LIRAGLUTIDE injection, solution
Liraglutide by
Drug Labeling and Warnings
Liraglutide by is a Prescription medication manufactured, distributed, or labeled by Teva Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LIRAGLUTIDE INJECTION safely and effectively. See full prescribing information for LIRAGLUTIDE INJECTION.
LIRAGLUTIDE injection, for subcutaneous use
Initial U.S. Approval: 2010WARNING: RISK OF THYROID C-CELL TUMORS
See full prescribing information for complete boxed warning.
- Liraglutide causes thyroid C-cell tumors at clinically relevant exposures in both genders of rats and mice. It is unknown whether liraglutide causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans, as the human relevance of liraglutide-induced rodent thyroid C-cell tumors has not been determined (5.1).
- Liraglutide is contraindicated in patients with a personal or family history of MTC or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Counsel patients regarding the potential risk of MTC and the symptoms of thyroid tumors (4, 5.1, 13.1).
RECENT MAJOR CHANGES
Indications and Usage………………………….……………............………….5/2025
Dosage and Administration, Patient Selection (2.1).....................…(Removed) 5/2025
Contraindications,
Pregnancy (4)………………………………….……............……(Removed) 5/2025
Warnings and Precautions,
Severe Gastrointestinal Adverse Reactions (5.7)………..…............………..10/2025
Pulmonary Aspiration During General
Anesthesia or Deep Sedation (5.10)……………...……………............….....11/2024
INDICATIONS AND USAGE
Liraglutide injection is a glucagon like peptide-1 (GLP-1) receptor agonist indicated in combination with a reduced-calorie diet and increased physical activity to reduce excess body weight and maintain weight reduction long term in:
- Adults and pediatric patients aged 12 years and older with body weight greater than 60 kg and obesity. (1)
- Adults with overweight in the presence of at least one weight-related comorbid condition. (1)
Limitations of Use:
DOSAGE AND ADMINISTRATION
- Inject liraglutide injection subcutaneously in the abdomen, thigh, or upper arm once daily at any time of day, without regard to the timing of meals. (2.1)
- The recommended dose of liraglutide injection is 3 mg daily. (2.2)
- Initiate at 0.6 mg per day for one week. In weekly intervals, increase the dose until a dose of 3 mg is reached. (2.2)
- If pediatric patients do not tolerate an increased dose during dose escalation, the dose may also be lowered to the previous level. Dose escalation for pediatric patients may take up to 8 weeks. (2.2)
- Pediatric patients who do not tolerate 3 mg daily may have their dose reduced to 2.4 mg daily. (2.2)
- Adult patients with type 2 diabetes should monitor blood glucose prior to starting liraglutide injection and during liraglutide injection treatment. (2.2)
DOSAGE FORMS AND STRENGTHS
Injection: 6 mg/mL solution in a 3 mL prefilled, single-patient-use pen that delivers doses of 0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg or 3 mg. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Acute Pancreatitis: Has been observed in patients treated with GLP-1 receptor agonists, including liraglutide. Discontinue if pancreatitis is suspected. (5.2)
- Acute Gallbladder Disease: If cholelithiasis or cholecystitis are suspected, gallbladder studies are indicated. (5.3)
- Hypoglycemia: Can occur in adults when liraglutide is used with an insulin secretagogue (e.g. a sulfonylurea) or insulin. The risk may be lowered by a reduction in the dose of concomitantly administered insulin secretagogues or insulin. In the pediatric clinical trial, patients did not have type 2 diabetes. Hypoglycemia occurred in liraglutide-treated pediatric patients. Inform all patients of the risk of hypoglycemia and educate them on the signs and symptoms of hypoglycemia. (5.4)
- Heart Rate Increase: Monitor heart rate at regular intervals. (5.5)
- Acute Kidney Injury Due to Volume Depletion: Monitor renal function in patients reporting adverse reactions that could lead to volume depletion. (5.6)
- Severe Gastrointestinal Adverse Reactions: Use has been associated with gastrointestinal adverse reactions, sometimes severe. Liraglutide is not recommended in patients with severe gastroparesis. (5.7)
- Hypersensitivity Reactions: Postmarketing reports of serious hypersensitivity reactions (e.g., anaphylactic reactions and angioedema). Discontinue liraglutide and other suspect medications and promptly seek medical advice. (5.8)
- Suicidal Behavior and Ideation: Monitor for depression or suicidal thoughts. Discontinue liraglutide if symptoms develop. (5.9)
- Pulmonary Aspiration During General Anesthesia or Deep Sedation: Has been reported in patients receiving GLP-1 receptor agonists undergoing elective surgeries or procedures. Instruct patients to inform healthcare providers of any planned surgeries or procedures. (5.10)
ADVERSE REACTIONS
Most common adverse reactions, reported in greater than or equal to 5% are: nausea, diarrhea, constipation, vomiting, injection site reactions, headache, hypoglycemia, dyspepsia, fatigue, dizziness, abdominal pain, increased lipase, upper abdominal pain, pyrexia, and gastroenteritis. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Teva at 1-888-838-2872 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Liraglutide delays gastric emptying. May impact absorption of concomitantly administered oral medications. Use with caution. (7)
USE IN SPECIFIC POPULATIONS
Pregnancy: May cause fetal harm. When pregnancy is recognized, discontinue liraglutide. (8.1)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 1/2026
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF THYROID C-CELL TUMORS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 Dosage in Adults and Pediatric Patients Aged 12 Years and Older
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Thyroid C-cell Tumors
5.2 Acute Pancreatitis
5.3 Acute Gallbladder Disease
5.4 Hypoglycemia
5.5 Heart Rate Increase
5.6 Acute Kidney Injury Due to Volume Depletion
5.7 Severe Gastrointestinal Adverse Reactions
5.8 Hypersensitivity Reactions
5.9 Suicidal Behavior and Ideation
5.10 Pulmonary Aspiration During General Anesthesia or Deep Sedation
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Oral Medications
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Weight Management Trials in Adults with Overweight or Obesity
14.2 Weight Management Trial in Pediatric Patients Ages 12 and Older with Obesity
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF THYROID C-CELL TUMORS
- Liraglutide causes dose-dependent and treatment-duration-dependent thyroid C-cell tumors at clinically relevant exposures in both genders of rats and mice. It is unknown whether liraglutide causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans, as the human relevance of liraglutide-induced rodent thyroid C-cell tumors has not been determined [see Warnings and Precautions (5.1) and Nonclinical Toxicology (13.1)].
- Liraglutide is contraindicated in patients with a personal or family history of MTC and in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Counsel patients regarding the potential risk of MTC with use of liraglutide and inform them of symptoms of thyroid tumors (e.g., a mass in the neck, dysphagia, dyspnea, persistent hoarseness). Routine monitoring of serum calcitonin or using thyroid ultrasound is of uncertain value for early detection of MTC in patients treated with liraglutide [see Contraindications (4), Warnings and Precautions (5.1)].
-
1 INDICATIONS AND USAGE
Liraglutide injection is indicated in combination with a reduced-calorie diet and increased physical activity to reduce excess body weight and maintain weight reduction long term in:
- Adults and pediatric patients aged 12 years and older with body weight greater than 60 kg and obesity.
- Adults with overweight in the presence of at least one weight-related comorbid condition.
Limitations of Use
- Liraglutide injection contains liraglutide. Coadministration with other liraglutide-containing products or with any other glucagon-like peptide-1 (GLP-1) receptor agonist is not recommended.
- The safety and effectiveness of liraglutide injection in pediatric patients with type 2 diabetes have not been established.
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
- Prior to initiation of liraglutide injection, train patients on proper injection technique. Refer to the accompanying Instructions for Use for complete administration instructions with illustrations.
- Inspect liraglutide injection visually prior to each injection. Only use if solution is clear, colorless, and contains no particles.
- Administer liraglutide injection in combination with a reduced-calorie diet and increased physical activity.
- Inject liraglutide injection subcutaneously once daily at any time of day, without regard to the timing of meals.
- Inject liraglutide injection subcutaneously in the abdomen, thigh, or upper arm. No dosage adjustment is needed if changing the injection site and/or timing.
- Rotate injection sites within the same region in order to reduce the risk of cutaneous amyloidosis [see Adverse Reactions (6.2)].
- If a dose is missed, resume the once-daily regimen as prescribed with the next scheduled dose. Do not administer an extra dose or increase the dose to make up for the missed dose.
- If more than 3 days have elapsed since the last liraglutide injection dosage, reinitiate liraglutide injection at 0.6 mg daily and follow the dosage escalation schedule in Table 1, to reduce the risk of gastrointestinal adverse reactions associated with reinitiation of treatment.
2.2 Dosage in Adults and Pediatric Patients Aged 12 Years and Older
- Initiate liraglutide injection with a dose of 0.6 mg daily for one week. Then follow the dosage escalation schedule in Table 1 to reduce the risk of gastrointestinal adverse reactions [see Warnings and Precautions (5.7) and Adverse Reactions (6.1)].
Table 1. Dosage Escalation Schedule Week
Daily Dose
1
0.6 mg
2
1.2 mg
3
1.8 mg
4
2.4 mg
5 and onward
3 mg
Adult Patients
- For adults, the recommended dosage of liraglutide injection is 3 mg daily, lower dosages are for titration only.
- Discontinue liraglutide injection if the patient cannot tolerate the 3 mg dosage.
- If patients do not tolerate an increased dose during dosage escalation, consider delaying dosage escalation for approximately one additional week.
- Evaluate the change in body weight 16 weeks after initiating liraglutide injection and discontinue liraglutide injection if the patient has not lost at least 4% of baseline body weight, since it is unlikely that the patient will achieve and sustain clinically meaningful weight loss with continued treatment.
- In adult patients with type 2 diabetes, monitor blood glucose prior to starting liraglutide injection and during liraglutide injection treatment.
Pediatric Patients
- For pediatric patients, the recommended maintenance dosage of liraglutide injection is 3 mg daily. Pediatric patients who do not tolerate 3 mg daily may have their maintenance dose reduced to 2.4 mg daily. Discontinue liraglutide injection if the patient cannot tolerate the 2.4 mg dose.
- If pediatric patients do not tolerate an increased dose during dosage escalation, the dose may also be lowered to the previous level. Dosage escalation for pediatric patients may take up to 8 weeks.
- Evaluate the change in BMI after 12 weeks on the maintenance dose and discontinue liraglutide injection if the patient has not had a reduction in BMI of at least 1% from baseline, since it is unlikely that the patient will achieve and sustain clinically meaningful weight loss with continued treatment.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Liraglutide injection is contraindicated in:
- Patients with a personal or family history of medullary thyroid carcinoma (MTC) or patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2) [see Warnings and Precautions (5.1)].
- Patients with a serious hypersensitivity reaction to liraglutide or to any of the excipients in liraglutide injection. Serious hypersensitivity reactions including anaphylactic reactions and angioedema have been reported with liraglutide [see Warnings and Precautions (5.7)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Thyroid C-cell Tumors
Liraglutide causes dose-dependent and treatment-duration-dependent thyroid C-cell tumors (adenomas and/or carcinomas) at clinically relevant exposures in both genders of rats and mice [see Nonclinical Toxicology (13.1)]. Malignant thyroid C-cell carcinomas were detected in rats and mice. It is unknown whether liraglutide will cause thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans, as the human relevance of liraglutide-induced rodent thyroid C-cell tumors has not been determined.
Cases of MTC in patients treated with liraglutide have been reported in the postmarketing period; the data in these reports are insufficient to establish or exclude a causal relationship between MTC and liraglutide use in humans.
Liraglutide is contraindicated in patients with a personal or family history of MTC or in patients with MEN 2. Counsel patients regarding the potential risk for MTC with the use of liraglutide and inform them of symptoms of thyroid tumors (e.g., a mass in the neck, dysphagia, dyspnea, persistent hoarseness).
Routine monitoring of serum calcitonin or using thyroid ultrasound is of uncertain value for early detection of MTC in patients treated with liraglutide. Such monitoring may increase the risk of unnecessary procedures, due to low test specificity for serum calcitonin and a high background incidence of thyroid disease. Significantly elevated serum calcitonin may indicate MTC, and patients with MTC usually have calcitonin values greater than 50 ng/L. If serum calcitonin is measured and found to be elevated, the patient should be further evaluated. Patients with thyroid nodules noted on physical examination or neck imaging should also be further evaluated.
5.2 Acute Pancreatitis
Acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis, has been observed in patients treated with GLP-1 receptor agonists, including liraglutide [see Adverse Reactions (6)].
After initiation of liraglutide, observe patients carefully for signs and symptoms of acute pancreatitis which may include persistent or severe abdominal pain (sometimes radiating to the back) and which may or may not be accompanied by nausea or vomiting. If pancreatitis is suspected, discontinue liraglutide injection and initiate appropriate management.
5.3 Acute Gallbladder Disease
In liraglutide clinical trials in adults, 2.2% of liraglutide-treated patients reported adverse events of cholelithiasis versus 0.8% of placebo-treated patients. The incidence of cholecystitis was 0.8% in liraglutide-treated patients versus 0.4% in placebo-treated patients. The majority of liraglutide-treated patients with adverse events of cholelithiasis and cholecystitis required cholecystectomy. Substantial or rapid weight loss can increase the risk of cholelithiasis; however, the incidence of acute gallbladder disease was greater in liraglutide-treated patients than in placebo-treated patients even after accounting for the degree of weight loss. If cholelithiasis is suspected, gallbladder studies and appropriate clinical follow-up are indicated.
5.4 Hypoglycemia
Adult patients with type 2 diabetes mellitus on an insulin secretagogue (e.g., sulfonylurea) or insulin may have an increased risk of hypoglycemia with use of liraglutide, including severe hypoglycemia. In patients with type 2 diabetes, monitor blood glucose prior to starting liraglutide and during liraglutide treatment [see Dosage and Administration (2) and Adverse Reactions (6.1)].
The risk of hypoglycemia may be lowered by a reduction in the dose of sulfonylurea (or other concomitantly administered insulin secretagogues) or insulin. Inform patients using these concomitant medications of the risk of hypoglycemia and educate them on the signs and symptoms of hypoglycemia.
In the pediatric clinical trial, patients did not have type 2 diabetes but were provided with blood glucose meters. Clinically significant hypoglycemia, defined as blood glucose <54 mg/dL, occurred in 1.6% of the liraglutide-treated patients compared to 0.8% of placebo-treated patients [see Adverse Reactions (6.1)]. Inform all pediatric patients of the risk of hypoglycemia and educate them on the signs and symptoms of hypoglycemia.
5.5 Heart Rate Increase
Mean increases in resting heart rate of 2 to 3 beats per minute (bpm) were observed with routine clinical monitoring in liraglutide-treated adult patients compared to placebo in clinical trials. More patients treated with liraglutide, compared with placebo, had changes from baseline at two consecutive visits of more than 10 bpm (34% versus 19%, respectively) and 20 bpm (5% versus 2%, respectively). At least one resting heart rate exceeding 100 bpm was recorded for 6% of liraglutide-treated patients compared with 4% of placebo-treated patients, with this occurring at two consecutive study visits for 0.9% and 0.3%, respectively. Tachycardia was reported as an adverse reaction in 0.6% of liraglutide-treated patients and in 0.1% of placebo-treated patients.
In a clinical pharmacology trial that monitored heart rate continuously for 24 hours, liraglutide treatment was associated with a heart rate that was 4 to 9 bpm higher than that observed with placebo.
In a pediatric clinical trial, mean increases from baseline in resting heart rate of 3 to 7 bpm were observed with liraglutide treatment.
Heart rate should be monitored at regular intervals consistent with usual clinical practice. Patients should inform health care providers of palpitations or feelings of a racing heartbeat while at rest during liraglutide treatment. For patients who experience a sustained increase in resting heart rate while taking liraglutide, liraglutide should be discontinued.
5.6 Acute Kidney Injury Due to Volume Depletion
There have been postmarketing reports of acute kidney injury, in some cases requiring hemodialysis, in patients treated with liraglutide [see Adverse Reactions (6.2)]. The majority of the reported events occurred in patients who had experienced gastrointestinal reactions leading to dehydration such as nausea, vomiting, or diarrhea [see Adverse Reactions (6.1)]. Monitor renal function in patients reporting adverse reactions to liraglutide that could lead to volume depletion, especially during dosage initiation and escalation [see Use in Specific Populations (8.6)].
5.7 Severe Gastrointestinal Adverse Reactions
Use of GLP-1 receptor agonists, including liraglutide, has been associated with gastrointestinal adverse reactions, sometimes severe [see Adverse Reactions (6)]. In liraglutide clinical trials, severe gastrointestinal adverse reactions were reported more frequently among patients receiving liraglutide (4.8%) than placebo (1.4%). Severe gastrointestinal adverse reactions have also been reported postmarketing with GLP-1 receptor agonists. Liraglutide is not recommended in patients with severe gastroparesis.
5.8 Hypersensitivity Reactions
There have been reports of serious hypersensitivity reactions (e.g., anaphylactic reactions and angioedema) in patients treated with liraglutide [see Contraindications (4) and Adverse Reactions (6.1, 6.2)]. If a hypersensitivity reaction occurs, the patient should discontinue liraglutide injection and other suspect medications and promptly seek medical advice.
Anaphylaxis and angioedema have been reported with other GLP-1 receptor agonists. Use caution in a patient with a history of anaphylaxis or angioedema with another GLP-1 receptor agonist because it is unknown whether such patients will be predisposed to these reactions with liraglutide.
5.9 Suicidal Behavior and Ideation
In liraglutide adult clinical trials, 9 (0.3%) of 3,384 liraglutide-treated patients and 2 (0.1%) of the 1,941 placebo-treated patients reported suicidal ideation; one of these liraglutide-treated patients attempted suicide.
In a liraglutide pediatric clinical trial, 1 (0.8%) of the 125 liraglutide-treated patients died by suicide. There was insufficient information to establish a causal relationship to liraglutide.
Patients treated with liraglutide should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior. Discontinue liraglutide in patients who experience suicidal thoughts or behaviors. Avoid liraglutide in patients with a history of suicidal attempts or active suicidal ideation.
5.10 Pulmonary Aspiration During General Anesthesia or Deep Sedation
Liraglutide delays gastric emptying [see Clinical Pharmacology (12.2)]. There have been rare postmarketing reports of pulmonary aspiration in patients receiving GLP-1 receptor agonists undergoing elective surgeries or procedures requiring general anesthesia or deep sedation who had residual gastric contents despite reported adherence to preoperative fasting recommendations.
Available data are insufficient to inform recommendations to mitigate the risk of pulmonary aspiration during general anesthesia or deep sedation in patients taking liraglutide, including whether modifying preoperative fasting recommendations or temporarily discontinuing liraglutide could reduce the incidence of retained gastric contents. Instruct patients to inform healthcare providers prior to any planned surgeries or procedures if they are taking liraglutide.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are described below or elsewhere in the prescribing information:
- Risk of Thyroid C-Cell Tumors [see Warnings and Precautions (5.1)]
- Acute Pancreatitis [see Warnings and Precautions (5.2)]
- Acute Gallbladder Disease [see Warnings and Precautions (5.3)]
- Risk for Hypoglycemia with Concomitant Use of Anti-Diabetic Therapy [see Warnings and Precautions (5.4)]
- Heart Rate Increase [see Warnings and Precautions (5.5)]
- Acute Kidney Injury Due to Volume Depletion [see Warnings and Precautions (5.6)]
- Severe Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.7)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.8)]
- Suicidal Behavior and Ideation [see Warnings and Precautions (5.9)]
- Pulmonary Aspiration During General Anesthesia or Deep Sedation [see Warnings and Precautions (5.10)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
Liraglutide was evaluated for safety in 5 double-blind, placebo controlled trials that included 3,384 overweight or obese adult patients treated with liraglutide for a treatment period up to 56 weeks (3 trials), 52 weeks (1 trial), and 32 weeks (1 trial) and one trial of 56 weeks in 125 pediatric patients with obesity aged 12 years and older [see Clinical Studies (14.1, 14.2)]. All patients received study drug in addition to a reduced-calorie diet and increased physical activity counseling. In the adult trials, patients received liraglutide for a mean treatment duration of 46 weeks (median, 56 weeks). Baseline characteristics included a mean age of 47 years, 71% female, 85% white, 39% with hypertension, 15% with type 2 diabetes, 34% with dyslipidemia, 29% with a BMI greater than 40 kg/m2, and 9% with cardiovascular disease. In one of the 56-week trials, a subset of patients (with abnormal glucose measurements at randomization) [see Clinical Studies (14.1)] were enrolled for a placebo-controlled 160-week period instead, followed by a 12-week off-treatment follow-up. For those participating in this 160-week period, patients received liraglutide for a mean treatment duration of 110 weeks (median, 159 weeks). For all trials, dosing was initiated and increased weekly to reach the 3 mg dose.
In adult clinical trials, 9.8% of patients treated with liraglutide and 4.3% of patients treated with placebo prematurely discontinued treatment as a result of adverse reactions. The most common adverse reactions leading to discontinuation were nausea (2.9% versus 0.2% for liraglutide and placebo, respectively), vomiting (1.7% versus less than 0.1%), and diarrhea (1.4% versus 0%).
Adverse reactions reported in greater than or equal to 2% of liraglutide-treated adult patients and more frequently than in placebo-treated patients are shown in Table 2. Adverse reactions reported in greater than or equal to 3% of liraglutide-treated pediatric patients and more frequently than in placebo-treated patients are shown in Table 3.
Table 2. Adverse Reactions Occurring in ≥2% of Liraglutide-treated Adult Patients and More Frequently than Placebo Placebo
N=1,941
%
Liraglutide
N=3,384
%
Nausea
13.8
39.3
Diarrhea
9.9
20.9
Constipation
8.5
19.4
Vomiting
3.9
15.7
Injection Site Reaction1
10.5
13.9
Headache
12.6
13.6
Hypoglycemia in T2DM2
6.6
12.6
Dyspepsia
2.7
9.6
Fatigue
4.6
7.5
Dizziness
5
6.9
Abdominal Pain
3.1
5.4
Increased Lipase
2.2
5.3
Upper Abdominal Pain
2.7
5.1
Gastroenteritis
3.2
4.7
Gastroesophageal Reflux Disease
1.7
4.7
Abdominal Distension
3
4.5
Eructation
0.2
4.5
Urinary Tract Infection
3.1
4.3
Flatulence
2.5
4
Viral Gastroenteritis
1.6
2.8
Insomnia
1.7
2.4
Dry Mouth
1
2.3
Asthenia
0.8
2.1
Anxiety
1.6
2
1 The most common reactions, each reported by 1% to 2.5% of liraglutide-treated patients and more commonly than by placebo-treated patients, included erythema, pruritus, and rash at the injection site.
2 Defined as blood glucose <54 mg/dL with or without symptoms of hypoglycemia in patients with type 2 diabetes not on concomitant insulin (Study 2, liraglutide N=423, Placebo N=212). See text below for further information regarding hypoglycemia in patients with and without type 2 diabetes. T2DM = type 2 diabetes mellitus.
Table 3. Adverse Reactions Occurring in ≥3% of Liraglutide-treated Pediatric Patients and More Frequently than Placebo in a 56 Week Clinical Trial Placebo
N=126
%
Liraglutide
N=125
%
Nausea
14.3
42.4
Vomiting
4
34.4
Diarrhea
14.3
22.4
Hypoglycemia1
4
15.2
Gastroenteritis
4.8
12.8
Dizziness
3.2
10.4
Pyrexia
7.1
8
Abdominal discomfort
0.8
4.8
Constipation
2.4
4.8
Dyslipidemia
3.2
4.8
Fatigue
3.2
4.8
Cough
3.2
4
Depression
2.4
4
Dyspepsia
2.4
4
Pain in extremity
2.4
4
Injection site pain
3.2
3.2
Flatulence
0
3.2
Increased Blood Creatine Kinase
2.4
3.2
Increased Lipase
0.8
3.2
Rash
0
3.2
1 Defined as blood glucose <70 mg/dL with symptoms of hypoglycemia. Pediatric patients did not have type 2 diabetes mellitus. See text below for more detailed hypoglycemia information. Hypoglycemia
Adult Patients with Type 2 Diabetes
In a clinical trial in adult patients with type 2 diabetes mellitus and overweight (excess weight) or obesity, severe hypoglycemia (defined as requiring the assistance of another person) occurred in 3 (0.7%) of 422 liraglutide-treated patients (all taking a sulfonylurea) and in none of the 212 placebo-treated patients. In this trial, among patients taking a sulfonylurea, hypoglycemia defined as a plasma glucose less than 54 mg/dL with or without symptoms occurred in 31 (28.2%) of 110 liraglutide-treated patients and 7 (12.7%) of 55 placebo-treated patients. The doses of sulfonylureas were reduced by 50% at the beginning of the trial per protocol. Among patients not taking a sulfonylurea, blood glucose less than 54 mg/dL with or without symptoms occurred in 22 (7.1%) of 312 liraglutide-treated patients and 7 (4.5%) of 157 placebo-treated patients.In a liraglutide clinical trial in adult patients with overweight (excess weight) or obesity with type 2 diabetes mellitus treated with basal insulin and liraglutide in combination with a reduced-calorie diet and increased physical activity and up to 2 oral anti-diabetes medications, severe hypoglycemia was reported by 3 (1.5%) of 195 liraglutide-treated patients and 2 (1%) of 197 placebo-treated patients. No meaningful difference in hypoglycemia, defined as blood glucose less than 54 mg/dL with or without symptoms, was reported between groups.
Adult Patients without Type 2 Diabetes
In liraglutide clinical trials in adult patients without type 2 diabetes mellitus, there was no systematic capturing or reporting of hypoglycemia; patients were not provided with blood glucose meters or hypoglycemia diaries. Spontaneously reported symptomatic episodes of unconfirmed hypoglycemia were reported by 46 (1.6%) of 2,962 liraglutide-treated patients and 19 (1.1%) of 1,729 placebo-treated patients. Fasting plasma glucose values obtained at routine clinic visits less than 54 mg/dL, irrespective of hypoglycemic symptoms, occurred in 2 (0.1%) liraglutide-treated patients and 1 (0.1%) placebo-treated patients.Pediatric Patients without Type 2 Diabetes
In a 56-week placebo-controlled clinical trial of pediatric patients without type 2 diabetes mellitus in which blood glucose meters were provided, 19 (15.2%) of liraglutide-treated patients had hypoglycemia with a blood glucose less than 70 mg/dL with symptoms as compared to 5 (4%) of placebo-treated patients. Four (4) events of hypoglycemia defined as a plasma glucose less than 54 mg/dL occurred in 2 (1.6%) of 125 liraglutide-treated patients and 1 event occurred in 1 (0.8%) of 126 placebo-treated patients. No severe hypoglycemic episodes, defined as requiring assistance of another person to actively administer carbohydrate, glucagon, or other resuscitative actions, occurred in the liraglutide treatment group.Acute Pancreatitis
In liraglutide clinical trials in adults, acute pancreatitis was confirmed by adjudication in 9 (0.3%) of 3,291 liraglutide-treated patients and 2 (0.1%) of 1,843 placebo-treated patients. In addition, there were 2 cases of acute pancreatitis in liraglutide-treated patients who prematurely withdrew from these clinical trials, occurring 74 and 124 days after the last dose. There were 2 additional cases in liraglutide-treated patients, 1 during an off-treatment follow-up period within 2 weeks of discontinuing liraglutide, and 1 that occurred in a patient who completed treatment and was off-treatment for 106 days.In a liraglutide pediatric clinical trial, pancreatitis was not independently adjudicated. Pancreatitis was reported in 1 (0.8%) liraglutide-treated patient and resulted in treatment discontinuation.
Gastrointestinal Adverse Reactions
In the adult clinical trials, approximately 68% of liraglutide-treated patients and 39% of placebo-treated patients reported gastrointestinal disorders; the most frequently reported was nausea (39% and 14% of patients treated with liraglutide and placebo, respectively). Severe gastrointestinal adverse reactions were reported more frequently among patients receiving liraglutide (4.8%) than placebo (1.4 %). There have been reports of gastrointestinal adverse reactions, such as nausea, vomiting, and diarrhea, associated with volume depletion and renal impairment. Most episodes of gastrointestinal events were mild or moderate and did not lead to discontinuation of therapy (6.2% with liraglutide versus 0.8% with placebo discontinued treatment as a result of gastrointestinal adverse reactions). The percentage of patients reporting nausea declined as treatment continued. Other common adverse reactions that occurred at a higher incidence among liraglutide-treated patients included diarrhea, constipation, vomiting, dyspepsia, abdominal pain, dry mouth, gastritis, gastroesophageal reflux disease, flatulence, eructation and abdominal distension. There have been reports of gastrointestinal adverse reactions, such as nausea, vomiting, and diarrhea, associated with volume depletion and renal impairment.In a pediatric clinical trial, 8% of patients treated with liraglutide versus no patients who received placebo discontinued treatment as a result of gastrointestinal adverse reactions. Most adverse reactions leading to discontinuation were due to vomiting and nausea (4.8% and 3.2% of liraglutide-treated patients, respectively).
Cardiovascular Safety
Cardiovascular safety was assessed (LEADER, NCT01179048) in 9,340 patients with inadequately controlled type 2 diabetes and cardiovascular disease randomized to liraglutide 1.8 mg or placebo in addition to standard of care treatments for type 2 diabetes for a median duration of 3.5 years. The primary endpoint was the time from randomization to first occurrence of a major adverse cardiovascular event (MACE) defined as: cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke. No increased risk for MACE was observed with liraglutide 1.8 mg. The total number of primary component MACE endpoints was 1,302 [608 (13.0%) with liraglutide 1.8 mg and 694 (14.9%) with placebo]. Liraglutide 1.8 mg (Victoza) is used in the treatment of type 2 diabetes mellitus in adults. The efficacy of liraglutide at doses below 3 mg daily has not been established for weight reduction.Asthenia, Fatigue, Malaise, Dysgeusia and Dizziness
Events of asthenia, fatigue, malaise, dysgeusia and dizziness were mainly reported within the first 12 weeks of treatment with liraglutide and were often co-reported with gastrointestinal events such as nausea, vomiting, and diarrhea.Immunogenicity
The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, the incidence of antibodies to liraglutide cannot be directly compared with the incidence of antibodies of other products.Patients treated with liraglutide may develop anti-liraglutide antibodies. Anti-liraglutide antibodies were detected in 42 (2.8%) of 1,505 liraglutide-treated adult patients with a post-baseline assessment. Antibodies that had a neutralizing effect on liraglutide in an in vitro assay occurred in 18 (1.2%) of 1,505 liraglutide-treated patients. Presence of antibodies may be associated with a higher incidence of injection site reactions and reports of low blood glucose. In clinical trials, these events were usually classified as mild and resolved while patients continued on treatment.
In a pediatric clinical trial, anti-liraglutide antibodies were detected in 14 (12%) of 117 liraglutide-treated patients with a post-baseline assessment; 5 (4.3%) had persistent antibodies as defined by more than 2 antibody visits at least 16 weeks apart. Two patients (1.7%) remained positive throughout the follow-up period; 1 (0.9%) had antibodies cross reactive to native GLP-1. No patients had neutralizing antibodies.
Allergic Reactions
Urticaria was reported in 0.7% of liraglutide-treated patients and 0.5% of placebo-treated patients. Anaphylactic reactions, asthma, bronchial hyperreactivity, bronchospasm, oropharyngeal swelling, facial swelling, angioedema, pharyngeal edema, type IV hypersensitivity reactions have been reported in patients treated with liraglutide in clinical trials. Cases of anaphylactic reactions with additional symptoms such as hypotension, palpitations, dyspnea, and edema have been reported with marketed use of liraglutide. Anaphylactic reactions may potentially be life-threatening.Breast Cancer
In liraglutide clinical trials in adults, breast cancer confirmed by adjudication was reported in 17 (0.7%) of 2,379 liraglutide-treated women compared with 3 (0.2%) of 1,300 placebo-treated women, including invasive cancer (13 liraglutide- and 2 placebo-treated women) and ductal carcinoma in situ (4 liraglutide- and 1 placebo-treated woman). The majority of cancers were estrogen- and progesterone-receptor positive. There were too few cases to determine whether these cases were related to liraglutide. In addition, there are insufficient data to determine whether liraglutide has an effect on pre-existing breast neoplasia.Papillary Thyroid Cancer
In liraglutide clinical trials in adults, papillary thyroid carcinoma confirmed by adjudication was reported in 8 (0.2%) of 3,291 liraglutide-treated patients compared with no cases among 1,843 placebo-treated patients. Four of these papillary thyroid carcinomas were less than 1 cm in greatest diameter and 4 were diagnosed in surgical pathology specimens after thyroidectomy prompted by findings identified prior to treatment.Colorectal Neoplasms
In liraglutide clinical trials in adults, benign colorectal neoplasms (mostly colon adenomas) confirmed by adjudication were reported in 20 (0.6%) of 3,291 liraglutide-treated patients compared with 7 (0.4%) of 1,843 placebo-treated patients. Six positively adjudicated cases of malignant colorectal neoplasms were reported in 5 liraglutide-treated patients (0.2%, mostly adenocarcinomas) and 1 in a placebo-treated patient (0.1%, neuroendocrine tumor of the rectum).Cardiac Conduction Disorders
In liraglutide clinical trials in adults, 11 (0.3%) of 3,384 liraglutide-treated patients compared with none of the 1,941 placebo-treated patients had a cardiac conduction disorder, reported as first degree atrioventricular block, right bundle branch block, or left bundle branch block.Hypotension
Adverse reactions related to hypotension (hypotension, orthostatic hypotension, circulatory collapse, and decreased blood pressure) were reported more frequently with liraglutide (1.1%) compared with placebo (0.5%) in liraglutide clinical trials in adults. Systolic blood pressure decreases to less than 80 mmHg were observed in 4 (0.1%) liraglutide-treated patients compared with no placebo-treated patients. One of the liraglutide-treated patients had hypotension associated with gastrointestinal adverse reactions and renal failure [see Warnings and Precautions (5.6)].Laboratory Abnormalities
Liver Enzymes
Increases in alanine aminotransferase (ALT) greater than or equal to 10 times the upper limit of normal were observed in 5 (0.15%) liraglutide-treated patients (two of whom had ALT greater than 20 and 40 times the upper limit of normal) compared with 1 (0.05%) placebo-treated patient during the liraglutide clinical trials. Because clinical evaluation to exclude alternative causes of ALT and aspartate aminotransferase (AST) increases was not done in most cases, the relationship to liraglutide is uncertain. Some increases in ALT and AST were associated with other confounding factors (such as gallstones).Serum Calcitonin
Calcitonin, a biological marker of MTC, was measured throughout the clinical development program [see Warnings and Precautions (5.1)]. More patients treated with liraglutide in the clinical trials were observed to have high calcitonin values during treatment, compared with placebo. The proportion of patients with calcitonin greater than or equal to 2 times the upper limit of normal at the end of the trial was 1.2% in liraglutide-treated patients and 0.6% in placebo-treated patients. Calcitonin values greater than 20 ng/L at the end of the trial occurred in 0.5% of liraglutide-treated patients and 0.2% of placebo-treated patients; among patients with pre-treatment serum calcitonin less than 20 ng/L, none had calcitonin elevations to greater than 50 ng/L at the end of the trial.Serum Lipase and Amylase
Serum lipase and amylase were routinely measured in the liraglutide clinical trials. Among liraglutide-treated patients, 2.1% had a lipase value at anytime during treatment of greater than or equal to 3 times the upper limit of normal compared with 1.0% of placebo-treated patients. 0.1% of liraglutide-treated patients had an amylase value at anytime in the trial of greater than or equal to 3 times the upper limit of normal versus 0.1% of placebo-treated patients. The clinical significance of elevations in lipase or amylase with liraglutide is unknown in the absence of other signs and symptoms of pancreatitis [see Warnings and Precautions (5.2)].6.2 Postmarketing Experience
The following adverse reactions have been reported during post-approval use of liraglutide, the active ingredient of liraglutide injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Gastrointestinal
Acute pancreatitis; hemorrhagic and necrotizing pancreatitis, sometimes resulting in death; ileus, intestinal obstruction, severe constipation including fecal impaction, nausea, vomiting and diarrhea leading to dehydration
Hepatobiliary
Hyperbilirubinemia, elevations of liver enzymes, cholestasis and hepatitis
Hypersensitivity
Rash, pruritus, angioedema and anaphylactic reactions
Neoplasms
Medullary thyroid carcinoma
Neurologic
Dysesthesia, headache
Pulmonary
Pulmonary aspiration has occurred in patients receiving GLP-1 receptor agonists undergoing elective surgeries or procedures requiring general anesthesia or deep sedation.
Renal
Acute kidney injury, sometimes requiring hemodialysis; increased serum creatinine
General Disorders and Administration Site Conditions
Allergic reactions: rash and pruritus
Immune System
Angioedema and anaphylactic reactions
Skin and Subcutaneous Tissue
Cutaneous amyloidosis, alopecia
-
7 DRUG INTERACTIONS
7.1 Oral Medications
Liraglutide causes a delay of gastric emptying, and thereby has the potential to impact the absorption of concomitantly administered oral medications. In clinical pharmacology trials, liraglutide did not affect the absorption of the tested orally administered medications to any clinically relevant degree. Nonetheless, monitor for potential consequences of delayed absorption of oral medications concomitantly administered with liraglutide injection.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on animal reproduction studies, there may be risks to the fetus from exposure to liraglutide during pregnancy. Liraglutide should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Additionally, weight loss offers no benefit to a pregnant patient and may cause fetal harm. When a pregnancy is recognized, advise the pregnant patient of the risk to a fetus, and discontinue liraglutide (see Clinical Considerations).Animal reproduction studies identified increased adverse embryofetal developmental outcomes from exposure during pregnancy. Liraglutide exposure was associated with early embryonic deaths and an imbalance in some fetal abnormalities in pregnant rats administered liraglutide during organogenesis at doses that approximate clinical exposures at the maximum recommended human dose (MRHD) of 3 mg/day. In pregnant rabbits administered liraglutide during organogenesis, decreased fetal weight and an increased incidence of major fetal abnormalities were seen at exposures below the human exposures at the MRHD (see Animal Data).
The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage of clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryofetal risk
Appropriate weight gain based on pre-pregnancy weight is currently recommended for all pregnant patients, including those who already have overweight or obesity, because of the obligatory weight gain that occurs in maternal tissues during pregnancy.Animal Data
Liraglutide has been shown to be teratogenic in rats at or above 0.8-times systemic exposures in obese humans resulting from the maximum recommended human dose (MRHD) of 3 mg/day based on plasma area under the time-concentration curve (AUC) comparison. Liraglutide has been shown to cause reduced growth and increased total major abnormalities in rabbits at systemic exposures below exposure in obese humans at the MRHD based on plasma AUC comparison.Female rats given subcutaneous doses of 0.1, 0.25 and 1 mg/kg/day liraglutide beginning 2 weeks before mating through gestation day 17 had estimated systemic exposures 0.8-, 3-, and 11-times the exposure in obese humans at the MRHD based on plasma AUC comparison. The number of early embryonic deaths in the 1 mg/kg/day group increased slightly. Fetal abnormalities and variations in kidneys and blood vessels, irregular ossification of the skull, and a more complete state of ossification occurred at all doses. Mottled liver and minimally kinked ribs occurred at the highest dose. The incidence of fetal malformations in liraglutide-treated groups exceeding concurrent and historical controls were misshapen oropharynx and/or narrowed opening into larynx at 0.1 mg/kg/day and umbilical hernia at 0.1 and 0.25 mg/kg/day.
Pregnant rabbits given subcutaneous doses of 0.01, 0.025 and 0.05 mg/kg/day liraglutide from gestation day 6 through day 18 inclusive, had estimated systemic exposures less than the exposure in obese humans at the MRHD of 3 mg/day at all doses, based on plasma AUC comparison. Liraglutide decreased fetal weight and dose-dependently increased the incidence of total major fetal abnormalities at all doses. The incidence of malformations exceeded concurrent and historical controls at 0.01 mg/kg/day (kidneys, scapula), greater than or equal to 0.01 mg/kg/day (eyes, forelimb), 0.025 mg/kg/day (brain, tail and sacral vertebrae, major blood vessels and heart, umbilicus), greater than or equal to 0.025 mg/kg/day (sternum) and at 0.05 mg/kg/day (parietal bones, major blood vessels). Irregular ossification and/or skeletal abnormalities occurred in the skull and jaw, vertebrae and ribs, sternum, pelvis, tail, and scapula; and dose-dependent minor skeletal variations were observed. Visceral abnormalities occurred in blood vessels, lung, liver, and esophagus. Bilobed or bifurcated gallbladder was seen in all treatment groups, but not in the control group.
In pregnant female rats given subcutaneous doses of 0.1, 0.25 and 1 mg/kg/day liraglutide from gestation day 6 through weaning or termination of nursing on lactation day 24, estimated systemic exposures were 0.8-, 3-, and 11-times exposure in obese humans at the MRHD of 3 mg/day, based on plasma AUC comparison. A slight delay in parturition was observed in the majority of treated rats. Group mean body weight of neonatal rats from liraglutide-treated dams was lower than neonatal rats from control group dams. Bloody scabs and agitated behavior occurred in male rats descended from dams treated with 1 mg/kg/day liraglutide. Group mean body weight from birth to postpartum day 14 trended lower in F2 generation rats descended from liraglutide-treated rats compared to F2 generation rats descended from controls, but differences did not reach statistical significance for any group.
8.2 Lactation
Risk Summary
There are no data on the presence of liraglutide in human milk, the effects on the breastfed infant, or effects on milk production. Liraglutide was present in the milk of lactating rats (see Data).The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for liraglutide and any potential adverse effects on the breastfed infant from liraglutide or from the underlying maternal condition.
Data
In lactating rats, liraglutide was present unchanged in milk at concentrations approximately 50% of maternal plasma concentrations.8.4 Pediatric Use
The safety and effectiveness of liraglutide as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management have been established in pediatric patients aged 12 years and older with body weight above 60 kg and an initial BMI corresponding to 30 kg/m2 or greater for adults (obese) by international cut-offs. Use of liraglutide for this indication is supported by a 56-week double-blind, placebo-controlled clinical trial in 251 pediatric patients aged 12 to 17 years, a pharmacokinetic study in pediatric patients, and studies in adults with obesity [see Clinical Pharmacology (12.3) and Clinical Studies (14.1, 14.2)].
In the pediatric clinical trial, there was one death due to suicide in a liraglutide-treated patient [see Warnings and Precautions (5.8)]; one liraglutide-treated patient had an event of pancreatitis [see Warnings and Precautions (5.2)]; more episodes of hypoglycemia confirmed by self blood glucose monitoring occurred in liraglutide-treated patients compared to placebo [see Warnings and Precautions (5.4) and Adverse Reactions (6.1)]; and mean increases in resting heart rate of 3 to 7 bpm from baseline were observed with liraglutide-treated patients [see Warnings and Precautions (5.5)].
The safety and effectiveness of liraglutide have not been established in patients less than 12 years of age.
8.5 Geriatric Use
In the liraglutide clinical trials, 232 (6.9%) of the liraglutide-treated patients were 65 years of age and over, and 17 (0.5%) of the liraglutide-treated patients were 75 years of age and over. No overall differences in safety or effectiveness were observed between these patients and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
There is limited experience with liraglutide in patients with mild, moderate, and severe renal impairment, including end‑stage renal disease.
8.7 Hepatic Impairment
There is limited experience in patients with mild, moderate, or severe hepatic impairment. Therefore, liraglutide should be used with caution in this patient population [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
Overdoses have been reported in clinical trials and postmarketing use of liraglutide. Effects have included severe nausea, severe vomiting and severe hypoglycemia. In the event of overdosage, consider contacting the Poison Help line (1-800-222-1222) or a medical toxicologist for additional overdosage management recommendations. Initiate appropriate supportive treatment according to the patient’s clinical signs and symptoms.
-
11 DESCRIPTION
Liraglutide injection contains liraglutide, an analog of the fragment 7-37 of the naturally occurring human glucagon-like peptide 1 (GLP-1[7 - 37]), containing one amino acid substitution (Arg for Lys at position 34 of the GLP-1 sequence) and an additional fatty acid chain. Liraglutide is a linear peptide with 31 amino acids and a γ-glutamyl-palmitoyl residue linked to the ɛ-amino group of Lys20. All amino acid residues with exception of the archiral glycines are in the L-configuration. The structural formula (Figure 1) is:
Figure 1. Structural Formula of liraglutide
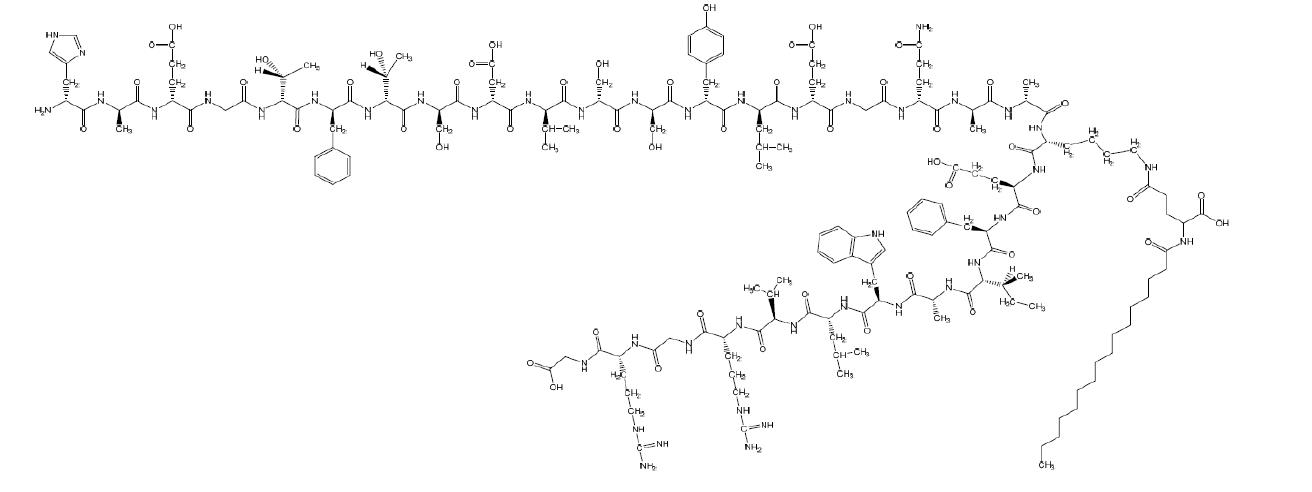
C172H265N43O51 M.W. 3751.26 Daltons
Liraglutide is manufactured by chemical synthesis. Liraglutide injection is a sterile, aqueous, clear, colorless solution for subcutaneous use. Each 1 mL of liraglutide injection solution contains 6 mg of liraglutide and the following inactive ingredients: phenol, 5.5 mg; propylene glycol, 14 mg; sodium phosphate dibasic dihydrate, 1.42 mg; and water for injection. Liraglutide injection has a pH of approximately 8.15, hydrochloric acid or sodium hydroxide may be added to adjust pH. Each prefilled pen contains a 3 mL solution of liraglutide injection equivalent to 18 mg liraglutide (free-base, anhydrous).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Liraglutide is an acylated human GLP-1 receptor agonist with 97% amino acid sequence homology to endogenous human GLP-1(7-37). Like endogenous GLP-1, liraglutide binds to and activates the GLP-1 receptor, a cell-surface receptor coupled to adenylyl cyclase activation through the stimulatory G-protein, Gs. Endogenous GLP-1 has a half-life of 1.5 to 2 minutes due to degradation by the ubiquitous endogenous enzymes, dipeptidyl peptidase 4 (DPP-4) and neutral endopeptidases (NEP). Unlike native GLP-1, liraglutide is stable against metabolic degradation by both peptidases and has a plasma half-life of 13 hours after subcutaneous administration. The pharmacokinetic profile of liraglutide, which makes it suitable for once-daily administration, is a result of self-association that delays absorption, plasma protein binding, and stability against metabolic degradation by DPP-4 and NEP.
GLP-1 is a physiological regulator of appetite and calorie intake, and the GLP-1 receptor is present in several areas of the brain involved in appetite regulation. In animal studies, peripheral administration of liraglutide resulted in the presence of liraglutide in specific brain regions regulating appetite, including the hypothalamus. Although liraglutide activated neurons in brain regions known to regulate appetite, specific brain regions mediating the effects of liraglutide on appetite were not identified in rats.
12.2 Pharmacodynamics
Liraglutide lowers body weight through decreased calorie intake. Liraglutide does not increase 24-hour energy expenditure.
As with other GLP-1 receptor agonists, liraglutide stimulates insulin secretion and reduces glucagon secretion in a glucose-dependent manner. These effects can lead to a reduction of blood glucose.
Gastric Emptying
Liraglutide delays gastric emptying.
Cardiac Electrophysiology (QTc) in healthy volunteers
The effect of liraglutide on cardiac repolarization was tested in a QTc study. Liraglutide at steady-state concentrations after daily doses up to 1.8 mg did not produce QTc prolongation. The maximum liraglutide plasma concentration (Cmax) in overweight and obese subjects treated with liraglutide 3 mg is similar to the Cmax observed in the liraglutide QTc study in healthy volunteers.
12.3 Pharmacokinetics
Absorption - Following subcutaneous administration, maximum concentrations of liraglutide are achieved at 11 hours post dosing. The average liraglutide steady state concentration (AUCτ/24) reached approximately 116 ng/mL in obese (BMI 30 to 40 kg/m2) subjects following administration of liraglutide. Liraglutide exposure increased proportionally in the dose range of 0.6 mg to 3 mg. The intra-subject coefficient of variation for liraglutide AUC was 11% following single dose administration. Liraglutide exposures were considered similar among three subcutaneous injection sites (upper arm, abdomen, and thigh). Absolute bioavailability of liraglutide following subcutaneous administration is approximately 55%.
Distribution - The mean apparent volume of distribution after subcutaneous administration of liraglutide 3 mg is 20 to 25L (for a person weighing approximately 100 kg). The mean volume of distribution after intravenous administration of liraglutide is 0.07 L/kg. Liraglutide is extensively bound to plasma protein (greater than 98%).
Metabolism - During the initial 24 hours following administration of a single [3H]-liraglutide dose to healthy subjects, the major component in plasma was intact liraglutide. Liraglutide is endogenously metabolized in a similar manner to large proteins without a specific organ as a major route of elimination.
Elimination - Following a [3H]-liraglutide dose, intact liraglutide was not detected in urine or feces. Only a minor part of the administered radioactivity was excreted as liraglutide-related metabolites in urine or feces (6% and 5%, respectively). The majority of urine and feces radioactivity was excreted during the first 6 to 8 days. The mean apparent clearance following subcutaneous administration of a single dose of liraglutide is approximately 0.9 to 1.4 L/h with an elimination half-life of approximately 13 hours, making liraglutide suitable for once daily administration.
Specific Populations
Elderly - Age had no effect on the pharmacokinetics of liraglutide based on a pharmacokinetic study in healthy elderly subjects (65 to 83 years) and population pharmacokinetic analyses of data from overweight and obese patients 18 to 82 years of age [see Use in Specific Populations (8.5)].Gender - Based on the results of population pharmacokinetic analyses, females have 24% lower weight adjusted clearance of liraglutide compared to males.
Race and Ethnicity - Race and ethnicity had no effect on the pharmacokinetics of liraglutide based on the results of population pharmacokinetic analyses that included overweight and obese patients of White, Black or African American, Asian and Hispanic/Non-Hispanic Ethnic groups.
Body Weight - Body weight significantly affects the pharmacokinetics of liraglutide based on results of population pharmacokinetic analyses conducted in patients with body weight range of 60 to 234 kg. The exposure of liraglutide decreases as baseline body weight increases.
Pediatric - A population pharmacokinetic analysis was conducted for liraglutide using data from 134 pediatric patients (12 to 17 years of age) with obesity. The liraglutide exposure in the pediatric patients was similar to that in adults with obesity [see Use in Specific Populations (8.4)].
Renal Impairment - The single-dose pharmacokinetics of liraglutide were evaluated in patients with varying degrees of renal impairment. Patients with mild (estimated creatinine clearance 50 to 80 mL/min) to severe (estimated creatinine clearance less than 30 mL/min) renal impairment and patients with end-stage renal disease requiring dialysis were included in the trial. Compared to healthy subjects, liraglutide AUC in mild, moderate, and severe renal impairment and in end-stage renal disease was on average 35%, 19%, 29% and 30% lower, respectively [see Use in Specific Populations (8.6)].
Hepatic Impairment - The single-dose pharmacokinetics of liraglutide were evaluated in patients with varying degrees of hepatic impairment. Patients with mild (Child Pugh score 5 to 6) to severe (Child Pugh score greater than 9) hepatic impairment were included in the trial. Compared to healthy subjects, liraglutide AUC in subjects with mild, moderate and severe hepatic impairment was on average 11%, 14% and 42% lower, respectively [see Use in Specific Populations (8.7)].
Drug Interactions
In vitro assessment of drug-drug interactions
Liraglutide has low potential for pharmacokinetic drug-drug interactions related to cytochrome P450 (CYP) and plasma protein binding.In vivo assessment of drug-drug interactions
The drug-drug interaction studies were performed at steady state with liraglutide 1.8 mg/day. The effect on rate of gastric emptying was equivalent between liraglutide 1.8 mg and 3 mg (acetaminophen AUC0-300min). Administration of the interacting drugs was timed so that Cmax of liraglutide (8 to 12 h) would coincide with the absorption peak of the co-administered drugs.Oral Contraceptives
A single dose of an oral contraceptive combination product containing 0.03 mg ethinylestradiol and 0.15 mg levonorgestrel was administered under fed conditions and 7 hours after the dose of liraglutide at steady state. Liraglutide lowered ethinylestradiol and levonorgestrel Cmax by 12% and 13%, respectively. There was no effect of liraglutide on the overall exposure (AUC) of ethinylestradiol. Liraglutide increased the levonorgestrel AUC0-∞ by 18%. Liraglutide delayed Tmax for both ethinylestradiol and levonorgestrel by 1.5 h.Digoxin
A single dose of digoxin 1 mg was administered 7 hours after the dose of liraglutide at steady state. The concomitant administration with liraglutide resulted in a reduction of digoxin AUC by 16%; Cmax decreased by 31%. Digoxin median time to maximal concentration (Tmax) was delayed from 1 h to 1.5 h.Lisinopril
A single dose of lisinopril 20 mg was administered 5 minutes after the dose of liraglutide at steady state. The coadministration with liraglutide resulted in a reduction of lisinopril AUC by 15%; Cmax decreased by 27%. Lisinopril median Tmax was delayed from 6 h to 8 h with liraglutide.Atorvastatin
Liraglutide did not change the overall exposure (AUC) of atorvastatin following a single dose of atorvastatin 40 mg, administered 5 hours after the dose of liraglutide at steady state. Atorvastatin Cmax was decreased by 38% and median Tmax was delayed from 1 h to 3 h with liraglutide.Acetaminophen
Liraglutide did not change the overall exposure (AUC) of acetaminophen following a single dose of acetaminophen 1000 mg, administered 8 hours after the dose of liraglutide at steady state. Acetaminophen Cmax was decreased by 31% and median Tmax was delayed up to 15 minutes.Griseofulvin
Liraglutide did not change the overall exposure (AUC) of griseofulvin following coadministration of a single dose of griseofulvin 500 mg with liraglutide at steady state. Griseofulvin Cmax increased by 37% while median Tmax did not change.Insulin Detemir
No pharmacokinetic interaction was observed between liraglutide and insulin detemir when separate subcutaneous injections of insulin detemir 0.5 Unit/kg (single-dose) and liraglutide 1.8 mg (steady state) were administered to patients with type 2 diabetes mellitus. -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
A 104-week carcinogenicity study was conducted in male and female CD-1 mice at doses of 0.03, 0.2, 1, and 3 mg/kg/day liraglutide administered by bolus subcutaneous injection yielding systemic exposures 0.2-, 2-, 10- and 43-times the exposure in obese humans, respectively, at the maximum recommended human dose (MRHD) of 3 mg/day based on plasma AUC comparison. A dose-related increase in benign thyroid C-cell adenomas was seen in the 1 and the 3 mg/kg/day groups with incidences of 13% and 19% in males and 6% and 20% in females, respectively. C-cell adenomas did not occur in control groups or 0.03 and 0.2 mg/kg/day groups. Treatment-related malignant C-cell carcinomas occurred in 3% of females in the 3 mg/kg/day group. Thyroid C-cell tumors are rare findings during carcinogenicity testing in mice. A treatment-related increase in fibrosarcomas was seen on the dorsal skin and subcutis, the body surface used for drug injection, in males in the 3 mg/kg/day group. These fibrosarcomas were attributed to the high local concentration of drug near the injection site. The liraglutide concentration in the clinical formulation (6 mg/mL) is 10-times higher than the concentration in the formulation used to administer 3 mg/kg/day liraglutide to mice in the carcinogenicity study (0.6 mg/mL).
A 104-week carcinogenicity study was conducted in male and female Sprague Dawley rats at doses of 0.075, 0.25 and 0.75 mg/kg/day liraglutide administered by bolus subcutaneous injection with exposures 0.5-, 2- and 7-times the exposure in obese humans, respectively, resulting from the MRHD based on plasma AUC comparison. A treatment-related increase in benign thyroid C-cell adenomas was seen in males in 0.25 and 0.75 mg/kg/day liraglutide groups with incidences of 12%, 16%, 42%, and 46% and in all female liraglutide-treated groups with incidences of 10%, 27%, 33%, and 56% in 0 (control), 0.075, 0.25, and 0.75 mg/kg/day groups, respectively. A treatment-related increase in malignant thyroid C-cell carcinomas was observed in all male liraglutide-treated groups with incidences of 2%, 8%, 6%, and 14% and in females at 0.25 and 0.75 mg/kg/day with incidences of 0%, 0%, 4%, and 6% in 0 (control), 0.075, 0.25, and 0.75 mg/kg/day groups, respectively. Thyroid C-cell carcinomas are rare findings during carcinogenicity testing in rats.
Studies in mice demonstrated that liraglutide-induced C-cell proliferation was dependent on the GLP-1 receptor and that liraglutide did not cause activation of the REarranged during Transfection (RET) proto-oncogene in thyroid C-cells.
Human relevance of thyroid C-cell tumors in mice and rats is unknown and has not been determined by clinical studies or nonclinical studies [see Boxed Warning, Warnings and Precautions (5.1)].
Liraglutide was negative with and without metabolic activation in the Ames test for mutagenicity and in a human peripheral blood lymphocyte chromosome aberration test for clastogenicity. Liraglutide was negative in repeat-dose in vivo micronucleus tests in rats.
In rat fertility studies using subcutaneous doses of 0.1, 0.25 and 1 mg/kg/day liraglutide, males were treated for 4 weeks prior to and throughout mating and females were treated 2 weeks prior to and throughout mating until gestation day 17. No direct adverse effects on male fertility was observed at doses up to 1 mg/kg/day, a high dose yielding an estimated systemic exposure 11-times the exposure in obese humans at the MRHD, based on plasma AUC comparison. In female rats, an increase in early embryonic deaths occurred at 1 mg/kg/day. Reduced body weight gain and food consumption were observed in females at the 1 mg/kg/day dose.
-
14 CLINICAL STUDIES
14.1 Weight Management Trials in Adults with Overweight or Obesity
The safety and efficacy of liraglutide for chronic weight management in conjunction with reduced caloric intake and increased physical activity were studied in three 56-week, randomized, double-blind, placebo-controlled trials. In all studies, liraglutide was titrated to 3 mg daily during a 4-week period. All patients received instruction for a reduced-calorie diet (approximately 500 kcal/day deficit) and physical activity counseling (recommended increase in physical activity of minimum 150 mins/week) that began with the first dose of study medication or placebo and continued throughout the trial.
Study 1 enrolled 3,731 patients with obesity (BMI greater than or equal to 30 kg/m2) or with overweight (BMI 27 to 29.9 kg/m2) and at least one weight-related comorbid condition such as treated or untreated dyslipidemia or hypertension; patients with type 2 diabetes mellitus were excluded. Patients were randomized in a 2:1 ratio to either liraglutide or placebo. Patients were stratified based on the presence or absence of abnormal blood glucose measurements at randomization. All patients were treated for up to 56 weeks. Those patients with abnormal glucose measurements at randomization (2,254 of the 3,731 patients) were treated for a total of 160 weeks. At baseline, mean age was 45 years (range 18 to 78), 79% were female, 85% were White, 10% were Black or African American, and 11% were Hispanic/Latino Ethnicity. Mean baseline body weight was 106.3 kg and mean BMI was 38.3 kg/m2.
Study 2 was a 56-week trial that enrolled 635 patients with type 2 diabetes and with either overweight or obesity (as defined above). Patients were to have an HbA1c of 7% to 10% and be treated with metformin, a sulfonylurea, or a glitazone as single agent or in any combination, or with a reduced-calorie diet and physical activity alone. Patients were randomized in a 2:1 ratio to receive either liraglutide or placebo. The mean age was 55 years (range 18 to 82), 50% were female, 83% were White, 12% were Black or African American, and 10% were Hispanic/Latino Ethnicity. Mean baseline body weight was 105.9 kg and mean BMI was 37.1 kg/m2.
Study 3 was a 56-week trial that enrolled 422 patients with obesity (BMI greater than or equal to 30 kg/m2) or with overweight (BMI 27 to 29.9 kg/m2) and at least one weight-related comorbid condition such as treated or untreated dyslipidemia or hypertension; patients with type 2 diabetes mellitus were excluded. All patients were first treated with a low-calorie diet (total energy intake 1,200 to 1,400 kcal/day) in a run-in period lasting up to 12 weeks. Patients who lost at least 5% of their screening body weight after 4 to 12 weeks during the run-in were then randomized, with equal allocation, to receive either liraglutide or placebo for 56 weeks. The mean age was 46 years (range 18 to 73), 81% were female, 84% were White, 13% were Black or African American, and 7% were Hispanic/Latino Ethnicity. Mean baseline body weight was 99.6 kg and mean BMI was 35.6 kg/m2.
The proportions of patients who discontinued study drug in the 56-week trials were 27% for the liraglutide-treated group and 35% for the placebo-treated group, and in the 160-week trial the proportions of patients who discontinued were 47% and 55%, respectively. In the 56-week trials, approximately 10% of patients treated with liraglutide and 4% of patients treated with placebo discontinued treatment due to an adverse reaction [see Adverse Reactions (6.1)]. The majority of patients who discontinued liraglutide due to adverse reactions did so during the first few months of treatment. In the 160-week trial the proportions of patients who discontinued due to an adverse reaction was 13% and 6% for liraglutide- and placebo-treated patients, respectively.
Effect of Liraglutide on Body Weight in 56-week Trials
For Study 1 and Study 2, the primary efficacy parameters were mean percent change in body weight and the percentages of patients achieving greater than or equal to 5% and 10% weight loss from baseline to week 56. For Study 3, the primary efficacy parameters were mean percent change in body weight from randomization to week 56, the percentage of patients not gaining more than 0.5% body weight from randomization (i.e., after run-in) to week 56, and the percentage of patients achieving greater than or equal to 5% weight loss from randomization to week 56. Because losing at least 5% of fasting body weight through lifestyle intervention during the 4- to 12-week run-in was a condition for their continued participation in the randomized treatment period, the results may not reflect those expected in the general population.Table 4 presents the results for the changes in weight observed in Studies 1, 2, and 3. After 56 weeks, treatment with liraglutide resulted in a statistically significant reduction in weight compared with placebo. Statistically significantly greater proportions of patients treated with liraglutide achieved 5% and 10% weight loss than those treated with placebo. In Study 3, statistically significantly more patients randomized to liraglutide than placebo had not gained more than 0.5% of body weight from randomization to week 56.
Table 4. Changes in Weight at Week 56 for Studies 1, 2, and 3 Study 1 (Obesity or overweight with comorbidity)
Study 2 (Type 2 diabetes with obesity or overweight)
Study 3 (Obesity or overweight with comorbidity following at least 5% weight loss with diet)
Liraglutide
N=2,487Placebo
N=1,244Liraglutide
N=423Placebo
N=212Liraglutide
N=212Placebo
N=210Weight
Baseline mean (SD) (kg)
106.2
(21.2)
106.2 (21.7)
105.7
(21.9)
106.5
(21.3)
100.4
(20.8)
98.7
(21.2)
Percent change from baseline (LSMean)
-7.4
-3
-5.4
-1.7
-4.9
0.3
Difference from placebo
(LSMean) (95% CI)
-4.5*
(-5.2; -3.8)
-3.7*
(-4.7; -2.7)
-5.2*
(-6.8; -3.5)
% of Patients losing greater than or equal to 5% body weight
62.3%
34.4%
49%
16.4%
44.2%
21.7%
Difference from placebo
(LSMean) (95% CI)
27.9*
(23.9; 31.9)
32.6*
(25.1; 40.1)
22.6*
(13.9; 31.3)
% of Patients losing greater than 10% body weight
33.9%
15.4%
22.4%
5.5%
25.4%
6.9%
Difference from placebo
(LSMean) (95% CI)
18.5*
(15.2; 21.7)
16.9*
(11.7; 22.1)
18.5*
(11.7; 25.3)
SD = Standard Deviation; CI = Confidence Interval
* p < 0.0001 compared to placebo. Type 1 error was controlled across the three endpoints.
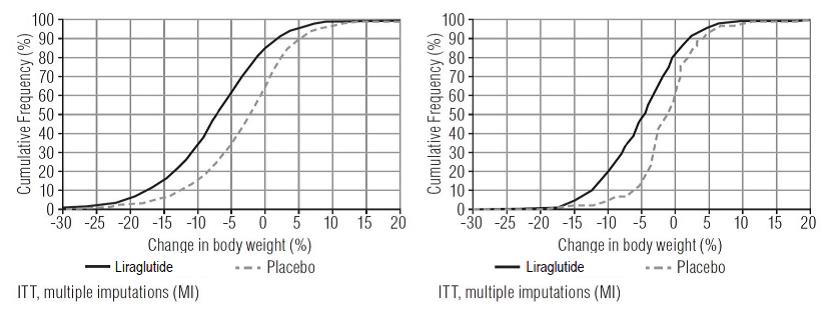
Includes all randomized subjects who had a baseline body weight measurement. All available body weight data during the 56 week treatment period are included in the analysis. In Studies 1 and 2 missing values for week 56 were handled using multiple imputations analysis. In Study 3 missing values for week 56 were handled using weighted regression analysis.The cumulative frequency distributions of change in body weight from baseline to week 56 are shown in Figure 2 for Studies 1 and 2. One way to interpret this figure is to select a change in body weight of interest on the horizontal axis and note the corresponding proportions of patients (vertical axis) in each treatment group who achieved at least that degree of weight loss. For example, note that the vertical line arising from ‑10% in Study 1 intersects the liraglutide and placebo curves at approximately 34% and 15%, respectively, which correspond to the values shown in Table 4.
Figure 2. Change in body weight (%) from baseline to week 56 (Study 1 on left and Study 2 on right)
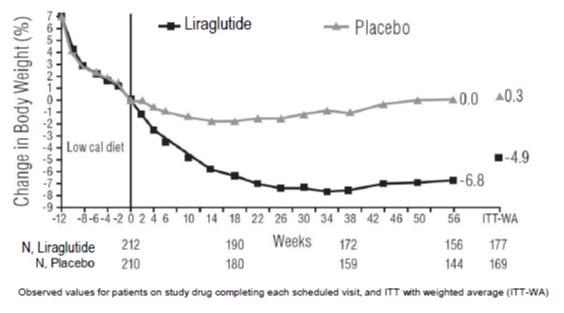
The time courses of weight loss with liraglutide and placebo from baseline through week 56 are depicted in Figure 3 and Figure 4.
Figure 3. Change from baseline (%) in body weight (Study 1 on left and Study 2 on right)
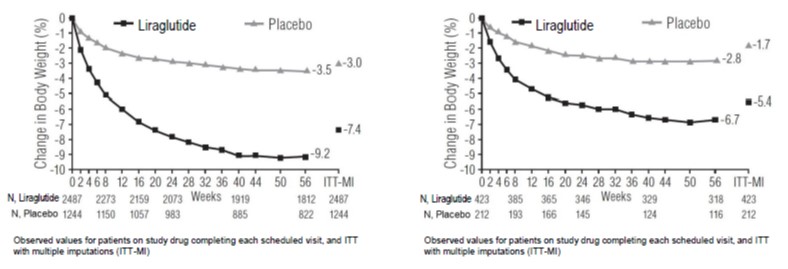
Figure 4. Change from baseline (%) in body weight during Study 3
Effect of Liraglutide on Body Weight in a 160-week Trial (Study 1, Subset of Patients with Abnormal Blood Glucose at Randomization)
The numbers and percentages of patients known to have lost greater than or equal to 5% body weight at week 56 and/or week 160 in Study 1 (patients with abnormal glucose at randomization only) are summarized in Table 5 for descriptive purposes.Table 5. Changes in Weight at Week 56 and Week 160 for Study 1 (Subset of Patients with Abnormal Blood Glucose at Randomization) Liraglutide
N=1,505Placebo
N=749Baseline mean body weight (SD) (kg)
107.5 (21.6)
107.9 (21.8)
Number (%) of patients known to lose greater than or equal to 5% body weight at 56 weeks
817 (56%)
182 (25%)
Number (%) of patients known to lose greater than or equal to 5% body weight at 160 weeks
424 (28%)
102 (14%)
Number (%) of patients known to lose greater than or equal to 5% body weight at both 56 weeks and 160 weeks
391 (26%)
74 (10%)
Number (%) of patients with weight assessment at 160 weeks
747 (50%)
322 (43%)
SD = Standard Deviation
Includes all randomized subjects who had a baseline body weight measurement. All available body weight data at 56 and 160 weeks are included in the analysis.Effect of Liraglutide on Anthropometry and Cardiometabolic Parameters in 56-week Trials
Changes in waist circumference and cardiometabolic parameters with liraglutide are shown in Table 6 for Study 1 (patients without diabetes mellitus) and Table 7 for Study 2 (patients with type 2 diabetes). Results from Study 3, which also enrolled patients without diabetes mellitus, were similar to Study 1.Table 6. Mean Changes in Anthropometry and Cardiometabolic Parameters in Study 1 (Patients without Diabetes) Liraglutide
N=2,487Placebo
N=1,244Baseline
Change from Baseline
(LSMean1)Baseline
Change from Baseline
(LSMean1)Liraglutide minus
Placebo
(LSMean)Waist Circumference (cm)
115
-8.2
114.5
-4
-4.2
Systolic Blood Pressure (mmHg)
123
-4.3
123.3
-1.5
-2.8
Diastolic Blood Pressure (mmHg)
78.7
-2.7
78.9
-1.8
-0.9
Heart Rate (bpm)2
71.4
2.6
71.3
0.1
2.5
HbA1c (%)
5.6
-0.3
5.6
-0.1
-0.2
Baseline
% Change from Baseline
(LSMean1)Baseline
% Change from Baseline
(LSMean1)Relative Difference of Liraglutide to Placebo
(LSMean)Total Cholesterol (mg/dL)*
193.8
-3.2
194.4
-0.9
-2.3
LDL Cholesterol (mg/dL)*
111.8
-3.1
112.3
-0.7
-2.4
HDL Cholesterol (mg/dL)*
51.4
2.3
50.9
0.5
1.9
Triglycerides (mg/dL)†
125.7
-13
128.3
-4.1
-7.1
Based on last observation carried forward method while on study drug
1 Least squares mean adjusted for treatment, country, sex, pre-diabetes status at screening, baseline BMI stratum and an interaction between pre-diabetes status at screening and BMI stratum as fixed factors, and the baseline value as covariate.
2 See Warnings and Precautions (5.5)
* Baseline value is the geometric mean
†Values are baseline median, median % change, and the Hodges-Lehmann estimate of the median treatment difference.Table 7. Mean Changes in Anthropometry and Cardiometabolic Parameters in Study 2 (Patients with Diabetes Mellitus) Liraglutide
N=423Placebo
N=212Baseline
Change from Baseline
(LSMean1)Baseline
Change from Baseline
(LSMean1)Liraglutide minus
Placebo
(LSMean)Waist Circumference (cm)
118.1
-6
117.3
-2.8
-3.2
Systolic Blood Pressure (mmHg)
128.9
-3
129.2
-0.4
-2.6
Diastolic Blood Pressure (mmHg)
79
-1
79.3
-0.6
-0.4
Heart Rate (bpm)2
74
2
74
-1.5
3.4
HbA1c (%)
7.9
-1.3
7.9
-0.4
-0.9
Baseline
% Change from Baseline
(LSMean1)Baseline
% Change from Baseline
(LSMean1)Relative Difference of Liraglutide to Placebo
(LSMean)Total Cholesterol (mg/dL)*
171
-1.4
169.4
2.4
-3.7
LDL Cholesterol (mg/dL)*
86.4
0.9
85.2
3.3
-2.3
HDL Cholesterol (mg/dL)*
45.2
4.8
45.4
1.9
2.9
Triglycerides (mg/dL)†
156.2
-14.5
155.8
-0.7
-13.5
Based on last observation carried forward method while on study drug
1 Least squares mean adjusted for treatment, country, sex, background treatment, baseline HbA1c stratum and an interaction between background treatment and HbA1c stratum as fixed factors, and the baseline value as covariate.
2 See Warnings and Precautions (5.5)
* Baseline value is the geometric mean
†Values are baseline median, median % change, and the Hodges-Lehmann estimate of the median treatment difference.14.2 Weight Management Trial in Pediatric Patients Ages 12 and Older with Obesity
Liraglutide was evaluated in a 56-week, double-blind, randomized, parallel group, placebo controlled multi-center trial in 251 pubertal pediatric patients aged 12 to 17 years, with BMI corresponding to 30 kg/m2 or greater for adults by international cut-off points1 and BMI of 95th percentile or greater for age and sex (NCT02918279). After a 12-week lifestyle run-in period, patients were randomized 1:1 to liraglutide once-daily or placebo once-daily. The liraglutide dose was titrated to 3 mg over a 4- to 8-week period based on tolerability as judged by the investigator. Escalation of the trial product was not allowed if the subject had a self-monitored plasma glucose (SMPG) <56 mg/dL or <70 mg/dL in the presence of symptoms of hypoglycemia during the week prior to or during the dose escalation visits. The proportion of patients who reached the 3 mg dose was 82.4%; for 8.8% of patients 2.4 mg was the maximum tolerated dose.
The mean age was 14.5 years: 40.6% of patients were male, 87.6% were White, 0.8% were Asian, 8% were Black or African American; 22.3% were of Hispanic or Latino ethnicity. The mean baseline body weight was 100.8 kg, and mean Body Mass Index (BMI) was 35.6 kg/m2.
The proportions of patients who discontinued study drug were 19.2% for the liraglutide-treated group and 20.6% for the placebo-treated group; 10.4% of patients treated with liraglutide and no patients treated with placebo discontinued treatment due to an adverse reaction [see Adverse Reactions (6.1)].
The primary endpoint was change in BMI SDS. At baseline, mean BMI SDS was 3.14 in the liraglutide group and 3.20 in the placebo group. At week 56, treatment with liraglutide resulted in statistically significant reduction in BMI SDS from baseline compared to placebo. The observed mean change in BMI SDS from baseline to week 56 was -0.23 in the liraglutide group and -0.00 in the placebo group. The estimated treatment difference in BMI SDS reduction from baseline between liraglutide and placebo was -0.22 with a 95% confidence interval of -0.37, -0.08; p=0.0022.
The time course of change in BMI SDS with liraglutide and placebo from baseline through week 56 are depicted in Figure 5.
Figure 5. Change from Baseline in BMI SDS
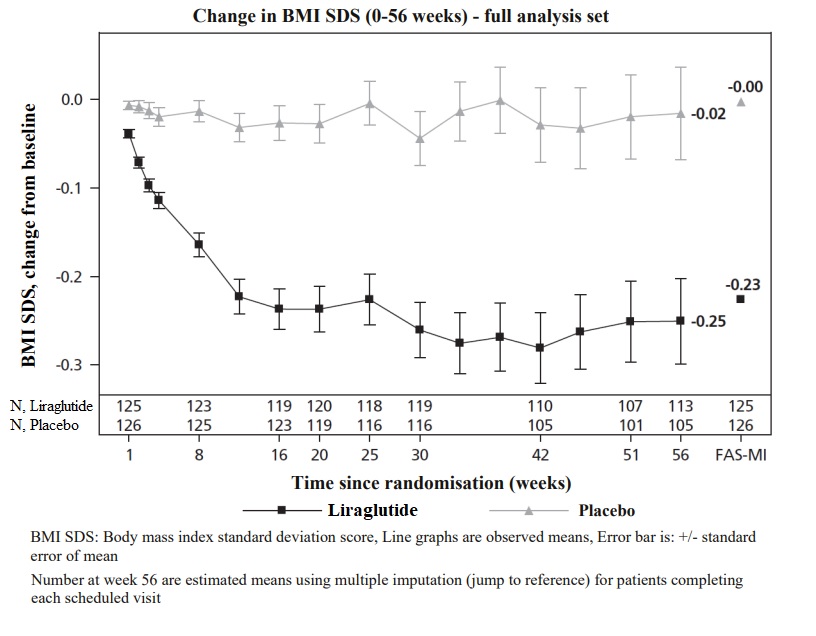
Changes in weight and BMI with liraglutide are shown in Table 8. Changes in waist circumference and cardiometabolic parameters with liraglutide are shown in Table 9.
Table 8. Changes in Weight and BMI at Week 56 for Study 4 (Pediatric Patients Ages 12 to Less than 18) Liraglutide
N=125Placebo
N=126Liraglutide minus
PlaceboBody Weight
Baseline mean Body Weight (kg)
99.3
102.2
Mean Change from Baseline (%)
-2.65
2.37
-5.01
BMI
Baseline mean BMI (kg/m2)
35.3
35.8
Mean Change from Baseline (%)
-4.29
0.35
-4.64
Proportion of patients with greater than or equal to 5% reduction in baseline BMI at week 56 (%)
43.3%
18.7%
24.6%
Proportion of patients with greater than or equal to 10% reduction in baseline BMI at week 56 (%)
26.1%
8.1%
18%
Full Analysis Set. For body weight and BMI, baseline values are means, changes from baseline at week 56 are estimated means (least-squares) and treatment contrasts at week 56 are estimated treatment differences. Missing observations were imputed from the placebo arm based on a jump to reference multiple (x100) imputation approach.
Table 9. Mean Changes in Anthropometry and Cardiometabolic Parameters in Study 4 (Pediatric Patients Ages 12 to Less than 18) Liraglutide
N=125Placebo
N=126Baseline
Change from Baseline
Baseline
Change from Baseline
Liraglutide minus
PlaceboWaist Circumference (cm)
105
-4.35
107
-1.42
-2.93
Systolic Blood Pressure (mmHg)
116
-1.21
117
0.84
-2.05
Diastolic Blood Pressure (mmHg)
72
0.77
73
-0.46
1.24
Heart Rate (bpm)*
75
1.87
78
-0.14
2.01
HbA1c (%)
5.3
-0.1
5.3
-0.03
-0.06
Baseline
% Change from Baseline
Baseline
% Change from Baseline
Relative Difference of Liraglutide to Placebo
Total Cholesterol (mg/dL)**
154.2
0.84
152.2
-0.03
0.88
LDL Cholesterol (mg/dL)**
85.5
1.74
82.5
3.01
-1.27
HDL Cholesterol (mg/dL)**
42.7
5.14
42.7
3.33
1.81
Triglycerides (mg/dL)**
109.1
-0.12
112.2
-1.35
1.23
*See Warnings and Precautions (5.5)
Full Analysis Set. Baseline values are means, changes from baseline at week 56 are estimated means (least-squares) and treatment contrasts at week 56 are estimated treatment differences. Missing observations were imputed from the placebo arm based on a jump to reference multiple (x100) imputation approach.
** Baseline values are geometric means. - 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
Liraglutide injection: 6 mg/mL clear, colorless solution in a 3 mL single-patient-use prefilled pen that delivers doses of 0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg or 3 mg is available in the following package size:
5 x liraglutide injection pen NDC: 0480-7250-46
Recommended Storage
Prior to first use, liraglutide injection should be stored in a refrigerator between 36ºF to 46ºF (2ºC to 8ºC). Do not store in the freezer or directly adjacent to the refrigerator cooling element. Do not freeze liraglutide injection and do not use liraglutide injection if it has been frozen.
After initial use of the liraglutide injection pen, the pen can be stored for 30 days at controlled room temperature 59°F to 86°F (15°C to 30°C) or in a refrigerator 36°F to 46°F (2°C to 8°C). Keep the pen cap on when not in use. Protect liraglutide injection from excessive heat and sunlight. Always remove and safely discard the needle after each injection and store the liraglutide injection pen without an injection needle attached. This will reduce the potential for contamination, infection, and leakage while also ensuring dosing accuracy.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
Instructions
Advise patients to take liraglutide injection exactly as prescribed. Instruct patients to follow the dose escalation schedule and to not take more than the recommended dose.Instruct adult patients to discontinue liraglutide injection if they have not achieved 4% weight loss by 16 weeks of treatment. Instruct pediatric patients 12 years of age and older to discontinue liraglutide injection if they have not achieved a BMI reduction of 1% from baseline after 12 weeks on the maintenance dose.
Risk of Thyroid C-cell Tumors
Inform patients that liraglutide causes benign and malignant thyroid C-cell tumors in mice and rats and that the human relevance of this finding has not been determined. Counsel patients to report symptoms of thyroid tumors (e.g., a lump in the neck, hoarseness, dysphagia or dyspnea) to their health care provider [see Boxed Warning, Warnings and Precautions (5.1)].Acute Pancreatitis
Inform patients of the potential risk for acute pancreatitis and its symptoms: severe abdominal pain that may radiate to the back, and which may or may not be accompanied by nausea or vomiting. Instruct patients to discontinue liraglutide injection promptly and contact their healthcare provider if pancreatitis is suspected [see Warnings and Precautions (5.2)].Acute Gallbladder Disease
Inform patients of the risk of acute gallbladder disease. Advise patients that substantial or rapid weight loss can increase the risk of gallbladder disease, but that gallbladder disease may also occur in the absence of substantial or rapid weight loss. Instruct patients to contact their healthcare provider for appropriate clinical follow-up if gallbladder disease is suspected [see Warnings and Precautions (5.3)].Hypoglycemia
Inform pediatric patients of the risk of hypoglycemia and educate all patients on the signs and symptoms of hypoglycemia. Inform adult patients with type 2 diabetes mellitus on an insulin secretagogue (e.g., sulfonylurea) or insulin that they may have an increased risk of hypoglycemia when using liraglutide injection and to report signs and/or symptoms of hypoglycemia to their healthcare provider [see Warnings and Precautions (5.4)].Heart Rate Increase
Inform patients to report symptoms of sustained periods of heart pounding or racing while at rest to their healthcare provider. Discontinue liraglutide injection in patients who experience a sustained increase in resting heart rate [see Warnings and Precautions (5.5)].Acute Kidney Injury Due to Volume Depletion
Inform patients of the potential risk of acute kidney injury due to dehydration associated with gastrointestinal adverse reactions. Advise patients to take precautions to avoid fluid depletion. Inform patients of the signs and symptoms of acute kidney injury and instruct them to promptly report any of these signs or symptoms or persistent (or extended) nausea, vomiting, and diarrhea to their healthcare provider [see Warnings and Precautions (5.6)].Severe Gastrointestinal Adverse Reactions
Inform patients of the potential risk of severe gastrointestinal adverse reactions. Instruct patients to contact their healthcare provider if they have severe or persistent gastrointestinal symptoms [see Warnings and Precautions (5.7)].Hypersensitivity Reactions
Inform patients that serious hypersensitivity reactions have been reported during postmarketing use of liraglutide injection. Advise patients on the symptoms of hypersensitivity reactions and instruct them to stop taking liraglutide injection and seek medical advice promptly if such symptoms occur [see Warnings and Precautions (5.8)].Suicidal Behavior and Ideation
Advise patients to report emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior. Inform patients that if they experience suicidal thoughts or behaviors, they should stop taking liraglutide injection [see Warnings and Precautions (5.9)].Pulmonary Aspiration During General Anesthesia or Deep Sedation
Inform patients that liraglutide injection may cause their stomach to empty more slowly which may lead to complications with anesthesia or deep sedation during planned surgeries or procedures. Instruct patients to inform healthcare providers prior to any planned surgeries or procedures if they are taking liraglutide injection [see Warnings and Precautions (5.10)].Never Share a Liraglutide Injection Pen Between Patients
Inform patients that they should never share a liraglutide injection pen with another person, even if the needle is changed. Sharing of the pen between patients may pose a risk of transmission of infection.Brands listed are the trademarks of their respective owners.
Manufactured In Croatia By:
Pliva Hrvatska d.o.o.
Zagreb, CroatiaManufactured For:
Teva Pharmaceuticals
Parsippany, NJ 07054Iss. 1/2026
-
MEDICATION GUIDE
MEDICATION GUIDE
Liraglutide (lir" a gloo' tide) Injection
for subcutaneous useWhat is the most important information I should know about liraglutide injection?
Serious side effects may happen in people who take liraglutide injection, including:
- Possible thyroid tumors, including cancer. Tell your healthcare provider if you get a lump or swelling in your neck, hoarseness, trouble swallowing, or shortness of breath. These may be symptoms of thyroid cancer. In studies with rats and mice, liraglutide injection and medicines that work like liraglutide injection caused thyroid tumors, including thyroid cancer. It is not known if liraglutide injection will cause thyroid tumors or a type of thyroid cancer called medullary thyroid carcinoma (MTC) in people.
- Do not use liraglutide injection if you or any of your family have ever had a type of thyroid cancer called medullary thyroid carcinoma (MTC), or if you have an endocrine system condition called Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
What is liraglutide injection?
Liraglutide injection is an injectable prescription medicine used for adults with obesity or overweight (excess weight) who also have weight related medical problems, and children aged 12 to 17 years with a body weight above 132 pounds (60 kg) and obesity to help them lose weight and keep the weight off.
- Liraglutide injection should be used with a reduced calorie diet and increased physical activity.
- Liraglutide injection is not recommended for people who also take liraglutide or other medicines called glucagon-like peptide-1 (GLP-1) receptor agonists.
- It is not known if liraglutide injection is safe and effective in children under 12 years of age.
- It is not known if liraglutide injection is safe and effective in children aged 12 to 17 years with type 2 diabetes.
Who should not use liraglutide injection?
Do not use liraglutide injection if:
- you or any of your family have ever had a type of thyroid cancer called medullary thyroid carcinoma (MTC) or if you have an endocrine system condition called Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
- you have had a serious allergic reaction to liraglutide or any of the ingredients in liraglutide injection. See the end of this Medication Guide for a complete list of ingredients in liraglutide injection. See “What are the possible side effects of liraglutide injection?” for symptoms of a serious allergic reaction.
Before taking liraglutide injection, tell your healthcare provider about all of your medical conditions, including if you:
- have or have had problems with your pancreas.
- have severe problems with your stomach, such as slowed emptying of your stomach (gastroparesis) or problems with digesting food.
- are scheduled to have surgery or other procedures that use anesthesia or deep sleepiness (deep sedation).
- have or have had depression or suicidal thoughts, or mental health issues.
- are breastfeeding or plan to breastfeed. It is not known if liraglutide passes into your breast milk. You and your healthcare provider should decide if you will use liraglutide injection or breastfeed.
Tell your healthcare provider about all the medicines you take including prescription, over-the-counter medicines, vitamins, and herbal supplements. Liraglutide injection may affect the way some medicines work and some other medicines may affect the way liraglutide injection works.
Tell your healthcare provider if you take diabetes medicines, especially insulin and sulfonylurea medicines. Talk with your healthcare provider if you are not sure if you take any of these medicines. Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I use liraglutide injection?
- Read the Instructions for Use that comes with liraglutide injection.
- Use liraglutide injection exactly as your healthcare provider tells you to.
- Your healthcare provider should show you how to use liraglutide injection before you use it for the first time.
- Use liraglutide injection with a reduced-calorie diet and increased physical activity.
- Liraglutide injection is injected under the skin (subcutaneously) in your stomach area (abdomen), upper leg (thigh), or upper arm. Do not inject into a muscle (intramuscularly) or vein (intravenously).
- Liraglutide injection is injected 1 time each day, at any time during the day.
- Start liraglutide injection with 0.6 mg per day in your first week. In your second week, increase your daily dose to 1.2 mg. In the third week, increase your daily dose to 1.8 mg. In the fourth week, increase your daily dose to 2.4 mg and in the fifth week onwards, increase your daily dose to the full dose of 3 mg. After that, do not change your dose unless your healthcare provider tells you to. Children may reduce their dose to 2.4 mg daily if the maximum dose is not tolerated.
- If you miss your daily dose of liraglutide injection, just take your next daily dose as usual on the following day. Do not take an extra dose of liraglutide injection or increase your dose on the following day to make up for your missed dose. If you miss your dose of liraglutide injection for 3 days or more, call your healthcare provider to talk about how to restart your treatment.
- Liraglutide injection may be taken with or without food.
- Change (rotate) your injection site with each injection. Do not use the same site for each injection.
- Do not share your liraglutide injection pen with other people, even if the needle has been changed. You may give other people a serious infection or get a serious infection from them.
- If you take too much liraglutide injection, call your healthcare provider or Poison Help line at 1-800-222-1222 or go to the nearest hospital emergency room right away.
- Throw away the used liraglutide injection pen after 30 days.
What are the possible side effects of liraglutide injection?
Liraglutide injection may cause serious side effects, including:
- See “What is the most important information I should know about liraglutide injection?”
- inflammation of the pancreas (pancreatitis). Stop using liraglutide injection and call your healthcare provider right away if you have severe pain in your stomach area (abdomen) that will not go away, with or without vomiting. You may feel the pain from your stomach area (abdomen) to your back.
- increased risk of low blood sugar (hypoglycemia) in adults with type 2 diabetes, especially those who also take medicines to treat type 2 diabetes mellitus such as an insulin or a sulfonylureas and in children who are 12 years of age and older without type 2 diabetes mellitus. Low blood sugar in patients with adults with type 2 diabetes and in children without type 2 diabetes mellitus who receive liraglutide injection can be both a serious and common side effect. Talk to your healthcare provider about how to recognize and treat low blood sugar. You should check your blood sugar before you start taking liraglutide injection and while you take liraglutide injection.
Signs and symptoms of low blood sugar may include:
- dizziness or light-headedness
- sweating
- confusion or drowsiness
- headache
- blurred vision
- slurred speech
- shakiness
- fast heartbeat
- anxiety, irritability, or mood changes
- hunger
- weakness
- feeling jittery
Talk to your healthcare provider about how to recognize and treat low blood sugar. You should check your blood sugar before you start taking liraglutide injection and while you take liraglutide injection.
- increased heart rate. Liraglutide injection can increase your heart rate while you are at rest. Your healthcare provider should check your heart rate while you take liraglutide injection. Tell your healthcare provider if you feel your heart racing or pounding in your chest and it lasts for several minutes.
- dehydration leading to kidney problems. Diarrhea, nausea, and vomiting may cause a loss of fluids (dehydration) which may cause kidney problems. It is important for you to drink fluids to help reduce your chance of dehydration. Tell your healthcare provider right away if you have nausea, vomiting, or diarrhea that does not go away.
- severe stomach problems. Stomach problems, sometimes severe, have been reported in people who use liraglutide injection. Tell your healthcare provider if you have stomach problems that are severe or will not go away.
-
serious allergic reactions. Stop using liraglutide injection, and get medical help right away if you have any symptoms of a serious allergic reaction including:
- swelling of your face, lips, tongue, or throat
- problems breathing or swallowing
- severe rash or itching
- fainting or feeling dizzy
- very rapid heartbeat
-
gallbladder problems. Liraglutide injection may cause gallbladder problems including gallstones. Some gallbladder problems need surgery. Call your healthcare provider if you have any of the following symptoms:
- pain in your upper stomach (abdomen)
- fever
- yellowing of your skin or eyes (jaundice)
- clay-colored stools
- depression or thoughts of suicide. You should pay attention to any mental changes, especially sudden changes, in your mood, behaviors, thoughts, or feelings. Call your healthcare provider right away if you have any mental changes that are new, worse, or worry you.
- food or liquid getting into the lungs during surgery or other procedures that use anesthesia or deep sleepiness (deep sedation). Liraglutide injection may increase the chance of food getting into your lungs during surgery or other procedures. Tell all your healthcare providers that you are taking liraglutide injection before you are scheduled to have surgery or other procedures.
The most common side effects of liraglutide injection in adults include:
- nausea
- diarrhea
- constipation
- vomiting
- injection site reaction
- low blood sugar (hypoglycemia)
- headache
- upset stomach (dyspepsia)
- tiredness (fatigue)
- dizziness
- stomach pain
- change in enzyme (lipase) levels in your blood
Additional common side effects in children are fever and gastroenteritis
Talk to your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of liraglutide injection. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Keep your liraglutide injection pen, pen needles, and all medicines out of the reach of children.
General information about the safe and effective use of liraglutide injection.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use liraglutide injection for a condition for which it was not prescribed. Do not give liraglutide injection to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about liraglutide injection that is written for health professionals.
What are the ingredients in liraglutide injection?
Active ingredient: liraglutide
Inactive ingredients: hydrochloric acid, phenol, propylene glycol, sodium hydroxide, sodium phosphate dibasic dihydrate, and water for injection
Brands listed are the trademarks of their respective owners.
Manufactured In Croatia By: Pliva Hrvatska, d.o.o., Zagreb, Croatia
For more information call Teva at 1-888-838-2872.
Manufactured For: Teva Pharmaceuticals, Parsippany, NJ 07054This Medication Guide has been approved by the U.S. Food and Drug Administration. Iss. 5/2025
-
INSTRUCTIONS FOR USE
INSTRUCTIONS FOR USE
Liraglutide (lir" a gloo' tide) Injection- Read these instructions carefully before using your liraglutide injection pen.
- Do not use your pen without proper training from your healthcare provider. Make sure that you know how to give yourself an injection with the pen before you start your treatment.
 If you are blind or have poor eyesight and cannot read the dose counter on the pen, do not use this pen without help. Get help from a person with good eyesight who is trained to use the liraglutide injection pen.
If you are blind or have poor eyesight and cannot read the dose counter on the pen, do not use this pen without help. Get help from a person with good eyesight who is trained to use the liraglutide injection pen.
- Start by checking your pen to make sure that it contains liraglutide injection, then look at the pictures below to get to know the different parts of your pen and needle.
- Your pen is a prefilled, dial-a-dose, single-patient-use pen. It contains 18 mg of liraglutide, and you can select doses of 0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg and 3 mg. Your pen is compatible with universal fit disposable pen needles up to a length of 8 mm, including NovoFine®. Compatible needles will state ISO11608-2 on the outer packaging. Your pen is not compatible with NovoTwist® disposable needles. Pen needles are not included with your liraglutide injection pen.
Liraglutide injection pen and needle (example)
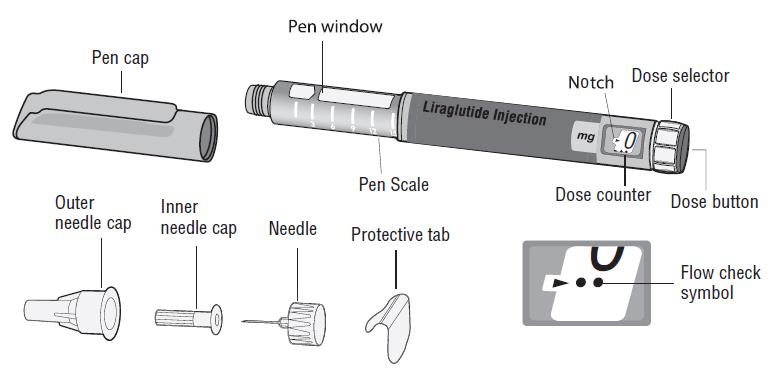
Step 1. Prepare your pen with a new needle
- Wash your hands with soap and water.
- Check the name and colored label of your pen, to make sure that it contains liraglutide injection. This is especially important if you take more than 1 type of medicine.
- Pull off the pen cap.
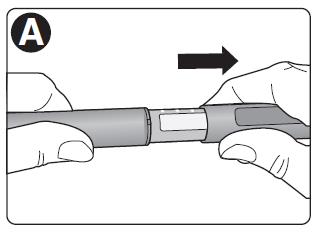
-
Check that liraglutide injection in your pen is clear and colorless.
Look through the pen window. If liraglutide injection looks cloudy, do not use the pen.
- Take a new needle, and tear off the paper tab.
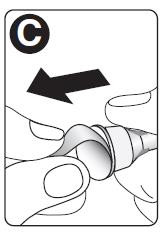
- Push the needle straight onto the pen. Turn until it is on tight.
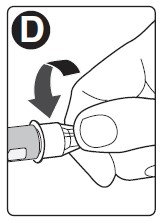
- Pull off the outer needle cap. Do not throw it away.
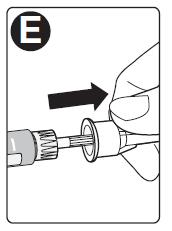
-
Pull off the inner needle cap and throw it away.
A drop of liraglutide injection may appear at the needle tip. This is normal, but you must still check the liraglutide injection flow, if you use a new pen for the first time.
 Always use a new needle for each injection. This will prevent contamination, infection, leakage of liraglutide injection, and blocked needles leading to the wrong dose. Never use a bent or damaged needle.
Always use a new needle for each injection. This will prevent contamination, infection, leakage of liraglutide injection, and blocked needles leading to the wrong dose. Never use a bent or damaged needle.
 Do not attach a new needle to your pen until you are ready to take your injection.
Do not attach a new needle to your pen until you are ready to take your injection.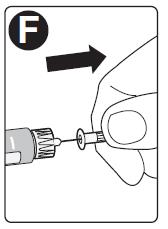
Step 2. Check the liraglutide injection flow with each new pen.
- Check the liraglutide injection flow before your first injection with each new pen.
If your liraglutide injection pen is already in use, go to Step 3 “Select your dose”. - Turn the dose selector until the dose counter shows the flow check symbol
( ).
).
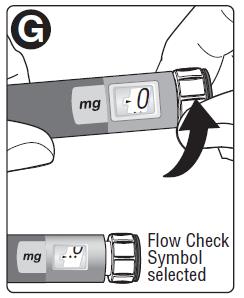
- Hold the pen with the needle pointing up.
Press and push in the dose button until the dose counter shows 0. The black arrow indicating 0 must appear in the notch.
A drop of liraglutide injection will appear at the needle tip. -
If no drop appears, repeat Step 2 above as shown in Figures G and H up to 6 times. If there is still no drop, change the needle and repeat Step 2 as shown in Figures G and H 1 more time.
Do not use the pen if a drop of liraglutide injection still does not appear. Contact Teva at 1-888-838-2872.
 Always make sure that a drop appears at the needle tip before you use a new pen for the first time. This makes sure that liraglutide injection flows.
Always make sure that a drop appears at the needle tip before you use a new pen for the first time. This makes sure that liraglutide injection flows.
If no drop appears, you will not inject any liraglutide injection, even though the dose counter may move. This may mean that there is a blocked or damaged needle. A small drop may remain at the needle tip, but it will not be injected.
A small drop may remain at the needle tip, but it will not be injected.
Only check the liraglutide injection flow before your first injection with each new pen.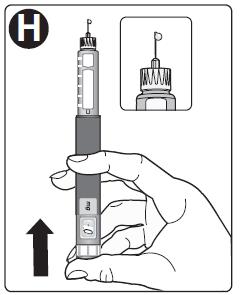
Step 3. Select your dose
-
Turn the dose selector until the dose counter shows your dose (0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg or 3 mg).
Make sure you know the dose of liraglutide injection you should use.
If you select the wrong dose, you can turn the dose selector forward or backwards to the correct dose.
 Always use the dose counter and the black arrow in the notch to see how many mg you select.
Always use the dose counter and the black arrow in the notch to see how many mg you select.
You will hear a “click” every time you turn the dose selector and it will extend from the pen body as the dose increases.
Do not set the dose by counting the number of clicks you hear.
Do not use the pen scale to set the dose. It does not show exactly how much liraglutide injection is left in your pen.
Only doses of 0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg or 3 mg can be selected with the dose selector. The black arrow indicating the selected dose must appear in the notch to make sure that you get a correct dose. The dose selector changes the dose. Only the dose counter and black arrow in the notch will show how many mg you select for each dose.
The dose selector changes the dose. Only the dose counter and black arrow in the notch will show how many mg you select for each dose.
You can select up to 3 mg each dose. When your pen contains less than 3 mg the dose counter stops before 3 mg is shown.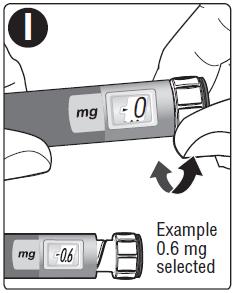
 How much liraglutide injection is left?
How much liraglutide injection is left?
- The pen scale shows you about how much liraglutide injection is left in your pen.
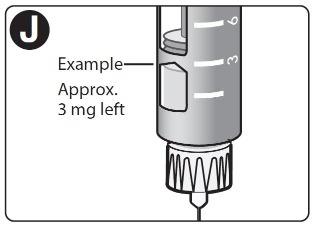
-
To see how much liraglutide injection is left, use the dose counter:
Turn the dose selector until the dose counter stops.
If it shows 3 mg, at least 3 mg are left in your pen. If the dose counter stops before 3 mg, there is not enough liraglutide injection left for a full dose of 3 mg.
 If you need more liraglutide injection than what is left in your pen
If you need more liraglutide injection than what is left in your pen
Only if trained or told by your healthcare provider, you may split your dose between your current pen and a new pen. Use a calculator to plan the doses as instructed by your healthcare provider. Be very careful to calculate correctly.
Be very careful to calculate correctly.
If you are not sure how to split your dose using 2 pens, then select and inject the dose you need with a new pen.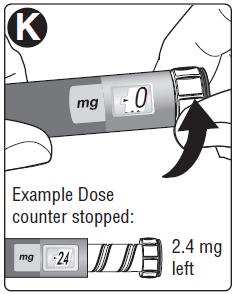
Step 4. Inject your dose
- Insert the needle into your skin as your healthcare provider has shown you.
- Make sure you can see the dose counter. Do not cover it with your fingers. This could stop the injection.
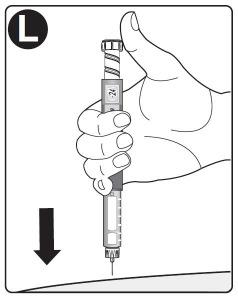
- Press and push down the dose button until the dose counter shows 0. The dose selector will retract into the body of the pen and will stop when the dose counter shows 0. The black arrow indicating 0 must appear in the notch.

- Keep the needle in your skin after the dose counter has returned to 0 and count slowly to 6.
- If the needle is removed earlier, you may see a stream of liraglutide injection coming from the needle tip. If this happens, the full dose will not be delivered.

-
Remove the needle from your skin.
If blood appears at the injection site, press lightly. Do not rub the area.
 Always watch the dose counter to know how many mg you inject. Push the dose button down until the dose counter shows 0.
Always watch the dose counter to know how many mg you inject. Push the dose button down until the dose counter shows 0.
How to identify a blocked or damaged needle?-
If 0 does not appear in the dose counter after continuously pressing the dose button, you may have used a blocked or damaged needle.
-
If this happens you have not received any liraglutide injection even though the dose counter has moved from the original dose that you have set.
How to handle a blocked needle?
Change the needle as described in Step 5, and repeat all steps starting with Step 1: “Prepare your pen with a new needle”.
Make sure you select the full dose you need.
Never touch the dose counter when you inject. This can stop the injection. You may see a drop of liraglutide injection at the needle tip after injecting. This is normal and does not affect your dose.
You may see a drop of liraglutide injection at the needle tip after injecting. This is normal and does not affect your dose.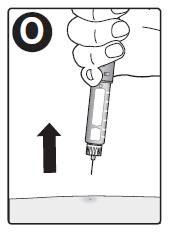
Step 5. After your injection
- Carefully remove the needle from the pen. Do not put the needle caps back on the needle, to avoid needle sticks.
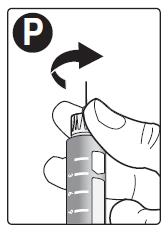
- Place the needle in a sharps container right away to reduce the risk of needle sticks.

- Put the pen cap on your pen after each use to protect liraglutide injection from light.
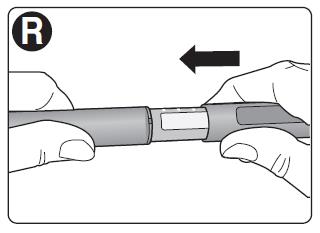
 If you do not have a sharps container, follow a 1-handed needle recapping method. Carefully slip the needle into the outer needle cap. Dispose of the needle in a sharps container as soon as possible.
If you do not have a sharps container, follow a 1-handed needle recapping method. Carefully slip the needle into the outer needle cap. Dispose of the needle in a sharps container as soon as possible. Never try to put the inner needle cap back on the needle. You may stick yourself with the needle.
Never try to put the inner needle cap back on the needle. You may stick yourself with the needle.
Always remove the needle from your pen.
This prevents contamination, infection, leakage of liraglutide injection, and blocked needles leading to the wrong dose. If the needle is blocked, you will not inject any liraglutide injection. Always dispose of the needle after each injection.
Always dispose of the needle after each injection. - Do not throw away in the household trash. Put the needle and any empty liraglutide injection pen or any pen used for 30 days still containing liraglutide injection in a FDA-cleared sharps disposal container right away after use.
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- made of a heavy-duty plastic
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out upright and stable during use
- leak-resistant
- properly labeled to warn of hazardous waste inside the container
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about the safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA’s website at: http://www.fda.gov/safesharpsdisposal
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
- Safely dispose of liraglutide injection that is out of date or no longer needed.
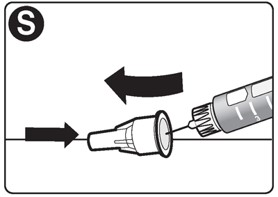
 Important
Important
- Caregivers must be very careful when handling used needles to prevent needle sticks and cross infection.
- Never use a syringe to withdraw liraglutide injection from your pen.
- Always carry an extra pen and new needles with you, in case of loss or damage.
- Always keep your pen and needles out of reach of others, especially children.
- Do not share your liraglutide injection pen or needles with anyone else. You may give an infection to them or get an infection from them.
- Always keep your pen with you. Do not leave it in a car or other place where it can get too hot or too cold.
Caring for your pen
- Do not drop your pen or knock it against hard surfaces. If you drop it or suspect a problem, attach a new needle and check the liraglutide injection flow before you inject.
- Do not try to repair your pen or pull it apart.
- Do not expose your pen to dust, dirt or liquid.
- Do not wash, soak, or lubricate your pen. If necessary, clean it with mild detergent on a moistened cloth.
How should I store my liraglutide injection pen?
- Store your new, unused liraglutide injection pens in the refrigerator at 36°F to 46°F (2°C to 8°C).
- Store your pen in use for 30 days at 59ºF to 86ºF (15ºC to 30ºC) or in a refrigerator at 36°F to 46°F (2°C to 8°C).
- The liraglutide injection pen you are using should be thrown away after 30 days, even if it still has liraglutide injection left in it.
- Do not freeze liraglutide injection. Do not use liraglutide injection if it has been frozen.
- Unused liraglutide injection pens may be used until the expiration date printed on the label, if kept in the refrigerator.
- Keep liraglutide injection away from heat and out of the light.
This Medication Guide and Instructions for Use have been approved by the U.S. Food and Drug Administration.
Brands listed are the trademarks of their respective owners.
Manufactured In Croatia By:
Pliva Hrvatska d.o.o.
Zagreb, CroatiaManufactured For:
Teva Pharmaceuticals
Parsippany, NJ 07054Iss. 5/2025
-
PRINCIPAL DISPLAY PANEL
NDC: 0480-7250-46
Liraglutide Injection
18 mg/3 mL
(6 mg/mL)
Single Patient Use Only
Discard pen 30 days after first use
REFRIGERATE – DO NOT FREEZE
For Subcutaneous Use Only
Compatible with universal fit disposable pen needles (e.g. NovoFine®)
Protect from light.
PHARMACIST: Dispense the accompanying Medication Guide to each patient.
Rx only
5 x 3 mL Prefilled Pens
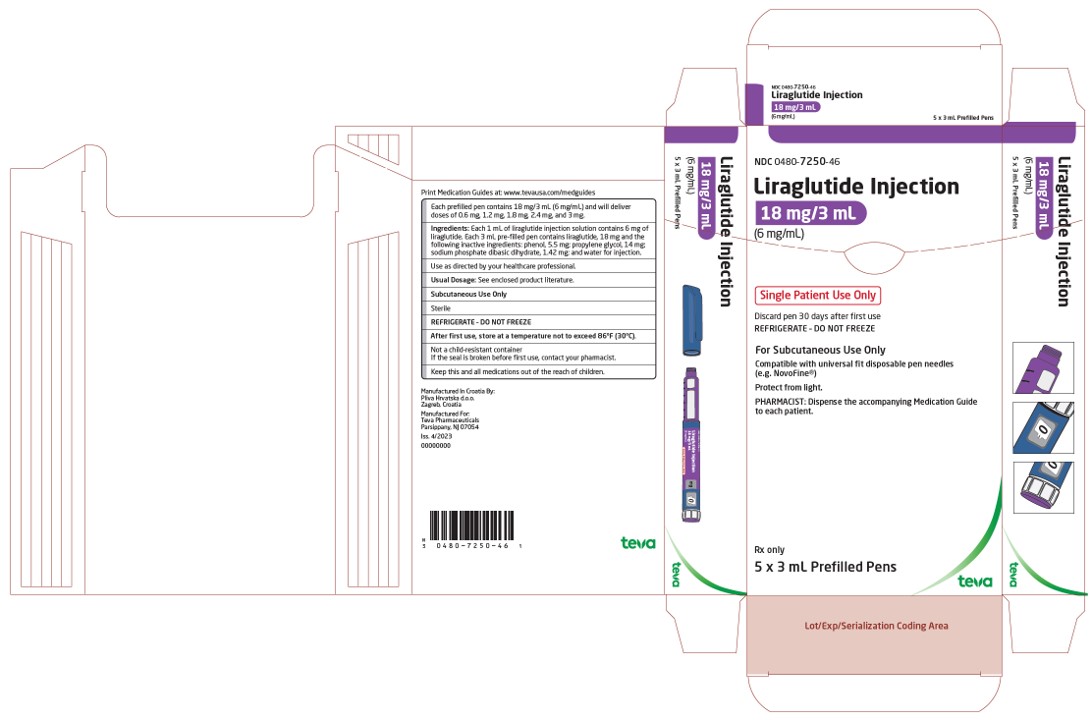
-
INGREDIENTS AND APPEARANCE
LIRAGLUTIDE
liraglutide injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0480-7250 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LIRAGLUTIDE (UNII: 839I73S42A) (LIRAGLUTIDE - UNII:839I73S42A) LIRAGLUTIDE 6 mg in 1 mL Inactive Ingredients Ingredient Name Strength PHENOL (UNII: 339NCG44TV) 5.5 mg in 1 mL PROPYLENE GLYCOL (UNII: 6DC9Q167V3) 14 mg in 1 mL SODIUM PHOSPHATE, DIBASIC, DIHYDRATE (UNII: 94255I6E2T) 1.42 mg in 1 mL WATER (UNII: 059QF0KO0R) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0480-7250-46 5 in 1 CARTON 08/28/2025 1 3 mL in 1 SYRINGE, PLASTIC; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA214568 08/28/2025 Labeler - Teva Pharmaceuticals, Inc. (022629579)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.