone. Likewise, peripheral edema was no more common in patients using the combination of nateglinide and rosiglitazone than in patients receiving rosiglitazone alone. The following table lists events that occurred more frequently in nateglinide patients than placebo patients in controlled clinical trials.
Common Adverse Events (≥2% in nateglinide patients) in Nateglinide Monotherapy Trials (% of patients) Preferred Term PlaceboN=458 NateglinideN=1441 Upper Respiratory Infection 8.1 10.5 Back Pain 3.7 4.0 Flu Symptoms 2.6 3.6 Dizziness 2.2 3.6 Arthropathy 2.2 3.3 Diarrhea 3.1 3.2 Accidental Trauma 1.7 2.9 Bronchitis 2.6 2.7 Coughing 2.2 2.4 Hypoglycemia 0.4 2.4 During post-marketing experience, rare cases of hypersensitivity reactions such as rash, itching and urticaria have been reported. Similarly, cases of jaundice, cholestatic hepatitis and elevated liver enzymes have been reported.
Laboratory Abnormalities
Uric Acid:There were increases in mean uric acid levels for patients treated with nateglinide alone, nateglinide in combination with metformin, metformin alone, and glyburide alone. The respective differences from placebo were 0.29 mg/dL, 0.45 mg/dL, 0.28 mg/dL, and 0.19 mg/dL. The clinical significance of these findings is unknown.
To report SUSPECTED ADVERSE REACTIONS contact AvKARE, Inc. at 1-855-361-3993; email drugsafety@avkare.com; or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
-
OVERDOSAGE
In a clinical study in patients with Type 2 diabetes, nateglinide was administered in increasing doses up to 720 mg a day for 7 days and there were no clinically significant adverse events reported. There have been no instances of overdose with nateglinide in clinical trials. However, an overdose may result in an exaggerated glucose-lowering effect with the development of hypoglycemic symptoms. Hypoglycemic symptoms without loss of consciousness or neurological findings should be treated with oral glucose and adjustments in dosage and/or meal patterns. Severe hypoglycemic reactions with coma, seizure, or other neurological symptoms should be treated with intravenous glucose. As nateglinide is highly protein bound, dialysis is not an efficient means of removing it from the blood.
-
DOSAGE AND ADMINISTRATION
Nateglinide Tablets USP should be taken 1 to 30 minutes prior to meals.
Monotherapy and Combination with Metformin or a Thiazolidinedione
The recommended starting and maintenance dose of nateglinide, alone or in combination with metformin or a thiazolidinedione, is 120 mg three times daily before meals.
The 60 mg dose of nateglinide, either alone or in combination with metformin or a thiazolidinedione, may be used in patients who are near goal HbA 1c when treatment is initiated.
Dosage in Geriatric Patients
No special dose adjustments are usually necessary. However, greater sensitivity of some individuals to nateglinide therapy cannot be ruled out.
Dosage in Renal and Hepatic Impairment
No dosage adjustment is necessary in patients with mild-to-severe renal insufficiency or in patients with mild hepatic insufficiency. Dosing of patients with moderate-to-severe hepatic dysfunction has not been studied. Therefore, nateglinide should be used with caution in patients with moderate-to-severe liver disease (see PRECAUTIONS, Hepatic Impairment).
-
HOW SUPPLIED
Pink color coated, round biconvex, beveled edge tablet debossed with “P 984” on one side and plain on the other side
Bottles of 100..........NDC: 42291-636-01
Orange color coated, oval shaped biconvex, tablet debossed with “P 985” on one side and plain on the other side
Bottles of 100........NDC: 42291-637-01
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). [See USP Controlled Room Temperature].
Dispense in a tight, light resistant containers.
Manufactured for:
AvKARE, Inc.
Pulaski, TN 38478
Mfg. Rev. 02/16
AV 04/16 (P) -
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
AvKARE
NDC 42291-636-01
Nateglinide Tablets, USP
60 mg
100 Tablets Rx Only
Each tablet contains:
Nateglinide, USP ................................ 60 mg
USUAL DOSAGE:
See accompanying prescribing information.
KEEP THIS AND ALL DRUGS OUT OF THE REACH OF CHILDREN.Dispense in a tight, light-resistant container as defined in the USP.
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
[See USP Controlled Room Temperature.]Manufactured for:
AvKARE, Inc.
Pulaski, TN 38478
Mfg. Rev. 10/10 AV 04/16 (P)N3 42291 63601 9

AvKARE
NDC 42291-637-01
Nateglinide Tablets, USP
120 mg
100 Tablets Rx OnlyEach tablet contains:
Nateglinide, USP ................................ 120 mg
USUAL DOSAGE:
See accompanying prescribing information.
KEEP THIS AND ALL DRUGS OUT OF THE REACH OF CHILDREN.Dispense in a tight, light-resistant container as defined in the USP.
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
[See USP Controlled Room Temperature.]Manufactured for:
AvKARE, Inc.
Pulaski, TN 38478
Mfg. Rev. 10/10 AV 04/16 (P)N3 42291 63701 6

-
INGREDIENTS AND APPEARANCE
NATEGLINIDE
nateglinide tablet, coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 42291-636(NDC:49884-984) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NATEGLINIDE (UNII: 41X3PWK4O2) (NATEGLINIDE - UNII:41X3PWK4O2) NATEGLINIDE 60 mg Inactive Ingredients Ingredient Name Strength POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE (UNII: FZ989GH94E) POLYVINYL ALCOHOL (UNII: 532B59J990) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color pink Score no score Shape ROUND Size 1mm Flavor Imprint Code P;984 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 42291-636-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 04/06/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077463 04/06/2016 NATEGLINIDE
nateglinide tablet, coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 42291-637(NDC:49884-985) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NATEGLINIDE (UNII: 41X3PWK4O2) (NATEGLINIDE - UNII:41X3PWK4O2) NATEGLINIDE 120 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE (UNII: FZ989GH94E) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color orange Score no score Shape OVAL Size 6mm Flavor Imprint Code P;985 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 42291-637-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 04/06/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077463 04/06/2016 Labeler - AvKARE, Inc. (796560394)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.