BENAZEPRIL HYDROCHLORIDE AND HYDROCHLOROTHIAZIDE tablet, film coated
Benazepril Hydrochloride and Hydrochlorothiazide by
Drug Labeling and Warnings
Benazepril Hydrochloride and Hydrochlorothiazide by is a Prescription medication manufactured, distributed, or labeled by H.J. Harkins Company, Inc., Eon Labs, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
SPL UNCLASSIFIED SECTION
Rx only
USE IN PREGNANCY
When used in pregnancy, ACE inhibitors can cause injury and even death to the developing fetus. When pregnancy is detected, benazepril hydrochloride and hydrochlorothiazide should be discontinued as soon as possible. See WARNINGS, Fetal/Neonatal Morbidity and Mortality.
-
DESCRIPTION
Benazepril hydrochloride is a white to off-white crystalline powder, soluble (> 100 mg/mL) in water, in ethanol, and in methanol. Benazepril hydrochloride's chemical name is 3-[[1-(ethoxycarbonyl)-3-phenyl-(1S)-propyl]amino]-2,3,4,5- tetrahydro-2-oxo-1H-1-(3S)-benzazepine-1-acetic acid monohydrochloride; its structural formula is:
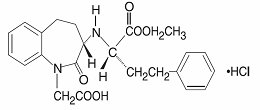
Its empirical formula is C24H28N2O5HCl, and its molecular weight is 460.96. Benazeprilat, the active metabolite of benazepril, is a nonsulfhydryl angiotensin-converting enzyme inhibitor. Benazepril is converted to benazeprilat by hepatic cleavage of the ester group.
Hydrochlorothiazide USP is a white, or practically white, practically odorless, crystalline powder. It is slightly soluble in water; freely soluble in sodium hydroxide solution, in n-butylamine, and in dimethylformamide; sparingly soluble in methanol; and insoluble in ether, in chloroform, and in dilute mineral acids. Hydrochlorothiazide's chemical name is 6-chloro-3,4-dihydro-2H-1,2,4-benzothiadiazine-7-sulfonamide 1,1-dioxide; its structural formula is:
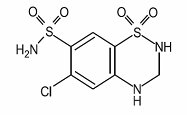
Its empirical formula is C7H8ClN3O4S2 and its molecular weight is 297.73. Hydrochlorothiazide is a thiazide diuretic.
The tablets are a combination of benazepril hydrochloride and hydrochlorothiazide USP. They are formulated for oral administration with a combination of 5 mg, 10 mg, or 20 mg of benazepril hydrochloride and 6.25 mg, 12.5 mg, or 25 mg of hydrochlorothiazide USP. The inactive ingredients of the tablets are colloidal silicon dioxide, crospovidone, hydrogenated castor oil, hypromellose, lactose monohydrate, poloxamer, polyethylene glycol, polysorbate, pregelatinized starch, titanium dioxide, and zinc stearate. The 10 mg/12.5 mg tablets also contain D&C red No. 27 and FD&C blue No. 1. The 20 mg/12.5 mg tablets also contain FD&C blue No. 2 and FD&C red No. 40. The 20 mg/25 mg tablets also contain FD&C red No. 40.
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Benazepril and benazeprilat inhibit angiotensin-converting enzyme (ACE) in human subjects and in animals. ACE is a peptidyl dipeptidase that catalyzes the conversion of angiotensin I to the vasoconstrictor substance, angiotensin II. Angiotensin II also stimulates aldosterone secretion by the adrenal cortex.
Inhibition of ACE results in decreased plasma angiotensin II, which leads to decreased vasopressor activity and to decreased aldosterone secretion. The latter decrease may result in a small increase of serum potassium. Hypertensive patients treated with benazepril alone for up to 52 weeks had elevations of serum potassium of up to 0.2 mEq/L. Similar patients treated with benazepril and hydrochlorothiazide for up to 24 weeks had no consistent changes in their serum potassium (see PRECAUTIONS).
Removal of angiotensin II negative feedback on renin secretion leads to increased plasma renin activity. In animal studies, benazepril had no inhibitory effect on the vasopressor response to angiotensin II and did not interfere with the hemodynamic effects of the autonomic neurotransmitters acetylcholine, epinephrine, and norepinephrine.
ACE is identical to kininase, an enzyme that degrades bradykinin. Whether increased levels of bradykinin, a potent vasodepressor peptide, play a role in the therapeutic effects of benazepril hydrochloride and hydrochlorothiazide remains to be elucidated.
While the mechanism through which benazepril lowers blood pressure is believed to be primarily suppression of the renin-angiotensin-aldosterone system, benazepril has an antihypertensive effect even in patients with low-renin hypertension.
Hydrochlorothiazide is a thiazide diuretic. Thiazides affect the renal tubular mechanisms of electrolyte reabsorption, directly increasing excretion of sodium and chloride in approximately equivalent amounts. Indirectly, the diuretic action of hydrochlorothiazide reduces plasma volume, with consequent increases in plasma renin activity, increases in aldosterone secretion, increases in urinary potassium loss, and decreases in serum potassium. The renin-aldosterone link is mediated by angiotensin, so co-administration of an ACE inhibitor tends to reverse the potassium loss associated with these diuretics.
The mechanism of the antihypertensive effect of thiazides is unknown.
Pharmacokinetics and Metabolism
Following oral administration of benazepril hydrochloride and hydrochlorothiazide, peak plasma concentrations of benazepril are reached within 0.5 to 1 hours. As determined by urinary recovery, the extent of absorption is at least 37%. The absorption of hydrochlorothiazide is somewhat slower (1 to 2.5 hours) and somewhat more complete (50% to 80%). In fasting subjects, the rate and extent of absorption of benazepril and hydrochlorothiazide from benazepril hydrochloride and hydrochlorothiazide tablets are not different, respectively, from the rate and extent of absorption of benazepril and hydrochlorothiazide from immediate-release monotherapy formulations.
The absorption of benazepril from benazepril hydrochloride tablets is not influenced by the presence of food in the gastrointestinal tract, but possible effects of food upon absorption of either component from benazepril hydrochloride and hydrochlorothiazide tablets have not been studied. The reported studies of food effects on hydrochlorothiazide absorption have been inconclusive. The absorption of hydrochlorothiazide is increased by agents that reduce gastrointestinal motility, but it is reported to be reduced by 50% in patients with congestive heart failure.
Cleavage of the ester group (primarily in the liver) converts benazepril to its active metabolite, benazeprilat. Peak plasma concentrations of benazeprilat are reached 1 to 2 hours after drug intake in the fasting state and 2 to 4 hours after drug intake in the nonfasting state. The serum protein binding of benazepril is about 96.7% and that of benazeprilat about 95.3%, as measured by equilibrium dialysis; on the basis of in vitro studies, the degree of protein binding should be unaffected by age, hepatic dysfunction, or - over the concentration range of 0.24 µmol/L to 23.6 µmol/L - concentration.
Hydrochlorothiazide is not metabolized. Its apparent volume of distribution is 3.6 L/kg to 7.8 L/kg, and its measured plasma protein binding is 67.9%. The drug also accumulates in red blood cells, so that whole blood levels are 1.6 to 1.8 times those measured in plasma.
In studies of rats given 14C-benazepril, benazepril and its metabolites crossed the blood-brain barrier only to an extremely low extent. Multiple doses of benazepril did not result in accumulation in any tissue except the lung, where, as with other ACE inhibitors in similar studies, there was a slight increase in concentration due to slow elimination in that organ.
Some placental passage occurred when benazepril was administered to pregnant rats. In humans, hydrochlorothiazide crosses the placenta freely, and levels in umbilical-cord blood are similar to those in the maternal circulation.
Benazepril is almost completely metabolized to benazeprilat, which has much greater ACE inhibitory activity than benazepril, and to the glucuronide conjugates of benazepril and benazeprilat. Only trace amounts of an administered dose of benazepril can be recovered unchanged in the urine; about 20% of the dose is excreted as benazeprilat, 4% as benazepril glucuronide, and 8% as benazeprilat glucuronide.
In patients with hepatic dysfunction due to cirrhosis, levels of benazeprilat are essentially unaltered. Similarly, the pharmacokinetics of benazepril and benazeprilat do not appear to be influenced by age.
The kinetics of benazepril are dose-proportional within the dosage range of 5 mg to 20 mg. Small deviations from dose-proportionality were observed when the broader range of 2 mg to 80 mg was studied, possibly due to the saturable binding of the compound to ACE.
The effective half-life of accumulation of benazeprilat following multiple dosing of benazepril hydrochloride is 10 to 11 hours. Thus, steady-state concentrations of benazeprilat should be reached after 2 or 3 doses of benazepril hydrochloride given once daily.
During chronic administration (28 days) of once-daily doses of benazepril between 5 mg and 20 mg, the kinetics did not change, and there was no significant accumulation. Accumulation ratios based on AUC and urinary recovery of benazeprilat were 1.19 and 1.27, respectively.
When dialysis was started two hours after ingestion of 10 mg of benazepril, approximately 6% of benazeprilat was removed in 4 hours of dialysis. The parent compound, benazepril, was not detected in the dialysate.
Benazepril and benazeprilat are cleared predominantly by renal excretion in healthy subjects with normal renal function. Nonrenal (i.e., biliary) excretion accounts for approximately 11% to 12% of benazeprilat excretion in healthy subjects. In patients with renal failure, biliary clearance may compensate to an extent for deficient renal clearance.
The disposition of benazepril and benazeprilat in patients with mild-to-moderate renal insufficiency (creatinine clearance > 30 mL/min) is similar to that in patients with normal renal function. In patients with creatinine clearance ≤ 30 mL/min, peak benazeprilat levels and the initial (alpha phase) half-life increase, and time to steady state may be delayed (see DOSAGE AND ADMINISTRATION).
Thiazide diuretics are eliminated by the kidney, with a terminal half-life of 5 to 15 hours. In a study of patients with impaired renal function (mean creatinine clearance of 19 mL/min), the half-life of hydrochlorothiazide elimination was lengthened to 21 hours.
Pharmacodynamics
Single and multiple doses of 10 mg or more of benazepril cause inhibition of plasma ACE activity by at least 80% to 90% for at least 24 hours after dosing. For up to 4 hours after a 10-mg dose, pressor responses to exogenous angiotensin I were inhibited by 60% to 90%.
Administration of benazepril to patients with mild-to-moderate hypertension results in a reduction of both supine and standing blood pressure to about the same extent, with no compensatory tachycardia. Symptomatic postural hypotension is infrequent, although it can occur in patients who are salt and/or volume depleted (see WARNINGS, Hypotension).
In single-dose studies, benazepril lowered blood pressure within 1 hour, with peak reductions achieved 2 to 4 hours after dosing. The antihypertensive effect of a single dose persisted for 24 hours. In multiple-dose studies, once-daily doses of 20 mg to 80 mg decreased seated pressure (systolic/diastolic) 24 hours after dosing by about 6-12/4-7 mmHg. The reductions at trough are about 50% of those seen at peak.
Four dose-response studies of benazepril monotherapy using once-daily dosing were conducted in 470 mild-to-moderate hypertensive patients not using diuretics. The minimal effective once-daily dose of benazepril was 10 mg; further falls in blood pressure, especially at morning trough, were seen with higher doses in the studied dosing range (10 mg to 80 mg). In studies comparing the same daily dose of benazepril given as a single morning dose or as a twice-daily dose, blood pressure reductions at the time of morning trough blood levels were greater with the divided regimen.
During chronic therapy with benazepril, the maximum reduction in blood pressure with any given dose is generally achieved after 1 to 2 weeks. The antihypertensive effects of benazepril have continued during therapy for at least 2 years. Abrupt withdrawal of benazepril has not been associated with a rapid increase in blood pressure.
In patients with mild-to-moderate hypertension, total daily doses of benazepril hydrochloride 20 mg to 40 mg were similar in effectiveness to total daily doses of captopril 50 mg to 100 mg, hydrochlorothiazide 25 mg to 50 mg, nifedipine SR 40 mg to 80 mg, and propranoloI 80 mg to 160 mg.
The antihypertensive effects of benazepril were not appreciably different in patients receiving high- or low-sodium diets.
In hemodynamic studies in dogs, blood pressure reduction was accompanied by a reduction in peripheral arterial resistance, with an increase in cardiac output and renal blood flow and little or no change in heart rate. In normal human volunteers, single doses of benazepril caused an increase in renal blood flow but had no effect on glomerular filtration rate.
In clinical trials of benazepril/hydrochlorothiazide using benazepril doses of 5 mg to 20 mg and hydrochlorothiazide doses of 6.25 mg to 25 mg, the antihypertensive effects were sustained for at least 24 hours, and they increased with increasing dose of either component. Although benazepril monotherapy is somewhat less effective in blacks than in nonblacks, the efficacy of combination therapy appears to be independent of race.
By blocking the renin-angiotensin-aldosterone axis, administration of benazepril tends to reduce the potassium loss associated with the diuretic. In clinical trials of benazepril hydrochloride and hydrochlorothiazide, the average change in serum potassium was near zero in subjects who received 5 mg/6.25 mg or 20 mg/12.5 mg, but the average subject who received 10 mg/12.5 mg or 20 mg/25 mg experienced a mild reduction in serum potassium, similar to that experienced by the average subject receiving the same dose of hydrochlorothiazide monotherapy.
-
INDICATIONS AND USAGE
Benazepril hydrochloride and hydrochlorothiazide tablets are indicated for the treatment of hypertension.
This fixed combination drug is not indicated for the initial therapy of hypertension (see DOSAGE AND ADMINISTRATION).
In using benazepril hydrochloride and hydrochlorothiazide tablets, consideration should be given to the fact that another angiotensin-converting enzyme inhibitor, captopril, has caused agranulocytosis, particularly in patients with renal impairment or collagen-vascular disease. Available data are insufficient to show that benazepril does not have a similar risk (see WARNINGS, Neutropenia/Agranulocytosis).
Black patients receiving ACE inhibitors have been reported to have a higher incidence of angioedema compared to nonblacks.
-
CONTRAINDICATIONS
Benazepril hydrochloride and hydrochlorothiazide is contraindicated in patients who are anuric.
Benazepril hydrochloride and hydrochlorothiazide is also contraindicated in patients who are hypersensitive to benazepril, to any other ACE inhibitor, to hydrochlorothiazide, or to other sulfonamide-derived drugs. Hypersensitivity reactions are more likely to occur in patients with a history of allergy or bronchial asthma.
Benazepril hydrochloride and hydrochlorothiazide is also contraindicated in patients with a history of angioedema with or without previous ACE inhibitor treatment.
-
WARNINGS
Anaphylactoid and Possibly Related Reactions
Presumably because angiotensin-converting enzyme inhibitors affect the metabolism of eicosanoids and polypeptides, including endogenous bradykinin, patients receiving ACE inhibitors (including benazepril hydrochloride and hydrochlorothiazide) may be subject to a variety of adverse reactions, some of them serious.
Head and Neck Angioedema
Angioedema of the face, extremities, lips, tongue, glottis, and larynx has been reported in patients treated with angiotensin-converting enzyme inhibitors. In U.S. clinical trials, symptoms consistent with angioedema were seen in none of the subjects who received placebo and in about 0.5% of the subjects who received benazepril. Angioedema associated with laryngeal edema can be fatal. If laryngeal stridor or angioedema of the face, tongue, or glottis occurs, treatment with benazepril hydrochloride and hydrochlorothiazide should be discontinued and appropriate therapy instituted immediately. When involvement of the tongue, glottis, or larynx appears likely to cause airway obstruction, appropriate therapy, e.g., subcutaneous epinephrine injection 1:1000 (0.3 mL to 0.5 mL) should be promptly administered (see PRECAUTIONS and ADVERSE REACTIONS).
Intestinal Angioedema
Intestinal angioedema has been reported in patients treated with ACE inhibitors. These patients presented with abdominal pain (with or without nausea or vomiting); in some cases there was no prior history of facial angioedema and C-1 esterase levels were normal. The angioedema was diagnosed by procedures including abdominal CT scan or ultrasound, or at surgery, and symptoms resolved after stopping the ACE inhibitor. Intestinal angioedema should be included in the differential diagnosis of patients on ACE inhibitors presenting with abdominal pain.
Anaphylactoid Reactions During Desensitization
Two patients undergoing desensitizing treatment with hymenoptera venom while receiving ACE inhibitors sustained life-threatening anaphylactoid reactions. In the same patients, these reactions were avoided when ACE inhibitors were temporarily withheld, but they reappeared upon inadvertent rechallenge.
Anaphylactoid Reactions During Membrane Exposure
Anaphylactoid reactions have been reported in patients dialyzed with high-flux membranes and treated concomitantly with an ACE inhibitor. Anaphylactoid reactions have also been reported in patients undergoing low-density lipoprotein apheresis with dextran sulfate absorption.
Hypotension
Benazepril hydrochloride and hydrochlorothiazide can cause symptomatic hypotension. Like other ACE inhibitors, benazepril has been only rarely associated with hypotension in uncomplicated hypertensive patients. Symptomatic hypotension is most likely to occur in patients who have been volume and/or salt depleted as a result of prolonged diuretic therapy, dietary salt restriction, dialysis, diarrhea, or vomiting. Volume and/or salt depletion should be corrected before initiating therapy with benazepril hydrochloride and hydrochlorothiazide.
Benazepril hydrochloride and hydrochlorothiazide should be used cautiously in patients receiving concomitant therapy with other antihypertensives. The thiazide component of benazepril hydrochloride and hydrochlorothiazide may potentiate the action of other antihypertensive drugs, especially ganglionic or peripheral adrenergic-blocking drugs. The antihypertensive effects of the thiazide component may also be enhanced in the postsympathectomy patient.
In patients with congestive heart failure, with or without associated renal insufficiency, ACE inhibitor therapy may cause excessive hypotension, which may be associated with oliguria, azotemia, and (rarely) with acute renal failure and death. In such patients, benazepril hydrochloride and hydrochlorothiazide therapy should be started under close medical supervision; they should be followed closely for the first 2 weeks of treatment and whenever the dose of benazepril or diuretic is increased.
If hypotension occurs, the patient should be placed in a supine position, and, if necessary, treated with intravenous infusion of physiological saline. Benazepril hydrochloride and hydrochlorothiazide treatment usually can be continued following restoration of blood pressure and volume.
Impaired Renal Function
Benazepril hydrochloride and hydrochlorothiazide should be used with caution in patients with severe renal disease. Thiazides may precipitate azotemia in such patients, and the effects of repeated dosing may be cumulative.
When the renin-angiotensin-aldosterone system is inhibited by benazepril, changes in renal function may be anticipated in susceptible individuals. In patients with severe congestive heart failure, whose renal function may depend on the activity of the renin-angiotensin-aldosterone system, treatment with angiotensin-converting enzyme inhibitors (including benazepril) may be associated with oliguria and/or progressive azotemia and (rarely) with acute renal failure and/or death.
In a small study of hypertensive patients with unilateral or bilateral renal artery stenosis, treatment with benazepril was associated with increases in blood urea nitrogen and serum creatinine; these increases were reversible upon discontinuation of benazepril therapy, concomitant diuretic therapy, or both. When such patients are treated with benazepril hydrochloride and hydrochlorothiazide, renal function should be monitored during the first few weeks of therapy.
Some benazepril-treated hypertensive patients with no apparent pre-existing renal vascular disease have developed increases in blood urea nitrogen and serum creatinine, usually minor and transient, especially when benazepril has been given concomitantly with a diuretic. Dosage reduction of benazepril hydrochloride and hydrochlorothiazide may be required. Evaluation of the hypertensive patient should always include assessment of renal function (see DOSAGE AND ADMINISTRATION).
Neutropenia/Agranulocytosis
Another angiotensin-converting enzyme inhibitor, captopril, has been shown to cause agranulocytosis and bone marrow depression, rarely in uncomplicated patients (incidence probably less than once per 10,000 exposures) but more frequently (incidence possibly as great as once per 1000 exposures) in patients with renal impairment, especially those who also have collagen-vascular diseases such as systemic lupus erythematosus or scleroderma. Available data from clinical trials of benazepril are insufficient to show that benazepril does not cause agranulocytosis at similar rates. Monitoring of white blood cell counts should be considered in patients with collagen-vascular disease, especially if the disease is associated with impaired renal function.
Fetal/Neonatal Morbidity and Mortality
ACE inhibitors can cause fetal and neonatal morbidity and death when administered to pregnant women. Several dozen cases have been reported in the world literature. When pregnancy is detected, benazepril hydrochloride and hydrochlorothiazide should be discontinued as soon as possible and monitoring of the fetal development should be performed on a regular basis.
The use of ACE inhibitors during the second and third trimesters of pregnancy has been associated with fetal and neonatal injury, including hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, and death. Oligohydramnios has also been reported, presumably resulting from decreased fetal renal function; oligohydramnios in this setting has been associated with fetal limb contractures, craniofacial deformation, and hypoplastic lung development. Prematurity, intrauterine growth retardation, and patent ductus arteriosus have also been reported, although it is not clear whether these occurrences were due to the ACE-inhibitor exposure.
In addition, use of ACE inhibitors during the first trimester of pregnancy has been associated with a potentially increased risk of birth defects. In women planning to become pregnant, ACE inhibitors (including benazepril hydrochloride and hydrochlorothiazide) should not be used. Women of child-bearing age should be made aware of the potential risk and ACE inhibitors (including benazepril hydrochloride and hydrochlorothiazide) should only be given after careful counseling and consideration of individual risks and benefits.
Rarely (probably less often than once in every thousand pregnancies), no alternative to ACE inhibitors will be found. In these rare cases, the mothers should be apprised of the potential hazards to their fetuses, and serial ultrasound examinations should be performed to assess the intraamniotic environment.
If oligohydramnios is observed, benazepril should be discontinued unless it is considered life-saving for the mother. Contraction stress testing (CST), a nonstress test (NST), or biophysical profiling (BPP) may be appropriate, depending upon the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury.
Infants with histories of in utero exposure to ACE inhibitors should be closely observed for hypotension, oliguria, and hyperkalemia. If oliguria occurs, attention should be directed toward support of blood pressure and renal perfusion. Exchange transfusion or peritoneal dialysis may be required as means of reversing hypotension and/or substituting for disordered renal function. Benazepril, which crosses the placenta, can theoretically be removed from the neonatal circulation by these means; there are occasional reports of benefit from these maneuvers, but experience is limited.
Intrauterine exposure to thiazide diuretics is associated with fetal or neonatal jaundice, thrombocytopenia, and possibly other adverse reactions that have occurred in adults.
No teratogenic effects were seen when benazepril and hydrochlorothiazide were administered to pregnant rats at a dose ratio of 4:5. On a mg/kg basis, the doses used were up to 167 times the maximum recommended human dose. Similarly, no teratogenic effects were seen when benazepril and hydrochlorothiazide were administered to pregnant mice at total doses up to 160 mg/kg/day, with benazepril:hydrochlorothiazide ratios of 15:1. When hydrochlorothiazide was orally administered without benazepril to pregnant mice and rats during their respective periods of major organogenesis, at doses up to 3000 mg/kg/day and 1000 mg/kg/day respectively, there was no evidence of harm to the fetus. Similarly, no teratogenic effects of benazepril were seen in studies of pregnant rats, mice, and rabbits; on a mg/kg basis, the doses used in these studies were 300 times (in rats), 90 times (in mice), and more than 3 times (in rabbits) the maximum recommended human dose.
Hepatic Failure
Rarely, ACE inhibitors have been associated with a syndrome that starts with cholestatic jaundice and progresses to fulminant hepatic necrosis and (sometimes) death. The mechanism of this syndrome is not understood. Patients receiving ACE inhibitors who develop jaundice or marked elevations of hepatic enzymes should discontinue the ACE inhibitor and receive appropriate medical follow-up.
Impaired Hepatic Function
Benazepril hydrochloride and hydrochlorothiazide should be used with caution in patients with impaired hepatic function or progressive liver disease, since minor alterations of fluid and electrolyte balance may precipitate hepatic coma (see WARNINGS,Hepatic Failure, above). In patients with hepatic dysfunction due to cirrhosis, levels of benazeprilat are essentially unaltered. No formal pharmacokinetic studies have been carried out in hypertensive patients with impaired liver function.
Systemic Lupus Erythematosus
Thiazide diuretics have been reported to cause exacerbation or activation of systemic lupus erythematosus.
Acute Myopia and Secondary Angle-Closure Glaucoma
Hydrochlorothiazide, a sulfonamide, can cause an idiosyncratic reaction, resulting in acute transient myopia and acute angle-closure glaucoma. Symptoms include acute onset of decreased visual acuity or ocular pain and typically occur within hours to weeks of drug initiation. Untreated acute angle-closure glaucoma can lead to permanent vision loss. The primary treatment is to discontinue hydrochlorothiazide as rapidly as possible. Prompt medical or surgical treatments may need to be considered if the intraocular pressure remains uncontrolled. Risk factors for developing acute angle-closure glaucoma may include a history of sulfonamide or penicillin allergy.
-
PRECAUTIONS
General
Derangements of Serum Electrolytes
In clinical trials of benazepril monotherapy, hyperkalemia (serum potassium at least 0.5 mEq/L greater than the upper limit of normal) occurred in approximately 1% of hypertensive patients receiving benazepril. In most cases, these were isolated values which resolved despite continued therapy. Risk factors for the development of hyperkalemia included renal insufficiency, diabetes mellitus, and the concomitant use of potassium-sparing diuretics, potassium supplements, and/or potassium-containing salt substitutes.
Conversely, treatment with thiazide diuretics has been associated with hypokalemia, hyponatremia, and hypochloremic alkalosis. These disturbances have sometimes been manifest as one or more of dryness of mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pains or cramps, muscular fatigue, hypotension, oliguria, tachycardia, nausea, and vomiting. Hypokalemia can also sensitize or exaggerate the response of the heart to the toxic effects of digitalis. The risk of hypokalemia is greatest in patients with cirrhosis of the liver, in patients experiencing a brisk diuresis, in patients who are receiving inadequate oral intake of electrolytes, and in patients receiving concomitant therapy with corticosteroids or ACTH.
The opposite effects of benazepril and hydrochlorothiazide on serum potassium will approximately balance each other in many patients, so that no net effect upon serum potassium will be seen. In other patients, one or the other effect may be dominant. Initial and periodic determinations of serum electrolytes to detect possible electrolyte imbalance should be performed at appropriate intervals.
Chloride deficits are generally mild and require specific treatment only under extraordinary circumstances (e.g., in liver disease or renal disease). Dilutional hyponatremia may occur in edematous patients; appropriate therapy is water restriction rather than administration of salt, except in rare instances when the hyponatremia is life-threatening. In actual salt depletion, appropriate replacement is the therapy of choice.
Calcium excretion is decreased by thiazides. In a few patients on prolonged thiazide therapy, pathological changes in the parathyroid gland have been observed, with hypercalcemia and hypophosphatemia. More serious complications of hyperparathyroidism (renal lithiasis, bone resorption, and peptic ulceration) have not been seen.
Thiazides increase the urinary excretion of magnesium, and hypomagnesemia may result.
Other Metabolic Disturbances
Thiazide diuretics tend to reduce glucose tolerance and to raise serum levels of cholesterol, triglycerides, and uric acid. These effects are usually minor, but frank gout or overt diabetes may be precipitated in susceptible patients.
Cough
Presumably due to the inhibition of the degradation of endogenous bradykinin, persistent nonproductive cough has been reported with all ACE inhibitors, always resolving after discontinuation of therapy. ACE inhibitor-induced cough should be considered in the differential diagnosis of cough.
Surgery/Anesthesia
In patients undergoing surgery or during anesthesia with agents that produce hypotension, benazepril will block the angiotensin II formation that could otherwise occur secondary to compensatory renin release. Hypotension that occurs as a result of this mechanism can be corrected by volume expansion.
Information for Patients
Angioedema
Angioedema, including laryngeal edema, can occur at any time with treatment with ACE inhibitors. A patient receiving benazepril hydrochloride and hydrochlorothiazide should be told to report immediately any signs or symptoms suggesting angioedema (swelling of face, eyes, lips, or tongue, or difficulty in breathing) and to take no more drug until after consulting with the prescribing physician.
Pregnancy
Female patients of childbearing age should be told about the consequences of exposure to ACE inhibitors. Discuss other treatment options with women planning to become pregnant. Patients should be asked to report pregnancies to their physicians as soon as possible.
Symptomatic Hypotension
A patient receiving benazepril hydrochloride and hydrochlorothiazide should be cautioned that lightheadedness can occur, especially during the first days of therapy, and that it should be reported to the prescribing physician. The patient should be told that if syncope occurs, benazepril hydrochloride and hydrochlorothiazide should be discontinued until the physician has been consulted.
All patients should be cautioned that inadequate fluid intake, excessive perspiration, diarrhea, or vomiting can lead to an excessive fall in blood pressure, with the same consequences of lightheadedness and possible syncope.
Laboratory Tests
The hydrochlorothiazide component of benazepril hydrochloride and hydrochlorothiazide may decrease serum PBI levels without signs of thyroid disturbance.
Therapy with benazepril hydrochloride and hydrochlorothiazide should be interrupted for a few days before carrying out tests of parathyroid function.
Drug Interactions
Potassium Supplements and Potassium-Sparing Diuretics
As noted above (PRECAUTIONS, General, Derangements of Serum Electrolytes), the net effect of benazepril hydrochloride and hydrochlorothiazide may be to elevate a patient's serum potassium, to reduce it, or to leave it unchanged. Potassium-sparing diuretics (spironolactone, amiloride, triamterene, and others) or potassium supplements can increase the risk of hyperkalemia. If concomitant use of such agents is indicated, they should be given with caution, and the patient's serum potassium should be monitored frequently.
Lithium
Increased serum lithium levels and symptoms of lithium toxicity have been reported in patients receiving ACE inhibitors during therapy with lithium. Because renal clearance of lithium is reduced by thiazides, the risk of lithium toxicity is presumably raised further when, as in therapy with benazepril hydrochloride and hydrochlorothiazide, a thiazide diuretic is co-administered with the ACE inhibitor. Benazepril hydrochloride and hydrochlorothiazide and lithium should be co-administered with caution, and frequent monitoring of serum lithium levels is recommended.
Gold
Nitritoid reactions (symptoms include facial flushing, nausea, vomiting and hypotension) have been reported rarely in patients on therapy with injectable gold (sodium aurothiomalate) and concomitant ACE inhibitor therapy.
Non-Steroidal Anti-Inflammatory Agents including Selective Cyclooxygenase-2 Inhibitors (COX-2 Inhibitors)
In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function, co-administration of NSAIDs, including selective COX-2 inhibitors, with ACE inhibitors, including benazepril, may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible. Monitor renal function periodically in patients receiving benazepril and NSAID therapy.
The antihypertensive effect of ACE inhibitors and thiazide diuretics may be attenuated by NSAIDs. The diuretic and natriuretic effects of thiazide diuretics may also be reduced when NSAIDs are co-administered.
Other
Benazepril has been used concomitantly with beta-adrenergic-blocking agents, calcium-blocking agents, cimetidine, diuretics, digoxin, and hydralazine without evidence of clinically important adverse interactions. Other ACE inhibitors have had less than additive effects with beta-adrenergic blockers, presumably because drugs of both classes lower blood pressure by inhibiting parts of the renin-angiotensin system.
Interaction studies with warfarin and acenocoumarol have failed to identify any clinically important effects of benazepril on the serum concentrations or clinical effects of these anticoagulants.
Insulin requirements in diabetic patients may be increased, decreased, or unchanged.
Thiazides may decrease arterial responsiveness to norepinephrine, but not enough to preclude effectiveness of the pressor agent for therapeutic use.
Thiazides may increase the responsiveness to tubocurarine.
The diuretic, natriuretic, and antihypertensive effects of thiazide diuretics may be reduced by concurrent administration of nonsteroidal anti-inflammatory agents.
Cholestyramine and colestipol resins: Absorption of hydrochlorothiazide is impaired in the presence of anionic exchange resins. Single doses of either cholestyramine or colestipol resins bind the hydrochlorothiazide and reduce its absorption from the gastrointestinal tract by up to 85% and 43%, respectively.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence of carcinogenicity was found when benazepril was given to rats and mice for 104 weeks at doses up to 150 mg/kg/day. On a body-weight basis, this dose is over 100 times the maximum recommended human dose; on a body-surface-area basis, this dose is 18 times (rats) and 9 times (mice) the maximum recommended human dose. No mutagenic activity was detected in the Ames test in bacteria (with or without metabolic activation), in an in vitro test for forward mutations in cultured mammalian cells, or in a nucleus anomaly test. At doses of 50 mg/kg/day to 500 mg/kg/day (38 to 375 times the maximum recommended human dose on a body-weight basis; 6 to 61 times the maximum recommended dose on a body-surface-area basis), benazepril had no adverse effect on the reproductive performance of male and female rats.
Under the auspices of the National Toxicology Program, rats and mice received hydrochlorothiazide in their feed for two years, at doses up to 600 mg/kg/day in mice and up to 100 mg/kg/day in rats. These studies uncovered no evidence of a carcinogenic potential of hydrochlorothiazide in rats or female mice, but there was equivocal evidence of hepatocarcinogenicity in male mice. Hydrochlorothiazide was not genotoxic in in vitro assays using strains TA 98, TA 100, TA 1535, TA 1537, and TA 1538 of Salmonella typhimurium (the Ames test); in the Chinese Hamster Ovary (CHO) test for chromosomal aberrations; or in in vivo assays using mouse germinal cell chromosomes, Chinese hamster bone marrow chromosomes, and the Drosophila sex-linked recessive lethal trait gene. Positive test results were obtained in the in vitro CHO Sister Chromatid Exchange (clastogenicity) test and in the Mouse Lymphoma Cell (mutagenicity) assays, using concentrations of hydrochlorothiazide of 43 µg/mL to 1300 µg/mL. Positive test results were also obtained in the Aspergillus nidulans nondisjunction assay, using an unspecified concentration of hydrochlorothiazide.
Hydrochlorothiazide had no adverse effects on the fertility of mice and rats of either sex in studies wherein these species were exposed, via their diets, to doses up to 100 mg/kg/day and 4 mg/kg/day, respectively, prior to mating and throughout gestation.
Nursing Mothers
Minimal amounts of unchanged benazepril and benazeprilat are excreted into the breast milk of lactating women treated with benazepril, so that a newborn child ingesting nothing but breast milk would receive less than 0.1% of the maternal doses of benazepril and benazeprilat. Thiazides, on the other hand, are definitely excreted into breast milk. Because of the potential for serious adverse reactions in nursing infants from hydrochlorothiazide and the unknown effects of benazepril in infants, a decision should be made whether to discontinue nursing or to discontinue benazepril hydrochloride and hydrochlorothiazide, taking into account the importance of the drug to the mother.
Geriatric Use
Of the total number of patients who received benazepril hydrochloride and hydrochlorothiazide in U.S. clinical studies of benazepril hydrochloride and hydrochlorothiazide, 19% were 65 or older while about 1.5% were 75 or older. Overall differences in effectiveness or safety were not observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Benazepril and benazeprilat are substantially excreted by the kidney. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
-
ADVERSE REACTIONS
Benazepril hydrochloride and hydrochlorothiazide has been evaluated for safety in over 2,500 patients with hypertension; over 500 of these patients were treated for at least 6 months, and over 200 were treated for more than 1 year.
The reported side effects were generally mild and transient, and there was no relationship between side effects and age, sex, race, or duration of therapy. Discontinuation of therapy due to side effects was required in approximately 7% of U.S. patients treated with benazepril hydrochloride and hydrochlorothiazide and in 4% of patients treated with placebo.
The most common reasons for discontinuation of therapy with benazepril hydrochloride and hydrochlorothiazide in U.S. studies were cough (1%; see PRECAUTIONS), "dizziness" (1%), headache (0.6%), and fatigue (0.6%).
The side effects considered possibly or probably related to study drug that occurred in U.S. placebo-controlled trials in more than 1% of patients treated with benazepril hydrochloride and hydrochlorothiazide are shown in the table below.
Reactions Possibly or Probably Drug Related Patients in U.S. Placebo-Controlled Studies Benazepril HCl and Hydrochlorothiazide
(N=665)
Placebo
(N=235)
N % N % “Dizziness” 41 6.3 8 3.4 Fatigue 34 5.2 6 2.6 Postural Dizziness 23 3.5 1 0.4 Headache 20 3.1 10 4.3 Cough 14 2.1 3 1.3 Hypertonia 10 1.5 3 1.3 Vertigo 10 1.5 2 0.9 Nausea 9 1.4 2 0.9 Impotence 8 1.2 0 0.0 Somnolence 8 1.2 1 0.4 Other side effects considered possibly or probably related to study drug that occurred in U.S. placebo-controlled trials in 0.3% to 1% of patients treated with benazepril hydrochloride and hydrochlorothiazide were the following:
Angioedema: Edema of the lips or face without other manifestations of angioedema (0.3%). See WARNINGS, Head and Neck Angioedema.
Cardiovascular: Hypotension (seen in 0.6% of patients), postural hypotension (0.3%), palpitations, and flushing.
Gastrointestinal: Vomiting, diarrhea, dyspepsia, anorexia, and constipation.
Neurologic and Psychiatric: Insomnia, nervousness, paresthesia, libido decrease, dry mouth, taste perversion, and tinnitus.
Dermatologic: Rash and sweating.
Other: Gout, urinary frequency, arthralgia, myalgia, asthenia, and pain (including chest pain and abdominal pain).
Other adverse experiences reported in 0.3% or more of benazepril hydrochloride and hydrochlorothiazide patients in U.S. controlled clinical trials, and rarer events seen in post-marketing experience, were the following; asterisked entries occurred in more than 1% of patients (in some, a causal relationship to benazepril hydrochloride and hydrochlorothiazide is uncertain):
Angioedema: Edema of the lips or face without other manifestations of angioedema. See WARNINGS, Head and Neck Angioedema.
Cardiovascular: Syncope, peripheral vascular disorder, and tachycardia.
Body as a Whole: Infection, back pain*, flu syndrome*, fever, chills, and neck pain.
Dermatologic: Photosensitivity and pruritus.
Gastrointestinal: Gastroenteritis, flatulence, and tooth disorder.
Neurologic and Psychiatric: Hypesthesia, abnormal vision, abnormal dreams, and retinal disorder.
Respiratory: Upper respiratory infection*, epistaxis, bronchitis, rhinitis*, sinusitis*, and voice alteration.
Other: Conjunctivitis, arthritis, urinary tract infection, alopecia, and urinary frequency*.
Fetal/Neonatal Morbidity and Mortality: See WARNINGS, Fetal/Neonatal Morbidity and Mortality.
Monotherapy with benazepril has been evaluated for safety in over 6000 patients. In clinical trials, the observed adverse reactions to benazepril were similar to those seen in trials of benazepril hydrochloride and hydrochlorothiazide. In post-marketing experience with benazepril, there have been rare reports of Stevens-Johnson syndrome, pancreatitis, hemolytic anemia, pemphigus, and thrombocytopenia. Another potentially important adverse experience, eosinophilic pneumonitis, has been attributed to other ACE inhibitors.
Hydrochlorothiazide has been extensively prescribed for many years, but there has not been enough systematic collection of data to support an estimate of the frequency of the observed adverse reactions. Within organ-system groups, the reported reactions are listed here in decreasing order of severity, without regard to frequency.
Unknown Frequency: small bowel angioedema, anaphylactoid reactions, hyperkalemia, agranulocytosis, neutropenia.
Cardiovascular: Orthostatic hypotension (may be potentiated by alcohol, barbiturates, or narcotics).
Digestive: Pancreatitis, jaundice (intrahepatic cholestatic) (see WARNINGS), sialadenitis, vomiting, diarrhea, cramping, nausea, gastric irritation, constipation, and anorexia.
Neurologic: Vertigo, lightheadedness, transient blurred vision, headache, paresthesia, xanthopsia, weakness, and restlessness.
Musculoskeletal: Muscle spasm.
Hematologic: Aplastic anemia, agranulocytosis, leukopenia, and thrombocytopenia.
Metabolic: Hyperglycemia, glycosuria, and hyperuricemia.
Hypersensitivity: Necrotizing angiitis, respiratory distress (including pneumonitis and pulmonary edema), purpura, urticaria, rash, and photosensitivity.
Skin: Erythema multiforme including Stevens-Johnson syndrome, exfoliative dermatitis including toxic epidermal necrolysis.
Clinical Laboratory Test Findings
Serum Electrolytes
See PRECAUTIONS.
Creatinine
Minor reversible increases in serum creatinine were observed in patients with essential hypertension treated with benazepril hydrochloride and hydrochlorothiazide. Such increases occurred most frequently in patients with renal artery stenosis (see PRECAUTIONS).
Other (Causal Relationships Unknown)
Other clinically important changes in standard laboratory tests were rarely associated with benazepril hydrochloride and hydrochlorothiazide administration. Elevations in blood urea nitrogen, uric acid, glucose, SGOT, and SGPT have been reported (see WARNINGS). In the somewhat larger patient population exposed to benazepril monotherapy in U.S. trials, the same abnormalities were reported, together with scattered accounts of hyponatremia, melena, electrocardiographic changes, leukopenia, eosinophilia, and proteinuria.
-
OVERDOSAGE
No specific information is available on the treatment of overdosage with benazepril hydrochloride and hydrochlorothiazide; treatment should be symptomatic and supportive. Therapy with benazepril hydrochloride and hydrochlorothiazide should be discontinued, and the patient should be observed. Dehydration, electrolyte imbalance, and hypotension should be treated by established procedures.
Single oral doses of 1 g/kg of benazepril caused reduced activity in mice, and doses of 3 g/kg were associated with significant lethality. Reduction of activity in rats was not seen until they had received doses of 5 g/kg, and doses of 6 g/kg were not lethal. In single-dose studies of hydrochlorothiazide, most rats survived doses up to 2.75 g/kg.
Data from human overdoses of benazepril are scanty, but the most common manifestation of human benazepril overdosage is likely to be hypotension. In human hydrochlorothiazide overdose, the most common signs and symptoms observed have been those of dehydration and electrolyte depletion (hypokalemia, hypochloremia, hyponatremia). If digitalis has also been administered, hypokalemia may accentuate cardiac arrhythmias.
Laboratory determinations of serum levels of benazepril and its metabolites are not widely available, and such determinations have, in any event, no established role in the management of benazepril overdose.
No data are available to suggest physiological maneuvers (e.g., maneuvers to change the pH of the urine) that might accelerate elimination of benazepril and its metabolites. Benazeprilat is only slightly dialyzable, but dialysis might be considered in overdosed patients with severely impaired renal function (see WARNINGS).
Angiotensin II could presumably serve as a specific antagonist-antidote in the setting of benazepril overdose, but angiotensin II is essentially unavailable outside of scattered research facilities. Because the hypotensive effect of benazepril is achieved through vasodilation and effective hypovolemia, it is reasonable to treat benazepril overdose by infusion of normal saline solution.
-
DOSAGE AND ADMINISTRATION
Benazepril is an effective treatment of hypertension in once-daily doses of 10 mg to 80 mg, while hydrochlorothiazide is effective in doses of 12.5 mg to 50 mg per day. In clinical trials of benazepril/hydrochlorothiazide combination therapy using benazepril doses of 5 mg to 20 mg and hydrochlorothiazide doses of 6.25 mg to 25 mg, the antihypertensive effects increased with increasing dose of either component.
The side effects (see WARNINGS) of benazepril are generally rare and apparently independent of dose; those of hydrochlorothiazide are a mixture of dose-dependent phenomena (primarily hypokalemia) and dose-independent phenomena (e.g., pancreatitis), the former much more common than the latter. Therapy with any combination of benazepril and hydrochlorothiazide will be associated with both sets of dose-independent side effects, but regimens in which benazepril is combined with low doses of hydrochlorothiazide produce minimal effects on serum potassium. In clinical trials of benazepril hydrochloride and hydrochlorothiazide tablets, the average change in serum potassium was near zero in subjects who received 5 mg/6.25 mg or 20 mg/12.5 mg, but the average subject who received 10 mg/12.5 mg or 20 mg/25 mg experienced a mild reduction in serum potassium, similar to that experienced by the average subject receiving the same dose of hydrochlorothiazide monotherapy.
To minimize dose-independent side effects, it is usually appropriate to begin combination therapy only after a patient has failed to achieve the desired effect with monotherapy.
Dose Titration Guided by Clinical Effect
A patient whose blood pressure is not adequately controlled with benazepril monotherapy may be switched to benazepril hydrochloride and hydrochlorothiazide tablets 10 mg/12.5 mg or 20 mg/12.5 mg. Further increases of either or both components could depend on clinical response. The hydrochlorothiazide dose should generally not be increased until 2 to 3 weeks have elapsed. Patients whose blood pressures are adequately controlled with 25 mg of daily hydrochlorothiazide, but who experience significant potassium loss with this regimen, may achieve similar blood-pressure control without electrolyte disturbance if they are switched to benazepril hydrochloride and hydrochlorothiazide tablets 5 mg/6.25 mg.
Use in Renal Impairment
Regimens of therapy with benazepril hydrochloride and hydrochlorothiazide tablets need not take account of renal function as long as the patient's creatinine clearance is > 30 mL/min/1.73 m2 (serum creatinine roughly ≤ 3 mg/dL or 265 µmol/L). In patients with more severe renal impairment, loop diuretics are preferred to thiazides, so benazepril hydrochloride and hydrochlorothiazide tablets are not recommended (see WARNINGS).
-
HOW SUPPLIED
Benazepril Hydrochloride and Hydrochlorothiazide Tablets, for oral administration, are available as:
5 mg/6.25 mg: White to off-white, oblong, film-coated tablets, debossed "E 124" on one side and scored on the other side and supplied as:
NDC: 0185-0124-01 bottles of 100
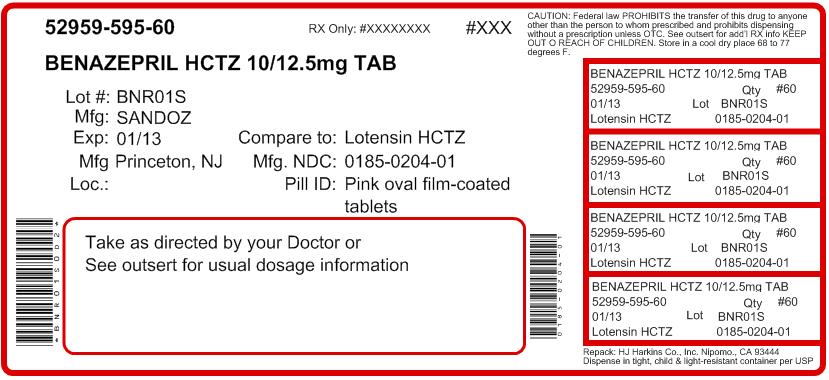
10 mg/12.5 mg: Pink, oblong, film-coated tablets, debossed "E 204" on one side and scored on the other side and supplied as:
NDC: 0185-0204-01 bottles of 100
20 mg/12.5 mg: Lavender, oblong, film-coated tablets, debossed "E 211" on one side and scored on the other side and supplied as:
NDC: 0185-0211-01 bottles of 100
20 mg/25 mg: Maroon, oblong, film-coated tablets, debossed "E 277" on one side and scored on the other side and supplied as:
NDC: 0185-0277-01 bottles of 100
Each strength is supplied in bottles that contain a desiccant.
Store at 20º to 25ºC (68º to 77ºF) [see USP Controlled Room Temperature]. Protect from light and moisture.
Dispense contents in a tight, light-resistant container as defined in the USP with a child-resistant closure, as required.
To report SUSPECTED ADVERSE REACTIONS, contact Sandoz Inc. at 1-800-525-8747 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Sandoz Inc.
Princeton, NJ 08540
OS8023
Rev. 10/11
Repacked by:
H.J. Harkins Company, Inc.
Nipomo, CA 93444
MF0124REV07/11
MG #18758
-
Benazepril Hydrochloride and Hydrochlorothiazide Tablets, 10 mg/12.5 mg x 100 Tablets - Label
NDC: 0185-0204-01
Benazepril Hydrochloride and Hydrochlorothiazide Tablets
10 mg/12.5 mg
Rx only
100 Tablets
Sandoz
-
INGREDIENTS AND APPEARANCE
BENAZEPRIL HYDROCHLORIDE AND HYDROCHLOROTHIAZIDE
benazepril hydrochloride and hydrochlorothiazide tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 52959-595(NDC: 0185-0204) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BENAZEPRIL HYDROCHLORIDE (UNII: N1SN99T69T) (BENAZEPRILAT - UNII:JRM708L703) BENAZEPRIL HYDROCHLORIDE 10 mg HYDROCHLOROTHIAZIDE (UNII: 0J48LPH2TH) (HYDROCHLOROTHIAZIDE - UNII:0J48LPH2TH) HYDROCHLOROTHIAZIDE 12.5 mg Inactive Ingredients Ingredient Name Strength COLLOIDAL SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 68401960MK) D&C RED NO. 27 (UNII: 2LRS185U6K) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) POLOXAMER 188 (UNII: LQA7B6G8JG) POLYETHYLENE GLYCOL (UNII: 3WJQ0SDW1A) POLYSORBATE 80 (UNII: 6OZP39ZG8H) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) ZINC STEARATE (UNII: H92E6QA4FV) HYDROGENATED CASTOR OIL (UNII: ZF94AP8MEY) Product Characteristics Color PINK Score 2 pieces Shape OVAL Size 13mm Flavor Imprint Code E204 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 52959-595-60 60 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076631 02/11/2004 Labeler - H.J. Harkins Company, Inc. (147681894) Establishment Name Address ID/FEI Business Operations Eon Labs, Inc. 012656273 manufacture
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.