LIBRELA- bedinvetmab injection injection, solution
Librela by
Drug Labeling and Warnings
Librela by is a Animal medication manufactured, distributed, or labeled by Zoetis Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
- CAUTION
-
DESCRIPTION
LIBRELA (bedinvetmab injection) is a sterile injectable solution containing 5, 10, 15, 20, or 30 mg/mL of bedinvetmab in 20 mM histidine buffer pH 5.0 [(0.027% w/v L- histidine and 0.382% w/v histidine HCl monohydrate), 8.5% w/v trehalose dihydrate, 0.005% w/v disodium EDTA dihydrate, 0.01% w/v L-methionine, and 0.1% w/v poloxamer 188]. Bedinvetmab is a canine IgG monoclonal antibody (mAb), in which the variable regions from canine B cell sequence were joined with canine IgG constant sequences, and is expressed through recombinant DNA techniques in Chinese hamster ovary (CHO) cells. Bedinvetmab binds to nerve growth factor (NGF) to reduce NGF’s effects. Such mAbs are commonly referred to as anti-NGF mAbs.
- INDICATION
-
DOSAGE AND ADMINISTRATION
Always provide the Client Information Sheet and discuss potential adverse drug events with the dog owner prior to administering each injection of LIBRELA (see Post-Approval Experience and Information for Dog Owners).
The minimum target dose of LIBRELA is 0.23 mg/lb (0.5 mg/kg) body weight, administered subcutaneously once a month. Dogs should be dosed by weight range according to the specific dosing information below.
The product does not contain a preservative. The full content of each vial is for single-use only. Once punctured, contents of the vial should be used immediately and any remaining solution should be discarded.
Dogs weighing ≥ 11 lb (≥ 5 kg):
Dogs should be dosed by weight range according to the Dosing Table below (Table 1). Dogs are given the full content of 1 or 2 vials of the appropriate concentration based on body weight. Aseptically withdraw the total dose into a single syringe and administer immediately.Table1. Dosing Table
Number and Strength (mg/mL) of LIBRELA Vials to be Administered Dog Body Weight in Pounds (lb) Dog Body Weight in Kilograms (kg) 5 mg/mL
orange10 mg/mL
blue15 mg/mL
green20 mg/mL
gold30 mg/mL
purple11-22.1 5-10 1 vial 22.2-44.1 10.1-20 1 vial 44.2-66.1 20.1-30 1 vial 66.2-88.2 30.1-40 1 vial 88.3-132.3 40.1-60 1 vial 132.4-176.4 60.1-80 2 vials 176.5-220.5 80.1-100 1 vial 1 vial 220.6-264.6 100.1-120 2 vials Dogs < 11 lb:
Aseptically withdraw 0.045 mL/lb (0.1 mL/kg) from a 5 mg/mL vial (orange vial) into a single syringe and administer immediately. Discard the vial after the dose has been withdrawn.
Effectiveness may not be achieved until after the second dose (see EFFECTIVENESS).
-
CONTRAINDICATIONS
LIBRELA should not be administered to dogs with known hypersensitivity to bedinvetmab.
LIBRELA should not be used in breeding dogs or in pregnant or lactating dogs. Immunoglobulin G class antibodies such as LIBRELA can pass through the placental blood barrier and be excreted in milk. Fetal abnormalities, increased rates of stillbirths and increased postpartum fetal mortality were noted in rodents and primates receiving anti-NGF monoclonal antibodies.
-
WARNINGS
User Safety Warnings
Not for use in humans. Keep this and all drugs out of reach of children.
For use in dogs only.
Hypersensitivity reactions, including anaphylaxis, could potentially occur in the case of accidental self-injection.
In case of accidental self-injection, seek medical advice immediately and show the package leaflet, vial or carton to the physician.
Pregnant women, women trying to conceive, and breastfeeding women should take extreme care to avoid accidental self-injection.
The importance of Nerve Growth Factor in ensuring normal fetal nervous system development is well-established and laboratory studies conducted on nonhuman primates with human anti-NGF antibodies have shown evidence of reproductive and developmental toxicity.
-
PRECAUTIONS
Administration of monoclonal antibodies may be associated with hypersensitivity reactions and delayed hypersensitivity reactions. If anaphylaxis or other hypersensitivity reaction occurs, discontinue use and institute appropriate therapy.
The safe use of this product with other monoclonal antibodies has not been evaluated. Use with caution in dogs with known hypersensitivity to other immunoglobulin therapy.
Evaluations were not made to determine if interactions occurred between LIBRELA and veterinary vaccines.
Treatment with LIBRELA may result in the formation of anti-bedinvetmab antibodies and potentially the loss of product effectiveness (see IMMUNOGENICITY).
The safe use of anti-NGF monoclonal antibodies with concurrent nonsteroidal anti-inflammatory drugs (NSAIDs) has not been established in dogs. In human clinical trials, rapidly progressing osteoarthritis (RPOA) has been reported in a small number of patients receiving humanized anti-NGF monoclonal antibody therapy. The incidence of these events increased in human patients receiving NSAID treatment long term in combination with an anti-NGF monoclonal antibody. RPOA has not been characterized or reported in dogs.
The safety and effectiveness of LIBRELA has not been evaluated in dogs less than 12 months of age.
LIBRELA has not been studied in dogs that have a history of cruciate ligament rupture within six months before initial product use as these cases were excluded from the field studies.
Long term effects which may occur more than 9 months after the use of LIBRELA have not been evaluated.
NGF is expressed within the heart and vasculature, and the long-term effects of reduced NGF in dogs with cardiac disease are unknown.
Primates receiving high doses of anti-NGF monoclonal antibodies had anatomical changes in postganglionic cell bodies (reduced size and number of neurons). The change in cell body size returned to normal after anti-NGF monoclonal antibody administration was discontinued. NGF is involved in the normal development of sensory and sympathetic nerve fibers in developing animals. This may be important with use of LIBRELA in young growing dogs.
-
ADVERSE REACTIONS
The safety of LIBRELA was assessed in a masked, controlled 84-day US field study evaluating the effectiveness of LIBRELA for the control of pain associated with osteoarthritis. Enrollment included 272 dogs, 135 dogs treated with LIBRELA and 137 dogs treated with a negative control (sterile saline). The enrolled dogs were at least 1 year of age (1 to 17 years old), weighed between 1.8 to 62.7 kg and were of various breeds or non-purebred. Dogs were dosed at 28-day intervals and received up to three injections. The most common adverse reactions reported during the study are summarized in Table 2 below.
Table 2. Number (%) of Dogs with Adverse Reactions Reported in the US Field Study
Adverse Reaction* LIBRELA
n (%)
(Total N = 135)Negative Control
n (%)
(Total N = 137)Urinary tract infection 15 (11.1) 11 (8.0) Bacterial skin infection 11 (8.1) 9 (6.6) Dermatitis 10 (7.4) 8 (5.8) Dermal mass 8 (5.9) 5 (3.6) Erythema 6 (4.4) 5 (3.6) Dermal cyst(s) 4 (3.0) 2 (1.5) Pain on injection 4 (3.0) 2 (1.5) Inappropriate urination** 4 (3.0) 1 (0.7) Histiocytoma 3 (2.2) 0 (0.0) *An adverse reaction may have occurred more than once in a dog; only the first occurrence was counted.
** Of these, two dogs treated with LIBRELA were among those reported with a urinary tract infection.
The safety of LIBRELA was also evaluated in a masked, controlled 84-day European field study evaluating the effectiveness of LIBRELA for the control of pain associated with osteoarthritis. Enrollment included 281 dogs, 138 dogs were treated with LIBRELA and 143 treated with a negative control (sterile saline). The enrolled dogs were at least 1 year of age (1 to 17.5 years old), weighed between 1.7 to 66 kg and were of various breeds or non-purebred. Dogs were dosed at 28-day intervals and received up to three injections. The most common adverse reactions reported during the study are summarized in Table 3 below.
Table 3. Number (%) of dogs with Adverse Reactions Reported in the European Field Study
Adverse Event Reported* LIBRELA
n (%)
(Total N = 138)Negative Control
n (%)
(Total N = 143)Increased Blood Urea Nitrogen 19 (13.8) 7 (4.9)
(BUN)**19 (13.8) 7 (4.9) Lethargy 5 (3.6) 0 (0.0) Emesis 4 (2.9) 1 (0.7) Anorexia 3 (2.2) 0 (0.0) Lameness 3 (2.2) 1 (0.7) Cough 3 (2.2) 1 (0.7) *An adverse reaction may have occurred more than once in a dog; only the first occurrence was counted.
** Two dogs treated with LIBRELA suffered serious adverse events and were euthanized during or after study completion: A 13-year old Bichon Frise had pre-existing increased urine protein-creatinine ratio and heart failure that worsened during study; the dog also had an increase in creatinine during the study and was diagnosed with renal failure and was euthanized 3 days after completing the study. An 8-year-old mixed breed dog had pancreatitis and was euthanized on Day 74. The remainder of the dogs that had elevations in the BUN did not have any obvious adverse events associated with this finding.
One dog in the LIBRELA group was diagnosed with pyelonephritis on Day 15; this dog had pre-existing increased serum BUN and creatinine and a recent history of urinary tract infection that was not confirmed resolved prior to enrollment. Non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen were initiated on Day 7 for osteoarthritis-associated joint pain but NSAIDs were discontinued on Day 10 due to anorexia and gastroenteritis; azotemia worsened at Day 13 and the dog received no further LIBRELA treatment.
One dog in the LIBRELA group with a history of atopy, developed mild alopecia and mild erythema on the injection site on Days 5 and 23. Both episodes of alopecia and erythema resolved with treatment.
A total of 89 dogs were enrolled in a 6-month, single arm, open labeled, uncontrolled continuation of the EU field study and received monthly subcutaneous injections of LIBRELA. The study provided additional field safety information.
One dog experienced acute gastroenteritis and recovered following treatment for abdominal pain, fever, vomiting, and anorexia. One large breed dog enrolled for stifle osteoarthritis developed acute forelimb lameness that was diagnosed as elbow dysplasia. Two dogs presented with rear limb paresis of unknown etiology, one of whom responded to ongoing NSAID treatment and one who did not.
-
Post-Approval Experience (2025)
The following adverse events are based on post-approval adverse drug experience reporting for LIBRELA. Not all adverse events are reported to FDA/CVM. It is not always possible to reliably estimate the adverse event frequency or establish a causal relationship to product exposure using these data.
The following adverse events in dogs are categorized in order of decreasing reporting frequency by body system and in decreasing order of reporting frequency within each body system:
Neurological: ataxia, seizures, paresis, proprioception deficits, paralysis
General: anorexia, lethargy, recumbency
Urinary: polydipsia, polyuria/pollakiuria, urinary incontinence
Gastrointestinal: vomiting, diarrhea
Musculoskeletal: muscle weakness, muscle tremors, lameness
In some cases, death (including euthanasia) has been reported as an outcome of the adverse events listed above. -
CONTACT INFORMATION
To report suspected adverse drug events, for technical assistance or to obtain a copy of the Safety Data Sheet (SDS), contact Zoetis Inc. at 1-888‑963-8471.
For additional information about reporting adverse drug experience for animal drugs, contact FDA at 1-888-FDA-VETS or www.fda.gov/reportanimalae. -
INFORMATION FOR DOG OWNERS
Always provide and review the Client Information Sheet with the dog owner prior to each injection of LIBRELA. Advise owners of the adverse reactions that may occur following the administration of LIBRELA including balance problems, trouble walking, weakness, trouble standing, seizures, drinking more, urinating more, loss of bladder control, vomiting, and diarrhea. Owners should be advised to contact their veterinarian if any of these signs or other signs of illness are observed. Advise dog owners that serious adverse reactions can occur and result in death or euthanasia (see Adverse Reactions and Post-Approval Experience).
Where a dog has not been able to exercise prior to treatment with LIBRELA, there is an increased risk of injury if the dog becomes more active after being treated with LIBRELA. Discuss an exercise plan with the dog owner to return the dog to activity. -
CLINICAL PHARMACOLOGY
Mechanism of Action
Bedinvetmab is a recombinant canine monoclonal antibody that binds to nerve growth factor (NGF), reduces NGF binding to the tropomyosin receptor kinase A (TrkA) and p75 neurotrophin receptor (p75NTR) receptors and decreases TrkA signal transduction in cell types involved in pain. In vitro binding studies suggest that bedinvetmab binds with high affinity to NGF but does not bind to other neurotrophins including human neurotrophin-3 (NT-3), canine and human NT-4, and human brain-derived neurotrophic factor (BDNF).
NGF has been found to be elevated in the osteoarthritic joints of dogs. Following a noxious stimulus, inflammatory cytokines and NGF are released by tissues of the joint.
NGF binds to TrkA/p75NTR receptors found on peripheral nerves, immune cells, endothelial cells, synoviocytes, and chondrocytes to induce peripheral sensitization, neurogenic inflammation, and increased pain perception. Bedinvetmab binds to NGF and prevents NGF/TrkA/p75NTR cellular signaling. In in vitro studies, bedinvetmab potently inhibits NGF-mediated signaling as measured by a reduction in TF-1 cell proliferation and functionally blocks NGF-induced neurite outgrowth in rat PC-12 neuronal cells.
NGF binds to TrkA receptors located on immune cells to elicit the release of additional proinflammatory mediators, including NGF itself. These inflammatory mediators lead to further peripheral sensitization involved in pain perception. Bedinvetmab reduces the expression of these inflammatory mediators in rat PC-12 neuronal cells.
Pharmacokinetics
In a 6-month laboratory study of healthy, adult Beagles administered LIBRELA at monthly doses ranging from 1-10 mg/kg, the area under the curve (AUC) and the maximum concentration (Cmax) increased nearly in proportion to dose and steady-state was achieved after approximately 2 doses. In a laboratory pharmacokinetic study in Beagles at 0.5-1.0 mg/kg, peak serum drug levels were observed at 4-7 days after subcutaneous dosing, the mean bioavailability relative to an intravenous dose was approximately 86%, and the elimination half-life was approximately 12 days.
In a field study at the labeled dose in dogs with osteoarthritis, the half-life was highly variable and averaged approximately 19 days (harmonic mean 15.8 days). Steady-state was achieved after 2 doses.
The metabolic pathway of bedinvetmab has not been characterized. As a canine IgG monoclonal antibody, bedinvetmab is expected to be degraded into small peptides and amino acids via catabolic pathways in a manner similar to endogenous IgG.
-
IMMUNOGENICITY
Antibodies binding to bedinvetmab (i.e., an anti-drug antibody, ADA), were detected using a multi-tiered ADA testing approach (screening, confirmatory, and titration). Testing the confirmed ADA samples for neutralizing activity of bedinvetmab was not performed. Due to limitations of the assay methods performed to evaluate immunogenicity (confirmatory and titration), clinically relevant conclusions or correlations were not determined from the immunogenicity data reported.
In the US Field Effectiveness Study, 267 of 272 enrolled dogs with osteoarthritis were evaluated for immunogenicity after receiving up to 3 doses of LIBRELA. The presence of pre-existing ADAs was confirmed in 5 out of 267 dogs; 4 dogs in the LIBRELA group and 1 dog in the control group. Three of these LIBRELA-treated dogs continued to have ADAs confirmed after treatment with LIBRELA. Of the remaining dogs evaluated for immunogenicity, the presence of ADAs was confirmed on Day 84 in 1 dog in the LIBRELA-treated group and 1 dog in the control group.
In the EU Field Effectiveness Study, 281 of 287 enrolled dogs with osteoarthritis were evaluated for immunogenicity after receiving up to 3 doses of LIBRELA. The presence of pre-existing ADAs was confirmed in 2 out of 281 dogs; both in the control group. Of the other 141 dogs in the control group, the presence of ADA was confirmed in 1 dog after receiving treatment with placebo (on Study Visit Day 56). Of the 138 LIBRELA-treated dogs, the presence of ADA was confirmed in 2 dogs after treatment with LIBRELA (1 dog on Study Visit Day 84 and 1 dog on Study Visit Study Day 28). Eighty-nine LIBRELA-treated dogs continued on with once monthly treatment for an additional six months, and 82 of these dogs were evaluated for immunogenicity after receiving up to 6 additional doses of LIBRELA. The presence of ADA was confirmed in an additional 2 dogs.
In the 6-Month Safety Study, the presence of ADAs was confirmed in 2 out of 8 negative control dogs and no ADAs were confirmed in any of the 24 dogs administered 7 doses of LIBRELA.
The observed incidence of antibody positivity in an assay is highly dependent on several factors including assay sensitivity and specificity, assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to LIBRELA with the incidence of antibodies to other products may not be appropriate.
-
EFFECTIVENESS
The overall evidence, based on the results of two field studies, supports the conclusion that LIBRELA is effective for the control of pain associated with osteoarthritis in dogs when given as a minimum of two doses administered one month apart.
A US field effectiveness study and a European (EU) field effectiveness study were conducted using a similar study design. Both studies included a group administered LIBRELA and a negative control group that was administered sterile saline. The primary effectiveness endpoint was treatment success (Yes/No) at Day 28 based on owner assessment of pain measured on the Canine Brief Pain Inventory (CBPI).1-2 CBPI treatment success was a secondary endpoint at Days 7, 14, 42, 56 and 84. Treatment success was defined as a reduction of ≥ 2 in Pain Interference Score (PIS) and ≥ 1 in Pain Severity Score (PSS) vs. Day 0. Dogs receiving rescue treatment (e.g., for lack of efficacy (LOE)) or withdrawn for LOE were counted as treatment failures starting on the day of rescue or withdrawal, respectively.
While the studies had similar success rates on Day 28 in the treatment groups administered LIBRELA (48% and 45.2%), the studies had differences in the success rates in the control groups. The success rate in the control group in the US study was 36.1% and the success rate of the control group in the EU study was 17.0%. Based on these results, there was a larger treatment effect size in the EU study as compared to the US study, such that the US study did not demonstrate a significant difference at Day 28. In the EU study, the primary effectiveness variable was successful and met statistical significance at Day 28 (P = 0.0018).
The CBPI data from both studies demonstrated a greater percentage of dogs achieving treatment success in the LIBRELA-treated vs. control groups at Day 42. This success rate was maintained with a third administration at Day 56 through the end of the study at Day 84. Taken together, the US and EU studies establish the effectiveness for LIBRELA (bedinvetmab injection) for the control of pain associated with osteoarthritis in dogs when given as a minimum of two doses administered one month apart.
US Field Effectiveness Study
An 84-day masked, randomized, controlled field study was conducted at 24 US veterinary clinics. The study enrolled 272 client-owned dogs with clinical signs of osteoarthritis confirmed by radiography and orthopedic examination. Enrolled dogs were randomized at an equal ratio into one of two treatment groups: LIBRELA (0.5 mg/kg, n = 135) or control (sterile saline, n = 137) and were treated on Days 0, 28, and 56. Dog age and body weight ranged from 1.0 to 17.0 years and 1.8 to 62.7 kg, respectively. The percentage of dogs considered treatment successes based on the owner CBPI assessment was greater in the LIBRELA-treated dogs compared to the control group for all assessments. The study failed to demonstrate statistical significance for effectiveness at Day 28; however, the difference in the percentage of treatment successes from Day 42 onward demonstrated a clinical effect in the LIBRELA group compared to the control group.
Table 4. Study #1: Least Squares Mean Percent Success by Assessment Day
Day Group N % Success 7 LIBRELA 125 30.3 Control 129 24.8 14 LIBRELA 129 41.4 Control 130 30.5 28 LIBRELA 128 48.0 Control 131 36.1 42 LIBRELA 121 54.8 Control 126 38.9 56 LIBRELA 122 57.8 Control 124 42.1 84 LIBRELA 118 57.1 Control 118 33.4
EU Field Effectiveness Study
An 84-day masked, randomized, controlled field study was conducted at 26 different study sites located in Portugal, Hungary, Ireland and Germany. The study enrolled 287 client-owned dogs with clinical signs of osteoarthritis confirmed by radiography and orthopedic examination. Dogs were randomized at an equal ratio into one of two treatment groups: LIBRELA (0.5 mg/kg, n = 141) or control (sterile saline, n = 146) and were treated on Days 0, 28, and 56. Dog age and body weight ranged from 1.0 to 17.5 years and 1.7 to 66.0 kg, respectively. The percentage of dogs considered treatment successes based on the owner CBPI assessment was greater for LIBRELA-treated dogs compared to the control group for all assessments. The study met statistical significance compared to the control at Day 28 (primary effectiveness endpoint; P = 0.0018). The difference in the percentage of treatment successes from Day 42 onward continued to demonstrate a clinical effect in the LIBRELA group compared to the control group.
Table 5. Study #2: Least Squares Mean Percent Success by Assessment Day
Day Group N % Success 7 LIBRELA 128 18.5 Control 130 4.0 14 LIBRELA 132 35.7 Control 132 9.6 28 LIBRELA 131 45.2 Control 131 17.0 42 LIBRELA 133 53.5 Control 134 21.4 56 LIBRELA 133 52.9 Control 134 20.6 84 LIBRELA 129 49.9 Control 132 24.3 -
TARGET ANIMAL SAFETY
6 Month Margin of Safety Study:
LIBRELA (bedinvetmab injection) 15 mg/mL and 30 mg/mL concentrations were administered subcutaneously to 11 to 12-month old, healthy Beagles (8 dogs per group) at doses of 1 mg/kg (1X), 3 mg/kg (3X), and 10 mg/kg (10X) every 28 days for seven consecutive doses. The control group (8 dogs) received sterile saline injections. Dogs weighed 5.6-11.7 kg at study initiation.
There were no clinically significant changes noted in neurological examinations, body temperature, heart and respiratory rate, blood pressure, electrocardiography, and organ weights. Detailed pathology evaluation of the shoulder, elbow, hip, and knee joints were conducted.
Vomiting and soft stool were noted across all groups throughout the study. Scabbing on the face, neck and thorax was seen across all groups except the 1 mg/kg group. Injection site redness was noted sporadically for 1 control dog, 2 dogs in the 1 mg/kg treatment group, 5 dogs in the 3 mg/kg treatment group, and 5 dogs in the 10 mg/kg treatment group. One dog in the 3 mg/kg treatment group had a temporary, mild swollen facial area 26 days after the first dose that resolved spontaneously. Two dogs in the 3 mg/kg treatment group had lymphadenopathy on the last study day with no related histopathology findings. One dog in the 10 mg/kg treatment group had an approximately 2.5 cm X 3.5 cm circular raised firm erythematous lesion with slight serosanguinous discharge and mild scabs of the shaved cervical area that resolved over 14 days.
One dog in the 1 mg/kg treatment group had an increasing ALP value over the course of the study that increased threefold above the high end of the reference range at study completion. There was no gross or histopathology correlate.
One dog in the 1 mg/kg treatment group had mild cartilage necrosis in the left ulna and an erosion in the cartilage of the right ulna. One dog in the 3 mg/kg treatment group had mild bilateral, femoral neck enthesophytes observed on radiographs pre-treatment. On end of study radiography and pathology evaluation, this dog had an osteophyte of the left acetabulum, mild left acetabulum remodeling and severe left femoral neck enthesophytes. Microscopically, mild to moderate cartilage degeneration with erosion and proteoglycan depletion was also noted in the left proximal femur and acetabulum. The mild right femoral neck enthesophytes were the same grade as pre-treatment. The findings may be progression of an underlying musculoskeletal condition; however, a potential relation to treatment cannot be ruled out.
None of the LIBRELA-treated dogs developed anti-drug antibodies due to bedinvetmab administration.
Additional Safety Studies:
In a two-week laboratory safety study, eight dogs concurrently received one subcutaneous injection of LIBRELA at the high end of the inherent dose band (1 mg/kg) and fourteen days of an injectable NSAID. This limited laboratory study did not provide sufficient data to support a conclusion on the safety of concurrent use of LIBRELA and NSAIDs.
In a 3-month exploratory laboratory safety study using a non-final formulation of bedinvetmab administered by subcutaneous injection monthly for four doses, a dog administered a 4 mg/kg dose had a reddened and/or swollen muzzle abrasion, with an elevated white blood cell count, and elevated globulin level and fibrinogen level. At one of the injection administrations, one dog administered a 4 mg/kg dose had a 4 cm X 2 cm injection site erythema with an eschar that resolved; and one dog administered a 1 mg/kg dose had 3 cm X 1 cm injection site erythema that resolved. Another dog administered a 1 mg/kg dose had injection site erythema, scabbing, and mucopurulent discharge for 18 days.
- STORAGE CONDITIONS
- HOW SUPPLIED
-
REFERENCES
1. Brown DC, Bell M, Rhodes L. Power of treatment success definitions when the Canine Brief Pain Inventory is used to evaluate carprofen treatment for the control of pain and inflammation in dogs with osteoarthritis. Amer J Vet Rsch 2013; 74(12):1467-1473.
2. Brown DC, Bell M, Rhodes L. ERRATUM to: Power of treatment success definitions when the Canine Brief Pain Inventory is used to evaluate carprofen treatment for the control of pain and inflammation in dogs with osteoarthritis. Amer J Vet Rsch 2014; 75(4):353.
- SPL UNCLASSIFIED SECTION
- Client Information Sheet
- PRINCIPAL DISPLAY PANEL - 5mg carton
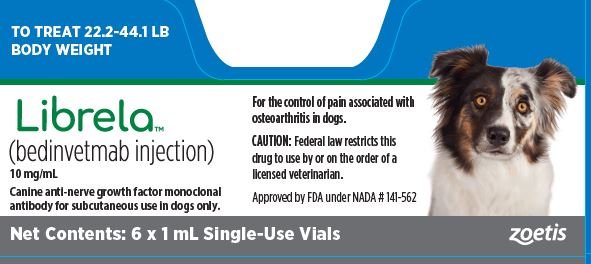
- PRINCIPAL DISPLAY PANEL - 10mg carton
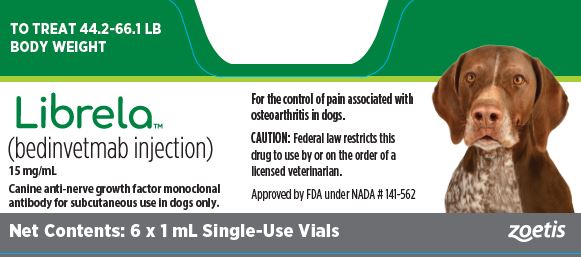
- PRINCIPAL DISPLAY PANEL - 15mg carton
- PRINCIPAL DISPLAY PANEL - 20mg carton
- PRINCIPAL DISPLAY PANEL - 30mg carton
-
INGREDIENTS AND APPEARANCE
LIBRELA
bedinvetmab injection injection, solutionProduct Information Product Type PRESCRIPTION ANIMAL DRUG Item Code (Source) NDC: 54771-2772 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BEDINVETMAB (UNII: 1AY63T2BE2) (BEDINVETMAB - UNII:1AY63T2BE2) BEDINVETMAB 5 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54771-2772-1 2 in 1 CARTON 2 NDC: 54771-2772-2 6 in 1 CARTON Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NADA NADA141562 07/14/2023 LIBRELA
bedinvetmab injection injection, solutionProduct Information Product Type PRESCRIPTION ANIMAL DRUG Item Code (Source) NDC: 54771-2778 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BEDINVETMAB (UNII: 1AY63T2BE2) (BEDINVETMAB - UNII:1AY63T2BE2) BEDINVETMAB 10 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54771-2778-1 2 in 1 CARTON 2 NDC: 54771-2778-2 6 in 1 CARTON Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NADA NADA141562 07/14/2023 LIBRELA
bedinvetmab injection injection, solutionProduct Information Product Type PRESCRIPTION ANIMAL DRUG Item Code (Source) NDC: 54771-2779 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BEDINVETMAB (UNII: 1AY63T2BE2) (BEDINVETMAB - UNII:1AY63T2BE2) BEDINVETMAB 15 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54771-2779-1 2 in 1 CARTON 2 NDC: 54771-2779-2 6 in 1 CARTON Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NADA NADA141562 07/14/2023 LIBRELA
bedinvetmab injection injection, solutionProduct Information Product Type PRESCRIPTION ANIMAL DRUG Item Code (Source) NDC: 54771-2780 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BEDINVETMAB (UNII: 1AY63T2BE2) (BEDINVETMAB - UNII:1AY63T2BE2) BEDINVETMAB 20 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54771-2780-1 2 in 1 CARTON 2 NDC: 54771-2780-2 6 in 1 CARTON Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NADA NADA141562 07/14/2023 LIBRELA
bedinvetmab injection injection, solutionProduct Information Product Type PRESCRIPTION ANIMAL DRUG Item Code (Source) NDC: 54771-2781 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BEDINVETMAB (UNII: 1AY63T2BE2) (BEDINVETMAB - UNII:1AY63T2BE2) BEDINVETMAB 30 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54771-2781-1 2 in 1 CARTON 2 NDC: 54771-2781-2 6 in 1 CARTON Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NADA NADA141562 07/14/2023 Labeler - Zoetis Inc. (828851555)
Trademark Results [Librela]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 LIBRELA 97768335 not registered Live/Pending |
Zoetis Services LLC 2023-01-25 |
 LIBRELA 90107142 not registered Live/Pending |
Zoetis Services LLC 2020-08-11 |
 LIBRELA 88569924 not registered Live/Pending |
Zoetis Services LLC 2019-08-07 |
 LIBRELA 87703473 not registered Live/Pending |
Zoetis Services LLC 2017-11-30 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.