MEDROXYPROGESTERONE ACETATE injection, suspension
medroxyprogesterone acetate by
Drug Labeling and Warnings
medroxyprogesterone acetate by is a Prescription medication manufactured, distributed, or labeled by Amneal Pharmaceuticals LLC, Amneal Pharmaceuticals of New York, LLC, Laboratorios Farmalan, S.A.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use MEDROXYPROGESTERONE ACETATE INJECTABLE SUSPENSION safely and effectively. See full prescribing information for MEDROXYPROGESTERONE ACETATE INJECTABLE SUSPENSION.
MEDROXYPROGESTERONE ACETATE injectable suspension, for intramuscular use
Initial U.S. Approval: 1959WARNING: LOSS OF BONE MINERAL DENSITY
See full prescribing information for complete boxed warning.
-
Women who use medroxyprogesterone acetate injectable suspension may lose significant bone mineral density. Bone loss is greater with increasing duration of use and may not be completely reversible. (5.1)
-
It is unknown if use of medroxyprogesterone acetate injectable suspension during adolescence or early adulthood, a critical period of bone accretion, will reduce peak bone mass and increase the risk for osteoporotic fracture in later life. (5.1)
-
Medroxyprogesterone acetate injectable suspension is not recommended as a long-term (i.e. longer than 2 years) birth control method unless other options are considered inadequate. (1, 5.1)
RECENT MAJOR CHANGES
Warnings and Precautions, Meningioma (5.4) 12/2025
INDICATIONS AND USAGE
Medroxyprogesterone acetate injectable suspension is a progestin indicated for use by females of reproductive potential to prevent pregnancy. (1)
Limitations of Use:
The use of medroxyprogesterone acetate injectable suspension is not recommended as a long-term (i.e., longer than 2 years) birth control method unless other options are considered inadequate. (1, 5.1)
DOSAGE AND ADMINISTRATION
The recommended dose is 150 mg of medroxyprogesterone acetate injectable suspension every 3 months (13 weeks) administered by deep, intramuscular (IM) injection in the gluteal or deltoid muscle. (2.1)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
- Active thrombophlebitis, or current or past history of thromboembolic disorders, or cerebral vascular disease. (4)
- Known or suspected malignancy of breast. (4)
- Known hypersensitivity to medroxyprogesterone acetate injectable suspension (medroxyprogesterone acetate or any of its other ingredients). (4)
- Significant liver disease. (4)
- Undiagnosed vaginal bleeding. (4)
WARNINGS AND PRECAUTIONS
- Thromboembolic Disorders: Discontinue medroxyprogesterone acetate in patients who develop thrombosis. (5.2)
- Cancer Risks: Monitor women with a strong family history of breast cancer carefully. (5.3)
- Meningioma: Discontinue medroxyprogesterone acetate if meningioma is diagnosed. Monitor patients for signs and symptoms of meningioma. (5.4)
- Ectopic Pregnancy: Consider ectopic pregnancy if a woman using medroxyprogesterone acetate becomes pregnant or complains of severe abdominal pain. (5.5)
- Anaphylaxis and Anaphylactoid Reactions: Provide emergency medical treatment. (5.6)
- Liver Function: Discontinue medroxyprogesterone acetate if jaundice or disturbances of liver function develop. (5.8)
- Carbohydrate Metabolism: Monitor diabetic patients carefully. (5.13)
ADVERSE REACTIONS
Most common adverse reactions (incidence > 5%): menstrual irregularities (bleeding or spotting) 57% at 12 months, 32% at 24 months, abdominal pain/discomfort 11%, weight gain > 10 lb at 24 months 38%, dizziness 6%, headache 17%, nervousness 11%, decreased libido 6%. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Amneal Pharmaceuticals LLC at 1-877-835-5472 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
Drugs or herbal products that induce certain enzymes, including CYP3A4, may decrease the effectiveness of contraceptive drug products. Counsel patients to use a back-up method or alternative method of contraception when enzyme inducers are used with medroxyprogesterone acetate. (7.1)
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 1/2026
-
Women who use medroxyprogesterone acetate injectable suspension may lose significant bone mineral density. Bone loss is greater with increasing duration of use and may not be completely reversible. (5.1)
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: LOSS OF BONE MINERAL DENSITY
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Prevention of Pregnancy
2.2 Switching from Other Methods of Contraception
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Loss of Bone Mineral Density
5.2 Thromboembolic Disorders
5.3 Cancer Risks
5.4 Meningioma
5.5 Ectopic Pregnancy
5.6 Anaphylaxis and Anaphylactoid Reaction
5.7 Injection Site Reactions
5.8 Liver Function
5.9 Convulsions
5.10 Depression
5.11 Bleeding Irregularities
5.12 Weight Gain
5.13 Carbohydrate Metabolism
5.14 Fluid Retention
5.15 Return of Fertility
5.16 Sexually Transmitted Infections
5.17 Monitoring
5.18 Interference with Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-Marketing Experience
7 DRUG INTERACTIONS
7.1 Changes in Contraceptive Effectiveness Associated with Co-Administration of Other Products
7.2 Laboratory Test Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Contraception
14.2 Bone Mineral Density Changes in Women Treated with Medroxyprogesterone Acetate
14.3 Bone Mineral Density Changes in Adolescent Females (12 to 18 Years of Age) Treated with Medroxyprogesterone Acetate
14.4 Bone Fracture Incidence in Women Treated with Medroxyprogesterone Acetate
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: LOSS OF BONE MINERAL DENSITY
- Women who use medroxyprogesterone acetate injectable suspension may lose significant bone mineral density. Bone loss is greater with increasing duration of use and may not be completely reversible [see Warnings and Precautions (5.1)].
- It is unknown if use of medroxyprogesterone acetate injectable suspension during adolescence or early adulthood, a critical period of bone accretion, will reduce peak bone mass and increase the risk for osteoporotic fracture in later life [see Warnings and Precautions (5.1)].
- Medroxyprogesterone acetate injectable suspension is not recommended as a long-term (i.e. longer than 2 years) birth control method unless other options are considered inadequate [see Indications and Usage (1) and Warnings and Precautions (5.1)].
-
1 INDICATIONS AND USAGE
Medroxyprogesterone acetate injectable suspension is indicated for use by females of reproductive potential to prevent pregnancy.
Limitations of Use:
The use of medroxyprogesterone acetate injectable suspension is not recommended as a long-term (i.e. longer than 2 years) birth control method unless other options are considered inadequate [see Dosage and Administration (2.1) and Warnings and Precautions (5.1)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Prevention of Pregnancy
Both the 1 mL vial and the 1 mL prefilled syringe of medroxyprogesterone acetate injectable suspension should be vigorously shaken just before use to ensure that the dose being administered represents a uniform suspension.
The recommended dose is 150 mg of medroxyprogesterone acetate injectable suspension every 3 months (13 weeks) administered by deep intramuscular (IM) injection using strict aseptic technique in the gluteal or deltoid muscle, rotating the sites with every injection. As with any IM injection, to avoid an inadvertent subcutaneous injection, body habitus should be assessed prior to each injection to determine if a longer needle is necessary particularly for gluteal IM injection.
Use for longer than 2 years is not recommended (unless other birth control methods are considered inadequate) due to the impact of long-term medroxyprogesterone acetate injectable suspension treatment on bone mineral density (BMD) [see Warnings and Precautions (5.1)]. Dosage does not need to be adjusted for body weight [see Clinical Studies (14.1)].
To ensure the patient is not pregnant at the time of the first injection, the first injection should be given ONLY during the first 5 days of a normal menstrual period or within the first 5-days post-partum. In post-partum mothers who exclusively breastfeed, administer medroxyprogesterone acetate injectable suspension during or after the sixth post-partum week. If the time interval between injections is greater than 13 weeks, the physician should determine that the patient is not pregnant before administering the drug. The efficacy of medroxyprogesterone acetate injectable suspension depends on adherence to the dosage schedule of administration.
2.2 Switching from Other Methods of Contraception
When switching from other contraceptive methods, medroxyprogesterone acetate injectable suspension should be given in a manner that ensures continuous contraceptive coverage based upon the mechanism of action of both methods, (e.g., patients switching from oral contraceptives should have their first injection of medroxyprogesterone acetate injectable suspension on the day after the last active tablet or at the latest, on the day following the final inactive tablet).
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
The use of medroxyprogesterone acetate injectable suspension is contraindicated in the following conditions:
- Active thrombophlebitis, or current or history of thromboembolic disorders, or cerebral vascular disease [see Warnings and Precautions (5.2)].
- Known or suspected malignancy of breast [see Warnings and Precautions (5.3)].
- Known hypersensitivity to medroxyprogesterone acetate injectable suspension (medroxyprogesterone acetate) or any of its other ingredients [see Warnings and Precautions (5.6)].
- Significant liver disease [see Warnings and Precautions (5.8)].
- Undiagnosed vaginal bleeding [see Warnings and Precautions (5.11)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Loss of Bone Mineral Density
Use of medroxyprogesterone acetate reduces serum estrogen levels and is associated with significant loss of bone mineral density (BMD). This loss of BMD is of particular concern during adolescence and early adulthood, a critical period of bone accretion. It is unknown if use of medroxyprogesterone acetate by younger women will reduce peak bone mass and increase the risk for osteoporotic fracture in later life.
A study to assess the reversibility of loss of BMD in adolescents was conducted with medroxyprogesterone acetate. After discontinuing medroxyprogesterone acetate in these adolescents, mean BMD loss at the total hip and femoral neck did not fully recover by 5 years (60 months) post-treatment in the sub-group of adolescents who were treated for more than 2 years [see Clinical Studies (14.3)]. Similarly, in adults, there was only partial recovery of mean BMD at the total hip, femoral neck, and lumbar spine towards baseline by 2 years post-treatment [see Clinical Studies (14.2)].
The use of medroxyprogesterone acetate is not recommended as a long-term (i.e. longer than 2 years) birth control method unless other options are considered inadequate. BMD should be evaluated when a woman needs to continue to use medroxyprogesterone acetate long-term. In adolescents, interpretation of BMD results should take into account patient age and skeletal maturity.
Other birth control methods should be considered in the risk/benefit analysis for the use of medroxyprogesterone acetate in women with osteoporosis risk factors. Medroxyprogesterone acetate can pose an additional risk in patients with risk factors for osteoporosis (e.g., metabolic bone disease, chronic alcohol and/or tobacco use, anorexia nervosa, strong family history of osteoporosis or chronic use of drugs that can reduce bone mass such as anticonvulsants or corticosteroids).
5.2 Thromboembolic Disorders
There have been reports of serious thrombotic events in women using medroxyprogesterone acetate (150 mg). However, medroxyprogesterone acetate has not been causally associated with the induction of thrombotic or thromboembolic disorders. Any patient who develops thrombosis while undergoing therapy with medroxyprogesterone acetate should discontinue treatment unless she has no other acceptable options for birth control.
Do not re-administer medroxyprogesterone acetate pending examination if there is a sudden partial or complete loss of vision or if there is a sudden onset of proptosis, diplopia, or migraine. Do not re-administer if examination reveals papilledema or retinal vascular lesions.
5.3 Cancer Risks
Breast Cancer
Women who have or have had a history of breast cancer should not use hormonal contraceptives, including medroxyprogesterone acetate, because breast cancer may be hormonally sensitive [see Contraindications (4)]. Women with a strong family history of breast cancer should be monitored with particular care.
The results of five large case-control studies assessing the association between depo-medroxyprogesterone acetate (DMPA) use and the risk of breast cancer are summarized in Figure 1. Three of the studies suggest a slightly increased risk of breast cancer in the overall population of users; these increased risks were statistically significant in one study. One recent US study1 evaluated the recency and duration of use and found a statistically significantly increased risk of breast cancer in recent users (defined as last use within the past five years) who used DMPA for 12 months or longer; this is consistent with results of a previous study2.
Figure 1: Risk estimates for breast cancer in DMPA users
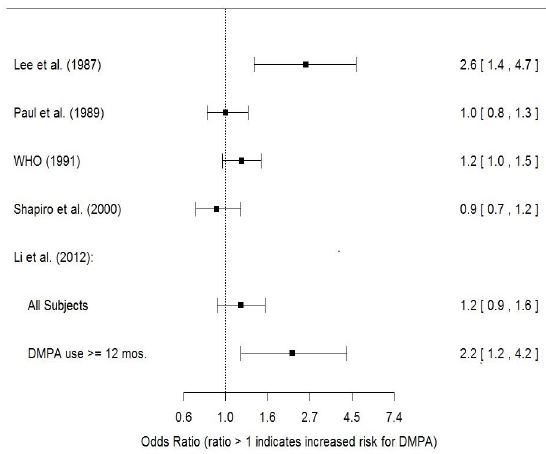
Odds ratio estimates were adjusted for the following covariates:
Lee et al. (1987): age, parity, and socioeconomic status.
Paul et al. (1989): age, parity, ethnic group, and year of interview.
WHO (1991): age, center, and age at first live birth.
Shapiro et al. (2000): age, ethnic group, socioeconomic status, and any combined estrogen/progestogen oral contraceptive use.
Li et al. (2012): age, year, BMI, duration of OC use, number of full-term pregnancies, family history of breast cancer, and history of screening mammography.
Based on the published SEER-18 2011 incidence rate (age-adjusted to the 2,000 US Standard Population) of breast cancer for US women, all races, age 20 to 49 years, a doubling of risk would increase the incidence of breast cancer in women who use medroxyprogesterone acetate from about 72 to about 144 cases per 100,000 women.
Cervical Cancer
A statistically nonsignificant increase in relative risk (RR) estimates of invasive squamous-cell cervical cancer has been associated with the use of medroxyprogesterone acetate in women who were first exposed before the age of 35 years (RR 1.22 to 1.28 and 95% CI 0.93 to 1.70). The overall, nonsignificant RR of invasive squamous-cell cervical cancer in women who ever used medroxyprogesterone acetate was estimated to be 1.11 (95% CI 0.96 to 1.29). No trends in risk with duration of use or times since initial or most recent exposure were observed.
Other Cancers
Long-term case-controlled surveillance of users of medroxyprogesterone acetate found no overall increased risk of ovarian or liver cancer.
5.4 Meningioma
Cases of meningiomas have been reported following repeated administration of medroxyprogesterone acetate, primarily with long term use. Monitor patients on medroxyprogesterone acetate for signs and symptoms of meningioma. Discontinue medroxyprogesterone acetate if a meningioma is diagnosed.
5.5 Ectopic Pregnancy
Be alert to the possibility of an ectopic pregnancy among women using medroxyprogesterone acetate who become pregnant or complain of severe abdominal pain.
5.6 Anaphylaxis and Anaphylactoid Reaction
Anaphylaxis and anaphylactoid reaction have been reported with the use of medroxyprogesterone acetate. Institute emergency medical treatment if an anaphylactic reaction occurs.
5.7 Injection Site Reactions
Injection site reactions have been reported with use of medroxyprogesterone acetate [see Adverse Reactions (6.2)]. Persistent injection site reactions may occur after administration of medroxyprogesterone acetate due to inadvertent subcutaneous administration or release of the drug into the subcutaneous space while removing the needle [see Dosage and Administration (2.1)].
5.8 Liver Function
Discontinue medroxyprogesterone acetate use if jaundice or acute or chronic disturbances of liver function develop. Do not resume use until markers of liver function return to normal and medroxyprogesterone acetate causation has been excluded.
5.9 Convulsions
There have been a few reported cases of convulsions in patients who were treated with medroxyprogesterone acetate. Association with drug use or pre-existing conditions is not clear.
5.10 Depression
Monitor patients who have a history of depression and do not re-administer medroxyprogesterone acetate if depression recurs.
5.11 Bleeding Irregularities
Most women using medroxyprogesterone acetate experience disruption of menstrual bleeding patterns. Altered menstrual bleeding patterns include amenorrhea, irregular or unpredictable bleeding or spotting, prolonged spotting or bleeding, and heavy bleeding. Rule out the possibility of organic pathology if abnormal bleeding persists or is severe, and institute appropriate treatment.
As women continue using medroxyprogesterone acetate, fewer experience irregular bleeding and more experience amenorrhea. In clinical studies of medroxyprogesterone acetate, by month 12 amenorrhea was reported by 55% of women, and by month 24, amenorrhea was reported by 68% of women using medroxyprogesterone acetate.
5.12 Weight Gain
Women tend to gain weight while on therapy with medroxyprogesterone acetate. From an initial average body weight of 136 lb, women who completed 1 year of therapy with medroxyprogesterone acetate gained an average of 5.4 lb. Women who completed 2 years of therapy gained an average of 8.1 lb. Women who completed 4 years gained an average of 13.8 lb. Women who completed 6 years gained an average of 16.5 lb. Two percent of women withdrew from a large-scale clinical trial because of excessive weight gain.
5.13 Carbohydrate Metabolism
A decrease in glucose tolerance has been observed in some patients on medroxyprogesterone acetate treatment. Monitor diabetic patients carefully while receiving medroxyprogesterone acetate.
5.14 Fluid Retention
Because progestational drugs including medroxyprogesterone acetate may cause some degree of fluid retention, monitor patients with conditions that might be influenced by this condition, such as epilepsy, migraine, asthma, and cardiac or renal dysfunction.
5.15 Return of Fertility
Return to ovulation and fertility is likely to be delayed after stopping medroxyprogesterone acetate. In a large US study of women who discontinued use of medroxyprogesterone acetate to become pregnant, data are available for 61% of them. Of the 188 women who discontinued the study to become pregnant, 114 became pregnant. Based on Life-Table analysis of these data, it is expected that 68% of women who do become pregnant may conceive within 12 months, 83% may conceive within 15 months, and 93% may conceive within 18 months from the last injection. The median time to conception for those who do conceive is 10 months following the last injection with a range of 4 to 31 months, and is unrelated to the duration of use. No data are available for 39% of the patients who discontinued medroxyprogesterone acetate to become pregnant and who were lost to follow-up or changed their mind.
5.16 Sexually Transmitted Infections
Patients should be counseled that medroxyprogesterone acetate does not protect against HIV infection (AIDS) and other sexually transmitted infections.
5.17 Monitoring
A woman who is taking hormonal contraceptive should have a yearly visit with her healthcare professional for a blood pressure check and for other indicated healthcare.
5.18 Interference with Laboratory Tests
The use of medroxyprogesterone acetate may change the results of some laboratory tests, such as coagulation factors, lipids, glucose tolerance, and binding proteins [see Drug Interactions (7.2)].
-
6 ADVERSE REACTIONS
The following important adverse reactions observed with the use of medroxyprogesterone acetate are discussed in greater detail in the Warnings and Precautions section(5):
- Loss of Bone Mineral Density [see Warnings and Precautions (5.1)]
- Thromboembolic disease [see Warnings and Precautions (5.2)]
- Breast Cancer [see Warnings and Precautions (5.3)]
- Anaphylaxis and Anaphylactoid Reactions [see Warnings and Precautions (5.6)]
- Bleeding Irregularities [see Warnings and Precautions (5.11)]
- Weight Gain [see Warnings and Precautions (5.12)]
6.1 Clinical Trials Experience
Clinical trials are conducted under widely varying conditions, therefore, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In the two clinical trials with medroxyprogesterone acetate, over 3,900 women, who were treated for up to 7 years, reported the following adverse reactions, which may or may not be related to the use of medroxyprogesterone acetate. The population studied ranges in age from 15 to 51 years, of which 46% were White, 50% Non-White, and 4.9% Unknown race. The patients received 150 mg medroxyprogesterone acetate every 3-months (90 days). The median study duration was 13 months with a range of 1 to 84 months. Fifty-eight percent of patients remained in the study after 13 months and 34% after 24 months.
Table 1: Adverse Reactions that Were Reported by More than 5% of Subjects
Body System*
Adverse Reactions [Incidence (%)]
Body as a Whole
Headache (16.5%)
Abdominal pain/discomfort (11.2%)
Metabolic/Nutritional
Increased weight > 10 lb at 24 months (37.7%)
Nervous
Nervousness (10.8%)
Dizziness (5.6%)
Libido decreased (5.5%)
Reproductive (Urogenital*)
Menstrual irregularities:
bleeding (57.3% at 12 months, 32.1% at 24 months)
amenorrhea (55% at 12 months, 68% at 24 months)
*Body System represented from COSTART medical dictionary.
Table 2: Adverse Reactions that Were Reported by between 1% and 5% of Subjects
Body System*
Adverse Reactions [Incidence (%)]
Body as a Whole
Asthenia/fatigue (4.2%)
Backache (2.2%)
Dysmenorrhea (1.7%)
Hot flashes (1.0%)
Digestive
Nausea (3.3%)
Bloating (2.3%)
Metabolic/Nutritional
Edema (2.2%)
Musculoskeletal
Leg cramps (3.7%)
Arthralgia (1.0%)
Nervous
Depression (1.5%)
Insomnia (1.0%)
Skin and Appendages
Acne (1.2%)
No hair growth/alopecia (1.1%)
Rash (1.1%)
Reproductive (Urogenital*)
Leukorrhea (2.9%)
Breast pain (2.8%)
Vaginitis (1.2%)
*Body System represented from COSTART medical dictionary.
Adverse reactions leading to study discontinuation in ≥ 2% of subjects: bleeding (8.2%), amenorrhea (2.1%), weight gain (2%).
6.2 Post-Marketing Experience
The following adverse reactions have been identified during post approval use of medroxyprogesterone acetate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
There have been cases of osteoporosis including osteoporotic fractures reported post-marketing in patients taking medroxyprogesterone acetate.
Table 3: Adverse Reactions Reported during Post-Marketing Experience
Body System*
Adverse Reactions
Body as a Whole
Chest pain, Allergic reactions including angioedema, Fever, Injection site abscess†, Injection site infection†, Injection site nodule/lump, Injection site pain/tenderness, Injection site persistent atrophy/indentation/dimpling, Injection-site reaction, Lipodystrophy acquired, Chills, Axillary swelling
Cardiovascular
Syncope, Tachycardia, Thrombophlebitis, Deep vein thrombosis, Pulmonary embolus, Varicose veins
Digestive
Changes in appetite, Gastrointestinal disturbances, Jaundice, Excessive thirst, Rectal bleeding
Hematologic and Lymphatic
Anemia, Blood dyscrasia
Musculoskeletal
Osteoporosis
Neoplasms
Cervical cancer, Breast cancer
Nervous
Paralysis, Facial palsy, Paresthesia, Drowsiness
Respiratory
Dyspnea and asthma, Hoarseness
Skin and Appendages
Hirsutism, Excessive sweating and body odor, Dry skin, Scleroderma, Melasma, Chloasma
Reproductive (Urogenital*)
Lack of return to fertility, Unexpected pregnancy, Changes in breast size, Breast lumps or nipple bleeding, Galactorrhea, Increased libido, Uterine hyperplasia, Vaginal cysts, Genitourinary infections, Dyspareunia
*Body System represented from COSTART medical dictionary.
†Injection site abscess and injection site infections have been reported; therefore, strict aseptic injection technique should be followed when administering medroxyprogesterone acetate in order to avoid injection site infections [see Dosage and Administration (2.1)]. -
7 DRUG INTERACTIONS
7.1 Changes in Contraceptive Effectiveness Associated with Co-Administration of Other Products
If a woman on hormonal contraceptives takes a drug or herbal product that induces enzymes, including CYP3A4, that metabolize contraceptive hormones, counsel her to use additional contraception or a different method of contraception. Drugs or herbal products that induce such enzymes may decrease the plasma concentrations of contraceptive hormones, and may decrease the effectiveness of hormonal contraceptives. Some drugs or herbal products that may decrease the effectiveness of hormonal contraceptives include:
- barbiturates
- bosentan
- carbamazepine
- felbamate
- griseofulvin
- oxcarbazepine
- phenytoin
- rifampin
- St. John’s wort
- topiramate
HIV protease inhibitors and non-nucleoside reverse transcriptase inhibitors: Significant changes (increase or decrease) in the plasma levels of progestin have been noted in some cases of co-administration of HIV protease inhibitors. Significant changes (increase or decrease) in the plasma levels of the progestin have been noted in some cases of co-administration with non-nucleoside reverse transcriptase inhibitors.
Antibiotics: There have been reports of pregnancy while taking hormonal contraceptives and antibiotics, but clinical pharmacokinetic studies have not shown consistent effects of antibiotics on plasma concentrations of synthetic steroids.
Consult the labeling of all concurrently-used drugs to obtain further information about interactions with hormonal contraceptives or the potential for enzyme alterations.
7.2 Laboratory Test Interactions
The pathologist should be advised of progestin therapy when relevant specimens are submitted.
The following laboratory tests may be affected by progestins including medroxyprogesterone acetate:
(a) Plasma and urinary steroid levels are decreased (e.g., progesterone, estradiol, pregnanediol, testosterone, cortisol).
(b) Gonadotropin levels are decreased.
(c) Sex-hormone-binding-globulin concentrations are decreased.
(d) Protein-bound iodine and butanol extractable protein-bound iodine may increase. T3-uptake values may decrease.
(e) Coagulation test values for prothrombin (Factor II), and Factors VII, VIII, IX, and X may increase.
(f) Sulfobromophthalein and other liver function test values may be increased.
(g) The effects of medroxyprogesterone acetate on lipid metabolism are inconsistent. Both increases and decreases in total cholesterol, triglycerides, low-density lipoprotein (LDL) cholesterol, and high-density lipoprotein (HDL) cholesterol have been observed in studies.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There is no use for contraception in pregnancy; therefore, medroxyprogesterone acetate should be discontinued during pregnancy.
Epidemiologic studies and meta-analyses have not found an increased risk of genital or non-genital birth defects (including cardiac anomalies and limb-reduction defects) following exposure to progestins before conception or during early pregnancy.
All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
8.2 Lactation
Risk Summary
Although medroxyprogesterone acetate is detectable in the milk of mothers receiving medroxyprogesterone acetate, milk composition, quality, and amount do not appear to be adversely affected. Effects on milk production and lactation initiation/duration remain unclear when administered before 6 weeks after delivery, therefore, in mothers who exclusively breastfeed, initiate medroxyprogesterone acetate during or after the sixth post-partum week [see Dosage and Administration (2.1)].
No adverse effects in breastfed infants would be expected with maternal use of progestins. Neonates and infants exposed to medroxyprogesterone acetate from breast milk have been studied and no adverse effects have been noted.
The developmental and health benefits of breast-feeding should be considered along with the mother’s clinical need for medroxyprogesterone acetate and any potential adverse effects on the breastfed child from medroxyprogesterone acetate or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Medroxyprogesterone acetate is indicated for the prevention of pregnancy and would therefore be expected to impair female fertility until cessation of treatment. Women may experience a delay in return to ovulation and fertility (conception) following discontinuation of medroxyprogesterone acetate [see Warnings and Precautions (5.15)].
8.4 Pediatric Use
Medroxyprogesterone acetate is not indicated before menarche. Use of medroxyprogesterone acetate is associated with significant loss of BMD. This loss of BMD is of particular concern during adolescence and early adulthood, a critical period of bone accretion. In adolescents, interpretation of BMD results should take into account patient age and skeletal maturity. It is unknown if use of medroxyprogesterone acetate by younger women will reduce peak bone mass and increase the risk of osteoporotic fractures in later life. Other than concerns about loss of BMD, the safety and effectiveness are expected to be the same for postmenarchal adolescents and adult women.
-
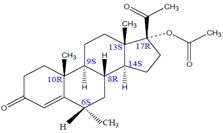
11 DESCRIPTION
Medroxyprogesterone Acetate Injectable Suspension, USP contains medroxyprogesterone acetate, USP, a derivative of progesterone, as its active ingredient. Medroxyprogesterone acetate, USP is active by the parenteral and oral routes of administration. It is a white to almost white; microcrystalline powder that is stable in air and that melts between 205°C and 209°C. It is freely soluble in chloroform and methylene chloride, soluble in acetone and dioxane, sparingly soluble in alcohol and methanol, slightly soluble in ether, and insoluble in water.
The chemical name for medroxyprogesterone acetate, USP is pregn-4-ene-3,20-dione,17-(acetyloxy)-6-methyl-, (6α)-17-hydroxy-6α-methylpregn-4-ene-3,20-dione acetate.
The structural formula is as follows:
Medroxyprogesterone acetate injectable suspension, USP, for intramuscular (IM) injection is available in vials and prefilled syringes, each containing 1 mL of medroxyprogesterone acetate sterile aqueous suspension 150 mg/mL.
Medroxyprogesterone acetate injectable suspension, USP vials and prefilled syringes:
Each mL of sterile aqueous suspension contains:
Medroxyprogesterone acetate, USP 150 mg
Polyethylene glycol 3350 28.9 mg
Polysorbate 80 2.41 mg
Sodium chloride 8.68 mg
Methylparaben 1.37 mg
Propylparaben 0.150 mg
Water for injection quantity sufficient
When necessary, pH is adjusted with sodium hydroxide or hydrochloric acid, or both.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Medroxyprogesterone acetate (MPA) inhibits the secretion of gonadotropins which primarily prevents follicular maturation and ovulation and causes thickening of cervical mucus. These actions contribute to its contraceptive effect.
12.2 Pharmacodynamics
No specific pharmacodynamic studies were conducted with medroxyprogesterone acetate.
12.3 Pharmacokinetics
Absorption
Following a single 150 mg IM dose of medroxyprogesterone acetate in eight women between the ages of 28 and 36 years old, medroxyprogesterone acetate concentrations, measured by an extracted radioimmunoassay procedure, increase for approximately 3 weeks to reach peak plasma concentrations of 1 ng/mL to 7 ng/mL.
Distribution
Plasma protein binding of MPA averages 86%. MPA binding occurs primarily to serum albumin. No binding of MPA occurs with sex-hormone-binding globulin (SHBG).
Elimination
Metabolism
MPA is extensively metabolized in the liver by P450 enzymes. Its metabolism primarily involves ring A and/or side-chain reduction, loss of the acetyl group, hydroxylation in the 2-, 6-, and 21-positions or a combination of these positions, resulting in more than 10 metabolites.
Excretion
The concentrations of medroxyprogesterone acetate decrease exponentially until they become undetectable (< 100 pg/mL) between 120 to 200 days following injection. Using an unextracted radioimmunoassay procedure for the assay of medroxyprogesterone acetate in serum, the apparent half-life for medroxyprogesterone acetate following IM administration of medroxyprogesterone acetate is approximately 50 days. Most medroxyprogesterone acetate metabolites are excreted in the urine as glucuronide conjugates with only minor amounts excreted as sulfates.
Specific Populations
The effect of hepatic and/or renal impairment on the pharmacokinetics of medroxyprogesterone acetate is unknown.
- 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
14.1 Contraception
In five clinical studies using medroxyprogesterone acetate, the 12-month failure rate for the group of women treated with medroxyprogesterone acetate was zero (no pregnancies reported) to 0.7 by Life-Table method. The effectiveness of medroxyprogesterone acetate is dependent on the patient returning every 3 months (13 weeks) for reinjection.
14.2 Bone Mineral Density Changes in Women Treated with Medroxyprogesterone Acetate
In a controlled, clinical study, adult women using medroxyprogesterone acetate (150 mg) for up to 5 years showed spine and hip bone mineral density (BMD) mean decreases of 5% to 6%, compared to no significant change in BMD in the control group. The decline in BMD was more pronounced during the first two years of use, with smaller declines in subsequent years. Mean changes in lumbar spine BMD of -2.86%, -4.11%, -4.89%, -4.93% and -5.38% after 1, 2, 3, 4, and 5 years, respectively, were observed. Mean decreases in BMD of the total hip and femoral neck were similar.
After stopping use of medroxyprogesterone acetate, there was partial recovery of BMD toward baseline values during the 2-year post-therapy period. Longer duration of treatment was associated with less complete recovery during this 2-year period following the last injection. Table 4 shows the change in BMD in women after 5 years of treatment with medroxyprogesterone acetate and in women in a control group, as well as the extent of recovery of BMD for the subset of the women for whom 2-year post treatment data were available.
Table 4: Mean Percent Change from Baseline in BMD in Adults by Skeletal Site and Cohort (5 Years of Treatment and 2 Years of Follow-Up)
Time in Study
Spine
Total Hip
Femoral Neck
Medroxyprogesterone acetate*
Control**
Medroxyprogesterone acetate*
Control**
Medroxyprogesterone acetate*
Control**
5 years
-5.38%
n=33
0.43%
n=105
-5.16%
n=21
0.19%
n=65
-6.12%
n=34
-0.27%
n=106
7 years
-3.13%
n=12
0.53%
n=60
-1.34%
n=7
0.94%
n=39
-5.38%
n=13
-0.11%
n=63
*The treatment group consisted of women who received medroxyprogesterone acetate for 5 years and were then followed for 2 years post-use (total time in study of 7 years).
**The control group consisted of women who did not use hormonal contraception and were followed for 7 years.
14.3 Bone Mineral Density Changes in Adolescent Females (12 to 18 Years of Age) Treated with Medroxyprogesterone Acetate
The impact of medroxyprogesterone acetate (150 mg) use for up to 240 weeks (4.6 years) was evaluated in an open-label non-randomized clinical study in 389 adolescent females (12 to 18 years of age). Use of medroxyprogesterone acetate was associated with a significant decline from baseline in BMD.
Partway through the trial, drug administration was stopped (at 120 weeks). The mean number of injections per medroxyprogesterone acetate user was 9.3. Table 5 summarizes the study findings. The decline in BMD at total hip and femoral neck was greater with longer duration of use. The mean decrease in BMD at 240 weeks was more pronounced at total hip (-6.4%) and femoral neck (-5.4%) compared to lumbar spine (-2.1%).
Adolescents in the untreated cohort had an increase in BMD during the period of growth following menarche. However, the two cohorts were not matched at baseline for age, gynecologic age, race, BMD and other factors that influence the rate of acquisition of BMD.
Table 5: BMD Mean Percent Change from Baseline in Adolescents Receiving ≥ 4 Injections per 60-week Period, by Skeletal Site and Cohort
Duration of Treatment
Medroxyprogesterone acetate
(150 mg IM)
Unmatched, Untreated
Cohort
N
Mean % Change
N
Mean % Change
Total Hip BMD
Week 60 (1.2 years)
Week 120 (2.3 years)
Week 240 (4.6 years)
113
73
28
-2.75
-5.40
-6.40
166 109
84
1.22
2.19
1.71
Femoral Neck BMD
Week 60
Week 120
Week 240
113
73
28
-2.96
-5.30
-5.40
166 108
84
1.75
2.83
1.94
Lumbar Spine BMD
Week 60
Week 120
Week 240
114
73
27
-2.47
-2.74
-2.11
167 109
84
3.39
5.28
6.40
BMD Recovery Post-Treatment in Adolescents
Longer duration of treatment and smoking were associated with less recovery of BMD following the last injection of medroxyprogesterone acetate. Table 6 shows the extent of recovery of BMD up to 60 months post-treatment for adolescents who received medroxyprogesterone acetate for two years or less compared to more than two years. Post-treatment follow-up showed that, in women treated for more than two years, only lumbar spine BMD recovered to baseline levels after treatment was discontinued. Adolescents treated with medroxyprogesterone acetate for more than two years did not recover to their baseline BMD level at femoral neck and total hip even up to 60 months post-treatment. Adolescents in the untreated cohort gained BMD throughout the trial period (data not shown) [see Warnings and Precautions (5.1)].
Table 6: BMD Recovery (Months Post-Treatment) in Adolescents by Years of Medroxyprogesterone acetate Use (2 Years or Less vs. More than 2 Years)
Duration of Treatment
2 years or less
More than 2 years
N
Mean % Change from baseline
N
Mean % Change from baseline
Total Hip BMD
End of Treatment
49
-1.5%
49
-6.2%
12 M post-treatment
33
-1.4%
24
-4.6%
24 M post-treatment
18
0.3%
17
-3.6%
36 M post-treatment
12
2.1%
11
-4.6%
48 M post-treatment
10
1.3%
9
-2.5%
60 M post-treatment
3
0.2%
2
-1.0%
Femoral Neck BMD
End of Treatment
49
-1.6%
49
-5.8%
12 M post-treatment
33
-1.4%
24
-4.3%
24 M post-treatment
18
0.5%
17
-3.8%
36 M post-treatment
12
1.2%
11
-3.8%
48 M post-treatment
10
2.0%
9
-1.7%
60 M post-treatment
3
1.0%
2
-1.9%
Lumbar Spine BMD
End of Treatment
49
-0.9%
49
-3.5%
12 M post-treatment
33
0.4%
23
-1.1%
24 M post-treatment
18
2.6%
17
1.9%
36 M post-treatment
12
2.4%
11
0.6%
48 M post-treatment
10
6.5%
9
3.5%
60 M post-treatment
3
6.2%
2
5.7%
14.4 Bone Fracture Incidence in Women Treated with Medroxyprogesterone Acetate
A retrospective cohort study to assess the association between medroxyprogesterone acetate and the incidence of bone fractures was conducted in 312,395 female contraceptive users in the UK. The incidence rates of fracture were compared between medroxyprogesterone acetate users and contraceptive users who had no recorded use of medroxyprogesterone acetate. The Incident Rate Ratio (IRR) for any fracture during the follow-up period (mean = 5.5 years) was 1.41 (95% CI 1.35, 1.47). It is not known if this is due to medroxyprogesterone acetate use or to other related lifestyle factors that have a bearing on fracture rate.
In the study, when cumulative exposure to medroxyprogesterone acetate was calculated, the fracture rate in users who received fewer than 8 injections was higher than that in women who received 8 or more injections. However, it is not clear that cumulative exposure, which may include periods of intermittent use separated by periods of non-use, is a useful measure of risk, as compared to exposure measures based on continuous use.
There were very few osteoporotic fractures (fracture sites known to be related to low BMD) in the study overall, and the incidence of osteoporotic fractures was not found to be higher in medroxyprogesterone acetate users compared to non-users.
Importantly, this study could not determine whether use of medroxyprogesterone acetate has an effect on fracture rate later in life.
-
15 REFERENCES
1. Li CI, Beaber EF, Tang, MCT et al. Effect of Depo-Medroxyprogesterone Acetate on Breast Cancer Risk among Women 20 to 44 years of Age. Cancer Research 2012;72:2028-2035.
2. Paul C, Skegg DCG, Spears GFS. Depot medroxyprogesterone (Depo-Provera) and risk of breast cancer. Br Med J 1989; 299:759-62.
-
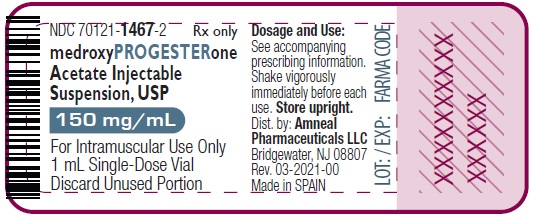
16 HOW SUPPLIED/STORAGE AND HANDLING
Medroxyprogesterone Acetate Injectable Suspension, USP is supplied in the following strengths and package configurations:
Package Configuration
Strength
NDC
Medroxyprogesterone acetate sterile aqueous suspension 150 mg/mL
1 mL single-dose vial in 1 carton
150 mg/mL
NDC: 70121-1467-2
25 x 1 mL single-dose vials in 1 carton
150 mg/mL
NDC: 70121-1467-5
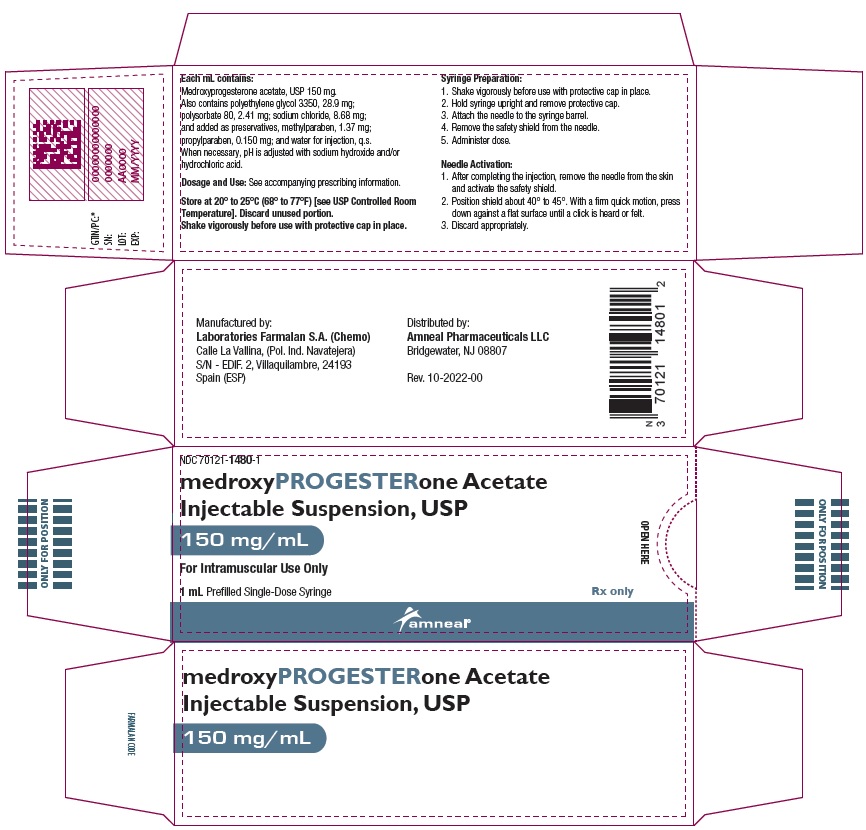
Medroxyprogesterone acetate prefilled syringes packaged with 22 gauge x 1 1/2 inch Needles
1 mL single-dose prefilled syringe
150 mg/mL
NDC: 70121-1480-1
Vials:
Vials MUST be stored upright at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. Shake vigorously immediately before use.
Prefilled Syringes:
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. Shake vigorously before use with protective cap in place.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
- Advise patients at the beginning of treatment that their menstrual cycle may be disrupted and that irregular and unpredictable bleeding or spotting results, and that this usually decreases to the point of amenorrhea as treatment with medroxyprogesterone acetate continues, without other therapy being required.
- Counsel patients about the possible increased risk of breast cancer in women who use medroxyprogesterone acetate [see Warnings and Precautions (5.3)].
- Counsel patients with a history of meningioma about the possible risk of worsening meningioma [see Warnings and Precautions (5.4)].
- Counsel patients that this product does not protect against HIV infection (AIDS) and other sexually transmitted infections.
- Counsel patients on Warnings and Precautions associated with use of medroxyprogesterone acetate.
- Counsel patients to use a back-up method or alternative method of contraception when enzyme inducers are used with medroxyprogesterone acetate.
This product’s labeling may have been updated. For the most recent prescribing information, please visit www.amneal.com.
Manufactured by:
Laboratories Farmalan S.A. (Chemo)
Calle La Vallina, (Pol. Ind. Navatejera)
S/N - EDIF. 2, Villaquilambre, 24193
Spain (ESP)Distributed by:
Amneal Pharmaceuticals LLC
Bridgewater, NJ 08807Rev. 01-2026-02
-
Patient Information
Medroxyprogesterone Acetate (med rox'' ee proe jes' ter one as' e tate)
Injectable Suspension, USP
Read this Patient Information carefully before you decide if medroxyprogesterone acetate injectable suspension is right for you. This information does not take the place of talking with your gynecologist or other healthcare professional who specializes in women’s health. If you have any questions about medroxyprogesterone acetate injectable suspension, ask your healthcare professional. You should also learn about other birth control methods to choose the one that is best for you.
What is the most important information I should know about medroxyprogesterone acetate injectable suspension?
Medroxyprogesterone acetate injectable suspension can cause serious side effects, including:
- Use of medroxyprogesterone acetate injectable suspension may cause you to lose calcium stored in your bone and decrease your bone mass. The longer you use medroxyprogesterone acetate injectable suspension, the greater your loss of calcium from your bones. Your bones may not recover completely when you stop using medroxyprogesterone acetate injectable suspension.
- If you use medroxyprogesterone acetate injectable suspension continuously for a long time (for more than 2 years), it may increase the risk of weak, porous bones (osteoporosis) that could increase the risk of broken bones, especially after menopause.
- You should not use medroxyprogesterone acetate injectable suspension for more than two years unless you cannot use other birth control methods.
- It is not known if your risk of developing osteoporosis is greater if you are a teenager or young adult when you start to use medroxyprogesterone acetate injectable suspension (see “What are the possible side effects of medroxyprogesterone acetate injectable suspension?”).
Medroxyprogesterone acetate injectable suspension is intended to prevent pregnancy. Medroxyprogesterone acetate injectable suspension does not protect against HIV infection (AIDS) and other sexually transmitted infections (STIs).
What is medroxyprogesterone acetate injectable suspension?
Medroxyprogesterone acetate injectable suspension is a progestin hormone birth control method that is given by injection (a shot) to prevent pregnancy.
How well does medroxyprogesterone acetate injectable suspension work?
Your chance of getting pregnant depends on how well you follow the directions for taking your medroxyprogesterone acetate injectable suspension. The more carefully you follow the directions (such as returning every 3 months for your next injection), the less chance you have of getting pregnant.
In clinical studies, about 1 out of 100 women got pregnant during the first year that they used medroxyprogesterone acetate injectable suspension.
The following chart shows the chance of getting pregnant for women who use different methods of birth control. Each box on the chart contains a list of birth control methods that are similar in effectiveness. The most effective methods are at the top of the chart. The box on the bottom of the chart shows the chance of getting pregnant for women who do not use birth control and are trying to get pregnant.
How should I take medroxyprogesterone acetate injectable suspension?
- Medroxyprogesterone acetate injectable suspension is given by your healthcare professional as a shot into your muscle (intramuscular injection). The shot is given in your buttock or upper arm 1 time every 3 months. At the end of the 3 months, you will need to return to your healthcare professional for your next injection in order to continue your protection against pregnancy.
-
To make sure that you are not pregnant before you take medroxyprogesterone acetate injectable suspension, the first injection should be given only:
- during the first 5 days of a normal menstrual period, or
- within the first 5 days after giving birth, if you are not breastfeeding, or
- at the 6th week after giving birth, if you are feeding your baby only breastmilk.
- Medroxyprogesterone acetate injectable suspension may be given at other times than those listed above, but you will likely need to have a pregnancy test first to show that you are not pregnant.
- During treatment with medroxyprogesterone acetate injectable suspension, you should see your healthcare professional every year for a blood pressure check and other healthcare needs.
Who should not use medroxyprogesterone acetate injectable suspension?
Do not use medroxyprogesterone acetate injectable suspension if you:
- have bleeding from your vagina that has not been explained
- have breast cancer now or in the past, or think you have breast cancer
- have had a stroke
- ever had blood clots in your arms, legs or lungs
- have problems with your liver or liver disease
- are allergic to medroxyprogesterone acetate or any of the other ingredients in medroxyprogesterone acetate injectable suspension. See the end of this leaflet for a complete list of ingredients in medroxyprogesterone acetate injectable suspension.
What should I tell my healthcare professional before taking medroxyprogesterone acetate injectable suspension?
Before taking medroxyprogesterone acetate injectable suspension, tell your healthcare professional if you have:
- risk factors for weak bones (osteoporosis) such as bone disease, use alcohol or smoke regularly, anorexia nervosa, or a strong family history of osteoporosis
- irregular or lighter than usual menstrual periods
- breast cancer now or in the past, or think you have breast cancer
- a family history of breast cancer
- an abnormal mammogram (breast X-ray), lumps in your breasts, or bleeding from your nipples
- have or have ever had a type of usually benign brain tumor called a meningioma
- kidney problems
- high blood pressure
- had a stroke
- had blood clots in your arms, legs or lungs
- migraine headaches
- asthma
- epilepsy (convulsions or seizures)
- diabetes
- depression or a history of depression
- any other medical conditions
If you are breastfeeding or plan to breastfeed, medroxyprogesterone acetate can pass into your breast milk. Talk to your healthcare professional about the best way to feed your baby if you take medroxyprogesterone acetate injectable suspension.
Tell your healthcare professional about all of the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements.
Medroxyprogesterone acetate injectable suspension and certain other medicines may affect each other, causing serious side effects. Sometimes the doses of other medicines may need to be changed while you are taking medroxyprogesterone acetate injectable suspension.
Some medicines may make medroxyprogesterone acetate injectable suspension less effective at preventing pregnancy, including those listed below.
Especially tell your healthcare professional if you take:
- medicine to help you sleep
- bosentan
- medicine for seizures
- griseofulvin
- an antibiotic
- medicine for HIV (AIDS)
- St. John’s wort
Know the medicines you take. Keep a list of your medicines with you to show your healthcare professional or pharmacist before you first start taking medroxyprogesterone acetate injectable suspension or when you get a new medicine.
Follow your healthcare professional’s instructions about using a back-up method of birth control if you are taking medicines that may make medroxyprogesterone acetate injectable suspension less effective.
What are the possible side effects of medroxyprogesterone acetate injectable suspension?
Medroxyprogesterone acetate injectable suspension can cause serious side effects, including:
- Effect on the bones: See "What is the most important information I should know about medroxyprogesterone acetate injectable suspension?".
Teenage years are the most important years to gain bone strength. The decrease in calcium in your bones is of most concern if you are a teenager or have the following problems:
- bone disease
- an eating disorder (anorexia nervosa)
- a strong family history of osteoporosis
- you take a drug that can lower the amount of calcium in your bones (drugs for epilepsy or steroid drugs)
- you drink a lot of alcohol (more than 2 drinks a day)
- you smoke
If you need a birth control method for more than 2 years, your healthcare professional may switch you to another birth control method instead of using medroxyprogesterone acetate injectable suspension. If you continue using medroxyprogesterone acetate injectable suspension, your healthcare professional may ask you to have a bone test, especially if you have other risks for weak bones.
When medroxyprogesterone acetate injectable suspension is stopped, your bones may start to regain calcium. However, in a study of teenage girls who used medroxyprogesterone acetate injectable suspension for more than 2 years, their hip bones did not completely recover by 5 years after they stopped using medroxyprogesterone acetate injectable suspension. Taking calcium and Vitamin D and exercising daily may lessen the loss of calcium from your bones.
- possible increased risk of breast cancer. Women who use medroxyprogesterone acetate injectable suspension may have a slightly increased risk of breast cancer compared to non-users.
- blood clots in your arms, legs, lungs, and eyes
- stroke
- a pregnancy outside of your uterus (ectopic pregnancy). Ectopic pregnancy is a medical emergency that often requires surgery. Ectopic pregnancy can cause internal bleeding, infertility, and even death.
- allergic reactions. Severe allergic reactions have been reported in some women using medroxyprogesterone acetate injectable suspension.
- loss of vision or other eye problems
- migraine headaches
- possible increased risk for growth of a meningioma (a usually benign brain tumor), primarily when the product is used for a long time.
- depression
- convulsions or seizures
- liver problems
Call your healthcare professional right away if you have:
- sharp chest pain, coughing up blood, or sudden shortness of breath (indicating a possible clot in the lung)
- sudden severe headache or vomiting, dizziness or fainting, problems with your eyesight or speech, weakness, or numbness in an arm or leg (indicating a possible stroke)
- severe pain or swelling in the calf (indicating a possible clot in the leg)
- sudden blindness, partial or complete (indicating a possible clot in the blood vessels of the eye)
- unusually heavy vaginal bleeding
- severe pain or tenderness in the lower abdominal area
- persistent pain, pus, or bleeding at the injection site
- yellowing of the eyes or skin
- hives
- difficulty breathing
- swelling of the face, mouth, tongue or neck
The most common side effects of medroxyprogesterone acetate injectable suspension include:
- irregular vaginal bleeding, such as lighter or heavier menstrual bleeding, or continued spotting
- weight gain. You may experience weight gain while you are using medroxyprogesterone acetate injectable suspension. About two-thirds of the women who used medroxyprogesterone acetate injectable suspension in the clinical trials reported a weight gain of about 5 pounds during the first year of use. You may continue to gain weight after the first year. Women who used medroxyprogesterone acetate injectable suspension for 2 years gained an average of 8 pounds over those 2 years.
- abdominal pain
- headache
- weakness
- tiredness
- nervousness
- dizziness
Tell your healthcare professional if you have any side effect that bothers you or does not go away.
These are not all the possible side effects of medroxyprogesterone acetate injectable suspension. For more information, ask your healthcare professional or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
What other information should I know before choosing medroxyprogesterone acetate injectable suspension?
- Pregnancy. When you take medroxyprogesterone acetate injectable suspension every 3 months, your chance of getting pregnant is very low. You could miss a period or have a light period and not be pregnant. If you miss 1 or 2 periods and think you might be pregnant, see your healthcare professional as soon as possible. You should not use medroxyprogesterone acetate injectable suspension if you are pregnant. However, medroxyprogesterone acetate injectable suspension taken by accident during pregnancy does not seem to cause birth defects.
- Nursing Mothers. Although medroxyprogesterone acetate can be passed to the nursing baby in the breast milk, no harmful effects on babies have been found. Medroxyprogesterone acetate injectable suspension does not stop the breasts from producing milk, so it can be used by nursing mothers. However, to minimize the amount of medroxyprogesterone acetate that is passed to the baby in the first weeks after birth, you should wait until your baby is 6 weeks old before you start using medroxyprogesterone acetate injectable suspension for birth control.
How will medroxyprogesterone acetate injectable suspension change my periods?
-
Change in normal menstrual cycle. The side effect reported most frequently by women who use medroxyprogesterone acetate injectable suspension for birth controls is a change in their normal menstrual cycle. During the first year of using medroxyprogesterone acetate injectable suspension, you might have one or more of the following changes:
- irregular or unpredictable bleeding or spotting
- an increase or decrease in menstrual bleeding
- no bleeding at all. In clinical studies of medroxyprogesterone acetate injectable suspension, 55% of women reported no menstrual bleeding (amenorrhea) after one year of use and 68% of women reported no menstrual bleeding after two years of use.
- Missed period. During the time you are using medroxyprogesterone acetate injectable suspension for birth controls, you may skip a period, or your periods may stop completely. If you have been receiving your shot of medroxyprogesterone acetate injectable suspension regularly every 3 months, then you are probably not pregnant. However, if you think that you may be pregnant, see your healthcare professional.
Unusually heavy or continuous bleeding is not a usual effect of medroxyprogesterone acetate injectable suspension and if this happens you should see your healthcare professional right away. With continued use of medroxyprogesterone acetate injectable suspension, bleeding usually decreases and many women stop having periods completely. When you stop using medroxyprogesterone acetate injectable suspension your menstrual period will usually, in time, return to its normal cycle.
What if I want to become pregnant?
Because medroxyprogesterone acetate injectable suspension is a long-acting birth control method, it takes some time after your last shot for its effect to wear off. Most women who try to get pregnant after using medroxyprogesterone acetate injectable suspension get pregnant within 18 months after their last shot. The length of time you use medroxyprogesterone acetate injectable suspension has no effect on how long it takes you to become pregnant after you stop using it.
General information about medroxyprogesterone acetate injectable suspension
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. This leaflet summarizes the most important information about medroxyprogesterone acetate injectable suspension. If you would like more information, talk with your healthcare professional. You can ask your healthcare professional for information about medroxyprogesterone acetate injectable suspension that is written for healthcare professionals.
What are the ingredients in medroxyprogesterone acetate injectable suspension?
Active ingredient: medroxyprogesterone acetate, USP
Inactive ingredients: polyethylene glycol 3350, polysorbate 80, sodium chloride, methylparaben, propylparaben, and water for injection. When necessary, pH is adjusted with sodium hydroxide or hydrochloric acid, or both.
This Patient Information has been approved by the U.S. Food and Drug Administration.
This product’s labeling may have been updated. For the most recent prescribing information, please visit www.amneal.com.
Manufactured by:
Laboratories Farmalan S.A. (Chemo)
Calle La Vallina, (Pol. Ind. Navatejera)
S/N - EDIF. 2, Villaquilambre, 24193
Spain (ESP)Distributed by:
Amneal Pharmaceuticals LLC
Bridgewater, NJ 08807
Rev. 01-2026-02 -
PRINCIPAL DISPLAY PANEL
NDC: 70121-1467-2
Medroxyprogesterone Acetate Injectable Suspension, USP
150 mg/mL (1 mL)
Rx only
(1 Single-Dose Vial in a Carton)
Amneal Pharmaceuticals LLC
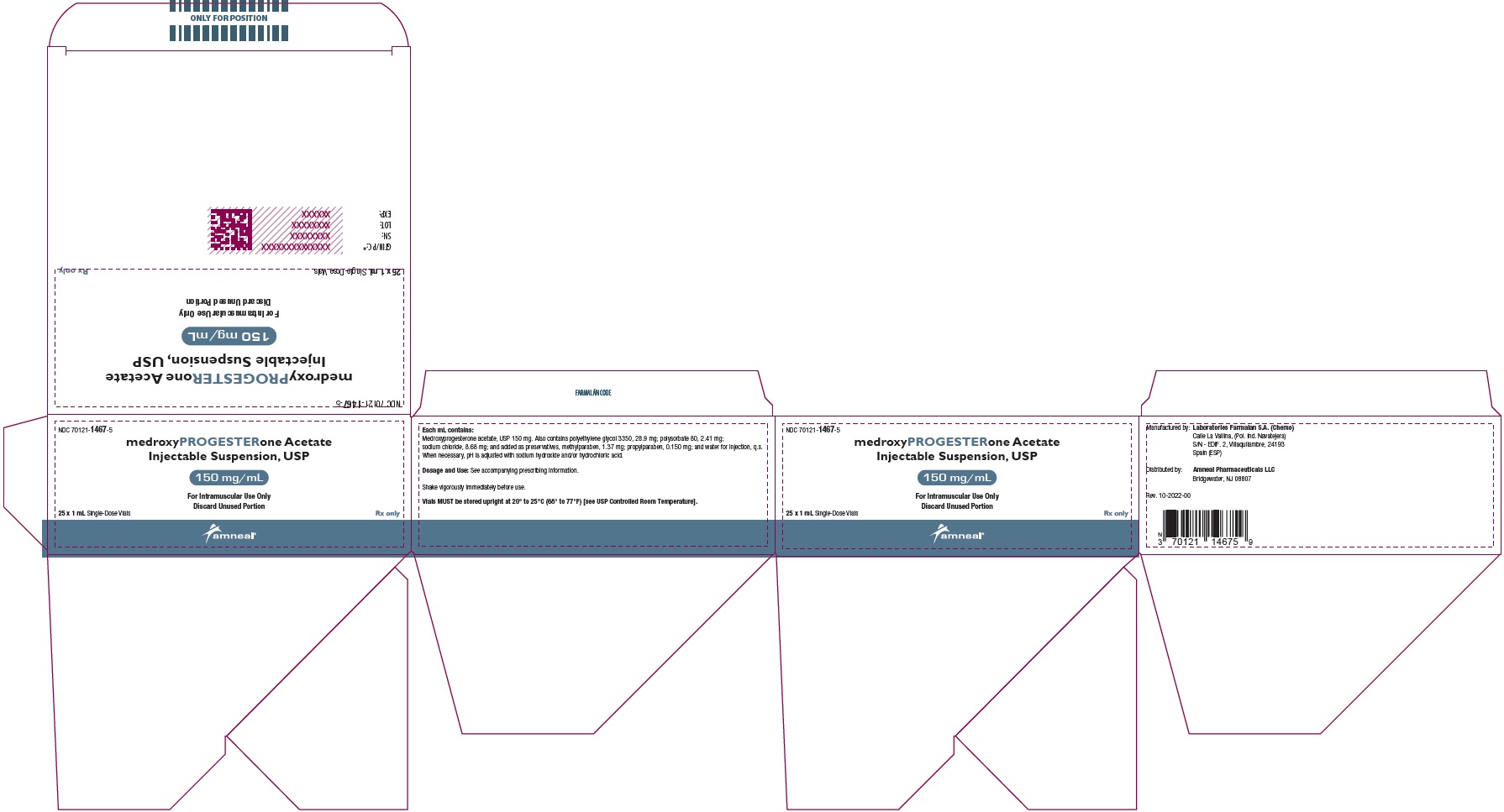
NDC: 70121-1467-5
Medroxyprogesterone Acetate Injectable Suspension, USP
150 mg/mL (1 mL)
Rx only
(25 x 1 mL Single-Dose Vials in a Carton)
Amneal Pharmaceuticals LLC
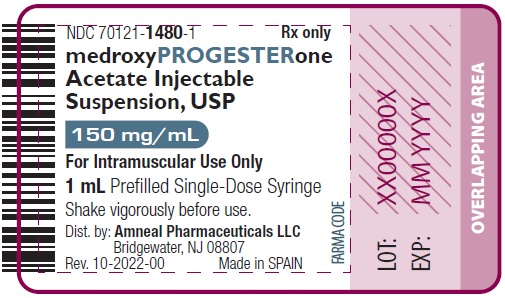
NDC: 70121-1480-1
Medroxyprogesterone Acetate Injectable Suspension, USP
150 mg/mL (1 mL)
Rx only
(1 Prefilled Single-Dose Syringe in a Carton)
Amneal Pharmaceuticals LLC
-
INGREDIENTS AND APPEARANCE
MEDROXYPROGESTERONE ACETATE
medroxyprogesterone acetate injection, suspensionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70121-1467 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MEDROXYPROGESTERONE ACETATE (UNII: C2QI4IOI2G) (MEDROXYPROGESTERONE - UNII:HSU1C9YRES) MEDROXYPROGESTERONE ACETATE 150 mg in 1 mL Inactive Ingredients Ingredient Name Strength POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) 28.9 mg in 1 mL POLYSORBATE 80 (UNII: 6OZP39ZG8H) 2.41 mg in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 8.68 mg in 1 mL METHYLPARABEN (UNII: A2I8C7HI9T) 1.37 mg in 1 mL PROPYLPARABEN (UNII: Z8IX2SC1OH) 0.150 mg in 1 mL WATER (UNII: 059QF0KO0R) SODIUM HYDROXIDE (UNII: 55X04QC32I) HYDROCHLORIC ACID (UNII: QTT17582CB) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70121-1467-2 1 in 1 CARTON 06/13/2023 1 1 mL in 1 VIAL; Type 0: Not a Combination Product 2 NDC: 70121-1467-5 25 in 1 CARTON 06/13/2023 2 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA215397 06/13/2023 MEDROXYPROGESTERONE ACETATE
medroxyprogesterone acetate injection, suspensionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70121-1480 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MEDROXYPROGESTERONE ACETATE (UNII: C2QI4IOI2G) (MEDROXYPROGESTERONE - UNII:HSU1C9YRES) MEDROXYPROGESTERONE ACETATE 150 mg in 1 mL Inactive Ingredients Ingredient Name Strength POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) 28.9 mg in 1 mL POLYSORBATE 80 (UNII: 6OZP39ZG8H) 2.41 mg in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 8.68 mg in 1 mL METHYLPARABEN (UNII: A2I8C7HI9T) 1.37 mg in 1 mL PROPYLPARABEN (UNII: Z8IX2SC1OH) 0.150 mg in 1 mL WATER (UNII: 059QF0KO0R) SODIUM HYDROXIDE (UNII: 55X04QC32I) HYDROCHLORIC ACID (UNII: QTT17582CB) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70121-1480-1 1 in 1 CARTON 06/13/2023 1 1 mL in 1 SYRINGE, GLASS; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA215397 06/13/2023 Labeler - Amneal Pharmaceuticals LLC (827748190) Registrant - Amneal Pharmaceuticals of New York, LLC (123797875) Establishment Name Address ID/FEI Business Operations Laboratorios Farmalan, S.A. 468284866 analysis(70121-1467, 70121-1480) , manufacture(70121-1467, 70121-1480) , sterilize(70121-1467, 70121-1480)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.