SEROSTIM- somatropin kit
Serostim by
Drug Labeling and Warnings
Serostim by is a Prescription medication manufactured, distributed, or labeled by EMD Serono, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use SEROSTIM® safely and effectively. See full prescribing information for SEROSTIM.
SEROSTIM (somatropin) for injection, for subcutaneous use
Initial U.S. Approval: 1987INDICATIONS AND USAGE
SEROSTIM is indicated for the treatment of HIV patients with wasting or cachexia to increase lean body mass and body weight, and improve physical endurance (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
- Single-dose administration (to be administered with Sterile Water for Injection) (3):
- SEROSTIM 5 mg/ vial
- SEROSTIM 6 mg/ vial
- Multi-dose administration (to be administered with Bacteriostatic Water for Injection):
- SEROSTIM 4 mg/ vial
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Acute Critical Illness: Increased mortality in patients with acute critical illness following open heart surgery, abdominal surgery or multiple accidental trauma, or those with acute respiratory failure has been reported after treatment with pharmacologic amounts of somatropin (5.1)
- Concomitant Antiretroviral Therapy: In vitro experimental systems have demonstrated the potential to potentiate HIV replication. No significant somatropin-associated increase in viral load was observed in clinical trials. HIV patients should be maintained on antiretroviral therapy for the duration of SEROSTIM treatment (5.2)
- Neoplasms: Monitor all patients with a history of any neoplasm routinely while on somatropin therapy for progression, recurrences, or development of a tumor (5.3)
- Impaired Glucose Tolerance/Diabetes: May be unmasked. Periodically monitor glucose levels. Dose adjustment of concurrent antihyperglycemic drugs in diabetics may be required (5.4)
- Intracranial Hypertension: Exclude preexisting papilledema. May develop and is usually reversible after discontinuation or dose reduction (5.5)
- Hypersensitivity: Serious hypersensitivity reactions may occur. In the event of an allergic reaction, seek prompt medical attention (5.6)
- Fluid Retention (edema, arthralgia)/Carpal Tunnel Syndrome: May occur frequently. Reduce dose as necessary (5.7)
- Pancreatitis: Consider pancreatitis in patients with persistent severe abdominal pain (5.9)
ADVERSE REACTIONS
Most common adverse reactions include (incidence >10%) tissue turgor (edema, myalgia, hypoesthesia) and musculoskeletal discomfort (arthralgia, pain in extremities) (6)
To report SUSPECTED ADVERSE REACTIONS, contact EMD Serono at 1-800-283-8088 ext 5563 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
DRUG INTERACTIONS
- Inhibition of 11β-Hydroxysteroid Dehydrogenase Type 1: May require the initiation of glucocorticoid replacement therapy. Patients treated with glucocorticoid replacement for previously diagnosed hypoadrenalism may require an increase in their maintenance doses (7.1)
- Cytochrome P450-Metabolized Drugs: Monitor carefully if used with somatropin (7.2)
- Oral Estrogen: Larger doses of somatropin may be required in women (7.3)
- Insulin and/or Oral/Injectable Hypoglycemic Agents: May require adjustment (7.4)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 6/2019
- Single-dose administration (to be administered with Sterile Water for Injection) (3):
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 HIV-associated wasting or cachexia
2.2 Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Acute Critical Illness
5.2 Concomitant Antiretroviral Therapy
5.3 Neoplasms
5.4 Impaired Glucose Tolerance/Diabetes
5.5 Intracranial Hypertension
5.6 Severe Hypersensitivity
5.7 Fluid Retention/Carpal Tunnel Syndrome
5.8 Lipoatrophy
5.9 Pancreatitis
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-Marketing Experience
7 DRUG INTERACTIONS
7.1 11β-Hydroxysteroid Dehydrogenase Type 1
7.2 Cytochrome P450-metabolized drugs
7.3 Oral Estrogen
7.4 Insulin and/or Other Oral/Injectable Hypoglycemic Agents
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Women
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
8.8 Gender Effect
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
SEROSTIM is administered by subcutaneous injection.
SEROSTIM therapy should be carried out under the regular guidance of a physician who is experienced in the diagnosis and management of HIV infection.
2.1 HIV-associated wasting or cachexia
The usual starting dose of SEROSTIM is 0.1 mg/kg subcutaneously once daily (up to a total dose of 6 mg). SEROSTIM should be administered subcutaneously once daily at bedtime according to the following body weight-based dosage recommendations:
Weight Range Dose - * Based on an approximate daily dosage of 0.1 mg/kg.
>55kg (>121 lb) 6 mg* SC daily 45-55 kg (99-121 lb) 5 mg* SC daily 35-45 kg (75-99 lb) 4 mg* SC daily <35 kg (<75 lb) 0.1 mg/kg SC daily Treatment with SEROSTIM 0.1 mg/kg every other day was associated with fewer side effects, and resulted in a similar improvement in work output, as compared with SEROSTIM 0.1 mg/kg daily. Therefore, a starting dose of SEROSTIM 0.1 mg/kg every other day should be considered in patients at increased risk for adverse effects related to recombinant human growth hormone therapy (i.e., glucose intolerance). In general, dose reductions (i.e., reducing the total daily dose or the number of doses per week) should be considered for side effects potentially related to recombinant human growth hormone therapy.
Most of the effect of SEROSTIM on work output and lean body mass was apparent after 12 weeks of treatment. The effect was maintained during an additional 12 weeks of therapy. There are no safety or efficacy data available from controlled studies in which patients were treated with SEROSTIM continuously for more than 48 weeks. There are no safety or efficacy data available from trials in which patients with HIV wasting or cachexia were treated intermittently with SEROSTIM.
2.2 Preparation and Administration
Each vial of SEROSTIM 5 mg or 6 mg is reconstituted with 0.5 to 1 mL Sterile Water for Injection, USP.
Each vial of SEROSTIM 4 mg is reconstituted in 0.5 to 1 mL of Bacteriostatic Water for Injection, USP (0.9% Benzyl Alcohol preserved). For patients sensitive to Benzyl Alcohol, SEROSTIM may be reconstituted with Sterile Water for Injection, USP [see Pediatric Use (8.4)].
When SEROSTIM is reconstituted with Sterile Water for Injection, USP, the reconstituted solution should be used immediately and any unused portion should be discarded.
When SEROSTIM is reconstituted with Bacteriostatic Water for Injection, USP (0.9% Benzyl Alcohol preserved) the reconstituted solution may be refrigerated (2-8°C/36-46°F) for up to 14 days.
Approximately 10% mechanical loss can be associated with reconstitution and administration from multi-dose vials.
To reconstitute SEROSTIM, inject the diluent into the vial of SEROSTIM aiming the liquid against the glass vial wall. Swirl the vial with a GENTLE rotary motion until contents are dissolved completely. DO NOT SHAKE. Parenteral drug products should always be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. SEROSTIM MUST NOT BE INJECTED if the solution is cloudy or contains particulate matter. Use it only if it is clear and colorless.
SEROSTIM can be administered using (1) a standard sterile, disposable syringe and needle, (2) a compatible SEROSTIM needle-free injection device or (3) a compatible SEROSTIM needle injection device. For proper use, refer to the Instructions for Use provided with the administration device.
Injection sites, which may be located on the thigh, upper arm, abdomen or buttock, should be rotated to avoid local irritation.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
-
Acute Critical Illness
Growth hormone therapy should not be initiated in patients with acute critical illness due to complications following open heart or abdominal surgery, multiple accidental trauma or acute respiratory failure [see Warnings and Precautions (5.1)]. -
Active Malignancy
In general, somatropin is contraindicated in the presence of active malignancy. Any preexisting malignancy should be inactive and its treatment complete prior to instituting therapy with somatropin. Somatropin should be discontinued if there is evidence of recurrent activity [see Warnings and Precautions (5.3)]. -
Hypersensitivity
SEROSTIM is contraindicated in patients with a known hypersensitivity to somatropin or any of its excipients. Systemic hypersensitivity reactions have been reported with postmarketing use of somatropin products [see Warnings and Precautions (5.6)]. -
Diabetic Retinopathy
Somatropin is contraindicated in patients with active proliferative or severe non-proliferative diabetic retinopathy.
-
Acute Critical Illness
-
5 WARNINGS AND PRECAUTIONS
5.1 Acute Critical Illness
Increased mortality in patients with acute critical illness due to complications following open heart surgery, abdominal surgery or multiple accidental trauma, or those with acute respiratory failure has been reported after treatment with pharmacologic amounts of somatropin. Two placebo-controlled clinical trials in non-growth hormone deficient adult patients (n=522) with these conditions revealed a significant increase in mortality (42% vs. 19%) among somatropin-treated patients (doses 5.3-8 mg/day) compared to those receiving placebo [see Contraindications (4)].
5.2 Concomitant Antiretroviral Therapy
In some experimental systems, somatropin has been shown to potentiate HIV replication in vitro at concentrations ranging from 50-250 ng/mL. There was no increase in virus production when the antiretroviral agents, zidovudine, didanosine or lamivudine were added to the culture medium. Additional in vitro studies have shown that somatropin does not interfere with the antiviral activity of zalcitabine or stavudine. In the controlled clinical trials, no significant somatropin-associated increase in viral burden was observed. However, the protocol required all participants to be on concomitant antiretroviral therapy for the duration of the study. In view of the potential for acceleration of virus replication, it is recommended that HIV patients be maintained on antiretroviral therapy for the duration of SEROSTIM treatment.
5.3 Neoplasms
Because malignancies are more common in HIV positive individuals, the risks and benefits of starting somatropin in HIV positive patients should be carefully considered before initiating SEROSTIM treatment and patients should be monitored carefully for the development of neoplasms if treatment with somatropin is initiated.
Monitor all patients with a history of any neoplasm routinely while on somatropin therapy for progression or recurrence of the tumor [see Contraindications (4)].
Monitor patients on somatropin therapy carefully for increased growth, or potential malignant changes of preexisting nevi.
5.4 Impaired Glucose Tolerance/Diabetes
Hyperglycemia may occur in HIV infected individuals due to a variety of reasons. In wasting patients, treatment with SEROSTIM 0.1 mg/kg daily and 0.1 mg/kg every other day for 12 weeks was associated with approximately 10 mg/dL and 6 mg/dL increases in mean fasting blood glucose concentrations, respectively. The increases occurred early in treatment. Patients with other risk factors for glucose intolerance should be monitored closely during SEROSTIM therapy.
During safety surveillance of patients with HIV-associated wasting, cases of new onset impaired glucose tolerance, new onset type 2 diabetes mellitus and exacerbation of preexisting diabetes mellitus have been reported in patients receiving SEROSTIM. Some patients developed diabetic ketoacidosis and diabetic coma. In some patients, these conditions improved when SEROSTIM was discontinued, while in others, the glucose intolerance persisted. Some of these patients required initiation or adjustment of antidiabetic treatment while on SEROSTIM.
In clinical trials of SEROSTIM conducted in HIV patients with lipodystrophy (an unapproved indication), evidence of dose-dependent glucose intolerance and related adverse reaction was observed at doses of 4 mg SEROSTIM daily and 4 mg SEROSTIM every other day for 12 weeks [see Adverse Reactions (6.1)].
5.5 Intracranial Hypertension
Intracranial hypertension (IH) with papilledema, visual changes, headache, nausea, and/or vomiting has been reported in a small number of patients treated with somatropin products. Symptoms usually occurred within the first eight (8) weeks after the initiation of somatropin therapy. In all reported cases, IH-associated signs and symptoms rapidly resolved after cessation of therapy or a reduction of the somatropin dose. Funduscopic examination should be performed routinely before initiating treatment with somatropin to exclude preexisting papilledema, and periodically during the course of somatropin therapy. If papilledema is observed by funduscopy during somatropin treatment, treatment should be stopped. If somatropin-induced IH is diagnosed, treatment with somatropin can be restarted at a lower dose after IH-associated signs and symptoms have resolved.
5.6 Severe Hypersensitivity
Serious systemic hypersensitivity reactions including anaphylactic reactions and angioedema have been reported with postmarketing use of somatropin products. Patients and caregivers should be informed that such reactions are possible and that prompt medical attention should be sought if an allergic reaction occurs [see Contraindications (4)].
5.7 Fluid Retention/Carpal Tunnel Syndrome
Increased tissue turgor (swelling, particularly in the hands and feet) and musculoskeletal discomfort (pain, swelling and/or stiffness) may occur during treatment with SEROSTIM, but may resolve spontaneously, with analgesic therapy, or after reducing the frequency of dosing [see Dosage and Administration (2.1)].
Carpal tunnel syndrome may occur during treatment with SEROSTIM. If the symptoms of carpal tunnel syndrome do not resolve by decreasing the weekly number of doses of SEROSTIM, it is recommended that treatment be discontinued.
5.8 Lipoatrophy
When somatropin is administered subcutaneously at the same site over a long period of time, tissue atrophy may result. This can be avoided by rotating the injection site [see Dosage and Administration (2.2)].
5.9 Pancreatitis
Cases of pancreatitis have been reported rarely in children and adults receiving somatropin treatment, with some evidence supporting a greater risk in children compared with adults. Published literature indicates that girls who have Turner syndrome may be at greater risk than other somatropin-treated children. Pancreatitis should be considered in any somatropin-treated patient, especially a child who develops abdominal pain.
-
6 ADVERSE REACTIONS
The following important adverse reactions are also described elsewhere in the labeling:
Acute Critical Illness [see Warnings and Precautions (5.1)]
Neoplasms [see Warnings and Precautions (5.3)]
Impaired glucose tolerance and diabetes mellitus [see Warnings and Precautions (5.4)]
Intracranial hypertension [see Warnings and Precautions (5.5)]
Severe hypersensitivity [see Warnings and Precautions (5.6)]
Fluid retention/Carpal tunnel syndrome [see Warnings and Precautions (5.7)]
Lipoatrophy [see Warnings and Precautions (5.8)]
Pancreatitis [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Clinical trials in HIV-associated wasting or cachexia:
In the 12-week, placebo-controlled Clinical Trial 2, 510 patients were treated with SEROSTIM. The most common adverse reactions judged to be associated with SEROSTIM were musculoskeletal discomfort and increased tissue turgor (swelling, particularly of the hands or feet), and were more frequently observed when SEROSTIM 0.1 mg/kg was administered on a daily basis [Table 1 and Warnings and Precautions (5)]. These symptoms often subsided with continued treatment or dose reduction. Approximately 23% of patients receiving SEROSTIM 0.1 mg/kg daily and 11% of patients receiving 0.1 mg/kg every other day required dose reductions. Discontinuations as a result of adverse reactions occurred in 10.3% of patients receiving SEROSTIM 0.1 mg/kg daily and 6.6% of patients receiving 0.1 mg/kg every other day. The most common reasons for dose reduction and/or drug discontinuation were arthralgia, myalgia, edema, carpal tunnel syndrome, elevated glucose levels, and elevated triglyceride levels.
Clinical adverse reactions which occurred during the first 12 weeks of study in at least 5% of the patients in either active treatment group and at an incidence greater than placebo are listed below, without regard to causality assessment.
Table 1: Controlled Clinical Trial 2 Adverse Reactions Occurring in at least 5% of Patients in one of the Treatment Groups, and at an Incidence Greater than Placebo Placebo 0.1 mg/kg every other day
SEROSTIM0.1 mg/kg daily
SEROSTIMPatients
(n=247)Patients
(n=257)Patients
(n=253)Body System
Preferred Term% % % Musculoskeletal System Disorders Arthralgia 11.3 24.5 36.4 Myalgia 11.7 17.9 30.4 Arthrosis 3.6 7.8 10.7 Gastrointestinal System Disorders Nausea 4.9 5.4 9.1 Body As A Whole - General Disorders Edema Peripheral 2.8 11.3 26.1 Fatigue 4.5 3.5 5.1 Endocrine Disorders Gynecomastia 0.4 3.5 5.5 Central and Peripheral Nervous System Disorders Paresthesia 4.5 7.4 7.9 Hypoesthesia 2.4 1.6 5.1 Metabolic and Nutritional Disorders Edema Generalized 1.2 1.2 5.9 Adverse reactions that occurred in 1% to less than 5% of trial participants receiving SEROSTIM during the first 12 weeks of Clinical Trial 2 thought to be related to SEROSTIM included dose dependent edema, periorbital edema, carpal tunnel syndrome, hyperglycemia and hypertriglyceridemia.
During the 12-week, placebo-controlled portion of Clinical Trial 2, the incidence of hyperglycemia reported as an adverse reaction was 3.6% for the placebo group, 1.9% for the 0.1 mg/kg every other day group and 3.2% for the 0.1 mg/kg daily group. One case of diabetes mellitus was noted in the 0.1 mg/kg daily group during the first 12-weeks of therapy. In addition, during the extension phase of Clinical Trial 2, two patients converted from placebo to full dose SEROSTIM, and 1 patient converted from placebo to half-dose SEROSTIM, were discontinued because of the development of diabetes mellitus.
The types and incidences of adverse reactions reported during the Clinical Trial 2 extension phase were not different from, or greater in frequency than those observed during the 12-week, placebo-controlled portion of Clinical Trial 2.
Adverse reactions from treatment with SEROSTIM in clinical trials in HIV lipodystrophy
SEROSTIM was evaluated for the treatment of patients with HIV lipodystrophy in two double-blind, placebo-controlled trials that excluded patients with a history of diabetes, impaired fasting glucose or impaired glucose (approximately 20% of the patients screened were excluded from study enrollment as a result of a diagnosis of diabetes or glucose intolerance). The studies included a 12-week double-blind, placebo-controlled, parallel group "induction" phase followed by maintenance phases of different durations (12 and 24 weeks, respectively). In the initial 12-week treatment periods of the two, placebo-controlled clinical trials, 406 patients were treated with SEROSTIM. Clinical adverse reactions which occurred during the first 12 weeks of both studies combined in at least 5% of the patients in either of the two active treatment groups are listed by treatment group in Table 2, without regard to causality assessment. The most common adverse reactions judged to be associated with SEROSTIM were edema, arthralgia, pain in extremity, hypoesthesia, myalgia, and blood glucose increased, all of which were more frequently observed when SEROSTIM 4 mg was administered on a daily basis compared with alternate days. These symptoms often subsided with dose reduction. During the 12-week induction phase, 1) approximately 26% of patients receiving SEROSTIM 4 mg daily and 19% of patients receiving SEROSTIM4 mg every other day required dose reductions; and 2) discontinuations as a result of adverse reactions occurred in 13% of patients receiving SEROSTIM 4 mg daily and 5% of patients receiving SEROSTIM 4 mg every other day. The most common reasons for dose reduction and/or drug discontinuation were peripheral edema, hyperglycemia (including blood glucose increased, blood glucose abnormal, and hyperglycemia), and arthralgia.
Table 2: Controlled HIV Lipodystrophy Studies 1 and 2 Combined –Adverse Reactions with >5% Incidence in Either Active Treatment Arm Placebo SEROSTIM
4 mg every other day*SEROSTIM
4 mg dailyPatients
(n=159)Patients
(n=80)Patients
(n=326)System Organ Class
Preferred Term% % % - * Study 22388 only
- † similar terms were grouped together and reported below
Musculoskeletal and connective tissue disorders Arthralgia 11.9 27.8 37.1 Pain in extremity 3.8 5.0 19.3 Myalgia 3.8 2.5 12.6 Musculoskeletal stiffness 1.9 3.8 8.0 Joint stiffness 1.3 3.8 7.7 Joint swelling 0.6 5.0 6.1 General disorders and administration site conditions Edema peripheral 3.8 18.8 45.4 Fatigue 1.9 6.3 8.9 Nervous system disorders Hypoesthesia 0.6 8.8 15.0 Paraesthesia 2.5 12.5 11.0 Investigations (Laboratory Evaluations) Blood glucose increased† 2.5 3.8 13.8 Metabolism and nutrition disorders Hyperglycemia† 0.6 8.8 7.1 Fluid retention 0.6 2.5 5.2 Gastrointestinal disorders Nausea 2.5 1.3 6.1 Glucose metabolism related adverse reactions: During the initial 12-week treatment periods of Studies 1 and 2, the incidence of glucose-related adverse reactions was 4% for the placebo group, 13% for the 4 mg every other day group and 22% for the 4 mg daily group.
Twenty-three patients discontinued due to hyperglycemia while receiving SEROSTIM during any phase of these studies (3.2% in the 12-week induction phases and 2.1% in the extension phases).
Breast-Related Terms: When grouped together, breast-related adverse reactions (e.g. nipple pain, gynecomastia, breast pain/mass/tenderness/swelling/edema/hypertrophy) had an incidence of 1% for the placebo group, 3% for the SEROSTIM 4 mg every other day group and 6% for the SEROSTIM 4 mg daily group.
Adverse reactions that occurred in 1% to less than 5% of trial participants receiving SEROSTIM during the first 12 weeks of HIV Lipodystrophy Studies 1 and 2 thought to be related to SEROSTIM include carpal tunnel syndrome, Tinel's sign and facial edema.
The adverse reactions reported for SEROSTIM 4 mg every other day during the maintenance phase of HIV Lipodystrophy Study 1 (Week 12 to Week 24) were similar in frequency and quality to those observed after treatment with SEROSTIM 4 mg every other day during the 12-week induction phase.
IGF-1 serum concentrations increased statistically in SEROSTIM-treated patients when compared to placebo (Table 3). In the SEROSTIM treated patients at baseline, the proportion of subjects with serum IGF-1 SDS levels ≥ +2 was approximately 10 to 20%, while with treatment with either dose regimen of SEROSTIM the percentage increased to 80 to 90% by Week 12.
Table 3: Change from Baseline to Week 12 in Serum IGF-1 SDS After Treatment with SEROSTIM 4 mg daily vs. Placebo (Modified ITT Population; Studies 1 and 2 Combined) Placebo SEROSTIM
4 mg every other daySEROSTIM
4 mg dailyTime Point Statistic (n=145) (n=79) (n=290) - * P-value from a Wilcoxon Signed Rank test on the change from baseline to Week 12.
- † Proportionally weighted least squares means from a two-way ANOVA model on raw data including effects for treatment, sex, and the treatment by sex interaction.
- ‡ P-value from a two-way ANOVA model on ranked data including effects for treatment, sex, and the treatment by sex interaction.
Baseline Mean (SD)
Range0.4 (1.4)
(-2.5, 4.8)1.3 (2.1)
(-2.0, 13.7)0.0 (1.6)
(-3.0, 11.9)Week 12 Mean (SD)
Range0.8 (1.6)
(-2.6, 6.7)5.1 (3.4)
(-0.7, 17.2)6.1 (5.0)
(-1.8, 29.2)Change from
Baseline toMean (SD)
Range0.4 (1.3)
(-2.9, 7.7)3.9 (3.1)
(-9.4, 11.8)6.1 (4.6)
(-2.4, 24.3)Week 12 p-value* <0.001 <0.001 <0.001 Mean† diff (SEM) 3.5 (0.5) 5.7 (0.4) p-value‡ <0.001 <0.001 As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influences by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to SEROSTIM with the incidence of antibodies to other products may be misleading.
After 12 weeks of treatment, none of the 651 study participants with HIV-associated wasting treated with SEROSTIM for the first time developed detectable antibodies to growth hormone (> 4 pg binding). Patients were not rechallenged. Data beyond 3 months is not available.
6.2 Post-Marketing Experience
The following adverse reactions have been identified during post approval use of SEROSTIM. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hypersensitivity: Serious systemic hypersensitivity reactions including anaphylactic reactions and angioedema have been reported with postmarketing use of somatropin products [see Warnings and Precautions (5.6)].
Endocrine:
- new onset impaired glucose tolerance
- new onset type 2 diabetes mellitus
- exacerbation of preexisting diabetes mellitus
- diabetic ketoacidosis
- diabetic coma
In some patients, these conditions improved when SEROSTIM was discontinued, while in others the glucose intolerance persisted. Some of these patients required initiation or adjustment of antidiabetic treatment while on SEROSTIM [see Warnings and Precautions (5.4)].
Gastrointestinal: Pancreatitis [see Warnings and Precautions (5.9)].
-
7 DRUG INTERACTIONS
Formal drug interaction studies have not been conducted. No data are available on drug interactions between SEROSTIM and HIV protease inhibitors or the non-nucleoside reverse transcriptase inhibitors.
7.1 11β-Hydroxysteroid Dehydrogenase Type 1
The microsomal enzyme 11β-hydroxysteroid dehydrogenase type 1 (11βHSD-1) is required for conversion of cortisone to its active metabolite, cortisol, in hepatic and adipose tissue. Somatropin inhibits 11βHSD-1. Patients treated with glucocorticoid replacement for previously diagnosed hypoadrenalism may require an increase in their maintenance or stress doses following initiation of somatropin treatment; this may be especially true for patients treated with cortisone acetate and prednisone since conversion of these drugs to their biologically active metabolites is dependent on the activity of 11βHSD-1.
7.2 Cytochrome P450-metabolized drugs
Limited published data indicate that somatropin treatment increases cytochrome P450 (CYP450)-mediated antipyrine clearance in man. These data suggest that somatropin administration may alter the clearance of compounds metabolized by CYP450 liver enzymes (e.g., corticosteroids, sex steroids, anticonvulsants, cyclosporine). Therefore, careful monitoring is advised when somatropin is administered in combination with drugs metabolized by CYP450 liver enzymes. However, formal drug interaction studies have not been conducted.
7.3 Oral Estrogen
Because oral estrogens may reduce the serum IGF-1 response to somatropin treatment, girls and women receiving oral estrogen replacement may require greater somatropin dosages [see Dosage and Administration (2)].
7.4 Insulin and/or Other Oral/Injectable Hypoglycemic Agents
Patients with diabetes mellitus who receive concomitant treatment with somatropin may require adjustment of their doses of insulin and/or other hypoglycemic agents [see Warnings and Precautions (5.4)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Reproduction studies have been performed in rats and rabbits. Doses up to 5 to 10 times the human dose, based on body surface area, have revealed no evidence of impaired fertility or harm to the fetus due to SEROSTIM. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, SEROSTIM should be used during pregnancy only if clearly needed.
8.3 Nursing Women
It is not known whether SEROSTIM is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when SEROSTIM is administered to a nursing woman.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients with HIV have not been established. Available evidence suggests that somatropin clearance is similar in adults and children, but no pharmacokinetic studies have been conducted in children with HIV.
In two small studies, 11 children with HIV-associated failure to thrive were treated subcutaneously with human growth hormone. In one study, five children (age range, 6 to 17 years) were treated with 0.04 mg/kg/day for 26 weeks. In a second study, six children (age range, 8 to 14 years) were treated with 0.07 mg/kg/day for 4 weeks. Treatment appeared to be well tolerated in both studies. The preliminary data collected on a limited number of patients with HIV-associated failure to thrive appear to be consistent with safety observations in growth hormone-treated adults with HIV wasting.
Benzyl alcohol, a component of this product, has been associated with serious adverse events and death, particularly in pediatric patients. The "gasping syndrome," (characterized by central nervous system depression, metabolic acidosis, gasping respirations, and high levels of benzyl alcohol and its metabolites found in the blood and urine) has been associated with benzyl alcohol dosages >99 mg/kg/day in neonates and low-birth weight neonates. Additional symptoms may include gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse. Practitioners administering this and other medications containing benzyl alcohol should consider the combined daily metabolic load of benzyl alcohol from all sources.
8.5 Geriatric Use
Clinical studies with SEROSTIM did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Elderly patients may be more sensitive to the action of somatropin, and therefore, may be more prone to develop adverse reactions. A lower starting dose and smaller dose increments should be considered for older patients [see Dosage and Administration (2)].
8.6 Hepatic Impairment
No studies have been conducted for SEROSTIM in patients with hepatic impairment [see Clinical Pharmacology (12.3)].
8.7 Renal Impairment
Subjects with chronic renal failure tend to have decreased somatropin clearance compared to those with normal renal function. However, no studies have been conducted for SEROSTIM in patients with renal impairment [see Clinical Pharmacology (12.3)].
8.8 Gender Effect
Biomedical literature indicates that a gender-related difference in the mean clearance of r-hGH could exist (clearance of r-hGH in males > clearance of r-hGH in females). However, no gender-based analysis is available for SEROSTIM in normal volunteers or patients infected with HIV.
- 10 OVERDOSAGE
-
11 DESCRIPTION
SEROSTIM is a human growth hormone (hGH) produced by recombinant DNA technology. SEROSTIM has 191 amino acid residues and a molecular weight of 22,125 daltons. Its amino acid sequence and structure are identical to the dominant form of human pituitary growth hormone. SEROSTIM is produced by a mammalian cell line (mouse C127) that has been modified by the addition of the hGH gene. SEROSTIM is secreted directly through the cell membrane into the cell-culture medium for collection and purification.
SEROSTIM is a sterile lyophilized powder intended for subcutaneous injection after reconstitution to its liquid form.
Vials of SEROSTIM contain either 4 mg, 5 mg, or 6 mg. Each vial contains the following:
Vials 4 mg 5 mg 6 mg Component Somatropin 4 mg 5 mg 6 mg Sucrose 27.3 mg 34.2 mg 41 mg Phosphoric acid 0.9 mg 1.2 mg 1.4 mg Each 4 mg multi-vial is supplied in a combination package with Bacteriostatic Water for Injection, USP (0.9% Benzyl Alcohol). The pH is adjusted with sodium hydroxide of phosphoric acid to give a pH of 7.4 to 8.5 after reconstitution.
Each 5 mg single-use vial is supplied in a combination package with Sterile Water for Injection, USP. The pH is adjusted with sodium hydroxide or phosphoric acid to give a pH of 6.5 to 8.5 after reconstitution.
Each 6 mg single-use vial is supplied in a combination package with Sterile Water for Injection, USP. The pH is adjusted with sodium hydroxide of phosphoric acid to give a pH of 7.4 to 8.5 after reconstitution.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
SEROSTIM is an anabolic and anticatabolic agent which exerts its influence by interacting with specific receptors on a variety of cell types including myocytes, hepatocytes, adipocytes, lymphocytes, and hematopoietic cells. Some, but not all of its effects, are mediated by insulin-like growth factor-1 (IGF-1).
12.2 Pharmacodynamics
Effects on Protein, Lipid and Carbohydrate Metabolism
A one-week study in 6 patients with HIV-associated wasting has shown that treatment with SEROSTIM 0.1 mg/kg/day improved nitrogen balance, increased protein-sparing lipid oxidation, and had little effect on overall carbohydrate metabolism.
Decreases in trunk fat and total body fat, and increases in lean body mass were observed during two double-blind, placebo-controlled studies wherein SEROSTIM vs. placebo were administered daily for 12 weeks to patients with HIV Lipodystrophy [see Clinical Studies (14)].
Effects on Nitrogen and Mineral Retention
In the one-week study in 6 patients with HIV-associated wasting, treatment with SEROSTIM resulted in the retention of phosphorous, potassium, nitrogen, and sodium. The ratio of retained potassium and nitrogen during SEROSTIM therapy was consistent with retention of these elements in lean tissue.
Physical Performance
Cycle ergometry work output and treadmill performance were examined in separate 12-week, placebo-controlled trials [see Clinical Studies (14)]. In both studies, work output improved significantly in the group receiving SEROSTIM 0.1 mg/kg/day subcutaneously vs placebo. Isometric muscle performance, as measured by grip strength dynamometry, declined, probably as a result of a transient increase in tissue turgor known to occur with SEROSTIM therapy.
12.3 Pharmacokinetics
Absorption: The absolute bioavailability after subcutaneous administration was determined to be 70 to 90%. The mean t½ after subcutaneous administration is significantly longer than that seen after intravenous administration in normal male volunteers down-regulated with somatostatin (approximately 4.0 hrs. vs. 0.6 hrs.), indicating that the subcutaneous absorption of somatropin is a rate-limiting process.
Distribution: The steady-state volume of distribution (Mean ± SD) following intravenous administration of somatropin in normal male volunteers is 12.0 ± 1.08 L.
Metabolism: Although the liver plays a role in the metabolism of GH, GH is primarily cleaved in the kidney. GH undergoes glomerular filtration and, after cleavage within the renal cells, the peptides and amino acids are returned to the systemic circulation.
Elimination: The t½ in nine patients with HIV-associated wasting with an average weight of 56.7 ± 6.8 kg, given a fixed dose of 6.0 mg somatropin subcutaneously was 4.28 ± 2.15 hrs, similar to that observed in normal male volunteers. The renal clearance of r-hGH after subcutaneous administration in nine patients with HIV-associated wasting was 0.0015 ± 0.0037 L/h. No significant accumulation of r-hGH appears to occur after 6 weeks of daily dosing as indicated.
Specific Populations:
Pediatric: Available evidence suggests that r-hGH clearances are similar in adults and children, but no pharmacokinetic studies have been conducted in children with HIV.
Gender: Biomedical literature indicates that a gender-related difference in the mean clearance of r-hGH could exist (clearance of r-hGH in males > clearance of r-hGH in females). However, no gender-based analysis is available in normal volunteers or patients infected with HIV.
Race: No studies have been conducted to determine the effect of race on the pharmacokinetics of SEROSTIM.
- 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
HIV-Associated Wasting or Cachexia
The clinical efficacy of SEROSTIM in HIV-associated wasting or cachexia was assessed in two placebo-controlled trials. All study subjects received concomitant antiretroviral therapy. There was no increase in the incidence of Kaposi's sarcoma (KS), lymphoma, or in the progression of cutaneous Kaposi's sarcoma in clinical studies of SEROSTIM. Patients with internal KS lesions were excluded from the studies. Potential effects on other malignancies are unknown.
Clinical Trial 1:
A 12-week, randomized, double-blind, placebo-controlled study followed by an open-label extension phase enrolled 178 patients with severe HIV wasting taking nucleoside analogue therapy (pre-HAART era). The primary endpoint was body weight. Body composition was assessed using dual energy X-ray absorptiometry (DXA) and physical function was assessed by treadmill exercise testing. Patients meeting the inclusion/exclusion criteria were treated with either placebo or SEROSTIM 0.1 mg/kg daily. Ninety-six percent (96%) were male. The average baseline CD4 count/microliter was 85. The results from one hundred forty (140) evaluable patients were analyzed (those completing the 12-week course of treatment and who were at least 80% compliant with study drug). After 12 weeks of therapy, the mean difference in weight increase between the SEROSTIM-treated group and the placebo-treated group was 1.6 kg (3.5 lb). Mean difference in lean body mass (LBM) change between the SEROSTIM-treated group and the placebo-treated group was 3.1 kg (6.8 lbs) as measured by DXA. Mean increase in weight and LBM, and mean decrease in body fat, were significantly greater in the SEROSTIM-treated group than in the placebo group (p=0.011, p<0.001, p<0.001, respectively) after 12 weeks of treatment (Figure 1). There were no significant changes with continued treatment beyond 12 weeks suggesting that the original gains of weight and LBM were maintained (Figure 1).
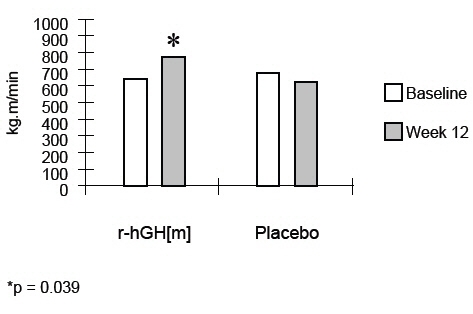
Treatment with SEROSTIM resulted in a significant increase in physical function as assessed by treadmill exercise testing. The median treadmill work output increased by 13% (p=0.039) at 12 weeks in the group receiving SEROSTIM (Figure 2). There was no improvement in the placebo-treated group at 12 weeks. Changes in treadmill performance were significantly correlated with changes in LBM.
Figure 1: Mean Changes in Body Composition
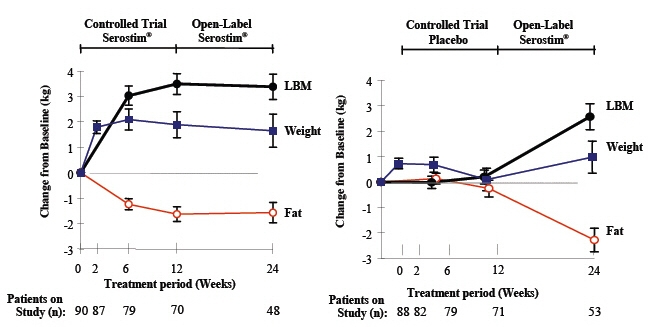
Figure 2: Median Treadmill Work Output
Clinical Trial 2:
A 12-week, randomized, double-blind, placebo-controlled study enrolled 757 patients with HIV-associated wasting, or cachexia. The primary efficacy endpoint was physical function as measured by cycle ergometry work output. Body composition was assessed using bioelectrical impedance spectroscopy (BIS) and also by dual energy X-ray absorptiometry (DXA) at a subset of centers. Patients meeting the inclusion/exclusion criteria were treated with either placebo, approximately 0.1 mg/kg every other day (qod) of SEROSTIM, or approximately 0.1 mg/kg daily at bedtime of SEROSTIM. All results were analyzed in intent-to-treat populations (for cycle ergometry work output, n=670). Ninety-one percent (91%) were male and 88% were on HAART anti-retroviral therapy. The average baseline CD4 count/µL was 446. Six hundred forty-six patients (646) completed the 12-week study and continued in the SEROSTIM treatment extension phase of the trial.
Clinical Trial 2 results are summarized in Tables 4 and 5:
Table 4: Mean (Median) of Cycle Work Output (kJ) Response after 12 weeks of Treatment ITT Population Placebo Half-Dose SEROSTIM* Full-Dose SEROSTIM† - * approximately 0.1 mg/kg every other day
- † approximately 0.1 mg/kg daily
- ‡ p<0.01
Cycle work output (kJ) n=222 n=230 n=218 Baseline 25.92
(25.05)27.79
(26.65)27.57
(26.30)Change from baseline -0.05
(-0.25)2.48
(2.30)2.52
(2.40)Percent change from baseline 0.2% 8.9% 9.1% Difference from Placebo Mean
(2-sided 95% C.I.)- 2.53‡
(0.81, 4.25)2.57‡
(0.83, 4.31)Median - 2.55 2.65 Table 5: Mean (Median) Change from Baseline for Lean Body Mass, Fat Mass and Body Weight Placebo Half-Dose SEROSTIM* Full-Dose SEROSTIM† N Mean
(Median)n Mean
(Median)n Mean
(Median)- * approximately 0.1 mg/kg every other day
- † approximately 0.1 mg/kg daily
Lean body mass (kg)
(by BIS)222 0.97
(0.67)223 3.89
(3.65)205 5.84
(5.47)Fat mass (kg)
(by DXA)94 0.03
(0.01)100 -1.25
(-1.23)85 -1.72
(-1.51)Body weight (kg) 247 0.69
(0.68)257 2.18
(2.15)253 2.79
(2.65)The mean maximum cycle work output until exhaustion increased after 12 weeks by 2.57 kilojoules (kJ) in the SEROSTIM 0.1 mg/kg daily group (p<0.01) and by 2.53 kJ in the SEROSTIM 0.1 mg/kg every other day group (p<0.01) compared with placebo (Table 4). Cycle work output improved approximately 9% in both active treatment arms and decreased <1% in the placebo group. Lean body mass (LBM) and body weight (BW) increased, and fat mass decreased, in a dose-related fashion after treatment with SEROSTIMand placebo (Table 5). The LBM results obtained by BIS were confirmed with DXA.
Patients' perceptions of the impact of 12 weeks of treatment on their wasting symptoms as assessed by the Bristol-Meyers Anorexia/Cachexia Recovery Instrument improved with both doses of SEROSTIMin Clinical Trial 2.
Extension Phase: All patients (n=646) completing the 12-week placebo-controlled phase of Clinical Trial 2 continued SEROSTIM treatment into an extension phase. Five hundred and forty eight of these patients completed an additional 12 weeks of active treatment. In these patients, changes in cycle ergometry work output, LBM, BW, and fat mass either improved further or were maintained with continued SEROSTIM treatment.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
SEROSTIM is available in the following forms:
- SEROSTIM single-use vials containing 5 mg with Sterile Water for Injection, USP. Package of 7 vials. NDC: 44087-0005-7
- SEROSTIM single-use vials containing 6 mg with Sterile Water for Injection, USP. Package of 7 vials. NDC: 44087-0006-7
- SEROSTIM multiple-use vials containing 4 mg with Bacteriostatic Water for Injection, USP (0.9% Benzyl Alcohol). Package of 7 vials. NDC: 44087-0004-7
16.2 Storage and Handling
Before reconstitution: Vials of SEROSTIM and diluent should be stored at room temperature, (15°-30°C/59°-86°F). Expiration dates are stated on product labels.
-
17 PATIENT COUNSELING INFORMATION
Patients being treated with SEROSTIM should be informed of the potential benefits and risks associated with treatment. Patients should be instructed to contact their physician should they experience any side effects or discomfort during treatment with SEROSTIM.
It is recommended that SEROSTIM be administered using sterile, disposable syringes and needles. Patients should be thoroughly instructed in the importance of proper disposal and cautioned against any reuse of needles and syringes. An appropriate container for the disposal of used syringes and needles should be employed.
Patients should be instructed to rotate injection sites to avoid localized tissue atrophy.
Never Share a SEROSTIM Pen or Needle Between Patients
Counsel patients that they should never share SEROSTIM or SEROSTIM injection devices with another person, even if the needle or nozzle is changed. Sharing of SEROSTIM or SEROSTIM injection devices between patients may pose a risk of transmission of infection.
Patients should be informed about the management of common side effects related to tissue turgor, glucose intolerance and musculoskeletal discomfort.
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - 4 mg Kit Carton
Serostim® 4 mg
(somatropin) for injection4 mg
For subcutaneous injection
Rx Only7 vials of SEROSTIM
7 vials of Bacteriostatic Water for Injection, USP (0.9 % Benzyl Alcohol)NDC: 44087-0004-7
EMD Serono
-
PRINCIPAL DISPLAY PANEL - 5 mg Kit Carton
Serostim® 5 mg
(somatropin) for injection5 mg
For subcutaneous injection
Rx Only7 vials SEROSTIM
7 vials Sterile DiluentNDC: 44087-0005-7
EMD Serono

-
PRINCIPAL DISPLAY PANEL - 6 mg Kit Carton
Serostim® 6 mg
(somatropin) for injection6 mg
For subcutaneous injection
Rx Only7 vials SEROSTIM
7 vials Sterile DiluentNDC: 44087-0006-7
EMD Serono
-
INGREDIENTS AND APPEARANCE
SEROSTIM
somatropin kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44087-0004 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44087-0004-7 1 in 1 CARTON 07/25/1997 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 7 VIAL 7 mL Part 2 7 VIAL, GLASS 24.5 mL Part 1 of 2 SEROSTIM
somatropin injection, powder, for solutionProduct Information Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SOMATROPIN (UNII: NQX9KB6PCL) (SOMATROPIN - UNII:NQX9KB6PCL) SOMATROPIN 4 mg in 1 mL Inactive Ingredients Ingredient Name Strength SUCROSE (UNII: C151H8M554) 27.3 mg in 1 mL PHOSPHORIC ACID (UNII: E4GA8884NN) 0.9 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020604 04/23/1996 Part 2 of 2 BACTERIOSTATIC WATER
bacteriostatic water injection, solutionProduct Information Route of Administration SUBCUTANEOUS Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) BENZYL ALCOHOL (UNII: LKG8494WBH) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 3.5 mL in 1 VIAL, GLASS; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020604 04/23/1996 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020604 07/25/1997 SEROSTIM
somatropin kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44087-0005 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44087-0005-7 1 in 1 CARTON 08/23/1996 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 7 VIAL 7 mL Part 2 7 VIAL 7 mL Part 1 of 2 SEROSTIM
somatropin injection, powder, for solutionProduct Information Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SOMATROPIN (UNII: NQX9KB6PCL) (SOMATROPIN - UNII:NQX9KB6PCL) SOMATROPIN 5 mg in 1 mL Inactive Ingredients Ingredient Name Strength SUCROSE (UNII: C151H8M554) 34.2 mg in 1 mL PHOSPHORIC ACID (UNII: E4GA8884NN) 1.2 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020604 04/23/1996 Part 2 of 2 STERILE WATER
sterile water injection, solutionProduct Information Route of Administration SUBCUTANEOUS Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020604 04/23/1996 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020604 08/23/1996 SEROSTIM
somatropin kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44087-0006 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44087-0006-7 1 in 1 CARTON 08/23/1996 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 7 VIAL 7 mL Part 2 7 VIAL 7 mL Part 1 of 2 SEROSTIM
somatropin injection, powder, for solutionProduct Information Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SOMATROPIN (UNII: NQX9KB6PCL) (SOMATROPIN - UNII:NQX9KB6PCL) SOMATROPIN 6 mg in 1 mL Inactive Ingredients Ingredient Name Strength SUCROSE (UNII: C151H8M554) 41.0 mg in 1 mL PHOSPHORIC ACID (UNII: E4GA8884NN) 1.4 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020604 04/23/1996 Part 2 of 2 STERILE WATER
sterile water injection, solutionProduct Information Route of Administration SUBCUTANEOUS Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020604 04/23/1996 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020604 08/23/1996 Labeler - EMD Serono, Inc. (088514898)
Trademark Results [Serostim]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 SEROSTIM 87207270 5195709 Live/Registered |
MERCK KGAA 2016-10-18 |
 SEROSTIM 78363301 2925322 Live/Registered |
Ares Trading S.A. 2004-02-05 |
 SEROSTIM 77390281 3720570 Dead/Cancelled |
Ares Trading S.A. 2008-02-06 |
 SEROSTIM 74510500 2012301 Live/Registered |
MERCK KGAA 1994-04-06 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.