MIX OF 5 STANDARD GRASS POLLEN- agrostis gigantea pollen, anthoxanthum odoratum pollen, dactylis glomerata pollen, phleum pratense pollen and poa pratensis pollen injection, solution MIX OF 6 STANDARD GRASS POLLEN- agrostis gigantea pollen, dactylis glomerata pollen, festuca pratensis pollen, lolium perenne pollen, phleum pratense pollen and poa pratensis pollen injection, solution MIX OF 7 STANDARD GRASS POLLEN- agrostis gigantea pollen, anthoxanthum odoratum pollen, dactylis glomerata pollen, festuca pratensis pollen, lolium perenne pollen, phleum pratense pollen and poa pratensis pollen injection, solution GRASS MIX 4-S- agrostis gigantea pollen, anthoxanthum odoratum pollen, dactylis glomerata pollen, festuca pratensis pollen, lolium perenne pollen, phleum pratense pollen and poa pratensis pollen injection, solution
GRASS MIX 4-S by
Drug Labeling and Warnings
GRASS MIX 4-S by is a Other medication manufactured, distributed, or labeled by ALK-Abello, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
WARNING
Standardized allergenic extract is intended for use by physicians who are experienced in the administration of standardized (BAU/mL) allergenic extracts for immunotherapy and the emergency care of anaphylaxis, or for use under the guidance of an allergy specialist. Standardized allergenic extracts are not directly interchangeable with allergenic extracts of the same labeled potency from different manufacturers. The initial dose of standardized extract must be based on skin testing as described in the warnings, dosage and administration section of this insert.
Patients should be instructed to recognize adverse reaction symptoms and cautioned to contact the physician's office if reaction symptoms occur. As with all allergenic extracts, severe systemic reactions may occur. In certain individuals, these life-threatening reactions may be fatal.
Patients should be observed for at least 20 - 30 minutes following treatment, and emergency measures, as well as personnel trained in their use, should be immediately available in the event of a life-threatening reaction. Patients with unstable asthma or steroid dependent asthmatics and patients with underlying cardiovascular disease are at greater risk to a fatal outcome from a systemic allergic reaction.
This product should not be injected intravenously. It is intended for percutaneous and subcutaneous use. See the warnings, precautions, adverse reactions and overdosage sections below.
Patients receiving beta-blockers may not be responsive to epinephrine or inhaled bronchodilators. Respiratory obstruction not responding to parenteral or inhaled bronchodilators may require theophylline, oxygen, intubation and the use of life support systems. Parenteral fluid and/or plasma expanders may be utilized for treatment of shock. Adrenocorticosteroids may be administered parenterally or intravenously. Refer to the warnings, precautions and adverse reaction sections below.
Sensitive patients may experience severe anaphylactic reactions resulting in respiratory obstruction, shock, coma and/or death. Adverse events are to be reported to MedWatch (1-800-FDA-1088), Adverse Experience Reporting, HFM-210 Center for Biologics Evaluation & Research, Food & Drug Administration, 1401 Rockville Pike, Rockville, MD 20852-1448.
ALK-Abello, Inc.
Port Washington, NY 11050U.S. Government License No. 1256
-
DESCRIPTION
Standardized allergenic extract of grass pollens from Timothy (Phleum pratense), Orchard (Dactylis glomerata), June (Poa pratensis), Red Top (Agrostis alba), Sweet Vernal (Anthoxanthum odoratum), Meadow Fescue (Festuca elatior), Perennial Rye (Lolium perenne), Bermuda Grass (Cynodon dactylon), in the accompanying vial are sterile, and contain glycerin 50% v/v and phenol 0.4% (preservative). Inert ingredients may include sodium chloride for isotonicity and sodium bicarbonate buffer.
Glycerinated pollen extracts, for subcutaneous injection for immunotherapy and/or percutaneous or intracutaneous testing (see Dosage and Administration section), are prepared from defatted dried pollen extracted in glycerinated Coca’s Fluid, filtered aseptically, and dispensed into multiple dose vials. These are subsequently tested for sterility, safety, and potency.
For ease in use and for lot-to-lot consistency, the potency is expressed in Bioequivalent Allergy Units (BAUs) per milliliter. A value of 10,000 BAU/mL is assigned to the CBER reference standard that can be diluted 1:0.5 million to produce intradermal ƩE (sum of Erythema) of 50 mm in highly puncture reactive subjects1. A value of 100,000 BAU/mL is assigned to the CBER reference standard that can be diluted 1:5 million to produce intradermal ƩE (sum of Erythema) of 50 mm in highly puncture reactive subjects. The relative potency of each lot of standardized extract has been compared to the official CBER reference standard by an acceptable assay such as ELISA Inhibition.2 When the potency is equivalent by ELISA Inhibition to the reference, the product is assigned 10,000 BAU/mL or 100,000 BAU/mL. Standardized grass pollen extracts, except for Bermuda, have potency designations of either 10,000 BAU/mL or 100,000 BAU/mL. Bermuda grass pollen extract is only available with a 10,000 BAU/mL potency designation.
In the ELISA Inhibition assay, a competitive binding assay, the wells of microtiter plates are coated using a characterized allergenic extract. Allergic sera is added to each well. The binding of IgE specific for the coating allergen is inhibited by concentrations of a test sample of an extract of the same allergen. The amount of IgE bound to the solid phase allergen (and subsequently the degree of inhibition) is determined using enzyme-labeled anti-human IgE antibodies and the appropriate substrate. The potency relative to a reference is determined using a parallel line bioassay method.
-
CLINICAL PHARMACOLOGY
Diagnostically (for skin testing) the allergen combines with IgE antibodies fixed to mast cells in the skin.3 This complexing causes an increase in cellular permeability and degranulation of the mast cells releasing chemical mediators. These mediators (such as histamine) are responsible for a local inflammatory response of wheal and erythema typical of a positive skin test reaction and also, the symptoms commonly associated with allergic disease. The more mediator released, the larger the reaction (wheal and erythema).
Treatment consists of the subcutaneous injection of gradually increasing doses of the allergens to which the patient is allergic. It has been demonstrated that this method of treatment induces an increased tolerance to the allergens responsible for the symptoms on subsequent exposure. Although the exact relationships between allergen, skin-sensitizing antibody (IgE) and the blocking antibody (IgG) have not been precisely established, clinically confirmed immunological studies have adduced evidence of the efficacy of hyposensitization therapy.
Numerous controlled studies have demonstrated the clinical efficacy of immunotherapy with cat, dust mites and some pollen, including grass pollen extracts.4 Nevertheless, responses are variable, and in a few studies patients reported no appreciable benefit.
Puncture test data with 10,000 BAU/mL Grass Pollen Extract CBER reference preparations, in 15 grass allergic patients yielded the following sizes of wheal and erythema (Σ = sum of longest diameter and orthogonal cross diameter). 5
A. Puncture bifurcated needle data with 10,000 BAU/mL CBER Reference Grass Pollen Extracts.
Reference FDA PΣErythema (mm) PΣWheal (mm) Pollen Lot # N Mean Range Mean Range Bermuda E4-Ber 15 90.3 43-123 15.7 7-31 June E3-Jkb 15 77.3 47-107 15.9 6-28 Meadow Fescue E4-MF 15 81.1 57-115 11.9 7-22 Orchard E4-Or 15 84.3 57-111 14.1 9-19 Perennial Rye E10-Rye 15 92.3 73-135 17.5 6-36 Red Top E4-Rt 15 77.1 42-98 14.1 8-19 Sweet Vernal E4-SV 15 81.2 28-123 15.7 8-30 Timothy E6-Ti 15 88.3 51-109 16.9 8-40 The intradermal dose (BAU50) of the CBER (FDA) Grass Pollen Extract Reference Preparation required producing a 50 mm Sum of Erythema was calculated based on titration in sensitive individuals.
B. Intradermal Dose of CBER Reference Grass Pollen Extracts for 50mm Sum of Erythema Diameter (BAU50) 5.
Reference FDA BAU 50/mL
Pollen Lot # Mean Range Bermuda E4-Ber 0.02 0.4-0.0003 June E3-Jkb 0.02 0.1-0.004 Meadow Fescue E4-MF 0.02 0.9-0.002 Orchard E4-Or 0.02 1.9-0.002 Perennial Rye E10-Rye 0.02 0.7-0.002 Red Top E4-Rt 0.02 0.8-0.004 Sweet Vernal E4-SV 0.02 1.0-0.002 Timothy E6-Ti 0.02 0.6-0.002 -
INDICATIONS AND USAGE
Indicated use of allergenic extracts is for the diagnosis and treatment (hyposensitization therapy) of patients who experience allergic symptoms due to exposure to grass pollen and who exhibit type I skin sensitivity when tested to those specific allergens.
Hyposensitization (injection) therapy is a treatment for patients exhibiting allergic reactions to seasonal pollens, dust mites, molds, animal danders, and various other inhalants in situations where the offending allergen cannot be avoided.
For previously untreated patients, prior to the initiation of therapy, clinical sensitivity to the standardized grass pollen extract should be established by careful evaluation of the patient's history confirmed by diagnostic skin testing. Hyposensitization should not be prescribed for sensitivities to allergens which can easily be avoided.
10,000 BAU/mL extracts are indicated for percutaneous testing. If negative, the 100,000 BAU/mL dose may be used. Availability of 10,000 and 100,000 BAU/mL dosages facilitate safe switching. Patients who tolerate dilutions prepared from the 10,000 BAU/mL dosage and require a higher dose may be treated with dilutions prepared from the 100,000 BAU/mL dosage.
100,000 BAU/mL concentrations may be especially useful when patients are hyposensitized to numerous allergens. Mixing of allergenic extracts dilutes the potency of each constituent. Using higher concentrations such as 100,000 BAU/mL allows for dilution with other extracts without sacrificing immunizing properties. CAUTION: The final potency of each individual component in a patient mixture should never exceed 10,000 BAU/mL. See also, DOSAGE AND ADMINISTRATION section for discussion of mixture labeling.
-
CONTRAINDICATIONS
A patient should not be immunized with preparations of allergens to which the patient has not demonstrated symptoms, IgE antibodies, positive skin tests, or properly controlled challenge testing. In most cases, immunotherapy is not indicated for those allergens that can be eliminated or minimized by environmental control.
Patients on beta-blockers are not candidates for immunotherapy, as they can be non-responsive to beta-agonists that may be required to reverse a systemic reaction (also see WARNINGS and ADVERSE REACTIONS). In the presence of active symptoms such as rhinitis, wheezing, dyspnea, etc., the indications of immunotherapy must be weighed carefully against the risk of temporarily aggravating the symptoms by the injection itself.
Also, there is some evidence, although inconclusive, that routine immunizations may exacerbate autoimmune diseases. 6,7,8 Hyposensitization should be given cautiously to patients with this predisposition. Patients with severe cardiorespiratory symptoms are at an additional risk during a systemic reaction. The physician must weigh risk to benefit in these cases.
-
WARNINGS
See warnings at the beginning of this package insert.
Patients should always be observed for at least 20 - 30 minutes after any injection. In the event of a marked systemic reaction (for a description of systemic reactions see Adverse Reaction Section), application of a tourniquet above the injection site and intramuscular administration of 0.2 mL to 1.0 mL (0.01 mg/kg) of Epinephrine Injection (1:1000) is recommended. This dose can be repeated after 15 minutes, as needed. Maximal recommended dose for children between 2 and 12 years of age is 0.5 mL. The tourniquet is then gradually released at 15 minute intervals. Patients under treatment with beta-blockers may be refractory to the usual dose of epinephrine. DO NOT GIVE ALLERGENIC EXTRACTS INTRAVENOUSLY.
Volume expanders and vasopressor agents may be required to reverse hypotension. Inhalation bronchodilators and parenteral aminophylline may be required to reverse bronchospasm. In cases of respiratory obstruction, oxygen and intubation may be necessary. Life-threatening reactions unresponsive to the above may require cardiopulmonary resuscitation.
A reduction in starting dose is recommended in the following circumstances:
1. change to a new lot of extract from the same manufacturer;
2. Change to a different manufacturers extract;
3. Change in the extract formula;
4. Change to an extract bearing a later expiration date;
5. When a prolonged lapse in time has occurred since the last injection.
Withhold allergenic extracts temporarily or reduce the dose in patients with any one of the following conditions:
- Severe rhinitis or asthma symptoms;
- Infection or flu accompanied by fever;
- Exposure to excessive amounts of clinically relevant allergen prior to therapy.
Allergenic extracts slowly become less potent with age. During the course of treatment, it may be necessary to continue therapy with a vial of extract bearing a later expiration date. The initial dose of the extract bearing the later expiration date should be lowered to a safe non-reaction-eliciting level. When switching one standardized extract with another, at least 75% reduction in dose is suggested.
Patients with unstable asthma or steroid dependent asthmatics and patients with underlying cardiovascular disease are at greater risk to a fatal outcome from a systemic allergic reaction12.
See also PRECAUTIONS and ADVERSE REACTIONS.
-
PRECAUTIONS
Information for Patients:
Patients should be instructed to describe any active allergic symptoms such as rhinitis, wheezing, dyspnea, etc. prior to injection including any late reactions from previous administration. Patients should be instructed to remain in the office for 20 to 30 minutes after injection to monitor for adverse reactions. Also, see ADVERSE REACTIONS and WARNINGS sections.
General:
1. In the presence of active symptoms such as rhinitis, wheezing, dyspnea, etc., the indications of immunotherapy must be weighed carefully against the risk of temporarily aggravating the symptoms by the injection itself. Objective assessment of pulmonary function such as Peak Expiratory Flow Rate (PEFR) before allergen administration and prior to discharge may be useful in unstable asthmatics to reduce the chances of exacerbation of the patient’s asthma. If the protective action of allergenic extract injections is considered essential for the patient's welfare, appropriate symptomatic therapy with antihistaminic, beta-adrenergic or other drugs might be needed either prior to or in conjunction with the allergenic extract injections.
2. Store allergenic extracts between 2o and 8oC at all times, even during use.
3. Injections are to be given subcutaneously with the usual sterile precautions using a Tuberculin syringe.
4. Care must be taken to avoid injecting into a blood vessel. Pull gently on syringe plunger to determine if a blood vessel has been entered (See boxed Warnings).
5. Use standard aseptic precautions when making dilutions.
6. Extracts in 50% glycerin can cause discomfort at the site of the injection during the injection. Glycerinated extracts diluted for intradermal testing must be diluted at least twenty-five-fold to less than 2% glycerin (by volume), as glycerin above this level can cause false positive intradermal skin tests. Use of negative control skin test containing an equal concentration of glycerin as the allergen when evaluating intradermal skin tests is recommended.
7. Standardized concentrates of allergenic extracts must be diluted prior to initiation of immunotherapy.
Pregnancy - Category C:
Animal reproduction studies have not been conducted with allergenic extracts. It is also not known whether allergenic extracts can cause fetal harm when administered to a pregnant woman, or can affect reproduction capacity.
Controlled studies of hyposensitization with moderate to high doses of allergenic extracts during conception and all trimesters of pregnancy have failed to demonstrate any risk to the fetus or to the mother13. However, on the basis of histamine's known ability to contract the uterine muscle, the release of significant amounts of histamine from allergen exposure of hyposensitization overdose should be avoided on theoretical grounds. Therefore, allergenic extracts should be used cautiously in a pregnant woman, and only if clearly needed.
Pediatric Use:
Children can receive the same dose as adults, however, to minimize discomfort associated with dose volume it may be advisable to reduce the volume of the dose by one-half and administer the injection at two different sites.
Geriatric Use:
Studies in geriatric patients have not been conducted. Physicians should consider risk to benefit of immunotherapy in this patient population.
Nursing Mothers:
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when allergenic extracts are administered to a nursing woman.
Drug Interactions:
Drugs can interfere with the performance of skin tests.9
Antihistamines: Response to mediator (histamine) released by allergens is suppressed by antihistamines. The length of suppression varies and is dependent on individual patient, type of antihistamine and length of time the patient has been on antihistamines. The duration of this suppression may be as little as 24 hours to several days.
Tricyclic Antidepressants: These exert a potent and sustained decrease of skin reactivity to histamine which may last for a few weeks.
Beta2 Agonists: Oral terbutaline and parenteral ephedrine, in general, have been shown to decrease allergen induced wheal.
Dopamine: Intravenous infusion of dopamine may inhibit skin test responses.
Beta Blocking Agents: Propranolol can significantly increase skin test reactivity (see boxed Warnings).
Other Drugs: Short acting steroids, inhaled beta2 agonists, theophylline and cromolyn do not seem to affect skin test response.
-
ADVERSE REACTIONS
Local:
Reactions at the site of injection may be immediate or delayed. Immediate wheal and erythema reactions are ordinarily of little consequence; but if very large, may be the first manifestation of a systemic reaction. If large local reactions occur, the patient should be observed for systemic symptoms for which treatment is outlined below. However, systemic reactions may occur in the absence of large local reactions.
Delayed reactions start several hours after injection with local edema, erythema, itching or pain. They are usually at their peak at 24 hours, and usually require no treatment. Antihistamine drugs may be administered orally.
The next therapeutic dose should be reduced to the dose which did not elicit a reaction, and subsequent doses increased more slowly, i.e., use of intermediate dilutions.
Systemic:
It should be noted that anaphylaxis and deaths following the injection of mite and other extracts, including grass pollen extracts have been reported by The British Committee on Safety in Medicine.10 Fatalities from immunotherapy in the United States since 1945 have been extensively reviewed by Lockey, R. F., et al.11 Reid, M.J., et al.12 and also more recently by Bernstein, D. I. et al.15. With careful attention to dosage and administration, such reactions occur infrequently, but it must be remembered that allergenic extracts are highly potent to sensitive individuals and OVERDOSE could result in anaphylactic symptoms. Therefore, it is imperative that physicians administering allergenic extracts understand and be prepared for the treatment of severe reactions.
Systemic reactions are characterized by one or more of the following symptoms: sneezing, mild to severe generalized urticaria, itching, other than at the injection site, extensive or generalized edema, wheezing, asthma, dyspnea, cyanosis, hypotension, syncope and upper airway obstruction. Symptoms may progress to shock and death. Patients should always be observed for at least 20 - 30 minutes after any injection. Volume expanders and vasopressor agents may be required to reverse hypotension. Inhalational bronchodilators and parenteral aminophylline may be required to reverse bronchospasm. Severe airway obstruction, unresponsive to bronchodilator, may require tracheal intubation and use of oxygen. In the event of a marked systemic reaction, application of a tourniquet above the injection site and the administration of 0.2 mL to 1.0 mL of Epinephrine Injection (1:1000) intramuscular is recommended. Maximal recommended dose for children under 2 years of age is 0.3 mL. Maximal recommended dose for children between 2 and 12 years of age is 0.5 mL. The tourniquet should not be left in place without loosening for 90 seconds every 15 minutes.
The next therapeutic injection of extract should be reduced to the dose which did not elicit a reaction, and subsequent doses increased more slowly; i.e., use of intermediate dilutions.
Adverse Events should be reported via MedWatch (1-800-FDA-1088), Adverse Experience Reporting, HFM-210 Center for Biologics Evaluation & Research, Food & Drug Administration, 1401 Rockville Pike, Rockville, MD 20852-1448.
- OVERDOSAGE
-
DOSAGE AND ADMINISTRATION
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
When diluting bulk extracts, use of Sterile Diluent for Allergenic Extracts or Sterile Diluent for Allergenic Extracts Normal Saline with HSA are recommended. Dilutions should be made with sterile disposable syringes using aseptic technique. Commonly 10 fold dilutions are used to achieve a desired concentration for intradermal testing or initiation and continuation of immunotherapy. For example transferring 0.5 mL of a 10,000 BAU/mL extract into 4.5 mL of diluent will yield 5 mL of extract at 1,000 BAU/mL. Prepare as many additional serial dilutions as necessary to reach the appropriate concentration.
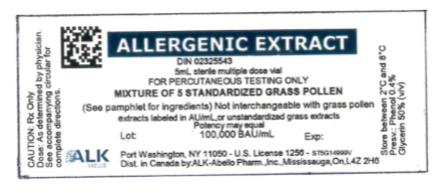
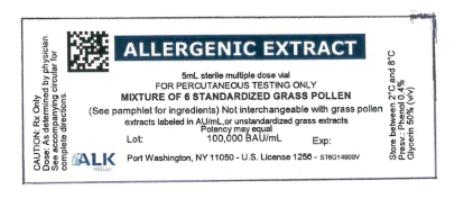
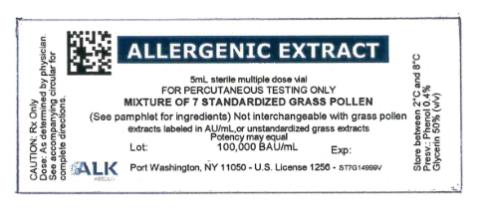
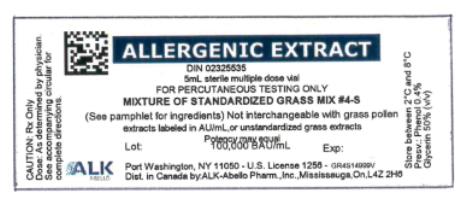
Stock mixtures of grass pollen extracts are compounded from individual grass pollen extracts. The total potency per milliliter (mL) of these mixtures is described on the container label, where space permits. The contribution each individual component is expressed in the supplemental labeling accompanying the vial.
Diagnosis - In diagnosing the sensitive individual, the symptom history must be associated with exposure to the allergen. Skin testing is used in conjunction with a definitive history for diagnosing individual sensitivities.
An excellent method of recording results is to cover the skin reaction with transparent tape, outline the erythema first then the wheal with an indelible pen, then remove the tape and transfer it to the patient's permanent record. For preferred results, it is recommended that the actual measurement of the extent of both responses be recorded. This can be accomplished by measuring the longest erythema diameter, then selecting the mid-point of that line and measuring at a 90o angle to that line to determine the orthogonal diameter. The sum of these two measurements is the sum of erythema (ΣE); the sum of wheal diameters is determined in a similar manner.
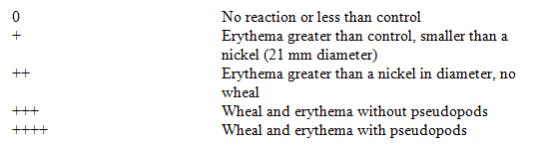
Patient's response is graded on the basis of the size of erythema and/or wheal.
Percutaneous (prick/scratch/puncture) test:
Prick, scratch, or puncture skin tests should be performed initially using a glycerinated extract at 10,000 BAU/mL.
What follows are general guidelines for percutaneous testing14. Different devices and/or techniques influence the size of the reaction, therefore it is important to refer to the device manufacturer's or distributor's instructions when grading reactions. As a negative control the diluent should be tested and included in the interpretation in the skin test reactions. Use of a positive control such as histamine base at 1 mg/mL should be used to assess skin test reactivity.
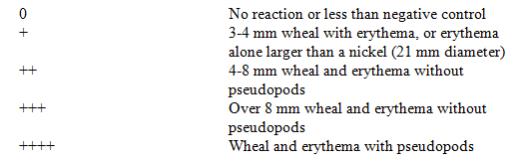
Intradermal test:
Intradermal testing should start with a dilute solution, usually in the range of 0.1 BAU/mL or less.
Glycerinated extracts diluted for intradermal testing may be diluted at least 25-fold to less than 2% glycerin (by volume) as glycerin above this level can cause false positive intradermal skin tests. Use a negative control skin test with glycerin content equal to the glycerin content of the allergen dose used for intradermal testing. Use of a positive control such as histamine base at 0.1 mg/mL or 0.01 mg/mL should be used to test reactivity.
On the forearm or upper outer aspect of the arm, using a 26 - 27 gauge, short bevel needle, inject intradermally 0.05 mL of the intradermal test solution. Skin whealing responses should be observed 10 - 20 minutes after administering the test.
A negative skin test is one where the sum of erythema was 0 or equal to the sum of the wheal. As a negative control, the diluent should be tested and included in the interpretation of the skin reactions. What follows are general guidelines intradermal testing 14.
Immunotherapy - Starting dose for immunotherapy is related directly to a patient's sensitivity as determined by carefully executed skin testing. Degree of sensitivity can be established by determination of D50 (the intradermal dose, base three, that produces a ΣE = 50 mm).1
A general rule is to begin at 1/10 of the dose that produces sum of erythema of 50 mm (approximately a 2+ positive skin test reaction). For example, if a patient exhibits a 2+ intradermal reaction to 1 BAU/mL, the first dose should be no higher than 0.05 mL of 0.1 BAU/mL. Dosage may be increased by 0.05 mL each time until 0.5 mL is reached, at which time the next 10-fold more concentrated dilution can be used, beginning with 0.05 mL, if no untoward reaction is observed.
If a tolerated dose of allergenic extract has been established, the initial dose from the new extract should be reduced to 25% of the previously well tolerated dose (see also Precautions).
Interval between doses in the early stages of immunotherapy is no more than once to twice a week, and may gradually be increased to once every two weeks. Generally, maintenance injections may be given as infrequently as once every two weeks to once a month.
Injections are given subcutaneously preferably in the arm. It is advantageous to give injections in alternate arms and routinely in the same area. In some patients, a local tolerance to the allergen may develop thus preventing a possible severe local reaction.
After inserting the needle, but before injecting the dose, pull plunger of the syringe slightly. If blood returns in the syringe, discard the syringe and contents and repeat injection at another site.
Bulk concentrated extracts must be diluted for initial therapy and intradermal skin testing. For recommended diluent, refer to DOSAGE AND ADMINISTRATION section.
Use standard aseptic precautions when making dilutions. The first dose of the new extract should be reduced at least 75% of the amount of the dosage from the previous extract.
Stability studies indicate that undiluted products will retain its potency under recommended storage conditions. Stability studies for undiluted forms of this product are not complete. It is recommended that minimal amounts of the concentrate be diluted so that the diluted product is used up within a relatively short period of time; i.e., preferably not more than four weeks.
-
HOW SUPPLIED
For percutaneous testing, 5 mL vial, 10,000 BAU/mL and 100,000 BAU/mL (except Bermuda grass 10,000 BAU/mL only) in glycerin 50% (v/v).
For immunotherapy, 10 mL, 30 mL, and 50 mL vials 10,000 BAU/mL in glycerin 50% (v/v), or 10 mL, 30 mL and 50 mL vials 100,000 BAU/mL in glycerin 50% (v/v). Bermuda is available only at 10,000 BAU/mL.
STORAGE: To maintain stability of allergenic extracts, proper storage conditions are essential. Bulk concentrates and diluted extracts are to be stored at 2o to 8o C even during use. Bulk or diluted extracts are not to be frozen. Do not use after the expiration date shown on the vial label.
-
REFERENCES
1Turkeltaub, P. C. et al. Office of Biologics Research and Review skin test method for evaluation of subject sensitivity to standardized allergenic extracts and for assignment of allergy units to reference preparations using the ID50EAL method. FDA CBER Methods of the Allergenic Products Testing Laboratory. 1993.
2Miller, CA; Boyle, KT; and Braun, M. ELISA Competition Assay - Quantitative Determination of Relative Potency of Allergenic Extracts. FDA CBER Methods of the Allergenic Products Testing Laboratory. 1993.
3Norman, P. S. The clinical significance of IgE. Hosp. Prac. 1975; 10:41-49.
4Nelson, H.S. Immunotherapy for inhalant allergens. In: Middleton et al. Allergy Principles and Practice 6th Ed. St. Louis: CV Mosby, 2003;1455.
5Data on file at FDA.
6Umetsu, D. T. et al. Serum sickness triggered by anaphylaxis: a complication of immunotherapy. J. Allergy Clin. Immunol. 1985; 76:713.
7Phannphak, P. and Kohler, P. F. Onset of polyarteritis nodosa during allergic hyposensitization treatment. Am. J. Med. 1980; 68:479.
8Frank, M.M. and Hester, C.G. Immune complexes and allergic disease. In: Middleton et al.: Allergy Principles and Practice 6th Ed. St. Louis: CV Mosby, 2003:997.
9Demoly, P., Piette, V., and Bousquet, J. In vivo methods for the study of allergy: skin test, techniques, and interpretation. In: Middleton et al.: Allergy Principles and Practice 6th Ed. St. Louis: CV Mosby, 2003:631.
10Committee on the Safety of Medicines. CSM update: desensitizing vaccines. Brit. Med. J. 1986; 293:948.
11Lockey, R. F. et al. Fatalities from immunotherapy (IT) and skin testing (ST). J. Allergy Clin. Immunol. 1987; 79:660.
12Reid, M. J. et al. Survey of fatalities from skin testing and immunotherapy. 1985-1989. J. Allergy Clin Immunol. 1993; 92:6.
13DuBuske L. M. et al. Special problems regarding Allergen Immunotherapy in Immunology and Allergy Clinics of North America, Greenburger, P.A. Ed. February 1992; 145-149.
14Freedman, SO; Asthma and Allergic Rhinitis II Clinical Aspects. In Freedman and Gold Clinical Immunology, 2nd Ed. Hagerstown, MD: Harper & Row, 1976: 131.
15Bernstein, D I, Wanner M. Borish L, Liss GM: Immunotherapy Committee, American Academy of Allergy, Asthma and Immunology. Twelve-year survey of fatal reactions to allergen injections and skin testing: 1990-2001. J. Allergy Clin Immunol. 204 Jun; 113(6); 1129-36.
Revision: November 2009
©ALK-Abello, Inc. 2009 187F
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
MIX OF 5 STANDARD GRASS POLLEN
agrostis gigantea pollen, anthoxanthum odoratum pollen, dactylis glomerata pollen, phleum pratense pollen and poa pratensis pollen injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 0268-8073 Route of Administration PERCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PHLEUM PRATENSE POLLEN (UNII: 65M88RW2EG) (PHLEUM PRATENSE POLLEN - UNII:65M88RW2EG) PHLEUM PRATENSE POLLEN 20000 [BAU] in 1 mL DACTYLIS GLOMERATA POLLEN (UNII: 83N78IDA7P) (DACTYLIS GLOMERATA POLLEN - UNII:83N78IDA7P) DACTYLIS GLOMERATA POLLEN 20000 [BAU] in 1 mL POA PRATENSIS POLLEN (UNII: SCB8J7LS3T) (POA PRATENSIS POLLEN - UNII:SCB8J7LS3T) POA PRATENSIS POLLEN 20000 [BAU] in 1 mL AGROSTIS GIGANTEA POLLEN (UNII: HU8V6E7HOA) (AGROSTIS GIGANTEA POLLEN - UNII:HU8V6E7HOA) AGROSTIS GIGANTEA POLLEN 20000 [BAU] in 1 mL ANTHOXANTHUM ODORATUM POLLEN (UNII: 2KIK19R45Y) (ANTHOXANTHUM ODORATUM POLLEN - UNII:2KIK19R45Y) ANTHOXANTHUM ODORATUM POLLEN 20000 [BAU] in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 0.005 g in 1 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.00275 g in 1 mL PHENOL (UNII: 339NCG44TV) 0.004 mL in 1 mL GLYCERIN (UNII: PDC6A3C0OX) 0.5 mL in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0268-8073-06 5.5 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103058 12/18/1997 MIX OF 6 STANDARD GRASS POLLEN
agrostis gigantea pollen, dactylis glomerata pollen, festuca pratensis pollen, lolium perenne pollen, phleum pratense pollen and poa pratensis pollen injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 0268-8074 Route of Administration PERCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PHLEUM PRATENSE POLLEN (UNII: 65M88RW2EG) (PHLEUM PRATENSE POLLEN - UNII:65M88RW2EG) PHLEUM PRATENSE POLLEN 16667 [BAU] in 1 mL DACTYLIS GLOMERATA POLLEN (UNII: 83N78IDA7P) (DACTYLIS GLOMERATA POLLEN - UNII:83N78IDA7P) DACTYLIS GLOMERATA POLLEN 16667 [BAU] in 1 mL POA PRATENSIS POLLEN (UNII: SCB8J7LS3T) (POA PRATENSIS POLLEN - UNII:SCB8J7LS3T) POA PRATENSIS POLLEN 16667 [BAU] in 1 mL AGROSTIS GIGANTEA POLLEN (UNII: HU8V6E7HOA) (AGROSTIS GIGANTEA POLLEN - UNII:HU8V6E7HOA) AGROSTIS GIGANTEA POLLEN 16667 [BAU] in 1 mL FESTUCA PRATENSIS POLLEN (UNII: A0WFQ8P6N1) (FESTUCA PRATENSIS POLLEN - UNII:A0WFQ8P6N1) FESTUCA PRATENSIS POLLEN 16667 [BAU] in 1 mL LOLIUM PERENNE POLLEN (UNII: 4T81LB52R0) (LOLIUM PERENNE POLLEN - UNII:4T81LB52R0) LOLIUM PERENNE POLLEN 16667 [BAU] in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 0.005 g in 1 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.00275 g in 1 mL PHENOL (UNII: 339NCG44TV) 0.004 mL in 1 mL GLYCERIN (UNII: PDC6A3C0OX) 0.5 mL in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0268-8074-06 5.5 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103058 12/18/1997 MIX OF 7 STANDARD GRASS POLLEN
agrostis gigantea pollen, anthoxanthum odoratum pollen, dactylis glomerata pollen, festuca pratensis pollen, lolium perenne pollen, phleum pratense pollen and poa pratensis pollen injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 0268-8076 Route of Administration PERCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PHLEUM PRATENSE POLLEN (UNII: 65M88RW2EG) (PHLEUM PRATENSE POLLEN - UNII:65M88RW2EG) PHLEUM PRATENSE POLLEN 14286 [BAU] in 1 mL DACTYLIS GLOMERATA POLLEN (UNII: 83N78IDA7P) (DACTYLIS GLOMERATA POLLEN - UNII:83N78IDA7P) DACTYLIS GLOMERATA POLLEN 14286 [BAU] in 1 mL POA PRATENSIS POLLEN (UNII: SCB8J7LS3T) (POA PRATENSIS POLLEN - UNII:SCB8J7LS3T) POA PRATENSIS POLLEN 14286 [BAU] in 1 mL AGROSTIS GIGANTEA POLLEN (UNII: HU8V6E7HOA) (AGROSTIS GIGANTEA POLLEN - UNII:HU8V6E7HOA) AGROSTIS GIGANTEA POLLEN 14286 [BAU] in 1 mL FESTUCA PRATENSIS POLLEN (UNII: A0WFQ8P6N1) (FESTUCA PRATENSIS POLLEN - UNII:A0WFQ8P6N1) FESTUCA PRATENSIS POLLEN 14286 [BAU] in 1 mL LOLIUM PERENNE POLLEN (UNII: 4T81LB52R0) (LOLIUM PERENNE POLLEN - UNII:4T81LB52R0) LOLIUM PERENNE POLLEN 14286 [BAU] in 1 mL ANTHOXANTHUM ODORATUM POLLEN (UNII: 2KIK19R45Y) (ANTHOXANTHUM ODORATUM POLLEN - UNII:2KIK19R45Y) ANTHOXANTHUM ODORATUM POLLEN 14286 [BAU] in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 0.005 g in 1 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.00275 g in 1 mL PHENOL (UNII: 339NCG44TV) 0.004 mL in 1 mL GLYCERIN (UNII: PDC6A3C0OX) 0.5 mL in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0268-8076-06 5.5 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103058 12/18/1997 GRASS MIX 4-S
agrostis gigantea pollen, anthoxanthum odoratum pollen, dactylis glomerata pollen, festuca pratensis pollen, lolium perenne pollen, phleum pratense pollen and poa pratensis pollen injection, solutionProduct Information Product Type STANDARDIZED ALLERGENIC Item Code (Source) NDC: 0268-8026 Route of Administration PERCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PHLEUM PRATENSE POLLEN (UNII: 65M88RW2EG) (PHLEUM PRATENSE POLLEN - UNII:65M88RW2EG) PHLEUM PRATENSE POLLEN 25000 [BAU] in 1 mL POA PRATENSIS POLLEN (UNII: SCB8J7LS3T) (POA PRATENSIS POLLEN - UNII:SCB8J7LS3T) POA PRATENSIS POLLEN 25000 [BAU] in 1 mL AGROSTIS GIGANTEA POLLEN (UNII: HU8V6E7HOA) (AGROSTIS GIGANTEA POLLEN - UNII:HU8V6E7HOA) AGROSTIS GIGANTEA POLLEN 25000 [BAU] in 1 mL DACTYLIS GLOMERATA POLLEN (UNII: 83N78IDA7P) (DACTYLIS GLOMERATA POLLEN - UNII:83N78IDA7P) DACTYLIS GLOMERATA POLLEN 25000 [BAU] in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 0.005 g in 1 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.00275 g in 1 mL PHENOL (UNII: 339NCG44TV) 0.004 mL in 1 mL GLYCERIN (UNII: PDC6A3C0OX) 0.5 mL in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0268-8026-06 5.5 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103058 12/18/1997 Labeler - ALK-Abello, Inc. (809998847)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.